Measles Cases Now Highest in US Since 2019
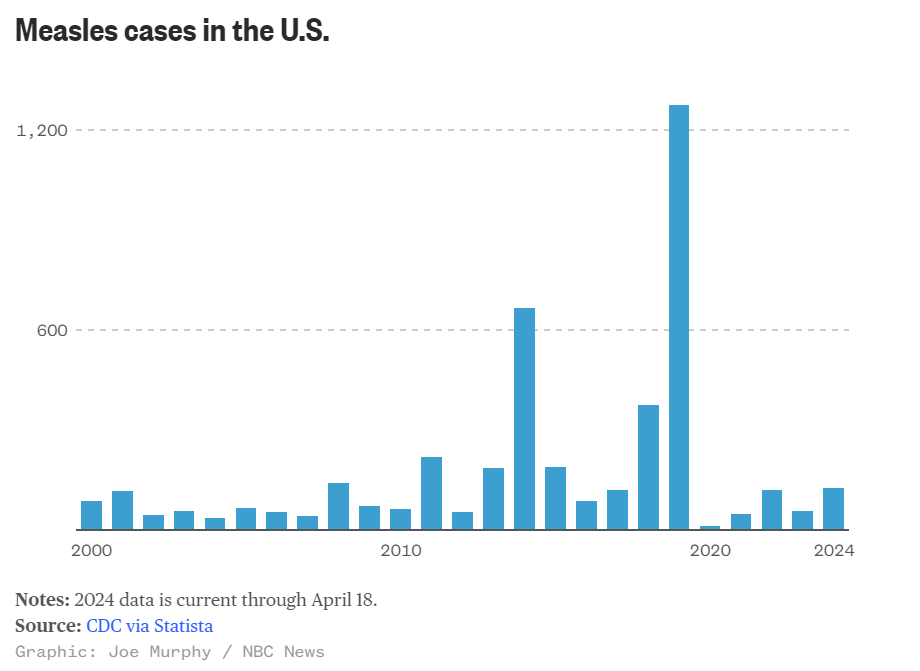
Several outbreaks, including one in Chicago, led to an early spike in measles cases this year. A chart shows how the case count compares to past years
(NBCNews, Aria Bendix and Joe Murphy) -- This year's measles case total is now the highest of the last five years. The United States has seen 125 cases across 17 states as — its largest annual tally since 2019, according to the Centers for Disease Control and Prevention.
From January to March, the U.S. recorded around 30% of the total cases seen since the beginning of 2020, according to a CDC report released earlier this month.
The authors warned that the rapid increase in cases "represents a renewed threat to elimination."
Most cases reported this year were linked to international travel, and the majority were among people who had not received a measles, mumps and rubella (MMR) vaccine or whose vaccination status was unknown.
Two doses of the vaccine are 97% effective, but the CDC said in an advisory to health care providers last month that "pockets of low [vaccination] coverage leave some communities at higher risk for outbreaks."
This year's early spike in measles cases was driven in part by outbreaks centered in a migrant shelter in Chicago, an elementary school in southeast Florida and a children’s hospital and a day care center in Philadelphia.
Chicago continues to confront its outbreak. As of Monday, its case count had reached 63, with the most recent recorded last week. More than half of the cases were among children under age 5.
Though disease experts have expressed concern about the early rise in cases, the U.S. isn’t close to its total from 2019, when the country nearly lost its measles elimination status. Most of the 1,249 cases that year were associated with outbreaks in Orthodox Jewish communities in New York.
Measles is highly contagious: An infected person can spread it to up to 90% of people close to them if those contacts aren’t immune. Thanks to widespread vaccination, measles was eliminated in the U.S. in 2000 — meaning that it’s no longer constantly present, though there are still occasional outbreaks.
Most people who get measles now are unvaccinated. Children in the U.S. are meant to get their first vaccine dose between 12 and 15 months and their second between 4 and 6 years old.
However, vaccination rates have fallen in the last few years. For nearly a decade, 95% of U.S. kindergartners had received two doses of the MMR vaccine. That rate fell to 94% in the 2020–21 year, then to 93% in the 2022–23 school year.
Measles symptoms usually start with a high fever, cough, conjunctivitis (pink eye) and runny nose. Two to three days later, people may notice tiny white spots in their mouth. On days three to five of symptoms, a blotchy rash often forms at the hairline before spreading to the rest of the body.
Some people may develop severe complications from measles, including pneumonia, swelling of the brain or a secondary bacterial infection. Before measles vaccines became available in 1963, around 48,000 people were hospitalized and 400 to 500 people died of the disease each year in the U.S.
Today, 1 in 5 unvaccinated people who get measles are hospitalized, and roughly 1 to 3 out of every 1,000 children with measles die from respiratory and neurological complications, according to the CDC.
Want to Slow Down Aging? There May Be A Cheap Way To Do It.

A drug taken by millions of people to control diabetes may do more than lower blood sugar
(NPR, Allison Aubrey) -- Research suggests metformin has anti-inflammatory effects that could help protect against common age-related diseases including heart disease, cancer, and cognitive decline.
Scientists who study the biology of aging have designed a clinical study, known as The TAME Trial, to test whether metformin can help prevent these diseases and promote a longer healthspan in healthy, older adults.
Michael Cantor, an attorney, and his wife Shari Cantor, the mayor of West Hartford, Connecticut both take metformin. "I tell all my friends about it," Michael Cantor says. "We all want to live a little longer, high-quality life if we can," he says.
Michael Cantor started on metformin about a decade ago when his weight and blood sugar were creeping up. Shari Cantor began taking metformin during the pandemic after she read that it may help protect against serious infections.
The Cantors are in their mid-60s and both say they feel healthy and have lots of energy. Both noticed improvements in their digestive systems – feeling more "regular" after they started on the drug,
Metformin costs less than a dollar a day, and depending on insurance, many people pay no out-of-pocket costs for the drug.
"I don't know if metformin increases lifespan in people, but the evidence that exists suggests that it very well might," says Steven Austad, a senior scientific advisor at the American Federation for Aging Research who studies the biology of aging.
An old drug with surprising benefits
Metformin was first used to treat diabetes in the 1950s in France. The drug is a derivative of guanidine, a compound found in Goat's Rue, an herbal medicine long used in Europe.
The FDA approved metformin for the treatment of type 2 diabetes in the U.S. in the 1990s. Since then, researchers have documented several surprises, including a reduced risk of cancer. "That was a bit of a shock," Austad says. A meta-analysis that included data from dozens of studies, found people who took metformin had a lower risk of several types of cancers, including gastrointestinal, urologic and blood cancers.
Austad also points to a British study that found a lower risk of dementia and mild cognitive decline among people with type 2 diabetes taking metformin. In addition, there's research pointing to improved cardiovascular outcomes in people who take metformin including a reduced risk of cardiovascular death.
As promising as this sounds, Austad says most of the evidence is observational, pointing only to an association between metformin and the reduced risk. The evidence stops short of proving cause and effect. Also, it's unknown if the benefits documented in people with diabetes will also reduce the risk of age-related diseases in healthy, older adults.
"That's what we need to figure out," says Steve Kritchevsky, a professor of gerontology at Wake Forest School of Medicine, who is a lead investigator for the Tame Trial.
The goal is to better understand the mechanisms and pathways by which metformin works in the body. For instance, researchers are looking at how the drug may help improve energy in the cells by stimulating autophagy, which is the process of clearing out or recycling damaged bits inside cells.
Researchers also want to know more about how metformin can help reduce inflammation and oxidative stress, which may slow biological aging.
"When there's an excess of oxidative stress, it will damage the cell. And that accumulation of damage is essentially what aging is," Kritchevsky explains.
When the forces that are damaging cells are running faster than the forces that are repairing or replacing cells, that's aging, Kritchevsky says. And it's possible that drugs like metformin could slow this process down.
By targeting the biology of aging, the hope is to prevent or delay multiple diseases, says Dr. Nir Barzilai of Albert Einstein College of Medicine, who leads the effort to get the trial started.
The ultimate in preventative medicine
Back in 2015, Austad and a bunch of aging researchers began pushing for a clinical trial.
"A bunch of us went to the FDA to ask them to approve a trial for metformin,' Austad recalls, and the agency was receptive. "If you could help prevent multiple problems at the same time, like we think metformin may do, then that's almost the ultimate in preventative medicine," Austad says.
The aim is to enroll 3,000 people between the ages of 65 and 79 for a six-year trial. But Dr. Barzilai says it's been slow going to get it funded. "The main obstacle with funding this study is that metformin is a generic drug, so no pharmaceutical company is standing to make money," he says.
Barzilai has turned to philanthropists and foundations, and has some pledges. The National Institute on Aging, part of the National Institutes of Health, set aside about $5 million for the research, but that's not enough to pay for the study which is estimated to cost between $45 and $70 million.
The frustration over the lack of funding is that if the trial points to protective effects, millions of people could benefit. "It's something that everybody will be able to afford," Barzilai says.
Currently the FDA doesn't recognize aging as a disease to treat, but the researchers hope this would usher in a paradigm shift — from treating each age-related medical condition separately, to treating these conditions together, by targeting aging itself.
For now, metformin is only approved to treat type 2 diabetes in the U.S., but doctors can prescribe it off-label for conditions other than its approved use.
Michael and Shari Cantor's doctors were comfortable prescribing it to them, given the drug's long history of safety and the possible benefits in delaying age-related disease.
"I walk a lot, I hike, and at 65 I have a lot of energy," Michael Cantor says. I feel like the metformin helps," he says. He and Shari say they have not experienced any negative side effects.
Research shows a small percentage of people who take metformin experience GI distress that makes the drug intolerable. And, some people develop a b12 vitamin deficiency. One study found people over the age of 65 who take metformin may have a harder time building new muscle.
"There's some evidence that people who exercise who are on metformin have less gain in muscle mass, says Dr. Eric Verdin, President of the Buck Institute for Research on Aging. That could be a concern for people who are under-muscled.
But Verdin says it may be possible to repurpose metformin in other ways "There are a number of companies that are exploring metformin in combination with other drugs," he says. He points to research underway to combine metformin with a drug called galantamine for the treatment of sarcopenia, which is the medical term for age-related muscle loss. Sarcopenia affects millions of older people, especially women.
The science of testing drugs to target aging is rapidly advancing, and metformin isn't the only medicine that may treat the underlying biology.
"Nobody thinks this is the be all and end all of drugs that target aging," Austad says. He says data from the clinical trial could stimulate investment by the big pharmaceutical companies in this area. "They may come up with much better drugs," he says.
Michael Cantor knows there's no guarantee with metformin. "Maybe it doesn't do what we think it does in terms of longevity, but it's certainly not going to do me any harm," he says.
Cantor's father had his first heart attack at 51. He says he wants to do all he can to prevent disease and live a healthy life, and he thinks Metformin is one tool that may help.
For now, Dr. Barzilai says the metformin clinical trial can get underway when the money comes in.
New WFU School of Medicine Study: Racial Discrimination Associated with Alzheimer's Disease

Study Suggests Racial Discrimination During Midlife Associated with Alzheimer’s Disease Pathology
Later in Life
(WakeHealth) -- Racial discrimination experienced during midlife is associated with Alzheimer’s disease pathology, according to a new study from researchers at Wake Forest University School of Medicine and the University of Georgia.
The findings appear online today in Alzheimer’s & Dementia: The Journal of the Alzheimer’s Association.
“We know that Black Americans are at an elevated risk of Alzheimer’s disease and other dementias compared to non-Hispanic white Americans, but we don’t fully understand all the factors that contribute to this disproportionate risk,” said Michelle Mielke, Ph.D., professor of epidemiology and prevention at Wake Forest University School of Medicine.
Mielke, who is a co-corresponding author of the study, said that these racial disparities cannot be attributed to only genetic differences and that research suggests that exposure to racism and its associated stress may increase the risk of dementia.
For the present study, the research team used 17 years of data, which included interviews and blood draws, from a sample of 255 Black Americans who participated in the Family and Community Health Study, a multi-site and longitudinal investigation, which was initiated in 1996 and included more than 800 families in the U.S.
Since the beginning of the Family and Community Health Study, data has been collected every two to three years to study the health and well-being of Black Americans.
In the current study, researchers analyzed serum biomarkers, which are associated with Alzheimer’s disease and related dementias, including serum phosphorylated tau181 (p-Tau181), a marker of Alzheimer’s pathology; neurofilament light (NfL), a non-specific marker of neurodegeneration; and glial fibrillary acidic protein (GFAP), a marker of brain inflammation.
To measure racial discrimination, the study team surveyed individuals about discriminatory events they experienced such as encountering disrespectful treatment by store owners, salespeople or police officers, being called racial slurs, being excluded from social activities, and not being expected to do well because of being a Black American.
“We found no correlations between racial discrimination and increased levels of the serum biomarkers in 2008 at Wave 5 when participants were a mean age of 46 years,” said Ronald L. Simons, Ph.D., professor of sociology at the University of Georgia and co-corresponding author of the study. “However, 11 years later when the study participants were roughly 57 years old, we found that increased discrimination during middle age significantly correlated with higher levels of both p-Tau181 and NfL.”
While additional research is needed to better understand the complexity of these processes, Mielke said it’s clear that future studies should also focus on the challenges and racism experienced by Black Americans to further understand their risk of dementia.
“These findings provide evidence that the chronic stress of racial discrimination often encountered by Black Americans in midlife become biologically embedded and contribute to Alzheimer’s disease pathology and neurodegeneration later in life,” Mielke said. “This research can help inform policies and interventions to reduce racial disparities and reduce dementia risk.”
This work was supported by the National Institute on Aging (RF1 AG077386 and R01 AG055393), and the National Heart, Lung, Blood Institute (R01 HL118045).
NCMS Proudly Graduates the 2024 Health Care Leadership and Management Class
Participants from across North Carolina Gather in Raleigh to celebrate!
On Sunday, April 21, 2024, NCMS proudly graduated it’s 2024 Health Care Leadership and Management (HCLM) class of clinicians and health care administrators. HCLM is led by NCMS members, Drs. Genie Komives, CMO, WellCare of NC, and Bryant Murphy, Vice Chairman for Clinical Operations at UNC HealthCare.
The scholars convened in Raleigh at NCMS headquarters last weekend for their final lecture session led by Jonathan Vehar titled, Mastering Leadership. The session culminated a year’s long training that included 1:1 coaching sessions, lecturing, and CBO site visits to glean new management strategies from CFOs, COOs, CEOs, and CMOs throughout the state. Sunday’s session highlighted the work of the scholars where they presented projects demonstrating leadership insights, strategic thinking, financial understanding, and innovation in tackling a real-world problem.
Team One members were comprised of Sankalp Puri, MD; Tambetta Ojong, MD, FAAFP; Nicole Six, LCSW; Kalpana Iyer, MBA. Their presentation was entitled, Fueling Hope: Your guide to beating food insecurity with flavor and fun.
Team Two members were comprised of Colby Dendy, MD, MPH, FAAP; John Nicholls, MD, JD, DFAPA; Debbie Naylor; and Kelly Phillips, MBA. Their presentation was entitled, Revolutionizing Mental Healthcare in Rural North Carolina.
The 2024 cohort participants hailed from Asheville to Wilmington, NC.
HCLM is a renowned leadership program designed to provide a strong framework for professionals in healthcare administrative roles. The program consists of intensive training sessions and tools to navigate organizational financial strategies, negotiate contracts, master leading C-suite executives and more. Scholars are nominated or self-identified as exceptional leaders in their healthcare community to join other elite healthcare leaders throughout NC. To learn how you can join the next HCLM cohort, contact Erica Neal, Manager, Professional Growth.
Congratulations to our 2024 HCLM graduates!
Foundation Friday! Doctors' Day Special Edition

Doctors’ Day Special Recognition
On Doctors’ Day, the NCMS Foundation offered a chance to extend special recognition to individual physicians by donating $10 to the Foundation in their honor. Thank you to generous donors who felt moved to pay public tribute to the following individuals.
Joseph Bell, MD
Chamaine Brooks-Locklear, MD
Cheryl Davis-Lowry, MD
Christina Hardin-Dial, MD
Ginger Jacobs Locklear, MD
Rachel Keever, MD
Shelly Lowery, MD
Gerri Mattson, MD
Robin Peace, MD
Joseph Roberts, MD
Gail Robinson, MD
Stephen Szabo, MD
John H. Wood, MD
Thank you once again for all you do for your patients each and every day!
"I would be dead." Ali Ingersoll is proof that the time is NOW for Prior Auth Reform

RALEIGH -- Ali Ingersoll has turned a tragic accident into a siren call for change in the American healthcare system. She was left paralyzed at 27 and spend seven years facing life altering diagnoses, surgeries, and mountain-after-mountains to climb as she fought for critical healthcare. Her fight for life happened in step with her fight with insurance companies for treatments, medicines, and equipment.
Along the way she became a professional speaker, disability consultant, fierce advocate, and Ms. Wheelchair America.
Ali’s powerfully authentic story serves as a testament to the power of resilience in order to empower others in adapting to the unknown and advocating for inclusivity.
She sat down with NCMS's Randy Aldridge to talk about the multitude of problems she has faced dealing with prior authorization and roadblocks from insurers. Her story is powerful, poignant, and, ultimately, uplifting.
https://youtu.be/2PkNsOG0QDw
After watching, please click here for how you can tell lawmakers that you support Prior Authorization Reform and how important it is to you and your patients. Feel free to share this video with them.
UnitedHealth Cyber Attack- How You Can Secure Your Practice
An Update on How to Secure Your Practice after UnitedHealth Cyber Attack
On February 21, Blackcat, a ransomware group, accessed Change Healthcare’s systems and 6 TB of data. This included medical and dental records, payment information, and patient information from a variety of Change Healthcare partners.
Sentinel, a risk management and benefit solutions company, has offered the following advice:
UNITEDHEALTH CYBERATTACK:
WHAT TO KNOW AND HOW TO PROTECT YOUR PRACTICE
WHO WAS THE TARGET?
The unlucky target was UnitedHealth Group’s Change Healthcare, which is a critical part of the country’s healthcare infrastructure. They coordinate payments, requests for insurers to authorize care, and more. Change Healthcare processes about 50% of medical claims in the U.S. for around 900,000 physicians, 33,000 pharmacies, 5,500 hospitals, and 600 laboratories.
WHEN WAS THE ATTACK?
On February 21, Blackcat, a ransomware group, accessed Change Healthcare’s systems and 6 TB of data. This included medical and dental records, payment information, and patient information from a variety of Change Healthcare partners.
WAS A RANSOM PAID?
Blackcat received $22 Million in Bitcoin on March 1. However, Change Healthcare has not confirmed any payment of a ransom.
WHO WAS AFFECTED?
Any Change Healthcare partners reliant on its systems for payment, claims, processing, etc.
IS CHANGE HEALTHCARE BACK UP AND RUNNING?
Its pharmacy network was 99% restored on March 7 and the electronic payments platform was running as of March 15. Its claims preparation software went back online on March 18.
HOW CAN YOU PROTECT YOURSELF?
- Enable Multi-Factor Authentication (MFA)
Most email platforms (Outlook, Gmail, etc.) allow you to adjust your settings to enable MFA at no cost. Additional MFA products are available for enhanced security.
- Use Difficult to Guess Passwords
Include uppercase, lowercase, numbers, and characters and update passwords regularly. Consider using phrases versus just words as a password.
- Ensure Employees Are Educated on Phishing Scams
To prevent phishing scams from infiltrating your company’s system, it is crucial to educate your employees on how to recognize them. If you need assistance in training your staff, Sentinel offers helpful webinar courses to ensure they are well-equipped to identify and avoid potential threats.
- Get In Touch with Sentinel
Our IT Service Provider Partners are experts in the field of cybersecurity and can help you assess your current controls, identify vulnerabilities, and recommend enhancements to improve your cybersecurity readiness. By working with our trusted partners, you can rest assured that your organization’s cybersecurity is in good hands. Go to sentinelra.com or call 855-490-2528.
Questions About Telehealth? New Guidance for NC Care

Need help telling your patients where to seek telehealth? Here is some simple guidance.
CAN I PROVIDE TELEMEDICINE TO PATIENTS OUT OF STATE?
The policy guidance of the North Carolina Medical Board to licensees practicing telemedicine is that the practice of medicine occurs in the state where the patient is located.¹ If providing medicine to patients in North Carolina, the provider should be licensed in North Carolina. If a North Carolina licensee is intending to practice medicine using telehealth technology, they should check with the licensing board in the state where the patient is located.² Most states require medical providers to be licensed where the patient is located.
ARE THERE EXEMPTIONS FOR OUT-OF-STATE PHYSICIANS CARING FOR NORTH CAROLINA PATIENTS?
- Provider to provider consultations across state lines where a NC licensee remains responsible for the care of the NC patient, but an out-of-state provider consults “on a irregular basis” is allowed.
- Episodic follow up care in which the patient is temporarily located in North Carolina but has an established relationship with an out-of-state provider (i.e. the patient is attending college or is vacationing in North Carolina) is allowed.⁴
WHAT ARE THE RULES FOR PRESCRIBING VIA TELEMEDICINE?
The North Carolina Medical Board expects proper prescribing and monitoring of controlled substances. Patient encounters conducted exclusively through telemedicine may not be deemed suitable. However, prescribing medications via telemedicine is at the professional discretion of the licensee, as long as it is in accordance with state and federal laws and the standards of practice.⁵
1. North Carolina Medical Board Position Statement, 5.1.4: Telemedicine
2. North Carolina Medical Board Position Statement, 5.1.4: Telemedicine
3. North Carolina Medical Board Position Statement, 5.1.4: Telemedicine
4.North Carolina Medical Board Position Statement, 5.1.4: Telemedicine
5.North Carolina Medical Board Position Statement, 5.1.4: Telemedicine
FOLLOW THIS LINK TO DOWNLOAD A FORM FOR YOUR OFFICE: Telehealth_Guidance
Doctors Call to Expand Syphilis Testing during Pregnancy Amid Recent Surge

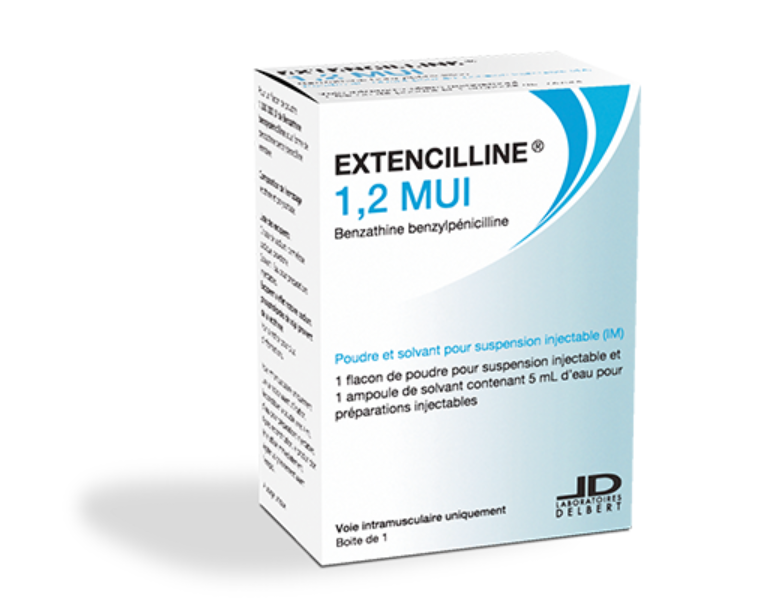
(The Hill, Miranda Nazzaro) -- The American College of Obstetricians and Gynecologists (ACOG) published new guidance April 18, recommending doctors screen pregnant individuals for syphilis three times during pregnancy.
Obstetricians, gynecologists and other obstetric care professionals are now advised to screen all pregnant individuals for syphilis at the first prenatal care visit, during the third trimester and again at birth.
Previous guidance recommended risk-based testing in the third trimester for those living in communities with high syphilis rates and for those at risk of acquiring the infection during pregnancy.
“There has been a near eightfold increase in congenital syphilis cases in the last decade or more, and from a public health perspective, we recognize that obstetrician–gynecologists and other obstetric care clinicians play a critical role,” Christopher Zahn, a fellow of ACOG, said in a statement.
Zahn said a timely diagnosis and treatment are “key” to reducing syphilis rates, noting the “majority” of cases can be prevented.
Syphilis is a sexually transmitted bacterial infection that can be contracted through direct contact with a sore, or through casual contact with objects like toilet seats, doorknobs, swimming pools, shared clothing or utensils. The infection can also spread from a pregnant person to a fetus.
More than 3,700 babies were born with congenital syphilis in 2022, marking the most cases in more than 30 years, the Centers for Disease Control and Prevention (CDC) said last year.
In its full advisory, the doctors coalition pointed to the CDC’s finding that nearly 9 in 10 congenital syphilis cases “could have been prevented with timely screening and treatment.”
Syphilis transmission to a fetus can lead to the baby having a low birth weight, and it increases the chances the mother will deliver too early or have a stillborn or miscarriage, according to the CDC.
At birth, a babies might not have signs or symptoms of the disease, but if they do not receive treatment, they can develop health issues within a few weeks. These problems include cataracts, deafness, seizures or death, the CDC added.
Benzathine penicillin G is the preferred treatment for syphilis during pregnancy, though the drug has been in short supply since last year. Pfizer, which is the only company manufacturing the drug, said last year it would take until at least the second quarter of 2024 to increase production enough to end the shortage.
Former NCMS President Named President of Duke Regional Hospital

Devdutta Sangvai Takes on His Next Leadership Challenge at Duke Regional
(Duke University School of Medicine, Synclaire Cruel) -- Having a love of science, an eagerness to help people, and a propensity for leadership has propelled Devdutta Sangvai, MD, MBA, into the role of President of Duke Regional Hospital. It’s the latest achievement in his 22-year career at Duke.
“I've been really lucky with the opportunities that I've had,” Sangvai said. “By having groups of people put their trust in me to take on challenges, I have been able to build experience and confidence.”
Sangvai was named interim president of Duke Regional in 2022 and then named president in 2023 by a national search committee. In just two years, Sangvai has already begun to drive positive change. “This is the strongest bond we’ve had with the divisions of family medicine and community health in the last 20 years,” he said. “We have more family medicine doctors and residents taking care of patients at the hospital, and they provide all of our newborn care.”
It's a role he’s long prepared for, having held several leadership positions while at Duke. “I always knew I was going to go into some form of administration, and family medicine provided the ideal clinical foundation for it,” Sangvai said. “It’s one of the ideal specialties needed for a community hospital because both sides are thinking about the patient, other providers the patient is seeing, and the patients’ living environment, which really takes community into context.”
As a family medicine provider and educator, he gained unique insight on how best to lead fellow providers and staff members. “Having faced some of the challenges family medicine providers experience, I can relate and put myself in their shoes,” he said.
“There's about 2,800 people who work here, and everyone aims to deliver the best care to our patients. To be in an atmosphere where you've got that level of spirit around you is inspiring and uplifting, and you find it in different ways.”
- Devdutta Sangvai, MD, MBA
Sangvai also managed to further open the lines of communication and build a stronger foundation with his team. “In some cases, the role of a leader is not necessarily to bring your own expertise, but to create a framework that facilitates an environment for others to share and leverage their knowledge.”
He’s continuously getting feedback from members about what’s working well and what’s not and is able to apply that information when making decisions. However, Sangvai finds that working with his team is the best part of the job.

“There's about 2,800 people who work here, and everyone aims to deliver the best care to our patients. To be in an atmosphere where you've got that level of spirit around you is inspiring and uplifting, and you find it in different ways,” he said.
“You cannot walk through a hallway without strangers saying, ‘Hello, how is your day?’ That care extends to the way we care for our patients,” Sangvai said. “When we do that for each other, it makes caring for our patients that much easier.”
His interest in leadership began very early in life. “Growing up, I had a real affinity for wanting to help make the lives of others better,” Sangvai said. “But I also always liked the idea of being a leader and growing the next generation of leaders.”
He got his first glimpse into the business of health care by joining the Organization of Student Representatives, the student arm of the American Association of Medical Colleges (AAMC). It’s also where he first connected with Lloyd Michener, MD, previous chair of the department.
“I got a better understanding of how much more there is to medicine than just the bedside. I started to think of it as the administrative backbone that all this clinical care is delivered on,” he said. It’s what drove him to pursue his MBA at Duke’s Fuqua School of Business after completing his family medicine and chief residencies at the Medical College of Ohio.
Sangvai then joined the Duke Department of Family Medicine and Community Health in 2001 as a faculty member. “I liked being able to care for patients not only early in life, but through the later years as well, and in many cases, even before they’re born,” he said. But it’s also where he got the opportunity to perform more administrative duties and gain leadership skills. In addition to seeing patients, he was instrumental in setting up community-based clinics, including Lyon Park and Walltown in Durham.
“The unfortunate thing is, the more administrative you do, the less time you have for clinic,” Sangvai said. Despite this, he still manages to treat patients at Duke Family Medicine Center. “It allows me to stay connected to patients, some of whom I've been seeing for over 20 years. It gives me a deeper appreciation of continuing to deliver care.”
He later became a faculty member in the Duke Departments of Pediatrics and Psychiatry & Behavioral Sciences. Additionally, Sangvai is currently Vice President for Population Health Management, and overseeing DUHS Case Management and Duke HomeCare & Hospice. Previously he was the Director of Medical Services for Student Health, Chief of the Division of Family Medicine, Medical director of DukeWell, and associate chief medical officer of Duke University Health System.
Sangvai also chaired the Durham County Hospital Corporation Board of Trustees and held positions within the North Carolina Medical Society, the American Medical Association, and the Association of American Medical Colleges.
As president of Duke Regional, Sangvai is most looking forward to combining the needs of society and Duke’s mission to make positive change in the surrounding community.
Plan Now! NCDHHS Livestream Town Hall: HPV and Cancer Prevention
The North Carolina Department of Health and Human Services will host a live fireside chat and tele-town hall on Tuesday, April 23, from 6 to 7 p.m., to discuss human papillomavirus (HPV) prevention as well as HPV-related cancer guidance, resources and care.
Event participants include:
- Cushanta Horton, MPH, Branch Head, Cancer Prevention and Control Branch, Division of Public Health, NCDHHS
- Nadja Vielot, Ph.D., Assistant Professor of Family Medicine, University of North Carolina at Chapel Hill
Around 85% of people will get an HPV infection at least once in their life. HPV is a common virus and can cause several types of cancers in people of all ages and genders. In North Carolina, rates of HPV-related cancers are higher than the national rates, with head and neck cancers among men accounting for much of that difference.
HPV vaccines help prevent more than 90% of HPV-related cancers, including cervical cancer. HPV vaccines are recommended beginning around age 11, but adults up to age 45 can also receive the vaccine. However, in North Carolina in 2022, nearly half of youth who were eligible for an HPV vaccine had not received all recommended doses.
Fireside chat and tele-town hall panelists will discuss the following:
- HPV prevention, detection and treatment
- Impacts of HPV-related cancers
- Importance of HPV vaccines and recommended screenings
- How to access health care providers, services and resources
Cancer impacts families and communities across North Carolina, from those who have experienced a diagnosis to their loved ones and caregivers. Resources are available to help people access health services, providers and care, stay up to date on vaccines and recommended screenings, manage a cancer diagnosis and find long-term support.
The fireside chat will stream live from the NCDHHS Facebook, Twitter and YouTube accounts, where viewers can submit questions. The event also includes a tele-town hall, which invites people by phone to listen in and submit questions. People can also dial into the event by calling 855-756-7520 Ext. 100654#.
Medicare's Push to Improve Chronic Care Attracts Businesses, but Not Many Doctors

Medicare enrollees with two or more chronic conditions are eligible for Chronic Care Management, which pays doctors to check in with those patients monthly. The service hasn't caught on.
(NPR, Phil Galewitz, Holly K. Hacker) -- Carrie Lester looks forward to the phone call every Thursday from her doctors' medical assistant, who asks how she's doing and if she needs prescription refills. The assistant counsels her on dealing with anxiety and her other health issues.
Lester credits the chats for keeping her out of the hospital and reducing the need for clinic visits to manage chronic conditions including depression, fibromyalgia and hypertension.
"Just knowing someone is going to check on me is comforting," says Lester, 73, who lives with her dogs, Sophie and Dolly, in Independence, Kansas.
At least two-thirds of Medicare enrollees have two or more chronic health conditions, federal data shows. That makes them eligible for a federal program that, since 2015, has rewarded doctors for doing more to manage their health outside office visits.
But while early research found the service, called Chronic Care Management, reduced emergency room and in-patient hospital visits and lowered total health spending, uptake has been sluggish.
Federal data from 2019 shows just 4% of potentially eligible enrollees participated in the program, a figure that appears to have held steady through 2023, according to a Mathematica analysis. About 12,000 physicians billed Medicare under the CCM mantle in 2021, according to the latest Medicare data analyzed by KFF Health News. (The Medicare data includes doctors who have annually billed CCM at least a dozen times.)
By comparison, federal data shows about 1 million providers participate in Medicare.
$62 per patient, per month
Even as the strategy has largely failed to live up to its potential, thousands of physicians have boosted their annual pay by participating, and auxiliary for-profit businesses have sprung up to help doctors take advantage of the program. The federal data showed about 4,500 physicians received at least $100,000 each in CCM pay in 2021.
Through the CCM program, Medicare pays to develop a patient care plan, coordinate treatment with specialists, and regularly check in with beneficiaries. Medicare pays doctors a monthly average of $62 per patient, for 20 minutes of work with each, according to companies in the business.
Without the program, providers often have little incentive to spend time coordinating care because they can't bill Medicare for such services.
Health policy experts say a host of factors limit participation in the program. Chief among them is that it requires both doctors and patients to opt in. Doctors may not have the capacity to regularly monitor patients outside office visits. Some also worry about meeting the strict Medicare documentation requirements for reimbursement and are reluctant to ask patients to join a program that may require a monthly copayment if they don't have a supplemental policy.
"This program had potential to have a big impact," says Kenneth Thorpe, an Emory University health policy expert on chronic diseases. "But I knew it was never going to work from the start because it was put together wrong."
He said most doctor's offices are not set up for monitoring patients at home. "This is very time-intensive and not something physicians are used to doing or have time to do," Thorpe says.
For patients, the CCM program is intended to expand the type of care offered in traditional, fee-for-service Medicare to match benefits that — at least in theory — they may get through Medicare Advantage, which is administered by private insurers.
But the CCM program is open to both Medicare and Medicare Advantage beneficiaries.
The program was also intended to boost pay to primary care doctors and other physicians who are paid significantly less by Medicare than specialists, says Mark Miller, a former executive director of the Medicare Payment Advisory Commission, which advises Congress. He's currently an executive vice president of Arnold Ventures, a philanthropic organization focused on health policy. (The organization has also provided funding for KFF Health News.)
Not "easy money"
Despite the allure of extra money, some physicians have been put off by the program's upfront costs.
"It may seem like easy money for a physician practice, but it is not," says Dr. Namirah Jamshed, a physician at UT Southwestern Medical Center in Dallas.
Jamshed says the CCM program was cumbersome to implement because her practice was not used to documenting time spent with patients outside the office, a challenge that included finding a way to integrate the data into electronic health records. Another challenge was hiring staff to handle patient calls before her practice started getting reimbursed by the program.
Only about 10% of the practice's Medicare patients are enrolled in CCM, she says.
Jamshed says her practice has been approached by private companies looking to do the work, but the practice demurred out of concerns about sharing patients' health information and the cost of retaining the companies. Those companies can take more than half of what Medicare pays doctors for their CCM work.
Dr. Jennifer Bacani McKenney, who runs a family medicine practice in Fredonia, Kansas, with her father — where Carrie Lester is a patient — says the CCM program has worked well.
She says having a system to keep in touch with patients at least once a month has reduced their use of emergency rooms — including for some who were prone to visits for nonemergency reasons, such as running out of medication or even feeling lonely. The CCM funding enables the practice's medical assistant to call patients regularly to check in, something it could not afford before.
For a small practice, having a staffer who can generate extra revenue makes a big difference, McKenney says.
While she estimates about 90% of their patients would qualify for the program, only about 20% are enrolled. One reason is that not everyone needs or wants the calls, she says.
While the program has captured interest among internists and family medicine doctors, it has also paid out hundreds of thousands of dollars to specialists, such as those in cardiology, urology and gastroenterology, the KFF Health News analysis finds. Primary care doctors are often seen as the ones who coordinate patient care, making the payments to specialists notable.
A federally funded study by Mathematica in 2017 found the CCM program saves Medicare $74 per patient per month, or $888 per patient per year — due mostly to a decreased need for hospital care.
The study quoted providers who were unhappy with attempts to outsource CCM work. "Third-party companies out there turn this into a racket," the study cites one physician saying, noting that companies employ nurses who don't know patients.
Nancy McCall, a Mathematica researcher who co-authored the 2017 study, says doctors are not the only resistance point. "Patients may not want to be bothered or asked if they are exercising or losing weight or watching their salt intake," she says.
How outsourcing works
Still, some physician groups say it's convenient to outsource the program.
UnityPoint Health, a large integrated health system based in Iowa, tried doing chronic care management on its own, but found it administratively burdensome, says Dawn Welling, the UnityPoint Clinic's chief nursing officer.
For the past year, it has contracted with a Miami-based company, HealthSnap, to enroll patients, have its nurses make check-in calls each month, and help with billing. HealthSnap helps manage care for more than 16,000 of UnityPoint Health's Medicare patients — a small fraction of its Medicare patients, which includes those enrolled in Medicare Advantage.
Some doctors were anxious about sharing patient records and viewed the program as a sign they weren't doing enough for patients, Welling says. But she says the program has been helpful, particularly to many enrollees who are isolated and need help changing their diet and other behaviors to improve health.
"These are patients who call the clinic regularly and have needs, but not always clinical needs," Welling says.
Samson Magid, CEO of HealthSnap, says more doctors have started participating in CCM since Medicare increased pay in 2022 for 20 minutes of work, to $62 from $41, and added billing codes for additional time.
To help ensure patients pick up the phone, caller ID shows HealthSnap calls as coming from their doctor's office, not from wherever the company's nurse might be located. The company also hires nurses from different regions so they may speak with dialects similar to those of the patients they work with, Magid says.
He says some enrollees have been in the program for three years and many could stay enrolled for life, which means they can bill patients and Medicare long-term.
New Report: Evidence of Racial Disparities in Healthcare Now Reported in Every US State

Researchers found health system performance is worse for many people of color.
(ABC News) -- Racial and ethnic disparities in health care are evident in every state, even those with robust health systems, according to a new analysis from the Commonwealth Fund.
In the analysis from the organization, which is aimed at promoting equitable health care, researchers found health system performance is markedly worse for many people of color compared to white people.
"Even among high performing states, we see significant disparities," Joseph Betancourt, M.D., President of the Commonwealth Fund, said in a report on the organization’s updated findings.
Six states were found to have better-than-average health system performance among all racial or ethnic groups, including Rhode Island, Massachusetts, Connecticut, Hawaii, New Hampshire and New York. However, even among these high-scoring health systems, racial disparities were observed.
"This report demonstrates that if you don't look under the hood, you won't identify where you're failing people and where you're leaving people behind," Betancourt said.
Particularly when looking at health outcomes, large disparities in premature deaths from avoidable causes are apparent in all states. Black, and American Indian and Alaska Native (AIAN) people are more likely to die before age 75 from preventable and treatable causes, including, but not limited to, some infections such as appendicitis and certain cancers, than white populations, according to the analysis.
There are also large disparities in health care access between white people and other racial or ethnic groups across all states. Despite coverage expansion by the Affordable Care Act in recent years, states' uninsured rates are generally higher and more variable for Black, Hispanic, and AIAN adults compared to Asian American, Native Hawaiian, and Pacific Islander (AANHPI) and white adults, according to the analysis. In particular, Hispanic people had the highest uninsured rates and cost-related difficulties in accessing care in almost all states.
"These groups have more problems accessing care and if quality of care is lower, then they have worse health outcomes compared to white people in many states," Senior Scientist David Radley, Ph.D., of the Commonwealth Fund, said in the report.
The analysis, which was done using publicly available databases reporting outcomes from more than 328,000,000 people during the years 2021 and 2022, concluded that achieving health equity requires policy action and health system action, including:
- Ensuring affordable, comprehensive, and equitable health insurance coverage for all
- Strengthening primary care
- Improving health care quality and delivery
- Health systems and providers prioritizing and centering equity
- Investing in social services
- Improving the collection and analysis of racial and ethnic data to identify gaps
- Developing equity-focused measures to inform and evaluate policy
"Some of the major takeaways of this work is that we still have a lot of work to do," Senior Scholar and Commonwealth Fund Vice President Sara R. Collins said in the organization’s report. "Maybe in a decade we'll look at this data and we'll see some of these gaps closing.”
Dr. Laurie Zephyrin, a senior vice president for the Commonwealth Fund, said undertaking the prescribed action will likely help.
"The reality is we can't improve healthcare if we're not accurately measuring and tracking these outcomes and experiences and using real data as a guidepost to ensure that we are advancing towards equity. ... All these comprehensive actions are truly a start. It really can help us move forward to advance health equity and address many of the inequities that we talked about today," she said in the report.
The Commonwealth Fund’s State Scorecard on Health System Performance series evaluated each state’s health care system and is a tool developed to understand health inequities and disparities. It uses 25 data indicators to designate a "State Health Equity Score," which indicates each state health system’s performance based on health care access, quality, service use and health outcome. Scores were also determined for each of five racial or ethnic groups (Black, AIAN, AANHPI and Latinx/Hispanic) during the years 2021 and 2022, notably incorporating post-pandemic effects on health disparities.
8th Annual Pirates vs. Cancer Event Raises $15k at ECU

ECU medical students lead Pirates vs. Cancer fundraiser for pediatric cancer patients
Some have watched loved ones fight the disease, while others have worked with cancer patients during clinical rotations. Other students and alumni have even been cancer patients themselves.
Whatever their unique experiences with cancer have been, the response has been powerful. Their encounters with cancer turned into a growing tradition that benefits children from across eastern North Carolina who are fighting cancer battles of their own.
The eighth annual Pirates vs. Cancer event on April 12 raised close to $15,000 for pediatric cancer patients at ECU Health’s James and Connie Maynard Children’s Hospital.

Several Brody School of Medicine faculty volunteered to be pied in the face by students as one of the event’s fundraising activities.
Led by Brody students, the fundraiser has gained popularity and momentum over the years, with volunteers having their hair cut and donated, getting their heads shaved and even — for special faculty volunteers — receiving a pie to the face in support of the cause.
“One thing that I love about Pirates vs. Cancer is that you are able to see with your own eyes the direct impact of this work on the children at Maynard Children’s Hospital,” said Carly Uhlir, Brody student and event coordinator for Pirates vs. Cancer. “We know that every dollar we raise will add up to make a difference. Kids with pediatric cancer are more than just patients — they are among the strongest and bravest in our community. I want to continue the Pirates vs. Cancer mission that the founders so strongly believed in years ago and that has transcended all these years.”
Dr. Cedric Bright, senior associate dean of admissions for Brody, volunteered to receive pies in the face during the event on the lawn of the Health Sciences Student Center.
“It does your heart good to help the students with this type of thing to support those that are going through trying times with cancer,” he said. “Patients teach us so much, and this is just one way of us trying to give back to those patients that teach us so much.”
Jillian Berntsen of Kinston had her hair cut as an audience looked on and cheered — much like the health care teams and supporters helping her daughter during her cancer journey.
Berntsen said her daughter is receiving in-patient care at Maynard Children’s Hospital, her latest stay stretching for nine weeks. Pirates vs. Cancer gave the family a welcome respite from the hospital walls.

Jillian Berntsen of Kinston had her hair cut as her family watched. Berntsen said her daughter is receiving in-patient care at Maynard Children’s Hospital. (ECU photos by Steven Mantilla.)
“There are so many things this hospital does, and the people we get to interact with have really become our family at this point from everything she’s been through,” Berntsen said. “We never really thought we’d have to experience anything like this and had no idea that things like this existed. This is the first time we’ve left the hospital in nine weeks, and knowing we had this to look forward to all week was something to get us through another week.”
The event was also eagerly anticipated by Brody students and community volunteers who wanted to help create a memorable and meaningful way to benefit pediatric patients. It has become part of a lifeline of support that keeps this special patient population equipped with resources to help them during their cancer journeys.
“The funds raised by PVC are critical to the maintenance of a positive environment for pediatric cancer patients here in Greenville,” said Grant Irons, Brody student and interdisciplinary chair of Pirates vs. Cancer.
Irons, who plans to pursue medical oncology as a specialty and spent time before medical school working with cancer patients, said the event also offers students a chance to see the realities of what some patients face and an opportunity to pause and look at the bigger picture.
“As future health care leaders, it is important to remember why we are here,” he said. “We entered the health care field to improve the lives of others. To become a well-rounded physician, I believe it is important to be involved outside of the classroom. There are endless opportunities to support our patient population here in Greenville, and I would encourage all health sciences students to lend a hand in these efforts.”
Dr. Cathleen Cook, Brody clinical associate professor of pediatric hematology/oncology and faculty advisor for Pirates vs. Cancer, said the event gives students exposure to the care of pediatric patients right here in eastern North Carolina.
“This fundraiser allows them the chance to see their financial contributions directly help these children while they are hospitalized in James and Connie Maynard Children’s Hospital and cared for in our ECU Pediatric Hematology/Oncology Clinic,” Cook said.
Previous donations through the event, she added, have been used to remodel an inpatient playroom, a space of respite for patients undergoing treatment. Pirates vs. Cancer also helps fund a portion of summer camps for pediatric hematology and oncology patients — Camp Rainbow and Camp Hope.
“Often, donors and volunteers are unaware of the administrative costs that are allocated from the proceeds and not able to see their donations at work,” Cook said. “For Pirates vs Cancer, 100% of the donations are re-invested in our pediatric patients, most specifically our oncology patients. It is my vision to continue to engage these future physicians annually and help support their goal of expanding this fundraiser.”
Brody student Katie Holt decided to get involved with the event to make an impact beyond fundraising. She served as this year’s president of Pirates vs. Cancer.
“Helping to put on this event is awe-inspiring because it puts into perspective the actual size of the Brody and health sciences community,” Holt said. “Applying to Brody, you are frequently told about the passion of the community in serving Greenville and eastern North Carolina. Helping to organize this event gives you a front-row seat to this passion in action.”
Holt said the annual event has caught on across the community.
“People I have never met have reached out to us to offer their help,” she said. “Businesses across the community donate their time and money. Employees from all different departments buy T-shirts to support us. Students across the many health sciences schools donate their hair. The event has shown us firsthand that ECU doesn’t just talk about serving others but goes above and beyond to invest in its community.”
Holt said the event, in addition to benefiting pediatric cancer patients, helps center medical students and remind them why they chose health care careers.
“Serving others, through this event or another community service program, benefits the community as well as serves to fight burnout and protect your mental health,” she said. “I know it has done this for me and many others on the Pirates vs. Cancer team by connecting us to something bigger than ourselves and keeping our sights fixed on a point beyond the next test.”
Uhlir said the event brings participants full circle in seeing their own life journeys while also understanding the magnitude of the battles other people face.
“It is both humbling and inspiring. As medical students, we often lose sight of the big picture. These patients have been through so much, so it is an amazing opportunity to be able to support them directly,” she said. “I also think back to all of the children I have known both personally and indirectly from the time I was a kid myself until now, and how this is such a great way of honoring their spirits.”
ECU Names Deans for College of Health and Human Performance, Graduate School

The East Carolina University Board of Trustees approved the appointment of Dr. Nicole Bromfield as dean of the College of Health and Human Performance and Dr. Debra L. Jackson as dean of the Graduate School during its meeting April 12.
Dr. Nicole Bromfield
Bromfield has been appointed dean of the ECU College of Health and Human Performance, effective July 1.
In addition to extensive international academic experience in a 25-year career, including as an assistant professor at the United Arab Emirates University from 2010-16, Bromfield is a seasoned scholar and administrator with 16 years in academic administration in multiple leadership positions.
Her most recent leadership role was as associate dean for academic affairs for the University of Houston’s Graduate College of Social Work, where she has been an associate professor since 2016. Under her four-year tenure as associate dean, the college enjoyed 30% enrollment growth and received a full program reaccreditation. She previously held administrative appointments at Virginia Commonwealth University as a director of student services and as a student services coordinator.

Dr. Nicole Bromfield
“Being selected as the next dean of East Carolina University’s College of Health and Human Performance is an incredible honor,” said Bromfield, who recently served as a Fulbright Research and Teaching Scholar for 20 months at the University of Namibia. “I am delighted to lead our vibrant HHP community dedicated to fostering holistic well-being through groundbreaking research, service and experiential learning, and to work with the college to further foster a welcoming and collaborative environment that supports each one of our talented faculty, staff and students in reaching their full potential. Our collective commitment to enhancing human well-being, academic excellence and collaborative innovation in research, teaching, service and community engagement will continue to guide us in advancing the college’s legacy and impact on eastern North Carolina and beyond.”
Bromfield has completed research projects in the United Arab Emirates, Bangladesh, India, Namibia and other nations. She co-authored a scholarly book, “From Intercountry Adoption to Global Surrogacy: A Human Rights History and New Fertility Frontiers,” and her research has been highlighted in various media outlets, including The Boston Globe, The National UAE newspaper and BBC News.
“Dr. Bromfield’s expertise, academic experiences, and alignment with the dimensions of College of Health and Human Performance are a few of the reasons why I am very excited to welcome Dr. Bromfield to our ECU team,” said Provost Robin Coger. “I also thank interim dean Stacey Altman for her leadership over the last couple of years in collaborating with the faculty, staff and students of CHHP to ensure the many strengths of this critical college.”
HHP has been led by Altman since July 1, 2022. Her tenure will continue until June 30 when she completes her 22 years of service to ECU. Altman is looking forward to welcoming the new dean.
“Dr. Bromfield’s breadth of experience and collaborative style is ideally suited to lead the HHP community to further success and positive impact as we continue to deliver on the promises associated with the ECU mission,” Altman said. “I look forward to supporting her transition to ECU and the position.”
Bromfield earned a doctoral degree in public policy and administration, with a specialization in health policy, from VCU. She holds two degrees from West Virginia University — a Master of Social Work, with a concentration in community organization, and a Bachelor of Arts in sociology and anthropology as a summa cum laude graduate. She has completed academic leadership training with Harvard University, the Council on Social Work Education, the National Association of Deans and Directors, and the University of Houston.
The College of Health and Human Performance offers a wide range of degrees, certificates and other credentials in health education and promotion, human development and family science, interior design and merchandising, kinesiology, recreation sciences and social work, as well as home to Army ROTC and Air Force ROTC. The college serves the region by providing transformative opportunities for students while collaborating and promoting holistic health and well-being.
Dr. Debra L. Jackson
Jackson has been named dean of East Carolina University’s Graduate School, effective July 1.
Jackson takes over for interim dean Dr. Kathleen Cox, who has held the position since July 2022 following the retirement of Dr. Paul Gemperline.
“The work of our Graduate School benefits all of ECU, and Dr. Jackson’s experience and collaborative leadership style will enable the next phases of the development and growth of our Graduate School,” said Coger. “I am also extremely grateful for the leadership of interim dean Kathleen Cox over the last couple of years. These two leaders have already met and are eager to work together and with their teams in the Graduate School and across the university.”

Dr. Debra L. Jackson
Jackson joins ECU after serving two decades at California State University, Bakersfield. In her most recent role as associate vice president for academic affairs and dean of academic programs, Jackson secured $7 million in funds to support student success.
Under her leadership, CSU Bakersfield received a five-year grant from the Department of Education for “Promoting Excellence in Graduate Education and Increasing Hispanic STEM Related Degree Completion.” She also helped secure the 2023 Award for Innovation in Promoting Success in Graduate Education from the Council of Graduate Schools for a California State University system-wide program titled “The Next Step: Building Career Readiness Among Graduate Schools across the CSU.”
“I am very excited to join the Pirate Nation family and look forward to working with the incredible team in the graduate school,” said Jackson.
While at CSU Bakersfield, Jackson also served as the associate dean for graduate and undergraduate studies, interim associate dean for the School of Arts and Humanities, coordinator for the Women, Gender and Sexuality Studies program, and the assessment coordinator for both the School of Arts and Humanities and General Education program. She recently completed a three-year term on the executive board of the Western Association of Graduate Schools.
She is an active member of the Bakersfield community, volunteering with the Women’s and Girl’s Fund, Girl Scouts of Central California South, and the Panama – Buena Vista Union School District Equity Task Force.
Jackson’s research addresses ethical, political and epistemological issues regarding sexual violence against women. She earned her Doctor of Philosophy from Purdue University in 2002 and an undergraduate degree in philosophy from Middle Tennessee State University in 1996.
ECU’s Graduate School enrolls over 5,000 students and offers 69 master’s degree programs, two intermediate degree programs, five professional doctoral programs, 13 research/scholarship doctoral programs and 77 graduate certificates.
Hit the Trail! It's a Great Time to See National Parks in North Carolina
It is National Park Week!
National Park Week is an annual celebration of America’s national parks – from iconic vistas to significant historical sites. This year, NPF invites you to celebrate our parks while learning more about the ways we all can help preserve these wonderful places.
Here are some spots in North Carolina
-
NATIONAL SCENIC TRAIL
Appalachian
Maine to Georgia, CT,GA,MA,MD,ME,NC,NH,NJ,NY,PA,TN,VA,VT,WV
The Appalachian Trail is a 2,190+ mile long public footpath that traverses the scenic, wooded, pastoral, wild, and culturally resonant lands of the Appalachian Mountains. Conceived in 1921, built by private citizens, and completed in 1937, today the trail is managed by the National Park Service, US Forest Service, Appalachian Trail Conservancy, numerous state agencies and thousands of volunteers.
-
PARKWAY
Blue Ridge
Blue Ridge Mountains of Virginia and North Carolina, NC,VA
A Blue Ridge Parkway experience is unlike any other: a slow-paced and relaxing drive revealing stunning long-range vistas and close-up views of the rugged mountains and pastoral landscapes of the Appalachian Highlands. The Parkway meanders for 469 miles, protecting a diversity of plants and animals, and providing opportunities for enjoying all that makes this region of the country so special.
-
NATIONAL SEASHORE
Cape Hatteras
Nags Head, Buxton, Ocracoke, NC
The sound of ocean waves, the starry night sky, or the calm of the salt marshes, you can experience it all. Shaped by the forces of water, wind, and storms these islands are ever changing. The plants, wildlife, and people who live here adapt continually. Whether you are enjoying the beach, kayaking the sound, or climbing the Cape Hatteras Lighthouse there is something for everyone to explore!
-
NATIONAL SEASHORE
Cape Lookout
Harkers Island, NC
A boat ride three miles off-shore brings you to the barrier islands of Cape Lookout National Seashore. Horse watching, shelling, fishing, birding, camping, lighthouse climbing, and touring historic villages--there’s something for everyone at Cape Lookout. Be sure to bring all the food, water, and supplies you need (and carry your trash out of the park) when visiting these remote beaches.
-
NATIONAL HISTORIC SITE
Carl Sandburg Home
Flat Rock, NC
“I make it clear why I write as I do and why other poets write as they do. After hundreds of experiments I decided to go my own way in style and see what would happen.” Carl Sandburg's free verse style of poetry, journalism, biography, children's stories, prose writing, and social activism provided a popular voice for the American people of the twentieth century.
-
NATIONAL HISTORIC SITE
Fort Raleigh
Manteo, NC
Fort Raleigh National Historic Site protects and preserves known portions of England's first New World settlements from 1584 to 1590. This site also preserves the cultural heritage of the Native Americans, European Americans and African Americans who have lived on Roanoke Island.
-
NATIONAL PARK
Great Smoky Mountains
the states of NC,TN
Ridge upon ridge of forest straddles the border between North Carolina and Tennessee in Great Smoky Mountains National Park. World renowned for its diversity of plant and animal life, the beauty of its ancient mountains, and the quality of its remnants of Southern Appalachian mountain culture, this is America's most visited national park. Plan your visit today!
-
NATIONAL MILITARY PARK
Guilford Courthouse
Greensboro, NC
"I never saw such fighting since God made me. The Americans fought like demons." - Lt. General Charles, Earl Cornwallis On March 15, 1781, six years into the American Revolution, General Greene and Lord Cornwallis' troops faced off at a small courthouse community. The battle would change the course of the Southern Campaign of the American Revolution.
-
NATIONAL BATTLEFIELD
Moores Creek
Currie, NC
In the early morning hours of February 27, 1776, Loyalist forces charged across a partially dismantled Moores Creek Bridge. Beyond the bridge, nearly 1,000 North Carolina Patriots waited quietly with cannons and muskets poised to fire. This battle marked the last broadsword charge by Scottish Highlanders and the first significant victory for the Patriots in the American Revolution.
-
NATIONAL HISTORIC TRAIL
Overmountain Victory
NC,SC,TN,VA
Stretching 330-miles through four states (Virginia, Tennessee, North and South Carolina) the Overmountain Victory National Historic Trail traces the route used by Patriot militia during the pivotal Kings Mountain campaign of 1780. Follow the campaign by utilizing a Commemorative Motor Route which uses existing state highways marked with the distinctive trail logo, or 87 miles of walkable trails.
-
NATIONAL HISTORIC TRAIL
Trail Of Tears
AL,AR,GA,IL,KY,MO,NC,OK,TN
Remember and commemorate the survival of the Cherokee people, forcefully removed from their homelands in Georgia, Alabama, and Tennessee to live in Indian Territory, now Oklahoma. They traveled by foot, horse, wagon, or steamboat in 1838-1839.
-
NATIONAL MEMORIAL
Wright Brothers
Kill Devil Hills, NC
Wind, sand, and a dream of flight brought Wilbur and Orville Wright to Kitty Hawk, North Carolina where, after four years of scientific experimentation, they achieved the first successful airplane flights on December 17, 1903. With courage and perseverance, these self-taught engineers relied on teamwork and application of the scientific process. What they achieved changed our world forever.
PAI Regulatory Advocacy Update

The latest Physician Advocacy Institute advocacy and federal regulatory developments.
PAI Files Amicus Curiae Brief in No Surprises Act Qualifying Payment Amount (QPA) Case Before U.S. Court of Appeals for the Fifth Circuit
PAI’s brief supports the Texas Medical Association’s (TMA) challenge to certain QPA calculation factors that allow insurers to skew the benchmark downward. Read more.
Federal Trade Commission (FTC), Department of Justice (DOJ) and Department of Health and Human Services (HHS) Prompt Investigation into Private Equity and Corporations’ Influence in Health Care
The cross-government public inquiry will investigate the effects of this trend on quality of care, patient health, workers’ safety and cost. PAI will weigh in. Read more.
Centers for Medicare and Medicaid Services (CMS) Releases Background on Federal Independent Dispute Resolution (IDR) Process Showing Physicians Prevailing in 77% of IDR Determinations
The resource shows a large volume of disputes submitted through the Federal IDR portal and substantial complexity in determining the disputes’ eligibility for the Federal IDR process. Read more.
President Biden Releases Fiscal Year (FY) 2025 Budget
The President's budget prioritizes investment in permanent premium tax credits, Medicaid coverage, drug price negotiation, mental health services and substance abuse treatment initiatives. Read more.
Substance Abuse and Mental Health Services Administration (SAMHSA) Issues Final Rule to Enhance Integrated Care and Confidentiality for Patients with Substance Use Conditions
The rule finalizes changes to the Confidentiality of Substance Use Disorder Patient Records regulations to protect the privacy of patients’ substance use disorder (SUD) treatment records. Read more.
CMS Ends Hospice Benefit Component of Value-Based Insurance Design (VBID) Model
CMS will conclude the Hospice Benefit Component at the end of 2024 and will not accept applications for calendar year (CY) 2025 due to escalating operational difficulties and decreasing participation. Read more.
HHS Releases 2023 Equity Action Plan Update
The 2023 update prioritizes child neglect prevention and care improvement, health care access, maternal health outcomes, behavioral health and diversity in clinical research. Read more.
For information on PAI’s advocacy initiatives, physician payment resources and research, please visit PAI’s website. Healthsperien’s Resource Updates page also has information on key issues in health policy and identifies potential reforms under the Biden Administration, Congress and in the states. Additionally, CMS releases their Quality Payment Program (QPP) Small Practices Newsletter, a monthly resource that provides small practices (15 or fewer physicians) with program updates, upcoming QPP milestones and resources to support their continued participation and success in the QPP. You can sign up here to receive this monthly resource.
PAI Files Amicus Curiae Brief in No Surprises Act QPA Case Before U.S. Court of Appeals for the Fifth Circuit
On March 26, PAI announced it filed an amicus curiae brief with the United States Court of Appeals for the Fifth Circuit supporting TMA’s third challenge to federal regulations implementing the No Surprises Act. In August 2023, United States District Court for the Eastern District of Texas Judge Jeremy D. Kernodle ruled partially in TMA’s favor. The ruling struck down provisions of federal agencies’ interim final rules that depressed the QPA and unbalanced the IDR process but upheld its minimal transparency requirements. The Administration subsequently appealed that decision.
PAI is joined on the brief by 15 state medical associations and six medical specialty societies. PAI’s brief supports TMA’s challenge to certain QPA calculation factors that allow insurers to skew the benchmark downward. The inclusion of “ghost rates”—prices for services a physician never or rarely provides—and out-of-specialty rates and the exclusion of incentive or bonus payments like those in value-based care arrangements depress the insurer-calculated QPA and make the IDR process inherently unfair. Addressing insurer payment practices that threaten patient access to care is foundational to PAI. That principle drives PAI’s support of TMA’s challenges to No Surprises Act implementation and will continue to guide its advocacy for as long as needed.
FTC, DOJ and HHS Prompt Investigation Into Private Equity and Corporations’ Influence in Health Care
On March 5, FTC, DOJ and HHS initiated a cross-government public inquiry to address the growing influence of private equity and other corporations within health care. Private equity and other corporate firms are increasingly participating in health care system transactions. The inquiry will investigate the effects of this trend on quality of care, patient health, workers’ safety and cost. The three agencies issued a Request for Information (RFI) soliciting public feedback about transactions conducted by health systems, private payers, private equity funds or alternative asset managers involving physicians, facilities or services. The RFI seeks comments regarding deals related to a wide range of health care entities and seeks to inform policy efforts to target consolidation and promote and preserve competition throughout the health care marketplace.
PAI is preparing an extensive comment letter in response to this RFI to share key research findings that document how practice acquisitions by private equity firms, insurer-owned entities, hospitals/health systems and large national pharmacies over the past decade have dramatically altered how physicians practice medicine in the United States. The related trend of physicians shifting from independent practice into employment has been equally dramatic, growing steadily every year over the past decade and nearing 80% at the start of 2024.
PAI will also share findings from the recently released employed physician survey for PAI by NORC at the University of Chicago that examined the experiences of physicians employed by hospitals and health systems, venture capital and private equity firms, health insurance companies and staffing agencies. Almost 60% of physicians who practice as employees of hospitals and other corporate entities reported that non-physician practice ownership results in a lower quality of patient care. Most physicians surveyed cited decreased time with patients and greater focus on financial success as factors negatively affecting quality at non-physician-owned medical practices. The survey demonstrates a belief among many employed physicians that corporate ownership may erode foundational aspects of the patient-physician relationship and impact patient outcomes.
CMS Releases Background on Federal IDR Process Showing Physicians Prevailing in 77% of IDR Determinations
On February 16, CMS released public use files for the Federal IDR process between January 1, 2023 and June 3, 2023. The resource notes that the first six months of 2023 were characterized by a large volume of disputes submitted through the Federal IDR portal and substantial complexity in determining disputes’ eligibility for the Federal IDR process. Between January 1, 2023 and June 30, 2023, disputing parties initiated 288,810 disputes through the Federal IDR portal. The number of disputes initiated through the Federal IDR portal over this six-month period was 13 times greater than the Departments of Treasury, Labor and HHS initially estimated for a full calendar year and has grown each quarter. Certified IDR entities rendered 83,868 payment determinations in the first six months of 2023. Physicians were the prevailing party in approximately 77% of payment determinations. Despite the increase in payment determinations, some disputing parties are still awaiting eligibility and payment determinations.
On December 28, PAI submitted a comment letter in response to a surprise billing proposed rule published by HHS. Physicians bear the brunt of the inefficient IDR process as medical practices across the nation experience significant payment delays awaiting eligibility and payment determinations. Widespread failure by insurers to make timely payments once determinations have been made exacerbate the issue further. PAI emphasized that the IDR process needs to be further refined, with input from physicians, to ensure that all parties have incentives to settle disputes more quickly and engage in fair contracting practices.
President Biden Releases FY 2025 Budget
On March 11, President Biden released his budget for FY 2025. The President's 2025 budget prioritizes significant health care investments and aims to expand access to high-quality services and lower costs. Key provisions include permanent premium tax credits, Medicaid coverage, drug price negotiation to reduce prescription costs, and initiatives targeting mental health services and SUD treatment. The budget also addresses health equity, veterans' health care needs and bolstering public health infrastructure. The table below highlights relevant provisions for physicians:

SAMHSA Issues Final Rule to Enhance Integrated Care and Confidentiality for Patients with Substance Use Conditions
On February 8, SAMHSA released a final rule that finalizes modifications to the Confidentiality of Substance Use Disorder Patient Records regulations, which protect the privacy of patients’ SUD treatment records. The rule was informed by the Coronavirus Aid, Relief, and Economic Security Act (CARES Act) that, among other things, required HHS to bring the Part 2 program into closer alignment with the Health Insurance Portability and Accountability Act of 1996 (HIPAA) Privacy, Breach Notification, and Enforcement Rules. The final rule includes the following modifications to Part 2:

CMS Ends Hospice Benefit Component of VBID Model
Beginning in CY 2021, the VBID Model permitted Medicare Advantage Organizations (MAOs) to incorporate the Medicare hospice benefit into their Medicare Advantage (MA) benefits package, known as the Hospice Benefit Component. Due to escalating operational difficulties and decreasing MAO participation, CMS announced on March 4 it will conclude the Hospice Benefit Component at the end of this year and will not accept applications for the CY 2025 Request for Applications for the component. The Hospice Benefit Component of the VBID Model aimed to alleviate coverage inconsistencies for MA enrollees electing hospice and assessed if MAOs covering the Medicare hospice benefit would enhance care quality while remaining budget neutral. Policies within the component, including comprehensive palliative care and concurrent care, fostered collaboration between MAOs and hospice physicians, aiming to mitigate care fragmentation at end-of-life stages. CMS gathered insights from various stakeholders to gauge the component's impact on care quality and safety. The decision to discontinue the Hospice Benefit Component does not indicate its success; CMS plans to evaluate it separately. CMS indicated that it would utilize the lessons learned from the Component and release clarifying guidance later this year.
HHS Releases 2023 Equity Action Plan Update
On February 14, HHS released the 2023 update to the Equity Action Plan related to its implementation of President Biden’s Executive Order on Further Advancing Racial Equity and Support for Underserved Communities Through The Federal Government. In alignment with the Biden-Harris Administration’s whole-of-government equity agenda, this Equity Action Plan supports HHS in advancing health equity and well-being for all. The plan includes the following five priority areas:

Since the release of the HHS’ first Equity Action Plan in 2022, HHS has proposed rules on language access and rules that prohibit discrimination based on disability. Additionally, HHS approved the provision of 12 months of continuous postpartum coverage through CMS in 42 states, D.C. and the Virgin Islands.
PAI is focused on addressing health equity issues for both patients and physicians, especially those in rural areas. This is a complex issue, and PAI will draw on the work of The Physicians Foundation, which has studied the problem of health-related social needs, as it works to advance policies that reduce inequities in health care delivery.
Meet Ali Ingersoll, the Quirky Quad, and Hear Her Take on Prior Auth Reform

Ali Ingersoll, the Quirky Quad, tells her life story, advocates for Prior Auth Reform
RALEIGH -- If you've never heard of Ali Ingersoll, this is your lucky day! She is a force of nature who has overcome unbelievable obstacles to emerge as healthcare advocate, public speaker, podcaster, disability consultant, and Ms. Wheelchair America!
Ali’s life took an unexpected turn when a tragic accident left her paralyzed at 27 leaving her paralyzed from the chest down. While she grappled with feelings of hopelessness through 7 years of life altering diagnoses, she was convinced her life had reached its end. Through her journey of self-discovery, she learned how to shift her thinking through harnessing the power of persistence to overcome incredible adversity.
She now calls herself the Quirky Quad, who normalizes disability "through dark humor and determination." Ali took some time to tell her story to the staff of the North Carolina Medical Society. Her presentation was both awe inspiring and motivational. She talked about how her accident led her down a daunting path of healthcare roadblocks and how she knocked them down one by one.
During her talk with NCMS staff she talked about the need for Prior Authorization reform in North Carolina, because, in her words, if she hadn't worked so hard she "would be dead."
Take a moment and hear her conversation. A full interview with Ali will be coming soon.
https://youtu.be/5j6elOh8n_U
Learn more about Ali here:
NCMS CEO Chip Baggett Addresses NHPCMS, Invites You to White Coat Day in June

New Hanover and Pender County Medical Society Gets Outline of NCMS Priorities from Chip Baggett
(WILMINGTON) -- North Carolina Medical Society EVP/CEO Chip Baggett greeted an excited crowd in Wilmington Wednesday night at the New Hanover Pender Counties Medical Society was treated to an evening hosted by NCMS.
Baggett outlined the strategic priorities of the NCMS and answered questions from the crowd. He stressed how NCMS is working for our members and for patients across the state. Issues included how NCMS is making it easier for you to care for your patients, ensuring you have a choice of where and how you practice, the NCMS Leadership College, and helping you care for yourself so you can continue to show up for your patients.
Guests included NCMS Board member Dr. Claude Jarrett and former NCMS President Dr. Michael Utecht.
The presentation ended with Baggett saying "We are a political animal, medicine is a political animal, society is a political animal, you as doctors are political animals. I think it is really important in a time where everybody is talking about absolutes, we need to be the example of how to live a better society. I believe you do that every single day. Every single day in your clinic you show up and talk to patients who you don't know everything about. You don't know everything that is going on in their life. You don't know what brought them to other problems in their life outside of medical issues. You sit down and have a conversation with them about their needs in that moment. Right then right there. You find a solution. You don't worry about if they voted for the person you voted for, you don't care if they are running for office, you don't care if they can pay their bill. You just see them and take care of them.
Go forth and befriend. Befriend those who don't look, live, love, or vote like you. May your friendships so confuse the world that the church and state have to change their rules to make sense of your friendships. I believe we are doing that. If we can get our friends to do what you are doing on a daily basis we will have a better society. "
Empowered Members Power Change
Flood the General Assembly with White Coats June 12!
There is power in numbers, and a great way to demonstrate that is by joining your colleagues for a day of legislative engagement in Raleigh!
We'll gather at the NCMS headquarters in the morning for a brief overview of the day (and breakfast!). Learn about the latest developments at the NC General Assembly and the best messaging to use when meeting with your legislators. Then head down to the Legislative Building to meet one-on-one with your representatives and attend committee meetings on important healthcare issues. We'll wrap up the day with a Legislative Reception at the NC Museum of History. Share your experiences from the day with other attendees and NCMS staff while enjoying light hors d'oeuvres and drinks!
Space is limited, so be sure to register soon!
Shining Red Eyes and Deafening Noise! The Cicadapocalypse Coming Any Time Now

First Time This Has Happened Since
Thomas Jefferson Was President!
Southeast Should See Them Soon
(CNN) -- In a matter of weeks, they will dig their way out from underground, red eyes shining, deafening song filling the air. It will be a confluence of creatures the likes of which hasn’t been seen in the United States since Thomas Jefferson was president — and won’t happen again until 2245. It’s a rare emergence of insects some are referring to as cicadapocalypse.
Billions of cicadas are set to surface this spring as two different broods — one that appears every 13 years, and another every 17 years — emerge simultaneously. The 13-year group, known as Brood XIX, or the Great Southern Brood, is the largest periodical cicada brood, stretching across the southeastern United States. The Northern Illinois Brood, or Brood XIII, emerges every 17 years.
“It’s rare that we see this size of double brood emergence,” said Dr. Jonathan Larson, an extension entomologist and assistant professor at the University of Kentucky. “We’re talking about an absolute oddity of nature, one of America’s coolest insects.”
Though the idea of a cicadapocalypse may seem foreboding, experts predict that the two broods won’t overlap significantly, and the bugs themselves, while loud and numerous, are harmless. Here’s what you need to know going into cicada season.
What to know about cicada broods
This spring’s bugs are part of a genus, or group, of cicadas in the eastern US known as the Magicicada, or periodical cicadas. Three species emerge on a 17-year cycle, and four species are on a 13-year cycle. (Scientists have long debated the significance of these numbers, which are both prime — some researchers have suggested that emerging on these prime-numbered years makes the periodical cicadas less likely to be killed by predators that have two- or three-year life cycles, but the jury’s still out.)
The pattern periodical species follow is different from that of “annual” cicadas, which don’t actually have an annual life cycle, even though you can see them every summer in much of the United States. The nymphs, or babies, of annual cicadas spend two to five years underground, slowly growing, until they are ready to emerge. There are just so many overlapping generations that there appears to be a steady stream of these cicadas every year.
It’s easy to tell annual and periodical cicadas apart. Annuals tend to emerge later in the year than periodicals. For instance, the “dog day” annual cicadas in the genus Neotibicen tend to show up in the dog days of summer, around August, whereas the periodicals make their appearance in the spring. While there are numerous species of annual cicadas, many of them are large and greenish. Periodical cicadas are smaller and mostly black, with bright red eyes and orange-tinged wings and legs.
Cicadas are divided into groups called broods based upon when they emerge. A brood can contain cicadas from multiple species. As long as they are adults in the same 13- or 17-year cycle at the same time, they count as members of the same brood.
When and where will the cicadas emerge?
This spring’s periodical cicadas will make their appearance when the soil temperature 8 inches (20 centimeters) deep reaches 64 degrees Fahrenheit (about 18 degrees Celsius). It will likely happen sometime in mid-May. The individual bugs’ adult life cycles are just a few weeks, but their emergence will be staggered, so there will be about six weeks of cicadas.
That month-and-a-half period will be jam-packed with loud singing, mating and then dying, like “the most macabre Mardi Gras that you’ve ever seen,” Larson said.
Parts of the Midwest and Southeast are due for cicadas this spring.
Northern Illinois, along with southern Wisconsin, eastern Iowa and northwest Indiana are likely to see bugs from Brood XIII; central and southern Illinois, most of Missouri and scattered areas of Kentucky, Tennessee, Virginia, Maryland, North Carolina, South Carolina, Georgia, Alabama, Mississippi, Louisiana and Arkansas are due to get Brood XIX bugs.
There are some areas of central Illinois where the two broods’ geographic ranges have historically been close to each other and could potentially overlap. However, predictions of a cicadapocalypse — in which Brood XIII and Brood XIX show up at the same place at the same time — are probably an exaggeration.
“We’re not even sure that they’re really going to overlap,” said Dr. Chris Simon, a professor of ecology and evolutionary biology at the University of Connecticut. Her research group at the university maintains a website of cicada information, which includes maps showing where the broods have historically emerged.
The double emergence of Broods XIX and XIII is rare, occurring every 221 years (when the 13-year and 17-year cicadas overlap, as 13 times 17 is 221). These two broods haven’t been aboveground at the same time since 1803, and after this year, they won’t be reunited until 2245.
However, the co-occurrence of different cicada broods, somewhere in the United States, isn’t quite as rare. Such an event last happened in 2015; it’ll happen again in 2037.
Preparing for cicadas
Even though a major overlap of the two cicada broods is unlikely, only getting one brood in an area still means countless bugs.
“You should expect lots and lots of cicada exoskeletons to be covering your trees and shrubs. You should expect to hear lots and lots of noise,” Larson said. The insects are likeliest to be in wooded areas near water, he added.
While the sheer volume of insects, along with their distinctive jackhammer-loud sounds and bright red eyes, might give some people pause, Larson notes that cicadas are harmless. They don’t pose a risk to garden plants. However, if you have young trees, cicadas could potentially damage them when the insects cut into branches to lay their eggs. You can mitigate this harm by covering the trees with cicada nets.
Cicadas won’t bite or sting you or your pets. If your dog eats a cicada or two, he said, the animal will be just fine.
Dogs aren’t the only ones tempted to nosh on cicadas; people have eaten them for thousands of years. “They have kind of a natural, sweet nut flavor,” Larson said. (If you’re allergic to shellfish though, you should avoid eating cicadas — a protein in shellfish that’s tied to allergies is also present in many insects.)
If you live in an area with cicadas making an appearance this spring, you can download community science apps to help researchers studying these bugs.
“The main thing we want people to know is that they should download the Cicada Safari app, which is free on the web, and all they have to do is photograph whatever cicadas they see,” Simon said. Those photographs are sent to scientists, who then map where and when the cicadas are emerging: information vital for scientists studying how climate change affects cicadas and predicting future cicada activity.
Beyond the bigger scientific story of cicadas, Larson said he hopes people will embrace cicada spring simply because it’s a rare chance to see some of the world’s most unusual bug behavior.
“These are some of the coolest insects in America,” Larson said. “I really hope that people will appreciate this for what it is: this unique natural phenomenon that you don’t get anywhere else. It’s beautiful.”
Kate Golembiewski is a freelance science writer based in Chicago who’s especially interested in zoology, thermodynamics and death.
Duke Researchers Lead International Study on Jardiance and Heart Failure

Therapy Shows Promise in Delaying Hospitalizations for Heart Failure
Diabetes drug did not prevent all cardiovascular outcomes, but it did affect hospitalizations
(DukeHealth News & Media) -- About 800,000 people in the U.S. suffer a heart attack every year, and about 30% of them will go on to develop heart failure. There are limited treatments to prevent or slow that development.
A large international study led by Duke researchers investigated whether the diabetes drug empagliflozin (marketed under the brand name Jardiance) might prevent heart failure in patients after they had suffered acute myocardial infarction (heart attack).
While the study found that the drug did not reduce deaths, secondary findings show it did slow the time to first hospitalization for heart failure and reduced the total number of subsequent heart failure hospitalizations.
The secondary findings are published in the journal Circulation and presented at the American College of Cardiology’s Annual Scientific Session on April 6. Other findings from the study, called EMPACT-MI, were also simultaneously published in the New England Journal of Medicine and the Journal of the American College of Cardiology.
Empagliflozin was originally approved for use in patients with diabetes, but investigators chose to study the drug based on earlier findings that it showed benefit in preventing active heart failure from becoming worse. The study was funded by two companies that manufacture the drug - Boehringer Ingelheim and Eli Lilly and Company.
The study enrolled 6,522 patients across 22 countries, with roughly half randomly assigned to receive the therapy and the other half placebo. Both groups otherwise received standard care. Investigators credit the study’s simple design to its broad reach.
The Duke Clinical Research Institute coordinated and led the conduct of the trial.
The study findings on lower rates of heart failure offer some hope and underscore the importance of preventing poor outcomes after a heart attack, according to principal investigator and corresponding author, Adrian Hernandez, M.D., director of the Duke Clinical Research Institute.
“Developing heart failure is one of our major public health problems, and any step that gets us closer to preventing it is a step in the right direction,” Hernandez said. “After a heart attack, we should really be focused on how to prevent problems, especially the development of heart failure. This therapy fills in that gap.”
Hernandez said he would be curious to investigate the secondary findings further, especially because there are so many different factors that can play out after a heart attack.
“Heart attacks are pretty dynamic – in the first 24 hours things can change for the better or the worse; you can end up having a small heart attack or a big one,” Hernandez said. “We don’t know if there could be a difference in results from the therapy depending on the type of event and the timing of giving a treatment. Those could be areas to consider.”
In addition to Hernandez, study authors for the Circulation publication include Jacob A. Udell, W. Schuyler Jones, Stefan D. Anker, Mark C. Petrie, Josephine Harrington, Michaela Mattheus, Svenja Seide, Isabella Zwiener, Offer Amir, M. Cecilia Bahit, Johann Bauersachs, Antoni Bayes-Genis, Yundai Chen, Vijay K. Chopra, Gemma Figtree, Junbo Ge, Shaun Goodman, Nina Gotcheva, Shinya Goto, Tomasz Gasior, Waheed Jamal, James L. Januzzi, Myung Ho Jeong, Yuri Lopatin, Renato D. Lopes, Béla Merkely, Puja B. Parikh, Alexander Parkhomenko, Piotr Ponikowski, Xavier Rossello, Morten Schou, Dragan Simic, Philippe Gabriel Steg, Joanna Szachniewicz, Peter van der Meer, Dragos Vinereanu, Shelley Zieroth, Martina Brueckmann, Mikhail Sumin, Deepak L. Bhatt, and Javed Butler.
Mortality Gap Widens Amid Holes in Rural Healthcare Access, South Has Widest Gap

City-country mortality gap widens amid persistent holes in rural health care access
As Roach tracked the health of Arizona residents, the gap between mortality rates of people living in rural areas and those of their urban peers was widening.
The research analyzed Centers for Disease Control and Prevention death data from two three-year periods — 1999 through 2001 and 2017 through 2019. In 1999, the natural-cause mortality rate for people ages 25 to 54 in rural areas was only 6% higher than for city dwellers in the same age bracket. By 2019, the gap widened to 43%.
The researchers found the expanding gap was driven by rapid growth in the number of women living in rural places who succumb young to treatable or preventable diseases. In the most rural places, counties without an urban core population of 10,000 or more, women in this age group saw an 18% increase in natural-cause mortality rates during the study period, while their male peers experienced a 3% increase.
Within the prime working-age group, cancer and heart disease were the leading natural causes of death for both men and women in both rural and urban areas. Among women, the incidence of lung disease in remote parts of the nation grew the most when compared with rates in urban areas, followed by hepatitis. Pregnancy-related deaths also played a role, accounting for the highest rate of natural-cause mortality growth for women ages 25 to 54 in rural areas.
The negative trends for rural non-Hispanic American Indian and Alaska Native people were especially pronounced. The analysis shows Native Americans 25 to 54 years old had a 46% natural-cause mortality rate increase over those two decades. Native women had an even greater mortality rate jump, 55%, between the two studied time periods, while the rate for non-Hispanic White women went up 23%.
The rural-urban gap grew in all regions across the nation but was widest in the South.
The increased mortality rates are an indicator of worsening population health, the study authors noted, which can harm local economies and employment.
As access to and quality of health services in rural areas continue to erode, rural health experts said, the USDA findings should spur stronger policies focused on rural health.
Alan Morgan, CEO of the National Rural Health Association, said he found the report "shocking," though, "unfortunately, not surprising."
The disparity warrants greater attention from state and national leaders, Morgan said.
The study does not address causes for the increase in mortality rates, but the authors note that differences in health care resources could compromise the accessibility, quality, and affordability of care in rural areas. Hospitals in small and remote communities have long struggled, and continued closures or conversions limit health care services in many places. The authors note that persistently higher rates of poverty, disability, and chronic disease in rural areas, compounded by fewer physicians per capita and the closure of hospitals, affect community health.
Roach said his past job as an epidemiologist included working with social vulnerability indexes, which factor in income, race, education, and access to resources like housing to get a sense of a community's resilience against adverse health outcomes. A map of Arizona shows that rural counties and reservations have some of the highest vulnerability rankings.
Janice C. Probst, a retired professor at the University of South Carolina whose work focused on rural health, said many current rural health efforts are focused on sustaining hospitals, which she noted are essential sources of health care. But she said that may not be the best way to address the inequities.
"We may have to take a community approach," said Probst, who reviewed the report before its release. "Not how do we keep the hospital in the community, but how do we keep the community alive at all?"
The disparities among demographics stood out to Probst, along with something else. She said the states with the highest rates of natural-cause mortality in rural areas included South Carolina, Mississippi, Georgia, Alabama, and others that have not expanded Medicaid, the joint federal and state health insurance program for low-income people, though there are efforts to expand it in some states, particularly Mississippi.
It's an observation the USDA researchers make as well.
"Regionally, differences in State implementation of Medicaid expansion under the 2010 Affordable Care Act could have increased implications for uninsured rural residents in States without expansions by potentially influencing the frequency of medical care for those at risk," they wrote.
Wesley James, founding executive director of the Center for Community Research and Evaluation, at the University of Memphis, said state lawmakers could address part of the problem by advocating for Medicaid expansion in their states, which would increase access to health care in rural areas. A large group of people want it, but politicians aren't listening to their needs, he said. James also reviewed the report before it was published.
According to KFF polling, two-thirds of people living in nonexpansion states want their state to expand the health insurance program.
Morgan added the study focused on deaths that occurred prior to the COVID-19 pandemic, which had a devastating effect in rural areas.
"COVID really changed the nature of public health in rural America," he said. "I hope that this prompts Congress to direct the CDC to look at rural-urban life expectancies during COVID and since COVID to get a handle on what we're actually seeing nationwide."
In Arizona, the leading cause of death for people 45 to 64 in 2021 in both rural and urban areas was COVID, according to Roach.
EPA Takes Action on PFAS Pollution in Drinking Water, NC Response

EPA Announces First-Ever National Standard to Address PFAS in Drinking Water, Delivers an Additional $1 Billion through President Biden’s Investing in America Agenda to Combat PFAS Pollution
WASHINGTON -- The Environmental Protection Agency announced on Wednesday, the first-ever national legally enforceable drinking water standard for PFAS, which will protect 100 million people from PFAS exposure, prevent tens of thousands of serious illnesses, and save lives. Per a release, the move "complements the Biden-Harris Administration’s commitment to combatting PFAS pollution and delivering clean water."
Details of the release:
President Biden has secured historic levels of funding to meet this new standard. Today, the Biden-Harris Administration is also announcing an additional $1 billion through President Biden’s Investing in America agenda to help every state and territory fund PFAS detection and treatment systems to meet the new standard. This funding is part of the $9 billion in dedicated funding through the President’s Bipartisan Infrastructure Law to address PFAS and other emerging contaminants in drinking water – the largest-ever investment in tackling PFAS pollution. An additional $12 billion in funding from the Bipartisan Infrastructure Law supports general drinking water investments, including PFAS treatment. The investments are part of the Justice40 Initiative, which aims to ensure that 40 percent of the overall benefits of certain federal investments flow to disadvantaged communities.
These actions will help tackle PFAS pollution that has devastated communities like Oakdale, outside of St. Paul, Minnesota, where decades of PFAS-containing waste dumped by a chemical plant has contaminated the community’s drinking water. In this area, cancer was found to be a far more likely cause of death in children than in neighboring areas. The funding announced today will build on funding from the President’s Bipartisan Infrastructure Law that is already helping communities address PFAS contamination, including a $33 million award for Tucson, Arizona to treat its PFAS-contaminated drinking water wells.
This funding also builds on President Biden’s action plan to address PFAS pollution, safeguard public health, and advance environmental justice – all while advancing the Biden Cancer Moonshot goal of cutting the cancer death rate by at least half by 2047 and preventing cancer before it starts by protecting communities from known risks associated with PFAS exposure.
As the first-ever Safe Drinking Water Act standard for PFAS – and the first for any new contaminants since 1996 – this rule sets health safeguards and will require public water systems to monitor and reduce the levels of PFAS in our nation’s drinking water, and notify the public of any exceedances of those levels. The rule sets drinking water limits for five individual PFAS, including the most frequently found PFOA and PFOS. Because PFAS can often be found together in mixtures, EPA is also setting a limit for any combination of four PFAS, including GenX Chemicals. This standard will reduce PFAS exposure in our drinking water to the lowest levels that are feasible for effective nationwide implementation.
Today’s announcements advance President Biden’s broader commitment to deliver clean water for every American. The President’s Bipartisan Infrastructure Law invests over $50 billion to upgrade water infrastructure – the largest investment in clean water in American history. This includes a historic $15 billion to replace toxic lead pipes and protect children from brain damage, as part of President Biden’s goal of replacing every lead pipe in the country within a decade.
Recent Federal Actions to Protect Communities from PFAS
Under President Biden’s leadership, nearly two dozen federal agencies and offices have made systematic and substantive progress to safeguard public health and protect the environment from PFAS in drinking water and beyond. This work is coordinated by the White House Council on Environmental Quality, which leads the Interagency Policy Committee on PFAS. Other new actions the Biden-Harris Administration has advanced to combat PFAS pollution over the past year include:
Protecting Firefighters from PFAS: The Biden-Harris Administration is committed to protecting firefighters from the harmful effects of PFAS contained in fire suppressing agents and firefighter gear. The Department of Defense is offering PFAS blood tests to military firefighters. The Federal Emergency Management Agency’s U.S. Fire Administration is working to reduce PFAS exposure and promoting access to early cancer screenings and participation in the National Firefighter Registry for Cancer led by the National Institute for Occupational Safety and Health as part of President Biden’s mission to end cancer as we know it.
Reducing PFAS in Fire Suppressants: The Department of Defense (DoD) qualified three fluorine-free foams to replace fluorinated Aqueous Film Forming Foam for shore-based firefighting activities at military installations, which the Federal Aviation Administration (FAA) has authorized for civilian airports. The FAA is assisting airports to transition to these new foams, and funding foam testing systems for airports that prevent environmental discharge. These changes will reduce the release of PFAS in the environment and protect the health of firefighters and local communities.
Supporting Healthcare Providers: The Agency for Toxic Substances and Disease Registry at the Centers for Disease Control and Prevention recently released the PFAS: Information for Clinicians resource guide. This information gives clinicians up-to-date resources and information they need to help patients with questions and concerns about PFAS exposure and health effects.
Phasing Out PFAS in Food Packaging: The Food and Drug Administration (FDA) announced the completion of the voluntary market phase-out of PFAS used on paper and paperboard food packaging, eliminating the primary source of dietary exposure to PFAS. FDA can now also test for 30 PFAS in a variety of foods to further protect people from dietary PFAS exposure.
Testing for and Cleaning Up PFAS Pollution: EPA continues to take key actions to address PFAS. For example, EPA is gathering data on 29 PFAS in the nation’s drinking water systems has collaborated with DoD to develop a method to test for 40 PFAS in various media including biosolids, groundwater, and fish tissue. EPA also updated its interim PFAS disposal and destruction guidance and has released a new method to test for 30 volatile fluorine-containing compounds in air including potential products of incomplete combustion of PFAS. DoD recently identified 40 installations where interim cleanup actions to prevent further PFAS migration are underway or will start in FY2024. These actions will address PFAS in groundwater to protect public health and the environment.
Reducing PFAS in Federal Procurement: EPA and the U.S. General Services Administration announced this week that custodial contracts for federal buildings will now only use cleaning products certified to ecolabels such as EPA’s Safer Choice and certain Green Seal standards, thereby avoiding products that contain intentionally added PFAS. This shift will protect the environment, federal custodial workers, other federal employees, and those visiting government buildings.
Response in North Carolina
NC Health News reports that on Wednesday, a host peakers including state and federal officials gathered at P.O. Hoffer Water Treatment Facility in Fayetteville to praise the new drinking water standards announced by the Environmental Protection Agency the day before. The safe drinking water standards set maximum contaminant levels for six PFAS, including GenX, which were manufactured at the Chemours Fayetteville Works plant.
All six chemicals found their way into the Cape Fear River, a contamination that was revealed in 2017. The river has been a source of contamination and consternation for people living in the lower Cape Fear basin ever since.
Governor Roy Cooper saying "[The administration] made a big promise that for the first time ever, we would set a national limit on PFAS in drinking water,” Cooper said. “Administrator [Michael] Regan and the Biden administration are delivering on that promise that they made not only to North Carolinians, but to all Americans across this country.”
“Drinking water contaminated with PFAS has plagued communities across this country for too long,” Michael Regan, EPA administrator, said on Tuesday on a call with the media. “President Biden has made tackling PFAS a top priority, investing historic resources to address these harmful chemicals and protect communities nationwide.”
Detlef Knappe, the North Carolina State University professor whose research led to the 2017 news story that revealed GenX, one class of PFAS in the Cape Fear River, said he was pleased by the EPA’s announcement and that North Carolina is ahead of many states in efforts to address PFAS.
NCMS Member Named Physician of the Year at AHHC H.O.M.E. Awards!

Dr. Deric Weiss AHHC H.O.M.E. Physician of the Year
NCMS Member Dr. David Tayloe, Jr. Recognized in US Congressional Record
NCMS Member, Congressman Greg Murphy, MD, Recognizes Dr. David Tayloe in the Congressional Record
April 7, 2024 -- Congressman Gregory Murphy, MD, honored NCMS member Dr. David Tayloe in the Congressional Record.
Here is statement:
"I was honored to recognize an incredible physician, Dr. David Tayloe, in the Congressional Record for his commitment to community healthcare and his passionate advocacy for children.
Dr. Tayloe has led an extraordinary life of servant leadership. Be it caring for children at his practice Goldsboro Pediatrics, spearheading pediatric advocacy in the North Carolina General Assembly, or serving as the President to the American Academy of Pediatrics. He has spent his life caring for the less fortunate at home and abroad. I am in awe of his stewardship.
Thank you for being such an incredible leader in Eastern North Carolina. We are lucky to have you!"
Dr. Tayloe is a North Carolina Medical Society Life Member, a member of the NCMS 1849 Society, and has served on the Goldsboro City School and the Wayne County Public School Boards of Education. He graduated from the UNC-Chapel Hill School of Medicine. He founded Goldsboro Pediatrics in 1978.
NCMS Member Dr. Leo Spector Featured in "Business NC"
OrthoCarolina’s CEO has MD-MBA cred
OrthoCarolina’s new leader merges business acumen with a surgical background.
 (BusinessNC, Kevin Ellis) -- When Charlotte spine surgeon Leo Spector returned to the classroom more than four years ago, his fellow students in the Duke University Executive MBA program peppered him with questions. A disconnect existed, he says, about the business of healthcare and his classmates’ familiarity with nonmedical corporations.
(BusinessNC, Kevin Ellis) -- When Charlotte spine surgeon Leo Spector returned to the classroom more than four years ago, his fellow students in the Duke University Executive MBA program peppered him with questions. A disconnect existed, he says, about the business of healthcare and his classmates’ familiarity with nonmedical corporations.
“Running a factory is not the same as running an operating room, although you can apply some of the same principles,” says Spector, who earned his MBA from Duke in 2020 and became CEO at Charlotte-based OrthoCarolina in January.
Spector, the son of a general orthopedic surgeon in Boston, started working at OrthoCarolina during a fellowship at its spine center 18 years ago. Around the same time, about 45 doctors who had been with Charlotte Orthopedic Specialists and Miller Orthopaedic Clinic formed the physician-owned practice in 2005.
Under previous CEOs Dr. Dan Murrey and Dr. Bruce Cohen, both surgeons like Spector, the practice has grown to about 112 physician shareholders, 472 medical providers and 1,700 employees. It has more than 30 orthopedic practices from Boone to Bennettsville, South Carolina, and as far west as Shelby.
Spine surgeon Murrey left in 2016 and is now chief physician executive for a large specialty care division owned by United Healthcare Group. Cohen, who is a foot and ankle surgeon, has returned to his general practice at OrthoCarolina.
While interviewing him for the job, Spector’s colleagues took note of his degree from Duke, which ranked as the fifth-best Executive MBA program last year, according to U.S. News
& World Report. “I think sort of tongue-in-cheek, they said, ‘OK, now that you’ve got your MBA, you’re ready to be the CEO, right?
“And I said, ‘I’m as ready to be the CEO with my MBA as I was ready to be a doctor with my MD,’ meaning, yeah, you’ve got the schoolwork, but you also have to get the actual practical experience,” says Spector.
Pursuing an MBA was a personal choice, supported by his wife and two children, who were 10 and 14 when he started the 18-month program. He says he had grown confident in his skill as a spine surgeon, a responsibility that terrified him when he was starting his practice. He knew his competency as a spine surgeon had grown when repairing a broken ankle caused him more anxiety than cutting into someone’s back, he notes.
CONSTANT GROWTH
Spector has always been interested in the business of medicine, which led him to leadership positions within OrthoCarolina, including chief quality officer and chair of
the Quality/Value Committee.
“I felt if I wanted to grow as an administrator, I should go back and get the formal education,” he says. “Life is all about learning and growing and constantly developing,” he adds. “Once you stop doing that, what’s the point?”
Spector and his wife, who have been married for 24 years, discussed the MBA’s cost and time commitment. Both agreed that if he didn’t pursue his goal, they’d regret the decision in 10 years. He isn’t sure if the degree factored into him getting the CEO position but counts that as a side benefit.
“I recommend business school to anybody. I really did love that 18-month period of time learning,” he says. “Business school is one of those places where every class is so applicable to life. Like, I took my negotiation class, and my wife didn’t like that because now I can negotiate with her on everything.”
He continued his medical practice during his MBA work and he’s still practicing two days a week. The program required him to spend one weekend a month at the Durham campus, with other coursework completed at night and on weekends. Approximately 20% of his class worked in the healthcare industry, and about half of those were physicians.
Nowadays, he spends a day per week seeing patients in a clinic setting, with a second day focused on surgeries. Keeping his hand in the practice of medicine remains important. “There’s obviously high stakes involved with spinal surgery, but like anything in life where there’s high risk there’s also high rewards,” he says. “There’s a great opportunity to really make a high impact in improving someone’s life and that’s what I love about the job.”
In the medical hierarchy, surgeons rank toward the top in pay. In 2022, orthopedic surgeons had the second-highest average annual compensation ($573,000) for specialists, behind plastic surgeons ($619,000), according to a report by Medscape news service.
“Every surgeon thinks they’re a rock star. You have to have a certain ego to think you should be able to cut open a human body and make it better,” he says. “No matter how big the ego is, they all learn that surgery is a very humbling experience. Typically, when your ego gets a little too big, it’s about to get deflated a little bit because unfortunately surgery doesn’t always go exactly the way we want it to despite the best efforts from the team and the surgeon. Those kinds of things help keep the ego in check.”
OrthoCarolina considers it important that a physician lead the practice. “Part of the desire to have an MD/CEO at OrthoCarolina is to have someone who is trained to take care of the patients every single day and sees the challenges that the providers (of care) face and the patient’s face,” says Spector.
He also sees the benefit of doing both. “When I’m working as an administrator, as the CEO, I can have that direct understanding of one-on-one with the tree (patient) and also that 10,000-foot view of the forest (practice.)”
LEARNING CURVE
Early into his CEO role, Spector says he’s learning about the roles and challenges of his different duties.
“As a surgeon, we’re very much used to being in charge,” he says. “As CEO, I can’t do everyone’s job at OrthoCarolina.” One job requires making quick decisions, the other listening, making sure different perspectives are heard. His Duke training helped him understand he didn’t need to be an expert in finance, marketing or business operations to be a successful CEO.
“My job as CEO is not to do everybody else’s job, it’s to make sure we have a great team and that we’re all pulling in the same direction, which is making sure we’re doing a great job of taking care of patients.”
OrthoCarolina is focused on improving access to care and trying to contain healthcare costs, he says. The enterprise is largely content with its existing markets, which benefit from the region’s strong population growth. The most recent clinic opening was in Fort Mill, South Carolina, one of the fastest-growing Charlotte suburbs.
OrthoCarolina and Durham-based EmergeOrtho employ about 50% of North Carolina’s orthopedic surgeons and account for about half of the musculoskeletal spending, says Spector. Emerge is larger, with about 270 physicians and specialists and 45 offices ranging from Beaufort to Waynesville. The two practices don’t compete in the same cities, except for Hickory, reflecting a conviction that direct competition wouldn’t serve anyone’s best interest, he says.
Last year, the two practices partnered with Optum Healthcare, a subsidiary of UnitedHealth Group, to help both practices control costs and improve outcomes. That partnership, called Health Innovation Value Enterprise, could grow into a “good model to other regions or states” to replicate, he says.
“There’s enough waste in the health care system — as in any industry — if we can help
get that out of the system, there’s plenty of savings to go around for patients to the government to doctors,” he says. Minneapolis-based UnitedHealth is the largest U.S.
health insurer.
Both OrthoCarolina and EmergeOrtho have resisted the trend in medicine to sell ownership stakes to private-equity companies. At least 15 PE-backed management companies own practices nationally, with dozens of sales occurring since 2017, KFF Health News reported last year.
OrthoCarolna’s leadership in its field in the Charlotte region means it works closely with the two dominant hospital systems, Atrium Health and Novant Health. Having both institutions benefits the region and physicians, Spector says. “Monopolies from a business standpoint are typically not the best,” he says. “So having some competition pushes both of them to be better and provide better service to the customer.”
In most cases, OrthoCarolina surgeons consider a patient’s primary healthcare provider and then schedule a procedure at the corresponding hospital. That provides easier access to patient medical records and coordination with primary doctors.
Spector says his life changed when he came to Charlotte for a fellowship at OrthoCarolina Spine Center. He planned to return to the Boston area, where he attended the University of Massachusetts Medical School and did a residency, and join his father’s medical practice. But his wife, whom he met while an undergrad at Colgate University in Hamilton, New York, fell in love with the area and its climate. Their oldest daughter was then 6 months old; she’s now a high school junior.
“Life takes interesting turns,” he says. “You just have to be open to where they take you.” The decision made a big difference in his career, he adds. “I don’t think I could have done what I do here if I were in Boston just because it’s so entrenched and not open to different people coming in.”
Spector says he has no timetable for how long he’ll remain in the dual roles. That decision will be balanced with his professional life, his medical practice and his family, he says.
The full article first appeared in Business NC
Going to See the NC State Wolfpack (Men and Women - Woo Hoo!)? Here Are Some Tips for Your Trip

A Historic Weekend for NC State! Both the Men's and Women's Basketball Teams
are Playing in the Final Four!
RALEIGH -- Fans of North Carolina State are getting ready to switch into high gear. On Friday, play begins for two teams hoping to make it to a National Championship! First up will be the women on Friday at 7pm. The Wolfpack take on Number One seed South Carolina. If they survive that matchup, they will take on the winner of the UConn-Iowa game on Sunday.
For the men, who are experiencing a Cinderella tournament that has many recalling State's historic 1983 championship under the legendary Jim Valvano, the action begins Saturday at 6:09pm when they take on Number One seed Purdue. If the men advance they will play the winner of the Alabama-UConn game on Monday.
If you are planning to attend either, here are some things to look forward to:
The women play in Cleveland at the Rocket Mortgage FieldHouse. There are lots of events happening while you're in town. Check out events like the Four Bounce, Party on the Plaza, a FREE open practice by all four teams, and a Super Saturday concert. All you need to know about the events is here.
The men will be in Phoenix at the State Farm Arena and the city is rolling out the welcome mat. Events include the March Madness Music Festival with the Jonas Brothers, The Final Four Fan Fest, and loads of dining deals across the city. All you need to know about the events is here.
Everyone at the NCMS is wishing both teams the best as they represent North Carolina this weekend!
Duke Awarded Up to $33 Million to Develop OA Therapies that Rebuild Bone and Joints
Along with Boston Children’s Hospital and UCLA Health, the federally funded project aims to alleviate the heavy cost burden of osteoarthritis
(DukeHealth) -- Duke Health is part of a multi-institution research team receiving funding from the federal Advanced Research Projects Agency for Health (ARPA-H) to develop an osteoarthritis treatment that regenerates joints.
The research project, which includes teams from Boston Children’s Hospital and the David Geffen School of Medicine at UCLA, was awarded a contract of up to $33 million, funded in two phases over five years. The project director is Benjamin Alman, M.D., chair of the Department of Orthopaedic Surgery at Duke University School of Medicine.
“We need a new approach to treat osteoarthritis, which is a leading cause of disability and represents a $128 billion cost burden on the U.S. health care system,” Alman said. “Regenerating cartilage and bone would be an effective therapy, and we have the technology, resources, and expertise in hand to make this a reality.”
The research team will base its proposed new therapy on recent evidence that joint tissues can heal. They will build on previous findings from project members, including the identification of small molecules and proteins that improve the cartilage regeneration process; the development of methods to deliver agents and target them to relevant joint tissues; the restoration of joint and bone tissue to a more normal “younger” state in animal studies; and an understanding of the genes and pathways needed to generate articular cartilage.
“We will achieve our goal of delivering a regenerative treatment for osteoarthritis by capitalizing on the expertise of our multi-site team, which includes biologists with extensive experience in bone and cartilage regeneration, as well as chemists and bioengineers with expertise in cutting-edge technologies to deliver therapeutic agents to the right place at the right time,” said Thomas Kremen, M.D., orthopaedic surgeon at UCLA Health and lead investigator for the planned clinical trial.
The researchers propose three therapies. The first would be an injection targeted into the joint to release regenerative factors in the bone supporting injured cartilage. The second would be an injection into the joint to regenerate cartilage tissue. A third therapy would be a systemic version of the injectable that could home in on diseased cartilage tissues in patients who have osteoarthritis in multiple joints.
By applying these therapies to specific cell populations over the appropriate time frame, the researchers hope to rebuild and rejuvenate a fully functional joint.
“Our team represents a collective and relentless effort to deliver a solution to those that suffer from joint pain,” said April Craft, Ph.D., assistant professor of orthopedic surgery at Boston Children's Hospital and Harvard Medical School and site director of the research project. “Our goal is to restore function to damaged joints by reactivating our own cells in a way that promotes healthy tissue regeneration.”
The researchers will collaborate across a centrally coordinated process to share findings quickly and capitalize on the diverse expertise within the team. Work will include developing pre-clinical large animal studies, planning for clinical trials with a diverse population of participants, and drafting an effective commercialization and technology transfer plan.
“A unique aspect of the work is considering the diversity of patients who would benefit from the treatment from the start of the project,” Alman said. “Osteoarthritis does not affect all populations equally, and the project will include an arm to identify populations that would benefit the most and to ensure that the proposed therapies are readily available to those patients.”
Funding is through ARPA-H's Novel Innovations for Tissue Regeneration in Osteoarthritis (NITRO) program. Its stated goal is to develop new ways to promote joint repair, including injectables that regenerate bones and cartilage, and replacement joints built from human cells.
ARPA-H is a federal agency established to advance high-potential, high-impact biomedical and health research that cannot be readily accomplished through traditional research or commercial activity.
With Cancer Diagnosis, Catherine, Princess of Wales, Shines Brighter Light on Rise in Disease Among Young People

Over the past 30 years, early-onset cancer rose 79 percent, one global study found
(Rachel Uda) -- When Catherine, Princess of Wales, revealed that she was diagnosed with cancer, it stunned the world.
She’s active, she apparently maintains a diet rich in antioxidants and raw fruits and veggies, and she’s only 42. But sadly, the princess is part of an alarming global trend. Studies show that more and more young people seem to be developing cancer. We’re taking a closer look at the latest research on young-onset cancer.
Studies show cancer is striking more young adults
A 2023 study found that over the past three decades, cases of early-onset cancer — defined as those appearing in people under age 50 — shot up a striking 79 percent, while death among younger cancer patients rose 28 percent.
The paper, published in BMJ Oncology, analyzed data from 204 countries and found that breast cancer accounted for the largest number of these, while windpipe and prostate cancers rose the fastest among younger patients over the 30-year period.
Another study focusing on U.S. patients found a modest bump in under-50 cases, but a substantial increase in people diagnosed between the ages of 30 and 39. Cancers among this group, from 2010 to 2019, rose about 19 percent. In line with the global analysis, breast cancer was found to be the most common among younger patients, while the fastest-growing cancers were gastrointestinal.
What’s causing the rise in cancer rates in young adults?
Researchers don’t know exactly. Experts have long pointed to alcohol, tobacco use, and poor sleep as factors. The rise in obesity and environmental factors like pollutants and toxic chemicals we may encounter in our water and food could play a role too.
Some of it simply has to do with the fact that more people are getting screened and diagnosed earlier, says Katherine Crew, M.D., an oncologist and associate professor of medicine and epidemiology at Columbia University Medical Center.
“We’re offering more patients genetic testing, and when they test positive, are screening those people at a younger age. Women with BRCA-1 or BRCA-2 mutations might start breast MRI screening in their mid-20s or patients with Lynch syndrome might start colonoscopies earlier too,” Dr. Crew tells us. “I think that’s part of what’s driving this.”
Another area of focus has been the gut microbiome, the trillions of bacteria, viruses, and fungi living in your intestinal tract. The composition of this universe of microorganisms can be easily thrown out of whack by antibiotics or diets heavy in processed foods, which has been linked to inflammation and certain cancers.
The chances that there’s a “smoking gun,” or one factor that’s behind this disturbing trend is unlikely, says Peter Liang, M.D., a gastroenterologist and assistant professor at NYU.
“It’s much more likely that it’s a combination of different factors that play a role,” Dr. Liang tells us.
That’s why researchers like him, who are trying to get to the bottom of the rise in early-onset cases, are looking at an impressive array of possible culprits. Surveys from Dr. Liang’s study, called the Colorectal Cancer in Adults at Young Onset (CRAYON), ask participants questions like what kinds of jobs they had as teenagers to determine if they could have been exposed to any toxins, if they were breastfed, and even if they were born by C-section. (One recent study found that women born by cesarean were more likely to develop CRC before 50.)
“We have to do more right now and we need answers to be able to figure out how to protect future generations,” he says.
2024 Dirty Dozen List of Fruits and Vegetables, Clean 15 Released

Report: Strawberries still have the most pesticides of any American produce
(Business Insider - Lauren Edmonds) -- Strawberries continue to reign supreme on the Environmental Working Group's annual "Dirty Dozen" list, which ranks fruits and vegetables by pesticide contamination.
The "Dirty Dozen" list is part of EWG's 2024 Shopper's Guide to Pesticides in Produce published on Wednesday. The report analyzed data collected from tests conducted by the USDA and FDA on 47,510 samples from 46 fruits and vegetables.
Both agencies take precautions to clean the produce before testing, with the USDA peeling or scrubbing produce before washing and the FDA only removing the dirt. Still, the report found that the analyzed produce contained 254 traces of pesticides.
The National Institute of Environmental Health Sciences reports that more than 800 pesticides are registered in the United States, "some of which are used in large quantities and may pose risks for a variety of health problems."
Here are the fruits and vegetables ranked on this year's "Dirty Dozen."
The report also listed Clean 15. The items with the lowest amounts of pesticide residues, according to the EWG analysis of USDA data. Here is that list:
- Avacados
- Sweet corn
- Pineapple
- Onions
- Papaya
- Sweet peas (frozen)
- Asparagus
- Honeydew Melon
- Kiwi
- Cabbage
- Watermelon
- Mushrooms
- Mangoes
- Sweet Potatoes
- Carrots
The full report is available by clicking here.
Register Now for 'Global Impact: Climate Change and Our Health'

Global Impact: Climate Change and Our Health, April 11
Thursday, April 11, 2024, 3:45pm EST
VIRTUAL
From poor air quality and flooding to extreme heat and years-long droughts, devastating weather events take a physical, emotional,
and financial toll on populations across the globe and here in the U.S. especially in marginalized communities. Are increased extreme weather events leading to a rise in health issues? Should those issues be looked at holistically or separately?
Join POLITICO on Thursday, April 11 for a conversation examining links between catastrophic weather events and medical challenges, and how industry and government can better collaborate to tackle disparities at the intersection of climate change and health care.
REGISTER HERE
Match Day Madness! NCMS Celebrates Milestone for All Physicians!

NCMS Match Day Social in Chapel Hill is Roaring Success!
NCMS celebrated Match Day with members, physicians, PAs, students, residents, friends, and supporters. It is a great example of the importance of being together! The North Carolina Medical Society provides the space and community to come together, across all specialties, to enhance the profession of medicine as colleagues and medical professionals.
You can be part of the fun and fellowship with your friends and peers. Make new friends and learn more about how NCMS can help you as you continue your career in medicine.
Our next regional meeting is heading to the beach! Look for more information about the event in Wilmington on April 10.
Happy Pi Day from NCMS!
Why shouldn't you eat too much pi?
You'll end up with a big circumference!
Happy Pi Day from the North Carolina Medical Society!
UNC Researchers Expand Understanding of How Body, Brain Communicate

Researchers Expand Our Understanding of How the Body and Brain Communicate
CHAPEL HILL - The human brain constantly receives information from the body, specifically from internal organs such as the heart and lungs. This information seldom reaches consciousness but is crucial for maintaining a healthy body and for influencing performance in the brain, including perception, emotion, and cognition. Now, researchers are investigating how exactly the brain processes the incoming stream of information from the heart and lungs, leading to a broader understanding of brain-body integration and the resulting health or disease.

Publishing their work in the Proceedings of the National Academy of Sciences (PNAS), co-senior authors Vibhor Krishna, MD, associate professor of neurosurgery at the UNC School of Medicine; Ali Rezai, MD, director of the Rockefeller Neuroscience Institute and associate dean of neuroscience at the West Virginia School of Medicine; and Olaf Blanke, MD, PhD, director of the laboratory of cognitive neuroscience at the Swiss Federal Institute of Technology, discovered that specific neurons in the thalamus are actively involved in processing cardiac and respiratory signals.
“Each heartbeat and every breath create a rich, incoming stream of sensory information for the human brain,” said Krishna. “However, a deeper understanding of how the brain integrates this information has remained elusive. We have been interested in discovering how the human brain achieves the integration of cardio-respiratory information and whether its breakdown is linked to any disorders of the brain, heart, or lungs observed in the clinic.”
Over the years, clinical and research teams collaborated to painstakingly study this integration using an established technique of microelectrode recording during deep brain stimulation surgery. Using a new approach to study single neurons in three different thalamic regions, the researchers were able to observe a direct functional involvement of thalamic and subthalamic neurons in processing cardio-respiratory signals. This information can help to better characterize how subcortical regions of the brain process signals through a functional pathway from internal organs.
To complete this work, the research team took advantage of microelectrode recordings during deep brain stimulation for patients undergoing treatment for neurological conditions. The researchers then used these recordings to investigate the activity of single neurons related to cardiac and respiratory functions in three subcortical regions: ventral intermedius nucleus and ventral caudalis nucleus of the thalamus, and the subthalamic nucleus.
They found that about 70% of the recorded neurons were modulated by either the heartbeat, the cardiac inter-beat interval, or the respiration.
These cardiac and respiratory response patterns varied largely across neurons both in terms of timing and their kind of modulation, the authors wrote. A substantial proportion of these visceral neurons – about 30% – were responsive to more than one of the tested signals, underlining specialization and integration of cardiac and respiratory signals in subthalamic nucleus and thalamic neurons.
“We think our work will be significant for several medical specializations, including cardiology, pulmonology, neurology, psychiatry, and psychological research,” Krishna said.
Rezai added, “Better understanding of the human brain is the next frontier. And interdisciplinary collaborations between functional neurosurgeons and neuroscientists will enable us to gain an unprecedented window into the inner functioning of the human brain.”
Applauding this research as a significant step forward, Nelson Oyesiku, MD, PhD, chair of the UNC Department of Neurosurgery, said, “We understand that the brain maintains homeostasis throughout the body through direct neurological and endocrine regulation. This research reveals that the incoming information from the heart and lungs is processed in the thalamic and subthalamic brain regions, besides other regions, enabling our brain to effectively assume its role in regulating bodily functions.”
(Article: Courtesy UNC Health)
NC Representative David Rouzer Joins Other Congress Members to Relaunch Congressional Primary Care Caucus

Five US Congress Members Relaunch Congressional Primary Care Caucus During State of Primary Care Briefing
WASHINGTON, DC - This week, Congressman David Rouzer (R-NC), Congresswoman Jen Kiggans (R-VA), Congressman Joe Courtney (D-CT), and Congresswoman Lisa Blunt Rochester (D-DE) relaunched the bipartisan Congressional Primary Care Caucus.
The Caucus, which was first created by Congressman Rouzer and Congressman Courtney in 2015, aims to educate Congress on the importance of a comprehensive, continuous, coordinated, and connected primary care system for patients and communities nationwide.
The Caucus’ relaunch was announced at the organization’s first official event of the year, a briefing on the State of Primary Care in America. The briefing featured industry stakeholders from the Bipartisan Policy Center, Primary Care Collaborative, the National Association of Community Health Centers, and Urban Health Plan who emphasized the critical role primary care plays in improving health outcomes and reducing preventable healthcare costs.
The group discussed ways policymakers can work to ensure Americans have access to affordable, high-quality primary care services in rural and medically underserved areas.
Statements from involved members of Congress and involved organizations:

"Tens of thousands of families across the country, including many of my constituents in rural Southeastern North Carolina, face a shortage in primary care physicians to address health issues early before they become advanced," said Rep. Rouzer. "I'm proud to join my colleagues in relaunching the bipartisan Primary Care Caucus to ensure our healthcare system focuses on patients and brings primary care closer to home. Thank you to each of our participants for joining us to help craft solutions where patients receive the very best care at the lowest possible price."
“As the only geriatric nurse practitioner in Congress, I am proud to serve as a Co-Chair of the bipartisan Primary Care Caucus,” said Congresswoman Kiggans. “I look forward to working with Representatives Blunt Rochester, Rouzer, and Courtney to recognize the importance of primary care in saving overall healthcare costs while improving patient health outcomes. We must work to make primary care more accessible and available to all Americans, especially to our underserved populations. It’s an honor to advocate for America’s primary care professionals and the patients who depend on them…!”
"Increasing access to primary care is one of the best ways to promote better health outcomes and lower overall health care costs,” said Rep. Joe Courtney. “As a co-founder of the Primary Care Caucus with Congressman Rouzer, Congresswoman Blunt-Rochester, and Congresswoman Kiggans, I am looking forward to advancing health care policy that recognizes the importance of primary care in underserved areas, particularly rural communities, and works to strengthen our primary care workforce nationwide."
“Comprehensive, continuous, and equitable primary care is an essential part of our health system,” said Rep. Lisa Blunt Rochester. “I’m proud to join Rep. Courtney, Rep. Rouzer, and Rep. Kiggans in relaunching the Primary Care Caucus – a bipartisan avenue that will continue to help us support patients and providers by increasing access to primary care, improving primary care services, and investing in our critical primary care workforce.”
“The relaunch of the Primary Care Caucus is an important step forward in addressing major challenges plaguing the health care system—including high costs and worsening outcomes. Thank you Rep. David Rouzer, Rep. Jen Kiggans, Rep. Joe Courtney, Rep. Lisa Blunt Rochester and each member of the Caucus for your leadership and for recognizing the important role primary care must play in fixing health care in America. We look forward to working with you on practical solutions that ensure everyone has access to high-quality primary care.” - Ann Greiner, President and CEO, Primary Care Collaborative
"As the largest primary care organization, the American Academy of Family Physicians commends the relaunch of the Congressional Primary Care Caucus and its commitment to advancing comprehensive healthcare solutions. This initiative underscores the vital role primary care plays in fostering a healthier nation, and we look forward to collaborative efforts that prioritize accessible, whole person care for all." – Stephanie Quinn, Senior Vice President of External Affairs and Practice Experience, American Academy of Family Physicians
"NACHC thanks Representatives Rouzer, Courtney, Blunt Rochester, and Kiggans for their leadership in standing up this important caucus. We look forward to working with this caucus to find long-term federal solutions for the primary care workforce and advancing our shared goal of making comprehensive and cost-effective primary care available for everyone nationwide." – Paloma Hernandez, MPH, Chair, National Association of Community Health Centers (NACHC) Board of Directors and President and CEO, Urban Health Plan, Inc.
Click here for more information on the Primary Care Caucus and to sign up for updates.
Important CMS Announcement For Physicians Impacted by Cyberattack, Change Healthcare Disruptions

Hospitals, doctors, and clinics express frustration that they have to wait even longer for reimbursements after hackers paralyzed the largest U.S. billing clearinghouse
The Centers for Medicare and Medicaid Services announced a new opportunity for physicians impacted by the cyberattack and resulting disruptions with Change Healthcare to request advanced Medicare payments to help with cash flow disruptions. The details of the program, terms, and the steps needed to apply can be found in the links below.
CMS Statement - https://www.cms.gov/newsroom/press-releases/cms-statement-continued-action-respond-cyberattack-change-healthcare
What Primary Election Results Mean for NCMS Members

The results are in. What comes next?
Throughout the electoral process, the North Carolina Medical Society (NCMS) remains vigilant in political engagement to advance our health policy priorities. The Society is engaging with candidates across the state and closely monitoring outcomes, focusing on candidates supported by NCMS.
The top-of-ballot results saw President Joe Biden and former President Donald Trump secure victories, setting up a rematch of the 2020 election. In North Carolina, Attorney General Josh Stein and Lieutenant Governor Mark Robinson both prevailed in what will be a nationally-watched gubernatorial showdown in November.
A trend emerged in North Carolina, with physician candidates demonstrating significant success in State House races. NCMS members Drs. Timothy Reeder, Grant Campbell, and Ralph Carter all navigating competitive primaries to secure victories. This highlights the increasing influence of medical professionals in both local and state politics. Dr. Reeder now faces Renee Kempner, Dr. Campbell is running against Joanne Chesley, and Dr. Carter faces longtime State Representative Garland Pierce.
The influence of physician candidates also extends to the State Senate level with NCMS member Dr. David Hill running unopposed as a Democrat in District 7, securing an automatic advancement to the General election. Retired Physician Assistant Mark Hollo also secured a victory for the Republican nomination in District 45. Hollo is a former member of the NC House. These developments underscore the growing presence of medical professionals in shaping state-level policies supported by the continuing advocacy of the NCMS and its members.
At the Federal level, the success of NCMS member candidates remains evident. Drs. Greg Murphy and Steve Feldman advanced automatically in their unopposed Congressional House primaries. Republican Dr. Murphy is the incumbent and Dr. Feldman is pursuing his first foray into elected office as a Libertarian. Their candidacies demonstrate the increasing recognition of the need for the medical profession to aid in shaping Federal policy that impacts NCMS members and patients in North Carolina.
The primary election showcases a dynamic political landscape, marked by significant voter engagement and the rising influence of physician and physician assistant candidates. As the 2024 electoral process progresses, the North Carolina Medical Society will continue to engage with these and other candidates and advocate for policies that prioritize the well-being of all North Carolinians.
The NCMS congratulates these member candidates for making a professional and personal commitment to run for public office. They reaffirm the vital role of healthcare professionals in shaping the future.
Super Tuesday Results and What They Mean for NCMS

Super Tuesday Results Are In.
What Does That Mean For You?
The North Carolina Medical Society has several member candidates for both state and federal office. Over the past several months, many of them have answered questions important to NCMS members. So what happened?
 On Friday, The NCMS Vice President of Advocacy, John Thompson, will have an analysis of the results and the impact they have on the next several months.
On Friday, The NCMS Vice President of Advocacy, John Thompson, will have an analysis of the results and the impact they have on the next several months.
Look for his report in Friday's edition of Morning Rounds.
NC Medicaid will now cover imported benzathine benzylpenicillin for syphilis
A message from Elizabeth Cuervo Tilson, MD, MPH, State Health Director and Chief Medical Officer of NC Department of Health and Human Services:
Dear Colleagues:
NC Medicaid will now cover imported benzathine benzylpenicillin (Extencilline) for use in outpatient medical drug claims. This new coverage is being added to address the ongoing national shortages of Bicillin® L-A (penicillin G benzathine injectable suspension).
While we have not heard of major shortages in North Carolina, we wanted to ensure that providers had access to every tool that may be available.
The statement on the policy change is available at https://www.ncdhhs.gov/news/press-releases/2024/03/04/ncdhhs-releases-statement-state-health-director-dr-elizabeth-cuervo-tilson-increasing-access
Provider guidance on extencilline is available at https://dailymed.nlm.nih.gov/dailymed/drugInfo.cfm?setid=5a026d0c-6f91-4ee3-b193-b2186a37e7ca
More detailed information on Medicaid billing is available at NC Medicaid to Cover Imported Benzathine Benzylpenicillin (Extencilline): Billing Guidelines | NC Medicaid (ncdhhs.gov)
CDC Recommending Additional Covid-19 Vaccine for Those Over 65

New Guidance From CDC on Vaccines for the Elderly
Arund 98% of the US population has some kind of immunity to Covid-19, whether from infection, vaccination, or both, according to the CDC. But health experts say this only gives some protection against infection or severe disease. In response, the CDC this week recommended people age 65 and older should get an additional dose of the current Covid-19 vaccine. The current Covid-19 vaccine, which was updated last fall, is considered highly effective and may cut the chances of getting a symptomatic infection by half. This comes as the CDC is considering a shift to its Covid-19 isolation guidance to say that people no longer need to isolate once they have been fever-free for 24 hours and their symptoms are mild or improving.
68-Year-Old Man Now in HIV Remission

(NiceNews.com) -- When Paul Edmonds learned he had AIDS in 1988, he viewed it as a death sentence. But therapies helped him take control of the illness for more than three decades — and now he’s in full-blown remission, all thanks to a cancer diagnosis.
Blood cancers are common in older HIV patients, according to the cancer center City of Hope, where Edmonds, pictured on the left with husband Arnold House, was treated for his leukemia. In 2019, he received a transplant of stem cells that had a rare genetic mutation that causes HIV resistance.
As a result, he became the fifth person in the world to be cured of leukemia and reach HIV remission, a milestone recorded earlier this month in a study published by The New England Journal of Medicine. Of those five people, Edmonds, 68, is the oldest and had HIV for the longest period, 31 years.
Though he initially kept his identity anonymous, Edmonds went public with his journey last year. “A big reason I want to tell my story is to bring some hope for people with HIV,” he said at the time. “And I want to remember all those we lost"
Hear Paul in his own words
WSJ: DOJ launches an antitrust probe into UnitedHealth Group

(Yahoo Finance - Seana Smith, Brad Smith) -- Department of Justice (DOJ) officials have launched an antitrust probe into the relationship between UnitedHealth Group's (UNH) insurance division and its Optum health services segment, according to Wall Street Journal reporting.
Yahoo Finance Health Reporter Anjalee Khemlani breaks down the details, highlighting the other challenges UnitedHealth is facing.
For more expert insight and the latest market action, click here to watch this full episode of Yahoo Finance Live.
Editor's note: This article was written by Luke Carberry Mogan.
Video Transcript
BRAD SMITH: Shares of UnitedHealth under pressure this morning after the US Department of Justice reportedly kicks off an antitrust investigation into the company's relationship between its insurance unit and health services arm, according to the Wall Street Journal. For more on this, we've got Yahoo Finance's Anjalee Khemlani here with us with more. Hey, Anj.
ANJALEE KHEMLANI: That's right, guys. Hey. Yeah, this report not surprising a lot of people who have either, you know, looked at United's strategy before, or those who are former employees. We've actually spoken to some of those folks ourselves here at Yahoo Finance.
And I'll say that some of the things listed in this report, including what the relationship is between the two sides, and whether or not the company is inflating costs and inflating claims from one side to the other, really touches on some points of concern that others have had over the years, especially as Optum has grown to be the largest, or one of the largest, employers of physicians. So really setting up the company for a hard look. And it is not a very good year for United.
If you take a look back in the past year, not only did they recently have that cyber attack on their Change Healthcare subsidiary, but they also are facing a class-action lawsuit for denying claims through AI for elderly Medicare Advantage members. So, it really has been a tough year for the company when it comes to a lot of the different moving parts of it. And it's interesting that this is the thing that has really hit the stock.
But what the results of that probe will be, of course, we will have to see. But I've heard over the past several months that, basically, what has happened is, you know, there has been looking like inflation of the business that Optum has done over time, making it look like a really strong growth company when really it was just one side of the company funneling to another. So, will be interesting to see if those claims pan out.
SEANA SMITH: And it's a story we are going to continue to track. Again, UnitedHealth under pressure, off just nearly 4% here.
Additional Reading
Eight ECU Brody School of Medicine Students Named to FCLC

(ECU News Service) -- Noor Baloch, Nolan Davis, Michael Denning, Charles Johnson, Hannah Rayala, Emmalee Todd, Ben Wise and Michael Wright will join students from other colleges and universities across the state who are interested in leadership and professional growth.
“The FCLC program provides us with a unique, structured ability to engage with our future colleagues on community-level projects that address the varied landscape of health, health equity and health care,” Denning said. “Gaining intense leadership training alongside other health professions students will allow me both introspection and outward reflection on my future role, as well as mechanisms to ensuring our patients are excellently and compassionately cared for.”
Prospective students are referred and nominated to the program by faculty, mentors and others at their respective colleges. The 2024 class includes 27 students representing disciplines including medicine and pharmacy from ECU, UNC Chapel Hill and Duke, Campbell, Wake Forest, Western Carolina and Wingate universities in North Carolina, as well as St. Georges University in Grenada.
FCLC is a partnership with North Carolina Area Health Education Centers (NC AHEC) to provide opportunities of leadership in an interprofessional health care environment and networking across institutions. The one-year program is designed to enhance health care experience through advocacy, change-driving and individual leadership skills.
Baloch said she wants to be a leader when it comes to ensuring proper care for her patients.
“I felt that in order to be the best leader I could be, I needed additional training alongside other health care professionals to really understand my role as a physician in a health care team as well as establish how I can best serve my patients in that way,” she said. “Through this program, I am able to understand my own leadership style as well as my faults so that I can work on them and ensure I am self-aware regarding how I lead interactions with my patients.”
The program emphasizes leading in interprofessional health care environments and networking across institutions. The interactive learning format encourages participants to engage with their peers and program leaders, faculty and speakers. They also participate in a project that gives them exposure to some of the major health policy challenges relevant to North Carolina.
“This is an incredible opportunity for these eight students to work with other interprofessional students across the state to develop the skills necessary to be a leader in health care tomorrow,” said Dr. Amanda Higginson, Brody’s associate dean for student affairs. “We know our Brody graduates go on to do amazing things; this wonderful program will further develop these students to both improve the health and well-being of the region, but also to augment the already great training they receive here to prepare them to become physicians who will meet the health care needs of the state, both critical mission goals of the school.”
The students will have hands-on experience cultivating leadership skills including team-leading, communication and career development.
“The purpose is to build leadership that centers on self-awareness and fosters authenticity that allows each student to act in alignment with their core values as a leader, encourage and assess information from different perspectives, and balance transparency,” according to the program website. “With the individual core as a foundation for leadership development, this course prepares students for the leadership journey, allowing the individual to establish a strong sense of purpose and understanding of who they want to be as a leader.”
Todd said the nature of medicine as a “team sport” necessitates the ability to collaborate with other health care professionals at any given time.
“In order to do this, it’s important to understand your own teamwork preferences and leadership style and be able to refine them to better suit your purposes,” she said. “I believe my participation in FCLC is providing me the opportunity to do exactly that, which will hopefully lay the groundwork for not just my own success in residency and beyond, but the success of the health care teams of which I will be part.”
Todd said the unique experience to explore a current health-related policy issue in North Carolina is valuable because it gives students a chance to propose potential solutions.
“So much of what impacts our patients’ health are factors that we can’t necessarily do anything about within a half-hour annual physical — their housing situation; the ease of their transportation to work or school; the accessibility of nutritious food, clean water and green space where they live,” she said. “Working towards policy change is one way that physicians can make an impact on these broader societal factors, and it’s something that I would like to be involved in throughout my career. FCLC is equipping me with the experience and skillset I need to begin to pursue this goal.”
NCMS CEO Chip Baggett is excited for the new students. "Helping create the next generation of leaders in North Carolina is one of the core missions of the North Carolina Medical Society," says Baggett. "These eight new students will be ready to face the rapidly evolving world of healthcare and safeguard the quality of patient care for years to come. The KIPL Leadership College Program is a nationally renowned curriculum that will foster these student's leadership skills and help them build a network in the healthcare community. I look forward to meeting them and seeing how they impact the future."
Michael Wright and Hannah Rayala also serve on the NCMS Student Council.
For more information on NCMS Professional Growth programs click here.
NCMS Regional Event in Charlotte Draws Enthusiastic Crowd
 The North Carolina Medical Society is on the road again!
The North Carolina Medical Society is on the road again!
NCMS members, guests, and friends joined together in Charlotte Wednesday to enjoy some time together and learn more about the Society's mission.
CEO Chip Baggett spoke on how NCMS is advocating on issues important to members like reforming Prior Authorization. He also talked about the NCMS strategic priorities of relieving your administrative burdens, our lobbying work on issues that impact your practice, and the long list of ways NCMS can help you grow professionally. As always, the NCMS is focused on protecting you, the practice of medicine, and your patients.
The medical community is being siloed and fractured at every turn.
This event is a great example of the importance of being together. The North Carolina Medical Society provides the space for the community to come together, across all specialties, to enhance the profession of medicine as colleagues and medical professionals.
If you are already a member, thank you for your continued support. If you are not a member, please consider JOINING NCMS TODAY!
We plan to continue these community conversations all over the state, so please be on the lookout for our next one!
Register Now! NC Allergy, Asthma, and Immunology Society Annual Meeting is May 18-19
| Download the meeting agenda.
Accommodations: Be sure to reserve your room at the Crabtree Valley Marriott before Thursday, April 25 to get our discounted rate of $159. Use this link to book today! Exhibiting Opportunities: Help ensure a successful meeting by sharing the exhibitor prospectus with the product and service representatives who call on your practice. Questions? Contact Megan Eberle at [email protected] or call 919-833-3836. |
Primary Care in Crisis! New Report From The Physicians Foundation
Scorecard Highlights State-Level Primary Care Performance & Lack of Physician Training in Underserved Communities
The second national Primary Care Scorecard released today reveals an intensifying primary care crisis and identifies five reasons why access to affordable, quality primary care services is expected to get worse.
Developed by researchers at the American Academy of Family Physicians’ Robert Graham Center and co-funded by the Milbank Memorial Fund and The Physicians Foundation, The Health of US Primary Care: 2024 Scorecard report and data dashboard examine critical measures of primary care performance nationally and across all states. Key findings include:
1. The primary care workforce is struggling to meet population demands.
- Despite a rapidly aging population with higher levels of chronic disease, the number of primary care physicians (PCPs) per person has decreased.
- The share of all clinicians practicing primary care (including nurse practitioners and physician assistants) stagnated around 28% between 2016 and 2021.
- PCPs declined from 68.4 to 67.2 per 100,000 people between 2012 and 2021.
- There has been a 36% jump in the share of U.S. children without a usual source of care over the last decade and a 21% increase among adults.
- Demand for PCPs will only increase with time. The National Institute of Health estimates that the number of people 50 or older with at least one chronic disease will increase by 99.5%, from 72 million in 2020 to 143 million by 2050.
2. The primary care sector is experiencing a workforce exodus and lacks real-world community training opportunities.
- Primary care residency does not mean primary care practice. In 2021, 37% of all physicians in training specialized in primary care, yet only 15% of all physicians were practicing primary care three to five years after residency. The remainder subspecialized or became hospitalists who do not work in community settings.
- In 2020, only 15% of primary care residents spent a majority of their time training in community settings (outside of hospitals and academic health centers) — signaling that many residents may lack adequate experience practicing in real-world clinical environments.
- In 2020, fewer than 5% of primary care residents spent the majority of their training in Teaching Health Centers or rural training tracks, two programs that historically serve disinvested communities. Research indicates physicians who train in Teaching Health Centers are more likely to practice in underserved communities.
3. The US continues to underinvest in primary care, despite diminishing supply and growing demand.
- The share of total US health care spending devoted to primary care stayed under 6% from 2012 to 2021.
- Since 2019, investment in primary care has steadily declined across all major health care payers; this decline has been most pronounced for Medicare reimbursements for primary care services and providers, which have dropped by 15%.
- The compensation gap between primary care physicians and specialists discourages residents from choosing primary care.
4. Cumbersome electronic health records burden primary care physicians.
- In 2022, more than 40% of family physicians rated the usability of their electronic health record (EHR) systems as unfavorable. Over 25% reported overall dissatisfaction with their current EHR system.
- According to the American Board of Family Medicine, 16% of family physicians reported spending four or more hours per day on EHRs, taking time away from patient care.
5. Inadequate research funding impacts primary care access and quality.
- Since 2017, only 0.3% of federal research funding (administered through the National Institutes of Health, the Centers for Disease Control and Prevention, the Agency for Healthcare Research and Quality, and the U.S. Food and Drug Administration) per year has been invested in primary care research, limiting new information on primary care systems, delivery models, and quality.
- A lack of adequate data on the prevalence of hybrid primary care payment (a combination of fee-for-service and per-person payments) and the training of nurse practitioners and physician assistants), for example, makes it difficult to track progress on the implementation of high-quality primary care.
“As more and more patients struggle to get appointments with primary care practices, policymakers must come together to address the primary care crisis,” said Milbank Memorial Fund President Christopher F. Koller. “By prioritizing investments in primary care and expanding our physician workforce today, we can ensure that everyone in every community has access to high-quality primary care in the future.”
Key State Scorecard Findings:
- Workforce: Alaska ranks second among all states, following Idaho (38.2%), for having 36.2% of its clinician workforce in primary care overall (compared to 28.6% nationally) and first for primary care clinician density in the most disadvantaged areas, with 269 clinicians per 100,000 people (compared to 111.7 clinicians per 100,000 people nationally).
- Training: North Dakota is the highest-ranked state for physician training measures, with a larger share of new doctors entering primary care (36.4%) each year than the national average (21.6%) and a high rate of physicians, physician assistants, and nurse practitioners working in primary care at 26.6%, 44.2%, and 39.4%, respectively.
- Investment: Oregon has the highest overall investment in primary care, with 7.7% of all health care spending going to primary care, compared to the national average (4.7%). The state also has the highest primary care spending for commercial payers (9.1%) and Medicaid (9.2%), compared to the national averages of 5.6% and 4.7% respectively.
The Scorecard was developed in response to a call for an annual tracking tool to inform primary care policy issued by the National Academies of Sciences, Engineering, and Medicine in their 2021 report, Implementing High-Quality Primary Care Rebuilding the Foundation of Health Care. This seminal report provides policy recommendations for federal and state governments, health care organizations, and payers to strengthen primary care.
“Primary care is the cornerstone of our health care system, playing a pivotal role in improving our nation’s health by delivering accessible and timely care to those in need,” said Ripley Hollister, MD, a board member of The Physicians Foundation and a practicing family physician. “The findings and recommendations from the second national Primary Care Scorecard highlight that investment in primary care is vital for the future of health care. The report implores us to embrace and advance solutions that support primary care and allow everyone to live longer, healthier lives.”
READ THE FULL REPORT
READ THE PRESS RELEASE
About The Physicians Foundation
The Physicians Foundation is a nonprofit seeking to advance the work of practicing physicians and help them facilitate the delivery of high-quality health care to patients. As the U.S. health care system continues to evolve, The Physicians Foundation is steadfast in strengthening the physician-patient relationship, supporting medical practices’ sustainability and helping physicians navigate the changing health care system. The Physicians Foundation pursues its mission through research, education and innovative grant making that improves physician wellbeing, strengthens physician leadership, addresses drivers of health and lifts physician perspectives. For more information, visit www.physiciansfoundation.org
About the Milbank Memorial Fund
The Milbank Memorial Fund works to improve population health and health equity by collaborating with leaders and decision makers and connecting them with experience and sound evidence. Founded in 1905, the Milbank Memorial Fund advances its mission by identifying, informing, and inspiring current and future state health policy leaders to enhance their effectiveness; convening and supporting state health policy decision makers to advance strong primary care and sustainable health care costs; publishing high-quality, evidence-based publications and The Milbank Quarterly, a peer-reviewed journal of population health and health policy. For more information, visit www.milbank.org
Looking for Help? Asthma Medication Now Approved to Help Some Food Allergies

Xolair, the brand name for the drug omalizumab, is first medication approved to reduce allergic reactions caused by accidental exposure to food triggers
(The Hill, WGN) -- For decades, asthma patients have used a drug to help them breathe better. Now, the Food and Drug Administration has given the nod to use that drug to reduce serious reactions from food allergies.
Xolair, the brand name for the drug omalizumab, became the first medication approved to reduce allergic reactions caused by accidental exposure to food triggers. Patients as young as age 1 with allergies can take the drug by injection every two to four weeks, depending on their weight and their body’s response to allergens.
Many people with allergies — and their families — live with constant anxiety about exposure to allergens and often avoid dining out and other social situations.
“To have this protection is going to be life-changing,” said Robert Wood, director of the pediatric allergy division at Johns Hopkins Children’s Center.
The FDA decision is based on a study led by Wood and funded by the National Institutes of Health. It showed that Xolair allowed about 68% of participants with peanut allergies to tolerate about 600 milligrams, or about 1/2 teaspoon, of peanut protein, compared with about 6% of those who received dummy injections.
The results were similar for other allergens such as tree nuts, milk, egg and wheat, a study abstract reported. Full results are expected to be presented at a meeting and published in a peer-reviewed journal later this month.
Wood estimated that 25% to 50% of people with food allergies, particularly children and young adults, would elect to use Xolair.
The drug has been used “off-label” to treat food allergies, said Ruchi Gupta, director of the Center for Food Allergy & Asthma Research at Northwestern University. She welcomed full approval of the product.
Xolair is a monoclonal antibody, a type of treatment that works by blocking the body’s natural response to allergens. It was first approved in 2003 and has been used to treat asthma, nasal polyps and chronic hives. It is produced by drugmakers Novartis and Roche and is distributed by a Roche subsidiary, Genentech.
“This really is a difference maker for patients and parents who have severe food allergies,” said Sai Nimmagadda, an allergist at Lurie Children’s in Chicago.
“Every day here at Lurie, you see two or three kids come in with a reaction,” Nimmagadda said.
“Patients on Xolair were able to tolerate higher quantities of food compared to placebo. It will prevent up to 40 percent of patients who have allergic reactions and 30,000 ER visits a year,” Nimmagadda said.
“It’s the first known medication with the indication to prevent food allergies,” Nimmagadda said.
That means relieving the constant fear of accidental, life-threatening allergies.
“What we’re noticing is patients who are on Xolair can tolerate up to two and a half peanuts before they have a reaction, up to three and a half cashews, up to about two teaspoons of milk and maybe up to a quarter teaspoon of egg,” Nimmagadda said. “So, it brings the threshold up a little bit. So, instead of trace amounts causing the allergic reaction, now you can feel safe you can have accidental exposures and not end up in the emergency room.”
“You don’t have the allergic effects when you ingest the food you are allergic to,” Nimmagadda said.
The most common side effects of Xolair are injection site reactions and fever, but the FDA noted that the drug has also been associated with joint pain, rash, parasitic infections, malignancies and abnormal laboratory tests. Xolair comes with a warning saying the treatment itself can cause anaphylaxis and must be started in a health care setting equipped to manage the reaction.
The medication is not approved for emergency treatment of allergic reactions.
The list price for Xolair ranges from about $2,900 a month for children to $5,000 a month for adults, according to Genentech. Most insured patients typically pay less out of pocket, the company said.
The Associated Press contributed to this report.
UNC Scientists Create New Drug Delivery System
Wireless Drug Patch Shows Promise as Chronic Disease Treatment Delivery System
 The Spatiotemporal On-Demand Patch’s exposed circuit will be covered by material resembling a Band-Aid. It can receive commands wirelessly from a smartphone or computer to schedule and trigger the release of drugs from individual microneedles.
The Spatiotemporal On-Demand Patch’s exposed circuit will be covered by material resembling a Band-Aid. It can receive commands wirelessly from a smartphone or computer to schedule and trigger the release of drugs from individual microneedles.
Led by Juan Song, PhD, at the UNC School of Medicine, and Wubin Bai, PhD, at the UNC College of Arts and Sciences, research suggests that a wearable patch featuring electrically triggered microneedles for on-demand drug delivery could be the next frontier in treatment of neurodegenerative disorders and neurological injuries.
(UNC Health Newsroom) -- CHAPEL HILL, NC – University of North Carolina at Chapel Hill scientists created a new drug delivery system, called the Spatiotemporal On-Demand Patch (SOP), which can receive commands wirelessly from a smartphone or computer to schedule and trigger the release of drugs from individual microneedles. The patch’s thin, soft platform resembles a Band-Aid and was designed to enhance user comfort and convenience, since wearability is a crucial factor for chronically ill patients.
The research team, led by Juan Song, PhD, professor of pharmacology at the UNC School of Medicine, and Wubin Bai, PhD, assistant professor of applied physical sciences at the UNC College of Arts and Sciences, tested the SOP in a mouse model, using melatonin in the microneedles to improve sleep.
This research, published in the journal Nature Communications, opens the door to researching this wirelessly controlled patch to deliver on-demand treatments for neurodegenerative disorders, including Alzheimer’s disease. To that end, the UNC School of Medicine and UNC Health funded a $25,000 pilot project to test the SOP in a mouse model of Alzheimer’s disease.
“SOP’s ability to enable joint delivery of multiple drugs could address various aspects of Alzheimer’s Disease, such as reducing beta-amyloid plaques, mitigating neuroinflammation and enhancing cognitive function,” said Bai, a co-senior author.
The open access paper titled, “Digital Automation of Transdermal Drug Delivery with High Spatiotemporal Resolution,” was co-authored by Yihang Wang of the Department of Applied Physical Sciences and Zeka Chen of the Department of Pharmacology. Bai said the research highlights not only a multidisciplinary collaboration but also a “passionate involvement of Carolina undergraduate students,” including Priyash Hafiz of the Department of Applied Physical Sciences, and Brayden Davis, Will Lipman, Tian Wang and Sicheng Xing of the UNC/NCSU Joint Department of Biomedical Engineering.
The patch, which has received a provisional patent, enables highly localized treatment – less than 1 square millimeter – of specific tissues, organs or regions within the body, and drug release can be triggered within 30 seconds in response to an electrical signal. Patients could wear more than one patch at a time which would reduce the need for doctors’ visits, or even trips to the hospital, for medical attention.
“The beauty of this device is that it can house dozens, if not hundreds, of concentrated drugs and can program their sequential release automatically,” said Song, who is a member of the UNC Neuroscience Center. “Rapid drug release can be crucial in emergency situations or when immediate therapeutic action is required.”
The microneedles are coated with gold, which protects the drugs and surrounding tissues. When a low-voltage electrical stimulus is applied through the patch, the gold coating disintegrates, exposing the drug-loaded microneedles to the skin and initiating the controlled release of the drugs.
“This level of specificity ensures precise and customized drug delivery, catering to the needs of different conditions or specific regions of the body,” said Wang. “This offers a novel approach to achieving controlled drug release through a combination of materials science and electrical engineering.”
The National Science Foundation and the National Institutes of Health funded this research.
David DeFusco, communications specialist at the UNC Department of Applied Physical Sciences, wrote the original news announcement. The UNC School of Medicine contact is Mark Derewicz, director of research and national news for UNC Health.
2024 Health of US Primary Care Scorecard Webinar is Wednesday
Primary care is the foundation of our health care system. Yet more and more people report not having a regular place for care. In the forthcoming second annual Primary Care Scorecard, Robert Graham Center researchers give five reasons why access to primary care is worsening.
Join the Milbank Memorial Fund and The Physicians Foundation on February 28, at 12 p.m. ET, for a webinar on how the nation and the states are performing on primary care workforce, financing, training and research funding measures — and how challenges within each of these areas contribute to poor access to primary care.
The Physicians Foundation's President, Gary Price, MD, will give opening remarks ahead of a panel discussion moderated by Frances Stead Sellers of The Washington Post. The panel will include:
· Rachel Block, Program Officer, Milbank Memorial Fund
· Margaret Flinter, APRN, PhD, Vice President and Clinical Director, Community Health Centers, Inc.
· Yalda Jabbarpour, MD, Director, The Robert Graham Center
· Kyu Rhee, MD, President and CEO, National Association of Community Health Centers
REGISTER NOW
About The Physicians Foundation
The Physicians Foundation is a nonprofit seeking to advance the work of practicing physicians and help them facilitate the delivery of high-quality health care to patients. As the U.S. health care system continues to evolve, The Physicians Foundation is steadfast in strengthening the physician-patient relationship, supporting medical practices’ sustainability and helping physicians navigate the changing health care system. The Physicians Foundation pursues its mission through research, education and innovative grant making that improves physician wellbeing, strengthens physician leadership, addresses drivers of health and lifts physician perspectives. For more information, visit www.physiciansfoundation.org
Want To Go To Medical School for Free? Here Is A Billion Ways It Is Now Possible

Albert Einstein College of Medicine to offer free tuition after billion-dollar gift
Dr. Ruth Gottesman, 93, who spent 55 years as the chair of the school’s board, made the historic donation in the name of her late husband, David “Sandy” Gottesman, who was an early investor of Berkshire Hathaway and a longtime friend of Berkshire’s famed CEO Warren Buffett.
Philip Ozuah, president and CEO of Montefiore Medicine, the school’s parent company, announced the “transformational gift” on Monday, saying that “this is the largest donation to any medical school in the country.”
Sandy Gottesman, who was the co-founder of New York-based investment firm First Manhattan Co., died in 2022.
The Gottesmans had long been involved in health care philanthropy. In 2010, their gift of $25 million to the Albert Einstein College of Medicine went towards creating the school’s Institute for Stem Cell Research and Regenerative Medicine. Sandy Gottesman also served on the board of New York’s Mount Sinai Hospital.
“I am very thankful to my late husband, Sandy, for leaving these funds in my care, and l feel blessed to be given the great privilege of making this gift to such a worthy cause,” said Dr. Ruth Gottesman in a news release.

Dr. Ruth Gottesman joined the medical school in 1968 and developed screening, evaluation and treatments for children with learning disabilities. In 1992, she founded the Adult Literacy Program at Einstein’s Children’s Evaluation and Rehabilitation Center, “the first of its kind.” She also served as the founding director of the school’s Emily Fisher Landau Center for the Treatment of Learning Disabilities, which opened in 1997.
Few educational donations rival the magnitude of Dr. Ruth Gottesman’s. In 2018, former New York mayor Michael Bloomberg donated $1.8 billion to his alma mater, Johns Hopkins University. And New York hospitals have long drawn the philanthropy of billionaires, with individual donations sometimes amounting to more than $100 million. Home Depot co-founder Ken Langone has heavily invested in New York University’s medical centers. In 2018, in part due to Langone’s donations, NYU’s School of Medicine became the first medical school in the country to offer free tuition to accepted students.
An October survey from the Association of American Medical Colleges found that 70% of medical students who graduated in 2023 have taken on some level of education debt. The average graduate left medical school owing more than $200,000, according to the AAMC.
“This donation radically revolutionizes our ability to continue attracting students who are committed to our mission, not just those who can afford it,” said Dr. Yaron Tomer, the dean at Albert Einstein. “We will be reminded of the legacy this historic gift represents each spring as we send another diverse class of physicians out across the Bronx and around the world to provide compassionate care and transform their communities.”