Mark Your Calendar for the Next DOCMS Meeting!
Join DOCMS at the University Club!
Wednesday, June 5, 2024 | 6:00pm - 8:00pm
University Club, 3100 Tower Boulevard, Suite 1700 - Durham, NC 27707
AGENDA:
- 6:00pm- 6:30pm – Socializing & Housekeeping
- 6:30pm- 7:30pm – Dinner & Guest Speaker
- 7:30pm- 7:45pm – Q&A
- 7:45pm- 8:00pm – DOCMS 2024 Business
“The Criminal Legal System, Incarceration and Health Disparities.”
Speakers:
Evan Ashkin, MD | Professor of Family Medicine UNC Chapel Hill and founder of the North Carolina Formerly Incarcerated Transition (FIT) Program
Tommy Green | FIT Program Community Health Worker
Registration link will be sent in May!
1 CME Credit is available! Click here for how to claim your credit.
DOCMS Members & Prospective Members - FREE to attend
Guests - $25 to attend (will be collected at meeting site)
NC Commission for the Blind Call for Nominees

The NCMS has an opportunity to appoint a new member to the NC Commission for the Blind. This appointment will fill an unexpired term until 6/30/25. Learn more about responsibilities of the NC Commission for the Blind here.
The commission serves in an advisory capacity on issues relating to services for persons with disabilities, especially independent living programs and services. The council also develops and submits a state plan to monitor, review and evaluate such issues and programs.
Physicians interested in the NC Commission for the Blind position should complete the application form and return it to Evan Simmons, [email protected], by Friday, May 10th. Interview Date for NC Commission for the Blind Appointment (Virtual): the evening of Tuesday, May 14th.
Calling All NCMS Physician and PA Members! Nominations Open for Leadership Positions
Want to be an NCMS leader?
Here's your opportunity to be part of our 175-year legacy!

The NCMS Nominating and Leadership Development Committee submits the following:
Call for Nominations:
- NCMS Board of Directors
- NC American Medical Association Delegation
- Nominating and Leadership Development Committee
Overview
The call for nominations for individuals to serve on the NCMS Board of Directors, NC American Medical Association Delegation, and Nominating and Leadership Development Committee are now open.
NCMS Board of Directors
- President Elect: OPEN
- Region 1 Representative: Claude Jarrett, MD (eligible for an additional term)
- At-Large Member: Jugta Kahai, MD (eligible for an additional term)
- At-Large Member: OPEN
View current NCMS Board of Directors here.
View the NCMS Board of Directors Job Description here.
NC American Medical Association Delegation
- AMA Delegate: E. Rebecca Hayes, MD (eligible for an additional term)
- AMA Delegate: Karen Smith, MD (eligible for an additional term)
- AMA Delegate: Royce Syracuse, MD (eligible for an additional term)
- AMA Delegate: OPEN
View current NC AMA Delegation here.
View the NC AMA Delegation Job Description here.
Nominating and Leadership Development Committee
NLDC Region 1: Joe Navejar, MD (eligible for an additional term)
NLDC Region 1: OPEN
NLDC Region 2: OPEN
NLDC Region 3: Labron Chambers, Jr., MD (eligible for an additional term)
NLDC Region 3: OPEN
NLDC Region 3: OPEN
NLDC Region 4: OPEN
NLDC Region 4: OPEN
NLDC Region 4: OPEN
View current NLDC members here.
View the NLDC Job Description here.
Nominations are due by May 13, 2024 (click here to view Nomination Form).
Process
Step 1: Candidates are nominated or may nominate themselves for a leadership position on the NCMS Board of Directors, NC American Medical Association Delegation, and Nominating and Leadership Development Committee (click here to view Nomination Form).
Step 2: Once a candidate submits their nomination form, they will receive an email confirmation and made aware of any follow-up if needed.
Step 3: Upon careful review of submitted materials, the Nominating and Leadership Development Committee (NLDC) will select candidates to be interviewed. Candidates will be notified via email by May 14, 2024, if they are selected for an interview. Interviews will take place via videoconference on Saturday, June 1, 2024.
Step 4: The NLDC will present the initial slate of candidates to NCMS membership on July 19, 2024, including a nomination form for Specialty Society-Component Society nominations. Specialty Society-Component Society nominations are due by August 9, 2024.
Step 5: Following any additional candidate interviews, the NLDC will select a final slate of candidates to be approved by the NCMS Board of Directors that will then be brought before the NCMS membership for a vote.
Step 6: The voting period for the elected positions will begin for all Active NCMS Members (Members who have paid 2024 dues) on October 14, 2024, and will end on October 30, 2024. Election results will be announced at the NCMS Annual Business Meeting on November 2, 2024.
All nominations and any information collected as part of the nominating process is strictly confidential.
For more information or questions about the nominating process, please contact Evan Simmons at [email protected].

NC Medicaid: Changes to the 1E-5 Obstetrical Services Policy

Coverage Policy 1E-5, Obstetrical Services has been revised with an effective date of April 1, 2024. Revisions are applicable to both NC Medicaid Managed Care and NC Medicaid Direct.
Updates include the following:
- LMP is to be recorded in Field 14 on the CMS-1500 (Professional Claim)
- CPT code 0500F (Initial Prenatal Care visit) is to be documented for the date of service when a pregnant beneficiary is seen and evaluated by an OB provider which includes an Obstetrician (OB), Certified Nurse Midwife, Nurse Practitioner or Physician’s Assistant This code is not to be used for any pregnancy confirmation visit prior to the initial assessment by the OB provider.
- If a practice or health department assumes care during a pregnancy, the initial visit with the OB provider will also be recorded with 0500F.
- CPT code 0503F (Postpartum Care Visit) is to be documented on claim line 1 at the postpartum visit. This applies to new and existing practice beneficiaries. If postpartum care is included in a global or package service, a claim may be submitted with only 0503F on claim line 1. The date of service will be the date of the first postpartum visit.
- Providers will have until July 1, 2025, to follow billing both 0500F and 0503F. After this date, claims for delivery will deny if 0500F is not in history in NCTracks. Global package claims will require 0500F on line 1 and delivery code on line 2 if not already submitted.
- Added group prenatal care, effective July 1, 2023, as an optional service that may be provided to pregnant beneficiaries. Medicaid shall pay an incentive for group prenatal care when five or more visits are attended and documented in the health record. Records of this attendance must be available to NC Medicaid Direct or the NC Medicaid Managed Care health plans upon request. For the incentive, providers will bill CPT code 99078 with modifier TH.
- Increased the allotted number of brief emotional assessments to four to align with Health Check guidelines.
Providers are encouraged to review Clinical Coverage Policy 1E-5, Obstetrical Services for a detailed overview of other general language and formatting updates to the policy. Additionally, providers can also see the Maternity Coverage and Service Reimbursement Updates bulletin for more details on other changes which were made to maternity coverage in October 2023.
Free Prostate Cancer Screening Event in Greensboro

According to Zero Prostate Cancer, North Carolina ranks 13th in the nation in incidence of prostate cancer.
Prostate cancer is a slow growing cancer that may not show symptoms in its early stages. Regular screening is important to detect the disease before it spreads.
Cone Health Cancer Center is hosting a free prostate cancer screening event on Monday, April 29th from 9 am-1 pm at Cone Health MedCenter for Women at 930 Third St., Greensboro.
The free screening open to men aged 45-69 who have not had a prostate cancer screening within the past year. The screening includes a digital rectal exam and Prostate-Specific Antigen (PSA) blood test.
Appointments can be made by calling 336-832-0849.
ALL IN: Caring For North Carolina’s Caregivers Initiative Launches to Improve Health Worker Well-being
Raleigh, N.C. (April 18, 2024) – The North Carolina Clinician and Physician Retention and Well-being (NCCPRW) Consortium today announced a new statewide initiative with the Dr. Lorna Breen Heroes’ Foundation, the only non-profit organization exclusively focused on health worker mental health and well-being. ALL IN: Caring for North Carolina’s Caregivers seeks to support the state’s hospitals and health systems in redesigning their workplace environments to help team members feel valued and supported while creating the best environments to deliver safe, quality patient care.
“This first-of-its-kind consortium has done incredible work to bring physicians, PAs, nurses and health systems together to promote well-being that goes beyond work-life balance for those who are providing care to others,” said Chip Baggett, JD, CEO of the North Carolina Medical Society. “With the launch of this initiative, we are not only acknowledging but taking action to change our system so we can improve the lives of our caregivers and ultimately health outcomes for their patients.”
Hospitals and health systems participating in the initiative commit to:
- Make a public commitment to their workforce’s well-being by eliminating local barriers to mental health care access for licensed health workers.
- Participate in a digital curriculum to enhance understanding of the drivers of burnout and successful approaches to improve well-being.
- Create and implement a 12-month action plan to accelerate systems change to operational and administrative burdens.
This initiative is being launched with a calling to North Carolina hospitals and health systems to remove one of the most substantial causes to health workers’ poor mental health and well-being – the fear of losing their credentials to work due to overly broad and invasive mental health questions on credentialing applications. These questions are stigmatizing and discriminatory, and they often cause health workers to avoid seeking the mental health care they may need. The hospitals and health systems that audit and change language on credentialing applications will be recognized as being ALL IN for prioritizing clinician well-being and be recognized as a Wellbeing First Champion.
Additionally, many state licensure boards include these stigmatizing and invasive questions around mental health in their applications, which determine whether a health worker is licensed to work in a specific state. North Carolina’s attestation model in physician licensing applications, which uses supportive language around mental health, has served as a gold standard for other states to audit and change their applications. By launching ALL IN: Caring for North Carolina’s Caregivers, North Carolina is expanding on its leadership and commitment to support the mental health and well-being of its healthcare workforce.
“By launching this initiative, we are taking an enormous leap forward to ensure North Carolina’s health workers have healthy, supportive work environments and access to the essential mental health resources they deserve,” said Corey Feist, JD, MBA, co-founder and CEO of the Dr. Lorna Breen Heroes’ Foundation. “The state of North Carolina continues to demonstrate leadership in this space and dedication to the well-being of its health workers, building on its work for physician licensing and the efforts of the NCCPRW. We encourage every hospital and health system in North Carolina to join us in this critical effort, as we strive to improve the mental health and well-being of our healthcare workforce.”
For hospitals and health systems interested in being recognized as a Wellbeing First Champion, download the Dr. Lorna Breen Heroes’ Foundation’s toolkit to remove intrusive mental health questions from credentialing applications.
About Dr. Lorna Breen Heroes’ Foundation
The Dr. Lorna Breen Heroes’ Foundation’s vision is a world where seeking mental health care is universally viewed as a sign of strength for health workers. We believe every health worker should have access to the mental health care and professional well-being support that they may need, at every moment in their career. We carry out this mission by accelerating solutions, advancing policies, and making connections that put our healthcare workforce’s well-being first. For more information, visit drlornabreen.org.
About North Carolina Clinician and Physician Retention and Well-being (NCCPRW) Consortium
The North Carolina Clinician and Physician Retention and Well-being Consortium (NCCPRW) is a collaborative initiative aimed at identifying and developing strategies to reduce stress and improve well-being among the healthcare workforce at the individual, organizational, and state level. Founded in 2016 in response to concerns raised by the North Carolina Medical Society (NCMS) regarding invasive language in licensing renewal materials, the Consortium has evolved into a proactive force advocating for the mental health and wellness of healthcare professionals. In 2024, the Consortium transitioned into a 501(c)(3) nonprofit organization to further its mission.
Identify your hospital champions and use the ALL IN Getting Started document to begin this critical work.
Share Your Thoughts on New Environmental Health Draft Policy

The North Carolina Medical Society's (NCMS) Policy Committee is charged with developing policies that align with the NCMS Mission and the NCMS Guiding Principles.
The Policy Committee recently came together to create a policy addressing environmental health. This policy will serve as an effective tool to guide and support NCMS advocacy efforts addressing environmental health in North Carolina.
The NCMS Policy Committee invites you to review the draft policy and share your feedback. The form will close on May 17th.
Feedback Wanted on Fiscal Impact of Prior Authorization

TELL US YOUR THOUGHTS ON PRIOR AUTH PRACTICES
NCMS and the North Carolina Medical Group Managers Association have partnered to create a survey on the fiscal impacts of prior authorizations on practices.
As we enter into short session at the legislature, we need to hear from YOU and your practice. Legislators in Raleigh need to be aware of the large impact this has on clinicians' ability to provide care.
Please take 5-10 minutes to fill out this survey.
The survey will close on April 26th.
New Career Opportunities Here in North Carolina

Walk in with a resume, walk out with a job
Join Cape Fear Valley on the 1st and 3rd Wednesday of every month from 9 a.m. to noon for Walk-in Wednesday. Walk in with a resume at one of their four locations and walk out with a job.
Walk-in Wednesday locations:
Cape Fear Valley Medical Center Front Lobby: 1638 Owen Drive, Fayetteville, NC 28304
Betsy Johnson Hospital: 800 Tilghman Drive, Dunn, NC 28334
Central Harnett Hospital: 215 Brightwater Drive, Lillington, NC 27546
Bladen County Hospital: 501 S Poplar St, Elizabethtown, NC 28337
To see open positions or apply now, visit http://capefearcareers.com. [source]
Register Now! Talking About Physician Suicide and "The Illusion of the Perfect Profession"

The North Carolina Medical Society Alliance is planning a free event on May 15 in Greensboro to address an important topic, physician suicide.
This event features speaker and author, Betsy Gall with a follow-up discussion from Dr. Joseph Jordan, CEO of the North Carolina Professionals Health Program (NCPHP).
Greensboro History Museum
130 Summit Ave.
Greensboro, NC 27401
May 15
6:15 pm – heavy hors d’oeuvres
7:00 pm – Program
Free admission
Download below flyer here (PDF).
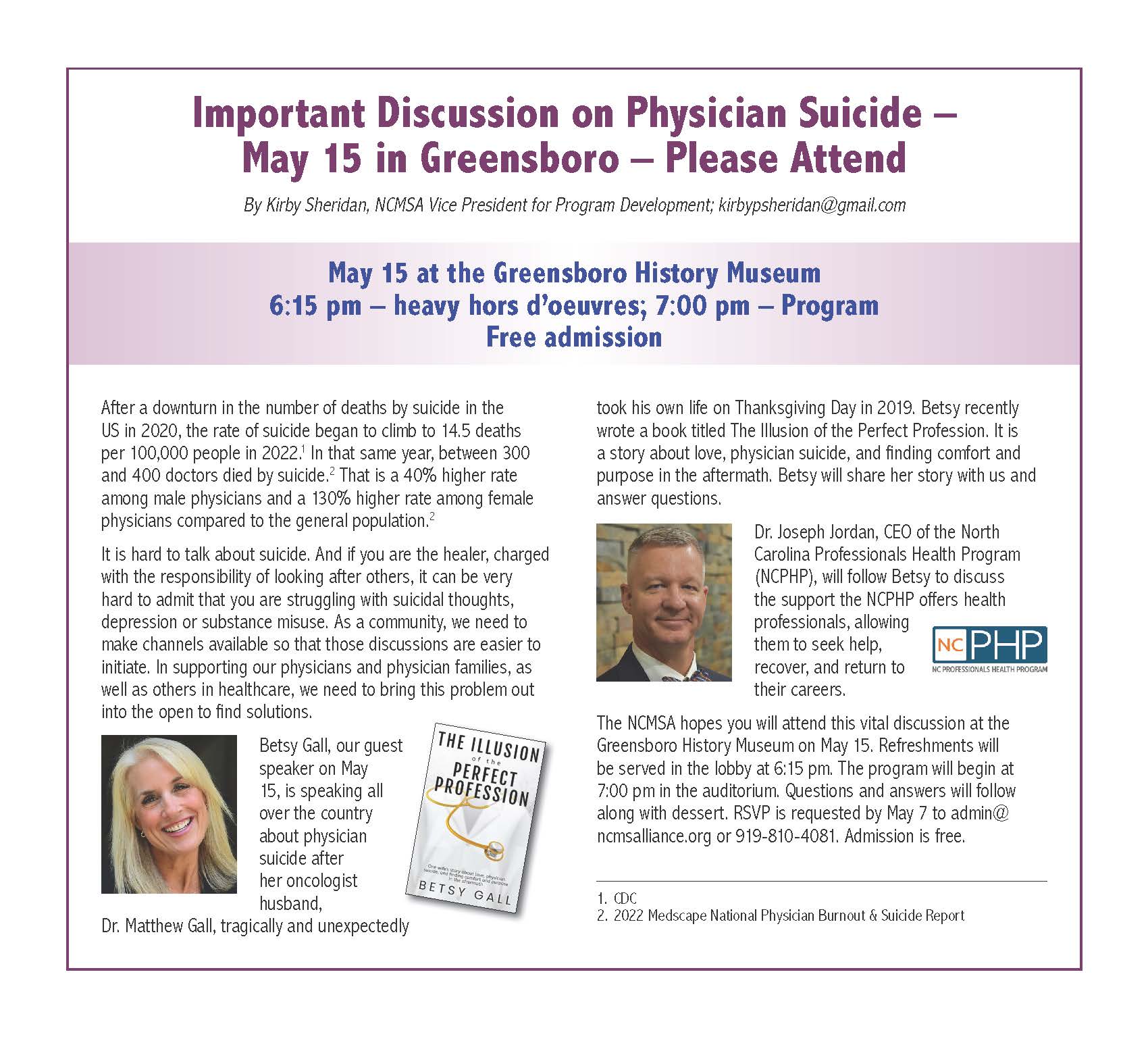
RSVP is requested by May 7 to [email protected] or 919-810-4081.
Preparing for the Possibility of Measles in NC

These days, many doctors have only seen measles in textbooks.
The CDC reports measles cases in 18 states across the country, and some doctors believe it’s only a matter of time before the illness appears in North Carolina. Now, the Orange County Health Department is preparing doctors to identify and treat an illness most of them have never seen.
“We haven’t seen an actual case in our clinics in a long time, and so we’ve lost that memory of what it looks like when a patient has it,” said Dr. Erica Pettigrew, Medical Director of the Orange County Health Department.
The Orange County Health Department is planning a measles symposium for healthcare providers in the community. The health department is also working closely with UNC Hospitals.
Continue to full article here.
NC Commission for the Blind Call for Nominees

The NCMS has an opportunity to appoint a new member to the NC Commission for the Blind. This appointment will fill an unexpired term until 6/30/25. Learn more about responsibilities of the NC Commission for the Blind here.
The commission serves in an advisory capacity on issues relating to services for persons with disabilities, especially independent living programs and services. The council also develops and submits a state plan to monitor, review and evaluate such issues and programs.
Physicians interested in the NC Commission for the Blind position should complete the application form and return it to Evan Simmons, [email protected], by Friday, May 10th. Interview Date for NC Commission for the Blind Appointment (Virtual): the evening of Tuesday, May 14th.
Register Now for Navigating Communication and De-Escalation Webinar

Navigating Communication and De-Escalation
Wednesday, May 29, 2024 • 1 - 3 p.m. • Live Webinar
Wednesday, June 12, 2024 • 1 -3 p.m. • Location: Live Webinar
Friday, May 31, 2024 • 1 - 4:15 p.m. • Location: SR-AHEC
Friday, June 21, 2024 • 1- 4:15 p.m. • Location: SR-AHEC
Today people are offended more easily and a lot less tolerant of anything that disrupts their day. In an environment that demands healthcare providers go above and beyond to keep their clients happy, today's healthcare provider must continually work to improve their communication and conflict resolution skills.
This session will explore why conflict occurs and the different types of response to the event and review tactics/strategies that can be used in the workplace to manage these intense moments that keep our team supported and safe.
Join for this interactive session with open discussion of the true challenges and practical approaches to better protect yourself (physically and psychologically) while you resolve conflict.
Download the flyer here (PDF).
Join Columbus Regional TODAY for a National Healthcare Decisions Day Event
Do you have questions about advanced directives, need to make yours, or assist a loved one in making theirs? Join Columbus Regional Healthcare System (CRHS) and Lower Cape Fear LifeCare for National Healthcare Decisions Day
We Want to Hear YOUR Prior Authorization Stories!
Are you frustrated with administrative headaches and how they impact your patients? Have you faced denials for a care plan within standard practice for a patient?
We want to hear your story!
As NCMS continues to push for passage of HB 649 in the coming legislative session, we need to hear how you and your patients have been impacted by prior authorization.
We are looking for stories from physicians to highlight and draw attention to this issue that is impacting the health of so many North Carolinians.
Please complete this quick survey so we can share your stories with legislators and tell them how Prior Authorization is negatively impacting the lives of North Carolinians!

NCMB Issues Call for Physician and PA Candidates
Applicants are needed for two physician seats, one physician assistant (PA) seat and one nurse practitioner (NP) seat on the North Carolina Medical Board for terms beginning November 1.
All positions must be filled by the process set down in statute (N.C. Gen. Stat. 90-2 and 90-3), which requires interested parties to apply via the Review Panel for the North Carolina Medical Board. The Review Panel is an independent body that nominates candidates for consideration by Governor Roy Cooper. By law, the Review Panel must nominate two candidates for each open seat.
One physician seat and both advanced practice provider seats are currently occupied by individuals who are eligible for reappointment. However, incumbents must apply for reappointment via the normal application process.
Applications will be accepted online through 4:45 p.m. on Thursday, June 27.
For more information visit this website.
The Review Panel will consider only physicians (MDs or DOs), PAs and NPs who hold active, unrestricted NC medical licenses. Applicants must be actively providing patient care at least part time and must have no history of disciplinary action within the past five years.
AMA Provides Follow-up Information & Resources on Change Healthcare Cyberattack

In follow-up to a virtual meeting held Wednesday, April 10, in conversation on the Change Healthcare cyberattack with Jon Blum, CMS’s Principal Deputy Administrator & Chief Operating Officer, and Roger Connor, Optum Insight’s Chief Executive Officer, the AMA is making the following information and resources available:
- The AMA Press Release on most recent Change Healthcare Cyberattack informal survey results is available online. The results show the ongoing, devastating impact of the Change Healthcare cyberattack, which threatens the viability of physician practices across the country, and, according to respondents, has serious implications for patient care.
- According to UnitedHealth Group (UHG), it continues to emphasize the availability of advance/accelerated payments to providers in need. Optum’s CEO emphasized that the program has more flexibility than it did originally. For more information, please visit Temporary Funding Assistance for Providers. This program is designed to help bridge the gap in short-term cash flow needs for providers impacted by the disruption of Change Healthcare's services. In particular, UHG encourages practices that find the amount prepopulated in the Optum Pay system insufficient to meet their financial needs to please contact UHG—either submit a request through the Temporary Funding Assistance Program Form or call 1-877-702-3253.
- UHG also stressed that it has no plans or timetable yet to require repayment of these funds. Until all claims submission and payment systems are back up and running, UHG is not requesting repayment. UHG indicated that a practice-level, phased approach will be used to ensure that an individual organization’s functionality has been restored before repayment is requested.
- More information about the CMS Change Healthcare/Optum Payment Disruption (CHOPD) program is available online. Physicians and other Medicare providers experiencing disruption because of the Change Healthcare outage can apply for “amounts representative of up to 30 days of Medicare claims payments.” HHS also distributed these resources (PDF) to assist physicians, pharmacists and hospitals, in the aftermath of the Change Healthcare cybersecurity attacks.
- The AMA will continue to raise issues of concern to UHG, CMS, state regulators, and other payers. Additional information from the AMA is also available on the Change Healthcare cyber outage webpage.
- If you know of a practice that is particularly struggling and needs help with UHG, please reach out to your AMA Field Representative.
Duke Health Researchers Publish Study on Hormone Modification

Duke researchers published a study on using hormone-modification technology to enable transgender women to lactate.
The report, titled “Novel Lactation Induction Protocol for a Transgender Woman Wishing to Breastfeed: A Case Report,” was published on March 27 in the National Library of Medicine. It is the fifth report ever published on lactation for a transgender woman, but is the only one that used metoclopramide for lactation induction.
Read the full article here.
Register Now for NC Medicaid Managed Care Special Webinar
Medicaid Managed Care
SPECIAL WEBINAR:
Total Cost of Care (TCOC) Dashboard Launch for Providers
This month, NC Medicaid is launching a Total Cost of Care (TCOC) Dashboard for Advanced Medical Homes (AMHs).
This tool will allow AMHs to access and analyze data related to resource use and total cost of health care received by Medicaid members assigned to their practices.
The TCOC Dashboard aims to help AMHs identify potential drivers of overuse and inefficiency and assist them in making informed decisions when engaging in value-based arrangements with Medicaid prepaid health plans.
Join for one of three opportunities to learn more about this important new tool.
In the webinar, NC Medicaid will provide an overview of the dashboard and its metrics, walk through the login process, and demonstrate various functionalities for users of the AMH TCOC Dashboard.
Wednesday, April 17 | 5-6 p.m.
Thursday, April 18 | 5-6 p.m.
Tuesday, April 30 | 11:30 a.m.-12:30 p.m.
NC Hospital System Recognized Nationally for Black Maternal Health Excellence

CHARLOTTE – Two Advocate Health hospitals have been recognized for their efforts in supporting Black maternal health by U.S. News & World Report for Black Maternal Health Week 2024. Atrium Health Pineville in Charlotte, North Carolina, and Aurora Medical Center – Grafton in Grafton, Wisconsin, are two of 26 hospitals nationwide identified by U.S. News for achieving excellent outcomes for cesarean section and unexpected newborn complications among Black patients.
U.S. News identified hospitals that were rated “high performing” in U.S. News’ Best Hospitals for Maternity Care, served at least 20 Black patients per year and had newborn complication rates of less than 2.62% and c-section rates of less than 23.9% (among hospitals providing a higher level of care) or 23.6% (among hospitals not providing a higher level of care) among Black patients.
"At Advocate Health, our commitment to advancing health equity hinges on prioritizing equity in maternal care,” said Kinneil Coltman, executive vice president and chief community and social impact officer for Advocate Health. “We're dedicated to dismantling disparities, ensuring every woman receives the quality care and support she deserves during birth and well beyond. Not only are we reducing preventable deaths, but we are on a mission to safeguard every mother's right to a safe birthing experience."
In the Southeast, Atrium Health is addressing Black maternal health disparities and mortality with an intentional recruitment of a more diverse residency class. In addition, last year Atrium Health expanded its mobile services and fleet of mobile medical units to serve its communities in need. The initiative – known as Atrium Health Women's Care Drive to Thrive – is one of the nation’s first mobile units dedicated solely dedicated to bringing OB-GYN care into underserved communities. Its goals include decreasing maternal mortality rates and unintended pregnancies.
“Our commitment to quality women’s health care – especially in our underserved communities – is an ever-expanding mission,” said Dr. Katie Borders, senior medical director for the women’s care service line, Southeast region, Atrium Health. “We are constantly striving to develop the best comprehensive women’s health program focused on equitable care for women at all life stages.”
Across sites of care in Illinois and Wisconsin, Advocate Health Care and Aurora Health Care are making huge strides in safely closing the gap in c-section rates between Black and white patients, closing the gap more than 30% over the last two years. All physicians and nurses participate in the Alliance for Maternal Health, a quality improvement initiative that shares maternal health best practices across the country. Aurora Grafton was named a top 10 hospital in the nation for overall maternity care by U.S. News this past December.
“This national recognition reaffirms the clinical excellence patients have come to expect from us,” said Dr. Ann Windsor, vice president of the women’s health service line at Advocate Health Care and Aurora Health Care. "It wouldn’t be possible without our dedicated team of OB-GYN physicians and nurses who provide high quality, individualized care to all their patients.”
Last year, 32 Advocate Health hospitals earned recognition on U.S. News & World Report’s 2023-24 “Best Hospitals” list – 30 adult hospitals plus Advocate Children’s Hospital, in Chicago, and Atrium Health Levine Children’s Hospital, in Charlotte. In addition, 15 Advocate Health hospitals were recognized by U.S. News & World Report in its annual recognition for “Best Hospitals for Maternity Care.” [source]

App Offers eRecovery Support for Substance Use Disorder

This app is not a substitute for clinical treatment, rather an additional tool that can help people connect with peers and get additional recovery supports.
Through a new partnership, the North Carolina Department of Health and Human Services (NCDHHS) is making available CHESS Health's proven eRecovery program to help thousands of North Carolinians struggling with substance use disorders to achieve long-term recovery.
CHESS Health's eRecovery program features the Connections app, a smartphone app that provides participants with immediate access to a team of certified peer recovery specialists available 24 hours a day, seven days a week. It offers moderated peer support groups, on-demand digital cognitive behavioral therapy programs and a robust set of recovery tools. This solution is offered free of charge for North Carolinians who choose to enroll through their provider and download the app, funded fully by NCDHHS.
The CHESS Health eRecovery program will be introduced in phases to more than 100 organizations across North Carolina over the next two years.
If you or someone you know is struggling or in crisis right now, help is available. Both the NCDHHS Peer Warmline and 988 are available to anyone, anytime. Call 1-855-PEERS NC (855-733-7762) or call or text 988 or chat at 988Lifeline.org. People who speak Spanish can now connect directly to Spanish-speaking crisis counselors by calling 988 and pressing option 2, texting "AYUDA" to 988, or chatting online at 988lineadevida.org or 988Lifeline.org.
Available Now! NC Dementia and Brain Health Outreach and Awareness Tool
NC DHHS has announced the availability of the North Carolina Dementia and Brain Health Toolkit. This resource is intended to increase awareness and promote education about:
- The importance of risk reduction, early diagnosis of Alzheimer’s disease and related dementias (ADRD),
- Prevention and management of chronic conditions and avoidable hospitalizations, and
- The role of caregiving for persons with dementia.
The Toolkit was developed for:
- Local public health agencies and their partners,
- Community-based organizations,
- Dementia care programs,
- Dementia-capable services within home and community-based service (HCBS) systems,
- Community health workers,
- Insurance companies,
- ADRD advocates, and
- Other professionals.
The purpose of the toolkit is to be a resource for staff, the public, older adults, adults with disabilities, and those who are caring for them about brain health and dementia.
NC DHHS and partner agencies (Division of Aging and Adult Services, and Division of Public Health), collaborated to build NC’s capacity to advance cognitive health as an integral component of public health through the North Carolina Building Our Largest Dementia Infrastructure Project (NC BOLD) by
1) Integrating cognitive health into ongoing public health efforts;
2) Implementing policy, environmental, and systems changes; and
3) Expanding the number of stakeholders engaging in collaboration and action to protect brain health.
To meet its objective, DHHS implemented selected CDC’s Healthy Brain Initiative (HBI) Road Map (RM) activities.
To access the Toolkit, click here.
NCTracks: Re-Verification Terminations Will Extend to the DMH/DD/SUS

The Affordable Care Act mandates that all Medicaid Providers must be revalidated every 5 years. This is to ensure that provider information is accurate and current. As part of this process, the provider’s credentials and qualifications will be evaluated to ensure they meet the professional requirements and are in good standing. The re-credentialing process also includes a criminal background check on all owners and managing relationships associated with the provider record.
Currently, if a provider does not complete the re-verification process, or the re-verification application is denied due to a negative background finding, failure to complete fingerprinting, bad data, or expired credentials (license/accreditation/certification per the Provider Permission Matrix), only the provider’s non-Division of Mental Health, Developmental Disabilities and Substance Use Services (DMH/DD/SUS) health plans terminate.
Effective May 19, 2024, an update to NCTracks will be made to the re-verification process. If a provider’s Medicaid health plan is terminated during the re-verification process, their DMH/DD/SUS health plans will also terminate.
Providers will be required to submit a re-enrollment application to continue to render services to NC Medicaid or State-funded beneficiaries.
More information about the re-verification process and links to training documents can be found on the Provider Re-Credentialing/Re-verification page.
New Resources Ahead of July 1st Tailored Plans Launch

Tailored Plans are a new kind of NC Medicaid Managed Care health plan for approximately 210,000 beneficiaries with a serious mental illness, a serious emotional disturbance, a severe substance use disorder, an intellectual/developmental disability or a traumatic brain injury in North Carolina. They will cover doctor visits, prescription drugs and services for mental health, substance use, I/DD and traumatic brain injury in one plan. Eligible North Carolinians who are covered by NC Medicaid Direct will be covered by a Tailored Plan beginning July 1. The name of their Medicaid plan will change but the services covered remain the same. A bilingual toolkit with accessible resources is now available for people impacted by the transition to Tailored Plans.
"Tailored Plans have the privilege and responsibility of serving North Carolinians with incredibly complex medical and behavioral needs — ensuring the plan operators are ready to support these members through this transition has been and continues to be our goal," said NC Health and Human Services Secretary Kody H. Kinsley. "Tailored Plans are another innovation to deliver on North Carolina's investments in behavioral health as foundational to whole person health."
Tailored Plans will ensure beneficiaries' needs are met regarding physical health, behavioral health and home and community-based services. Tailored Plans will also provide services that support well-being, such as food, transportation and housing.
"Tailored Plans are a step forward in improving the quality of life for people in North Carolina with serious mental illness, substance misuse, intellectual or developmental disabilities and traumatic brain injury," said Kelly Crosbie, MSW, LCSW, Director of the NCDHHS Division of Mental Health, Developmental Disabilities, and Substance Use Services. "We are working with consumers, families, providers and the Tailored Plans to ensure the community has the resources they need to understand and manage the transition into Tailored Plans more easily. We created the Tailored Plan toolkit to make this information more accessible."
The Tailored Plans toolkit was developed with input from the community and includes resources for partners and advocates to help people understand what to expect during the transition to Tailored Plans. The toolkit, which is available in English and Spanish, includes:
- New website content
- A presentation deck explaining Tailored Plans, answers to common questions and resources to help eligible beneficiaries navigate the process
- A printable flyer letting people know what actions they should take before July 1
- Social media posts highlighting important information
The NC Medicaid Enrollment Broker will mail a letter in mid-April to anyone moving to a Tailored Plan. Tailored Plan beneficiaries will need to choose a primary care provider between April 15 and May 15, 2024. If you don't choose a PCP by May 15, the Tailored Plan will assign one to you. People can change their PCP through January 31, 2025. 31, 2025.
Tailored Plans will be managed by the Local Management Entities Alliance Health, Partners Health Management, Trillium Health Resources and Vaya Health. At a legislative committee hearing last week, NC Medicaid officially announced that all Tailored Plans are ready to go live on July 1.
For more information about Tailored Plans, visit: medicaid.nc.gov/tailored-plans. To access the toolkit, visit: medicaid.nc.gov/tailored-plans/toolkit.
Registration Now Open for the Inaugural Collaborative Care Model Behavioral Health Care Manager Summit
Registration Now Open!
Inaugural Collaborative Care Model (CoCM) Behavioral Health Care Manager (BHCM) Summit
Thursday, May 16, 2024
9 am- 3:15 pm
McKimmon Center
1101 Gorman St, Raleigh, NC 27606
Register today for the inaugural Collaborative Care Model (CoCM) Behavioral Health Care Manager (BHCM) Summit, presented jointly by NC AHEC and Southern Regional AHEC.
This event will be held on Thursday, May 16 at the McKimmon Center in Raleigh.
Explore the pivotal role of BHCMs in CoCM and their significant impact. This summit will feature esteemed national and state CoCM experts, including representatives from the AIMS Center at the University of Washington, as well as state government representatives.
Attendees will benefit from insightful presentations by experienced CoCM BHCMs, integrated behavioral health Subject Matter Experts, university graduate education, and patient perspectives. Additionally, gain valuable insights from a primary care practice team that has successfully implemented CoCM in their clinic.
Download the Summit flyer here.
Don't miss out on this free training opportunity.
Calling All NCMS Physician and PA Members! Nominations Open for Leadership Positions
Want to be an NCMS leader?
Here's your opportunity to be a vital part of our 175-year legacy!

The NCMS Nominating and Leadership Development Committee submits the following:
Call for Nominations:
- NCMS Board of Directors
- NC American Medical Association Delegation
- Nominating and Leadership Development Committee
Overview
The call for nominations for individuals to serve on the NCMS Board of Directors, NC American Medical Association Delegation, and Nominating and Leadership Development Committee are now open.
NCMS Board of Directors
- President Elect: OPEN
- Region 1 Representative: Claude Jarrett, MD (eligible for an additional term)
- At-Large Member: Jugta Kahai, MD (eligible for an additional term)
- At-Large Member: OPEN
View current NCMS Board of Directors here.
View the NCMS Board of Directors Job Description here.
NC American Medical Association Delegation
- AMA Delegate: E. Rebecca Hayes, MD (eligible for an additional term)
- AMA Delegate: Karen Smith, MD (eligible for an additional term)
- AMA Delegate: Royce Syracuse, MD (eligible for an additional term)
- AMA Delegate: OPEN
View current NC AMA Delegation here.
View the NC AMA Delegation Job Description here.
Nominating and Leadership Development Committee
NLDC Region 1: Joe Navejar, MD (eligible for an additional term)
NLDC Region 1: OPEN
NLDC Region 2: OPEN
NLDC Region 3: Labron Chambers, Jr., MD (eligible for an additional term)
NLDC Region 3: OPEN
NLDC Region 3: OPEN
NLDC Region 4: OPEN
NLDC Region 4: OPEN
NLDC Region 4: OPEN
View current NLDC members here.
View the NLDC Job Description here.
Nominations are due by May 13, 2024 (click here to view Nomination Form).
Process
Step 1: Candidates are nominated or may nominate themselves for a leadership position on the NCMS Board of Directors, NC American Medical Association Delegation, and Nominating and Leadership Development Committee (click here to view Nomination Form).
Step 2: Once a candidate submits their nomination form, they will receive an email confirmation and made aware of any follow-up if needed.
Step 3: Upon careful review of submitted materials, the Nominating and Leadership Development Committee (NLDC) will select candidates to be interviewed. Candidates will be notified via email by May 14, 2024, if they are selected for an interview. Interviews will take place via videoconference on Saturday, June 1, 2024.
Step 4: The NLDC will present the initial slate of candidates to NCMS membership on July 19, 2024, including a nomination form for Specialty Society-Component Society nominations. Specialty Society-Component Society nominations are due by August 9, 2024.
Step 5: Following any additional candidate interviews, the NLDC will select a final slate of candidates to be approved by the NCMS Board of Directors that will then be brought before the NCMS membership for a vote.
Step 6: The voting period for the elected positions will begin for all Active NCMS Members (Members who have paid 2024 dues) on October 14, 2024, and will end on October 30, 2024. Election results will be announced at the NCMS Annual Business Meeting on November 2, 2024.
All nominations and any information collected as part of the nominating process is strictly confidential.
For more information or questions about the nominating process, please contact Evan Simmons at [email protected].

Are You Taking Advantage of Collaborative Care Model Training Series?
The North Carolina Department of Health and Human Services (DHHS) has partnered with NC AHEC to provide educational and practice-based support to primary care practices interested in implementing the Collaborative Care Model (CoCM) -- a team-based, interdisciplinary approach to deliver evidence-based diagnoses, treatment, and follow-up care for patients with mild to moderate behavioral health needs.
CoCM is an integrated modality that provides patients with medical and behavioral health care in a primary care setting. An increasing number of primary care settings are incorporating behavioral health services. Benefits of CoCM include better patient outcomes, improved patient and provider satisfaction, and reduction in health care costs. In addition, using CoCM may reduce health disparities in access to behavioral health. Most payors in North Carolina already cover the CoCM billing codes.
NC AHEC is offering CoCM virtual learning opportunities, including Education Modules designed for providers interested in learning about the CoCM. Currently, 15 modules are available, with additional modules being added regularly.
Modules currently available on demand include (listed in order of release date):
Module 15: Improving CoCM Quality Using Technology
Module 14: Collaborative Care in Perinatal Populations
Module 13: Diversity, Equity, and Inclusion in Collaborative Care: A Review of the Evidence in Minority Populations and Next Steps
Module 12: Collaborative Care Model in Substance Use Disorders
Module 11: Primary Care Provider Engagement
Module 10: Best Practices in Pediatric Collaborative Care
Module 9: Behavioral Health Care Manager (BHCM) Best Practices
Module 8: Best Practices for Collaborative Care Management Behavioral Health Care Manager
Module 7: Brief Therapeutic Interventions
Module 6: Billing the Codes and the General Business Model for Collaborative Care
Module 5: The Role of the Psychiatric Consultant in the Collaborative Care Model
Module 4: Collaborative Care Management for Primary Care Providers
Module 3: Putting Collaborative Care Principles into Practice: Planning for Clinical Practice Change
Module 2: Laying the Foundation for Collaborative Care Through Practice Transformation
Module 1: Collaborative Care Model (CoCM) Rationale and Evidence
View a collection of informercials to learn more about CoCM and how it’s being implemented in practices statewide!
Visit NC AHEC's Collaborative Care Model Webpage here.
Take advantage of this useful and helpful training opportunity today.
NC Health System Performs First-in-the-State Valve Replacement
For the first time in the state of North Carolina, the structural heart team at UNC Hospitals has performed a transcatheter tricuspid valve replacement in the clinical setting. The implant, which was only the 12th in the United States, is a revolutionary treatment for patients living with tricuspid valve regurgitation (TR), a common type of heart valve disease.
 (Left to Right) Thelsa Thomas Weickert, MD; Matthew A. Cavender, MD, MPH, FACC;
(Left to Right) Thelsa Thomas Weickert, MD; Matthew A. Cavender, MD, MPH, FACC;
John Vavalle, MD, MHS, FACC; and John S. Ikonomidis, MD, PhD.(image credit: UNC Health)
“We now have a percutaneous, minimally invasive way to fix tricuspid valve regurgitation and offer valve replacement without the need for open heart surgery,” said John Vavalle, MD, MHS, FACC, medical director of the Structural Heart Disease Program at UNC Hospitals and associate professor of medicine at the UNC School of Medicine. “It’s only at a place like UNC, where there is this spirit of collaboration and this desire to push the technology forward, that you can do this kind of work.”
Read the full story here.
Mark Your Calendar: 2024 Second Primary Election

To complete the state’s primary election cycle, a second primary (run-off election) will take place on May 14, 2024. The statewide ballot will include the following contests:
- Republican nomination for lieutenant governor:
- Hal Weatherman
- Jim O’Neill
- Republican nomination for state auditor:
- Jack Clark
- Dave Boliek
- Republican nomination for U.S. House District 13:
- Kelly Daughtry
- Brad Knott
County-level second primaries will also be held for
- Republican nomination for the South Point Township District on the Gaston County Board of Commissioners:
- Jim Bailey
- Ronnie Worley
- A third seat on the Orange County Schools Board of Education:
- Jennifer Moore
- Bonnie Hauser
All voters who live in the district for which a second primary is conducted and are registered with the political party of the candidates are eligible to vote in the second primary.
Unaffiliated voters who live in that district and either didn’t vote in the primary, or who voted the ballot of the party for which the second primary is being held, would also be eligible.
In counties where second primaries are held, new registration of voters is not permitted between the first and second primaries. Therefore, same-day voter registration is not available during early voting for the second primary. However, individuals who become eligible to vote between the primary and second primary and who are otherwise eligible to vote in the second primary may register and vote on the day of the second primary — May 14th.
Early voting for the May 14th second primary election begins Thursday, April 25, and ends at 3 p.m. on Saturday, May 11. Early voting sites and schedules are available on the State Board of Elections website at: Early Voting Site Search. A printable list of locations and voting hours is also available at: Early Voting Sites for the May 14, 2024 Election (PDF).
Key dates and deadlines for the 2024 second primary election in North Carolina:
- March 30, 2024: County boards of elections begin mailing absentee ballots to eligible voters who submitted an absentee ballot request form.
- April 25, 2024: In-person early voting begins.
- May 7, 2024: Absentee ballot request deadline (5 p.m.).*
- May 11, 2024: In-person early voting ends (3 p.m.).
- May 14, 2024: Election Day.
- May 14, 2024: Absentee ballot return deadline (7:30 p.m.).*
*Voter registration and absentee voting deadlines are different for military and overseas citizen voters.
Exciting Member Perk: Discount Subscription to Our State Magazine (with a bonus to NCMS!)
Get a discount on the premiere state magazine and a donation will be made to NCMS.
If you need another reason why it's good to be an NCMS member, this is it!
Click here to go to Our State Magazine. Don't forget to use promo code DSMDS
NCMS Has Retirement Solutions for You!
Are you ready to retire?
You can take advantage of all the power of the NCMS and plan for the future with our Retirement Solutions!
Caleb Sanderson talks about our new program to help YOU be ready for your next chapter.
Become a member of the North Carolina Medical Society and join thousands of your friends and colleagues.
Click here for more reasons why you should join today.
Registration Closing Soon for the 2nd Annual Smoky Mountain Primary Care Conference

2nd Annual Smoky Mountain Primary Care Conference
Kern Auditorium, Lake Junaluska Conference Center
Lake Junaluska, NC
April 27, 2024
The Smoky Mountain Medical Society is sponsoring a CME program on Saturday, April 27 at the Lake Junaluska Conference Center. This program is geared toward primary care providers and nurses in Western North Carolina, covering the topics of Diabetes & Weight Loss Medications, COPD, Anticoagulants, Adult & Pediatric Rheumatology for the Rural PCP, Urinary Incontinence and Behavioral Health: What to Do While Waiting for a Referral.
Learn more and register here.
NC Medicaid State Fiscal Year 2023 Annual Report Available Online

NC Medicaid published its State Fiscal Year Annual Report on its website at medicaid.ncdhhs.gov/reports/annual-reports-and-tables.
The public report summarizes the investments the Department has made in the health of North Carolinians and the impact of those investments.
The report highlights key investments and efforts NC Medicaid made in its programs and services as part of the Department’s commitment to whole-person care and value health outcomes for beneficiaries across the state in state fiscal year 2023 (July 1, 2022 – June 30, 2023).
Key milestones in the report include:
- North Carolina reached a historic milestone on March 27, 2023, when Governor Cooper signed HB 76 into law, expanding Medicaid coverage to more than 600,000 people across the state.
- For the tenth consecutive year, NC Medicaid ended the state fiscal year within budget, closing at $119 million under budget.
- Began unwinding the continuous Medicaid coverage provided during the federal COVID-19 Public Health Emergency. The Department began recertifying eligibility for Medicaid beneficiaries on April 1, 2023.
- Launched Tailored Care Management Dec. 1, 2022, providing beneficiaries with personalized care through a single designated care manager.
- Expanded the Healthy Opportunities Pilot to include Interpersonal Violence (IPV) services.
For additional information, contact [email protected].
2024 NCMS Candidate Series - Dr. Greg Murphy

2024 NCMS Candidate Series Featuring Dr. Greg Murphy
The 2024 North Carolina Medical Society Candidate Series has an exclusive interview featuring Dr. Greg Murphy, who is running for reelection to the third Congressional District of North Carolina.
In this episode, Dr. Murphy talks about his career as a physician in Greenville and his plans to improve access to quality healthcare across the state. He also discusses the importance of a strong healthcare system for veterans and the elderly, the fate of Medicare in the state, and Prior Authorization.
All candidates who are members of NCMS and are running for either state or federal office have been extended invitations to articulate their perspectives on these crucial subjects. Stay tuned for forthcoming interviews with other candidates leading up to the November election.
See the full interview with Dr. Murphy here:
https://youtu.be/htj0felgovw
Health System Names New Chief Physician Executive Officer for Patient Experience
 Roxie Cannon Wells, MD
Roxie Cannon Wells, MD
Winston-Salem-based Novant Health has named Roxie Cannon Wells, MD, as chief physician executive officer for patient experience.
In her new role, Dr. Wells will help steer the system's patient experience strategy, supporting both employed and independent clinicians.
According to the press release, Wells has over 25 years of healthcare experience, most recently serving as senior vice president and chief physician executive and strategy office for Novant's coastal region. She is also a past chair of the North Carolina Healthcare Association and has served on the board of trustees for the American Hospital Association.
Dermatologists Encouraged to Consider Skin Cancer, Infection Risks in Posttransplant Skin Disease

SAN DIEGO — The number of solid organ transplant survivors is on the rise, a dermatologist told colleagues, and they face unique challenges from higher risks for skin cancer and skin infections because of their suppressed immune systems.
"There are over 450,000 people with a solid organ transplant living in the United States. If you do the math, that works out to about 40 organ transplant recipients for every dermatologist, so there's a lot of them out there for us to take care of," Sean Christensen, MD, PhD, associate professor of dermatology, Yale University, New Haven, Connecticut, said at the annual meeting of the American Academy of Dermatology 2024. "If we expand that umbrella to include all types of immunosuppression, that's over 4 million adults in the US."
Christensen encouraged dermatologists to be aware of the varying risks for immunosuppressive drugs and best screening practices for these patients, and to take advantage of a validated skin cancer risk assessment tool for transplant patients.
Continue to the full article here.
Need Help? The Physician Support Line is Here for You!

Physician Support Line is a national, free, and confidential support line made up of hundreds of volunteer psychiatrists joined together in the determined hope to provide peer support for physicians and medical students.
Physician Support Line was created with the mission of physicians supporting physicians as they navigate the many professional and personal intersections of their lives.
For many, discrimination, bigotry, and intolerance towards disadvantaged and unjustly marginalized groups is an undeniable detriment to every aspect of their mental well-being. Volunteer psychiatrists at Physician Support Line are from diverse backgrounds. Physician Support Line promises to provide emotional support and a safe space for physicians and medical students who are affected by discrimination, bigotry, and intolerance.
- Free, Confidential & Anonymous
- No appointment necessary
- Call for any issue, not just a crisis
- Open Monday to Friday (except federal holidays)
Contact the national support line at 1-888-409-0141 or visit them online here.
Join Dr. Damon Tweedy for a Lively Conversation on His Latest Book Release
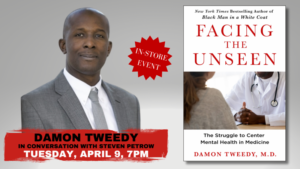
From the New York Times bestselling author of
Black Man in a White Coat
comes a powerful and urgent call to center
psychiatry and mental health care
within the mainstream of medicine
Quail Ridge Books-North Hills
4209-100 Lassiter Mill Road
Raleigh, NC 27609
Tuesday, April 9, 2024
7:00pm
ABOUT THE EVENT
Tickets include a signed copy of FACING THE UNSEEN, guaranteed entry to the event, and a seat in the reserved section. Dr. Tweedy will be in conversation with Steven Petrow. Tweedy will sign books after the program.
ABOUT THE BOOK
As much as we all might wish that mental health problems, with their elusive causes and unsettling behaviors, simply did not exist. Millions of people suffer from them, sometimes to an extreme extent. Many others face addiction to alcohol and other drugs, as overdose and suicide deaths abound. Yet the vast majority of doctors receive minimal instruction in treating these conditions during their lengthy medical training. This mismatch ignores the clear overlap between physical and mental distress, and too often puts psychiatrists on the outside looking in as the medical system continues to fail many patients.
In Facing The Unseen, bestselling author, professor of psychiatry, and practicing physician Damon Tweedy guides us through his days working in outpatient clinics, emergency rooms, and hospitals as he meets people from all walks of life who are grappling with physical and psychological illnesses. In powerful, compassionate, and eloquent prose, Tweedy argues for a more comprehensive and integrated approach where people with mental illness have a health care system that places their full well-being front and center.
ABOUT THE AUTHOR
DAMON TWEEDY, MD is a professor of psychiatry at Duke University School of Medicine and staff physician at the Durham Veteran Affairs Health System. His first book, Black Man in a White Coat, was a New York Times bestseller, selected by TIME magazine as one of the Top 10 non-fiction books of that year. He has also published articles about race, medicine, and mental health in medical journals and print publications including The New York Times and The Washington Post.
Piedmont Laureate STEVEN PETROW is an award-winning journalist and book author who is best known for his Washington Post and New York Times essays on aging, health, and civility. He’s also an opinion columnist for USA Today, where he writes about civil discourse and manners.
NCDHHS Urges Vaccination for Mpox as Cases Increase Statewide
NCDHHS Announces Statewide Increase in Mpox Cases, Urges Vaccine
The North Carolina Department of Health and Human Services is reporting a statewide increase in mpox cases. Over the past six months, 45 cases have been reported in 12 counties across North Carolina.
The national mpox outbreak began in late May 2022 and peaked from July to August 2022. A total of 703 cases were reported in North Carolina that year, and only nine cases occurred in 2023.
The mpox virus, formerly known as monkeypox, is primarily spread by prolonged close contact, typically skin-to-skin, that occurs during sexual activity. It is the associated rash, scabs or body fluid which contain the virus. Although anyone can become infected with mpox, cases have predominantly occurred among gay, bisexual or other men who have sex with men.
Fortunately, a safe and effective vaccine is available that reduces the risk of mpox infection, hospitalization and death. Those who are already fully vaccinated with two doses do not need to receive additional mpox vaccine doses.
"It is important people know how to protect themselves against mpox infection as we have seen cases increasing across North Carolina over recent months," said Dr. Erica Wilson, medical director for the medical consultation unit in the NCDHHS Division of Public Health. "The JYNNEOS vaccine is an important tool and North Carolina has an ample supply of vaccine."
Vaccines are currently free and available throughout North Carolina, regardless of immigration status. The two-dose JYNNEOS vaccine series is recommended for anyone at risk for mpox and aged 18 years and older, which includes the following:
- Anyone who has or may have multiple or anonymous sex partners; or
- Anyone whose sex partners are eligible per the criterion above; or
- People who know or suspect they have been exposed to mpox in the last 14 days; or
- Anyone else who considers themselves to be at risk for mpox through sex or other intimate contact.
The mpox vaccine locator can be used to find local vaccine providers.
Anyone who develops mpox symptoms should seek medical care. Symptoms include a rash on any part of the body, like the genitals, hands, feet, chest, face or mouth. The rash can initially look like pimples or blisters and may be painful or itchy. The rash will go through several stages, including scabs, before healing. Some people experience flu-like symptoms before the rash, while others get a rash first followed by other symptoms. In some cases, a rash is the only symptom experienced.
Other mpox symptoms can include:
- Fever
- Chills
- Swollen lymph nodes
- Exhaustion
- Muscle aches and backache
- Headache
- Respiratory symptoms (i.e. sore throat, nasal congestion or cough)
People with mpox are usually sick for about two to four weeks and can spread the virus from shortly before symptoms start until their rash is completely healed, meaning until the scabs fall off and new skin appears. Some patients may benefit from antiviral treatment, including those with severe illness or people with HIV that is not well controlled or other immune compromising conditions. Antiviral treatment may also help treat painful or severe mpox disease involving the eyes, mouth, throat, genitals and anus.
NCDHHS is working closely with local health departments and community partners to provide education about mpox, when to get tested and improve vaccine access for people at higher risk. These efforts to enhance communication, education and outreach include social media campaigns, distributing educational materials, the Mpox Equity Report, the Mpox Communications Toolkit and the Take Pride Now campaign.
More information about the virus, how to limit the risk of infection, and how to get vaccinated can be found on the North Carolina Mpox and CDC Mpox websites. [source]
BCBSNC: Additional Behavioral Health Care Services Reimbursable as Telehealth

Starting April 10, 2024, Blue Cross NC will begin reimbursing additional behavioral health inpatient and outpatient services performed via Telehealth visits according to the updated Telehealth Reimbursement Policy.
These additional behavioral health services include inpatient or outpatient daily care evaluative and/or discharge management services. Claims will still need to be billed with the appropriate place of service, procedure code and modifier combination for reimbursement.
This policy applies to Commercial, Host and Federal Employee Program (FEP). This will not apply to IPP Home or Medicare Advantage including Experience Health.
Your Feedback Needed to Improve the Medicaid Clinician Experience

NCMS's partners, Carolina Complete Health (CCH) and Carolina Complete Health Network (CCHN) will host their 2nd Annual Medicaid Managed Care Town Hall at the 2024 CPP Annual Meeting during NCMS LEAD Conference in November. In preparation for that session, we want to hear from clinicians across North Carolina who provide care to Medicaid enrollees.
Please share your experiences, challenges and successes, suggestions, and questions to help inform future programs, resources, opportunities, and collaborations that will improve health outcomes and enhance the overall care experience for Medicaid clinicians and enrollees.
All Medicaid clinicians are invited to complete this form, regardless of contract status with any of the PHPs.
Provide your feedback here.
Spring into Life Saving! Give a Little, Save a Lot!

Spring into Life Saving Blood Drive
Iredell Health System, along with The Blood Connection, is hosting a blood drive on Tuesday, April 9, which will take place from 11 a.m. – 4 p.m. at Iredell Mooresville, located at 653 Bluefield Road.
You can make a life-altering difference in your community by donating blood. Donating blood is crucial for saving lives in emergencies, surgeries, and for treating various medical conditions. It helps ensure a steady supply of blood for patients in need. You can save three local lives in less than one hour through a blood donation.
Donors need to be at least 18 years old, weigh at least 110 pounds, and be in general good health. Make sure to bring a photo ID with you to your appointment. To schedule an appointment for the Iredell Mooresville blood drive, visit donate.thebloodconnection.org/donor/schedules/sponsor_code and enter “7864.”
Each donor will receive reward points for a $50 eGift Card with numerous popular options to choose from.
The blood drive is open to the public, and appointments are recommended.
Thank you for your support during this time of such critical need.
CDC Warns of Rise in Invasive Meningococcal Disease

Healthcare Workers Should be on Alert, Even if Patient Shows No Signs
The CDC announced there has been an increase in cases of the rare “invasive meningococcal disease." According to an advisory, healthcare workers should be on alert, even if patients do not exhibit typical symptoms.
"In 2023, 422 cases were reported in the United States, the highest annual number of cases reported since 2014," the CDC said. "As of March 25, 2024, 143 cases have been reported to CDC for the current calendar year, an increase of 62 cases over the 81 reported as of this date in 2023."
The bacteria Neisseria meningitidis is what causes meningococcal disease — and according to the CDC, it can cause symptoms such as fever, nausea or vomiting, altered mental status and rapid breathing. The disease, which can reach the bloodstream, is known to “worsen rapidly” and “become life-threatening within hours.”
Read the full article here.
NCDHHS: "Fight the Bite!" Avoid Tick- and Mosquito-Borne Disease

Warm Weather Means it is Time to 'Fight the Bite'
As warmer weather approaches, the North Carolina Department of Health and Human Services is urging North Carolinians to "Fight the Bite" by taking measures to reduce their risk of tick- and mosquito-borne diseases. In 2023, almost 900 cases of tick- and mosquito-borne illnesses were reported across the state.
April is Tick and Mosquito Awareness Month, and NCDHHS is announcing the return of the Fight the Bite campaign to increase awareness about the dangers of vector-borne diseases and educate residents about measures they can take to protect themselves. Students K-12 have been invited to submit an educational poster for the annual campaign contest.
"Recent tick and mosquito surveillance show both are present in North Carolina and their bites have the potential to cause serious disease," said Alexis M. Barbarin, Ph.D., State Public Health Entomologist. "We encourage all North Carolinians to explore the outdoors safely by taking protective measures like using DEET or other EPA-approved repellants."
Rocky Mountain spotted fever, Lyme disease and other tick-borne diseases can cause fever, headache, rashes, flu-like illness and other symptoms that can be severe. Lyme disease accounted for roughly 37% of all tick-borne diseases reported last year. While not reportable conditions, Southern Tick Associate Rash Illness and Alpha-gal syndrome have also been identified in North Carolina. Alpha-gal syndrome is an allergic reaction to red (mammalian) meat that has been linked to the bite of certain ticks. Most diagnoses of tick-borne diseases are reported between June and September.
Ticks live in wooded, grassy and brushy areas, and frequenting these areas can put you in contact with ticks and increase your potential exposure to vector-borne diseases. To reduce exposure to ticks:
- Use repellent that contains DEET (or other EPA approved replicants) on exposed skin and wear clothing treated with a pesticide called permethrin. Use caution when applying to children.
- Check yourself and your children for ticks if you have been in a tick habitat and remove them promptly.
- Reduce tick habitats with selective landscaping techniques.
The mosquito-borne diseases most often acquired in North Carolina are West Nile virus, eastern equine encephalitis and La Crosse encephalitis. Nationally, North Carolina was second to only Ohio in reported cases of infections from La Crosse virus between 2003 and 2022.
Most mosquito-borne diseases reported in North Carolina are acquired while traveling outside the continental United States, including cases of malaria, dengue, chikungunya and Zika.
To reduce exposure to mosquitoes:
- Use mosquito repellent that contains DEET (or equivalent) when outside. Use caution when applying to children.
- Consider treating clothing and gear (such as boots, pants, socks and tents) with 0.5% permethrin.
- Install or repair screens on windows and doors and use air conditioning if possible.
- "Tip and Toss" — reduces mosquito breeding by emptying standing water from flowerpots, gutters, buckets, pool covers, pet water dishes, discarded tires and birdbaths at least once a week.
- Talk with your primary care provider or local health department if you plan to travel to an area where exotic mosquito-borne diseases occur.
- Always check your destination to identify appropriate prevention methods. Travel associated health risk information is available at https://wwwnc.cdc.gov/travel
The annual Fight the Bite Campaign is a poster artwork contest between NCDHHS, local health departments and K-12 schools that uses illustration to increase awareness of tick- and mosquito-borne diseases in North Carolina. Entries are due by Monday, April 8, and information regarding contest submission and deadlines can be found on the NCDHHS website. Winners of this statewide awareness poster contest will be announced at the end of April.
For more information on vector-borne diseases in North Carolina, please visit the NCDHHS Vector-Borne Diseases webpage.
It’s Official! Tailored Plans Launches July 1st.
It’s official! Tailored Plans will launch on July 1.
At a recent legislative committee hearing, NC Medicaid shared that the Local Management Entities (LMEs) that will run Tailored Plans – Alliance Health, Partners Health Management, Trillium Health Resources, and Vaya Health – are all ready to go live.
Tailored Plans include services for people with serious mental health issues, substance use issues, intellectual and developmental disabilities, and traumatic brain injury.
People with NC Medicaid Direct who receive services for these needs may be moved to a Tailored Plan. The name will change, but the services will not.
From the NCMS Archives:
NC Medicaid Tailored Plan Update
NCDHHS Delays Medicaid Managed Care Tailored Plans
New Medicaid Managed Care Tailored Plans Launch Soon
Two NC Hospitals Make Business NC's Top 20
 (image credit: Hendersonville Lightning)
(image credit: Hendersonville Lightning)
UNC Health Pardee and AdventHealth made the top 20 in the annual best hospital rankings by Business North Carolina. Pardee claimed the 12th spot, while AdventHealth ranked No. 19. Both made top 10 in patient satisfaction surveys with Pardee also winning a high ranking for two types of surgeries.
In the magazine's annual ranking of the state’s best hospitals, Duke University Hospital earned the top spot, followed by Moses Cone Hospital in Greensboro, UNC Medical Center, Duke Raleigh and UNC Rex Healthcare. Mission Hospital tied for sixth.
Read the full article here.
More States Confirm Cases of Bird Flu as it Continues Spread Across Country

Contaminated water or feed may have caused dairy cows to become infected with the H5N1 avian influenza virus.
Recently, Texas officials issued a health alert about the first confirmed case of a human infection with a bird influenza virus that has found its ways into dairy cows.
The U.S. Department of Agriculture (USDA) says it has confirmed that the virus has infected cattle at farms in Texas, Kansas, New Mexico, and Michigan, while Idaho has a “presumptive” outbreak at one dairy farm.
The USDA stressed that the “current risk to the public remains low.” Contamination of commercial milk is of “no concern,” the agency said in a statement, because pasteurization reliably kills viruses, and milk from sick cows is not being sold. The Centers for Disease Control and Prevention (CDC) says people should not drink raw milk or products like cheese that are made from it. [source]
Recommendations for Clinicians
Providers should consider the possibility of avian influenza A(H5N1) virus infection in people who have symptoms of influenza and relevant exposure history. This includes people who have had close contact with a person with suspected or confirmed avian influenza A(H5N1) infection, affected animals, or unpasteurized milk from dairy farms with suspected avian influenza A(H5N1). A close contact is defined as a person who is within 6 feet of a confirmed or probable avian influenza A(H5N1) case for a prolonged period of time, or who had direct contact with infectious secretions while the case was likely to be infectious (beginning 1 day prior to illness onset and continuing until the resolution of illness).
Symptoms of avian influenza A(H5N1) infection in humans may include:
- Fever (temperature of 100°F [37.8°C] or greater) or feeling feverish or chills
- Cough
- Sore throat
- Runny or stuffy nose
- Headaches
- Fatigue
- Eye redness (conjunctivitis)
- Difficulty breathing/shortness of breath
- Diarrhea
- Nausea
- Vomiting
- Seizures
Join NCMS for a Regional Meeting With NHPCMS in Wilmington!
New Hanover-Pender County Medical Society and North Carolina Medical Society invite you to a joint meeting!
Pine Valley Country Club
500 Pine Valley Dr.
Wilmington, NC 28412
April 10th
6-8pm
Are You Feeling More Like a Factory Line Worker Than a Health Care Professional?
Join us to learn how we are working to put YOU back in health care decision making!
Here's what you can expect:
-
-
-
-
-
-
- 6:00pm - Socializing
- 6:30pm - Complimentary dinner
- 6:45pm - NHPCMS Scholarship Presentation & Announcements
- 7:10pm - NCMS Regional Meeting with Chip Baggett, NCMS EVP-CEO
- Discussion to follow
- 8:15pm - Adjourn
-
-
-
-
-
REGISTER NOW
Physicians, PAs, Residents, and Students
You do not need to be a member to register.
Questions? Contact Toni Hill, [email protected].
Measles Remain in Spotlight as Cases Continue to Rise Nationwide

As cases of measles continue to rise, health officials continue to stress the importance of vaccinations.
As of March 28, 2024, a total of 97 measles cases have been reported by several states: Arizona, California, Florida, Georgia, Illinois, Indiana, Louisiana, Maryland, Michigan, Minnesota, Missouri, New Jersey, New York City, New York State, Ohio, Pennsylvania, Virginia, and Washington. [source]

Symptoms of measles may include fever, cough, runny nose, watery eyes and a rash of red spots. According to the CDC, approximately 1 in 5 unvaccinated people in the US who get measles will be hospitalized, approximately 1 in every 20 children will develop pneumonia, and others may develop a dangerous swelling in the brain called encephalitis. Up to 3 of every 1,000 children who become infected with measles may die from respiratory and neurologic complications.
Thanks to a highly effective vaccine, measles is preventable. Experts recommend that children get the measles, mumps and rubella, or MMR, vaccine in two doses: the first between 12 months and 15 months of age, and a second between 4 and 6 years old. One dose is about 93% effective at preventing measles infection; two doses are about 97% effective. [source]
Register Now for NC Medicaid Managed Care Special Webinar
Medicaid Managed Care
SPECIAL WEBINAR:
Total Cost of Care (TCOC) Dashboard Launch for Providers
This month, NC Medicaid is launching a Total Cost of Care (TCOC) Dashboard for Advanced Medical Homes (AMHs).
This tool will allow AMHs to access and analyze data related to resource use and total cost of health care received by Medicaid members assigned to their practices.
The TCOC Dashboard aims to help AMHs identify potential drivers of overuse and inefficiency and assist them in making informed decisions when engaging in value-based arrangements with Medicaid prepaid health plans.
Join for one of three opportunities to learn more about this important new tool.
In the webinar, NC Medicaid will provide an overview of the dashboard and its metrics, walk through the login process, and demonstrate various functionalities for users of the AMH TCOC Dashboard.