North Carolina Events Recognize World AIDS Day
World AIDS Day is a global movement to unite people in the fight against HIV and AIDS. Since 1988, communities have stood together on World AIDS Day to show strength and solidarity against HIV stigma and to remember lives lost.
World AIDS Day exists to shine a light on the real experiences of people living with HIV today, while celebrating the strength, resilience and diversity of the communities most affected. It is a moment to inspire the leadership needed to create a future where HIV doesn’t stand in the way of anyone’s life.
This year’s theme for World AIDS Day is “World AIDS Day 35: Remember and Commit.” This annual event serves as a reminder of the global struggle to end HIV-related stigma, an opportunity to honor those we have lost, and a rallying cry to commit to working toward a day when HIV is no longer a public health threat.
This year marks the 35th commemoration of this important day. Over the past 35 years, there has been significant progress in addressing HIV and AIDS thanks to advancements in medical research, increased access to treatment and prevention, and a broader understanding of the virus.
What's the story behind the red ribbon?
The red ribbon is the universal symbol of awareness and support for people living with HIV. It was first devised in 1991, when twelve artists met to discuss a new project for Visual AIDS, a New York HIV-awareness arts organization.
It was there that they came up with what would become one of the most recognized symbols of the decade: the red ribbon, worn to signify awareness and support for people living with HIV. The artists wanted to create a visual expression of compassion for people living with HIV and chose red for its boldness, and for its symbolic associations with passion, the heart and love.
You can purchase red ribbons, or red ribbons brooches from National AIDS Trust’s shop.
Here are some events happening across North Carolina
Check for local events where you live as well.
Walking faster linked to ‘significantly lower risk’ of developing type 2 diabetes

Until now it was unclear what walking speed was needed to reduce risk of type 2 diabetes
(The Guardian, Naomi Klein) -- Walking faster is linked to a significantly lower risk of developing type 2 diabetes, according to the first global study of its kind.
Type 2 diabetes is one of the world’s major health threats, with its prevalence rising sharply in the last three decades, according to the World Health Organization.
More than 537 million people have been diagnosed, but millions more are estimated to be in the dark about the fact they have the condition. It is a major cause of blindness, kidney failure, heart attacks, stroke and lower limb amputation.
Researchers have known for years that walking – and doing so frequently – is associated with a lower risk of type 2 diabetes. Until now, though it has remained unclear what walking speed is needed to reduce the risk of type 2 diabetes.
Now a worldwide analysis of studies shows that a brisk walk or striding is better for reducing your risk of type 2 diabetes that walking at a slower pace. The pooled data analysis of the available evidence was published online in the British Journal of Sports Medicine.
Researchers found people who walked faster than 1.86mph (3km/h) were less likely to develop the condition, while those with a speedier stride of more than 3.7mph (6km/h) lowered their risk by 39%.
While physical activity is known to be associated with a lower risk of developing type 2 diabetes, researchers from Imperial College London, the University of Medical Sciences in Iran and Oslo New University College in Norway wanted to figure out the optimal walking speed.
The team looked at 10 studies published between 1999 and 2022, which included follow-up periods of between three and 11 years. A total of 508,121 adult patients from across the UK, Japan and the US were included..
Compared with strolling at less than 3km/h, an average or normal walking speed of 3-5km/h was associated with a 15% lower risk of type 2 diabetes – irrespective of the time spent walking.
The risk reduced even further with a faster pace, with a fairly brisk walk of between 5km/h and 6km/h associated with a 24% lower risk.
“While current strategies to increase total walking time are beneficial, it may also be reasonable to encourage people to walk at faster speeds to further increase the health benefits of walking,” researchers said.
There were some limitations to the research. Three studies included were rated as having a moderate risk of bias, while the remaining seven were rated as having a serious risk.
The researchers also acknowledged that people with a faster walking speed are more likely to be fitter, with greater muscle mass and better overall health.
But there are plausible explanations for the findings, they explained.
Walking speed is an important indicator of overall health and a key indicator of functional capacity.
Faster walking speed is associated with better cardiorespiratory fitness and muscle strength, both of which are linked to diabetes risk – and brisk walking is good for weight loss, which helps to improve insulin sensitivity.
Neil Gibson, senior physical activity adviser at Diabetes UK, welcomed the findings.
He said the “study highlights what we already know, that being physically active, which can include brisk walking, can help lower a person’s risk of developing type 2 diabetes and that increasing the intensity of activity, such as by walking faster, gives greater overall health benefits”.
“We welcome further research to confirm whether, and to what extent, picking up the pace boosts the positive effects walking can have on reducing the risk of developing type 2 diabetes.
“Walking is cost-free, simple and for most people can be integrated into regular activities like getting to work, shopping and visiting friends.
“While progressing to a faster pace is usually recommended for greater health gains, it’s important that people walk at a pace that they can manage and is suitable for them.”
Are You Ready for Tomorrow?

Medicaid expansion starts December 1. Are you ready?
The state of North Carolina is expecting a flood of new patients in waiting rooms on December 1, when Medicaid expansion lets roughly 600,000 people gain greater access to healthcare. In advance of potentially full waiting rooms and confusion, the NC Department of Health and Human Services has issued some tips. Here is some help:
WHAT PROVIDERS NEED TO KNOW AND DO
- A robust provider network ready to serve newly enrolled beneficiaries is critical to success. To become a Medicaid enrolled provider, visit the NCTracks Provider Enrollment webpage.
- Once enrolled, providers can contract with the health plans in their area. See the NCMedicaid Provider Contracting with Health Plans webpage for more information.
- If you are a currently enrolled Medicaid provider, check to make sure your information is correct in NCTracks, including whether you are accepting new patients. See the NCTracks Manage Change Request FAQs for more information about the managed change request process.
- Monitor your secure NCTracks Provider Message Inbox and Status and Management page for notification of required actions, like reverification.
- New program aid categories will be created for beneficiaries eligible due to Medicaid expansion. These will display for eligibie beneficiaries in Category of Eligibilty section of the NCTracks Recipient Eligibility Verfication feature:
- Managed Care Enrolled (full Medicaid benefit):
- MXPNN – Adult Medicaid Expansion, Categorically Needy
- MCPGN -- Adult Medicaid Expansion, Categorically Qualified Alien
- Emergency Services Only:
- MXPFN – Adult Medicaid Expansion, Categorically Needy Non-Qualified Alien, Emergency Services only
- MXPHN – Adult Medicaid Expansion, Categorically Needy, Emergency Services only
- Managed Care Enrolled (full Medicaid benefit):
HOW CAN PROVIDERS ASSIST NC MEDICAID BENEFICIARIES?
- Providers can help by offering services to beneficiaries enrolled in these program and encouraging patients to apply. The Department will also be sharing a toolkit with resources to share with your patients and community.
- Individuals can apply for Medicaid in one of four ways:
- Online (https://epass.nc.gov/) - English and Spanish portal available
- Paper application
- In person at their local Department of Social Services (DSS) office
- By calling their local DSS office
- More information on applying for Medicaid coverage is available at https://ncgov.servicenowservices.com/sp_beneficiary?id=bnf_apply:
- Interested individuals may review the NC Medicaid eligibility criteria for more information before applying.
- It may take up to 45 days for someone to find out if they are eligible. Incomplete applications may take longer. Applications submitted online often process faster. If an individual cannot apply online, they may utilize one of the other options listed above to apply.
We want to hear from you! How are you preparing for tomorrow? Please respond in the comments.
Could Lidocaine Kill Cancer Cells?
Lidocaine May Be Able to Kill Certain Cancer Cells by Activating Bitter Taste Receptors
Preclinical study explains the previously observed anti-cancer effect of the common anesthetic drug
(Penn Medicine News) -- Lidocaine—often used as numbing agent for outpatient medical procedures—activates certain bitter taste receptors through two unique mechanisms that result in cancer cell death, according to researchers from the Perelman School of Medicine at the University of Pennsylvania. Their findings, published today in Cell Reports, pave the way for a clinical trial to test the addition of lidocaine to the standard of care therapy for patients with head and neck cancers. The local anesthetic drug has long been suggested to have beneficial effects in cancer patients, but it wasn’t known how or why.
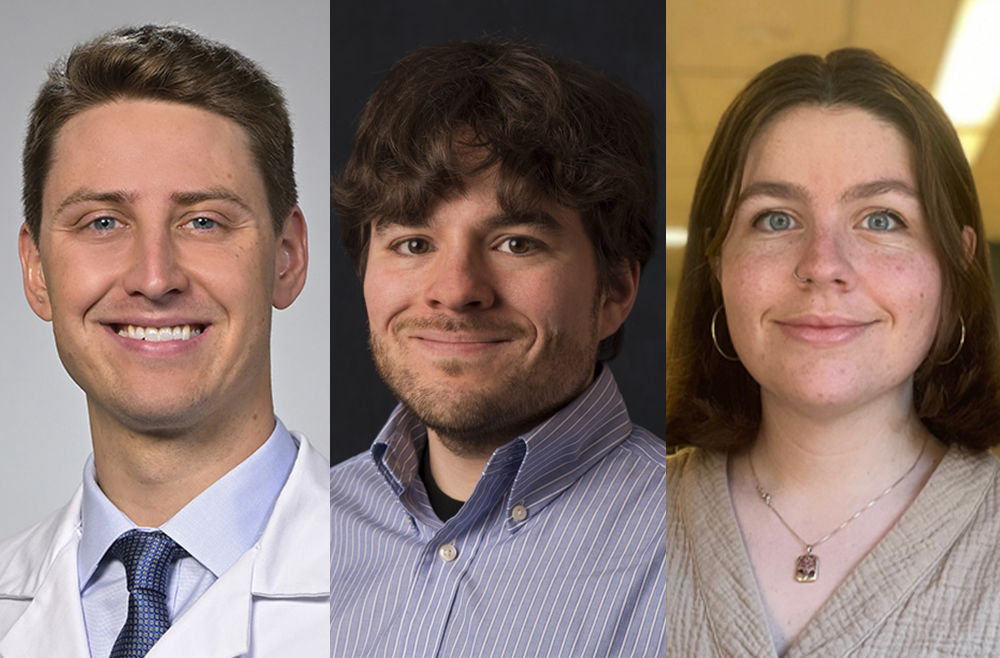
The preclinical study was led by Robert Lee, PhD, and Ryan Carey, MD, both assistant professors of Otorhinolaryngology - Head & Neck Surgery, and Zoey Miller, a Pharmacology graduate student at Penn and member of Lee’s lab. The team found that lidocaine activates the bitter taste receptor T2R14, which is elevated in various cancer cells. When this receptor is activated, it starts a process called apoptosis, causing the cancer cells to die. The specific mechanisms that allow lidocaine to activate T2R14 are mitochondrial calcium ion overload, which produces reactive oxygen species that can damage biomolecules, and proteasome inhibition, together resulting in cell death.
Previous work by the team showed that bitter taste receptors are found in many oral and throat cancer cells, where they trigger apoptosis, and that increased expression of these bitter receptors is correlated with improved survival outcomes in patients with head and neck cancer. In April 2023, a multi-institutional randomized clinical trial published in the Journal of Clinical Oncology found that breast cancer survival increased when lidocaine was administered before surgery.
“We’ve been following this line of research for years but were surprised to find that lidocaine targets the one receptor that happened to be most highly expressed across cancers,” Lee said. “T2R14 is found in cells throughout the body. What’s incredibly exciting is that a lot of existing drugs that activate it, so there could be additional opportunities to think about repurposing other drugs that could safely target this receptor.”
While T2R14 helps the body perceive bitter taste in the mouth, the function of the receptor in other cells throughout the body is unclear. Lidocaine is typically injected into the skin or other tissues to prevent pain by blocking nerve signals and could easily be directly injected near or around accessible oral tumors.
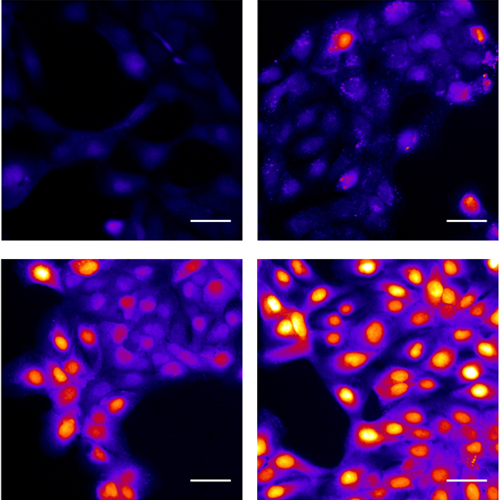
“Speaking as a head and neck surgeon, we use lidocaine all the time,” Carey said. “We know lidocaine is safe, we’re comfortable using it, and it’s readily available, which means it could be incorporated into other aspects of head and neck cancer care fairly seamlessly.”
The study, which was done primarily in cell lines of head and neck squamous cell carcinomas (HNSCCs), also found that T2R14 is particularly elevated in HNSCCs associated with the human papillomavirus (HPV), which is now the dominant form of HNSCC. As a result of these findings, Carey is planning to develop a clinical trial at Penn Medicine’s Abramson Cancer Center to test the addition of lidocaine to standard care for HPV-associated HNSCCs.
“While we’re not suggesting the lidocaine could cure cancer, we’re galvanized by the possibility that it could get an edge on head and neck cancer treatment and move the dial forward, in terms of improving treatment options for patients with this challenging form of cancer,” Carey said.
The study was supported by the National Institutes of Health (T32GM008076, R01DC016309, R01AI167971, and R21DC020041), the Blavatnik Family Foundation, the American Head and Neck Society, and the McCabe Foundation.
To learn more about clinical trials at Abramson Cancer Center and eligibility to participate click here or call 1-855-216-0098 to speak to a clinical trial navigator.
Don't be 'Sus', This List Will Help You Talk to Your Teenage Patients. No 'Cap'!
'Bet', this annual list of slang terms could have you saying 'Yeet'

(USA Today, Anthony Robledo) -- IYKYK and if you don't, well there's always Urban Dictionary.
Online language learning platform Preply released their 2023 survey of the most commonly used slang terms that parents of teenagers are most familiar with. While words like "salty" and "extra" transferred over from last year's list, other slang terms have broken through this year.
The report surveyed 682 parents with children between the ages of 12 and 18 and found that only 2% knew every slang term on the list. About 3 in 5 parents in the study said they try to stay keep up with slang to communicate with their teenagers, usually by using Google.
"Using language to understand and connect with another person is a part of life that we continue to experience in different ways from one person to another," the report reads.
Most common slang words in 2023
"Sus," short for suspicious, is the most used slang term by teenagers in 2023, according to parents in the survey. The term gained popularity thanks to the online murder mystery game Among Us. About 62% of teenagers use the word "sus" to call out questionable behavior or suggest one has a devious motive.
The second and third most common slang terms are "bet" and "yeet." The report said 59% of the parents have heard their teenagers say "bet" to express agreement or good news while 57% say "yeet" when aggressively throwing an object deemed worthless.
These are the most common slang terms, according to the parent survey, along with their Urban Dictionary defintion.
- Sus - "Giving the impression that something is questionable or dishonest; suspicious."
- Bet - "An expression that means 'I agree', 'good news'."
- Yeet - "To violently throw an object that you deem to be worthless, inferior or just plain garbage."
- Salty - ""When you are upset over something little."
- Cap - "Another word for lying. It can be used like no cap or you can say stop capping."
- Extra - "Being over the top, excessive, dramatic behavior."
- Bussin' - "What you would say if something was really good."
- Bougie - "Used to describe someone as high class, literally or figuratively."
- Sheesh - "An expression when you’re impressed or amazed by something."
- Drip - ""When something is very cool. Can be used to describe an outfit/accessory, person, song, etc."
- Oof - "Can be used to express discomfort, stress, or sadness."
- Finna - "Abbreviation of 'fixing to'. Normally means 'going to'."
- Shook - "Being shocked or surprised. When you can't believe what you're seeing."
- Simp - "When someone does way too much for a person they like."
- Mid - "Used to insult or degrade something or an opposing opinion, labeling it as average or poor quality."
- Hold This L/You Took An L - "What someone says to another person when they lose at something."
- IYKYK - "If You Know You Know."
- NPC - "Someone, regardless of their views, who doesn't think for themselves."
For the full list with over 35 terms see the full survey.
What slang do parents understand the most?
"Salty" is the slang term parents are most familiar with followed by "bougie" and "sus." These are the following words the parents surveyed were most familiar with:
- Salty (70%)
- Bougie (67%)
- Sus (65%)
- Bet (63%)
- Extra (62%)
- Cap (57%)
- Finna (56%)
- Shook (54%)
- Simp (53%)
- Yeet (52%)
Bussin, finna and cap are the most hated slang words
Some slang is more acceptable than others to parents. The survey found that there the five most despised terms they hate to hear their teenagers use (and what percentage of parents hate them).
- Bussin (21%)
- Finna (16%)
- Cap (14%)
- Yeet (14%)
- Simp (13%)
Let's keep it real:Merriam-Webster picks 'authentic' as 2023 word of the year
Old Memories Help Us Learn New Things, According to Science (and Snails)!

(Makika Spitulski) -- It’s often said that we’re “learning by experience” when we try new things, practice skills, and make mistakes. In other words, our memories of past experiences can shape our perceptions of ourselves, the world, and even the future. Though we can all probably think of examples that back up this phenomenon, how this works in our brains is more obscure.
New research on snails is inching us closer to an explanation. The study — published in the journal Science Advances — not only showed a connection between past and future learning, but also shed light on how we can potentially put ourselves in a position to learn based on our memories.
Per Quanta Magazine, researchers altered the perception of snails during two types of training: strong and weak. In the former, the mollusks were first placed in petri dishes containing water mixed with a fruity flavor, which they seemed to feel neutral about. They then received a sugar solution — which they promptly devoured. The scientists found that even a day later, the snails began associating the fruit-flavored water with sugar and, therefore, were more likely to consume the water. (Think: Pavlov’s experiment, but with snails instead of dogs.)
For the weak training, snails were first placed in dishes containing a different flavored water, and then given a less highly concentrated sugar snack. In these tests, the snails did not positively associate the flavored water with sugar.
The scientists then went a step further and analyzed snails given a strong training followed by a weak training. They found the snails with strong training still learned from the weak training. However, when the weak training preceded the strong training, a memory of the weak training did not occur. Meaning, prior strong learning boosted the following weak learning.
According to the researchers, the strong training primed the snails for a “learning-rich period.” This period allowed associations to occur with cues that otherwise would go unnoticed, which could possibly benefit their survival. For instance, the snails could potentially be trained to find food sources nearby and enhance their sensitivity to threats.

The study also showed a learning-rich period could last about a half hour to four hours after strong training. Once this period was over, the snails stopped forming long-term memories, per Quanta, even though they still had the memory of the strong training. So, they still retained those memories but weren’t making new ones.
Why is the period not longer? Making long-term memories is “energetically costly” for the brain, the study authors wrote. So it’s actually a good thing this process doesn’t last too long. In fact, senior research fellow at the University of Sussex and lead author Michael Crossley told Quanta Magazine, if it did, “that could be detrimental to the animal.”
In this sense, snails and humans are similar. With so many things happening constantly around us, our brains must distinguish what to hold onto and what to let go of. It’s why many of us can’t recall what we ate for lunch yesterday, yet still remember the specifics of a day from decades ago.
The takeaway: Change in perception can help “link past and future memory storage,” per the study. With this awareness, a subject can be alerted to “learning-rich periods” and take advantage of those times to stimulate focused learning that is ideal for long-term memory formation and robust learning.
Of course, snails have smaller and simpler brains than humans. But still, this insight offers a glimpse into how memories are made, how they connect to the future, and even what we can do to put ourselves in an optimal position to learn.
Inspired by the snail school? Here are three tips to make more long-term memories, maybe even starting today:
1. Have more firsts: According to the TED Institute, one study found that more than 70% of people’s vivid memories were first-time experiences or unique events, like first kisses and jobs. So consider checking out a new fitness class or traveling somewhere you haven’t been before. It may stick with you longer than you think.
2. Embrace the peculiar: Another study found that “peculiar” experiences that are somewhat familiar while still feeling novel stand out in our memory. Maybe go a bit out of your comfort zone and try something slightly out of your regular routine, like trying a new entree at a restaurant you love, going bird watching at your local park, or extending a random act of kindness to a neighbor.
3. Pay more attention: An MIT study showed that when we pay more attention, we’re more likely to make memories. So if you want to remember something, be mindful to observe the smells, the sights, the sounds, and the way you feel.
NCMS Board Member, Dr. Karen Smith, Talks Medicaid Expansion, Access to Care
More people in NC will have health insurance on Dec. 1, but there’s more to do to improve access
(NC Newsline, Lynn Bonner) -- North Carolina will reach a milestone Dec. 1 when an estimated 600,000 low-income people become eligible to enroll in health insurance under Medicaid expansion.
North Carolina is the 40th state to expand Medicaid and allow people with incomes up to 138% of the federal poverty level to enroll in the government health insurance plan. That’s equivalent to an annual income of $41,400 for a family of four, or $20,120 for an individual.
State officials estimate that 600,000 people will be eligible for the insurance and have prepared to enroll 300,000 people on the first day.
Medicaid expansion became an option for states in 2014 and studies have shown that it has led to improved health. People in expansion states, for example, better manage their diabetes and high blood pressure.
Health care advocates worked for years to convince North Carolina Republican legislators to adopt expansion. Under a law President Joe Biden signed in 2021, the state will receive a $1.6 billion signing bonus over two years. Expansion will come at no cost to the state.

Photo: https://karensmithmd.com/
Dr. Karen Smith, a family doctor with a practice in rural Hoke County, is eager to see the broader effects of expansion, including the increased financial security that will come when families just getting by won’t have to channel precious dollars toward high medical bills.
“How can an individual even try to maintain health and get up and go to work, have a job and bring money into that household, and if they become ill, they have to take money out of the household,” she said in an interview.
North Carolina tied with Tennessee as the states with the 10th-highest uninsured rate last year at 9.3%, according to the U.S. Census. The national average was 8%.
Counties with high percentages of people without insurance were much more likely to have many health care consumers with medical debt in collections, an Urban Institute study found.
In a string of counties in eastern and northeastern North Carolina, at least 27% of consumers had medical debt in collections. North Carolina had 12 of the top 100 counties in the nation with the highest rates of medical debt. Two counties, Lenoir and Greene, were in the top 10.
In a presentation the Saturday before Thanksgiving to the Old North State Medical Society, an organization for Black doctors, Smith advised attendees to prepare their practices for newly insured patients.
Smith began practicing in Hoke as part of an NC Medicaid Society Foundation program that recruits primary care doctors to work in rural areas and medically underserved areas. She agreed to a three-year commitment and has been there 32 years.
“I love taking care of the people here,” she said.
Health care in rural counties
Medicaid expansion is expected to be of particular help in rural counties, where residents are more likely to be uninsured.
Getting services to rural residents will be key to fulfilling Medicaid expansion’s promise of a healthier state. It’s in some of those counties, though, where healthcare is contracting.
Martin General Hospital in Williamston closed in August and its operator filed for bankruptcy. At the time, Gov. Roy Cooper criticized the legislature for slow-walking Medicaid expansion. The General Assembly voted for expansion in March, but the move was not final until the budget was finalized in early October.
Last January, ECU Health announced it would close five rural clinics after its rural health system lost $46 million in 2022. The decision was “primarily driven by financial pressures including a disproportionate number of uninsured or underinsured patients as well as labor costs for travel staff,” ECU Health said in a January press release.
ECU said in a statement it had relocated services offered at those five clinics and does not plan to reopen them.
“ECU Health vocally advocated for Medicaid expansion for nearly a decade and has been equally vocal on the need for continued investment in rural health care across the state,” the health system said in a statement.
“We are grateful to legislators for not only the passage of Medicaid expansion, but other vital programs that will support our rural academic health mission. Similar to many other rural health systems across the nation, ECU Health is focused on necessary transformation as we respond to current economic realities and adjust to the continued shortage of nurses and providers.”

Photo: Screenshot from NC Newsline interview
Kody Kinsley, state Department of Health and Human Services secretary, said in an interview with NC Newsline editor Rob Schofield that his agency and the state Department of Commerce are preparing a report on the “biggest gaps in the healthcare and caregiving workforce” and steps needed to close them. “It’ll give us more of a roadmap,” Kinsley said.
But those strategies for filling those gaps wouldn’t work if more people didn’t have a way to pay for their care, Kinsley said.
Medicaid expansion and increased Medicaid rates are “the foundational investment that sustains this other stuff,” he said.
Federally funded community health clinics have been working for years in underserved areas. These health clinics see patients whether or not they have insurance and bill uninsured patients on a sliding scale based on their income.

Photo: https://www.ncchca.org
The community health clinics expect to continue treating those patients, but now more of them will have insurance. Having more insured patients will mean the clinics can “reinvest in their communities,” said Alice Pollard, vice president for operations and strategy for the NC Community Health Care Association.
The association’s 43 members saw 750,000 patients last year.
The clinics have been spreading the word about Medicaid expansion and expect new patients will seek them out once they have insurance.
Finding medical care
Increasing access to substance abuse treatment was one of the selling points for Medicaid expansion.

Photo: https://www.med.unc.edu/
Dr. Michael Baca-Atlas, a family doctor and addiction medicine specialist, said he was thrilled when Medicaid expansion became a reality.
“I’m excited for patients, said Baca-Atlas, who works at UNC REACH Enhanced Primary Care, a Raleigh medical clinic. People will be able to get on life-saving medications and won’t have to worry about not being able to see a specialist because they don’t have insurance, he said.
But the state does not have enough doctors to treat all the newly insured residents who might seek treatment for substance use disorders, he said. Enhanced outpatient services will be critical to meeting the need, he said. The problem will be less pronounced in Wake than in surrounding counties.
“There is absolutely going to be a need to enhance outpatient services across the state,” Baca-Atlas said.
Newly insured residents will be eligible for an array of medical services, including dental care. The problem will be finding dentists who will take new Medicaid patients.
The main reason dentists won’t take new Medicaid patients is because rates have not increased since 2008, said Dr. Steve Cline, vice president of the NC Oral Health Collaborative.
The collaborative works to reduce oral health disparities.
“We fought hard for Medicaid expansion,” he said, but it won’t solve the problem of people being able to secure dental appointments.
The next step for those interested in better oral health for low-income people is to convince legislators that the state needs to increase Medicaid rates for dental care, Cline said.
There is data on how many people go to hospital emergency rooms with dental problems, he said, but that doesn’t tell the whole story.
Pollard, the community health association vice president, said some community clinics are working with the DHHS to increase medication-assisted treatment for opioid use disorders. And clinics are increasingly offering dental services, she said.
“There’s a lot of different puzzle pieces that have to fit together so that we as a state can make sure that people are having access to the care they need where they need it,” Pollard said. “Medicaid expansion is a huge piece of that puzzle. It’s like we can see the image now in the puzzle we have to put together. Having that is such a key in being able to invest in the other solutions.”
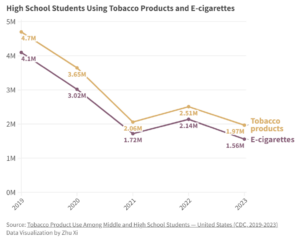
CDC: High School E-Cigarette Use Declining, NC JUUL Settlement Helping

(The Daily Tar Heel, Audrey Kashatus) -- Use of e-cigarettes declined from 14.1 to 10 percent among high school students from 2022 to 2023, according to this year's Centers for Disease Control and Prevention National Youth Tobacco Survey.
This 2023 decline comes about two years after N.C. Attorney General Josh Stein reached a $40 million settlement in his lawsuit against JUUL, an e-cigarette company. JUUL began paying the settlement in 2021 and will continue until 2027, according to a press release on Stein's website.
The company was required in the settlement to make changes to its business practices to avoid appealing to younger people and fund programs to prevent e-cigarette addiction in North Carolina.
It is illegal to sell tobacco products to people under 21 years old.
Seth Noar, a distinguished professor in the Hussman School of Journalism and Media who specializes in health communication, said a reason for the recent decline could be because e-cigarette use rates in 2019 were the highest they had been in nearly two decades after the emergence of products like JUUL.
According to the National Youth Tobacco Survey, 27.5 percent of high school students used e-cigarettes in 2019.
The Orange Partnership for Alcohol and Drug Free Youth, which has been working to prevent youth substance use since 2008, collaborates with Orange County Schools, Gayane Chambless, the program director for the partnership, said.
Chambless said the partnership has historically encouraged peer education about vape-related harms in local middle and high schools. Peer education allows students to identify concerns about vaping and how the partnership plan to address it, she said.
According to Chambless, peer education was also beneficial in discovering the right needs for high school students.
"What we saw was the high schoolers' response being, 'It's not helpful,' because they were already addicted," she said.
She said high school students often need more resources to quit vaping, rather than prevention resources.
“Being able to hear what is needed by those in the community that you're serving is really important,” she said.
Noar said he researches health communication, specifically messages about vaping and e-cigarette usage. He said the most effective campaigns among high school students are messages about the health impacts of vaping.
“What seems to work the best is really trying to help young people understand what it's like to be addicted, the consequences and the negative impact that addiction can have on your life,” Noar said.
PAVe, Parents Against Vaping e-cigarettes, is an organization dedicated to helping parents recognize warning signs of children vaping, giving them resources on how to help their children quit and educating parents, according to Shana Bedi, the education and regional advocacy manager for PAVe.
Bedi said PAVe was started by parents who had no public health background, but who felt their children were being targeted by the e-cigarette industry in schools.
In addition to educating parents, she said PAVe also works with all adults who come into contact with children who are vaping — including teachers, superintendents, principals, counselors and school nurses
Bedi said most young people who start vaping either experience pressure from their peers or underlying mental health issues. She said it is important to address these root causes of e-cigarette use to prevent people from becoming addicted.
Chambless said the Orange Partnership received a Partnerships for Success grant from the Substance Abuse and Mental Health Services Administration that totals $1.8 million over five years for Orange County.
She said the partnership has been researching what factors are causing mental health issues and increased substance use in high school students. She said one reason is lack of social engagement, especially after the COVID-19 pandemic.
The grant will be used to address this issue and create more pro-social opportunities for students in schools, she said.
Though there has been a decline in high school students using e-cigarettes, Bedi said PAVe will not reach its goal until rates drop to zero percent.
“We don't want any kids vaping, we don't want the industry targeting our kids,” she said.
United Nations Takes Action on PFAS in NC as Residents Prepare for Exposure Study

The United Nations has recognized the PFAS contamination crisis occurring in the Lower Cape Fear Region as a violation of international human rights law.
The Cape Fear River is the primary drinking water supply for over 1.5 million residents in NC.
On Thanksgiving Day, the U.N. published five letters to Dupont, Chemours, Corteva, the United States and the Netherlands. The letters are in response to a communication filed on behalf of Clean Cape Fear, which is seeking compensation for human rights violations connected to PFAS exposures coming from the Chemours Fayetteville Works Facility.
Clean Cape Fear is a grassroots community action group working to restore and protect soil, water, and food supplies from PFAS contamination.
Tanner Blue with WWAY in Wilmington reports that Clean Cape Fear says the acknowledgement feels warranted.
“I will say at first this is really validating" said Clean Cape Fear Co-Founder Emily Donavan. "There’s a lot of people that in our community that do feel that their rights have been violated, and it’s been very frustrating to watch a company like DuPont and now Chemours, kind of be given safe harbor, or really just a slap on the wrist.”
Chemours, the Netherlands and Corteva have responded to the United Nations. The United States and DuPont have not.
As those letters come to light, some in North Carolina are rolling up their sleeves to give blood and learn more about PFAS exposure.

Navassa, a predominantly Black community in Brunswick County, gets its drinking water from the Cape Fear River. So does its neighbor Wilmington, which is about six miles southeast. That makes the town’s residents prime candidates to join the GenX Exposure Study, a multisite study where environmental health researchers are examining the blood of people who’ve been exposed to per- and polyfluoroalkyl substances (PFAS), which have contaminated waterways throughout the state.
In 2017, the year that GenX chemicals, which are a class of PFAS, were found in the Cape Fear River, N.C. State University epidemiologist Jane Hoppin and colleagues, including East Carolina University epidemiologist Suzanne Lea, launched the GenX Exposure Study to answer some of the many questions about the potential health impacts of the chemicals on humans.
Before the launch of the GenX Exposure Study, Lea and Hoppin had worked together on environmental health issues as part of the Center for Human Health and the Environment at N.C. State University. The center brings together researchers within the university and those from the East Carolina University’s Brody School of Medicine, North Carolina Central University and the N.C. Department of Health and Human Services to investigate and lessen environmental effects on humans.
Lea recalls developing an action plan soon after Detlef Knappe, a professor in the N.C. State University Dept. of Civil, Construction and Environmental Engineering, shared research with the Wilmington Star News that detailed the presence of GenX compounds in the Cape Fear River.
“I said [to Jane], ‘Let me call the health director with the New Hanover County Health Department and see what we can do,’” Lea said. “And we wrote a grant to the National Institute of Health, and the New Hanover County health director talked to the city council and county commissioners and we started …”
In the lower Cape Fear Region, the study includes public water users in New Hanover and Brunswick counties and well water users in Bladen, Cumberland and Robeson counties, whose wells have been tested for contamination by Chemours or the N.C. Department of Environmental Quality.
Chemours’ Fayetteville Works plant, on the border of Cumberland and Bladen counties, has been fingered as the culprit in the GenX contamination in the lower Cape Fear, both for dumping chemicals into the river and for the PFAS that came out of smokestacks and drifted on the wind to surrounding municipalities.
In the upper Cape Fear Region, the study includes residents of Pittsboro whose drinking water comes from the Haw River — a tributary of the Cape Fear — where contaminants emanating from industries in Greensboro and elsewhere have added to the level of chemicals.
Since 2017, the study has recruited roughly 1,400 participants, and researchers want to add more African Americans, Lea said.
“We really feel like at least 20 percent of that total group should be African Americans to reflect the size in our state,” she said.
African Americans account for roughly 22 percent of North Carolina’s population, according to U.S. Census data.
(This story contains reporting by Will Atwater of NC Health News and Tanner Blue of WWAY)
Additional Reading:
Navassa residents roll up their sleeves to participate in PFAS exposure study
Fighting PFAS contamination in the Lower Cape Fear Region
Overview of PFAS in North Carolina
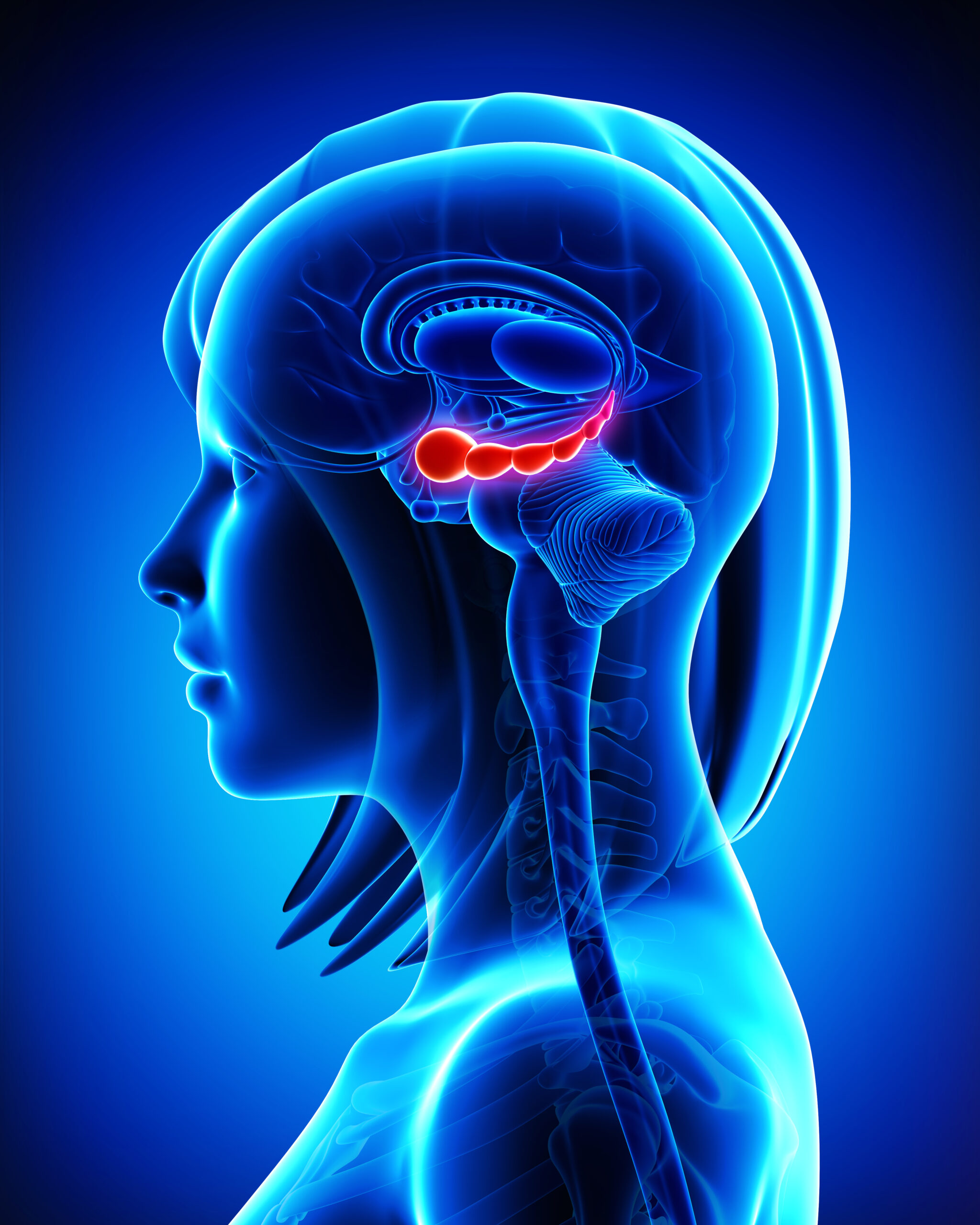
New Duke Study: Hippocampus Takes the Lead in Brain’s Memory Dance

(Duke University School of Medicine, Shantell M. Kirkendoll) -- Based on brain images and memory tests, the Duke study published Nov. 27 in the Journal of Neuroscience reveals a finely tuned memory dance choreographed by the hippocampus, the brain’s memory center.
The hippocampus doesn’t store detailed object information. Instead, it influences how the cortex stores such information that would be needed later, ensuring that memories are coded in a way that meets future needs and tasks.
This research can help identify specific brain regions that can be stimulated to bring back healthy brain activity in individuals experiencing memory decline, such as Alzheimer’s disease.
“What is exciting about this study is that it shows that the details supporting memory processes are fundamentally driven by the interaction between the hippocampus and the cortex, but not by each region independently,” said senior author of the study Simon W. Davis, PhD, an assistant professor in the Department of Neurology at Duke University School of Medicine and a member of the Center for Cognitive Neuroscience.
“This is a much more contemporary way of seeing the brain,” he said.
The hippocampus is believed to help in forming episodic memories by connecting pieces of information stored in the cortex. However, the exact process by which the hippocampus and cortex work together to store memories is not entirely clear.
“The study suggests that the strength of interactions between the hippocampus and other brain regions during memory encoding can predict subsequent memory,” said lead study author
Shenyang Huang, a graduate student at Duke University.
To better understand how brain regions process features of objects, researchers used functional MRI, a brain imaging technique, to observe 19 study participants as they tried to memorize images of real-world objects like pizza, birds, and clothing.
They later tested the participants on their memory of both the concept of the objects and the specific details.
Their findings revealed that certain brain regions exhibited a heightened sensitivity to visual characteristics, while others were more attuned to semantic, or meaning-related, information.
The hippocampus plays a critical role in adjusting the memory impact of cortical representations that are most relevant to future memory needs, or what authors referred to as “transfer-appropriate representations.”
In the realm of remembering how things look, the strength of visual representations in the ventromedial occipital cortex is crucial, coordinated with hippocampal activity and information patterns during encoding.
Similarly, when it comes to grasping the meaning or concept of objects in subsequent conceptual memory, the strength of semantic representations in the left inferior frontal gyrus and angular gyrus is key.
While new medications offer hope for those with age-related memory disorders, researchers at Duke are exploring alternative interventions including transcranial magnetic stimulation (TMS).
“As we search for reliable targets for TMS, it’s important to emphasize cortical targets that link to the hippocampus in an informed matter, so they can boost meaningful conversations in the brain,” said Davis, who also has appointments in the Department of Pathology and the Department of Psychiatry and Behavioral Sciences at the Duke School of Medicine, and in the Department of Psychology and Neuroscience at Duke.
Davis and colleagues gained support from the National Institutes of Health to explore how older adults with memory impairments may benefit from individualized magnetic brain stimulation.
“The efficacy of that intervention—and our understanding of why it works—will be based on studies like this showing how cortical-hippocampal communication forms strong memories,” Davis said.
Additional authors: Cortney M. Howard and Roberto Cabeza of Duke University; Mariam Hovhannisyan of University of Arizona and Maureen Ritchey of Boston College
UNC School of Medicine Researchers Named in Clarivate's 2023 List of Highly Cited Researchers

Twenty UNC School of Medicine and 21 other UNC-Chapel Hill researchers have been named in Clarivate’s 2023 list of Highly Cited Researchers™, scientific pioneers from around the world whose names are drawn from the publications that rank in the top 1% by citations for field and publication year in the Web of Science™ citation index.
(UNC Health and UNC School of Medicine Newsroom) -- UNC-Chapel Hill researchers have been recognized in Clarivate’s 2020 list of Highly Cited Researchers™. The list includes 20 UNC School of Medicine and 21 other UNC-Chapel Hill researchers who have demonstrated significant influence in their chosen field or fields through the publication of multiple highly cited papers during the last decade. Their names were drawn from the publications that rank in the top 1% by citations for field and publication year in the Web of Science™ citation index.
Clarivate™ is considered a global leader in providing trusted insights and analytics to accelerate the pace of innovation. Since 2001, the Highly Cited Researchers™ list has identified global research scientists and social scientists who have demonstrated exceptional influence reflected through their publication of multiple papers. In determining the “who’s who” of influential researchers, the Institute for Scientific Information™ at Clarivate draws on the data and analysis performed by bibliometric experts and data scientists. It also uses the tallies to identify the countries and research institutions where these scientific elite are based.
Here are the names of the UNC School of Medicine researchers who have been featured in the 2023 list.
Xi-Ping Huang, PhD, Pharmacology
Sidney Smith, MD, Medicine
John Buse, MD, PhD, Medicine
Ke Cheng, PhD, Biomedical Engineering
Kenneth Dinnon, Microbiology & Immunology
Gianpietro Dotti, PhD, Microbiology & Immunology, UNC Lineberger
Katherine Hoadley, PhD, Genetics, Lineberger
Leaf Huang, PhD, Biomedical Engineering, UNC Lineberger
Charles Perou, PhD, Genetics, UNC Lineberger
Scott Randell, PhD, Medicine, Cell Biology & Physiology, UNC Lineberger, Marsico Lung Institute
Barbara Salvodo, PhD, Microbiology & Immunology, UNC Lineberger
Martin Styner, PhD, Psychiatry
Jenny Ting, PhD, Genetics, Microbiology & Immunology, UNC Lineberger
Yanqi Ye, PhD, Biomedical Engineering
David van Duin, MD, PhD, Medicine, Microbiology & Immunology, UNC Lineberger
Ralph Baric, PhD, Microbiology & Immunology, UNC Lineberger, UNC Global Health
Timothy Sheahan, PhD, Microbiology & Immunology
Bryan L. Roth, MD, PhD, Pharmacology, UNC Lineberger
Patrick Sullivan, MD, Genetics, Psychiatry
John McCorvy, PhD, Pharmacology (formerly of UNC SOM, now U. of Wisconsin)
More information on Clarivate Highly Cited Researchers can be found here.
CDC: Covid Variant BA.2.86 Triples in New Estimates
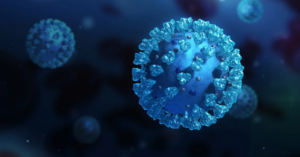
(CBS News Health Watch, Alexander Tin) -- Nearly 1 in 10 new COVID-19 cases in the U.S. are from the BA.2.86 variant, the Centers for Disease Control and Prevention estimated Monday, nearly triple what the agency estimated the highly mutated variant's prevalence was two weeks ago.
Among the handful of regions with enough specimens reported from testing laboratories, BA.2.86's prevalence is largest in the Northeast: 13.1% of cases in the New York and New Jersey region are blamed on the strain.
Monday's figures mark the first time BA.2.86's prevalence has surged enough to be listed as a standalone variant on the CDC's estimates. Scientists first warned of the highly mutated strain's discovery over the summer.
"In previous Nowcast updates, BA.2.86 was too uncommon to be shown separately and was grouped with other BA.2 strains," the CDC said Monday.
Before this point, officials have said the vast majority of new COVID-19 cases have been blamed on the XBB variant and a crowd of XBB's closely related descendants. Those include the HV.1 and EG.5 variants that are currently predominant nationwide.
However, this latest estimate – 8.8% through Nov. 25 – is virtually triple what it was on Nov. 11, when 3.0% of new cases were estimated to be BA.2.86. The CDC typically publishes its variant estimates every other Friday, but had delayed last week's release until after the Thanksgiving holiday weekend.
"It is important to note that early projections tend to be less reliable, since they depend on examining growth trends of a smaller number of sequences, especially as laboratory-based testing volume for SARS-CoV-2 has decreased substantially over time," the agency said.
The World Health Organization also recently stepped up its classification of BA.2.86 and its descendants to a "variant of interest" after a rise in cases from the strain.
Early data on BA.2.86 suggests it does not appear to lead to worse or different symptoms than previous strains, the WHO said in its Nov. 21 risk evaluation, but noted a "substantial rise" in recent BA.2.86 reports.
The CDC said it did not disagree with the WHO's assessment that BA.2.86 likely posed a "low" public health risk, adding that for now the strain "BA.2.86 does not appear to be driving increases in infections or hospitalizations in the United States."
It comes as the CDC has begun to track a renewed increase in indicators tracking COVID-19's spread across the U.S. headed into the winter.
After weeks of largely slowing or flat trends, the CDC said this month that figures like emergency department visits had begun to increase nationwide from COVID-19. Virtually all regions of the country are now seeing at least slight increases.
Some of the highest increases are in the Midwestern region covering Illinois, Indiana, Michigan, Minnesota, Ohio and Wisconsin, where trends are nearing levels not seen since early January.
Is the JN.1 variant to blame?
Since August, BA.2.86's broad array of mutations did not appear to be enough for the strain to gain a foothold over XBB and its descendants. Months of the highly mutated variant's spread only resulted in a small share of cases throughout the world.
But scientists in recent weeks have been studying a steep increase in a BA.2.86 descendant called JN.1, which quickly rose to become the fastest-growing subvariant worldwide.
Many cases have been reported in Europe, which has seen increasing cases from BA.2.86 and its descendants.
Authorities in France said on Nov. 13 that JN.1 was largely driving that country's increase in BA.2.86 infections, climbing to 10% of sequences in the country. Early investigations of JN.1 had not turned up any worrying signals so far compared to other BA.2.86 infections, they said, though more in-depth analyses were underway.
Data from recent weeks tallied from the GISAID virus database suggests as much as a third of COVID-19 variants reported from labs in the U.S. have been of JN.1.
"Currently, JN.1 is the most common version of BA.2.86 in the U.S. CDC projects BA.2.86 and its offshoots like JN.1 will continue to increase as a proportion of SARS-CoV-2 genomic sequences," CDC spokesperson Jasmine Reed told CBS News in an email.
Last month, the CDC said it expected COVID-19 tests and treatment would remain effective against JN.1, which is closely related to BA.2.86 aside from a single change to its spike protein that early research suggests is enabling it to spread faster.
This season's vaccines are also expected to work against JN.1 similar to what was estimated for its BA.2.86 parent, the agency said.
Save The Date! NCMS 2024 White Coat Day and Legislative Reception
Get Out of the Office and Into Your White Coat!
NCMS is Planning Only ONE White Coat Day in 2024! Our Biggest Advocacy Day of the Year!
The North Carolina Medical Society is planning to flood the General Assembly with white coats in our biggest White Coat Day yet! It is time to show your elected leaders what is important to you and the profession of medicine.
We are thrilled to invite you to the 2024 NCMS White Coat Day and Legislative Reception! Join us on June 12, 2024 for meetings with legislators at the General Assembly and an evening at the Merrimon-Wynne House.
The goal: Hundreds of NCMS members on-site! Help us make our voice be heard like never before.
Registration is open! Secure your spot by registering today!
Duke Researchers Discover Our Eyes and Ears “Talk” to Each Other Through Subtle Sounds

(Hear.com) -- It’s a well-known fact that the body is interconnected, but a new study is magnifying just how closely eyes and ears work together. Publishing their findings last week, Duke University scientists discovered that they can pinpoint where someone is looking simply by listening to their ears.
“You can actually estimate the movement of the eyes, the position of the target that the eyes are going to look at, just from recordings made with a microphone in the ear canal,” professor and study senior author Jennifer Groh said in a press release. Similarly, the team found that by knowing where someone was looking, they could predict the waveform of the subtle ear sound.
So where exactly do these “ear squeaks” come from? According to Groh, they may occur when “eye movements stimulate the brain to contract either middle ear muscles, which typically help dampen loud sounds, or the hair cells that help amplify quiet sounds,” the release explains.
While their purpose is still uncertain, Groh has a hunch: “We think this is part of a system for allowing the brain to match up where sights and sounds are located, even though our eyes can move when our head and ears do not.” Now, the researchers plan to use this discovery to examine whether these ear squeaks could enhance perception and how they could be used to develop improved hearing tests.
Listen to the sounds the ears make as the eyes move here.
Time to Say Goodbye! Food Scientists Say What to do With Thanksgiving Leftovers
How Long Do Thanksgiving Leftovers Last?
Food scientists break down what food is the first to go bad and simple ways of extending leftovers’ shelf life

Is it time to get rid of your Thanksgiving favorites?
(Scientific America, Jocelyn Solis-Moreira) -- After days of planning and hours of cooking, the last thing you want to do is toss out your lavish Thanksgiving meal. It’s practically become tradition to feast on leftover turkey for days after the holiday. But how long can you really get away with eating that meat, or those extra mashed potatoes or slices of pumpkin pie, without risking an upset stomach—or worse? What are the best ways to preserve food to keep flavors fresh?
Scientific American spoke with food scientists about the health and safety of storing leftovers, as well as other Thanksgiving Day cooking and exposure factors that can speed up the time it takes food to reach what public health agencies call “the danger zone.”
What are some guidelines for storing leftovers?
The U.S. Department of Agriculture’s Food Safety and Inspection Service recommends throwing out refrigerated leftovers after three to four days. If foods are kept in the freezer, they can usually still be consumed for three to four months. There is some flexibility in these rules, however.
“I like to go by the USDA’s guidelines, but I am not a stickler to it,” says Bryan Quoc Le, a food scientist and a faculty research fellow at Pacific Lutheran University and author of 150 Food Science Questions Answered. “Personally, I sometimes push [refrigerated leftovers] to four or five days, depending on the type of food.”
Smell is a common indicator people use to see if food has gone bad. A foul odor may suggest that certain bacteria, mold or other microorganisms have gotten the best of your leftovers. But surprisingly, spoilage bacteria generally don’t cause illness. (Although people might feel sick from the revolting scent and taste.) Disease-causing bacteria typically do not change food’s smell, flavor or appearance. That’s why a sniff test isn’t always reliable, says Jennifer Quinlan, a food safety expert and a professor of nutrition sciences at Drexel University. Instead Quinlan emphasizes the importance of taking preventive steps when cooking, such as avoiding cross contamination and not leaving raw or cooked food sitting out for too long.
Why do leftovers seem to go bad so quickly?
Le explains there are several factors that influence how long certain items stay fresh. Animal-derived foods such as meat and dairy have a higher likelihood of containing pathogens that, given enough time, can grow on leftovers and make people sick. The most common pathogenic bacteria are Staphylococcus aureus, Salmonella and Escherichia coli. Le recommends throwing away dairy and meat products by the end of the third day after initially cooking them.
The food’s composition also matters. Water or moisture can help bacteria, yeast and other microorganisms grow faster, while high sugar or salt content can slow down some microbial growth. Such sweet or salty foods are more likely to get contaminated by spoilage microorganisms that make your food smell and look rotten—but they are less likely to cause life-threatening infections, Le explains. These foods are a little safer to eat for longer periods of time, compared with dairy or meat products without such content.
Acidity is another factor. Canned cranberry sauce, for example, has a pH of about 2.4. Le says only a few pathogens can survive in such acidic conditions. Meat and dairy, on the other hand, have a neutral pH, making them a more hospitable environment for microorganisms. Additionally, meat and dairy products are rich in nutrients—fats, sugars, proteins and minerals—that microorganisms need to grow. Fresh vegetables or other plant-based dishes do not have such an array of microbe-supporting nutrients, so only a select number grow in these types of foods. Baked goods also tend to lack such nutrients and to have a high sugar content.
When should one start storing food?
Food safety experts say dishes should be sealed and stored in the fridge immediately—ideally, under two hours after the food is prepared, at which point the risk of illness begins to increase. Bacteria and other microorganisms thrive at room temperature (between 68 and 74 degrees Fahrenheit), Le says. Some bacteria such as Clostridium perfringens, one of the most common culprits of food poisoning, can withstand the oven’s heat when a turkey is baking and can potentially cross contaminate other foods, including stuffing and gravy. “That’s a really bad [bacterium] that you don’t want to leave out for too long because it grows at room temperature and produces toxins,” Quinlan warns.
The USDA says leaving food that has an internal temperature of 40 to 140 degrees Fahrenheit out on the table is typically considered the “danger zone,” Le notes, because harmful bacteria can rapidly divide and contaminate the food. “Every 20 minutes the food is left out in room temperature, microorganisms are doubling in number.”
The Centers for Disease Control and Prevention recommends refrigerating perishable food in under two hours after preparation. If the food has been sitting at temperatures above 90 degrees F, such as in a hot car, the agency recommends refrigerating or discarding it within an hour.
Le warns leaving out food to cool to room temperature may put it in the danger zone for a longer period of time, increasing the risk of bacterial growth. He advises putting food in the fridge even if it is still warm. Dividing large amounts of food into smaller portions and putting them in shallow containers can help hot food cool down more quickly.
How does refrigeration help preserve leftovers?
When food temperature drops to refrigeration level—at or below 40 degrees F—it decreases the metabolism of most microorganisms, Le says. Lower temperatures slow down many of the chemical processes that normally allow microbes to reproduce and extract energy from food sources. But this does not mean the fridge is killing the bacteria. Rather it keeps them in suspended animation, Le says. Once you reheat the food, he adds, “they're going to come back to life.”
Freezing leftovers can make them last about two to three months, depending on the fat content. As with refrigeration, the colder temperature temporarily stops pathogens from dividing and reproducing. Although frozen foods can be stored longer, Le says that there is a trade-off: supercold temperatures can cause freezer burn, which changes the flavor of the food the longer it’s stored.
What’s the best way to package and store leftovers?
Limiting the oxygen accessible to pathogens such as bacteria and mold can help slow their growth. Quinlan advises packing leftovers with vacuum-sealed food storage containers or wrapping them tightly.
For wrapping, Le recommends using double layers of aluminum foil and plastic wrap for extra protection. Plastic wrap is permeable to oxygen but not to water. Aluminum foil blocks both oxygen and water, making it better at depriving microorganisms of the resources they need to divide.
Where you place your leftovers in the fridge is also important. “The temperature in the fridge fluctuates throughout the night, even when it’s closed,” Le says. He recommends putting leftovers like meats and dairy, which are the first to go bad, closer to the center of the fridge. This makes them more likely to remain near a constant temperature. Put food that is the slowest to spoil, such as high-acid cranberry sauce or sugary sweet potatoes, by the door or the edge of the fridge. Experts say these tips can help extend the shelf life of leftovers, allowing you to spend more time enjoying them instead of throwing them away.
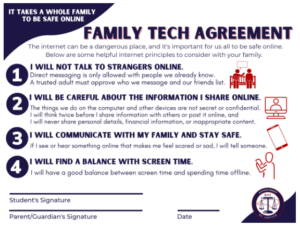
NC Officials: Teen Sexual Extortion Cases Rising Online

(NC Health News - Jennifer Fernandez) -- As teens spend more time on social media, parents need to watch for signs that they are being exploited, North Carolina officials warn.
Between 2021 and 2022, the FBI saw a 600 percent increase in “sextortion” cases in North Carolina, state Attorney General Josh Stein said in a recent webinar. In sextortion cases, a criminal threatens to expose or publish sexual content of the victim if the victim doesn’t provide more sexual imagery, meet in person for sex or pay the extortioner with money or gift cards.
In October, the FBI issued a warning about an increase in financially motivated sextortion schemes online in the U.S. In these cases, victims are typically males aged 14 to 17, with some as young as 10. Girls are more often extorted for more compromising photos or to meet for sex. Boys have been targeted increasingly as a way to get money, federal authorities said.
Offenders contact victims through online gaming, gaming consoles, live streaming or video platforms, instant messaging apps and social media.
“Several young people have taken their own life (sic) based on the feelings of fear and shame that result from sextortion and subsequent financial targeting,” Donald Alway, the assistant director in charge of the FBI’s Los Angeles Field Office, said in a news release.
Tips for kids to stay safe online
- Chat only with known friends. Block or ignore messages from strangers.
- Realize that “chat is flat,” meaning there’s often no context, you can’t hear inflection in voices, and you should seek clarification if you’re not sure about something.
- Chat carefully without full trust at first. For example, if you think the person is someone you know, ask questions that can only be answered by that person. Videos and photos are not proof that a person is who they claim to be.
- Realize that chats and media are saved, shared and reviewed. Snapchat messages, for example, can be retrieved even though the main premise of the app is that everything gets deleted.
- Realize that everyone online puts on a persona.
- Limit what you share online, especially personal information. Predators learn details about victims through open social media accounts. Don’t share passwords.
- Be suspicious if someone you meet while playing a video game or through another online forum suggests changing to a different app or other method to communicate.
- Encourage children to report suspicious behavior to a trusted adult.
Source: State Bureau of Investigation, FBI
Growing concern
Last year, the National Center for Missing and Exploited Children’s CyberTipline received more than 32 million reports of suspected child sexual exploitation.
Child pornography makes up the vast majority of reports. The next largest category is enticement, which includes sextortion. That category grew by 82 percent from 2021 to 2022, mostly due to a spike in financial sextortion, according to the center’s annual report.
In North Carolina, tips to the state about cyber child exploitation more than tripled from 2019 to 2022 and are on track to grow higher this year, according to N.C. State Bureau of Investigation Special Agent Kevin Roughton, commander of the state’s Internet Crimes Against Children Task Force.
The state received 4,930 cyber tips in 2019. The number of tips is expected to top 26,000 this year, he said during the latest “Protecting the Next Generation of North Carolinians” webinar, which focused on online crimes against children.
“Tips have continued to go up month over month, year over year,” Roughton said. “So this is a problem that is not going away. It is only increasing.”
Shifting landscape
The social media landscape is constantly shifting, especially among teens who tend to be more open to trying new technologies.
YouTube led, with 95 percent of teens 13 to 17 saying they have used the app or site. TikTok followed at 67 percent, with Instagram (62 percent) and Snapchat (59 percent) rounding out the leaders.
The FBI said sextortion schemes happen in online environments where young people feel most comfortable.
In a recent North Carolina case, the defendant was accused of using Snapchat and Instagram to solicit a 15-year-old girl, said Boz Zellinger, special deputy attorney general for special prosecutions with the N.C. Department of Justice.
“Know what’s out there on your kids’ phones and what they’re using,” he said during the “Protecting the Next Generation” webinar.
Not just stranger danger
More than half of U.S. teenagers (51 percent) say they spend at least four hours every day on social media, according to a Gallup survey conducted earlier this year.
While not every online interaction results in exploitation, at least 15.6 percent of young adults in the U.S. have experienced at least one type of sexual abuse online before the age of 18, according to a 2022 report published in JAMA Network Open.
The surge in financial sextortion cases has tended to involve predators from outside the U.S. targeting teens here, according to the FBI. However, that is not the case for most other types of online sexual exploitation of children.
“The prevailing image of online sexual abuse is that it mostly involves stranger predators who stalk kids with technology,” co-author David Finkelhor, professor of sociology and director of the Crimes against Children Research Center at the University of New Hampshire, said in a news release. “But the reality is very diverse.”
Finkelhor and his co-authors said that professionals planning prevention and intervention strategies for online sexual abuse should understand that online abuse is often an extension of dating abuse, sexual bullying and sexual harassment. In many cases, perpetrators are not strangers; they also aren’t all adults. They can be peers or somewhat older young adult friends.
They can also be trusted community members, such as teachers, coaches and even mall Santas, Zellinger said.
“These folks that abuse children online can come from every walk of life,” he said.
Roughton warned of a misconception that predators are lurking on the “dark web.” They are on the platforms children use every day, he said.
Of the cyber tips received in North Carolina last year, 56 percent came from four sources — Facebook, Google, Instagram and Snapchat, he said.
“Our children need to understand what these dangers are and how they can protect themselves,” Roughton said.
If You Are a Victim:
- Do not comply with the predator's demands. They may still publish the material
- Block them
- Don't delete any affected profiles or messages, which can be used as evidence and help authorities locate and stop the predator
- Report their account to the platform(s). (Find information on how to do that at www.missingkids.org/IsYourExplicitContentOutThere or go to cybertipline.org to make a report.)
- Call your local FBI field office or 800-225-5324, or make a report at tips.fbi.gov.
- Children who need to speak to someone can get help through multiple channels:
- Email [email protected] or call 800-843-5678.
- Text HOME to 741741 to connect with a volunteer crisis counselor at the Crisis Text Line.
- Call or text 988 to reach the Suicide and Crisis Lifeline.Source: National Center for Missing and Exploited Children, FBI
Medicaid Expansion Begins Friday, NC Raising Rates for Behavioral Health Providers

Rate Change is First Since 2012
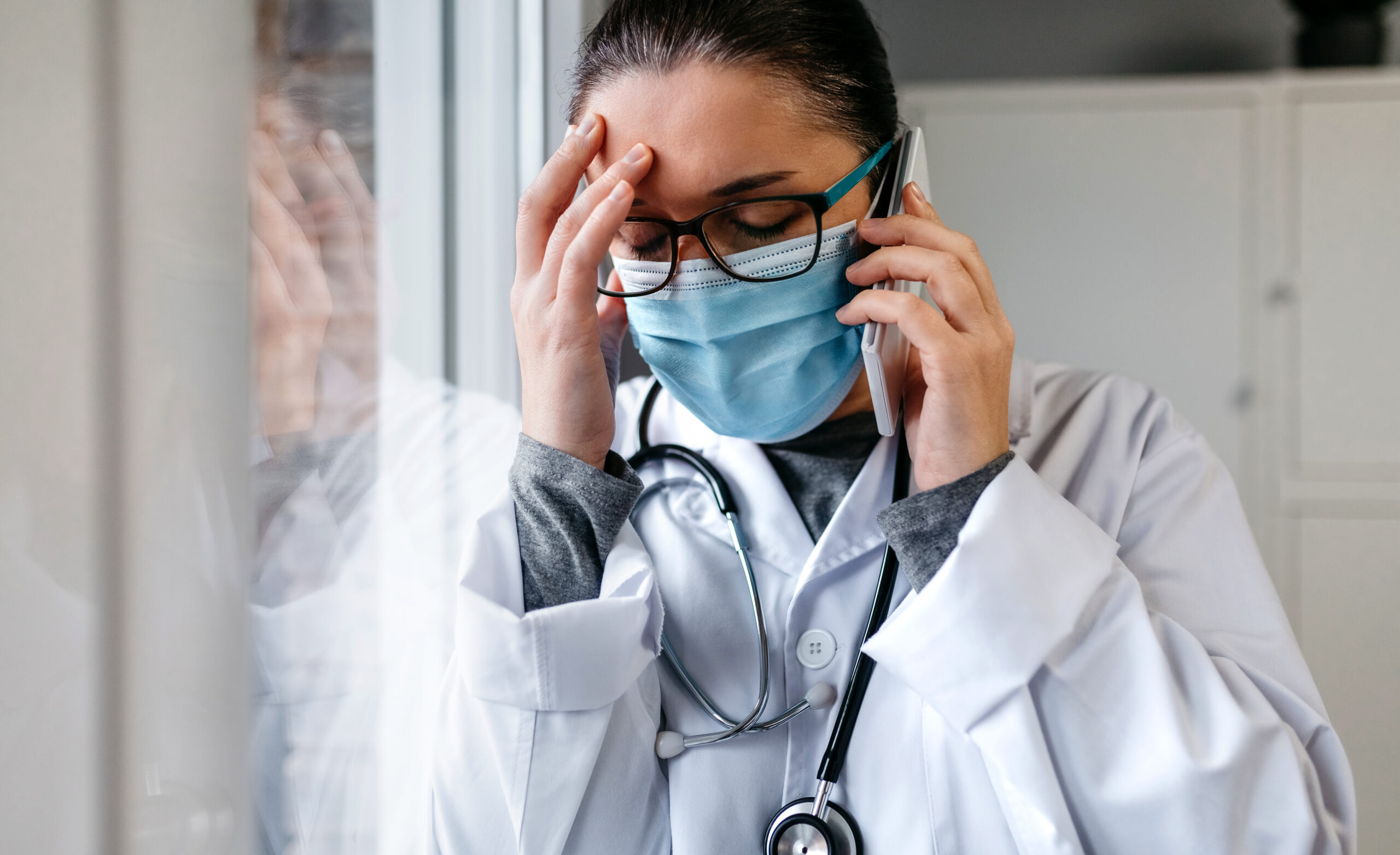
(NC Health News - Jamie Baxley) -- Medicaid expansion, a decade-in-the-making measure that is expected to provide health insurance to more than 600,000 low-income North Carolinians, will take effect in less than two weeks.
But the coverage created by expansion is only useful if eligible residents have access to health care providers that accept Medicaid. That’s particularly true for people looking for mental health care, which has been in even higher demand since the COVID-19 pandemic.
Behavioral health providers of all types across the state— but particularly mental health practitioners — have complained for years that they are not adequately reimbursed for services covered by the government-funded program. In fact, they often lose money by treating Medicaid patients, and that has prompted an exodus of providers from the program.
The N.C. Department of Health and Human Services hopes to make the situation more tenable by raising the minimum reimbursement rates for behavioral health care for the first time since 2012.
The new rates announced Wednesday by DHHS will apply to most Medicaid-covered treatments for mental health and substance use disorder. They will also apply to services for patients with intellectual and developmental disabilities, along with services for patients living with traumatic brain injury.
In an interview with NC Health News, Kody Kinsley, head of DHHS, said the increased rates, which take effect on Jan. 1, will be permanent thanks to $200 million in recurring funds allocated by the General Assembly.
“It’s a huge investment in our provider community,” he said. “It’s a huge investment in increasing the amount of provider workforce, and it’s going to open up the tap and access for people who so desperately need it.”
Behavioral health providers, he added, couldn’t “stay in business on the rates that were being paid.”
“We’re in a situation where we hear all the time every single day that we don’t have providers,” state Sen. Sydney Batch (D-Raleigh) said on a bipartisan panel this week at the North Carolina Institute of Medicine annual meeting. “I know a lot of therapists that are not practicing because the reimbursement rates are too low.”
Under the current fee schedule, facilities are paid less than $500 a day for inpatient psychiatric care. They will receive nearly $900 under the new rate, according to Kinsley. Reimbursement for inpatient psychiatric care is expected to increase by 30 percent overall.
“You can have a child in the ED and you will get $3,000 a day, potentially, for that child if they’re sick, but if they’ve had a mental health crisis, you’re gonna get pennies on the dollar,” Batch said. “We do not value behavioral health at the same level as we do physical health.”
Psychiatrists will also see more than double the reimbursement for psychological assessments, a process which, if done well, can take several hours, if not longer. DHHS says the new rate will pay $229 per assessment, up from $100.
Psychiatric residential treatment facilities, however, will not see an increase — at least not for the time being. Kinsley said DHHS is working to establish a separate, long-term rate structure for providers in those settings.
“We didn’t do a rate increase on PRTFs right this moment because we have a different process underway [for them],” he said. “We’re trying to determine not just how do we increase their rate, but how do we pay for quality?”
Expansion approaches
The rate changes were announced ahead of an anticipated surge in Medicaid enrollment in North Carolina.
On Friday, the state’s long-standing income limit for eligibility will increase to 138 percent of the federal poverty level. That means single adults, a population that has been effectively ineligible for coverage under the current criteria, will qualify if they make less than $20,000 a year.
The first residents expected to benefit from the expansion are those currently enrolled in so-called Medicaid family plans, which offer fewer benefits than traditional Medicaid. DHHS estimates that 300,000 family plan enrollees will be automatically upgraded to full coverage.
Kinsley said the department is making an “all hands on deck” effort to ensure that expansion is implemented as smoothly as possible. Still, he stopped short of promising a totally seamless rollout.
“I’m confident that we’re going to have a bolus of people that come forward on [Dec. 1] that is going to be larger than what the performance of the statewide system, as far as our staff and our DSS office, can manage all on one day,” Kinsley said, referring to the Division of Social Services. “That’s normal for any type of new launch — any new product launch — that you bring out.”
He likened the state to an Apple store “with a line down the street” waiting to buy the latest iPhone. DHHS, he said, anticipates seeing “some full waiting rooms” once expansion goes live.
But the bigger challenge, according to Kinsley, might be sustaining that excitement after the initial rush.
“While I want a really smooth Day One, I also want to keep that energy up so that, come April, we’re still trying to find every potential person in this state that is eligible and get them enrolled,” Kinsley said. “Eighty percent of the people that are going to be in the Medicaid expansion benefit are coming from working families. These are hardworking people who maybe have multiple jobs and are taking care of their kids and are getting ready for the holidays.”
More than 2.8 million North Carolinians were enrolled in Medicaid as of October, according to data from DHHS.
Hungry Again? Here is the Science Behind Your Craving

(Katie Couric Media, Tess Bonn) -- Whether your loyalties lie with a bag of potato chips or a bar of chocolate, the fact is we all get cravings. More than 90 percent of people have experienced them at one point or another — often, of course, at the most inopportune times, like right before a long meeting or going to sleep.
If you’ve ever been woken up by a hankering for peanut butter and jelly or followed a fantasy toward a slice of pizza, you’ve probably wondered, why?! Basically, up until now, the popular belief was that the body drove these cravings, so if you were craving red meat, that was thought to be a sign of having low iron. But Kent Berridge, Ph.D., says the bulk of scientific evidence has now largely struck down this notion that dates back to the 1930s. As with most things, there are a few exceptions, such as sodium or calcium deficiencies. But our desires for certain foods are largely driven by our brains.
Still, some questions linger. What’s with the cravings that come right after we’ve eaten a meal? Well, cravings and hunger are two very different experiences.
“We can crave even when we’re full because the brain is still able to be tempted by palatable foods around us,” says Dr. Berridge, a professor of psychology and neuroscience at the University of Michigan.
The age-old question is: Should you ignore these cravings or give in to them? Dr. Berridge weighs in on this tricky topic and so much more.
The science behind food cravings
As it turns out, food cravings can be pretty complex because they can stem from various mental and physical factors. Oftentimes, food cravings can be triggered by your brain trying to fulfill an emotional need, such as reducing stress and anxiety. During these episodes, three regions of the brain — the hippocampus, insula, and caudate — are all activated almost as intensely as those parts of the brain would in someone with active drug addictions, according to a study published in NeuroImage. Specifically, memory parts of the brain like the hippocampus associate a specific food with a reward that drives these cravings.
Beyond physiological, lifestyle changes may play a role, too. For instance, chronic lack of sleep or quality rest suppresses a hormone known as leptin that regulates fat storage and calories burned while simultaneously triggering ghrelin, a hormone that causes hunger. Hydration is important, too: Not getting enough fluids, whether water or otherwise, can also exacerbate cravings, especially those on the sweeter side. That’s because when you’re not getting enough water it can be difficult for organs that use water, such as the liver, to release the food-storing substance known as glycogen or stored glucose, which is a type of sugar you get from the foods you eat. This, in turn, causes your body to crave sweets instead of water.
Why we crave certain foods
If you happen to gravitate toward a certain type of food time and time again, there’s a reason for that, according to Dr. Berridge. “We crave foods that we’re familiar with,” he says.
We’ve probably all had that chocolate craving and thought to ourselves, “why can’t I crave carrots?” It’s a fair point: Our cravings usually aim for sweet and fatty foods rather than fruits and vegetables. A part of it has to do with the fact that these greasier and sweeter foods are obviously tastier and more appetizing. And biology may be to blame there because, in the prehistoric era, our ancestors had to take advantage of these tasty treats where and when they could get them because they weren’t as readily available, Dr. Berridge says. That’s definitely not the case now — we can run to our nearest grocery store or order delivery from our favorite fast-food restaurant whenever we want.
Though this is not as common, some people also even crave non-food items like paper, dirt, or laundry detergent. Dr. Berridge says this tends to be a sign of pica, a condition driven by iron, calcium, or zinc deficiencies.
Should you fight cravings?
Counter to what you might think, you shouldn’t fight your cravings. The key to keeping them in check is to acknowledge them, rather than try to avoid them. “Trying to suppress hankerings often doesn’t work because suppressing means focusing on it, and when we focus on it, we’re more likely to give in,” Dr. Berridge tells us.
That said, it’s a good idea to come up with a plan for when you start itching for something to eat, especially since we tend to lean toward more fatty and sugary foods. Do you want to indulge, and will your craving be satiated if you do? Indulging in cravings is not wrong. However, we understand the concerns if you lean toward greasy or fatty foods and your cravings seem like bottomless pits. One option is to try to discover a more nutritious alternative to the specific thing you crave. If you crave the sugary fruit roll-ups of your youth, have you tried dried fruit as a substitute? Other techniques like mindfulness or starting a cravings journal can help you decide when to give into the urge and when to abstain and identify any potential triggers, like stress or anxiety. Studies have found that stress can drive up your cortisol hormones, which may be linked to hunger, cravings, and compulsive eating behaviors.
The bottom line
Various mental and physical factors cause food cravings. But the good news is that they’re rarely a sign that you’re lacking the nutrients found in that food. And getting them isn’t necessarily negative — after all, they’ve been key to our survival as humans. “We wouldn’t have evolved and succeeded in evolving if we didn’t have cravings,” Dr. Berridge tells us. “They’re what makes us seek food, mates, and the crucial things in life.”
Curi Capital to Merge with RMB Capital, Expanding Offerings for Physicians, PAs, and Their Families

CHICAGO & RALEIGH, Nov. 21, 2023 – Curi, a national healthcare advisory firm comprised of three distinct businesses: Curi Advisory, Curi Capital and Curi Insurance, announced a definitive agreement to acquire a majority stake of RMB Capital (“RMB”), a registered investment advisory firm with more than $9.6 billion in assets under advisement1. As part of the agreement, Curi Capital, a registered investment advisory firm with approximately $1.6 billion in assets under advisement2, will merge with RMB. The transaction is expected to close by the end of the year. Terms were not disclosed.
“Curi is dedicated to being the trusted partner that our clients instinctively call on to drive success in their professional and personal lives, with a continued focus on physicians and the healthcare community," said Jason Sandner, CEO, Curi. “This investment and partnership with RMB, coming on the heels of Curi’s recent merger with Constellation, strategically advances that commitment. We’re well positioned, now nationally and with differentiated healthcare and financial services expertise, to meet and serve our clients across all of their needs.”
Combined, Curi Capital and RMB Capital will build on histories of generating value for individuals, families, and institutions. Both organizations have a legacy of putting clients at the center of all decisions and actions, which will continue to drive the mission for the combined organization.

RMB founding partner and CEO Dick Burridge will move into a new role as Executive Chairman and remain in his role as co-Chief Investment Officer. Curi Capital CEO Dimitri Eliopoulos will serve as CEO of the combined Curi RMB Capital entity. Eliopoulos worked in a variety of roles at RMB from the firm’s inception in 2005, eventually becoming RMB’s president of wealth management before taking the CEO position at Curi Capital in early 2020. The remainder of the RMB and Curi Capital leadership teams will also stay in place.
“As we were looking for a partner, Curi Capital, under Dimitri’s leadership, was an unparalleled fit,” Burridge said. “In just under four years, Dimitri has overseen incredible growth while building a client-centric, values-driven culture. This combination will enable a seamless transition into an exciting new era for our firm. This is an energizing new chapter, but one firmly rooted in our history.”
“I am beyond thrilled to bring together our two organizations that are focused on and inspired by the individuals and families whose lives we impact. Returning to work with so many incredible colleagues and friends who have shaped my approach to people, culture and client service, is a dream and an honor,” said Eliopoulos. “This merger sets us up to be a powerful organization with an experienced and passionate leadership team, and a clearly differentiated offering for our clients.”
Curi RMB Capital will be headquartered in Chicago. Curi Capital’s current Raleigh headquarters will remain an important office in the Southeast for the combined entity. All of the approximately 180 employees of both firms will be retained, and the company expects to hire additional staff in 2024.
Beyond the alignment between leadership and the firm’s values and cultures, the combined firm will leverage many other overlapping strengths, including a commitment to put the best interests of clients at the center of decision making, and sharing a long-term investment perspective. Curi’s resources will enable the firm to make strategic investments to optimize the business over the long term. Additionally, there is significant geographic synergy, allowing the new entity to connect back to the broader Curi family and its healthcare advisory focus.
For more information about the merger between Curi Capital and RMB, please visit rmbcap.com/curi-rmb.
Forward-looking statements made in this statement, such as those related to the merger, potential post-merger performance, growth opportunities, integration, and our expectations and intentions that are not historical facts, reflect our current views with respect to future events and financial performance. William Blair & Company served as financial advisor and Vedder Price served as legal advisor to RMB. Piper Sandler & Company served as financial advisor and Kilpatrick Townsend & Stockton served as legal advisor to Curi.
About Curi
Curi (curi.com) is a full-service advisory firm that serves more than 50,000 physicians, healthcare providers, and organizations across the U.S. Equal parts fierce healthcare advocates, smart business leaders, and thoughtful partners, Curi’s advisory, capital, and insurance offerings deliver valued advice that is grounded in client priorities and elevated by their outcomes. From data-driven advisory services to private wealth offerings, to tailored insurance solutions and beyond, Curi delivers performance that is time-tested and trusted—in medicine, business, and life. Curi holds an “A” (Excellent) financial strength rating from AM Best.
About Curi Capital
Curi Wealth Management, LLC, dba Curi Capital (curicapital.com), is a registered investment advisor, headquartered in Raleigh, N.C., that provides full-service financial advisory solutions, including personalized wealth management, retirement plan solutions, and investment guidance to high-net-worth individuals, ultra-high-net worth families, and businesses. Experienced and accessible, Curi Capital’s advisors actively listen and proactively create tailored solutions that help clients build true wealth, however they define it.
Curi Capital is registered with the U.S. Securities and Exchange Commission (SEC). Registration of an investment advisor does not imply any specific level of skill or training and does not constitute an endorsement of the firm by the SEC. A copy of Curi Capital’s current written disclosure brochures, filed with the SEC, which discuss, among other things, Curi Capital’s business practices, services and fees, are available through the SEC’s website at: www.adviserinfo.sec.gov.
About RMB Capital
RMB (rmbcap.com) is an independent advisory firm focused on helping clients achieve long-term goals. RMB brings in-house, institutional-quality investment expertise together with deep, holistic planning teams to deliver and implement customized strategies for each client. RMB serves individuals, family offices, and institutions.
Headquartered in Chicago, RMB also has offices in Denver; Jackson Hole, Wyo.; Lake Forest, Ill.; Milwaukee; Minneapolis; Oakbrook Terrace, IL; St. Joseph, Mich.; and Washington D.C. To learn more about RMB, visit rmbcapital.com.
1 Total assets under advisement (“AUA”) presented here differs from regulatory assets under management (“RAUM”) reported on RMB Capital’s Form ADV. AUA reflects net assets under management for private funds and mutual funds managed by RMB Capital, while RAUM reflects gross assets under management. AUA also includes RMB retirement plan clients’ assets under advisement, which are not included in RMB Capital’s RAUM. AUA estimated as of 9/30/23.
2 AUA presented here differs from RAUM reported on Curi Capital’s Form ADV. AUA represents Curi Capital’s RAUM plus the value of other assets advised by Curi Capital. For example, AUA includes, but is not limited to, private equity holdings, physical assets, retirement plan assets, and other non-traditional assets advised by Curi Capital.Total AUA estimated as of 9/30/23.
NCMS Releases New Firearms Policy
RALEIGH -- On November 4, 2023, the North Carolina Medical Society adopted a new Firearms Policy. The full text is here:
The North Carolina Medical Society (NCMS) recognizes firearm injury as a public health crisis, that requires a community-aligned approach of public policy and practice to successfully address. The need for effective measures, evidence-based data, and public education and awareness, is imperative to mitigate the injury and death caused by firearms.
The North Carolina Medical Society supports measures and actions to improve firearm safety and education, reduce firearm morbidity and mortality, and increase access to needed supports and services for people in North Carolina.
Therefore, the North Carolina Medical Society:
1. Supports the role and training of the clinician in preventing firearm injury and promoting firearm safety.
2. Supports community awareness campaigns and educational programs aimed at firearm owners, especially those with children or at-risk individuals in the home, about the importance of safe storage, safe use, and the efficacy of firearm safety locks in decreasing intended or unintended firearm-related injuries or death.
3. Supports the enforcement of safe storage and firearm safety lock requirements for firearm owners, as well as the implementation of statewide storage options outside of the home for firearm owners with children or at-risk factors.
4. Supports state funding and implementation of comprehensive, multidisciplinary violence prevention and intervention and/or mitigation programs, developed with community input and considerations.
5. Supports a statewide education and awareness campaign, including increased availability of behavioral health services, centered on firearm-related suicide prevention for all ages.
6. Supports the rights of health care organizations/facilities/practices to enhance the safety of all persons onsite through the enactment of policies that restrict or prohibit firearms on the premises.
7. Supports the enactment of legislation and policy that allows for the temporary removal of firearms from persons at risk of harming themselves or others.
8. Supports strengthening efforts and enforcement to regulate the sale or transfer of guns through permitting and universal background checks.
9. Supports restrictions on the sale of high-capacity magazines and a full ban on the unauthorized creation of 3D printed firearms and firearm components.
10. Supports engineering changes to improve public safety (such as trigger locks, trigger cables, and safe storage options).
11. Supports evidence-driven research and reporting to further inform future firearm safety and education, and violence prevention initiatives.
To find a line to the NCMS Firearm policy and other policies approved CLICK HERE
Just in Time For Thanksgiving! Why Do We Get Hangry?

(NiceNews) -- Most of us are familiar with the concept of “hanger” — when we get so hungry that we become emotional and often angry. Though it’s a common phenomenon (and one that has undoubtedly caused many fights over where to get dinner), it’s not known exactly why it happens.
A recent study conducted by University College London researchers began to unravel the connection between hunger and the brain, finding that, in mice, a hunger hormone produced in the gut had a direct impact on the hippocampus. “The hippocampus — which is a part of the brain really important for using our memories to make decisions — can actually respond to hunger hormones directly, and this allows the hippocampus to control our decisions based on how hungry we are,” lead author Andrew MacAskill told Newsweek.
He explained that the part of the hippocampus they focused on is also “highly involved in emotion,” which could explain why we get hangry. The main takeaway, though, is that hunger can alter how we learn. The team said the research could have applications in preventing and treating eating disorders, as well as in studying memory-related conditions like dementia.
“Realizing that hunger can directly influence the way we learn is really important for understanding how our learning and memory can go wrong, for example, in mental illness or in Alzheimer’s disease, where previously hunger signaling was not really thought about,” said MacAskill. “Maybe by including hunger in how we think about these problems we can find better ways to treat them.”
Tips for Hanger Management
John Thompson Joins NCMS as Vice President of Advocacy
The North Carolina Medical Society is happy to announce the addition of John Thompson as the Vice President of Advocacy. In this new capacity, Thompson will direct NCMS engagement in state legislative matters and activities, as well as working with our stakeholder organizations and individuals to advance the Society’s priorities.
Before joining the North Carolina Medical Society, Thompson served as the Vice President of Government Relations for the North Carolina Healthcare Association where he led advocacy efforts before the North Carolina legislature. He secured a multi-billion dollar Directed Payment Plan (HASP) for hospitals, helped negotiate Certificate of Public Need reform, and was successfully involved in negotiation on Medicaid expansion.
Prior to that, Thompson owned the public policy consulting firm, The Paratum Group in Raleigh and was a member of the 82nd Airborne Division, stationed at Fort Brag for 5 years. He is a graduate of North Carolina State University.
According to NCMS CEO Chip Baggett, “We are very pleased to be adding John, who brings the skill and experience needed to successfully enhance our operations and meet our goals. We fully expect him to be an asset for years to come and look forward to introducing him to our members across the state.”
Of joining NCMS, Thompson says, “I am very excited to be joining the North Carolina Medical Society. As someone with close ties to the healthcare community, I look forward to working for clinicians and protecting their ability to work directly with their patients. That is a sacred relationship that needs to be protected at all costs.”
Thompson will be reaching out to members and legislators soon. He can be contacted before then at [email protected] or 919-833-3836, EXT 4169.
Rosalynn Carter, Humanitarian, Mental Health Activist, and former First Lady, dies at 96

(CNN - Keith Allen and Kate Andersen rower) -- Rosalynn Carter, who as first lady worked tirelessly on behalf of mental health reform and professionalized the role of the president’s spouse, died Sunday at the age of 96, according to the Carter Center.
Rosalynn Carter passed away peacefully with family by her side at her home in Plains, Georgia, the center said in a statement.
“Rosalynn was my equal partner in everything I ever accomplished,” her husband, former President Jimmy Carter, said. “She gave me wise guidance and encouragement when I needed it. As long as Rosalynn was in the world, I always knew somebody loved and supported me.”
The Carter Center announced Friday that the former first lady had entered hospice care. She was diagnosed with dementia in May. Her husband began home hospice care in February, following a series of hospital stays.
Jimmy Carter was defeated in a landslide by Ronald Reagan four years after being elected. His single term in the White House included forging a rare peace agreement between Israel and Egypt that continues to this day, but it was also marked by soaring inflation and the Iran hostage crisis. Through it all, Rosalynn was by his side, and often whispering in his ear.
The Carters redefined and revolutionized the post-presidency and, through their joint efforts, they worked on world peace and human rights on behalf of the Carter Center, a nongovernmental Atlanta-based organization founded to “wage peace, fight disease and build hope.”
After leaving the White House, the couple traveled to hot spots around the world, including visits to Cuba, Sudan and North Korea, monitoring elections and working to eradicate Guinea worm disease and other neglected tropical diseases. Jimmy Carter won the Nobel Peace Prize in 2002.
“The Carter Center is a shared legacy. She’s been there digging latrines right next to him,” said the Carters’ friend Jill Stuckey, a leader at Maranatha Baptist Church, where both Carters attended and where Jimmy Carter taught Sunday school.
Rosalynn Carter’s most lasting individual legacy will be her efforts to diminish the stigma attached to people with mental illnesses and her fight for parity and access for mental health treatment. She also devoted her time to the Rosalynn Carter Institute for Caregiving at her alma mater, Georgia Southwestern State University, to help families and professional caregivers living with disabilities and illnesses.
In 1999, then-President Bill Clinton presented both Carters with the Presidential Medal of Freedom, the country’s highest civilian honor. He said they had “done more good things for more people in more places than any other couple on Earth.”
The ‘Steel Magnolia’
Rosalynn and Jimmy Carter shared what many would call a true American story and a genuine lifelong partnership.
In 2015, when the 39th president announced his brain cancer diagnosis, he was asked of which accomplishment he was proudest. He did not hesitate to say that it was marrying Rosalynn: “That’s the pinnacle of my life.”
He shared at another point the secret of his enduring marriage.
“Rosalynn has been the foundation for my entire enjoyment of life. … First of all, it’s best to choose the right woman, which I did. And secondly, we give each other space to do our own things,” he told Jake Tapper on CNN’s “The Lead” in July 2015.
It was likely that Eleanor Rosalynn Smith would cross paths with Jimmy Carter in their small hometown of Plains, Georgia. They grew up at a time when candy cost a nickel and everyone in town knew one another.
“Occasionally someone would open a restaurant, but it would never last very long,” Rosalynn wrote in her memoir, “First Lady from Plains.”
Rosalynn did not grow up with much money. Her mother was a dressmaker and her father was an automobile mechanic who died from cancer when she was 13. She helped raise her younger siblings and considered her father’s death the end of her childhood.
The Carters met through Jimmy’s sister, Ruth, who was Rosalynn’s closest friend. When Rosalynn saw a photo of Carter on Ruth’s bedroom wall she thought, “He was the most handsome man I’d ever seen.” She even asked Ruth if she could take his photograph home with her.
Both devout Southern Baptists, Jimmy and Rosalynn met after a church meeting and soon began dating. They were married not long after his graduation from the Naval Academy when she was 18 and he was 21.
“When we got married, I think I was kin to everybody that Jimmy wasn’t,” Rosalynn wrote in her memoir. “Once we got married, we were kin to everybody in town.”
As the wife of a naval officer, Rosalynn moved frequently and she managed a large household. The Carters had three children in quick succession: John William (“Jack”), the year after their wedding in Norfolk; James Earl (“Chip”) III, less than three years later in Hawaii; and Donnel Jeffrey (“Jeff”) in New London, Connecticut, in 1952. Their only daughter, Amy Lynn, was born in 1967, a year after Carter lost his first bid for Georgia governor.
Jimmy Carter had been accepted to an elite nuclear submarine program but resigned his commission in Schenectady, New York, after his father died so that they could return to Plains in 1953 to look after the family farm. He decided to relocate the family without asking Rosalynn’s opinion. Rosalynn was so furious that she refused to talk to him the entire drive south.
After that, Jimmy Carter said he consulted with his wife on all major decisions.
Later nicknamed the “Steel Magnolia” by the press – a reference she did not mind, saying once in an interview with C-SPAN that “steel is tough and magnolia is southern” – Rosalynn was naturally shy and her knees would knock together when she had to give a speech in the early days of her husband’s political career in the 1960s.
But by the time he announced his presidential campaign in December 1974, she was a seasoned politician herself.
Describing her transformation from housewife to political partner, Carter aide Stuart Eizenstat said, “This shy woman blossomed in the most wonderful way.”
It was not long before she would number the president’s jokes so that he would not repeat any of them to the same group. She even started taking memory classes to remember faces and names and typed thank you letters to people her husband had met on the campaign trail. She stayed up until the early hours of the morning to work on her speeches.
First lady from Plains
Carter ran for president as a Washington outsider seeking to distance himself from the paranoia and cynicism of former President Richard Nixon. He had a group of Georgia volunteers, known as the “Peanut Brigade,” campaign for him.
Rosalynn hit the road with a vengeance, and when she arrived in a small town, she scoped out the tallest antennae and headed there – the local television and radio stations – to offer herself up for an interview. In her memoir, she wrote that some of the smaller stations with few employees had no idea who Jimmy Carter was.
Rosalynn came prepared, carrying a list of five or six questions she wanted asked. Nine times out of 10, she said, the station used the questions she suggested.
“I was getting my message across,” she said in her memoir.
For 18 months during the presidential campaign, she went to 105 communities in Iowa and spent 75 days in Florida in support of her husband.
“My nervousness began to disappear when I realized people seemed pleased to meet me, though I still had trouble with a dry throat and sometimes a trembling voice when I approached an interview or a speech,” she wrote in her memoir.
Carter won a narrow victory, capturing just 51% of the popular vote and 297 electoral votes to defeat President Gerald Ford, who had assumed the presidency upon Nixon’s resignation in 1974.
The Carters ignored security concerns and broke with tradition when they decided to walk hand-in-hand with their daughter Amy down Pennsylvania Avenue after the inauguration ceremony. It was part of their mutual desire to connect with people and move away from what they saw as Nixon’s imperial presidency.
Rosalynn even wore the same gold-embroidered sleeveless coat over a blue chiffon dress that she wore to her husband’s inauguration as governor in 1971 to the galas for his 1977 inauguration as president. It was designed by Mary Matise for Jimmae and she bought it from a store in Americus, Georgia.
As a young girl, she had admired then-first lady Eleanor Roosevelt, an influential global leader who took on issues such as civil rights and poverty. Once in the White House, Rosalynn helped to transform the office of first lady and became the first to hire a chief of staff whose government salary and rank were equal to the president’s chief of staff.
She was the first first lady to work out of the East Wing. Before her, first ladies worked from an office on the second or third floors of the White House in the family’s private residence. And under her watch, full-time positions in the East Wing grew by almost 20%. But her ambitious approach to the role drew criticism, particularly her controversial decision to sit in on her husband’s Cabinet meetings.
As first lady she fought for the passage of the Equal Rights Amendment, which would have amended the Constitution to outlaw civil rights discrimination based on sex.
Steven Hochman, who has worked with the Carters since 1981 and is director of research at the Carter Center, said Rosalynn did not hesitate to disagree with her husband in public as the years went on. During speeches, the former president liked to tell audience members that one of his elementary school teachers used to tell her students that “any child could be president.”
“Mrs. Carter would correct him,” Hochman recalled in an interview. “She’d say, ‘No, she never said that. She said, any boy could be president.’”
In her memoir, Rosalynn recalled eating lunch with her husband in the Oval Office every Wednesday, similar to the vice president’s weekly lunch with the president. The ritual came about because Rosalynn had pressing topics to discuss, including their personal finances, their children and the issues she deeply cared about, including mental health.
Before those weekly lunches, when the president stepped off the elevator on the second floor at the end of the day, she would approach him with an onslaught of questions and suggestions. She talked to mothers about how high fuel prices were affecting their family budgets and she met with children in struggling schools, and she wanted to bring these issues to his attention.
Once he suggested a weekly lunch, she began to organize such conversations, putting important notes in a brown leather folder. The folder sat on her desk in her bedroom and she stuck notes in it throughout the week. By the time she brought it with her to their Wednesday lunch, it was packed.
Mental health crusade
Rosalynn Carter’s signature issue was mental health. When she was campaigning for her husband during his 1970 race for governor, she was overwhelmed by the number of people who asked her what she would do for a relative dealing with mental illness.
“One day, when Jimmy was speaking at a rally, I got in line with everybody else to shake hands with him,” she recalled decades later in an interview with the Carter Center. “He saw who I was, grinned, and asked, ‘What are you doing here?’ ‘I came to see what you are going to do about mental health when you are governor,’ I replied.”
She had a distant cousin with mental illness and she remembered running and hiding when she would hear him coming down the streets of their small town singing loudly. “He probably wanted nothing more than friendship and recognition, yet he was different, and when I heard him, my impulse was to flee,” the former first lady wrote in her memoir.
The experience left such a deep impression on her that she devoted much of her time in the White House to advocating for better care for people with mental illnesses. As Georgia’s first lady, she helped shift treatment to community mental health centers, and in the White House, she helped her husband create a Presidential Commission on Mental Health.
The day the commission was announced, Rosalynn Carter told the press that she had just gotten a note informing her that the Department of Justice prohibited the president from appointing a close relative, such as a wife, to a civilian position. Up until then, she had been planning to chair the committee.
“There is, however, no problem with you being designated as honorary chairperson,” she said, amid laughter from reporters. “So I’m going to be a very active honorary chairperson.”
In 1979, she became the second first lady to testify before Congress (Eleanor Roosevelt was the first) when she spoke about the need for mental health reform.
As first lady, she tried to be in the family’s private quarters to greet 9-year-old daughter Amy by 4 p.m. on school days, and at 6:30 p.m. they had dinner together most nights. Amy was the first presidential child to attend a public school since Theodore Roosevelt’s son.
‘I am much more political than Jimmy’
In the White House, Rosalynn would urge her husband to put off controversial decisions until after his reelection. She freely admitted, “I am much more political than Jimmy and was more concerned about popularity and winning reelection.”
She lobbied to have her husband fire Secretary of Health, Education and Welfare Joe Califano. According to longtime Carter family friend and White House aide Jerry Rafshoon, she was angry at Califano over an anti-smoking campaign, fearing that it would hurt Carter’s standing in tobacco-producing North Carolina.
“I wanted Jimmy to fire Joe Califano long before he ever did,” she wrote in her memoir, “and my reasons were purely political.”
She opposed Carter’s Rose Garden strategy not to campaign against his 1980 Democratic primary challenger, Massachusetts Sen. Ted Kennedy, and instead to stay holed up in the White House negotiating the release of American hostages in Iran.
She also did not agree with Carter’s decision to bar alcohol from White House social events, though they did ultimately serve wine and spiked punch. The impression of out-of-touch Southern Baptists in the White House created a “stereotype that we never lived down,” she said.
She was sent to Central and South America to deliver a serious message on human rights. At first, leaders and the press were skeptical about a first lady taking such an important political trip, but eventually they realized that she had a direct line to the president.
She brought home tangible achievements: Ecuador pledged to sign and ratify the American Convention on Human Rights; the military leader of Peru vowed to give up power (four years later Rosalynn attended the inauguration of the democratically elected president of Peru); and the president of Colombia pressed to move negotiations forward on the Panama Canal.
Rafshoon recalled that it was Rosalynn’s idea to hold the Middle East peace talks at Camp David, which became her husband’s greatest achievement as president. She wanted the negotiation to happen there because of Camp David’s tranquil and isolated location in the Maryland mountains. At the 13-day Camp David summit, Rosalynn took almost 200 typed pages of notes. But any accomplishments of the Carter presidency were ultimately overshadowed by a 444-day hostage crisis in Iran, in which revolutionary students stormed the US Embassy in Tehran and took more than 60 Americans hostage.
The brunt of campaigning in 1980 fell to Rosalynn as Jimmy Carter decided to stay in the White House to handle the crisis. She checked in several times a day from the campaign trail, and when she could not speak with her husband, she talked with Carter’s national security adviser, the late Zbigniew Brzezinski, who discussed how to handle the crisis. “I kept her abreast because I knew she would be discussing those issues with the president,” Brzezinski said in an interview.
Her biggest regret in life was her husband losing reelection in 1980.
“I’d like people to know that we were right, that what Jimmy Carter was doing was best for our country, and that people made a mistake by not voting for him,” she said in her memoir.
The Carter Center
Rosalynn and Jimmy Carter had four children, 12 grandchildren and several great-grandchildren. When the Carters left the White House in 1981, they returned to Plains and embarked on the longest and most ambitious post-presidency in American history.
With the exception of Harry and Bess Truman, the Carters are the only post-World War II president and first lady to return to their hometown and, since their return, Rosalynn worked to revitalize the working-class community, revamping the local inn and adding a butterfly garden.
She and her husband were active members of the Maranatha Baptist Church, where she served as a deacon. But they are perhaps most famous for their humanitarian work with the Carter Center, to which they devoted 51 weeks a year (the remaining week they spent working for Habitat for Humanity).
In a 2016 interview, Rosalynn reflected on the nearly four decades that had passed since leaving Washington.
“I missed having Jimmy in the Oval Office taking care of our country,” she said. “I have never felt as safe as I did when he was there. I still have a bully pulpit to work on issues I like, and because he was president, I have unlimited opportunities. It is a good life.”
NC Delegation Travels to AMA House of Delegates Interim Meeting - AMA Highlights

NATIONAL HARBOR, MD -- Delegates to the American Medical Association (AMA) met in National Harbor, MD to discuss a wide-ranging list of issues. The event brought together physician and medical student leaders from across the nation to shape guiding policies on emerging health care topics. Over 100 resolutions were considered addressing topics impacting patient care and the profession, and more than 20 educational sessions were offered.
The AMA’s House of Delegates is the policy-making body at the center of American medicine, bringing together an inclusive group of physicians, residents, and medical students representing every state and medical specialty. Working in a democratic process, delegates create a national physician consensus on issues in public health, science, ethics, business, and government to provide safer, better quality, and more efficient health care for patients.
The policies adopted at this meeting by the House of Delegates include:
Removing Physicians from Cost-Sharing Collections
As health insurers require patients to pay a larger share of health care bills, many physicians do not feel comfortable or adequately equipped to be the collection point for cost-sharing between insurers and patients. In response, the AMA has established new policy supporting the removal of physicians from the middle of cost-sharing between insurers and patients and require insurers to collect deductibles, copays or coinsurance from patients.
Delegates voted to adopt policy instructing the AMA to “support requiring health insurers to collect patient cost-sharing and pay physicians their full allowable amount for health care services provided, unless physicians opt-out to collect such cost-sharing on their own.”
“Requiring physicians to engage in the collection of cost-sharing at the point-of-service negatively impacts many physicians,” said AMA Trustee Marilyn J. Heine, M.D. “Alternative methods of collecting cost-sharing that place the onus on insurers can relieve private practices, especially small and rural practices, of significant administrative burdens that divert financial resources and staff away from patient care.”
The AMA’s Recovery Plan for America’s Physicians is working to remove unnecessary and costly burdens so physicians can focus on patients and keep practices open and sustainable.
Opposing encroachment of administrators on medical decision-making
Growth in the number of health care administrators—those with administrative roles such as Chief Medical Officer or Chief Health Officer—has outpaced growth in the number of clinical physicians. Conflicting goals such as the ethical duties of physicians versus the financial obligations of administrators have created tension and disconnect between the two groups. In response, delegates voted to adopt policy instructing the AMA to advocate for resistance against encroachment of administrators upon physician’s medical decision making.
“The large-scale employment of physicians has brought about a change to the profession that has resulted in conflict,” said AMA Trustee David H. Aizuss, M.D. “Traditional physician autonomy in patient care is now being influenced by pressures motivated by cost versus high quality patient care.”
The key concern regarding this change to the profession is that this new organizational and economic reality of medicine will ultimately harm patients as physicians may feel pressured to make decisions based on cost instead of high-quality patient care such as admitting patients from the emergency department who could be treated as outpatients or to discharge Medicare patients ahead of time.
“We must continue to oppose encroachment of administrators upon medical decision making of attending physicians that is not in the best interest of patients,” said Dr. Aizuss.
Calling for increased flexibility for buprenorphine prescribing for opioid use disorder
The nation’s worsening opioid overdose epidemic prompted the AMA House of Delegates today to call for the elimination of dose limit barriers for adequate buprenorphine treatment for patients with opioid use disorder (OUD). Currently, patients and physicians encounter strict dose limits set by health insurance companies and other payers based on drug labels approved by the United States Food and Drug Administration (FDA) decades ago, when illicitly manufactured fentanyl was not a major cause of mortality, as it is today. Buprenorphine reduces the risk of opioid overdose death, eases opioid withdrawal symptoms and cravings, and helps sustain recovery for patients with an OUD.
“Illicitly manufactured fentanyl and other synthetic opioids have created a far more dangerous and deadly epidemic in recent years, claiming more than 109,000 lives in 2022,” said Bobby Mukkamala, M.D., chair of the AMA Substance Use and Pain Care Task Force. “As the drug overdose epidemic evolves, health systems and insurers must adapt. Our colleagues in addiction medicine are seeing efficacy of using buprenorphine products at higher doses than the current FDA-approved labeling, but health insurers and others prevent patients from receiving this medication in a timely manner. Removing these outdated dosage caps will ensure physicians can prescribe life-saving medications without delay.”

The North Carolina delegation included NCMS President Eileen Raynor, MD and past president Arthur Apolinario, MD. Other participating members of the delegation were Delegation Chair Rebecca Hayes, MD, Darlyne Menscer, MD, NCMS Board of Directors Member Karen Smith, MD, Mary Ann Contogiannis, MF, Wake Forest University medical student Alex Soltany, and Royce Syracuse, MD. NCMS CEO Chip Baggett and VP of External Affairs Alan Skipper also attended.
Issues of particular importance noted by North Carolina delegation members include:
- Prevention of imminent payment cuts and ensuring the sustainability of Medicare
Directive of the AMA House of Delegates:
RESOLVED, that our AMA immediately create and disseminate, in major news outlets, a press release outlining the current problems within the Medicare system and how it will affect access to care with a call to action to help those with Medicare keep their physicians and the high-quality care they deserve.
- Strengthening network adequacy
Policy adopted by the AMA House of Delegates
That our American Medical Association (AMA) support establishment and enforcement of a minimum federal network adequacy standard requiring all health plans to contract with sufficient numbers and types of physicians and other providers, including for mental health and substance use disorder, such that both scheduled and unscheduled care may be provided without unreasonable travel or delay.
- Drug shortages
Policy adopted by the AMA House of Delegates
Our AMA opposes the practice of preferring drugs experiencing a in shortage on approved pharmacy formularies when other, similarly effective drugs, in patient-appropriate formulations, are available in adequate supply yet but otherwise excluded from formularies or coverage plans.
Doctor Raynor remarked: "The issues of greatest urgency to our North Carolina colleagues and our patients which were addressed by the AMA House of Delegates were averting the impending cut to Medicare reimbursement; enacting an adjustment in Medicare physician payment to allow for inflation; achieving network adequacy for patients and providers; and prevention of pharmacy formulary limitations that limit patient access to medications."
The AMA House also addressed resolution on cannabis, medical aid-in-dying, and the corporate practice of medicine staffing emergency departments. The House will convene in June for the 2024 Annual Meeting of the AMA.
TO READ THE FULL AMA INTERIM MEETING REPORT CLICK HERE.
On The Lighter Side - November 17, 2023 - The Leonids Are Coming and So Are the Holidays!
Here are some things NCMS employees, members, and YOU are talking about this Weekend and Beyond!
Leonid meteor shower: All you need to know in 2023
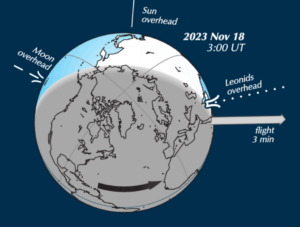
The famous Leonid meteor shower will be free of moonlight on the shower’s peak morning, November 18. You might also try watching on the morning of November 17.
Predicted peak: is predicted** for November 18, 2023, at 5:33 UTC.
When to watch: Watch late on the night of November 17 until dawn on November 18. The morning of November 17 might be worthwhile, too.
Duration of shower: November 3 through December 2.
Radiant: Rises around midnight, highest in the sky at dawn.
Nearest moon phase: In 2023, first quarter moon falls on November 20. So there will very little interference from moonlight in 2023.
Expected meteors at peak, under ideal conditions: Under a dark sky with no moon, you might see 10 to 15 Leonid meteors per hour.
For more information click here.
The Rink is back!

Enjoy the thrill of ice skating in a winter wonderland created in the heart of downtown Raleigh! THE RINK presented by UNC Health features a natural ice skating rink with stunning views of the Raleigh skyline. All you need to know to lace up your skates is here.
Time for the 41st Annual Seagrove Pottery Festival

Join the largest pottery community in the U.S. Saturday and Sunday as everyone comes together with traditional craftspeople to sell their wares. The festival features potters market, auction of signed and dated pottery, demonstrations and food vendors. All you need to know is here.
The holidays are kicking off this weekend!

Trans-Siberian Orchestra, Sunday 3-7pm, Greensboro Coliseum Complex, Greensboro
Straight No Chaser, Sunday 3-7, Durham Performing Arts Center, Durham
If you have an event you would like added to On The Lighter Side, email Randy Aldridge at [email protected].
Is Life Expectancy Gap Between Men and Women Widening?

(AXIOS - Jacob Knutson) -- The life expectancy gap between women and men in the U.S. widened again in 2021, meaning men currently die nearly six years before women, according to research published in JAMA on Monday.
Why it matters: Women have outlived men for more than a century, but since hitting a low in 2010, the gap has steadily broadened over the past decade.
- The trend is occurring alongside a decrease in overall life expectancy in the U.S. It has fallen for two consecutive years, most recently dropping from 77 years in 2020 to 76.1 years in 2021.
Of note: The life expectancy disparity between men and women hasn't been this wide since 1996 and is roughly a year above the low of 4.8 years that was recorded in 2010.
Driving the news: Researchers said the COVID-19 pandemic was the greatest contributor to the gap's growth, as men died from the virus died more often than women, potentially owing to social factors and health behaviors.
- The second greatest cause was a rise in unintentional injuries, like vehicle accidents and drug overdoses, which killed a record 106,000 people in the U.S. in 2021.
- Homicides, heart disease and suicides also contributed to the worsening life expectancy for men.
Between the lines: Scientists have hypothesized that discrepancy could be caused by differences in some biological functions.
- But environmental and societal factors also influence men's exposure to health risks and their tendency to access health services less often than women.
- For example, men are more likely to experience homeless, make up over 90% of the country's prison population and are more likely to be a victim of fatal violence or suicide.
What they're saying: While drug overdose and homicide rates have increased for both men and women, men constitute a disproportionate share of those types of deaths, said Brandon Yan, a co-author of the research and a UC San Francisco resident physician, in a statement.
- "We have brought insights to a worrisome trend," Yan said. "Future research ought to help focus public health interventions towards helping reverse this decline in life expectancy."
The big picture: The phenomenon isn't unique to the U.S., as women generally outlive men around the world — though particularly in wealthy countries, according to the World Health Organization.
- The gap is less stark in low-income countries, though that's largely because both men and women often lack access to health care.
- In new population estimates published last week, the U.S. Census Bureau projected that women will continue living longer than men over the remainder of the century.
Go deeper: Census projects U.S. population bust by 2080
Duke Scientists Create Brain Implant That May Enable Communication From Thoughts Alone

(Duke News - Dan Vahaba) -- A speech prosthetic developed by a collaborative team of Duke neuroscientists, neurosurgeons, and engineers can translate a person’s brain signals into what they’re trying to say.
Appearing Nov. 6 in the journal Nature Communications, the new technology might one day help people unable to talk due to neurological disorders regain the ability to communicate through a brain-computer interface.
“There are many patients who suffer from debilitating motor disorders, like ALS (amyotrophic lateral sclerosis) or locked-in syndrome, that can impair their ability to speak,” said Gregory Cogan, Ph.D., a professor of neurology at Duke University’s School of Medicine and one of the lead researchers involved in the project. “But the current tools available to allow them to communicate are generally very slow and cumbersome.”
Imagine listening to an audiobook at half-speed. That’s the best speech decoding rate currently available, which clocks in at about 78 words per minute. People, however, speak around 150 words per minute.
The lag between spoken and decoded speech rates is partially due to the relatively few brain activity sensors that can be fused onto a paper-thin piece of material that lays atop the surface of the brain. Fewer sensors provide less decipherable information to decode.
To improve on past limitations, Cogan teamed up with fellow Duke Institute for Brain Sciences faculty member Jonathan Viventi, Ph.D., whose biomedical engineering lab specializes in making high-density, ultra-thin, and flexible brain sensors.
For this project, Viventi and his team packed an impressive 256 microscopic brain sensors onto a postage stamp-sized piece of flexible, medical-grade plastic. Neurons just a grain of sand apart can have wildly different activity patterns when coordinating speech, so it’s necessary to distinguish signals from neighboring brain cells to help make accurate predictions about intended speech.
“I like to compare it to a NASCAR pit crew. We don't want to add any extra time to the operating procedure, so we had to be in and out within 15 minutes. As soon as the surgeon and the medical team said ‘Go!’ we rushed into action and the patient performed the task.”
Greg Cogan, Ph.D.
After fabricating the new implant, Cogan and Viventi teamed up with several Duke University Hospital neurosurgeons, including Derek Southwell, M.D., Ph.D., Nandan Lad, M.D., Ph.D., and Allan Friedman, M.D., who helped recruit four patients to test the implants. The experiment required the researchers to place the device temporarily in patients who were undergoing brain surgery for some other condition, such as treating Parkinson’s disease or having a tumor removed. Time was limited for Cogan and his team to test drive their device in the OR.
“I like to compare it to a NASCAR pit crew,” Cogan said. “We don't want to add any extra time to the operating procedure, so we had to be in and out within 15 minutes. As soon as the surgeon and the medical team said ‘Go!’ we rushed into action and the patient performed the task.”
The task was a simple listen-and-repeat activity. Participants heard a series of nonsense words, like “ava,” “kug,” or “vip,” and then spoke each one aloud. The device recorded activity from each patient’s speech motor cortex as it coordinated nearly 100 muscles that move the lips, tongue, jaw, and larynx.
Afterwards, Suseendrakumar Duraivel, the first author of the new report and a biomedical engineering graduate student at Duke, took the neural and speech data from the surgery suite and fed it into a machine learning algorithm to see how accurately it could predict what sound was being made, based only on the brain activity recordings.
For some sounds and participants, like /g/ in the word “gak,” the decoder got it right 84% of the time when it was the first sound in a string of three that made up a given nonsense word.
Accuracy dropped, though, as the decoder parsed out sounds in the middle or at the end of a nonsense word. It also struggled if two sounds were similar, like /p/ and /b/.
Overall, the decoder was accurate 40% of the time. That may seem like a humble test score, but it was quite impressive given that similar brain-to-speech technical feats require hours or days-worth of data to draw from. The speech decoding algorithm Duraivel used, however, was working with only 90 seconds of spoken data from the 15-minute test.
Duraivel and his mentors are excited about making a cordless version of the device with a recent $2.4M grant from the National Institutes of Health.
“We're now developing the same kind of recording devices, but without any wires,” Cogan said. “You'd be able to move around, and you wouldn't have to be tied to an electrical outlet, which is really exciting.”
While their work is encouraging, there’s still a long way to go for Viventi and Cogan’s speech prosthetic to hit the shelves anytime soon.
“We're at the point where it's still much slower than natural speech,” Viventi said in a recent Duke Magazine piece about the technology, “but you can see the trajectory where you might be able to get there.”
This work was supported by grants from the National Institutes for Health (R01DC019498, UL1TR002553), Department of Defense (W81XWH-21-0538), Klingenstein-Simons Foundation, and an Incubator Award from the Duke Institute for Brain Sciences.
CITATION: “High-resolution Neural Recordings Improve the Accuracy of Speech Decoding,” Suseendrakumar Duraivel, Shervin Rahimpour, Chia-Han Chiang, Michael Trumpis, Charles Wang, Katrina Barth, Stephen C. Harward, Shivanand P. Lad, Allan H. Friedman, Derek G. Southwell, Saurabh R. Sinha, Jonathan Viventi, Gregory B. Cogan. Nature Communications, November 06 2023. DOI: 10.1038/s41467-023-42555-1
TO READ FULL ARTICLE AND SEE GRAPHICS CLICK HERE
US Climate Assessment: Climate Change Impacting Every Facet of American Life, Including Health

(AP - Seth Borenstein and Tammy Webber) -- Revved-up climate change now permeates Americans’ daily lives with harm that is “already far-reaching and worsening across every region of the United States,” a massive new government report says.
The National Climate Assessment, which comes out every four to five years, was released Tuesday with details that bring climate change’s impacts down to a local level. Unveiling the report at the White House, President Joe Biden blasted Republican legislators and his predecessor for disputing global warming.
“Anyone who willfully denies the impact of climate change is condemning the American people to a very dangerous future. Impacts are only going to get worse, more frequent, more ferocious and more costly,” Biden said, noting that disasters cost the country $178 billion last year. “None of this is inevitable.”
Overall, Tuesday’s assessment paints a picture of a country warming about 60% faster than the world as a whole, one that regularly gets smacked with costly weather disasters and faces even bigger problems in the future.
Since 1970, the Lower 48 states have warmed by 2.5 degrees (1.4 degrees Celsius) and Alaska has heated up by 4.2 degrees (2.3 degrees Celsius), compared to the global average of 1.7 degrees (0.9 degrees Celsius), the report said. But what people really feel is not the averages, but when weather is extreme.
With heat waves, drought, wildfire and heavy downpours, “we are seeing an acceleration of the impacts of climate change in the United States,” said study co-author Zeke Hausfather of the tech company Stripe and Berkeley Earth.
And that’s not healthy.
Climate change is ”harming physical, mental, spiritual, and community health and well-being through the increasing frequency and intensity of extreme events, increasing cases of infectious and vector-borne diseases, and declines in food and water quality and security,” the report said.
Compared to earlier national assessments, this year’s uses far stronger language and “unequivocally” blames the burning of coal, oil and gas for climate change.
The 37-chapter assessment includes an interactive atlas that zooms down to the county level. It finds that climate change is affecting people’s security, health and livelihoods in every corner of the country in different ways, with minority and Native American communities often disproportionately at risk.
In Alaska, which is warming two to three times faster than the global average, reduced snowpack, shrinking glaciers, thawing permafrost, acidifying oceans and disappearing sea ice have affected everything from the state’s growing season, to hunting and fishing, with projections raising questions about whether some Indigenous communities should be relocated.
The Southwest is experiencing more drought and extreme heat – including 31 consecutive days this summer when Phoenix’s daily high temperatures reached or exceeded 110 degrees – reducing water supplies and increasing wildfire risk.
Northeastern cities are seeing more extreme heat, flooding and poor air quality, as well as risks to infrastructure, while drought and floods exacerbated by climate change threaten farming and ecosystems in rural areas.
In the Midwest, both extreme drought and flooding threaten crops and animal production, which can affect the global food supply.
In the northern Great Plains, weather extremes like drought and flooding, as well as declining water resources, threaten an economy dependent largely on crops, cattle, energy production and recreation. Meanwhile, water shortages in parts of the southern Great Plains are projected to worsen, while high temperatures are expected to break records in all three states by midcentury.
In the Southeast, minority and Native American communities -- who may live in areas with higher exposures to extreme heat, pollution and flooding — have fewer resources to prepare for or to escape the effects of climate change.
In the Northwest, hotter days and nights that don’t cool down much have resulted in drier streams and less snowpack, leading to increased risk of drought and wildfires. The climate disturbance has also brought damaging extreme rain.
Hawaii and other Pacific islands, as well as the U.S. Caribbean, are increasingly vulnerable to the extremes of drought and heavy rain as well as sea level rise and natural disaster as temperatures warm.
The United States will warm in the future about 40% more than the world as a total, the assessment said. The AP calculated, using others’ global projections, that that means America would get about 3.8 degrees (2.1 degrees Celsius) hotter by the end of the century.
Hotter average temperatures means weather that is even more extreme.
“The news is not good, but it is also not surprising,” said University of Colorado’s Waleed Abdalati, a former NASA chief scientist who was not part of this report. “What we are seeing is a manifestation of changes that were anticipated over the last few decades.”
The 2,200-page report comes after five straight months when the globe set monthly and daily heat records. It comes as the U.S. has set a record with 25 different weather disasters this year that caused at least $1 billion in damage.
“Climate change is finally moving from an abstract future issue to a present, concrete, relevant issue. It’s happening right now,” said report lead author Katharine Hayhoe, chief scientist at the Nature Conservancy and a professor at Texas Tech University. Five years ago, when the last assessment was issued, fewer people were experiencing climate change firsthand.
Surveys this year by The Associated Press-NORC Center for Public Affairs Research show that.
In September, about 9 in 10 Americans (87%) said they’d experienced at least one extreme weather event in the past five years — drought, extreme heat, severe storms, wildfires or flooding. That was up from 79% who said that in April.
Hayhoe said there’s also a new emphasis in the assessment on marginalized communities.
“It is less a matter ... of what hits where, but more what hits whom and how well those people can manage the impacts,” said University of Colorado’s Abdalati, whose saw much of his neighborhood destroyed in the 2021 Marshall wildfire.
Biden administration officials emphasize that all is not lost and the report details actions to reduce emissions and adapt to what’s coming.
By cleaning up industry, how electricity is made and how transport is powered, climate change can be dramatically reduced. Hausfather said when emissions stops, warming stops, “so we can stop this acceleration if we as a society get our act together.”
But some scientists said parts of the assessment are too optimistic.
“The report’s rosy graphics and outlook obscure the dangers approaching,” Stanford University climate scientist Rob Jackson said. “We are not prepared for what’s coming.”
For First Time, Gene-Editing Provides Hints For Lowering Cholesterol

(Morning Edition - Rob Stein) -- For the first time, researchers have produced evidence that gene-editing can cut high cholesterol, a major risk factor for the nation's leading killer.
Preliminary results from a study involving 10 patients born with a genetic condition that causes very high cholesterol found that editing a gene inside the liver can significantly reduce levels of "bad cholesterol."
The experimental treatment needs to be tested on more patients who would be followed for much longer to confirm the approach is safe and effective. But the results are being hailed as a potential landmark proof-of-concept that could eventually provide a powerful new way to prevent heart attacks and strokes.
"These data are really very exciting," says Dr. Deepak Bhatt, director of the Mount Sinai Fuster Heart Hospital and a professor of cardiovascular medicine at Icahn School of Medicine at Mount Sinai in New York.
Bhatt, who was not involved in the research, stressed that much more research is needed to resolve important open questions. However, "this could have an enormous impact on cardiovascular disease," Bhatt says.
A new way to treat heart disease
The data from the highly anticipated study, which is being conducted by Verve Therapeutics, Inc., in Boston, were presented Sunday at an American Heart Association meeting in Philadelphia.
"What we're trying to do is develop an entirely new way to treat heart disease," Dr. Sekar Kathiresan, Verve's executive officer, told NPR in an interview. "We're super excited. This is the first-ever evidence that one can actually rewrite a single DNA letter in the human liver and have a clinical effect. So we're thrilled."
But some other independent scientists also remain cautious.
"Hopefully it will work. But there are many many aspects that are really still fuzzy," including the long-term safety, says Dr. Eric Topol, a cardiologist and professor of molecular medicine at Scripps Research in California. "There's considerable uncertainty here."
Heart disease kills about 695,000 people each year in the U.S.
High levels of a form of cholesterol known as low-density lipoprotein (LDL) cholesterol narrow arteries, blocking blood to the heart and brain and setting the stage for heart attacks and strokes.
Verve studied patients born with familial hypercholesterolemia, a genetic disorder that affects an estimated 1-in-250 people, which causes extremely high LDL.
Patients can take drugs, including a popular class known as statins, to reduce LDL levels. But while those drugs are very safe and effective, many patients fail to take them regularly as needed, leaving them vulnerable. So the hope is the gene-editing treatment could not only treat those with the genetic condition, but also provide a one-time therapy for anyone at risk.
"This same medication should be helpful for any garden-variety patient without the genetic disease," says Kathiresan.
Researchers used a form of gene-editing known as CRISPR, which enables scientists to make very precise changes in DNA much more easily than ever before. Specifically, they used a newer version of CRISPR known as "base-editing," which gives scientists the power to rewrite individual letters in the genetic code.
In this case, the editing occurred in liver cells in the organ inside the body. Other approaches to gene-editing have required removing cells from the body, editing them in the lab and then infusing them back into patients.
For the trial, which is ongoing, scientists are infusing different doses of a CRISPR base-editing molecule that makes it way to the liver to edit a gene called PCSK9, which is necessary for the production of LDL cholesterol.
Of the 10 patients treated so far, ages 29 to 69, all were in the United Kingdom and New Zealand. Only three of the patients received a dose high enough to cause a beneficial reduction in LDL. Two patients experienced reductions in their LDL levels of 39% and 48%. The one patient who received the highest dose experienced a reduction in LDL of 55% that has lasted at least six months so far.
"This is really the first-ever evidence that one can actually rewrite a single DNA letter in the liver of a living human being and have a clinical effect," Kathiresan.
Mohammed Kahn, 47, of London, was one of the most recent patients treated in the study. Kahn's father died at age 42 and two of his older brothers have already had heart attacks. Kahn's already had a procedure to treat narrowed arteries to his heart.
"It's a brilliant approach," Kahn said in an interview with NPR. "It's fantastic. I hope for the best. I'm very very optimistic that this will be working in my body."
Cholesterol treatment is just the beginning
Gene-editing is generating enormous excitement because the technique could lead to new treatments for many genetic diseases, including cancer, heart disease, AIDS, Alzheimer's and other ailments.
In fact, the Food and Drug Administration is poised to approve the first gene-editing treatment next month for the devastating blood disorder sickle cell disease.
"This is exciting for Verve, for the patients, but also more broadly if you look at my entire field," says Fyodor Urnov, professor of molecular therapeutics at University of California, Berkeley.
When he heard about the study's results, Urnov says, "My heart skipped a beat in a good way, in the hopes that these data are the first step towards a future where many peoples heart don't skip a beat and remain healthier for longer."
But others caution this approach faces a higher bar than the sickle cell treatment, especially because both are expected to cost millions of dollars per patient. Unlike for sickle cell, there are already very safe, effective and inexpensive cholesterol-lowering drugs for heart disease.
One key worry is the editing may cause inadvertent genetic changes known as "off-target" effects that could cause health problems years later.
"We don't know much about off-target effects of genome-editing," Topol says. "So even though this is targeting a specific gene that is tied to very high cholesterol, it could have other effects in the genome that are unintended."
"There are a lot of uncertainties. This is a very bold approach but we'll have to see," Topol says.
Do Twins Live Longer?

Good News If You've Had a Friend Since Birth!
(Intersetingfacts.com) -- What are the health benefits of having a close friend — like identical twins close — for your entire life? Well, according to research from the University of Washington, the positive effects on life expectancy can be astounding. In 2016, UW scientists analyzed data gathered in the Danish Twin Registry, one of the world’s oldest registries on identical and fraternal twins. The data the scientists reviewed included information on nearly 3,000 same-sex twins who survived beyond the age of 10 from 1870 to 1900. With the data being over a century old, scientists could ensure that all subjects in the study had completed their natural life spans. The study found that twins enjoyed a significantly higher survival rate compared to the overall Danish population, an advantage that peaked for male twins when they were in their mid-40s and for female twins in their early 60s. At those ages, male twins were more likely to be alive by 6 percentage points — meaning that in a group of 100 Danish men back then, if 84 were still alive at age 45, for twins the number was 90. For female twins, the difference at the peak was 10 percentage points.
While both fraternal and identical twins outperformed their non-twin counterparts, identical twins showed even greater gains in life expectancy over fraternal twins, leading scientists to theorize that identical twins perhaps form deeper bonds due to an enhanced ability to predict their sibling’s needs. The strength of social bonds in relation to health outcomes isn’t unique to twins, though. A similar effect has been observed between married, or otherwise partnered, couples and single people, which is known as the marriage protection effect. Both examples show the vital need humans have for strong social connections, and connections don’t get much stronger than the bond — and DNA — shared between identical twins.
US Childhood Vaccination Exemptions Reach Highest Level Ever, NC Exemptions Also Rising
More parents than ever are questioning routine childhood vaccinations

(AP - Mike Stobbe) -- The proportion of U.S. kindergartners exempted from school vaccination requirements has hit its highest level ever, 3%, U.S. health officials said Thursday.
More parents are questioning routine childhood vaccinations that they used to automatically accept, an effect of the political schism that emerged during the pandemic around COVID-19 vaccines, experts say.
Even though more kids were given exemptions, the national vaccination rate held steady: 93% of kindergartners got their required shots for the 2022-2023 school year, the same as the year before, the Centers for Disease Control and Prevention said in a report Thursday. The rate was 95% in the years before the COVID-19 pandemic.
“The bad news is that it’s gone down since the pandemic and still hasn’t rebounded,” said Dr. Sean O’Leary, a University of Colorado pediatric infectious diseases specialist. “The good news is that the vast majority of parents are still vaccinating their kids according to the recommended schedule.”
All U.S. states and territories require that children attending child care centers and schools be vaccinated against a number of diseases, including, measles, mumps, polio, tetanus, whooping cough and chickenpox.
All states allow exemptions for children with medical conditions that prevents them from receiving certain vaccines. And most also permit exemptions for religious or other nonmedical reasons.
In the last decade, the percentage of kindergartners with medical exemptions has held steady, at about 0.2%. But the percentage with nonmedical exemptions has inched up, lifting the overall exemption rate from 1.6% in the 2011-2012 school year to 3% last year.
Last year, more than 115,000 kindergartners were exempt from at least one vaccine, the CDC estimated.
Ten states — all in the West or Midwest — reported that more than 5% of kindergartners were exempted from at least one kind of required vaccine. Idaho had the highest percentage, with 12% of kindergartners receiving at least one exemption. In contrast, 0.1% had exemptions in New York.
The rates can be influenced by state laws or policies can make it harder or easier to obtain exemptions, and by local attitudes among families and doctors about the need to get children vaccinated.
“Sometimes these jumps in exemptions can be very local, and it may not reflect a whole state,” said O’Leary, who chairs an American Academy of Pediatrics committee on infectious diseases.
Hawaii saw the largest jump, with the exemption rate rising to 6.4%, nearly double the year before.
In North Carolina, non-medical exemptions rose from 0.7 percent to 1.8 percent over a decade through the 2021-22 school year, the most recent CDC data show.
Officials there said it’s not due to any law or policy change. Rather, “we have observed that there has been misinformation/disinformation impacting people’s decision to vaccinate or not via social media platforms,” officials at the state’s health department said in a statement.
Connecticut and Maine saw significant declines, which CDC officials attributed to recent policy changes that made it harder to get exemptions.
Health officials say attaining 95% vaccination coverage is important to prevent outbreaks of preventable diseases, especially of measles, which is extremely contagious.
The U.S. has seen measles outbreaks begin when travelers infected elsewhere came to communities with low vaccination rates. That happened in 2019 when about 1,300 measles cases were reported — the most in the U.S. in nearly 30 years. Most of the cases were in were in Orthodox Jewish communities with low vaccination rates.
One apparent paradox in the report: The national vaccination rate held steady even as exemptions increased. How could that be?
CDC officials say it’s because there are actually three groups of children in the vaccination statistics. One is those who get all the shots. A second is those who get exemptions. The third are children who didn’t seek exemptions but also didn’t get all their shots and paperwork completed at the time the data was collected.
“Last year, those kids in that third group probably decreased,” offsetting the increase in the exemption group, the CDC’s Shannon Stokley said.
Additional Reading
Centers for Disease Control and Prevention
NCDHHS: Public Health Alert for Congenital Syphilis
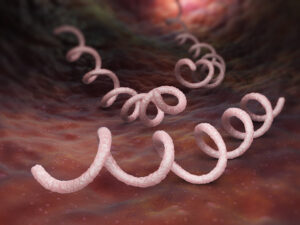
The North Carolina Department of Health and Human Services has issued a public health alert for congenital syphilis.
Five syphilis-related stillbirth or neonatal deaths in babies have been reported so far in 2023. None were reported in 2022.
From 2012 to 2022 there was a 547% increase in reported syphilis cases among women with an associated 5600% increase in congenital syphilis infections.
This increase mirrors the national trend as described this week by the Centers for Disease Control
Cases are Rising
Congenital syphilis infections are on the rise in North Carolina and they are PREVENTABLE by early detection and rapid treatment of the mother's infection.
NCDHHS is working to improve access to testing, as well as community awareness about this growing epidemic, so that pregnant women and the people who love them have access to information and treatment.
North Carolina Case Review Findings
Findings of congenital syphilis cases in North Carolina from 2016 to 2022 indicate infants end up with congenital syphilis when:
- There is no or late entry of pregnant women into prenatal care.
- There was prenatal care but incomplete syphilis testing during pregnancy.
- Mother received delayed, no, or inadequate treatment for her stage of syphilis infection.
- The exposed newborn was not appropriately evaluated or treated at birth for congenital syphilis.
36% Increase in congenital syphilis cases in 2022

Your Role as a Provider
As a clinician, you play an important role in preventing congenital syphilis. Here's how you can do your part:
- Complete a sexual health history for all your patients.
- Test all pregnant women for syphilis at the first prenatal visit, between 28-30 weeks gestation, AND at delivery (this is required by NC state law).
- Treat patients with syphilis immediately and per the CDC STI treatment guidelines. If you do not have access to benzathine penicillin, contact your local health department immediately.
- Advise your patients to notify all sex partners of their exposure to prevent re-infection. People can anonymously notify sex partners using TellYourPartner.org.
- Know mother’s delivery syphilis test results before the newborn goes home.
-
Immediately report syphilis and congenital syphilis infections to Public Health.
ADDITIONAL READING
Congenital Syphilis Resource Page
NCMS: Spike in Syphilis Cases in Newborns Leading to Stepped-Up Prevention Measures
Continued Rise in Female and Congenital Syphilis Infections
The Time is Now to Vaccinate Your Patients, FDA Greenlights Novavax Updated COVID Vaccine
Novavax COVID-19 Vaccine, Adjuvanted (2023-2024 Formula) is now authorized and ACIP recommended
Now that Novavax COVID-19 Vaccine, Adjuvanted (2023-2024 Formula) has received FDA authorization for emergency use in the US for individuals aged 12 and older, it is also included in ACIP’s recommendation for use of authorized/approved 2023-2024 XBB COVID-19 vaccines. The vaccine was studied globally in approximately 45,000 participants.1
Limitations of Vaccine Effectiveness: The Novavax COVID-19 Vaccine, Adjuvanted may not protect all vaccine recipients.
When you discuss the Novavax COVID-19 vaccine to your patients, you're helping them choose the only non-mRNA COVID-19 vaccine option built on a well-established protein subunit platform. This is similar to how some vaccines, such as hepatitis B or flu, are made.2
The Novavax COVID-19 vaccine is available through these distributors:
Cardinal Health, Inc.: 1-833-358-8326
FFF Enterprises, Inc.: 1-800-843-7477
Henry Schein, Inc.: 1-800-772-4346
McKesson Medical-Surgical, Inc.: 1-855-571-2100
McKesson Plasma & Biologics: 1-855-571-2100
AmeriSource Bergen or Cencora: 1-855-571-2100
LEARN MORE ABOUT THE NOVAVAX COVID-19 VACCINE HERE
Please see Important Safety Information below.
Emergency Use Authorization (EUA)
The Novavax COVID-19 Vaccine, Adjuvanted (2023-2024 Formula) has not been approved or licensed by the FDA, but has been authorized for emergency use by FDA, under EUA to prevent Coronavirus Disease 2019 (COVID-19) for use in individuals 12 years of age and older.
The emergency use of this product is only authorized for the duration of the declaration that circumstances exist justifying the authorization of emergency use of the medical product under Section 564(b)(1) of the FD&C Act unless the declaration is terminated or authorization revoked sooner.
To learn more about the robust efficacy of the Novavax COVID-19 Vaccine, please visit us.novavaxcovidvaccine.com/hcp.
IMPORTANT SAFETY INFORMATION
Authorized Use
Individuals previously vaccinated with any COVID-19 vaccine: A single dose is administered at least 2 months after receipt of the last previous dose of COVID-19 vaccine. Individuals not previously vaccinated with any COVID-19 vaccine: Two doses are administered 3 weeks apart. The safety data for Novavax COVID-19 Vaccine, Adjuvanted (2023-2024 Formula) are based on studies of the Novavax COVID-19 Vaccine, Adjuvanted (Original monovalent) [no longer authorized for use in the U.S.] and of the Novavax monovalent vaccine (Omicron BA.1); bivalent vaccine (Original and Omicron BA.1); bivalent vaccine (Original and Omicron BA.5); and monovalent vaccine (Omicron BA.5) [none of which has been authorized or approved in the U.S.].
Contraindications
Do not administer the Novavax COVID-19 Vaccine, Adjuvanted to individuals with a known history of a severe allergic reaction (e.g., anaphylaxis) to any component of the Novavax COVID-19 Vaccine, Adjuvanted, or to individuals who had a severe allergic reaction (e.g., anaphylaxis) following a previous dose of a Novavax COVID-19 Vaccine, Adjuvanted.
Warnings and Precautions
Management of Acute Allergic Reactions: Appropriate medical treatment to manage immediate allergic reactions must be immediately available in the event an acute anaphylactic reaction occurs following administration of the Novavax COVID-19 Vaccine, Adjuvanted. Monitor Novavax COVID-19 Vaccine, Adjuvanted recipients for the occurrence of immediate adverse reactions according to the Centers for Disease Control and Prevention guidelines.
Myocarditis and Pericarditis: Clinical trials data provide evidence for increased risks of myocarditis and pericarditis following administration of the Novavax COVID-19 Vaccine, Adjuvanted (see Full EUA Fact Sheet). The CDC has published considerations related to myocarditis and pericarditis after vaccination, including for vaccination of individuals with a history of myocarditis or pericarditis https://www.cdc.gov/vaccines/covid-19/clinical-considerations/interim-considerations-us.html#myocarditis-pericarditis
Syncope (fainting): May occur in association with administration of injectable vaccines. Procedures should be in place to avoid injury from fainting.
Altered Immunocompetence: Immunocompromised persons, including individuals receiving immunosuppressant therapy, may have a diminished immune response to the Novavax COVID-19 Vaccine, Adjuvanted.
Limitations of Vaccine Effectiveness: The Novavax COVID-19 Vaccine, Adjuvanted may not protect all vaccine recipients.
Adverse Reactions
Adverse reactions reported in clinical trials following administration of the Novavax COVID-19 Vaccine, Adjuvanted include injection site pain/tenderness, fatigue/malaise, muscle pain, headache, joint pain, nausea/vomiting, injection site redness, injection site swelling, fever, chills, injection site pruritus, hypersensitivity reactions, lymphadenopathy-related reactions, myocarditis, and pericarditis.
Myocarditis, pericarditis, anaphylaxis, paresthesia, and hypoesthesia have been reported following administration of the Novavax COVID-19 Vaccine, Adjuvanted outside of clinical trials. Additional adverse reactions, some of which may be serious, may become apparent with more widespread use of the Novavax COVID-19 Vaccine, Adjuvanted.
Reporting Adverse Events and Vaccine Administration Errors
The vaccination provider enrolled in the federal COVID-19 Vaccination providers must report the events listed below following administration of the Novavax COVID-19 Vaccine, Adjuvanted (2023-2024 Formula) to the Vaccine Adverse Event Reporting System (VAERS):
- vaccine administration errors whether or not associated with an adverse event,
- serious adverse events (irrespective of attribution to vaccination),
- cases of myocarditis,
- cases of pericarditis,
- cases of Multisystem Inflammatory Syndrome (MIS)
- cases of COVID-19 that results in hospitalization or death
Complete and submit reports to VAERS online: https://vaers.hhs.gov/reportevent.html. For further assistance with reporting to VAERS, call 1-800-822-7967. The reports should include the words “Novavax COVID-19 Vaccine, Adjuvanted (2023-2024 Formula) EUA” in the description section of the report.
To the extent feasible, report adverse events to Novavax, Inc. using the following contact information or by providing a copy of the VAERS form to Novavax, Inc. Website: www.NovavaxMedInfo.com, Fax Number: 1-888-988-8809, Telephone Number: 1-844-NOVAVAX (1-844-668-2829).
Please see the Novavax COVID-19 Vaccine, Adjuvanted (2023-2024 Formula) Fact Sheet for Healthcare Providers Administering Vaccine (Vaccination Providers) and EUA Full Prescribing Information.
References: 1. Novavax COVID-19 Vaccine, Adjuvanted EUA Fact Sheet for Healthcare Providers. Novavax Inc. October 2023. 2. U.S. Department of Health & Human Services. Vaccine Types. https://www.hhs.gov/immunization/basics/types/index.html. Updated July 7, 2021. Accessed August 7, 2023.
Additional Reading
FDA greenlights Novavax's updated COVID vaccine
NCDHHS Contacting 300,000 People Eligible for Full Medicaid Benefits Starting December 1

Up to 300,000 People Receiving Notifications of Benefits Starting Dec. 1
Because of Medicaid Expansion
This week, NCDHHS began contacting up to 300,000 people via text messages, calls and emails who are enrolled in Medicaid’s limited family planning program to let them know they will be eligible for full NC Medicaid benefits starting Dec. 1.
Up to 300,000 people who are enrolled in Medicaid’s limited family planning program will receive a letter from their local Department of Social Services (DSS) letting them know they will receive full coverage on Dec. 1. They will also receive a packet from their health plan that includes a new Medicaid ID card. Additionally, anyone with health coverage through HealthCare.gov will need to cancel their plan once they are enrolled in NC Medicaid.
Not everyone with limited family planning program benefits will be automatically enrolled in full coverage through NC Medicaid. Some people may have income that exceeds the new Medicaid eligibility levels, even though qualifying income levels are higher than in the past. If your income has recently changed and you think you may be eligible, update your information in ePASS or by contacting your local DSS.
For more information about expanded eligibility for NC Medicaid, go to the NCDHHS website where you will find a toolkit of resources for organizations to spread the word to their communities.
Making Children Smile! Tech Transforms Casts into Works of Art

(Courtesy: Lauren Hando) -- This orthopedic technician can now add “artist” to his resume. Luis Ruiz, who works at Children’s Hospital Los Angeles, transforms his young patients’ casts into adorable pieces of art.
Ruiz has painted thousands of casts over the past decade or so, customizing the plaster with everything from cartoon characters to sports teams.
And while the best part for the children may be admiring the artwork, for him, it’s seeing their smiles.
“The kids just bring me joy,” Ruiz told People. “I’m kind of a fun guy and a little kid myself inside, and I like having fun and making kids smile, and they make me smile.”
It all began “about 10 years ago, [when] a little boy asked me to draw a happy face on his cast,” he recalled. Though he was initially hesitant, Ruiz agreed after the youngster continued to insist on the drawing. He had warned him, “‘You know what, I’m really not good at drawing. I’d rather not. I might mess it up.'”
But after seeing the little boy’s reaction to his art, Ruiz became inspired to share his artistic talents with all the children in need of casts.
Ruiz has come a long way since drawing that smiley face. He began with permanent markers, but now uses oil-based paint pens as they work better on the material.
“I was not very good,” Ruiz shared. “But as time went by, little by little, I got better and better, to a point where now I can almost do anything they ask for.”

More than anything, these drawings give the children something fun to talk about “instead of having to explain what happened to them.”
One of his most memorable cast paintings was for a young girl with cancer who wanted a Wonder Woman emblem.
“It made her very happy to go around with that [drawing], because she got a lot of compliments on it,” Ruiz explained.
His work shows what a big impact a little paint can have.
On The Lighter Side - Halloween Edition!
Here are some things NCMS employees, members, and YOU are talking about this Weekend and Beyond!
Fall Temps are Bringing Lots of Concerts to North Carolina!

Friday
- Joan Baez, The Cary Theater, Cary
- Lorrie Morgan, Givens Performing Arts Center, Pembroke
- Dropkick Murphys, White Oak Amphitheater, Greensboro
- North Carolina Symphony, Martin Marietta Center, Raleigh
- Paw Patrol Live! The Great Pirate Adventure, Ovens Auditorium, Charlotte
- Wheel of Fortune Live! Tanger Center, Greensboro
Saturday
- Nick Offerman, Tanger Center, Greensboro
- Buddy Guy, Harrah's Cherokee Casino, Cherokee
- North Carolina Symphony - Halloween Spooktacular, Martin Marietta Center, Raleigh
- Luke Bryan, Credit One Stadium, Charleston, SC
Sunday
- Matthew West, RJ Reynolds Auditorium, Winston-Salem
- John Cleese, DPAC, Durham
- North Carolina Opera presents La Traviata, Martin Marietta Center, Raleigh
Fall also means lots and lots of sports action across the state!

Friday
- Charlotte Hornets vs Detroit Pistons, Spectrum Center, Charlotte
- Carolina Hurricanes vs. San Jose Sharks, PNC Arena, Raleigh
Saturday
- Florida State at Wake Forest, noon
- Clemson at NCSU, 2pm
- Duke at Louisville, 3:30pm
- UNC at Georgia Tech, 8pm
Sunday
- Carolina Panthers vs. Houston Texans, Bank of America Stadium, Charlotte
DON'T FORGET IT'S HALLOWEEN!!!

Here is a list of events happening across the state until Tuesday!
- Blowing Rock Halloween Festival, Saturday 3-8pm, Blowing Rock Parks and Rec. Center
- Halloween in Huntersville, Saturday 5:30pm, Huntersville
- Halloween Fun Fest, Saturday 7-10pm, Salisbury
- Halloween Double Feature, Saturday 6-11pm, Dorothea Dix Park, Raleigh
- Halloween Hootenanny, Friday and Saturday, Bryson City
- Beary Scary Halloween, Grandfather Mountain, Linville
- Halloween at Boo-tanical Garden, Cape Fear Botanical Garden, Fayetteville
- Boollantyne, The Amp Ballantyne, Charlotte
- Kooky Spooky, Friday, Marbles Kids Museum, Raleigh
If you have an event you would like added to On The Lighter Side, email Randy Aldridge at [email protected].
CDC: Health Workers Facing Mental Health Crisis

(CNN) -- Researchers from the US Centers for Disease Control and Prevention are sounding the alarm on a mental health crisis for health workers around the country.
Using nationwide survey data between 2018 and 2022, a new report from the agency found that nearly half of health workers reported feeling burned out in 2022, up from under a third four years prior. Health workers’ reports of being harassed at work more than doubled, as well.
The report, released on Tuesday, also shows that health workers face worse mental health outcomes than employees in other industries.
The findings come on the heels of the largest health care worker strike in US history, in which 75,000 unionized employees of Kaiser Permanente cited feelings of burnout and chronic staffing shortages during a walkout in five states and the District of Columbia.
“While usually health workers care diligently for others in their time of need, it is now our nation’s health workers who are suffering, and we must act,” said Dr. Debra Houry, the CDC’s chief medical officer.
Even before the pandemic, Houry added, health workers’ jobs were demanding: Providers face long hours and unpredictable schedules, exposure to infectious diseases, and often-challenging interactions with patients and their families.
Previous research has found that health care workers — especially nurses, health support workers and health technicians — face an increased risk of suicide compared with people who don’t work in the medical field.
“Caring for people who are sick can also be intensely stressful and emotional,” Houry said. “Although you do everything you can to save a life, I still remember some of the tough patient cases I had, where I gave the bad news about an advanced cancer diagnosis to a working spouse or the time I was unable to resuscitate the young toddler after a car crash.
“After a shift like this, I would have to put on a good front and take care of my own family. And in doing this, I didn’t always pay enough attention to my own wellness needs.”
According to Houry, the Covid-19 pandemic made workplace challenges worse, with health care providers facing a wave of patients, long hours and supply shortages. Those stresses fueled a rise in mental health complications, suicidal ideation, and like large parts of the US adult population, substance abuse challenges.
The study found that health care workers reported an increase in poor mental health days between 2018 and 2022. In the survey, 44% of health workers reported wanting to look for a new job, up from 33% in 2018.
In contrast, the number of other essential workers who intended to look for a new job dropped over the same period.
Meanwhile, the number of health care workers who experienced harassment — including violent threats, bullying and verbal abuse from patients and coworkers — shot up from 6% to 13% during the study period.
According to the CDC report, harassment had major impacts on health workers’ mental health: Health workers who reported being harassed were 5 times as likely to report anxiety compared to those who were not. Those who faced harassment were over three times as likely to report depression and nearly six times as likely to report burnout, as well.
For instance, 85% of health workers who experienced harassment reported feeling anxiety, compared with 53% of those who did not. Sixty percent of harassment victims reported experiencing depression, nearly double the number of health workers who had not suffered harassment.
Those consequences, however, are preventable with improved workplace policies and practices, the report says.
The study found that health workers who trusted their management, had enough time to complete their work and received support from supervisors were less likely to report burnout.
“We’re calling on employers to take this information to heart and take immediate preventive actions,” said Casey Chosewood, director of the National Institute for Occupational Safety and Health’s Office for Total Worker
The report also recommended that employers encourage “cross-level employee participation” in decision-making: health workers who helped with decision-making had about half the likelihood of reporting depression symptoms. Chosewood recommended that supervisors support their employees by monitoring staffing needs and seriously addressing harassment reports.
The CDC’s National Institute for Occupational Safety and Health also plans to launch a national campaign this fall to help hospital leaders address challenges to health workers’ well-being — part of an ongoing initiative by the agency to raise awareness about health workers’ mental health challenges.
“The bottom line is this: We must take the research we have and act,” Chosewood said. “To label our current and long-standing challenge a ‘crisis’ is an understatement. Patients in our communities, really all of us, will fare better when our health workers are thriving.”
Health. “Supportive work environments had a positive impact on health workers.”
TO READ FULL REPORT FROM CENTERS FOR DISEASE CONTROL AND PREVENTION CLICK HERE.
NCDHHS Encouraging Mpox Vaccinations After New Cases Reported
NCDHHS Encourages Mpox Vaccination for People at Higher Risk After Recent Cases Reported

In addition to the two cases, the mpox virus was recently detected in one out of 12 wastewater sites where monitoring is being conducted. These cases and wastewater detections were all in different counties, suggesting an increased spread of mpox in North Carolina.
Numbers and cases have been low due to vaccinations and community engagement, but now is the time to get vaccinated if you are at higher risk for mpox and have not yet received the vaccine. Eligibility criteria have expanded to include:
- Anyone who has or may have multiple or anonymous sex partners;
- Anyone whose sex partners are eligible per the criteria above;
- People who know or suspect they have been exposed to mpox in the last 14 days;
- Anyone else who considers themselves to be at risk for mpox through sex or other intimate contact.
Take steps to lower your risk during sex or at social gatherings, like using a condom correctly every time you have sex. Avoid close contact with people who have a rash that looks like mpox, avoid contact with objects and materials a person with mpox has used and wash your hands often.
Read more about how the disease is spread, symptoms of mpox, and what NCDHHS is doing to enhance communication efforts with local health departments and community partners, in a news release.
NC Universities Setting New Revenue Records From Research, Tech Created by Students and Faculty
Duke University brings in record money from its startups and technology

(Axios Raleigh - Zachery Eanes) -- The Triangle's research universities are setting new revenue records from research and technology created by their students and faculty.
Driving the news: Duke University reported bringing in a massive $102.5 million in licensing and equity payments from technology and startups formed on its campus in its fiscal year 2023, which ended June 30.
- It caps an incredibly consistent run by the university, which has brought in more than $50 million via technology created on the campus for the past five years.
Why it matters: The Triangle university ecosystem — the origin of the Research Triangle moniker — has long been the economic backbone of the region, reliably attracting talent, jobs, and money to the region.
- The startups formed by their faculty and students have gone on to become some of its largest employers, including names like Quintiles, now known as IQVIA (UNC); SAS Institute and Wolfspeed (N.C. State); Precision Biosciences (Duke) and RTI International (all three universities).
State of play: The universities have, over the past decade, become much more focused on turning the intellectual property formed on their campuses into financial windfalls.
- In addition to Duke's success, UNC broke its licensing and equity record in 2021 (thanks to Bayer's $4 billion acquisition of Chapel Hill-founded gene therapy company AskBio).
- And since 2015, N.C. State has formed the most startups of any school in the area.
What's happening: Duke can attribute its success to a hot streak of drugs entering the market as well as startups filing for initial public offerings or being acquired, according to Robin Rasor, the school's associate vice president of translation and commercialization.
- In its past fiscal year, five Duke-related startups were acquired, including Durham-based Isolere Bio and InnAVasc Medical.
- The school has also seen six different IPOs in the past five years, which has provided a reliable stream of equity payments.
- Duke Capital Partners, the university's early-stage investment firm, has also become more active in supporting young startups with capital, including investing $10.8 million into 12 startups in fiscal year 2023.
What they're saying: Rasor, who has worked at universities for three decades, said there's been a big shift within schools in recent years.
- Younger faculty are more interested in forming companies, she said, and universities are providing more infrastructure for them to do so.
- "Most of the [faculty] recruits coming in are already innovators ... and they're very interested in what the [startup] environment is going to be like," Rasor told Axios. "That's a big change, and … it's important to have that kind of environment so we can recruit the best and the brightest."
What we're watching: Of the 15 startups formed at Duke in the past year, 66% are headquartered in North Carolina.
- That's a decline from previous years, according to Rasor, who said remote work trends may be leading to more of the university's startups to relocate — even as more Duke students seem to be staying in the area after graduation.
- She said the Triangle's critical mass of talent continues to improve but many startups still weigh whether Boston or the Bay Area might be a better fit.
Register Here for Addiction Medicine Learning Series Webinars
Starting January 2023, all DEA-registered practitioners are required to participate in 8 hours of training in addiction medicine. This Addiction Medicine Series meets the requirements set forth by the DEA and provides participants a broad overview on addiction treatment. This series provides education on a variety of key topics in addiction medicine, including inequities in addiction, impacts of stigma, basics about addiction treatment, integrating addiction treatment in the primary care setting, and treatment of substance use in special populations including the adolescent population, those with mental illness and those with chronic pain.
The registration links for all 8 models are included below:
The End of a Bygone Era: Removal of the X-waiver Next Steps in Buprenorphine Prescribing
Addiction In Primary Care
Responding to Pediatric Substance Use
Treating Chronic Pain and Addictions
Understanding the Impacts of Stigma: Substance Use Disorder
Addiction and Mental Illness
The Impact of Stigma and Bias on Substance Use Disorder Diagnosis and Treatment
Current State of MOUD Access
Additional Resources Related to These Topics
Duke's first Nobel Prize Winner, Robert Lefkowitz, Celebrates 50 Years!
Nobel Laureates Highlight Symposium Celebrating Robert J. Lefkowitz’s 50 Years at Duke
(Durham, Duke Med School - Dave Hart) -- After completing a residency and fellowship at Harvard and Massachusetts General Hospital, Robert J. Lefkowitz, MD, arrived at Duke University School of Medicine to begin his first faculty job in the summer of 1973. 
He’s been here ever since — conducting pioneering research that has changed the landscape of medicine, mentoring more than 200 trainees, and becoming Duke University’s first Nobel Prize winner, when he was awarded the 2012 prize in chemistry.
On Oct. 2-3, the School of Medicine hosted a remarkable gathering of luminaries (including seven Nobel Laureates, two former chancellors, and a five-time NCAA championship men’s basketball coach) for a symposium to celebrate Lefkowitz’s 50 years at Duke and the discoveries that advance human health.
Duke University Executive Vice President for Health Affairs and School of Medicine Dean Mary E. Klotman, MD, welcomed the large audience in Page Auditorium. She noted that Lefkowitz’s rise as a pioneering biomedical scientist and Duke’s rise as a world-class biomedical institution went hand in hand. Duke provided Lefkowitz with the resources, intellectual freedom, and trainees and colleagues to pursue his groundbreaking research. In turn, his excellence, mentorship, and championing of basic science have attracted other top scientists and elevated Duke’s research environment.

“Duke wouldn’t be the same if not for Bob, and Bob wouldn’t be the same if not for Duke,” she told the large audience. “We are here to celebrate the golden anniversary of a remarkable relationship.”
The event featured lectures by some of the world’s leading researchers, reminiscences from some of Lefkowitz’s closest friends and colleagues, and words of wisdom for students, trainees, and junior faculty about how to achieve and sustain success, in science and in life.
Participants included Nobel Prize Laureates Peter Agre, MD; Michael S. Brown, MD; Joseph Goldstein, MD; Roderick MacKinnon, MD; Stanley Prusiner, MD; Harold E. Varmus, MD; and Brian Kobilka, MD, who was a postdoctoral fellow in Lefkowitz’s lab and shared the 2012 Nobel Prize.
Also taking the stage were leading scientists including Helen H. Hobbs, MD; Gary H. Gibbons, MD; Irving L. Weissman, MD; and Stuart H. Orkin, MD, as well as a host of Duke leaders past and present. Lefkowitz and Klotman joined Duke University President Vincent E. Price, PhD, and former Duke men’s basketball coach Mike Krzyzewski for a lively panel discussion on “Sustaining Success in the Spotlight.”
Chancellor Emeritus for Health Affairs Victor J. Dzau, MD, recalled “how exciting it was to be here as chancellor and bathe in his glory” when Lefkowitz won the 2012 Nobel Prize for his pioneering research on G-protein coupled receptors, which provided the targets for more than one-third of all current prescription drugs.
“For fifty years Bob has been an icon, a role model, and a scientist whose contributions have changed and saved so many lives,” said Dzau, now president of the National Academies of Sciences, Engineering, and Medicine.
Agre, who won the 2003 Nobel Prize in Chemistry and was vice chancellor for science and technology at Duke from 2005-2008, presented his recent research on malaria in sub-Saharan Africa. He also recalled the moment that all Nobel Laureates remember: that life-changing phone call from Sweden. “It’s a very pleasant experience,” he admitted.
Goldstein, who won the 1985 Nobel Prize in Physiology or Medicine, first met Lefkowitz in 1968 when they were in the same cohort of “Yellow Berets” — young physicians commissioned into the National Institutes of Health and the Public Health Service during the Vietnam War. He urged young researchers to approach science with a sense of adventure.
“Have the courage to take risks,” he said. “Try new approaches and avoid bandwagon research. If scientists don’t take risks, science will stagnate.”
Varmus, who won the Nobel Prize in Physiology or Medicine in 1989, was a medical school classmate of Lefkowitz’s at Columbia and also a fellow Yellow Beret.
“The scientific life has changed in many ways, but discovery remains a joy,” Varmus said. “The path to a career is longer and harder, but there are more branches to choose from. The demography of science has become more diverse, but we still have a long way to go. Basic and applied science have moved closer together, but the demand for application threatens broad inquiry. One thing remains the same: friendships are essential for a fulfilling life in science.”
One of Lefkowitz’s closest friends, Duke Chancellor Emeritus for Health Affairs Ralph Snyderman, MD, joined the faculty in 1972, just before Lefkowitz did. The two soon took up the habit of running together — an activity they continued, five or six days a week, for some 30 years.
“We once calculated that we ran over 50,000 miles together,” Snyderman said. “We were like brothers without the sibling rivalry. What I think differentiates Bob as a scientist is the courage to do the really hard experiments and the persistence to stick with it. He has incredibly high standards. He’s totally focused, and he is totally committed to the people who work with him.”
Lefkowitz himself spoke passionately about the need for young scientists to find the right mentor. For many of them over the past 50 years, that mentor has been Lefkowitz: many of his trainees have achieved great prominence and won major awards, including the Nobel Prize. He succeeds, he said, when they succeed.
“I’ve never led anything bigger than my lab,” he said. “But I’ve tried very hard to help my trainees use their powers to maximum effect. Training in science is an apprenticeship. It’s experiential. It requires you to pour yourself completely into your goal.”
Lefkowitz, who turned 80 in April, was moved by the large contingent of alumni from his lab who returned to Duke to reconnect and share in the celebration.
“What an incredible few days we just shared,” he said. “I want to thank everybody who took the time to join in, and especially those who came from long distances to help me celebrate these two very special landmarks in my life. Never have the words been truer than when I say, ‘I couldn't have done it without you.’”
Duke School of Medicine Makes Surprise Discovery That Could Change MS Treatments
Surprise Discovery Reveals Key Factor in Multiple Sclerosis

(Duke Med School - Shantell M. Kirkendoll) -- Researchers at Duke University School of Medicine studying multiple sclerosis made an unexpected discovery that could reshape the understanding of MS treatments.
They identified a protein that boosts the aggressive migration of immune cells into the central nervous system which leads to MS, an autoimmune disease affecting about 1 million adults in the United States. The intrusion of a specific type of immune cell called Th17 is particularly harmful to the brain and spinal cord.
But when Duke scientists blocked the protein integrin α3, slowing Th17 cells from reaching and damaging the central nervous system, they saw major improvement in mice, according to a study published Oct. 13 in Science Immunology.
“We were studying the role of another gene when we stumbled upon integrin α3,” said co-lead author Maria Ciofani, PhD, associate professor in the Department of Integrative Immunobiology at Duke School of Medicine. “We found that when it’s missing, the Th17 cells don’t develop as effectively, and more importantly, they face difficulties entering the central nervous system. This means less damage.”
The Th17 cells, which are vital for the body to fight fungal and bacterial infections, don’t usually cause diseases. But for people with MS, these cells are mistakenly activated and end up attacking the central nervous system.
The Duke team is the first to reveal the selective abundance of integrin α3 on Th17 cells. The protein helps Th17 cells to form connections with other cells, which in turn helps the cells grow and become more aggressive.
But in the absence of the protein, Th17 cells get locked outside the blood-brain barrier, the brain’s protective shield.
While probing inflammatory T cells and disabling a particular gene—a routine practice to grasp its function—researchers stumbled upon a surprise. The altered mice were fully shielded from the MS-like symptoms typically seen in such models.
“They were walking around like nothing happened,” Ciofani said. “When we looked carefully, we found that none of the Th17 cells were entering the central nervous system. It was an opportunity to look at the machinery that controls these cells.”
With the help of computational approaches, Ciofani's team, including co-lead study author Eunchong Park, PhD, identified integrin α3. Park, a scientist at AstraZeneca, is a former graduate student in the Department of Integrative Immunology and member of the Center for Advanced Genomic Technologies.
There’s currently no MS drug that targets integrins on Th17 cells, but the drug natalizumab does target another kind of T cell, Th1 cells, that can also contribute to MS. But natalizumab has its side effects, emphasizing the need for alternative treatments.
“One concern about targeting integrin α3 is that these Th17 cells are vital for our body’s defense against infections,” Ciofani said. “We’ve done preliminary tests to see if inhibiting integrin α3 stops Th17 cells from performing their protective roles, and so far, it seems they can still do their jobs.”
Since integrin α3 is so essential for the harmful actions of Th17 cells, it could be a potential target for new MS treatments.
If scientists could develop a drug that blocks or reduces the function of this protein, it might reduce the severity of MS or prevent its onset.
Additional Duke authors include William E. Barclay; Alejandro Barrera; Tzu-Chieh Liao, Harmony R. Salzler; Timothy E. Reddy; and Mari L. Shinohara.
Funding was provided by National Institute of Health grants R01-GM115474; R01-AI156186; R01-NS120417; RG-4536B2/1; and UM1-HG009428 and a Kwanjeong Educational Foundation Scholarship.
2023 LEAD Recap: State Health Director Gives Annual Report to NCMS
 The 2023 LEAD Conference featured several panels and speakers over two days and a highlight was the annual report from the Department of Health and Human Services. On Saturday, Elizabeth Cuervo Tilson, MD, MPH, State Health Director and Chief Medical Officer offered the annual report to the NCMS. Here are some highlights of her report:
The 2023 LEAD Conference featured several panels and speakers over two days and a highlight was the annual report from the Department of Health and Human Services. On Saturday, Elizabeth Cuervo Tilson, MD, MPH, State Health Director and Chief Medical Officer offered the annual report to the NCMS. Here are some highlights of her report:
EXECUTIVE SUMMARY
As the world continues to recover from one of the largest public health threats in recent history, this past year in North Carolina heralded a transition from COVID-19-specific recovery efforts to broader initiatives aimed at safeguarding and bolstering the overall health of North Carolinians. We leveraged the invaluable lessons learned and the partnerships fortified throughout the pandemic to continue to improve our responses to health challenges. Systems that have been chronically underfunded were further strained by the stressors of the pandemic, mandating thoughtful strategic investment in those systems. We have prioritized activities to advance whole person health and created roadmaps for strategic investment in the health of our people. This annual report outlines our national, state level, and agency strategic priorities and programming to further our commitment to health and opportunity for every North Carolinian.
America’s Health Rankings serves as an annual report for states built upon the World Health Organization’s definition of health. North Carolina’s overall health ranking relative to other U.S. states has consistently improved annually, evidencing our public health successes. In the 2022 Annual Report, North Carolina was ranked 30, up from 34 and 41 in the prior two years, respectively. As in years past, many health indicators on which North Carolina needs to improve are driven in part by North Carolina’s large uninsured population.
Medicaid expansion was signed into law by Governor Roy Cooper in March 2023 and represents a critical step forward to improve the health of North Carolinians and enable a substantial economic investment in the state. Operationalization of Medicaid expansion will be an integral step to improve health in North Carolina. The North Carolina Department of Health and Human Services was given final authority to implement Medicaid expansion through enactment of the state budget in early October, allowing for a launch date of December 1, 2023. We have a new website, bilingual toolkit and a sign-up form to stay updated on the most current information and share with your partners, patients, and stakeholders.
Healthy North Carolina 2030, released in 2020, lays out 21 ambitious, population-level goals and shared objectives for the entire state to solve “wicked problems” and improve the health of North Carolinians for this decade. It aims to mobilize and coordinate a broad array of private sector, public sector, and community organizations that can play a role in making North Carolinians healthier. The North Carolina State Health Improvement Plan (NC SHIP) builds upon HNC 2030 to help create a unified strategy across multiple stakeholders to drive improvement in the indicators throughout the decade covered by HNC 2030. The NC SHIP documents are iterative, describe the process for improvement, and report on progress of any improvements. 2023 NCSHIP lays out the efforts of statewide cross-sector collaboration and launches a Year of Action.
NCDHHS works toward five strategic priorities, guided by our strategic plan. Three priorities are areas of activity that bring together multiple divisions and external partners. They are Behavioral Health and Resilience, Child and Family Well-being, and a Strong and Inclusive Workforce. Two priorities are fundamental ways that we approach our work across the department. Our Health Equity Portfolio synthesizes and guides efforts across NCDHHS and beyond to erase gaps in whole-person health. Our Data Office works the numbers to tell us how we are doing.
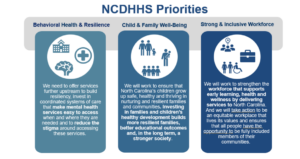
As we move out of the COVID pandemic, we have the tools needed to manage COVID-19 like we do other respiratory illnesses, including access to vaccines, testing, and treatment. In addition, we have expanded our focus to other respiratory diseases including Influenza and Respiratory Syncytial Virus and communicable diseases, including Mpox, syphilis and HIV for which there are disparities in rates of infections within our population
Our Public Health Infrastructure has been chronically underfunded and the COVID-19 pandemic brought mainstream attention to public health across the globe and highlighted the challenges of this underfunded patchwork of public health infrastructure to respond to the crisis. These challenges and recommendations to response have been identified by the North Carolina Institute of Medicine's Task Force on the Future of Local Public Health in NC. This report highlights work to strengthen public health foundational capabilities, infrastructure, and workforce to be able to respond to future threats more readily. Finally, this report also serves as the Annual Report on the North Carolina Division of Public Health Strategic Plan as required by Public Health Accreditation Board, and highlights work being done to meet DPH Strategic Priorities.
The full report is available here.
Join NCMS for 2024 National Advocacy Conference in Washington

October 16, 2023
Join us on Capitol Hill
The AMA’s National Advocacy Conference is scheduled for February 12-14, 2024. This yearly event offers an opportunity for personal involvement in the health policy debate on Capitol Hill. We need increased NCMS member engagement with our members of Congress, so mark your calendar and stay tuned for forthcoming details.

2024 National Advocacy Conference
Save the date and join us for our return to Capitol Hill.
February 12-14, 2024
Grand Hyatt / Washington, DC
Plan now to join your colleagues as we advocate for
patients and the medical profession on . . .
Prior Authorization Relief
Medicare Payment Reform
Step Therapy Reform
Workforce Shortage Solutions
Physician Wellness
Registration and additional information coming soon.
https://www.ama-assn.org/about/events/national-advocacy-conference
2023 LEAD Conference and Gala is Another Success!

RALEIGH -- The 2023 LEAD Healthcare Conference and Golden Stethoscope Awards Gala has concluded! Over the course of two days, attendees, including members of the North Carolina Medical Society, guests, speakers, and exhibitors, gathered at the Sheraton Imperial Hotel in RTP for engaging discussions, camaraderie, and educational sessions. The agenda encompassed a range of vital subjects, such as women's reproductive health and Black maternal well-being, trending topics for young physicians and physician assistants, clinician well-being, and the latest developments in the healthcare field.
On Friday morning, the event commenced with a keynote address from Dr. Amy Bryant, who delved into the topic of women's reproductive health. This was followed by the screening of the Aftershock video and a panel discussion centered on Black maternal health, skillfully moderated by Dr. Karen L. Smith. Joining her on stage were Belinda Pettiford, MPH, and Maria Small, MD, MPH, contributing to the insightful dialogue.
Throughout the day, attendees had the opportunity to engage in networking sessions with peers and gain valuable insights from a diverse array of exhibitors who offered comprehensive support to meet the needs of physicians. The exhibitors included financial advisors, workforce support providers, technology consultants, and a myriad of experts prepared to address the challenges and opportunities within the future of healthcare in North Carolina.
On the first day, there was a panel discussion titled 'Voice of the Young Physician and Physician Assistant,' skillfully moderated by Shawn Scott from NCMS. The panel featured Hans Arora, MD, Jasmine Hemmings, PA-C, Joshua Penninger, PA-C, and Sherry Wang, MD, offering valuable insights. Additionally, attendees enjoyed a lunch session and a Sponsor Showcase discussion on Asthma Care presented by Sanofi-Regeneron. There was also an informative advocacy class led by Seth Palmer, along with the annual CPP Meeting. Throughout the day, the NCMS Board of Directors, Board of Trustees, CCH, and CCHN conducted extensive meetings, culminating in the announcement of new board members on Saturday.
Friday afternoon was brimming with enlightening MedTalks featuring Leadership College Scholars, including Julia Wulforst, PA-C, Jennifer Kipp, DPM, Carla Holder, MD, Susie Fitzgerald, DO, Christine Khandelwal, DO, Michalina Kupsik, MD, Katie Lowry, MD, Jacqueline Njapa, MD, and Dana Point, MD. The MedTalks were followed by a meeting of the Opioid Task Force.
The day reached its climax with a joyous celebration of the Kanof Institute for Professional Leadership. The evening featured a cocktail reception, including a warm Welcome Reception and the formal presentation of graduation certificates to the 2023 KIPL class. The gathering was a moment to reflect on and commemorate the 20-year legacy of Leadership College.
Saturday began with the NCMS PAC Advocacy Breakfast, featuring a presentation by CEO Chip Baggett, who offered insights into the changing landscape of political division in the United States and strategies for advancing both the nation and the NCMS. Attendees enjoyed breakfast while several prizes and raffle items were distributed, and further interactions with exhibitors took place.
Following this, Elizabeth C. Tilson, MD, MPH, the State Health Director and the Chief Medical Officer for the Department of Health and Human Services and Ronald B. May, MD, delivered a presentation on the Public Health Commission.
The morning continued with an chance to see posters created by residents, fellows, and medical students from across the state, along with a final opportunity to engage with exhibitors. After that, NCMS President Dr. Arthur Apolinario participated in a panel discussion alongside NCMS Board members Andrew Lamb, MD, and Claude Jarrett, MD, FAAOS, focusing on the topic of 'When the Physician is the Patient.' The discussion was expertly moderated by NCMS' Dr. Kristina Natt och Dag. The NCMS Annual Meeting was also held Saturday afternoon.
Saturday night marked the moment when the festivities shifted into high gear at the 2023 Golden Stethoscope Awards Gala! The event was kicked off by NCMS' Randy Aldridge and Chip Baggett, who extended a warm welcome to past, present, and future NCMS presidents on the stage. A touching farewell was delivered by Past President Dr. Michael Utecht to President Dr. Arthur Apolinario, who presented him with the presidential pin. Dr. Apolinario, affectionately known as "Dr. Art," then directed his attention to incoming president, Dr. Eileen Raynor, MD, FACS, FAAP. He administered the oath of office and bestowed upon her the President's Medallion. Dr. Raynor then addressed the gathering with her inaugural speech as NCMS president.
Several awards were given including the Golden Stethoscope Awards. They went to:
- Dr. Karen Harum from Region 1
- Dr. Holly Biola from Region 2
- Dr. Joseph Bell from Region 3
- Dr. Alan Story from Region 4
The 2023 T. Reginal Harris Award was given to Dr. Jeffrey Kuremsky
The 2023 John Huske Anderson Award went to Brooks Bell
The 2023 E. Harvey Estes, Jr. Physician Community Service Award went to Dr. Peter Morris.
All of that was followed by a presentation on 20 years of NCMS Leadership College by Kristina Natt och Dag.
The evening wrapped up with comments from CEO Chip Baggett and dancing! All-in-all, it was another wonderful annual conference for the North Carolina Medical Society.
NCMGMA Salary and Benefits Survey Now Open
NCMGMA Salary and Benefits Survey is Open
EASIER Data Collection is Here!
Complete your survey by November 22nd
This comprehensive study is designed to bring our members the information they need to see trends specific to the healthcare industry, and provide comparative information your organization can use to assist in making crucial business decisions.
NEW! If you participated last year, you can copy last year's data into this year's survey, effectively reducing the time it takes to complete the survey! New positions have also been added this year, including a traveling nurse position.
Data collection is now open through Wednesday, November 22nd.
Complete 75% to gain access to complimentary reporting!
Access to the Site:
- Link: https://benchmark.ncmgmasalarysurvey.com/
- Enter your Username & Password to begin entering in data:
- If you've forgotten your password, please use the prompt on the page to assist.
New User? Click here to get started
Survey Information:
- Once logged in, check out the Support Page to find the:
- Survey Positions listing: sort by Category, Department or Position.
- Survey Worksheet, a downloadable spreadsheet used to help compile data to get you started prior to entering in data.
- User Guide, which will help answer many of your how-to questions. It can also be found on the Support page in the survey, once logged in.
- The Survey is divided into sections that contain categories of questions. You can begin in any section and complete the survey questions in any order.
- The progress bar on the home page will track your overall progress and the icons will help you see any areas not completed.
- Come back as often as needed to complete the survey. All data is saved as you go.
In order to access results when they are released (December), participants must complete all required questions and a minimum 75% of the survey
Questions:
If you have any questions about the 2023 Salary & Benefits Survey, please contact the NCMGMA offices at [email protected]
NCMS Member, Representative Dr. Kristin Baker Not Running for Re-Election
NCMS Member, Representative Dr. Kristin Baker Decides Against Another Term

2023 SHD Report, CPH Agenda Released for October 14 Meeting

State Health Director Elizabeth Cuervo Tilson, MD, MPH, has announced the CPH agenda and State Health Director Annual Report for the October 14 meeting in Durham.
COMMISSION FOR PUBLIC HEALTH
Commission Conjoint Meeting with the NC Medical Society
October 14, 2023
9:00 a.m.
Sheraton Imperial Hotel Raleigh-Durham Airport at RTP
Room: Imperial 1234
4700 Emperor Boulevard
Durham, NC 27703
I-140 at Exit 282
AGENDA
A. Call to Order Dr. Ron May
B. Invocation
C. Ethics - Conflict of Interest Statement
1. State Health Director’s Annual Report Dr. Betsey Tilson
2. New Business
3. Adjournment
Zoom
Link: https://us06web.zoom.us/j/89924373359
Meeting ID: 899 2437 3359
Passcode: LEAD2023
Phone: +13052241968,,89924373359#
View the Annual Report here: State Health Director Annual Report 2023 FINAL
Get Ready for December! NCDHHS Releases Medicaid Expansion Toolkit

RALEIGH -- The North Carolina Department of Health and Human Services has released a Tool Kit for the long-awaited expansion of Medicaid in the state. The bilingual kit includes all you need to know to spread the word to your patients and answers some frequently asked questions.
The kit includes:
- Day 1 Flyer: An overview of who is eligible and how to enroll.
- Newsletter Template: Content to include in your newsletters and emails.
- Social Media: Graphics and posts to share on your channels.
- Family Planning Flyer: Information for the approximately 300,000 people who receive limited benefits through Family Planning Medicaid who will be automatically enrolled in full Medicaid.
- Medicaid Essentials Deck: A presentation to share with your community on who is eligible and how to enroll.
- FAQ: Answers to common questions.
- ePass Video: An overview of how to apply online through ePass.
A complete look at all the information from NCDHHS can be found here.
To stay updated with the latest information, be notified when the application process goes live, and receive the newest resources, complete this sign-up form.
On the Lighter Side - October 6, 2023 - Jazz, 9 to 5, Football, Plus Lots and Lots of Seafood!
Here are some things NCMS employees, members, and YOU are talking about this Weekend and Beyond!
Fall football is in full swing!

Tonight
- Cornell at Harvard, 7pm (ESPNU)
Saturday
- Maryland at Ohio State, noon (Fox)
- Marshall at NC State, 2pm (CW Network)
- Virginia Tech at Florida, 3:30pm
- Syracuse at UNC, 3:30pm
- Wake Forest at Clemson, 3:30pm (ACC Network)
Don't duck out on the Duck Jazz Festival!

On the Outer Banks, Columbus Day weekend has become synonymous with the lively sounds of jazz. Plenty of music and fun in Duck! More information is here.
Stumble out of bed for 9 to 5 in High Point

Set in the male-dominated 1980’s workplace, audiences will be rooting for Violet, Doralee, and Judy as they face off against their sexist, egotistical, oppressive boss. Witty dialogue, powerful songs, and hilarious scenes make 9 to 5 an instant classic. Music from Grammy Award winner Dolly Parton shines bright, and will have you humming along and dancing in your seats. Tickets are still available here.
You won't go hungry in Morehead City this weekend!

The North Carolina Seafood Festival is among the most popular free festivals in the state. It takes place on the first weekend of October in Morehead City, attracting more than 200,000 attendees. All you need to know is here.