Researchers Study Link Between Vigorous Exercise, Cognition, High-Risk Hypertension Patients

People with high blood pressure have a higher risk of cognitive impairment, including dementia, but a new study from researchers at Wake Forest University School of Medicine suggests that engaging in vigorous physical activity more than once a week can lower that risk.
The findings appear online in Alzheimer’s & Dementia: The Journal of the Alzheimer’s Association.
“We know that physical exercise offers many benefits, including lowering blood pressure, improving heart health and potentially delaying cognitive decline,” said Richard Kazibwe, M.D., assistant professor of internal medicine at Wake Forest University School of Medicine and lead author of the study. “However, the amount and the intensity of exercise needed to preserve cognition is unknown.”
Learn more about the findings here.
Meet Legislators from Both Sides of the Aisle at the NCMS Legislative Reception!
Meet YOUR lawmakers at the
NCMS Legislative Reception June 12th!
On Wednesday, June 12, the North Carolina Medical Society will welcome legislators from both sides of the aisle to our 2024 NCMS Legislative Reception, including Rep. Kristin Baker, Rep. Timothy Reeder, Rep. Larry Potts, Senators Todd Johnson and Jay Chaudhuri, and many others.
The NCMS Legislative Reception has a host of legislators and staff members ready to talk with you about the issues YOU think are important. June 12th is the chance for you to be empowered and to power change. Register now for the most important advocacy event of the year.
If you want to enhance your visibility, plan to come early that morning for our White Coat Day, one of our largest gatherings of physicians and PAs to date! The NCMS is planning to flood the General Assembly with white coats to remind Senators and Representatives of the power we have to influence change.
We'd love to see you at both! View the agenda for the day, which includes breakfast, meetings with legislators, lunch with NCDHHS Secretary Kody Kinsley, and the Legislative Reception to round out the event.
$50 for members; $75 for non-members; free for students and residents.
NCMB's Call for Physician and PA Candidates Closing Soon
Applicants are needed for two physician seats, one physician assistant (PA) seat and one nurse practitioner (NP) seat on the North Carolina Medical Board for terms beginning November 1.
All positions must be filled by the process set down in statute (N.C. Gen. Stat. 90-2 and 90-3), which requires interested parties to apply via the Review Panel for the North Carolina Medical Board. The Review Panel is an independent body that nominates candidates for consideration by Governor Roy Cooper. By law, the Review Panel must nominate two candidates for each open seat.
One physician seat and both advanced practice provider seats are currently occupied by individuals who are eligible for reappointment. However, incumbents must apply for reappointment via the normal application process.
Applications will be accepted online through 4:45 p.m. on Thursday, June 27.
For more information visit this website.
The Review Panel will consider only physicians (MDs or DOs), PAs and NPs who hold active, unrestricted NC medical licenses. Applicants must be actively providing patient care at least part time and must have no history of disciplinary action within the past five years.
Don't Miss Friday's Shaping Access to Reproductive Health Care Webinar
Shaping Access to Reproductive Health Care:
Financing and Delivery Systems
June 7, 2024 | 12-1:30 p.m. ET
June 12, 2024 | 12-1:30 p.m. ET
The National Academies Standing Committee on Reproductive Health, Equity, and Society will organize a two-part public webinar series to explore the ways in which public and private financing, institutions, and systems shape access to comprehensive reproductive health care.
Part one (June 7) will focus on the coverage and limitations of public and private reproductive health care financing, the relationship between financing mechanisms and equitable access to reproductive health care, and strategies to increase access to comprehensive reproductive health care services in the United States.
Part two (June 12) will focus on the influence of public and private institutions and systems on access to and delivery of reproductive health care services.
New NC Food Program is Ensuring Your Smallest Patients Stay Fed This Summer

North Carolina will receive around $120 million in federal benefits to feed over a million school children in North Carolina this summer. The first benefits from the SUN Bucks program will begin to be issued to eligible families across the state next week.
"Summer can be a hard time for children who rely on our public schools for a healthy school breakfast and lunch," said Governor Cooper. "Nearly one in six North Carolina children face food insecurity at home and this effort helps make sure they get the nutritious food they need."
North Carolina is one of only three states in the Food and Nutrition Services Southeast Region to take advantage of the new USDA program. The purpose of SUN Bucks, also referred to as Summer EBT, is to provide food assistance to school-aged children and help bridge the financial gap for families during the summer months.
Learn more about this cross-sector collaboration here.
2024 AMPAC Campaign School Now Open for Registration
AMPAC is excited to announce that the 2024 Campaign School will be returning in-person July 25-28 at the AMA offices in Washington, DC and registration is now open!
Running an effective campaign can be the difference between winning and losing a race. That's why the Campaign School is designed to give you the skills and strategic approach you will need on the campaign trail. Our team of political experts will teach you everything you need to know to run a successful campaign. Under the direction of our lead trainers, participants will be broken into campaign staff teams to run a simulated congressional campaign using what they’ve learned during group sessions on strategy, vote targeting, social media, advertising and more.
Attendees may include physicians, spouses of physicians, residents and medical students and state medical society staff interested in becoming more involved in politics. Participants range from those attracted to grassroots efforts to those considering becoming a candidate for public office. No matter where you are in the process, you will develop a new understanding of how campaigns are run. As a graduate of the AMPAC program, candidates will rely on you to give them advice on strategy, message, and campaign plans.
Please note the following:
- The Candidate Workshop is open to AMA physician members, member spouses, residents, medical students and state medical society staff.
- Registration fee is $350 for AMA members and member spouses/$1000 for non-AMA members. This fee is waived for AMA residents and students; however, space is limited and the AMPAC Board will review and select four participants from the pool of qualified resident and student applicants.
- Faculty, materials, and all meals during the meeting are covered by the AMA. Participants are responsible for their registration fee, travel to/from Washington, DC and hotel accommodations (AMPAC staff will provide you with a list of nearby hotels within walking distance of the AMA offices).
- Participants will be required to bring a laptop or Wi-Fi enabled tablet with them.
Space is limited and the deadline to register is July 1 (or sooner if maximum capacity is reached).
Learn more about the 2024 AMPAC Campaign School and how to register here.
For additional information on the 2024 Campaign School, contact us at [email protected] or (202) 789-7455.
NCMS 2024 NCMS Photo Contest is Waiting for You!
Photo submissions are currently being accepted for 2024!
Now in its 16th year, the NCMS Photo Contest is an annual tradition that has gained national recognition, and we want you to be a part of it! Submissions are currently being accepted for the 2024 contest. Think you have the perfect picture to send in?
Check out the rules here.
We've already received several breathtaking submissions! Keep them coming!
Deadline to submit is Friday, June 14, 2024
Violence in the Healthcare Workplace

This single data point was like a punch to the gut ...
Nearly one in three medical professionals who responded to a recent North Carolina Medical Board licensee survey reported they had either witnessed or been involved in a violent incident with patients in the last year.
In this episode of MedBoard Matters, host, Jean Fisher Brinkley talks with NCMS Past President Representative Timothy Reeder, MD who was the primary sponsor of a bill, now a law, called the Hospital Violence Protection Act.
... a grim reminder of the high-stakes, high-stress environment licensees work in.
Your Feedback Needed to Improve the Medicaid Clinician Experience

NCMS's partners, Carolina Complete Health (CCH) and Carolina Complete Health Network (CCHN) will host their 2nd Annual Medicaid Managed Care Town Hall at the 2024 CPP Annual Meeting during NCMS LEAD Conference in November. In preparation for that session, we want to hear from clinicians across North Carolina who provide care to Medicaid enrollees.
Please share your experiences, challenges and successes, suggestions, and questions to help inform future programs, resources, opportunities, and collaborations that will improve health outcomes and enhance the overall care experience for Medicaid clinicians and enrollees.
All Medicaid clinicians are invited to complete this form, regardless of contract status with any of the PHPs.
Provide your feedback here.
NC Matters: Serious Mental Illness in the Perinatal Period

This online self-paced learning course will discuss best practices for supporting pregnant and postpartum patients who experience serious mental illness.
Topics reviewed will include symptomology and treatment options, along with practical strategies for primary care and obstetric providers. The intersection of serious mental illness and health equity will also be explored, considering issues such as family planning, working with historically marginalized populations, and providing care for patients who have experienced trauma.
2024 NCMS Candidate Series - Mark Hollo, PA-C

2024 NCMS Candidate Series Featuring Mark Hollo, PA-C
The 2024 North Carolina Medical Society Candidate Series has an exclusive interview with retired PA Mark Hollo, who is running for North Carolina Senate District 45.
In this episode, Hollo talks about rural access to healthcare, Medicaid expansion, Prior Authorization, and the future of healthcare in North Carolina.

All candidates who are members of NCMS and are running for either state or federal office have been extended invitations to articulate their perspectives on these crucial subjects. Stay tuned for forthcoming interviews with other candidates leading up to the November election.
See the full interview with Mr. Hollo here:
https://youtu.be/7DjJRg6GcS8
Don't Miss Wednesday's DOCMS Meeting: The Criminal Legal System, Incarceration and Health Disparities
Join DOCMS at the University Club!
Wednesday, June 5, 2024 | 6:00pm - 8:00pm
University Club, 3100 Tower Boulevard, Suite 1700 - Durham, NC 27707
AGENDA:
- 6:00pm- 6:30pm – Socializing & Housekeeping
- 6:30pm- 7:30pm – Dinner & Guest Speakers
- 7:30pm- 7:45pm – Q&A
- 7:45pm- 8:00pm – DOCMS 2024 Business
“The Criminal Legal System, Incarceration and Health Disparities.”
Speakers:
Evan Ashkin, MD | Professor of Family Medicine UNC Chapel Hill and founder of the North Carolina Formerly Incarcerated Transition (FIT) Program

Dr. Evan Ashkin is a professor of Family Medicine at the University of North Carolina at Chapel Hill. His work is focused on addressing health disparities and gaps in care for marginalized populations. Dr. Ashkin founded the North Carolina Formerly Incarcerated Transition (FIT) Program in 2017 to help address the absence of linkages to care for people released from incarceration with chronic disease, mental illness and/or substance use disorder. The FIT Program now operates in 7 counties across North Carolina. Dr Ashkin also directs the North Carolina Technical Assistance Center, supporting programs for people at risk for incarceration and overdose.
Tommy Green | FIT Program Community Health Worker
Tommy Green, hailing from Oxford, North Carolina, overcame an 11-year, 8-month sentence at 22 years old. Emerging from North Carolina's toughest prisons, he transitioned from freelance security to Assistant Operations Manager of a $20 million company. Now, as Lead Community Health Worker for NC Formerly Incarcerated Transition Program and Program Manager for Orange County Health Department, Tommy is also an Adjunct UNC Family Medicine Instructor, co-owns Success While In Transition INC, and co-directs a nonprofit called Wounded Healers. His impactful work, is featured in the Washington Post, Health Affairs, and other local media, focuses on supporting post-incarceration transition and aiding substance abuse recovery.
1 CME Credit is available! Click here for how to claim your credit.
DOCMS Members & Prospective Members - FREE to attend
Guests - $25 to attend (will be collected at meeting site)
Register Now! Shaping Access to Reproductive Health Care
Shaping Access to Reproductive Health Care:
Financing and Delivery Systems
June 7, 2024 | 12-1:30 p.m. ET
June 12, 2024 | 12-1:30 p.m. ET
The National Academies Standing Committee on Reproductive Health, Equity, and Society will organize a two-part public webinar series to explore the ways in which public and private financing, institutions, and systems shape access to comprehensive reproductive health care.
Part one (June 7) will focus on the coverage and limitations of public and private reproductive health care financing, the relationship between financing mechanisms and equitable access to reproductive health care, and strategies to increase access to comprehensive reproductive health care services in the United States.
Part two (June 12) will focus on the influence of public and private institutions and systems on access to and delivery of reproductive health care services.
Automated Tool Anticipates Hospital Disease Outbreaks

Outbreaks at hospitals are a common and costly issue—an estimated one in every 31 hospitalized patients in the US has at least one hospital-acquired infection at any given time, costing healthcare systems “billions of dollars” annually, according to the US Department of Health and Human Services.
Researchers from the CDC, Harvard Pilgrim Health Care Institute, HCA Healthcare, and the University of California, Irvine Health have developed an automated tool that can anticipate hospital disease outbreaks.
The tool can help medical professionals anticipate outbreaks of hundreds of pathogens and is meant to be an “early warning system” for hospitals, according to a CDC-funded study.
The researchers found that the tool had helped achieve a 64% reduction in the size of potential outbreaks in a pre-pandemic clinical trial (dubbed the Cluster trial) involving 82 HCA-owned hospitals across 16 states.
Find the full article here.
Happy Birthday to Our Members Celebrating This Month!
Grab your party hats and noisemakers and let’s celebrate!
Ana R. Abaroa Salvatierra, MD
Scott M. Abernathy, MD
Nicole Abinanti-Kotula, MD
Dina S. N. Ahmad, MD
T. Rupert Ainsley, Jr., MD, FACP
Reece Linden T. Alkire, DO
Alexandra A. Allaun, PA
Matthew C. Alleman, MD
R. D. Almkuist, II, MD
Hussam Alsarraf, MD, MS
Radhalakshmi D. Aluru, MD
Daniel E. Anderson, MD
Ruth K. Anderson, MD
W. Banks Anderson, Jr., MD
Aimee R. Andrews, MD
Lucy M. Angle, PA-C
Francis C. Aniekwensi, MD
Katherine L. Armstrong, MD
Gretchen S. Arnoczy, MD
Rana A. Asfour, PA-C
Susheel V. Atree, MD
Nadir M. Attiah, MD
Leslie W. Baker, MD
Richard J. Baltaro, MD, PhD
Aaron L. Barnard, PA-C
Kristen A. Barrantes, PA-C
Samantha D. Barrett, PA-C
Andrew C. H. Barton, MD
Amy R. Baruch, MD
James F. Barwick, Jr., MD
Ted A. Bauman, MD
Bethany E. Beasley, MD
Karen L. Belvin, PA-C
Mark A. Bernat, MD, JD
Alex D. Bibbey, MD
Robert H. Bilbro, MD
Gerald R. Binion, MD
Ganesh Bissram, MD
Thomas L. Blackstone, MD, FAAP
Veita J. Bland, MD
Danielle M. Bliss, MD
Amy L. Blumenthal, MD, FACOG
Stacey A. Blyth, MD
Helen H. Bosse, MD
Benjamin P. Boudreaux, MD
Laura M. Bowen, MD
Alec D. Bower, DO
Deanna M. Boyette, MD
William T. Bradford, MD
George L. Bradley, Jr., DO, FAAFP
Judy Ann M. Brangman, MD
Ray M. Braquet, MD
Eric P. Brestel, MD
John G. Briggs, Jr., MD
Peter R. Bronec, MD
Adam P. Brown, MD
Michael W. J. Brown, MD
Samantha T. Brown, PA-C
Jeffrey Browne, MD
Robert A. Brownstein, MD
Kevin F. Bruning, PA-C
Michelle R. Bucknor, MD, MBA
Mushtaq A. Bukhari, MD
Timothy P. Bukowski, MD, FACS, FAAP
Kaleigh L. Burke, MD
W. Rowell Burleson, MD
Steven J. Burnham, MD
Royce A. Burns, MD
Victor W. Bustard, MD
Darius K. Byramji, MD
Joseph B. Callahan, MD
Nathan H. Calloway, MD
Sean T. Canale, MD, FACS
Ian L. Cannon, MD
Paul V. Caporossi, MD
D. Spencer Carney, MD
Raymond M. Carroll, MD
Michael J. Casale, MD
Steven L. Case, MD
Robert C. Chadderdon, MD
Moreblessings R. Chakanyuka, MD, FAAP
William P. Chalfant, MD
Donald V. Chamblee, MD
Erin E. Chaney, MD
Simon W. Chao, MD
Don C. Chaplin, MD
Stephanie A. Chase, MD
Yin J. Chen, MD
Anika S. Cherry, MD
Joshua K. Cho, MD
David A. Ciaccia, DO
Jason M. Ciapponi, PA-C
Jerfi D. Cicin, DO
Edgardo J. Cintron Diaz, MD
David C. Clark, Jr., MD
Richard L. Clark, MD
D. Keith Clarke, MD
Dennis M. Clemens, MD
Jonathan D. Clemente, MD
Brittany C. Clemmons, PA-C
Ashley P. Clower, MD
Yank D. Coble, Jr., MD
Neal R. Cole, PA-C
Gordon D. Coleman, MD
Karrie A. Comstock, PA-C
Charles A. Cook, MD
William B. Corkey, MD
Jeffrey L. Coston, DO
Joshua K. Cox, MD
Nicholas R. Crews, MD
Pamela J. Culp, MD
Claire A. Cunniff, MD
Kathryn A. Cziraky, MD
Stephen M. Dahlstedt, MD
Thomas M. Dalton, MD
Richard T. Z. Dalyai, MD
Anthony M. Daniels, MD
Joanna M. Dauber, DO
James F. Davidson, IV, MD
Delina J. Davis-Cooley, PA-C
Richard H. Dean, MD
Kristopher W. Decker, PA-C
Brian S. DeLay, MD
Daniel L. DeLo, MD
Colby B. Dendy, MD
T. Craig Derian, MD
Alisha T. DeTroye, PA-C
Andrea K. Dickerson, MD
Sarah A. Djali, PA-C
Patricia C. Doerr, MD
Mary A. Dooley, MD, MPH
Trevor J. Doolittle, PA-C
Bradford D. Drury, MD
Robert T. Duffey, MD
Robert L. Dufour, MD
James P. Dugan, MD
Eldon S. Dummit, Jr., MD
William M. Dunlap, MD
David R. Duralia, MD
Suzanne E. Eaton-Jones, MD
Bryan T. Edwards, PA-C
Inga Edwin, MD
Dennis G. Egnatz, MD, FACOEM
Robert R. Ehinger, MD
Lisa A. Emrich, MD
Matthew A. Engelbrecht, MD
Betsy M. English, MD
Kristi L. English-Brown, MD
Silverio C. Enojado, Jr., MD
Kimberly M. Erickson, MD
Guirguis A. Eskandar, DO
Keivan Ettefagh, MD
A. Ray Evans, MD
Matthew G. Ewend, MD
Joseph S. Farmer, IV, PA-C
Richard W. Farnum, II, MD
Stephen L. Farris, MD
Kenneth A. Fath, MD
Justin P. Favaro, MD, PhD
Michael Favorito, MD
Ronald A. Fazio, PA-C
Samantha L. Feldmeyer, PA-C
Eric K. Fitzcharles, MD
James E. Fleischli, MD
David Fleischman, MD, FACS
Lawrence M. Fleishman, MD
Bethany S. Flinchum, PA-C
Russell P. A. Ford, MD
Constance C. Foreman, MD
Leslie F. Fort-Barrie, MD
John T. Foster, MD
Kathleen M. Foster, MD, FACOG
Hannah E. Fratantuono, PA-C
David W. Frazier, MD
L. Davis Frederick, III, MD
Ronald M. Friedman, MD
Jeffrey I. Frohock, Jr., MD
Elizabeth Fuller, PA
Joel L. Gallagher, MD
Roy P. Gallinger, MD
Harry A. Gallis, MD
Lee Ann Garner, MD
April L. Gay, MD
Emile L. Gebel, MD
William M. Geideman, MD
Matthew J. Gerber, MD
Edward R. Gerrard, MD
Richard D. Goldner, MD
Ishwar H. Gopichand, MD
LaLonda M. Graham, MD
Lisa M. Grana, MD
Deborah G. Grant, PA-C
Christa L. Gray, MD
Carrie L. Green, PA-C
John L. Green, MD
Kevin W. Greene, PA-C
Gregory T. Greenwood, MD
Robert S. Greenwood, MD, FAAP, FAAN
Greg L. Griewe, MD
Davida J. Griffin, PA-C
J. Laird Griffin, MD
Nicholas E. Grivas, MD
Richard H. Gross, MD
Guy J. Guarino, MD
Ananda R. Gurram, MD
Sanford D. Guttler, MD
Michele A. Haber, MD
William E. Hall, MD
Matthew J. Hallman, MD
George W. Hamby, MD
Nancy L. Hancock, MD, MPH
Cherissa C. Hanson, MD, FAAP
John S. Hanson, MD
J. Robinson Harper, Jr., MD, FACC
Jessica B. Harrell, MD
Amy U. Harrelson, PA-C
Timothy E. Harris, MD
Patrick R. L. Hayes, MD
Donald V. Heck, MD
Todd E. Helton, MD, PhD
Robert A. Henderson, MD
Jill L. Hendra, DO
Ryan M. Hendricker, MD
Andrew A. Hendricks, MD
Alexia M. Hernandez-Soria, MD
C. Dana Hershey, Jr., MD
Jacqueline M. Hicks, DO
Sean T. Hicks, PA-C
James E. Hill, Jr., PA-C, MEd
Kristina A. Hines, DO
Carl W. Hoffman, MD
George A. Howard, III, MD
Eric R. Howell, MD
Duncan B. Hughes, MD
Darrin R. Hursey, MD
Charles H. Hutchins, MD
Robert P. Hutchins, MD
Aidevo S. Igbide, MD
Andrew N. Illobre, PA-C
Taylor T. Irvin, PA
Matthew Isaacs, MD
Mark G. Jablonski, MD
Laura L. Jacimore, MD
James W. Jacobs, MD
Nicole Jacobs, MD
Sanjay B. Jagannath, MD
Haddy M. Jarmakani, DO
Thomas J. Jaski, MD
Sharrah E. Jenkins, MD
Jisha John, MD
Dakota C. Johnson, MD
David S. Johnson, MD, FAAP
Eric V. Johnson, MD
Thomas M. Johnson, MD
Scott R. Johnston, MD
Daniel B. Jones, MD
David T. Jones, MD
Shayna D. Jones, MD
Barbara M. Jordan, MD
R. Stephen Joyner, MD
Jeffrey C. Kafer, MD
Russel R. Kahmke, MD
Radhika Kalisetti, MD
Alice L. Kamil, MD
Karen A. Kartheiser, MD, FAAP
Philip D. Kath, MD
Peter J. Kauffman, PA-C, BS
Lisa G. Keeton, MD
Thomas B. Kelso, II, MD, PhD
Darin N. Kennedy, MD
Jacqueline F. Kerkow, MD
George W. Kernodle, Jr., MD, FACR, FACP
Sarah T. Kerr, PA-C
Imad Khan, DO
Parviz Khoshnevis, MD
George G. Kim, MD
Peter M. Kindschuh, MD
Walter L. King, Sr., MD
William W. King, MD
David J. Kirby, MD
Stephen M. Kirkland, MD
Margaret A. Kirkley, MD
Keith P. Kittelberger, MD
David I. Klumpar, MD
Stephen D. Knowlton, MD
Kalavathi Kolappa, MD
Gordon G. Koltis, MD
Meghana Konanur, MD
Hervy B. Kornegay, Jr., MD
Brian R. Kosobucki, MD
David C. Kowalski, MD
Micah H. Krempasky, MD
Emily S. Kuchinos, PA-C
Marshall A. Kuremsky, MD
Brian S. Kuszyk, MD, FACR
Robert Lacin, MD
William H. Lagarde, MD, FAAP
Elizabeth A. H. Lahti, MD
James R. Lakey, MD
Sanjiv S. Lakhia, DO
Jeremy R. Landvater, MD
Delano R. Lang, Jr., MD
Charles W. Lapp, MD
Tracy H. Lathrop, MD
Craig T. Lauder, DO
Linda W. Lawrence, MD
Ellen T. Lawson, MD
Kathryn E. Leet, PA-C
Eric M. LeFebvre, MD
Bruce A. Leonard, MD
Ryan T. Li, MD
Xiaohuan Li, MD
Edward G. Lilly, III, MD
David O. Lincoln, MD
Karin S. Linthicum, MD
Joseph O. Lizotte, PA
Heather A. Loesch, MD
Lloyd D. Lohr, MD
William E. Long, MD, CCD
Justin P. Loucks, PA-C
Barbara A. Lowry, MD
Shantae L. Lucas, MD
John J. Lund, MD
Michael J. Lund, MD
Joel Lutterman, MD
Benjamin J. Lyles, MD
William W. MacDonald, MD
Yvonne Mack, MD
Ragini T. Madan, MD
Michael J. Maggitti, MD
Laura K. Magnuson, MD
Larry D. Mann, MD, FAAP
Mark D. Marchand, MD
Mark J. Marchese, MD
Albert W. Marr, MD
David F. Martin, MD
Kirk J. Matthews, Jr., MD
Ralph J. Maxy, MD, FAAOS
Andrea R. Mazzoni, MD
Andrew D. McBride, MD
Olivia J. McCallum, MD, FACOG
Clement L. McCaskill, DO
Mary H. McConnell, MD
Robert H. McConville, Jr., MD
Thomas M. McCutchen, Jr., MD
Shelly McElhanon, PA-C
Denis M. McGillicuddy, MD
Matthew J. McGirt, MD
Daniel McKearney, PA-C
Stephen E. McKim, MD
Charles A. McLaughlin, III, MD
Jonathan O. McLean, MD, FACC
Walter C. McLean, Jr., MD
Michelle M. McMoon, PA-C, PhD
Elena B. McNeill, MD
John H. Meier, MD
Hannah I. Messer, MD
Louise D. Metz, MD
Martin B. Meyerson, MD
Jeffrey A. Michelson, MD
Paul A. Midkiff, MD
Tarra W. Millender, MD
Andrew C. Miller, II, MD
David C. Miller, MD
D. Edmond Miller, MD
Justin A. Miller, MD
Andrew J. Mincey, MD
Michael F. Minozzi, III, MD
Karin R. Minter, MD, MPH, FAAP
Thomas B. Mobley, III, MD
Jahan J. Mohiuddin, MD
Mary Frances Moody, MD
Joseph O. Moore, MD
Stephen C. Moore, MD
Joseph C. Moran, MD
Chris E. Morgan, MD
Vicki M. Morris, MD
Sarah A. Morton, PA-C
Malana K. Moshesh, MD
T. Scott Mouser, MD
William F. Mullis, MD
John C. Mundy, MD
Felix R. Muniz, MD
John B. Murphy, Jr., MD
Cody A. Myrick, PA-C
Luiz Nascimento, MD
Patricia K. Naslund, MD
Walter E. Neal, Jr., MD
Venkat Rama Krishna R. Neelagiri, MD
Saroj Neupane, MD
Charles J. Niemeyer, MD
Douglas A. Nigbor, MD
J. Gray Norris, MD
Adrienne M. Novey, PA-C
Richmond K. Nuamah, MD
Ashley N. Oladipo, MD
H. Newland Oldham, Jr., MD
William G. Orrison, MD
Kaitlin C. Osbourn, PA-C
Lewis J. Overton, MD
Winifred A. Owumi, MD
Michael A. Papagikos, MD
Gwenevere C. Parker, MD
Delip V. Patel, MD
Ketan A. Patel, MD
Pavan A. Patel, MD
Raj N. Patel, MD, MS
Roopen R. Patel, MD
Swapnesh M. Patel, MD
Dwayne E. Patterson, MD
F. M. Simmons Patterson, Jr., MD, FACC, FACP
Meryl A. Paul, MD
Larry A. Pearce, MD
Coryell J. Perez, MD
Jonathan D. Perry, MD
Brandon M. Peters, MD
Drew C. Peterson, MD
Frank W. Petraglia, MD
Ashok P. Pillai, MD
Christine F. Piller, MD
Gregory T. Pleasants, MD
James F. Plowden, MD
Dana C. Point, MD
Gerald L. Points, II, MD
Sujani Poonuru, MD
Glen E. Powell, II, MD
Sanjay K. Premakumar, MD
Courtney M. Prim, PA-C
Amelia Pugh-Wilson, MD
Liana Puscas, MD, MHS
Dominic S. Putala, DO
John V. Puthenveetil, MD
Jerald D. Pyles, MD
Robert P. Quarles, MD
Jeffrey J. Ralston, DO
Lorena O. Ramos, PA-C
Anshul M. Rao, MD
Innanje R. Rao, MD, FACC
Misha Raza, PA-C
Christopher S. Reavill, MD
S. L. Record, Jr., MD
Deepa Reddy, MD
Indira Reddy, MD
Timothy J. Reeder, MD, MPH, FACEP
Donald B. Reibel, MD
Richard B. Reiling, MD, FACS
Robert A. Renjel, MD
Mark H. Rescino, PA-C
Bradley H. Restel, MD
Theodore B. Rheney, Jr., MD
Alleen D. Richards, MD
Gaa O. Richardson, MD
George W. Riddick, Jr., MD
William A. Rieck, Jr., DO
Clifford R. Riester, MD
Sarah J. Ro Ellis, MD
Gail M. Robinson, MD
John M. Robinson, DO
Michael D. Rodman, MD
Chantel S. Roedner, MD
Corianne D. Rogers, MD
Garrett L. Rogers, MD
John C. Rossitch, MD
Duncan P. Rougier-Chapman, MD
Stephen H. Royal, MD, FACC
Brandon S. Rubens, MD
Tinsley W. Rucker, MD
Katherine M. Ruiz González, MD
Jerome Ruskin, MD
Walter R. Sabiston, MD
Satinder P. S. Saini, MD, FACP
Russell A. Salton, III, MD
Bryan M. Saltzman, MD
W. Ray Samuels, MD
Daniel J. Sanza, PA-C
Jay F. Saunders, MD
Michael T. Scannell, MD
Yolanda V. Scarlett, MD
Priscille Schettini, MD
Robert E. Schneider, MD
Elizabeth J. Scott, MD
Michele L. Scott, MD
Kayla J. Scudder, PA-C
Soma Sengupta, MD
Andrew J. Sewalish, PA-C
James L. Seward, MD
Donald T. Shafer, MD
Meera U. Shah, PA-C, MSPAS
Daniel M. Shapiro, MD
Scott B. Shawen, MD
Kirstin A. Shepperson, PA-C
Shailesh C. Shirolkar, MD
Ruchi Shrestha, MD
Ethan Shroll, MD
Michael A. Sieracki, PA-C
Harold R. Silberman, MD
H. Paul Singh, MD
Chirapa Sinthusek, MD
Lee Ann B. Skladan, MD, FAAP
Sanjeev Slehria, MD
Catherine M. Sloop, MD
John A. Smid, MD
Jane S. Smith, MD
John R. Smith, Jr., MD
Mark D. Smith, MD
Robert L. Smith, MD
Roger E. Smith, MD
Stephen B. Smith, MD
Brian C. Sninsky, MD
Elizabeth A. Snow, MD
John J. Soltys, MD
Peeter A. Soosaar, MD
Margaret K. Sparks, MD
James D. Spivey, MD
Bryan D. Springer, MD
Robyn L. Stacy-Humphries, MD
James E. Stanislaw, MD
Tabitha B. Staradumsky, PA
Michael J. Steger, PA
Hunter S. Stolldorf, MD
P. Gale Stone, MD
Charles W. Stout, MD
Kyle W. Strader, MD
David E. Strom, MD
Matthew L. Strupp, PA-C
Dennis O. Stuart, MD
Leslie S. Suchar, PA
Anna N. P. Sullivan, PA-C
Robert J. Sullivan, Jr., MD, MPH
William G. Sullivan, MD
Ronald F. Sural, MD
Beth E. Susi, MD, FACP
Laddeus L. Sutton, MD, FACC
Michael F. Sweeney, MD
Charles F. Sydnor, MD
Jeja B. Syeda, MD
Julia K. Taber, MD
Lori A. Tackman, MD
J. R. Tamisiea, MD
Kristopher A. Tantillo, MD
Ashley H. Tapscott, DO
David M. Tarter, MD
Lloyd J. Taylor, PA-C
Zachary R. Taylor, MD
Bala Gangadhara R. Thatigotla, MD
Jonathan G. Thomas, MD
Michael J. Thomas, MD, PhD, FACE, ECNU
Jason W. W. Thomason, MD
R. Bradley Thomason, III, MD, FACS
Amy L. Thompson, PA-C
Gwennaelle C. M. Thompson, PA-C
John A. Thompson, Jr., MD
Stephen R. Tibbels, MD
Paul J. Tobben, MD
Kaitlin M. Torres, PA-C
Steven L. Tracy, MD
Douglas R. Trocinski, MD
Kristen M. Trulear-Jackson, MD
Bair E. Tsytsik, MD
Donna M. Tuccero, MD
John W. Tucker, PA-C
Melissa Turner, PA-C
Ronald VanDerNoord, MD
Jonas J. Varaly, DO
Dwan Q. Varner, MD
Sameer Vemuri, MD
Susan Vettichira, MD
Ian A. Villanueva, MD
Harold D. Wackerle, MD
Jeffrey M. Waldman, MD
Michelle D. Wall, PA-C
Terry W. Wallace, MD
John T. Ward, MD
Robert J. Ward, MD
David R. Warden, IV, MD
Harrill G. Washburn, Jr., MD
Brady C. Way, MD
Kenneth D. Weeks, III, MD
Bradley K. Weisner, MD
Danielle L. Wellman, MD
David M. Wells, MD
Stephen R. Wells, MD
Adam C. Wenzlik, MD
Gary V. Wertman, II, DO
Robert S. Westrol, MD
Evan N. Wheeler, DO
Clifford R. Wheeless, III, MD
Richard L. White, Jr., MD
C. Phillip Whitworth, MD
William J. Wiggs, Jr., MD
Benjamin S. Wiles, DO
Randall N. Willard, MD
Elliott F. Williams, MD
Jack D. Williams, MD
Kasey L. Williams, PA-C
Kayla M. Williams, MD
Sonya E. Williams, MD
N. Alford Wilson, MD
Russell C. Wilson, MD
Jodi M. Winkel, MD
L. Dale Withers, MD
Sydnor T. Withers, Jr., MD
Brian S. Wood, MD
Sally D. Wood, MD
Brandon K. Woodard, MD
Paige C. Woodham, MD
Leon F. Woodruff, Jr., MD
John J. Wrenn, MD
Stephanie E. Wu, MD
Jeremy G. Yates, DO
Edward B. Yellig, MD
Peter R. Young, MD
W. Lee Young, III, MD
John Zannis, MD
Jessica Zhang, MD
Richard L. Zhang, MD
Adam J. Zolotor, DrPH, MD
Carolina Complete Health Institutes High Dollar Pre-Payment Review for Inpatient Claims
Effective August 1, 2024, Carolina Complete Health will institute high dollar pre-payment review requirements for hospital inpatient claims with a header or total billed amount greater than $250k.
Beginning August 1, 2024, any hospital inpatient claim billed to Carolina Complete Health greater than $250k will be subject to a pre-payment review.
What to expect:
- Proactive submission of itemized bill: For any hospital inpatient claim greater than $250k, please include an itemized bill along with the claim submission.
- If an itemized bill is not included with the original claim, it will cause delay and/or partial payment.
If you have questions, please contact your Provider Engagement Administrator. If you need your Provider Engagement Administrator's contact information, please email [email protected]
It's Heating Up Outside! Operation Fan Heat Relief Can Help Your Patients Stay Cool!

The North Carolina Department of Health and Human Services’ Division of Aging is partnering with the N.C. area agencies on aging and local service providers to distribute fans to eligible recipients through Operation Fan Heat Relief from May 1–Oct. 31.
People 60 and older, as well as adults with disabilities, are eligible to sign up for assistance from May 1–Oct. 31 at local aging agencies across the state. Since 1986, the relief program has purchased fans for older adults and adults with disabilities, providing them with a more comfortable living environment and reducing heat-related illnesses.
The program is made possible by donations from Duke Energy Carolinas, Duke Energy Progress, Dominion and Valassis. Operation Fan Heat Relief allows regional area agencies on aging and local provider agencies to purchase fans for eligible individuals. Local provider agencies can also purchase a limited number of air conditioners based on a person’s specific health conditions.
Last year, the division received $86,000 in donations, allowing for the distribution of 3,097 fans and 21 air conditioners.
As individuals age and develop chronic medical conditions, they are less likely to sense and respond to changes in temperature, and they may also be taking medications that can worsen the impact of extreme heat. Operation Fan Heat Relief helps vulnerable adults at risk for heat-related illnesses stay safe during the summer.
In addition to applying for fans, people age 60 and older, as well as adults with disabilities, can take the following steps during high temperatures:
- Increase fluid intake
- Spend time in cool or air-conditioned environments regularly
- Reduce strenuous activity during the afternoon
- Speak with their physician before summer about how to stay safe while taking medication that can affect the body's ability to cool itself (e.g., high blood pressure medications)
For more details, individuals may contact their area agency on aging or the Division of Aging at 919-855-3400.
More information about Operation Fan and Heat Relief, including tips on preparing for extreme heat and a list of local agencies distributing fans, is available at www.ncdhhs.gov/divisions/aging/operation-fan-heat-relief.
New Findings Suggest Introducing Peanuts in Infancy Prevents Peanut Allergy into Adolescence

New findings from a study sponsored and co-funded by the National Institutes of Health’s National Institute of Allergy and Infectious Diseases (NIAID), provide conclusive evidence that achieving long-term prevention of peanut allergy is possible through early allergen consumption. The results were published in the journal NEJM Evidence.
Feeding children peanut products regularly from infancy to age 5 years reduced the rate of peanut allergy in adolescence by 71%, even when the children ate or avoided peanut products as desired for many years.
“Today’s findings should reinforce parents’ and caregivers’ confidence that feeding their young children peanut products beginning in infancy according to established guidelines can provide lasting protection from peanut allergy,” said NIAID Director Jeanne Marrazzo, M.D., M.P.H. “If widely implemented, this safe, simple strategy could prevent tens of thousands of cases of peanut allergy among the 3.6 million children born in the United States each year.”
Read more on these findings here.
CMS Adds MIPS EUC Hardship Option

Due to the ongoing efforts by the AMA, CMS has added an option to cite the cyberattack when requesting the 2024 Merit-based Incentive Payment System (MIPS) Extreme and Uncontrollable Circumstances (EUC) hardship exception.
To account for the increased number of physicians that have been impacted by a cyberattack this year, CMS has specifically added a drop-down tab in the application to indicate the EUC is due to the Change cyberattack. When in the EUC portal, physicians should select the event type as “ransom/malware”. Once a physician clicks on the event type “ransom/malware” a drop-down box will appear asking whether the event pertains to the Change Healthcare Cyberattack. Reference page 8 in the 2024 MIPS EUC Application User Guide for more details. The 2024 MIPS EUC portal is now open, and physicians have until December 31, 2024, to file a hardship application and avoid a 2026 MIPS negative payment adjustment.
When applying for a hardship, physicians have the option to request reweighting of up to four MIPS categories. Reweighting of all performance categories will result in avoiding a MIPS penalty of up to -9 percent in 2026. As a reminder, if a physician or group submits data, it will override the hardship exception and the physician or group may be scored.
Don't Miss AMA's Medicare Physician Payment Mid-Year Update

Register now for this Advocacy Insights webinar on June 4 at Noon CT to hear about the latest AMA efforts on Medicare physician payment reform: what’s happening on Capitol Hill, how the AMA’s grassroots campaign is raising the volume, and what to expect on the regulatory side—particularly as the proposed rule for the 2025 Medicare physician fee schedule is expected later this summer.
Speakers include:
- Margaret Garikes, vice president, Federal Affairs, AMA
- Rob Jordan, vice president, Political Affairs, AMA
- Jason Marino, director, Congressional Affairs, AMA
Moderated by Jesse M. Ehrenfeld, MD, MPH, president, American Medical Association
Mark Your Calendar! Substance Use Disorder Medication Assisted Treatment and Recovery Event
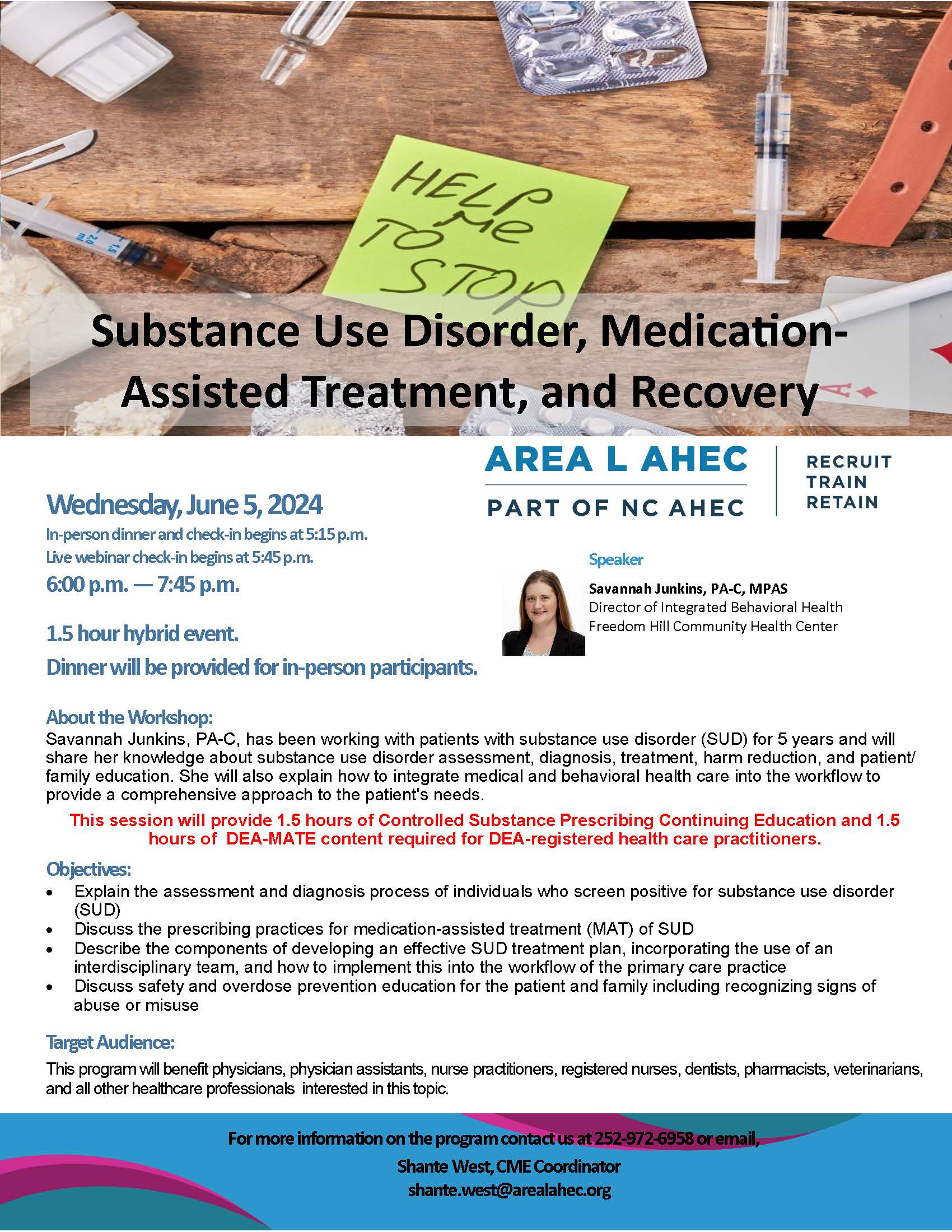
Download the full-version pdf with registration information here.
COVID Vaccine Program for Uninsured Ending Soon

A federal program providing free COVID-19 vaccines to uninsured and underinsured adults is shutting down this summer, before the fall rollout of updated vaccines to fight against the latest variants.
The Centers for Disease Control and Prevention (CDC) said its Bridge Access Program will end in August because of a lack of funding. The program has provided more than 1.4 million free COVID-19 vaccines since it launched in September 2023 at a cost of more than $1 billion.
Continue to the full article here.
Don't Miss June's Lunch & Learn Webinar: Navigating the Healthcare Workforce

June Lunch & Learn Webinar
Navigating the Healthcare Workforce:
Insights into Employee Turnover and Retention Trends
Tuesday, June 18 | 12:00 PM - 1:00 PM EDT | Zoom
Dive deep into the heart of healthcare operations with our illuminating session, “Navigating the Healthcare Workforce: Insights into Employee Turnover and Retention Trends.” In today’s ever-evolving healthcare landscape, the ability to decipher the nuanced patterns of employee turnover and retention is not just advantageous; it’s essential for organizational longevity and the delivery of exceptional patient care. This session is your gateway to the latest data-driven insights and emerging trends that are reshaping the dynamics of the healthcare workforce.
Delve into the intricacies of turnover analysis, uncovering the pivotal drivers behind employee departures. But we don’t stop there. We’ll guide you through a landscape of innovative retention strategies, equipping you with actionable knowledge to fortify your workforce and foster a culture of resilience and engagement within your healthcare institution.
From identifying key pain points to implementing best practices, this session promises to empower you with the tools and strategies necessary to thrive in the competitive realm of healthcare staffing. Don’t miss out on this opportunity to elevate your workforce management skills and drive sustainable success in healthcare delivery.

Registration
This webinar is free, but you must be registered to attend. Space is limited so register early! After you register, you will receive an emailed confirmation with webinar and phone-in instructions. Please check your spam/junk folder if you do not see the confirmation email after you register.
Questions
Please contact the NCMGMA offices at [email protected].
Continuing education credit may be granted through your professional organization (MGMA, PAHCOM, AHIMA, etc.). Please self-submit for these organizations.
BSBSNC Foundation Announces Funding Opportunity for Youth Mental and Behavioral Health

Blue Cross and Blue Shield of North Carolina Foundation is issuing a funding opportunity to expand access to youth mental and behavioral health services supporting near-term opportunities which leverage a trained workforce that goes beyond specialty trained clinical and professional roles and which provides initial support and connection to resources that can assist youth in getting the support they need.
Grants ranging from $75,000 to $500,000 per year for up to three years will support models that are effective in the short-term (1-3 years) in supporting better access to care and resources for youth navigating mental and behavioral health challenges, as well as increasing accessibility to services that can lead to greater prevention and earlier intervention.
Learn more about this opportunity here.
Discuss Vaping Prevention and Support for NC Youth at NCDHHS Live Fireside Chat and Tele-town Hall

The North Carolina Department of Health and Human Services will host a live fireside chat and tele-town hall, TODAY, Wednesday, May 29, from 6 to 7 p.m., to discuss vaping prevention and resources for youth in North Carolina as well as ways parents and caregivers can support their families.
Event participants below include state and local experts on vaping prevention and support, as well as a parent with firsthand experience of how devastating the consequences of youth vaping can be:
- Shayla Hayes, Youth Engagement Coordinator, Tobacco Prevention and Control Branch, Division of Public Health, NCDHHS
- Ray Riordan, Director of Local Policy and Programs, Tobacco Prevention and Control Branch, Division of Public Health, NCDHHS
- Tricia Howard, MSN, MHA, PMHNP-BC, Lead Nurse, Durham Public Schools
- Charlene Zorn, Parent Advocate and Solomon’s Stepmom
E-cigarettes — also known as vapes — are the most commonly used tobacco product among middle and high school students in the United States. More than two million students currently use vapes and one in four of these students vape every day. However, most middle and high school students who vape want to quit and have tried to quit.
Fireside chat and tele-town hall panelists will discuss the following:
- Signs a child or teen may be vaping and how to help
- Ways parents and caregivers can talk to youth about vaping
- How to find health information, care and providers for youth
- Resources to help prevent youth from vaping or help them quit
It’s important to talk to kids about vaping early, even before they are teens, as most tobacco use starts during youth. Resources are available across the state to help parents and caregivers navigate conversations with youth about vaping, access vaping prevention tips and guidance, and find support for their family if a young person is vaping.
The fireside chat will stream live from the NCDHHS Facebook, Twitter (X) and YouTube accounts, where viewers can submit questions. The event also includes a tele-town hall, which invites people by phone to listen in and submit questions. People can also dial into the event by calling 855-756-7520 Ext. #106458.
The North Carolina Department of Health and Human Services will host a live Spanish-language Cafecito and tele-town hall on Thursday, May 30, from 6 to 7 p.m. Get the details here.
Upcoming Webinar Highlights the Crucial Role of a Diverse Workforce in Achieving Health Equity

Diversifying the Health Center Workforce: Elevating Cultural Humility & Equitable Care
Wednesday, June 5 | 3:00 pm
Connect with the Association of Clinicians for the Underserved (ACU) STAR² Center, the Migrant Clinicians Network (MCN) and The National LGBTQIA+ Health Education Center for a collaborative two-part webinar highlighting the crucial role of a diverse workforce in achieving health equity.
The first session will focus on how to integrate principles of Justice, Equity, Diversity, and Inclusion (JEDI) into recruitment and retention efforts within a healthcare setting. The second session will shine a light on the specific needs and challenges faced by migrant populations and LGBTQIA+ communities.
Don't miss this opportunity to learn strategies for building diverse, culturally humble healthcare teams that are essential for advancing health equity across diverse communities.
New Coronavirus Variant Becomes Dominant Strain in US.
According to Centers for Disease Control and Prevention (CDC), a new coronavirus variant, KP.2, a member of the so-called FliRT variants, has become the dominant coronavirus strain in the United States. While FliRT variants have certain mutations in common, they are still part of the Omicron family of the coronavirus.
There are many questions surrounding this new variant:
- What should people know about this new variant?
- What are the symptoms of infection?
- Do vaccines still work against the new strain?
- Is a home test still reliable?
- How long should people isolate if they contract KP.2?
- Who should take antiviral treatments if they contract this type of Covid-19?
- And what is the guidance for immunocompromised individuals — should they start masking again?
Get the answers to these concerns here.
Meningococcal Disease Cases Linked to International Travel
The Centers for Disease Control and Prevention (CDC) recently issued a Health Alert Network Health Advisory to alert clinicians to cases of meningococcal disease linked to travel to the Kingdom of Saudi Arabia (KSA). Since April 2024, 12 cases of meningococcal disease linked to KSA travel: United States (5 cases), France (4 cases), and the United Kingdom (3 cases).
Recommendations for Healthcare Clinicians
- Recommend vaccination with MenACWY conjugate vaccine for people considering travel to KSA to perform Hajj or Umrah (pilgrims) in addition to routine meningococcal vaccination for adolescents and other people at increased meningococcal disease risk
- Maintain a heightened index of suspicion for meningococcal disease among symptomatic people who have recently been in KSA and among close contacts of people who have recently been in KSA, regardless of vaccination status
- Immediately notify state, tribal, local, or territorial health departments about any suspected or confirmed cases of meningococcal disease in the United States
- Preferentially consider using rifampin, ceftriaxone, or azithromycin instead of ciprofloxacin as prophylaxis for close contacts in the United States of meningococcal disease cases associated with travel in KSA
Got a Minute? Respond to the Maternal and Child Health Survey

On behalf of the North Carolina Title V Program, you are invited to respond to this survey as part of the 2025 Title V Needs Assessment, a requirement of the Maternal and Child Health (MCH) Block Grant application and a critical element of the MCH program planning process for the NC Department of Health and Human Services.
The mission of the NC Title V Maternal and Child Health (MCH) Block Grant Program is to support and promote the health and well-being of NC individuals including mothers, infants, children, youth, and their families to reduce inequities and improve outcomes.
The findings of the assessment are used to identify priorities and to guide resource allocation and program planning within the following five MCH domains, acknowledging that many issues are cross-cutting or related:
- Women/Maternal Health
- Perinatal/Infant Health
- Child Health
- Adolescent Health
- Children with Special Health Care Needs
Please take a moment to complete this quick survey. We also welcome you to share this survey opportunity with your patients.
Thank you for your time.
A Spanish-version of the survey is available here.
Federal Trade Commission Announces Webinar on Noncompete Rule

On May 31, 2024, at 1:00 PM ET, the FTC will host an online overview of the final rule banning noncompetes, focused on healthcare.
Chair Lina Khan will kick off the session before turning it over to the Office of Policy Planning. The briefing will include a summary of the rule with a focus on healthcare and time for answering questions submitted in advance using the email address provided below. The briefing is free and expected to last 30 minutes.
The FTC invites you to submit questions in advance by email at [email protected]. In the subject line, please include “Healthcare Briefing”.
If you are interested in attending, please register in advance using this link. After registering, you will receive a confirmation email containing information about joining the webinar.
Resources, guides, and multi-language model notices are available on the Noncompete Rule page at www.ftc.gov/noncompetes.
NCMS at Work for You: AI Regulations and Healthcare Outreach

During the May meetings of the North Carolina Medical Board (NCMB), a range of pressing issues in healthcare regulation were discussed, with a particular focus on the integration of artificial intelligence (AI) and outreach initiatives.
NCMS staff attended these meetings. Below is an outline of what was discussed:
Navigating AI in Healthcare
The Policy Committee delved into the complexities surrounding the incorporation of AI technologies in medical practice, spurred by the introduction and discussion of a report from the Federation of State Medical Boards (FSMB). Emphasizing the need for proactive regulation, the FSMB underscored NCMB's obligation to develop clear guidelines for the ethical and effective utilization of AI. Despite the rapid evolution of AI technology, the committee stressed the importance of upholding professional standards and patient safety, irrespective of technological advancements.
Recognizing the absence of established benchmarks in this rapidly evolving field, the committee grappled with the challenge of creating novel guidelines tailored to AI implementation. Drawing parallels to the approach taken with telemedicine, the committee proposed a broad yet adaptable policy framework, echoing the sentiment that informed consent, transparency, and accountability are paramount in AI utilization. Dr. Jan Rhyne's presentation shed light on the multifaceted applications of AI in healthcare, from predictive analytics to clinical documentation, prompting discussions on delineating the responsibilities of physicians and AI systems.
The board is not currently drafting a policy but doing more research and having more discussion on this topic.
Regulatory Updates and Outreach Efforts
In addition to AI regulation, the Policy Committee addressed various regulatory updates and outreach initiatives aimed at engaging diverse stakeholders in healthcare. Revisions to policies regarding conflicts in healthcare settings, licensee use of innovative treatments, and contact protocols before prescribing were approved, reflecting the committee's commitment to adaptability and responsiveness.
The Outreach Committee highlighted efforts to enhance public engagement and educational outreach. From presentations to medical societies to the exploration of mobile phone application feasibility, the committee is actively seeking innovative avenues to connect with communities and disseminate vital healthcare information.
Looking Ahead
As the landscape of healthcare continues to evolve, the NCMB remains dedicated to navigating complex regulatory challenges while prioritizing patient care and safety. With AI regulation and outreach initiatives at the forefront of its agenda, the NCMB Policy Committee is poised to drive meaningful change in North Carolina's healthcare landscape, fostering innovation, inclusivity, and excellence in medical practice.
Expansion of 'Right To Try' Law Passes NC Senate committee

State lawmakers want to expand North Carolina's "Right To Try" law that allows some patients to try experimental drugs or medical treatments.
The legislature passed the first "Right To Try" law in 2015. It allows doctors to provide some medications and treatments that aren't approved by the Federal Drug Administration. Only patients with terminal or life-threatening conditions are eligible.
A bill that passed its first Senate committee vote Wednesday would expand the law to new genomic and genetic treatments.
"These are treatments that are still in research and experimental phases," said Sen. Benton Sawrey, R-Johnston, the bill's sponsor. "So they have not gone through some of the necessary trials. There's an example of a medication to treat a rare brain disorder that's been approved in Europe since 2020. Patients are currently leaving the United States to go to Europe to receive that genetic treatment and then coming back here."
The bill would not require insurance to cover any of the experimental treatments, and the producer of the drug or treatment wouldn't be legally responsible if the patient dies. No one spoke against the bill. (source)
Local Health System Performs Landmark Heart Valve Surgery
 (image credit: Atrium Health)
(image credit: Atrium Health)
Minimally invasive procedure promises faster recovery and alternative to open-heart surgery
CHARLOTTE, N.C. – Atrium Health Sanger Heart & Vascular Institute has successfully completed the first commercial tricuspid clip procedure in the Carolinas, performed in May at Atrium Health Carolinas Medical Center. This achievement marks a significant milestone in the treatment of tricuspid regurgitation (TR), offering new hope to patients who are not candidates for traditional open-heart surgery.
Tricuspid regurgitation is a condition where the tricuspid valve, located between the right atrium and right ventricle of the heart, fails to close properly, allowing blood to flow backward. This can lead to symptoms such as severe shortness of breath, swelling in the legs and abdomen and a significant reduction in quality of life. Until recently, treatment options for TR were limited to medical management or high-risk open-heart surgery.
"This is an exciting day for our team and our patients," said Dr. Michael Rinaldi, an interventional cardiologist and the medical director of the structural heart program at Atrium Health Sanger Heart & Vascular Institute. "We have been eagerly anticipating the opportunity to bring this innovative technology to our community. The tricuspid clip offers a life-changing option for patients who previously had limited treatment choices.”
The tricuspid clip procedure is a minimally invasive technique designed to address this condition. Performed through a catheter inserted into the vein, the device is guided to the heart using advanced imaging technologies. Once in place, the clip grasps and pulls the leaflets of the tricuspid valve together, reducing the regurgitation and significantly improving the patient's symptoms and quality of life.
Rinaldi and Dr. Markus Scherer, director of cardiac CT and structural heart imaging at Atrium Health Sanger Heart & Vascular Institute, along with a team of cardiac imaging experts, successfully guided the tricuspid clip into place using the latest technology in cardiovascular care.
The recent approval of the tricuspid clip device by the U.S. Food and Drug Administration (FDA) was based on the positive results of the TRILUMINATE pivotal trial. Atrium Health Sanger Heart & Vascular Institute was a key participant in this landmark study, which has set a new standard for the management of severe tricuspid regurgitation.
The tricuspid clip procedure offers numerous benefits over traditional surgical methods. It is a same-day procedure, allowing patients to return home the next day. Recovery times are significantly shorter, with most patients resuming normal activities within one week. Additionally, the risks associated with the procedure are much lower compared to open-heart surgery.
Sanger Heart & Vascular Institute has established itself as a global leader in pioneering innovative heart treatments. Nearly 20 years ago, the institute distinguished itself by becoming one of the first centers worldwide to perform the groundbreaking mitral clip procedure as part of an early feasibility study. This procedure has since become a cornerstone in the field of structural heart interventions. Today, Sanger remains a leader in structural heart interventions, training other institutions in these advanced techniques.
"This is an important project for our entire institution," said Rinaldi. "We were one of the first 10 centers in the world to perform mitral clip procedures, and now we are leading the way with the tricuspid clip. This is an addition to a number of regional firsts. We were the first to perform tricuspid clip in the Carolinas, the first to perform tricuspid clip and trans-catheter tricuspid replacement in the Carolinas as part of clinical trials and we are authors on multiple publications on trans-catheter mitral and tricuspid therapies.”
“Sanger Heart & Vascular Institute remains committed to advancing heart care through cutting-edge technologies and multidisciplinary collaboration,” said Rinaldi. “As a leader in structural heart interventions, Atrium Health Sanger Heart & Vascular Institute will continue to pioneer new treatments and train other physicians ensuring that patients receive the best possible care.” (source)
CDC Warns Deadly Mpox Outbreak Abroad Poses Global Threat
The Centers for Disease Control and Prevention is warning Americans about a deadlier form of mpox that’s spreading rapidly through the Democratic Republic of the Congo (DRC), saying it “poses a global threat.” MPox cases in the U.S. have declined since their peak in August 2022, but health officials are urging caution. So far, no cases of this deadlier strain have been detected in the U.S., but the CDC is ramping up surveillance for mpox and advising people at high risk of infection to get vaccinated and take precautions.
The deadlier of two forms of the mpox virus — known as clade I — has driven cases in the DRC to a record high. Nearly 20,000 suspected mpox cases were diagnosed there between January 1, 2023, and April 14, 2024, according to a recent CDC report. Almost 1,000 people died of the infection and more than two-thirds of those were children.
For now, the deadlier clade is chiefly affecting countries in Central Africa, including the DRC and Cameroon. None of the 343 samples taken from people with mpox in the U.S. that the CDC tested between December 1, 2023, and April 14, 2024, belonged to clade I.
Continue to the full article here.
Update from the Office of Congressman Greg Murphy, M.D.

Washington, D.C. — Congressman Greg Murphy, M.D. issued the following statement:
"As a physician I have, for the last 30 years, taken care of thousands and thousands of patients. It is now my turn to be one. After a series of tests and scans, I have been diagnosed with a base of skull tumor called a pituitary macroadenoma. It is thought to be a benign tumor, however, given its size and location, and its subsequent ability to affect vital structures in the brain, I am scheduled to have it surgically removed. As every patient should, I have the utmost faith in my physicians and surgeons to get me through this and back on the road to full recovery.
I have been, and will continue to be, a tireless advocate for those who take care of patients. The doctors, nurses, and medical staff who train and sacrifice for years and years to care for others have answered the highest call of humanity and should be appreciated for such. They are not compensated or appreciated enough. I am blessed to have the supportive love of my wife Wendy and our entire family, as well as my incredible staff, in addition to the wonderful, amazing, and patriotic constituents of North Carolina’s Third District.
The prognosis is excellent, and I hope to be back to work full-time soon. I am, as are all things, in the hands of God and am at absolute peace. I appreciate your thoughts and prayers and hope everyone understands our desire for privacy at this time."
Self-Screening HPV Tests Aim to Make Cervical Cancer Screenings More Accessible

According to the CDC, human papillomavirus (HPV) virus is the main cause of cervical cancer, which affects about 12,000 women in the United States each year. But now, there may be a way to assure cervical cancer screenings are more accessible.
The FDA has approved a new method of self-screening for HPV. The approval for self-screening is reserved for the doctor's office currently, but at-home tests may be available in the future.
The new self-screening option helps make HPV testing more accessible, but it does not replace regular physical exams, including Pap smears, according to Joshua G. Cohen, MD, FACOG, FACS, the medical director of the gynecologic cancer program and a board-certified gynecologic oncologist at City of Hope Orange County in Irvine, California.
The American Cancer Society recommends cervical cancer screenings starting at age 25. Women ages 25 to 65 have the option to get the HPV test or a combined HPV and Pap smear test every five years or a Pap smear alone every three years.
Find the full article here.
Got a Minute? Respond to the Maternal and Child Health Survey

On behalf of the North Carolina Title V Program, you are invited to respond to this survey as part of the 2025 Title V Needs Assessment, a requirement of the Maternal and Child Health (MCH) Block Grant application and a critical element of the MCH program planning process for the NC Department of Health and Human Services.
The mission of the NC Title V Maternal and Child Health (MCH) Block Grant Program is to support and promote the health and well-being of NC individuals including mothers, infants, children, youth, and their families to reduce inequities and improve outcomes.
The findings of the assessment are used to identify priorities and to guide resource allocation and program planning within the following five MCH domains, acknowledging that many issues are cross-cutting or related:
- Women/Maternal Health
- Perinatal/Infant Health
- Child Health
- Adolescent Health
- Children with Special Health Care Needs
Thank you for your time.
NCDHHS Shares Safety Practices for a Healthy Summer Ahead of Memorial Day Weekend

Ahead of the Memorial Day weekend, the North Carolina Department of Health and Human Services is emphasizing the importance of safe swimming, heat safety and safe grilling practices to help prevent illness, injury and death.
Swimming:
Drowning remains the leading cause of death for children between ages 1-4 nationwide and is preventable. NCDHHS urges everyone to adopt the following safety measures while enjoying North Carolina’s many beaches, lakes, rivers and pools:
- Active Supervision: Always keep an eye on children near water. Drowning often occurs quickly and quietly without the dramatic signs seen on TV.
- Secure Pool Areas: Ensure gates or doors to pool areas are securely closed and locked when not in use. Never prop open gates or remove pool ladders when the pool is unattended.
- Water Awareness: Stay informed about local water conditions, including the presence of strong currents, undertows or sudden depth changes.
- Health Precautions: Avoid swimming if you or a family member has diarrhea to prevent the spread of illness.
- Water Disinfectant: Make sure any pool or spa water is treated with the proper chemicals to prevent spread of waterborne illness. Local health departments check water disinfectant levels and safety equipment at all public pools, spas and splash pads during the annual pool permitting and inspection process.
Heat Safety:
According to the 2020 North Carolina Climate Science Report, most parts of the state are expected to see at least two to three additional weeks of very hot days (maximum temperature of 95°F or higher) in the coming years. Prolonged exposure to heat can lead to dehydration, overheating, heat illness and even death. Last year, North Carolina had more than 3,900 emergency department visits for heat-related illness from May to September.
To protect yourself and others from heat-related illness, take the heat seriously and do not ignore danger signs like nausea, headache, dizziness or lightheadedness, confusion, and rapid or erratic pulse. Get to a cool place, drink water slowly and seek medical help if conditions don’t improve. Children, adults 65 and older, pregnant women, athletes, outdoor workers, people without access to air conditioning and those with chronic health conditions are most vulnerable to the health effects of extreme heat.

Grilling
Most of the top foodborne illnesses reported each year statewide happened May through August. By adhering to the following safety guidelines, North Carolinians can help ensure their gatherings are healthy and enjoyable:
- Hygiene First: Always wash your hands with soap and water for at least 20 seconds before and after handling any food or operating the grill.
- Avoid Cross-Contamination: Keep raw meats, poultry and seafood separate from cooked and ready-to-eat foods to prevent bacterial spread.
- Cook Thoroughly: Use a food thermometer to check meats are cooked to the correct internal temperatures to kill harmful bacteria.
- Proper Food Storage: Promptly refrigerate or freeze leftovers to slow the growth of bacteria. Consume or discard leftovers within three to four days to prevent foodborne illness.
- Regular Cleaning: Clean and sanitize grill surfaces and utensils before and after each use to avoid cross-contamination.
Working to Improve the Mental Health of North Carolina Clinicians
Healthcare leaders in North Carolina have made a new commitment to improve the mental health of clinicians.
Following last month’s launch of the ALL IN: Caring for NC Caregivers initiative between The North Carolina Clinician and Physician Retention and Well-being Consortium (NCCPRW) and The Dr. Lorna Breen Heroes’ Foundation, NCMS CEO Chip Baggett, JD & The Foundations CMO Stefanie Simmons, MD, FACEP joined Ron Southwick, senior editor of Chief Healthcare Executive for a conversation around the ALL IN initiative, the impact of the Consortium, the Foundation’s efforts on a national level, and removing administrative burdens.
Find the full article and video here.
Text taken from the article:
Baggett and Simmons spoke with Chief Healthcare Executive in a joint conversation, and Simmons had a realization as Baggett recited some of the administrative burdens on clinicians.
“The thing that stands out to me the most is none of those were actual patient care issues,” Simmons says. “These are all of the things that get in between healthcare workers and their relationship and their ability to care for patients.”
“Some of those administrative burdens are inescapable, but some of them are changeable,” she says. “And some of them can be addressed by organizations and others can be addressed at the state level. And so where we can get those barriers out of the way of a healthcare worker and their patient, having that connection and that healing relationship, it has a huge impact on burnout and also ability to have effective, efficient patient care.”
Dr. Karyn Hargett Posthumously Honored with Samuel L. Katz, M.D. Excellence in Immunization Award!

The late Dr. Karyn Hargett, medical director of the Old North State Medical Society (ONSMS) COVID Project, was posthumously honored with the Samuel L. Katz, M.D. Excellence in Immunization Award at the 2024 North Carolina Immunization Conference held on May 9, 2024, at the Sheraton Imperial Hotel at Research Triangle Park, NC.
The purpose of this award is to recognize outstanding individuals or agencies/organizations that have developed innovative strategies, projects, or programs to increase childhood, adolescent, and adult immunization coverage rates. Nominees were assessed based on tenets such as effectiveness, innovation, and project replication ability.
Under the expert direction of Dr. Hargett, ONSMS was able to get into rural communities and make a tremendous difference. During the course of the COVID Project, ONSMS vaccination teams provided over 31,000 vaccinations and 3500 tests at over 1500 events.
Dr. Karen Smith, an active member of the Downeast COVID team and the 2023 NC Rural Leadership Award warmly remembers Dr. Hargett with these words, "(She) was methodically meticulous to ensure ONSMS reports were correct, public vaccination was done with safety in mind and the reputation of physicians who believe in and care for the community was echoed throughout North Carolina.

Mark Your Calendar for the Next DOCMS Meeting!
Join DOCMS at the University Club!
Wednesday, June 5, 2024 | 6:00pm - 8:00pm
University Club, 3100 Tower Boulevard, Suite 1700 - Durham, NC 27707
AGENDA:
- 6:00pm- 6:30pm – Socializing & Housekeeping
- 6:30pm- 7:30pm – Dinner & Guest Speakers
- 7:30pm- 7:45pm – Q&A
- 7:45pm- 8:00pm – DOCMS 2024 Business
“The Criminal Legal System, Incarceration and Health Disparities.”
Speakers:
Evan Ashkin, MD | Professor of Family Medicine UNC Chapel Hill and founder of the North Carolina Formerly Incarcerated Transition (FIT) Program

Dr. Evan Ashkin is a professor of Family Medicine at the University of North Carolina at Chapel Hill. His work is focused on addressing health disparities and gaps in care for marginalized populations. Dr. Ashkin founded the North Carolina Formerly Incarcerated Transition (FIT) Program in 2017 to help address the absence of linkages to care for people released from incarceration with chronic disease, mental illness and/or substance use disorder. The FIT Program now operates in 7 counties across North Carolina. Dr Ashkin also directs the North Carolina Technical Assistance Center, supporting programs for people at risk for incarceration and overdose.
Tommy Green | FIT Program Community Health Worker
Tommy Green, hailing from Oxford, North Carolina, overcame an 11-year, 8-month sentence at 22 years old. Emerging from North Carolina's toughest prisons, he transitioned from freelance security to Assistant Operations Manager of a $20 million company. Now, as Lead Community Health Worker for NC Formerly Incarcerated Transition Program and Program Manager for Orange County Health Department, Tommy is also an Adjunct UNC Family Medicine Instructor, co-owns Success While In Transition INC, and co-directs a nonprofit called Wounded Healers. His impactful work, is featured in the Washington Post, Health Affairs, and other local media, focuses on supporting post-incarceration transition and aiding substance abuse recovery.
1 CME Credit is available! Click here for how to claim your credit.
DOCMS Members & Prospective Members - FREE to attend
Guests - $25 to attend (will be collected at meeting site)
2024 AMPAC Campaign School Now Open for Registration
AMPAC is excited to announce that the 2024 Campaign School will be returning in-person July 25-28 at the AMA offices in Washington, DC and registration is now open!
Running an effective campaign can be the difference between winning and losing a race. That's why the Campaign School is designed to give you the skills and strategic approach you will need on the campaign trail. Our team of political experts will teach you everything you need to know to run a successful campaign. Under the direction of our lead trainers, participants will be broken into campaign staff teams to run a simulated congressional campaign using what they’ve learned during group sessions on strategy, vote targeting, social media, advertising and more.
Attendees may include physicians, spouses of physicians, residents and medical students and state medical society staff interested in becoming more involved in politics. Participants range from those attracted to grassroots efforts to those considering becoming a candidate for public office. No matter where you are in the process, you will develop a new understanding of how campaigns are run. As a graduate of the AMPAC program, candidates will rely on you to give them advice on strategy, message, and campaign plans.
Please note the following:
- The Candidate Workshop is open to AMA physician members, member spouses, residents, medical students and state medical society staff.
- Registration fee is $350 for AMA members and member spouses/$1000 for non-AMA members. This fee is waived for AMA residents and students; however, space is limited and the AMPAC Board will review and select four participants from the pool of qualified resident and student applicants.
- Faculty, materials, and all meals during the meeting are covered by the AMA. Participants are responsible for their registration fee, travel to/from Washington, DC and hotel accommodations (AMPAC staff will provide you with a list of nearby hotels within walking distance of the AMA offices).
- Participants will be required to bring a laptop or Wi-Fi enabled tablet with them.
Space is limited and the deadline to register is July 1 (or sooner if maximum capacity is reached).
Learn more about the 2024 AMPAC Campaign School and how to register here.
For additional information on the 2024 Campaign School, contact us at [email protected] or (202) 789-7455.
Mark Your Calendar for LEAD 2024! It's Our 175th Anniversary!

SAVE THE DATE
2024 Marks the 175th Anniversary of the
North Carolina Medical Society!
We're planning a sensational celebration in honor of this milestone occasion, and we want you to be a part of it!
November 1-2, 2024
Grandover Resort, Greensboro, NC
Get more details at www.ncms-lead.com.
Stay tuned for more information at www.ncmedsoc.org and watch your Morning Rounds newsletter for the latest details.

AMA Issues Call for AMPAC Board of Directors Applicants

The American Medical Association is currently soliciting applications to fill three vacancies on the AMPAC Board of Directors.
In 2024, two members of the AMPAC Board will reach maximum tenure and one member has resigned creating three vacancies. New members will be appointed by the AMA Board of Trustees at the September 2024 meeting. Members of the AMPAC Board serve a two-year term and may be eligible to serve three additional terms for a maximum tenure of eight years.
Applicants must submit the Board-approved application, a three-page (maximum) executive CV, and may submit one letter of recommendation. For additional information on the application process and to download the most current AMPAC application form (pdf), please visit our website.
All applicants must also complete a Conflict of Interest (COI) disclosure statement. This process has been automated by the AMA Office of the General Counsel, and a secure link will be emailed to each applicant. Application materials will not be considered until the COI disclosure has been completed.
Please submit AMPAC applications to [email protected] no later than Thursday, August 15, 2024 @5:00 PM Central Time.
Funding Opportunity: Behavioral Health Service Expansion Funding

This Notice of Funding Opportunity (NOFO) announces the opportunity to apply for funding under the fiscal year (FY) 2024 Behavioral Health Service Expansion (BHSE) program. BHSE will support health centers to increase access to behavioral health services through starting or expanding mental health and substance use disorder (SUD) services.
Health Resources and Services Administration (HRSA) is making available $240 million to increase support for HRSA-funded health centers to respond to the need for mental health and substance use disorder (SUD) services.
HRSA extended the Grants.gov deadline to Friday, May 24. The deadline for applying in HRSA’s Electronic Handbooks (EHBs) is unchanged — it remains Friday, June 21.
Visit the Apply for FY 2024 Behavioral Health Service Expansion webpage for additional information, including how to apply.
HRSA has posted frequently asked questions for additional guidance.
Side-by-Side Webinar with NCDHHS' Mental Health Division

Join staff from NCDHHS' Division of Mental Health, Developmental Disabilities and Substance Use Services on June 3 at 2 p.m. to learn more about policies and programs that affect the Mental Health, Intellectual and Developmental Disabilities, Substance Use Services and Traumatic Brain Injury community.
The goal of these monthly webinars is to bring everyone together in one (virtual) place to share ideas for public policy that will improve the lives of North Carolinians. This group includes consumers, families, advisory groups, LME/MCOs, community members and partner organizations. Side by side, we will work together to improve our system.
Register for the webinar on June 3 via Zoom and see a flyer for more information.
Capitol Chronicle: NC Internal Medicine Physicians Convey Patient Care Priorities to Congress

North Carolina Internal Medicine Physicians Convey
Patient Care Priorities to Congress
On May 15, 2024, a contingent of North Carolina internal medicine physicians traveled to Capitol Hill to meet with North Carolina’s members of US Senate, US House and their staff. The occasion was the American College of Physicians’ 2024 Leadership Day and participants included:
The group’s trip to Capitol Hill included visits to all 14 House offices and 2 Senate offices. The issues presented included:
- Medicare physician payment reform
- Need for increased residency slots
- Step therapy relief

NC Group with Rep./Dr. Greg Murphy
Do you know your state and federal legislators? More importantly, do your legislators know you?
The NCMS can help you connect with policy makers as a constituent and advocate!
 Thank you for making a difference!
Thank you for making a difference!
Don't Forget to Register for AMA Advocacy Insights Webinar
What’s exacerbating the physician shortage crisis—and what’s needed to fix it
Wednesday, May 22, 2024
2:00 PM-3:00 PM CT
The U.S. is facing a shortage of between 13,500 and 86,000 physicians by 2036—a deficiency that is almost certain to be compounded by rising rates of physician burnout and early retirement. The physician workforce, like our general population, is aging, with nearly 45% of active physicians in the U.S. aged 55 and older. Addressing the physician workforce issue is crucial to ensuring patients have access to care where and when they need it.
Register for this Advocacy Insights webinar on May 22 at 2 p.m. CT to learn about how increasing residency training slots, addressing visa issues for international medical graduates, ensuring access to care in rural areas, and addressing factors impacting physician burnout—including Medicare physician payment instability and administrative burdens—can help bolster the physician workforce.
Moderator:
- Jesse M. Ehrenfeld, MD, MPH, president, American Medical Association
Speakers:
- John Andrews, MD, vice president of graduate medical education innovations, AMA
- Alexis Pierce, JD, senior attorney, Division of Legislative Counsel, AMA
- Christopher Sherin, assistant director, Division of Congressional Affairs, AMA
CMS Call for Comment: Intention to Collect Public Information

The Centers for Medicare & Medicaid Services (CMS) is announcing an opportunity for the public to comment on CMS' intention to collect information from the public.
Under the Paperwork Reduction Act of 1995 (PRA), federal agencies are required to publish notice in the Federal Register concerning each proposed collection of information (including each proposed extension or reinstatement of an existing collection of information) and to allow 60 days for public comment on the proposed action.
Interested persons are invited to send comments regarding our burden estimates or any other aspect of this collection of information, including the necessity and utility of the proposed information collection for the proper performance of the agency's functions, the accuracy of the estimated burden, ways to enhance the quality, utility, and clarity of the information to be collected, and the use of automated collection techniques or other forms of information technology to minimize the information collection burden.
DATES:
Comments must be received by July 15, 2024.
ADDRESSES:
When commenting, please reference the document identifier or OMB control number. To be assured consideration, comments and recommendations must be submitted in any one of the following ways:
- Electronically. You may send your comments electronically to http://www.regulations.gov. Follow the instructions for “Comment or Submission” or “More Search Options” to find the information collection document(s) that are accepting comments.
- By regular mail. You may mail written comments to the following address: CMS, Office of Strategic Operations and Regulatory Affairs, Division of Regulations Development, Attention: Document Identifier/OMB Control Number: __, Room C4-26-05, 7500 Security Boulevard, Baltimore, Maryland 21244-1850.
To obtain copies of a supporting statement and any related forms for the proposed collection(s) summarized in this notice, please access the CMS PRA website by copying and pasting the following web address into your web browser: https://www.cms.gov/?Regulations-and-Guidance/?Legislation/?PaperworkReductionActof1995/?PRA-Listing.
FOR FURTHER INFORMATION CONTACT:
William N. Parham at (410) 786-4669.
SUPPLEMENTARY INFORMATION:
Contents
This notice sets out a summary of the use and burden associated with the following information collections. More detailed information can be found in each collection's supporting statement and associated materials (see ADDRESSES ).
CMS-10123/10124 Fast Track Appeals Notices: NOMNC/DENC
Under the PRA (44 U.S.C. 3501-3520), federal agencies must obtain approval from the Office of Management and Budget (OMB) for each collection of information they conduct or sponsor. The term “collection of information” is defined in 44 U.S.C. 3502(3) and 5 CFR 1320.3(c) and includes agency requests or requirements that members of the public submit reports, keep records, or provide information to a third party. Section 3506(c)(2)(A) of the PRA requires federal agencies to publish a 60-day notice in the Federal Register concerning each proposed collection of information, including each proposed extension or reinstatement of an existing collection of information, before submitting the collection to OMB for approval. To comply with this requirement, CMS is publishing this notice.
Information Collection
- Type of Information Collection Request: Revision of a currently approved collection; Title of Information Collection: Fast Track Appeals Notices: NOMNC/DENC; Use: The purpose of the NOMNC is to help a beneficiary/enrollee decide whether to pursue a fast appeal by a Quality Improvement Organization (QIO) and informs them on how to file a request. Consistent with §§ 405.1200 and 422.624, SNFs, HHAs, CORFs, and hospices must provide notice to all beneficiaries/enrollees whose Medicare-covered services are ending, no later than two days in advance of the proposed termination of service. This information is conveyed to the beneficiary/enrollee via the NOMNC.
If a beneficiary/enrollee appeals the termination decision, the beneficiary/enrollee and the QIO, consistent with §§ 405.1200(b) and 405.1202(f) for Traditional Medicare, and §§ 422.624(b) and 422.626(e)(1)-(5) for MA plans, will receive a detailed explanation of the reasons services should end. This detailed explanation is provided to the beneficiary/enrollee using the DENC, the second notice included in this renewal package. Form Number: CMS-10123/10124 (OMB control number: 0938-0935); Frequency: Yearly; Affected Public: Private sector, Business or other for-profits and Not-for-profit institutions; Number of Respondents: 32,384; Number of Responses: 21,322,379; Total Annual Hours: 3,962,194. (For policy questions regarding this collection contact Janet Miller at [email protected].)
Researchers Wrestle with Accuracy of AI Technology Used to Create New Drug Candidates
Artificial intelligence (AI) has numerous applications in healthcare, from analyzing medical imaging to optimizing the execution of clinical trials, and even facilitating drug discovery.
AlphaFold2, an artificial intelligence system that predicts protein structures, has made it possible for scientists to identify and conjure an almost infinite number of drug candidates for the treatment of neuropsychiatric disorders. However recent studies have sown doubt about the accuracy of AlphaFold2 in modeling ligand binding sites, the areas on proteins where drugs attach and begin signaling inside cells to cause a therapeutic effect, as well as possible side effects.
In a new paper, Bryan Roth, MD, PhD, the Michael Hooker Distinguished Professor of Pharmacology and director of the NIMH Psychoactive Drug Screening Program at the University of North Carolina School of Medicine, and colleagues at UCSF, Stanford, and Harvard determined that AlphaFold2 can yield accurate results for ligand binding structures, even when the technology has nothing to go off of. Their results were published in Science.
Continue to the full article here.