CDC: Health Workers Facing Mental Health Crisis

(CNN) -- Researchers from the US Centers for Disease Control and Prevention are sounding the alarm on a mental health crisis for health workers around the country.
Using nationwide survey data between 2018 and 2022, a new report from the agency found that nearly half of health workers reported feeling burned out in 2022, up from under a third four years prior. Health workers’ reports of being harassed at work more than doubled, as well.
The report, released on Tuesday, also shows that health workers face worse mental health outcomes than employees in other industries.
The findings come on the heels of the largest health care worker strike in US history, in which 75,000 unionized employees of Kaiser Permanente cited feelings of burnout and chronic staffing shortages during a walkout in five states and the District of Columbia.
“While usually health workers care diligently for others in their time of need, it is now our nation’s health workers who are suffering, and we must act,” said Dr. Debra Houry, the CDC’s chief medical officer.
Even before the pandemic, Houry added, health workers’ jobs were demanding: Providers face long hours and unpredictable schedules, exposure to infectious diseases, and often-challenging interactions with patients and their families.
Previous research has found that health care workers — especially nurses, health support workers and health technicians — face an increased risk of suicide compared with people who don’t work in the medical field.
“Caring for people who are sick can also be intensely stressful and emotional,” Houry said. “Although you do everything you can to save a life, I still remember some of the tough patient cases I had, where I gave the bad news about an advanced cancer diagnosis to a working spouse or the time I was unable to resuscitate the young toddler after a car crash.
“After a shift like this, I would have to put on a good front and take care of my own family. And in doing this, I didn’t always pay enough attention to my own wellness needs.”
According to Houry, the Covid-19 pandemic made workplace challenges worse, with health care providers facing a wave of patients, long hours and supply shortages. Those stresses fueled a rise in mental health complications, suicidal ideation, and like large parts of the US adult population, substance abuse challenges.
The study found that health care workers reported an increase in poor mental health days between 2018 and 2022. In the survey, 44% of health workers reported wanting to look for a new job, up from 33% in 2018.
In contrast, the number of other essential workers who intended to look for a new job dropped over the same period.
Meanwhile, the number of health care workers who experienced harassment — including violent threats, bullying and verbal abuse from patients and coworkers — shot up from 6% to 13% during the study period.
According to the CDC report, harassment had major impacts on health workers’ mental health: Health workers who reported being harassed were 5 times as likely to report anxiety compared to those who were not. Those who faced harassment were over three times as likely to report depression and nearly six times as likely to report burnout, as well.
For instance, 85% of health workers who experienced harassment reported feeling anxiety, compared with 53% of those who did not. Sixty percent of harassment victims reported experiencing depression, nearly double the number of health workers who had not suffered harassment.
Those consequences, however, are preventable with improved workplace policies and practices, the report says.
The study found that health workers who trusted their management, had enough time to complete their work and received support from supervisors were less likely to report burnout.
“We’re calling on employers to take this information to heart and take immediate preventive actions,” said Casey Chosewood, director of the National Institute for Occupational Safety and Health’s Office for Total Worker
The report also recommended that employers encourage “cross-level employee participation” in decision-making: health workers who helped with decision-making had about half the likelihood of reporting depression symptoms. Chosewood recommended that supervisors support their employees by monitoring staffing needs and seriously addressing harassment reports.
The CDC’s National Institute for Occupational Safety and Health also plans to launch a national campaign this fall to help hospital leaders address challenges to health workers’ well-being — part of an ongoing initiative by the agency to raise awareness about health workers’ mental health challenges.
“The bottom line is this: We must take the research we have and act,” Chosewood said. “To label our current and long-standing challenge a ‘crisis’ is an understatement. Patients in our communities, really all of us, will fare better when our health workers are thriving.”
Health. “Supportive work environments had a positive impact on health workers.”
TO READ FULL REPORT FROM CENTERS FOR DISEASE CONTROL AND PREVENTION CLICK HERE.
NCDHHS Encouraging Mpox Vaccinations After New Cases Reported
NCDHHS Encourages Mpox Vaccination for People at Higher Risk After Recent Cases Reported

In addition to the two cases, the mpox virus was recently detected in one out of 12 wastewater sites where monitoring is being conducted. These cases and wastewater detections were all in different counties, suggesting an increased spread of mpox in North Carolina.
Numbers and cases have been low due to vaccinations and community engagement, but now is the time to get vaccinated if you are at higher risk for mpox and have not yet received the vaccine. Eligibility criteria have expanded to include:
- Anyone who has or may have multiple or anonymous sex partners;
- Anyone whose sex partners are eligible per the criteria above;
- People who know or suspect they have been exposed to mpox in the last 14 days;
- Anyone else who considers themselves to be at risk for mpox through sex or other intimate contact.
Take steps to lower your risk during sex or at social gatherings, like using a condom correctly every time you have sex. Avoid close contact with people who have a rash that looks like mpox, avoid contact with objects and materials a person with mpox has used and wash your hands often.
Read more about how the disease is spread, symptoms of mpox, and what NCDHHS is doing to enhance communication efforts with local health departments and community partners, in a news release.
NC Universities Setting New Revenue Records From Research, Tech Created by Students and Faculty
Duke University brings in record money from its startups and technology

(Axios Raleigh - Zachery Eanes) -- The Triangle's research universities are setting new revenue records from research and technology created by their students and faculty.
Driving the news: Duke University reported bringing in a massive $102.5 million in licensing and equity payments from technology and startups formed on its campus in its fiscal year 2023, which ended June 30.
- It caps an incredibly consistent run by the university, which has brought in more than $50 million via technology created on the campus for the past five years.
Why it matters: The Triangle university ecosystem — the origin of the Research Triangle moniker — has long been the economic backbone of the region, reliably attracting talent, jobs, and money to the region.
- The startups formed by their faculty and students have gone on to become some of its largest employers, including names like Quintiles, now known as IQVIA (UNC); SAS Institute and Wolfspeed (N.C. State); Precision Biosciences (Duke) and RTI International (all three universities).
State of play: The universities have, over the past decade, become much more focused on turning the intellectual property formed on their campuses into financial windfalls.
- In addition to Duke's success, UNC broke its licensing and equity record in 2021 (thanks to Bayer's $4 billion acquisition of Chapel Hill-founded gene therapy company AskBio).
- And since 2015, N.C. State has formed the most startups of any school in the area.
What's happening: Duke can attribute its success to a hot streak of drugs entering the market as well as startups filing for initial public offerings or being acquired, according to Robin Rasor, the school's associate vice president of translation and commercialization.
- In its past fiscal year, five Duke-related startups were acquired, including Durham-based Isolere Bio and InnAVasc Medical.
- The school has also seen six different IPOs in the past five years, which has provided a reliable stream of equity payments.
- Duke Capital Partners, the university's early-stage investment firm, has also become more active in supporting young startups with capital, including investing $10.8 million into 12 startups in fiscal year 2023.
What they're saying: Rasor, who has worked at universities for three decades, said there's been a big shift within schools in recent years.
- Younger faculty are more interested in forming companies, she said, and universities are providing more infrastructure for them to do so.
- "Most of the [faculty] recruits coming in are already innovators ... and they're very interested in what the [startup] environment is going to be like," Rasor told Axios. "That's a big change, and … it's important to have that kind of environment so we can recruit the best and the brightest."
What we're watching: Of the 15 startups formed at Duke in the past year, 66% are headquartered in North Carolina.
- That's a decline from previous years, according to Rasor, who said remote work trends may be leading to more of the university's startups to relocate — even as more Duke students seem to be staying in the area after graduation.
- She said the Triangle's critical mass of talent continues to improve but many startups still weigh whether Boston or the Bay Area might be a better fit.
Register Here for Addiction Medicine Learning Series Webinars
Starting January 2023, all DEA-registered practitioners are required to participate in 8 hours of training in addiction medicine. This Addiction Medicine Series meets the requirements set forth by the DEA and provides participants a broad overview on addiction treatment. This series provides education on a variety of key topics in addiction medicine, including inequities in addiction, impacts of stigma, basics about addiction treatment, integrating addiction treatment in the primary care setting, and treatment of substance use in special populations including the adolescent population, those with mental illness and those with chronic pain.
The registration links for all 8 models are included below:
The End of a Bygone Era: Removal of the X-waiver Next Steps in Buprenorphine Prescribing
Addiction In Primary Care
Responding to Pediatric Substance Use
Treating Chronic Pain and Addictions
Understanding the Impacts of Stigma: Substance Use Disorder
Addiction and Mental Illness
The Impact of Stigma and Bias on Substance Use Disorder Diagnosis and Treatment
Current State of MOUD Access
Additional Resources Related to These Topics
Duke's first Nobel Prize Winner, Robert Lefkowitz, Celebrates 50 Years!
Nobel Laureates Highlight Symposium Celebrating Robert J. Lefkowitz’s 50 Years at Duke
(Durham, Duke Med School - Dave Hart) -- After completing a residency and fellowship at Harvard and Massachusetts General Hospital, Robert J. Lefkowitz, MD, arrived at Duke University School of Medicine to begin his first faculty job in the summer of 1973. 
He’s been here ever since — conducting pioneering research that has changed the landscape of medicine, mentoring more than 200 trainees, and becoming Duke University’s first Nobel Prize winner, when he was awarded the 2012 prize in chemistry.
On Oct. 2-3, the School of Medicine hosted a remarkable gathering of luminaries (including seven Nobel Laureates, two former chancellors, and a five-time NCAA championship men’s basketball coach) for a symposium to celebrate Lefkowitz’s 50 years at Duke and the discoveries that advance human health.
Duke University Executive Vice President for Health Affairs and School of Medicine Dean Mary E. Klotman, MD, welcomed the large audience in Page Auditorium. She noted that Lefkowitz’s rise as a pioneering biomedical scientist and Duke’s rise as a world-class biomedical institution went hand in hand. Duke provided Lefkowitz with the resources, intellectual freedom, and trainees and colleagues to pursue his groundbreaking research. In turn, his excellence, mentorship, and championing of basic science have attracted other top scientists and elevated Duke’s research environment.

“Duke wouldn’t be the same if not for Bob, and Bob wouldn’t be the same if not for Duke,” she told the large audience. “We are here to celebrate the golden anniversary of a remarkable relationship.”
The event featured lectures by some of the world’s leading researchers, reminiscences from some of Lefkowitz’s closest friends and colleagues, and words of wisdom for students, trainees, and junior faculty about how to achieve and sustain success, in science and in life.
Participants included Nobel Prize Laureates Peter Agre, MD; Michael S. Brown, MD; Joseph Goldstein, MD; Roderick MacKinnon, MD; Stanley Prusiner, MD; Harold E. Varmus, MD; and Brian Kobilka, MD, who was a postdoctoral fellow in Lefkowitz’s lab and shared the 2012 Nobel Prize.
Also taking the stage were leading scientists including Helen H. Hobbs, MD; Gary H. Gibbons, MD; Irving L. Weissman, MD; and Stuart H. Orkin, MD, as well as a host of Duke leaders past and present. Lefkowitz and Klotman joined Duke University President Vincent E. Price, PhD, and former Duke men’s basketball coach Mike Krzyzewski for a lively panel discussion on “Sustaining Success in the Spotlight.”
Chancellor Emeritus for Health Affairs Victor J. Dzau, MD, recalled “how exciting it was to be here as chancellor and bathe in his glory” when Lefkowitz won the 2012 Nobel Prize for his pioneering research on G-protein coupled receptors, which provided the targets for more than one-third of all current prescription drugs.
“For fifty years Bob has been an icon, a role model, and a scientist whose contributions have changed and saved so many lives,” said Dzau, now president of the National Academies of Sciences, Engineering, and Medicine.
Agre, who won the 2003 Nobel Prize in Chemistry and was vice chancellor for science and technology at Duke from 2005-2008, presented his recent research on malaria in sub-Saharan Africa. He also recalled the moment that all Nobel Laureates remember: that life-changing phone call from Sweden. “It’s a very pleasant experience,” he admitted.
Goldstein, who won the 1985 Nobel Prize in Physiology or Medicine, first met Lefkowitz in 1968 when they were in the same cohort of “Yellow Berets” — young physicians commissioned into the National Institutes of Health and the Public Health Service during the Vietnam War. He urged young researchers to approach science with a sense of adventure.
“Have the courage to take risks,” he said. “Try new approaches and avoid bandwagon research. If scientists don’t take risks, science will stagnate.”
Varmus, who won the Nobel Prize in Physiology or Medicine in 1989, was a medical school classmate of Lefkowitz’s at Columbia and also a fellow Yellow Beret.
“The scientific life has changed in many ways, but discovery remains a joy,” Varmus said. “The path to a career is longer and harder, but there are more branches to choose from. The demography of science has become more diverse, but we still have a long way to go. Basic and applied science have moved closer together, but the demand for application threatens broad inquiry. One thing remains the same: friendships are essential for a fulfilling life in science.”
One of Lefkowitz’s closest friends, Duke Chancellor Emeritus for Health Affairs Ralph Snyderman, MD, joined the faculty in 1972, just before Lefkowitz did. The two soon took up the habit of running together — an activity they continued, five or six days a week, for some 30 years.
“We once calculated that we ran over 50,000 miles together,” Snyderman said. “We were like brothers without the sibling rivalry. What I think differentiates Bob as a scientist is the courage to do the really hard experiments and the persistence to stick with it. He has incredibly high standards. He’s totally focused, and he is totally committed to the people who work with him.”
Lefkowitz himself spoke passionately about the need for young scientists to find the right mentor. For many of them over the past 50 years, that mentor has been Lefkowitz: many of his trainees have achieved great prominence and won major awards, including the Nobel Prize. He succeeds, he said, when they succeed.
“I’ve never led anything bigger than my lab,” he said. “But I’ve tried very hard to help my trainees use their powers to maximum effect. Training in science is an apprenticeship. It’s experiential. It requires you to pour yourself completely into your goal.”
Lefkowitz, who turned 80 in April, was moved by the large contingent of alumni from his lab who returned to Duke to reconnect and share in the celebration.
“What an incredible few days we just shared,” he said. “I want to thank everybody who took the time to join in, and especially those who came from long distances to help me celebrate these two very special landmarks in my life. Never have the words been truer than when I say, ‘I couldn't have done it without you.’”
Duke School of Medicine Makes Surprise Discovery That Could Change MS Treatments
Surprise Discovery Reveals Key Factor in Multiple Sclerosis

(Duke Med School - Shantell M. Kirkendoll) -- Researchers at Duke University School of Medicine studying multiple sclerosis made an unexpected discovery that could reshape the understanding of MS treatments.
They identified a protein that boosts the aggressive migration of immune cells into the central nervous system which leads to MS, an autoimmune disease affecting about 1 million adults in the United States. The intrusion of a specific type of immune cell called Th17 is particularly harmful to the brain and spinal cord.
But when Duke scientists blocked the protein integrin α3, slowing Th17 cells from reaching and damaging the central nervous system, they saw major improvement in mice, according to a study published Oct. 13 in Science Immunology.
“We were studying the role of another gene when we stumbled upon integrin α3,” said co-lead author Maria Ciofani, PhD, associate professor in the Department of Integrative Immunobiology at Duke School of Medicine. “We found that when it’s missing, the Th17 cells don’t develop as effectively, and more importantly, they face difficulties entering the central nervous system. This means less damage.”
The Th17 cells, which are vital for the body to fight fungal and bacterial infections, don’t usually cause diseases. But for people with MS, these cells are mistakenly activated and end up attacking the central nervous system.
The Duke team is the first to reveal the selective abundance of integrin α3 on Th17 cells. The protein helps Th17 cells to form connections with other cells, which in turn helps the cells grow and become more aggressive.
But in the absence of the protein, Th17 cells get locked outside the blood-brain barrier, the brain’s protective shield.
While probing inflammatory T cells and disabling a particular gene—a routine practice to grasp its function—researchers stumbled upon a surprise. The altered mice were fully shielded from the MS-like symptoms typically seen in such models.
“They were walking around like nothing happened,” Ciofani said. “When we looked carefully, we found that none of the Th17 cells were entering the central nervous system. It was an opportunity to look at the machinery that controls these cells.”
With the help of computational approaches, Ciofani's team, including co-lead study author Eunchong Park, PhD, identified integrin α3. Park, a scientist at AstraZeneca, is a former graduate student in the Department of Integrative Immunology and member of the Center for Advanced Genomic Technologies.
There’s currently no MS drug that targets integrins on Th17 cells, but the drug natalizumab does target another kind of T cell, Th1 cells, that can also contribute to MS. But natalizumab has its side effects, emphasizing the need for alternative treatments.
“One concern about targeting integrin α3 is that these Th17 cells are vital for our body’s defense against infections,” Ciofani said. “We’ve done preliminary tests to see if inhibiting integrin α3 stops Th17 cells from performing their protective roles, and so far, it seems they can still do their jobs.”
Since integrin α3 is so essential for the harmful actions of Th17 cells, it could be a potential target for new MS treatments.
If scientists could develop a drug that blocks or reduces the function of this protein, it might reduce the severity of MS or prevent its onset.
Additional Duke authors include William E. Barclay; Alejandro Barrera; Tzu-Chieh Liao, Harmony R. Salzler; Timothy E. Reddy; and Mari L. Shinohara.
Funding was provided by National Institute of Health grants R01-GM115474; R01-AI156186; R01-NS120417; RG-4536B2/1; and UM1-HG009428 and a Kwanjeong Educational Foundation Scholarship.
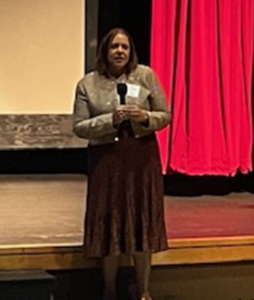
2023 LEAD Recap: State Health Director Gives Annual Report to NCMS
 The 2023 LEAD Conference featured several panels and speakers over two days and a highlight was the annual report from the Department of Health and Human Services. On Saturday, Elizabeth Cuervo Tilson, MD, MPH, State Health Director and Chief Medical Officer offered the annual report to the NCMS. Here are some highlights of her report:
The 2023 LEAD Conference featured several panels and speakers over two days and a highlight was the annual report from the Department of Health and Human Services. On Saturday, Elizabeth Cuervo Tilson, MD, MPH, State Health Director and Chief Medical Officer offered the annual report to the NCMS. Here are some highlights of her report:
EXECUTIVE SUMMARY
As the world continues to recover from one of the largest public health threats in recent history, this past year in North Carolina heralded a transition from COVID-19-specific recovery efforts to broader initiatives aimed at safeguarding and bolstering the overall health of North Carolinians. We leveraged the invaluable lessons learned and the partnerships fortified throughout the pandemic to continue to improve our responses to health challenges. Systems that have been chronically underfunded were further strained by the stressors of the pandemic, mandating thoughtful strategic investment in those systems. We have prioritized activities to advance whole person health and created roadmaps for strategic investment in the health of our people. This annual report outlines our national, state level, and agency strategic priorities and programming to further our commitment to health and opportunity for every North Carolinian.
America’s Health Rankings serves as an annual report for states built upon the World Health Organization’s definition of health. North Carolina’s overall health ranking relative to other U.S. states has consistently improved annually, evidencing our public health successes. In the 2022 Annual Report, North Carolina was ranked 30, up from 34 and 41 in the prior two years, respectively. As in years past, many health indicators on which North Carolina needs to improve are driven in part by North Carolina’s large uninsured population.
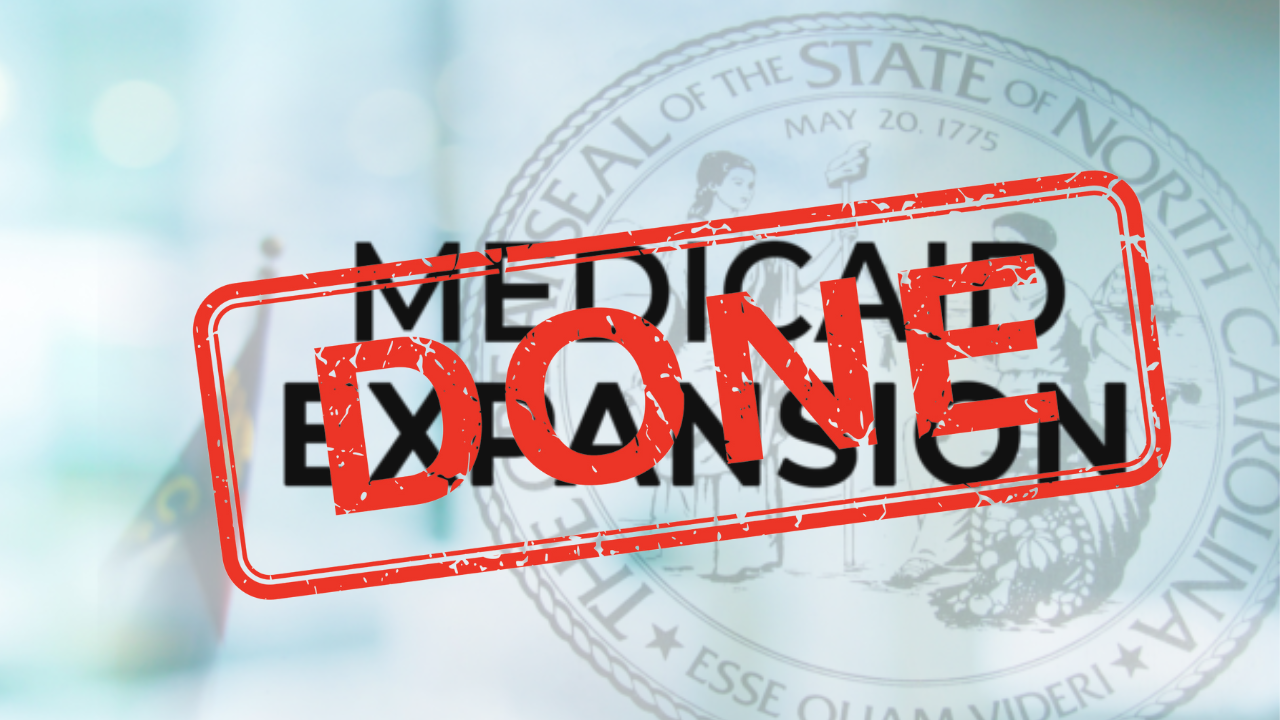
Medicaid expansion was signed into law by Governor Roy Cooper in March 2023 and represents a critical step forward to improve the health of North Carolinians and enable a substantial economic investment in the state. Operationalization of Medicaid expansion will be an integral step to improve health in North Carolina. The North Carolina Department of Health and Human Services was given final authority to implement Medicaid expansion through enactment of the state budget in early October, allowing for a launch date of December 1, 2023. We have a new website, bilingual toolkit and a sign-up form to stay updated on the most current information and share with your partners, patients, and stakeholders.
Healthy North Carolina 2030, released in 2020, lays out 21 ambitious, population-level goals and shared objectives for the entire state to solve “wicked problems” and improve the health of North Carolinians for this decade. It aims to mobilize and coordinate a broad array of private sector, public sector, and community organizations that can play a role in making North Carolinians healthier. The North Carolina State Health Improvement Plan (NC SHIP) builds upon HNC 2030 to help create a unified strategy across multiple stakeholders to drive improvement in the indicators throughout the decade covered by HNC 2030. The NC SHIP documents are iterative, describe the process for improvement, and report on progress of any improvements. 2023 NCSHIP lays out the efforts of statewide cross-sector collaboration and launches a Year of Action.
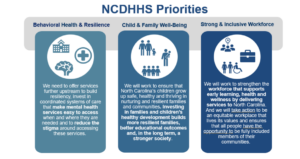
NCDHHS works toward five strategic priorities, guided by our strategic plan. Three priorities are areas of activity that bring together multiple divisions and external partners. They are Behavioral Health and Resilience, Child and Family Well-being, and a Strong and Inclusive Workforce. Two priorities are fundamental ways that we approach our work across the department. Our Health Equity Portfolio synthesizes and guides efforts across NCDHHS and beyond to erase gaps in whole-person health. Our Data Office works the numbers to tell us how we are doing.
As we move out of the COVID pandemic, we have the tools needed to manage COVID-19 like we do other respiratory illnesses, including access to vaccines, testing, and treatment. In addition, we have expanded our focus to other respiratory diseases including Influenza and Respiratory Syncytial Virus and communicable diseases, including Mpox, syphilis and HIV for which there are disparities in rates of infections within our population
Our Public Health Infrastructure has been chronically underfunded and the COVID-19 pandemic brought mainstream attention to public health across the globe and highlighted the challenges of this underfunded patchwork of public health infrastructure to respond to the crisis. These challenges and recommendations to response have been identified by the North Carolina Institute of Medicine's Task Force on the Future of Local Public Health in NC. This report highlights work to strengthen public health foundational capabilities, infrastructure, and workforce to be able to respond to future threats more readily. Finally, this report also serves as the Annual Report on the North Carolina Division of Public Health Strategic Plan as required by Public Health Accreditation Board, and highlights work being done to meet DPH Strategic Priorities.
The full report is available here.
Join NCMS for 2024 National Advocacy Conference in Washington

October 16, 2023
Join us on Capitol Hill
The AMA’s National Advocacy Conference is scheduled for February 12-14, 2024. This yearly event offers an opportunity for personal involvement in the health policy debate on Capitol Hill. We need increased NCMS member engagement with our members of Congress, so mark your calendar and stay tuned for forthcoming details.

2024 National Advocacy Conference
Save the date and join us for our return to Capitol Hill.
February 12-14, 2024
Grand Hyatt / Washington, DC
Plan now to join your colleagues as we advocate for
patients and the medical profession on . . .
Prior Authorization Relief
Medicare Payment Reform
Step Therapy Reform
Workforce Shortage Solutions
Physician Wellness
Registration and additional information coming soon.
https://www.ama-assn.org/about/events/national-advocacy-conference
2023 LEAD Conference and Gala is Another Success!

RALEIGH -- The 2023 LEAD Healthcare Conference and Golden Stethoscope Awards Gala has concluded! Over the course of two days, attendees, including members of the North Carolina Medical Society, guests, speakers, and exhibitors, gathered at the Sheraton Imperial Hotel in RTP for engaging discussions, camaraderie, and educational sessions. The agenda encompassed a range of vital subjects, such as women's reproductive health and Black maternal well-being, trending topics for young physicians and physician assistants, clinician well-being, and the latest developments in the healthcare field.
On Friday morning, the event commenced with a keynote address from Dr. Amy Bryant, who delved into the topic of women's reproductive health. This was followed by the screening of the Aftershock video and a panel discussion centered on Black maternal health, skillfully moderated by Dr. Karen L. Smith. Joining her on stage were Belinda Pettiford, MPH, and Maria Small, MD, MPH, contributing to the insightful dialogue.
Throughout the day, attendees had the opportunity to engage in networking sessions with peers and gain valuable insights from a diverse array of exhibitors who offered comprehensive support to meet the needs of physicians. The exhibitors included financial advisors, workforce support providers, technology consultants, and a myriad of experts prepared to address the challenges and opportunities within the future of healthcare in North Carolina.
On the first day, there was a panel discussion titled 'Voice of the Young Physician and Physician Assistant,' skillfully moderated by Shawn Scott from NCMS. The panel featured Hans Arora, MD, Jasmine Hemmings, PA-C, Joshua Penninger, PA-C, and Sherry Wang, MD, offering valuable insights. Additionally, attendees enjoyed a lunch session and a Sponsor Showcase discussion on Asthma Care presented by Sanofi-Regeneron. There was also an informative advocacy class led by Seth Palmer, along with the annual CPP Meeting. Throughout the day, the NCMS Board of Directors, Board of Trustees, CCH, and CCHN conducted extensive meetings, culminating in the announcement of new board members on Saturday.
Friday afternoon was brimming with enlightening MedTalks featuring Leadership College Scholars, including Julia Wulforst, PA-C, Jennifer Kipp, DPM, Carla Holder, MD, Susie Fitzgerald, DO, Christine Khandelwal, DO, Michalina Kupsik, MD, Katie Lowry, MD, Jacqueline Njapa, MD, and Dana Point, MD. The MedTalks were followed by a meeting of the Opioid Task Force.
The day reached its climax with a joyous celebration of the Kanof Institute for Professional Leadership. The evening featured a cocktail reception, including a warm Welcome Reception and the formal presentation of graduation certificates to the 2023 KIPL class. The gathering was a moment to reflect on and commemorate the 20-year legacy of Leadership College.
Saturday began with the NCMS PAC Advocacy Breakfast, featuring a presentation by CEO Chip Baggett, who offered insights into the changing landscape of political division in the United States and strategies for advancing both the nation and the NCMS. Attendees enjoyed breakfast while several prizes and raffle items were distributed, and further interactions with exhibitors took place.
Following this, Elizabeth C. Tilson, MD, MPH, the State Health Director and the Chief Medical Officer for the Department of Health and Human Services and Ronald B. May, MD, delivered a presentation on the Public Health Commission.
The morning continued with an chance to see posters created by residents, fellows, and medical students from across the state, along with a final opportunity to engage with exhibitors. After that, NCMS President Dr. Arthur Apolinario participated in a panel discussion alongside NCMS Board members Andrew Lamb, MD, and Claude Jarrett, MD, FAAOS, focusing on the topic of 'When the Physician is the Patient.' The discussion was expertly moderated by NCMS' Dr. Kristina Natt och Dag. The NCMS Annual Meeting was also held Saturday afternoon.
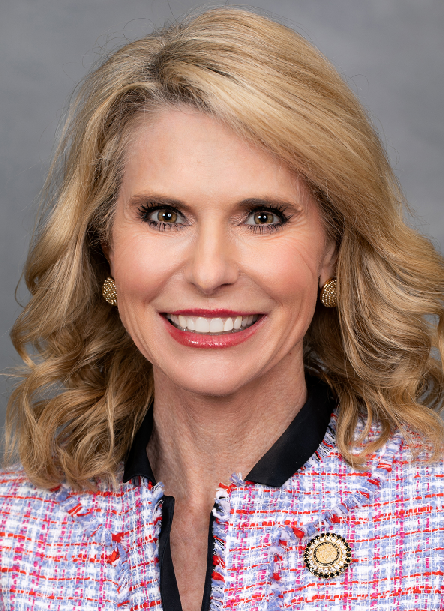
Saturday night marked the moment when the festivities shifted into high gear at the 2023 Golden Stethoscope Awards Gala! The event was kicked off by NCMS' Randy Aldridge and Chip Baggett, who extended a warm welcome to past, present, and future NCMS presidents on the stage. A touching farewell was delivered by Past President Dr. Michael Utecht to President Dr. Arthur Apolinario, who presented him with the presidential pin. Dr. Apolinario, affectionately known as "Dr. Art," then directed his attention to incoming president, Dr. Eileen Raynor, MD, FACS, FAAP. He administered the oath of office and bestowed upon her the President's Medallion. Dr. Raynor then addressed the gathering with her inaugural speech as NCMS president.
Several awards were given including the Golden Stethoscope Awards. They went to:
- Dr. Karen Harum from Region 1
- Dr. Holly Biola from Region 2
- Dr. Joseph Bell from Region 3
- Dr. Alan Story from Region 4
The 2023 T. Reginal Harris Award was given to Dr. Jeffrey Kuremsky
The 2023 John Huske Anderson Award went to Brooks Bell
The 2023 E. Harvey Estes, Jr. Physician Community Service Award went to Dr. Peter Morris.
All of that was followed by a presentation on 20 years of NCMS Leadership College by Kristina Natt och Dag.
The evening wrapped up with comments from CEO Chip Baggett and dancing! All-in-all, it was another wonderful annual conference for the North Carolina Medical Society.
NCMGMA Salary and Benefits Survey Now Open
NCMGMA Salary and Benefits Survey is Open
EASIER Data Collection is Here!
Complete your survey by November 22nd
This comprehensive study is designed to bring our members the information they need to see trends specific to the healthcare industry, and provide comparative information your organization can use to assist in making crucial business decisions.
NEW! If you participated last year, you can copy last year's data into this year's survey, effectively reducing the time it takes to complete the survey! New positions have also been added this year, including a traveling nurse position.
Data collection is now open through Wednesday, November 22nd.
Complete 75% to gain access to complimentary reporting!
Access to the Site:
- Link: https://benchmark.ncmgmasalarysurvey.com/
- Enter your Username & Password to begin entering in data:
- If you've forgotten your password, please use the prompt on the page to assist.
New User? Click here to get started
Survey Information:
- Once logged in, check out the Support Page to find the:
- Survey Positions listing: sort by Category, Department or Position.
- Survey Worksheet, a downloadable spreadsheet used to help compile data to get you started prior to entering in data.
- User Guide, which will help answer many of your how-to questions. It can also be found on the Support page in the survey, once logged in.
- The Survey is divided into sections that contain categories of questions. You can begin in any section and complete the survey questions in any order.
- The progress bar on the home page will track your overall progress and the icons will help you see any areas not completed.
- Come back as often as needed to complete the survey. All data is saved as you go.
In order to access results when they are released (December), participants must complete all required questions and a minimum 75% of the survey
Questions:
If you have any questions about the 2023 Salary & Benefits Survey, please contact the NCMGMA offices at [email protected]
NCMS Member, Representative Dr. Kristin Baker Not Running for Re-Election
NCMS Member, Representative Dr. Kristin Baker Decides Against Another Term

2023 SHD Report, CPH Agenda Released for October 14 Meeting

State Health Director Elizabeth Cuervo Tilson, MD, MPH, has announced the CPH agenda and State Health Director Annual Report for the October 14 meeting in Durham.
COMMISSION FOR PUBLIC HEALTH
Commission Conjoint Meeting with the NC Medical Society
October 14, 2023
9:00 a.m.
Sheraton Imperial Hotel Raleigh-Durham Airport at RTP
Room: Imperial 1234
4700 Emperor Boulevard
Durham, NC 27703
I-140 at Exit 282
AGENDA
A. Call to Order Dr. Ron May
B. Invocation
C. Ethics - Conflict of Interest Statement
1. State Health Director’s Annual Report Dr. Betsey Tilson
2. New Business
3. Adjournment
Zoom
Link: https://us06web.zoom.us/j/89924373359
Meeting ID: 899 2437 3359
Passcode: LEAD2023
Phone: +13052241968,,89924373359#
View the Annual Report here: State Health Director Annual Report 2023 FINAL
Get Ready for December! NCDHHS Releases Medicaid Expansion Toolkit

RALEIGH -- The North Carolina Department of Health and Human Services has released a Tool Kit for the long-awaited expansion of Medicaid in the state. The bilingual kit includes all you need to know to spread the word to your patients and answers some frequently asked questions.
The kit includes:
- Day 1 Flyer: An overview of who is eligible and how to enroll.
- Newsletter Template: Content to include in your newsletters and emails.
- Social Media: Graphics and posts to share on your channels.
- Family Planning Flyer: Information for the approximately 300,000 people who receive limited benefits through Family Planning Medicaid who will be automatically enrolled in full Medicaid.
- Medicaid Essentials Deck: A presentation to share with your community on who is eligible and how to enroll.
- FAQ: Answers to common questions.
- ePass Video: An overview of how to apply online through ePass.
A complete look at all the information from NCDHHS can be found here.
To stay updated with the latest information, be notified when the application process goes live, and receive the newest resources, complete this sign-up form.
On the Lighter Side - October 6, 2023 - Jazz, 9 to 5, Football, Plus Lots and Lots of Seafood!
Here are some things NCMS employees, members, and YOU are talking about this Weekend and Beyond!
Fall football is in full swing!

Tonight
- Cornell at Harvard, 7pm (ESPNU)
Saturday
- Maryland at Ohio State, noon (Fox)
- Marshall at NC State, 2pm (CW Network)
- Virginia Tech at Florida, 3:30pm
- Syracuse at UNC, 3:30pm
- Wake Forest at Clemson, 3:30pm (ACC Network)
Don't duck out on the Duck Jazz Festival!

On the Outer Banks, Columbus Day weekend has become synonymous with the lively sounds of jazz. Plenty of music and fun in Duck! More information is here.
Stumble out of bed for 9 to 5 in High Point

Set in the male-dominated 1980’s workplace, audiences will be rooting for Violet, Doralee, and Judy as they face off against their sexist, egotistical, oppressive boss. Witty dialogue, powerful songs, and hilarious scenes make 9 to 5 an instant classic. Music from Grammy Award winner Dolly Parton shines bright, and will have you humming along and dancing in your seats. Tickets are still available here.
You won't go hungry in Morehead City this weekend!

The North Carolina Seafood Festival is among the most popular free festivals in the state. It takes place on the first weekend of October in Morehead City, attracting more than 200,000 attendees. All you need to know is here.
If you have an event you would like added to On The Lighter Side, email Randy Aldridge at [email protected].
On the Lighter Side - September 29, 2023 - Fall Festivals, Disney, Tim Allen, Plus Lots and Lots of College Football!
Here are some things NCMS employees, members, and YOU are talking about this Weekend and Beyond!
Temps may be cooling down, but entertainment is heating up! Here is a list of festivals this weekend:

- 2023 Lumbee Pow Wow, Maxton
- IBMA Bluegrass Live, Raleigh
- Carolina Indie Fest, Sanford
- North Carolina Muscadine Festival, Kenansville
- NC Bourbon and Spirits Festival, Weldon
- Blue Ridge Pride Fest, Asheville
- Mountain Makers Craft Festival, Waynesville
Disney on Ice skates into Charlotte!

Experience the magic and enchantment as Disney On Ice returns to Bojangles Coliseum! . Get ready to be captivated by stunning ice skating, dazzling costumes, and breathtaking choreography that will transport you to a realm where dreams come true. Times and tickets are here.
See comedy legend Tim Allen tonight!
Get ready for a night of laughter and entertainment as a Tim Allen takes the stage in Charlotte! Don't miss your chance to witness this comedy icon live in action. Secure your tickets now for an unforgettable evening of laughter at Ovens Auditorium! More info is here.
And don't forget about football!

Tonight
- Louisville at NC State, 7pm (ESPN)
Saturday
- Florida at Kentucky, noon (ESPN)
- Texas A&M at Arkansas, noon (SEC ESPN Network)
- Clemson at Syracuse, noon (ABC)
- Virginia at Boston College, 2pm (CW Network)
- Georgia at Auburn, 3:30pm (CBS)
- Michigan at Nebraska, 3:30pm (Fox)
- Indiana at Maryland, 3:30pm (BTN)
- Notre Dame at Duke, 7:30pm (ABC)
- South Carolina at Tennessee, 7:30pm (SEC ESPN Network)
- Appalachian State at UL Monroe, 8pm (ESPN+)
- Alabama at Mississippi State, 9pm (ESPN)
If you have an event you would like added to On The Lighter Side, email Randy Aldridge at [email protected].
Medicaid Expansion Will Go Live Friday, December 1, 2023! NCMS CEO and Board President Respond
Medicaid expansion will finally become available to 600,000 working North Carolinians on Friday, December 1, 2023.
The move comes after the North Carolina House and Senate completed votes on the conference report Friday and sent the state budget to Governor Roy Cooper. The new budget contains funding authorization for Medicaid Expansion as well as a number of other priorities for the North Carolina Medical Society. Cooper can sign the law, veto it, or allow it to become law in 10 days without his signature. Cooper has chosen to let the budget become law without his signature because of elements not related to Medicaid expansion.
NCMS CEO Chip Baggett says of the monumental announcement, "This marks the completion of thirteen years of work by NCMS and countless other groups to secure access to medical coverage for 600,000 working North Carolinians. That alone makes it worth every bit of blood, sweat, and tears that went into this legislative effort. I am very proud of the efforts that NCMS, and countless other groups have made toward realizing this dream!"
NCMS Board of Directors President, Dr. Arthur Apolinario recorded this message:
https://www.youtube.com/watch?v=Tptu8ovRzW4
The North Carolina Medical Society has been actively involved in securing Medicaid expansion for over a decade. Here are some key articles:
"Someone Else's Shoes" Premieres! NCMS Member Produces Film on Founding of St. Agnes Hospital
NCMS Member Produces Documentary on
Trailblazers at St. Agnes Hospital
"Today’s doctors of color stand on the shoulders of giants like Bishop Henry Beard Delany, who saved one of the largest hospitals for Blacks on the East Coast in the early 1900s, Dr. Paul McGill, the first Black orthodontist in Charlotte, Dr. Kenneth Chambers, one of the first board-certified Obstetrician-Gynecologists in Charlotte, and Dr. Brenda Armstrong who is one of the first black students at Duke Medical School." -- Dr. Cheryl Walker-McGill.
These remarkable narratives, along with many others, come to life in "Someone Else's Shoes," a documentary crafted by Cheryl Walker-McGill, MD, a member of the North Carolina Medical Society. The documentary premiered on Friday, September 23, at the Seby B. Jones Auditorium at St. Augustine’s University. It sheds light on the enduring legacy of St. Agnes Hospital and the trailblazing African Americans who tirelessly worked to enhance healthcare accessibility in North Carolina.
The film delves into the founding of St. Agnes Hospital in Raleigh in 1896, marking one of the state's pioneering Black-owned and operated hospitals. In just a single generation following the emancipation of people from slavery on local plantations, this hospital emerged as the gold standard for medical care accessible to African Americans across the region spanning from Washington D.C. to Atlanta, Georgia. The chapter of St. Agnes Hospital came to a close in 1961 with the inauguration of Wake Memorial Hospital, now known as Wake Med.
Subsequent to the film premiere, Chip Baggett, CEO of the North Carolina Medical Society, participated in a panel discussion concerning the ongoing struggle for equitable healthcare access. He emphasized the historical significance of these discussions, drawing parallels between St. Agnes Hospital's transformative role in the 19th and 20th centuries and its potential to once again serve as a cornerstone for meeting the healthcare needs of the community and nurturing the next generation of healthcare professionals in the 21st century. "Tonight is very special to me," Baggett said, "it is an honor to bring together the past and the future to build a stronger North Carolina."
Other panelists included Linda Dallas, a professor at St. Augustine University; Dr. Brian Shackleford, President of the Old North State Medical Society; and Scot McCray, CEO of Advance Community Health Center. The discussion encompassed topics such as workforce-related challenges, the pursuit of equity objectives outlined in Health North Carolina 2030, and the paramount importance of preserving the legacy of St. Agnes Hospital and its visionary founders.
The premiere event generated significant enthusiasm for the future prospects of the St. Agnes Hospital site. Grants earmarked for a feasibility study have already bolstered initiatives aimed at preserving the site and constructing a health education facility at St. Augustine’s University focused on addressing social drivers of health as well as health equity. The NCMS looks forward to continuing to partner with St. Augustine's University in this endeavor.





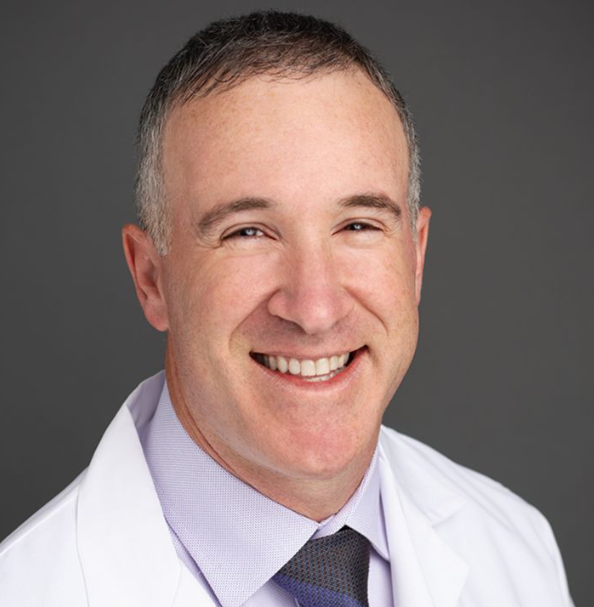
NCMS Member Dr. Seth Bleier Testifies before House Ways and Means Committee, Full Testimony Included
NCMS Member Dr. Seth Bleier testifies before House Ways and Means Committee
Will be on panel about implementation of No Surprises Act
The North Carolina Medical Society is happy to announce that our member Dr. Seth Bleier of Wake Emergency Physicians, has been invited by the Ways and Means Committee of the US House of Representatives to testify on a panel about the implementation of the No Surprises Act. The meeting is on Tuesday, September 19th at 10 am.
The NCMS supports protecting patients from unanticipated bills due to non-network medical services and is working to improve the federal rules governing the process for negotiating payment disputes between physicians and health insurers.
Dr. Bleier is testifying through coordination with the American College of Emergency Physicians. Great strides have been made toward gaining relief from surprise medical bills. The NCMS continues to collaborate with state and federal partner organizations to support litigation challenging portions of the rules that unfairly disadvantage physicians.
The North Carolina Medical Society supports the following actions to protect patients:
- Discontinue attempts to fix surprise bills on a case-by-case basis through any post-service reconciliation process for insured patients.
- Require robust network adequacy standards and up-front arbitration of contracts between physicians/providers and insurers before services are rendered to prevent non-network medical bills for insured patients.
- Maintain the existing shared principles of holding the patient harmless, providing fair compensation for medical services, and protecting access to care for patients.
- Study ways to address similar concerns for the uninsured.
The following is the Testimony of Seth Bleier, MD:
Testimony of Seth Bleier, MD, FACEP
Vice President of Finance, Wake Emergency Physicians, PA (WEPPA)
House Committee on Ways and Means
Hearing on “Reduced Care for Patients: Fallout from Flawed Implementation of Surprise Medical Billing Protections”
September 19, 2023
Chairman Smith, Ranking Member Neal, and members of the Committee, thank you for the opportunity to testify during today’s hearing, entitled “Reduced Care for Patients: Fallout from Flawed Implementation of Surprise Medical Billing Protections.”
My name is Seth Bleier, MD, FACEP, and I am a board-certified emergency physician from Raleigh, North Carolina. I currently serve as the Vice President of Finance for Wake Emergency Physicians, PA (WEPPA), I am also a member and fellow of the American College of Emergency Physicians (ACEP) which represents nearly 40,000 members, and a member of the North Carolina College of Emergency Physicians. On behalf of our practice and the emergency medicine specialty as a whole, we appreciate the Committee's ongoing commitment to ensuring the No Surprises Act is implemented fairly and according to congressional intent.
Wake Emergency Physicians, PA is an emergency medicine practice serving central North Carolina. Since our founding in 1992, we have always been physician-owned, and have never had any corporate or private equity backing or interests. Every owner regularly works in our emergency departments. WEPPA currently employs more than 200 dedicated emergency medicine specialists, comprised of about 120 residency trained, board certified emergency physicians and 95 advanced practice providers. We serve in 11 different emergency departments across four different hospital systems in the region. Four of those emergency departments are located in rural communities. Our providers care for more than 450,000 patients every year. Our goal is and has always been to be in-network with every payer, and until the first regulations for the NSA were issued, we were in-network with all four major insurance carriers in our region of the state.
To be clear, the No Surprises Act is a critical bipartisan accomplishment that removes patients from the middle of billing disputes between physicians and insurers, and we strongly supported this goal. In an emergency where seconds and minutes are often a matter of life or death, patients should never have to think about their insurance coverage or whether they will receive a bill they did not expect.
Beyond these important patient protections, the law established an equitable solution to resolve billing disagreements - at least in intent. Unfortunately, the implementation of the law to date has proven to be exceptionally challenging for smaller practices like ours. While we have so far been able to weather some of the impacts, if these challenges are not resolved, we are deeply concerned that practice models like ours may not be viable in the near future, and access to lifesaving emergency care may be severely affected, especially for rural and underserved patients.
As noted above, WEPPA had historically been in-network with all major carriers in our region of North Carolina. Most of those contracts had been in place for at least a decade without any changes or updates. Not only did our reimbursement rates not increase, they have actually significantly decreased due to factors such as inflation not being included in the contracts, as well as an increased patient burden due to high deductibles without the ability to pay.
In November 2021, WEPPA and many other physician groups in the state received letters from one of these insurers demanding significant cuts to our contract rates. The letters explicitly cited the Interim Final Rule on the NSA as justification for the reduction, and stated that if we did not agree to these new payment terms, our contract would be terminated. Thankfully this did not come to pass, but we have since had two other payers unilaterally terminate a long-standing contract. These insurers are now paying at rates that are up to 70 percent less than our previous contracts for what are now out of network services. These actions have pushed about 9 to 10 percent of our total patients out of network.
Our practice is a critical safety net for a substantial portion of our patients and for our communities. Approximately 44 percent of our patients are either uninsured or covered by Medicaid, which pays far less than the cost of care. 26 percent of our patients are covered by Medicare or TRICARE, and the remaining 30 percent are covered by commercial insurance. While these newly out-of-network patients only represent about 9 to 10 percent of our total patient population, it represents about one-third of our total commercial population and is a significant reduction in our practice’s reimbursements.
Adding to this burden is the fact that the IDR process has been virtually inaccessible for small practices once we are out of network. Many smaller practices have been advised by their billing contractors to avoid going through IDR altogether as the costs outweigh any benefit. Most emergency department provider bills are less than $1,000. We cannot afford to challenge every underpayment when just the non-refundable portion of the arbitration fee is $50, much less $350. Even though the government’s own statistics show providers prevail the majority of the time over insurers in IDR, to date we have only submitted about 200 IDR claims. Batching rules, the IDR processing backlog, and delay tactics by payers (for example, failing to abide by the arbitrators ruling and promptly remitting payment for cases won by the provider group, as has happened to WEPPA, or in some cases, not paying at all) have also contributed to this substantial burden. Now that at least some of these issues have been resolved due to recent court decisions and the resulting pending regulatory changes, we do hope to reengage with the IDR process when the portal reopens.
This increased focus on our collections and the rates being paid by insurers takes up valuable provider and staff time as well as resources that we would rather devote to patient care. We would rather not be forced to submit IDR claims. We WANT to go back to being in-network with every payer and our long-lasting contracts in place prior to passage of the NSA show that we always did our best to be in network. If these conditions persist, we may be forced to confront a financial reality where we must reduce salaries, reduce physician and advanced practice provider staffing hours, cut positions, or make difficult decisions about what areas we can realistically serve. The current climate not only threatens our ability to provide “everyday” emergency care, but it also significantly diminishes our readiness for a major disaster, mass casualty event, pandemic, or other significant event.
Frequently throughout the surprise billing debate at the federal level, emergency physicians as a profession were vilified by erroneous assertions that they purposely stay out of network so that they can charge higher rates. But our group and countless others are evidence of local, community-based emergency department (ED) practice groups who have been (or were) in long-term, stable contracts with the major insurers, and who would continue to be in network were it not for the regulatory implementation of the No Surprises Act – particularly the continued efforts to establish an artificially-low payment standard via the Qualifying Payment Amount (QPA).
Emergency physicians provide care under circumstances and laws that are unique among other physician and provider specialties. We provide more uncompensated care than any other physicians, as the federal Emergency Medical Treatment and Labor Act (EMTALA) requires that anyone coming to an emergency department must be stabilized and treated, regardless of their insurance status or ability to pay. The burden of uncompensated care only continues to grow, particularly in communities with high populations of uninsured patients. Additionally, in order to ensure 24/7/365 access to the emergency department, we work under stricter staffing and standby requirements than other types of medical providers so that we can meet the needs of patients who experience a wide range of emergencies every day, such as heart attacks, strokes, trauma, and mental health conditions, or as we have all experienced over the course of the last several years, the ravages of the global COVID-19 pandemic.
Those who support the approach that has been taken to date in implementing the No Surprises Act have suggested that cutting reimbursements to physicians and providers will enable insurers to lower premiums, allowing for more affordable and accessible coverage for Americans. Yet there is nothing in the law, or in its regulatory implementation, to ensure that happens. Several of our contracts were in place for a decade without any sort of increase to the negotiated reimbursement rates. If rising costs were “forcing” insurers to raise premiums year-over-year, it was not due to our contracts. In the meantime, insurers continue to see record profits, in no small part due to lower health care utilization during the height of the COVID-19 pandemic. Premiums for employer-sponsored family health coverage continue to grow, averaging $22,463 in 2022 and representing a 20 percent increase since 2017.[1] Meanwhile, UnitedHealth Group posted nearly $5 billion in quarterly profit in the final quarter of 2022, and more than $20 billion total over the year – a more than 16 percent increase from 2021.[1] We remain skeptical that any savings, borne on the backs of providers under the implementation of the law to date, will ever be passed on to consumers.
Emergency departments throughout the country are already under immense strain due to the ongoing ED “boarding” crisis, where patients must wait hours, days, and even months for care or to be transferred to the appropriate setting they need and deserve. This has exacerbated physician stress and burnout – a persistent, pervasive issue for emergency physicians who consistently report the highest rates of burnout among any physician specialty (65 percent in 2021).[2] Continued cuts of this magnitude combined with growing frustrations in our attempts to negotiate in good faith for reasonable and fair contracts will have ripple effects throughout our practice, throughout the health care system in North Carolina, and throughout our country.
There is no doubt that these effects will be felt even more deeply in our rural and underserved communities, where the health care safety net is already under threat. Many emergency physician practices will be unable to afford to continue to operate in the areas where patients need them most, and millions of your constituents will have less access to the lifesaving emergency care they need and deserve. The growing trends of health care consolidation will only accelerate as practices are unable to endure the weight of these economic pressures.
WEPPA is only one practice, but sadly we know our experience is not unique. We believe the No Surprises Act clearly struck a delicate balance as to not tip the scales too far in favor of any party, but the regulations have not been consistent with the law that Congress passed. Thank you once again for your attention to these issues and for the opportunity to be here to share our experience. I look forward to any questions you may have.
[1] https://www.fiercehealthcare.com/content/which-payer-raked-most-cash-last-year-answer-likely-wont-surprise-you
[2] https://www.prnewswire.com/news-releases/medscape-physician-burnout-and-depression-report-burnout-worsening-depression-increasing-301732504.html
[1] https://www.kff.org/report-section/ehbs-2022-section-1-cost-of-health-insurance/
Ways and Means Committee Press Release Following Hearing.
Maui Recovery Remains Slow, Hawaii Medical Association Reports Huge Need for Help

As Island Transitions from Response to Recovery, the Need for Help Continues in All Sectors Including Healthcare
For more than 15,000 people, Monday marks a big step to rebuilding their lives. It is the first day that reentry begins for people who were living in the impact zone of the Maui wildfire. To date, 97 bodies have been recovered, 80 have been identified. There are 23 active investigations into missing persons for unaccounted individuals. Reports say Maui is losing more than $13 million per day and recovery of the important tourist industry is lagging.
Marc Anderson of the Hawaii Medical Association tells NCMS VP Alan Skipper that there is "still a huge recovery need and an ongoing effort to meet the needs of those impacted by the fire." He as supplied NCSM with the Hawaii Medical Association's detailed report of ways physicians are helping with Maui support.
The report has several key findings:
- Disillusionment is increasing. People are grieving and also wanting to protest over reentry issues.
- Clinics in West Maui are open with no appointments necessary. Health insurance is not required and translation services are available.
- Challenges remain in outreach for the displaced elderly population.
- Particulate level analysis is ongoing and could take weeks.
- Mental health triage continues.
The report has detailed and time-stamped recovery efforts since the fire. It includes links to volunteer options, healthcare resources, and the latest news.
To read the full report from the Hawaii Medical Association click here.
Here are some options to make donations:
- The American Psychiatric Association (APA) Foundation has created a Maui Disaster Relief Fund in partnership with the Hawai’i Psychiatric Medical Association and in support of the Hawai’i Community Foundation’s Maui Strong fund.
- To kick start these fundraising efforts, the APA Foundation will match up to $25,000
- Donate online at the American Psychiatric Association Foundation Maui Donation page
- Kākoʻo Maui fund: The Council for Native Hawaiian Advancement, Alakaina Foundation Family, and Kako’o Haleakala will match up to $100,000 in donations for Kako’o Maui. Funds will go to families and businesses. You can donate here .
- American Red Cross of Hawaii: They’re asking for your monetary donations and for volunteers. Click here for details.
- Hawaii Emergency Management Agency: Donations and volunteer support information at ready.hawaii.gov or 808-733-4300.
- Maui United Way: The Fire Disaster Relief Fund is providing financial assistance through grants to nonprofits at the forefront of relief efforts, as well as directly to households that have been deeply affected. Those who would like to donate may do so at mauiunitedway.org/disasterrelief.
- The Hawaii Salvation Army will start providing meals for thousands displaced in Maui emergency shelters. They are asking for monetary donations and large volume meal donations from restaurants and certified kitchens to aid in mass meal service at Maui shelters. All money donated for disaster relief will go to disaster operations. Donate to Hawaii Salvation Army here
- The Hawaii Community Foundation Maui Strong Fund will support Maui communities affected by recent fires, including response and recovery efforts. The proceeds from our bake sale will go to this fund. Donate to the Hawaii Community Foundation Maui Strong Fund here
- UH Maui College students and their families are directly impacted by the fires, whether they have lost homes, businesses, or jobs. As the new school year starts, you can help keep students, faculty, staff, and their families resilient during this unprecedented emergency. Donate to the UH Maui College Student Aid Fund here.
- The UH Maui College Faculty and Staff are in the same situation as students. Donate to the UH Maui College Faculty and Staff Aid fund here.
- Matson: Nonprofit organizations needing assistance in getting goods to Maui are asked to apply for such assistance on the company’s website at matson.com/community.
- United Public Workers: Donate nonperishable items at any UPW headquarters across the state from 6 a.m. to 7 p.m. Locations of headquarters are: Oahu: 1426 N. School St.; Hawaii island: 362 E. Lanikaula St.; Maui: 841 Kolu St.; and Kauai: 2970 Kele St. Suite 213.
- Hawaii Restaurant Association: To contribute food, water, medical supplies or shelter from Maui or Oahu, fill out the form at tinyurl.com/2a9jfjdy.
Biden administration seeks to remove medical bills from credit reports

(CNN-Tami Luhby) -- Millions of Americans with unpaid medical bills would no longer have that debt show up on credit reports under proposals being considered by the Consumer Financial Protection Bureau. The agency, which is soliciting feedback from small businesses that may be affected, expects to issue a proposed rule next year, the bureau said Thursday.
If the rule is finalized, consumer credit companies would be barred from including medical debt and collection information on reports that creditors use to make underwriting decisions.
Creditors would only be able consider non-medical information when evaluating borrowers’ loan applications. And debt collectors would no longer be able to use the listing of medical debt on credit reports as leverage to pressure consumers into paying questionable bills, the bureau said.
“Research shows that medical bills have little predictive value in credit decisions, yet tens of millions of American households are dealing with medical debt on their credit reports,” said CFPB Director Rohit Chopra. “When someone gets sick, they should be able to focus on getting better, rather than fighting debt collectors trying to extort them into paying bills they may not even owe.”
Roughly 20% of Americans reported having medical debt, according to a 2022 report from the bureau. But Chopra stressed that many health care bills contain mistakes.
“Families are often barraged with a string of confusing and error-ridden bills, and too many of us have ended up in a doom loop of disputes between insurance companies and health care providers,” he said. “These bills, even ones where the patient doesn’t owe anything further, can end up being reported on the patient’s credit report.”
The proposals under consideration are the latest step in the bureau’s efforts to curb the impact of medical debt on consumers. CFPB and other agencies are also looking into medical billing practices, including costly products such as medical credit cards and installment loans.
The White House has also sought to help lessen Americans’ medical debt burden as part of its effort to help people contend with inflation and higher costs of living. Last year, it laid out a four-point plan to help protect consumers, including having the bureau investigate credit reporting companies and debt collectors that violate patients’ and families’ rights.
Medical debt has lowered people’s credit scores, which affects their ability to buy a home, get a mortgage or own a small business, Vice President Kamala Harris said in a call with reporters on Thursday.
“We know credit scores determine whether a person can have economic health and well-being, much less the ability to grow their wealth,” she said. “Today, we are offering a solution to fix this problem … Together, these measures will improve the credit scores of millions of Americans so that they will better be able to invest in their future.”
Also last year, the three largest credit reporting agencies – Equifax, Experian and TransUnion – announced they would remove nearly 70% of medical debt from consumer credit reports.
The agencies no longer include medical debt that went to collections on consumer credit reports once it has been paid off. That eliminated billions of dollars of debt on consumer records.
In addition, unpaid medical collection debt no longer appears on credit reports for the first year, whereas the previous grace period was six months. That gives people more time to work with their health insurers or providers to address the bills. And medical collection debt of less than $500 is no longer included on credit reports.
On The Lighter Side - September 22, 2023 - Fall Foliage, Octoberfest, and the Jonas Brothers!
Here are some things NCMS employees, members, and YOU are talking about this Weekend and Beyond!
Tomorrow is the first day of fall! Here is your Fall Foliage Predictions for NC!
October is when North Carolina (especially the mountains) will have peak colors. October 23 will be the best weekend for fall colors across much of the state, but look for things to start popping in early October. The western portion of the state will have the best viewing spots. Here is a look at when you Fall color peaks occur so you can plan your trip!
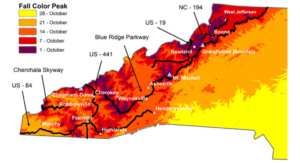
Fall color along the Blue Ridge Parkway is an event that everyone should see. The mixture of vibrant colors with some of the most beautiful scenic vistas in the world, is truly magical.
To find out the 22 best stops along the Parkway to see fall color click here. Make sure you let NCMS know your favorite spots!
It is also time for Grahamtoberfest!

The 3rd Annual Grahamtoberfest is tomorrow! Enjoy Beer Tents, Food Trucks, Live Music, Vendors, Beer Garden, Crafts and Contests. Click here for all you need know!
Carolina in the Fall Music and Food Festival in Wilkesboro

Food, food, and more food! The Carolina in the Fall Music and Food Festival brings together a famous lineup of food trucks, paired with some of the hottest performers in the state. It last all weekend and it is fun for the whole family. More details on the festival are here.
Fall means more college football!

- Florida State vs Clemson at Death Valley, noon
- Ole Miss vs. Alabama at Bryant–Denny Stadium, 3:30pm
- Duke vs. Connecticut at UConn, 3:30pm
- Ohio St. vs. Notre Dame at Notre Dame, 7:30pm
- UAB vs. Georgia at UGA, 7:30pm
- UNC vs. Pittsburgh at Acrisure Stadium, 8pm
What A Man Gotta Do? Get out of the Waffle House and be Cool! The Jo Bros are coming to town!
On Thursday, you will be able to hear the crowd for miles close to the PNC Arena! Here is what you need to know!
If you have an event you would like added to On The Lighter Side, email Randy Aldridge at [email protected].
Town of Manteo Approves Partnership with NCMS Foundation

In June of 2022, the Outer Banks Family Medicine - Manteo clinic notified nearly 2,500 patients they would have to find a new primary care physician. In a letter from Outer Banks Medical Group, patients were told that the two temporary providers at the Manteo practice would not be renewing their contracts and therefore, the practice would no longer be able to provide them care. The patients at the Manteo practice were also informed that no other providers with the Outer Banks Medical Group were accepting new patients
The Outer Banks Medical Group is part of the Outer Banks Hospital, a partnership between ECU Health (formerly Vidant) and Chesapeake Regional Healthcare.
The temporary providers were covering patients previously cared for by Dr. Johnny Farrow, Dr. Jennifer Harrison and Dr. Warren Blackburn. Farrow and Harrison are now at Surf Urgent Care in Kill Devil Hills, and Blackburn has since retired.
In response to a public outcry, the Dare County Board of Commissioners established to a Healthcare Task Force to address the growing healthcare concerns in Manteo, Roanoke Island, and the rest of Dare County. Physician shortages continue to be an issue across the country. According to the Association of American Medical Colleges there will be an estimated shortage of between 37,800 and 124,000 physicians across the nation by 2034.

The task force created the Committee on Recruitment and Retention, which included North Carolina Medical Society Vice President of Solutions, Franklin Walker, in an effort to engage community members with special experience and expertise. Walker presented information on CPP and the newly launched CPP 2.0 programs to offer insight into NCMS Foundation’s (NCMSF) recruitment and retention programs.
On September 6, 2023, the Dare County Board of Commissioners approved a recommendation influenced by the committee, and set forth by the taskforce, to establish a formal partnership with NCMSF to build an active program of recruitment and retention of primary care providers through loan repayment programs, preceptorships and student rotations. The goal is for the collaboration to be the basis of maintaining an adequate supply of primary care providers, nurses, and other essential health personnel long term.
To address the shortage of mental health providers, the task force anticipates making recommendations in 2024 based on the CPP 2.0 model. The partnership will also leverage NCMSF’s expertise to identify issues that make healthcare recruitment and retention difficult, such as salary scales, the housing crisis, and lack of specialty care.
The North Carolina Medical Society Foundation is the philanthropic arm of the North Carolina Medical Society. The mission of the North Carolina Medical Society Foundation is to improve access to quality health care for all North Carolinians. Our portfolio of programs demonstrates our commitment to this vision.
For more information on NCMSF or to donate, click here.
Mental Health Awareness 5K Run/Walk in Lumberton Honors Dr. Jeffrey P. Campbell

The Mental Health Awareness 5K/Walk, honoring Dr. Jeffery P. Campbell is Saturday, September 23 at the Downtown Lumberton Pocket Park in Lumberton. It is co-hosted by Robeson County Medical Society and Robeson Road Runners. Proceeds will be donated to NC Professionals Health Program.
The 5K/Walk will begin in Downtown Lumberton and makes its way along the scenic Lumber River before heading through the quiet Tanglewood neighborhood. A straight shot down Elm St. will get runners to the finish line! This is not a timed race. Participants are encouraged to go at their own pace, including walking.
The first 75 registrants will receive a shirt.
For more information and to register click here.
Clean Classrooms for Carolina Kids Program Launches, NCDHHS has Message for NCMS Members
Program Designed to Eliminate Exposure to Lead and Asbestos

NCDHHS, in partnership with the NC Department of Public Instruction (NCDPI) and RTI International, announced that the Clean Classrooms for Carolina Kids™ program is ready to help public schools, licensed child care centers and family child care homes identify and eliminate exposure to lead and asbestos hazards in building infrastructure. The program is an expansion of Clean Water for Carolina Kids™, which previously tested all child care centers in the state for lead in water at drinking and food preparation taps. Lead and asbestos are known health hazards with no safe level of exposure.
Mark Benton, Chief Deputy Secretary for Health at DHHS, told NCMS:
"The wellbeing of children and families is a top priority for the NC Department of Health and Human Services. Our partnership with NCDPI and RTI on “Cleaner Classrooms for NC Kids” – that identifies and eliminates lead and asbestos hazards in schools and child care centers – is key to ensuring NC’s children are able to learn and grow in safe, healthy environments."
Public school facilities will be contacted by the NCDPI, while licensed child care centers and family child care homes will be contacted by NCDHHS' Division of Child Development and Early Education when it is time to enroll, beginning this month. In total, $150 million of American Rescue Plan Act funding was allocated by Gov. Cooper and approved in the legislative budget.
The program funding will be available until November 30, 2026.
To read announcement from RTI International click here.
Physicians Foundation 2023 Survey of America's Physicians Uncovers Future of Medicine is in Jeopardy
The Physicians Foundation and The Dr. Lorna Breen Heroes' Foundation Call for Systemic Change to Improve Current and Future Physicians' Wellbeing
BOSTON, Sept. 14, 2023 -- The Physicians Foundation announces its new survey, 2023 Survey of America's Current and Future Physicians, with findings that demonstrate a critical need for systemic changes within the health industry to help improve the future of medicine. Similar to previous years, the state of physician wellbeing remains low; however, residents and medical students report even lower states of wellbeing. In recognition of National Physician Suicide Awareness (NPSA) Day on September 17, The Physicians Foundation and The Dr. Lorna Breen Heroes' Foundation are accelerating systems change through Vital Signs: The Campaign to Prevent Physician Suicide to improve the wellbeing of physicians at all stages of their careers.
"Our country and health care system has been through a tremendous amount of stress and change in recent years. We're seeing how the pandemic, staff shortages, healthcare consolidation and more are exacerbating a system that already needed to see change and causing record levels of burnout," said Gary Price, MD, president of The Physicians Foundation. "The Foundation's latest survey demonstrates these impacts on both current and future physicians, signifying that systemic change must happen now to help improve the future of medicine. This NPSA Day and beyond, we hope that everyone will join us in our urgent call to support physicians in creating a health care system that is strong and sustainable."
The State of Wellbeing Remains Low
For the third year in a row, six in ten (58%) physicians often have feelings of burnout, compared to four in ten before the pandemic in 2018. Like their physician colleagues, six in 10 (61%) residents often have feelings of burnout. Whereas, seven in ten (71%) medical students report often having feelings of burnout. Furthermore, more than half of physicians (51%) know of a physician who has ever considered, attempted or died by suicide, remaining consistent since 2021. Though just starting their careers, a shocking proportion of students (45%) know a colleague or peer who has considered suicide, compared to residents (38%) and physicians (36%).
Despite high levels of stress, burnout and mental health distress, stigma and structural barriers prevent current and future physicians from seeking the care and support they need, with the majority of physicians (78%), residents (79%) and medical students (76%) agreeing that there is stigma surrounding mental health and seeking mental health care among physicians.
Creating a Culture of Wellbeing Among Future Physicians
In the face of these challenges, the survey suggests that residents and medical students strive to support themselves and each other. Agreement is significantly higher among residents and medical students compared to physicians for reporting that they know suicidal warning signs (physicians, 71%; residents, 83%; and medical students, 77%) and that they have checked in with a colleague experiencing mental distress (physicians, 35%; residents, 63%; and medical students, 67%). Residents (29%) and students (47%) are also significantly more likely to have sought medical attention for mental health in the past year, compared to physicians (19%). Lastly, six in ten medical students (60%) agree that physician wellbeing is a topic of conversation in medical school classes.
To better support the future physician workforce, The Physicians Foundation and The Dr. Lorna Breen Heroes' Foundation launched Dear FutureDoc, a new initiative from the Vital Signs campaign around NPSA Day. The goals of Dear FutureDoc are to encourage future physicians to reflect on their own mental health and wellbeing, to support each other and share their hopes for the future of physician wellbeing.
Dear FutureDoc includes three main resources:
- Note to Self: A notecard that medical students, residents and physicians can use to write a personal message to their future selves for encouragement.
- Note to Others: A notecard that future and current physicians can use to write an encouraging message to a peer or colleague.
- Selfie Sign: A sign to use as a background to take a selfie and post on social media with a message about their hopes for the wellbeing of physicians in 20 years.
Solutions to Improve the Future of Medicine
The future of medicine is dependent on change to offer the right resources and eliminate barriers that impact physicians' wellbeing. Physicians, residents and students have identified the solutions they need. At the top of the list, physicians (80%) and residents (85%) agree that reducing administrative burdens, such as low-value work, insurance approvals and unnecessary mandatory training, is helpful to improving wellbeing. Additionally, the survey found that at least half of physicians and residents report insurance requirements (physicians, 76%; residents, 77%), documentation protocols (physicians, 71%; residents, 67%), regulatory policies (physicians, 60%; residents, 50%) and mandatory training requirements (physicians, 53%; residents, 54%) as often or always hindering their autonomy to deliver high-quality, cost-efficient care.
"Ensuring the wellbeing of physicians, medical students and residents demands cultural and systemic changes," said Corey Feist, co-founder and president of the Dr. Lorna Breen Heroes' Foundation. "Through our Caring for Caregivers program we are working with hospitals, health systems and medical groups to reduce administrative burdens and remove barriers to access mental health care. Additionally, we launched a new Medical Student Coalition to empower medical students to reflect on the challenges that they face and the solutions that they need. We envision a future where seeking mental health services is universally viewed as a sign of strength for the physicians of today and tomorrow."
KEY FINDINGS:
The Physicians Foundation’s 2023 Survey of America’s Current and Future Physicians focuses on the state of physician, resident and medical student wellbeing as well as physician practice environments—and the solutions needed to improve both. The survey was conducted from June 8 through June 28, 2023, and the data presented is based on 2,114 responses. Complete methodology is available on page 64 of the full report.
Key findings of the survey include the following:
The state of physician wellbeing—for both current and future physicians—remains low.
- For the third year in a row, six in 10 physicians often have feelings of burnout, compared to four in 10 before the pandemic in 2018.
- Like their physician colleagues, six in 10 residents often have feelings of burnout.
- Whereas, seven in 10 medical students report often have feelings of burnout. Medical students’ overall wellbeing is lower than both residents and physicians.
- Three-quarters of medical students have felt inappropriate feelings of anger, tearfulness or anxiety, much more compared to residents (68%) and physicians (53%).
- More than half of medical students (55%) have felt hopeless or that they have no purpose, greater compared to residents (43%) and physicians (34%).
- More than two-thirds of medical students report withdrawing from family/friends/co-workers, significantly higher compared to residents (52%) and physicians (42%).
- Nearly two-thirds of medical students have felt levels of debilitating stress, much more compared to residents at 45%.
Additionally, current and future physicians alike report stigma and structural barriers negatively affect their overall wellbeing and mental health.
- Nearly eight in 10 physicians (78%), residents (79%) and medical students (76%) agree that there is stigma surrounding mental health and seeking mental health care among physicians.
- Approximately half of physicians (48%), residents (48%), and students (55%) said they know a physician/colleague/peer who said they would not seek mental health care.
- Four in 10 physicians were either afraid or knew another physician fearful of seeking mental health care given questions asked in medical licensure/credentialing/insurance applications.
- Nearly five in 10 residents and medical students were either afraid or knew another colleague fearful of seeking mental health care given questions asked in medical licensure/credentialing/insurance applications.
The full report, including methodology, demographics of respondents, and questions asked is available here.
Learn more and access the resources and solutions mentioned at NPSADay.org.
The report conclusion is here:
The Physicians Foundation’s 2023 Survey of America’s Current and Future Physicians finds that the state of physician wellbeing—for both current and future physicians—remains low. For the third year in a row, approximately six in 10 physicians often have feelings of burnout. Most physicians (78%) still agree that there is stigma surrounding mental health care for physicians, while the proportion of physicians who report seeking medical attention for a mental health problem (19%) has remained stagnant since 2022. Within the past year, nearly one-quarter (24%) of physicians know a colleague who has said they would not seek mental health support. Additionally, less than a third of physicians (31%) agree that their workplace culture prioritizes physician wellbeing, declining from 36% a year ago. More than half of physicians (51%) know of a physician who has ever considered, attempted or died by suicide, remaining consistent since 2021. One-fifth (20%) know a colleague who has either considered, attempted or died by suicide specifically in just the past 12 months. Meanwhile, the portion of physicians who know the warning signs to look for in themselves or colleagues that may be suicidal (71%) decreased compared to 2022 (78%). Not only must we do better for today’s physicians, but we must also help create a better reality for the physicians of tomorrow. Residents also report a low state of wellbeing—while medical students report an even lower state of wellbeing, compared to both physicians and residents. More than six in 10 residents (61%) and seven in 10 students (71%) report experiencing feelings of burnout. Though just starting their careers, a shocking proportion of students (45%) know a colleague or peer who has considered suicide, compared to residents (38%) and physicians (36%).
More than half of physicians (51%) know of a physician who has ever considered, attempted or died by suicide, remaining consistent since 2021. One-fifth (20%) know a colleague who has either considered, attempted or died by suicide specifically in just the past 12 months. Meanwhile, the portion of physicians who know the warning signs to look for in themselves or colleagues that may be suicidal (71%) decreased compared to 2022 (78%).
Not only must we do better for today’s physicians, but we must also help create a better reality for the physicians of tomorrow. Residents also report a low state of wellbeing—while medical students report an even lower state of wellbeing, compared to both physicians and residents. More than six in 10 residents (61%) and seven in 10 students (71%) report experiencing feelings of burnout. Though just starting their careers, a shocking proportion of students (45%) know a colleague or peer who has considered suicide, compared to residents (38%) and physicians (36%).
About The Physicians Foundation
The Physicians Foundation is a nonprofit seeking to advance the work of practicing physicians and help them facilitate the delivery of high-quality health care to patients. As the U.S. health care system continues to evolve, The Physicians Foundation is steadfast in strengthening the physician-patient relationship, supporting medical practices' sustainability and helping physicians navigate the changing health care system. The Physicians Foundation pursues its mission through research, education and innovative grant making that improves physician wellbeing, strengthens physician leadership, addresses drivers of health and lifts physician perspectives. For more information, visit www.physiciansfoundation.org.
About the Dr. Lorna Breen Heroes' Foundation
The Dr. Lorna Breen Heroes' Foundation is a 501(c)3 non-profit organization founded by the family of Dr. Lorna Breen. The mission of the Foundation is to reduce burnout of health care professionals and safeguard their wellbeing and job satisfaction. Their vision is that obtaining mental health support services is universally viewed as a strength and job requisite for health care professionals. The Foundation has three main tactics to achieve long-term change:
- Advise the health care industry on wellbeing initiatives that provide holistic mental health support.
- Build awareness on mental health prevalence to reduce the stigma; and
- Fund research and programs that seek to reduce health care professional burnout and improve their wellbeing.
The Dr. Lorna Breen Heroes' Foundation, alongside Harvard T.H. Chan School of Public Health, Thrive Global and the CAA Foundation and Creative Artists Agency, co-founded and co-lead ALL IN: WellBeing First for Healthcare, a coalition that focuses on systems-level, evidence-based solutions to improve healthcare worker mental health and well-being and shift the cultural stigma around health workers accessing mental health services.
About the Physicians Foundation's 2023 Survey of America's Current and Future Physicians
Each year, the Physicians Foundation assesses physician sentiment surrounding the practice environment and patient care, so we can understand where things stand and drive change to enhance physician practice and improve patient health outcomes. In 2023, the survey was conducted online among U.S. physicians, medical residents and clerkship/clinical rotation medical students, who were derived from Medscape's proprietary database. The survey was fielded from June 8 through June 28, 2023.
On The Lighter Side - September 15, 2023 - Fall Festivals, Football, and ZZ Top!
Here are some things NCMS employees, members, and YOU are talking about this Weekend and Beyond!
Fall is almost here! Get ready for Sweater Weather at the Mountain Heritage Festival!

28th Annual Mountain Heritage Festival in Sparta is Saturday! Vendors line historic Main Street in celebration of the area's rich mountain heritage, offering local handmade arts and crafts, a wide range of foods, live music and dancing, and the Kids Korner! More info and a schedule of events is here.
Marine Corps Half Marathon is Saturday!

Run this bucket list event that draws people from the entire East Coast to Jacksonville, NC. This flat scenic route winds through US Marine Corps Base Camp Lejeune with views of the New River, Morgan Bay, and Farnell Bay. A unique feature of this event is the Hero’s Mile, where signs are displayed along the route honoring military service members who have made the ultimate sacrifice post 9/11. How to attend and register is here.
Carolina Panthers take on New Orleans Saints Monday in Charlotte

Saints travel to face Panthers in NFC South dust-up Monday at 4:15pm. Catch the game at Bank of America Stadium in Charlotte. Read more on FOX Sports.
College football is back!

- Florida State vs. Boston College at BC, noon
- Notre Dame vs. Central Michigan at Notre Dame, 2:30pm
- UNC vs. Minnesota at Chapel Hill, 3:30pm
- South Carolina vs. Georgia at UGA, 3:30pm
- Duke vs. Northwestern at Duke, 3:30pm
- NC Central vs. UCLA at UCLA, 5 pm
Carolina Concerts and Shows

Tonight
- ZZ Top at Coastal Credit Union Music Pavilion, Raleigh
- Lorrie Morgan, Newton Performing Arts Center, Newton
- The Oak Ridge Boys, Newbery Opera House, Newberry, SC
- Chicago, the musical, Belk Theater, Charlotte
Saturday
- Widespread Panic, Live Oak Pavilion, Wilmington
- The Gatlin Brothers, COMMA Performing Arts Center, Morganton
- CeCe Winans, FaithFest, Wilkesboro
- Daniel Tosh, Steven Tanger Center, Greensboro
- Uncle Kracker, Cape Fear Vineyard, Elizabethtown
Sunday
- Daniel Tosh, Ovens Auditorium, Charlotte
- Noah Cyrus, Lincoln Theatre, Raleigh
If you have an event you would like added to On The Lighter Side, email Randy Aldridge at [email protected].
KIPL Alumni Featured at NC Chamber Health Care Conference

DURHAM -- The 2023 NC Chamber Health Care Conference met Thursday to discuss the evolving health care landscape on the state and national level. The meeting brought together leaders in the health care industry to gather ideas on AI, value-based care, well-being and mental health practices.
The experts and speakers included several alumni of the esteemed Kanof Institute for Physician Leadership.

Dr. Anuradha Rao-Patel, Associate Vice President, Senior Medical Director Government Markets, Blue Cross and Blue Shield of North Carolina is a KIPL graduate and NCMS member. She spoke on the role Artificial Intelligence plays in health care to help drive innovation, speed up care delivery, and drive-up access and outcomes while decreasing costs.

Dr. Dev Sangvai, President Duke Regional Hospital and Vice President for Population Health Management, Duke University Health System is a KIPL graduate, NCMS member, former HCLM Chair, and former President of NCMS. He was featured on the panel discussing value-based care. The focus of his panel was the direct impact of health care costs on business growth and the overall economy of North Carolina is undeniable. Improving health outcomes and making costs predictable and affordable for businesses while keeping employees as healthy as possible is imperative if we are to remain a top state for business while competing in today’s global economy. Gain insight as our panelists discuss real-life business scenarios of their health care benefits.

Dr. Art Apolinario, Board President, North Carolina Medical Society is a KIPL graduate as well. He was part of an interactive session with health care leaders to learn how and where collaborating can yield benefits and value for employees, businesses, and our communities.
Among the other speakers and panel members where Michael Martine of IBM, Corey Mercy of Google, Gary Salamido, President and CEO of NC Chamber, Hugh Tilson, Jr. of NC AHEC, Kayt Leonard of SAS Global Health, Robert Shaw of Smith Anderson, and NCDHHS Secretary Kody Kinsley.

(L-R, Dr. William Lawrence, Dr. Michael Utecht, Dr. Damion McHugh, Dr. Art Apolinario)
If you would like to learn more about the Kanof Institute for Physician Leadership click here.
State Treasurer Report: NC Hospitals Charge Huge Markups, Hide Prices. NC Healthcare Association Responds.
NC State Treasurer Dale R. Folwell, CPA, released report showing extreme variations in hospital prices, huge price markups from Medicare rates, and widespread failures in price transparency.
NC Healthcare Association: Hospitals are not price setters and do not negotiate with Medicare nor Medicaid; transparency is a work in progress and a majority of NC hospitals are already in compliance.

(Raleigh) — North Carolina State Treasurer Dale R. Folwell, CPA, released a report saying “too many North Carolina hospitals are violating federal rules to hide prices from patients. The anti-competitive infractions thwart patients’ ability to make informed decisions about their health care.”
Among the findings:
- NC hospitals levy price markups of up to 1,120% on routine care and basic services. The most expensive subset charged commercially insured patients as much as 1,670 percent more than other hospitals for the same service.
- Workers lose 20 percent of every paycheck to health care costs with hospital systems receiving almost half of the health care spending in the United States. North Carolina’s public employees and taxpayers face a $24 billion unfunded liability for the State Health Plan.
- Services such as a urinalysis can carry a 1,120 percent median markup from Medicare, forcing patients to pay a median $28.80, while Medicare pays a median of just $2.36. The majority of North Carolina hospitals self-reported profiting off Medicare rates over six years.
- The largest price disparities appear in radiological services. Hospitals inflated their $1,167.23 median commercial price for a CT scan of the brain by 976 percent from Medicare’s $108.44 median rate. These disparities have ties to state Certificate of Need (CON) laws, which restrict the supply of health care equipment and facilities.
- Across the majority of the 16 common shoppable services, hospitals charged uninsured patients more than 150 percent more than Medicare rates. A fourth of the 16 analyzed shoppable services had a higher markup on “cash” prices than on commercial rates.
- The most expensive subset of North Carolina hospitals charged commercially insured patients as much as 1,670 percent more than other hospitals for the same service.

The North Carolina Healthcare Association responded to the report directly to the North Carolina Medical Society. NCHA says it supports “transparency around patient care quality, safety and other data and information to support consumer decision-making. It is the right thing to do and is in the best interests of our patients and communities.”
Highlights of NCHA response:
- The effort toward pricing transparency is a work in progress for all U.S. hospitals.
- The suggestion that hospitals “hide” prices from patients is absolutely false. A majority of North Carolina hospitals are already compliant.
- Hospitals do not negotiate with Medicare nor Medicaid. Government payers reimburse healthcare providers a set amount which is typically not sufficient to reimburse providers for care they deliver to patients.
- Hospitals do negotiate with commercial payers and those negotiations are conducted between two mature organizations at arms-length, like other legal business arrangements.
FDA: Common Over-the-Counter Decongestant Doesn’t Work

(NBC News - Berkeley Lovelace, Jr.) -- A key ingredient in many over-the-counter cold and allergy medications called phenylephrine doesn’t work to get rid of nasal congestion, a Food and Drug Administration advisory panel concluded Tuesday.
The unanimous vote, which specifically declared oral formulations of phenylephrine ineffective, is expected to disrupt the market for OTC cold and allergy remedies, where consumers largely prefer pills over nasal sprays.
Phenylephrine — found in drugs including Sudafed PE, Vicks Nyquil Sinex Nighttime Sinus Relief and Benadryl Allergy Plus Congestion — is the most popular oral decongestant in the United States, generating almost $1.8 billion in sales last year, according to data presented Monday by FDA officials.
The drug is thought to relieve congestion by reducing the swelling of blood vessels in the nasal passages.
The panel’s vote reflects damning evidence provided by the FDA that found that when phenylephrine is taken orally, a very small amount of the drug actually reaches the nose to relieve congestion.
Susan Blalock, a retired professor at the UNC Eshelman School of Pharmacy in North Carolina and an advisory committee member, said the evidence is "pretty compelling that this medication is not effective. I don’t think additional data are needed to support that conclusion."
The FDA will now need to decide whether to revoke the drug’s OTC designation as “generally recognized as safe and effective.” The designation, typically used for older drugs, allows drugmakers to include an ingredient in OTC products without the need to file an FDA application.
Without the designation, products containing the ingredient may need to be removed from store shelves, or manufacturers may have to develop new formulations. A spokesperson for the FDA declined to say when the agency will make a final decision. The FDA usually sides with its advisory committees.
"This drug and this oral dose should have been removed from the market a long time ago," said Jennifer Schwartzott, a patient representative from New York. "The patient community requires and deserves medications that treat their symptoms safely and effectively and I don’t believe that this medication does."
Phenylephrine gained popularity in the early 2000s as a replacement for pseudoephedrine, the decongestant used in Sudafed, which was moved behind the pharmacy counter in 2006 in an attempt to curb its misuse as an ingredient to make methamphetamine.
During the two-day meeting, FDA scientists presented the results of five studies conducted over the past two decades on the effectiveness of oral phenylephrine. All the studies concluded that the decongestant was no more effective than a placebo.
They also re-evaluated the initial findings used to support its OTC use. The agency found that the results were inconsistent, did not meet modern standards for study design and may have had data integrity issues.
“In conclusion, we do believe that the original studies were methodologically unsound and do not match today’s standard. By contrast, we believe the new data are credible and do not provide evidence that oral phenylephrine is effective as a nasal decongestant,” said Dr. Peter Starke, an FDA official who led the review of phenylephrine.
The concern goes beyond ineffectiveness; phenylephrine can come with side effects such as headaches, insomnia and nervousness. At higher doses, it can increase blood pressure.
The panel is not questioning the effectiveness of nasal spray phenylephrine, which is still thought to provide temporary relief from congestion.
Representatives for the Consumer Healthcare Products Association, a group that represents OTC drug manufacturers, did not offer any new evidence to counter the FDA’s claims that the drug is ineffective during their presentation Monday.
The group instead said that if oral phenylephrine were not available over the counter, it would be a significant burden to consumers.
The group shared a survey that found 1 in 2 households in the U.S. used an oral decongestant over the last year. It also found people prefer oral decongestants over nasal spray 3 to 1.
The group also said that other effective alternative options would not be as easily accessible, a claim disputed by advisory committee members.
"We do have an effective alternative in pseudoephedrine," said committee member Dr. Maryann Amirshahi, a professor of emergency medicine at Georgetown University School of Medicine, referring to the ingredient found in Sudafed. "That bar to the product really isn't as high as was described."
Patients who want to buy Sudafed must request it from a pharmacist.
FDA Approves Updated Covid Vaccines from Pfizer and Moderna as Hospitalizations Rise

(CNBC - Annika Kim Constantino) -- The Food and Drug Administration on Monday approved updated Covid vaccines from Pfizer and Moderna, putting the shots on track to reach Americans within days as U.S. hospitalizations from the virus rise.
The new vaccines, which target the omicron variant XBB.1.5, are approved for people 12 and older and are authorized under emergency use for children 6 months through 11 years old, according to an FDA release.
A CDC advisory panel is scheduled to meet Tuesday to vote on a recommendation on the use of those jabs. After the CDC director signs off on those recommendations, the shots can be administered at pharmacies, health clinics and other vaccine distribution sites.
The Biden administration said in August that it expects new single-strain vaccines from Pfizer, Moderna and Novavax targeting XBB.1.5 to be available to the public in mid-September.
The FDA did not announce a decision Monday on an updated Covid shot from Novavax, but the company said in a statement that the agency is still reviewing its vaccine. Shares of Novavax closed nearly 13% lower Monday following the approval of the other updated jabs.
Novavax’s vaccine uses protein-based technology, a decades-old method deployed in routine vaccinations against hepatitis B and shingles. Meanwhile, Pfizer’s and Moderna’s shots use messenger RNA, which teaches cells how to make proteins that trigger an immune response against Covid.
While the shots do not target the variants dominant now, the vaccine makers have said the shots will still offer protection against those strains as children return to school and the weather gets cooler.
“We expect this season’s vaccine to be available in the coming days, pending recommendation from public health authorities,” Pfizer CEO Albert Bourla said in a release following the approval.
Bourla and Moderna CEO Stéphane Bancel, in a separate statement, urged Americans to receive their updated Covid shot during the same appointment as their annual flu shot.
Hospitalizations have increased for seven straight weeks, and rose more than 15% for the week ending Aug. 26, to 17,418, according to the latest data from the CDC. But that number remains below the surge the nation saw in summer 2022, when hospitalizations climbed to more than 40,000.
The uptick is fueled by newer — but closely related to XBB.1.5 — strains of the virus such as EG.5, or Eris. That omicron strain accounted for 21.5% of all cases as of Sept. 2, according to the CDC.
Meanwhile, XBB.1.5 is declining in the U.S., the CDC said.

Pfizer, Moderna and Novavax have released early trial data indicating their new shots provide protection against Eris.
Both Pfizer and Moderna have also said their updated shots produced a strong immune response against BA.2.86, a highly mutated omicron subvariant that health officials are watching closely.
“The updated vaccines are expected to provide good protection against COVID-19 from the currently circulating variants,” the FDA said in the release Monday.
The agency noted that last year’s Covid boosters from Pfizer and Moderna are no longer authorized in the U.S.
The upcoming vaccine rollout will be the first since the end of the U.S. Covid public health emergency, which expired in May.
The end of that declaration means the federal government will shift vaccine distribution to the private market, where manufacturers will sell their updated shots directly to health-care providers at higher prices. Previously, the government purchased vaccines directly from manufacturers at a discount to distribute to all Americans for free.
Private insurers and government payers such as Medicare, which cover the vast majority of Americans, are expected to provide the vaccines to people for no fee. Federal efforts such as the Biden administration’s Bridge Access Program aim to provide free Covid shots to uninsured people.
The Biden administration will urge Americans to receive an updated Covid shot this fall, White House press secretary Karine Jean-Pierre said last week.
“Vaccinations against Covid-19 remains the safest protection for avoiding hospitalization, long-term health outcomes, and death,” Jean-Pierre said during a briefing.
But it’s unclear how many Americans will actually roll up their sleeves to get another shot in the coming months.
Only around 17% of the U.S. population — around 56 million people — have received Pfizer’s and Moderna’s latest boosters since they were approved in September 2022, according to the CDC.
ADDTIONAL READING
FDA Signs Off on Updated Covid-19 Vaccines That Target Circulating Variants
New Covid Vaccine Booster Could be Available This Week After FDA Approval
As Hurricane Season Peaks, Is Your Practice Prepared?
Is Your Practice Ready to Face a Hurricane?
North Carolina is in the middle of Hurricane Season and in a period of active tropics. Natural disasters can happen anywhere, at any time—and they can create widespread damage. A disaster can overwhelm an office practice, causing physical damage such as shattered windows, flood debris, power outages, disrupted telephone service, computer and technology system outages, unsafe drinking water, patient record destruction, medication exposure to temperature and humidity extremes, contaminated instruments and supplies, and building structure failure.
Clinicians may be forced to relocate their practices quickly―sometimes permanently―or move scheduled procedures to different facilities. For public safety, practices may be forced to close for days or even weeks. These disruptions can be catastrophic to the delivery of essential healthcare services to patients and, potentially, to the long-term financial well-being of the office and the individual providers.
Is your practice prepared for a disaster? Here are some tips:
Plan Now
Before the next disaster strikes, make sure your practice has a written plan in place. A checklist, ordered by priority and customized to specific types of disasters, can provide the framework for a comprehensive plan. The checklist should include these elements:
- Backup and recovery methods for electronic data, including the EHR and billing records. Methods could involve cloud storage or remote servers. Retain at least one copy of the backup offsite. All backup and recovery systems must be compliant with HIPAA.
- An inventory with photographs of tangible assets, such as medications, durable medical equipment, medical or dental devices and machinery, office and clinical supplies used during the provision of services, computers, artwork, fixtures, and furniture.
- Copies of important legal documents, such as licenses, leases, permits, contracts, deeds, insurance policies and certificates of coverage, tax records, office policies and procedures, and personnel files. These documents must be readily accessible if a disruption occurs.
- A list of important telephone contacts and email addresses, such as practice staff, healthcare professionals, vendors, insurance agents, licensing agencies, practice attorneys, and emergency response officials.
- A full-circle call tree for staff that outlines who contacts whom with mobile and alternative contact numbers.
- Instructions for setting up instant messaging technology (e.g., with chat messenger apps) that enables staff to communicate without a wireless network or cellular data connection.
- Instructions for securing the records of patients undergoing diagnostic testing and a list of outstanding diagnostic studies requiring follow-up.
- Guidelines for maintaining HIPAA compliance. The U.S. Department of Health and Human Services (HHS) provides protected health information guidance for planning and response to emergency situations (see Emergency Situations: Preparedness, Planning, and Response). Although the HIPAA Privacy Rule is not suspended during a natural disaster or other type of emergency, the HHS Secretary may waive certain provisions of the Privacy Rule (see “Is the Privacy Rule suspended during a national or public health emergency?”). The Office of Civil Rights may also issue notifications of temporary enforcement discretion. (For example, see the HHS notifications related to HIPAA and COVID-19.)
- Copies of certificates of insurance for your professional malpractice coverage and all product lines (such as general liability, cybersecurity, and employment practices) or instructions for contacting your agents or insurers directly to obtain proof of coverage and policy terms. These documents will be necessary if you are forced to temporarily relocate your practice or convert your delivery of care to a virtual format.
- Steps to follow upon returning from evacuation to ensure continuity of care and operational readiness to resume office functions.
Once your plan is in place, reevaluate it regularly and update all information—including disaster policies and procedures, contacts, insurance coverages, and legal documents.
If Disaster Strikes
Planning today makes accomplishing the following tasks easier in the event of a disaster:
Communication
- Stay current on emergency directives from state and local governmental disaster relief and recovery entities. Consider registering for text message, social media, and email alerts.
- Contact staff immediately to determine return-to-work time frames as permitted.
- Implement virtual staff briefings at the beginning and end of each day.
- Create temporary telephone, fax, and answering services if necessary.
- Notify external vendors and business associates about your practice interruption and targeted resumption of operation.
- Establish patient telephone triage. (Find more information in our article “Telephone Triage and Medical Advice Protocols.”)
- Establish telehealth services as capabilities permit. (For more information, see our article “Top Seven Tips for Telehealth.”)
- Implement temporary controls to ensure HIPAA compliance.
Patient records
- Determine and document the extent of damage to, or loss of, electronic and paper patient records and filing systems.
- Attempt to restore all damaged charts and relevant business records, and document inventory findings.
- Check the websites of your state licensing board and federal agencies, such as HHS and CMS, for specific guidance pertaining to lost or damaged records.
- Reconstruct lost charts at the next patient encounter and include a notation that the record is a re-creation.
- Date and initial all late entries and duplicate information in context of recovery efforts.
- Document all efforts to restore and protect existing records.
- Contact your insurance carrier for restorative services and/or claim procedures.
- Reestablish a filing system and temporary storage if necessary.
- Obtain legal guidance for patient notification during recovery efforts.
Computers and systems
- Contact computer service vendors to ensure the integrity and recovery of your systems.
- Inventory and document damage to hardware and software.
- Verify insurance coverage for repair or replacement costs and losses.
- Evaluate applicable warranties and consider contracting with an information technology restoration service.
- Reestablish filing systems and internal programs.
- Ensure data backup and periodically test compliance.
Office building
- Notify the building owner and your property insurance company regarding damage.
- Review inspection reports for identified damage and the schedule for repairs, and determine what impact the findings have on practice operations.
- Take appropriate measures regarding mold growth and removal if the building has suffered water or flood damage.
- Flush hot and cold water lines for 10 minutes if the building has been vacant for a week or more.
- Create an inventory of all equipment and medications that may have been exposed to water, extremes in temperature, or other contaminants. Repair, replace, or discard damaged items appropriately.
Practice and rehearse the plan’s protocols at least twice a year with all professional, administrative, and clerical staff, and participate in a community-based drill, if available. Address any areas that need improvement. An effective disaster preparedness plan will help ensure patient and staff safety and keep your practice focused on delivering care during an emergency.
The North Carolina Department of Public Safety has prepared a NC Hurricane Guide. It has tips for you and your family in the event of imminent tropical impacts. Here is a guide for you to use at home:
NCDPS North Carolina Hurricane Guide
NCDHHS has also put together a list of resources so you can be best prepared for the Atlantic Hurricane Season:
NCDHHS Disaster Preparation and Recovery Guide
To track any tropical disturbance, the NOAA National Hurricane Center has a website to keep you up to date:
National Hurricane Center Tracking Center
NCMS Capitol Chronicle - Advocacy Engagement with Congresswoman Virginia Foxx

August 26, 2023
Advocacy Engagement with Congresswoman Virginia Foxx
During Congress’ recent recess, NCMS members have been meeting with North Carolina’s members of Congress.
NCMS Vide President of External Affairs Alan Skipper, Dr. Jeffrey Keverline of Lenoir, and Dr. Brad Christoph of Hudson travelled to Boone for a meeting with th Congresswoman Virginia Foxx. They shared key messages on legislation under consideration in Washington.
Issues discussed included:
- The urgency of Medicare Physician Payment Reform
- Step Therapy’s impact on patient care and outcomes
- How Prior Authorization is delaying care and driving up healthcare cost.

Do you know your state and federal legislators?
More importantly, do your legislators know you?
Where Should Opioid Settlement Dollars Be Spent?

(Healthcare Brew, Shannon Young) -- With states set to receive more than $50 billion in opioid settlement funds over the next 15 years, advocates are urging policymakers to ensure the money is spent on public health interventions, like harm reduction efforts, and other programs that directly help people affected by substance use disorder.
A coalition of 130+ organizations that work on the opioid epidemic frontlines released a roadmap in late August to guide settlement fund spending. The $50+ billion from settlements reached with drugmakers, distributors, and sellers—including Johnson & Johnson, Purdue Pharma, and others—will be distributed to states and Washington, DC; councils in many of the states are to decide how that money will be used.
Mariah McGough, spokesperson for grassroots advocacy group Vocal-NY, said the 10-page document is “a warning to policymakers that if these funds are mishandled and funneled into criminalization, it’s only going to make [the opioid] crisis worse and cost more lives.”
The roadmap calls for investments in public health, housing supports, community-based organizations, and other efforts that address “collateral consequences of drug war policies.”
The coalition touted Rhode Island’s decision to dedicate $2 million of its settlement dollars to support an overdose prevention center and Kentucky’s move to grant $1 million to four legal aid groups that support people who use drugs as examples of “good spending.”
“We know what works, and we also know what doesn’t work,” Vinay Krishnan, national field organizer for the Center for Popular Democracy, said at a recent virtual news conference. “We know that police, prisons, carceral approaches—criminalization—do not work. You can’t arrest your way out of a public health crisis.”
The roadmap argued that the $50 billion should not be used for criminalization or incarceration, family separation, abstinence-only treatment and education, or bolstering state general fund revenues. The coalition pointed to Louisiana’s decision to allocate 20% of its settlement funds to sheriffs and Maine’s plan to spend some of its money on a program embedded with police as examples of “problematic spending.”
The coalition further contended that decisions on opioid settlement fund spending should be transparent and include people and communities directly affected by the “war on drugs,” including active drug users. No state, the document noted, is “fully adopting” the coalition’s priorities.
“While the roadmap, and the signers of the roadmap, come from different states and regions and political landscapes, we are united in calling for divestment from criminalization and investment in life-saving harm reduction strategies,” McGough said.
States have already started receiving opioid settlement funds, which are expected to be distributed through 2038.
FDA Could Greenlight New COVID-19 Booster Any Day, Shots Will Not Be Covered by Federal Government
The shots could become available next week, after the Centers for Disease Control and Prevention also signs off.

(NBC News, Berkeley Lovelace Jr. and Monica Alba) -- he Food and Drug Administration plans to greenlight updated versions of the Covid boosters as early as Friday, according to four people familiar with the agency’s plans.
The latest shots are designed to target the XBB.1.5 omicron subvariant. Though that strain is no longer dominant, the boosters should still protect against current circulating subvariants, which are closely related, the drug makers and experts say.
The Friday timeline for authorization is not firm, and it could slide into early next week, two of the sources said.
That could prompt further criticism from some doctors who say federal health agencies are acting too slowly in the booster rollout as Covid cases and hospitalizations are once again rising.
Two sources indicated the FDA is exploring the possibility of granting the boosters a full approval license instead of an emergency use authorization, a departure from the approach used for previous Covid vaccine authorizations. However, it remains uncertain whether that is still the intended course of action.
After the FDA’s signoff, the Centers for Disease Control and Prevention and its advisory committee will issue their own recommendations about who should get the shots and how they should be used. The agency’s Advisory Committee on Immunization Practices is expected to vote at a scheduled meeting Tuesday. The CDC’s director, Dr. Mandy Cohen, could sign off on the boosters shortly after the meeting, allowing vaccinations to begin.
About 97% of adults have some level of protective immunity, according to data shared by government officials. However, because immunity from previous infections and vaccinations diminishes over time, officials aim to shore up protection as people spend more time indoors during the fall and the winter.
For the first time since Covid vaccines have been available, however, the cost of the shots will not be covered by the federal government.
Pfizer and Moderna have indicated the list price for the vaccines will be $110 to $130 per dose.
Whether and when someone will be able to get the shots will depend on their insurance coverage, said Jennifer Kates, the director of the Global Health & HIV Policy Program at KFF, a nonprofit health policy organization.
Most people with private and public health insurance should continue to pay nothing out of pocket for the vaccines, Kates said. If a person gets the vaccine out of network, however, it could carry a cost.
Some people without insurance may be able to get boosters free from safety net providers, such as community health centers, but others may have to pay the full cost. The Biden administration has also announced a “bridge” program that will offer uninsured people access to free boosters at least through the end of 2024.
Novavax’s vaccine, which has not been granted full FDA approval yet but instead is available through emergency use authorization, will continue to be covered, Kates said.
What Can We Learn From Death of Jimmy Buffett?
Merkel Cell Carcinoma is Uncommon, But Rates Have Tripled in Past Two Decades

(ABC News, Mary Kekatos) -- "Margaritaville" singer Jimmy Buffett died on Sept. 1 after a four-year battle with a rare skin cancer.
Buffet's website revealed he had been diagnosed with Merkel cell carcinoma, but had been able to perform until recently, when his health began to decline.
Here's what you need to know about MCC, including signs and symptoms, what causes it and how it's treated.
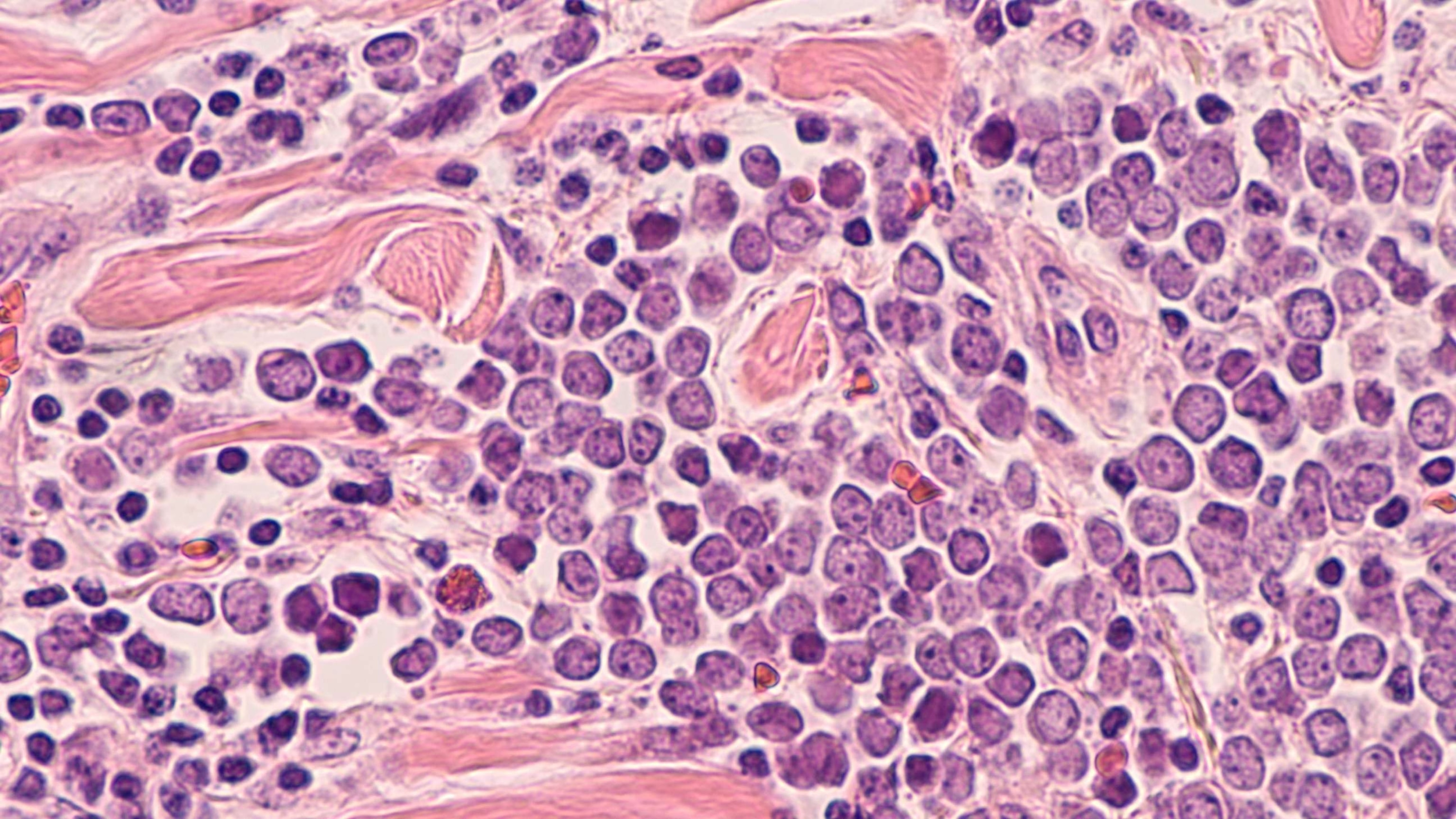
What is MCC?
Merkel cell carcinoma is much less common than the main types of skin cancer, such as basal cell carcinoma, squamous cell carcinoma and melanoma.
MCC is very rare -- about 40 times rarer than melanoma -- with an estimated 3,000 cases every year in the U.S., according to the Skin Cancer Foundation (SCF).
MCC is a neuroendocrine cancer, meaning it is a cancer of the cells that are connected to nerves, which likely play a role in touch sensation.
It is a rare, aggressive form of cancer that has a high risk of recurring and spreading within two to three years of being initially diagnosed, the SCF says.
What are the symptoms?
The first symptom of MCC is typically a fast-growing, painless tumor on part of the skin that is sun-exposed, according to the National Cancer Institute.
The nodules are usually shiny or pearly and may appear skin-colored in shades of red, blue or purple. However, they may appear dome-shaped or raised, firm or itchy, the Cleveland Clinic says.
A health care provider, such as a dermatologist, may perform a full-body skin exam to look for any abnormal spots as well as an exam of the lymph nodes because the cancer can spread quickly.
If the provider suspects MCC, they may perform a biopsy, which includes removing skin cells so they can be examined for signs of cancer.
What are the stages of MCC?
After a diagnosis is made, a patient's lymph nodes are often checked because of how quickly MCC can spread to this region, according to the SCF.
The next step is staging to identify how far along the cancer is. For this, the medical team will use the TNM system.
"T" stands for size of the original tumor, "N" for whether it has spread to the lymph nodes and "M" for metastasis, or spread.
Stage 0 indicates MCC cells have been found but not beyond the top layer of skin, the SCF says. Stages 1 and 2 involve smaller and larger tumors, respectively. In stage 2, the tumors may have spread to connective tissue, muscles or bones.
In stage 3, the tumors have spread to the lymph nodes or a lymph vessel between the original tumor and the nodes. In stage 4, the tumors have spread to the lymph nodes, organ or other parts of the body.
How is MCC treated?
Although MCC is rare, it is treatable when found in an early stage.
Depending on the stage of the disease and the patient's health, treatment involves surgically removing any tumors and potentially chemotherapy, radiation or immunotherapy.
If the cancer has spread to the lymph nodes, a patient may undergo a lymph node dissection, which is a surgical procedure in which some or all of the lymph nodes are removed.
How can I prevent MCC?
Males, those older than age 70, those with weakened immune systems and people with light-colored skin are more likely to develop MCC, according to the American Cancer Society.
Although these risk factors cannot be controlled, there are some steps that can be taken to lower the odds of MCC diagnosis.
This includes undergoing annual skin checks with a dermatologist, performing skin checks at home, lowering exposure to ultraviolet rays either from the sun or tanning beds and to practice sun safety when outdoors, such as covering the skin, wearing sunscreen and using hats or sunglasses.
ABC News' Dr. Mark Abdelmalek contributed to this report.
Scientists grow whole model of human embryo, without sperm or egg

A stem-cell derived human embryo model showing blue cells (embryo), yellow cells (yolk sac) and pink cells (placenta).
Scientists have grown an entity that closely resembles an early human embryo, without using sperm, eggs or a womb.
(BBC News, James Gallagher) -- The Weizmann Institute team say their "embryo model", made using stem cells, looks like a textbook example of a real 14-day-old embryo.
It even released hormones that turned a pregnancy test positive in the lab.
The ambition for embryo models is to provide an ethical way of understanding the earliest moments of our lives.
The first weeks after a sperm fertilizes an egg is a period of dramatic change - from a collection of indistinct cells to something that eventually becomes recognizable on a baby scan.
This crucial time is a major source of miscarriage and birth defects but poorly understood.
Starting material
Embryo research is legally, ethically and technically fraught. But there is now a rapidly developing field mimicking natural embryo development.
This research, published in the journal Nature, is described by the Israeli team as the first "complete" embryo model for mimicking all the key structures that emerge in the early embryo.
"This is really a textbook image of a human day-14 embryo," Prof Hanna says, which "hasn't been done before".
Instead of a sperm and egg, the starting material was naive stem cells which were reprogrammed to gain the potential to become any type of tissue in the body.
Chemicals were then used to coax these stem cells into becoming four types of cell found in the earliest stages of the human embryo:
- epiblast cells, which become the embryo proper (or fetus)
- trophoblast cells, which become the placenta
- hypoblast cells, which become the supportive yolk sac
- extraembryonic mesoderm cells
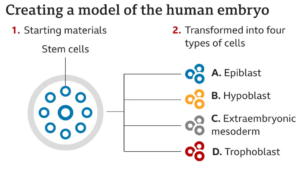
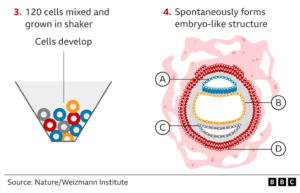
About 1% of the mixture began the journey of spontaneously assembling themselves into a structure that resembles, but is not identical to, a human embryo.
"I give great credit to the cells - you have to bring the right mix and have the right environment and it just takes off," Prof Hanna says. "That's an amazing phenomenon."
The embryo models were allowed to grow and develop until they were comparable to an embryo 14 days after fertilization. In many countries, this is the legal cut-off for normal embryo research.
I can see the trophoblast, which would normally become the placenta, enveloping the embryo. And it includes the cavities - called lacuna - that fill with the mother's blood to transfer nutrients to the baby.
There is a yolk sac, which has some of the roles of the liver and kidneys, and a bilaminar embryonic disc - one of the key hallmarks of this stage of embryo development.
'Making sense'
The hope is embryo models can help scientists explain how different types of cell emerge, witness the earliest steps in building the body's organs or understand inherited or genetic diseases.
Already, this study shows other parts of the embryo will not form unless the early placenta cells can surround it.
There is even talk of improving in vitro fertilization (IVF) success rates by helping to understand why some embryos fail or using the models to test whether medicines are safe during pregnancy.
Prof Robin Lovell Badge, who researches embryo development at the Francis Crick Institute, tells me these embryo models "do look pretty good" and "do look pretty normal".
"I think it's good, I thinks it's done very well, it's all making sense and I'm pretty impressed with it," he says.
But the current 99% failure rate would need to be improved, he adds. It would be hard to understand what was going wrong in miscarriage or infertility if the model failed to assemble itself most of the time.
Legally distinct
The work also raises the question of whether embryo development could be mimicked past the 14-day stage.
This would not be illegal, even in the UK, as embryo models are legally distinct from embryos.
"Some will welcome this - but others won't like it," Prof Lovell-Badge says.
And the closer these models come to an actual embryo, the more ethical questions they raise.
They are not normal human embryos, they're embryo models, but they're very close to them.
"So should you regulate them in the same way as a normal human embryo or can you be a bit more relaxed about how they're treated?"
Prof Alfonso Martinez Arias, from the department of experimental and health sciences at Pompeu Fabra University, said it was "a most important piece of research".
"The work has, for the first time, achieved a faithful construction of the complete structure [of a human embryo] from stem cells" in the lab, "thus opening the door for studies of the events that lead to the formation of the human body plan," he said.
The researchers stress it would be unethical, illegal and actually impossible to achieve a pregnancy using these embryo models - assembling the 120 cells together goes beyond the point an embryo could successfully implant into the lining of the womb.
UNC Adams School of Dentistry Wants to Know What You Think About Dental Provider-Administered Vaccinations

The UNC Adams School of Dentistry (ASOD) invites you to participate in a survey-based research study titled, Assessing Views and Perceptions of Dental Provider Vaccination Administration in North Carolina. This project is being conducted by Dr. Mark Veazie, a pediatric dental resident at the ASOD.
The aim of this research study is to examine the views of physicians and pharmacists on dental providers being able to provide vaccinations in the state of North Carolina. Hearing the views of current vaccine administrators will help us better understand how dental providers fit into the vaccination landscape.
If you agree to participate, the survey will take approximately less than 5 minutes of your time. You survey responses will remain anonymous, unless you opt to participate in an additional voluntary interview after survey completion. If you are interested, you will have an opportunity to indicate so at the end of the survey. The optional interview will take approximately 30-40 minutes of your time. Your identity and responses during both the survey and interview will remain confidential. Should you have any questions about this project or your participation, please reach out to Dr. Veazie (832) 419-4922 or [email protected].
Thank you for considering participating in this research study! You have until September 30, 2023 to complete the sutdy.
To take this brief survey, please click the link here: https://unc.az1.qualtrics.com/jfe/form/SV_e2uumJkwmwm8j5A
On The Lighter Side - September 8, 2023 - Hopscotch, the Stones, the Blue Ridge Parkway, and Late Summer Concerts
Here are some things NCMS employees, members, and YOU are talking about this Labor Day Weekend!
Hopscotch Music Festival Takes Over Raleigh!

Hopscotch Music Festival is an annual three-day music festival in downtown Raleigh running this Thursday - Sunday. With more than 120 bands, Hopscotch is known for adventurous lineups, memorable performances, and a fan-friendly atmosphere. Passes are still available by clicking here.
They Still Can't Get No Satisfaction!

For the first time in nearly twenty years, the Rolling Stones will release a new original album next month. Ronnie Wood, Keith Richards, and Jagger announced their forthcoming album, Hackney Diamonds, in London along with their new song, “Angry.” At 76, 79, and 80, respectively, the Stones are rolling. Hackney Diamonds includes collaborations with Stevie Wonder and Lady Gaga.
The Calendar May Say Summer, But Thoughts of Fall Have Many Planning Road Trips!

CNN has named the Blue Ridge Parkway an American favorite road trip! It is made even more spectacular by a breathtaking display of fall colors. It’s home to Mother Nature’s longest-lasting show of fall foliage, and with thousands of feet in elevation, there is no shortage of scenic overlooks. Worried you’ll miss the leaves? Mount Mitchell and Grandfather Mountain change color in early October, while areas like Chimney Rock hold out until early November.
Lineup of Late Summer Concerts

TODAY
- Judah & the Lion, Greenfield Lake Amphitheater, Wilmington
- Yung Bleu, QC Sound Stage, Charlotte
TOMORROW
- Sam Hunt, Coastal Credit Union Music Pavilion, Raleigh
- Outlaw Music Festival, PNC Music Pavilion, Charlotte
- Ray LaMontagne, Harrah's Cherokee Center, Asheville
- Billy Ocean, Wilson Center, Wilmington
SUNDAY
- Bishop Briggs, The Fillmore, Charlotte
MONDAY
- Lil Baby, PNC Arena, Raleigh
- CeCe Winans, Bojangles Coliseum, Charlotte
- Travis Scott, Spectrum Center, Charlotte
WEDNESDAY
- Nick Carter, Wilson Center, Wilmington
THURSDAY
- Judy Collins, 18 Biltmore Ave., Asheville
If you have an event you would like added to On The Lighter Side, email Randy Aldridge at [email protected].
CDC Health Alert Network Advisory: Increased RSV Activity in Southeastern US. New Prevention Tools Available

The Centers for Disease Control and Prevention (CDC) is issuing this Health Alert Network (HAN) Health Advisory to notify clinicians and caregivers about increases in respiratory syncytial virus (RSV) activity across some parts of the Southeastern United States in recent weeks, suggesting a continued shift toward seasonal RSV trends observed prior to the COVID-19 pandemic. Historically, such regional increases have predicted the beginning of RSV season nationally, with increased RSV activity spreading north and west over the following 2–3 months. RSV can cause severe disease in infants, young children, and older adults.
In anticipation of the onset of the 2023-2024 RSV season, CDC encourages clinicians to prepare to implement new RSV prevention options. Monoclonal antibody products, including a new, long-acting product, nirsevimab (BeyfortusTM, Sanofi and AstraZeneca), are available to protect infants and some young children at higher risk for severe RSV disease. For all infants ages <8 months, and infants and children ages 8–19 months who are at increased risk of severe RSV, clinicians should start to offer nirsevimab when it becomes available (expected by early October).
Also, two new vaccines are available to protect older adults from severe RSV disease. For adults ages 60 years and older, clinicians should offer a single dose of an RSV vaccine, either RSVPreF3 (Arexvy, GSK) or RSVpreF (AbrysvoTM, Pfizer), based on shared clinical decision-making between the healthcare provider and the patient. Clinicians should also talk to their patients about other vaccines available this fall to help prevent respiratory infections. Clinicians should consider testing symptomatic patients with high-risk conditions for COVID-19, influenza, and RSV to inform treatment decisions. Healthcare personnel, childcare providers, and staff at long-term care facilities should stay home and not go to work when they have fever or symptoms of respiratory infection to reduce the spread of respiratory infections including RSV.
Background
RSV is an RNA virus, and transmission occurs primarily via respiratory droplets when a person coughs or sneezes, or through direct contact with a contaminated surface. Infants, young children, and older adults, especially those with chronic medical conditions, are at increased risk of severe disease from RSV infection. CDC estimates that every year RSV causes approximately 58,000–80,000 hospitalizations (1,2) and 100–300 deaths (3,4) in children ages <5 years, as well as 60,000–160,000 hospitalizations (5,6) and 6,000–10,000 deaths (3,4,7) among adults ages 65 years and older.
In the United States, the annual RSV season has historically started in the fall and peaked in winter. However, this pattern was disrupted during the COVID-19 pandemic, likely due to public health measures to reduce the spread of COVID-19 that also reduced the spread of RSV. RSV activity was limited between May 2020 and March 2021, followed by an atypical season with onset in May 2021 that peaked in July and August and continued through the end of 2021 (8). In 2022, RSV activity began in the summer, peaking across the United States in October and November, and rapidly declining by winter. Despite the disruptions in timing, RSV activity continued its geographic pattern of starting in Florida and the southeast before spreading to northern and western parts of the continental United States in 2021 and 2022.
In recent weeks, CDC has observed an increase in RSV activity in parts of the Southeastern United States. Nationally, the weekly percentage of positive detections reported to the National Respiratory and Enteric Virus Surveillance System (NREVSS), a national laboratory-based surveillance network, has remained below the season onset threshold of polymerase chain reaction (PCR) test positivity of 3.0% for 2 consecutive weeks. However, NREVSS data show increases in weekly PCR positivity above 3.0% in Florida beginning in the week ending July 22, 2023, and the 3-week moving average of PCR positivity has been greater than 5.0% for the past 4 weeks. More robust data are available through Florida’s sentinel surveillance, which also shows PCR positivity just under 5.0% for the most recent week. In Georgia, CDC has also observed an increase in rates of RSV-associated hospitalizations reported to RSV-NET, a population-based surveillance system. Among children ages <4 years, RSV-associated hospitalization rates increased from 2.0 hospitalizations per 100,000 population for the week ending August 5, 2023, to 7.0 hospitalizations per 100,000 population for the week ending August 19, 2023, with the majority occurring among infants ages <1 year. Due to reporting delays, surveillance data may be less complete in the 2 most recent weeks.
In 2023, new prevention tools for RSV have become available.
- Nirsevimab is a long-acting monoclonal antibody approved by the Food and Drug Administration (FDA) to protect infants and some young children at increased risk for severe RSV disease. Nirsevimab is safe and efficacious. In clinical trials, one dose of nirsevimab administered as an intramuscular injection protected infants for at least 5 months (the length of an average RSV season) and reduced the risk of severe RSV disease by about 80% (9). The incidence of serious adverse events was not increased among nirsevimab recipients compared with placebo recipients in the clinical trials (9).
- RSVPreF3 and RSVpreF are recombinant protein vaccines that are both approved by FDA for use in adults ages 60 years and older to prevent RSV-associated lower respiratory tract disease. During the first RSV season after vaccination, each vaccine was more than 80% efficacious in preventing RSV-associated lower respiratory tract disease (10). A small number of participants in clinical trials (6 of 38,177 total participants aged ≥60 years who received either vaccine) developed inflammatory neurologic events within 6 weeks after RSV vaccination, but it was unclear whether these events were related to RSV vaccination (10).
On August 21, 2023, FDA approved the RSVpreF vaccine (AbrysvoTM, Pfizer) for use in pregnant people during weeks 32 through 36 of gestation for the prevention of RSV-associated lower respiratory tract disease in infants from birth through 6 months of age. CDC’s Advisory Committee on Immunization Practices (ACIP) will consider the evidence for a policy recommendation about RSV vaccination in this population in the future. CDC and FDA will continue to monitor the safety and effectiveness of RSV vaccines and nirsevimab, review data as collected, keep the public informed of findings, and use data to make recommendations – consistent with standard practices for all immunization products.
Recommendations for Clinicians
A clinician’s recommendation is one of the most important factors in whether patients choose to accept a prevention product or vaccine. As we head into respiratory virus season this fall, it’s important to understand new prevention tools, recommend them to patients who could benefit, and use them effectively to prevent severe RSV disease.
-
- Monoclonal antibodies for infants and young children: Clinicians should start to offer nirsevimab when it becomes available (expected by early October) for all infants ages <8 months, and for infants and for children ages 8–19 months who are at increased risk for severe RSV disease (see specific recommendations below). Nirsevimab may not be readily available in all birthing hospitals or primary care settings this RSV season. RSV seasonality in tropical climates and Alaska may be less predictable and clinicians in these areas should consult state, local, or territorial guidance on timing of nirsevimab administration.
CDC recommends nirsevimab for the following groups:
-
-
- All infants ages <8 months born during or entering their first RSV season should receive 1 dose of nirsevimab.
- Infants born shortly before or during the RSV season should receive nirsevimab within their first week of life.
- Infants not born shortly before or during this RSV season should receive nirsevimab shortly before the start of their first RSV season or as early as feasible during the season.
- Infants and children ages 8–19 months who are at increased risk for severe RSV disease, such as those who are severely immunocompromised, should receive 1 dose of nirsevimab shortly before entering or during their second RSV season.
- All infants ages <8 months born during or entering their first RSV season should receive 1 dose of nirsevimab.
-
Dosage of nirsevimab:
All infants ages <8 months:
-
-
- 50 mg dose administered as a single injection for infants weighing <5 kg [<11 lb]
- 100 mg dose administered as a single injection for infants weighing ≥5 kg [≥ 11 lb]
-
Infants and children ages 8–19 months who are at increased risk for severe RSV disease:
-
-
- 200 mg dose administered as two 100 mg injections
-
Another prevention product, palivizumab (Synagis®, SobiTM), is available for children <24 months of age with certain conditions that place them at increased risk for severe RSV disease. Where nirsevimab is not available during this RSV season, the American Academy of Pediatrics (AAP) recommends that eligible infants and older babies should continue to receive palivizumab until nirsevimab becomes available.
- RSV vaccines for older adults: CDC recommends that adults ages 60 years and older may receive a single dose of RSV vaccine (either product) using shared clinical decision-making to prevent RSV-associated lower respiratory tract disease. Clinicians should discuss RSV vaccination with adults ages 60 years and older. Vaccination should be prioritized in adults ages 60 years and older who are most likely to benefit, including those with certain chronic medical conditions associated with increased risk of severe RSV disease, such as heart disease (e.g., heart failure, coronary artery disease), lung disease (e.g., chronic obstructive pulmonary disease [COPD], asthma), and immunocompromising conditions. Adults with advanced age and those living in nursing homes or other long-term care facilities are also at increased risk of severe RSV disease and may benefit from RSV vaccination.
- Healthcare providers should also talk to their patients about other vaccines (e.g., COVID-19, influenza) available this fall to help prevent respiratory illness.
- Healthcare providers can co-administer the vaccines for which a patient is eligible in the same visit, including RSV, COVID-19, and influenza vaccines. When deciding whether to co-administer other vaccines with RSV vaccine at the same visit, providers can consider whether the patient is up to date with currently recommended vaccines, the feasibility of their returning for additional vaccine doses, their risk of acquiring vaccine-preventable disease, the vaccine reactogenicity profiles, and patient preferences.
- Clinicians should consider testing patients with symptoms of acute respiratory illness and high-risk conditions for respiratory pathogens to inform patient management. Although treatment for RSV is supportive, diagnostic testing can help identify patients who might benefit from medications to treat other respiratory pathogens, such as COVID-19 and influenza. Real-time reverse transcription-polymerase chain reaction (rRT-PCR) is the preferred method for testing for respiratory viruses.
- Healthcare personnel, childcare providers, and staff of long-term care facilities should stay home and not go to work when they have fever or symptoms of respiratory infection.
Recommendations for the Public
- Expectant parents, parents of infants under the age of 8 months, and parents with older babies (through age 19 months) at increased risk of severe RSV disease should talk with their healthcare providers about using monoclonal (preventive) antibodies to protect against RSV this season. Infants under the age of 8 months should receive preventive antibodies to protect against RSV this season.
- Adults ages 60 years and older should talk to their healthcare provider about whether RSV vaccination is appropriate for them.
- Stay home and away from others when you are sick. If you are at increased risk of severe illness, contact your healthcare provider to see if you would benefit from early diagnostic testing. Treatments for influenza and COVID-19 are available that, if given within days of symptoms starting, can reduce your risk of hospitalization and death.
For More Information
- CDC – RSV Information for Healthcare Providers
- CDC – RSV National Trends – NREVSS
- CDC – RSV Surveillance and Research
- CDC – RSV Symptoms and Care
- CDC – Preventing RSV (Respiratory Syncytial Virus)
- RSV Vaccination: What Older Adults 60 Years of Age and Over Should Know | CDC
- Healthcare Providers: RSV Vaccination for Adults 60 Years of Age and Over | CDC
- Shared Clinical Decision-making: RSV Vaccination for Adults 60 Years and Older
- Frequently Asked Questions About RSV Vaccine for Adults | CDC
Register Now! 35th Fall Foliage Cancer Conference is October 20, 2023
35th Annual Fall Foliage Cancer Conference Update on Breast Cancer
Omni Grove Park Inn Asheville
The 35th Annual Fall Foliage Cancer Conference – Update on Breast Cancer in Asheville will be held on October 20-21, 2023 at the Omni Grove Park Inn Resort & Spa. The event has been approved for 10.0 AMA PRA Category 1 Credit.
Accreditation Statement: This live activity has been planned and implemented in accordance with the accreditation requirements and policies of the Arizona Medical Association (ArMA) through the joint providership of MORE Foundation and Community Cancer Education, Inc. MORE Foundation is accredited by ArMA to provide continuing medical education for physicians.
Credit Statement: MORE Foundation designates this live activity for a maximum of 10.0 AMA PRA Category 1 Credits™. Physicians should only claim credit commensurate
with the extent of their participation in the activity.
ASRT: The American Society of Radiologic Technologists has approved this activity for Category A credits. You must attend all day to receive credit. Friday 4.75 Saturday 7.00
Conference Location and Accommodations:
The conference will be held in the Sammons Wing at Asheville’s historic Omni Grove Park Inn on Friday, October 20th and Saturday October 21st, 2023. Those wishing overnight accommodations are asked to make their own reservations with a hotel of their choice.
Learn more about the event and register here.
New Study: Eye-Tracking Tool May Help Diagnose Autism Quickly and Accurately

(Jacqueline Howard and Deidre McPhillips, CNN) -- Most families of children with autism may face long wait times to diagnose their child with the disorder, and once a diagnosis is made, it sometimes may not be definitive. Now, two studies released Tuesday suggest that a recently developed eye-tracking tool could help clinicians diagnose children as young as 16 months with autism – and with more certainty.
“This is not a tool to replace expert clinicians,” said Warren Jones, director of research at the Marcus Autism Center at Children’s Healthcare of Atlanta and Nien Distinguished Chair in Autism at Emory University School of Medicine, who was an author on both studies.
Rather, he said, the hope with this eye-tracking technology is that “by providing objective measurements that objectively measure the same thing in each child,” it can help inform the diagnostic process.
The tool, called EarliPoint Evaluation, is cleared by the US Food and Drug Administration to help clinicians diagnose and assess autism, according to the researchers.
Traditionally, children are diagnosed with autism based on a clinician’s assessment of their developmental history, behaviors and parents’ reports. Evaluations can take hours, and some subtle behaviors associated with autism may be missed, especially among younger children.
“Typically, the way we diagnose autism is by rating our impressions,” said Whitney Guthrie, a clinical psychologist and scientist at the Children’s Hospital of Philadelphia’s Center for Autism Research. She was not involved in the new studies, but her research focuses on early diagnosis of autism.
It will always be important to take into account what the family and specialist observe in the child, but families may reflect on a child’s behaviors differently based on their unique backgrounds or experiences, Guthrie said.
“Some of these new technologies are more objective. They don’t rely on humans who are imperfect by nature,” she said. “They’re also potentially more scalable and feasible.”
How tracking eyes may help
The technology works by tracking the eye movements of children as they watch videos of other children’s social interactions.
A child without autism may focus their attention on the hand gestures of one child in the video who’s pointing toward something for another child in the video to look at. That child also may look at the face of another child who looks sad or smiling. But a child with autism would not pay attention to the hand gestures or facial expressions at all, and this can be identified in their eye movements.
“We use scenes like that to test whether or not children are paying attention to the information that we expect typically developing children of that same age to,” Jones said.
In one of the new studies, published in the medical journal JAMA, 475 children ages 16 to 30 months were assessed for autism at six specialty clinics in the United States. The children were enrolled in the study between April 2018 and May 2019, and the eye-tracking tool was included in the assessments.
The researchers found that, relative to expert clinical diagnosis alone, measurements of the children’s eye-tracking and social engagements with the videos had a 71% sensitivity, meaning they helped accurately diagnosis autism 71% of the time, and 80.7% specificity, meaning they helped designate a child without autism about 80% of the time.
Among the children, 335 had an autism diagnosis that their clinicians were “certain” of without using the eye-tracking tool. When the eye-tracking tool was used for just this group, the researchers found that it showed a sensitivity of 78%, and specificity was 85.4% when expert clinicians were certain of their diagnoses.
The findings suggest that using measurements of how children look at and learn from the social interactions in the videos may offer a biomarker for diagnosing autism, helping shorten the time needed to make a diagnosis and accelerate the child’s treatment.
The other study, published in JAMA Network Open, found that among 719 children ages 16 to 30 months, eye-tracking-based measurements had a sensitivity of 81.9% and specificity of 89.9%. In another group of 370 children, ages 16 to 45 months, the eye-tracking measurements had a sensitivity of 80.6% and specificity of 82.3%.
In that study, 14 video scenes were presented to the children, each about 54 seconds long, on average.
Overall, the researchers told CNN, the data shows the technology to have about 80% sensitivity and specificity.
In the studies, the eye-tracking measurements – which collected data at 120 times per second and within 12 minutes of video watching – predicted expert clinician assessments “with a high degree of accuracy,” according to a news release, and were consistent with gold standard expert clinical diagnoses.
“To me, there is no other return of investment for what we do in science and in public health than giving access to families to early diagnosis that will make possible early intervention and support that are going to optimize the outcomes of the children for the rest of their lives,” said Ami Klin, director of the Marcus Autism Center and division chief of autism and developmental disabilities at the Emory University School of Medicine, who was an author of both studies.
“In our health care system, those families are thinking about the concerns that they have about their children – and they go to bed every night for months, if not years, waiting for an answer, knowing very well that the earlier they get to that answer the earlier their child is going to benefit from the kinds of treatments that can improve their lives,” Klin said. “For the first time, we have an objective biomarker-based tool that can increase access. And my greatest hope is that this is going to be one of the tools that we can use to decrease the health care disparities that affect minority, low-income and rural families.”
‘The equity issue … is very significant’
Medical experts have long known that autism evaluation, and subsequent diagnosis, have been “really, really suboptimal” for children of color, as well as those living in rural and underserved communities, including urban areas, said Dr. Kristin Sohl, professor of pediatrics at the University of Missouri School of Medicine and chair of the autism subcommittee for the American Academy of Pediatrics.
Children in those groups disproportionately are diagnosed with autism later than their non-minority or non-rural peers.
“The equity issue in autism is very significant,” Sohl said.
“When you have a little child who is showing characteristics of autism very early but they are not able to even be remotely identified – meaning no one has even thought about it until they’re in kindergarten – that is a huge disadvantage for that individual child,” said Sohl, who was not involved in the new research.
Diagnostic tools like eye-tracking technology and other clinician resources may help reduce those disparities – and improve rates of early diagnosis overall – by enabling specialists to build more capacity into their practices and by helping broaden the pool of doctors who feel equipped to diagnose autism.
“There are many, many children who are very well-served by their community clinicians. And yet we’ve got to help our primary care clinicians have a much better appreciation for autism,” Sohl said. “Diagnostic age is often a reflection of the time that a parent has waited.”
Studies from the US Centers for Disease Control and Prevention have found that early detection of autism in children has improved, but disparities remain in practices to identify and diagnose the condition.
“Devices like this can be so helpful in the hands of a skilled generalist, because they can take that piece of information and use it to look at the other data that they have and then say, ‘Yes, I’m confident that this is autism,’ or ‘No, this isn’t, and here’s what I need to do,’” Sohl said.
But more work is needed before an eye-tracking test becomes commonplace, Geraldine Dawson of the Duke Center for Autism and Brain Development in North Carolina wrote in an editorial published Tuesday alongside the new studies.
“There remains work to be done before an eye-tracking test is used in clinical practice. Demonstrating that an eye-tracking test improves diagnostic certainty would require following children whose diagnosis was uncertain longitudinally to determine whether the test improves prediction of a later definitive autism diagnosis,” she wrote.
“The intended use of the eye-tracking test is to aid clinicians in making an autism diagnosis in young children who have been referred to a specialty clinic for evaluation,” Dawson wrote. “By integrating multiple sources of information— including the eye-tracking test, parent report, and clinical observations—the accuracy, certainty, and efficiency of autism diagnostic assessment could potentially be improved, resulting in fewer missed cases and allowing more children to receive empirically validated early therapies from which they could benefit.”
ADDITIONAL READING
- Why More Girls Are Being Diagnosed With Autism
- 8 Often-Overlooked Signs of Autism Most Common in Women
- Why Autism in Black and Latino Children is Often Overlooked
CCH and CCHN Need to Hear From YOU before LEAD Conference

At the 2023 NCMS LEAD Conference and Golden Stethoscope Awards Gala, the only provider-led health plan in NC Medicaid, Carolina Complete Health (CCH) and the NCMS-owned company that works exclusively with CCH, Carolina Complete Health Network (CCHN), will hold a session to hear from clinicians who see patients with Medicaid coverage.
We want to hear from you in advance, about the issues you need top priority attention to make Medicaid more efficient and to improve results for those with Medicaid coverage.
Please complete this FEEDBACK FORM to let us know what issues you think should be addressed. Our plan is to identify groups of clinicians to address each major issue and develop ideas for implementation.
Thanks in advance for your participation!
If you still need to register for LEAD please click here.
NCDHHS Immunization Provider Webinar Scheduled

The North Carolina Department of Health and Human Services is hosting a Immunization Provider Webinar on fall vaccines tomorrow, September 6, from 12:30 - 1pm ET.
Here is what you need to know:
Immunization Provider Webinar
Wednesday, September 6th from 12:30-1pm ET
Join ZoomGov Meeting
https://www.zoomgov.com/j/1614064331?pwd=RTUxWWhvWTBGbzdhY2tlY1hvY2JVdz09
Meeting ID: 161 406 4331
Passcode: 906994
One tap mobile
+16692545252,,1614064331# US (San Jose)
+16468287666,,1614064331# US (New York)
Dial by your location
+1 669 254 5252 US (San Jose)
+1 646 828 7666 US (New York)
+1 669 216 1590 US (San Jose)
+1 551 285 1373 US
Meeting ID: 161 406 4331
Find your local number: https://www.zoomgov.com/u/abVG7wmcav
Duke School of Medicine Brings Leaders From Around the World Together to Talk Mental Health

From Left: David Johnson, a deputy assistant secretary of the U.S. Department of Health and Human Services; Kody Kinsley, North Carolina Secretary of Health and Human Services; Ling-Fong Lee, Senior Counselor to the Minister of Taiwan Ministry of Health and Welfare; Jilma Meneses, secretary of the Washington Department of Social and Health Services; and Chris Jones, commissioner of the North Dakota Department of Health & Human Services.
(Duke University School of Medicine, Shantell M. Kirkendoll) -- A recent health forum organized by the Duke University Policy and Organizational Management Program (POMP) brought together health and social services leaders from across the globe to the Duke University School of Medicine to discuss mental health.
The forum titled “Rebuilding Emotional Resilience and Mental Well-Being,” featured presentations by Kody Kinsley, North Carolina Secretary of Health and Human Services; Ling-Fong Lee, Senior Counselor to the Minister of Taiwan Ministry of Health and Welfare; Jilma Meneses, secretary of the Washington Department of Social and Health Services; and Chris Jones, commissioner of the North Dakota Department of Health & Human Services.
Each shared their unique regional challenges and innovative solutions to address the issue, which includes a shortage of mental health providers; rising rates of depression, anxiety, and opioid use; and the need for a more community-based approach to care.
But one of the key themes of the event was the need to reach people where they are.
“The solution resides in proximity to the voices we serve,” said event moderator David Johnson, a deputy assistant secretary of the U.S. Department of Health and Human Services. “Reaching the heart of our communities is essential.”
POMP, which is affiliated with the Duke University Center for International and Global Studies, coordinated the Aug. 28 health forum to discuss policies affecting issues ranging from infectious disease to long-term care. The mental health panel discussion was the highlight of the meeting, as it focused on a topic recognized as the potential next global pandemic.
Among experts, there was an emphasis on collective action, using digital tools to bridge gaps, and fostering an environment where every individual feels heard and supported.
Mental health as public health priority
A unifying message that emerged throughout the discussions was shifting mental health from the peripheries of health care to its core.
“Mental health has long been seen as a secondary issue,” Kinsley said. “Addressing mental health concerns directly correlates with a decrease in costs associated with other chronic diseases.”
North Carolina’s deeply underfunded mental health system is confronting an urgent need for reform.

Kinsley shared ambitious plans for the state, focusing on crisis prevention and strengthening the mental health infrastructure within schools and the criminal justice system.
The state also recently expanded its partnership with Duke Health to support a psychiatric access line that helps health care providers and educators respond to behavioral health issues.
Still there is a pressing need to move mental health from a secluded tertiary issue to the forefront of public health agendas. “We really need a public health response to behavioral health,” Kinsley said.
Jones pivoted the conversation towards broader health concerns, emphasizing the interconnectedness of behavioral, economic, and physical health.
He urged investment in robust community-driven support systems, revealing that North Dakota had significantly reduced its number of institutionalized children. “Out of sight, out of mind is never the solution,” he said.
Silent crisis unfolds
While there are challenges in addressing mental health, another crisis unfolding is opioid use disorder (OUD), specifically fentanyl use, said Meneses, who advocated for a national campaign to discuss its profound impact on communities.
One community particularly affected by OUD is the American Indian and Alaska Native community. Recent data reveals that among AIAN Medicaid beneficiaries aged 18-64, 15% were diagnosed with OUD – a rate more than double the overall substance use disorder prevalence among Medicaid beneficiaries.
This disturbing trend also resonates with higher rates of homelessness and arrest rates.
“However, every challenge presents an opportunity,” she said. “Supporting resilience and recovery is paramount. It’s all about collaboration and alignment.”
The focus, therefore, shifts to various agencies within Washington working in tandem from the Department of Social and Health Services to the Department of Children, Youth and Families. Together they provide a continuum of care, ensuring every individual, no matter their challenges, gets the support they deserve.
A community-integrated approach to care is not just preferable but essential for mental health advancement, leaders concluded.
Taiwan embraces technology
In Taiwan, community mental health centers collaborate with schools. But the collaboration doesn’t stop at current students. Recognizing the distinct challenges faced by those who have recently graduated or discontinued their education, Taiwan is also rolling out a unique support program for young adults.
They are harnessing technology to amplify their reach: a simple scan of a QR code on posters signaling ‘Let us listen to you,’ instantly guides individuals to nearby mental health centers and clinics.
“Every government globally shares a common responsibility – to empower its citizens to face life’s challenges with increased confidence and resilience,” said Lee, the senior counselor. “We’re proud to be playing a part in this global endeavor.”
International AIDS Conference: NC Researchers See Pathway to AIDS-Free World

(NC Health News, Lee Storrow) -- Across the globe, scientists, doctors, public health practitioners and community-centered groups are continuing their work to combat the transmission of HIV.
And they’re turning the tide against the disease.
Australia has made historic advancements in this area, and the country is on the verge of eliminating HIV, with new diagnoses of HIV among gay and bisexual men in Australia falling by 57 percent over the past decade. In inner-city Sydney, that number has dropped by 88 percent.
“These encouraging findings from inner city Sydney show just how far we have come since the early days of the AIDS pandemic before we had effective testing, treatment or prevention tools,” Sharon Lewin, IAS President, IAS 2023 International Chair and infectious disease expert at the University of Melbourne in Australia, said in a news release.
This year’s International Conference on HIV Science was in Brisbane, Australia, at the end of July. The location is fitting, given that the country is on track to achieve international 95-95-95 targets: 95 percent of all people living with HIV knowing their status, 95 percent of people diagnosed with HIV receiving sustained antiretroviral therapy, and 95 percent of all people receiving that therapy achieving viral suppression by a 2025 benchmark.
Over the four days of the conference, which is hosted by the International AIDS Society, more than 5,000 representatives from more than 100 countries gathered to share lessons learned, scientific breakthroughs and areas for improvement around the collective efforts to mitigate the transmission of HIV and other communicable diseases.
First Lady Tests Positive for Covid-19 as World Faces Fourth Virus Season Since Pandemic
First lady Jill Biden tested positive for Covid-19 Monday, President Joe Biden tested negative, per the White House. Her diagnosis comes amid renewed attention to Covid-19 as the world approaches the fourth virus season since the height of the pandemic.
It also comes as concern grows about the Covid-19 variants EG.5 and BA.2.86. In August, EG.5 became the dominant variant in the United States, and the World Health Organization classified it as a “variant of interest,” meaning it has genetic changes that give it an advantage and its prevalence is growing.
BA.2.86 is much less widespread, making up only a tiny fraction of cases, but scientists are alarmed by how many mutations it carries.
EG.5
While severe illness in older adults and people with underlying conditions is always a concern, as is long Covid in anyone who gets infected, experts say EG.5 does not pose a substantial threat — or at least no more of one than any of the other major variants currently circulating.
“It’s a concern that it’s increasing, but it doesn’t look like something that’s vastly different from what’s already been circulating in the U.S. for the past three to four months,” said Andrew Pekosz, a professor of molecular microbiology and immunology at Johns Hopkins University Bloomberg School of Public Health. “So I think that’s what tempers my concern about this variant, at this point in time.”
Even the W.H.O. stated in its announcement that, based on the available evidence, “the public health risk posed by EG.5 is evaluated as low at the global level.”
The variant was identified in China in February 2023 and was first detected in the United States in April. It is a descendant of the Omicron variant XBB.1.9.2 and has one notable mutation that helps it to evade antibodies developed by the immune system in response to earlier variants and vaccines. That advantage may be why EG.5 has become the dominant strain worldwide, and it could be one reason Covid cases have been rising again.
That mutation “may mean that more people are susceptible because the virus can escape a little bit more of that immunity,” Dr. Pekosz said.
But EG.5, which has also been called Eris, does not appear to have any new capacities when it comes to its contagiousness, its symptoms or its likelihood of causing severe illness. Diagnostic tests and treatments such as Paxlovid continue to be effective against it, Dr. Pekosz said.
Dr. Eric Topol, executive vice president of Scripps Research in La Jolla, Calif., said he isn’t overly worried about the variant; however, he would feel better if the new vaccine formulation, which is expected to be rolled out in the fall, was already available. The updated booster was developed based on another variant that is genetically similar to EG.5. It is expected to provide better protection against EG.5 than last year’s shot, which targeted the original coronavirus strain and a much earlier Omicron variant that is only distantly related.
“My main concern is for the people at high risk,” Dr. Topol said. “The vaccines that they’ve had are too far removed from where the virus is right now and where it’s going.”
BA.2.86
The other new variant that scientists are watching closely is BA.2.86, nicknamed Pirola. Descended from a different Omicron variant, BA.2.86 has been definitively tied to 29 cases of Covid across four continents, but experts suspect it is more widespread.
Scientists are particularly concerned about this variant because of the number of mutations it carries. Many of them are in the spike protein, which is what the virus uses to infect human cells and what our immune systems use to identify it. According to Jesse Bloom, a professor at the Fred Hutchinson Cancer Center who specializes in virus evolution, the mutations in BA.2.86 represent “an evolutionary jump similar in size” to the changes in the first Omicron variant compared to the original coronavirus strain.
Data released this week on X (formerly Twitter) by scientists in China showed that BA.2.86 is so different from previous versions of the virus that it easily escapes antibodies produced in response to earlier infections — even more than EG.5 does. The data (which have not yet been published or peer-reviewed) suggest that the updated vaccine will be less effective against it, too.
CDC data also shows a slight increase in hospital admissions, emergency department visits and positive Covid-19 tests — but not nearly as high as in past summers.
(Dana G. Smith, New York Times, and Alexandra Meeks, CNN)
NC Stroke Advisory Council Releases Survey Results on Scope of Services in State

North Carolina’s Stroke Advisory Council has published the results of its survey to gain understanding of the scope of stroke services provided by all North Carolina hospitals. An article on the results has been published in the Journal of Stroke and Cerebrovascular Diseases - Statewide Availability of Acute Stroke Treatment, Services, and Programs: A Survey of North Carolina Hospitals.
In addition to assessing stroke treatment in the state’s hospitals, the Council also examined differences in stroke care capabilities between urban, suburban, and rural hospitals and trends over the past 2 decades. The survey was conducted over the October 2020-April 2021 period and results were compared to survey results in 1998, 2003 and 2008.
The survey had a 100% response rate from all 111 hospitals contacted. Notable results include:
- Among 108 hospitals providing acute stroke care, 12 (11%) were Comprehensive Stroke Centers or Thrombectomy-Capable Stroke Centers
- All Comprehensive Stroke Centers or Thrombectomy-Capable Stroke Centers responding were located in urban or suburban areas
- 38% of urban/suburban hospitals were non-certified
- 48% of rural hospitals were non-certified
- Non-contrast computed tomography (CT), CT angiography, and alteplase treatment were widely available (100%, 95%, and 99%, respectively)
- Endovascular thrombectomy was solely available in urban/suburban hospitals (29%)
- Of non-tertiary hospitals, 81% were using telestroke for treatment and transfer decisions
- Compared to prior survey results, the availability of CT angiography (76% in 2008 to 95% in 2020-2021), alteplase treatment (69% in 2008 to 99% in 2020-2021), and acute stroke clinical pathways (47% in 2008 to 90% in 2020-2021) increased
- Having an in-house neurologist on staff dropped from approximately 55% in prior surveys to 21%
The study concludes that rural North Carolina hospitals are less likely to have advanced diagnostic imaging and treatment capabilities for acute stroke, and identifies the need for in-house neurologists and use of telestroke services need to be points of emphasis going forward.
NCMS President Apolinario, Past President Utecht Going OVER THE EDGE for Special Olympics!
The NCMS Over the Edge Team Needs Your Donation!

NCMS current President Dr. Arthur Apolinario and former president Dr. Michael Utecht are going Over the Edge to raise money for the 2023 NC Special Olympics. They will be rappelling 30 stories down the 150 Fayetteville St. building in downtown Raleigh on September 30. One other NCMS staff member will be joining them. That fearless person will be announced later this month!
In an article for The Sampson Independent, Dr. Apolinario says "with your help I can take fundraising to new heights in this experience of a lifetime. Every dollar raised will help support nearly 40,000 Special Olympics athletes across the state!"
“I’m really excited about this and really nervous about it, because I’ve never done anything like this in my life,” Apolinario said, “but, it’s for a really good cause, Special Olympics. “One of the benefits of me being president of the North Carolina Medical Society, is they’re huge supporters. So that’s what’s affording me the ability to do this experience.”

To read the full article on Dr. Art click here.
The North Carolina Medical Society team is currently in 4th place! You help us get to first by donating here.
On The Lighter Side – September 1, 2023, Labor Day Weekend Means Apples, Jazz, Tennis, Band Battles, and Concerts!
Here are some things NCMS employees, members, and YOU are talking about this Labor Day Weekend!
John Coltraine International Jazz & Blues Festival

Check out Keb' Mo', Dave Koz, and Samara Joy and others Saturday and Sunday in Highpoint. Since its inception, the John Coltrane International Jazz and Blues Festival has succeeded in bringing the very top names in jazz, paid homage to the blues, and celebrated the life and musical legacy of the jazz genres greatest artists. The festival attracts a growing audience and enjoys a burgeoning reputation as the destination for Labor Day weekend. For all you need to know click here.
2023 Charlotte HBCU Labor Day Classic: Battle of the Bands

The perfect safe event for the entire family, food trucks, vendors and more. Come see 9 HBCU Bands put on halftime shows like never before. Check it out Sunday at 3pm at American Legion Memorial Stadium in Charlotte. For tickets click here.
NC Apple Festival in Hendersonville
The Apple Festival is held on Labor Day Weekend each year (Friday through Monday) to recognize the importance of the apple and the apple industry to Henderson County and North Carolina. All you need to know is here.
It's time once again for the Chaos Slam! US Open keeping everyone guessing again this year!

Djokovic, Gauff, Alcaraz, Swiatek, Medvedev, Pegula, Jabeur, Tiafoe, and more are still looking to the title as the US Open continues (it ends September 10). Americans will be glued to their TVs this weekend to see all the action. Click here to find out all you need.
The unofficial end of summer weekend means lots of concerts!

TONIGHT
- ZZ Top, PNC Music Pavilion, Charlotte
- Moon Taxi, Greenfield Lake Amphitheater, Wilmington
- Band of OZ, 97 Pinebridge, Spruce Pine
SATURDAY
- Late Night Music Fest, Greensboro Coliseum, Greensboro
- Nickelback, Veterans United Home Loans Stadium, Virginia Beach, VA
- Scream Tour, Koka Booth Amphitheatre, Cary
- Dave Koz, John Coltrane Statue, High Point
- 3 Doors Down, Skyla Credit Union Amphitheater, Charlotte
SUNDAY
- 5 Seconds of Summer, Red Hat Amphitheater, Raleigh
- Billie Eilish, Coastal Credit Union Midtown Park, Raleigh
- Michael McDonald, Enmarket Arena, Savannah, GA
- Duke Symphony Orchestra Pops Concert, Duke University, Durham
- Emmylou Harris, Earl Scruggs Center, Shelby
If you have an event you would like added to On The Lighter Side, email Randy Aldridge at [email protected].
New Study: Patients Have Better Outcomes with Female Surgeons

Differences in technique, speed and risk-taking suggested as reasons for surgery by men leading to more problems
(The Guardian, Ian Sample) -- People who are operated on by female surgeons are less likely to experience complications and need follow-up care than when males wield the scalpel, according to two major studies that suggest male surgeons have important lessons to learn.
Doctors in Canada and Sweden reviewed more than 1m patient records from two separate medical registers and found that patients seen by female surgeons had significantly better outcomes with fewer problems in the months after the operation.
The researchers are investigating potential reasons for the differences, but the records suggest that female surgeons tend to operate more slowly and may achieve better results by taking their time in the operating theatre.
Dr Christopher Wallis, who led one of the studies at Mount Sinai hospital in Toronto, said the findings should prompt male surgeons to reflect on their approach to surgery and learn from female colleagues for the benefit of their patients. “As a male surgeon, I think these data should cause me and my colleagues to pause and consider why this may be,” he said.
Wallis’s team looked at medical complications, readmission to hospital, and death rates after surgery in nearly 1.2 million Ontario patients between 2007 and 2019. The records included 25 different surgical procedures on the heart, brain, bones, organs and blood vessels.
The analysis, reported in Jama Surgery, showed that 90 days after an operation, 13.9% of patients treated by a male surgeon had “adverse post-operative events”, a catch-all term that includes death and medical complications ranging from problems that require further surgery to major infections, heart attacks and strokes. The equivalent figure for patients seen by female surgeons was 12.5%.
Patients seen by female surgeons fared better one year after surgery too, with 20.7% having an adverse postoperative event, compared with 25% of those seen by male surgeons. When the doctors looked purely at deaths post-surgery, the difference was even starker: patients treated by male surgeons were 25% more likely to die one year after surgery than those treated by female surgeons.
A second study of 150,000 patients in Sweden, also published in Jama Surgery, paints a similar picture. Dr My Blohm and colleagues at the Karolinska Institute in Stockholm reviewed patient outcomes after surgery to remove the gallbladder. They found that patients treated by female surgeons suffered fewer complications and had shorter hospital stays than those treated by men. The female surgeons operated more slowly than their male colleagues and were less likely to switch from keyhole to open surgery during an operation.
Blohm said that, as with all observational studies, the results should be treated with caution, but the findings suggest that surgical technique and risk-taking might explain some of the differences observed. “In some countries there is a general belief that male surgeons are superior to female surgeons,” she said. “Interestingly, most previously published studies indicate that female surgeons are at least as good as male surgeons, or as in this case even slightly better.”
Wallis said there were “numerous lessons” to learn. “Men and women differ in how they practice medicine. Embracing or adopting some practices that are more common among female physicians is likely to improve outcomes for my patients,” he said. “Since undertaking this work, I have certainly done this personally and would encourage my colleagues to do the same: use this as a moment for introspection.”
Beyond attracting more women to surgery, Wallis said there was a need to “evolve” surgery to ensure it better retained women and promoted them to positions of influence. “There is a wealth of data that we have a so-called leaky pipeline with diminishing numbers of women in senior positions,” he said.
In an accompanying editorial, Prof Martin Almquist at Skåne University hospital in Sweden writes: “The fact that female surgeons had operations with fewer complications but longer operation times suggests that the Navy Seal mantra ‘slow is smooth, and smooth is fast’ also applies to surgery.”
Tim Mitchell, President of the Royal College of Surgeons of England, said the findings added to a growing literature pointing to differences in patient outcomes for male and female surgeons.
“This association is interesting and important,” he said. “However, association is not causation, and one possible explanation may have to do with case complexity. The authors tried to take the case mix into account by adjusting for confounders, but residual confounding factors cannot be ruled out. I agree that the ideal of the surgeon as the ‘lonesome cowboy’ belongs to an era long gone.”