Join Us for NCMS White Coat Day – April 30th!
Join NCMS and Bring Your Colleagues to the 2025 NCMS White Coat Day!
We are excited to invite you to the NCMS White Coat Day on April 30th from 8 AM - 7 PM at the General Assembly!
This will be a full day of important discussions with legislators from across the state about critical issues such as prior authorization reform and scope of practice changes.
The day’s events will begin promptly at 8 AM at the NCMS office in Raleigh with breakfast and a debrief on NCMS’ legislative priorities. Then, you will head to the North Carolina General Assembly for a full schedule of meetings with legislators.
Lunch will be served at NCMS from 12-1:30pm with an exciting guest speaker.
The day concludes with a tour of either the Governor’s Mansion or NC State Capitol, followed by a Legislative Reception.
This is a fantastic opportunity to engage directly with lawmakers and help shape the future of healthcare policy in North Carolina. We hope you can join us!
Please register by April 23rd. We look forward to seeing you there!
Click here to register!
Duke Study: Less Invasive Lung Cancer Surgeries on the Rise
Lung cancer surgery is shifting to less invasive procedures
(Duke News, Shantell M. Kirkendoll) -- Lung cancer surgery is shifting toward less invasive procedures, particularly for younger and healthier patients, according to a new study led by Duke University School of Medicine analyzing two decades of data.
Traditionally, removing an entire lobe of the lung – lobectomy—was the gold standard for early-stage lung cancer. But the study in the March issue of JTO Clinical and Research Reports shows a shift to more patients opting for less invasive procedures like segmentectomy and wedge resection.
These techniques remove only the part of the lung affected by cancer, allowing patients to keep more of their healthy lung tissue and breathing ability, while helping them live longer.
“This is a very encouraging finding for the entire community of professionals caring for lung cancer patients,” said study corresponding author Xiaofei Wang, PhD, professor in the Department Biostatistics and Bioinformatics at Duke medical school.
The study was based on patient data from 76,466 lung cancer cases in the National Cancer Database between 2004 and 2020.
But researchers warn that clinical trials tracking patients throughout their treatment are needed to prove if these surgical trends lead to better patient outcomes.
According to the study, lobectomy procedures declined from 75.2% to 67.6% of lung cancer surgeries. Meanwhile segmentectomy – a procedure that removes a smaller portion of the lung – more than doubled, rising from 4.3% to 9.7%. Wedge resections remained steady, increasing slightly from 20.5% to 22.8%
“Looking at the surgical care of early-stage non-small cell lung cancer over the past two decades we’re seeing remarkable improvements in survival outcomes and surgical quality, thanks to advancements in surgical techniques, tumor detection and classification, and peri-operative care,” said Wang, a member of the Duke Cancer Institute and expert in cancer survival analysis.
Lung cancer causes 1 in 5 cancer deaths, with smoking as the leading risk. While most lung cancer cases are diagnosed around age 70, cases are rising among younger adults who have never smoked.
The problem is that early-stage lung cancer is hard to catch. Symptoms—like back pain, a chronic cough, chest pain, and shortness of breath—can be vague or mistaken for other health conditions.
The study found that younger patients, age 18-69, with fewer underlying health conditions, and smaller cancer tumors measured at 2 cm or less, about the width of the top edge of a pencil, were increasingly opting for the less extensive surgeries.
“This is a notable shift from past trends, when these procedures were mainly for older and sicker patients who may not tolerate a larger procedure like lobectomy,” said Eden Z. Deng, the study's first author and a graduate of Duke University who worked on the study with the Department of Statistical Science. “Since 2004, segmentectomy has maintained overall survival rates comparable to lobectomy, and wedge resection appears to be quickly catching up in the most recent five years we studied.”
Wedge resections initially had worse survival outcomes but have improved with five-year survival reaching 79.9% in lung cancer cases treated between 2016 and 2019. Segmentectomy showed comparable five-year survival rates to lobectomy – 80.6% versus 83.6% over the study period.
Early detection through screening and improved tumor staging has allowed doctors to identify patients who may recover well with one of the less aggressive surgeries instead of a full lobectomy. Advances in robotic and video-assisted techniques have also made these smaller lung surgeries easier to perform.
The study was supported in part by the National Institutes of Health and the National Institute of Aging (R01 AG066883).
In addition to Deng, Wang and Altorki, study authors include senior study author Nasser Altorki, MD, Weill Cornell Medicine; Jianrong Zhang, MD, MPH, University of Melbourne, Victoria Australia; Thomas E. Stinchcombe, MD, Duke Cancer Institute; and Chi-Fu (Jeffrey) Yang, MD, Department of Surgery Massachusetts General Hospital and Harvard Medical School.
Governor Josh Stein Urges Congress to Protect North Carolinians’ Health Care and Oppose Cuts to Medicaid Funding

Gov. Josh Stein Urges Congress to Change Course on Proposed Cuts to Medicaid
Governor Josh Stein sent a letter to Congressional leaders urging them to change course on proposed federal cuts to the Medicaid program and laying out what’s at stake in North Carolina.
“Medicaid is a lifeline for more than 3 million North Carolinians and disproportionately serves our rural population,” said Governor Josh Stein. “I strongly urge Congress to oppose cuts to Medicaid funding so that hundreds of thousands of North Carolinians do not lose their health care and our rural health care system is not devastated.”
North Carolina’s Medicaid program contributes at least $28 billion to the state’s economy every year and is crucial to the wellbeing of the state’s most vulnerable people, including children, seniors, and individuals with disabilities. In 29 mostly rural counties, 40 percent or more of the population depends on Medicaid for health care. Over the past 11 years, North Carolina’s Medicaid program has been efficiently managed with no cost overruns.
In March 2023, North Carolina’s General Assembly passed Medicaid expansion with overwhelming bipartisan support. Since it passed, Medicaid expansion has enabled more than 640,000 North Carolinians to access affordable health care, and it has stabilized struggling rural hospitals to maintain health care access throughout the state. One of the proposed cuts would lower the enhanced federal match for the expansion population, which would trigger an immediate end to Medicaid expansion in North Carolina, leaving 640,000 North Carolinians without health care coverage immediately.
Any reductions in Medicaid funding would jeopardize access to critical health care for these groups, putting their well-being and the stability of the health care system at risk, including a loss of $6 billion in federal funds to health care providers.
Click here to read the full text of Governor Stein’s letter to Congress.
Action Alert - Medicare Payment Fix. Contact your member of Congress ASAP!

March 5, 2025
Action Alert - Medicare Payment Fix
Contact your member of Congress ASAP!
Over the past two decades, Medicare physician payment rates have declined by 33%, when adjusted for the cost of running a practice. The payment cuts for the past five consecutive years have left physicians and practices struggling to manage practice costs while fulfilling the commitment to meeting the care needs of their elderly and chronically ill patients.
The last Congress failed to pass legislation that would have addressed these issues in its end-of-year funding package. As a result, a 2.8% cut to physician Medicare payments went into effect on January 1, 2025
Congress must pass legislation to mitigate the cut and needs to act again now!
Rep. Greg Murphy, MD, urologist from Greenville, NC who represents North Carolina’s 3rd congressional district, has taken the lead in a legislative fix for the payment dilemma. On January 31, 2025, he, along with a bipartisan group of House colleagues, introduced H.R. 879 / Medicare Patient Access & Practice Stabilization Act, which would reverse the 2.8% cut to Medicare physician payment and provide a positive inflationary update.
Building support for this legislation among our members of Congress is urgent and crucial. The time to act is now and we need you to contact your member of the US House of Representatives today and urge them to cosponsor this important bill. The more bipartisan support that we can build, the greater the likelihood of it getting enacted.
If your member of Congress responds that she/he is already a cosponsor, thank them and ask them to help build support for the legislation. Please take action today.
Thank you.
CONTACT CONGRESS NOW
Your Mother May Not Approve, But Researchers Are Working to Understand Why Swearing Helps With Pain!
Swearing is linked with increased pain tolerance and strength
Researchers are working to understand why swearing may help in a number of circumstances, with a major focus on pain, and how it can more effectively be used in a clinical setting.
(The Washington Post, Sam Jones) -- If you stub your toe or slam your finger in a door, there’s a good chance the first thing out of your mouth is a four-letter word. But although swearing is a near-universal feature of language, it is still considered taboo by many.
Swearing is “a drug-free, calorie-neutral, cost-free means of self-help,” said Richard Stephens, a researcher and senior lecturer in psychology at Keele University in England.
Researchers are working to understand the mechanisms underlying swearing’s impact in a number of circumstances, with a major focus on pain. With that knowledge, Stephens said, swearing can more effectively be used in a clinical setting.
Pain reduction through swearing
In 2009, Stephens and his colleagues published the first study linking swearing with hypoalgesia — a reduced sensitivity to pain. Subjects were asked to participate in a cold pressor task, in which they held their hands in ice water for as long as possible while repeating either a swear word of their choosing or a non-swear word. Swearing was associated with not only increased pain tolerance but also decreased perceived pain.
Studies followed showing similar, yet sometimes varied, effects. In 2020, for instance, Stephens and Robertson investigated the use of the swear “f---” compared with a neutral word and two made-up swear words — “fouch” and “twizpipe” — and found that swearing was linked with increased pain tolerance but had no significant effect on pain perception.
That association between swearing and increased pain tolerance is not specific to the English language. In 2017, Robertson and Stephens published a study investigating the cross-cultural effect of swearing on pain, comparing Japanese and English speakers. In Japan, Robertson said, swearing is not socially ingrained the way it is in Britain, so she doubted that it would have the same effect.
While doing the cold presser task, native English speakers repeated either the swear “f---” or a control word — “cup” — and native Japanese speakers repeated a Japanese word that means s--- or a control word “kappu,” meaning cup. Regardless of language, swearing was linked with greater pain tolerance. “Which I wasn’t expecting at all, because I was expecting to see that social effect,” Robertson said.
Swearing has benefits beyond physical pain
In addition to pain tolerance, swearing has been linked to bolstered social bonds, improved memory, and even an alleviation of the social pain of exclusion or rejection. “Neurologically, the pathways for physical pain and emotional pain are the same,” Robertson said. “So when you have heartbreak, it’s the same neural structures. It’s the same biological blueprint, and that’s why it feels so visceral, because it literally is.”
More recently, swearing has been shown to be linked with an increase in strength. Looking at the impact of swearing on strength was a logical progression, Stephens said, because he and others had shown that swearing while in pain often was associated with increased heart rate, similar to what happens during a “fight or flight” stress response, where your body releases a surge of adrenaline and blood is diverted to your muscles to prepare for action.
In 2018, Stephens and his colleagues found that, in an anaerobic power test on a bike, swearing was linked with an improvement in participant strength. However, they were unable to identify any physiological variable — including heart rate — that correlated with the finding. Stephens has since shifted his focus more to the psychological. “My research has been trying to understand what’s the psychological mechanism by which swearing brings about these effects, both for pain and for physical strength,” he said.
But what exactly connects swearing with greater strength and pain tolerance remains a mystery.
Over the past few years, Stephens has focused on state disinhibition theory: “the idea that, by swearing, we just get ourselves in a place where we’re more disinhibited, and in a disinhibited state, we push ourselves further, go for it a little bit more,” he said. “So we’ll put up with the ice-cold water for a few more seconds, or [in a strength task] we’ll squeeze on the hand gripper with a little more force.”
The optimal swearing dosage
Up until this point, testing the link between swearing and pain has been done in a controlled, laboratory setting.
Nick Washmuth, professor of physical therapy at Samford University in Alabama, is focused on the potential for swearing to be used in a clinical context, which means understanding not only the mechanisms by which swearing affects pain but also how a person’s environment, age, how much they already swear in their everyday lives, the intensity of the swear word and other variables could influence the effect.
“We need to better understand those factors and how they play a role to be able to prescribe swearing in a medical sense, in a clinical sense,” Washmuth said. “Is there an optimal dosage for swearing?”
For those who would like to use swearing to help with pain or increase strength, Washmuth suggested starting by selecting a swear word that feels powerful, that you would naturally use if you stubbed your toe, for instance.
“If no word comes to mind, the f-word is the most commonly self-selected swear word by participants in these studies and is considered one of the most powerful swear words out there,” he said. “Swear at a steady pace once a second to once every three seconds, at a normal speech volume.”
But if audible swearing is not your thing, do not despair. Washmuth is now studying whether internal swearing could do the trick.
“Swearing out loud is frowned upon in many public places, right? So we’re trying to determine if you can swear using your inner monologue to get the same effect,” Washmuth said. “Can you swear in your head to decrease pain or improve strength?”
To Solve Doctor Shortages, Some States Ease Licensing for Foreign-Trained Physicians

The changes involve residency programs
(NPR, Arielle Zionts) -- A growing number of states have made it easier for doctors who trained in other countries to get medical licenses, a shift supporters say could ease physician shortages in rural areas.
The changes involve residency programs — the supervised, hands-on training experience that doctors must complete after graduating medical school. Until recently, every state required physicians who completed a residency or similar training abroad to repeat the process in the U.S. before obtaining a full medical license.
Since 2023, at least nine states have dropped this requirement for some doctors with international training, according to the Federation of State Medical Boards. More than a dozen other states are considering similar legislation.
About 26% of doctors who practice in the U.S. were born elsewhere, according to the Migration Policy Institute. They need federal visas to live in the U.S., plus state licenses to practice medicine.
Proponents of the new laws say qualified doctors shouldn't have to spend years completing a second residency training. Opponents worry about patient safety and doubt the licensing change will ease the doctor shortage.
Lawmakers in Republican- and Democratic-leaning states have approved the idea at a time when many other immigration-related programs are under attack. They include Florida, Iowa, Idaho, Illinois, Louisiana, Massachusetts, Tennessee, Virginia, and Wisconsin.
The changes come as President Trump moves to tighten many immigration rules, although he has defended a federal H-1B visa program that many foreign doctors rely on.
Supporters of the new licensing laws include Zalmai Afzali, an internal medicine doctor who finished medical school and a residency program in Afghanistan before fleeing the Taliban and coming to the U.S. in 2001.
He said most physicians trained elsewhere would be happy to work in rural or other underserved areas.
"I would go anywhere as long as they let me work," said Afzali, who now treats patients who live in rural areas and small cities in northeastern Virginia. "I missed being a physician. I missed what I did."
It took Afzali 12 years to obtain copies of his diploma and transcript, study for exams, and finish a three-year U.S.-based residency program before he could be fully licensed to practice as a doctor in his new country.
But a commission of national health organizations questions whether loosening residency requirements for foreign-trained doctors would ease the shortage. Doctors in these programs could still face licensing and employment barriers, it wrote in a report that makes recommendations without taking a stance on such legislation.
Erin Fraher, a health policy professor at the University of North Carolina who advises the commission and studies the issue, said lawmakers who support the changes predict they will boost the rural health workforce. But it's unclear whether that will happen, she said, because the programs are just getting started.
"I think the potential is there, but we need to see how this pans out," Fraher said.
Many of the state bills to ease residency requirements have been based on model legislation from the Cicero Institute, a conservative think tank that sent representatives to testify to legislatures after proposing such programs in 2020.
The new pathways are open only to internationally trained physicians who meet certain conditions. Common requirements include working as a physician for several years after graduating from a medical school and residency program with similar rigor to those found in the U.S.
Even without having to complete a U.S. residency, foreign-trained doctors face a complicated process to get licensed. Applicants have to deal with paperwork including setting up malpractice insurance and in some states they have to find physicians who will supervise them. They also must pass the standard three-part exam that all physicians take to become licensed in the U.S.
Those who qualify are granted a restricted license to practice, and can receive full licensure after several years.
Afzali struggled to support his family while trying to get his medical license. His jobs included working at a department store for $7.25 an hour and administering chemotherapy for $20 an hour. Afzali said nurse practitioners at the latter job had less training than him but earned nearly four times as much.
"I do not know how I did it," he said. "I mean, you get really depressed."
'Poor answer' to the rural doctor shortage
About 10 of the laws or bills for the new pathway also require the doctors to work for several years in a rural or underserved area.
But states without this requirement, such as Tennessee, may not see an impact in rural areas, researchers from Harvard Medical School and Rand Corp. argued in the New England Journal of Medicine. In addition to including that condition, states could offer incentives to rural hospitals that agree to hire doctors from the new training pathways, they wrote.
Lawmakers, physicians, and health organizations that oppose the changes say there are better ways to safely increase the number of rural doctors.
Barbara Parker is a registered nurse and former Republican lawmaker in Arizona, where the legislature is considering a bill for at least the fourth year in a row.
"It's a really poor answer to the doctor shortage," said Parker, who voted against the legislation last year.
Parker said making it easier for foreign-trained physicians to practice in the U.S. would unethically poach doctors from countries with greater health care needs. And she said she doubts that all international residencies are on par with those in the U.S. and worries that granting licenses to physicians who trained in them could lead to poor care for patients.
She is also concerned that hospitals are trying to save money by recruiting internationally trained doctors over those trained in the U.S. The former often will accept lower pay, Parker said.
"This is driven by corporate greed," she said.
Parker said better ways to increase the number of rural doctors include raising pay, expanding loan repayment programs for those who practice in rural areas, and creating accelerated training for nurse practitioners and physician assistants who want to become doctors.
Setting standards to protect patients
The advisory commission — recently formed by the Federation of State Medical Boards, the Accreditation Council for Graduate Medical Education, and Intealth, a nonprofit that evaluates international medical schools and their graduates — published its recommendations to help lawmakers and medical boards make sure these new pathways are safe and effective.
The commission and Fraher said state medical boards should collect data on the new rules, such as how many doctors participate, what their specialties are, and where they work once they gain their full licenses. The results could be compared with other methods of easing the rural doctor shortage, such as adding residency programs at rural hospitals.
"What is the benefit of this particular pathway relative to other levers that they have?" Fraher said.
The commission noted that while state medical boards can rely on an outside organization that evaluates the strength of foreign medical schools, there isn't a similar rating for residency programs. Such an effort is expected to launch in mid-2025, the commission said.
The group also said states should require supervising physicians to evaluate participants before they're granted a full license.
Afzali, the physician from Afghanistan, said some internationally trained primary care doctors have more training than their U.S. counterparts, because they had to practice procedures that are done only by specialists in the U.S.
But he agreed with the commission's recommendation that states require doctors who did residencies abroad to have supervision while they hold a provisional license. That would help ensure patient safety while also helping the physicians adjust to cultural differences and learn the technical side of the U.S. health system, such as billing and electronic health records, the commission wrote.
CDC Now on the Ground in Texas as Measles Outbreak Grows

CDC says it’s on the ground in Texas as measles outbreak grows to 159 cases
(CNN, Neha Mukherjee) -- A measles outbreak in Texas has grown to 159 cases, and the US Centers for Disease Control and Prevention says it is now on the ground in that state to respond. The agency posted on X that it’s partnering with the Texas Department of State Health Services.
“This partnership – known as an Epi-Aid – is a rapid response by CDC’s Epidemic Intelligence Service (EIS) to tackle urgent public health issues like disease outbreaks. EIS officers provide local officials onsite support for 1-3 weeks, aiding in quick decision-making to control health threats. The local authority leads the investigation while collaborating with CDC experts,” the post said.
Previously, the CDC had provided lab support and measles-mumps-rubella (MMR) vaccines to Texas to help the outbreak response.
In an update Tuesday, Texas reported 159 measles cases, including 22 people who are hospitalized. The majority of the cases are in Gaines County, which is home to a large unvaccinated Mennonite population.
Texas announced last week the first death in the outbreak, a school-age child who was not vaccinated and had no underlying health conditions. It was the first measles death in the US since 2015 and the first in a child in the US since 2003.
Speaking to Fox News on Tuesday, US Health and Human Services Secretary Robert F. Kennedy Jr. described delivering vitamin A and providing ambulance assistance from Gaines County. He also described treatments with a steroid, budesonide, and an antibiotic, clarithromycin, as well as cod liver oil.
“What we’re trying to do is really to restore faith in government and to make sure that we are there to help them with their needs and not particularly to dictate what they ought to be doing,” Kennedy said.
Kennedy also referenced vaccines in a portion of the interview aired on Fox Business on Tuesday afternoon, saying, “in highly unvaccinated communities like the Mennonites, it’s something we recommend, but we also understand there is a lot of mistrust of the vaccines.”
“There are people who should not be vaccinated in the community because they have autoimmune problems or other immune problems. If you do get vaccinated, you are protecting those people from a possible spread.”
Kennedy, who has a long history of anti-vaccine activism, did not explicitly recommend vaccinating against measles in an opinion piece posted on Fox News’ website on Sunday.
“The decision to vaccinate is a personal one,” he wrote. “Vaccines not only protect individual children from measles but also contribute to community immunity.”
‘Man With the Golden Arm’: Grandfather Whose Rare Blood Saved Millions of Babies Dies Aged 88

(The Independent, Maroosha Muzaffar) -- James Harrison, who helped save more than two million babies by donating blood over 1,100 times across six decades, has died at 88.
According to the Australian Red Cross Lifeblood, Harrison, also known as the “man with the golden arm”, had the “precious antibody in his blood” that was used to make a “lifesaving medication called Anti-D, given to mothers whose blood is at risk of attacking their unborn babies”.
Harrison died in his sleep at Peninsula Village Nursing Home on the NSW Central Coast on 17 February.
He began donating in 1954 at 18 and continued regularly until his retirement in 2018 at 81. According to Australian Red Cross Lifeblood, he has helped save the lives of more than 2.4 million Australian babies.
Harrison’s daughter, Tracey Mellowship, fondly remembered him as a generous soul with a wonderful sense of humour.
“James was a humanitarian at heart, but also very funny,” Ms Mellowship said.
“In his last years, he was immensely proud to become a great grandfather to two beautiful grandchildren, Trey and Addison.
“As an Anti-D recipient myself, he has left behind a family that may not have existed without his precious donations.”
She added: “He was also very proud to have saved so many lives, without any cost or pain. It made him happy to hear about the many families like ours, who existed because of his kindness.
“He always said it does not hurt, and the life you save could be your own.”
Harrison’s rare antibodies were crucial in developing Anti-D, the treatment that has protected millions of newborns from Rhesus disease (or Haemolytic Disease of the Foetus and Newborn) – a condition in which a pregnant woman’s blood attacks her unborn baby’s red blood cells, potentially leading to brain damage or even death.

It occurs when a mother has RhD-negative blood, while her baby inherits RhD-positive blood from the father. If the mother has been sensitised to RhD-positive blood – often during a previous pregnancy – her immune system may produce antibodies that attack the baby’s blood as a foreign threat.
“James was a pioneer of our Anti-D programme. More than 3 million doses of Anti-D containing James’ blood have been issued to Aussie mothers with a negative blood type since 1967,” Lifeblood said in a statement on their website.
“He has changed my world and I’m sure he’s done that for many other families, making him a very incredible human,” said Rebecca Ind, a recipient of Harrison’s blood donations during and after her pregnancy 12 years ago.
In 1999 Harrison was awarded the Medal of the Order of Australia – one of the country’s most prestigious honours – for his extraordinary dedication to the Lifeblood and Anti-D programme. His kindness leaves a “remarkable legacy, and he has put the challenge out to the Australian community to beat it”, Lifeblood said in the statement.
“I hope it’s a record that somebody breaks, because it will mean they are dedicated to the cause,” Harrison said of his last donation at the age of 81.
“It becomes quite humbling when they say, ‘oh you’ve done this or you’ve done that or you’re a hero,’” Harrison said at the time. “It’s something I can do. It’s one of my talents, probably my only talent, is that I can be a blood donor.”
At 14, Harrison underwent major chest surgery and relied on the generosity of blood donors to survive. Determined to give back, he vowed to donate as soon as he was eligible – and at 18, he kept his promise, despite a fear of needles.
More than a decade later, doctors discovered that his blood contained a rare antibody essential for producing Anti-D injections. Committed to helping others, Harrison willingly switched to plasma donation, ensuring his contributions could save as many lives as possible.
“James was a remarkable, stoically kind, and generous person who was committed to a lifetime of giving and he captured the hearts of many people around the world,” Lifeblood chief executive officer Stephen Cornelissen was quoted as saying by Australia’s Nine News.
“It was James’ belief that his donations were no more important than any other donors’, and that everyone can be special in the same way that he was.
“James extended his arm to help others and babies he would never know a remarkable 1173 times and expected nothing in return.”
Robyn Barlow, coordinator of Australia’s Rh Program – designed to prevent Haemolytic Disease of the Foetus and Newborn (HDFN) – said she had been friends with Harrison for nearly 60 years after first recruiting him as a donor.
“He made my job very easy because he was so keen to donate all the time,” Barlow told 7NEWS.com.au.
“I never had to worry about him – I never had to call and say: ‘when you’re coming’, nothing like that, he was there standing in front of me.”
In an interview with NPR in 2015, Harrison said: “I was always looking forward to donating, right from the operation, because I don’t know how many people it took to save my life.”
Several reports pointed out that doctors were not entirely sure why and how Harrison developed this rare blood antibody, though they suspect it may be linked to the transfusions he received at 14 after his surgery.
“Every batch of Anti-D that has ever been made in Australia has come from James’ blood,” Jemma Falkenmire, of the Australian Red Cross Lifeblood (then known as Australian Red Cross Blood Service), told CNN in 2015. “And more than 17 per cent of women in Australia are at risk, so James has helped save a lot of lives.”
Fewer than 200 people in Australia donate Anti-D, yet their contributions help an estimated 45,000 mothers and babies each year, according to the Australian Red Cross Lifeblood.
Scientists from WEHI (Walter and Eliza Hall Institute of Medical Research) in Melbourne, in collaboration with Lifeblood, are working on a project called “James in a Jar” to grow the Anti-D antibody in the lab. Using blood and immune cells from Harrison and other donors, the team has successfully recreated and cultivated the antibody, according to Lifeblood.
This breakthrough could one day help prevent Haemolytic Disease of the Foetus and Newborn, benefiting pregnant women not just in Australia but worldwide, the statement said.
The Independent is the world’s most free-thinking news brand, providing global news, commentary and analysis for the independently-minded. We have grown a huge, global readership of independently minded individuals, who value our trusted voice and commitment to positive change. Our mission, making change happen, has never been as important as it is today.
NC DHHS: Register Now For Community Partners Webinar on Medicaid

Community Partners Webinar – An Update on Medicaid
The Community Partners webinar series is designed to provide updates on NC Medicaid and key Medicaid initiatives.
Join us Wednesday, March 19 from 3-4 p.m. for the next session in our ongoing webinar series. The webinar will provide an informational overview on Medicaid.
To register for the webinar, simply click on the registration link below. Feel free to share the webinar invitation and registration link with other community partners you think would be interested in attending.
Community Partners Webinar – An Update on Medicaid
Wednesday, March 19 from 3-4 p.m.
Click here to register
For more information or questions contact us at [email protected]
*Close captioning is available in English and Spanish. If additional accessibility and communication accommodations are needed, please email [email protected] with the details of your request.
NCMS Member Dr. Debra Bynum Elected to Alliance for Academic Internal Medicine’s Association of Program Directors in Internal Medicine Council

Debra Bynum, MD, MMEL, FACP, has been elected to the Alliance for Academic Internal Medicine’s Association of Program Directors in Internal Medicine Council. Dr. Bynum is a professor of medicine in the UNC Division of Geriatric Medicine, Vice Chair for Education in the UNC Department of Medicine and the Program Director of the UNC Internal Medicine Residency Program.
The Alliance for Academic Internal Medicine (AAIM) promotes the advancement and professional development of its members who prepare the next generation of internal medicine physicians and leaders through education, research, engagement, and collaboration.
A call for nominations was open to members September 11-October 9. Individual councils selected the final candidates for the ballot after review of all eligible nominations. Elections were open to members January 15-February 2. All candidates are elected by a majority of the ballots cast; councils retain authority to appoint individuals to serve in roles with unexpected openings.
Dr. Bynum is a member of the North Carolina Medical Society.
UVA: Discovery Leads To New Way to Prevent Cold Sores

Scientists have discovered how the herpes virus reactivates by hijacking the immune system, opening the door to new treatments.
(Rebecca Shavit) -- Scientists have uncovered a surprising strategy used by the herpes simplex virus (HSV-1) to rewaken in the body. A new study from the University of Virginia School of Medicine has identified a viral protein, UL12.5, that plays a key role in triggering viral reactivation.
The discovery challenges conventional understanding of how the virus escapes dormancy and could lead to new treatments for both cold sores and genital herpes.
The Herpes Virus: A Persistent Pathogen
HSV-1 is a highly contagious virus that infects over 60% of people under 50 worldwide, according to the World Health Organization. Once inside the body, the virus establishes a lifelong presence, lying dormant in nerve cells until reactivated by stress, illness, or even sun exposure.
When HSV-1 infects a cell, the immune system detects its presence through pattern recognition receptors (PRRs), which sense viral components. These receptors activate pathways designed to eliminate the infection. However, viruses have evolved mechanisms to evade or manipulate these defenses.
A particularly surprising discovery is that HSV-1 does not merely wait for favorable conditions to reactivate—it actively participates in its own reawakening by triggering an immune response.
The Role of UL12.5 in Viral Reactivation
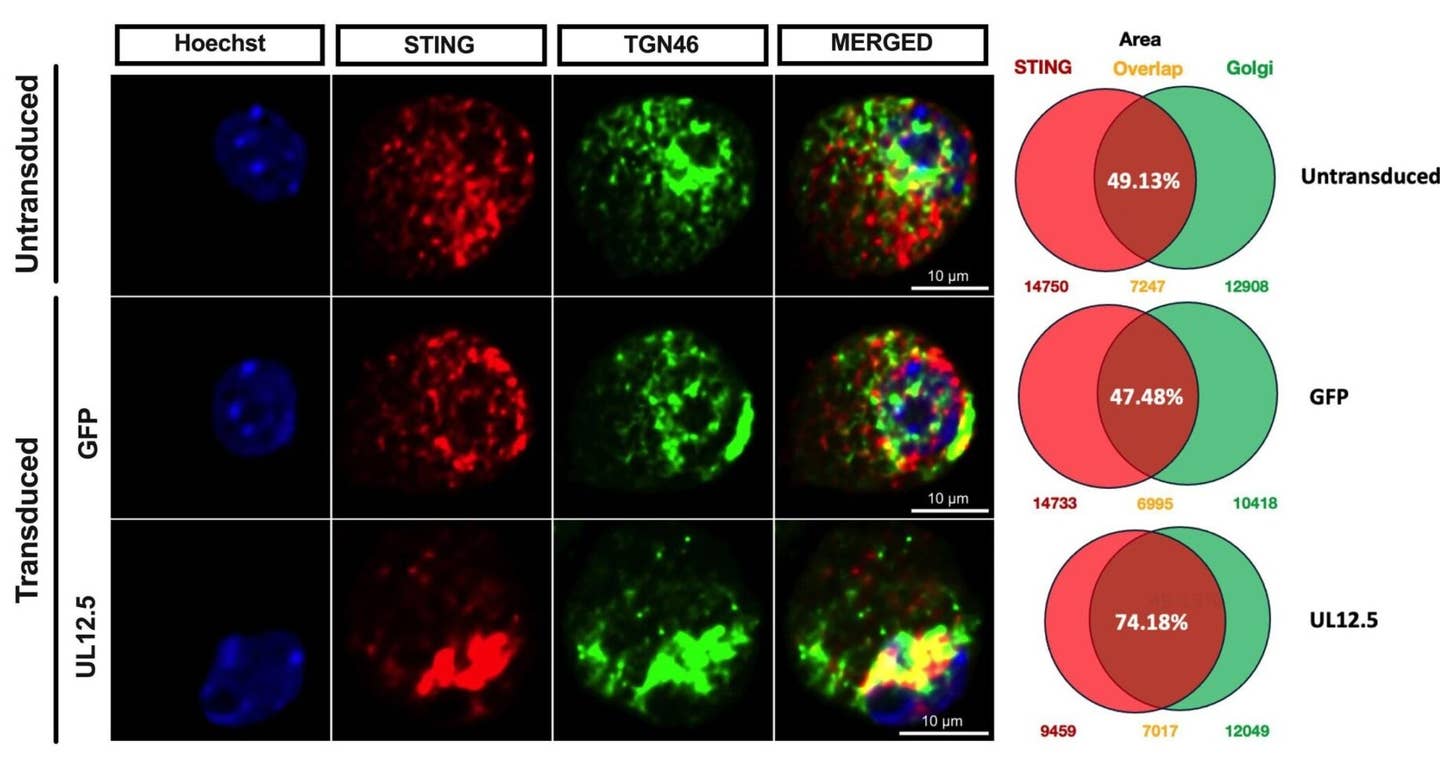
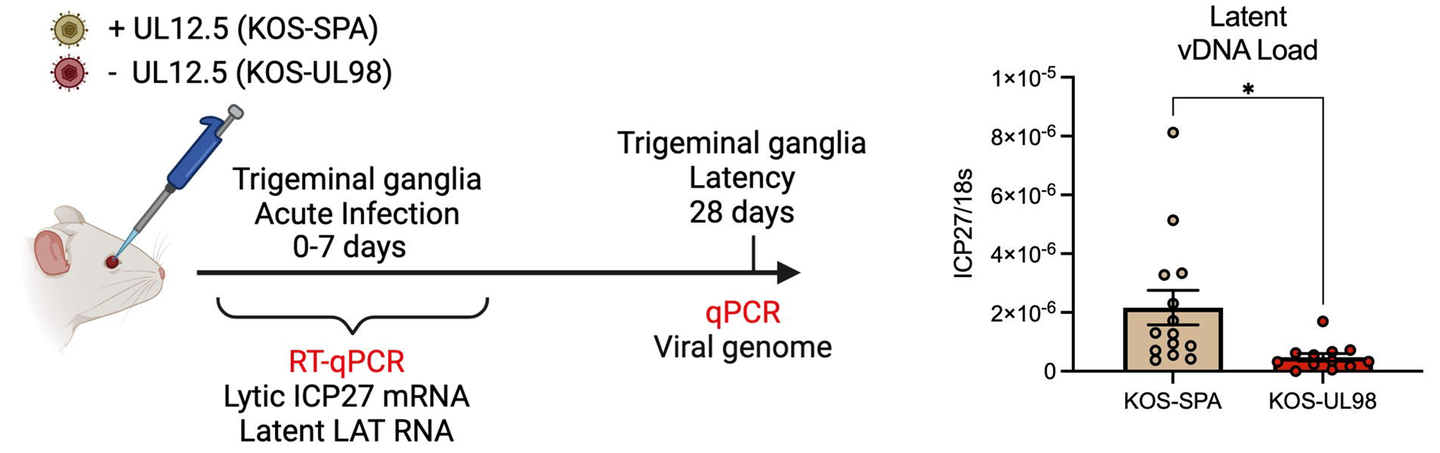
Researchers at UVA, led by Anna Cliffe, Ph.D., found that HSV-1 expresses the protein UL12.5, which stimulates the immune system in a way that paradoxically aids viral reactivation.
UL12.5 targets mitochondria, the cell’s energy-producing structures, causing them to release mitochondrial DNA (mtDNA) into the cytosol. This triggers the cGAS-STING pathway, a major immune response mechanism that typically fights infections.
Under normal circumstances, cGAS detects foreign DNA in the cytosol and activates STING, which initiates the production of interferons and other antiviral molecules.
However, HSV-1 exploits this pathway to reawaken from dormancy. By inducing mitochondrial stress and the release of mtDNA, UL12.5 sets off a chain reaction that promotes viral gene expression and reactivation.
“We were surprised to find that HSV-1 doesn’t just passively wait for the right conditions to reactivate – it actively senses danger and takes control of the process,” said researcher Patryk Krakowiak. “Our findings suggest that the virus may be using immune signals as a way to detect cellular stress—whether from neuron damage, infections, or other threats—as a cue to escape its host and find a new one.”
Implications for Treatment and Prevention
Understanding how HSV-1 manipulates the immune system opens the door to new therapeutic strategies. Current antiviral drugs, such as acyclovir, only suppress viral replication during active infection but cannot prevent reactivation. The discovery of UL12.5’s role in awakening the virus suggests that targeting this protein could prevent outbreaks.
“We are now following up on this work to investigate how the virus is hijacking this response and testing inhibitors of UL12.5 function,” Cliffe said. “Currently, there are no therapies that can prevent the virus from waking up from dormancy, and this stage was thought to only use host proteins. Developing therapies that specifically act on a viral protein is an attractive approach that will likely have fewer side effects than targeting a host protein.”
The study also found that in cases where another infection was present, HSV-1 did not require UL12.5 for reactivation. Instead, the immune response triggered by the second infection was sufficient to wake up the virus. This suggests that HSV-1 can use multiple pathways to reactivate, further complicating treatment strategies.
The Connection to Neurodegenerative Disease
Beyond cold sores and genital herpes, HSV-1 has been linked to serious neurological conditions. Some research suggests that chronic inflammation from repeated HSV-1 reactivation may contribute to diseases such as Alzheimer’s. The ability of HSV-1 to manipulate immune pathways in neurons raises concerns about its long-term effects on brain health.
The virus establishes latency in neurons, where it remains dormant until certain conditions trigger reactivation. The absence of viral proteins during latency means that HSV-1 relies on host signaling pathways to initiate reactivation. One such pathway involves interleukin-1β (IL-1β), a key inflammatory cytokine. Previous studies have shown that IL-1β can induce HSV-1 reactivation by increasing neuronal excitability.
“Our findings identify the first viral protein required for herpes simplex virus to wake up from dormancy, and, surprisingly, this protein does so by triggering responses that should act against the virus,” Cliffe explained. “This is important because it gives us new ways to potentially prevent the virus from waking up and activating immune responses in the nervous system that could have negative consequences in the long term.”
 Schematic of the in vitro HSV latent infection and reactivation model. Neuronal infection was carried out in the presence of acyclovir (ACV; 50 μ M). Reactivation was induced using LY294002 (20 μ M) in the presence of WAY-150138 (20 μ M) to limit cell to-cell spread. (CREDIT: PNAS)
Schematic of the in vitro HSV latent infection and reactivation model. Neuronal infection was carried out in the presence of acyclovir (ACV; 50 μ M). Reactivation was induced using LY294002 (20 μ M) in the presence of WAY-150138 (20 μ M) to limit cell to-cell spread. (CREDIT: PNAS)
With these new insights, scientists hope to develop treatments that prevent HSV-1 reactivation at its earliest stage. Inhibiting UL12.5 or blocking mitochondrial DNA release could be a strategy for reducing outbreaks and preventing the long-term inflammatory effects associated with recurrent infections.
The research has been published in the Proceedings of the National Academy of Sciences (PNAS), marking a significant step forward in understanding how herpes viruses manipulate the immune system.
NC Medicaid Annual Health Disparities Report Released, Needs Your Feedback
Please take a moment and complete this brief survey.
North Carolina Medicaid’s Program Evaluation Team recently released the 2022 NC Medicaid Annual Health Disparities Report (Link) which highlights health disparities identified within quality measures for the NC Medicaid beneficiary population. We are reaching out to you to see if you would be willing to review the 2022 NC Medicaid Annual Health Disparities Report and complete a brief survey to provide feedback (survey linked here).
The purpose of the 2022 NC Medicaid Annual Health Disparities Report is to not only identify disparities, but to highlight opportunities NC Medicaid and its partners have to address them. In addition to the full report, we released 6-page brief highlighting key takeaways from the report (Link).
NC Medicaid is committed to championing equitable health outcomes for the 3 million North Carolinians it serves and acknowledges that progress requires active community and partner involvement. As this is the first year that this report has been released, it is critical to engage with partners, like yourself, to shape this important annual report into a responsive, partner-engaged, useful, and relevant tool.
The survey will be open until Monday April 14th 2025. You do not have to review the entire 2022 Annual Health Disparities Report to provide feedback; we are grateful for any level of engagement you have the capacity to offer.
Please contact [email protected] with any questions or concerns regarding the report or survey. Please also feel free to pass along this email/survey link to anyone who might be interested in leaving feedback on the NC Medicaid Annual Health Disparities Report. We look forward to receiving your feedback!
Duke Health and Novant Health Launch Transformative Partnership

Duke Health: Together, the organizations will expand access to affordable, high-quality care for North Carolina communities
DURHAM and WINSTON-SALEM, N.C. -- Duke Health and Novant Health are working together to develop new campuses across North Carolina that will expand access to affordable, high-quality care. The two organizations share a commitment to developing novel partnerships to improve health outcomes for more communities across the region and provide an exceptional patient experience for all.
“We’re taking bold steps to bring the excellence and innovation of Duke Health to more patients, in more ways, across more communities,” said Craig Albanese, MD, chief executive officer of Duke University Health System, “and we’re energized by the possibilities of what we can accomplish in collaboration with Novant Health for communities across our region.”
The two organizations believe collaboration is the way forward for reaching new heights and helping their team members and patients succeed.
“We have a shared vision for what healthcare can look like, and our collaboration means the communities we serve together will benefit from our combined focus on quality, innovation, and excellence in patient care and experience,” said Carl S. Armato, CPA, MBA, president and chief executive officer, Novant Health.
Patients and community members can expect many benefits from these sites, including improved access to care, enhanced specialty services, and telehealth and virtual care options.
Quality is core to this collaboration, and both organizations share a commitment to high-quality care for North Carolina communities. Clinicians from Novant Health and Duke Health will be available in new locations, increasing access to both primary care and advanced specialty treatments. More locations mean shorter wait times and more appointment availability. The collaboration will also explore ways to empower patients with more opportunities to connect with specialists virtually.
The organizations expect construction for the first sites to begin this summer and fall, with each site to open approximately 18 months after the start of construction. Additional updates will be shared as the collaboration progresses in the coming months.
10 Ways North Carolina Health Care Providers Are Harnessing AI

Is NC Leading the Way on Artificial Intelligence?
(NC HealthNews, Emily Vespa and Michelle Crouch) --
Co-published with The Charlotte Ledger
Faced with a growing health care worker shortage and provider burnout, some North Carolina health care leaders have said there is great promise in artificial intelligence systems.
The state’s health care systems have been early adopters of AI tools — overt and invisible — that are shaping the patient and provider experience. Across North Carolina, AI is helping providers predict health risks, communicate with patients and manage administrative tasks.
Here are 10 ways North Carolina health care providers are using AI.
1. AI helps doctors diagnose lung cancer
Some Atrium Health doctors are using AI to help catch lung cancer in its early stages.
When pulmonologists find a lung nodule on a scan, they consider factors such as the patient’s medical history to assess lung cancer risk. Physicians might recommend a lung biopsy to a high-risk patient, but they avoid an unnecessary procedure if a patient is low risk.
Like many health systems across the country, Atrium Health and WakeMed have turned to AI to help manage the flood of messages their clinical teams receive through patient portals.
Since the pandemic, the number of messages to doctors has skyrocketed, adding to clinicians’ already packed workloads and increasing stress.
WakeMed has reduced patient portal messages by 12 to 15 per provider per day by using AI to draft responses, filtering out unnecessary messages and forwarding some messages to other staff members, according to an article in Becker’s Hospital Review.
At Atrium, AI drafts “initial responses to patient messages that the team then edits before sending,” a spokesman said in an email.
NCMS at Work: 2025 Advocacy Summit Explores Economic Trends, AI, and Legislative Impact

NCMS holds crucial summit on the future of healthcare in NC
Healthcare professionals, policymakers, and industry experts gathered for a crucial summit addressing the future of healthcare in North Carolina. The event featured discussions on healthcare economic trends, legislative policies, and the integration of artificial intelligence (AI) in clinical and administrative settings.
The summit kicked off with a Healthcare Economic Forecast where industry expert Ed Gaines, JD, provided an in-depth analysis of the financial trends shaping healthcare across the state and the nation. His session underscored the growing financial pressures on healthcare systems and the importance of policy adaptation.
A major legislative topic of the day legislative innovation. Senator Benton Sawrey (R-Johnston) outlined the evolving role of Clinical Pharmacist Practitioners professionals in healthcare teams. His discussion emphasized how expanding the responsibilities of Clinical Pharmacist Practitioners could enhance patient care and alleviate burdens on primary care physicians.
Artificial Intelligence emerged as a dominant theme at the Advocacy Summit, with multiple breakout sessions exploring its implications in healthcare. The Artificial Intelligence & Prior Authorization session, led by Dr. Deborah Kaye, examined how AI can streamline the prior authorization process, reducing administrative delays and improving patient access to care. A broader discussion on AI’s role in healthcare, with UNC Chief Information Officer David McSwain, showcased how emerging technologies are transforming diagnostics, patient management, and clinical decision-making.
The Healthcare Legislative Panel brought together lawmakers actively shaping healthcare policy in North Carolina including Representative Tim Reeder, MD (R-Pitt) and Senator Jay Chaudhuri (D-Wake). Their discussion focused on pressing legislative efforts, including initiatives to address provider shortages and improve healthcare access across rural and urban communities.
Innovative solutions were also explored through breakout sessions, including one on the Interstate Licensure Compact, which aims to ease medical licensing across state lines to improve provider mobility and address workforce shortages. Another session examined the role of mobile clinics, highlighting how these units can expand healthcare access to underserved populations and assist in future natural disasters.
The event concluded with a Town Hall Discussion, where attendees engaged with North Carolina Medical Society CEO Chip Baggett on policy issues affecting their practices and communities.
With a packed agenda addressing critical topics, this year’s healthcare summit underscored the need for collaborative policy-making and innovation to navigate the evolving landscape of healthcare in North Carolina.
New Study: Blood Test Can Help Diagnose, Track ALS Patients

A blood test can help doctors detect ALS
(HealthDay News, Dennis Thompson) -- A blood test can help doctors detect ALS, or amyotrophic lateral sclerosis, and predict how the degenerative disease will progress in patients, a new study suggests.
People with ALS have three times higher blood levels of neurofilament light chain proteins, which are produced when nerve cells are injured or die, than people with other
A blood test looking for neurofilament light chain proteins accurately identified ALS patients more than 80% of the time, researchers said.
The test also can help predict survival for people with ALS, results show.
Within a year, more than 40% with neurofilament light chain proteins below a certain set point were still alive. None with levels above that point remained alive.
"While more research needs to be done to confirm these findings, having better information about prognosis is valuable for people with ALS and their families as well as the doctors who treat them," senior researcher Dr. Sylvain Lehmann, director of the University of Montpellier's Institute for Neurosciences in France, said in a news release.
ALS, also known as Lou Gehrig's disease, is a progressive disease that affects nerve cells in the brain and spinal cord. Nerves that signal and control muscles degenerate, causing patients to lose control of their movement.
For the study, researchers compared blood samples from 139 patients with ALS against 70 from patients with other similar brain disorders like lower motor neuron disease and primary lateral sclerosis.
The research team looked specifically at three potential types of blood markers: neurofilament light chain proteins, glial acidic proteins and phosphorylated tau 181.
Glial acidic proteins are released when cells work to repair injury, and phosphorylated tau 181 is linked to the buildup of toxic amyloid proteins in the brain, a hallmark of Alzheimer's disease.
"Having an effective biomarker can be highly valuable -- in addition to helping in making the diagnosis, it can help in predicting prognosis, evaluating what stage of the disease people are in, and tracking their progress or their response to treatments," Lehmann said.
Results showed that neurofilament light chain protein levels provide a much better means of detecting and tracking ALS than the other two measures.
The other two markers produced accurate results only about 50% of the time, researchers said.
NIH Study: New 4D Brain Map Reveals Potential Early Warning Signs of Multiple Sclerosis

March is Multiple Sclerosis Awareness Month. The National Institutes of Health is out with a new study on potential early warning signs.
New 4D Brain Map reveals potential early warning signs of multiple sclerosis
NIH study reveals key players underlying disease onset and repair.
Using an animal model of multiple sclerosis (MS), researchers at the National Institutes of Health (NIH) have created a four-dimensional brain map that reveals how lesions similar to those seen in human MS form. These findings, published in Science, provide a window into the early disease state and could help identify potential targets for MS treatments and brain tissue repair.
The researchers, led by postdoctoral fellow Jing-Ping Lin, Ph.D., and senior investigator Daniel S. Reich, M.D., Ph.D., both at NIH’s National Institute of Neurological Disorders and Stroke (NINDS), combined repeated MRI imaging with brain-tissue analysis, including gene expression, to track the onset and development of MS-like lesions. They uncovered a new MRI signature that can help detect brain regions at risk for damage weeks before any visible lesions occur. They also identified “microenvironments” within affected brain tissue based on observed patterns of neural function, inflammation, immune and support cell responses, gene expression, and levels of damage and repair.
“Identifying the early events that occur after inflammation and teasing apart which are reparative versus which are damaging, can potentially help us identify MS disease activity sooner and develop treatments to slow or stop its progression,” said Dr. Reich.
MS is caused by the body’s immune system attacking the protective covering of nerve fibers, called myelin. This leads to inflammation, loss of myelin, and formation of “lesions” or “plaques” within the brain tissue. Most of what is known about MS progression has come from analysis of postmortem human brain tissue, usually obtained decades after the initial onset of disease. This means missing early changes that occurred prior to the onset of symptoms.
To mimic the conditions of the human brain, the researchers opted not to use a mouse model for MS, instead advancing a model that uses the marmoset, a nonhuman primate. Compared to mouse brains, marmoset and human brains have a higher ratio of white matter (the “wires” of the brain) to gray matter (neuronal cell bodies). The marmoset model creates multiple lesions that closely resemble those seen in human MS and that can be tracked in real time using MRI imaging. Because these lesions can be induced experimentally, the model offers a look at the earliest stages of inflammation and immune responses that lead to MS-like demyelination.
One key player identified was a specific type of astrocyte, one of the support cell types in the brain, that turns on a gene called SERPINE1 or plasminogen activator inhibitor-1 (PAI1). They found SERPINE1-expressing astrocytes in vulnerable brain borders before visible damage occurs, clustering near blood vessels and the fluid-filled ventricles of the brain and signaling future areas of lesion development. These astrocytes also appeared to influence the behavior of other cells near the lesion area, including the ability of immune cells to enter the brain and contribute to inflammation, as well as the precursor cells involved in myelin repair.
Given that SERPINE1-expressing astrocytes accumulated at the edges of growing lesions, where damage happens but healing also begins, their potential dual role in coordinating signals that could lead to either tissue repair or further damage was an unexpected wrinkle that will require further study. It’s possible that the earliest responses could be a part of a protective mechanism that becomes overwhelmed as the injury progresses. It’s also possible that the same mechanism could itself become disease-causing.
“If one imagines a fort under siege, initially the walls might hold off the attack,” said Dr. Reich. “But if those walls are breached, all the defenses inside can be turned against the fort itself.”
These findings may also have implications for brain injuries beyond what is seen in MS. While there are different types of focal brain injuries, including traumatic brain injury, stroke, inflammation, and infection, there is a finite number of ways the tissue can react to injury. In fact, many of the reactions seen here to inflammation, stress, and tissue damage are likely to be common across injury types, and the brain map created in this study can act as a resource to allow comparisons to be made in a more human-like context.
The scientific teams are building a new model of a different autoimmune condition affecting brain borders. They are also looking to expand their data set to include aged animals, which could help improve our understanding of progressive MS, a disease state with a significant and unmet therapeutic need.
This study was supported in part by the Intramural Research Program at the NIH with additional support from the Dr. Miriam and Sheldon G. Adelson Medical Research Foundation and the National Multiple Sclerosis Society.
About the National Institute of Neurological Disorders and Stroke (NINDS): NINDS is the nation’s leading funder of research on the brain and nervous system. The mission of NINDS is to seek fundamental knowledge about the brain and nervous system and to use that knowledge to reduce the burden of neurological disease.
About the National Institutes of Health (NIH): NIH, the nation's medical research agency, includes 27 Institutes and Centers and is a component of the U.S. Department of Health and Human Services. NIH is the primary federal agency conducting and supporting basic, clinical, and translational medical research, and is investigating the causes, treatments, and cures for both common and rare diseases. For more information about NIH and its programs, visit www.nih.gov.
Happy Birthday to All These NCMS Members!

Grab your party hats and noisemakers and let’s celebrate!
Happy birthday to all of these NCSM members!
Robert B. Abrahams, DO
Yousef S. Abumostafa, MD
Ian Adam, MD
Mia R. Adkins, MD
Amir Aghajanian, MD
Mamatha Agrawal, MD
Lysle K. Ailstock, MD
Raul C. Aizcorbe, MD
Muhammad S. Alam, MD
Kyle A. Alexander, MD
Kimberly A. Alford, MD
David J. Allison, MD
- Kevin Allred, PA-C
Ishwari S. Amin, PA-C
Rakesh D. Amin, MD
David T. Anderson, MD
Jeffery S. Anderson, MD
Vincent C. Andracchio, MD
Jacob C. Andrews, DO
Tanya E. Anim, MD
Jamie M. Anthony, MD
Nicole E. Aristy, MD, FAAP
Robert F. Armstrong, MD
Vikram Arora, DO
Melanie R. Artho, MD
Michael S. Artman, MD, FAAP
Isaac Asemota
Adedayo O. Ashana, MD
Malick V. Bachabi, MD
- Russell Bailey, MD, FACC
Stephanie L. Balkman, PA-C
James D. Ball, MD
Elizabeth B. Baltaro, MD
Edwin C. Bartlett, Sr., MD
Joshua S. Baru, MD
Julie M. Bass Ransom, PA-C
Edgar H. Batcheller, Jr., MD
Darren A. Bates, PA-C
Shayne E. Bates, MD
Thomas E. Bates, MD
Alan S. Baumgarten, MD, MPH
Jeffrey S. Beecher, DO
Amber M. Beg, MD
Christiana J. Bernal, MD
Joe D. Bernard, MD
Gregory M. Bertics, MD
Margaret L. Bertrand, MD
Navin C. Bhojwani, MD
Preecha Bhotiwihok, MD, MPH
George A. Binder, MD
Richard E. Bird, MD
Taylor M. Bishop, MS, PA-C
Jeffrey R. Blackburn, MD
Jamie E. Bleyer, MD
Zachary T. Blom, MD
Bruce S. Boliek, MD
Rodolfo Bonatti, MD
Jeffrey Borders, MD
Jared B. Bowns, MD
Brian A. Boyd, MD
Robin Boyd-Kranis, MD
Tyler C. Bradley, PA-C
Ashley J. F. Brandon, MD
Andrew R. Brant, MD
Lori C. Bridges, PA-C
George M. Brinson, MD
Thomas E. Brock, MD
Brian K. Brodwater, MD
Jeffrey A. Brody, MD
Melissa C. Brooks, MD
Bradley J. Broussard, MD
Cynthia J. H. Brown, MD
Jared W. Brown, MD
Richard F. Bruch, MD
Matthew J. Bruehl, MD
Vardaman M. Buckalew, Jr., MD
Philippe I. Bulauitan, MD
Donald K. Bulla, PA-C
Joseph M. Bumgarner, MD
Edwin K. Burkett, MD
Aaron M. Burman, PA-C
- Patrick Burney, MD
Merle R. Busby, MD
Parag Butala, MD
Jerome M. Butler, Jr., MD
Brian R. Cabarrus, MD
Elaine S. Cabinum-Foeller, MD, FAAP
Dwayne D. Callwood, MD
Thomas K. Carlton, Jr., MD
Dennis D. Carmichael, MD
Laurel E. Carter, MD
Margaret F. Carter, MD
Steven R. Carter, MD
Virginia F. Casey, MD
- Daniel Catz, MD
Margaret E. K. Champion, MD
John S. Chang, MD
Dev R. Cheti, MD
John C. Childress, III, MD
Katherine E. Chockley-Nystrom, PA-C
Christina H. Choe, MD
Pola A. Chojecka, MD
Michele M. Clancy, MD
Robert E. Clark, MD, PhD
Jim R. Cleary, MD
David A. Clements, II, MD
Margaret R. Clifton, DO
- Leslie Clinton, Jr., MD
Timothy E. Cloninger, MD
Michael R. Coan, MD
Ann S. Collins, MD
Matthew P. Conti, DO
Adelaide R. Cooke
Dana D. Copeland, MD
Donald L. Copeland, MD
Mark W. Cornelius, MD
Alexandra F. Covington, PA
Kennedy Cowan, PA-C
Karen D. Coward, MD
Kirsten S. Cox, MD
James S. Coxe, III, MD
William L. Craig, III, MD
Larry M. Crane, MD
Adam C. Creech, MD
Matthew A. Creighton, MD
Lori K. Crihfield, DO
Daniel L. Crocker, MD
Charles C. Crowell, III, MD
John B. Crudup, III, MD
Nathan S. Cuka, MD
Edith R. Curry, MD
Richard F. Curtis, MD
Matthew A. Daka, MD
Thomas L. D'Alessio, MD
Michael B. Daley, MD
Julie Daniel, DO
Laura F. Danile, MD
John D. Davis, Jr., MD
Jeffrey R. Daw, MD
Troy C. Dawley, DO
Lindsey E. de Guehery, MD, FACP
Gary J. DeFilipp, MD
Bridget M. Degele, MD
Derek W. DelMonte, MD
Eric J. DeMaria, MD
William T. Derry, MD
Maureen Despres, MD
Jane D. Dewire, MD
Crystal M. Dickson, MD, MPH
Robin Dimitrious, MD
Steven A. Dingeldein, MD
Jakub M. Dmochowski, MD
Robert M. Doline, MD
Shannon B. Dowler, MD
Shannon M. Drohan, MD
Douglas A. Drossman, MD
Elizabeth D. Dryden, PA-C
Josiah W. Duke, MD
Melissa B. Duncan, MD
Thaddeus L. Dunn, MD
Sarah K. Dusel, PA-C
Daniel P. Dwyer, MD
Caroline A. Early, MD
- Shelton Earp, III, MD
- Stephen Edwards, MD
Kent R. Edwards, Jr., MD
Vance H. Edwards, MD
Bryan A. Ehlert, MD
Carl J. Eisenberg, MD
Mohamed T. El-Kara, MD
Sherif O. El-Mahdy, MD
- Mark Englehardt, MD
Paul N. Erckman, MD
Heath B. Ergas, MD
John M. Erickson, MD
Vaishali G. Escaravage, MD, FAAD
William M. Eubanks, Jr., MD
Uzma S. Faheem, MD
William L. Fangman, MD
John C. Faris, MD
Justin D. Faulkner, MD
Callie R. Faust, PA
Robert A. Ferguson, DO
Daniel H. Fertel, MD
Zachary B. Fisher, MD
Nicholas J. Fitzsimons, MD
Gitanjali M. Fleischman, MD
Herbon E. Fleming, MD
Joseph P. Flynn, DO
Adam W. Fosnaugh, MD
John D. Franklin, MD
Earl A. Frantz, DO
Darrell W. Freeman, MD
Jon E. Fromke, MD
Elaina K. Furr, DO
Robert H. Gaither, MD
Amanda R. W. Galluppi, PA-C
Michael L. Garner, MD
John W. Garrett, MD
Timothy M. Gast, PA-C
Matthew P. Geib, DO
Mathew George, MD
Wood B. Gibbs, MD
Herman A. Godwin, Jr., MD
Kyle T. Golden, DO
Jason F. Goldie, MD
Barbara L. Goldman, PA-C
Tristan Gonzalez Sanz, MD
Allison C. Gordon, PA-C
Daniel S. Gordon, MD
Hormoze A. Goudarzi, MD
Matthew R. Grafenberg, MD
William M. Gramig, III, MD
Patrick D. Green, MD
Thomas M. Green, Jr., DO
Chad C. Greer, MD
Amardeep S. Grewal, MD
Amy M. Griffin, MD
John P. Grimm, MD
Sarah R. Grossman, MD
Kelly R. Grove, DO, FAAP
Leah M. Gruber, PA
Mark J. Gruchacz, MD
Marc F. Guerra, MD
David R. Guillen, MD
Alison P. Guptill, MD
Shauna L. Guthrie, MD, MPH
Amy Guttmann, MD
Jason C. Haag, MD
Trevor Hackman, MD
Jeremy M. Hackworth, MD
Elizabeth S. Hagenmaier, DO
Gene T. Hamilton, MD
Jonathan A. Hancher, MD
Charin L. Hanlon, MD, FACP
Perry M. Harmon, MD
Willard C. Harrill, MD, FACS
James A. Harris, MD, FACS
Tina G. Harris, MD
David L. Harshman, MD
Omer A. Hassan, MD
Robert E. Hassler, MD
James H. Hawkins, Jr., MD
Seth C. Hawkins, MD
Sherman M. Hawkins, Jr., MD
Steven B. Heavner, MD
Kathryn J. Hecker-Magee, MD
Sadananda B. Hegde, MD
William D. Heizer, MD
Joel H. Heller, MD
George P. Henderson, Jr., MD
Richard R. Henderson, MD
Mark D. Henin, MD
Victoria M. Herriott, MD
Marc A. Herschelman, DO
John D. Hewitt, MD
David L. Hill, MD, FAAP
Shannon N. Hill, MD
Nancy M. Hill-Price, MD
Thomas R. Hinson, Jr., MD
Jason G. Ho, MD
Marcus A. Hodges, MD
Bennett R. Hollenberg, MD
Adrian W. Holtzman, MD
Andrea L. B. Honeycutt, MD
Janice R. Hong-Messier, MD
James B. Hooker, MD, MPH
William W. Hope, MD, FACS
Jeffrey J. Horvath, MD
Robert G. Howard, Jr., MD
Edward V. Hudson, MD
Michael B. Huggins, MD
Karrar Husain, MD
Farah S. B. A. Hussain, MD
Lourdes Illa-Sanchez, MD
Isaac L. Jaben, MD
William R. Jacobs, MD
Elizabeth G. Jarvis, MD
Casey V. Jeffreys, MD
Jerome E. Jennings, MD
Sarah C. Jernigan, MD
Jolene R. Jewell, MD
Andrew E. Johansen, MD
Charles S. Johnson, MD
Kenneth L. Johnson, II, MD
Kamlyn Jones, MD
Steven A. Josephson, MD, FACP
Patrick K. Jowdy, MD
Walton K. Joyner, Jr., MD
Beatriz E. Juncadella, MD, FAAP
Hassan Kahi, MD
Ciamack Kamdar, MD
Barry K. S. G. Kang, MD
Leonardo Kapural, MD, PhD
Kenneth S. Karb, MD
Stephen L. Kash, MD
Jane B. Kehaya, MD
Mary K. Keith, MD
Jessica K. Kim, DO
Paul S. Kim, MD
Sarah Kim, MD
Seung W. Kim, MD
Stephen W. Kimmel, MD
Edgar W. Kirby, IV, MD
David Kirk, MD
Alvin P. Kitchin, Jr., MD
Bert J. Klein, III, MD
Steven D. Klein, MD
John T. Klimas, MD
Christine T. Knettel, MD
Margaret M. Kocsis, MD
Dennis D. Kokenes, MD
Aaron Kollross, MD
Kenyn L. Koop, MD
Amy M. Kornegay, PA-C, MPAS
Jonathan H. Kornegay, MD
Walter T. Koscielniak, III, MD, FAAP
Jeffrey M. Kotzan, MD
Michael V. Krasnokutsky, MD
Ronald E. Krum, MD
Andrew J. Kubinski, DO, MS
Jeffrey G. Kuremsky, MD
Andrew S. Laird, PA-C
Venkatesh Lakshman, MD
David R. Lane, MD
Fred D. Lassiter, MD
Adeyemi A. Lawal, MD
Mary Katherine Lawrence, MD
Robert L. Lawrence, MD
Mary Lou Lawson, MD
Daniel P. Leas, MD
Daniel P. Lee, DO
Jinoo T. Lee, MD
Julie V. Levengood, MD
Ronald H. Levine, MD
Frederic E. Levy, MD
Jay B. Levy, MD
Caroline H. Lewis, PA
Katherine M. Lewis, MD
Andrew I. Light, MD
Alexander J. Lim, MD
Dimitrios P. Lintzeris, DO
Timothy L. Lockamy, DO
Hillary E. Lockemer, MD
Thomas T. Long, III, MD
Sonya B. Longest, MD
William P. Lorio, MD
Jennifer M. Lovin, MD
Macie N. Lucas, PA-C
Donald T. Lucey, MD
Edward B. Mabry, MD
Damien C. Macaluso, MD
- Alexis MacDonald, Jr., MD
Kevin A. MacDonald, MD
Graham L. Machen, MD
David M. Macknet, MD
John P. Mahaney, Jr., MD
Alden B. Maier, MD, FACS
Anita M. Makowski, PA-C
Morton D. Malkin, MD
Michael S. Mallonee, MD
Vijaysinha A. Mandhare, MD
Peter G. Mangone, MD
Allegra L. Marino, PA-C
Charles F. Marshall, Jr., MD
Charles R. Martin, MD
Michael M. Marushack, MD
- Benno Marx, MD
David P. Mason, MD, FACOG
Dylan P. Matthews, MD
Robert D. Matthews, MD
Karen E. Mayer, MD
Bradley T. McCall, MD
Samuel G. McCaskill, Jr., MD
John T. McCormick, MD
Marion M. McCrary, MD
Gordon R. McDevitt, Jr., MD
Michael McFayden
Christopher E. McGowan, MD
James S. McGrath, MD, MPH
Scott T. McGraw, MD
Sheppard A. McKenzie, III, MD
Joseph T. McLamb, MD
Michael E. McLeod, MD
Thomas K. McMahan, MD
- Eugene McMurry, Jr., MD
Ryan P. McWey, MD
Andrew M. Mealin, DO
Everett Melcher
Stephen J. Melson, MD
Matthew J. Merritt, DO
Allyson C. Metro, MD
Jobe C. Metts, III, MD
Michael A. Meuse, MD
- Alexander Mewborn, Jr., MD
Stephen C. Meyers, MD
Joel B. Miller, MD
Justin D. Miller, MD
Leona A. Miller, MD
Meagan P. Miller, PA-C
David D. Miner, MD
Richard W. Minielly, MD
Bonnie E. Minnick, PA-C
Henry T. Mixon, MD
Mark B. Moeller, MD
Ali S. Mofrad, MD
Joseph A. Molitierno, Jr., MD
Michelle J. Moore, PA-C
Scott M. Moore, MD
Marie A. Moser, MD
Derek W. Moss, MD
Gregory J. Mosteller, MD, FACEP
Gary J. Mullen, Jr., MD
James B. Muller, MD
Robert L. Munt, Jr., MD
Gregory F. Murphy, MD, FACS
Sean M. Murphy, MD
Laura W. Murray, MD
Ethan J. Musgrave, MD
John S. Muus, MD
Wissam E. Nadra, MD
Manjula Nagaraja, MD
Aswani S. Naidu, MD
Patrick J. Nailer, MD
Musharraf Navaid, MD
Shahla Naz, MD
Deanna M. Neigh, PA-C
Ronald J. Neimkin, MD
Matthew J. Newsome, MD
Chelsea K. Ngongang, MD
Nathaniel P. Nonoy, MD
Christopher J. Norbet, MD
Ray G. Norby, MD
Sylvanus W. Nye, MD
Ada T. Ogunsiakan, MD
Alfred E. Okeke, MD, FACE
Andrea S. Orr, PA-C
Nicomedes G. Osalvo, PA-C
Jesse E. Otero, MD
Jason T. Owens, PA-C
Jill M. Pappalardi, MD
Brittany N. Papworth, MD
Kinjal R. Parikh, DO
Norman H. Parks, MD
Laura A. Parra, MD
Cornelius T. Partrick, MD
Ann S. Pate, MD
Bhavesh B. Patel, MD, MBA
Bindit S. Patel, MD
Chirag K. Patel, MD
Mahendra S. Patel, MD, FACP
Shil K. Patel, MD
Viral D. Patel, MD
Nadine Pechter, MD
Uma B. Pendem, MD
Joshua J. Penninger, MMS, PA-C
Jennifer F. Pensado, DO
James R. Perrott, MD
James L. Perruquet, MD
Kirk D. Peterson, MD
Wesley F. Phillips, MD
Andy Phung, DO
Edward T. Plyler, MD
George Podgorny, MD
John J. Poggi, MD
Ronald D. Polite, MD
Morris A. Pollock, MD
Frederick L. Potts, III, MD
Demetri T. Poulis, MD, FACS
Jess A. Powell, III, MD
Thomas G. Powers, MD
Steven D. Prakken, MD
David H. Priest, MD
Randall L. Proctor, Jr., MD
Magally Prosper, MD
- Watson Pugh, Jr., MD
Matthew K. Rapp, MD
Eric Rappaport, MD
Deborah L. Rasmus, MD
Michael G. Ribadeneyra, MD
John R. Rice, MD
Lucian C. Rice, Jr., MD
Donna M. Richardson, MD, MBA
- Paul Rieker, Jr., MD
- Wayne Riggins, MD
Rebecca C. H. Riley, MD
Kenneth M. Robert, MD
Surry P. Roberts, MD
Justin D. Rodriguez, MD
Kevin P. Rooney, PA-C
Manfred S. Rothstein, MD
Perry J. Roy, MD
Mary K. Rudyk, MD
Donald B. Russ, MD
Michael B. Russell, MD
Sarah D. Ryan, MD, FAAP
Isami Sakai, DO
Richard G. Saleeby, Jr., MD
Rodrigo T. Samodal, Jr., MD
Joseph L. Sampson, Jr., MD
Geetha Samuel, MD
Terry Sarantou, MD, FACS
Adam W. Saucerman, MD
Mariam S. Sauer, MD
Shannon M. Sawin, MD
Lauren A. Scarfo, PA-C
Robert S. Schaefer, MD
Jill A. Schaeffer, MD
Charles P. Scheil, MD
Shadley C. Schiffern, MD
Herbert M. Schiller, MD
Gregory F. Schimizzi, MD
David M. Scholle, MD
Brandon W. Schoonover, PA-C
Amanda L. Schuman, PA-C
Curtis W. Schupbach, MD
Joshua D. Schwartz, MD
Amanda A. Scott, MD
Blake K. Scott, MD
Zeni Scott, MD
Daniel P. Seeburg, MD, PhD
Christian D. Selby, PA-C
John W. Sensenbrenner, MD
William D. Shaw, Jr., MD
Ronald B. Shealy, MD
Rashid A. Sheikh, MD
Kellie Shell, MD
Meredith L. Shillinglaw, PA-C
Amy J. Shipley, MD
Melissa F. G. Shipley, MD
- Philip G. Singer, MD
Adrienne H. Singleton, MD
Brent M. Skiver, DO
Benjamin D. Smith, MD
Daniel J. Smith, MD
Todd C. Snyder, MD
Ralph Snyderman, MD
Michael F. Soboeiro, MD
Anjali Solanki, DO
Taylor R. Sorensen, PA-C
Andrea H. Sparr, PA-C
Blake A. Stacey, MD
Daniel J. Stackhouse, MD
Ronald J. Stanley, MD
Joslin Stanton, DO
Eric C. Statz, MD
Laura A. Steinmeyer, MD
Sharon R. Stephenson, MD, FACOG
Amy E. Stinson, DO
Krista M. Stocke, PA-C
Leon E. Stockton, MD
Jennifer K. Stoddard, MD
Taylor J. Stone, MD
Megan K. Straughan, MD
Jacob J. Subash, MD
- Alan Summers, MD
John P. Surratt, MD
Carisa M. Sutherland, MD
Mark J. Sutherland, MD
Dylan J. Suttle, MD
Charlotte A. Sweeney, MD, FACOG
John T. Sweeney, MD
Charlie L. Sykes, Jr., MD
Michael G. Taggart, MD
Christopher P. Tanzie, MD
James A. Tart, MD
Syed T. Tasleem, MD
David H. Tate, MD
David T. Tayloe, Jr., MD, FAAP
Britton E. Taylor, MD
Jeffrey S. Taylor, MD
Antonia G. Tettamanti, MD
Vipul V. Thakkar, MD
- Alexander Thomas, MD
Laura O. Thomas, MD
Bridget N. Thompson, PA-C
Christopher M. Thompson, MD
Corey A. Thompson, MD
Ricky A. Thompson, MD
Timothy A. Tolson, MD
Shannon K. Tomlinson, MD
Kevin M. Trapani, DO
Joseph E. Tripp, MD
Richard D. Ulstad, PA-C
Hiren M. Umrania, MD
Bailey H. Underhill, PA-C
Henry A. Unger, MD, FACS
Paul A. Vadnais, MD
Bradley S. Van Dyke, MD
Christopher J. Van Ooteghem, PA-C
William J. Vanarthos, MD
Rajat Varma, MD
Irene Vasko, DO
Marie O. Ventre, MD
Ronald J. Viola, MD
Paul E. Viser, MD
Joshua I. Vogel, MD
George M. Wadie, MD, FACS
Joshua A. Wallace, MD
Daniel B. Wallihan, MD
Matthew C. Ward, MD
Jeffrey D. Warden, MD
Raymond G. Washington, Jr., MD
Bradley J. Wasserman, MD, FAAP
Tyler S. Watters, MD
- Boyd Watts, MD
Samuel H. Weatherford, PA-C
William J. Weatherly, MD
Joseph J. Wehner, MD
James E. Weilbaecher, Jr., MD
Elizabeth S. Weinberg, MD, FACS
Stefan C. Weiss, MD, FAAD
Carl L. Welch, MD
Earl P. Welch, Jr., MD
Kimberly E. Wells, MD
Mark G. Wertman, MD
Jennifer K. E. Whitham, MD
Donna J. Whitt, MD
Thomas B. Wiggins, MD
Aaron T. Wild, MD
Rhoderick T. Williams, Jr., MD
William T. Williams, Jr., MD
Kristin J. Williams Brown, MD
Sarah B. Wilson, MD
Andrew Win, MD
Emily R. Wirt, PA-C
Daniel E. Wise, MD
James B. S. Wise, MD
Colleen L. Wisnosky, PA-C
James C. Womble, MD
John H. Wood, III, MD
Michael G. Woodcock, MD
Tanya Sue Woodson, PA-C
Robert W. Woodward, MD
Alfred H. Woodworth, MD
Joe H. Woody, MD
Aldona Z. Wos, MD
Eileen M. Wright, MD
Farhad K. Yazdi, MD
James A. Yoder, MD
Chad A. York, PA-C
Christina Zanakis-Reids, MD
Matthew L. Zerden, MD
- Jean Zhang, MD
Dr. Jack Allison to Give Lecture at ECU. "The Convergence of Emergency Medicine and Public Health: To Brody via Africa and Beyond"
"The Convergence of Emergency Medicine and Public Health: To Brody via Africa and Beyond"
Wednesday, March 5, 2025 at 3:30pm
Presented by Jack Allison, MD/MPH, FACEP, FACPM
The in-person lecture will be held in the Evelyn Fike Laupus Gallery, fourth floor of Laupus Library.
You may also attend the event virtually through this link. Please be aware that while streaming is available to all, only those with an ECU email address are able to access the live Q&A via Panopto. However, we will be taking questions from this email ([email protected]) during the live session.
Speaker bio:
Dr. Jack Allison served as a Peace Corps Volunteer in Malawi, Africa, 1967-69. His public health education was punctuated by many original songs and jingles which became quite popular with Malawians throughout the country.
Jack has had a distinguished career in academic emergency medicine, with an emphasis on public health, acting as Chair and Medical Director of Emergency Medicine programs in Charleston, South Carolina, and the Brody School of Medicine at East Carolina University. He founded the Department of Emergency Medicine at ECU-SOM in 1980. Dr. Allison became the second endowed Chair of Emergency Medicine internationally.
Additionally, Dr. Allison responded to the earthquake in Haiti in January 2010 by treating hundreds of quake victims. In February 2012, he volunteered in Kenya and Somalia where he provided both emergency care and public health education to hundreds of Somali refugees; then in October, he volunteered in Zambia where he helped to install 112 shallow water wells. Since 2017, Jack has been a senior consultant to the Fulbright Association’s WASH project in Malawi.
Allison’s avocation is singing and songwriting. He has written over 150 songs and jingles and recorded 135 of those. Since 1967, he has raised $170,000 with his music, and he and his wife, Sue Wilson, have given away all of those monies to various charitable organizations, including $30,000 to help feed Malawian AIDS orphans.
This event is free and open to the public. Refreshments will be provided.
Presentation description: Dr. Allison will review the history of emergency medicine — nationally, internationally and at the Brody School of Medicine. Additionally, he will also share his myriad experience in public health education, especially via the medium of his original music. In 2024, he was considered for the North Carolina Music Hall of Fame.
Directions and Parking Information
If you’d like to travel by bus from Main Campus, take bus 302 from the Main Campus Student Center to the Allied Health Sciences Building. Click here for the 302 bus schedule.
This presentation is part of the Ruth and John Moskop History of Medicine Lecture Series.
Individuals requesting accommodation under the Americans with Disabilities Act (ADA) should contact the ADA Coordinator at least 48 hours prior to the event at (252) 737-1018 (voice/TTY) / [email protected]
For any questions about the event, please contact me at [email protected].
Capitol Chronicle: NC Neurologists Go To Capitol Hill

February 26, 2025
North Carolina Neurologists go to Capitol Hill
Over the dates of February 23-25, 2025, neurologists from across the country traveled to Washington, DC for the annual congressional advocacy event of the American Academy of Neurology. Attendees from North Carolina participating in 2025 Neurology on the Hill included:
- Zahra Cain-Akbar, DO
Cape Fear Valley Health / Wade, NC - Robert Frere, MD, FAAN
ECU Health / Greenville, NC - Amy Guzik, MD, FAAN
Wake Forest University School of Medicine / Winston Salem, NC - Casey Jeffreys, MD
Raleigh Neurology Associates / Raleigh, NC - Sneha Mantri, MD, MS
Duke University Medical Center / Durham, NC - Sara Sacco, MD
Carolinas Headache Clinic / Matthews, NC - Alan Skipper, CAE
Senior Officer, External Affairs / NC Medical Society
Senior Executive Director / NC Neurological Society
The group visited all 16 offices of North Carolina’s members of the Senate and House.

The Issues and “asks” presented included:
Medicare Payment Fix
A 2.8% cut to Medicare physician payment took effect January 1, 2025 – the fifth year in a row that physicians have had to absorb Medicare payment reductions. The primary ask of House members was to support HR 879 / Medicare Patient Access and Practice Stabilization Act which would eliminate the cut for 2025 as well as add a positive payment adjustment to account for the inflationary increase in practice costs. Rep. Greg Murphy, MD (NC-3) from Greenville, NC is the lead sponsor on the bill and in the four weeks since its introduction, the bill has gained 100 bipartisan cosponsors.
A companion bill has yet to be introduced in the Senate, which was the ask of Senator Ted Budd and Sen. Thom Tillis.
Medicare Telehealth Flexibilities Extension
The year-end federal funding package passed by Congress in December included an extension of the Medicare Telehealth Flexibilities that originated during the COVID-19 pandemic. The impact and value of expanded telehealth availability and coverage has been proven and the impending expiration of the telehealth flexibilities at the end of March has raised serious concern. The ask of Congress from the neurology community as well as from the entire medical profession is to, at a minimum, re-extend the flexibilities with a strong preference expressed for permanency.
Neuroscience Research Support
Support for research specific to neurological disease has been an ongoing point of emphasis due to the aging population and the associated increase in incidence of neurological disease. The message for sustaining and expanding research funding has increased with urgency as research funding has become a target to achieve savings in the federal budget. This past week’s trip to Capitol Hill offered an opportunity to demonstrate the value of the work done by the NIH National Institute for Neurological Disorders and BRAIN Initiative.
Do you know your legislator? More importantly, does your legislator know you?
JAMA Investigation: Medicaid Spending and Health-Related Social Needs in the North Carolina Healthy Opportunities Pilot Program

Medicaid Spending and Health-Related Social Needs in the North Carolina Healthy Opportunities Pilots Program
Key Points
Question Is North Carolina Medicaid’s Healthy Opportunities Pilots 1115 waiver program, which provides nonmedical services to address health-related social needs, associated with lower Medicaid spending?
Findings This comparative interrupted time series evaluation found that spending increased near program enrollment, followed by a significantly decreasing trend in spending relative to what would have been expected in the absence of the program.
Meaning Because lower need for expensive health services can indicate better health, these findings are consistent with the idea that programs to address health-related social needs may help improve health for Medicaid beneficiaries.
Abstract
Importance Health-related social needs are drivers of worse health and high health care spending. In North Carolina Medicaid’s 1115 waiver, the Healthy Opportunities Pilots (HOP) program allows for nonmedical services to address health-related social needs, such as healthy food boxes and housing navigation, financed by Medicaid, in 3 regions of North Carolina.
Objective To determine whether individual participation in the HOP program is associated with lower Medicaid spending.
Design, Setting, and Participants Comparative interrupted time series evaluation using North Carolina Medicaid data from March 2021 through November 2023. The 13 227 HOP enrollees were compared with 73 469 Medicaid beneficiaries reporting a health-related social need (a HOP eligibility criterion), but who were ineligible for HOP due to county of residence.
Exposure Participation in HOP.
Main Outcomes and Measures The primary outcome was the sum of spending by Medicaid on medical and HOP services per beneficiary per month. Secondary outcomes included health care use (emergency department visits, inpatient admissions, and outpatient visits).
Results Among 13 227 HOP and 73 469 comparison group members, the mean age was 23.4 (SD, 18.8) years, 63.9% were female, 42.4% were Black, and 57.4% were White (participants could report >1 race). Mean monthly preindex spending was $828 (SD, $5105). Of HOP enrollees, 89% received at least 1 HOP service, and 85% of services were food services. The comparative interrupted time series analysis estimated that spending increased at the month of HOP enrollment (change in level, $687; 95% CI, $420-$954). However, the trend in spending for HOP participants was differentially lower (change in trend, −$85 per beneficiary per month; 95% CI, −$122 to −$48; P < .001) relative to a counterfactual scenario without HOP. Taken together, these findings indicated that monthly spending was equivalent to estimated counterfactual expenditures by month 8 after starting HOP and lower thereafter. Emergency department visit trend was differentially lower for HOP participants (−6 per 1000 person-months; 95% CI, −8 to −4). There was no statistically significant differential trend in hospitalizations (−1 per 1000 person-months; 95% CI, −2 to 0) or outpatient visits (1 per 1000 person-months; 95% CI, −7 to 9).
Conclusions and Relevance Results of this study suggest that the HOP program was associated with increased spending at enrollment, followed by a subsequently lower spending trend.
Click here for full article and link to full text.
Duke, UNC Hospitals Rated Among World's Best

World's Best Hospitals 2025
(Newsweek, Alexis Kayser) -- Few decisions carry more weight than selecting a hospital for yourself or a loved one. This choice is often made while feeling unwell or after a stressful diagnosis—making it all the more difficult. That's why ready information about where world-class medical care is available can make all the difference in ensuring the best possible outcomes.
According to global data platform Statista, the number of hospitals worldwide is projected to reach 215,977 by 2026. With an overwhelming number of hospitals to choose from, most available resources fail to provide a full overview of the options.
To close the gap and help prospective patients find the best care possible, Newsweek and Statista are proud to present the World's Best Hospitals 2025, which shares the top hospitals worldwide, as well as ranked by country, to provide choices that are tailored for your needs.
This year's ranking lists the best hospitals in 30 countries: Australia, Austria, Belgium, Brazil, Canada, Chile, Colombia, Denmark, Finland, France, Germany, India, Israel, Italy, Japan, Malaysia, Mexico, Netherlands, Norway, Saudi Arabia, Singapore, South Korea, Spain, Sweden, Switzerland, Taiwan, Thailand, the United Arab Emirates, the United Kingdom and the United States. These countries were selected based on multiple comparability factors, such as standard of living, life expectancy, population size, number of hospitals and data availability.
The ranking is based on an extensive evaluation process, including an online survey of thousands of medical experts (doctors, hospital managers and health care professionals), patient experience data, hospital quality metrics and a PROMs Implementation Survey. Patient-Reported Outcome Measures (PROMs) are defined as standardized, validated questionnaires completed by patients to measure their perception of their functional well-being and quality of life.
Over 2,400 hospitals were ranked this year, but the list also highlights the top 250 hospitals worldwide. Among these standouts are Mayo Clinic - Rochester, Cleveland Clinic, Toronto General - University Health Network, The Johns Hopkins Hospital and Karolinska Universitetssjukhuset.
Having reliable and accessible data is essential when selecting a hospital for treatment. We hope this list is a trusted resource for patients, families and health care leaders seeking insights into the world's top medical institutions.
Click for link to complete list
DHHS: 1 Dead in NC from Listeria Outbreak

A Listeria outbreak linked to recalled frozen supplemental shakes has resulted in one death in North Carolina and at least 12 deaths nationwide
(WRAL, DHHS) -- One person in North Carolina has died from a listeria outbreak linked to frozen supplemental shakes, the Department of Health and Human Services said Wednesday.
DHHS confirmed two cases in the state so far.
Nationwide, there have been at least 12 deaths as part of an outbreak of Listeria monocytogenes infections linked to the frozen supplemental shakes, the US Food and Drug Administration said Monday.
The Sysco Imperial and Lyons ReadyCare shakes are manufactured by Prairie Farms Dairy Inc. in Fort Wayne, Indiana. The shakes were mainly distributed to hospitals and long-term care facilities. Prairie Farms and distributor Lyons Magnus have recalled the shakes.
The FDA is conducting an onsite investigation.
Sen. Thom Tillis, Colleagues Introduce Bipartisan Legislation to Increase Access to Rural Healthcare
WASHINGTON, D.C. – Senator Thom Tillis, alongside Senators Amy Klobuchar (D-MN), Susan Collins (R-ME), and Jacky Rosen (D-NV), introduced the Conrad State 30 and Physician Access Reauthorization Act, bipartisan legislation to increase the number of doctors working in rural and medically underserved areas.
“Too many rural areas in North Carolina and across the country lack the health care workforce needed to provide quality and timely care,” said Senator Tillis. “This bipartisan legislation will allow American-trained doctors to help fill those gaps so we can expand access to critical health care in medically underserved and health professional shortage areas.”
“The Conrad 30 program continues to be a vital lifeline for rural and underserved communities facing physician shortages,” said Ram Alur, M.D., President, Physicians for American Healthcare Access. “However, without reforms, recruiting and retaining international medical graduates (IMGs) will become increasingly difficult. This reauthorization strengthens incentives for IMGs and streamlines the waiver process for employers, making it easier to recruit physicians in areas with persistent shortages. These updates will strengthen the U.S. position in the global competition for top medical talent and uphold access to care in underserved areas. Physicians for American Healthcare Access applauds Senators Klobuchar, Collins, Rosen, and Tillis for their leadership on this bipartisan legislation.”
Background:
The Conrad State 30 and Physician Access Reauthorization Act would reauthorize the Conrad 30 programs, which allows international doctors who have completed their residency training in the U.S. to remain in the country under the condition that they practice in areas experiencing physician shortages
Generally, doctors from other countries working in America on J-1 visas are required to return to their home country after their residency has ended for two years before they can apply for another visa or green card. The Conrad 30 program allows doctors to stay in the United States without having to return home if they agree to practice in an underserved area for three years. The “30” refers to the number of doctors per state that can participate in the program.
This legislation extends the Conrad 30 program for three years, improves the process for obtaining a visa, and allows for the program to be expanded beyond 30 slots if certain thresholds are met, while protecting small states’ slots. The bill also allows the spouses of doctors to work and provides worker protections to prevent the doctors from being mistreated. The legislation also allows physicians who serve in a Veterans Affairs (VA) facility or health professional shortage area for 5 years to get expedited consideration for a green card.
The legislation has been endorsed by more than 50 organizations, including the American Medical Association, the American Hospital Association, the Association of American Medical Colleges, the American Academy of Neurology, the Association for Advancing Physician and Provider Recruitment, and Physicians for American Healthcare Access.
Full text of the bill is available HERE.
Save Room For Cake! New Study Sheds Light on Why We Always Seem to Have Room for Dessert

Why Sweets Are Enticing Even After a Big Meal
If you have a sweet tooth, you’ve probably said something along the lines of “there’s always room for dessert.” Well, that saying has some real science behind it, according to a recent study.
To better understand why it’s so enticing to eat something sweet even after a big meal — sometimes called the “dessert stomach” phenomenon — researchers first turned to mice. After feeding the mice to the point of being fully satiated and then giving them sugar, they found that the same neurons that signaled fullness also released a natural opiate, thus triggering a feeling of reward. When scientists blocked that opiate pathway, mice refrained from eating additional sugar when full.
As for humans, the team conducted scans on volunteers and found that the same region of the brain reacted to sugar. “From an evolutionary perspective, this makes sense: Sugar is rare in nature, but provides quick energy,” study lead Henning Fenselau explained in a news release. “The brain is programmed to control the intake of sugar whenever it is available.”
NCMS Joins Long List of Medical Societies and Associations to Urge U.S. Congress to Include Changes to Forthcoming Bill on Medicare

The following is a letter to House Speaker Mike Johnson, Senate Majority Leader John Thune, House Democratic Leader Hakeem Jeffries, and Senate Democratic Leader Charles Schumer.
The North Carolina Medical Society has been added to the list of national medical societies, state medical societies, and medical associations.
Dear Speaker Johnson, Majority Leader Thune, Leader Schumer, and Leader Jeffries:
The undersigned national medical societies and state medical associations write to collectively urge Congress to include in the forthcoming March 2025 appropriations bill, provisions that both reverse the latest round of Medicare payment cuts and provide physicians with a meaningful payment increase that reflects ongoing inflationary pressures. Our organizations were surprised and deeply disappointed that the final version of the American Relief Act 2025 failed to include any financial relief for physicians. America’s physicians are united in urging Congress to use the forthcoming March appropriations bill as an opportunity to provide physicians with desperately needed fiscal relief that is imperative to ensuring that seniors retain access to health care services under Medicare.
Following Congressional inaction to stop the cuts finalized by Centers for Medicare and Medicaid Services’ (CMS) Calendar Year (CY) 2025 Medicare Physician Fee Schedule (MPFS) Final Rule, payments for physicians treating Medicare patients were reduced by an additional 2.83 percent, effective January 1, 2025. The decision to allow previously enacted partial patches to earlier rounds of physician payment reductions to expire without any new relief marks the fifth consecutive year of Medicare physician payment cuts, a truly startling trend that threatens to exacerbate access to care issues throughout the United States. As a result, the unfortunate reality is that physicians’ Medicare payments have now been reduced by 33 percent since 2001, when adjusted for inflation in practice costs. In addition, CMS concluded in the CY 2025 MPFS Final Rule that the Medicare Economic Index (MEI), a cumulative measure of the individual costs of running a practice, will increase by 3.5 percent this year. Expecting physicians to provide the same level of care to America’s seniors despite being underpaid by over 30 percent and witnessing exponential growth in the cost of providing medical services is simply unsustainable. This cycle threatens to undermine the overarching stability of the Medicare program.
The decision by Congress to extend a variety of other expiring hospital, ambulance, and telehealth provisions in the American Relief Act 2025 without providing physicians any relief was equally troubling. Furthermore, our members understandably think that the federal government has essentially turned its back on physicians following the recent CMS announcement that Medicare Advantage (MA) plans will receive an average payment increase of 4.33 percent from 2025 to 2026. While MA plans receive an increase beyond the expected health care inflation rate, Congress has not acted to incorporate a temporary or permanent inflationary adjustment to the MPFS to ensure adequate access to care. Thankfully, a bipartisan collection of federal lawmakers has introduced, yet again, another solution to this serious policy issue. Representatives Greg Murphy, MD (R-NC), Jimmy Panetta (D-CA), Mariannette Miller-Meeks, MD (R-IA), and Kim Schrier, MD (D-WA), along with several other bipartisan House members, have introduced an updated version of the Medicare Patient Access and Practice Stabilization Act, H.R. 879. This bipartisan bill will prospectively, specifically between April 1 and December 31, 2025, stop the latest round of payment cuts in full. The bill also provides physicians with a crucial two percent payment increase, which is about half of the MEI estimate for this year. Therefore, we urge Congressional leadership to adopt the Medicare Patient Access and Practice Stabilization Act as part of the forthcoming legislation to fund the government beyond mid-March.
The time for legislative action is now. America’s physicians and the millions of patients we treat can no longer accept any excuses, such as an overcrowded legislative calendar, competing policy priorities, or an inability to achieve bipartisan consensus, as reasons for not including provisions that reverse the latest round of cuts and provide a crucial payment update in next appropriations package. We appreciate the opportunity to outline the many fiscal challenges facing physician practices and stand ready to assist with the overarching effort to expeditiously enact this much needed legislation. Our Medicare beneficiaries and the physicians who treat them deserve the stability that this legislation will provide.
Sincerely,
- American Medical Association
- Academy of Physicians in Clinical Research
- American Academy of Allergy, Asthma & Immunology
- American Academy of Dermatology Association
- American Academy of Emergency Medicine
- American Academy of Facial Plastic and Reconstructive Surgery
- American Academy of Family Physicians
- American Academy of Hospice and Palliative Medicine
- American Academy of Neurology
- American Academy of Ophthalmology
- American Academy of Otolaryngic Allergy
- American Academy of Otolaryngology – Head and Neck Surgery
- American Academy of Physical Medicine and Rehabilitation
- American Academy of Sleep Medicine
- American Association for Hand Surgery
- American Association of Hip and Knee Surgeons
- American Association of Neurological Surgeons
- American Association of Neuromuscular & Electrodiagnostic Medicine
- American Association of Orthopaedic Surgeons
- American Association of Public Health Physicians
- American College of Allergy, Asthma and Immunology
- American College of Cardiology
- American College of Emergency Physicians
- American College of Gastroenterology
- American College of Lifestyle Medicine
- American College of Medical Genetics and Genomics
- American College of Mohs Surgery
- American College of Physicians
- American College of Radiation Oncology
- American College of Radiology
- American College of Rheumatology
- American College of Surgeons
- American Epilepsy Society
- American Gastroenterological Association
- American Geriatrics Society
- American Orthopaedic Foot & Ankle Society
- American Psychiatric Association
- American Society for Clinical Pathology
- American Society for Dermatologic Surgery Association
- American Society for Gastrointestinal Endoscopy
- American Society for Laser Medicine & Surgery, Inc.
- American Society for Radiation Oncology
- American Society for Surgery of the Hand Professional Organization
- American Society of Addiction Medicine
- American Society of Anesthesiologists
- American Society of Cataract & Refractive Surgery
- American Society of Echocardiography
- American Society of Hematology
- American Society of Interventional Pain Physicians
- American Society of Nephrology
- American Society of Neuroradiology
- American Society of Nuclear Cardiology
- American Society of Plastic Surgeons
- American Society of Regional Anesthesia and Pain Medicine
- American Society of Retina Specialists
- American Society of Transplant Surgeons
- American Thoracic Society
- American Urogynecologic Society
- American Urological Association, Inc.
- American Venous Forum
- Association for Clinical Oncology
- Association of American Medical Colleges
- College of American Pathologists
- Congress of Neurological Surgeons
- Endocrine Society
- Heart Rhythm Society
- International Pain and Spine Intervention Society
- Medical Group Management Association
- Outpatient Endovascular and Interventional Society
- Renal Physicians Association
- Society for Cardiovascular Angiography and Interventions
- Society for Vascular Surgery
- Society of American Gastrointestinal and Endoscopic Surgeons
- Society of Critical Care Medicine
- Society of Hospital Medicine
- Society of Interventional Radiology
- Society of Nuclear Medicine and Molecular Imaging
- The American Society of Breast Surgeons
- The American Society of Dermatopathology
- The Society of Thoracic Surgeons
- Medical Association of the State of Alabama
- Alaska State Medical Association
- Arizona Medical Association
- Arkansas Medical Society
- California Medical Association
- Colorado Medical Society
- Connecticut State Medical Society
- Medical Society of Delaware
- Medical Society of the District of Columbia
- Florida Medical Association
- Medical Association of Georgia
- Hawaii Medical Association
- Idaho Medical Association
- Illinois State Medical Society
- Indiana State Medical Association
- Iowa Medical Society
- Kansas Medical Society
- Kentucky Medical Association
- Louisiana State Medical Society
- Maine Medical Association
- MedChi, The Maryland State Medical Society
- Massachusetts Medical Society
- Michigan State Medical Society
- Minnesota Medical Association
- Mississippi State Medical Association
- Missouri State Medical Association
- Montana Medical Association
- Nebraska Medical Association
- Nevada State Medical Association
- New Hampshire Medical Society
- New Mexico Medical Society
- North Carolina Medical Society
- Medical Society of New Jersey
- Medical Society of the State of New York
- North Dakota Medical Association
- Ohio State Medical Association
- Oklahoma State Medical Association
- Oregon Medical Association
- Pennsylvania Medical Society
- Rhode Island Medical Society
- South Carolina Medical Association
- South Dakota State Medical Association
- Tennessee Medical Association
- Texas Medical Association
- Utah Medical Association
- Vermont Medical Society
- The Medical Society of Virginia
- Washington State Medical Association
- West Virginia State Medical Association
- Wisconsin Medical Society
- Wyoming Medical Society
First Death Reported in Measles Outbreak, First Measles Death in U.S. Since 2015

An unvaccinated child has died in the Texas measles outbreak
(AP, Devi Shastri) -- A child who was not vaccinated has died from measles in West Texas, the first death in an outbreak that began late last month and the first from measles in the U.S. since 2015.
The death was a “school-aged child who was not vaccinated” and had been hospitalized last week, the Texas Department of State Health Services said Wednesday in a statement.
Covenant Children’s Hospital in Lubbock didn’t immediately respond to a request for comment, nor did Texas Gov. Greg Abbott’s office. Texas Tech University Health Sciences Center spokesperson Melissa Whitfield first confirmed the death, which happened overnight, to The Associated Press on Wednesday morning.
The measles outbreak in rural West Texas has grown to 124 cases across nine counties, which state health officials have said is Texas’ largest in nearly 30 years. There are also nine cases in eastern New Mexico.
The U.S. Centers for Disease Control and Prevention confirmed this is the first measles death in the country since 2015. Measles cases were the worst in almost three decades in 2019, and there was a rise in cases in 2024, including an outbreak in Chicago that sickened more than 60.
The outbreak is largely spreading in the Mennonite community in West Texas, where small towns are separated by vast stretches of oil rig-dotted open land but connected due to people traveling between towns for work, church, grocery shopping and other errands.
Texas health department data shows the vast majority of cases in the area are among people younger than 18. The measles, mumps and rubella vaccine — which is safe and highly effective at preventing infection and severe cases — is recommended for children between 12 and 15 months old for the first shot, with the second coming between 4 and 6 years old.
The vaccine series is required for kids before entering kindergarten in public schools nationwide. But the measles cases in West Texas have been concentrated in a “close-knit, undervaccinated” Mennonite community, state health department spokesperson Lara Anton has said, especially among families who attend small private religious schools or are homeschooled.
Gaines County, which has 80 cases, has one of the highest rates in Texas of school-aged children who opt out of at least one required vaccine, with nearly 14% of K-12 children in the 2023-24 school year.
Earlier this month, new federal health secretary Robert F. Kennedy Jr. said a panel would investigate the childhood vaccine schedule that prevents measles and other dangerous diseases.
Measles is a respiratory virus that can survive in the air for up to two hours. Up to 9 out of 10 people who are susceptible will get the virus if exposed, according to the U.S. Centers for Disease Control and Prevention. Most kids will recover from the measles if they get it, but infection can lead to dangerous complications like pneumonia, blindness, brain swelling and death.
The U.S. Centers for Disease Control is providing “technical assistance, laboratory support and vaccines as needed” to West Texas, the agency told the AP, but the state health department is taking the lead in the outbreak investigation.
Make Your Plans Now! NC AHEC Medicaid Managed Care Webinar

Medicaid Managed Care
Virtual Office Hours
NC Medicaid Initiatives & Updates
Thursday, March 6 noon - 1pm
Please join us on Thursday, March 6 from noon to 1pm to hear about NC Medicaid initiatives and updates, including:
- Education/Training Transcripts
- New Ordering/Prescribing/Referring Provider Guidelines
- Delegated Enrollment & Credentialing Committee
- Telehealth
- Annual Federal Fee Increase
- Children & Family Specialty Plan Update
- Multi-Factor Authentication/NCID Update
To register click here.
AMA Survey: Physicians Say Prior Authorization Stands in the Way of Medically Necessary Care
Physicians surveyed by the AMA say that PA can cause care delays or force patients to abandon treatment. They warn denials could increase as insurers adopt AI to review claims.
(HealthcareDive, Susanna Vogel)
Dive Brief:
- Physicians say prior authorization continues to pose barriers to offering timely and medically necessary treatment, according to a new survey from the American Medical Association.
- Nearly all of the physicians surveyed in December said prior authorization resulted in care delays at least some of the time and had a negative impact on patient clinical outcomes.
- Most respondents said prior authorization denials had increased over the last five years, with nearly a third of respondents reporting their requests are often or always denied. Physicians reported concerns denial rates could grow further as insurers adopt artificial intelligence tools to review claims.
Dive Insight:
Physicians have long criticized prior authorization requirements, saying the process puts additional administrative requirements on providers and requires patients to jump through hoops to get necessary medical care.
Almost one in three physicians surveyed by the AMA said prior authorization criteria are rarely or never evidence-based. The majority of respondents said prior authorization led to overall higher medical utilization, with 77% of physicians reporting patients had to first attempt an ineffective initial treatment.
At times, prior authorization can lead to care delays that significantly impact a patient’s health, respondents said. More than a fourth of physicians said prior authorization led to a serious adverse event for a patient in their care. Twenty-three percent reported a patient was hospitalized due to prior authorization, while 18% said prior authorization contributed to a life-threatening event and 8% said patients suffered a disability.
Physicians are concerned that prior authorization denials could accelerate in the coming years if more insurers turn to AI to review claims.
While major insurers, including Blue Shield of California, claim that using AI to review prior authorization documents will reduce burden on physicians by providing near instantaneous decisions, the AMA is skeptical the tools will benefit providers.
In a press release accompanying the survey, the AMA cited a Senate report from October that found AI denied claims up to 16 times more than when a human reviewed them.
“Emerging evidence shows that insurers use automated decision-making systems to create systematic batch denials with little or no human review, placing barriers between patients and necessary medical care,” said Bruce Scott, AMA president, in a press release. “Medical decisions must be made by physicians and their patients without interference from unregulated and unsupervised AI technology.”
Lawmakers have expressed interest in overseeing insurers’ use of the tech and several insurers have been sued over their use of algorithms to review claims. Still, it is unlikely that insurers will back down from using the technology, experts previously told Healthcare Dive. Instead, it’s more likely that providers will need to adopt their own AI to submit claims.
UNC: A Fresh Approach to Family-Centered Care for Adult ICUs

Co-led by UNC School of Medicine’s David Y. Hwang, MD, newly released updated guidelines from the Society of Critical Care Medicine (SCCM) reveal how family centered care for adult ICUs is paramount and an invaluable approach.
Imagine one of your family members being incredibly ill and admitted into the ICU. A range of emotions creep up like fear, anxiety, uncertainty and a desperate desire to see that family member recover. This impact on loved ones attempting to assist to the needs of the critically ill patient can often result in despair and hopelessness.

Building resilience during this physical and emotional hospital stay often involves a multi-centered approach to the planning, delivery, and evaluation of health care that is beneficial among patients, families, and health care professionals. To continue the efforts in making sure patients are receiving the highest quality care, an official set of newly updated international guidelines from the Society of Critical Care Medicine (SCCM) has now been released regarding best practices and clear recommendations for support of family members for adult ICU patients.
“Our hope is that as critical care evolves post-COVID that family-centered care will be central to the care of patients more than ever before,” said David Y. Hwang, MD, FAAN, FCCM, FNCS, professor of neurology, division chief of neurocritical care at the UNC School of Medicine, and corresponding author of the paper. “Between the recommendations themselves and an accompanying implementation toolkit, the guidelines package provides a practical roadmap for adult units that are looking to identify areas of improvement and implement positive changes for their patients’ families.”
Co-led by Hwang and Dr. Mona Hopkins of Brigham Young University, the guidelines published in Critical Care Medicine is the third iteration for family-centered care in adult ICUs; the last iteration was in 2017. The guidelines consist of four content sections: engagement of families, support of family needs, communication support, and support of ICU clinicians providing family-centered care. A multi-professional panel was established to publish these evidence-based recommendations. This panel issued 17 statements related to optimal family-centered care in adult ICUs, including one strong recommendation, 14 conditional recommendations, and two best-practice statements.
Following the 2017 guidelines, the 2020 COVID pandemic ignited negative effects on ICU family presence. The new guidelines issue a strong recommendation for ICUs to liberalize or to allow less restrictive hours of ICU family presence policies post-COVID. As COVID spread around the world, family presence in inpatient settings temporarily came to a halt. With the pandemic behind us, the recommendations make the case that defaulting family presence options to become more flexible by improving family visiting hours can promote equity and clinician-family trust in decision making. One meta-analysis performed for the guidelines found that liberalized policies demonstrated increased family satisfaction, possible increase in patient satisfaction, and reduced family and patient symptoms of anxiety and depression.
“There’s been a movement in ICUs in general for all families to be at the bedside with their loved ones,” said Hwang. “During COVID when there was a lot of visitor restrictions, the culture kind of shifted a bit. Following the pandemic, our writing team’s hope is that the default practice should shift back to being as inclusive as possible when it comes to visiting hours, as long as leadership believes that safety is being respected.”
The guidelines included conditional recommendations for family participation in bedside care. This approach involves having family members participate in hands-on care for their loved ones in manners that medical teams feel to be safe. As an example: if a loved one needs routine oral care in the ICU, a family member who is willing could be trained to help with this activity at the bedside, instead of on the sidelines.
“Some ICUs that are on the leading edge of this have a menu of things that they are comfortable in letting families do when they’re visiting their loved ones in ICU,” said Hwang. “If family members feel as though it would be therapeutic to be involved in bedside care, then they can be trained in things on the menu and have those opportunities. The hope is that this recommendation can help with the family’s mental health, too.”
The potential of losing a loved one can bring on a surge of emotions and stress. Attending to family mental health and psychological needs was also listed in the conditional recommendations. The panel in particular suggested providing spiritual and bereavement support to families of patients who have died in the ICU. Additional interventions for supporting families involved brochures or booklets; condolence letters; and meetings with specific care teams, such as palliative care, psychologists, or specially trained nurses. In meta-analyses performed for the guidelines, evidence pointed towards a connection between supporting ICU family mental health and improved family satisfaction and reduction of patient PTSD.
Burnout, fatigue, anxiety, and moral distress can all describe the state of a clinician’s well-being, especially those providing critical care services. The beginning of the COVID-19 pandemic fueled the flames of this burnout epidemic at an alarming rate. These new guidelines included another conditional recommendation in addressing the support of clinical teams in their efforts to provide family-centered care. To meet this need, recommendations suggest structured programs to support clinicians in promoting the delivery of family-centered ICU care. By supporting the clinician’s resilience and mental health, these efforts can create a domino effect in compassionate and empathetic care to patients’ families. The guidelines reveal that identifying and reducing these barriers could promote a positive impact in the healthcare setting.
A best practice statement was also issued that ICUs implement practices to identify and reduce barriers to help promote equitable critical care delivery for patients’ families. Some of these practices include offering families the option of being present on ICU rounds, offering family presence during resuscitation, providing family educational programs, providing ICU diaries, and providing communication skills training to clinicians. Another best practice statement recommended ICUs to implement supportive features to meet family needs during the patient’s hospital stay like rest spaces, areas of personal care, and spaces to interact with staff.
Decreasing family anxiety and depression and improving family satisfaction is at the heart of providing family-centered care. Maintaining quality care and physician wellness is also key for optimal hospital morale. The guidelines conclude that further research needs to be implemented to understand effective protocols for supporting and engaging families remotely and continuing to identify interventions that positively affect families, patients and clinician outcomes. Hwang acknowledges that these are important next steps in supporting family members of ICU patients.
Written by: Brittany Phillips, communications specialist, UNC Health | UNC School of Medicine
11 Dead After Supplemental Shakes Linked to Listeria Cases in 21 States Including NC

(WTV), FDA) -- Frozen shakes sold to nursing homes and other institutions are being recalled after a listeria outbreak in 21 states that has caused 11 deaths, according to the Federal Food and Drug Administration.
The shakes have made at least 38 people ill, with 37 hospitalizations, the FDA said Friday.
Frozen supplemental shakes under the brands Sysco Imperial and Lyons ReadyCare have been voluntarily recalled, the FDA said. The shakes were primarily given to hospital patients and long-term care patients.
States with cases include Alabama, California, Colorado, Connecticut, Florida, Illinois, Indiana, Maryland, Michigan, Minnesota, Missouri, North Carolina, Nevada, New York, Ohio, Oklahoma, Pennsylvania, Tennessee, Texas, Washington and West Virginia.
The outbreak dates to 2018 but has persisted through 2025, including 20 cases from 2024 to 2025, according to the Centers for Disease Control and Prevention. Investigators had been previously unable to identify the source.
Symptoms of listeria infection include fever, muscle aches, nausea, tiredness, vomiting, and diarrhea. In more severe cases, symptoms may include headache, stiff neck, confusion, loss of balance, and convulsions.
“Listeria can survive in refrigerated temperatures and can easily spread to other foods and surfaces,” the FDA stated.
The FDA’s investigation is ongoing.
ICYMI: North Carolina Doctors, Patients, Lawmakers Call for Health Insurance Reform in 2025

An attempt to limit insurers' use of prior authorization is expected to be a top priority this session for a bipartisan group of North Carolina state lawmakers. That's likely to provoke a battle with state health insurers, who say it's an essential tool to help control health care costs.
*This report first appeared on WRAL on January 29, 2025, by Laura Leslie, WRAL capitol bureau chief
An attempt to limit insurers’ ability to require advance approval before covering a patient’s medical care is expected to be a top priority this legislative session for a bipartisan group of North Carolina lawmakers — an effort likely to provoke a battle with state health insurers, who say it’s an essential tool to help control health care costs.
But doctors say the practice, known as prior authorization, comes with its own set of costs, and for some patients and families, it's about much more than dollars.
That’s the case for Amanda Watson. Diagnosed with Stage 4 metastatic breast cancer in 2023, she’s been through more than a year of painful and debilitating chemotherapy, radiation and surgery — all to buy a little more time with her young sons, Judson and John William.
Instead, she’s spending hours each day on the phone, fighting to get insurance approval for the medical care she and her doctor say she needs.
“What kind of cost can you put on the time with your children or family when you're being told your days are limited?” Watson told WRAL News. “I could have spent that time in a different way that would be more meaningful to my family, my boys.”
Watson told her story at a news conference Tuesday, held by lawmakers and doctors who say prior authorization has gotten out of hand.
Dr. John Meier, president of the North Carolina Medical Society, said prior authorization began as a tool for complex medical cases, but it’s now being required for routine needs like scans, tests and even some generic drugs.
More than 95% of doctors’ requests are eventually approved, Meier said, but at a tremendous cost to doctors and patients.
“It becomes a game of chicken,” Meier said. “Who's going to wear out? Who's going to drop the ball first?”
State Rep. Grant Campbell, R-Cabarrus, is a practicing OB-GYN and Watson’s former doctor. He said prior authorization is about helping insurers’ bottom line, not patients.
“This is about delaying care,” Campbell said. “This is about forcing patients and physicians to settle for cheaper, less effective care, or ultimately hoping the patient gives up and pays out of pocket.”
Campbell, fellow Rep. Dr. Tim Reeder, R-Pitt, and other lawmakers are pushing to pass reforms this year they say will benefit patients. The proposal is likely to be similar to a bill that passed the House in 2023 but failed to pass the Senate. This time, they say, they believe they have backing in the Senate as well.
Health insurers say prior authorization helps them control costs and reduce waste in the healthcare system. Restricting it, they say, could lead to higher costs for patients.
Peter Daniel, executive director of the North Carolina Association of Health Plans, says insurers are willing to work with stakeholders and lawmakers on “meaningful regulatory reforms.”
“We all share the same goals of bringing costs down while improving quality of patient care,” said Daniel, whose group represents the state’s insurers.
Watson says the current system has its costs, too, for patients like her.
“It makes you question everything about your being,” Watson said. “It makes you wonder, ‘Am I worth fighting for? Is this fight worth it?’”
Daniel declined to comment on Watson’s case, but called it a “horrible situation.”
“We stand ready to try to find solutions to very vexing problems,” Daniel said.
Family Ties: IDD Caucus finds inspiration close to home

Family Ties: IDD Caucus Finds Inspiration Close to Home
(NC Insider, Matthew Sasser) -- When Rep. Zach Hawkins first ran for office in 2018, his two sons were diagnosed with autism.
He now co-chairs the General Assembly’s Intellectual and Developmental Disabilities (IDD) Caucus, which is welcoming new members and gearing up for the 2025 long session.
“It gave me a purpose that I didn’t know I needed,” said Hawkins, a fourth-term Democrat from Durham. “I didn’t know that I was going to have this as a platform, as one of the No. 1 things I focus on.”
Early in Hawkins’ tenure as a legislator, the General Assembly passed an expansion bill that gave families outside the Mecklenburg and Raleigh-Durham hubs access to critical IDD resources and services.
“That crowning achievement was the moment I was like, ‘We have to get this caucus back going again and I’m going to lead it as long as I’m here,’” Hawkins said. “When you are at the Legislature, you have this deep feeling that you are speaking for so many other families who don’t even have the time, resources or know-how to advocate [for those with intellectual disabilities].”
The IDD Caucus hasn’t met yet this year but has already received support from legislators with personal ties to the IDD community. Potential legislative efforts of the caucus could include a push for higher pay for direct care workers, more in-home services for people with IDD and looking at special needs teacher retention.
More than 230,000 people across the state —including children over age 3 and adults — have an intellectual or developmental disability, according to estimates.
Hawkins said the caucus will work on an IDD omnibus bill that captures the goals of various partner organizations and will serve as a road map for legislators.
Every caucus in the Legislature has to reconstitute every biennium. This session, Hawkins; Sen. Michael Lee, R-Wilmington; Sen. Sydney Batch, D-Wake; and Rep. Mitchell Setzer, R-Catawba, co-chair the IDD Caucus.
“I think because the caucus gets together in an informal setting to hear from folks, it is necessarily a little more conducive to a conversation,” Lee said. “It paves the way for a discussion for people who want to learn more.”
There’s plenty of ground to cover: workforce development, the North Carolina Department of Health and Human Services, vocational rehab and the intricacies of where state and federal funding is necessary.
“They should all kind of dovetail together, but they don’t,” Lee said. “That’s where the caucus is a good concept to talk about a lot of these issues.”
Higher pay for professional services
The IDD Caucus plans to tackle numerous legislative priorities this year.
Hawkins said there is a revolving door of direct support professionals working with the IDD community. These employees often make just $8 or $9 an hour and could make more at other jobs requiring a lot less work.
The 2023 budget authorized NC Innovation Waivers for only 250 people with IDD. The waivers are part of the federally funded Medicaid program that provides long-term care and services for individuals in their homes rather than institutions.
Thousands of people have received waivers in the past. But there is a waiting list of 15,000 people, which was the reason for the lower number of approved waivers, Hawkins said.

If pay for professionals who work with people with IDD were increased, it is hoped the number of those on the waiting list would decrease and as many as 750 Innovation Waivers could be added this session, Hawkins said.
“The top priorities are making sure that we receive the resources for direct support professionals and that we increase the innovation waivers,” Hawkins said at a news conference last May in support of House Bill 1003, which did not pass beyond its first reading. He said those legislative wishes will continue into the 2025 session.
Educational achievements
A major success story from the General Assembly and IDD Caucus has been the Access to Achievement pilot program started in 2021 at Brunswick and Catawba Valley community colleges to serve students with intellectual disabilities. The program served 157 students when it was launched; 55 received job offers after completing training.
Since the program’s inception, 13 additional community colleges have joined the effort to maximize access to degrees, credentials and employment opportunities for students with IDD. The General Assembly has allocated nearly $4 million for the expansion.
“Successful programs like this don’t just exist anywhere else in the country,” Lee said. “You really need a coalition of the willing to make something successful. This is not something that you can just set up [and have it be] another programmatic piece of the puzzle.”
Lee’s involvement with the IDD community began 18 years ago with his son’s birth. He said he’s seen what is and isn’t available for families and children across the special needs and IDD community. He also has witnessed some of the failures to meet the needs of what he considers “the most underserved population that is out there.”

A key ingredient of Access to Achievement is creating a school community with same-aged peers, Lee said.
Before the advent of the program, IDD students, who are typically family-dependent, would often “fall off the map” when they aged out of available resources. Financial benefits can provide a safety net, but the sense of purpose from contributing to one’s community — such as through employment — was missing, Lee said. That lack of purpose contributed to mental health issues down the road.
“That would happen to typically developing people who graduate from school and have nowhere to go to work,” Lee said, adding that excluding people with IDD from the workforce is a missed opportunity.
Approximately 1 in 9 working-age adults in North Carolina have a disability.
“If you talk to employers, [people with IDD are] the most dedicated,” Lee said. “They’re not just on time; they’re early. They work very hard and care deeply about the work they’re doing. They’re happy to be working.”
North Carolina is an innovator in funding and supporting a program such as Access to Achievement. Lee said finding a solution isn’t easy when a template from another state isn’t available.
“There’s a lot more that will come from it, not just an expansion of the existing program, but I think there’s a lot more we can do in the future,” Lee said. “We can solve a lot of workforce issues by bringing more people into the workforce that have been overlooked.”
Lisa Estep, chair of the State Board of Community Colleges Finance Committee, was critical to getting the program started alongside Lee. Their efforts earned praise from Tom Looney, chairman of the state board of the North Carolina Community College System, at a meeting in January.
“What we would like to do is continue to grow it to any college that would like to be a part of the program,” Looney said. “We have students out there graduating from high schools with uncertain economic opportunities and we’re trying to provide opportunities, which is what community college is all about. Not only are they getting skills, but there’s a job at the end of it.”
Classroom challenges
North Carolina suspends more students with disabilities than any other state, often because of misunderstood behaviors and vacant positions for teachers with expertise in educating students with IDD.
According to WCNC-TV, more than 2,600 students with disabilities received out-of-school suspensions or expulsions lasting more than 10 days that school year, while nearly 19,000 received 10 days or fewer.
“That is something we have to tackle,” Hawkins said. “We have a teacher vacancy across the state that is growing in the special needs space. You can’t have a substitute — that needs to be someone that is highly trained, so we need to do a better job of recruitment.”
About 1,200 special education teacher positions were vacant in the fall of 2023 and others were filled by unqualified staff, according to the North Carolina Department of Public Instruction.
Beyond the Access to Achievement success, Hawkins also highlighted his work with Rep. Dean Arp, R-Union, and former Rep. Jeffrey Elmore. Together, they secured $3 million in funding for NC State and NC Central University in a workforce development plan for the IDD community.
“Everybody in North Carolina should be able to maximize their given potential,” Hawkins said, adding that IDD Caucus legislators are keeping an eye on many areas.

New advocate for IDD community
Even before he began considering a career as a lawmaker, freshman legislator Rep. Jonathan Almond, R-Cabarrus, already had a source of guidance for his role in office.
Almond’s twin boys, who recently turned 7, are mostly nonverbal. He said it’s been a yearslong journey of understanding how to “unlock that door” and tackle the challenges that follow. During the COVID-19 pandemic, uncertainty surrounding the masking policy and how it would affect his children’s development kick-started Almond’s interest in politics.
“I think that’s one of the biggest reasons that God asked me to run for office — my personal experience with the special needs community,” he said. “I hope to be an advocate like Rep. Hawkins and just try to bring more awareness and support to that community while I’m in Raleigh.”
Almond said he is working with Rep. Paul Scott, R-Cleveland, to reformulate the funding calculation for Exceptional Children’s curriculum. He’s also hopeful he can start to look at what is causing higher rates of childhood diseases and disorders, including autism, and how the Legislature can help families dealing with this reality.
‘Huge wins’
There will be a day in March when members of the IDD community can visit the General Assembly and speak with lawmakers.
“We’ve had huge wins over the last two sessions just because we were an organized caucus,” Hawkins said.
That optimism is spilling over into 2025. He’s encouraged by the presence of two freshman legislators — Reps. Almond and Bryan Cohn, D-Granville — who will bring their personal experience to the IDD Caucus.
“We’re really excited about what the future holds,” Hawkins said. “I didn’t even know we would be bringing in members that had personal experience [to share]. That just lets me know we’re going to be even more powerful going forward.”
As Prior Authorization Burden Grows, So Does Momentum for Change
 AMA: Physicians must show legislators how prior authorization harms patients. Then they need to tell them again—with the data to back it up
AMA: Physicians must show legislators how prior authorization harms patients. Then they need to tell them again—with the data to back it up
*Links to NCMS efforts on prior authorization are at end of this article.
(AMA News Wire, Andis Roberznieks) -- Through prior authorization, insurance companies create barriers to treatment—and even the sickest patients aren’t spared from this ordeal.
“Of all the patients and all the conditions that we care for, cancer patients are probably some of the ones for whom the delays and the denials and the claim of ‘that's experimental’ has probably the greatest impact,” AMA President Bruce A. Scott, MD, said while moderating a panel discussion on prior authorization at the 2025 AMA State Advocacy Summit held last month in Carlsbad, California.
Dr. Scott asked panelist Lucy Culp, The Leukemia & Lymphoma Society’s vice president for state government affairs, if prior authorization delays were getting better or worse.
“The evidence is really clear that the prior authorization volume continues to increase,” Culp said.
“When we put the call out to our patients: What are the challenges you're facing with insurance? By and large, prior auth is the first thing we hear,” she said.
Culp’s organization serves blood cancer patients from across the country, many of whom are seeking financial assistance and help navigating their care.
“Because these are not just incredibly complicated-to-treat diseases, they're extraordinarily expensive to treat, which means that—unless you are Warren Buffet-level wealthy—you are relying on insurance to access your care,” she said.
Culp told of a cancer patient in Wisconsin who was prescribed 12 rounds of chemotherapy by her doctor, and for each one the patient’s health plan required a separate prior authorization.
“That's just one example, and it shows the real challenge patients face and how intrusive their plans are in their overall care decisions,” she said.

Along with the patient and physician, it’s clear that “there's a third person in the exam room—and it's their insurance company,” Culp said.
Insurance companies’ overuse of prior authorization is causing patients real harm—in some instances even resulting in death. Nearly one-quarter of the 1,000 physicians the AMA surveyed (PDF) in late 2023 reported that prior authorization has led to a serious adverse event for a patient in their care, including 7% who said prior auth led to a patient’s disability or permanent bodily damage, congenital anomaly or birth defect or death.
The AMA is fighting to fix prior authorization by challenging insurance companies to eliminate care delays, patient harms and practice hassles.
Egregious action boosts bottom line
Also on the panel was Ron Howrigon, CEO of Fulcrum Strategies, a health care consulting firm specializing in payer-contract negotiation and strategic planning for physician practices. Prior to founding the firm in 2004, Howrigon spent nearly two decades working for some of the country’s largest health insurers.
Howrigon said prior authorization is getting worse and predicted it will continue to worsen in an effort to improve company bottom lines.
He cited the example of UnitedHealth Group Inc., whose stock sold for $7.50 a share 25 years ago and now sells for $520. And the pressure is on to keep the price climbing upward.
It seems as though payers believe that “the only way to do that is to make things harder” for patients, Howrigon said. “The most egregious stuff are things you can't make up.”
The most recent example of an egregious prior authorization practice came earlier that day, Howrigon said.
He received an email that morning from a rheumatology group that told him a patient of theirs was denied access to a biosimilar that had been prescribed.
That didn’t concern the physician that much because there is another medication that was very similar to the one prescribed, making it a “Coke-or-Pepsi” level decision, Howrigon said. The problem arose when the physician called the manufacturer and learned that the approved medication would not be available for months.
Rather than approve the originally prescribed biosimilar, the insurance company replied that this was “a pharmacy problem.”
“No, it's a patient problem,” Howrigon said. “These stories are everywhere. Every single physician I work with has some of these egregious stories about where this thing derails and how it delays and denies the care they want to give to patients.”
Insurers fully or partially denied 3.2 million prior authorization requests in 2023, according to a KFF report. Dr. Scott cited other findings from the report showing that only 11.7% of Medicare Advantage prior authorization denials are appealed—even though 81.7% of those appeals achieved complete or partial success in overturning a decision to deny prescribed care.
Bring the data—and patients’ stories
State lawmakers are fighting back, as more than 30 states already have introduced legislation this year to reform some part of the prior authorization process, according to the AMA Advocacy Resource Center.
Last year, states enacted 13 prior authorization-reform bills, measures that aimed to cut the volume of prior authorization requirements, reduce patient-care delays, improve transparency on prior authorization rules and boost prior auth data reporting.
Those efforts at the state level build on major 2024 federal regulatory changes to cut care delays and electronically streamline the prior authorization process for physicians treating patients in Medicare Advantage and other health plans regulated by the federal government. Together, the changes will save physician practices an estimated $15 billion over 10 years.
Legislators need to hear stories like those told by Culp and Howrigon, said T. Christian Miller, a journalist with the nonprofit news organization ProPublica. Last year, Miller wrote about how the Cigna-owned company, EviCore by Evernorth, promised client companies that, for every dollar they paid Evicore, they would pay out $3 fewer in claims.
“They love to deny things,” former AMA president Barbara L. McAneny, MD, says in Miller’s article.
Miller noted that the stories that Culp and Howrigon told have the power to persuade lawmakers and public opinion.
“Those are the stories, the individual pieces, that move mountains—and then you can back that up with data that shows this is not a unique or one-off case,” Miller said. “And that begins to attract the attention of the influencers, the policymakers, who see this as not just an aberration but a pattern.”
Dr. Scott urged the audience to visit the AMA advocacy website, FixPriorAuth.org, to share their stories about how their patients, family members or practices have been harmed by prior authorization.
A majority of the members of the U.S. House of Representatives—135 Democrats and 86 Republicans—did officially co-sponsor the bipartisan Improving Seniors’ Timely Access to Care Act of 2024 (H.R. 8702). But during the lame-duck session, Dr. Scott noted in a statement in December, Congress “missed a golden opportunity to improve patient care by refusing to include prior authorization reform in the final package—a reform with vast bipartisan support in both chambers.”
READ MORE
- NCMS Holds Successful Press Conference on Prior Authorization Reform
- NCMS Pushes for Prior Authorization Reform with Bipartisan Support from Lawmakers
- NCMS CEO Chip Baggett Featured in Podcase About Prior Authorization
- States Cranking Up Oversight of Health Insurers, NCMS Focusing on Prior Authorization in 2025
- Take Action on Prior Authorization NOW! Sign Our Petition Today!
- Share Your Prior Authorization Story!
Rep. Greg Murphy, MD with Updates from Eastern NC and Washington, DC

Representative Greg Murphy, MD (R-NC District 3) issued his latest updates from Eastern NC and from Washington, DC. They include a visit from a delegation from the NCMS to talk about protecting Medicare for patients and physicians. Here is the article from Neuse News.
Quote of the Week
In honor of President George Washington's birthday this past week, I would like to share a quote from our nation's first president:
“Human happiness and moral duty are inseparably connected.”
This past week, I returned to beautiful Eastern North Carolina for our February District Work Period. Despite the below-freezing temperatures and snow flurries brought by the recent winter storm, I was able to meet with constituents, community leaders, small business owners, and advocacy groups. I always strive to be an accessible representative and look forward to taking your concerns and priorities with me back to Congress.
In Washington, the House is working to aggressively pass President Trump’s agenda into law, including through an annual process called budget reconciliation. We are working to deliver meaningful solutions to the numerous challenges facing our nation, including on border security, energy independence, and building an economy that uplifts all Americans. This comes at a pivotal time in our history and we have a chance to enact transformational change that will impact generations to come. The American people deserve a federal government that is transparent and a good steward of taxpayer dollars.
I will continue fighting for the values of North Carolina's Third Congressional District. If you wish to stay more engaged and aware of what is happening in Washington and our District, please follow me on my socials linked above or here: Instagram, Twitter, Facebook, and YouTube.
Key Votes
Agent Raul Gonzalez Officer Safety Act
Border Patrol Agent Raul Gonzalez was tragically killed in the line of duty during a high-speed chase with an illegal immigrant while trying to protect our southern border.
CBP agents put their lives on the line every day to keep our communities safe from criminals attempting to cross our borders. Congress must do its part in protecting our courageous law enforcement officers and enact stronger penalties for illegals evading police.
I voted YES on the Agent Raul Gonzalez Officer Safety Act. Read the full text of the bill here.
Midnight Rules Relief Act
Congress is responsible for writing and enacting laws, not unelected bureaucrats in the last hours of a departing administration. Last-minute regulations, known as “midnight rules,” are a blatant attempt to constrain incoming administrations from implementing their agenda. Republicans are restoring the integrity of our system of checks and balances by ensuring elected officials retain the power to legislate our agencies efficiently.
I voted YES on the Midnight Rules Relief Act to allow Congress to disapprove multiple rules through one joint resolution if they were issued during the last year of a president’s term in office. Read the bill’s text here.
Introduced Bipartisan Legislation to Offer Hyperbaric Oxygen Therapy to Veterans
America tragically loses 17 or more veterans to suicide each day. Post-traumatic stress disorder and traumatic brain injuries (TBIs) can be effectively treated using Hyperbaric Oxygen Therapy. As a surgeon, I have used HBOT for years on patients who needed help healing their wounds.
Since entering office, advocating for new treatment pathways for our veterans has been one of my top priorities. I am proud to re-introduce the Veterans National Traumatic Brain Injury Treatment Act, which builds on legislation I sponsored and got passed while serving in the North Carolina State Assembly to make HBOT accessible for veterans in North Carolina.
We must do more for our veterans who have made so many sacrifices for the safety and well-being of our nation.
Read my press release here.
Read my OpEd in the Daily Reflector here.
Introduced Legislation to Establish a National Plan for Epilepsy Research and Treatment
It is a privilege to co-lead the re-introduction of the National Plan for Epilepsy Act, bipartisan and bicameral legislation to improve patient outcomes and prioritize effective treatments.
One in 26 people will develop a form of epilepsy in their lifetime and 3.4 million Americans currently live with epilepsy. As a physician of over 35 years, I have taken care of countless patients who deal with epilepsy every day. This medical challenge faces so many individuals and families.
As Co-Chair of the Epilepsy Caucus, I am proud of the awareness we are raising about epilepsy and the meaningful action we are taking to create a brighter future!

Ways and Means Health Subcommittee Hearing on Modernizing American Health Care
An unhealthy America doesn’t just affect our health care industry; it has costly effects on our economy. Six in 10 Americans have at least one chronic disease, such as cardiovascular disease, diabetes, cancer, and obesity, which are among the leading causes of death in the U.S. Furthermore, Medicare and Medicaid spend a whopping $384 billion annually to treat such diseases.
The Ways and Means Health Subcommittee held a hearing examining how healthier options and better incentives can bend the cost curves from our nation’s declining health. For instance, employers can incentivize employees to take charge of their health and wellness, which reduces health care costs and increases labor productivity.
Watch my remarks here.

House Administration Committee Hearing Reviewing House Committees' Budgets
The House Administration Committee is responsible for overseeing the operations of the House of Representatives, including our committees’ budgets. Last week, we hosted the Chairman and Ranking Member of each committee to review their budget requests for the 119th Congress.
We must ensure that your taxpayer dollars are used appropriately and efficiently to conduct the People’s business.

Received an Update on Hurricane Helene Recovery Efforts from NC National Guard
Ensuring that Western North Carolina receives the necessary support for recovery from Hurricane Helene has remained a top priority of mine. I appreciate the visit from North Carolina National Guard’s Major General Todd Hunt, who shared an update with me on the guard’s ongoing response.
I will continue to support the folks out west and I am extremely grateful for our dedicated National Guardsmen who have been on the ground throughout the past four months. Please join me in praying for our National Guard and those they are serving in the mountains.

Welcoming Craven County Educators to Washington
Craven County is lucky to have Elizabeth Hodge and Nardi Routten, two outstanding educators!
It was also a pleasure to formally congratulate Nardi on receiving the Presidential Award for Excellence in Mathematics and Science Teaching. It is the highest award K-12 teachers can receive for instruction in those two subjects by the federal government.
Meeting with Jewish Federations of North America on our Fight Against Antisemitism
It was an honor to meet with representatives from the Jewish Federations of North America. We discussed the rise in antisemitism in the health care industry and medical education.
The United States must stand with our ally Israel. Antisemitism has no place in ANY institution.
Meeting with NC Healthcare Professionals on the Challenges Facing American Physicians
Physicians across the state are experiencing massive Medicare reimbursement cuts, making it harder for patients to receive high-quality, affordable care.
NC healthcare professionals stopped by my office to talk about how the rising costs and declining pay from Medicare are affecting their practices. In our discussion, I brought up my Medicare Patient Access and Practice Stabilization Act, which supports physicians and protects access to care for Medicare beneficiaries.
In Congress, I will continue to advocate strongly for our physicians who dedicate themselves to building a healthier America every day.

Protecting Medicare for Patients and Physicians with the American Medical Association
I was honored to speak at the American Medical Association’s Patients Action Network event. I highlighted the consequences of the Medicare payment crisis and the urgent need for permanent, sustainable reform to ensure access to care for America’s patients.
Time is running out to address the issues facing Medicare. American physicians are at a breaking point, and the ability for millions of Medicare patients to receive high-quality, affordable care is at risk. Congress must pass my Medicare Patient Access and Practice Stabilization Act so that our seniors can continue to access the medical care they deserve.
Read the rest of the article by clicking here.
In Memoriam: NCMS Past President Dr. Henry James Carr, Jr.
Dr. Henry James Carr, Jr.
August 27, 1929 - February 22, 2025

NCMS Past President Dr. Henry James Carr, Jr. died February 22, 2025 at the age of 95
(Royal Hall Funeral Home) -- Dr. Henry James Carr, Jr., 95, joined his Lord and Savior peacefully from his home on Saturday, February 22, 2025.
He was born on August 27, 1929, to the late Meda Iola Spell and the late Henry James Carr from Roseboro, NC. Preceding him in death was his brother, Harold Spell Carr.
Left to cherish his memory are his wife of 68 years, Barbara Ruddle Carr, of the home, four sons: Henry James Carr, III (Becky) of Clinton; William Curtis Carr (Nancy) of Clinton; David Ruddle Carr (Kathy) of Winston-Salem; Robert Spell Carr (Wendy) of Clinton; one daughter, Meda Carr Piner (Andy) of Greenville, NC; his sister, Ava Marie Carr Lavery (Bill) from Mt. Pleasant, SC; 19 grandchildren; 24 great-grandchildren with another one on the way, and many cherished nieces and nephews.
Henry received his medical degree from Duke University School of Medicine in 1954 following his studies at Elon College and Wake Forest University. He met the love of his life while training at Pennsylvania Hospital in Philadelphia. After serving in the Unites States Air Force as a physician and surgeon in Hahn, Germany, he and Barbara returned to his native North Carolina in 1961 to join a small internal medicine practice in Sampson County. In 1988, he accepted a position with NC State Health Department, treating tuberculosis patients in health departments and prisons throughout NC. During his career, Henry served his profession with honor and enthusiasm as president of the Sampson County Medical Society, president of the NC College of Internal Medicine, and finally as president of the North Carolina Medical Society (NCMS) from 1987-1988. He served on numerous NCMS committees, including the Executive Committee for approximately twenty years and served on the NCMS Executive Council as chair of the North Carolina delegation to the American Medical Association. Henry served for six years as president of the North Carolina Medical Society Foundation, the philanthropic and service arm of the NCMS, helping to recruit physicians to rural and medically under-served communities in North Carolina and improving access to health care for the uninsured. In addition, he was a founder and former chairman of the board and president of the Medical Mutual Insurance Company, which serves the professional liability insurance needs of NC physicians. Henry was a founding director and former vice president of Carolina Doctors Care, a statewide preferred provider organization created by the NCMS for its members, and former director and secretary of its subsidiary, Health Care Savings. Henry was awarded the Distinguished Alumnus Award by the Duke Medical Alumni Association and, later, The Order of the Long Leaf Pine.
Some of Henry and Barbara’s happiest times were made in Sebring, Florida and Topsail Beach, NC with their children, grandchildren, and great-grandchildren.
The family wishes to thank his loyal caretakers including Connie, Alma, Marguerite, Kay, Pearl, Carolyn, Shnetta, Ann, Jenny, Shannon, Jalissa, Val, Constance, and Helen and the team from 3HC for their diligent and compassionate care.
Funeral service will be held on Sunday, March 2nd at 1:00 pm at First Methodist Church of Clinton, NC with Reverend Matt Seals officiating. The family will receive friends following the service in the church fellowship hall. A private burial with military honors will follow in the Clinton Cemetery.
In lieu of flowers, memorials may be made in Dr. Carr’s memory to First Methodist Church of Clinton, NC and Emma Anderson Memorial Chapel of Topsail Beach, NC.
Condolences may be sent to the family by visiting www.royalhallfuneralhome.com.
Duke and Duke-NUS Forge New Frontiers in Climate Health Research with S$1 Million Funding

-
The two institutions awarded more than S$1 million to accelerate five promising areas of research collaboration
-
Dedicated Research Collaboration Pilot Project grant combines expertise from Singapore and the US for bigger impact
-
First time in the grant’s 15-year history that it focuses exclusively on the effects of climate change on human health
Duke University and Duke-NUS Medical School are proud to announce the recipients of their latest Research Collaboration Pilot Project grants, totaling more than S$1 million. These grants underscore the synergy between the institutions and their shared commitment to addressing the urgent challenges posed by global warming and climate change on human health.
For the first time in its 18-year history, this year’s grant initiative is dedicated entirely to climate-related health research, emphasizing the partnership’s focus on making meaningful contributions to this critical global issue. Each of the five innovative projects brings together top researchers from Duke and Duke-NUS, reflecting a strategic alignment that leverages unique strengths from both institutions, with the objective of developing international research teams that will advance basic, translational and clinical research.
For each project, the Duke Principal Investigator (PI) will receive US$100,000 and the Duke-NUS PI will receive S$100,000 for a period of two years.
Climate is an area of synergy between the institutions as both Duke and Duke-NUS have made tackling this global threat a priority. Faced with increasing temperatures, urbanization and environmental pollution, affecting industrialised nations such as Singapore, the USA and low- and middle-income countries, Duke and Duke-NUS are bringing together experts from different specialties to investigate and address the impact of climate change on human health.
Patrick Tan, Senior Vice-Dean for Research at Duke-NUS, said:
“Our decision to focus this year's grants on climate change stems from our recognition of the escalating health impacts due to increasingly extreme weather conditions. By combining Duke's robust research capabilities with Duke-NUS's strategic location and expertise, we are uniquely positioned to lead efforts that anticipate and mitigate health crises arising from climate change.”
This partnership not only aims to produce world-class research but also to develop practical solutions that can be implemented in regions most affected by climate change, including both the US and Singapore, as well as other parts of the world.
“These new Duke and Duke-NUS investigator teams are the first of many steps required to foster global connections and research needed to address the critical public health challenge of climate change and its health impacts,” said Robert M Tighe, MD, an associate professor of medicine and leader of Duke University School of Medicine’s climate research strategy.
“This effort continues the ever-strengthening relationship between Duke and Duke-NUS with a new focus on climate and health research. I look forward to seeing how these projects develop.”
After a competitive review process involving 40 initial proposals, five exceptional projects listed below were selected under the Research Collaboration Pilot Projects funding. This year’s theme is dedicated to tackling health issues arising from climate change, reflecting both institutions' commitment to innovative and impactful research.
- Climate change and health: Exploring how heat exposure contributes to urinary stone disease, with implications for preventive healthcare practices.
- Community resilience: Investigating the perceptions and experiences of health effects related to climate change among vulnerable older adults in Durham, North Carolina, USA, and Singapore to enhance health communication strategies.
- Environmental impact: Assessing the acute cardiopulmonary outcomes related to wildfire smoke and heat exposure in Southeast Asia, aiming to inform public health responses and policy.
- Vulnerable populations: Conducting an interdisciplinary analysis of heat stress and kidney health among communities on the climate frontlines in Sri Lanka, using a planetary health approach to better understand and mitigate these impacts.
- Infectious diseases: Studying how environmental factors and market dynamics influence the regional spread of infections in Madagascar, to improve disease prevention and control strategies.
| TITLE: Climate change, heat exposure and urinary stone disease
PIs: Charles Scales (Duke PI), Chong Tsung Wen (Duke-NUS PI) SUMMARY: The research will focus on understanding the relationship of increasing temperatures from climate change, the incidence and health care utilization for kidney stone disease and assessing disproportionate impact of climate change on vulnerable populations. The investigations will link temperature data with medical records on a geospatial basis over time, to understand relationships between temperature, local infrastructure and health care utilization for stone disease. The results will provide key data to support the development of interventions to increase heat resilience among individuals at risk for stone disease. In addition, understanding risk factors disproportionately impacting vulnerable populations offers the opportunity to increase climate-related health equity in both Singapore and North Carolina. |
| TITLE: Perception and lived experience of health effects of climate change among vulnerable older adults residing in Durham and Singapore – informing health communication interventions
PIs: Hanzhang Xu (Duke PI), Rahul Malhotra (Duke-NUS PI) SUMMARY: Climate change, manifested through extreme weather events, temperature fluctuations and rising sea levels, poses significant health risks for older adults, aged 60 years and older. Additionally, vulnerable older adults – those with low socio-economic status, those living alone and those with multiple chronic conditions – face increased climate change-related health risks given their limited access to information and resources, existing physiological decline and potential disruptions to their healthcare and social support. Study findings will inform targeted health communication interventions aimed at enhancing climate change resilience among vulnerable older adults, and influence healthcare policies on ageing and climate change in Durham and Singapore. |
| TITLE: Impact of wildfire smoke and heat on acute cardiopulmonary outcomes in Southeast Asia
PIs: Vijay Krishnamoorthy (Duke PI), Marcus Ong Eng Hock (Duke-NUS PI) SUMMARY: Climate change is increasing the frequency and severity of extreme heat events and amplifying wildfire intensity. Communities, healthcare professionals, and policymakers urgently need high-quality data to guide decision-making. Vulnerable populations are most affected by climate change, making it crucial to produce evidence on the extent of this impact. High-resolution data on the health benefits of climate action can form the backbone of international climate mitigation policies and applied to climate change models of future warming scenarios. |
| TITLE: Heat stress, kidney health and lived experience of communities in the climate frontlines in Sri Lanka: an interdisciplinary population health analysis through a planetary health lens
PIs: Nishad Jayasundara (Duke PI), Renzo Guinto (Duke-NUS PI) SUMMARY: This interdisciplinary mixed-method study aims to unpack the connections between heat stress, kidney health and lived experience of communities affected by these interlocking challenges in the climate frontlines in Sri Lanka. It will be investigated through epidemiological approaches that build on an existing cohort as well as through key informant interviews of farmers and health system and community health needs assessment. |
| TITLE: Linking environments and markets to understand regional spread of infections along networks in Madagascar
PIs: Charles Nunn (Duke PI), Gavin Smith (Duke-NUS PI) SUMMARY: Climate change is having both direct and indirect impacts on Madagascar’s rural populations, who are primarily small-holder farmers engaged in subsistence agriculture. One of the primary ways this population is addressing climate-induced food insecurity is by selling livestock, which requires travel from their rural villages to more central markets via the taxi brousse (bush taxi) system. This process entails placing livestock into crowded spaces, either on a taxi brousse (for travel) or in markets (for sale), leading to potential viral mixing and the emerging of panzootic and/or pandemic diseases. The results of this project will allow for competitive external proposals at the intersection of climate change, adaptation, global health security and emerging infectious disease. |
Proposals were rigorously evaluated based on scientific merit and the potential for successful collaboration between Duke and Duke-NUS co-principal investigators (Co-PIs). This process ensures that only the most promising and collaborative projects receive funding.
Since 2009, the Duke-Duke-NUS partnership has funded 64 projects with a total of S$7.29 million, demonstrating a long-standing commitment to fostering innovative research that addresses some of the most urgent health challenges facing the world today. This year’s focus on climate health is a continuation of this mission, pushing the boundaries of what can be achieved through international research collaboration.
Beyond the Horizon: The Changing Landscape of Rare Disease Treatments

Help celebrate Rare Disease Day this year!
On Friday, February 28th, the National Organization for Rare Disorders (NORD) Center of Excellence and the Program for Precision Medicine in Health Care (PPMH) will be hosting a Symposium, “Beyond the Horizon: The Changing Landscape of Rare Disease Treatments.” During this symposium, speakers will address:
- The past, present, and future of rare disease research and treatment at UNC
- The patient and family experience with rare disease diagnosis and treatment
- Rare disease community engagement and philanthropy at UNC
The symposium will be from 2pm-5pm on Friday February 28 in MacNider 321.
There are options for in-person and virtual attendance. Please RSVP here.
The speaker list includes: Jonathan Berg, MD, PhD; Muge Calikoglu, MD, MPH; Sam Young, PhD; Matthew Hirsch, PhD; Yael Shiloh-Malawsky, MD; Senyene Hunter, MD, PhD; Carlee Friar, BS; Patricia Sullivan; Eleanor Bolton; Karen Hogan, DNP, RN; & Mary Gard, MA
The full agenda can be found on the website.
If you have any questions, please email [email protected].
🎉It's New Member Monday!🎉

Join us in welcoming these new members to the North Carolina Medical Society!
- Krishna Chaitanya Alluri, MD
- Philip N. K. B. Asamoah, MD
- Vanessa K. Bair, PA C
- Sabina Custovic, DO
- Sunny R. Franken, PA
- Byron Gaing, MD
- Monika D. Gonzalez Kroll, PA C
- Christopher A. Hess, MD
- Prarthana P. Jain, DO
- Laurence B. Kempton, MD
- Charlotte Lanier
- Liza G. Schaffner, MD
- Demetra V. Schermerhorn, MD
- Janelle White, MD
We are thrilled to have you!
Not a member but would like to be? Joining is simple. Visit our membership center here.
NCMS Foundation Partner Alliance Medical Ministry is Seeking a Full Time Physician, MD, or DO

PRIMARY CARE PHYSICIAN SOUGHT BY ALLIANCE MEDICAL MINISTRY
Position: Primary Care Physician AMM is seeking a full time Physician, MD or DO, to work closely with the Medical Director to carry out the mission of Alliance Medical Ministry; provide compassionate, culturally appropriate holistic care; and grow the capacity to serve the eligible uninsured population. The physician provides preventive and direct medical care, telehealth, contributes to wellness programs, and teams with nurses and medical assistants to lead the delivery of high-quality health services. Physicians may serve as supervisor for PA’s or NP’s and as preceptors for medical students or advanced practice providers students. This is a quality-of-life position for an individual inspired by Mission driven work with underserved populations.
Alliance Medical Ministry is a 501c3 free/charitable clinic providing comprehensive primary medical care for working uninsured adults. AMM is a Patient Centered Medical Home whose professional medical staff has a mission to reduce health disparities in Wake County. Primary Care Providers collaborate with a team of nurses, medical assistants, behavioral health counselors, social worker, community health workers, registered dietitian, farmer/wellness coordinator, and administrative experts to deliver compassionate healthcare. AMM’s multidisciplinary team aims to address the physical, mental, social, and spiritual issues important for each patient to achieve optimal health.
Mission: Alliance Medical Ministry provides access to compassionate, whole-person primary care for working, uninsured adults in order to reduce health disparities in Wake County.
Contact for more information:
Edwin K. Burkett, MD, MBA, CPE
Medical Director
919.250.3320 Office
NCDHHS Announces First Pediatric Flu Death of Season

NCDHHS Urges Flu Vaccination for Children Ages 6 Months and Older
NCDHHS recently reported two pediatric flu-related deaths, the first for the 2024-2025 flu season. According to the Respiratory Virus Summary Dashboard, North Carolina has seen a rise in flu cases in combination with continued COVID-19 activity.
Flu vaccinations are especially important for children who are at higher risk of developing severe disease or complications, including those younger than 5 years old, especially under 2 years, or those with chronic health conditions like asthma, diabetes or a weakened immune system.
The CDC recommends all children ages 6 months and older receive a seasonal flu vaccine and an updated COVID-19 vaccine. Parents should also talk with their health care provider about options to protect infants from severe RSV disease, including vaccines for pregnant women during weeks 32 through 36 of pregnancy.
For more information on respiratory viruses, including how to access vaccines, testing and treatment in your community, visit vaccines.gov/en, flu.ncdhhs.gov or covid19.ncdhhs.gov.
'A Real Game Changer': UNC is Part of a Groundbreaking Food Allergy Study

Their work showed that a treatment that has helped asthma patients for more than two decades could lessen — or even prevent — acute allergic reactions to foods.
(NC HealthNews, Jennifer Fernandez) -- Kristen Bush remembers the first time her firstborn suffered a severe allergic reaction.
Braylon was 7 months old, and he had just started eating solid foods. That night, it was a few pieces of one of those little puff cereals. About an hour later, Bush was nursing her son before bed.
“He just kept, like, choking and coughing and choking. And we were like, ‘What is going on?’” she recalled.
When she unzipped his onesie, Bush saw Braylon’s body was covered in hives. They used an Epipen that their pediatric allergist had given them as a precaution, then took him to the hospital where their baby boy was monitored for a few hours before going home.
Neither she nor her husband, Josh, has allergies. There’s no history of allergies in either of their families.
“In the beginning, it was a little bit hectic, I would say, and stressful,” Bush said about learning how to deal with her son’s food allergies.
She signed up Braylon, who’s now 5, for a study at UNC Chapel Hill that is aimed at helping kids and adults who are allergic to multiple foods. Braylon tested as allergic to peanuts, milk, wheat, eggs, tree nuts, sunflower and sesame.
Last year, the Food and Drug Administration approved the medicine used to treat Braylon during the study — co-authored by three UNC Chapel Hill researchers — to treat food allergies based on the study’s early-phase results. Their work showed that a treatment called omalizumab, which has helped asthma patients for more than two decades, could lessen — or even prevent — acute reactions to food allergies.
“As a parent of a kid who has allergies, it gives me peace of mind,” Bush said. “[It] also gives him a lot more food freedom.”
‘A real game changer’
“Omalizumab is going to be a real game changer when it comes to food allergy,” said Edwin Kim, chief of the Division of Pediatric Allergy and Immunology and director of the UNC Food Allergy Initiative at the UNC School of Medicine.
Kim worked on the study with colleagues Corinne Keet, professor of pediatrics and associate director of UNC Children’s Research Institute, and Mike Kulis, a pediatric allergy and immunology associate professor and member of UNC Children’s Research Institute. Researchers at Johns Hopkins and Stanford universities led the project.
“This gives us something that we can offer in the clinic now that will provide a level of protection,” said Kim, who sees patients with allergies in his practice.

The patient must stay on the medication to benefit from the effects. And it’s an injection, which some people won’t like.
“It will help a lot of people out there, but it won’t be for everybody,” Kim said.
Some patients may decide to stay on the medication long term. For others, it might be for specific time periods. He’s seeing those decisions in his clinical practice.
“The people that have expressed probably the most interest are people that are experiencing transitions in their lives,” he said.
He gave the example of a college student leaving home and learning to cook for themselves for the first time after having a parent supervise their food intake. Another example, he said, is when young children first attend school.
Allergies increasing in children
More than 33 million people in the U.S. have a serious and potentially life-threatening food allergy, according to Food Allergy Research & Education, a Virginia-based nonprofit. The group says that food allergy sends a patient to the emergency room every 10 seconds.
The number of children with at least one food allergy has been steadily growing, with 5.6 million children — nearly 8 percent — allergic to some type of food. That’s equal to one in 13 children, or about two per classroom.
So what causes an allergic reaction? When our bodies encounter a foreign substance, whether it’s a virus or a bacteria or a food molecule, pet dander or certain foods, specialized immune system cells known as B cells kick into action. The B cells produce proteins known as antibodies that target those foreign substances, surround it and help our bodies process it for removal. With an allergen, the body perceives it as a threat, flooding the system with antibodies and other chemicals, going into overdrive to attack the usually harmless substance.
This overreaction by the immune system leads to symptoms ranging from watery eyes and hives to breathing problems and even death when severe cases aren’t treated quickly.
There’s no cure for allergies, although children often outgrow allergies to such protein-rich foods as milk, egg, wheat and soy. Children with allergies to peanuts, tree nuts and shellfish generally remain allergic into adulthood, research shows.
Medication can help manage symptoms. Now omalizumab, which is sold under the brand name Xolair, can be used to lessen or avoid severe food allergies.
From asthma to food
Omalizumab is a monoclonal antibody — a lab-made protein that acts like an antibody. Monoclonal means these antibodies are cloned copies of a single antibody.
The U.S. Food and Drug Administration first approved omalizumab in 2003 to treat moderate to severe asthma. In 2014, the FDA expanded its use to treat hives and again in 2020 to treat chronic sinus inflammation. Last year, the agency approved omalizumab to be used for food allergies, based on preliminary data from the trial that involved Kim and the other UNC researchers.
“We’ve always suspected that it should work for food allergy,” Kim said. “It’s just we had to actually do the studies to prove it.”
In 2019, researchers began studying omalizumab’s use for food allergies with funding from the National Institute of Allergy and Infectious Diseases, part of the National Institutes of Health.
UNC School of Medicine was one of 10 sites participating in the multi-stage trial that enrolled 177 children and three adults. Twenty-five North Carolina families participated.
Participants received injections every two to four weeks over a four- to five-month period. Nearly 67 percent who finished the full treatment could eat what amounted to two and a half peanuts without an allergic reaction, the university said in a news release. That was much higher than in the placebo group, where fewer than 7 percent could eat that much peanut protein without an allergic reaction.
It also represented a six-fold increase in how much peanut protein the participants could tolerate at the beginning of the trial.
The treatment increased the amount of peanut, tree nuts, egg, milk and wheat that children with multiple food allergies could consume without an allergic reaction.
“The way the medicine works is it grabs all of this allergic antibody, whether it’s for one food or all the foods, and gets rid of all of it,” Kim said. “But what’s important to keep in mind for patients is that it doesn’t get rid of the actual cells in the body that make those antibodies.
He explained that when patients stop the medication, B cells — which can remember foreign substances for years after encountering them — will make the antibody again.
“Over a period of time, and we don’t know, maybe a couple of months, something like that, we anticipate that the allergy would come back,” he said.
Participating in the study
The families involved in the study were very committed, Kim said. The study kicked off in 2019, but was paused during the COVID-19 pandemic.
“Not a single parent, not a single family dropped out of the study when it restarted,” Kim said.
The Bush family spent two years going to Chapel Hill every two to four weeks. They live in Charlotte, so that’s a two-and-a-half hour drive each way.
Braylon participated in all three phases of the study. It started out with injections of the medicine. That evolved to oral immunotherapy, where he was given small amounts of the allergen to build up his tolerance. The final phase was transitioning into solid, everyday foods.
During the oral immunotherapy, Bush said they tried everything to entice Braylon to eat the small protein samples. They added it to applesauce or put sprinkles on it.
“But doing something every day and getting them to eat something every day was definitely a challenge,” she said.
Kim said the families went through a lot because they had to expose their children to foods that they knew would cause an allergic reaction.
“These kids … were having allergic reactions multiple times in the study to prove that this was working,” Kim said. “They stayed committed and helped to actually make this a reality for everybody else that’s out there.”
Social isolation
For children, food allergies can have a big impact on their ability to socialize. They even get bullied, teased or harassed over their allergies, research shows.
Parents often avoid going to restaurants or find one or two that they trust, Kim said. He said parents also may limit or avoid visits to friends’ homes.
One study showed that more than a quarter of parents who were surveyed during food allergy appointments said their children do not participate in camp or sleepovers. Ten percent said they homeschool their children to avoid exposure to foods that trigger allergies.
About two in five students with food allergies have at least one allergic reaction while at school or a school-related activity, according to a recent report by the advocacy organization Food Allergy Research & Education. The group also said that about eight in 10 food allergy reactions in schools take place in the classroom.
Bush always has snacks with her when they go to parties or events in case Braylon can’t eat some of the food that’s there. That way he always has some special food just for him so he doesn’t feel left out.
She said their school has been great about letting her know when there are events coming up with food so that she can be prepared.
Their family also makes sure to share information about allergies with people, including to not give food with kids unless you know they aren’t allergic to it.
In social gatherings, adults don’t think twice about encouraging a child to grab some food, Bush said.
“One of the first times we had been together with friends, I wanted to … slap a sticker and … a hat on [Braylon] that said … ‘I have allergies, do not feed me,’” she said.
Pushing science forward
More than a year after finishing his part in the study, Braylon can now better tolerate foods that once led to severe allergic reactions. He can have a slice of pizza or the occasional store-bought cupcake. That’s life-changing for a kid, Bush said.
“For him to be able to … go to a restaurant and not have a fear of … something happening, or us not having to be as strict with what he’s eating, has been a really exciting moment for our family,” she said.
While Braylon is no longer taking omalizumab, he must eat small amounts of the foods he is allergic to every day to maintain the tolerance he has built up. He gets a Reese’s Cup, some pretzels, and either a cheese stick or yogurt. He calls them his “allergy snacks.”
“He doesn’t understand the gravity of the situation, but it’s like, you helped science kind of push this forward,” Bush said.
National Geographic recently recognized the omalizumab study as one of the top medical breakthroughs in 2024, and the New England Journal of Medicine cited it among its list of studies that “stand out among the year’s most notable and impactful in clinical medicine” in 2024.
“It makes me excited that we were able to be part of it and that [Braylon] played a role in making sure that it was studied properly and successfully,” Bush said. “I’m really proud of him for going through it.”
Get your REAL ID – Deadline: May 7, 2025
Get your REAL ID – Deadline: May 7, 2025
The deadline for obtaining a REAL ID is May 7, 2025. The Transportation Security Administration (TSA) has issued a reminder that, as of that date, every air traveler 18 years of age and older must have a REAL ID-compliant state-issued driver’s license, state-issued identification card or another acceptable form of ID to board a commercial aircraft.
More information and Frequently Asked Questions on REAL ID can be found at REAL ID FAQs | Homeland Security.
FEMA Extends Application Deadline for North Carolinians Affected by Tropical Storm Helene
At the request of the state of North Carolina, Tropical Storm Helene survivors now have until March 8, 2025, to apply for assistance with FEMA.
With the extended deadline, FEMA still strongly urges survivors to apply as soon as possible. After the deadline of March 8, you may still submit documents, update your contact information and stay in contact with FEMA regarding your application, but you must apply before the deadline.
FEMA assistance may include funds for temporary housing such as rental assistance or reimbursement for hotel costs; funds to support the repair or replacement of a primary home, including privately-owned access routes, such as driveways, roads, or bridges; and funds for disaster-caused expenses, such as repair or replacement of personal property and vehicles, funds for moving and storage, medical, dental, child care and other miscellaneous items.
Homeowners and renters in Alexander, Alleghany, Ashe, Avery, Buncombe, Burke, Cabarrus, Caldwell, Catawba, Cherokee, Clay, Cleveland, Forsyth, Gaston, Graham, Haywood, Henderson, Iredell, Jackson, Lee, Lincoln, Macon, Madison, McDowell, Mecklenburg, Mitchell, Nash, Polk, Rowan, Rutherford, Stanly, Surry, Swain, Transylvania, Union, Watauga, Wilkes, Yadkin and Yancey counties and the Eastern Band of Cherokee Indians with uninsured losses from Tropical Storm Helene may apply for FEMA assistance.
There are several ways to apply:
- Visit a Disaster Recovery Center (DRC) to find the center location nearest you go to fema.gov/drc.
- Go online to DisasterAssistance.gov.
- Download the FEMA App for mobile devices.
- Call the FEMA helpline at 800-621-3362 between 7 a.m. and midnight. Help is available in most languages. If you use a relay service, such as video relay (VRS), captioned telephone or other service, give FEMA your number for that service.
ALL IN: Caring for North Carolina's Caregivers Phase 2 Kick-Off is February 25
NCCPRW is looking to have every NC health system and hospital partner on statewide initiative
The North Carolina Clinician and Physician Retention and Well-being (NCCPRW) Consortium, in collaboration with the Dr. Lorna Breen Heroes’ Foundation, launched ALL IN: Caring for North Carolina’s Caregivers. This initiative is dedicated to supporting healthcare organizations across North Carolina in redesigning their workplace environments to better support their staff’s wellbeing and mental health.
As we continue advancing ALL IN: Caring for North Carolina’s Caregivers, we are eager to have every North Carolina health system and hospital partner with us in this important statewide initiative.
Join us on ZOOM - Tuesday, February 25, 2025, 2:00 – 3:00 p.m. ET for our Phase 2 Kick-Off
During this session, we’ll be sharing what teams can expect from their participation in Phase 2: Learn the Wellbeing Systems Approach, and how it will set teams up for success in Phase 3: Integrate Wellbeing into Operational Improvement.
Note: Phase 1 is not a pre-requisite for Phases 2 and 3.
If your organization would like to participate in the kick-off meeting or has any questions, please reach out to Monecia Thomas, Executive Director, NCCPRW at [email protected].
NCMS at Work: Medical Care Commission

North Carolina Health Commission Meeting
Key Updates
The North Carolina Health Commission recently convened to discuss major healthcare initiatives, funding, and regulatory updates affecting the state. NCMS staff attended this event to keep you informed and advocate for member voices. Find details from the meeting here:
New Appointment to the Commission
Michelle F. Jones, MD, a family physician and NCMS member, has been appointed to the commission, bringing her expertise in community health and patient care.
Bond Program & Healthcare Expansion
With $4.7 billion in outstanding debt from bond series, the commission discussed the impact of Medicaid expansion, which is expected to drive new hospital construction projects across the state.
Duke Health Project Proposal
Duke Health presented a proposal addressing hospital acquisitions and facility expansion, highlighting their $1.1 billion in charity care and $4.8 million in bad debt. The approved motion includes:
- Lake Norman Hospital Refinancing – 123-bed acute care hospital with 24 physicians
- Duke Health Cary Phase II Expansion – Emergency department, imaging, ambulatory surgery center, and infusion services
- Bond Premium – Approximately $460 million
- Regulatory & Licensing Updates
Several healthcare regulations were reviewed and approved for public comment, including:
- Nursing Pool Licensure
- Mammogram & Pap Smear Certification
- Healthcare Personnel Registry
- Hospital Transfers & Discharges
- Emergency Medical Services & Trauma Rules
- Ambulatory Surgical Facility Licensing
- Hospital Licensing Rules
*These updates will ensure healthcare facilities maintain high standards for safety, licensing, and patient care.
For more details, view the full agenda and packet here.
Bird Flu Cases Confirmed in North Carolina Waterfowl

Cases rise across nation as NCDHHS speak out
A bird found dead at a Hendersonville lake has tested positive for bird flu, according to local officials.
The Henderson County Department of Public Health announced on Tuesday that on February 8, officials were notified of five dead birds at Osceola Lake, a privately owned lake in Hendersonville. One of the birds was submitted to the state for bird flu testing and yielded a positive result for H5N1, or bird flu.
The health department has provided guidance to the owner of the lake as well as to homeowners, guests and others who have been allowed to use the lake for recreational purposes.
The owner has also posted signage stating contact with birds should be avoided.
The bird is at least the third confirmed case of bird flu in western North Carolina. In 2024 a dead duck found at Lake Louise tested positive for bird flu, and in January waterfowl at a Buncombe County park also tested positive.
Also in January a small game flock of birds also tested positive for bird flu.
Bird flu is a disease that can affect most species of birds and some mammals, according to the N.C. Department of Health and Human Services. These viruses naturally spread among wild aquatic birds worldwide and can also infect domestic poultry and other birds and animals, health officials said.
The risk of bird flu spreading to humans is low, according to health officials, and most cases happen when someone has direct contact with an infected bird or their feces.
"Avian influenza viruses rarely infect people," NCDHHS officials said.
Symptoms of bird flu include fever, cough, shortness of breath, runny nose and red, irritated eyes.
"Birds, their feces and saliva should be avoided by the public," health officials urge. "People should avoid contact with sick or dead animals."
If a dead bird needs to be disposed of, health officials recommend wearing gloves or using a plastic bag turned inside out. Those who have direct contact with wild birds or sick animals are also advised to wear protective equipment.
"Wild birds can be infected with the virus even if they don't look sick," Health Department officials said.
Click here for a list of bird flu cases in North Carolina over the past few years.
*This article contains information from Spectrum 1 and WSPA
AMA Honors NC Public Health Official with Government Service Award
AMA honors North Carolina public health official with Government Service Award
The American Medical Association (AMA) presented Cumberland County (N.C.) Public Health Director Jennifer Green, PhD, MPH., with the AMA Award for Outstanding Government Service. Having served in her current role since 2019, Green has overseen the delivery and promotion of public health services, strategies, and initiatives in Cumberland County. She played a key role during the COVID-19 pandemic, mobilizing the community, distributing resources, and setting up drive-thru vaccine clinics that prompted Gov. Roy Cooper to praise the County’s response as a shining example of high-quality local government.
The award was presented during the AMA’s annual National Advocacy Conference (NAC) in Washington, DC.

“Across the country, local public health officials played a critical role in combatting COVID-19, educating local communities, and saving lives. Jennifer Green epitomizes that commitment and leadership,” said AMA Board Chair Michael Suk, M.D., JD, MPH, MBA. “For her dedication to improving the lives of people – both during and well beyond the COVID-19 pandemic – and for her creative approach to helping address public health challenges in Cumberland County, it is an honor to present Jennifer Green with the AMA Award for Outstanding Career Public Servant at the Local Level.”
“Dr. Green has provided exemplary care to our citizens with innovative programs and ideas,” said Cumberland County Commissioner Glenn Adams, who nominated her for the award. “She has had a tremendous impact on the lives of our citizens and the health of our county.”

In addition to her vital work during the COVID-19 pandemic, Green opened a WIC clinic to expand the scope of services and promote healthy babies and mothers. She created Healthy Conversations, which promotes public health education by training barbers and stylists to be advocates who can influence positive health behaviors in under-resourced communities. She created the Maternal Health project to address the disparities of mothers of color in seeking pre- and post-natal health care. And she is leading efforts to combat the opioid epidemic in her community by working to establish a recovery resource center.
UNC Study: Some Viruses ‘Freeze’ Their RNA to Replicate
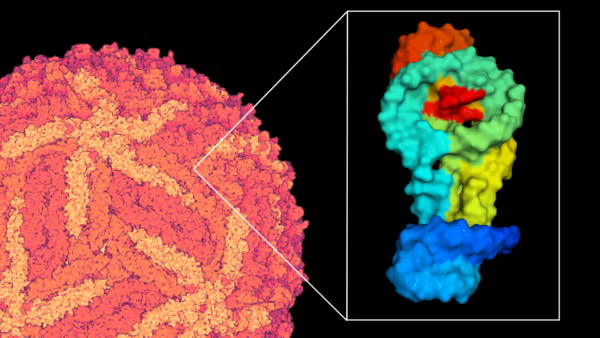
Researchers have discovered that RNA in Zika virus can freeze itself in time to further its spread in the body, revolutionizing how researchers study disease-causing viruses.
(UNC Health Newsroom) -- They say that change takes time. Well, that’s not the case for RNA.
The small biological molecule acts like a switchboard operator, capable of changing its shape every few milliseconds so it can manipulate biological functions in the body. It has big jobs to carry out, after all, like copying genetic information into every living cell and activating the immune response.
A new multidisciplinary study from biophysicists and virologists at the UNC School of Medicine challenges this idea of shape-shifting RNA. Helen Lazear, PhD, associate professor of microbiology and immunology, and Qi Zhang, PhD, professor of biochemistry and biophysics, have discovered that a type of RNA in Zika virus, a mosquito-borne virus, can essentially freeze itself in time in an effort to make more copies of itself and further its spread in the body.
Their findings have not only sent ripples through the field of virology, but it has also given researchers new ammo in the fight against RNA viruses. Their study, which was published in Nature Chemical Biology, paves the way for new therapies that can “un-freeze” these RNA structures to combat other mosquito-borne RNA viruses.
“We know that Zika virus and related viruses rely on these very stable RNA structures to replicate,” said Lazear. “By adjusting the stability of this RNA in the lab, we showed that we can shorten its lifespan and make it harder for the virus to grow and spread. We’re excited to expand on our research to learn more about how these viruses cause human disease and ways to combat them.”
A Surprising Discovery

Researchers in the Qi Zhang’s lab made the discovery back in 2017, when they were performing routine imaging experiments using nuclear magnetic resonance (NMR) imaging. The technology, much like an MRI that is used in humans, allows scientists to visualize shapes and motions of biological molecules, such as RNA, DNA, and proteins, in astounding atom-by-atom detail.
However, lab members were quick to realize that the Zika virus RNA was stuck in this configuration for days—approximately one million times longer than other types of RNA.
Further investigation by the Zhang and Lazear labs revealed that this frozen, stable RNA structure plays an important role in viral replication. They found that this particular configuration can effectively put up a “molecular wall” that protects the viral RNA from being degraded by the host cell, altogether enhancing the ability of the virus to make more copies of itself.
Antivirals and Preparing for Emerging Disease
After analyzing the RNA structure and its mechanisms further, researchers have gotten a better understanding of its strength and also its weakness. If researchers can determine how exactly the RNA structure maintains this strong defense, they might be able to develop new therapies that can disrupt that interaction and interfere with further replication of the virus.

Zika virus is just one of many RNA viruses, termed flaviviruses, that are spread by mosquitoes and ticks around the world, including West Nile virus which is found in North Carolina. As a result, researchers are working to develop new and effective vaccines and to learn more about these viruses before they emerge.
“While some flaviviruses are important causes of disease globally, some of these viruses don’t currently cause large outbreaks but have the potential to do so in the future,” said Lazear.
“It’s really important that we learn about these viruses and have the tools to work with them, so that we’re ready to respond to future emerging outbreaks.”
Revolutionizing How Scientists Understand RNA Molecules
In the field of biochemistry and biophysics, much of their time is spent on analyzing and detailing the shapes of molecular structures. Understanding their shape allows researchers to learn more about their ins-and-outs, such as how they bind to receptors, activate biochemical pathways, or how they function in the body.
Over the last decade, the field has taken a large leap forward with new technologies that can predict molecular structures using AI. However, the latest findings in the Zhang and Lazear labs add a whole new dimension that scientists may need to consider when understanding RNA viruses: time.
“This paper really changed the paradigm of the field,” said Zhang, who is also co-director of UNC RNA Discovery Center at the UNC Lineberger Comprehensive Cancer Center. “We need to start appreciating how long these RNA structures live. Perhaps in the future, we could use AI-based technologies that can not only predict space, but also predict lifetime.”
Zhang is the leader of a recently launched research initiative, called the RNA-targeted Innovation in Drug Exploration (RIDE), in the UNC Department of Biochemistry and Biophysics and co-director of the RNA Discovery Center. Leveraging their latest knowledge about RNA viruses, Zhang and Lazear will further explore drug targeting in RNA viruses, alongside other experts in microbiology, virology, and biochemistry at UNC-Chapel Hill.
Rhese Thompson, PhD, a recent graduate in the Zhang lab, was lead author on the paper. Other authors include Derek Carbaugh, PhD, and Joshua Nielsen in the Lazear lab, Edgar Faison and Bo Zhao, PhD, in the Zhang lab; Jeffrey Bonin, PhD; Rita Meganck, PhD, in the Marzluff lab; Nathan Nicely, PhD, associate professor of Pharmacology; William Marzluff, Kenan Distinguished Professor of Biochemistry and Biophysics at UNC-Chapel Hill; Aaron Frank, PhD, assistant professor of Chemistry and Biophysics at the University of Michigan, Ann Arbor; Ciara Witt, PhD, in the Frank lab; and Atul Rangadurai, PhD, from Duke University.
Funding for this project came from the Emerging Challenges in Biomedical Research (ECBR) pilot award program from the UNC School of Medicine’s Office of Research, the Jefferson-Pilot Award from the UNC School of Medicine, UNC – Chapel Hill, the National Institutes of Health, and the Burroughs-Wellcome Fund.
Researchers would like to acknowledge the Biomolecular NMR Laboratory, which receives funding from the National Cancer Institute of the National Institutes of Health under award number P30CA016086, for spectrometer maintenance and use.
Measles Cases Are Rising in US as Texas Outbreak Grows
A measles outbreak in Texas has grown to 48 cases, all of whom are unvaccinated.
CDC: No cases reported in NC yet.
(ABC News, Mary Kekatos) -- Measles is continuing to spread across the United States as an outbreak in Texas rapidly grows and cases are confirmed in nearby states, according to health officials.
In western Texas, a measles outbreak doubled from 24 confirmed cases on Tuesday to 48 cases on Friday, according to the Department of State Health Services (DSHS). This marks the largest measles outbreak in the state in more than 30 years, according to a DSHS spokesperson.
All of the cases are in unvaccinated individuals or individuals whose vaccination status is unknown, and 13 people have been hospitalized so far. Gaines County is the epicenter of the outbreak, with 42 cases confirmed among residents, according to DSHS.
Meanwhile, in neighboring New Mexico, three unrelated cases of measles were confirmed last week in Lea County, which borders Gaines County, according to the New Mexico Department of Health (NMDOH).
"While a connection to the Texas outbreak is suspected, it remains unconfirmed," according to a news release from the NMDOH.
The Centers for Disease Control and Prevention has separately confirmed 14 cases in five states so far this year, which does not include the recent Texas or New Mexico cases or recently confirmed cases in Georgia.
Public health experts who work in the field of infectious diseases told ABC News they're concerned about the rise in cases and that it could lead to a far bigger outbreak among those who are unvaccinated or undervaccinated.

"This current measles outbreak is very concerning when it comes to the potential for measles to become a lot more widespread," said Dr. Alok Patel, a pediatrician at Stanford Children's Health, and an ABC News contributor. "What we're seeing right now is a crack in the foundation of a building, and we do not want this building to collapse, and so the minute you see a small outbreak of measles -- especially in an un- or under-vaccinated population -- this is a textbook example of how measles can quickly spread."
"A small measles outbreak could be the start of a public health catastrophe that is completely preventable," he added.
Vaccine exemptions among children in Gaines County -- the epicenter of the Texas outbreak -- have grown dramatically in the past few years.
Read full story here.
The NC DHHS reported a confirmed case of measles in a child in Mecklenburg County in September of 2024. That was the first confirmed case in North Carolina since 2018.