Updates to Requirements For All DEA-Registered Practitioners. What it Means for Your Practice.

Beginning June 27, the DEA registration will require applicants – both new and renewing – to complete a new, one-time, eight-hour training focusing on substance use disorder, with exceptions for some practitioners.
On December 29, 2022, the Consolidated Appropriations Act of 2023 enacted this training requirement for all Drug Enforcement Administration (DEA)-registered practitioners on the treatment and management of patients with opioid or other substance use disorders.
Below is information on this new requirement:
Who is responsible for satisfying this new training requirement?
- All DEA-registered practitioners, with the exception of practitioners that are solely veterinarians.
How will practitioners be asked to report satisfying this new training requirement?
- Beginning on June 27, 2023, practitioners will be required to check a box on their online DEA registration form—regardless of whether a registrant is completing their initial registration application or renewing their registration—affirming that they have completed the new training requirement.
What is the deadline for satisfying this new training requirement?
- The deadline for satisfying this new training requirement is the date of a practitioner’s next scheduled DEA registration submission—regardless of whether it is an initial registration or a renewal registration—on or after June 27, 2023.
- This one-time training requirement affirmation will not be a part of future registration renewals.
How can practitioners satisfy this new training requirement?
There are multiple ways that practitioners can satisfy this new training requirement:
- First, the following groups of practitioners are deemed to have satisfied this training:
- Group 1: All practitioners that are board certified in addiction medicine or addiction psychiatry from the American Board of Medical Specialties, the American Board of Addiction Medicine, or the American Osteopathic Association.
- Group 2: All practitioners that graduated in good standing from a medical (allopathic or osteopathic), dental, physician assistant, or advanced practice nursing school in the United States within five years of June 27, 2023, and successfully completed a comprehensive curriculum that included at least eight hours of training on:
-
- Treating and managing patients with opioid or other substance use disorders, including the appropriate clinical use of all drugs approved by the Food and Drug Administration for the treatment of a substance use disorder; or
-
- Safe pharmacological management of dental pain and screening, brief intervention, and referral for appropriate treatment of patients with or at risk of developing opioid and other substance use disorders.
- Second, practitioners can satisfy this training by engaging in a total of eight hours of training on treatment and management of patients with opioid or other substance use disorders from the groups listed below. A few key points related to this training:
-
- The training does not have to occur in one session. It can be cumulative across multiple sessions that equal eight hours of training.
-
- Past trainings on the treatment and management of patients with opioid or other substance use disorders can count towards a practitioner meeting this requirement. In other words, if you received a relevant training from one of the groups listed below—prior to the enactment of this new training obligation on December 29, 2022—that training counts towards the eight-hour requirement.
-
- Past DATA-Waived trainings count towards a DEA registrant’s 8-hour training requirement.
-
- Trainings can occur in a variety of formats, including classroom settings, seminars at professional society meetings, or virtual offerings.
What accredited groups may provide trainings that meet this new requirement?
- The American Society of Addiction Medicine (ASAM)
- The American Academy of Addiction Psychiatry (AAAP)
- American Medical Association (AMA)
- The American Osteopathic Association (AOA), or any organizations accredited by the AOA to provide continuing medical education
- The American Dental Association (ADA)
- The American Association of Oral and Maxillofacial Surgeons (AAOMS)
- The American Psychiatric Association (APA)
- The American Association of Nurse Practitioners (AANP)
- The American Academy of Physician Associates (AAPA)
- The American Nurses Credentialing Center (ANCC)
- Any other organization accredited by the Accreditation Council for Continuing Medical Education (AACCME) or the Commission for Continuing Education Provider Recognition (CCEPR), whether directly or through an organization accredited by a State medical society that is recognized by the ACCME or CCEPR
- Any other organization approved or accredited by the Assistant Secretary for Mental Health and Substance Use, the ACCME, or the CCEPR
For information regarding the DEA Diversion Control Division, click here.
If you have any additional questions on this issue, please contact the Diversion Control Division Policy Section at (571) 362-3260.
Buprenorphine Quick Start Guide
DEA Telemedicine Flexibilities for Controlled Substances Extended Through November

The Drug Enforcement Administration (DEA) announced that COVID-19 telemedicine flexibilities for controlled substances will be temporarily extended for six months – through November 11, 2023.
For any practitioner-patient telemedicine relationships that have been or will be established up to November 11, 2023, the full set of telemedicine flexibilities regarding prescription of controlled medications established during the COVID-19 PHE will be extended for one year – through November 11, 2024.
New Hope for Patients with One of the Deadliest Forms of Cancer
Scientists have reported that a new vaccine designed to treat pancreatic cancer prevented the disease from returning in 50% of patients who received it.
In a small study published by Nature, scientists said they tested the vaccine on 16 patients in New York City, and half of the patients were still remaining cancer-free after 18 months — a success for the trial.
Scientists at the German firm BioNTech developed a vaccine that can be tailored to a pancreatic cancer patient's unique genetic makeup, to train their immune system to destroy pancreatic cancer cells.
New York's Memorial Sloan Kettering Cancer Center took tumor samples from 16 patients and sent them to Germany. There, a team of scientists at BioNTech — the company that co-developed COVID-19 vaccines with Pfizer — analyzed the proteins in each sample's cancer cells.
Like the COVID vaccines, these utilized messenger RNA to instruct a patient's immune system to destroy the cancer cells. The key difference was each vaccine being tailor-made to each patient's mRNA.
Pancreatic cancer is notoriously hard to detect and treat. It is widely known as a "silent disease" because symptoms, including abdominal pain and weight loss, often don't arise until the cancer cells have spread to blood vessels and tissue, at which point treatment is difficult.
Read the full article here.
NC Responds to End of Covid-19 Health Emergency

Though the Public Health Emergency declared to respond to COVID-19 has ended, North Carolina will continue to distribute the federally funded COVID-19 vaccines and tests for free to individuals who are uninsured while supplies last.
When supplies of federally purchased vaccines run out, they will be available like flu shots and other routine vaccinations, covered by Medicare, Medicaid, private insurance or out-of-pocket costs for the uninsured. Visit MySpot.nc.gov to learn more or NCDHHS.gov/LHD to contact your local health department.
Community-based organizations can order free tests through June 26, 2023, to distribute in their regions. Visit MySpot.nc.gov/tests for more information.
Federal Test to Treat locations will continue to provide treatment at no cost to those who are uninsured or underinsured, although a fee may be charged for evaluation.
Read the NCDHHS full press release here.
NCMS Member Daniel Fox Receives Old North State Award from Governor Roy Cooper

RALEIGH (WakeMed, May 4, 2023)- Daniel Fox, MD, WakeMed’s executive medical director of Inpatient Hospital & Critical Care Medicine and NCMS member, was recently presented with the Old North State Award from Governor Roy Cooper. Fox was recognized for his excellence in patient care, service, and leadership of the WakeMed Pulmonary & Critical Care team throughout the COVID-19 pandemic. Nominated by his colleagues, he received letters and signatures of support from more than 150 members of the WakeMed community.
The Old North State Award is presented by the governor to recognize “dedication and service beyond expectation and excellence to the Great State of North Carolina.” Recipients must have 20 or more years of service in the state to be considered for this honor.
A pulmonary and critical care medicine physician, Fox treats patients in WakeMed’s intensive care units and provides outpatient pulmonary care services. Throughout the pandemic, Fox worked countless ICU shifts alongside his colleagues while rapidly implementing new COVID therapies and strategies that helped save lives. He ensures every patient receives the most up-to-date, evidence-based care.
His clinical focus includes caring for patients with complex lung diseases including autoimmune disease, asthma, and interstitial lung disease, with a special interest in patients with pulmonary hypertension and pulmonary embolism.
Fox earned his medical degree from the University of North Carolina at Chapel Hill School of Medicine. He completed a residency program in internal medicine at Duke University Medical Center followed by fellowship programs in pulmonary and critical care medicine and pulmonary vascular disease at the University of Colorado Health Sciences Center. He is board certified in internal medicine, pulmonary medicine, and critical care medicine. [source]
TBT: Celebrating 20 years of Leadership in Medicine! Here is David E. Melon's MEDTalk from 2019
This year the North Carolina Medical Society is celebrating 20 years of Leadership in Medicine!
Here is a Throwback Thursday to Dr. David E. Melon's MEDTalk from 2019. Look for a new TBT every Thursday until the 2023 LEAD Conference, October 13-14.
https://youtu.be/-RT_tgghDZk
The 2023 LEAD conference registration is NOW OPEN. Click here for more information.
Please contact Erica Hall at NCMS to organize a class table of your own.
In Memoriam: Former NCMS Team Member Lucia Peel.

The North Carolina Medical Society family is saddened to learn of the passing of a former team member, Lucia Peel. Lucia died Monday, May 8, 2023 at ECU Cancer Center in Greenville, N.C. She was 65.
Lucia served on the Society’s government affairs team from 1994 to 1998 and was integral to advancing NCMS legislative advocacy priorities. She was instrumental in the Medical Society’s engagement in key health policy issues, including Tort Reform, Antitrust Exemptions for Physicians, Patient Safety Regulation, and Managed Care Regulation.
We send heartfelt condolences to the family.
Biggs Funeral Home in Williamston is assisting the family and arrangements are pending.
May is Skin Cancer Awareness Month

The NC Dermatology Association, in partnership with the American Academy of Dermatology, remind us that May is Skin Cancer Awareness Month and an occasion to raise awareness of the most common cancer. It’s estimated that every day about 9,500 people in the United States are diagnosed with skin cancer.
NC Medical Society members are reminded that the entire care community can help educate their patients that . . .
- Many skin cancers could be prevented if people would protect their skin from the sun and stop using tanning beds.
- People of all colors and ages get skin cancer.
- When found early, skin cancer is highly treatable.
- Because skin cancer begins on the skin, you can find it early by performing skin self-exams.
- If you find a spot on your skin that’s growing, bleeding, or changing in any way, see the skin cancer expert, a board-certified dermatologist. This appointment could save your life.
Resources are available from the AAD on a variety of related subjects:
Spread the word – Prevent Skin Cancer!
In 2022, NCMS ran a series of skin care tips from our members called Melanoma Monday. Here are those posts:
Melanoma Monday: Are your ready for summer?
Melanoma Monday: Survive the 4th with Beautiful Skin!
Melanoma Monday: Healthy Life, Healthy Skin
Melanoma Monday: Have Fun at the Lake and Keep Your Skin Safe
Melanoma Monday: Be Safe While You Enjoy A Day at the Beach!
Melanoma Monday: Fun on the Boat Skin Safety
Melanoma Monday: Fun at the Pool!
Melanoma Monday: Summer Skin Care for People Over 55
Melanoma Monday: Keeping Your Skin Clean in Summer!
Melanoma Monday: Fun in the Mountains!
New Study Offers Solution for Reducing Postpartum Hemorrhage

According to a landmark study published by researchers from the World Health Organization (WHO) and the University of Birmingham, a new solution, known as E-MOTIVE, could provide a major breakthrough in reducing deaths from childbirth-related bleeding.
The study, which involved over 200 000 women in four countries, found that objectively measuring blood loss using a simple, low-cost collection device called a ‘drape’ and bundling together WHO-recommended treatments - rather than offering them sequentially - resulted in dramatic improvements in outcomes for women. Severe bleeding – when a woman loses more than a liter of blood after birth - was reduced by 60%, and they were less likely to lose their life.
The recommended E-MOTIVE package includes early and accurate detection of postpartum hemorrhage (PPH) using a blood-collection drape. This is complemented by an immediate treatment bundle where indicated, including uterine massage, medicines to contract the womb and stop the bleeding, intravenous fluid administration, an examination and, when needed, escalation to advanced care.
The Center for Disease Control and Prevention (CDC) characterizes PPH as a severe bleeding by the mother after delivery, labels it a significant public health problem, and the leading cause of death among women during childbirth. Women with von Willebrand disease (VWD)--a hereditary bleeding disorder, caused by a deficiency in the levels and/or function of von Willebrand factor (VWF)--are more likely to experience PPH and are 10 times more likely to die from childbirth complications than women without VWD [source].
Read the full article here.
Catawba Valley Medical Center Awarded America's Best Hospitals for Stroke Care

Catawba Valley Medical Center (CVMC) has been named one of America’s Best Hospitals for Stroke Care by the Women’s Choice Award®, America’s trusted referral source for the best in healthcare. The award signifies that CVMC is in the top seven percent of 4,729 U.S. hospitals offering stroke care services.
Hospitals that meet the stroke center certification requirement, must then meet or exceed the following performance measures from the Centers for Medicare and Medicaid Services (CMS): Hospitals must also score in the top 80% of all hospitals in the percent of patients receiving Head CT scan results within 45 minutes, and cannot have received a rating of Worse than the National Rate for the Deaths from Serious Treatable Complications measure.
CVMC is one of 360 award recipients representing the hospitals that have met the highest standards for stroke care in the U.S. by the Women’s Choice Award.
To learn more about CVMC's award-winning Stroke care, visit CatawbaValleyHealth.org/Stroke.
Congratulations, Catawba Valley Medical Center, for helping to make North Carolina healthier!
Newborn Genomic Screening: Helpful or Harmful?

Experts are divided about how helpful DNA sequencing data really are. The tests often identify mutations that raise someone’s risk of developing a condition, but don’t necessarily cause the disease. Uncertain results may confuse doctors and scare families — causing them to seek doctors’ visits and treatments that most ultimately won’t require, adding to unnecessary health care costs. There are also concerns about false positives and false negatives with sequencing. But a new study has found that among rare disease physicians — the ones to whom worried parents will turn — there is emerging consensus that these sorts of tests should be used on a broader scale.
When 238 rare-disease doctors across the U.S. were surveyed by a research team at Mass General Brigham in Boston, 88% of them agreed that DNA sequencing to screen for certain treatable childhood disorders should be made available to all newborns. The study was published Monday in JAMA Network Open.
Continue to the full article here.
Be sure to share your thoughts in the comments.
CCHN Seeks Provider Advisory Committee Participation

Carolina Complete Health Network is currently seeking provider participation for its Provider Advisory Committee.
The purpose of the CCHN Provider Advisory Committee is to provide input on Carolina Complete Health (CCH) provider incentive programs, administrative practices, and supports development of provider scorecard indicators, useful analyses of the data, and effective means of helping providers improve their performance.
For this committee, the participating providers must be physicians, physician assistants, or nurse practitioners that are particularly interested in these areas. This committee meets once per quarter for one hour.
CCHN is a subsidiary of the North Carolina Medical Society and co-founders of a first-of-its-kind partnership with Centene Corporation, the North Carolina Community Health Center Association and other providers across North Carolina. CCHN offers North Carolina practitioners a platform to improve clinical and administrative processes, as well as a unique voice in governance over medical policy. They combine the best of leading-edge national expertise with deep-rooted local knowledge of what works here in North Carolina.
Carolina Complete Health Network’s mission is to empower physicians and clinicians to provide state-of-the-art care to Medicaid beneficiaries resulting in BETTER HEALTH and GREATER HEALTH EQUITY at LOWER COST.
If interested in this opportunity, please contact Katie McKay at [email protected].
CMS Proposes New Rule on Publishing of Post Payment Rates - Will it Affect Your Practice?

The Center for Medicare and Medicaid Services (CMS) has issued a proposed regulation that, if finalized, would require state Medicaid/CHIP programs to post payment rates for all services on their webpage.
While the proposal does not explicitly mention Federally Qualified Health Centers (FQHCs), it appears to require the publication of FQHC-specific PPS rates. States would also be required to compare their payments to Medicare rates for the same services, and to establish maximum wait times for managed care patients to receive certain types of appointments.
See page 399 of the NPRM.
First LEAD Sponsor Secured!
SouthState Bank is the first to confirm sponsorship at the 2023 LEAD Conference!
SouthState will have an exhibit booth, so make plans to attend LEAD on October 13 & 14 and visit SouthState's booth representatives. Thank you SouthState Bank!
Find out how your company can be involved or sponsor the LEAD Conference here.
Devastating News for the First Pediatric Practice in Morehead City, NCMS Members Affected.

On April 28, police were dispatched to a burglar alarm at the Carteret County Clinic for Adolescents and Children on John Platt Drive, but when they arrived, they saw flames.
Of the rebuilding, Dr. Margaret Merrick, a provider at the practice, says: "Of course, it is going to be a long process, but the community has been very supportive, and we have a great team with a very positive outlook."
72 hours after the fire, that resulted in a total loss, the clinic was able to re-open, in part thanks to the generosity of Carolina Center for Surgery and Carteret OBGYN.
The Carteret County Clinic for Adolescents and Children will see patients at its new location at 221-B Professional Circle, Morehead City.
On its Facebook page, the clinic gives shout outs to many who helped including: Oceanside Pediatrics and Kids Rule Pediatrics and Carteret Healthcare and Oceanside Pediatrics. They also give thanks to Morehead City Fire Department, Morehead City Police Department, Atlantic Beach Fire Department, and Beaufort Fire Department.
No injuries or loss of life (including the fish) were sustained in the fire. The cause is under investigation.
Practitioners at Carteret County Clinic:
Katharine Moorehead, MD (NCMS member)
Margaret Merrick, MD, FAAP
Loreli Rowe, MD (NCMS member)
Keep Your Patients Cool this Summer with Help from Operation Fan Heat Relief!

As temperatures begin rising, the North Carolina Department of Health and Human Services’ Division of Aging and Adult Services is partnering with the NC Area Agencies on Aging and local service providers to distribute fans to eligible recipients through Operation Fan Heat Relief (OFHR).
Beginning May 1, your patients aged 60 and older, as well as adults with disabilities, are eligible to sign up for OFHR assistance at local aging agencies across the state.
Click here to access a list of the 2023 OFHR Local Providers
The OFHR program runs from May 1 to October 31. More information about Operation Fan Heat Relief is available here. Individuals may also contact their area agency on aging or the Division of Aging and Adult Services at 919-855-3400.
Join WCMS for some Crafty Mother's Day Fun!

Join the Wake County Medical Society (WCMS) for a Mother’s Day craft, suitable for any children up to the early teen years.
Local artist and teacher Suzanne Brown will lead children through a charming ceramic project suitable for Mother’s Day (hint, hint….).
Bring your children or grandchildren for a fun, family activity, and then enjoy the sights of downtown Raleigh with free parking at the North Carolina Medical Society (NCMS).
The NCMS is within five blocks of Marbles Kids Museum, the NC Museum of Natural Science, NC Museum of History, and much more!
Pre-registration is appreciated the cost is $10 and payable onsite.
For more information, call 919-621-5919 or email [email protected].


NCDHHS to Hold Next Mental Health Town Hall in Wake County

The next NCDHHS Mental Health Town Hall has been scheduled. The event will be held in Wake County and will be a community discussion on improving minority mental health across North Carolina.
May 11, 2023 • 6:00 - 8:00 p.m.
Wake Tech Community College
1636 Graduation Way, Raleigh, NC 27603
Building L, Student Services Building, 2nd Floor Conference Center
Get more information about the event and register here.
Visit the NCDHHS website to watch recordings of previous town halls. County representatives interested in hosting a Mental Health Town Hall can contact Annelyse Iglesias via email at [email protected].
NCMS Legislative Review - May 5, 2023

Health took center stage last week as many health-related bills passed each chamber. Legislators in Raleigh faced the crossover deadline, which is a date set by which a bill must pass at least one chamber to continue in the legislative process. The deadline was Thursday, May 4th, and took effect for all bills that do not contain appropriations or fees.
The main bill on the forefront of the health space is SB 20, Care for Women, Children, and Families Act. Among other provisions, it would make it unlawful after the 12th week of gestation to have an abortion in North Carolina with other gestational exceptions for fetal anomalies, rape/incest, and medical emergencies. SB 20 did pass both the House and Senate, now heading to the desk of Governor Roy Cooper, who will likely veto it. NCMS issued a statement opposing the bill and NCMS staff are still working to fully understand how the bill will impact access to reproductive healthcare and create new administrative burdens for members.
With the crossover deadline looming, many NCMS supported bills have passed the House. Below is a summary of some:
HB 576: Healthcare Practitioner Transparency Act – also known as “truth in advertising” – This legislation would require a healthcare practitioner to properly identify their license, certification, or registration (MD, DO, etc.) and would not allow the display of any misleading information.
HB 809: Hospital Violence Prevention Act – This legislation seeks to minimize the likelihood of violence by ensuring health care facilities develop safety protocols to address risks identified by hospital employees, security personnel, and local law enforcement.
HB 560: Diagnostic Imaging Parity – Would provide health coverage parity for breast cancer diagnostic imaging and would require coverage for certain other types of imaging.
HB 739: Update Requirements/Advance Healthcare Directives – This patient-focused legislation facilitates access to health care powers of attorney and advance health care directives by modernizing and enhancing the advance care planning process.
Lastly, the NCMS worked tirelessly to remove language repealing protections for minor consent from HB 808. The law currently provides that minors can give consent for medical services in the diagnosis and treatment of pregnancy, abuse of controlled substances, emotional disturbance, and venereal disease. The NCMS remains opposed to the bill due to its interference with the patient-clinician relationship, but we are pleased that the minor consent protections have been preserved.
WHO: Covid-19 No Longer a Global Health Emergency

The World Health Organization (WHO) has declared COVID-19 no longer a global health emergency. The decision was made on the advice of the Covid-19 emergency committee, a panel of independent experts.
“It’s with great hope that I declare COVID-19 over as a global health emergency,” WHO Director-General Tedros Adhanom Ghebreyesus said.
The U.N. health agency’s officials said that even though the emergency phase was over, the pandemic hasn’t ended, noting recent spikes in cases in Southeast Asia and the Middle East. WHO says thousands of people are still dying from the virus every week, and millions of others are suffering from debilitating, long-term effects.
In the U.S., the public health emergency declaration made regarding COVID-19 is set to expire on May 11, when wide-ranging measures to support the pandemic response, including vaccine mandates, will end.
Read more about the decision here.
COVID-19 Reporting Requirements Expire With End of PHE This Month

The Division of Public Health of the NC Department of Health and Human Services has issued notice that, as of May 12, 2023, physicians will no longer be required to report cases of COVID-19 or deaths due to the coronavirus. The May 4, 2023 notice also announced that labs will no longer have to report COVID-19 test results as of the end of the expiration of the declared Public Health Emergency on May 11.
The DHHS/DPH memo can be accessed at here for further details.
Could Mental Health First-Aid Training Help You Better Engage Your Patients?

Mental Health First Aid is a skills-based training course that teaches participants to identify, understand and respond to mental health and substance use challenges.
This basic course on mental health and substance abuse conditions will give you the skills to notice and engage individuals experiencing these symptoms which cause suffering. Through engagement, you can offer understanding and invite them to expand their care team with resources that can help. You will receive a certificate of completion at the end of this course. This course is foundational and part of the training curriculum for NCServes Providers & Staff, Peer Supports, and Community Stakeholders.
Upcoming Trainings:
• Virtual: May 17, 2023
• Virtual: June 5, 2023
• In-Person Raleigh, NC: June 15, 2023
• Virtual: June 27, 2023
• Virtual: July 11, 2023
Learn more and register here.
*Trainings are limited to 30 participants. Register early to secure your spot!
Foundation Friday! Thank You to These NCMS Foundation Donors.

Today, the NCMS Foundation recognizes donors who have joined us on the journey to help make health and well-being attainable for all North Carolinians. These individuals are contributing to make sure clinicians are where they are needed most and that clinician leaders are lighting the way.
Thank you for your continued support to help North Carolinians lead healthier lives.
Learn more about how YOU can make a difference too here.
Richard T. Weisenburger, DO
Joshua I. Vogel, MD
Danilo Bernardo, MD, FACP
Christian G. Anderson, MD
Johnathan D. Williams, MD
Eugene H. Paschold, MD
Karen H. Harum, MD, FAAP
Karen E. Wood, MD
Shannon B. Dowler, MD
First-Ever RSV Vaccine Approved by FDA For Older Adults

The Food and Drug Administration has approved the first-ever vaccine to combat severe respiratory syncytial virus, or RSV, in older adults, giving your patients 60 and older another level of protection.
According to trial data, Arexvy, developed by GlaxoSmithKline, was 82% effective at preventing lower respiratory tract illness caused by RSV and 94% effective in those who had at least one underlying medical condition.
RSV infects nearly everyone by age 2 and is the leading cause of hospitalizations among newborns and younger children; it also strikes late in life, causing more than 177,000 hospitalizations and 14,000 deaths among older adults each year.
Read the full article here.
Statewide Consortium with Key Stakeholders in Healthcare to Move the Needle on Stress and Burnout.
Reignited in September 2022, the North Carolina Clinician and Physician Retention and Well-being (NCCPRW) Consortium is focused on making North Carolina one of the healthiest states to practice medicine. Made up of key stakeholders from organizations across the state, NCCPRW is exploring and identifying drivers of clinician and physician stress and burnout to address wellbeing at the organizational and societal level. You can visit here to find well-being resources.
NCMS PAC Thankful Thursday!
On this Thankful Thursday, we are recognizing some of our NCMS PAC Investors! Thank you for your continued support and investment to your patients and profession. Contact Hannah Rice ([email protected]) to learn more about how you can make a difference.
Alexander Chiaramonti, MD
Donna L. Shelton, PA-C
Greg Griggs, MPA
Lyndon K. Jordan, III, MD, FACR
Matilda W. Nicholas, MD, PhD
Mohammed A. Hannan, MD
Vanessa L. Everett, MD
Wake County Medical Society Plans Membership Activities

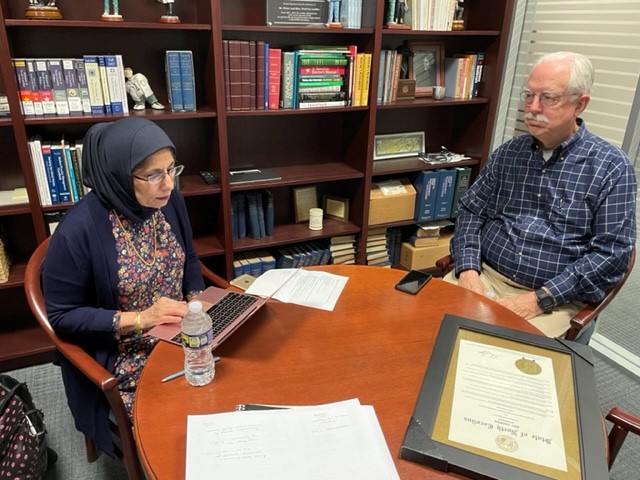
Wake County Medical Society (WCMS) Alliance President Zohra Osman (l) plans for membership activities with the WCMS President Ted Kunstling, MD. Both the WCMS and the Alliance work tirelessly to support medical care in the community and the clinicians who provide it.
Happy Birthday to These Members Celebrating This Month!

Grab your party hats and noise makers and let’s celebrate!
Ole S. Aassar, MD
William B. Abernethy, Jr., MD
Surafeal G. Abraha, MD
Peter K. Acheampong, MD
Maureen N. Achuko, MD
Douglas H. Adams, MD, MPH
Van L. Adams, MD
Henry T. Adkins, Jr., MD
Kerry E. Agnello, DO
Julian S. Albergotti, Jr., MD
Dustin B. Alderson, MD
Fuad Y. Aleskerov, MD
Chelley K. Alexander, MD
Erin B. Allen, PA-C
Diane E. Alligood, MD
Sridevi Allu, MD
Ghiath M. Almasri, MD
Terrence P. Almengual, MD
David A. Altman, MD
Harry T. Ameredes, MD
Ginette A. Archinal, MD
Brooktiete Asseres, MD
Emily L. Averbook, MD
Ramesh Avva, MD
P. William Aycock, Jr., MD
Richard E. Babb, PA-C
Gopal H. Badlani, MD
Hasan A. Baloch, MD
John A. Bardini, MD
Victor R. Barnes, MD
James D. Barnwell, MD
Katherine E. Barrett, MD
Robert P. Barringer, MD
Scott J. Bartkoski, MD
Dwight D. Bates, MD
Mckenzie A. Bauman, PA-C
John N. Beard, MD
George H. Beckwith, MD
Matthew T. Bennett, MD
Brendan C. Berry, MD
Jessica E. Berry, PA-C
David S. Bertrand, PA-C
Michelle M. Bertsch, MD
Gideon Besson, MD
Bhavna Bhat, MD
Pouru P. Bhiwandiwalla, MD
William A. Biggers, Jr., MD
Andrew T. Billingsley, MD
Mott P. Blair, IV, MD
Robert A. Blake, MD
Jonathan W. Blank, MD
Kelly T. Blount, PA-C
Elizabeth R. Blyth, MD
Ann L. Bogard, MD
Michael A. Bohl, II, MD
Andrew J. Bojanowski, PA-C
Debra A. Bolick, MD
E. Arthur Bolz, MD
W. Kent Bonney, MD, FAAP
David W. Boone, MD
Bryon J. Boulton, MD
Benjamin C. Bowen, MD
Kellie M. Bowen, PA
James R. Bowers, MD
Umar Bowers, MD
Brian P. Bowman, MD, PhD
Douglas R. Boyette, MD, FACC
Thomas A. Brackbill, MD
J. Lawrence Brady, Jr., MD
Jonathan L. Brandon, MD
Amy E. Brantley, PA-C
David S. Brantley, MD
Charles C. Bremer, MD
Mathijs H. Brentjens, MD
Sarah L. Brewington, MD, FAAP
Dewey H. Bridger, III, MD
James W. Britt, MD, FAAP
Robert C. Brock, MD
Seth C. Brody, MD
Per G. Brolinson, DO
Rebecca M. Brooks, MD
Robert A. Buchanan, Jr., MD
Robert T. Buchanan, MD
Barry D. Bunn, MD
James O. Burke, Jr., MD
Pamela A. M. Burleson, PA-C
Scott J. Burner, MD
Henry W. Burnett, MD
John W. Burnett, Jr., MD
M. Alan Burns, MD
Philip D. Burton, MD
Robert H. Butler, MD
Christopher S. Byrd, MD
Chasitty C. Calhoun, PA-C
Gregory J. Cannon, MD, FACEP
Jeffrey P. Carley, DO
Mark V. Cavaliere, PA-C
T. Brent Chafin, MD
Eric D. Challgren, MD
Peter G. Chan, MD
Pat R. Chappell, MD
Julie S. W. Childers, MD
Monique V. Chireau, MD
Natalie Chrismer, PA-C
Ann Y. Chung, MD
Ian T. Churnin, MD
Justin E. Cimring, MD, FAAP
Kenneth J. Clark, Jr., MD
Lee A. Clark, Jr., MD
Talaya B. Clark, MD
Noellee T. Clarke, MD
John R. Collier, Jr., MD
Michelle S. Collins, MD
David M. Colonna, MD
Christopher D. Connolley, MD
Christopher C. Copenhaver, MD
Christopher D. Corso, MD
Daniel E. Couture, MD
Michael R. Cram, MD
Steven T. Crawford, MD
Trey B. Creech, MD
William D. Crocker, MD
Peter P. Cullen, MD
Lawrence M. Cutchin, MD
Charles L. Czermak, Jr., MD
Seema N. Daigle, MD
Vincent Q. Dam, MD
Danielle M. D'Angelo, PA-C
Nicholas J. D'Avanzo, MD
Melissa S. Davies, DO
Drew E. Davis, MD
W. Hodges Davis, MD
Philip C. Deaton, MD
Robert Deepe, MD
Timothy B. Deering, MD
Martin C. DeGraw, MD
Maria V. Delbono, DO
David T. Dellaero, MD
Donna P. Denier, MD
Priyank K. Desai, MD
Sunil J. DeSai, MD, FACC
Gary J. DeSalvo, MD, DMD
Gautam Dev, MD
Sanjeev K. Deveshwar, MD
Abigail G. DeVries, MD
Tejpal S. Dhillon, MD
Janice F. Dickerson, MD
F. Keels Dickson, MD
Milan M. DiGiulio, MD
Jennifer M. Dimovski, MD
Christopher A. Dixon, DO
Michael L. Dockery, MD
Robert P. Doolittle, MD
Benedict R. Dorsam, PA-C
Nirali M. Dubal, MD, MPH, FAAP
Eric D. Duberman, MD
David A. Dubow, MD
Andrew C. Dukowicz, MD
Jennifer A. Durand-Smith, MD
Edward B. Eadie, Jr., MD
John K. Earl, MD
Randy C. Efird, MD
Dave S. Eichman, MD
Maxlyn L. Ellison, MD
Kelly A. Erola, MD
Vicky Erwin, DO
George K. Escaravage, Jr., MD
James M. Essenberg, MD
E. Harvey Estes, Jr., MD
Bradley H. Evans, MD
D. Evan Evans, MD
Joanna L. P. Evans, MD
William J. Faircloth, MD
Nicholas Farina, MD
Johnny L. Farrow, MD
Sarah L. Fernandez, PA
James V. Ferris, MD
Karen E. Fieselman Stroud, MD, FAAP
Mario G. Fiorilli, MD, MPH, FACPM, FACP
Michael J. Fisher, MD
Otis N. Fisher, MD
James P. Flanagan, MD
Anna M. Fleischman, MD
D. Francis Fleming, Jr., MD, FAAN
Robert A. Flores, MD
Theresa M. Flynn, MD
Toinette H. Fontrier, MD
William W. Fore, MD
Garett R. Franklin, MD
Jonathan P. Fritz, MD
Michael M. Fujimagari, MD
Mary Susan K. Fulghum, MD
Melany Furimsky, DO
Jeffrey G. Gaca, MD
Vikram Gahlot, MD
Robert T. Gallaher, MD, FACP
Dionne P. Galloway, MD
Kenneth R. Gallup, Jr., MD
Jacques P. Ganem, MD
Christopher A. Gardner, MD
Donald N. Gardner, MD
John B. Garrett, Jr., MD
Carolyn M. Garrett Piggott, MD
Sheli R. Garrett-Albaugh, DO
Robert W. Garrison, MD
W. Blake Garside, MD
Michael S. Gart, MD
Leonardo Gendzel, MD
Steven M. Genkins, MD
Michael B. Gentry, MD
Boyan A. Georgiev, MD
P. Pressly Gilbert, MD
Russell V. Gilchrist, DO
C. Lee Gilliatt, Jr., MD
Ronald A. Gioffre, MD
Nathan C. Givens, MD
Brian M. Go, MD
Rolf P. Gobien, MD
Ismael R. Goco, MD
Ronald L. Godbold, MD
Manlio A. Goetzl, MD
David A. Goff, MD
John P. Goldfield, MHS, PA-C
Elizabeth L. Golding, DO
Thomas E. Goodin, III, MD
James O. Goodwin, MD
Maje D. Goodwin, MD
G. Michael Gould, DO
Hannah E. Grabow, PA
Mark L. Graham, II, MD
Arthur G. Green, III, MD
Lawrence H. Greenblatt, MD, FACP
Jerry H. Greenhoot, MD
Ashton T. Griffin, III, MD
Christopher P. Griffin, MD
Elaine C. Griffin, MD
Robert L. Groat, MD
Jeremy G. Gue, MD
Melinda S. Guglielmetti, PA-C
Manu A. Gupta, MD
Paul P. Gwyn, Jr., MD
Robert D. Hagan, Jr., DO
Paul D. Hain, MD
Chad R. Haldeman-Englert, MD
Colin D. Hall, MD
Harold L. Hall, III, MD
John C. Hamrick, Jr., MD
Padma B. Hari, MD, FACC, FASE
David B. Harker, MD
Steven D. Harlan, MD
John S. Harman, MD
Mark D. Harris, MD
Zachary P. Harris, MD
Oliver J. Hart, Jr., MD
D. Daniel Hassell, III, MD
Amber G. Hatch, MD
Samuel P. Hawes, III, MD
Gordon L. Hazen, PA
Timothy R. Heacock, MD
Benjamin L. Hechler, MD
John H. Heinzerling, II, MD
Masoud S. Hejazi, MD
Nicole L. Helmke, MD
Sydney E. Hendry, MD
Thomas Herfurth, MD
Kevin O. Herman, MD
Ruthann A. Heron-Davis, MD
Benjamin W. Herrick, MD
Richard S. Herring, MD
Robert A. Highland, MD
Dennis L. Hill, MD
Patricia K. Hill, MD
Jeremy T. Hines, MD
John C. Hisley, MD
Beverly M. Hockenberger, PA-C
Matthew L. Hoimes, MD
Edward M. Hollander, MD
Robert O. Holmes, Jr., DO
John B. Holt, MD
Tamara S. Housman, MD
Thaddeus D. Houston, MD
Hampton A. Howell, MD
Catherine M. Hren, MD
F. Alan Hubbard, MD
Anthony G. Hucks-Folliss, MD
Janice Huff, MD
Sarah P. Hughes, MD
Matthew W. Hunt, MD
Charles D. Hunter, PA-C
C. Blake Hutchinson, MD
Kimberly F. Ingersoll, MD
Karen M. Isaacs, MD, MPH
Bradley D. Isbister, MD
Rodger D. Israel, MD, MPH
Jonathan D. Jaffe, DO
Amanda H. Janda, PA-C
Thomas E. Jarrett, MD
Casey D. Jenkins, MD
Larry P. Jenkins, MD
Megan E. Jenkins, PA-C
Robert L. Jobe, MD
John A. Johnson, DMD, MD
Lorin E. Johnson, MD
P. Byron Johnson, MD
Gregory L. Jones, MD
Robyn R. Jordan, MD, PhD
Ranjit Joseph, MD
Gurdev S. Judge, MD
Richard D. Kane, MD
Elizabeth P. Kanof, MD
James C. Karegeannes, MD
May M. Kassem, MD
Raghu R. Katuru, MD
Samuel L. Katz, MD
Amantia Kennedy, MD
Scott R. Kennedy, MD
Danielle D. R. Keyton, DO
Neelam S. Khan, MD
Stephen D. Kicklighter, MD
Stanley G. Kinkaid, MD
Alan N. Kirollos, MD
Mark Kirsch, MD
Philip J. Kittner, MD
Valerie D. Knight, PA-C
Harvey D. Kohn, MD, FACOG
Alonzo D. Kornegay, MD
Janelle L. Krasovich, MD
Arthur F. Kriner, MD
Kourtney L. Krohn, DO
Lauree S. Kruyer, PA-C
Alyson R. Kuroski-Mazzei, DO
Cherie M. Kuzmiak, DO
Mark S. LaFave, MD
Melissa J. Lamrissi, MD
Steven E. Landau, MD
Patrick E. Lantz, MD
Clark A. LaPrelle, II, PA-C
E. Joseph LeBauer, MD
James D. LeClair, MD
Esther J. Lee, MD
Jay U. Lee, MD
Robert H. Lee, MD
David P. Lensch, MD
Dante N. Lewis, MD
Jody P. Lewis, MD
Lori B. Lilley, MD
Clinton R. Lincoln, MD
William C. Lippert, MD
Andrew L. Lizek, MD
L. Phillip Lloyd, PA-C
Ginger N. Locklear, MD
William S. Logan, MD
Christine T. Lomboy, MD
Christopher M. Long, MD
Christopher E. Lord, MD
Jason B. Lowe, MD
Christie H. Lowery, PA-C
Michael H. Lowry, MD
Scott N. Lurie, MD
Matthew D. Lyons, MD
Frederick H. Mabry, III, MD
Andrea J. Machnitz, MD
Homa Magsi, MD
Danielle L. Mahaffey, MD, MMM
Mohammed A. Mah'Moud, MD
Jimmy J. C. Mali, MD
Craig A. Mangum, MD
Jennie C. Mangun, MD
Christopher H. Mann, MD
Matthew A. Manning, MD
Sami W. Mardam-Bey, MD
Jordan A. Margo, MD
Marie-Claire Marroum-Kardous, MD
Maria N. Marshall, PA-C
Melanie K. Marshall, MD, DDS
Robert N. Marshall, III, MD
Kristie C. Martin, PA-C, MMS
Willis E. Martin, MD
Damien M. Marycz, MD
James E. Masters, MD
Marjorie E. Matthews, MD
Robert C. Matthews, MD
Michael A. McCall, MD
William McCall, Jr., MD
E. Lee McConnell, III, MD
Leslie A. McCutcheon, PA-C
Noel B. McDevitt, MD
James P. McDonald, MD
Wyman T. McGuirt, MD
Peter F. McIlveen, MD
James D. McLeod, MD
William J. Meggs, MD, PhD
Mark W. Memolo, MD
Michael K. Merz, MD
Robert S. Meyer, MD, FAAFP
Assad Meymandi, MD, PhD
Melinda B. Michelson, MD
Igor D. Middlebrook, DO
Marcia G. Miedema, PA-C
Aaron J. Miller, MD
Donald S. Miller, MD
Jordan H. Miller, MD
Stacey H. Miller, MD
John K. Min, MD
Gregory J. Mincey, MD
Madhur Mittal, MD, FAAP
Michael J. Modrow, PA-C
Vikki M. Mollette, PA-C
Thomas J. Monaco, Jr., MD
Arl V. Moore, Jr., MD
David F. Moore, Jr., MD
Edgar C. Moore, Jr., DO
John H. Moore, III, MD
John R. Moore, IV, MD
Kenneth E. Moore, MD
Laura P. Moore, MD
Franklin J. Mooring, MD
Koreen Morgan, PA-C
Richard E. Morgan, MD
Tiffany M. Morgan, MD
William G. Morrel, IV, MD
Luke L. Morrison, PA-C
Allison Mullin, PA-C
Colin B. Muncie, MD
John C. Murray, MD
Jennifer H. Myatt, MD
Perry B. Myrick, MD
David A. Nachamie, MD
Madjimbaye C. Namde, MD
Sharad Nangia, MD
David C. Napoli, MD
Madison A. Nation, MD
Vandana Nayal, MD
Mark H. Neely, MD
Leonard D. Nelson, Jr., MD
W. Michael Nesbit, MD
Bryan R. Neuwirth, MD, DDS
Howard W. Newell, Jr., MD, FACP
George B. Newsome, MD
Cynthia M. Norris, MD
Abigail W. North, PA-C
Michael Norton, MD
Pedro J. Nunez, MD
Suzanne H. Nutt, MD
Okechukwu E. Nwoko, MD
Daniel M. Oberer, MD
Megan M. O'Brien, PA
Todd E. Ogrodowczyk, MD
Sarah J. Olenick, MD, PhD
James H. Oliver, III, MD
Kenneth L. Oliver, MD
David E. Ormond, MD
Samuel L. Orr, MD
Albert J. Osbahr, MD, MSCM, FACOEM
Thomas A. Ostergard, MD
Gerald V. Otteni, MD
Dean P. Ouano, MD
Preeti P. Ozarkar, MD
Shyamal K. Palit, MD
Gilbert F. Palmer, MD
Sravan Panuganti, DO
Sophia C. N. Paraschos, MD
Yoosun Park, MD
Susan R. Parlow, MD
Justine M. Parmele, MD, FAAP
Thomas E. Parrish, PA-C
Joshua G. Paschall, MD
Pooja S. Patel, MD
Sushma M. Patel, MD
LaTisha D. Patterson, PA-C
Scott M. Paviol, MD
Gerald Pelletier, Jr., MD
Brian A. Perry, II, MD
Catherine R. Perry, PA-C
Rachel L. Perry, PA-C
Robert D. Peters, MD
Cobern V. Peterson, Jr., MD
J. Duncan Phillips, MD, FACS, FAAP
Mark L. Phillips, MD
Douglas W. Picton, MD
Stephanie J. Plummer, DO
Ricardo O. Pojol, MD, FAAP
David C. Pollock, MD
James M. Polo, MD
Jonathan R. Prentice, PA-C
Thomas L. Presson, MD
Carina A. M. Pringle, PA-C
Nicole Proscia, MD
Annie C. Pugh, MD
Sankalp Puri, MD, FACEP
Aveline Quinlan, MD
J. Laurence Ransom, MD
Tariq Rashid, MD
Candice M. Ray, MD
Jeremy K. Reading, MD
Whitman L. Reardon, MD
Kavya E. Reddy, MD
Michael S. Rees, MD
Thomas E. Register, Jr., MD
Mark E. Reiber, MD
Gregory E. Reichert, DO
David P. Reilly, MD
John L. Remington, MD
Stefan A. Renaud, DO
Mary E. Renze, PA-C
Katlyn E. Rhodes, PA-C
Daniel C. Richard, MD
Brad A. Richter, MD
Erin L. Riley, PA-C
Diana Rivera, PA-C
G. Don Roberson, MD
Virgil O. Roberson, III, MD
W. Earl Roberson, MD
William S. Roberts, MD, FACC
Laurie C. Robinson, MD
Taylor J. Robinson, PA-C
Christopher P. Rodgers, MD
Thomas J. Rojy, Jr., MD
Hal J. Rollins, Jr., MD
Ronald Ross J. Romanelli, PA
Jacqueline L. Rookwood, MD
Steven D. Roos, MD
Raymond T. Rosario, MD
Anelia P. Rose, MD
Michael L. Ross, MD
Glen D. Rowe, DO
Kristina D. Rowe, MD
Samuel J. Roy, MD, DDS
Paul F. Rush, MD
Annemarie I. Russell, MD
John H. Russell, MD
Karel F. Rybnicek, MD
Maged H. Saad, MD
Steven M. Salisbury, II, MD
Bailey Sanders, MD
David L. Sappenfield, MD
Joshua D. Sarett, MD, FACEP
Julia M. M. Sargent, DO
Nakshatra Saxena, MD
Robert E. Schaaf, MD, FACR
Randie Schacter, DO
Debra Schardt-Sacco, DMD, MD
Herman E. Schmid, Jr., MD
Andrew M. Schneider, MD
Gregory G. Schnier, MD
G. Kenneth Scholl, Jr., MD
Jennifer B. Scott, PA-C
Melissa S. Scott, PA-C
Craig J. Secosan, MD
Khaing Z. See, MD
William Lawrence Selby, Sr., MD
Thomas J. Sena, MD
Phillip P. Shadduck, MD
Kinchit K. Shah, MD
Poorvi J. Shah, MD
Pratish A. Shah, MD
Sanjay B. Shah, MD
Frank C. Sheldon, MD
Brian T. Sherrington, MD, FAAP
Kristen M. Shipherd
Marc T. Silver, MD
J. Dale Simmons, MD
Rebecca K. Simpkin, MD
Francis J. Sincox, Jr., MD
Kelley B. Singer, MD
Kimberly R. Singletary, MD
Stephen J. Sladicka, MD
Robert F. Sloop, Jr., MD
Thomas W. Smith, MD
Garrett W. Snyder, DO
Lewis C. Sommerville, MD
John P. Sorge, MD
Diana M. Spahlinger McCarthy, MD, MPH, MS
Sharon Y. Speed, MD
Richard S. Stack, MD
Mark J. Stallworth, MD
Sarah E. Starr, DO
Rebecca R. Steffens, MD
Jane L. Steiner, MD
G. Terry Stewart, MD
Volker W. Stieber, MD
Hunter G. Strader, Jr., MD
Michael Y. Streahle, PA-C
Ashley R. Strickland, MD
Lindsay C. Strowd, MD
Bryan D. Stup, MD
Jennifer J. Styons, MD
Raymond C. Sullivan, Jr., MD
Kevin M. Supple, MD
Angelito C. Sy, MD, FAAP
Jeremy P. E. Sylvanus, MD
Stephen A. Szabo, MD
Gamal Tadros, MD
Paul J. Talerico, MD
Amanda T. Taylor, PA-C
Jacob M. Taylor, PA-C
Jimmy L. Taylor, MD
Robert E. Taylor, MD
Myra L. Teasley, MD
Hillary A. Tester, PA-C
Daniel M. Thailer, MD
Leelee Thames, MD
Christopher L. Tharrington, MD
Ann H. Thomas, PA-C
David S. Thomas, MD
Sandhya A. Thomas-Montilus, MD
Jennifer A. Thompson, MD
Sean L. Thompson, PA-C
Brian D. Thorp, MD
W. Virgil Thrash, MD
Sheel Y. Tolia, DO
Gary M. Toppin, PA-C
Nancy L. Tove, MD
G. Reginald Tucker, Jr., MD
Murray W. Turner, MD
Steven H. Turner, MD
Liliane Z. Tyson, MD
Thurlow R. Underhill, MD
Deepu S. Ushakumari, MD
Raja S. Vadlamudi, MD, MPH, FACP
Robert C. Vanderberry, Jr., MD
Rupashree Varadarajan, MD
Ajay K. Veeragandham, MD
Bernard Velardo, MD
Anne M. Verlangieri, MD
H. Ryland Vest, Jr., MD
Sajeev P. Vettichira, MD
Anton Vlasov, DO
S. Elizabeth von Biberstein, MD, FACS
Jaime S. Wagner, DO
John G. Wagnitz, MD
Constance E. Walker- McMullan, MD
Benjamin E. Wall, MD
Jack G. Wall, MD
Juliann S. Wallner, MD
Zane T. Walsh, Jr., MD
Alex J. Warren, MD
Toni Anne Washington, MD
Lawrence J. Watts, MD
Robert M. Wein, MD
Eryn S. Wells, MSPH, PA-C
Hamilton J. Wells, MD
Patricia W. Wesson, MD
Robert L. West, MD
James W. Wheatley, MD
William B. Wheatley, MD
John W. Whelan, Jr., MD
Winfry E. Whicker, MD
James Allen Whitaker, III, MD
Miles W. Whitaker, MD
Jeffrey J. White, MD
James D. Whitehouse, MD
Robert E. Wiggins, Jr., MD
Christy B. Wild, PA
Caroline L. Wilds, MD
Lauren E. Wilkinson, PA-C
Virgil V. Willard, II, MD
Aerik A. Williams, MD
Jefferson G. Williams, MD
Randall W. Williams, MD
Adam K. Wilson, MD
Nicole M. Wilson, DO
Ted R. Winneberger, MD
Lynne S. Wirth, MD
Beverly F. Womack, MD
Francis P. Wong, MD
Frances O. Wood, MD, FACC
Katherine G. Wu, MD
Chileatha D. Wynn, PA
Richard T. W. Wynn, MD
Wendell G. Yarbrough, MD
Joanna E. York, MD
Maghen K. York, PA
N. William Young, Jr., MD
Robert J. Young, III, PA-C
Robert L. Young, DO
Daniel C. Zedek, MD
Adam S. Zivony, MD
Wins Keep Coming as NCMS Works Hard for YOU!

The NC House has passed several pieces of NCMS-supported legislation recently. Below is a brief summary of several:
HB 576: Healthcare Practitioner Transparency Act - also known as "truth in advertising" - This legislation would require a healthcare practitioner to properly identify their license, certification, or registration (MD, DO, etc.) and shall not display any deceptive or misleading information.
HB 560: Diagnostic Imaging Parity - Would provide health coverage parity for breast cancer diagnostic imaging and would require coverage for certain other types of imaging.
HB 739 - Update Requirements/Advance Healthcare Directives - This patient-focused legislation facilitates access to health care powers of attorney and advance health care directives by modernizing and enhancing the advance care planning process.
Stay tuned to our Morning Rounds newsletter and social channels for more legislative updates.
You can catch up on past legislative updates here.
In Memoriam: NCMS Lifetime Member Dr. Lee Andrew Clark, Jr.

Lifetime NCMS member Lee Andrew Clark, Jr., MD, died April 21, 2023. He was 92.
Dr. Clark attended medical school at UNC, Chapel Hill. In medical school he was inducted into the Alpha Omega Alpha Honor Medical Society. He was President of his medical school class, the class of 1956.
A board-certified Ophthalmologist, Dr. Clark practiced Ophthalmology in Wilson, N.C. from 1962 until 2018, served as Wilson County’s representative to the North Carolina Medical Society, as President of the Wilson County Medical Society, and chaired the Ophthalmological section of the North Carolina Medial Society. He served on the North Carolina Governor’s Advisory Council on Comprehensive Health Planning and also served on the admissions board of UNC’s medical school.
Dr. Clark joined the North Carolina Medical Society in 1963!
Read Dr. Clark's full obituary here.
Experts Warn Teen Eating Disorders More Severe Than Ever

Hospitalizations for eating disorders spiked during the pandemic, doubling among adolescent girls, according to the Centers for Disease Control and Prevention. While most teens have returned to a normal life of in-person school, sports and social activities, eating disorders, especially anorexia, remain at an all-time high, experts warn.
Eating disorder-related health visits — which include hospital stays, pediatrician visits, telehealth talk therapy, and everything in between — more than doubled among people younger than 17 in the past five years, according to a recent report from the data company Trilliant Health. From 2018 through mid-2022, visits among this age group jumped 107.4% across all eating disorders, from around 50,000 visits at the beginning of 2018 to more than 100,000 in 2022. Visits related to anorexia nervosa, which has the highest death rate of any mental illness, jumped 129.26%.

Read the full article here.
NCDHHS Establishes Action Plan Focused on the Well-Being of NC Children

The North Carolina Department of Health and Human Services (NCDHHS) has established a vision for children and families in North Carolina that children are healthy and thrive in safe, stable and nurturing families, schools and communities. A key component of supporting child and family well-being is addressing nutrition security for all North Carolinians. Nutrition security is defined as having consistent and equitable access to healthy, safe, affordable foods essential to optimal health and well-being.
In North Carolina, about 10.9% of the population – about 1.2 million people – are experiencing food insecurity. About 394,000 of those individuals are children, with about one in six children facing hunger. NCDHHS is committed to decreasing the food insecurity rate from 10.9% to 10.0% by December 2024.
The NCDHHS State Action Plan for Nutrition Security outlines an innovative, multi-pronged strategy for achieving that vision – including related goals outlined in the NC Early Childhood Action Plan, Healthy North Carolina 2030, the State Health Improvement Plan, and the NCDHHS Strategic Plan 2021-2023.
Read more about the plan here.
NCMS Supports an Inflationary Adjustment for Medicare Reimbursement

The North Carolina Medical Society has reached out to each of our members of Congress encouraging their support of legislation which would tie the Medicare physician payment schedule to the Medicare Economic Index. H.R. 2474 / Strengthening Medicare for Patients & Providers Act would institute an annual inflation-based update to the Medicare reimbursement formula and put physicians on par with other Medicare providers. The failure of Medicare payment policy to account for inflationary adjustments has resulted in a 22% decline in reimbursement over the past 20 years and has jeopardized North Carolina’s 2.1 million Medicare beneficiaries’ access to care. Through its letter to Congress , the NCMS has partnered with other medical societies in advocating for our members and their patients. Please join in that effort by reaching out to your member of Congress. The AMA has set up an easy online messaging tool for you to reinforce our message, so please do so today.
NCMS Legislative Review: April 28, 2023

What a week!
As discussed last week, NCMS aided in the creation of a new bill to address Prior Authorization, HB 649: Ensure Timely/Clinically Sound Utiliz. Review.
In just one week, the bill passed the House Health Committee, House Rules Committee, and was unanimously passed by all members of the House! In a 112-0 vote in favor of the legislation, the bill has passed its first chamber and will now head to the Senate for their consideration.
House Bill 649 started with physician advocacy and passed the House due to physician advocacy.
NCMS members came together in a Payer Relations Taskforce to identify challenges physicians face in this realm. That taskforce determined that Prior Authorization was their biggest concern for physicians and their patients. This led NCMS staff to work with Representative Baker, Representative Reeder, Representative Potts, and Representative Sasser to create House Bill 649.
NCMS is very thankful to the bill's sponsors and cosponsors for their hard work.
We look forward to the next steps in the Senate!
An Endoscopic Procedure May Help Eliminate the Need for Insulin in People with Type 2 Diabetes

Early research suggests an investigational outpatient endoscopic procedure may help eliminate the need for insulin in people with type 2 diabetes.
Re-cellularization via electroporation therapy (ReCET) uses a specialized catheter to deliver alternating electric pulses to the duodenum to induce cellular regeneration. This process is thought to improve insulin sensitivity, in part, by altering gut hormones and nutritional sensing, principal investigator Jacques Bergman, MD, PhD, said.
"This might be a game changer in the management of type 2 diabetes because a single outpatient endoscopic intervention was suggested to have a pretty long therapeutic effect, which is compliance-free, as opposed to drug therapy that relies on patients taking the drugs on a daily basis," said Bergman, professor of gastrointestinal endoscopy at Amsterdam University Medical Center, Netherlands.
Read more about the procedure here.
NCDHHS Webinar to Provide Updates from Division of Mental Health, NC Medicaid, and More

NCDHHS is holding an update webinar on May 4 from 3-4 p.m. for clinicians, practice managers, quality improvement professionals and care coordinators to provide updates from the Division of Mental Health, Developmental Disabilities and Substance Abuse Services and Division of Health Benefits (NC Medicaid).
Proposed NC Bill May Impact NC Commission for Public Health

NC House Bill 621 seeks to modify the way new vaccines are reviewed by the NC Commission for Public Health.
If approved, the bill would require the Commission to wait at least three years following FDA approval of a new vaccine before adding the vaccine to the immunizations required by the State. However, the bill would also allow an FDA-approved vaccine to be added that has been approved for less than the minimum three-year period upon the recommendation by both the North Carolina Medical Society Board of Directors and the North Carolina Pediatric Society Board of Directors.
NCMS staff will keep members updated as this bill moves through the legislative process.
On Point: Doctors: If NC Enacts a 12-Week Ban on Abortion, More Women Will Die by Dr. Beverly Gray and Dr. Jonas Swartz
On Point submissions are individual member viewpoints and not North Carolina Medical Society policy.


Doctors: If NC enacts a 12-week ban on abortion, more women will die
Sunday, April 23, 2023 in the Charlotte Observer and News & Observer
By Dr. Beverly Gray and Dr. Jonas Swartz
Esse quam videri.
Our state motto – “To be, rather than to seem” – should encapsulate the values of North Carolinians. We should stand for truth, honesty, and transparency. But anti-abortion legislation referenced recently by House Speaker Tim Moore aims to do the exact opposite and will put women in danger. Speaker Moore told the media that Republicans have reached an agreement about a 12-week abortion ban, despite outcry from the medical community about the impacts of bans on the women and families of our state. If enacted, such legislation would devastate a woman’s ability to exercise reproductive autonomy and control her health care.
We are OBGYNs who provide comprehensive obstetric and gynecologic care. We see patients on some of their happiest days and some of their saddest. We both provide abortion care because we trust our patients to make the best decisions for their bodies and their families. We also know and love people who have had abortions. We have seen the care we provide save lives and give people their lives back.
Since the Dobbs v. Jackson Women’s Health U.S. Supreme Court decision, we have also seen the struggles patients in neighboring states overcome to access basic health care. We are currently watching a legal soap opera play out over access to mifepristone, the most common medication abortion drug, despite decades of safe and effective use. Now in many states, patients seeking to end an unwanted pregnancy at six weeks—a five-minute clinic procedure—must take multiple days off work, find care for their kids, travel to another state and find a place to stay, not to mention having the means to cover the cost. In just the six months after Dobbs, over 30,000 women were forced to continue their pregnancies because of these barriers.
If this anti-abortion effort becomes law in North Carolina, the repercussions would be dire both for individual patients and for the public health of our state. Abortion is incredibly safe. These laws hinder our ability to offer evidence-based, safe care. Our country is facing a maternal mortality crisis, and states with abortion bans have maternal mortality rates three times higher than states without bans. Abortion care is part of comprehensive health care and restricting access will mean that more women will die in our state. Like other health outcomes, maternal mortality also has extreme health disparities, meaning the burden of death and injury from pregnancy fall on people of color and people living in poverty. These are the same people who anti-abortion legislators are punishing by cutting off access to life-saving care.
Who should you trust on this issue? The North Carolina Medical Society, the North Carolina Obstetrics and Gynecological Society, the American College of Obstetricians and Gynecologists, the American Medical Association and the World Health Organization all oppose abortion bans. Trust the 1,300 medical professionals from North Carolina who co-signed a letter supporting abortion access in our state. They understand that access to care saves lives.
If you don’t trust doctors, trust your fellow North Carolinians. Fifty-seven percent of us either want to keep the laws as they are in North Carolina or expand access. We know that, for some, abortion has not been a dinner table discussion. But now is the moment to bring it up with our friends at churches, barbecues, and basketball games.
This potential legislation is harmful to women's health and well-being, which is why we vehemently oppose it. Though purporting to be in the best interest of the health of North Carolinians, it will prove to be harmful to the very citizens it aims to help. Women must have the right to make their own decisions about their reproductive health, and they must have access to essential health care services. This is our opportunity to be a beacon of truth, honesty, and health, rather than seeming to. We must stand up and oppose laws that will harm the families in our state. Call your legislator today and tell them why you support access to reproductive health care and oppose these dangerous abortion bans.
Drs. Beverly Gray and Jonas Swartz are associate and assistant professors, respectively, of Obstetrics and Gynecology at Duke University.
Legislation on COVID Vaccine Mandates Passes NC House, How it Could Affect Your Business
House Bill 98, Medical Freedom Act, passed the House 73-41, with three Democrats and all present Republicans voting in favor, and was sent to the Senate.
Beginning in January 2024, the state’s public schools, community colleges and universities would also be prohibited from requiring students to get the COVID-19 vaccination or a booster shot. Private schools and businesses could still require their students or employees to receive the vaccine.
Rep. Brian Biggs, a Randolph County Republican and one of the bill’s primary sponsors, expressed his concerns on the House floor that such requirements pressure and rush people to make a serious medical decision before taking the time to consider if it’s the right choice for them.
“It’s not intended for everyone,” he said of the COVID-19 vaccine. “It’s not a one size fits all. We just want to give people the option.”
North Carolina law requires students at public, private and religious colleges and universities to receive other immunizations in most circumstances, including for mumps, measles and polio. The coronavirus vaccine is not currently required.
Rep. Maria Cervania, a Wake County Democrat and epidemiologist, explained the early development of coronavirus vaccines and touted their importance in preventing more deaths.
“To say it’s discrimination to choose not to show proof of the vaccine when we’re trying to control outbreak and death ... is derelict to my profession and to other medical professionals,” she said during floor debate.
The bill includes certain exceptions for jobs and educational programs at facilities certified by the Centers for Medicare and Medicaid Services that require their employees to get the shot.
The NCMS will continue to monitor this bill and bring you more as it moves through the Senate.
A Notice for Your Hispanic Patients: Uterine Cancer on the Rise in Hispanic Women

New research suggests uterine cancer, generally more common in older women and is long known to disproportionately affect Black women, is now rising rapidly among reproductive-aged Hispanic women.
In 2018, Hispanic women had the highest uterine cancer rate among young reproductive-aged women between ages 35 and 39. Cases have been rising a steady 4% each year since 2001.
Experts are trying to figure out what is causing the disparity and raise awareness among medical professionals and patients to get screened.
One option to lower risk for uterine cancer is taking a contraceptive, said NCMS member and gynecologic oncologist Dr. Lucybeth Nieves-Arriba at Novant Health.
But that might not be an option if a patient has obesity or smokes because of complications like blood clots, she said. That’s why it’s essential, she said, to work with a clinical team for a personalized plan to catch it early and evaluate options.
“With awareness, in any doctor these little flashlights should turn on: If they see somebody that is obese and having irregular periods, they cannot just brush it off,” she said.
Read the full article here.
NCMS PAC Thankful Thursday!
On this Thankful Thursday, we are recognizing some of our NCMS PAC Investors! Thank you for your continued support and investment to your patients and profession. Contact Hannah Rice ([email protected]) to learn more about how you can make a difference.
Christian G. Anderson, MD
Current Patterson, MD
Danilo R. Bernardo, MD, FACP
George A. Howard, III, MD
John M. Lafferty, MD
Kim K. Briscoe, MD
AdventHealth Hendersonville Renews Prestigious Breast Cancer Care Accreditation

The National Accreditation Program for Breast Centers (NAPBC), a quality program administered by the American College of Surgeons (ACS) has granted accredited status to AdventHealth Hendersonville’s Cancer Services.
The NAPBC accreditation standards address a center’s leadership, clinical services, research, community outreach, professional education, and quality improvement for patients.
“We are so proud of our Cancer Services team for once again meeting the demanding standards set by NAPBC to demonstrate their commitment to every breast cancer patient in our care,” shares Brandon Nudd, FACHE, President and Chief Executive Officer for AdventHealth Hendersonville.
Congratulations, AdventHealth!
Read the full press release here.
NCMS Celebrates National Osteopathic Medicine Week

It's National Osteopathic Medicine Week
April 17-23 is National Osteopathic Medicine Week, or NOM Week.
NOM Week is a national observance dedicated to spotlighting the osteopathic medical profession and raising awareness about the distinctiveness of osteopathic medicine. The week also celebrates the unique approach DOs bring to health care.
Learn more about NOM Week and how to participate in NOM Week celebrations here.
Could an Ancient Virus be Key to Fighting Lung Cancer?
A new study has found that remnants of ancient viruses that remain in human DNA can help people fight lung cancer.
Scientists found that these endogenous retroviruses are dormant in most people but can be awoken in cancer tissue.
In both mice and human tissue, scientists discovered that when these cells are activated, they can elicit an immune response from B cells, which are white blood cells that create illness-busting antibodies.
Read the full article here.
On Point: Here is What Prior Authorization Means to Physicians by NCMS President Dr. Arthur Apolinario
On Point submissions are individual member viewpoints and not North Carolina Medical Society policy.

Here is what prior authorization means to physicians.
I am a suboxone MAT provider. I get people off heroin and opiate addiction using office-based therapy.
Today I have a patient in trouble.
She is 21 years old, doing well after 2 years on therapy, and pregnant. I have to make a decision for her.
She must come off suboxone and go on buprenorphine immediately to prevent NOWS in the baby or it will suffer withdrawal syndrome. If she goes without the medication altogether, she can go into immediate withdrawal and lose the baby.
I can protect her, but my hands are tied. The Medicaid managed care company will not fill the correct medication without prior authorization.
I referred her to the UNC High Risk Pregnancy Clinic and changed her medication immediately. That wasn’t allowed. We sent records proving she was in a very dangerous situation and she was denied again. At this point she had not taken the new medication and we are in the second day of trying to protect her and her baby. When a pregnant woman withdraws from opiates she may miscarry.
My nurse spent four hours, half a day, working on this by making phone calls. I told her I needed a medical director on the phone to review the records and get this medicine expedited. Finally, it was approved.
It took another several hours to find a pharmacy that had the medicine. Thankfully, through hours and hours of unnecessary work, she had the medicine in her hands.
If that had taken longer, her next choice would be to return to the streets and buy street drugs again.
That is what prior authorization creates for physicians.
2023 NCMS Photo Contest Now Open
Photo submissions are currently being accepted for 2023!
Now in its 15th year, the NCMS Photo Contest is an annual tradition that has gained national recognition, and we want you to be a part of it! Think you have the perfect picture to send in?
Check out the rules here.
Virtual Event: Top Execs from NC Hospitals Discuss the State of Healthcare

On Tuesday, May 9th, top executives of some of the largest hospitals in NC will discuss how to navigate the mounting challenges considering economic pressures, federal reimbursement changes, certificate of need adjustments, and the private and public insurance ecosystem.
These executives will address the opportunities and challenges facing hospital systems in North Carolina, and what may happen in terms of process and public policy to the industry that could benefit many other supporting industries that consider the health care sector as the linchpin of their success.
Our panelists are:
Dr. Craig Albanese, CEO, Duke University Health System
Dr. Wesley Burks, CEO, UNC Health
Dr. Mary Jo Cagle, CEO Cone Health
Ken Haynes, President, Southeast Region, Atrium Health
Jeff Lindsay, EVP and Chief Operating Office, Novant Health
Moderator: Zac Ezzone, Staff Writer, Triangle Business Journal
Learn more about this virtual event and register here.
Syphilis Cases on the Rise in North Carolina, Especially in Women and Babies

According to the North Carolina Department of Health and Human Services, Syphilis cases in North Carolina are on the rise, increasing 23 percent from 2021 to 2022.
Cases among women jumped from 360 in 2019 to 837 in 2022, a 133 percent increase, according to preliminary data. This increase in syphilis infections among women is also causing an increase in syphilis in babies, called congenital syphilis (CS). Congenital syphilis increased 31 percent in 2022 (55 cases) compared with 2021 (42 cases). In 2012, there was one reported case of congenital syphilis. [source]
Read more and learn about North Carolina's public health law requirements on screening all pregnant women for syphilis here.
NCMS Legislative Review: April 14, 2023

With General Assembly members on spring break last week, NCMS has been getting caught up on a torrent of bills filed. All bills being considered by the Senate are now filed, with many impactful ones filed at the last minute.
Of note is SB 639, which, among many provisions, would change current minor consent law. As currently written, minors can consent to treatment for pregnancy, venereal disease, emotional disturbance, and abuse of controlled substances. This bill would remove those exceptions and only allow consent for these treatments from emancipated minors.
Here some the other bills of note we are tracking:
SB 467/HB 552, MOMnibus Act: Various policies and appropriations for programs based around birth peoples, especially black women.
SB 491/HB 587, NC Genetic Counselors Workforce Act: Would establish a Genetic Counselors Licensure Board and formally regulate the process of genetic counseling.
SB 513/HB557, North Carolina Healing Arts Commission: Would allow naturopathic doctors to prescribe with a formulary and more through a licensing process. Also creates a healing arts commission and create licensure for reflexologists and music therapists.
SB 597, Pharmacists/Collaborative Practice: Would create new rules that would expand pharmacist/physician collaborative practice which would expand pharmacist scope to allow testing and therapy.
SB 624/HB576, Health Care Practitioner Transparency Act: Would require name badges with licensure status on them to be worn in medical settings.
SB 641, Medical Ethics Defense (MED) Act: Would not allow termination or other career impediments for health care professionals/payers who refuse to participate or pay for certain medical practices based on conscience (defined as moral, religious, or ethical beliefs and principals, as well as these same values in a company's publishes guidelines, mission, etc.).
Find the full summary of the above bills here.
North Carolina Health Experts Address Rural Medicine

The North Carolina Healthcare Association welcomed rural health experts from around the state to speak on how their hospitals and health systems in rural North Carolina are reimagining health care to ensure their communities have the resources they need close to home.
Executives and rural healthcare leaders from St. Luke’s Hospital, UNC Health Wayne, UNC Health Blue Ridge, Dosher Memorial Hospital, and ECU Health spoke on their efforts to improve access and care in rural communities with outside-of-the-box thinking and collaborative partnerships.
Listen to this informative discussion here.