NCMS CPP Elevates Healthcare in Dare County and Neighboring Counties Through New Preceptor Hub

NCMS Preceptor Hub is partnership with Manteo Community Health Center in Manteo, Engelhard, and Ocracoke (photo: The Coastland Times)
Improved Healthcare Coming to Dare County
The North Carolina Medical Society (NCMS) in conjunction with the Town of Manteo Healthcare Task Force is happy to announce the formation of a Preceptor Hub in Dare County. Initially, the Hub will be a partnership between the Manteo Community Health Center in Manteo, Engelhard, and Ocracoke, the town of Manteo, and the NCMS. Additional medical practices with preceptors will be added in the future. UNC-Chapel Hill, Campbell University, Elon University, and Wake Forest University will send students to the Hub.
A Preceptor Hub is a community of experienced medical practitioners who supervise medical students, providing training and clinical education. They provide the experiential part of the curriculum by helping student physicians gain clinical medical knowledge by caring for real patients.
The Preceptor Hub in Dare County comes after Outer Banks Medical Group told more than 2,400 patients that it would no longer provide services due to practitioner retirements, resignations or temporary providers not renewing their contracts.
NCMS Vice President Franklin Walker has been instrumental in the formation of the hub, working for more than two years to bring help to the people of Dare County.
Walker says, “The North Carolina Medical Society takes its commitment to the health of North Carolinians very seriously. This Preceptor Hub is a chance for us to bring our expertise and experience to a part of the state that needs quality healthcare. Through our Community Practitioner Program (CPP), we place physicians and PAs in underserved areas and improve access to care. We are very excited to help the people of Dare County.”

NCMS CEO Chip Baggett is also excited about what NCMS is doing for the area. "For over two years, Franklin Walker and the CPP team have dedicated their efforts to enhancing healthcare in Dare and its neighboring counties. The establishment of this Preceptor Hub reflects the commitment of NCMS to always lead toward improved healthcare for North Carolinians. We take pride in our robust partnerships with Manteo Community Health Center and the Town of Manteo Healthcare Task Force. We are also excitedly anticipating the arrival of students from UNC-Chapel Hill, Campbell University, Elon, and Wake Forest, the NCMS to see their contributions to assist the residents of this region."

Joe Rockenstein, CEO of Manteo Community Health Center adds, “We must preserve the future of healthcare by embracing the precepting of the present. With this program, we hope to do that for all the communities we serve in eastern North Carolina.”
Town of Manteo Healthcare Task Force Chairman Malcolm Fearing stated, “Nearly two years ago, our community was in a state of crisis because we had thousands of community members who lost their access to healthcare. We cast a wide net looking for resources to assist our community. Mr. Walker and the North Carolina Medical Society Foundation have been alongside us in the trenches helping to find sustainable solutions to build our provider network for patient care. This preceptorship program will allow students to hone their skills here on the Outer Banks. We are confident that we will prove to them that we all know this is an amazing place to live, work, and raise a family. We are tremendously grateful to have this kind of program coming to Dare County.”
NCMS Community Practitioner Program is helping underserved communities across the state. If you have questions about a Preceptor Hub in your area, please contact Franklin Walker at [email protected].
Some photos from today's meeting:
NCMS Past President Dr. Arthur Apolinario Featured in AMA Medicare Ad as AMA Advocacy Conference Begins
Dr. Arthur Apolinario Joins AMA Campaign to Fix Medicare
 Former North Carolina Medical Society President Dr. Arthur Apolinario adds his voice to the fight to fix the Medicare payment system in a new ad.
Former North Carolina Medical Society President Dr. Arthur Apolinario adds his voice to the fight to fix the Medicare payment system in a new ad.
In the advertisement currently running on social media, Apolinario says, "You have all the physicians of the United States speaking as one voice and making sure the message gets heard."
The American Medical Association National Advocacy Conference is currently underway in Washington, DC. One of the top agenda items is pushing Congress to pass legislation to reverse the 3.37 percent Medicare physician payment cuts that took effect on January 1, 2024. The AMA says failure to reverse the cuts will be harmful to the continued viability of physician practices and their ability to care for patients.
The NCMS currently has several members at the conference including NCMS Vice President of External Affairs Alan Skipper, NCMS President Dr. Eileen Raynor, NCMS Board of Directors member Dr. Karen Smith, and NCMS AMA Delegate Dr. Mary Ann Contogiannis.
To see Dr. Apolinario's ad click here.
Here is the list of the North Carolina Medical Society AMA Delegates:
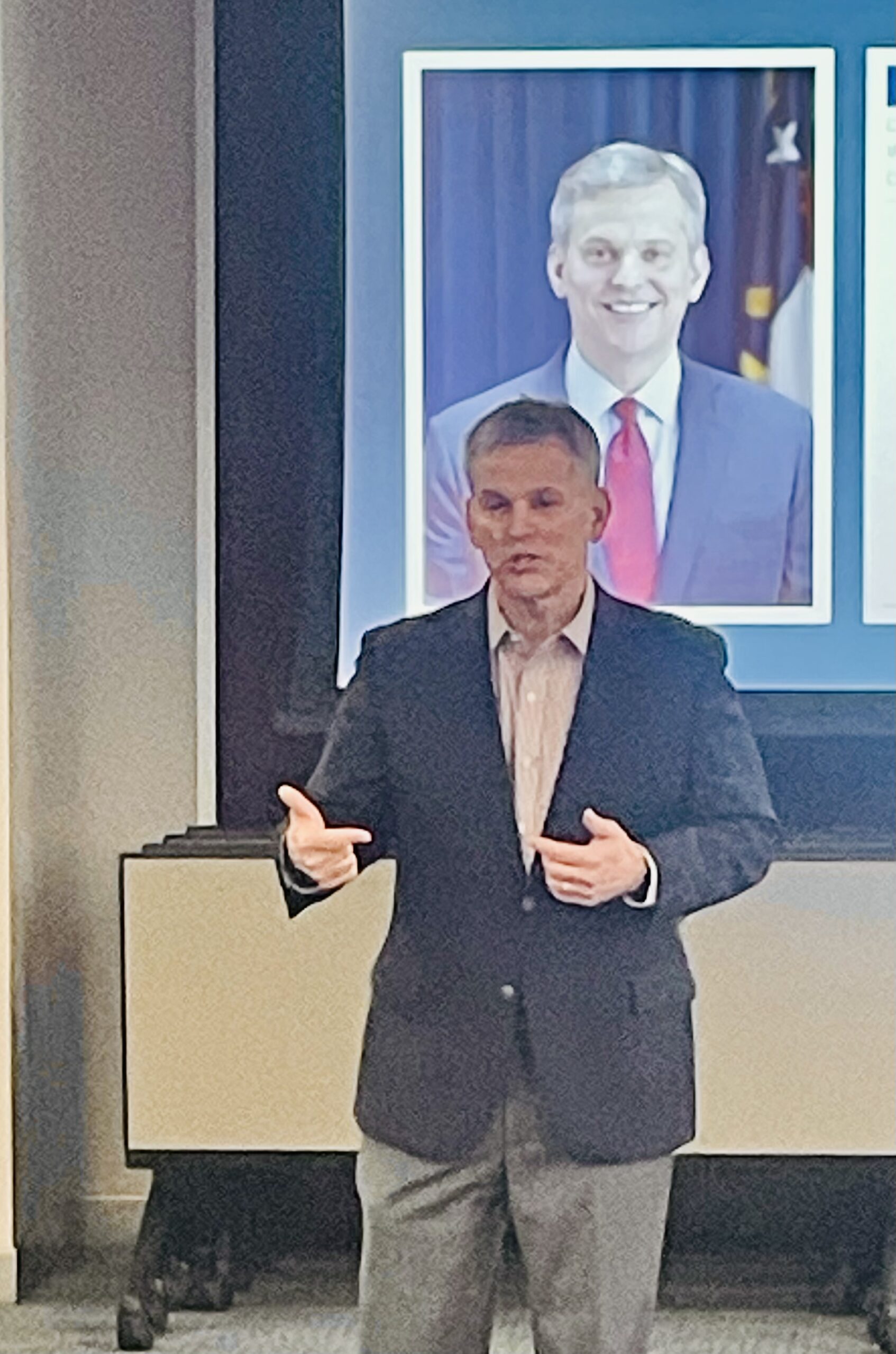
NCMS CEO Chip Baggett Gives Advocacy Update to NC Chapter of American College of Physicians

Chip Baggett Addresses American College of Physicians
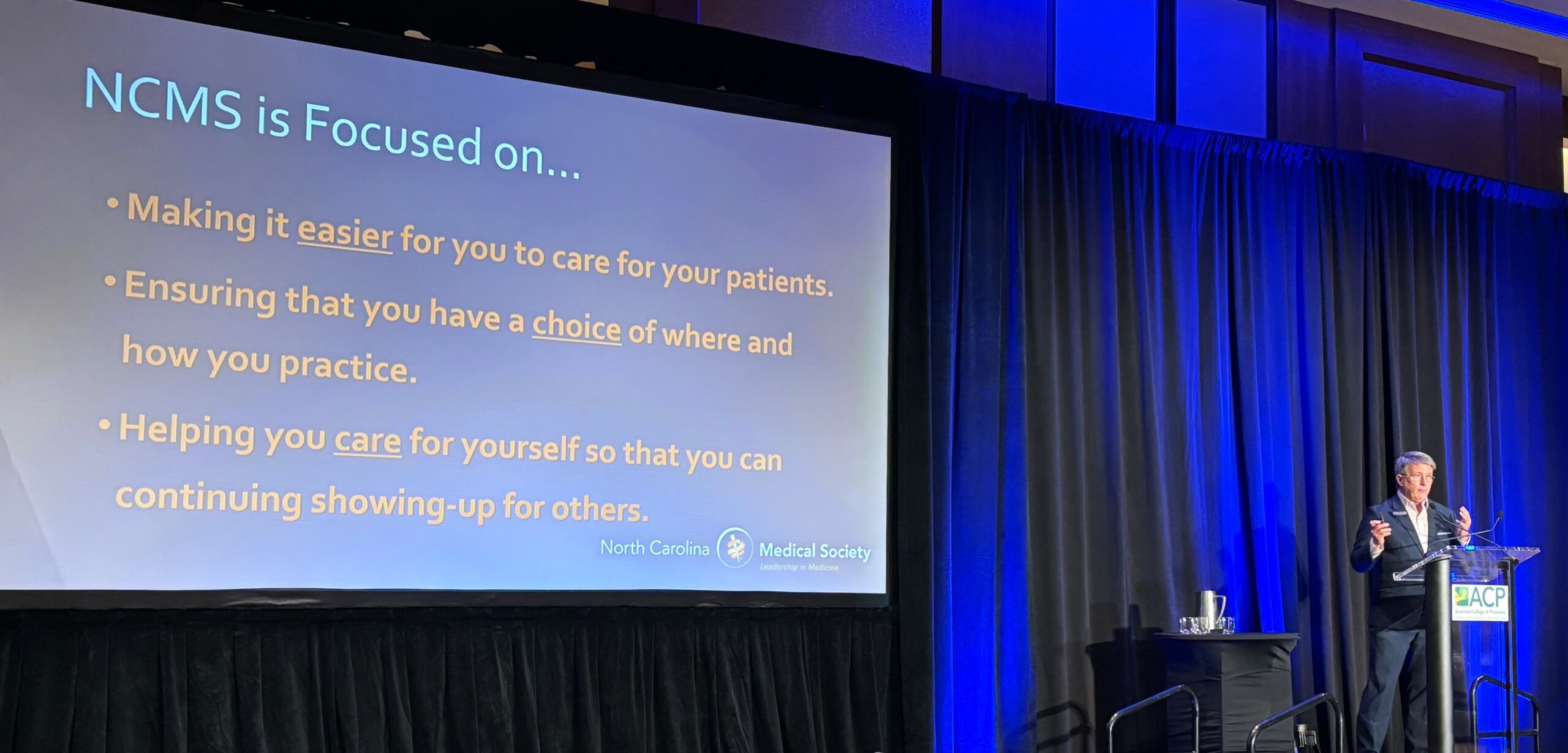
RALEIGH -- The North Carolina Medical Society CEO Chip Baggett addressed the North Carolina Chapter of the American College of Physicians (ACP) Friday in Raleigh. His advocacy update focused on making it easier for physicians to care for patients, making sure physicians have a choice of where and how to practice, and a strong commitment by NCMS to physician wellness.
Key initiatives of the NCMS
- Passage of Prior Authorization/Utilization Management reform legislation currently being considered by the North Carolina General Assembly and the United States Congress.
- Creation of a single, unified credentialing process recognized by government and commercial payers, hospitals, and licensing boards.
- Advocacy for streamlined licensure and renewal process at the North Carolina Medical Board that includes renewal every two years instead of annually.
- Obtaining a Medicaid and Medicare Physician Fee Schedule rate update to adjust for inflation.
- Recruitment of a minimum of 40 new physicians, PAs, and other healthcare team members through the NCMS Community Practitioner Program.
- A Task Force on practice employment issues and structural improvements.
- Improve daily lives of NCMS members through the North Carolina Clinician and Physician Retention and Wellbeing Consortium.
- Recruit 16 practice partnerships to send participants to the NCMS Kanof Institute for Physician Leadership for next 5 years.
- Identify sustainable funding for NCMS Future Clinician Leaders College.
Other highlights of the event include MOC credits, the Residents and Students Poster Competition, special interest roundtables, and the presentation of the 2024 Laureate and Volunteerism Awards.
The ACP event also included NCMS members Marion M. McCrary, MD, FACP and Lawrence Greenblatt, MD, FACP.
Here is the full list of speakers:
- Noel Ivey, MD, FACP
- Michelle E. Perkons, MD
- Denise Pong, MD, MPH
- Former NCMS BOD Member Fatima Syed, MD, MSc, FACP
- Diana B. McNeill, MD, MACP
- J. Bryan Sexton, PhD
- John V. Duronville, MD
- Rebecca Lumsden, MD MS
- Kevin L. Thomas, MD
- Bruce T. Peyser, MD
- Liza I. Genao, MD
- Aatif M. Husain, MD
- Mehri S. McKellar, MD
- Mithu Maheswaranathan, MD
- NCMS PAC Investor Suchita Shah Sata, MD, FACP, SFHM
- David P. Boyte, MD, MBA
- Ruchi S. Doshi, MD, MPH
- Katherine N. Neal, MD
- Bruce T. Peyser, MD, FACP
- Poonam Sharma, MD, SFHM
- Girish Kalra, MD
- Christopher D. Fink, DO
- Neha Kayastha, MD
- William S. Yancy, Jr., MD, MHS
- Christopher A. Jones, MD, FAAHPM, MBA
Chief Resident Presentations:
- Kathryn M. Langley, MD (UNC)
- Alyssa MacKay, DO (Atrium Health)
- Elaina K. Furr, DO (MAHEC)
- Vasili Katsadouros, DO (Cone)
- Joshua Walters, MD (ECU)
- Ashley Bird-Humrickhouse, DO (NHRMC)
- Nathan A. Hirshman, MD (Duke)
- Zachary Pruitt, MD (WFU)
- Randall Reagan, DO (UNC Blue Ridge)


CDC: Syphilis cases at highest levels since 1950s
Racial and Ethnic Minorities Disproportionately Affected
The number of syphilis cases in the U.S. are on the rise. According to a new report from the Centers for Disease Control and Prevention, cases increased by nearly 80% to more than 207,000 between 2018 and 2022.
Rates increased among all age groups, including newborns, and in all regions of the country. In 2022, 3,755 cases of babies born with syphilis in the U.S. were reported, which reflects an alarming 937% increase in the past decade, the CDC said.
The report continued that racial and ethnic minorities are most disproportionately affected due to "long standing social inequities that often lead to health inequalities."
Experts point to various reasons for the increase, including increases in substance abuse tied to risky sexual behavior, decrease in condom use, ongoing social and economic conditions and reduction in sexually transmitted infections (STI) services at the state and local level.
"Because STIs often do not show symptoms, and screening is necessary for timely diagnosis and treatment, changes in access to sexual health care can affect the number of infections diagnosed and reported," the CDC said.
The stigma surrounding STIs can also keep people from seeking care, and "buries the truth that all people deserve quality sexual health care," said Laura Bachmann, acting director of the CDC's Division of STD Prevention, in an interview with NPR. "It also can cause issues at the provider level when it comes to talking with people about these issues."
The CDC said that its findings signal an urgent need for a closer look at public health efforts and prevention strategies.
"Some people face tremendous barriers to STI prevention and health services," said Bachmann in a statement. "So, the most important work is often outside the clinic, whether it be reaching out to communities with testing, interviewing patients to offer services to their partners, or delivering treatment directly to someone."
She added that there is still a need for more innovation around diagnosis, treatment and prevention.
"In the United States, syphilis was close to elimination in the 1990s, so we know it's possible to reverse this epidemic," said Jonathan Mermin, director of CDC's National Center for HIV, Viral Hepatitis, STD, and TB Prevention, in a statement. "I have hope for innovative prevention tools – such as a pill after sex that prevents STIs, and better tests for syphilis – but they will only be successful if they reach the people who will benefit. And that is going to require coordinated and sustained efforts at the federal, state, and local levels."
The U.S Department of Health and Human Services is also continuing to address the issue through the establishment of a federal task force last year.
"Addressing the resurgence of syphilis and congenital syphilis requires a concerted effort," said Admiral Rachel Levine, assistant secretary for health and chair of the National Syphilis and Congenital Syphilis Syndemic Federal Task Force, in a statement. "We can collectively work towards reducing the incidence of syphilis and its devastating consequences, and we will turn the tide on the syphilis epidemic."
Without the appropriate funding however, it's difficult for communities to follow through with the recommendations by government officials, said Elizabeth Finley, director of communications at the National Coalition of STD Directors.
Over the past year, there has been a shortage of Bicillin, an antibiotic used to treat syphilis. In addition, last year states lost funding for STD prevention, affecting their ability to respond to syphilis.
"The 2022 data is devastating to see, but it's already a year old," said Finley. As a result, she said that "we have every reason to believe that the 2023 numbers will be much worse."
The CDC report also included data on other sexually transmitted infections, stating that "reported gonorrhea cases declined for the first time in at least a decade while reported chlamydia cases were level."
There were more than 2.5 million cases of syphilis, gonorrhea, and chlamydia reported in the U.S. in 2022 alone.
Without treatment, syphilis can cause serious health problems including damage to the heart and brain, and can cause blindness, deafness and paralysis. If transmitted during pregnancy, it can cause miscarriage, infant death and lifelong medical issues. With the right antibiotics, the STI is curable.
Additional Reading:
Syphilis Among Newborns Continues to Rise
Does Morning After Pill for STI Work?
Old Drug Offers New Stop for STI
The Most Important Part of Super Bowl LVIII? The Commercials! Here Are All The Ones Already Released
Super Bowl LVIII will air on CBS this year, and stream live on Paramount+
Yes, we are all excited to see the San Francisco 49ers and the Kansas City Chiefs on Sunday. Yes, we are all excited to see Usher perform the halftime show, Yes, we are all wondering if Taylor Swift will be there. But, really aren't we all just watching for the ads?
Well, the NCMS is here to help! Here is a look at all of the 2024 Super Bowl commercials released so far!
2024 Super Bowl commercials (so far)!
Advertisers take the Super Bowl very seriously. They know around 1/3 of all Americans watch, and ads can go for millions of dollars. Because of that, advertisers often go all out, lining up celebrity-filled TV spots designed to raise interest in their products.
Paramount Plus Super Bowl commercial
What do Miami Dolphins quarterback Tua Tagovailoa, Patrick Stewart, Drew Barrymore, Arnold from "Hey Arnold" and Peppa Pig all have in common? They're all in the Paramount streaming service's new Super Bowl ad.
In the TV spot, the assorted characters are trapped on an icy glacier, unable to throw a rope to safety. When Tagovailoa says he could make the throw to the top, if there was a football.
Patrick Stewart suggests they use Arnold's football-shaped head to throw the rope all the way.
"We throw the child," the legendary actor plainly states. Despite reservations from some of his fellow stranded explorers, Stewart gets into some old-timey football gear and throws a perfect spiral — straight into the wall...as Creed sings "Higher."
Lamenting his inability to throw just a few feet higher, Stewart out wishes for some "pigskin" to toss. The commercial ends with a pan to Peppa Pig, potentially their last hope to avoid freezing to death.
While a condensed version is likely to be played at the Super Bowl because even a 30-second ad can cost millions of dollars, the full commercial clocks in just under two minutes.
Google's Super Bowl LVIII ad
Google's heartstring-pulling ad follows a blind man as he uses “Guided Frame” — Google's AI-powered accessibility feature for the Pixel camera that uses a combination of audio cues, high-contrast animations and tactile vibrations — to take pictures of the people and places in his life.
M&M Super Bowl commercial with several NFL greats
Retired Miami Dolphins quarterback Dan Marino, Buffalo Bills’ Bruce Smith and wide receiver Terrell Owens never got a Super Bowl ring, but M&M’s and Scarlett Johansson present the “Almost Champions” ring to the almost winners.
“Almost Champions” ring to the almost winners.


OREO Super Bowl ad with Kris Jenner
In OREO's 30-second Super Bowl spot, the iconic chocolate sandwich cookie is imagined at big events throughout the past, helping people make important decisions that altered the course of history.
In ancient Troy, two guards decide to "twist on it" when a man shows up at their gate with the trojan horse -- cream on the right, they let him in. Whoops! We all know how that one turned out. An OREO also helps two UFO witnesses decide not to report their alien sighting.


Then in a flashback scene to pre-"Keeping Up with the Kardashians" days, Kris Jenner, matriarch of the Kardashian empire and long-time OREO fan, is on the phone.
"So every little detail about our family will be on TV?" she asks. "Who would watch that?"
Jenner says she'll "twist on it" to decide, and pulls the cookie apart, and appears to decide to go for it. "Hope you can keep up," she says.
Booking.com Super Bowl ad with Tina Fey
Actress Tina Fey has so many choices on the online travel agency booking.com site she has to hire body doubles: an influencer type played by her 30 Rock co-star, Jane Krakowski, to stay at a fancy hotel, a bigfoot handled by another 30 Rock co-star, Jack McBrayer, to stay at a cabin, and even actress Glenn Close, who stays on a farm.
Doritos Super Bowl ad with Jenna Ortega
Two grandmotherly women ("Dina" and “Mita”) chase after “Top Gun: Maverick” actor Danny Ramirez, who took the last bag of Doritos Dinamita from a store shelf, leaving actress Jenna Ortega behind.


Mountain Dew Baja Blast Super Bowl commercial with Aubrey Plaza
Aubrey Plaza is always having a blast, whether she is stuck in an elevator or being abducted by aliens — or reuniting with her “Parks and Rec” co-star Nick Offerman while riding dragons.


Starry Super Bowl commercial with Ice Spice


"I just needed something more refreshing, more crisp," she says. After the rejection, the spurned soda/lover's head explodes in a fountain of clear soda.
Pringles Super Bowl commercial with Chris Pratt
The Pringles ad features Chris Pratt sporting the chip mascot's iconic mustache. Once a cashier notices and posts about the 'stache, the race is on, with more people commenting about his striking resemblance to the Pringles man.


By the end of the spot, Pratt has starred in a movie about the Pringles mascot, alongside a mustachioed child in a wagon on the prairie. It ends with the same clerk from the beginning of the clip asking "do I get a cut?" Pratt then offers her a tube of Pringles.
Dove Super Bowl LVIII commercial
Dove's ad begins seemingly whimsically showing young girls having mishaps playing sports to the tune of "It’s the Hard Knock Life."


But the ad cuts starkly to a girl looking self-consciously in the mirror. The message: low body-confidence leads to girls quitting sports, not the mishaps.
Budweiser 2024 Super Bowl ad
In Anheuser-Busch's nostalgic spot, a snowstorm threatens to derail a delivery of Budweiser to a small-town bar. But a team of Clydesdales and a Labrador retriever team up to help Budweiser make the delivery.


Experts say the feel-good spot strikes the right chord for Anheuser-Busch, which is trying to win back consumer sentiment following last year’s conservative backlash against Bud Light after the brand sent a commemorative can to transgender influencer Dylan Mulvaney. Bud Light also angered supporters of transgender rights who felt it abandoned Mulvaney.
Bud Light Super Bowl commercial with Post Malone
Speaking of Bud Light, they've also released their Super Bowl ad, aiming for some low-stakes chuckles with their commercial. In the newly-released spot, dubbed "Easy Night Out," a group of friends is hanging out in a garage. As one cracks open a Bud Light from the refrigerator, he unleashes the Bud Light Genie.


"Wishes? Yeah, it's my thing," the Bud Light Genie says. Want to be filthy rich? No problem! Need a sweet new set of wheels? How about a stretch DeLorean limo ride to the bar, where Bud Light magically replenishes itself at the tables. As the night gets crazier and the genie keeps granting wishes, NFL Hall of Famer Peyton Manning, Grammy nominee Post Malone and UFC CEO Dana White all make appearances.
T-Mobile Super Bowl spot with Jason Momoa
Jason Momoa shows off his singing chops in an ad that shows Scrubs duo Zach Braff and Donald Faison singing about T-Mobile home internet to the tune of “Flashdance ... What a Feeling." “Flashdance” star Jennifer Beals pops in to spray Momoa with water and ask him to sing it again — without his shirt.
Michelob ULTRA Super Bowl ad stars Lionel Messi and Ted Lasso star Jason Sudeikis
The Michelob commercial this year is pretty simple. While waiting for a beer at a beachside bar, Lionel Messi takes some time to have some fun with a soccer ball — namely dribbling circles around everybody else on the beach. It also features a brief cameo from "Ted Lasso" star Jason Sudeikis, who comments how the two of them "go way back."


At the end of the relaxingly low-key commercial, the bartender calls for the soccer icon to pick up his drink, and Messi kicks a goal into a volleyball net hanging between a pair of palm trees.
Hellmann's Super Bowl commercial
And a Hellmann's ad focusing on food waste starring Kate McKinnon features a cat that becomes a celebrity and dates Pete Davidson.


In the ad, McKinnon mistakes the cat's meow for the word "mayo," catapulting the "talking" cat to fame with a book deal, keynote speech and eventual red carpet moment with the former SNL cast member.
Kawasaki
A Kawasaki ad shows people riding in their Ridge “side by side” off-road vehicles growing mullets because the vehicle is “business in the front and a party in the back.”
The vehicle's ability to grow 80s hairstyles extends past the occupants, with a bald eagle and a tortoise also growing some luscious locks.
Uber Eats Super Bowl commercial with Jennifer Anniston, David Schwimmer, and David and Victoria Beckham
The ad for Uber Eats is all about being forgetful. From forgetting to put on pants in the morning to forgetting an old Friend, we all lose track of some things.
But the commercial, as it goes through the various forgetful scenarios, reminds watchers to always remember one thing: Uber Eats, because the delivery app has more than just food. You can get office supplies, flowers or beauty products through the app.
And isn't that worth forgetting something else to make room for?
DoorDash
The food delivery app's commercial is simple: they're offering to deliver everything (and yes, we mean everything) being advertised by the other ads during the big game, for free, to one lucky person.
In a teaser, DoorDash says they'll give out a promo code during their game-day ad, which can be redeemed here for a shot to win.
That means everything from Doritos to a new car to tax services. In fact, DoorDash doesn't know everything they're giving away for this promotion. "Who knows what else? We haven't fully thought this thing through," the teaser's narrator says.
Popeyes
Popeyes new it had to go big or go home for its first Super Bowl commercial.
The chicken chain's commercial, released on Feb. 6, features comedian and actor Ken Jeong trying Popeyes' new wings.
In the 60-second ad, Jeong is seen thawing out after he cryogenically froze himself in 1972. Jeong's character waited over 50 years for the "better" wing to be created.
Along with trying an array of Popeyes wings, Jeong goes on a venture to try all the things of the modern age: delivery drones, electric scooters, self-driving cars, robot vacuums and even goldendoodles.
Dunkin' Donuts
Ben Affleck and Dunkin' Donuts are a match made in heaven.
Affleck, who is the official brand ambassador for the coffee chain, returns for another Super Bowl ad this year.
In the minute-long teaser, Affleck is seen watching a news segment calling him the "boredest man in the world" as he sits beside his wife Jennifer Lopez.
The ad cuts to Affleck as he pursues his new dream of becoming a pop star. He's heading into studios, talking to producers and employing the help of TikTok star Charlie D'Amelio for some dance lessons.
Affleck is even seen pitching his "crazy" dream to JLO over the phone.
Latest Trends in Health Technology from 2024 Consumer Electronics Show
Healthcare’s Transformative Technologies at CES 2024
(Caroline Scott, Consumer Technology Association Contributing Editor) -- In recent years, and as was seen at CES 2024, the healthcare industry has benefited from a significant transformation furthered by the integration of digital technologies. The advent of digital technologies across the healthcare landscape has revolutionized the way we approach wellness, making
therapies and a wide range of other services more accessible, personalized and efficient. Promoting these advances, CTA continues to play a catalyzing role in helping industry players shape the future of healthcare through innovation and collaboration. Here’s a closer look at how CTA with CES – the world’s most powerful technology show owned and operated by CTA – have helped foster innovation in the interest of improved wellness and healthcare innovators across the U.S.
Digital Technologies and the Future of Healthcare
The digital health sector employs a wide range of technologies and applications designed to enhance healthcare delivery, improve patient outcomes and streamline medical processes. One of the key advantages of digital health is its ability to empower individuals to take control of their health and well-being. From wearable devices that monitor vital signs to mobile apps that provide real-time health insights, digital health technologies enable individuals to track and manage their health proactively.
Furthermore, digital health can break down traditional barriers to healthcare access. Telehealth, for example, allows individuals to consult with healthcare professionals remotely, eliminating geographical constraints and providing timely medical advice. This is particularly crucial in rural and underserved areas where access to healthcare services may be limited.
And for women, digital health tech is particularly promising as a leveler of imbalances in access to quality care. According to CTA’s most recent study, The Future of Women's Digital Health Solutions, two-thirds (66%) of U.S. women state that digital health solutions are the future of healthcare. Some 64% agree that digital health will aid in lowering healthcare cost. More than half (58%) say digital health solutions will reduce healthcare disparities. Our article, Assessing & Addressing the State of Women’s Healthcare, further explores underrepresentation and underfunding of research in healthcare for women. These are among the challenges digital health tech is countering, as was evidenced across the show floor. A rundown of this and other topics in digital health conference programming at CES 2024 is available on demand.
Healthcare Goes Where You Do with Digital Tech
Wearable medical devices extend beyond basic fitness tracking, offering features like continuous glucose monitoring, ECG monitoring and stress management. CES showcased innovative telehealth solutions designed to enhance the virtual healthcare experience. From immersive virtual reality consultations to remote patient monitoring, telehealth technologies are evolving to provide more comprehensive and engaging healthcare services.
The integration of digital therapeutics, increasingly in wearable and mobile formats, gained prominence at CES with the addition of apps and platforms that deliver evidence-based interventions for various medical conditions. These digital therapeutics aim to complement traditional treatments and improve patient outcomes.
CES 2024 featured breakthroughs in wearable and mobile health tech, and scores of startup products and services for improved wellbeing. The show also reprised the popular Digital Health Summit. Panel topics included health equity, innovations in mental health, women’s healthcare, generative AI and much more.
The Healthcare Network Effect at CES 2024
After a great success at CES 2023, the Digital Health Mixer returned in full force at CES 2024. The informal networking event brought diverse digital-health innovators together to exchange insights and ideas.
In 2023, the Digital Health Mixer attracted nearly 350 attendees. In 2024, the event drew more than 500 attendees. The networking at this venue has consistently fostered important collaborations among healthcare visionaries. It also has proved invaluable for facilitating seamless exchanges of critical information. These connections help continue the conversation long after the show’s close, year after year.
As we navigate the digital age, the importance of digital health tech cannot be overstated. The transformative impact of these technologies, coupled with the advocacy and support of innovative organizations and experts that align with CTA, is paving the way for a more connected, patient-centric healthcare landscape. CES 2024 served as a testament to the power and promise of digital health, offering a glimpse into a healthcare future that’s both technologically advanced and more completely human-centered.
It's not too soon to save the date for CES 2025, January 7-10, in Las Vegas. In the meantime, explore how CTA’s digital health team is working for business innovation and sample extensive on-demand content relevant to this critical topic. Stay tuned for more updates as our work continues in the interest of progress in digital health tech.
Additional Reading:
CES 2024 Sector Trends: Digital Health
Healthcare Leaders Share Takeaways from CES
NCMS Past President Dr. Philip Brown to Present at CARE Project Professional Collaborative
'Do You Speak Patient: TELL ME' by Dr. Philip Brown at CARE Collaborative
(WRIGHTSVILLE BEACH) -- Dr. Philip Brown is speaking at the 6th Annual CARE Project NC Parent Professional Collaborative. Brown is a Past President of the North Carolina Medical Society, former Chief Physician Executive at New Hanover Regional Medical Center, and Chief Community Impact Officer at Novant Health.
The CARE Project Executive Director Dr. Johnnie Sexton, Au.D. says, "Dr. Brown’s ability to bring simplicity out of chaos to help lead organizations and individuals to accountable action is particularly needed in today’s environment. We are inundated with facts and data points that can be and are spun to obscure truth, creating clarity requires both quantitative and qualitative information. His transformational leadership is effective because he is willing to listen, hear and understand diverse perspectives through connection and earned trust.
Click here to attend.
Flu Activity Picking Up Across Country, Including North Carolina

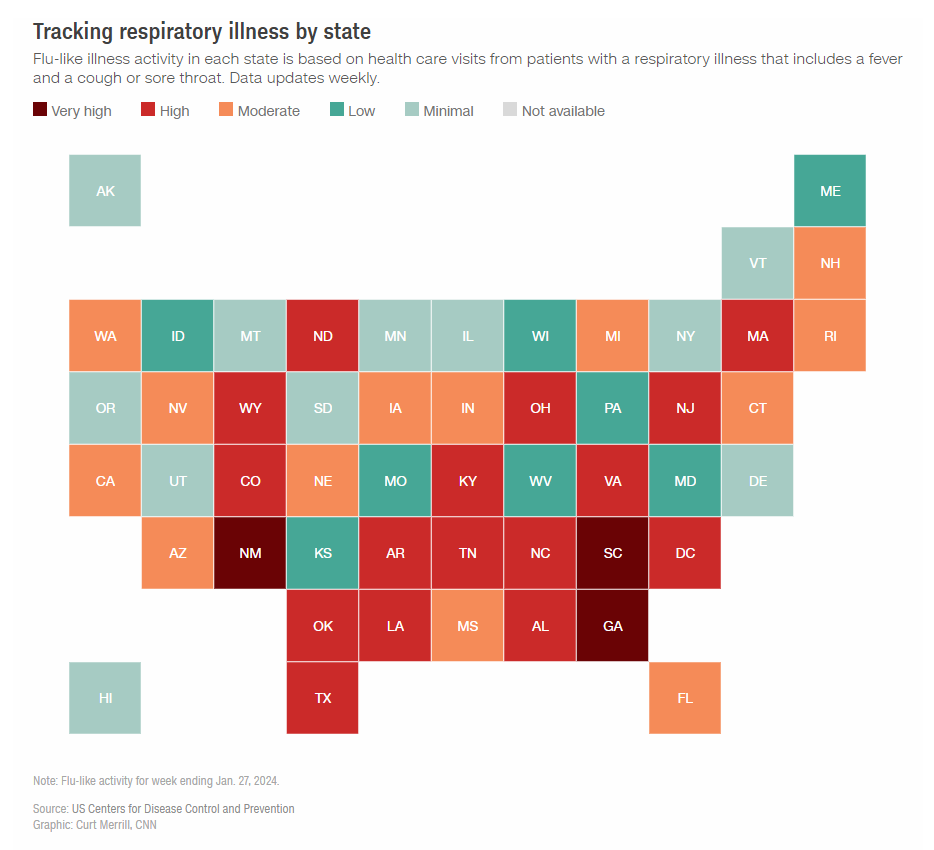
More than a third of all states are still experiencing high or very high levels of respiratory illness this season, according to the CDC.
Respiratory virus season in the US isn’t over yet
(CNN, Diedre McPhillips) -- After a few weeks of decline, some measures show that flu activity is starting to pick up again and respiratory virus levels remain high overall in the United States.
During the week ending January 27, more than 82,000 people who visited an emergency department were diagnosed with influenza, according to data from the US Centers for Disease Control and Prevention — an 8% bump, or about 6,000 more than the week before. The test positivity rate for flu also ticked up in the US overall.
A second surge of flu activity after the winter holidays is common, but experts say it’s notoriously difficult to predict exactly how long or how severe the full season will be. Sometimes this surge is the start of a full second wave, but it could also be a minor blip before a more consistent decrease, the CDC says.
A traditional second wave of influenza usually comes after a more significant downturn, when influenza B viruses start to overtake influenza A viruses that were predominantly circulating, said Alicia Budd, who leads domestic flu surveillance for the CDC.
There’s no evidence of that happening yet, but it’s too early to rule anything out, she said.
“We’re still at the midpoint of the season,” Budd said. “It’s too early to tell exactly where we are in our ultimate trajectory. We just don’t know yet. But we are still seeing a lot of activity right now.”
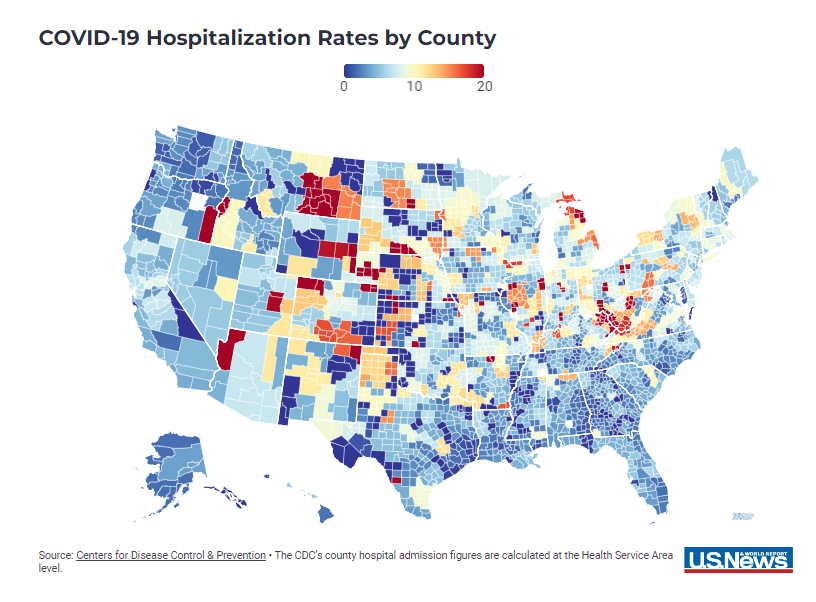
Covid-19 and RSV also continue to circulate at high levels. Emergency department visits for Covid-19 and RSV have been declining for a month, but there were still more than 50,000 emergency department visits and about 23,000 hospitalizations for Covid-19 during the week ending January 27, CDC data shows.
The downward trend for Covid-19 is coming as expected, and the peak for flu may be shifting a bit later this season, said Dr. Michael Mina, an epidemiologist and chief science officer of eMed, a telehealth company focused on at-home testing.
“It’s not so much that flu is now replacing Covid, it’s just like: Covid did its thing and now it’s coming down,” he said. “(Covid is) doing exactly the identical thing as it’s done, and in this case, we just have a flu season that shifted a little bit to the right. Flu shifts by orders of months actually from year to year. Covid is a little bit more consistent.”
While national trends are helpful, expert say that local trends are the best way to gauge risk and make decisions about how to stay safe and healthy.
Overall, 18 states and Washington, DC, are still experiencing high or very high levels of respiratory illness, according to the CDC. New data from the CDC’s Center for Forecasting Analytics suggests that flu infections are growing in four states — Florida, New York, Oklahoma and Texas — and likely growing in five others: Arkansas, Kentucky, Massachusetts, North Carolina and South Carolina. Wastewater surveillance suggests that Covid-19 levels are highest in the South, with forecasted case increases in South Carolina, in particular.
Experts say that trends in the US have stayed within expected ranges so far this respiratory virus season. But the burden of disease is still very high. The CDC estimates that there have been at least 20 million illnesses, 230,000 hospitalizations and 14,000 deaths from flu so far this season.
“It’s normal in terms of the amount of activity but it is a very, very high burden,” Budd said.
There is early data to suggest that the latest Covid-19 vaccine and this year’s flu shot offer strong protection this season, and experts say it’s still not too late to get vaccinated. They also urge the public to practice etiquette — hand washing, covering coughs and sneezes, staying home when sick — to avoid unnecessary spread.
“That’s how we can help each other,” Budd said.
NCMS Past President Dr. Palmer Edwards Appointed to NC Commission for Public Health

NCMS is Honored to Appoint Palmer Edwards, MD to the NC Commission for Public Health
(RALEIGH) -- The North Carolina Medical Society Nominating and Leadership Development Committee has appointed Dr. Palmer Edwards to the North Carolina Commission for Public Health. He fills the unexpired term of Douglas Sheets, MD. Edward's term will expire on November 30, 2027.
Edwards was born in Washington, NC and attended the University of North Carolina at Chapel Hill. He now lives in Winston-Salem with his wife Marty. Over the years, Edwards has served on various committees at the NCMS and been involved in the NCMS Foundation. He is currently a Foundation Trustee. He has been a member of the NCMS since 1992.
The Commission for Public Health is the public health rulemaking body for North Carolina. It is authorized and directed by the N.C. General Assembly to adopt rules to protect and promote the health of the public and to adopt rules necessary to implement public health programs administered by the Division of Public Health. The Commission was first established by the N.C. General Assembly in 1877 as the State Board of Health. It was renamed the Commission for Health Services in 1973 and became the Commission for Public Health in 2007. The Division of Public Health is staff to the Commission. The North Carolina General Assembly has invested the Commission for Public Health with statutory responsibilities to support the mission of the public health system, which is to promote and contribute to the highest level of health possible for the people of North Carolina.
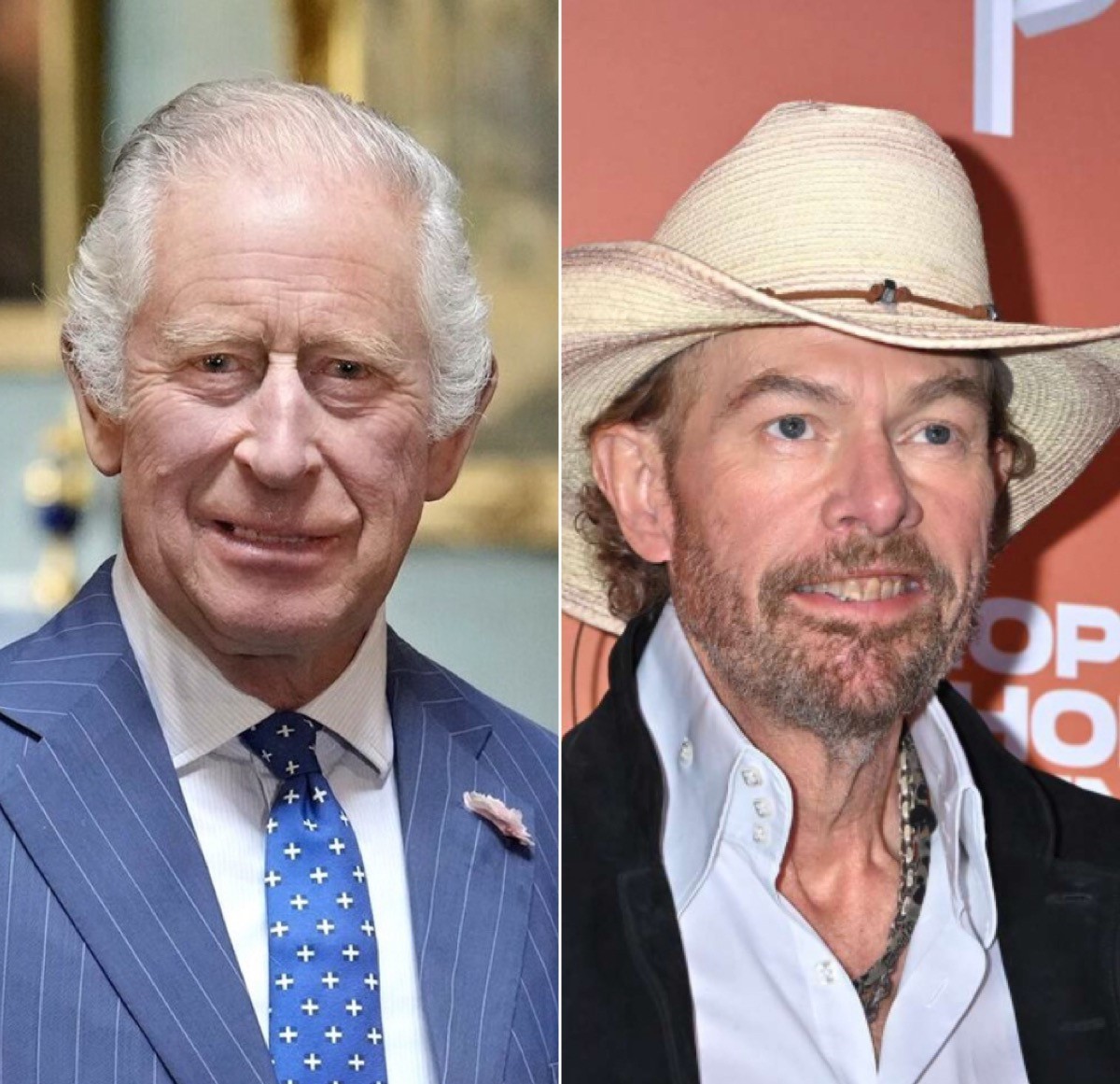
Toby Keith and King Charles Bring Attention to Cancer in Men
How to help your patients when they receive a cancer diagnosis
With the announcement of the death of country music superstar Toby Keith from Stomach Cancer and the cancer diagnosis of Britain's King Charles, the spotlight is shining brightly on men's health. Men are less likely than women to address their health. A recent study by the Cleveland Clinic found that only 3 out of 5 men get annual physicals and 40 percent of men ONLY go to the doctor when they think they have a serious medical condition.
Piedmont Healthcare found that men with a cancer diagnosis are likely to isolate themselves and suppress their emotions.
How men process cancer
Whether dealing with their own cancer diagnosis or that of a loved one, it is common for men to:
- Think asking for support is a sign of weakness. "Men are less likely to seek support because we think we will be perceived as weak," notes Buttimer. "Actually, the opposite is true. It takes a lot of strength to ask for help."
- Believe emotions are reserved for women. As caregivers, men may be tempted to ignore their emotions so they can support their loved one.
- Isolate themselves."When dealing with emotional issues or challenges that scare them, men tend to be loners," explains Buttimer. "It is an instinct for men to want to go into their 'man cave' to figure things out. In our culture, many men believe they are supposed to go it alone and tough it out during trying times, including cancer."
- Try to fix the problem."Men are 'supposed' to fix it, whatever it is," he says. "We pressure ourselves to figure out a solution and if we can't, we may believe something is wrong with us."
In response to the myriad of ways people cope with a cancer diagnosis, the Mayo Clinic released these tips for your patients:
Cancer diagnosis: 11 tips for coping
Learning that you have cancer can be hard. Some people say they felt anxious, afraid or overwhelmed when they were first diagnosed. If you aren't sure what to do to cope, here are 11 ideas to help you deal with a cancer diagnosis.
Get the facts about your cancer diagnosis
Try to get as much basic, useful information as you can. This will help you to make decisions about your care.
Write down your questions and concerns. Bring them with you when you see your health care provider.
You may ask:
- What kind of cancer do I have?
- Where is the cancer?
- Has it spread?
- Can my cancer be treated?
- What is the chance that my cancer can be cured?
- What other tests or procedures do I need?
- What are my treatment options?
- How will the treatment benefit me?
- What can I expect during treatment?
- What are the side effects of the treatment?
- When should I call my health care provider?
- What can I do to prevent my cancer from coming back?
- How likely are my children or other family members to get cancer?
- What happens if I don't get treatment?
Consider bringing a family member or friend with you to your first few appointments. They can help you remember what you hear.
Think about how much you want to know about your cancer. Some people want all the facts and details. This helps them be part of the decision-making process. Others want to learn the basics and leave details and decisions to their health care providers. Think about which works best for you. Let your health care team know what you'd like.
Keep the lines of communication open
Have honest, two-way communication with your loved ones, health care providers and others. You may feel alone if people try to protect you from bad news by not talking about it. Or you might feel alone or less supported if you try to look strong and not share your feelings. If you and others show your real emotions, you can help support each other.
Anticipate possible physical changes
The best time to plan for changes to your body is right after your cancer diagnosis and before you begin treatment. Prepare yourself now so that you'll be able to deal with everything later.
Ask your health care provider what may change. Medicines may make you lose your hair. Advice from experts about clothing, makeup, wigs and hairpieces may help you feel more comfortable and attractive. Insurance often helps pay for wigs and other devices to help you adapt.
Also think about how treatment will affect your daily life. Ask your provider whether you will be able to continue your usual routine. You may need to spend time in the hospital or have many medical appointments. If your treatment will make it hard to perform your daily duties, make arrangements for this.
Plan ahead for your finances. Figure out who will do routine household chores. If you have pets, ask someone to take care of them.
Maintain a healthy lifestyle
A healthy lifestyle can improve your energy level. Choose a healthy diet. Get enough rest. These tips will help you manage the stress and fatigue of the cancer and its treatment.
If you can, have a consistent daily routine. Make time each day for exercising, getting enough sleep and eating meals.
Let friends and family help you
Your friends and family can run errands, take you to appointments, prepare meals and help you with household chores. This can give those who care about you a way to help during a difficult time.
Also urge your family to accept help if it's needed. A cancer diagnosis affects the entire family. It also adds stress, especially to the ones who take care of you. Accepting help with meals or chores from neighbors or friends can help your loved ones from feeling burned out.
Review your goals and priorities
Figure out what's really important in your life. Find time for the activities that are most important to you and give you the most meaning. Check your calendar and cancel activities that don't meet your goals.
Try to be open with your loved ones. Share your thoughts and feelings with them. Cancer affects all of your relationships. Communication can help lower the anxiety and fear that cancer can cause.
Try to maintain your lifestyle
Keep your lifestyle, but be open to changing it. Take one day at a time. It's easy to forget to do this during stressful times. When the future is not sure, organizing and planning may suddenly seem like too much work.
Consider how your diagnosis will impact your finances
Many unexpected financial issues can happen after a cancer diagnosis. Your treatment may require time away from work or home. Consider the costs of medicines, medical devices, traveling for treatment and parking fees at the hospital.
Many clinics and hospitals keep lists of resources to help you financially during and after your cancer treatment. Talk with your health care team about your options.
Questions to ask include:
- Will I have to take time away from work? If I do, what will happen with my benefits?
- Will my friends and family need to take time away from work to be with me?
- Will my insurance pay for these treatments?
- Will my insurance cover the cost of medicines?
- How much will I have to pay?
- If insurance won't pay for my treatment, are there programs that can help?
- Do I qualify for disability benefits?
- How does my diagnosis affect my life insurance?
- Who do I call to talk about what my insurance will cover?
Talk to other people with cancer
It can be hard for people who have not had cancer to understand how you're feeling. It may help to talk to people who have been in your situation. Other cancer survivors can share their experiences. They can tell you what to expect during treatment.
Talk to a friend or family member who has had cancer. Or connect with other cancer survivors through support groups. Ask your health care provider about support groups in your area. You can contact your local chapter of the American Cancer Society. Online message boards also bring cancer survivors together. Start with the American Cancer Society's Cancer Survivors Network.
Fight stigmas
Some old stigmas about cancer still exist. Your friends may wonder if your cancer is contagious. Co-workers may doubt you're healthy enough to do your job. Some may avoid you because they're afraid to say the wrong thing. Many people will have questions and concerns.
Determine how you'll deal with others. In general, others will follow what you do. Remind friends that cancer shouldn't make them afraid to be around you.
Develop your own ways to deal with cancer
Just as each person's cancer treatment is different, so are the ways of dealing with cancer. Ideas to try:
- Practice ways to relax.
- Share your feelings honestly with family, friends, a spiritual adviser or a counselor.
- Keep a journal to help organize your thoughts.
- When faced with a difficult decision, list the pros and cons for each choice.
- Find a source of spiritual support.
- Set aside time to be alone.
- Remain involved with work and leisure activities as much as you can.
- Be ready to say no. This is the time to focus on you.
What helped you through rough times before your cancer diagnosis can help ease your worries now. This may include a close friend, religious leader or a favorite activity. Turn to these comforts now. Also be open to trying new ways to deal with your cancer.
Get Ready! North Carolina Will be Part of Solar Eclipse in April

Millions of Americans live in the path of 2024’s solar eclipse. See where to watch
(CNN, Matt Stiles, Kenneth Uzquiano, Ashley Strickland, and Will Mullery) -- One of the year’s most anticipated celestial events — a total solar eclipse — will put on a dramatic show April 8 as it crosses over Mexico, the United States and Canada.
A total solar eclipse occurs when the moon passes between Earth and the sun, completely blocking the sun’s face and causing the golden orb to temporarily disappear from view. The phenomenon has inspired myths and folklore for millennia.
The event will be visible to millions — including 32 million people in the US alone — who live along the route the moon's shadow will travel during the eclipse, known as the path of totality. For sky-gazers in the areas experiencing totality, the moon’s shadow will completely cover the sun. Those along the very center line of the path will see an eclipse that lasts between 3 ½ and 4 minutes, according to NASA.
The total duration for all phases of the eclipse, however, lasts for hours. Since the moon doesn’t just suddenly appear between Earth and the sun, the event begins with a partial eclipse. The moon's shadow will slowly move across the sun's face during the approach to totality, causing the sun to appear like a sharpening crescent. Depending on your location, the partial eclipse can last between 70 to 80 minutes, according to NASA.
The eclipse will first appear over the South Pacific Ocean and begin its journey across North America. Mexico’s Pacific coast is the first point of totality on the path, expected at 11:07 a.m. PT (2:07 p.m. ET) and the eclipse is expected to end on the Atlantic coast of Newfoundland at 5:16 p.m. local time (3:46 p.m. ET).
During totality, the sky will darken as if it’s dusk or dawn. Depending on humidity and cloud cover, expect to feel a roughly 10-degree Fahrenheit (5-degree Celsius) drop in temperature when the sun disappears from view, according to NASA.
Look out for Baily’s beads just before and after the sun disappears. This scintillating phenomenon occurs when the sun’s rays shine around valleys on the lunar horizon, creating glowing drops of light around the moon.
The location that will experience the longest duration of totality is near Torreón, Mexico, where the peak of the eclipse will last 4 minutes and 28 seconds. But you don’t have to be squarely in the path of this solar spectacle to witness some of its wonders.
Millions more outside of the path of totality, across an area that includes 49 US states, will see a partial solar eclipse, in which the moon blocks a portion of the sun and appears to take a crescent-shaped “bite” out of it.
And be sure to find a pair of certified ISO 12312-2 compliant eclipse glasses ahead of the big day to safely view every stage of the eclipse and enjoy the celestial show while you can. Another total solar eclipse won’t be visible across the contiguous US again until August 2044.
Click here to see how the eclipse will impact your location.
CDC: Preterm Births in US is Rising

US Has Worse Maternal Mortality Rate of Any Undeveloped Nation
The CDC released new data showing the percentage of babies delivered preterm (before 37 weeks) jumped to nearly 8.7% in 2022. The 12% increase from 2014 represents hundreds of thousands of babies each year and poses a threat: Preterm birth is the leading cause of death and health conditions for infants and children. The study also found Black mothers were almost twice as likely as white mothers to give birth early.
Why is this happening?
It’s not always clear — but experts say giving birth later in life can raise risks. It comes as about one in five women in the US are having their first child after age 35. One expert also reportedly pointed to obesity as a potential factor in rising rates. Obesity doesn’t cause early births but complications associated with it, like preeclampsia, can. Stress can also play a role, and it’s possible other environmental factors can, too. Experts suggest pregnant people should see their doctor sooner if they’re experiencing headaches, changes in urination, and increased blood pressure.
The US has the worst maternal mortality rate of any developed nation. Now, this latest report points to another challenge some new mothers face as more than two million live in counties without access to maternity care.
North Carolina Among States Rethinking Reading

States, including NC, rethink reading
(Axios, Erica Pandey) -- Dozens of cities and states across America are overhauling the way their schools teach reading — attempting to close gaps exacerbated by the pandemic.
Why it matters: Nearly 40% of U.S. fourth graders are below the basic proficiency level for reading, according to a standard national exam.
By the numbers: 37 states and D.C. have passed laws or enacted policies changing up the way reading is taught — pursuing new methods that are backed up by studies.
Zoom out: Reading curriculums in America’s schools haven’t kept up with decades of science and research into how kids learn.
- Many districts have long used an approach dubbed “balanced literacy,” which directs teachers to read aloud to kids, inspire a love of books, and teach strategies like guessing words based on pictures or memorizing them.
- The new approach, called “the science of reading,” teaches it much more explicitly. It relies on methods that have evidence demonstrating their efficacy, and stresses some key pillars including vocabulary, comprehension and phonics.
Between the lines: The ability to understand language and stories develops naturally in kids, just like walking and talking, but reading does not, says Tiffany Hogan, director of the the Speech and Language Literacy Lab at MGH Institute in Boston.
- So the balanced literacy approach, which relies on kids’ intuition to pick up reading, only works for some students.
- Studies have shown that phonics-based instruction, however, is effective at raising test scores across the board.
That doesn't mean teachers should abandon stories and take a sterile approach to teaching literacy, says Hogan. Instead, explicit instruction on how to read words and inspiring a love for books should come together, she says.
How we got here: The reading debate had a breakout moment due to the collision of a number of trends over the last few years, The New York Times reports.
- Many parents — home with their kids for the first time during the pandemic — noticed problems with their reading and started a grassroots movement to convince lawmakers and educators to make changes, Hogan said. “The fire was burning, and that threw on the gasoline."
- A podcast from Emily Hanford of American Public Media that dove into the war between teaching methods — and zoomed in on the students who were falling through the cracks — got millions of listens and spread awareness of the issue.
- And some early adopters of the new methods saw stunning results.
Zoom in: Mississippi climbed from 49th out of 50 states for fourth-grade reading proficiency in 2013 to 21st in 2022.
- State legislators and educators tried a number of strategies, including screening kids for literacy, hiring literacy coaches for teachers, and emphasizing phonics.
- “After Mississippi, other states started paying attention,” Hogan said.
Reality check: Most states are rethinking reading, but the progress could take years or decades.
- The system is populated with educators who were taught entirely different methods, and "the resistance is real," said Mark Seidenberg, a psychologist at the University of Wisconsin.
- And teachers across the country are being asked to embrace a great deal of change when burnout levels are high and many are leaving the profession.
On top of that, even those who are open to new methods will have to go back to school to get up to speed per their states' new laws.
- "There's the question of 'Will these professional development programs and trainings be good enough?'" Seidenberg said.
What to watch: The reading movement has thus far focused on elementary school students and preventing problems in their futures, Hogan says. Next, districts will have to grapple with achievement gaps in middle and high school.
- Just 31% of eighth graders and 37% of twelfth graders are at or above basic proficiency. "As students get older, reading ability is a foregone conclusion," says Hogan. "And it shouldn't be."
Five Children With Hereditary Deafness Can Hear for the First Time After Gene Therapy

Researchers "Really Excited" to Test Gene Therapy on Other Types of Genetic Deafness
(NPR, Rod Stein) -- For the first time, gene therapy is showing promise for treating inherited deafness, researchers reported Wednesday.
A study involving six children born with a genetic defect that left them profoundly deaf found that an experimental form of gene therapy restored at least some hearing for five of them.
"We are absolutely thrilled," says Zheng-Yi Chen, an associate scientist at Mass Eye and Ear's Eaton-Peabody Laboratories and associate professor of Otolaryngology–Head and Neck Surgery at Harvard Medical School in Boston. Chen led the research, which was published in the journal The Lancet.
"This is really the first time that hearing has been restored in any adult or children by a new approach — a gene therapy approach," Chen tells NPR in an interview.
For the first time, gene therapy is showing promise for treating inherited deafness, researchers reported Wednesday.
A study involving six children born with a genetic defect that left them profoundly deaf found that an experimental form of gene therapy restored at least some hearing for five of them.
"We are absolutely thrilled," says Zheng-Yi Chen, an associate scientist at Mass Eye and Ear's Eaton-Peabody Laboratories and associate professor of Otolaryngology–Head and Neck Surgery at Harvard Medical School in Boston. Chen led the research, which was published in the journal The Lancet.
"This is really the first time that hearing has been restored in any adult or children by a new approach — a gene therapy approach," Chen tells NPR in an interview.
"Before the treatment they couldn't hear a thing. You could put the loudest sound in the ear and they don't hear anything," Chen says. "And now they can hear."
The children's hearing isn't completely normal — they may still need hearing aids — but improved significantly, Chen says. The treatment appears safe. The children have been followed for between six months and a year so far.
"It worked as well as we imagined," Chen says. "This really was beyond our expectations."
Chen and his colleagues have continued to treat additional patients and will follow the study subjects in the hope that the improvement is permanent.
"This is a very big deal. It's a new dawn for hearing loss," Chen says.
A first for treatment of hereditary deafness
Other researchers agreed.
"This is an incredibly important clinical study," said Dr. Lawrence Lustig, who chairs Columbia University's Department of Otolaryngology - Head & Neck Surgery, says in an email to NPR. "It is the first time it has been shown that genetic deafness can be treated with gene therapy in humans."
Hearing loss affects more than 1.5 billion people worldwide, including about 26 million who are born deaf, according to Mass Eye and Ear. For hearing loss in children, more than 60% stems from genetic causes.
The otoferlin defect accounts for an estimated 1% to 8% of genetic deafness, meaning as many as 100 children are born with the condition in the U.S. each year, Lustig wrote.
Several other groups are pursuing similar gene therapies for genetic deafness and will report their findings Feb. 3 at the annual meeting of the Association for Research in Otolaryngology.
Help Improve Child Welfare System with NCMS, Carolina Complete Health

A special message from NCMS CEO Chip Baggett
The North Carolina Medical Society is proudly part of the partnership that established Carolina Complete Health (CCH), the only Provider-Led Plan established to deliver Medicaid Managed Care in North Carolina.
As we turn to a new year, CCH needs your unique insights. It is looking to learn from providers about your experiences with children and families involved in the foster care system.
This letter outlines how you can get involved in the “Foster Share” Listening Series. I hope you'll take the time to help CCH, and your foster care families, as it looks to improve the experience for children and families in the foster care community.
Register for Listening Series:
Read Revised Policy Paper:
NCMS Member Dr. Seth Hawkins Inducted as a Fellow of The Explorers Club

Morganton doctor named Fellow of The Explorers Club
(The News-Herald) -- Dr. Seth Collings Hawkins of Morganton was recently inducted as a Fellow of The Explorers Club.
The Explorers Club is headquartered in New York City where it was founded in 1904. With current Chapters across the globe, The Explorers Club has been supporting scientific expeditions and field study in all disciplines for over a century.
Hawkins is an anthropologist, writer, and physician, double double-boarded in both emergency medicine and EMS (field medicine). He has decades of experience supporting expeditions throughout the world, particularly in the disciplines of medicine and anthropology.
He serves as medical advisor/director for the NC Outward Bound School, NC State Parks, the Student Conservation Association, Recreational Equipment, Inc (REI), and the National Association for Search and Rescue. He is also the Local Emergency Medical Advisor for all US Forests in North Carolina and the National Park Service Outer Banks (Cape Lookout and Cape Hatteras National Seashores). He is co-author of Vertical Aid: Essential Wilderness Medicine for Climbers, Trekkers, and Mountaineers, editor of the textbook Wilderness EMS, co-editor of the new second edition of Expedition & Wilderness Medicine, and founder of multiple wilderness medicine organizations, as well as medical director for multiple wilderness EMS teams and schools. He earned his Fellowship in the Academy of Wilderness Medicine (FAWM) with the inaugural class in 2007, and also became the first physician designated a Master Fellow by the Academy of Wilderness Medicine in 2014, with specialization in wilderness EMS.
He earned his Fellowship in the Academy of EMS with the inaugural class in 2014. He serves as Associate Professor of Emergency Medicine at Wake Forest University School of Medicine and is the Associate Director of the Wake Forest University School of Medicine Wilderness Medicine Fellowship. He is also currently a graduate student at The University of North Carolina at Charlotte in its dual degree anthropology-public health master’s degree program. He has published widely in the wilderness medicine literature, including as coauthor of several Wilderness Medical Society clinical practice guidelines. He earned his Diploma in Mountain Medicine at the University of New Mexico International Mountain Medicine Center in its 2023-24 Diploma class.
As well as supporting and participating in expeditions around the world, closer to his home in the US state of North Carolina (NC), Hawkins has run the Carolina Wilderness EMS Externship every year since 2011.
This program, frequently cited by its participants as the “best month of medical school,” takes two medical students/resident physicians and intensively trains them in wilderness EMS and expedition medicine over a one-month residential period. The program originated in Burke County, NC, as a county-based program, but in 2021 it became expeditionary and now uses the entire state of North Carolina as its classroom.
Dr. Hawkins comments for NCMS Members:
I very much see activities with The Explorers Club being consistent with an overall theme in my medical career: ensuring the quality of medical care delivered in wilderness areas is equivalent (or even sometimes superior) to the care delivered in other spaces. For sure the type of care may be different, but there is no intrinsic reason the quality should be less. More specifically here in North Carolina, my work is directed towards patients with a medical situation, for example, at the top of Attakulla (now known as Mt. Mitchell), in the waters or the shores of the Outer Banks, or deep in the forests of the Smoky Mountains. From both a medical and a public health perspective, their medical care is as important as the care of anyone anywhere else, and in some senses the stakes are higher. The spirit of The Explorers Club is one of curiosity and scientific enquiry into the interstitial and remote spaces of the world, and I’m excited to bring a medical perspective to that spirit.
In its most recent iteration in September of 2023, Hawkins and Externs David Baskin (Wake Forest University) and Brian Drury (Brown University) collectively traversed more than 18,000 kilometers in only four weeks. Their training and medical care operations took them throughout North Carolina, including both the highest mountain and the deepest gorge in eastern North America as well as a remote Atlantic Ocean island where emergency transport is only accomplished by helicopter or ferry. They trained with one of the oldest North American medical communities, the Eastern Band of Cherokee Indians, and one of the newest, the US Forest Service’s recently established EMS system. They slept on sea dunes and by rivers and mountains throughout the state, with more than half of the work completely in the field, sleeping in tents and training in the natural environment. The Externship also includes the Wake Forest-UNC WildMed Lake Weekend, where dozens of medical students travel to Lake James State Park in North Carolina and paddle out to a water-only accessible peninsula where they train in wilderness and expedition medicine skills for a weekend.
More internationally, Hawkins has contributed to scientific and expeditionary work in Australia, India, Costa Rica, England, Finland, Bhutan, Vietnam, China and Canada, among other locations. His expeditionary interests include both full-scale expeditions and smaller microadventures, a concept popularized by Alastair Humphrey.
Hawkins’s membership as a Fellow of The Explorers Club was advanced by current members Dr. Gregory H. Bledsoe, founder of the Expedition Medicine National Conference and lead editor of Expedition and Wilderness Medicine, and Dr. Kenneth Kamler, author of Doctor on Everest and Surviving the Extremes.
NCMS BOD, Committee Chairs, Staff Have Busy Weekend in Raleigh (Including Visit from Attorney General Josh Stein)
Attorney General Stein Addresses NCMS Board, Staff, Committee Chairs
RALEIGH -- The North Carolina Medical Society is kicking off 2024 with two days of meetings and planning, plus a visit from Gubernatorial candidate Josh Stein.
Attorney General Stein laid out his priorities for healthcare in a speech over lunch on Saturday. Stein says he is committed to improving the working environment of healthcare professionals, dedication to an expanded healthcare workforce in rural areas, and the protection of things such as telehealth. He also said he believes in the strongest support for the rights of patients and their physicians to make their own healthcare decisions.
Stein is running for Governor this year in a crowded field that includes NC Lieutenant Governor Mark Robinson. Robinson was also invited to address the NCMS group but had other commitments.
Meetings included a seminar on Friday afternoon that went over NCMS priorities and guidelines for NCMS Committees. The full list of committees and ways you can get involved can be found by clicking here.
On Saturday, the NCMS Board of Directors met along with staff and several committee chairs to discuss the NCMS 2024 strategic priorities, a report from the Secretary-Treasurer, an update on the 2024 LEAD Conference, and a look at the 2024 election.
The North Carolina Medical Society has several member candidates. We are currently featuring them in interviews in our 2024 Candidate Series. Look for those interviews in Morning Rounds and on our website.
Photos of AG Stein speech:
Photos of the weekend's Committee Training;
Photos of BOD Meeting:
World's First Malaria Vaccine Program for Children Begins

Cameroon starts world’s first malaria vaccine program for children
(ASSOCIATED PRESS) -- Cameroon will be the first country to routinely give children a new malaria vaccine as the shots are rolled out in Africa.
The campaign due to start Monday was described by officials as a milestone in the decades-long effort to curb the mosquito-spread disease on the continent, which accounts for 95% of the world’s malaria deaths.
“The vaccination will save lives. It will provide major relief to families and the country’s health system,” said Aurelia Nguyen, chief program officer at the Gavi vaccines alliance, which is helping Cameroon secure the shots.
The Central Africa nation hopes to vaccinate about 250,000 children this year and next year. Gavi said it is working with 20 other African countries to help them get the vaccine and that those countries will hopefully immunize more than 6 million children through 2025.
In Africa, there are about 250 million cases of the parasitic disease each year, including 600,000 deaths, mostly in young children.
Cameroon will use the first of two recently approved malaria vaccines, known as Mosquirix. The World Health Organization endorsed the vaccine two years ago, acknowledging that that even though it is imperfect, its use would still dramatically reduce severe infections and hospitalizations.
The GlaxoSmithKline-produced shot is only about 30% effective, requires four doses and protection begins to fade after several months. The vaccine was tested in Africa and used in pilot programs in three countries.
GSK has said it can only produce about 15 million doses of Mosquirix a year and some experts believe a second malaria vaccine developed by Oxford University and approved by WHO in October might be a more practical solution. That vaccine is cheaper, requires three doses and India’s Serum Institute said they could make up to 200 million doses a year.
Gavi’s Nguyen said they hoped there might be enough of the Oxford vaccines available to begin immunizing people later this year.
Neither of the malaria vaccines stop transmission, so other tools like bed nets and insecticidal spraying will still be critical. The malaria parasite mostly spreads to people via infected mosquitoes and can cause symptoms including fever, headaches and chills.
FDA: Don't Use Neptune's Fix, Dangerous 'Gas Station Heroin' Showing Up in NC

Tianeptine Poses Serious Risks as NC Cities Report it on Local Store Shelves
Lawmakers sent a letter to the FDA Thursday taking the first steps toward banning the dangerous substance tianeptine, known as 'gas station heroin.'
Tianeptine is not regulated by the FDA, but WRAL News discovered it is still winding up on local store shelves. Often times it is being marketed as a dietary supplement or a mood booster and is sold as Neptune's Fix Elixer.
States across the U.S. have reported a rise in overdoses due to the drug, according to the FDA. The drug is already banned in nine states, including bordering states Tennessee and Georgia.
Thursday's letter received bipartisan support and was led by Reps. Jeff Jackson (D-NC) and Rick McCormick (R-Ga.). Rep. Wiley Nickel (D-NC) was also among signees.
The FDA is warning consumers to not purchase or use any Neptune’s Fix products, or any other product with tianeptine -- a potentially dangerous substance that is not FDA-approved for any medical use but is illegally sold with claims to improve brain function and treat anxiety, depression, pain, opioid use disorder and other conditions.
FDA has received severe adverse event reports after use of Neptune‘s Fix products, including seizures and loss of consciousness leading to hospitalization. Consumers who experience a bad reaction to any tianeptine product should seek immediate medical help.
Neptune Fix’s labels state the product contains tianeptine, but may contain other harmful ingredients not listed on the label. These products, like other tianeptine products, can be purchased online and at gas stations, vape or smoke shops, or other locations. FDA is testing these products and will provide more information as it becomes available. FDA also continues to warn consumers about risks of using tianeptine.
Health care professionals and consumers should report adverse events or side effects related to the use of this product to FDA's MedWatch Safety Information and Adverse Event Reporting Program:
- Complete and submit the report online at MedWatch Online Voluntary Reporting Form, or;
- Download and complete the form, then submit it via fax at 1-800-FDA-0178.
On The Lighter Side - January 19, 2024 - Basketball, Hockey, Pasta, and a Beloved Duo!
Here are some things NCMS employees, members, and YOU are talking about this Weekend and Beyond!
College Basketball is full-court action this weekend!

Men's Basketball
Saturday
- #4 UNC vs. Boston College, 2:15pm
- #7 Duke vs. Pittsburgh, 8pm
- #2 Purdue vs. Iowa, 2pm
- #3Kansas vs. West Virginia, 4pm
- #1UConn vs. Villanova, 8pm
Sunday
- #10 Memphis vs. Tulane, 1pm
- #14 Illinois vs. Rutgers, 1pm
Women's Baskteball
Sunday
- #4 NC State vs. Duke, noon
- #15 Florida State vs. Virginia, 2pm
- #19 Notre Dame vs. Wake Forest, 2pm
- #13 Louisville vs. #23 UNC, 2pm
The Carolina Hurricanes hit the ice TONIGHT!

The Carolina Hurricanes take on the Detroit Red Wings at 7pm tonight. Players to watch include Seth Jarvis and Sebastian Aho. Will the Canes pull out a win! Check it out on ESPN+ or get tickets here.
It is Pasta Festival Time in Asheville!

Make fresh pasta, learn new recipes, and have fun for the whole family Saturday. All you need to know is here.
There will be Two Less Lonely People In The World Saturday with Air Supply!

See the famed duo at the Crown Theater in Fayetteville, Saturday at 7:30pm. Tickets can be purchased here.
If you have an event you would like added to On The Lighter Side, email Randy Aldridge at [email protected].
New Report: Colon Cancer Killing More Younger Women and Men Than Ever

Experts are stumped as to why colorectal cancer is rising dramatically among people in their 30s and 40s
(NBC - Erika Edwards and Jessica Herzberg) -- Colorectal cancer is the deadliest cancer for men under age 50 — and the second deadliest cancer among women in the same age group, behind breast cancer.
The incidence of colon cancer has been rising for at least the last two decades, when it was the fourth-leading cause of cancer death for both men and women under 50.
Among men and women of all ages, lung cancer remains the leading cause of cancer death. Prostate cancer is second for men, and breast cancer is second for women. Colorectal cancer is third, overall, for both sexes.
Even as overall cancer deaths continue to fall in the U.S., the American Cancer Society is reporting for the first time that colon and rectal cancers have become leading causes of cancer death in younger adults. The finding was published Wednesday in CA: A Cancer Journal for Clinicians.
Cancer is traditionally a disease among the elderly, although the percentage of new cases found in people 65 and older has fallen from 61% in 1995 to 58%. The decrease, attributed mainly to drops in prostate and smoking-related cancers, has occurred even though the proportion of people in that age group has grown from 13% to 17% in the general population.
In contrast, new diagnoses among adults ages 50 to 64 have increased since 1995, from 25% to 30%.
Rates of breast and endometrial cancer, as well as mouth and throat disease, have been on the rise. The report did not break down those diagnoses by age.
The findings reflect what cancer doctors have observed for years.
"For a couple of decades now, we have been noticing that the patients coming into our clinic seem to be younger and younger," said Dr. Kimmie Ng, the director of the Young Onset Colorectal Cancer Center at Dana-Farber Cancer Institute in Boston. "What this report now cements for us is that these trends are real." Ng was not involved with the new report.
Dr. William Dahut, the chief scientific officer at the American Cancer Society, said younger people tend to be diagnosed at later stages, when the cancer is more aggressive.
"So it's not only having a colorectal cancer — it's colorectal cancer that’s more difficult to treat, which is why we’re seeing these changes in mortality," Dahut said.
The diagnosis of late-stage colorectal cancer was a shock to Sierra Fuller, 33, of Acton, Massachusetts, just outside Boston. It was around Christmas 2021 when Fuller noticed blood in her stool when she went to the bathroom. With no family history of colon cancer, she figured the problem was most likely an annoying hemorrhoid.
Weeks later, the blood deposits worsened, and she started having abdominal pain.
"It was a month from when I got the symptoms to when I sought help, and I realize that I was pushing it," she said. Tests revealed she had stage 3b colorectal cancer. That usually means the cancer has started to spread through the colon and possibly to nearby lymph nodes, but not any farther, according to the American Cancer Society.
It was a blow to Fuller and her husband, who had just started talking about whether to try for a baby. They decided to freeze embryos before Fuller's treatment protocol, which would include radiation, chemotherapy and surgery.
It is an example of how cancer uniquely affects young patients.
"People younger than 65 are less likely to have health insurance and more likely to be juggling family and careers," Dahut said in a news release announcing the new report. "Also, men and women diagnosed younger have a longer life expectancy in which to suffer treatment-related side effects, such as second cancers."
Just over a year later, Fuller is cancer-free but must get regular scans and blood tests. She said that she feels good but that she is "always going to have that worry" that her cancer will return.
"If I have to go through this again, whatever that looks like, I'll cross that bridge if it comes," Fuller said.
Why is cancer rising in younger people?
Doctors do not know why cancer, especially colorectal cancer, is becoming more common in younger adults. Some hypothesize that increasing obesity rates, sedentary behavior and unhealthy diets could be playing roles.
"But honestly, the patients we're seeing in clinic often do not fit that profile," said Dr. Kimmie Ng, the director of the Young Onset Colorectal Cancer Center at Dana-Farber Cancer Institute in Boston. "A lot of them are triathletes and marathon runners. I mean, super healthy people."
Ng suspects something in the environment may be behind the rise.
"What we suspect may be happening is that whatever combination of environmental factors is responsible for this, that it’s likely changing our microbiomes or our immune systems, leading us to become more susceptible to these cancers at a younger age," Ng said.
How to protect against colorectal cancer
Colonoscopy screening is generally recommended starting at age 45. People with family histories of the illness may need to begin screening earlier.
A person whose parent was diagnosed with colon cancer at age 50, for example, would need to start screening at age 40, Dahut said.
However, only about a third of people diagnosed with colon cancer have some kind of family history or predisposition to the cancer.
Maintaining a healthy body weight and minimizing red meat in the diet may help reduce risk, Ng said.
Signs that could signal a problem, Ng said, include blood in the stool, abdominal pain, unintentional weight loss and changes in bowel habits.
"If it's getting worse, if it's not going away, you know, that's when somebody really needs to start paying attention and talk to their primary care doctor about what's happening," she said.
93-Year-Old Rowing Champ Has Scientists Reconsidering Beliefs About Aging
This 93-Year-Old Indoor Rowing Champion Has the Cardiovascular Engine of a 40-Year-Old

In a recent study, scientists were shocked and had to reconsider two beliefs about aging and longevity.
(The Washington Post, Gretchen Reynolds) -- For lessons on how to age well, we could do worse than turn to Richard Morgan.
Lessons on aging from active older people
Highest heart rate on record
Exercising 40 minutes a day
- Consistency: Every week, he rows about 30 kilometers (about 18.5 miles), averaging around 40 minutes a day.
- A mix of easy, moderate and intense training: About 70 percent of these workouts are easy, with Morgan hardly laboring. Another 20 percent are at a difficult but tolerable pace, and the final 10 at an all-out, barely sustainable intensity.
- Weight training: Two or three times a week, he also weight-trains, using adjustable dumbbells to complete about three sets of lunges and curls, repeating each move until his muscles are too tired to continue.
- A high-protein diet: He eats plenty of protein, his daily consumption regularly exceeding the usual dietary recommendation of about 60 grams of protein for someone of his weight.
How exercise changes how we age
NCCPRW Meets to Talk Future of North Carolina Clinician and Physician Well-Being
Well-Being Consortium Meets at NCMS Headquarters in Raleigh
RALEIGH -- The North Carolina Clinician and Physician Retention and Well-Being Consortium met Thursday at the NCMS headquarters in Raleigh. The agenda included a history of the Consortium by NCMS COO Shawn Scott and a look forward from NCMS CLO Ashley Rodriguez.
The meeting also included an update from Corey Feist from the Dr. Lorna Breen Heroes' Foundation about the Foundation’s partnership with the Consortium to lead the All In: Caring 4 NC’s Caregivers campaign. This initiative is designed to improve and protect the mental health and well-being of clinicians in NC and will be a core focus of the Consortium’s work for 2024.
In attendance were executives from around the state including Thomas Mansfield, CEO of the NC Medical Board, Rep. Timothy Reeder, President of the NCMSF Board of Trustees, NCMS Board member Dr. Charul Haugan, and members of the North Carolina Medical Board.
Here are some photos from the event:
2024 NCMS Candidate Series - Dr. Mary Ann Contogiannis

2024 NCMS Candidate Series Featuring Dr. Mary Ann Contogiannis
The 2024 North Carolina Medical Society Candidate Series kicks off with an exclusive interview featuring Dr. Mary Ann Contogiannis, who is vying for the US House - NC6 seat. Dr. Contogiannis delves into topics such as the impact of Medicare on North Carolina's senior citizens, the workforce shortage, prior authorization, and her vision for the future of medical care in the state.
 All candidates who are members of NCMS and are running for either state or federal office have been extended invitations to articulate their perspectives on these crucial subjects. Stay tuned for forthcoming interviews with other candidates leading up to the November election.
All candidates who are members of NCMS and are running for either state or federal office have been extended invitations to articulate their perspectives on these crucial subjects. Stay tuned for forthcoming interviews with other candidates leading up to the November election.
See the full interview with Dr. Contogiannis here:
https://youtu.be/eiu5pXai7y8
New Law Helps Military Service Members, Spouses Who Work as Physicians and PAs Practice in NC

2024 Brings Changes for Military Physicians and PAs
(Alan Wooten, The Center Square) -- For practicing physicians on North Carolina’s military bases, the new year brings change in state law that will provide help to them and those that can use their services.
Much of a broad bill passed in the General Assembly this year and signed by Democratic Gov. Roy Cooper on Sept. 29 went into effect immediately. A portion impacting relocating military members will be enacted Feb. 1.
North Carolina is home to six major military installations, chief among them Fort Liberty – the base formerly known as Fort Bragg and almost always recipient of any presidential “911 call.”
The Health & Human Services Workforce Act will allow “military relocation licenses for physician and physician assistant servicemembers and spouses.” The state board can issue a “military relocation license” to a “physician or physician assistant not otherwise actively licensed by the Board who meets” certain requirements.
Five criteria include being in the U.S. armed forces or a spouse of a service member; in North Carolina pursuant to military orders for military service; licensed in another jurisdiction with “substantially equivalent” or exceeding requirements of North Carolina; in good standing within that jurisdiction, with no disciplinary actions in the last five years or pending investigations by an occupational licensing board; and actively practicing medicine an average of 20 hours per week in the two years before relocating to North Carolina.
The Army’s Fort Liberty and Pope Air Force Base are in the southeastern part of the state; Seymour Johnson Air Force Base is in eastern North Carolina; and Marine Corps Air Station Camp Lejeune and MCAS New River are along the coast, not more than an hour's drive from the more inland MCAS Cherry Point. Two Coast Guard bases are on the northern coast at Elizabeth City; and the Military Ocean Terminal Sunny Point is on the southern coast in Brunswick County.
Among other things within the legislation are statutes related to over-the-counter hearing aids; credentialing of behavior analysts; optometry laws; audiology laws; oversight of Nurse Aide 1 education; requirement of law enforcement officers in certain hospital emergency departments; punishment for assault convictions against certain personnel; Medicaid reimbursements for dental procedures in ambulatory centers; and an updated definition of a bar in the sanitation statutes.
State-Funded Businesses to Consolidate to Reshape NC's Mental Health System
Consolidation to reshape NC’s mental health system
(NC Health News - Jaymie Baxley) -- Two state-funded businesses that manage behavioral health services for low-income residents say they will consolidate to create a single organization to serve 46 counties across eastern North Carolina.
Trillium Health Resources will take control of Eastpointe Human Services under the agreement, which was signed Saturday by the companies’ CEOs. The arrangement will reshape the state’s managed care system for providing care to Medicaid participants with mental health needs, substance use disorders and intellectual or developmental disabilities.
Eastpointe and Trillium are part of a network of six local management entities that operate as managed care organizations (known as LME-MCOs). That network oversees the treatment of those patients. A third such organization, the Sandhills Center, will dissolve in connection with the consolidation, leaving North Carolina with four LME-MCOs.
The consolidation flows from a directive issued in November by Sec. Kody Kinsley, head of the N.C. Department of Health and Human Services. He had been instructed by the General Assembly to reduce the state’s existing number of LME-MCOs to streamline the anticipated rollout of specialized plans for Medicaid participants who require more intensive services than typical beneficiaries.
DHHS has repeatedly delayed the implementation of these so-called tailored plans at the request of the LME-MCOs. Sandhills Center, in particular, struggled to secure tailored plan contracts with providers.
“Our goal is to get the tailored plan operators to a place where they can manage their patient population and the complex risks that they have in a smooth way,” Kinsley said in an interview Monday with NC Health News. “We’ve heard loud and clear from the provider community that their position is ‘less is more’ when it comes to managed care organizations. Getting the LME-MCOs [down] to four is a great opportunity to streamline the number of managed care companies that these providers have to contract with.”
He added that DHHS will be working closely with senior leaders from the consolidated LME-MCOs to prepare for the launch of tailored plans, which is now scheduled for July 1.
‘Sea change moment’
Nearly all of the counties served by Trillium, Eastpointe and Sandhills Center will be combined into one region, which will be managed by a yet-to-be-named company operated by Trillium. The consolidation is scheduled to take effect on Jan. 1, and the organization must have a new name and branding in place by the start of 2025.
“This is really a consolidation of entities that have different strengths,” Kinsley said. “And I think in recognition that they’re coming together as a consolidation, they should come up with a new name to recognize this step forward.”
In a joint statement on Monday, the companies promised that “all existing employees who desire employment and are in good standing will retain their positions.” The companies must “ensure that staff are offered compensation that is no less than employees’ current compensation,” according to the consolidation agreement.
Joy Futrell, CEO of Trillium, will become CEO of the new organization, while Eastpointe CEO Sarah Stroud will serve as its president. The agreement states that Anthony Ward, CEO of Sandhills Center, will be placed in an executive position.
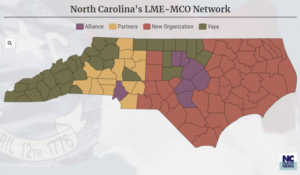 “We will continue to keep members as our primary focus,” Futrell said in a news release. “We know the next few months will contain many new opportunities, but believe the hard work that Trillium, Eastpointe, and Sandhills Center have already put forth will lead to a successful consolidation.”
“We will continue to keep members as our primary focus,” Futrell said in a news release. “We know the next few months will contain many new opportunities, but believe the hard work that Trillium, Eastpointe, and Sandhills Center have already put forth will lead to a successful consolidation.”
The new organization’s board will be made up of 22 members. Eleven of the members will come from Trillium’s board, and the other 11 will picked from the boards of Eastpointe and Sandhills.
“We’re still going to have to have more conversations in the future about how we have a board that will be representative of all the regions that they now share,” Kinsley said.
Three counties that were served by Sandhills Center and Eastpointe have been assigned to other LME-MCOs. Davidson County chose to change management entities to Partners Health Management; Harnett County moved to Alliance Health; and Rockingham County moved to Vaya Health.
While Kinsley acknowledged that the consolidation “was not an easy process,” he praised the companies for working together to “better serve the people of North Carolina.”
“I think we all know that the behavioral health system desperately needs it,” he said of the new organization. “This is a big sea change mo
The Biggest Health and Medicine Stories of 2023. There is Plenty to be Awed by.

In world with so much urgent and depressing news, it can be hard to take a moment and reflect on all of the encouraging scientific and medical progress that has happened. But looking back at 2023, there was plenty on the health beat to be awed by.
(Scientific-American, Tanya Lewis) -- From the arrival of the first safe and effective vaccines for a common respiratory disease to the first U.S. Food and Drug Administration–approved CRISPR gene editing treatment, these were some of the biggest stories in the health world this year.
NEW WEIGHT-LOSS DRUGS REVEALED NEW TRICKS
A new generation of drugs that result in significant weight loss appeared on the scene a few years ago with dramatic effects. This past year we learned a lot more about other potential benefits of the drugs, which include Novo Nordisk’s Wegovy and Ozempic and Eli Lilly’s Mounjaro. These range from reducing the risk of heart attack or stroke to possibly treating addiction. But the medications come with side effects such as gastrointestinal problems and muscle loss. They’re not cheap, either—they can cost around $1,000 or more out of pocket—and it’s not clear whether insurance will cover them. Still, these drugs are driving significant interest as we continue to learn more about them.
THE COVID PUBLIC HEALTH EMERGENCY ENDED
The federal public health emergency put in place to combat the COVID pandemic ended on May 11. The end of the public health emergency marked the conclusion of a set of policies that made it easier and cheaper to access COVID tests, vaccines and treatments, as well as telehealth visits. Consumers must now obtain many of these things with coverage through private insurance, Medicare, or Medicaid or bear the cost themselves. SARS-CoV-2, the virus that causes COVID, continues to circulate and pose a threat to public health. But in May the World Health Organization declared that disease no longer constituted a public health emergency of international concern and said that it was time to transition to long-term management of the COVID pandemic.
WE GOT CLOSER TO XENOTRANSPLANTS
There’s an enormous need for organ transplants, but donor organs are in short supply. Improvements in transplant science have made more organs available and usable. Yet too many people still die waiting for one. Now some scientists are exploring another approach: transplanting organs from nonhuman animals. In the past year they have made significant progress in such “xenotransplants.” Following the first transplant of a genetically engineered pig heart into a human in early 2022, this year doctors completed the second such transplant. (Both surgeries were performed on a compassionate use basis because the recipients were terminally ill.) Sadly, the man who received the heart in the latest surgery died after six weeks, likely because his immune system rejected the organ. Other researchers completed successful xenotransplant experiments in people who had suffered brain death, and monkeys that received pig kidneys survived for up to two years. Scientists are hopeful that they can improve the procedures enough to test these techniques in clinical trials in people soon.
RSV VACCINES FINALLY ARRIVED
Respiratory syncytial virus (RSV) causes annoying coldlike symptoms in most people, yet in very young children or older adults the disease can be deadly. For decades scientists have tried to develop a vaccine to protect against RSV, but a series of disastrous clinical trials in the 1960s ended up making the illness more severe, leading to the deaths of two children. Researchers persisted, however, and as of this year, several safe and effective RSV vaccines were approved by the FDA to protect pregnant people and older adults. The agency also approved an antibody drug that protects children after they’re born.
THE FIRST CRISPR-BASED TREATMENT WAS APPROVED
Nearly a decade after it was first discovered, the gene editing method known as CRISPR is resulting in its first treatments. In December the FDA approved the first CRISPR-based treatment for sickle cell disease. The new therapy is known as exa-cel and made by the biotech companies Vertex Pharmaceuticals and CRISPR Therapeutics. It deactivates a faulty gene for the hemoglobin protein, which transports oxygen around the body. Without the treatment, the gene causes blood cells to develop a sicklelike shape, making them clog up blood vessels. The illness, which disproportionately affects Black people, causes debilitating pain and fatigue. The new treatment, as well as another gene therapy approved at the same time, prevented symptoms of the disease for a year in clinical trials. But longer follow-up is needed to see if there are any side effects, and the cost could make it hard for many people to access.
WE GAINED NEW INSIGHT INTO LONG COVID
Even as the immediate danger of COVID has receded somewhat, tens of millions of people continue to be affected by long COVID—a cluster of symptoms such as fatigue, body aches and brain fog that linger long after an infection. The causes of long COVID are still mysterious, yet as Stephani Sutherland wrote in our March issue, it increasingly resembles a neurological disease. Not only does it cause cognitive problems with memory, attention, sleep and mood, but it also has symptoms such as pain and postexertional malaise—extreme fatigue after exercise—that seem to stem from the autonomic nervous system, the autopilot system that controls breathing and digestion, among other things. This new understanding could help guide treatments.
CHAT-BASED AI SYSTEMS ENTERED MEDICINE
When ChatGPT was released in November 2022, it caused ripples throughout numerous fields—and medicine was no exception. This chat-based artificial intelligence program made by the company OpenAI—along with large language models made by Google and others—is capable of generating text that convincingly mimics human writing. People have already begun to use these programs to diagnose medical conditions, and while the AIs appear surprisingly accurate in some early studies, doctors caution that they are not a substitute for professional medical care. Other people are turning to AI chatbots for therapy. Such apps could help meet the growing demand for mental health services, but as with using them for medical advice, experts urge caution.
FIRST FACE AND EYE TRANSPLANT WAS COMPLETED
Xenotransplants weren’t the only groundbreaking type of transplant to occur this year. In May doctors in New York City completed the first partial face and whole-eye transplant in an Arkansas man who had suffered severe electrical burns while working as a lineman. While corneal transplants are routine, this was the first time an entire human eye was transplanted and remained healthy six months later, according to the transplant team. The recipient, 46-year-old Aaron James, has not regained sight in that eye, but doctors say the eye’s retinal tissue is intact, and there are signs it may be sending signals to the brain. The feat opens the door to restoring the appearance—and possibly, one day, the function—of people who have had traumatic eye injuries.
Put your favorite health and medicine story of 2023 in the comments!
10 Biggest Health Risks Many Face During Christmas

**This article is with thanks to the South Coast Medical Group
The 10 Biggest Health Risks Many Face During Christmas
Christmas is a wonderful time of year, but it is also a time when people make their way into the ER with some unusual injuries. Before you curl up on the couch with a loved one and enjoy Elf, Christmas Vacation or Miracle on 34th Street, please take 2 minutes to read these reminders for having a safe and healthy holiday season.
1. Decorating Injuries
Slow down Clark Griswold!
Although you may be excited to put up the Christmas lights, there are many risks that come with that. One of the biggest risks is trying to hang the Christmas lights in hard to reach places on an unsteady ladder.

Tens of thousands of people get injured each year doing this simple task. The best way to stay safe is to stabilize a ladder on a flat surface before using, wear sturdy shoes, and decorate before you have too much eggnog.
2. Electric Shocks
In addition to ladder safety, it is important to be careful hanging lights, especially if they are plugged in. Old light sets that have spent several 11-month increments twisted up in storage can become brittle, and the wires may end up exposed. Be careful of any faulty lights that could cause you to get shocked. Faulty lights can also contribute to Christmas tree fires. Also, be mindful of how many things are going into one outlet.

3. Colds and Contagious Illnesses
Typically around the holidays, you are surrounded by many more people compared to normal. This year, the pandemic changes things, but it is still important to be mindful of who you are seeing and to avoid touching your face and consistently wash your hands. Even if you are limiting your contact, social distancing, and consistent mask usage can help you avoid germs.

4. Overeating
It’s hard to pass up mom’s signature dish during the holidays, and it seems like we never run out of sweets in December, but be careful. Overindulgence can cause weight gain that may only seem like a couple of pounds in the winter, but that gain could be a trend you don’t want to continue. Obesity comes with a whole new set of health issues. Try to be mindful of how much you are eating and drinking, and try to portion control. You know how wild the holidays are for Kevin McCallister.

5. Food Poisoning
In addition to overeating, another risk associated with food is food poisoning. Food poisoning can be caused by:
- Eating food that has sat out long without being refrigerated
- Food not cooked to a proper temperature
- Food exposed to cross-contamination
The best way to avoid this is to follow the food safety guidelines outlined by the CDC. Food poisoning can ruin all that fun, even dancing, during the holidays.

6. Anxiety
Anxiety can be a real challenge for many this holiday season, and the source of it can vary from person to person. Some people feel anxious being alone, while others feel anxious being around relatives they don’t see very often. Others simply develop anxiety for shopping or preparing for the season. Money issues can cause people a lot of stress. To help, take time to yourself and start your shopping and cleaning earlier.

7. Deep Cuts
The holidays call for a lot of preparation, and we’ve seen plenty of accidents in the kitchen and around the home related to sharp objects. Lacerations and cuts are a common injury, and they can come from chopping food for dinner, cutting wrapping paper for gifts or picking up broken glass from ornaments and decorations. There is no way to avoid these cuts entirely, but the best way to prevent them is by being careful and slowing down. Most of these accidents happen when you are in a rush.

8. Smoke Inhalation and Burns
If you think about it, there are many flammable items in your home during the holidays. These items include Christmas trees, burning candles, fireplaces, and food that is getting cooked in your home. When burning or cooking these items, you will want to make sure you keep an eye out for them, and never leave those items unattended. If you are deep-frying a turkey over the holidays, make sure you have ample space and protective clothing. When that cold turkey hits the hot oil, injury-causing accidents can happen.
Who hasn’t seen The Santa Clause? These things happen!

9. Choking
We know you’re excited to dig into Grandma’s homemade pumpkin or pecan pie, but please slow down when you eat. Also, avoid overstuffing yourself with stuffing. Choking on our favorite food is a serious health concern during the holidays.
Another thing to look out for is small toys that your pets and younger children may mistake for food. Watch over your pets and children and make sure that there are no small toys or parts laying around. Also, since it’s the season of chocolate, make sure it is kept at a safe distance away from our four-legged friends.
Nobody loved a good meal like Shaggy and Scooby, but please do so safely!

10. Binge Drinking
The holidays are a time to celebrate, but it doesn’t mean you need to go overboard. Please enjoy alcohol responsibly, and if your celebrations exceed your expectations, take a rideshare home, cozy up on the couch for the night where you’re celebrating, or get a ride from a friend.
If you’re a real Family Guy, maybe Peter Griffin will be your designated driver.

What have we missed? Leave tips for your colleagues below!
Poison Centers See Nearly 1,500% Increase in Calls Related to Injected Weight-Loss Drugs. Are Your Patients At Risk for Overdose?

Calls to poison centers increase
(CNN - Brenda Goodman) -- Poison control centers across the US say they are seeing a steep increase in calls related to semaglutide, an injected medication used for diabetes and weight loss, with some people reporting symptoms related to accidental overdoses.
Some have even needed to be hospitalized for severe nausea, vomiting and stomach pain, but their cases seem to have resolved after they were given intravenous fluids and medications to control nausea.
From January through November, the America’s Poison Centers reports nearly 3,000 calls involving semaglutide, an increase of more than 15-fold since 2019. In 94% of calls, this medication was the only substance reported.
In most of the calls, people reported dosing errors, said Dr. Kait Brown, clinical managing director of the association.
“Oftentimes, it’s a person who maybe accidentally took a double dose or took the wrong dose,” Brown said.
Compounded versions may require different doses
Semaglutide was approved by the US Food and Drug Administration in 2017. It is sold as Ozempic when used for diabetes and Wegovy when used for weight loss. Even when used as directed by a doctor, people can have stomach and bowel side effects, including nausea, vomiting and constipation, especially when they start the drugs.
After celebrities began openly embracing Ozempic on social media in 2022 as a way to lose weight, demand overwhelmed supply. It went into shortage in the FDA’s database in March 2022, which opened the door for certain qualified pharmacies to make compounded versions.
The compounded versions of semaglutide are often different from the patented drug. Many contain semaglutide salts called semaglutide sodium and semaglutide acetate. The FDA says the salt forms of the drug have not been tested and approved to be safe and effective the way the patented form of the medication has, and thus they don’t qualify for the compounding exemption in the law for drugs in shortage. In other cases, the compounded versions are sold in unapproved dosages.
The FDA has sent letters to at least two online sellers warning them to stop. Drugmaker Novo Nordisk has sued to stop six medical spas, medical clinics and weight loss clinics from selling knock-off versions.
But these compounded versions are popular because they may cost less out-of-pocket, especially if the treatment isn’t covered by insurance.
The FDA warned the public in June against taking compounded versions of the medication if the prescription forms were available. The agency said it had received adverse event reports after people used compounded versions of the drug.
Poison control centers say the reported symptoms don’t allow them to know whether the calls stem from the patented drugs or the compounded versions, Brown said, but some state poison center directors say they believe that compounded versions are behind many of the calls.
Calls to poison centers increase
Dr. Joseph Lambson, director of the New Mexico Poison and Drug Information Center, detailed what happened to three people who called the Utah Poison Control hotline, which saw calls related to semaglutide nearly quadruple between 2021 and 2022. He wrote about the cases in the Journal of the American Pharmacy Association
Two of the callers had accidentally taken 10 times the standard dose of the drug.
“We were getting reports of people giving themselves doses we had never heard of before,” Lambson said. “That’s kind of what sparked our interest” in tracking the calls.
The name-brand drugs are sold in pre-filled pens, which come with some safeguards. Patients dial to the correct dose and click to inject, so it’s harder to make mistakes. Ordinarily, people start at lower doses and work up over time to the therapeutic amount so their bodies can adjust.
Compounded versions, however, typically come in multidose glass vials, and patients draw their own doses into syringes. It’s easy to get confused.
“This is where we see a lot of errors. They end up drawing too much,” Lambson said.
One of the calls Lambson’s team received was from a 37-year-old woman who accidentally gave herself 1 milliliter instead of 0.1 milliliter – 10 times the recommended amount – as her first dose for weight loss.
A 50-year-old man accidentally gave himself 50 units instead of 5 units as his first dose for weight loss. He vomited for two days and had nausea for a week.
“I think that whenever we have to rely on a patient to discern what the right dose is, to draw up and then administer, you’re putting more chances in there for there to be errors,” Brown said.
A third caller, a 33-year-old woman, reported getting semaglutide at a spa but didn’t know the dose. She went to the ER for persistent vomiting and abdominal pain. She got an anti-nausea medication and IV fluids, and she was discharged later that day.
Julie Weber, director of the Missouri Poison Center, said it got 28 calls related to semaglutide in 2021. This year, through October, it has had 94.
Calls about semaglutide stand out in the data in other way, too. Although most calls to poison centers concern young kids who’ve accidentally ingested something, these calls are from adults ages 40 to 70, with the largest group in the 60-to-69 range.
Weber says the calls they see in their system aren’t only related to injections of compounded forms of the drug. Weber said many of their calls are related to the click pen that comes with the prescription drug.
In one case, a caller said they were having trouble with the pen and accidentally dialed it all the way up, giving themselves an entire month of doses at once.
“They misunderstood the pen. They did not know how to use it properly and dialed it up too and took like the whole pen instead of just the dose that was supposed to happen,” Weber said.
In other cases, reported at this year’s meeting of the American College of Medical Toxicology from the New York City Poison Control Center, people needed to be hospitalized. One of those patients accidentally took 20 times the recommended amount.
In a written statement, Novo Nordisk, the manufacturer of Ozempic and Wegovy, said patient safety is its top priority.
“We are taking multiple steps to ensure responsible use of our semaglutide medicines which are detailed on semaglutide.com,” the statement said.
There’s no specific antidote for a semaglutide overdose. The drug has a half-life of about a week, meaning it takes one week to clear half of it from your body. Emergency departments and hospitals can only help support patients with intravenous fluids and anti-nausea drugs as the drug works its way out out of their bodies.
In addition to nausea and vomiting, the Missouri Poison Center warns people who think they may have overdosed to watch for signs of low blood sugar, or hypoglycemia, which can be dangerous. Hypoglycemia is more common with semaglutide if you are also taking other medications for diabetes.
According to the Missouri Poison Center, signs of a semaglutide overdose include:
- Feeling lightheaded or dizzy
- Feeling shaky or jittery
- Sweating, chills and clamminess
- Irritability or impatience
- Headache
- Weakness
- Fatigue
- Nausea and/or vomiting
- Seizures
- Confusion
- Passing out
If you think you have overdosed on a weight loss drug, Brown said the best thing to do is call your local poison control center or the national hotline at 800-222-1222.
“That way, one of the specialists will be able to take specific information to their case regarding how much they administered, the type of overdose they’re experiencing … and decide if they’re safe to stay at home or if they are going to need to seek medical attention, especially if they’ve developed symptoms,” Brown said.
UNC-Chapel Hill Named National HIV Residency Pathway Consortium Site

UNC-Chapel Hill was recently named a National HIV Residency Pathway Consortium Site and awarded a year-long, $68,000 grant to support its efforts in training family medicine and internal medicine residents in caring for people with HIV. UNC’s site Investigators, Rick Moore, MD, and Louise Rambo King, MD, have a storied history of caring for patients with HIV.
(UNC Health Newsroom) -- UNC-Chapel Hill recently was named a National HIV Residency Pathway Consortium Site and awarded a year-long, $68,000 grant to support its efforts in training family medicine and internal medicine residents in caring for people with HIV. UNC’s site Investigators, Rick Moore, MD, and Louise Rambo King, MD, have a storied history of caring for patients with HIV.
This Health Resources and Services Administration (HRSA) grant through the National HIV Pathway Consortium (NHRPC) is part of a broader effort to enhance training in the management of HIV within primary care residencies at several sites throughout the country.
King and Moore work in partnership to lead longitudinal, integrated training in HIV care for training track residents to enable them to independently provide care for people with HIV in their clinical practices and thereby enhance access to HIV care on the state and national level.
“We are delighted to be part of this sub-award from HRSA to promote an area of concentration in HIV medicine for family medicine and internal medicine residents at UNC,” King said. “There is a real need for primary care physicians who are able to care for people living with HIV. This grant will give us the resources to support this area of concentration and develop it so that it is sustainable for the future.”
“This grant gives us the opportunity to strengthen and deepen experiences within the HIV and viral hepatitis training program,” Moore said. “We are thrilled to be taking part in this grant and what it allows us to do for resident education and development.”
“We are grateful for the collaboration between the family medicine and internal medicine departments and the invaluable contributions from the UNC infectious diseases division and the NC AIDS education training center, housed at UNC,” King said. “We are definitely better together!”
NHRPC is supported by the HRSA HIV/AIDS Bureau Ryan White Program through funding provided to the New England AIDS Education and Training Center, and is led by Philip Bolduc, MD, at UMass Memorial Health.
Could A Saliva Test Help Diagnose Cancer in the Future?

- The global number of cancer cases is expected to hit 28.4 million by 2040.
- For most cancers, early detection and treatment can provide better outcomes.
- Researchers from the University of Gothenburg in Sweden have found that structural changes in sugar molecules that occur in cancer cells can help identify specific types of cancers.
- Scientists believe this research could eventually be used to develop a blood or saliva test for detecting cancer.
(Medical News Today - Corrie Pelc) -- In 2020, about 19.3 million new cases of cancer were diagnosed around the world, and that number is expected to reach 28.4 million cases by 2040.
Although there are currently no cures for any type of cancer, for most cancers the earlier it is detected and treated, the better the outcome. For this reason, scientists are constantly exploring new ways to identify cancer quickly.
Contributing to this effort, a team of researchers from the University of Gothenburg in Sweden, has recently found that structural changes in sugar molecules called glycans that occur in cancer cells can help identify specific types of cancer.
Scientists believe that with the help of artificial intelligence (AI), this research could eventually be used to develop a blood or saliva test for detecting cancer.
This study was recently published in the journal Cell Reports Methods.
What are glycans?
According to Dr. Daniel Bojar, associate senior lecturer in bioinformatics at the University of Gothenburg and lead author of this study, glycans are complex sugar molecules that are attached to proteins and fats in our bodies.
“They are intricate chains of different sugar units linked together in various ways,” Dr. Bojar explained to Medical News Today. “If those connections are changed, the function of the glycan changes. In cancer, several processes can change glycans.”
“Mutations in the tumor may change the proteins that build up these sugar chains, leading to altered glycans,” he continued. “Additionally, inflammation and various other systemic conditions that may accompany a tumor also have a known impact on which glycan structures are being produced.”
While scientists know that glycans are systematically changed in cancer, aiding the tumor in its development, Dr. Bojar said most of this knowledge is not based on rigorous statistical analysis, compared to standards in other scientific fields.
“We were convinced that we could gain more insights from these molecules with newly developed methods,” he continued. “As the most information-rich type of molecule in our bodies, it is a natural proposition for a data scientist to use this information for predictions.”
“Further, glycans are present on proteins and particles secreted by the tumor and can thus be found in convenient locations such as saliva or blood, which allows us to remotely monitor the tumor without having to perform an actual biopsy,” Dr. Bojar added.
AI-powered cancer detection method
For this study, Dr. Bojar and his team analyzed tumor and healthy tissue data from about 220 people with diagnosed cancers, focusing on gastric, skin, liver, prostate, colorectal, and ovarian cancers.
“Our main concern here was to select types of cancer for which high-quality glycan data was available so that our results would be more reliable,” he said when asked why they decided to focus on those types of cancer.
Using a new method of studying the substructures of glycan using AI, the scientists were able to identify differences in the substructure of the glycan depending on the type of cancer.
“Glycans are structurally very complex, much more so than proteins or DNA, and are best understood with advanced analytical methods such as AI,” Dr. Bojar explained. “Further, the way that glycans are currently measured — via mass spectrometry — typically leads to very heterogeneous data, including missing data points due to a lack of sensitivity. This has really hindered the field from making robust assessments from this type of data in many cases.”
“Methods such as AI allow us to improve the data quality, which we have shown in the paper describing this method, and this allows us to identify these relevant substructures with high statistical significance.”
– Dr. Daniel Bojar
Potential for early-stage cancer detection
While this study focused on specific types of cancer, Dr. Bojar said there is no reason to think this test would not translate to other types of cancer.
“Especially the glycans that we find to be present in most or all of the types of cancer we analyzed should also be present in other types of cancer,” he added.
Dr. Bojar also said a blood or saliva test developed through this research could possibly result in a faster detection of cancer in its early stages, although further research would be required to determine conclusively.
“Another benefit of this technique is that cancer can be monitored, since samples such as saliva or blood are minimally invasive, compared to biopsies for example,” he continued. “This could also extend to monitoring for re-emergence of a treated tumor, which could be rapidly done using the method we present.”
For the next steps in this research, Dr. Bojar said they plan to collect more cancer data, specifically from saliva samples of lung cancer patients, to extend and improve their results.
“In parallel, we plan to use the universal as well as specific cancer markers we have identified so far and develop tests for them, using specific glycan-binding proteins that allow for rapid and reliable measurement of patient state,” he continued. “This would then be also much cheaper than mass spectrometry and is only possible because we now know what we are looking for.”
“While it is hard to judge when such a test would be commonly available to patients, we are planning to validate these tests on clinical samples of patients within the next four to five years,” he added.
Breaching new ground for cancer testing
MNT also spoke with Dr. Richard Reitherman, a board-certified radiologist and medical director of breast imaging at MemorialCareBreast Center at Orange Coast Medical Center in Fountain Valley, CA, about this study. Dr. Reitherman was not involved in this research.
“When cancers are detected, they’re detected by multiple means,” Dr. Reitherman explained. “The blood usually carries the usual components of red blood cells, platelets, proteins, [and] white cells, but it also carries DNA, RNA, proteins, glycoproteins, glycans, [and] lipids that are not normal, and therefore they test to recognize those. They are shed from the cancer cells elsewhere in the body because the bloodstream happens to go everywhere.”
“It’s kind of like panning for gold,” he noted. “You have the river running down, but you have to put your dish in there with its proper sieve, and it has to be the right size and the right place in the river, or you’re never going to detect the gold nuggets. And once you detect the gold nuggets, you can start to develop strategies of therapy for a particular cancer at whatever stage it is, so this is really exciting.”
Dr. Reitherman also said that he was very excited about the use of AI in this study.
“AI is becoming increasingly essential in the analysis of metadata, which is what this is,” he told us. “These studies generate so many data points and metrics of what they’re measuring, whether it’s glycans or proteins, DNA, [and] RNA in the blood or the saliva, that we can no longer rely upon little spreadsheets where smart people can look and say, oh, this means this, and this means that.”
Just in Time for Holiday Travel: Coronavirus Subvariant JN.1 Growing Fast in US
(CNN - Brenda Goodman) -- The US Centers for Disease Control and Prevention estimates that the coronavirus subvariant JN.1 is now causing about 20% of new Covid-19 infections in this country, and it’s the fastest-growing strain of the virus. It’s already dominant in the Northeast, where it is estimated to cause about a third of new infections.
JN.1 is descended from BA.2.86, or Pirola, a subvariant that came to the world’s attention over the summer because of the large number of changes to its spike proteins: more than 30. Scientists feared that it was so mutated that it would completely escape the protection of vaccines and antibodies against Covid-19, perhaps sparking another tidal wave of illness the way the original Omicron variant did in 2021.
That never happened, but BA.2.86 hung around, growing very slowly in some countries, including the US. Some studies suggested that it never really took off because it may have lost some of its ability to infect our cells.
Enter JN.1, which is two generations removed – a granddaughter, so to speak – of BA.2.86. JN.1 has only one change to its spike protein compared with its ancestor, but that seems to have been enough to make it a fitter and faster virus.
The CDC estimates that prevalence of JN.1 more than doubled in the US between late November and mid-December. It seems to be getting an assist from holiday travel and waning immunity.
“When I just look at the growth curve, it is rising quite sharply, and it seems to coincide with the Thanksgiving break in terms of timing,” said Dr. Shishi Luo, who heads infectious diseases for the genomic sequencing company Helix.
Variant trackers say they expect it to become the leading coronavirus variant around the world in a matter of weeks.
“It’s already pretty clear that it is highly competitive with existing XBB variants and looks like it’s on track to become the next sort of globally dominant group of variants,” said Dr. T. Ryan Gregory, an evolutionary biologist at the University of Guelph in Ontario, who has been tracking the evolution of the virus that causes Covid-19.
The mutation in JN.1’s spike is at a position that Gregory said seems to help the virus escape our immunity.
Studies by researchers at Columbia University and in China suggest that there’s about a twofold decrease in the ability of our antibodies to neutralize this subvariant. Although that’s not a huge drop, it could portend another wave of infections on the horizon.
Several countries in Europe – including Denmark, Spain, Belgium, France and the Netherlands – have seen exponential growth of JN.1 and, with it, rising hospitalizations. It’s also growing quickly in Australia, Asia and Canada.
That’s happening in the United States too, thanks to waning immunity. Too many Americans have chosen to forego the latest round of vaccination for Covid-19, and they may also have passed it up last year. As a result, their immunity hasn’t had the important upgrades that help the body fend off the worst consequences of Covid-19 infections.
As of December 9, only about 18% of adults had received the latest Covid-19 vaccine, about the same low proportion of the population that got them last year, according to the CDC.
The CDC has called on doctors to work harder to get their patients vaccinated, emphasizing that it’s not too late in the season to benefit from the shots.
The CDC also warned that in the past four weeks, hospitalizations for Covid-19 have risen 51%. With hospitalization rates for flu and RSV also on the rise, the agency noted that a continued increase could strain hospital capacity.
The good news is that a recent study from Dr. David Ho’s lab at Columbia University found that the current Covid-19 vaccine, which was designed to boost the body’s ability to fight of the XBB family of variants, also offers good protection against BA.2.86 and its offshoots, including JN.1.
That finding “strongly supports the official recommendation to widely apply the updated Covid-19 vaccines to further protect the public,” the study’s authors wrote.
Last week, the World Health Organization issued a statement supporting the upgraded Covid-19 vaccines against XBB.1.5 because of the broad protection they offer against a variety of variants.
“Fewer people are getting the booster, and fewer people are getting Paxlovid,” an antiviral that can reduce the risk of hospitalization and death from Covid-19, said Dr. Alex Greninger, assistant director of the Clinical Virology Laboratory at the University of Washington.
“There was a lot of work to get those vaccines and get those drugs available, so it’s just extra sad when those tools aren’t being used,” he said.
NC Medicaid Providing Free Educational Materials for Your Patients

NC Medicaid is providing free, printed educational materials for partners to distribute to individuals and families seeking more information about Medicaid expansion and enrollment. Sign up today for these informative materials that include NC Medicaid Toolkit materials and swag items available in English and Spanish. Materials will begin shipping (at no cost) in January.
To order your materials, please fill out the print materials order form by January 8, 2024
Plan Now to Attend 2024 AMA National Advocacy Conference

Join us on Capitol Hill
The AMA’s National Advocacy Conference is scheduled for February 12-14, 2024. This yearly event offers an opportunity for personal involvement in the health policy debate on Capitol Hill. We need increased NCMS member engagement with our members of Congress, so mark your calendar and stay tuned for forthcoming details.
Some helpful details and links . . .
- Preliminary agenda – additional details forthcoming
- Event registration
- Hotel reservations
Sign up today!
https://www.ama-assn.org/about/events/national-advocacy-conference
A Shorter Scan Could End Your MRI Nightmares

A typical test could take 40 minutes; a “fast MRI” can be done in as little as 10.
(Katie Couric Media - Rachel Uda) -- Getting an MRI is not exactly a comfortable experience. You’re stuck in a big metal tube and instructed to remain perfectly still while what sounds like a car alarm triggered at arm’s length reverberates around you. But it can be a lifesaving test, especially for the millions of women who have dense breasts. MRIs — scans that use magnetic fields and radio waves to image soft tissue in places ranging from the brain’s white matter to the ligaments in your knees — are an important tool to detect tumors. And they’re particularly good at picking up on breast cancer that other screening methods like mammograms might miss. Unfortunately, they’re pricey and, for the claustrophobic, they can be somewhat of a harrowing process.
Fortunately, a cheaper and much quicker method has been developed. Here’s everything you need to know about the aptly named abbreviated MRI, or fast MRI, and whether it could be a good option for you.
What is a fast MRI?
The fast MRI process is fairly similar to the typical breast MRI: You’re given contrast (a special dye that appears on the scan) through an IV, and you still have to lay in the tube and endure that ear-splitting noise. But instead of lasting 40 minutes, the abbreviated MRI can be done in as little as 10.
The conventional procedure takes up to 16 sets of images, but this new technique usually relies on just three. The screening provides less detail of the chest wall and the “kinetics” of a particular area — or how it moves over time — but in studies, it’s proven to be still highly effective at spotting cancer, says Wendie Berg, M.D., Ph.D., a leading radiology researcher at the University of Pittsburgh Medical Center.
“You lose a little bit of information, but not much,” she tells us.
And because it can be done so quickly, clinicians hope it’ll entice more high-risk women, who may have avoided MRIs out of fear, to get screened. In a study Dr. Berg helped run in 2009, she found that about a quarter of women with an elevated risk of breast cancer refused a free full-length MRI because of claustrophobia.
For now, fast MRIs typically refer to these breast screenings. But researchers are also trying to speed up other types of MRIs, like those mapping the liver or brain, chiefly through artificial intelligence. Clinicians have found that with A.I. software, fewer pictures are needed to develop highly detailed scans of the valves of the heart, for example, which cuts down on how long the test takes.
Who should consider a fast MRI?
Fast MRI is a valuable additional screening tool for women with dense breasts, who are at average risk. (Women known to be high risk because they carry a genetic mutation, have a strong family history, or have had chest radiation should have a full MRI, says Carrie Rochman, M.D., an associate professor at the University of Virginia School of Medicine.) About 40 percent of women are thought to have dense breasts, which makes them harder to screen. Their breasts have high levels of fibrous and glandular tissue, which on mammograms appear white — similar to tumors.
If you fall into this category, your doctor may recommend a digital breast tomosynthesis (also called DBT or 3-D mammography), which is more effective but still not quite as good as an abbreviated MRI, Dr. Berg says. According to a 2016 study that compared the two techniques in 1,444 women, fast MRI caught tumors in 17 cases, while DBT only detected seven.
In the past few years, the tool has slowly become more popular, but it’s still not widely used because it’s often not covered by insurance. (Some states require insurance providers to cover MRIs for certain women at higher risk. In those cases, coverage “generally” extends to fast MRIs, if it’s billed in a specific way — using what’s called a modifier 52 — that indicates it’s a partial or reduced procedure, Dr. Berg says.)
The self-pay model, where women pay for the exam entirely on their own, is also fairly common and is used in more than 200 facilities. According to Dr. Berg, the cost can vary from $250 to $850.
But a new bill could make the test much more affordable. Under the Find It Early Act, a bill that Katie helped introduce this year in Congress, insurance providers would be required to cover screening and diagnostic breast imaging at no out-of-pocket cost for high-risk women and those with dense breasts. The law would cover mammograms, ultrasounds, MRIs, and fast MRIs.
The technique is just another tool in our arsenal to catch breast cancer earlier in more women — and ultimately save lives.
Wake Forest University School of Medicine Research Roundup

Recently published findings and publications from Wake Forest University School of Medicine faculty
Study Finds Differences in Time Perception Consistent with Varying Clinical Symptoms of Parkinson’s Disease
WINSTON-SALEM, N.C. – Dec. 13, 2023 – Scientists from Wake Forest University School of Medicine have shown that the way patients with Parkinson’s disease perceive time may be indicative of underlying conditions that are known to be dopamine-dependent.
“For example, we could predict whether a patient had a behavioral addiction disorder or depression simply based on how they experienced the passing of a few hundred milliseconds,” said Kenneth Kishida, Ph.D., associate professor of physiology and pharmacology at Wake Forest University School of Medicine and principal investigator.
For the study, the research team measured how patients with Parkinson’s disease perceived the passing of (very short) intervals of time. This process is thought to be affected by dopamine, a neurotransmitter that’s made in the brain and acts as a chemical messenger, communicating between nerve cells in the brain and the rest of the body.
The study findings were recently published in Parkinsonism & Related Disorders.
“One potential impact of this work is the possible development of a behavioral biomarker that could augment diagnosis and treatment strategies for patients in neurology, psychiatry and those receiving deep-brain stimulation in neurosurgery,” Kishida said.
The study team is also conducting additional research to monitor subsecond fluctuations in dopamine in patients with these same conditions to gain insight into the mechanisms that dopamine influences and how these mechanisms are altered in patients with depression, addiction disorders and dopaminergic movement disorders.
The study was supported by grants from the National Institutes of Health: KL2TR00142, R01DA048096, R01MH121099, R01NS092701 and R01MH124115, and a Biotechnology and Biological Sciences Research Council grant: BBR01583X1.
Preclinical Study Suggests Bacterial Components Inside Abdominal Fat – Not the Amount of Fat – Impact Health
WINSTON-SALEM, N.C. – Dec. 13, 2023 –A new preclinical study from scientists at Wake Forest University School of Medicine is shedding light on the bacterial components inside abdominal fat and their impact on health.
The study was recently published in Obesity.
Cardiovascular disease is the leading cause of death and disability. Risk for cardiovascular disease is driven by diabetes, high blood pressure and unhealthy blood cholesterol levels, which are all often seen in people who are overweight or obese. However, this cluster of risk factors, known as metabolic syndrome, also occurs in thin people while many overweight people are also very healthy.
“More than 10% of lean individuals also have metabolic syndrome,” said Kylie Kavanagh, D.V.M., professor of pathology and comparative medicine at Wake Forest University School of Medicine and corresponding author of the study. “And 30% of individuals with obesity do not meet the metabolic syndrome criteria, so there are other factors to consider.”
One consideration in need of evaluation is the bacteria within our intestines, on our skin and in our tissues.
For the study, the research team analyzed the bacteria of visceral adipose tissue, which is the fat tissue deep inside the abdomen, in nonhuman primates (NHP) with varying metabolic statuses.
“In unhealthy lean and obese NHP models, we found that the microbiome was enriched withmore gram-negative bacterium,” Kavanagh said.
According to Kavanagh, gram-negative bacteria tend to be more pathogenic and incite more inflammation where they are detected.
The researchers discovered that the bacteria populated the fat tissue and were unrelated to weight. Further, the immune systems in the unhealthy models were less able to calm the local inflammation induced by this bacterium.
“This research highlights pathways for potential treatment of metabolically unhealthy people with or without obesity,” Kavanagh said.
The study was supported with grants from the National Heart, Lung and Blood Institute, R01HL142930, and the National Institutes of Health, ULTR001420.
Study Shows New Approach in Maintaining Islet Health
WINSTON-SALEM, N.C. – Dec. 13, 2023 – Islets are clusters of cells in the pancreas that detect blood glucose and produce insulin. The use of pancreatic islet transplantation to provide a replacement for the lost insulin-producing cells has proven to be a valuable therapy for treating Type 1 diabetes, but it is effective only for a short time. A major reason behind this failure is that islets do not do well once they are removed from their natural environment.
But now a study from scientists at Wake Forest University School of Medicine shows a new approach to maintaining islet health in a laboratory setting, which is significant for islet transplantation.
The study was recently published in Acta Biomaterialia.
“I believe this is the first study to show the importance of the extracellular matrix (ECM) in maintaining islet health long term” said Amish Asthana, Ph.D., assistant professor of surgery at Wake Forest University School of Medicine and co-principal investigator of the study.
The ECM is a large network of proteins and other molecules that surround, support and give structure to cells and tissues in the body.
For the study, the researchers sought to increase the lifespan and function of islets by recreating the islet’s natural environment, using an organ decellularization technology.
Current decellularization methods use harsh detergent-based solutions that disrupt the fibrous nature of the ECM. They also remove many critical signaling molecules present in the ECM like growth factors and cytokines, thereby reducing its potency. However, the team recently developed a novel, non-detergent-based decellularization method that preserves the molecular integrity and molecular factors.
Using the gentler decellularization process, scientists observed improved islet function.
“The knowledge from this study can lead to advancements in the field of pancreatic tissue engineering,” said Giuseppe Orlando, M.D., Ph.D., an associate professor of surgery at Wake Forest University School of Medicine, a transplant surgeon at Atrium Health Wake Forest Baptist and principal investigator of the study.
The authors said the findings are significant because the banking of healthy islets could potentially revolutionize clinical islet transplantation. Maintaining long-term islet function can also potentially result in the development of long-term models to study the pathophysiology of the disease and test potential treatments.
The study was supported by grants from the European Union's Horizon2020 research and innovation program No. 646272; the National Center for Advancing Translational Sciences; National Institutes of Health No. UL1TR001420, National Institute of Diabetes and Digestive and Kidney Diseases No. R01 DK116875 and the Diabetes Research Institute Foundation.
Conflict of Interest: Orlando is a board member for Seraxis Inc., a biotechnology company with an emphasis on islet replacement therapy. Orlando also has two patents pending related to the decellularization process and insulin-secreting cells. He also holds a patent related to organ and tissue decellularization.
Silver Nanoparticle-induced Photothermal Therapy Shows Promise in Treating Breast Cancer Cells
WINSTON-SALEM, N.C. – Dec. 13, 2023 – What impact do bacteria living inside breast cancer cells have on treatment response and outcomes?
It’s a question that researchers at Wake Forest University School of Medicine explored in a study recently published in Pharmaceutics.
“Breast cancer can harbor intracellular bacteria, which may have an impact on metastasis and therapeutic responses,” said Nicole Levi, Ph.D., associate professor of plastic and reconstructive surgery at Wake Forest University School of Medicine and the study’s corresponding author.
Silver nanoparticles are known for their antimicrobial activity, and they are FDA-approved for effectively killing a variety of cancer cells. Photothermal therapy is a relatively new cancer therapy that converts light into heat energy to kill cancer cells and bacteria.
“Cancer cells with bacteria inside of them can be resistant to traditional treatments, and the bacteria are difficult to kill when they reside inside,” Levi said. “So, our study looked at the impact of silver nanoparticle-induced photothermal therapy.”
The research team found that both tumorigenic and non-tumorigenic breast cells are resistant to heat or silver nanoparticles, when bacteria are present.
“Our findings demonstrate that the application of brief photothermal heating of cells using silver nanoparticles offers a synergistic benefit in killing both infected and non-infected cells,” Levi said.
Additional research is needed to evaluate how reducing intracellular bacteria can improve responses to breast cancer treatments such as chemotherapy.
Non-Hispanic Black Children Receive Pharmacologic Restraint More Often Than Other Racial Groups
WINSTON-SALEM, N.C. – Dec. 13, 2023 – A new study shows that among children hospitalized for mental health crises, non-Hispanic Black children were at the highest odds of pharmacologic restraint compared to other racial/ethnic groups.
The study findings were recently published in Pediatrics.
“Children in mental health crises are increasingly admitted to children’s hospitals to wait for inpatient psychiatric placement,” said Ryan Wolf, M.D., assistant professor of pediatrics at Wake Forest University School of Medicine. “During their stay, behavioral problems and acute agitation may occur.”
Pharmacologic restraint involves the administration of medications for acute agitation.
For the study, researchers conducted a retrospective study of children admitted for a primary mental health condition from 2018-2022 at 41 children’s hospitals in the U.S. and analyzed 61,503 hospitalizations.
Pharmacologic restraint was used in 7,309 hospitalizations or 11.9%. Non-Hispanic White children represented 54.8% of the group compared to 19.8% non-Hispanic Black children. Non-Hispanic Black children had the highest use of pharmacological restraint (14.8%) among all racial/ethnic groups.
“These findings indicate the urgent need for implicit bias training and de-escalation training,” Wolf said. “It’s crucial that health care systems and providers address these disparities in mental health care.”
Wolf conducted this research at Monroe Carell Jr. Children’s Hospital at Vanderbilt.
What to know about the RSV vaccine approved for pregnant people

- The RSV virus affects about 64 million people around the world each year, causing about 160,000 deaths.
- RSV may cause severe symptoms, leading to hospitalizations and possible death, in newborn infants and older adults.
- Health officials recommend pregnant people get Pfizer’s maternal RSV vaccine during the third trimester of pregnancy to protect their baby during the first six months of life.
The Centers for Disease Control and Prevention (CDC) recently issued a health advisory alerting healthcare providers about low vaccination rates against influenza, COVID-19, and respiratory syncytial virus (RSV).
The CDC warns that low vaccination rates may lead to more severe disease and increased healthcare capacity strain during peak respiratory virus season.
RSV is an infection of the lungs and respiratory tract that globally affects about 64 million people every year and causes about 160,000 deaths each year.
For most healthy adults, RSV presents mild symptoms similar to the common cold.
In vulnerable populations — such as newborn infants and older adults 65 years and older — RSV can cause severe symptoms and develop into conditions such as pneumonia and bronchiolitis, potentially leading to hospitalization.
For this reason, the CDC and the American College of Obstetricians and Gynecologists (ACOG) recommend that pregnant mothers receive the maternal RSV vaccine made by Pfizer during the third trimester to pass antibodies to their unborn baby.
Getting the maternal RSV vaccine could help protect infants from severe illness from birth through the first 6 months of life.
Why should pregnant people get the RSV vaccine?
Dr. Laura E. Riley, chief OB-GYN at New York-Presbyterian/Weill Cornell Medical Center and chair of the Department of Obstetrics and Gynecology at Weill Cornell Medicine in New York City, told Medical News Today that RSV is dangerous for babies and young children, as it can cause serious respiratory illness.
“In fact, [RSV] is the leading reason infants are hospitalized in the United States,” she said. “We should do everything we can to protect babies from RSV, and that’s why the vaccine is so important.”
Dr. Silvia M. Abularach, an obstetrician-gynecologist affiliated with multiple hospitals in Maryland, including Mercy Medical Center in Baltimore, agreed.
“For the first few weeks of life, infants are not able to mount a vaccination response and immunity and adequate immunity response,” Dr. Abularach explained to MNT.
“So that’s why infants don’t get vaccinated for a couple of months. The first few months of life is the most vulnerable time for these infants.”
“The take-home point is [that RSV] is not going to kill a young mother,” noted Dr. G. Thomas Ruiz, a board-certified OB-GYN and lead OB-GYN at MemorialCare Orange Coast Medical Center in Fountain Valley, CA. “They’re not going to get very sick — they’re going to get cold-like symptoms and maybe a cough. It doesn’t tend to affect adults.”
“But [RSV] can be a devastating disorder for newborns, leading to hospitalization and death from pneumonia,” Dr. Ruiz continued. “So you’re really [getting] the vaccine to protect your baby.”
Which RSV vaccine is approved for pregnant people?
Currently, the only RSV vaccine FDA approved as a maternal vaccine is Pfizer’s Abrysvo vaccine.
The pharmaceutical company GSK plc also makes an RSV vaccine called Arexvy. However, the FDA has only approved it for use in older adults 60 and older.
Dr. Riley advised that pregnant people who want to arm themselves with accurate information on the vaccine they should be taking can talk with a healthcare professional or visit credible websites from organizations and agencies such as the CDC.
“Abrysvo is the only RSV vaccine approved for use in pregnancy,” Riley noted.
“Not all doctors’ offices and pharmacies have Abrysvo yet. Pregnant people can search for pharmacies that have the vaccine on the Abrysvo website,” she added.
Dr. Abularach said a pregnant person can always ask their doctor to confirm which RSV vaccine they should have.
“If they choose to go to a commercial pharmacy like CVS or Walgreens, which have them available now — obviously confirmation there as well — asking the question to make sure that they’re getting the right vaccine,” she added.
It is recommended that pregnant people get the maternal RSV vaccine between 32–36 weeks gestation to prevent RSV in their infants once they’re born.
“The idea is to vaccinate the mothers in this particular window to protect these infants at their most vulnerable time, which is immediately after birth and for the first six months, especially for infants that are born during the RSV season,” Dr. Abularach explained.
“The antibodies [the infants] get is via the mother and the placenta, so that process takes about two weeks. A mother who is vaccinated at least two weeks in advance of the baby’s birth would allow the baby that protection,” she added.
Dr. Jourdan Triebwasser, assistant professor of maternal-fetal medicine at the University of Michigan Health, added that ACOG recommends the maternal RSV vaccine for pregnant individuals during RSV season, which runs from September through January in most regions of the U.S.
“Thousands of infants under (the) age (of) 6 months are hospitalized each year nationwide because of RSV infection,” Dr. Triebwasser told MNT.
“While some babies may only need observation or supplemental oxygen, others need intensive care and mechanical ventilation. Vaccination during pregnancy is a powerful tool to reduce the risk for your baby,” Dr. Triebwasser said.
Is the RSV vaccine safe during pregnancy?
The RSV vaccine Abrysvo made by Pfizer Inc. was approved by the Food and Drug Administration (FDA) in August 2023 for use as a maternal vaccine to help protect infants at birth and through the first 6 months of life.
The FDA approval was based on results from the vaccine’s phase 3 clinical trial where no safety signals were detected in either pregnant study participants or the children born after they received the vaccine.
Dr. Ruiz told MNT the RSV vaccine is incredibly safe, and there’s no reason for a pregnant person not to get one unless they are allergic to the vaccine’s carrier medium.
He also said another benefit of the maternal RSV vaccine is that it’s preservative-free.
“Preservative-free means there’s less things within the vaccine that’s going to cause an allergic reaction [for] the mom,” Dr. Ruiz explained.
“(With) the maternal vaccine, they make sure to give them something that is as nonreactive to the body as possible, so the term we use is preservative-free.”
Dr. Triebwasser noted the RSV vaccine is a recombinant antigen vaccine, meaning it’s not a live virus vaccine.
“Some people are hesitant to receive vaccines during pregnancy, although we have a lot of data on older vaccines, including the flu vaccine, that maternal vaccination is safe for the pregnant person and babies. There may be an association between RSV vaccination and preterm birth, although that is not certain. To limit (the) potential risk of preterm birth, the recommendation is to give (the) RSV vaccine at 32–36 weeks.”
— Dr. Jourdan Triebwasser, assistant professor of maternal-fetal medicine
What are the side effects of the maternal RSV vaccine?
According to Dr. Edward Liu, chief of infectious diseases at Hackensack Meridian Jersey Shore University Medical Center, currently, the reported side effects of the RSV vaccine seem mild and include:
- pain at the injection site
- muscle ache
- sore arms
- headache
- nausea
“No side effects are reported for babies,” Dr. Liu continued. “(The) RSV vaccine cannot be given to a newborn infant. Babies’ immune systems are not fully developed and sometimes do not respond to vaccines.”
Dr. Abularach agreed and stated the studies that have so far been published about the RSV vaccine in pregnant women have not reported any safety concerns.
“The main side effects have been mild to sort of moderate,” she continued. “And it’s really the same side effects that you would expect with most vaccines — pain at the injection site, muscle pain, sometimes nausea or headache, relatively mild things. Some people have concerns about vaccines, and we always recommend that they discuss that with their provider, and shared decision-making takes place between the provider and the patient, so this would be no exception — we would recommend that as well.”
— Dr. Silvia M. Abularach, OB-GYN
Are there alternatives to the RSV vaccine?
If a pregnant person does not want to get the maternal RSV vaccine, there is another option to protect the baby from the disease.
“A new injection nirsevimab is a manufactured antibody product that can be given to babies to protect against RSV,” he explained. “Nirsevimab is limited in its availability and may not be covered by insurance.”
Nirsevimab is available to infants from birth up to 8 months old, who are at highest risk for severe illness from RSV.
Dr. Riley noted that a newborn might be able to get a dose of nirsevimab — which is a monoclonal antibody — before they leave the hospital or birth center if a pregnant person was not able to get the RSV vaccine in their area or had not heard about it.
“Nirsevimab is a shot containing lab-made antibodies that protect against RSV,” Dr. Riley explained. “It is not a vaccine, but it helps the baby build immunity against the virus. Both the vaccine during pregnancy and nirsevimab after birth are safe, effective options for protecting the baby from RSV.”
“It may be hard to get nirsevimab this fall and winter. An OB-GYN may be able to help someone find out if nirsevimab will be available for their baby after birth,” Dr. Riley noted.
Good Holiday News! Most People in World Feel Cared for by Others

Most People in the World Feel Cared for by Others, Survey Finds
A survey of about 143,000 individuals across 142 countries found that most people — 7 in 10 — feel very or fairly supported by those around them.
The Global State of Social Connections survey, conducted by Meta and Gallup last year, defined social support as “how much you feel cared for by people.” The newly released report offered some important insights into just how essential that support is for humans’ overall well-being.
Of those who felt very supported, 71% said they did not experience stress a lot of the day before the survey, and 67% did not experience physical pain during much of the day before. The report noted that these results, connecting social support to lower stress and physical pain, “may have implications for creating strategies to help people cope.”
Social support may be an important ingredient in a recipe to improve people’s health and well-being,” it read. “Yet, this ingredient may not be as readily available in more challenging environments, and people may lack support despite feeling connected to one another. In environments like these, social safety net programs such as affordable health care, housing assistance, or retirement income can help substitute when people lack support from each other.”
READ MORE ON THE FINDINGS HERE
New Study: Vaccine Cuts Odds of Skin Cancer Recurrence in Half

(CBS - Kate Gibson) -- A vaccine shows promising results in treating the most deadly form of skin cancer, Moderna and Merck announced on Thursday.
Those with severe melanomas who received the vaccine and Merck's cancer drug Keytruda were 49% less likely to die or have their cancer come back after three years than those who were given only Keytruda, the biotech companies said in a news release.
The findings are based on an ongoing randomized trial involving 157 patients with high-risk stage III/IV melanoma who first had surgery to completely remove cancerous growths. Patients received one milligram of the mRNA vaccine every three weeks for nine doses, and 200 milligrams of Keytruda every three weeks for about a year versus Keytruda alone for approximately a year.
The companies have begun Phase 3 trials of mRNA-4157 with Keytruda for people with stage III and IV melanoma. The Food and Drug Administration earlier this year designated the treatment as a breakthrough therapy in order to expedite the development and review of drugs meant to treat life-threatening diseases.
"We look forward to sharing these data with people impacted by the disease and the broader scientific community," Kyle Holen, M.D., Moderna's senior vice president and head of development, therapeutics and oncology, stated.
The results are a vindication of sorts for Moderna's strategy to develop new uses for messenger RNA technology used in its COVID-19 vaccine. Cambridge, Massachusetts-based Moderna said in November it anticipates a steep decline in revenue next year, fueling worries about its capacity to finance multiple product launches planned for 2024 and 2025.
Skin cancer is the most common form of cancer, with melanoma accounting for only about 1% of skin cancer cases in the U.S. That said, it causes a large majority of skin cancer deaths, according to the American Cancer Society. It estimates about 97,610 new melanomas will be diagnosed in the U.S. this year, resulting in 7,990 deaths.
Moderna's stock has cratered this year, falling 50%. On Thursday, its shares shot up 12% in mid-day trading to $87.93.
Rahway, New Jersey-based Merck shares treaded water, down 0.2% at $106.16.
NC Pushes Back Medicaid Unwinding for Children
The state also is pursuing waivers to protect children further by keeping them enrolled longer before eligibility reviews, reducing the times children may temporarily lose coverage.
(NC Health News, Jennifer Fernandez) -- North Carolina children insured through Medicaid will remain covered for another year as the state works its way through recertifications of everyone on the program.
Health experts praise the move, which they say should help protect children from losing coverage over procedural issues when they would otherwise still be eligible during the process known as the “unwinding,” where states have been disenrolling people who gained Medicaid during the pandemic.
In April 2020, Congress passed a policy preventing states from kicking people off of the Medicaid rolls for the duration of the national public health emergency. That mandate expired this spring.
North Carolina, which requested a waiver to extend eligibility for children on Oct. 31, is only the second state after Kentucky to be approved.
“We believe continuing health care coverage for children is not only in the best interest of North Carolina, but it will also help reduce the immediate workload of County DSS staff,” the North Carolina Department of Health and Human Services said in an email, referring to the county Department of Social Services offices, which are handling Medicaid unwinding alongside a massive Medicaid expansion that is expected to add 600,000 beneficiaries in the state.

Leo Cuello, research professor at the Georgetown University McCourt School of Public Policy’s Center for Children and Families
The state is also seeking other waivers that would benefit North Carolina children by keeping younger kids continuously enrolled in the program through age 5 and older children enrolled for two years before needing recertification. Another waiver being sought would keep some children who have aged out of foster care enrolled in Medicaid through age 26. Those waivers are pending before the Centers for Medicare and Medicaid Services.
“The big picture in North Carolina right now is pretty good” when it comes to children and Medicaid, said Leo Cuello, a research professor at the Georgetown University McCourt School of Public Policy’s Center for Children and Families.
‘Unwinding’ ends some children’s enrollment
As with adult enrollment, the number of children covered by North Carolina Medicaid in the state swelled during the pandemic. For kids, enrollment grew from 1,168,602 in March 2020, to 1,382,255 this May.
The continuous coverage requirement allowed beneficiaries to skip Medicaid’s renewal process for about three years during the pandemic. All participants, even those who no longer qualified for the program, were automatically re-enrolled during the period.
North Carolina began the process of “unwinding this excess enrollment,” in June. Before the waiver to extend enrollment was approved, children were subject to being disenrolled during the process.
Nationally, more than 2.8 million children have lost Medicaid coverage since states resumed eligibility reviews.
However, the reasons for children losing coverage are not always clear. Some may have lost coverage because the state determined they were no longer eligible, while others may have been disenrolled due to procedural issues, such as their parents not returning paperwork on time, even if they were still eligible.
“Federal researchers prior to this process beginning projected that three out of four kids who lose Medicaid would remain eligible. And that’s a much higher number than what’s expected for adults,” said Joan Alker, executive director and co-founder of the Center for Children and Families, during a November webinar on how unwinding is affecting children across the country.
Fewer uninsured children
The rate of uninsured children had been steadily declining in the country from 2008 through 2016 before it began rising again.
Advocates say the pandemic-era changes to Medicaid have improved health insurance coverage for children, who make up about half of all program participants.
North Carolina had the fifth largest decline in the number of uninsured children from 2019 to 2022, according to a recent report by Georgetown University’s Center for Children and Families that analyzed the U.S. Census Bureau’s 2022 American Community Survey.
The state’s rate of uninsured children improved from 5.8 percent to 4.8 percent in that time.
Nationally, the rate is 5.1 percent. The District of Columbia has the lowest rate of uninsured children at 1.4 percent. Texas has the highest rate at 10.9 percent.
Thirty-six states saw a decline in the number and rate of uninsured children.
“Unfortunately, this progress is likely short-lived” because of Medicaid unwinding, Alker said, adding that for children, Medicaid enrollment is “declining rapidly.”
Coverage dropping
During the pandemic, North Carolina’s Medicaid rolls grew from a total of 2.1 million beneficiaries in March 2020 to just under 3 million people qualifying for coverage in May of this year. Enrollment for children through age 18 grew by 213,653 beneficiaries during that time, state data shows.
Through October, DHHS reports 162,138 people in North Carolina have lost coverage as part of the redetermination process. The vast majority, about 87.5 percent, were disenrolled for procedural reasons, such as not returning paperwork.
It’s not clear how many of those are children.
As part of unwinding, states are required to share information on the process. However, only 21 states publicly break down disenrollments by age group, according to KFF, a foundation that focuses on health policy. North Carolina is not one of them.
In those states that do track by age, children accounted for about 4 in 10 disenrollments through Dec. 7, according to KFF’s analysis of data.
North Carolina does break down overall enrollment in Medicaid, including by age group. That dashboard shows there are about 53,000 fewer children covered under the program since unwinding began.
While North Carolina doesn’t track data on children disenrolled during unwinding, NC DHHS noted that “children historically retain coverage at recertification because income thresholds for them are higher and it is uncommon for their eligibility to change.” So, sometimes, even if a parent is not eligible for Medicaid, their children might remain in the program.
Before the COVID-19 public health emergency, “nearly 80% of children retained Medicaid coverage during the recertification process,” NC DHHS said.
One in four children disenrolled typically enroll again within 12 months, NC DHHS said, citing a 2021 study by the Duke Margolis Center for Health Policy.
The study’s authors added, though, that even short lapses in coverage, or “churn,” can have adverse effects on a child’s health.
The effects of ‘churn’
“Every day a child spends without coverage is a detriment to their well-being and a serious risk to their health,” pediatrician Valerie Smith said during the Center for Children and Families’ webinar last month.
Smith, who works at a clinic in Tyler, Texas, shared stories of families whose children have lost coverage already during unwinding. One boy newly diagnosed with attention deficit disorder could not get the medicine he needed. Medicaid had helped a young girl survive catastrophic acute kidney failure — but she recently lost coverage, and her mother doesn’t know what they will do if the daughter needs more care for her illness.
“We know that when someone is uninsured, they’re more likely to delay or go without the care they need,” Smith said. “This means that kids might be unable to get follow-up care for injuries and newly diagnosed chronic conditions, or they may be skipping doses of their medication.”
According to the Duke Margolis study, even short disruptions in insurance coverage mean children are “less likely to receive preventive care, and are more likely to seek emergency care for ambulatory conditions.”
Medicaid unwinding could also lead to wider racial and ethnic disparities in health insurance coverage, as children of color make up a disproportionate share of Medicaid enrollment and may face more barriers to staying covered, the Center for Children and Families said.
“It’s clear that when families have easier access to these programs, health outcomes for young people improve across the board,” Smith said.
Protecting children
In North Carolina, 9 out of 10 people who remain on Medicaid after going through redetermination have been approved through an “ex parte” process. In these cases, the state uses information from various programs to determine eligibility and automatically renews coverage.
The state is best in the nation for ex parte approvals, according to KFF.
That high rate helped minimize the impact on children being disenrolled through procedural determinations, where something as simple as not returning paperwork could lead to a coverage lapse, according to Cuello with the Center for Children and Families.
“Procedural determinations are much more harmful because you’re almost always terminating a kid who was eligible,” he said.
Cuello said the state is doing “a lot of things to reduce the harm.”
He also said the state should be commended for pursuing the various continuous enrollment options, which he called “the real long term solution to drive down the renewal termination rate.”
Alker also pointed to North Carolina as a good example for handling children during unwinding by extending their eligibility for another year.
“We hope more governors will think about doing that (to) protect children during the process,” she said.
Before You Buy! Toy Safety Warning

Amazon, Walmart and Target stop selling water beads marketed toward children
(CNN, Ramishah Maruf) -- Amazon, Target and Walmart have voluntarily stopped selling water beads marketed for children after government officials, lawmakers and public health professionals called for a ban on the toys.
Water beads are tiny balls made out of extremely absorbent polymer material. When exposed to liquid, they can expand to 100 times their initial size and weight, according to the Consumer Product Safety Commission.
Because they can grow inside the body once ingested, these toys pose immense health risks to young children, say experts.
And, because they’re mostly made up of water, typical X-rays often do not pick them up. In a safety alert in September, the CPSC reported that these beads “can cause severe discomfort, vomiting, dehydration, intestinal blockages and life-threatening injuries” and may require surgery to remove.
They’re sold as popular children’s toys to promote counting or develop motor skills. But the water beads have drawn scrutiny from lawmakers and the CPSC.
Last month, US Rep. Frank Pallone Jr. of New Jersey introduced legislation aimed at instating a national ban on beads marketed to kids.
“They are specifically marketed to kids. In a single small package you can have 25, 50, or even 75 thousand of these beads and it just takes one to cause harm to a child,” Pallone said in a November news conference. “They are not labeled as dangerous to small children, there’s no warning, and they’re not hard to get.”
An Amazon spokesperson confirmed the company updated its water bead policy on Tuesday. The e-retailer said it would remove listings for water beads if it refers to or includes images of children, or is described using toy, sensory play, arts or crafts.
“In the interest of safety, Amazon will no longer allow the sale of water beads that are marketed to children, including as toys, art supplies or for sensory play,” a company spokesperson said. “We work hard to ensure the products offered in our store are safe, and we have teams dedicated to developing and updating our policies, evaluating listings, and continuously monitoring our store to prevent unsafe and noncompliant products from being listed.”
In a statement Tuesday, Target also said it will no longer sell water beads marketed to children, in-store or online.
Walmart, in an email sent Tuesday, said protecting customers is its top priority.
“We decided to voluntarily stop selling expanding water bead toy and craft items marketed to young children and have already taken steps to remove them from our stores and online,” a spokesperson in an email.
Consumer Reports first reported the voluntary bans on Amazon and Walmart.
In the same November news conference in which Pallone introduced the legislation, CPSC Chairman Alex Hoehn-Saric said, “It is far too easy for beads to be lost, dropped, and a short time later a baby or small child ends up finding them, picking them up and ingesting them.”
CPSC urges parents and caregivers to remove products from the proximity of small children.
Most recently, in September, Buffalo Games recalled “Chuckle & Roar Ultimate Water Beads Activity Kits” sold exclusively at Target after one infant death was reported.
– CNN’s Eva Rothenberg contributed to this report.
Advancements in Medical Care Could be Saving Lives Amid Conflicts Around World

Innovations such as portable labs are helping save more lives, experts say
(ABC News, Mary Kekatos) -- Performing medicine can be difficult in any setting but perhaps no more challenging than during a humanitarian crisis.
Doctors, nurses, and other medical professionals are often performing under extreme duress with a limited number of tools compared to working in a traditional hospital setting.
There have been medical advances over the centuries when it comes to battlefield medicine both in the training and the equipment used, but more recent improvements in care may be helping save more lives in wars, such as the one in Ukraine and ongoing Israel-Hamas conflict, than were available a decade or two ago.
Experts told ABC News that some of the innovations are in the technology used -- such as portable laboratories -- to organizational changes, such as making sure civilians are also receiving basic health care on top of surgical care to prevent a separate public health crisis from emerging.
Social media helping doctors
In past humanitarian conflicts, when telegrams or landline calls were the standard form of communication, it was hard for doctors treating patients in conflict zones to ask for help or advice from their colleagues abroad.
In conflict zones, whether it's a local doctor or a doctor who has been deployed from another country, medical professionals are often treating patients with conditions they are not familiar with.
Dr. Tom Weiser, clinical professor of surgery in the field of trauma, critical care, and emergency general surgery at Stanford University School of Medicine, said the advent of social media and connectivity has been a major asset to doctors working in conflict zones.
"Being able to reach out to colleagues, and ask advice about, 'Hey, I have this thing that I've never seen before,'" he told ABC News. "I may be a plastic surgeon or a gynecologist and now I've been recruited into this conflict, [someone] who has surgical skills but is now suddenly operating or asked to operate beyond his or her normal scope of practice."
Weiser added, "I would say that probably the biggest change is the ability to receive advice or perspective from those who might have had an experience who is not necessarily sitting next to you or leaning over your shoulder, but can [be] just a phone call or WhatsApp or Telegram or a YouTube video away."
Portable laboratories
One of the recent innovations of Doctors Without Borders or Médecins Sans Frontières (MSF) is the "Mini-Lab," which is designed to be a transportable clinical laboratory that is easy to set up and is affordable when MSF workers are deployed.
According to MSF, it can be set up in areas where traditional laboratories are lacking, and even non-experts can use it after brief training.
"That's something that you can kind of deploy to a conflict zone within limits," Dr. Amber Alayyan, MSF's deputy program manager for Palestine, told ABC News.
"So, with that, it's a miniature microbiology lab and that's been quite revolutionary in the sense that we can deploy that quite quickly," Alayyan added.
Alayyan said this helped with longer-term surgical missions or "surgical programs that especially in the situation like in Gaza, or in other places that we've seen sort of more 'modern conflicts' whether it's we've not used it in the Ukraine, but that kind of setup or in Syria, where you have a lot of very severe injuries."
Alayyan explained that in conflicts with severe injuries and surgeries that don't have the best hygiene, there is a high potential for wounds to get infected.
"That's where something like the mini-lab would come into play," she said.
Staff can use the mini-lab to determine what kind of disease or infection someone has and from there, figure out how to treat it.
Advancements in amputations
Over the years, there have been a number of innovations in the field of amputation from the introduction of tools such as artery forceps in the 16th century to techniques to make the surgery more effective.
Although doctors often try to save a limb, Weiser said that over the past few decades, medical professionals have realized some limbs may be so badly damaged, especially in conflict, that amputation may be more beneficial.
"Fundamentally, a lot of people can spend a lot of time salvaging limbs that then are fairly useless to the person because they've just lost so much tissue that you might have a limb, say a foot, that's still there but the patient kind of drags it along and it's actually more of a hindrance, especially for somebody who's otherwise young and healthy than if you had done an amputation," he said. "I do think that we've learned not to try and overtreat limbs that really aren't going to be functional."
He added that it's also important to make this realization quickly to prevent a patient from going through multiple unnecessary surgeries.
"You can put somebody through many, many operations and then, at the end of the day, realize you've done all these operations, you got all these anesthetics, you've done all this reconstruction or attempted reconstruction, and you still don't have a functional extremity," Weiser said.
Access to basic primary care
Alayyan said there has been more of an emphasis in recent conflicts compared to past conflicts to provide basic primary care to those affected.
"I can't emphasize enough the need for people to look at primary care during a conflict and what I mean by that are vaccinations, making sure that the diseases that would be prone to epidemic levels are under control, that basic hygiene is under control, that basic health is being looked after," she said.
She said the term "lifesaving care" doesn't just mean treating the injuries experienced during war but also making sure basic health needs are met.
"In the past, lifesaving meant surgery, surgery, surgery. And I think that what we've seen…from day one of a conflict, sure you have many people who are injured, you have many surgical needs," Alayyan said.
"But the health system will surely collapse in many of these situations and then you run into -- the longer conflict goes on -- the longer children have gone without vaccines, the longer women have gone without prenatal care," she added.
Alayyan said when she was working on the Syria conflict in 2013, there was a big focus on surgery and injuries but not on primary care or chronic diseases.
"What you see is that after a few months, kids are born, they don't have their vaccinations," she said. "Children who were born in a period of time, like say six months, where they haven't had any vaccines, and those are the kids who are gonna grow up who are going to be more prone to getting measles, et cetera, versus the kids who already like one or two who have already gotten around to vaccines."
With adults in Syria, Alayyan said that due to a lack of focus on chronic diseases, and not getting patients their medications or treatments, many started to experience severe health issues.
"So, there has been more of a focus of bringing chronic diseases to the table in emergency operations and emergency humanitarian support," she said.
However, Alayyan said Gaza is a distinct situation because there are no safe zones or places to ago amid intense fighting from Israeli forces.
"The Israeli army has sent out flyers or texts saying 'Leave this area now and go to this [other] area' but then the population goes to that area, and then it's still being bombed," she said. "So there's not actually a safe place for them to go and it's very, very difficult for us as healthcare providers to provide any kind of care when there isn't a safe area where we can actually do that."
Both Alayyan and Weiser spoke about the importance of medical professionals needing to feel they are safe when they are treating patients in conflict zones.
"We can do a lot more when we know that we have access to our population, that we ourselves are protected, that the hospitals and the clinics where we're working are not under fire, and the current conflict, obviously in Gaza, is a case in point for that, but it's not the only one," Alayyan said.
Is An End to Breast Cancer in Sight? A Groundbreaking Vaccine Shows Promise
(CBS News - Ashley Sharp) -- An estimated one in eight women will develop breast cancer in their lifetime, killing on average 42,000 women a year in the United States.
What if there was a vaccine that would significantly lower each woman's chance of ever getting it in the first place? In that question lies what could be the answer to one day eliminating the deadly disease.
A groundbreaking vaccine created through decades of research at the Cleveland Clinic and developed by Anixa Biosciences in San Jose, California is driving innovation by targeting triple-negative breast cancer, the disease's deadliest and most aggressive form.
"This vaccine could potentially eliminate breast cancer," said Dr. Amit Kumar, Anixa CEO.
The vaccine's findings from its first trial with 16 women were published Wednesday, with each participant reporting no bad side effects and no resurgence of their cancer so far.
Jennifer Davis, a brave woman from small-town Ohio, was the first woman in the world to get the vaccine in October 2021.
"This is how we advance medicine. It's important to be a part of those things," Davis said. "I am just beyond grateful."
When Davis heard the dreaded words "you have cancer" in September 2018, it came six months after her first alert to an abnormality on a routine mammogram and ultrasound.
At the time, her biopsy turned up negative for cancer.
"I really wanted to believe everything was OK, but I knew something wasn't right," Davis said.
At 41 years old, she had no history of cancer. Still, she could feel a lump growing and decided to go for a second opinion and a second biopsy.
She was diagnosed with triple-negative breast cancer. Her mind instantly went to her family and three children.
"It was very hard to tell them and try and be strong for them," Davis said. "With triple negative, there is nothing for us to take — no pill or anything to prevent recurrence. The rate is high and outcomes are poor if it does come back."
After chemotherapy, a double mastectomy and radiation, Davis was finally free of cancer, but she was not free of the fear that lingers.
"I was always nervous and afraid of it coming back," she said.
So when she learned of an experimental vaccine trial while receiving her cancer care at the Cleveland Clinic, she thought, "What do I have to lose?"
"It was something that was going to give me peace of mind," Davis said. "If this could work for me, then I wouldn't have to worry about a recurrence."
She became the first woman in the world to take the breast cancer vaccine.
A registered nurse herself, what eased her mind was the fact that in years of trials in animals, there had been no cancer recurrence and no anaphylactic reaction.
"That was all I needed to hear," said Davis, who reports that in the two years since taking the vaccine, she has never felt better.
The vaccine has been studied for more than two decades at the Cleveland Clinic, pioneered by pre-clinical research led by the late Dr. Vincent Tuohy.
Inspired by this and what it could mean for the future of cancer diagnosis, Dr. Kumar approached the clinic about developing the vaccine.
"I looked at it and I saw the vision," Kumar said.
So how does it work?
"Is it, in essence, teaching your body not to grow a tumor?" CBS13 reporter Ashley Sharp asked.
"That's exactly right. It's teaching your body to destroy the cells that can grow a tumor," Kumar said.
If a virus shows up in the body, the immune system teaches itself how to destroy it, knowing, easily, which cells are bad.
In cancer, it is more difficult, Dr. Kumar explained.
"All of the cells that become cancerous in your body came from normal, healthy cells," Kumar said. "The difference is not big, so the immune system has a harder time recognizing a cancer cell and distinguishing it from a healthy cell."
According to the Cleveland Clinic, the vaccine works by targeting a lactation protein called α-lactalbumin, which is no longer found after lactation in normal, aging tissues. It is, however, present in most triple-negative breast cancer patients. If breast cancer develops, the vaccine is designed to instruct the immune system to attack the tumor and keep it from growing entirely.
"The results are incredibly promising," Kumar said. "The vision is one day to be able to give this to any woman who wants to prevent cancer from ever occurring in her body. It's a small step and we have many more steps to go, but it's incredible if we can make this happen."
It's a promising find for the future of fighting cancer that started with one woman but hopefully ends with every woman.
"The bigger picture of this is overwhelming for me," Davis said.
The second vaccine trial is set to start in 2024, this time with 600 women instead of 16. This study will be on a much larger scale, where half the women will get the vaccine and the other half will get a placebo.
The hope is that within five years, they can get FDA approval to distribute the vaccine to the public.
The Science of Swoon! New Discovery May Explain Why People Faint

(NPR - Jon Hamilton) -- A newly discovered pathway between the heart and brain may explain why healthy people faint.
The pathway appears to carry signals from the heart's lower pumping chambers to an area of the brainstem that controls heart rate, blood pressure and breathing, says Vineet Augustine, a neurobiologist at the University of California San Diego.
When scientists stimulate nerve cells along that pathway in mice, Augustine says, "the heart rate immediately dips, they wobble around a little bit and then they fall over."
The finding, published in November in the journal Nature, offers a biological explanation for fainting that isn't caused by an underlying medical condition.
"A lot of people faint at the sight of blood," Augustine says, "or when they're having blood drawn or exposed to a very intense emotional stimulus."
The study also offers a clearer picture of how the brain and body usually work together to keep us from passing out, says Robert Wilson, a neurologist at the Cleveland Clinic who was not involved in the research.
"There's this whole orchestra that responds to how blood is flowing, that tells the heart how to speed up, how much to pump," Wilson says.
Understanding that orchestra has become especially urgent since the arrival of COVID-19. The disease often affects a person's autonomic system, which regulates functions including heart rate, blood pressure and breathing.
In the past, autonomic disorders didn't get much attention, Wilson says. "Then COVID occurred, and a lot of the long COVID patients have autonomic dysfunction, dizziness, fainting, and it's a big deal."
Old science, new understanding
About 40% of people pass out at some point in their lives. Most of the time, there's no medical reason.
Doctors call this sort of fainting vasovagal syncope, and it occurs when there is a sudden drop in heart rate and blood pressure. That reduces blood flow to the brain, which shuts down the circuits that keep us conscious.
Research dating back to the 19th century links this type of fainting to the vagus nerve, a wandering tract that connects the brain to internal organs including the heart, lung and gut.
"But what was not clear was which part of the vagus nerve," Augustine says. "The vagus nerve is big. It's a major highway between the body and the brain."
Scientists once thought the vagus nerve was merely a way for the brain to control internal organs. But studies show it's a two-way street. The gut, for example, can affect the brain.
Augustine's team figured that this might be true of the heart as well.
"We were trying to argue [that] the heart also sends signals back to the brain which can influence its function and behavior," he says.
The team used genetic tools and advanced imaging techniques to study a cluster of sensory neurons in the vagus nerve of mice.
By identifying which genes were switched on in each neuron, the researchers were able to identify a distinct population of cells that hadn't been studied.
Then, using a technology that makes certain tissues transparent, the team showed that these cells form a fiber communication pathway that leads from the heart's ventricles (the lower pumping chambers) to the area postrema, a region of the brainstem best known for its ability to induce vomiting.
The researchers used laser light to stimulate the pathway in mice, which caused not only fainting but several other signs seen in people as they lose consciousness. The mice's pupils would dilate, their eyes would roll back, their breathing and heart rate would slow, and their blood pressure would plummet.
Swooning's many unknowns
Scientists are just beginning to understand how the heart and brain communicate.
For example, it has been less than a decade since researchers explained the baroreflex, which keeps blood flowing to the brain whether we're sitting or standing.
That finding helped Ardem Patapoutian of Scripps Research win a share of a Nobel Prize in 2021. It also has given researchers a target for treatment of conditions that affect the baroreflex.
Augustine once worked with Patapoutian. Now, his team's apparent discovery of a fainting reflex could help patients with other disorders that affect blood flow to the brain.
Wilson agrees.
"This is probably a new door to go through for treatments and for understanding," he says.
Right now, Wilson says, he has limited options when it comes to treating people who become lightheaded or faint.
"Sometimes people just need to avoid triggers," he says, "and sometimes people might need an actual medication."
Often the medication used to prevent fainting simply raises a person's blood pressure. The new study could lead to treatments that more directly address the underlying problem.
NCMS Member Dr. Jonas Swartz Receives Dogwood Award
Jonas Swartz, MD, MPH, Receives Dogwood Award
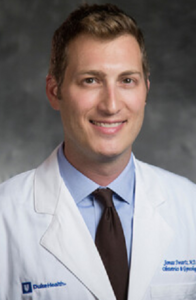
Jonas Swartz, MD, MPH, director of Family Planning at Duke Health, has been awarded a 2023 Dogwood Award by North Carolina Attorney General Josh Stein. These awards are given out annually to recognize people who are working to improve the health, safety and well-being of their fellow North Carolinians. Dr. Swartz was among 34 recipients selected for the recognition. He has been a staunch supporter of women's reproductive rights and has played an integral role in the Duke Reproductive Health Equity & Advocacy Mobilization (DREAM) Team to advocate for policies that preserve and enhance women's health care access.
PAI Research Digest – Special Edition. A Look at Quality of Patient Care at Non-Physician Owned Practices.

PAI partnered with NORC at the University of Chicago to examine the “employed” physician experience—from the impact on patient care, to clinical decision making, to influences and factors driving the growing trend of corporate practice. The survey provides an unprecedented inside look at the shifting physician employment landscape and offers key insights into the implications of the last decade’s dramatic increase in corporations owning physician practices for both patients and physicians.
Among the survey’s broad range of findings, most concerning is that nearly 60% of physicians practicing in hospital- or corporate-owned settings say non-physician ownership reduces the quality of patient care—with more than 80% of these physicians citing reduced autonomy as a driving factor.
Report: The Impact of Practice Acquisitions and Employment on Physician Experience and Care Delivery
PAI and NORC at the University of Chicago | 2023
Key Findings
CARE DELIVERY
Physicians report concerning trends in care delivery, indicating reduced autonomy, strained patient relationships and diminished communication due to ownership changes.
- Almost 60% of physicians reported that reduced autonomy was one of the top negative impacts of ownership changes on patient care quality
- Nearly half of physicians (45%) reported that ownership changes worsened their relationships with patients
Decreased time and communication were reported (80%) as top negative impacts of ownership changes on the physician-patient relationship.
CLINICAL DECISION MAKING
Physician responses underscore the complexities involved in making clinical decisions for their patients, including employers’ policies that influence these decisions.
- 56% of respondents said that cost of care to the patient has some impact on their clinical decision making
- 47% of respondents said that practice policies or incentives led them to adjust treatment options to reduce costs
- 37% of physicians report moderate or low autonomy in making clinical decisions
- 61% of respondents have moderate or low autonomy to refer patients outside of their ownership structure/system
- 70% of respondents report their employer uses incentives for physicians to see more patients
45% of physicians reported policies that influence or limit their decision making on drug therapies for patients
ADMINISTRATION
Two-thirds of physicians report having little or no involvement in practice management policies.
- Over 40% of respondents expressed dissatisfaction with workforce-related issues including hiring, staff management and administrative support
- Respondents expressed high satisfaction with medical equipment (53%), technology training (36%) and the quality of technology/EHR policies and procedures (37%) at their current practice
Interestingly, more than half (52%) of respondents lacked awareness of a formal process to resolve disputes at their workplace
CAREER PATH & EMPLOYMENT TRENDS
Physicians who moved from independent practice to employment cited a myriad of factors that influenced their decisions with work-life balance and compensation ranking the highest.
- Government and private insurer reimbursement cuts were driving factors in choosing employed positions for over half of physicians who responded to the survey (both 53%)
- 60% of respondents stated that their current employer required them to sign a non-compete agreement
Frustrations with current employment are reflected in the 44% of respondents who said they would join a union if available and amongst the compelling reasons they cited for wanting to retire early—burnout (74%) ranked the highest
Are You Ready? Shipping Deadlines Start Next Week!
When is the Christmas shipping deadline for 2023? See the last days to order and mail packages.
The holiday shopping season is in full swing and it won't be long before time runs out on deadlines for mailing Christmas packages. Shippers, as well as retailers, have announced Christmas 2023 cutoff dates for getting gifts to their destinations on time.
USPS Christmas deadline
The United States Postal Service has announced its cutoff dates for deliveries in time for Christmas.
- December 16 is the cutoff for 5-day shipping using USPS Ground Advantage and First-Class Mail services.
- If you pay for 4-day-shipping, you have until December 18 to mail parcels and have them arrive under the tree by Christmas.
- Consumers have until December 21 if they use the USPS's Priority Mail Express 1-day shipping option.
Keep in mind, the USPS won't be delivering regular mail on Christmas Day. And because Christmas Eve falls on a Sunday this year, the last scheduled day for regular USPS delivery is Saturday, December 23.
For Priority Mail Express mail, if a holiday premium is paid, the last scheduled delivery day is Sunday, December 24.
Postage costs vary depending on the type of parcel you are mailing and its destination.
FedEx Christmas deadline
With FedEx, the deadline for mailing Christmas packages also varies depending on the service.
- The last day to ship a package using FedEx Ground Economy services is December 13.
- For FedEx Ground 5-day shipping, it's December 15.
- For 1-day shipping, it's December 21 — the Thursday before the holiday.
FedEx also offers express services that buy last-minute gift-givers more time.
- The last day to ship packages so that they arrive on or before Sunday, December 24 is Friday, December 22, via FedEx SameDay delivery.
All FedEx services, except for FedEx Custom Critical, are closed on Christmas Day.
UPS Christmas deadline
UPS, which is also closed on Christmas, recommends the following deadlines for package deliveries in time for the big holiday.
- Ship gifts by December 19 using UPS's 3-day delivery option, called UPS 3 Day Select, so they'll arrive on December 23.
- Ship by December 21 under UPS Next Day Air services.
- Customers have until December 22 with the shipper's Saturday delivery options.
Major retailers
Some major retailers have announced their own purchase deadlines for timely holiday delivery.
- Bookseller Barnes and Noble says December 16 is the last day for Christmas delivery with its standard shipping option. Expedited shipping lets shoppers purchase gifts online until December19. Picking up items in stores is also an option.
- Order from outdoor retailer REI by 9 a.m. PT on December 19 for Christmas delivery via standard shipping. Pick up goods in-store for faster retrieval.
Where you might want to order even earlier
- Given that it personalizes items, custom card and giftmaker Shutterfly has earlier shipping cutoff dates. If selecting basic economy shipping, Shutterfly's last day to order for Christmas is December 14, to allow for 6-10 days for production and delivery. Visit the site for more details.
- Similarly, many sellers on Etsy, a marketplace where independent makers sell handcrafted goods, make gifts that take time to fabricate and require more lead time to guarantee delivery by Christmas.
(Dates from CBSNEWS.COM)
Planning to Travel Over the Holidays? Here Are the COVID-19 Hot Spots Across the U.S.
The Top COVID-19 Hot Spots in the U.S.
These are the counties with the highest recent rates of new COVID-19 hospital admissions per capita.
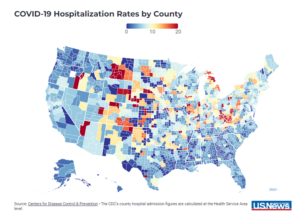
(US News, Christopher Wolf) -- COVID-19 hospitalizations in the U.S. again rose week over week, according to the latest figures from the Centers for Disease Control and Prevention.
The U.S. tallied approximately 19,400 new hospitalizations of people with COVID-19 over the seven days ending Nov. 25, according to provisional data – about 1,700 more than the total for the previous week and a rise of approximately 10%. The uptick marks the third weekly increase in a row after COVID hospitalizations in the U.S. had largely been trending downward since early September, when they totaled about 21,000.
Relative to population, data points to 5.9 new COVID-19 hospital admissions per 100,000 people for the week through Nov. 25. Nearly all states across the U.S. had a “low” level of hospitalizations per 100,000 people, according to the CDC. The exceptions – West Virginia (15.4) and South Dakota (12.0) – were characterized by the CDC as each having a “medium” level of hospitalizations. Compared with the week prior, Indiana had the highest percentage increase among states in its rate of new COVID-19 hospitalizations, at 38%. Alaska saw the largest decrease among states at 21%.
Among patients visiting a subset of emergency departments, data indicates 1.7% of visits nationally involved a COVID-19 diagnosis – a rate up about 11% from the week before. New Mexico (3.9%) and West Virginia (3.4%) saw the highest rates.
Notably, the CDC’s county hospital admission figures are calculated at the Health Service Area level, which can span multiple counties. This means counties within the same HSA will share the same admission rates in the data. Areas also may be listed as having insufficient data.
The counties with the highest rates of COVID-19 hospital admissions per 100,000 people:
- Union County, New Mexico (73.9)
- Letcher County, Kentucky (46.4)
- Richardson County, Nebraska (38.2)
- Pawnee County, Nebraska (38.2)
- Decatur County, Kansas (37.2)
- Hitchcock County, Nebraska (37.2)
- Red Willow County, Nebraska (37.2)
- Sheridan County, Kansas (37.2)
- Greene County, Illinois (36.8)
- Morgan County, Illinois (36.8)
- Scott County, Illinois (36.8)
- Petroleum County, Montana (34.7)
- Fergus County, Montana (34.7)
- Logan County, West Virginia (34.4)
- Mingo County, West Virginia (34.4)
- Pike County, Kentucky (34.4)
- Orange County, Indiana (33.8)
- Lawrence County, Indiana (33.8)
- Adams County, Idaho (31.9)
- Malheur County, Oregon (31.9)
- Washington County, Idaho (31.9)
- Payette County, Idaho (31.9)
- Phillips County, Colorado (31.1)
- Logan County, Colorado (31.1)
- Sedgwick County, Colorado (31.1)
- Knox County, Illinois (27.1)
- Warren County, Illinois (27.1)
Because hospitalization rates are calculated per 100,000 people, it’s worth noting that even a small number of hospitalizations can lead to a relatively high hospitalization rate for small communities.
Other measures also can give a sense of the current state of COVID-19. For example, though the CDC has ceased publishing a "community level" metric that incorporated COVID-19 case rates and hospital admissions – as well as the average percentage of hospital beds occupied by COVID-19 patients – participating health departments submit data from sampling and testing of wastewater for the virus to the CDC via the National Wastewater Surveillance System.
Since the U.S. passed 1 million cumulative deaths tied to COVID-19 in the spring of 2022, approximately 156,000 additional people have died in connection with the disease, according to provisional data from the CDC.
While the latest tallies are down from a recent peak of about 1,400 deaths in a week in September – and well below the maximum peak of around 26,000 deaths in a week in early 2021 – data indicates hundreds of people still have died in connection with COVID-19 of late. West Virginia saw 5.5% of its total deaths attributed to COVID-19 during the week ending Nov. 25, according to provisional data, with an additional 10 states seeing shares higher than the national percentage of 2.5%.
Doctors May Have Identified a Possible New Syndrome in Newborns Linked to Fentanyl Exposure

New syndrome in newborns exposed to fentanyl possibly found
(NBC News, Erika Edwards) -- At least 10 babies — possibly more than 12 — have been identified with what doctors believe to be a new syndrome related to exposure to fentanyl in the womb.
All of the infants have distinctive physical birth defects, such as cleft palate and unusually small heads. No common genetic cause has been uncovered — all were born to mothers who said they'd used street drugs, particularly fentanyl, while they were pregnant.
"This is concerning," said Dr. Elizabeth Cherot, the president of the March of Dimes. "As we see these shared characteristics identified, we may be unroofing a real syndrome." Cherot hasn't personally cared for any of the babies.
Six babies were identified at Nemours Children's Health in Wilmington, Delaware, two in California and one each in Massachusetts and Rhode Island. Erin Wadman, a genetic counselor at Nemours, and her colleagues published their findings recently in Genetics in Medicine Open.
The aha moment linking the infants came in August 2022, when Wadman was called upon to consult in the case of a baby who'd been born with birth defects.
"I was sitting there in the appointment, and I was just like this face looks so familiar. This story sounds so familiar. And I was just thinking about how this patient reminded me so much of a patient I'd seen earlier in the year and then other patients I'd seen," Wadman said. "That's when we were like we think we might have stumbled on something really big here."

In addition to cleft palate, the 10 infants have unusually small bodies and heads. They tend to have drooping eyelids. Their noses tend to turn upward, and their lower jaws are often undersized. Their feet may point down and inward, and two of their middle toes are webbed. Baby boys may have genital irregularities. Some have trouble feeding, and their thumbs may not be fully formed. The physical similarities reminded Wadman and a Nemours colleague, Dr. Karen Gripp, a geneticist, of a syndrome called Smith-Lemli-Opitz. In those cases, genetic variants affect how fetuses process cholesterol, which is necessary for normal cell function and brain development.
None of the babies were found to have the Smith-Lemli-Opitz variant or any others that would put them at risk for such defects, however. Gripp, who is also a pediatrician, and Wadman suspect that fentanyl may be causing similar disruptions to cholesterol metabolism during pregnancy.
"Although fentanyl's effect on cholesterol metabolism has not been directly tested, based on indirect evidence, it is biologically plausible that it affects cholesterol metabolism in the developing fetus," the authors wrote in the new report.
The babies tested positive for fentanyl exposure when they were born, but the Nemours team suspect they had been exposed to significant amounts of the drug throughout the entire pregnancies.
Still, Wadman said much more work is needed to confirm the findings, "even to prove that it is, indeed, the fentanyl and not anything that's laced in it or other drug that we're missing."
Possible causes
No proof yet links fentanyl to the cases, and in fact there are many possible causes. It could be that other street drugs or contaminants in the fentanyl supply are causing the defects. Even mosquito-borne diseases, such as Zika, have been known to lead to microcephaly (unusually small heads) if babies are exposed in utero, though there is no evidence Zika plays a role in the cases.
The women in the study were "also taking many drugs," said Dr. Nora Volkow, the director of the National Institute on Drug Abuse. "It's very hard to determine is this just the effect of fentanyl or is this really the effects of other drugs or other combination?"
"Having said that, reports like this one are very important, because they shed light on issues that we need to systematically investigate," Volkow said.
Last year, NIDA launched a large research project called the Healthy Brain and Child Development Study aimed at following women and their children from pregnancy through age 10. "It's a prospective study to evaluate consequences of drug exposures during pregnancy," Volkow said.
The fentanyl-cholesterol theory may be proven — or not — through ongoing work at the University of Nebraska Medical Center in Omaha.
Dr. Karoly Mirnics, the director of UNMC's Munroe-Meyer Institute, has dedicated research to studying the impact of a variety of drugs on cholesterol metabolism.
That is because cholesterol is "essential for everything in your body, for every cell membrane, for every function," Mirnics said. "If there is no cholesterol, there is no life."
Mirnics plans to study the blood of the babies identified at Nemours and elsewhere to answer looming questions:
- Is the underlying cause fentanyl or some kind of contamination of the drug?
- Does it depend on how much fentanyl gets to the fetus?
- Is the problem some kind of interaction between the drug and genetics of either the mother or the baby?
- Why would some babies exposed to fentanyl or other drugs during gestation develop defects while others don't?
"I have no idea," Mirnics said, "but I'm going to figure it out."
More cases?
While fentanyl use has skyrocketed in recent years, even among pregnant women, there is no indication that birth defects are rising.
About 3% of babies are born every year with birth defects, according to the National Center for Birth Defects and Developmental Disabilities at the Centers for Disease Control and Prevention. The group declined to comment on the Nemours research.
"We haven't seen this specific syndrome, but babies [exposed to fentanyl] are often born growth-restricted, smaller than they need to be," said Dr. Brian Smith, the Samuel L. Katz distinguished professor of pediatrics at Duke University Medical Center in Durham, North Carolina. They are "profoundly irritable" and often don't eat or sleep well, he said.
The new findings from Nemours have prompted other experts to take another look at babies who may have been similarly affected.
Dr. Howard Saal, a clinical geneticist at Cincinnati Children's and the University of Cincinnati, believes he has seen two babies "fairly recently" with the same birth defects who were exposed to street drugs in utero.
"Their pattern of anomalies fits very closely with what has been described in this report," Saal said. "I may have seen more cases in the past but didn't put 2 and 2 together."
And Dr. Ahmed Ahmed, a medical geneticist in the department of Maternal Fetal Medicine at the Cleveland Clinic, believes he, too, has seen cases. But complications related to drug use during pregnancy are "invisible," he said. "There is no ultrasound or blood test that we can do to determine the impact an exposure may have had on the fetus."
"We see similar anomalies, and we go the whole nine yards with diagnostic testing. But the results come back negative," Ahmed said. "Deep down inside, you think that it is related to the substance abuse, the fentanyl or others, but you are unable to prove it."
Ahmed said he and his team are amenable to sharing notes with the Nemours team to further the research. For now, he will use the information to counsel women, ideally before they become pregnant.
"I can use this paper to highlight that there is a potential risk for structure defects," Ahmed said.
Dr. Sonja Rasmussen, a medical geneticist at Johns Hopkins School of Medicine in Baltimore, praised the "astute clinicians" at Nemours for first noticing what could be an important trend.
"That's how fetal alcohol syndrome was recognized. That is how isotretinoin [the acne medication Accutane] that causes a distinct pattern of birth defects was recognized," said Rasmussen, one of the first to describe the defects associated with Zika virus while she was at the CDC.
The best 'yes'
Lindsay Carlisle, 40, of Washington Township, New Jersey, knew exactly what she was seeing when she first laid eyes on little Sammy in July 2021. He'd been born nearly two months earlier, addicted to opioids, and he had other medical problems. Carlisle had been called in as a possible foster parent, but she felt right away that Sammy would become her adoptive son.

"Initially, we never were on board with having a medically complex child, just because we didn't think we could handle it. We weren't really equipped," Carlisle said. "But then I said 'yes,' and it was the best 'yes' I've ever said."
Now 2 years old, Sammy requires large amounts of therapy. He faces several developmental and physical delays. His joints aren't well-formed, Carlisle said, and he lacks hand strength. He isn't yet talking, but he can make sounds. He depends on a feeding tube to eat. He has required a procedure to correct a heart defect.
His case is one of the 10 described in the Nemours report.
A public health crisis
If the syndrome is linked to in utero fentanyl use, it appears to be rare.
Dr. Stephen Patrick, a neonatologist and the director of the Vanderbilt Center for Child Health Policy in Nashville, Tennessee, said he has never treated such a patient. He has, however, cared for many babies born addicted to fentanyl and other drugs — all without the physical defects described in the new report.
That doesn't mean fentanyl use during pregnancy, especially from drugs obtained illegally, is safe. It is associated with preterm birth, stillbirth and neonatal abstinence syndrome.
It's clear, Patrick said, that substance abuse during pregnancy is dangerously common, having reached new highs during the coronavirus pandemic.
"Pregnant women are dying at record rates. Infants are the fastest-growing group entering foster care, mostly for parental substance use. The minority of pregnant women are getting into treatment," Patrick said. "This is a big public health crisis."
The path ahead
Researchers will continue to follow the babies over time. The oldest is now 3 years old. Further research may show that a subset of infants has some kind of underlying genetic risk that made them more susceptible to in utero fentanyl exposure.
The hope is to move genetics research forward.
"For most babies that are born with a birth defect, we don't know the cause," Rasmussen said. "Every time we can get a little bit closer to understanding what's going on, it's really helpful for families to understand their chances of this happening again in future pregnancies."

Meanwhile, the newly identified syndrome means children like Sammy have unclear paths moving forward.
"We don't really know exactly what this means for him, cognitively, because there is no one there to say, well, this is what happened and this is what they did," Carlisle said. "We're just kind of winging it."
She hopes to meet other families in the Nemours research group. The Carlisles officially adopted Sammy in February.
"I promised him I would give him the very best life that anyone could ever want from the day I met him," Carlisle said. "He's just magical."
Dr. Mandy Cohen: The Threat of Respiratory Illnesses is Underway and Hospitalizations Are on the Rise

(CNN) -- Dr. Mandy Cohen, director of the US Centers for Disease Control and Prevention, updated a congressional subcommittee Thursday about cases of respiratory illness in the US due to three viruses: flu, the coronavirus and respiratory syncytial virus, or RSV.
“RSV season is in full swing,” Cohen told the House Energy and Commerce Subcommittee on Oversight and Investigations.
“Flu season is just beginning across most of the country, though accelerating fast, and while we’re seeing relatively low levels of Covid, Covid is still the primary cause of new respiratory hospitalizations and deaths, with about 15,000 hospitalizations and about 1,000 deaths every single week,” she said.
“We are seeing a lot of RSV, particularly in the southern part of the country, so we’re near peak is what I would say for RSV,” Cohen said.
“We are also at the beginning of flu season,” she said. “We’re actually having a pretty, what I would say, typical flu season. We do expect to see a lot more flu cases over the course of December and January.”
Covid is also rising again and continues to be the biggest threat of the three, she said.
“Covid is still the respiratory virus that is putting the most number of folks in the hospital and taking their lives,” she said.
Cohen added that it remains important for Americans to get vaccinated, since there are now vaccines against all three of these respiratory illnesses. Should a person get sick, it’s also critical to be tested and get treatment, as most antiviral drugs are most effective when given early in an infection.
More than a third of adults and children have gotten their flu shot this year, according to the latest data from the CDC. But only about 16% of adults and 6% of children have gotten the new Covid-19 vaccine, rates that the CDC has said are lower than it would like to see. About 15% of older adults 60 and up have gotten the new RSV vaccine.
Respiratory virus activity is especially high in the Southern and Western US. Warren County in Ohio said this week that it’s experiencing an “outbreak” of pediatric pneumonia cases, with a large uptick in the number at one time. The pathogens involved include adenovirus, Streptococcus pnuemoniae and Mycoplasma pneumoniae, bacteria that have been linked to a rising number of respiratory infections in China. Mycoplasma commonly causes mild respiratory infections, typically in crowded settings like schools, college residence halls and long
Respiratory virus season is especially affecting children. In the week ending November 18, more than 10% of doctor’s visits among children younger than 5 in the US were for influenza-like illnesses – about three times higher than the average for all ages and well above the national baseline, according to data from the US Centers for Disease Control and Prevention.
Pediatric hospital beds are filling up, too. About three-quarters of pediatric hospital beds are in use nationwide, federal data shows, and capacity hasn’t been this strained since mid-December 2022.
Hospitalizations for respiratory viruses – including Covid-19, flu and RSV – have been on the rise for months. Although Covid-19 represents the vast majority of respiratory virus hospitalizations overall, RSV is the most common culprit among children, with weekly admission rates rising 69% since the first week of October.