NCMS Talks 20 Years of Leadership Training and Opportunities to Prepare Tomorrow's Leaders Today!
20 Weeks Until NCMS LEAD Conference and Golden Stethoscope Awards Gala!
Learn more about how NCMS has been training leaders for two decades as we countdown to October 13!
https://youtu.be/AdPl-5ALUnU
As the NCMS prepares to celebrate 20 years of leadership training, we bring you a bit of history on the program. Kristina Natt och Dag, VP of Education and Training, and Erica Hall, NCMS Manager of Education and Training sit down with Randy Aldridge to talk about the Kanof Institute for Physician Leadership (KIPL) and the programs that are helping train tomorrow's leaders.
Listen and learn why you should apply for one of these phenomenal programs today!
To learn more about Leadership College and KIPL click here.
To register for the 2023 LEAD Conference and Awards Gala, or to be an exhibitor, click here.
Celebrating 20 Years of Leadership Training. KIPL Alumni Spotlight: Joshua F. Smith, MMS, PA-C, DFAAPA
CELEBRATING 20 YEARS OF LEADERSHIP TRAINING!

Joshua F. Smith, MMS, PA-C, DFAAPA started his career practicing Family Medicine, but transitioned to Duke Otolaryngology in 2006. He has been in this position since then and was recently promoted to Clinical Director of Advanced Practice Providers (APP) in Otolaryngology. Most of his time is utilized seeing patients in the outpatient clinic and supporting my APP team administratively.
KIPL Influence
KIPL helped me to realize that there were many leadership opportunities out there, I just had to be confident enough to take them. Since graduating from KIPL, I have served in multiple leadership roles at work and through my affiliation with the NC Academy of PAs. I have been a committee chair, chief delegate to the American Academy of Physician Assistants House of Delegates and President of the NCAPA. I have also participated in state and federal advocacy for my profession.
Daily Motivation and Mantra
The main reason I go to work every day is because I have this opportunity to help my patients. The truth is, I find working in Otolaryngology to be a lot of fun. I quite enjoy the challenge.
My daily mantra is "Stay positive. It is a privilege to be allowed into a patient's private life. Every small success adds up and makes a huge difference in the end."
To learn more about leadership training opportunities at NCMS click here.
To register for the 2023 LEAD Conference and Golden Stethoscope Awards Gala or to become a sponsor click here.
NCTracks: Feedback Needed to Improve User Experience

The North Carolina Department of Health and Human Services (NCDHHS) is implementing a new Provider Data Management/Credentialing Verification Organization (PDM/CVO) solution scheduled to launch in 2024.
This solution will be designed to improve the user experience and address NC Medicaid program needs. It will also align with Centers for Medicare & Medicaid Services (CMS) standards and conditions to support seamless coordination, integration, and interoperability.
To fully accomplish the goal of providing the best outcomes for clinicians, NCDHHS is asking for your assistance in sharing your past and present experiences with the current system by completing the Provider Data Management/Credentialing Verification Organization Survey.
The survey is designed to capture highlights and challenges (i.e., pain points) of the current system, and features that would make your credentialing team more effective.
The deadline to complete the survey is Friday, June 23, 2023.
NCMS LEAD 2023 Annual Conference: Call for Panelists

The North Carolina Medical Society is looking for young physicians, less than 10 years out of training, to serve on a panel at the LEAD 2023 Annual Conference.
Topics that will be discussed:
- What you want the healthcare system to look like in 10, 20, and 30 years
- The future of AI and tech
- Concerns and fears within the healthcare system
The panel will take place on Friday, October 13 from 11am-12pm. Please submit any inquires to Megan Eberle at [email protected].
Submissions are due by Monday, July 31.
To register for the 2023 LEAD Conference and Golden Stethoscope Awards Gala or to become a sponsor click here.
HRSA Makes Changes to COVID-19 Survey Frequency

In response to CHC feedback and to other factors, HRSA is reducing the frequency of the COVID-19 survey.
Beginning with the report of June data in July, the survey will become monthly, rather than biweekly.
HRSA uses the information collected on the COVID-19 surveys to optimize COVID-19 testing and vaccination; track health center capacity and the impact of COVID-19 on operations, patients, and staff; and better understand training and technical assistance, funding, and other health center resource needs.
Visit the COVID-19 Health Center Survey Interactive Data Dashboards here.
Become a National Health Service Corps Site. Applications Now Being Accepted.

Eligible healthcare facilities can now apply for approval to become a National Health Service Corps (NHSC) site.
The National Health Service Corps is a federal government program administered by the U.S. Department of Health and Human Services, Health Resources and Services Administration, Bureau of Health Workforce and created to address a growing primary care workforce shortage.
NHSC programs provide scholarships and student loan repayment to health care professionals in exchange for a service commitment to practice in designated Health Professional Shortage Areas (HPSAs). NHSC-approved sites provide outpatient, comprehensive primary health care services to people in HPSAs.
All National Health Service Corps-approved sites receive the benefits of online, interactive access to the Health Workforce Connector, an online platform that allows you to:
• Create, manage, and advertise new job vacancies and training positions
• Search candidate profiles where you can learn about the qualification factors, experience, and other relevant information that highlight a candidate’s competencies
• View a comprehensive list of job seekers and students who have expressed interest in a position you advertised on the Health Workforce Connector
Learn more about the program and how to apply here.
Uptick in Hand, Foot and Mouth Disease Expected this Summer

UNC Health is warning of an expected increase in hand, foot, and mouth disease (HFMD) this summer in central North Carolina.
According to the Centers for Disease Control and Prevention (CDC), HMFD is a common viral illness caused by different strains of coxsackievirus. It occurs mostly during the summer and early autumn, and it is a short-term infection that occurs most frequently in children younger than 5 years old.
The first signs of HMFD usually are high fever, decreased appetite, sore throat, and feeling tired. Painful blisters in the mouth, and skin rashes (bright red dots, sometimes with clear blisters) can appear on the hands and feet, and sometimes the buttocks.
While there is not specific treatment for HMFD, the illness is usually not serious and most people with the disease get better on their own in 7 to 10 days, according to the CDC.
Read the full article here.
And the Winners of the NCMS PAC Raffle Are...
The winners of the NCMS PAC Cash Raffle Are...
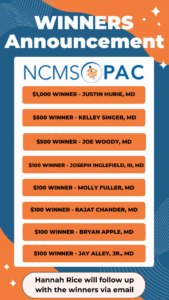
Congratulations!
Thank you to all of our investors! We raised over $5,600 for NCMS PAC!
In Memoriam: NCMS Lifetime Member Dr. Frank Wilson
NCMS Lifetime member Dr. Frank Wilson died Wednesday, May 31. He was 93.
For 47 years, Wilson was a member and leader in the UNC Department of Orthopedics, the School of Medicine, the University at large, and the profession of orthopedic surgery. From 1967 to 1996, he served as the Chief of the Division, and then Department, of Orthopedics.
He authored more than 100 medical research publications, over 50 book chapters, 8 books, and mentored over 100 Orthopedic residents.
In addition to his many other contributions to medicine, Wilson was a leader at the state level in his service to the NC Medical Society and the NC Orthopedic Association (NCOA). He was a founding member of the NCMS Sports Medicine Committee. He served as President of the NCOA in 1976 and was recognized by the NCOA in 1997 with the association’s Honored Surgeon Award.
Read Wilson's full obituary here.
Foundation Friday! Thank You to These NCMS Foundation Donors.

Today, the NCMS Foundation recognizes donors who have joined us on the journey to help make health and well-being attainable for all North Carolinians. These individuals are contributing to make sure clinicians are where they are needed most and that clinician leaders are lighting the way.
Susan H. Andersen, MD
Carl W. Berk, MD
Neil A. Conti, MD
Shannon M. Drohan, MD
Elizabeth H. Hawes, PA-C
Alyssa K. Henson, DO
Obinna O. Ikwechegh, MD
Christopher M. Johnson, MD
Ketarah C. Robinson, MD
John L. Scheitler, MD
Thank you for your continued support to help North Carolinians lead healthier lives.
Learn more about how YOU can make a difference too here.
UNC Partnership Launches New Statewide Suicide Prevention Program

UNC-Chapel Hill has launched a new statewide program for local communities across North Carolina aimed at decreasing suicide rates.
The new suicide prevention program is a partnership between the UNC Suicide Prevention Institute and Carolina Across 100 — an initiative to work with all 100 counties to fix pandemic-related problems.
Through collaboration with school systems, nonprofits, and healthcare providers, the program hopes to identify the specific needs of communities to design suitable suicide-prevention strategies and increase mental health resources.
Carolina Across 100 seeks applications from communities that are interested in working across sectors to prevent suicides and improve mental and behavioral health in the state. Teams will build collaboratives within their communities and benefit from peer learning with each other to better understand the context and impacts of suicide and related issues, as well as design and implement strategies to respond effectively.
Applications are now open. The deadline to apply is July 28.
Read the full article here.
NCMS PAC Thankful Thursday!
On this Thankful Thursday, we are recognizing some of our NCMS PAC Investors! Thank you for your continued support and investment to your patients and profession. Contact Hannah Rice ([email protected]) to learn more about how you can make a difference.
Aerik A. Williams, MD
Ava M. Swayze, DO
Daniel M. Zirkman, MD
John G. Albertini, MD
Lawrence H. Greenblatt, MD, FACP
Thomas E. Lawrence, MD
William G. Pittman, III, MD
TBT: Celebrating 20 years of Leadership in Medicine! Here is William Huang, MD's MEDTalk from 2021
This year the North Carolina Medical Society is celebrating 20 years of Leadership in Medicine!
Here is a Throwback Thursday to Dr. William Huang's MEDTalk from 2021 on burnout amongst dermatologists. Look for a new TBT every Thursday until the 2023 LEAD Conference, October 13-14.
https://youtu.be/-Qd-nffqf48
The 2023 LEAD conference registration is NOW OPEN. Click here for more information.
Please contact Erica Hall at NCMS to organize a class table at the LEAD Gala of your own.
Sign Up Now for Our 1st Virtual KIPL Alumni Event in July!

If you are a Kanof Institute for Physician Leadership Alumni/Scholar, we have some wonderful opportunities for you, starting with the first virtual training event next month!
Join us for our first KIPL Alumni event, a comprehensive training program on suicide prevention for clinicians. This virtual event is designed to provide you with the knowledge, skills, and tools necessary to identify, assess, and support colleagues who may be at risk of suicide.
Suicide is a growing public health concern and each year in the U.S., roughly 300 - 400 physicians die by suicide. As clinician leaders, it is crucial to be able to recognize the warning signs and provide the appropriate interventions to prevent suicide. This workshop will provide you with the latest evidence-based practices and strategies for preventing suicide.

Led by Dr. Rebecca Mathews, PhD, LCMHCS, LPC-S, CBGT, CHST - Clinical Assistant Professor with the Counseling and Educational Development (CED) Department at UNC Greensboro, Dr. Mathews is highly experienced and knowledgeable in the field of suicide prevention and will provide you with practical tools and strategies that you can apply in your clinical practice.
Don't miss out on this opportunity to enhance your knowledge and skills in suicide prevention. This training program is suitable for all clinicians in any role.
Two dates are available for the Question, Persuade, Refer: Suicide Prevention Training:
July 25, 2023 | 3:30pm - 5:00pm | Zoom Meeting
July 26, 2023 | 6:30pm - 8:00pm | Zoom Meeting
Space for these exclusive Zoom trainings is limited to just 35 attendees per session; please register soon!
For questions or more information, please contact us at [email protected]. We look forward to seeing you there!
Help NCMS Grow! Membership Advisory Committee is Seeking Volunteers
Help the North Carolina Medical Society Grow!

Do you have an engaging, innovative personality? Are you interested in helping the North Carolina Medical Society grow and retain its membership so it can be the best that it can be? Consider volunteering for the NCMS Membership Advisory Committee!
The NCMS Membership Advisory Committee, charged with attracting a diverse and inclusive membership while maximizing the NCMS experience, meets virtually once per quarter. Typical agenda items include reviewing membership numbers and demographics and discussing ways to better recruit and retain NCMS members.
NCMS Vice President, External Affairs Alan Skipper says: “We continue to face many critical legislative and regulatory issues, both in Raleigh and in Washington, and our potential for success is directly proportionate to both the size and strength of our membership. Every member matters.”
Committee members must be NCMS members.
If you are interested in learning more or being appointed to the Membership Advisory Committee, contact Frank Snyder at [email protected].
Celebrating 20 Years of Leadership Training. KIPL Alumni Spotlight: Blaine Paxton Hall.
CELEBRATING 20 YEARS OF LEADERSHIP TRAINING!

As the North Carolina Medical Society prepares to celebrate 20 years of Leadership College and the Kanof Institute for Physician Leadership, we are looking back at some of our alumni. For the next 20 weeks, until our annual LEAD Conference and Golden Stethoscope Awards Gala, we will be sharing stories of people who have completed their training and how that influenced them (plus some sage life advice!).
Enjoy getting to know more about Blaine Paxton Hall!
Blaine Paxton Hall, MHS-CL, PA-Emeritus, DFAAPA attended Wake Forest University School of Medicine where he obtained his Physician Assistant training. Dr. Hall later went on to earn his Masters in Health Science in Clinical Leadership (MHS-CL) from Duke University School.
Highlights from Blaine Paxton Hall, MHS-CL, PA-Emeritus, DFAAPA
I chose Medicine because several of my own life experiences caused me to have keen intuition into the suffering of others. I knew that I could deeply reach people and show them authentic empathy and compassion.
KIPL Influence
My final project for the Leadership College was an educational program for MDs and PAs on an "Overview of Healthcare for the Transsexual Patient." This was the direct impetus for my subsequent speaking, teaching, writing and consulting activities. And it gave me the confidence to continue to advocate and push for the Duke Adult Gender Medicine Clinic which I founded, and which was launched January 3rd, 2018.
Words to Live By
Seek to Relieve Suffering. That has always guided me; and is the most important thing I can do as a healthcare provider.
Some healthcare providers think they are bigshot healers; but they are absolutely not! Healing comes from within the patient themselves and/or from God and/or is unknown.
Dr. Hall’s NCMS Involvement
- Charter member of the PA section of the NCMS (1993 or 1994)
- Leadership College Scholar grad (2007)
- Served on the NCMS Foundation Board of Trustees (2019 through 2022)
- Currently serving on the Policy Committee
- Lifetime Member of NCMS.
To learn more about leadership training opportunities at NCMS click here.
To register for the 2023 LEAD Conference and Golden Stethoscope Awards Gala or to become a sponsor click here.
Study: Cocoa Flavanols May Combat Age-Related Memory Loss

A new study suggests a daily flavanol (a kind of antioxidant found in certain fruits, veggies, tea, and cocoa) supplement might help stall or even reverse age-related memory loss.
Researchers randomly assigned more than 3,500 older adults to take either a daily flavanol supplement or a placebo pill for three years. The supplement contained 500 milligrams (mg) of flavanols extracted from cocoa, which was within the 400 to 600 mg range recommended by the Academy of Nutrition and Dietetics as part of a healthy diet.
Participants completed a series of short-term memory tests designed to measure subtle changes in skills like word recall that tend to erode with advanced age. They also completed diet surveys that assessed the overall healthiness of foods they consumed and how often they ate foods known to be rich in flavanols.
For the people who had the lowest-quality diets and consumed the fewest flavanol-rich foods, supplements made a significant difference. In memory test, their scores were 16 percent higher after one year of taking flavanol supplements than they were at the start of the study.
Read the full article here.
North Carolina Selected by CMS for its Making Primary Care Model

The Centers for Medicare & Medicaid Services (CMS) has announced that North Carolina is among eight states selected to participate in its Making Care Primary (MCP) practice model initiative. The innovation effort model seeks to improve care for patients by:
1) expanding and enhancing care management and care coordination,
2) equipping primary care clinicians with tools to form partnerships with health care specialists, and
3) leveraging community-based connections to address patients’ health needs as well as their health-related social needs.
The MCP Model will provide funding to build infrastructure, make primary care services more accessible, as well as better coordinate care with specialists.
CMS’ objective is to achieve savings over time through better preventive care and reducing potentially avoidable costs. The MCP model will run for 10.5 years, beginning July 1, 2024, and will engage state Medicaid agencies private payers.
Additional information is available from CMS here.
Novant Health: New Tiered Strategy to Address Disparities in Maternal and Infant Health

Novant Health recently announced its three-tiered strategy to address disparities in maternal and infant health, with a focus on the following three areas:
- Improving access to early and adequate prenatal care
- Recognizing and addressing deficits in social determinants of health (SDoH)
- Mitigating unconscious bias through proactive education and training
Infant mortality, fetal death and stillbirths occur at a higher rate in Black children. The drastic disparities centered on the maternal and infant health experience will be a central focus of Novant Health’s strategic approach.
Reads Novant's full press release here.
Poor Heart Health Linked to Risk of Musculoskeletal Disorders. What to Look Out For in Your Patients.

Studies show that conditions such as diabetes, obesity, and metabolic syndrome increase the risk of developing musculoskeletal conditions, and that cardiovascular disease risk is linked to the development of musculoskeletal conditions such as carpal tunnel syndrome (CTS), when a major nerve in the hand is squeezed or compressed as it travels to the wrist.
Musculoskeletal conditions are characterized by muscle, bone, joint, and connective tissue impairment that affects movement. Understanding more about the risk factors underlying musculoskeletal conditions could aid the development of treatment and prevention strategies.
In a study, researchers analyzed healthcare data from 1,224 workers in fields including manufacturing, healthcare, office jobs, and food processing. The study assessed for four common musculoskeletal conditions:
- CTS: pain in the wrist from repetitive grasping movements with the hands
- Rotator cuff tendinopathy: pain and weakness when moving the shoulder often caused by repetitive overhead activities such as throwing, raking, or washing cars
- Lateral epicondylopathy or ‘tennis elbow: pain, burning, or aching along the outside of the forearm and elbow that occurs when the forearm muscles become damaged from overuse
- Medial epicondylopathy or ‘golfer’s elbow’: pain in the inside of the elbow from overuse of forearm muscles
The study found that participants at a 15% higher than average risk of cardiovascular disease were four times more likely to develop a musculoskeletal disorder than those with lower risk.
Read the full article here.
Don't Miss June's Lunch & Learn Webinar!
Join us for the next Lunch & Learn Webinar: UnitedHealthcare – Interoperability & Point of Care Assist
Tuesday, June 20, 2023 | 12:00 PM - 1:00 PM EDT | Zoom
The opportunity in front of us is so important as we build future technology solutions to improve access to health care, health care information and decision support. This happens with interoperability, which is integrating UnitedHealthcare’s technology directly into your EMR which then seamlessly passes actionable data to you, all while the patient is in the room.
It’s interoperability that will help each of us obtain the goals of improving access to care while providing you with information to help you make decisions. We will learn about the top EMRs UnitedHealthcare has partnered with to share data and insights with you right in your EMR workflow and see a demonstration of how this looks in an EMR environment.
Webinar Speaker

Marci Miller is the Network Engagement Director for the Mid-South, Gulf States & Carolinas for UnitedHealthcare. She has been with UnitedHealthcare since 2012 and was one of the first on-site customer advocates for UnitedHealthcare, serving the Walmart Home Office in Bentonville, Arkansas.
Registration is complimentary; however, space is limited. After registering, you will receive a confirmation email containing information about joining the meeting. Thank you! We look forward to having you join us for this presentation.
If you have any questions, please contact the NCMGMA offices at [email protected].
AMA: New One-Stop-Shop Website on Medicare Physician Payment System

The American Medical Association (AMA) has launched fixmedicarenow.org, a one-stop-shop for all the information, resources and ways you can make your voice heard to ensure that Congress works to address the critical issues physicians, and their patients, face due to the flawed Medicare physician payment system.
The AMA has been fighting for Medicare physician payment reform for well over a decade, and the system remains on an unsustainable path. Temporary patches and ongoing cuts to the Medicare physician payment system have left physician practices and patient access to care at serious risk. Payment cuts, freezes and redistributions have further exacerbated the challenge, yet Congress and the administration are still not focused on fixing the root of the problem—the payment system itself.
It's essential that leaders in Washington work with the physician community on immediate, preventative measures, as well as long-term solutions that will reform the payment model once and for all.
Visit the Fix Medicare Now website here.
Scientists Make First-Time Advancement with Amyloidosis of the Heart Reversal

Researchers led by scientists from University College London have, for the first time, reported the spontaneous recovery of 3 patients with transthyretin cardiac amyloidopathy (ATTR-CM), a rare but severe and progressive heart condition where sticky, toxic proteins build up in the heart muscle and cause heart failure. They believe that the recovery may have been due to an immune response, suggesting that antibody treatments could be effective against the condition.
Antibodies were found in the three men that specifically targeted amyloid deposits. These amyloid-targeting antibodies were not found in other patients whose condition progressed as normal.
If these antibodies can be harnessed, they could be combined with new therapies being trialed that suppress TTR protein production. This would enable clinicians to clear away amyloid as well as prevent further amyloid deposition, according to researchers.
Read the full article here.
An Amino Acid Showed Promising Results in Mice. Could it Be a Fountain of Youth for Humans?

New research shows higher levels of taurine, an amino acid found in meat and shellfish, help slow aging in animals. Now, researchers want to know if it could possibly do the same for humans.
Taurine is a popular supplement added to many energy drinks and touted to promote sharper brain function.
In experiments with mice and monkeys, researchers found that supplementing middle-aged animals led to better health.
In mice, the supplementation led to less weight gain, increased bone density, improved muscle endurance and strength, reduced insulin resistance, a better-functioning immune system and a 10% longer lifespan, which in humans would be about seven or eight years.
In monkeys, supplementation prevented age-related weight gain, improved fasting blood sugar levels, increased bone density and led to healthier livers and improved immune system function.
Read the full article here.
Popular Social Media Weight Loss Supplement: All Hype or Actually Helpful?

On social media, Berberine, a natural compound found in several plants, is the latest supplement craze, gaining attention as a "natural" weight loss option.
Two of the side effects with this supplement can include diarrhea and gastrointestinal upset but also may include constipation, nausea or abdominal discomfort or swelling.
Advocates for Berberine claim it may help suppress appetite, lower cholesterol, aid in gut health and control blood sugar and blood pressure, but experts caution about a lack of sufficient data and oversight for the pill.
Is it safe for your patients? Read the full article here.
New Study: Reanimated Hearts Could Change Landscape of Organ Donations

A new study found that a method of heart transplantation known as donations after circulatory death (DCD), which uses machines to reanimate donor hearts from people who have died, is just as good as traditional heart transplantation.
The study published in the New England Journal of Medicine noted that the adjusted six-month survival rate of patients undergoing the new method was 94%, compared with 91% among patients who underwent the traditional method.
The study included 180 participants, with 90 patients in each group. Not only did patients in the DCD group have equivalent — if not better — survival outcomes, they also received their transplants slightly faster, waiting on average 24 days compared with 31 days for patients in the traditional group.
Read more about this potentially groundbreaking advancement here.
Do You Know What is Required to Operate a Syringe Services Program? NCMS is Here to Help.

In order to operate a Syringe Services Program (SSP) within your Health Center Program scope of project and use new or existing Health Center Program funds, your health center must request prior approval from HRSA via EHBs.
HRSA must review and approve the prior approval request before Health Center Program funding can be used to support proposed SSP costs, as allowable.
Your health center’s state or local health department, in conjunction with CDC, must also have determined that the jurisdiction your health center is located within “is experiencing, or is at risk for, a significant increase in hepatitis infections or an HIV outbreak due to injection drug use.”
For full information, see the Health Center Program Compliance FAQs webpage.
Further federal guidance on SSPs is available at:
- HRSA-Specific Implementation Guidance to Support Certain Components of SSPs (PDF) – Published on HIV.gov, 2016
- CDC’s SSPs webpage
- HIV.gov’s SSPs webpage
NCSEPS Calling for Resident/Fellow/Student Poster Submissions
The North Carolina Society of Eye Physicians and Surgeons (NCSEPS) invites residents, fellows and students to submit posters of original or re-used basic research, clinical research, or a case presentation, for NCSEPS 2023 poster competition on September 8-10 at the beautiful Omni Grove Park Inn. Cash prizes will be given to the winning resident, student and fellow posters as judged by a panel of ophthalmologists. Register for the meeting today!
The deadline for submissions is July 24. Please submit poster abstracts to [email protected]. You will be notified which submissions are accepted shortly after the submission deadline. For complete details and the submission form, please download the call for poster abstracts.
Posters should be set up Friday evening, September 8th, and residents, fellows, and students should attend to their poster during the early morning and midmorning breaks on Saturday, September 9th. The posters should be left up through the end of the mid-afternoon break on Saturday, and the winning submissions will be announced prior to the conclusion of the meeting.
Please encourage your residents, fellows, and students to participate. Poster abstract submissions are due on or before July 24th and may be sent via email with the subject line "NCSEPS 2023 Poster Submission" to [email protected]. We will accommodate as many posters as space permits. Posters should be no more than 4' x 4' in size. You will be notified which submissions are accepted shortly after the submission deadline.
For any questions, please contact Megan Eberle at 919-623-3838 or [email protected].
As in the past, registration fees are waived for residents, fellows or students to attend the NCSEPS Annual Meeting. We hope to see you in September!
Artificial Sweetener Ingredient Linked to Genetic Damage. Are Your Patients at Risk?

A recent study has found that a chemical found in sucralose can break up DNA, showing that Sucralose-6-acetate, an impurity formed during sucralose production, was found to break up DNA strands and cause other types of genetic damage.
Researchers exposed human blood cells to sucralose in a series of in-vitro experiments. Not only did they check for markers of cell damage and genotoxicity, but they also found that it damages gut tissue. This leads to what they call “leaky gut syndrome,” which is when your gut lining becomes more permeable. Instead of toxins and waste products being filtered out through the kidneys, they instead are absorbed into the bloodstream via the stomach.
The study has raised concerns about the safety of sucralose, which is found in many diet sodas, sugar-free gum, and other products.
Read the full article here.
NCMS PAC Thankful Thursday!
On this Thankful Thursday, we are recognizing some of our NCMS PAC Investors! Thank you for your continued support and investment to your patients and profession. Contact Hannah Rice ([email protected]) to learn more about how you can make a difference.
Jeffrey T. Kornegay, MD
Jonathan D. Jaffe, DO
Manjunath Markandaya, MD
Marshall C. Freeman, MD
Rahul K. Kakkar, MD
Richard T. Weisenburger, DO
TBT: Celebrating 20 years of Leadership in Medicine! Here is Shauna Guthrie, MD's MEDTalk from 2018
This year the North Carolina Medical Society is celebrating 20 years of Leadership in Medicine!
Here is a Throwback Thursday to Dr. Shauna Guthrie's MEDTalk from 2018. Look for a new TBT every Thursday until the 2023 LEAD Conference, October 13-14.
https://youtu.be/6UF8gBbCTVM
The 2023 LEAD conference registration is NOW OPEN. Click here for more information.
Please contact Erica Hall at NCMS to organize a class table of your own.
Hormone Patches for Menopause Symptoms May Have Lower Blood Pressure Risk Than Pills

New research suggests patches or creams may be safer for women who use hormone therapy to relieve hot flashes and other menopause symptoms than pills.
The University of Calgary team examined health records of more than 112,000 women ages 45 and older who filled prescriptions for at least six months’ worth of estrogen-only hormone treatment between 2008 and 2019. They tracked which women went on to develop high blood pressure at least a year after starting treatment.
While the differences weren’t huge, women who took estrogen pills had a 14% higher risk of developing hypertension compared to those using skin patches or creams, the researchers reported.
Read full article here.
Former NCMS Director of Health System Advocacy Kristen Spaduzzi Joins CCHN

Former NCMS Director of Health System Advocacy Kristen Spaduzzi has joined NCMS partner Carolina Complete Health Network (CCHN) as Director, Value-Based Programs. This is an exciting opportunity for Kristen and the NCMS, as she carries forward her NCMS experience to the Medicaid network.
Kristen joined NCMS in April 2017. She was integral in helping practices navigate issues with payers and to develop their business models to embrace value-based care.
Kristen, thank you for being a resource for practices and for increasing NCMS value to members!
Send Kristen your well wishes in the comments.
New Solution to Medicaid FQHC Taxonomy Site Enrollment/Re-Verification Problems

The North Carolina Community Health Center Association (NCCHCA) reported some Federally Qualified Health Center (FQHC) sites were being suspended from Medicaid or losing their FQHC taxonomy based on how Medicaid was verifying Medicare participation by the FQHC. This disproportionately affected FQHC sites which do not typically enroll with Medicare (e.g., pharmacy, dental, and pediatric practices). Fortunately, NCCHCA and Medicaid have worked together to identify a solution.
Effective immediately, when verifying an FQHC’s participation in Medicare as a prerequisite for Medicaid enrollment or re-enrollment of a practice site under the FQHC taxonomy, NC Medicaid’s vendor GDIT will verify that an FQHC site meets the Medicare participation requirement if any site under the same FQHC organizational name and tax identification number is also enrolled in Medicare.
In effect, this this will allow confirmation based on the “parent” organization, without requiring that “child” sites or those typically serving non-Medicare populations or services to enroll in Medicare. This applies to reverification of existing FQHC sites as well as existing FQHC organizations adding new sites and locations.
Duke Cancer Center: Black Men May Benefit More from Metastatic Prostate Cancer Drug Combo

Interim results from a study led by the Duke Cancer Institute suggest that a drug combination that shows little overall survival benefit in white men with advanced prostate cancer has a far greater effect in Black men with the disease.
Funded by Janssen Pharmaceuticals, the study known as Panther, administered the hormone therapies apalutamide and abiraterone acetate plus prednisone to parallel groups of Black and white participants with metastatic prostate cancer.
Two years from the start of treatment with the two hormonal therapies, only 14% of Black study participants have died, compared to 33% of the white participants.
Read the full article here.
Behavioral Health Urgent Care Center for Children Opens in Wake County

Children dealing with a mental health crisis now have a new option to get help at a first-of-its-kind behavioral health urgent care center.
The Hope Center for Youth and Family Crisis opened Monday in Fuquay-Varina. It's designed to help families with children ages 5 to 20. The center provides 24/7 access to care, 365 days a year.
The center provides access to assessment, stabilization and treatment planning in a safe, secure and therapeutic environment, and can potentially reduce the strain on EMS as well as hospitals and law enforcement.
Read the full article here.
AstraZeneca's Lung Cancer Therapy Cuts Death Risk in Certain Post-Surgery Lung Cancer Patients

Trial data showed that Tagrisso, AstraZeneca's lung cancer therapy, cut the risk of death by more than half in patients with a certain form of lung cancer and diagnosed early enough to have the tumor surgically removed.
In a 682-patient trial called ADAURA, Tagrisso was evaluated against a placebo in earlier-stage EGFR-mutated NSCLC patients who had undergone surgery to remove their primary tumor.
The majority of such patients eventually see their cancer return despite surgery and add-on chemotherapy.
In the trial, Tagrisso or a placebo was given to patients to assess whether the AstraZeneca therapy could keep their cancer at bay.
Data showed Tagrisso slashed the risk of death by 51% compared to placebo.
Read the full article here.
Foundation Friday

Today, the NCMS Foundation recognizes donors who have joined us on the journey to help make health and well-being attainable for all North Carolinians. These individuals are contributing to make sure clinicians are where they are needed most and that clinician leaders are lighting the way.
Thank you for your continued support to help North Carolinians lead healthier lives.
Learn more about how YOU can make a difference too here.
Stephen N. Lang, MD
James T. Marino, MD
J. Lloyd Michener, MD
Sarah J. Olenick, MD, PhD
Steven W. Sawyer
David E. Strom, MD
Thomas G. Trautmann, MD
Daniel M. Williams, MD
L. Dale Williams, MD, FACS, RVT
There's Still Time to Complete KIPL Alumni Survey!

Our survey is still open, so if you haven't had the chance we'd love to hear your feedback!
Alumni feedback plays a crucial role in shaping the value and effectiveness of the KIPL leadership programs. Your feedback provides us with a comprehensive understanding of each program's strengths and weaknesses, highlighting areas where adjustments or enhancements may be necessary to make sure these programs remain highly relevant and valuable to you.
We have just launched our 5-year needs assessment and would like to hear from you.
TBT: Celebrating 20 years of Leadership in Medicine! Here is Sheila Stallings, MD's MEDTalk from 2021
This year the North Carolina Medical Society is celebrating 20 years of Leadership in Medicine!
Here is a Throwback Thursday to Dr. Sheila Stallings's MEDTalk from 2021. Look for a new TBT every Thursday until the 2023 LEAD Conference, October 13-14.
https://youtu.be/Mipim8oVLjI
The 2023 LEAD conference registration is NOW OPEN. Click here for more information.
Please contact Erica Hall at NCMS to organize a class table of your own.
Happy Birthday to These NCMS Members Celebrating This Month!
Grab your party hats and noise makers and let’s celebrate!
Ana R. Abaroa Salvatierra, MD
Nicole Abinanti-Kotula, MD
Srinivasan V. Adayapalam, MD
Anna M. Afonso, MD
Dina S. N. Ahmad, MD
T. Rupert Ainsley, Jr., MD, FACP
Matthew C. Alleman, MD
Robert L. Allen, MD
R. D. Almkuist, II, MD
Radhalakshmi D. Aluru, MD
Daniel E. Anderson, MD
Ruth K. Anderson, MD
W. Banks Anderson, Jr., MD
Aimee R. Andrews, MD
Lucy M. Angle, PA-C
Katherine L. Armstrong, MD
Rana A. Asfour, PA-C
Susheel V. Atree, MD
Nadir M. Attiah, MD
Leslie W. Baker, MD
Rebecca R. Bakkestuen, PA-C
Richard J. Baltaro, MD, PhD
Aaron L. Barnard, PA-C
Kristen A. Barrantes, PA-C
Samantha T. Barrett, PA
Andrew C. H. Barton, MD
Amy R. Baruch, MD
Mark B. Batts, MD
Ted A. Bauman, MD
Bethany E. Beasley, MD
Karen L. Belvin, PA-C
Mark A. Bernat, MD, JD
Alex D. Bibbey, MD
Robert H. Bilbro, MD
Gerald R. Binion, MD
Katherine C. Bishop, MD
Ganesh Bissram, MD
Thomas L. Blackstone, MD, FAAP
Stephen J. Blaha, MD
Veita J. Bland, MD
Danielle M. Bliss, MD
Stacey A. Blyth, MD
William H. Bobbitt, III, MD
Helen H. Bosse, MD
Benjamin P. Boudreaux, MD
Laura M. Bowen, MD
Alec D. Bower, DO
Deanna M. Boyette, MD
Vance W. Brabham, IV, MD
William T. Bradford, MD
George L. Bradley, Jr., DO, FAAFP
Judy Ann M. Brangman, MD
Ray M. Braquet, MD
Eric P. Brestel, MD
John G. Briggs, Jr., MD
Peter R. Bronec, MD
Adam P. Brown, MD
Daniel E. Brown, MD
Michael W. J. Brown, MD
Samantha T. Brown, PA-C
Jeffrey Browne, MD
Robert A. Brownstein, MD
Kevin F. Bruning, PA-C
Gregory M. Bugaj, MD
Mushtaq A. Bukhari, MD
Timothy P. Bukowski, MD, FACS, FAAP
Kaleigh L. Burke, MD
W. Rowell Burleson, MD
Steven J. Burnham, MD
Royce A. Burns, MD
Bret O. Burquest, MD
Victor W. Bustard, MD
Darius K. Byramji, MD
Joseph B. Callahan, MD
Nathan H. Calloway, MD
Sean T. Canale, MD, FACS
Ian L. Cannon, MD
Paul V. Caporossi, MD
Michael T. Capps, MD
Diana M. Cardona, MD
D. Spencer Carney, MD
Raymond M. Carroll, MD
Michael J. Casale, MD
Steven L. Case, MD
Deena M. Castellion, MD
Terri B. Cates, MD
Robert C. Chadderdon, MD
Moreblessings R. Chakanyuka, MD, FAAP
William P. Chalfant, MD
Donald V. Chamblee, MD
Erin E. Chaney, MD
Simon W. Chao, MD
Don C. Chaplin, MD
Stephanie A. Chase, MD
Robert C. Chen, MD
Yin J. Chen, MD
Joshua K. Cho, MD
David A. Ciaccia, DO
Jerfi D. Cicin, DO
Edgardo J. Cintron Diaz, MD
David C. Clark, Jr., MD
Richard L. Clark, MD
D. Keith Clarke, MD
Dennis M. Clemens, MD
Jonathan D. Clemente, MD
Brittany C. Clemmons, PA-C
Ashley P. Clower, MD
Yank D. Coble, Jr., MD
Neal R. Cole, PA-C
Gordon D. Coleman, MD
Karrie A. Comstock, PA-C
Yvette R. Cook, MD
William B. Corkey, MD
Jeffrey L. Coston, DO
Joshua K. Cox, MD
Bonnie Coyle Ronco, MD
Carole M. F. Craib, MD
Nicholas R. Crews, MD
John A. Crowe, Jr., MD
Pamela J. Culp, MD
Claire A. Cunniff, MD
Kathryn A. Cziraky, MD
Stephen M. Dahlstedt, MD
Thomas M. Dalton, MD
Richard T. Z. Dalyai, MD
Anthony M. Daniels, MD
James F. Davidson, IV, MD
Delina J. Davis-Cooley, PA-C
G. Scott Dean, MD
Richard H. Dean, MD
Kristopher W. Decker, PA-C
Brian S. DeLay, MD
Daniel L. DeLo, MD
Colby B. Dendy, MD
Ronald G. Dennis, MD
Alisha T. DeTroye, PA-C
Renee' R. Deweese, MD
Andrea K. Dickerson, MD
Mary A. Dooley, MD, MPH
Trevor J. Doolittle, PA
Bradford D. Drury, MD
Robert T. Duffey, MD
Robert L. Dufour, MD
James P. Dugan, MD
Eldon S. Dummit, Jr., MD
William M. Dunlap, MD
David R. Duralia, MD
Alfred D. Earwood, MD
Suzanne E. Eaton-Jones, MD
Timothy D. Edmisten, MD, FACS
Bryan T. Edwards, PA-C
Inga Edwin, MD
Dennis G. Egnatz, MD, FACOEM
Robert R. Ehinger, MD
Lisa A. Emrich, MD
Matthew A. Engelbrecht, MD
Betsy M. English, MD
Kristi L. English-Brown, MD
Silverio C. Enojado, Jr., MD
Kimberly M. Erickson, MD
Guirguis A. Eskandar, DO
Keivan Ettefagh, MD
A. Ray Evans, MD
Matthew G. Ewend, MD
Bryn A. Eyerman, PA-C
Sean M. Fahey, MD
Richard T. Falter, Jr., MD
Joseph S. Farmer, IV, PA-C
Richard W. Farnum, II, MD
Stephen L. Farris, MD
Kenneth A. Fath, MD
Justin P. Favaro, MD, PhD
Ronald A. Fazio, PA-C
Samantha L. Feldmeyer, PA
Eric K. Fitzcharles, MD
James E. Fleischli, MD
David Fleischman, MD, FACS
Lawrence M. Fleishman, MD
Bethany S. Flinchum, PA-C
Russell P. A. Ford, MD
Constance C. Foreman, MD
Leslie F. Fort-Barrie, MD
William J. Fortuner, II, MD
John T. Foster, MD
Kathleen M. Foster, MD, FACOG
David W. Frazier, MD
L. Davis Frederick, III, MD
Ronald M. Friedman, MD
Jeffrey I. Frohock, Jr., MD
Elizabeth Fuller, PA
Fred S. Gachet, Jr., MD
Roy P. Gallinger, MD
Harry A. Gallis, MD
April L. Gay, MD
Emile L. Gebel, MD
William M. Geideman, MD
Matthew J. Gerber, MD
Edward R. Gerrard, MD
Richard D. Goldner, MD
Celeste M. Good, MD
LaLonda M. Graham, MD
Lisa M. Grana, MD
Christa L. Gray, MD
Carrie L. Green, PA
John L. Green, MD
Kevin W. Greene, PA-C
Gregory T. Greenwood, MD
Robert S. Greenwood, MD, FAAP, FAAN
Robert J. Gregory, MD
Greg L. Griewe, MD
J. Laird Griffin, MD
Newton B. Griffin, MD
Nicholas E. Grivas, MD
Richard H. Gross, MD
Guy J. Guarino, MD
Ananda R. Gurram, MD
Sanford D. Guttler, MD
Michele A. Haber, MD
William E. Hall, MD
Matthew J. Hallman, MD
George W. Hamby, MD
Nancy L. Hancock, MD, MPH
Cherissa C. Hanson, MD, FAAP
John S. Hanson, MD
J. Robinson Harper, Jr., MD, FACC
Jessica B. Harrell, MD
Amy U. Harrelson, PA-C
Timothy E. Harris, MD
Angela P. Haskins, MD
Patrick R. L. Hayes, MD
Donald V. Heck, MD
Todd E. Helton, MD, PhD
Robert A. Henderson, MD
Jill L. Hendra, DO
Ryan M. Hendricker, MD
Andrew A. Hendricks, MD
Alexia M. Hernandez-Soria, MD
C. Dana Hershey, Jr., MD
Jacqueline M. Hicks, DO
James E. Hill, Jr., PA-C, MEd
Michael Hoaglin, MD
Carl W. Hoffman, MD
George A. Howard, III, MD
Eric R. Howell, MD
Duncan B. Hughes, MD
Darrin R. Hursey, MD
Charles H. Hutchins, MD
Robert P. Hutchins, MD
Aidevo S. Igbide, MD
Andrew N. Illobre, PA-C
Laura L. Jacimore, MD
James W. Jacobs, MD
Nicole Jacobs, MD
Sanjay B. Jagannath, MD
Haddy M. Jarmakani, DO
Thomas J. Jaski, MD
Sharrah E. Jenkins, MD
Courtney L. Jennings Powell, PA-C
Randall R. Joe, MD
David S. Johnson, MD, FAAP
Eric V. Johnson, MD
Matthew R. Johnson, MD
Thomas M. Johnson, MD
Scott R. Johnston, MD
Daniel B. Jones, MD
David T. Jones, MD
Kathleen R. Jones, PA-C, MPAS
Shayna D. Jones, MD
Barbara M. Jordan, MD
David A. Jordan, MD
R. Stephen Joyner, MD
Jeffrey C. Kafer, MD
Russel R. Kahmke, MD
Radhika Kalisetti, MD
Alice L. Kamil, MD
Karen A. Kartheiser, MD, FAAP
Philip D. Kath, MD
Peter J. Kauffman, PA-C, BS
Lisa G. Keeton, MD
Richard A. Keever, MD
Thomas B. Kelso, II, MD, PhD
Darin N. Kennedy, MD
Jacqueline F. Kerkow, MD
George W. Kernodle, Jr., MD, FACR, FACP
Sarah T. Kerr, PA-C
William S. Ketcham, MD
Imad Khan, DO
Parviz Khoshnevis, MD
George G. Kim, MD
Peter M. Kindschuh, MD
Walter L. King, Sr., MD
William W. King, MD
David J. Kirby, MD
Stephen M. Kirkland, MD
Margaret A. Kirkley, MD
Keith P. Kittelberger, MD
David I. Klumpar, MD
Stephen D. Knowlton, MD
Kalavathi Kolappa, MD
Gordon G. Koltis, MD
Hervy B. Kornegay, Jr., MD
Brian R. Kosobucki, MD
David C. Kowalski, MD
Micah H. Krempasky, MD
Emily S. Kuchinos, PA-C
Marshall A. Kuremsky, MD
Brian S. Kuszyk, MD, FACR
Robert Lacin, MD
William H. Lagarde, MD, FAAP
Elizabeth A. H. Lahti, MD
James R. Lakey, MD
Sanjiv S. Lakhia, DO
Jeremy R. Landvater, MD
Delano R. Lang, Jr., MD
Charles W. Lapp, MD
Michele C. Larson, MD
Tracy H. Lathrop, MD
Craig T. Lauder, DO
Linda W. Lawrence, MD
Ellen T. Lawson, MD
Frank W. Leak, MD
Michelle A. LeBlanc, MD
Kathryn E. Leet, PA-C
Eric M. LeFebvre, MD
Bruce A. Leonard, MD
Ryan T. Li, MD
Xiaohuan Li, MD
Edward G. Lilly, III, MD
David O. Lincoln, MD
Karin S. Linthicum, MD
Joseph O. Lizotte, PA
Heather A. Loesch, MD
Lloyd D. Lohr, MD
William E. Long, MD, CCD
Howard W. Loveless, Jr., MD
Jack A. Lucas, MD
Shantae L. Lucas, MD
John J. Lund, MD
Michael J. Lund, MD
Joel Lutterman, MD
Benjamin J. Lyles, MD
William W. MacDonald, MD
Yvonne Mack, MD
Ragini T. Madan, MD
Laura K. Magnuson, MD
Larry D. Mann, MD, FAAP
Mark D. Marchand, MD
Mark J. Marchese, MD
Albert W. Marr, MD
David F. Martin, MD
Kirk J. Matthews, Jr., MD
Ralph J. Maxy, MD, FAAOS
Andrea R. Mazzoni, MD
Andrew D. McBride, MD
Olivia J. McCallum, MD, FACOG
Clement L. McCaskill, DO
Mary H. McConnell, MD
Robert H. McConville, Jr., MD
Thomas M. McCutchen, Jr., MD
Shelly McElhanon, PA-C
Denis M. McGillicuddy, MD
Matthew J. McGirt, MD
Daniel McKearney, PA-C
Stephen E. McKim, MD
James W. McLane, MD
Charles A. McLaughlin, III, MD
Jonathan O. McLean, MD, FACC
Walter C. McLean, Jr., MD
Charlotte E. McManaman, MD
Michelle M. McMoon, PA-C, PhD
Elena B. McNeill, MD
John H. Meier, MD
Areg L. Mekerian, DO
Hannah I. Messer, MD
Louise D. Metz, MD
Martin B. Meyerson, MD
Jeffrey A. Michelson, MD
Paul A. Midkiff, MD
Tarra W. Millender, MD
Andrew C. Miller, II, MD
David C. Miller, MD
D. Edmond Miller, MD
John S. Miller, MD
Justin A. Miller, MD
Andrew J. Mincey, MD
Michael F. Minozzi, III, MD
Karin R. Minter, MD, MPH, FAAP
Thomas B. Mobley, III, MD
Jahan J. Mohiuddin, MD
William G. Montgomery, MD
Mary Frances Moody, MD
Joseph O. Moore, MD
Stephen C. Moore, MD
Thomas R. Moore, MD
Chris E. Morgan, MD
Mark M. J. Morris, MD
Vicki M. Morris, MD
Seth D. Morrison, MD
Sarah A. Morton, PA-C
Malana K. Moshesh, MD
H. Curtis Mostellar, III, MD
T. Scott Mouser, MD
William F. Mullis, MD
John C. Mundy, MD
Felix R. Muniz, MD
John B. Murphy, Jr., MD
Cody A. Myrick, PA-C
Luiz Nascimento, MD
Patricia K. Naslund, MD
Walter E. Neal, Jr., MD
Venkat Rama Krishna R. Neelagiri, MD
Saroj Neupane, MD
Charles J. Niemeyer, MD
J. Gray Norris, MD
Adrienne M. Novey, PA-C
Richmond K. Nuamah, MD
Robert D. O'Connor, MD
Ashley N. Oladipo, MD
H. Newland Oldham, Jr., MD
Jennifer J. Olson, MD
William G. Orrison, MD
Kaitlin C. Osbourn, PA-C
Lewis J. Overton, MD
Winifred A. Owumi, MD
Diego F. Pabon, MD
Scott P. Palmer, MD
Michael A. Papagikos, MD
Gwenevere C. Parker, MD
Delip V. Patel, MD
Pavan A. Patel, MD
Raj N. Patel, MD, MS
Roopen R. Patel, MD
Swapnesh M. Patel, MD
Dwayne E. Patterson, MD
F. M. Simmons Patterson, Jr., MD, FACC, FACP
Meryl A. Paul, MD
Larry A. Pearce, MD
Wieslawa Pekal, MD
Coryell J. Perez, MD
Jonathan D. Perry, MD
Brandon M. Peters, MD
Drew C. Peterson, MD
Frank W. Petraglia, MD
M. Jay Petruska, DO
Ashok P. Pillai, MD
Christine F. Piller, MD
Gregory T. Pleasants, MD
James F. Plowden, MD
Dana C. Point, MD
Gerald L. Points, II, MD
Sujani Poonuru, MD
Glen E. Powell, II, MD
Sanjay K. Premakumar, MD
Courtney M. Prim, PA-C
Amelia Pugh-Wilson, MD
Sonya Purushothaman, MD
Liana Puscas, MD, MHS
John V. Puthenveetil, MD
Jerald D. Pyles, MD
Robert P. Quarles, MD
Jeffrey J. Ralston, DO
Andres Ramgoolam, MD, FAAP
Lorena O. Ramos, PA-C
Anshul M. Rao, MD
Innanje R. Rao, MD, FACC
Misha Raza, PA-C
Christopher S. Reavill, MD
S. L. Record, Jr., MD
Deepa Reddy, MD
Indira Reddy, MD
Timothy J. Reeder, MD, MPH, FACEP
Donald B. Reibel, MD
Richard B. Reiling, MD, FACS
Mark H. Rescino, PA-C
Theodore B. Rheney, Jr., MD
Gaa O. Richardson, MD
George W. Riddick, Jr., MD
Clifford R. Riester, MD
Sarah J. Ro Ellis, MD
Gail M. Robinson, MD
John M. Robinson, DO
Michael D. Rodman, MD
Chantel S. Roedner, MD
Anita E. Rogers, PA-C
Garrett L. Rogers, MD
John C. Rossitch, MD
Duncan P. Rougier-Chapman, MD
Candra E. Rowell Bass, MD
Stephen H. Royal, MD, FACC
Brandon S. Rubens, MD
Tinsley W. Rucker, MD
Jerome Ruskin, MD
Walter R. Sabiston, MD
Satinder P. S. Saini, MD, FACP
Nabil P. Salameh, MD
Russell A. Salton, III, MD
Bryan M. Saltzman, MD
W. Ray Samuels, MD
Donna T. Sanders, MD
Irma M. Santiago Lago, MD
Daniel J. Sanza, PA
Madhankumar Sathyamoorthy, MD
Jay F. Saunders, MD
Michael T. Scannell, MD
Robert E. Schneider, MD
Paul O. Schricker, MD
Elizabeth J. Scott, MD
Michele L. Scott, MD
Kayla J. Scudder, PA-C
Merritt J. Seshul, MD, MBA, FACS
Andrew J. Sewalish, PA-C
James L. Seward, MD
Donald T. Shafer, MD
Daniel M. Shapiro, MD
William F. Shaw, Jr., MD
Scott B. Shawen, MD
Kirstin A. Shepperson, PA-C
Richard C. H. Shieh, MD
Shailesh C. Shirolkar, MD
Ruchi Shrestha, MD
Michael A. Sieracki, PA-C
Harold R. Silberman, MD
J. Daniel Singer, MD
H. Paul Singh, MD
Chirapa Sinthusek, MD
Lee Ann B. Skladan, MD, FAAP
Sanjeev Slehria, MD
Catherine M. Sloop, MD
John A. Smid, MD
Jane S. Smith, MD
John R. Smith, MD
John R. Smith, Jr., MD
Mark D. Smith, MD
Robert L. Smith, MD
Roger E. Smith, MD
Stephen B. Smith, MD
Brian C. Sninsky, MD
Elizabeth A. Snow, MD
John J. Soltys, MD
James D. Spivey, MD
Bryan D. Springer, MD
Robyn L. Stacy-Humphries, MD
Martin W. Stallings, MD
James E. Stanislaw, MD
Tabitha B. Staradumsky, PA
Michael J. Steger, PA
Christopher J. Steyskal, PA
Charles S. Stinson, MD
Hunter S. Stolldorf, MD
P. Gale Stone, MD
Richard J. Stork, MD
Charles W. Stout, MD
Kyle W. Strader, MD
David E. Strom, MD
Matthew L. Strupp, PA-C
Hal M. Stuart, MD
Susan D. Sturgess, MD
Leslie S. Suchar, PA
Anna N. P. Sullivan, PA-C
Robert J. Sullivan, Jr., MD, MPH
William G. Sullivan, MD
Ronald F. Sural, MD
Beth E. Susi, MD, FACP
Laddeus L. Sutton, MD, FACC
Michael F. Sweeney, MD
Charles F. Sydnor, MD
Elizabeth L. Sydnor-Jones, PA-C
Jeja B. Syeda, MD
Julia K. Taber, MD
Lori A. Tackman, MD
J. R. Tamisiea, MD
Kristopher A. Tantillo, MD
Ashley H. Tapscott, DO
David M. Tarter, MD
Chris Taylor, PA-C
Lloyd J. Taylor, PA-C
Hiromi Terawaki, MD
David N. Thies, MD
Barbara L. Thomas, MD
Jonathan G. Thomas, MD
Michael J. Thomas, MD, PhD, FACE, ECNU
Jason W. W. Thomason, MD
R. Bradley Thomason, III, MD, FACS
Amy L. Thompson, PA-C
Gwennaelle C. M. Thompson, PA-C
John A. Thompson, Jr., MD
Stephen R. Tibbels, MD
Paul J. Tobben, MD
Kaitlin M. Torres, PA-C
Steven L. Tracy, MD
Douglas R. Trocinski, MD
Kristen M. Trulear-Jackson, MD
Stephen E. Turk, MD
Melissa Turner, PA-C
Ian W. Udell, MD
Ronald VanDerNoord, MD
Jonas J. Varaly, DO
Dwan Q. Varner, MD
Sameer Vemuri, MD
Francis G. Vento, MD
Susan Vettichira, MD
Elisa P. Vicario, PA-C
Ian A. Villanueva, MD
Harold D. Wackerle, MD
Jeffrey M. Waldman, MD
Michelle D. Wall, PA-C
Terry W. Wallace, MD
John T. Ward, MD
Robert J. Ward, MD
David R. Warden, IV, MD
Harrill G. Washburn, Jr., MD
Franklin S. Watkins, MD
Brady C. Way, MD
Kenneth D. Weeks, III, MD
Bradley K. Weisner, MD
Danielle L. Wellman, MD
David M. Wells, MD
Stephen R. Wells, MD
Adam C. Wenzlik, MD
Gary V. Wertman, II, DO
Robert S. Westrol, MD
Evan N. Wheeler, DO
Clifford R. Wheeless, III, MD
Richard L. White, Jr., MD
Walter C. Whitehurst, Jr., MD
Kori B. Whitley, MD
Robert B. Whitmore, III, MD
M. Kathryn Whitten, MD
C. Phillip Whitworth, MD
William J. Wiggs, Jr., MD
Benjamin S. Wiles, DO
Randall N. Willard, MD
Elliott F. Williams, MD
Jack D. Williams, MD
Sonya E. Williams, MD
N. Alford Wilson, MD
Russell C. Wilson, MD
Jodi M. Winkel, MD
L. Dale Withers, MD
Sydnor T. Withers, Jr., MD
Sally D. Wood, MD
Paige C. Woodham, MD
Leon F. Woodruff, Jr., MD
John J. Wrenn, MD
Stephanie E. Wu, MD
Jiulong Yang, MD
Jeremy G. Yates, DO
Edward B. Yellig, MD
Peter R. Young, MD
W. Lee Young, III, MD
John Zannis, MD
Jessica Zhang, MD
Richard L. Zhang, MD
Adam J. Zolotor, DrPH, MD
June is Pride Month! NCDHHS Launches 'Take Pride Now Campaign'

The North Carolina Department of Health and Human Services is launching the Take Pride Now campaign to encourage sexual health. This campaign promotes safer sex practices, including sexually transmitted infections (STIs) prevention, testing and treatment. NCDHHS and its partners encourage North Carolinians, especially those at higher risk for STIs, to take three steps to help limit the spread:
- TAKE part in safer sex practices. These can lower the risk of exposure to STIs which are spread mostly by unprotected sexual contact.
- PRIDE yourself in prioritizing your sexual health by getting tested regularly for STIs and vaccinated against mpox (formerly known as monkeypox), if eligible.
- NOW is the time to take the first steps. If left untreated, sexually transmitted infections can lead to more health complications.
The Take Pride Now campaign is being launched in advance of Pride month in June and at a time when the U.S. is seeing a resurgence of mpox cases in other parts of the country. As people travel to and attend Pride events, it is important to be vaccinated for mpox, if eligible, and take other steps to stay healthy before, during and after these celebrations. Mpox vaccine is available across the state for people who meet any of the following criteria:
- Anyone who had close contact in the past two weeks with someone who has been diagnosed with mpox; or
- Gay, bisexual, or other men who have sex with men, or transgender individuals, who are sexually active; or
- People who have had sexual contact with gay, bisexual, or other men who have sex with men, or transgender individuals in the past 90 days; or
- People living with HIV, or taking medication to prevent HIV (PrEP), or who were diagnosed with syphilis in the past 90 days.
"Take pride in your health — If you’re at risk for mpox, now is the time to get your vaccine,” said NCDHHS Secretary Kody H. Kinsley. “Mpox vaccines are safe and effective in reducing risk of transmission and severe disease.”
North Carolina has seen 708 mpox cases through the end of April 2023. Gay, bisexual, and other men who have sex with men continue to make up most of the cases, as they have since the outbreak began in 2022. Mpox cases are higher for Black and Hispanic or Latino men. However, this group only makes up 27% of the vaccinations distributed so far in North Carolina. NCDHHS is working with all levels of government and in partnership with community organizations to decrease this disparity. Vaccination remains a crucial tool for reducing risk of transmission and disease severity.
As of April 26, 2023, 26,091 JYNNEOS vaccine doses have been administered across the state. JYNNEOS is a safe and effective mpox vaccine to reduce the risk of infection and reduce severity of disease. The vaccine requires two doses at least 28 days apart, and it takes 14 days after getting the second dose of JYNNEOS to reach maximum protection.
For the latest information on mpox and sexual health education efforts in North Carolina, including where to locate testing and mpox vaccines, visit ncdhhs.gov/TakePrideNow.
NCMS Member Honored as 2023 Doctor of the Year

In April, NCMS member Dr. Mindy Merritt was selected as the 2023 Physician of the Year in Carteret County.
The Physician of the Year award is given to a physician who consistently achieves high standards in the practice of medicine and is looked upon as a role model by his or her peers.
Merritt leads Carteret Health Care's Breast Program in the Cancer Center. Under her leadership, Carteret Health Care's Cancer earned accreditation from the National Accreditation Program for Breast Centers (NAPBC) of the American College of Surgeons, making it only one of thirteen facilities in North Carolina who currently have earned accreditation by the NAPBC.
CONGRATULATIONS, Dr. Merritt!
Extend your congratulations to in the comments.
Little-Known REM Sleep Disorder Linked to Neurodegenerative Brain Diseases

A little-known and poorly understood sleep disorder that occurs during the rapid eye movement, or REM, stage of sleep is believed to foreshadow neurodegenerative brain diseases such as Parkinson’s disease and dementia with Lewy bodies.
The disorder, known as REM sleep behavior disorder, or RBD, affects around 1% of the general population worldwide and about 2% of adults over 65.
RBD is not well understood. In some cases, a clear cause cannot be identified. In other cases, the disorder may be caused by something specific, such as obstructive sleep apnea, narcolepsy, psychiatric disorders, use of antidepressants, autoimmune disorders and brain lesions, which are areas of damaged brain tissue.
In both situations, REM sleep behavior disorder may be associated with synucleinopathies, a group of neurodegenerative disorders in which aggregates of the protein α-synuclein accumulate in brain cells. The most common of these neurodegenerative disorders is Parkinson’s disease and may be the disease's first symptom.
Read the full article here.
North Carolina Medical Board names new CEO
The North Carolina Medical Board has named Thomas W. Mansfield, JD, as its new Chief Executive Officer. Prior to accepting the position of CEO, Mansfield served as the organization’s Chief Legal Officer and has led the Legal Department since 2001. Mansfield was selected by the Board after an extensive executive search in accordance with its bylaws.
“Thom has deep knowledge and experience in medical regulation and is well positioned to make sure the North Carolina Medical Board continues to be a leader in the nation,” said Dr. Michaux Kilpatrick, NCMB President.
“It is an honor to be named as the Chief Executive of the oldest continuously operating medical board in the nation,” Mansfield said. “Medical regulation is a collaborative process, and I am committed to maintaining that collaboration for the benefit and protection of the people of North Carolina. I look forward to working with the Board members and staff to advance the mission and vision of the North Carolina Medical Board.”
Mansfield will begin his role on June 1, 2023. He will replace outgoing CEO David Henderson, JD, who announced his plans to retire in fall 2022.
In Memoriam: NCMS Lifetime Member Dr. James Jones, Sr.

NCMS Lifetime member Dr. James Grady Jones Sr., "The Country Doctor," passed away on Tuesday, May 16. He was 89.
Jones was well known across the state as an influential family physician and professor of medicine at East Carolina University with a distinguished record of service to the state. He was particularly dedicated to efforts of recruiting and training physicians to deliver care to the poor and rural communities in eastern North Carolina.
Jones was instrumental in the development of the Family Medicine program at East Carolina University's new school of medicine and served as the founding chair of the Department of Family Medicine and Associate Dean for Rural Health for two decades.
Described as a "Giant in medicine in North Carolina," Jones was known for his famous saying, " The quality of your health care should NOT be determined by your ZIP Code."
Jones joined the North Carolina Medical Society in 1961.
Read the full obituary here.
2023 Child Health Report Card: NC Failing in Areas of Youth Mental Health
The NC Child and the NC Institute of Medicine recently released the 2023 Child Health Report Card.
The report shows North Carolina earned failing grades in several key areas: mental health, school health, housing and economic security, and birth outcomes, but made progress in preconception health and maternal health support, and substance use.
Below is a snapshot of the grades in the 2023 report:
A – Insurance Coverage
B – Environmental Health; Health Services Utilization and Immunization; Preconception and Maternal Health and Support;
C – Teen Births; Breastfeeding; Oral Health;
D – Education; Healthy Eating and Active Living; School Health; Child Abuse and Neglect; Tobacco, Alcohol, and Substance Use;
F – Birth Outcomes; Mental Health; School Health; Housing and Economic Security

The authors of the report recommended several approaches to improving children’s mental health:
- Removing barriers to mental health care;
- Enhancing the availability of mental health care and crisis intervention in public schools, particularly in rural areas where specialty care is less available; and
- Making it harder for children and youth to get access to lethal means of self-harm (e.g., safe storage of firearms and prescription drugs).
View the 2023 Child Health Report Card here.
NCMS at Work: White Coat Day

On May 23, NCMS teamed up with the North Carolina Rheumatology Association (NCRA) for a White Coat Day.
There were eight physicians, fellows, and residents in attendance, and they were able to meet with six North Carolina Representatives and Senators. We discussed the SAVE Act and prior authorization.
A big thank you to everyone who attended and advocated for the health of all North Carolinians!
Interested in hosting a White Coat Day? Contact Hannah Rice to get more information, [email protected].
Early Onset of Type 2 Diabetes Linked to Dementia Risk

New data findings suggest that people who develop type 2 diabetes before age 60 years are at threefold greater risk for dementia compared to those who don't develop diabetes. The data from the prospective Atherosclerosis Risk in Communities (ARIC) cohort also suggest that the previously identified increased risk for dementia among people with prediabetes appears to be entirely explained by the subset who go on to develop type 2 diabetes.
Of the 11,656 ARIC participants without diabetes at baseline in 1990-1992 (age 46-70 years), 20.0% had prediabetes (defined as A1c 5.7%-6.4% or 39-46 mmol/mol). During a median follow-up of 15.9 years, 3143 participants developed diabetes. The proportions of patients who developed diabetes were 44.6% among those with prediabetes at baseline versus 22.5% of those without.
Dementia developed in 2247 participants over a median follow-up of 24.7 years. The cumulative incidence of dementia was 23.9% among those who developed diabetes versus 20.5% among those who did not.
This new study is the first to examine the effect of diabetes in the relationship between prediabetes and dementia, as well as the age of diabetes onset on subsequent dementia.
Read the full article here.
Study: A Little Exercise Could Reap Big Benefits

A new study looking at the exercise habits of 577,909 adults in the US found that just 10 minutes of regular aerobic exercise (or "cardio") a week can substantially cut the risk of death from flu or pneumonia.
The relative risk of dying from flu or pneumonia dropped by 21 percent on average in this 10-150 weekly minutes group, compared with those who did no exercise at all, based on 20 years of data.
Logging 150-300 and 301-600 minutes per week of moderate-to-vigorous physical activity (MVPA) was associated with 41 percent and 50 percent reductions in risk, compared with no activity at all. However, no extra benefits were seen past 600 minutes per week, suggesting a plateauing effect.
The team also looked at muscle-strengthening activity (MSA): the recommended weekly amount for this is at least two sessions per week. Taken with MVPA, those who met both targets averaged a 48 percent reduction in risk of death from flu or pneumonia, compared with those who met neither target.
Read full article here.