NC Controlled Substances Reporting System Launches Clinical Alert Program

In December, the NC Controlled Substances Reporting System (NC CSRS) launched clinical alerts, which notify prescribers when a patient has met or exceeded one or more high-risk thresholds.
An alert is triggered when a patient fills controlled substance prescriptions written by 7+ prescribers and filled at 7+ pharmacies within 3 months.
It's important to note that an alert does not indicate illegal or inappropriate behavior. It should be used as a conversation starter to better understand the patient’s specific situation and/or needs.
Learn more about the NC CSRS clinical alert program here.
Norovirus Outbreaks on the Rise Nationwide

According to data from the Centers for Disease Control and Prevention (CDC). Norovirus, a common stomach bug, is surging.
Norovirus is a very contagious virus that causes vomiting and diarrhea. It is sometimes called the "stomach flu" or the "stomach bug." However, norovirus illness is not related to the flu. The flu is caused by the influenza virus. Norovirus causes acute gastroenteritis, an inflammation of the stomach or intestines. Most people with norovirus illness get better within 1 to 3 days.
Anyone can get infected and sick with norovirus. If eaten raw, oysters and other filter-feeding shellfish can contain viruses and bacteria that can cause illness or death. Anyone who consumes raw shellfish is at risk of contracting norovirus. Children younger than 5 years old, older adults, and people with weakened immune systems are more likely to develop severe infections.
Norovirus spreads very easily and quickly in different ways:
- Having direct contact with someone with norovirus, like caring for them, sharing food or eating utensils with them, or eating food handled by them.
- Eating food or drinking liquids that are contaminated with norovirus.
- Touching contaminated objects or surfaces and then putting your unwashed fingers in your mouth.
Take these steps to protect yourself and others from Norovirus:
- Wash your hands well and often.
- Cook shellfish thoroughly and wash fruits and vegetables.
- Clean and disinfect contaminated surfaces.
- Wash laundry in hot water.
- Stay home when sick for 2 days (48 hours) after symptoms stop.
Join Us in Fayetteville for the Next NCMS Regional Meeting!
Feeling More Like a Factory Line Worker Than a Health Care Professional???
Join North Carolina Medical Society members and staff to learn ways NCMS is working to put YOU back in health care decision making!
Luigi's Italian Chophouse and Bar
528 N McPherson Church Road
Fayetteville, NC 28303
Thursday, January 16
6-8pm
Here's what you can expect:
- Complimentary drinks, food and socializing with your colleagues
- An overview on ways NCMS is fighting for physicians and PAs
- Time for You to share solutions, concerns, and ask questions
REGISTER NOW
Physicians, PAs, Residents, and Students
You do not need to be a member to register.
Questions? Contact Toni Hill, [email protected].
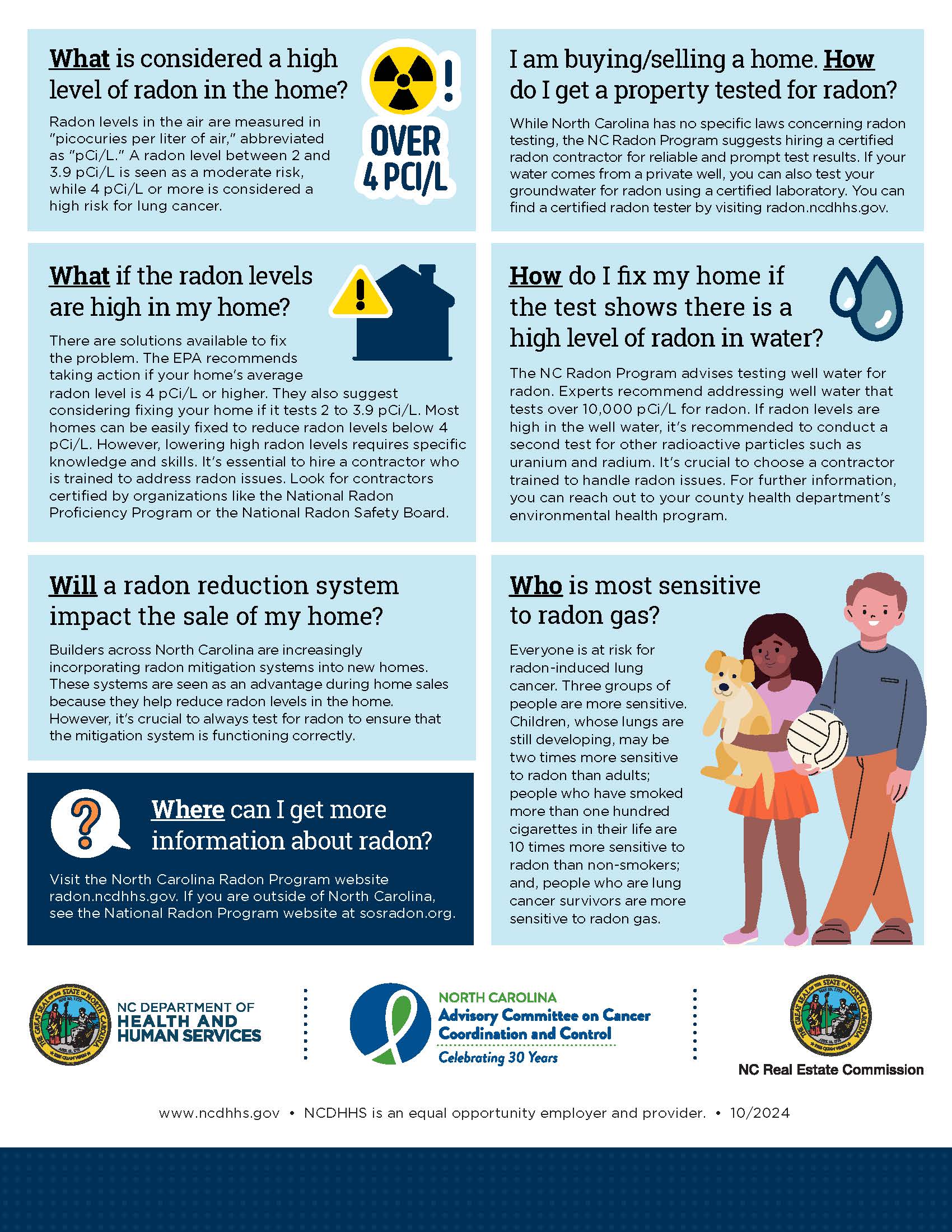
Free Residential Radon Test Kits Now Available! Take Action for Radon Action Month!
In recognition of National Radon Action Month, the North Carolina Department of Health and Human Services is providing 2,000 free radon test kits available beginning January 1, 2025, at radon.ncdhhs.gov. Radon exposure is preventable, and testing is the only way to know if you or your family is at increased risk.
Radon is an odorless, colorless gas released from the ground into outdoor air but can accumulate and reach harmful levels when trapped in homes and other buildings. Radon is responsible for approximately 450 deaths annually in North Carolina, and radon exposure is the number one environmental cause of lung cancer statewide.
"Everyone in North Carolina, from the coast to the mountains, is exposed to some level of radon," said Phillip Gibson, NC Radon Program Coordinator. "The question is not if you are exposed, but whether the level of exposure could be dangerous to your health. Testing for radon is the only way to know."
To support increased radon testing and mitigation, NCDHHS recently published a collection of data to help North Carolinians understand the risk of radon in their communities. Recent data show more than three-quarters of all North Carolina counties have elevated levels of radon present. A level of four picocuries per liter (pCi/L) or higher in your home is considered unsafe. County-level data and recommendations are available on the NCDHHS radon webpage.
Statewide surveys also reveal radon impacts different communities at differing rates. White people are 30% more likely to know about radon than their non-white peers. Efforts are underway to increase equitable awareness through outreach to community organizations and through additional resources available in 16 different languages.
The 2023 North Carolina State Health Improvement Plan and North Carolina Cancer Control Plan includes reducing radon exposure through testing and mitigation as a key strategy to improving life expectancy in North Carolina. In addition to providing free radon test kits and observing Radon Action Month, the department will continue to work to increase education and awareness in communities across the state to ensure people take appropriate action to protect themselves and their families from dangerous levels of radon.
Visit radon.ncdhhs.gov for more information and to order your free test kit while supplies last. Limit one test kit per household. For more information on radon mitigation, visit the NCDHHS radon mitigation webpage.
RELATED READING
What You and Your Patients Should Know About Radon
Grant Opportunity: Telehealth Infrastructure Grant Program

The NC Office of Rural Health has released Wave 2 of the Telehealth Infrastructure Grants funding opportunity!
In Session Law 2023-134, the North Carolina General Assembly (NCGA) appropriated $5,000,000 in SFY 2024 and $15,000,000 in SFY 2025 in receipts (State funds) from the ARPA Temporary Savings Fund to the Office of Rural Health (ORH) in the Department of Health and Human Services to provide competitive grants to rural healthcare providers for Telehealth related items including:
- equipment
- high-speed internet access
- telehealth-related training to staff and patients
- technology equipment to patients
- internet service support for patients to help facilitate telehealth access*
- other infrastructure needed to establish telehealth services
*Eligible rural healthcare patients can benefit from internet service and associated equipment rentals, including modems, routers, and hotspot devices through the Telehealth Infrastructure grant. To receive this support, patients must meet at least one of the eligibility criteria defined below:
- Total household income that is at or below 200% of the federal poverty guidelines or,
- Participation in any ONE of these government benefit programs:
- Lifeline
- Supplemental Nutrition Assistance Program (SNAP)
- Medicaid
- Federal Public Housing Assistance (FPHA) (including Housing Choice Voucher (HCV) Program (Section 8 Vouchers), Project-Based Rental Assistance (PBRA)/202/811, Public Housing, and Affordable Housing Programs for American Indians)
- Veterans Pension and Survivors Benefit
- Supplemental Security Income (SSI)
- Free and Reduced-Price School Lunch or Breakfast Program including through the USDA Community Eligibility Provision
- Federal Pell Grant (current award year)
- Special Supplement Nutrition Program for Women, Infants, and Children (WIC)
Priority will be given to independent primary care practices and independent obstetrics and gynecology (OB-GYN) practices.
For more information, eligibility, and other requirements, click here. Deadline to apply is Friday, January 31, 2025.
Mark Your Calendar! Saving Time: Practice Innovation Boot Camp

This two-day, in-person AMA STEPS Forward® Innovation Academy boot camp is specifically designed for clinical and operational change agents looking to eliminate unnecessary work and free up more time to focus on what matters most–patient care.
Gain proven tools to implement in the following areas:
- Getting rid of stupid stuff
- De-implementation (STOP this and START that)
- Debunking regulatory myths
- EHR inbox optimization
- Team-based care practice fundamentals
- Building bridges between clinicians and administrators
- Reducing barriers to taking PTO
- Making the business case to leadership
Through breakout sessions, interactive activities, thought sharing, tactical strategy breakdowns and how-to examples, this boot camp will equip attendees with the time-saving tools and strategies needed to reform their organizations and enhance professional satisfaction.
Don’t miss this opportunity to gain best practices from top physician experts, network with like-minded peers, engage in cross-sector collaboration, and learn from each other’s successes and mistakes.
Space is limited. Learn more, including how to register, here.
Funding Opportunity: Collaborative Care Management
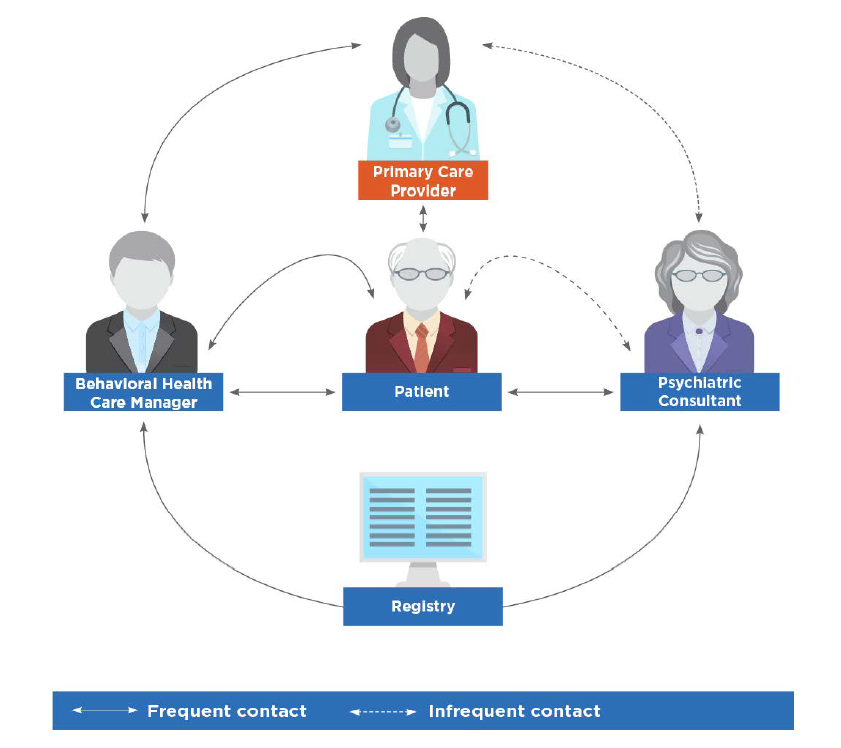 image credit: American Psychiatric Association
image credit: American Psychiatric Association
On behalf of the North Carolina Department of Health and Human Services (NCDHHS), Community Care of North Carolina (CCNC) is accepting applications for the Collaborative Care Management (CoCM) capacity building funding for primary care practice entities.
Collaborative Care Management (CoCM) is an evidence-based behavioral health integration model designed to support primary care clinicians as they assess and treat patients with mild to moderate behavioral health conditions.
CoCM improves patient outcomes, increases satisfaction for both patients and providers, and reduces healthcare costs and stigma related to mental health and substance use disorders. The model complements other integrated models, including the North Carolina Psychiatric Access Line (NC-PAL).
The NC General Assembly has allocated $5 million for capacity building of Medicaid-enrolled primary care practices across the state to adopt CoCM. NCDHHS is contracting with Community Care of North Carolina (CCNC) to manage the CoCM Capacity Building award program in partnership with NC AHEC. The goal is to increase access to evidence-based behavioral healthcare for primary care practices and their patients through the use of the CoCM model.
For more information and how to apply, visit the Community Care of North Carolina Collaborative Care Management Capacity Building Fund Application.
If you are a primary care entity serving Medicaid patients and are interested in learning about CoCM and related capacity building fund opportunities, we invite you to watch the recorded webinar from October 30, 2024 for an overview, here.
Hurricane Helene Note: CCNC is keenly aware that some practices in Western North Carolina are still recovering from the storm and may find it difficult to apply for funds at this time. Efforts will be made to ensure that practices impacted by the hurricane will still have an opportunity to apply for inclusion in the program.
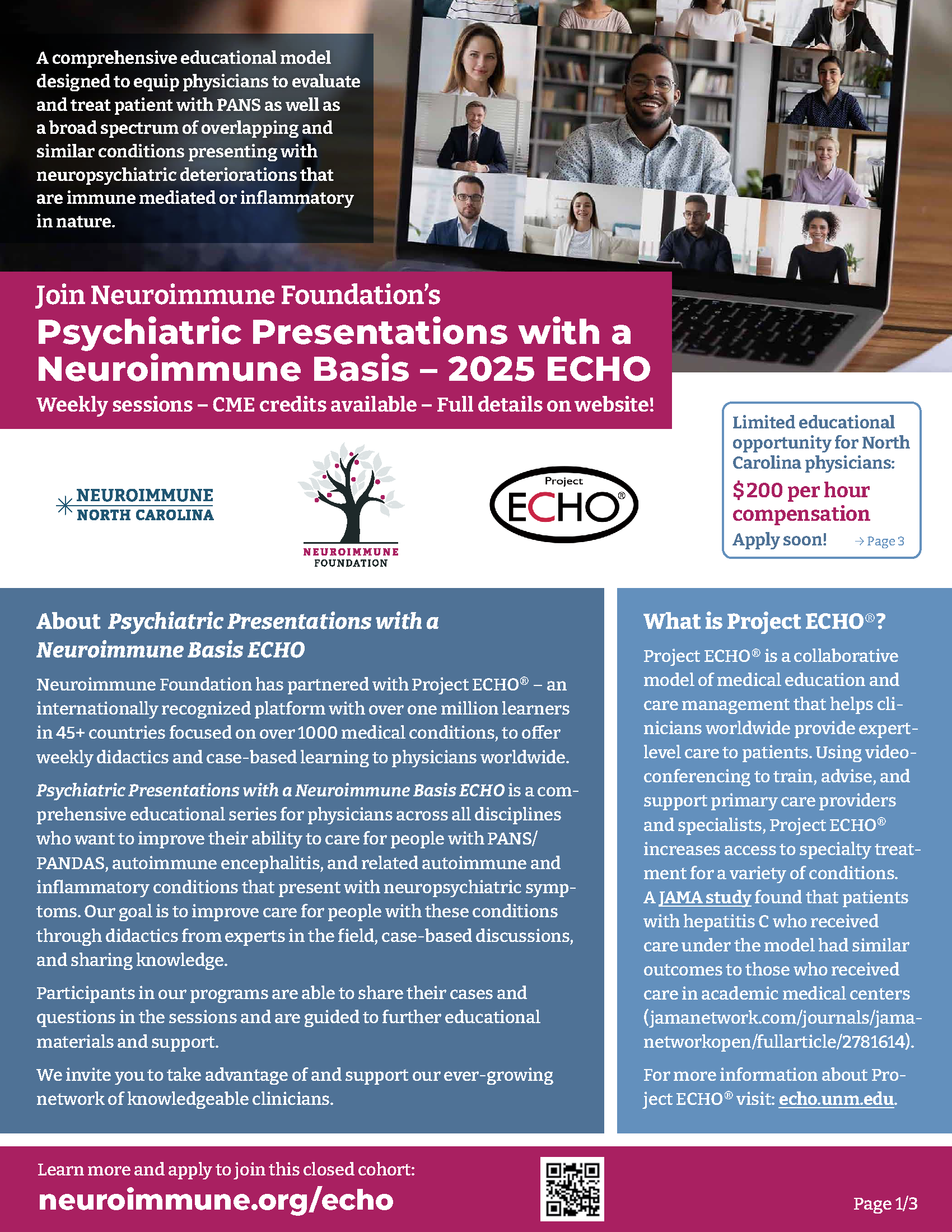
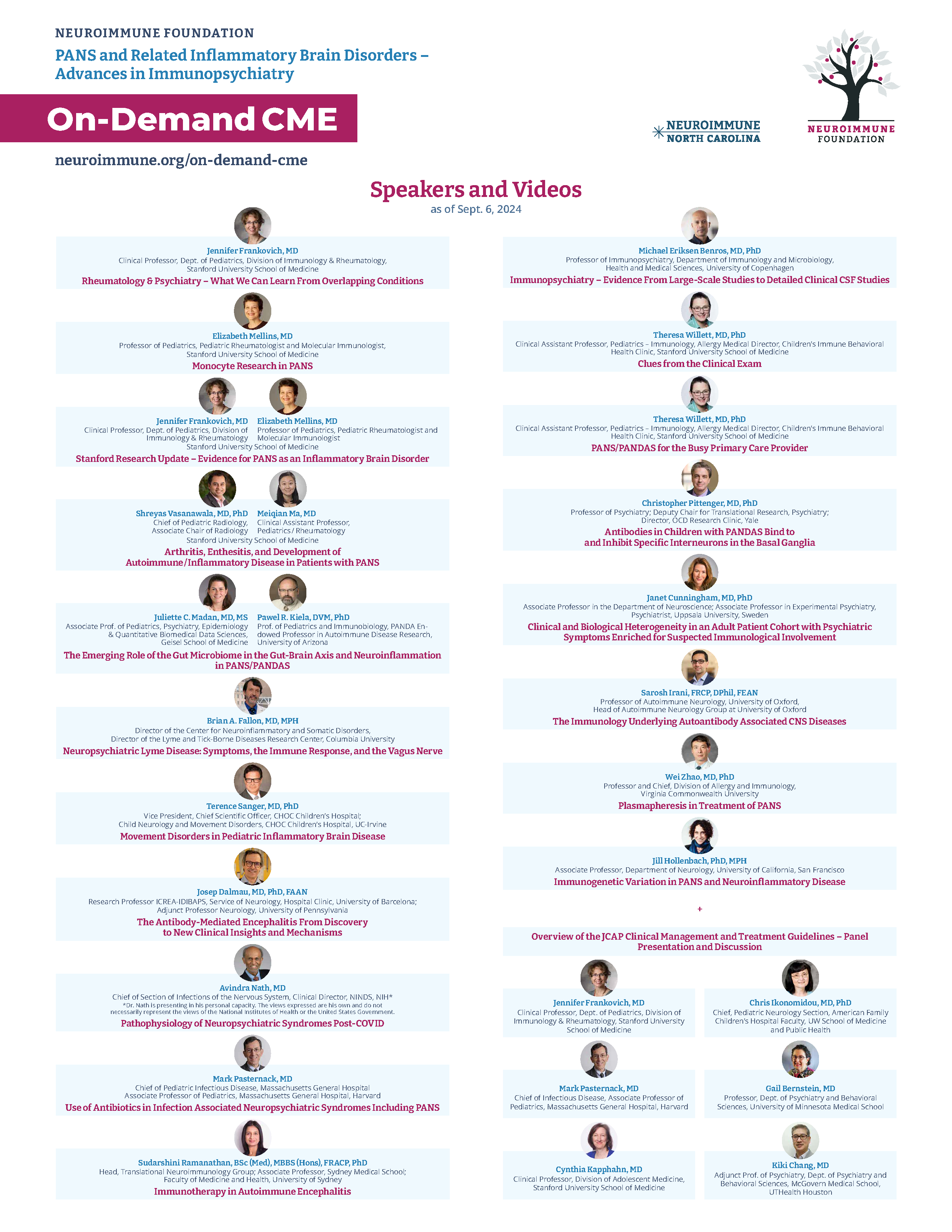
Register Now! Psychiatric Presentations with a Neuroimmune Basis ECHO
Neuroimmune Foundation has partnered with Project ECHO® – an internationally recognized platform with over one million learners in 45+ countries focused on over 1000 medical conditions, to offer weekly didactics and case-based learning to physicians worldwide.
Download the pdf document here.
Register here.
New Tool Helps Practices Track Fee-for-service and Value-based Financial Performance
NC AHEC Practice Support developed a new Financial Health Scorecard for your practice. The scorecard is intended for practices in need of a no-cost resource to track their fee-for-service and value-based financial performance, and prioritize strategic opportunities for improvement. Practice Support coaches are available to assist with training, and any identified opportunities for quality improvement, EHR/HIE optimization and workflow optimization based on best practices for your specialty.
If you need assistance from a Practice Support coach, please contact us at [email protected].
Diabetes Performance Improvement in Primary Care

This self-paced educational activity aims to inform the learner about the status of diabetes and chronic kidney disease in primary care. This activity will explore barriers and facilitators to promote patient engagement in treatment. This activity will focus on performance improvement methods and activities which promote health among patients with diabetes.
Medicare Payment Cut Impact Survey Results Are In!

Medicare Payment Cut Impact Survey Results
Over the two-week period of November 14-28, 2024, the North Carolina Medical Society surveyed physicians across North Carolina regarding the 2.8% Medicare physician payment cut scheduled to take effect on January 1, 2025. Just under 500 responses were received. The initial data from the responses, summarized below, accentuates the dire situation that will result from another cut in Medicare physician payment.
The NCMS continues to advocate for a positive adjustment to Medicare payment for 2025 and has joined many state and national partner societies in an appeal to Congress to at least avert the impending cut.
Survey Results
- Are you enrolled as a Medicare provider?
Yes – 92.5%
No – 7.5%
If Medicare payment kept up with inflation, would you become a participating Medicare provider?
Yes – 11%
No - 37%
- How will another Medicare payment cut affect your practice?
| I will reduce the number of appointment slots for existing Medicare patients | 36.0 % |
| I will continue to see existing Medicare patients but not accept new Medicare patient | 23.5 % |
| I will discontinue seeing Medicare patients (unenroll) | 3.5 % |
| No change | 3.5 % |
| Unsure | 1.0 % |
| Other (see below) | 32.5 % |
“Other” / Comments:
“Will make it difficult to hire new staff to meet the increasing demands.”
“There will be longer wait times for patients to be seen.”
“Will do the best i can as a physician.”
“I will retire from practice. This is not sustainable.”
“We turn no one away but still need to keep the doors open. These consistent cuts are not making it easy.”
“Will affect payment for Medicaid”
“We are still evaluating the situation but all of the above are possible”
“Longer waits”
“I will close or leave my rural practice or have to move to a larger corporation that can handle the cuts”
“I may have to stop practicing”
“I will do the best I can, if cost too much will have to cut back on all, already 2-3 week wait”
“I will continue to take care of my Medicare patients at my personal cost”
“I will have to retire. I am just breaking even with Medicare and can no longer afford to stay in business.”
“Medicare cuts will influence private insurance reimbursements and therefore cutting ALL insurances is a risk”
“I may have to close my practice completely”
“Will make it harder to stay in business and seeing all Medicare patients”
“We are urgent care. Have yet to decide”
“It will cost the hospital that supports my practice”
“All of our MD's are taking a pay cut due to declining Medicare reimbursement”
“Affects financials significantly”
“Will greatly decrease number of slots for Medicare new patients”
“Do not have an option but will be very disheartening for future”
- What practice operation factors are impacted by Medicare payment?
| Ability to meet operational expenses (overhead, payroll) | 62.0 % |
| Ability to implement system/tech upgrades | 48.0 % |
| Ability to hire/retain staff | 47.0 % |
| Ability to recruit physicians to join the practice | 44.0 % |
- Medicare payment rates impact other payment rates (Medicaid, State Health Plan, Tricare). Will a cut in Medicare payment result in a reduction in your other patient populations . . .
Medicaid
Yes 76 %
No 24 %
State Health Plan
Yes 67 %
No 33 %
Tricare
Yes 65 %
No 35 %
U.S. Life Expectancy Hits Highest Level Since Pandemic

U.S. life expectancy rose last year, hitting its highest level since the beginning of the Covid pandemic, according to a report from the Centers for Disease Control and Prevention.
The report, released Thursday, found that life expectancy at birth was 78.4 years in 2023. That's a significant rise — nearly a full year — from the life expectancy of 77.5 years in 2022.
From 2019 to 2021, U.S. life expectancy dropped from 78.8 years to 76.4.
"The increase we had this year — the 0.9 year — that's unheard of prior to the pandemic," said Ken Kochanek, a statistician at the National Center for Health Statistics who co-authored the report.
“Life expectancy in the United States never goes up or down any more than one- or two-tenths,” he said. “But then when Covid happened, you had this gigantic drop, and now we have a gigantic drop in Covid. So, you have this gigantic increase in life expectancy.”
Covid deaths fell significantly last year: Whereas Covid was the fourth leading cause of death in 2022, it was the 10th in 2023, according to the new report. Last year, Covid was the underlying or contributing cause of more than 76,000 deaths, according to an August CDC report, compared with more than 350,000 such deaths in 2020.
For the full article, click here.
Submit Your Comments: DHHS Clinical Policy Change

The Division of Health Benefits (DHB), Clinical Policy Section, is revising Clinical Policy 2A-1 Acute Inpatient Hospital Services and is soliciting input prior to making changes to the policy.
North Carolina Medicaid Direct is proposing the following revision:
• Changing readmission review timeframe from 72 hours to 30 days
You can review the posted policy here.
Please submit your comments here by January 3, 2025.
NC Expands and Professionalizes Family Peer Support for Families of Children with Complex Behavioral Health Needs

The North Carolina Department of Health and Human Services today announced a $4 million investment to expand and professionalize family peer support services statewide. This initiative is designed to improve outcomes for children and families by ensuring that families navigating complex systems have access to support and guidance from someone who truly understands their journey. The investment will strengthen the behavioral health workforce by offering support for 40 new Certified Family Peer Specialists that combined will help nearly a thousand families each year.
Family peer support partners are parents, caregivers or family members with lived experience raising children with behavioral health challenges. These trained professionals help families navigate systems such as behavioral health, education, child welfare and juvenile justice, while also advocating for and connecting the families they serve to critical services and supports.
“Family peer support is about meeting families where they are with compassion and expertise,” said NCDHHS Deputy Secretary for Opportunity and Well-Being Susan Osborne. “This investment will help us build a highly trained and certified workforce of family peers who can provide critical guidance and support to families navigating the behavioral health system.”
NCDHHS is partnering with UNC Greensboro (UNCG) to implement the initiative under the umbrella of the UNCG NC Youth and Family Voices Amplified program. UNCG NC Voices Amplified is a statewide initiative that trains individuals with lived experience to become family and youth peer support partners and assists provider agencies in integrating family partners with the services they provide. UNCG will conduct evaluations to assess the new initiative’s impact, including tracking families’ progress and satisfaction with family peer support services.
Participants will be credentialed through the National Federation of Families as Certified Family Peer Specialists, ensuring a high standard of training and professionalism. These efforts aim to transform family peer support in North Carolina into a funded professional position, helping to create a new trauma-informed, family-focused service area within the behavioral health workforce.
“Family and youth peer support is an evidence-informed practice that improves health outcomes, while reducing overall costs of services,” said UNCG NC Voices Amplified project director Willow Burgess-Johnson. “Family peer support partners improve quality of life for those struggling with behavioral health issues and for the people who love and care for them. We’re so excited to see this important support become increasingly accessible for North Carolinians.”
By investing in family peer support, NCDHHS aims to:
- Reduce need for out-of-home placements for children with complex behavioral health needs
- Support reunification and permanency for children and families involved in the child welfare system
- Decrease the number of nights children spend in emergency departments waiting for an appropriate placement or treatment option by connecting more families to community-based supports
- Build a strong behavioral health workforce that reflects and understands the unique challenges faced by families of children with complex needs
- Empower families to advocate for themselves and their children
This initiative is part of the department’s broader $835 million investments in behavioral health, including $80 million in services to transform the child behavioral health system and improve outcomes for children and families with complex behavioral health needs. The goal is to create an integrated system of care in North Carolina’s homes, communities and schools to ensure children have access to the level of care they need, helping to prevent crisis and keep children with their families whenever safely possible. The department continues to invest in a continuum of services that expand equitable access to high-quality, trauma-informed, family-centered care.
To learn more about family peer support, visit the NC Youth and Family Voices Amplified FAQ page. [source]
CDC Confirms First Severe Case of H5N1 Bird Flu in US

A patient has been hospitalized with a severe case of avian influenza A(H5N1) virus ("H5N1 bird flu") infection in Louisiana. This marks the first instance of severe illness linked to the virus in the United States. The case was confirmed by the Centers for Disease Control and Prevention (CDC) on Friday, December 13. Since April 2024, there have been a total of 61 reported human cases of H5 bird flu reported in the United States.
Partial viral genome data of the H5N1 avian influenza virus that infected the patient in Louisiana indicates that the virus belongs to the D1.1 genotype related to other D1.1 viruses recently detected in wild birds and poultry in the United States and in recent human cases in British Columbia, Canada, and Washington state. This H5N1 bird flu genotype is different than the B3.13 genotype detected in dairy cows, sporadic human cases in multiple states, and some poultry outbreaks in the United States. Additional genomic sequencing and efforts to isolate virus from clinical specimens from the patient in Louisiana are underway at CDC.
While an investigation into the source of the infection in Louisiana is ongoing, it has been determined that the patient had exposure to sick and dead birds in backyard flocks. This is the first case of H5N1 bird flu in the U.S. that has been linked to exposure to a backyard flock. A sporadic case of severe H5N1 bird flu illness in a person is not unexpected; avian influenza A(H5N1) virus infection has previously been associated with severe human illness in other countries during 2024 and prior years, including illness resulting in death. No person-to-person spread of H5 bird flu has been detected. This case does not change CDC's overall assessment of the immediate risk to the public's health from H5N1 bird flu, which remains low.
This case underscores that, in addition to affected commercial poultry and dairy operations, wild birds and backyard flocks also can be a source of exposure. People with work or recreational exposures to infected animals are at higher risk of infection and should follow CDC's recommended precautions when around animals that are infected or potentially infected with H5N1 avian influenza virus. This means that backyard flock owners, hunters and other bird enthusiasts should also take precautions.
The best way to prevent H5 bird flu is to avoid exposure whenever possible. Infected birds shed avian influenza A viruses in their saliva, mucous, and feces. Other infected animals may shed avian influenza A viruses in respiratory secretions and other bodily fluids (e.g., in unpasteurized cow milk or 'raw milk').
- As a general precaution, whenever possible, people should avoid contact with sick or dead animals, in particular wild birds, and poultry.
- For individuals with direct/close contact with wild birds or sick or dead poultry or other animals, wear recommended personal protective equipment (PPE). Wild birds can be infected with avian influenza A viruses even if they don't look sick.
- Do not touch surfaces or materials (e.g., animal litter or bedding material) contaminated with saliva, mucous, or animal feces from wild or domestic birds or other animals with confirmed or suspected avian influenza A virus infection.
For more information on H5 bird flu in the U.S. and CDC's response, including regularly updated case counts, visit the H5 Bird Flu: Current Situation page. [source]
NCMS Recognizes NCMS Disaster Relief Fund Contributors

A heartfelt THANK YOU to these individuals and organizations for their contribution to the NCMS Disaster Relief Fund. Your generous donation is far more than just a financial contribution; it’s a lifeline for the many affected by Hurricane Helene, and vital in providing support to healthcare professionals and communities impacted by this disaster.
We invite you to spread the word about the NCMS Disaster Relief Fund and stay engaged with us as we work together to help restore our Western North Carolina neighbors.
We are grateful to have you in our community!
- American Medical Association Foundation
- Ana Ayala
- Katherine Beavers
- Sandeepkumar J. Gupta, MD
- Portia Marsh
- Physicians East, PA
- Bangladesh Medical Association of North Carolina
- Rebecca S. Carlin, MD
- Carolina Complete Health Inc.
- Anonymous
- James M. Provenzale, MD
- Moulton Family Fund
- Puraven Beauty and Wellness
- UBS Financial Services, Inc.
- Donald P. Wilcox
- American Medical Association Foundation
- Atlantic Internal Medicine
- Amar M. Amaresh, MD
- Edwin C. Bartlett, Sr., MD
- Deanna M. Boyette, MD
- Edwin K. Burkett, MD
- Cobb County (GA) Medical Society
- John A. Fagg, MD
- Barbara Hodde
- Martha G. Peck, MD
- Gary Price, MD
- Eugene E. Wright, Jr., MD
- Kathy F. Wright
- Curi
- Anonymous
- Christopher T. Grubb, MD
- Lyndon K. Jordan, III, MD, FACR
- Katie Lowry, MD, MPH
- Laura J. Luckadoo, MD
- Robeson Pediatrics
- Kirby Sheridan
- Catherine L. Sotir, MD
- Vinod C. Vallabh, MD
- Ian D. Archibald, MD
- Preecha Bhotiwihok, MD, MPH
- John W. Black, MD
- Anonymous
- Gay M. Bowman
- Georgi N. Brockway, MD
- Michael T. Brohawn
- Anonymous
- Carolina Complete Health Network
- Sharon M. Foster, MD, FAAP
- Donna C. Graves, MD
- M. Mark Hester, MD
- Suneya G. Hogarty, DO
- Marius J. Ilario, MD
- Linda W. Lawrence, MD
- Douglas S. McFarlane, MD
- Mark B. Moeller, MD
- Anonymous
- Raleigh Orthopaedic Clinic, PA
- Timothy J. Reeder, MD, MPH, FACEP
- Alan J. Rosenbaum, MD
- Anonymous
- Marshall Z. Schwartz, MD
- Douglas D. Sheets, MD, FACOG
- W. Alan Skipper, CAE
- Jennifer K. Stoddard, MD
- STUSQU, PLLC
- Lisa W. H. Thompson, MD
- Cheryl L. Walker-McGill, MD, MBA
- Craig E. Webb, MHS, PA-C
- Johnathan D. Williams, MD
- Anonymous
- Idil Aktan, MD
- R. D. Almkuist, II, MD
- American Board of Pediatrics Inc
- Caroline D. Ames, MD, FACS
- James H. Antoszyk, MD
- Joy Avery
- Timothy M. Beittel, MD
- Anonymous
- Anonymous
- Cedar Mount Behavioral Health, PA
- Center For Pain Management, PLLC
- Melissa M. Coale, MD
- Anonymous
- Kim D. Dansie, MD
- Jackie M. Davis-Jones
- Jessica F. Doerrler, PA
- Patricia Duncan
- Peter A. Eweje, MD
- Mark W. Featherston, MD
- Anonymous
- Joanne M. Fruth, MD
- Lisa M. Gangarosa, MD
- Highland Medical Associates
- Anonymous
- Joseph P. Hunstad, MD, FACS
- Kitsie Jones
- Christopher P. Jordan, MD
- Kerry Kendall
- Eugenie M. Komives, MD, FAAFP
- Ted R. Kunstling, MD, FCCP
- Andrew S. Lamb, MD
- Keith LaScalea, MD
- Anonymous
- Elizabeth G. Livingston, MD
- Anonymous
- Laura L. Martinez, MD
- Darlyne Menscer, MD
- Ashley Newton
- J. Thomas Newton, MD
- Carolyn O'Conor, MD
- Michael K. Patrick, MD
- Patricia Petrick, MD
- Emily Rayes-Prince, MD
- Anonymous
- Corianne D. Rogers, MD
- Nimesh B. Shah, MD
- Kristen M. Shipherd
- Maria J. Small, MD
- Anonymous
- Michol Stanzione, DO
- Steele Creek Dermatology
- Al Steren, MD and Diane Snyder Steren, MD
- Martha Strange, MD
- Thomas M. Swantkowski, MD, AGAF, FACG
- Marian L. Swinker, MD, MPH
- Christopher L. Tebbit, MD
- Monecia Thomas, PhD
- Dimitri G. Trembath, MD
- Michael J. Utecht, MD, FACEP
- Lynnea Villanova, MD
- Bonnie E. Wagner, PA-C
- Rebecca Y. Weinshilboum, DO
- Carl J. Westcott, MD
- Thomas R. White, MD
- Anonymous
- Women's HealthCare Consultant PC
- Nagarjuna Yerra, MD
- Michael Bartiss, MD / Family Eye Care of the Carolinas
- David Boone, MD
- Carolina Complete Health
- Karl Chiang, MD
- John Chretien, MD
- Anonymous
- Kelly Fedoriw, MD
- Carolyn Ferree, MD
- Alison Gardner, MD
- John Goldfield, MHS, PA-C
- Akilah Grimes, MD
- Sandra Jackson / Eastern Pediatrics
- Matthew Katz, MS / MCK Health Strategies
- Melissa Kenny
- Donna McGee, MD
- Larry Napolitano, Jr., MD
- Michael P. Reddy-Miller, MD
- Anonymous
- Andrew Pasternak, MD
- Antonio Ramirez, MD
- Beth Remhof
- Jennifer Root, MD
- Richard Savage, MD
- Anonymous
- Soma Sengupta, MD
- Nimesh Shah / Noble Hospitality Investment
- Amanda Trimpey, MD, MPH, FACOEM
- Yunxiang Zhu, MD
*Please note: List reflects donations received through Tuesday, December 17.
Could VR Devices Deliver Relief to High-impact Chronic Pain Patients?

AppliedVR continues to build out clinical evidence to support the use of immersive therapeutics to address chronic pain.
The company's flagship virtual reality device for chronic lower back pain delivered meaningful reductions in pain intensity for patients, particularly for high-impact chronic pain patients, according to a recent clinical study.
A secondary analysis of a large randomized controlled trial evaluated how AppliedVR's VR therapy to treat chronic low back pain at home affected patients who experience pain more intensely. Researchers sought to determine whether the therapy could produce greater levels of pain relief for high-impact chronic pain patients, or individuals with chronic pain that is accompanied by at least one major activity restriction, such as being unable to work outside the home, go to school or do household chores.
These patients are often the most difficult and costly to treat. This patient population is more likely to report severe pain, more mental health and cognitive impairments, worsening health and more difficulty with self-care.
"High-impact chronic pain patients represent roughly 25% of the entire chronic pain population. But because they are high impact, they consume a lot more of the resources and can be much more challenging," AppliedVR co-founder and CEO Matthew Stoudt said in an interview. "They tend to use significantly higher doses of opioids compared to those with less severe chronic pain, and they have about five times the hospital use."
Read the full article here.
HO-HO-HO, to the ER Y'all Go ... If You're Not Practicing Proper Food Safety!
No one wants to spend their holiday recovering from food poison. Proper food safety practices can make a huge difference in preventing illness and keeping your holiday festive and fun!

Avoiding these holiday cooking mistakes can help ensure that holiday meal is safe and enjoyable for everyone:
- Undercooking the Turkey
Undercooked poultry can harbor harmful bacteria like Salmonella. Always check the internal temperature with a thermometer to ensure it reaches proper temp. - Not Thawing Meat Properly
Thawing meat on the counter can cause bacteria to multiply. Always thaw in the fridge or in cold water (changing the water every 30 minutes). - Cross-Contaminating Raw Meat
Using the same cutting board for raw meat and vegetables without sanitizing it can spread harmful bacteria like E. coli. Use separate boards for raw meat and other ingredients. - Not Washing Hands After Handling Raw Meat
Touching raw meat without washing your hands can transfer bacteria to other foods and surfaces, leading to foodborne illnesses. - Not Storing Leftovers Promptly
Leaving leftovers at room temperature for too long (over 2 hours) can lead to bacterial growth. Store them in the fridge within two hours to avoid food poisoning. - Using Expired Ingredients
Baking or cooking with expired ingredients, especially dairy or eggs, can lead to foodborne illnesses. Check expiration dates carefully. - Not Cooking Stuffing to the Right Temperature
Stuffing cooked inside poultry can retain moisture and bacteria, which can lead to food poisoning. Make sure it reaches proper temp. - Using a Non-Calibrated Meat Thermometer
If your meat thermometer isn’t working correctly, you may end up eating undercooked meat, risking bacterial contamination. - Serving Undercooked Potatoes
Undercooked potatoes, particularly in dishes like mashed potatoes or gratins, can cause gastrointestinal issues due to harmful bacteria. - Not Washing Vegetables Properly
Raw vegetables can be contaminated with harmful bacteria or pesticides. Always wash them thoroughly to reduce the risk of illness. - Leaving Leftovers Out Overnight
Leaving food out overnight allows bacteria to multiply rapidly, particularly in creamy or dairy-based dishes. Always refrigerate leftovers promptly. - Not Heating Leftovers to a Safe Temperature
Reheating leftovers to only lukewarm temperatures can leave harmful bacteria alive. Reheat to a proper temp to kill germs. - Eating Raw Cookie Dough or Cake Batter
Raw eggs and unbaked flour can contain Salmonella and E. coli, respectively. Avoid tasting raw dough or batter, especially for children and the elderly. - Using a Dirty Dishcloth
Using a dishcloth that hasn’t been sanitized can spread bacteria to your food, especially when wiping counters and utensils after handling raw meats. - Not Storing Perishables Correctly
Perishables like dairy, meats, and eggs should be stored at the right temperature. Leaving them out too long can cause bacterial growth. - Using Non-Food-Grade Containers
Storing food in containers not designed for food storage (like old yogurt containers) could introduce toxins or cause contamination. - Not Properly Sealing Leftovers
Storing leftovers in loosely covered containers or improperly sealed plastic bags can expose them to bacteria or mold growth. - Serving Dishes That Have Been Sitting Too Long
Food that sits out too long at room temperature can grow dangerous bacteria. Always serve food as soon as it’s cooked or keep it warm safely. - Serving Underprepared Fish
Undercooked fish can harbor parasites or harmful bacteria, such as Vibrio, which causes food poisoning. - Not Cooking Eggs Thoroughly
Raw or undercooked eggs can lead to Salmonella infections. Make sure eggs are fully cooked, especially in dishes like eggnog, custards, or hollandaise sauce. - Leaving Raw Meat Near Ready-to-Eat Foods
If raw meat touches fruits, vegetables, or ready-to-eat foods without being properly separated, it can cause cross-contamination. - Using a Single Cutting Board for All Ingredients
Using the same cutting board for raw meats, fruits, and vegetables can spread harmful bacteria. Always use separate boards for different types of food. - Not Cleaning the Oven
A dirty oven can harbor old food residues that may cause contamination or even burn and produce harmful fumes during cooking. - Improperly Storing Canned Goods
Canned goods that are improperly stored or damaged can lead to botulism, a potentially fatal foodborne illness. Always inspect cans before use. - Not Following Food Safety Guidelines for Holiday Sweets
Holiday sweets like homemade candies and cakes may contain raw ingredients or unsafe temperatures that can result in bacterial growth if not handled properly.
Join NCMS Board Member Dr. Karen Smith Thursday for a Discussion on Cardiovascular Disease
Join the conversation on cardiovascular health with NCMS Board member Dr. Karen Smith, alongside other healthcare professionals, this Thursday, December 19, at 7:00 pm.
About Us Open My Heart Foundation
The Open My Heart Foundation (OMHF) is a 501c3 charitable organization.
The mission of the Open My Heart Foundation is to help eliminate heart health disparities among African American Women and Women of Color through education, support and advocacy. This includes monthly support group meetings, heart healthy food and produce, education by experts in the field of heart health and wellness, including fitness, yoga and professional trainers. They also provide community resources and hospital visitation. The Open My Heart Foundation helps to fill in a gap for much needed medical treatment, equipment and assistance with co-pays.
What You and Your Patients Should Know About Radon
Beginning January 1, 2025, the North Carolina Radon Program is making available one Radon kit per home. Once received, please use the kit as soon as you receive it. If you do not receive your kit within two weeks of ordering, please immediately contact AirChek at 800.247.2435 or 828.684.0893. Each kit is completely free. The kit, the return postage, and the kit analysis has been prepaid. There is no charge to you. If you damage the kit or accidentally dispose of the kit, replacements are not available.
12 Holiday Scams on Santa's Naughty List!
It's the most wonderful time of the year ... for scammers!
The Better Business Bureau has compiled a list of the top 12 holiday scams this holiday season, with guidance on how to avoid most of them: always exercise caution with social media ads promoting discounted items, holiday events, job opportunities, and donation requests, as well as direct messages from strangers. If you are asked to make a payment or donation by wire transfer, through a third party, or by prepaid debit or gift card, treat it as a red flag.

Don't let these scams steal your holiday joy:
1. Misleading social media ads
2. Social media gift exchanges
3. Holiday apps
4. Fake toll collection texts
5. Free gift cards
6. Temporary holiday jobs
7. Impostor scams
8. Fake charities
9. Fake shipping notifications
10. Advent calendars
11. Holiday wishlist items
12. Puppy scams

Read more about these scams here.
With Red Dye No. 3 Under FDA Scrutiny, a Ban Could Come Soon!

Since 2022, the Food and Drug Administration has been reviewing a petition to ban food dye, Red No. 3. Now, a decision could come soon.
The petroleum-based dye has been used for more than 50 years in thousands of products including candy, snack foods, and soda. Questions about the dye's potential health effects go back decades.
The FDA banned the use of the Red No. 3 in cosmetics and medicated ointments and lotions back in 1990. Research showed the dye could cause cancer in animals in high doses. But the agency concluded it was safe in the amounts used in food.
The agency says it has evaluated the safety of Red No. 3 "multiple times" since its original approval for use in food in 1969.
Lawmakers in 11 states have introduced legislation to ban Red No. 3 in foods. North Carolina currently has no legislation seeking the ban of Red No. 3. [source]
What do you think? Should Red No. 3 be banned? Let us know in the comments.
Inflammatory Foods Linked to Increased Incidence of Dementia

Diets higher in inflammatory foods were tied to an increased incidence of dementia in older adults, longitudinal data from the Framingham Heart Study Offspring cohort showed.
Over 13 years of follow-up, higher Dietary Inflammatory Index (DII) scores averaged across three time points were linearly associated with an increased incidence of all-cause dementia (HR 1.21, 95% CI 1.10-1.33, P<0.001), reported Debora Melo van Lent, PhD, of UT Health San Antonio in Texas, and co-authors.
Similarly, higher DII scores were linearly associated with an increase in Alzheimer's disease dementia (HR 1.20, 95% CI 1.07-1.34, P=0.002), the researchers reported in Alzheimer's & Dementia. Findings were adjusted for demographic, lifestyle, and clinical covariates.
"Although these promising findings need to be replicated and further validated, our results suggest that diets that correlate with low DII scores may prevent late-life dementia," van Lent and colleagues noted.
Previous cross-sectional research from the Framingham Heart Study Offspring cohort showed that higher DII scores -- indicating more pro-inflammatory foods consumed -- correlated with smaller total brain and gray matter volumes and larger lateral ventricular volume.
Other cohort studies, including a 3-year study in Greece, tied diets with high inflammatory potential to an increased risk of incident dementia. And clinical trial data showed the MIND diet -- a hybrid of the Mediterranean diet and the DASH (Dietary Approaches to Stop Hypertension) diet that is rich in anti-inflammatory foods -- had a similar effect on cognition and brain MRI outcomes as mild caloric restriction over 3 years, possibly due to high adherence of the control group to lifestyle advice.
Full article is here.
NCMS at Work for YOU: 2024 End of Session Legislative Report
As the largest physician organization in the state, the NCMS devotes significant resources to advocating physician viewpoints in the public policy arena. Success in these endeavors requires direct physician involvement. All physicians are encouraged to devote some time to understanding the medical issues addressed by the General Assembly and to work with the NCMS to assure the views of the medical community are presented to policy makers in an organized and effective fashion.
Thank you to all our members who engaged in advocacy this year! We look forward to continuing the fight for the health of all North Carolinians in 2025!
Below you will find the NCMS 2024 End of Session Report:


ADDITIONAL LINKS OF INTEREST:
Secure Your Spot at the NCMS Advocacy Summit!
Mark Your Calendar! 11th Annual Heart to Heart Event

Dosher Memorial Hospital Foundation will hold its 11th annual Heart to Heart event on Thursday, February 6, 2025, at the St. James Community Center from 5 to 7 p.m. February is heart health awareness month, and the 2025 event will feature important heart health education, food, wine, raffles and a 50/50. Reservations are $30 per person. The Foundation is seeking event sponsors. Reservations and sponsorships can be purchased online at dosher.org/foundation or by calling (910) 457-3936.
Lynda Stanley, president and CEO of Dosher Memorial Hospital, said, “Heart to Heart has become a much-anticipated event in the last 11 years. Not only is it an opportunity to support local healthcare, but it is also an evening full of education, great food, entertainment, and camaraderie among friends. We look forward to an enjoyable evening.”
Foundation Director Antonette (Toni) McAndrews added, “This event is both fun and educational and the Foundation is very grateful for all sponsors, donors and supporters.”
The Dosher Memorial Hospital Foundation was established and began operating in March 2010. The Foundation’s primary responsibility is to encourage a steady flow of funds to the hospital from individuals and organization within the hospitals’ service area. These funds enable Dosher Hospital to continue providing its patients with the finest healthcare equipment, programs and services possible, as well as provide the resources necessary for construction, expansion and remodeling projects.
For more information about the Dosher Memorial Hospital Foundation, visit www.dosher.org or call (910) 457-3936. [source]
Interested in Becoming an Independent Medical Reviewer for the NC Medical Board?

NCMB relies on professional opinions provided by independent outside medical reviewers to help determine the outcome of disciplinary cases that involve questions about the quality of medical care provided to patients. Independent outside medical reviews help the Board establish whether accepted and prevailing standards of care were met and, if not, how care departed from accepted standards. Below are some of our FAQs on the outside reviewer process.
Q: Why does the Medical Board need outside medical reviewers?
A: Outside reviewers are truly critical to the Board’s case review process. NCMB’s success depends on its ability to draw on the knowledge and experience of medical experts regarding standards of care in their areas of practice.
Q: What is the specific service outside medical reviewers provide to the Board?
A: The reviewer’s role is to determine whether standards of care were met at the time of treatment. Reviewers are provided with bookmarked electronic copies of medical records, which they evaluate. They also receive a worksheet for the case review and provide their opinions to the Board in the form of a written report.
Q: Are outside medical reviewers compensated?
A: Yes. Reviewers are compensated at a rate of $175 per hour for the time spent reviewing records and writing their reports. It is also a wonderful way for clinicians to serve patients and the medical profession, by ensuring that standards of care are upheld in North Carolina.
Q: May outside medical reviewers remain anonymous or will the clinician under investigation know who reviewed his or her care?
A: Generally, yes, reviewers can remain anonymous. On rare occasions, when a case proceeds to a public hearing, reviewers may be asked to provide testimony. This is not needed in a significant majority of cases where outside reviews are sought.
Q: Am I at risk of being sued for serving as a medical reviewer or testifying at a hearing for the Board?
A: No, reviewers for the Board are provided statutory immunity from civil liability and will not be held liable in any civil proceeding for testifying before the Board in good faith and without fraud or malice.
To indicate your interest in providing outside medical reviews, contact [email protected].
Read the Expert Reviewer Manual.
Could Personalizing Complete Blood Count Test Improve Patient Care?

Using personalized rather than standard reference points for the routine blood test known as a complete blood count (CBC) could improve assessments of patient health and diagnosis of diseases in earlier stages while patients still appear healthy, according to a study led by Harvard Medical School researchers at Massachusetts General Hospital.
CBC screening is valuable for assessing a patient’s overall health using a single blood sample. Currently, the results of CBC tests are analyzed using a one-size-fits-all reference. The new analysis suggests that this approach can overlook natural variations and deviations in health.
In a retrospective analysis of more than 12,000 adults who received multiple CBC tests across 20 years, the researchers showed that these reference intervals are far from widely generalizable.
Read the full article with findings here.
NCDHHS Receives 1115 Medicaid Waiver Approval

A Message from NCDHHS: In 2018, NCDHHS won approval from the Federal government to try an innovative approach to improving North Carolinian’s health. Recognizing that health doesn’t just happen at the doctor’s office or in a hospital, the Centers for Medicare/Medicaid Services (CMS), under the previous Administration, gave NCDHHS the flexibility through an 1115 Medicaid waiver to invest in housing, food, transportation and more for high-needs Medicaid recipients. The premise behind this was a simple one: people stay healthier, and the state saves money in the long run.
The North Carolina General Assembly saw the value in this approach and has supported these efforts by funding the Healthy Opportunities Pilots. Earlier this year we got good news, it’s working. Participants had fewer emergency department visits and less inpatient hospitalizations, and the state is spending about $85 less in medical costs per participant per month. And now, in recognition of these strong results, CMS has just approved a new 1115 waiver renewing the flexibilities behind this success and expanding more opportunities to build on these innovations.
This approval is a necessary, but not a final, step to helping more North Carolinians stay healthy and further bending the healthcare cost curve for the state. With this approval, we now have a menu of options for North Carolina to potentially take advantage of. NCDHHS will meet with stakeholders, partners, and most importantly legislators, to discuss what opportunities are now available and how we may be able to come together to implement them. An overview of the key components of this new 1115 waiver approval are below:
- Allows for Healthy Opportunities Pilots that invest in non-medical drivers of health like food, transportation and housing to be taken statewide (beyond the current three regions),
- Opens up access for people who are incarcerated to get NC Medicaid health coverage up to 90 days prior to their release providing them critical health services and helping to break the expensive cycle of incarceration,
- Enables more behavioral health resources for North Carolinians and boosts the behavioral health workforce,
- Extends federal authority for North Carolina’s successful Medicaid Managed Care program,
- Makes it possible for children to remain covered by NC Medicaid for longer periods of time, reducing burdensome paperwork for families and counties, and
- Continues availability to evidence-based substance use disorder treatments for Medicaid beneficiaries while they are in a qualifying facility.
Since the Healthy Opportunity Pilots launched in three rural regions in 2022, North Carolina has served more than 26,000 high-needs Medicaid enrollees to keep them healthier and prevent illness rather than just waiting to treat it. And we’ve proven it’s more cost-effective.
The community-based organizations that we worked with to implement the Healthy Opportunities Pilots have been essential and excellent partners, though none of this past success would have been possible without the support from the General Assembly. We’re proud these shared accomplishments have improved lives and laid the foundation for us to partner again and make an even bigger impact. We will be sharing this news of the approval from CMS with other interested parties, which will generate excitement as we contemplate how to move forward together. We will follow up soon to provide additional details on the 1115 waiver approval and what steps we could begin to take.
Thank you again for your support to improve the health and well-being of all North Carolinians.
Durham-Orange Medical Society Holds Final Member Meeting of the Year

On December 11, the Durham-Orange Medical Society hosted its final membership meeting of 2024, featuring a dynamic and interactive presentation by Anthony Galanos, MD, PA, a Palliative Care Specialist at Duke. Dr. Galanos’ talk, titled "Communication, Emphasis on Empathy, and Reading the Room", sparked meaningful discussions as he used role-play exercises to explore effective communication strategies with patients and their families during emotionally charged, end-of-life conversations.
The meeting concluded with heartfelt thanks to Dr. Priscille Schettini for her leadership as the 2024 DOCMS President. The evening wrapped up with congratulations to Dr. Hans Arora, who will serve as the 2025 DOCMS President.

Secure Your Spot at the NCMS Advocacy Summit!
Whether you're a healthcare professional, community leader, or passionate individual, the NCMS Advocacy Summit provides a platform to discuss, learn, and collaborate on shaping the future of healthcare.
We are thrilled to invite you to the NCMS Advocacy Summit, a groundbreaking event dedicated to exploring and advancing crucial topics in healthcare. Join us on March 1, 2025, from 9 am to 5 pm at the StateView Hotel, located at 2451 Alumni Drive, Raleigh, NC 27606.
Event Highlights:
- Engaging Sessions: Delve into discussions on Access to Care Solutions, Corporate Practice of Medicine, AI in Healthcare, and much more!
- Diverse Perspectives: Gain insights from esteemed speakers representing various states and local community leaders, providing a comprehensive view of healthcare advocacy.
- Networking Opportunities: Connect with professionals who share your passion for healthcare advocacy. The last session of the day will be a townhall allowing leaders from specialty and county societies to speak.
Registration is Open, but Space is Limited! Don't miss this opportunity to be part of a transformative event. Secure your spot today by registering today!
We look forward to your participation in this impactful event.
Future NC Proton Beam Therapy Center Receives Historic Gift

An anonymous donor has made a $50 million gift to Duke University Health System toward the development of a proton beam therapy center.
The donation is the largest philanthropic gift received by Duke University Health System.
“This is a historic gift, both for Duke and for the state of North Carolina,” said Vincent E. Price, Ph.D., president of Duke University. “The Duke Proton Center will have a profound impact on cancer care in our region, and we are very grateful for the generous donor support that is making these advances possible.”
Duke’s proton beam therapy facility is expected to open by 2029, with a total projected cost of $120 million. At capacity, it is projected to provide proton therapy to about 800 patients each year.
Continue to the full article here.
Encourage Your Patients to Explore Family Health History
KNOWING IS HALF THE BATTLE
As families come together during the holidays, encourage your patients to explore their family health history. Cone Health's Chad Haldeman-Englert, MD, explains how your relatives' medical background can be a powerful tool for improving your own health.
When delving into your family's health history, it's essential to consider the following:
- Three-Generation Pedigree: Focus on your siblings, parents and grandparents.
- Age of Onset: The earlier a condition occurs, the more significant it may be.
- Specific Conditions: Pinpoint conditions like cancer, heart disease, diabetes, dementia, and chronic kidney disease.
- Rare Conditions: Unusual or rare conditions can indicate a genetic predisposition.
Leveraging Your Family Health History
Once you've gathered this information, share it with your healthcare provider and take proactive steps to improve your health:
- Genetic Testing: Learn more about genetic testing to identify specific genetic markers that may increase your risk for certain conditions.
- Explore participation in our community health research program, called GeneConnect, that helps you understand your genetic risk for certain cancers and a cause of heart disease, as well as your regional ancestry and genetic traits related to your health. Visit conehealth.com/geneconnect to learn more.
- Early Screening: Early screening can detect potential health issues before they become serious.
- Lifestyle Modifications: Adopting healthy habits like regular exercise, a balanced diet, and stress management can help mitigate genetic risks.
How to Start the Conversation
Talking about health can be a sensitive topic, but it's essential for your well-being. Here are some tips to initiate the conversation:
- Be Gentle: Approach the topic with empathy and understanding.
- Respect Privacy: If someone is uncomfortable sharing, don't push them.
Federal Provider Enrollment Application Fee Increase for 2025
The federal fee for Medicaid enrollment has increased to $730 for calendar year 2025
The Centers for Medicare & Medicaid Services (CMS) Federal Register 89 FR 95215 (see Medicare, Medicaid, and Children's Health Insurance Programs; Provider Enrollment Application Fee Amount for Calendar Year 2025) finalized provisions related to the imposition of application fees as part of the Medicaid provider enrollment process for institutional providers and suppliers. The fee will vary from year to year pursuant to the consumer price index for all urban consumers (CPI-U).
The federal fee for Medicaid enrollment will increase from $709 to $730 for calendar year 2025, and effective January 1, 2025, will be required as noted on the Provider Permission Matrix for:
- Initial enrollment;
- Re-enrollment;
- Adding a new owner or a new site location; and
- Re-verification.
Additional information regarding the federal fee can be found on the public-facing NCTracks provider portal Federal Fee and NC Application Fee FAQs page.
Questions:
- NCTracks Call Center: 800-688-6696
- Provider Ombudsman: 866-304-7062
Double Trouble: Diabetes and Falls

People with diabetes are at higher risk for falls. Etiologies include vision changes from retinopathy, damage to both peripheral and central nerves, side effects from medicines, and co-morbidities like osteoarthritis. Through use of a case study illustrating a familiar primary care patient encounter, learners will apply new knowledge, so they can anticipate and intervene appropriately in their work. An optional module on conducting the Diabetic Foot Exam is included. There is no charge for this online course. Course registration is generously supported by the Division of Health Benefits.
New Breakthrough Treatment for Parkinson’s Disease
For more than 50 years, oral levodopa has been considered the gold standard in treatment for Parkinson’s Disease.
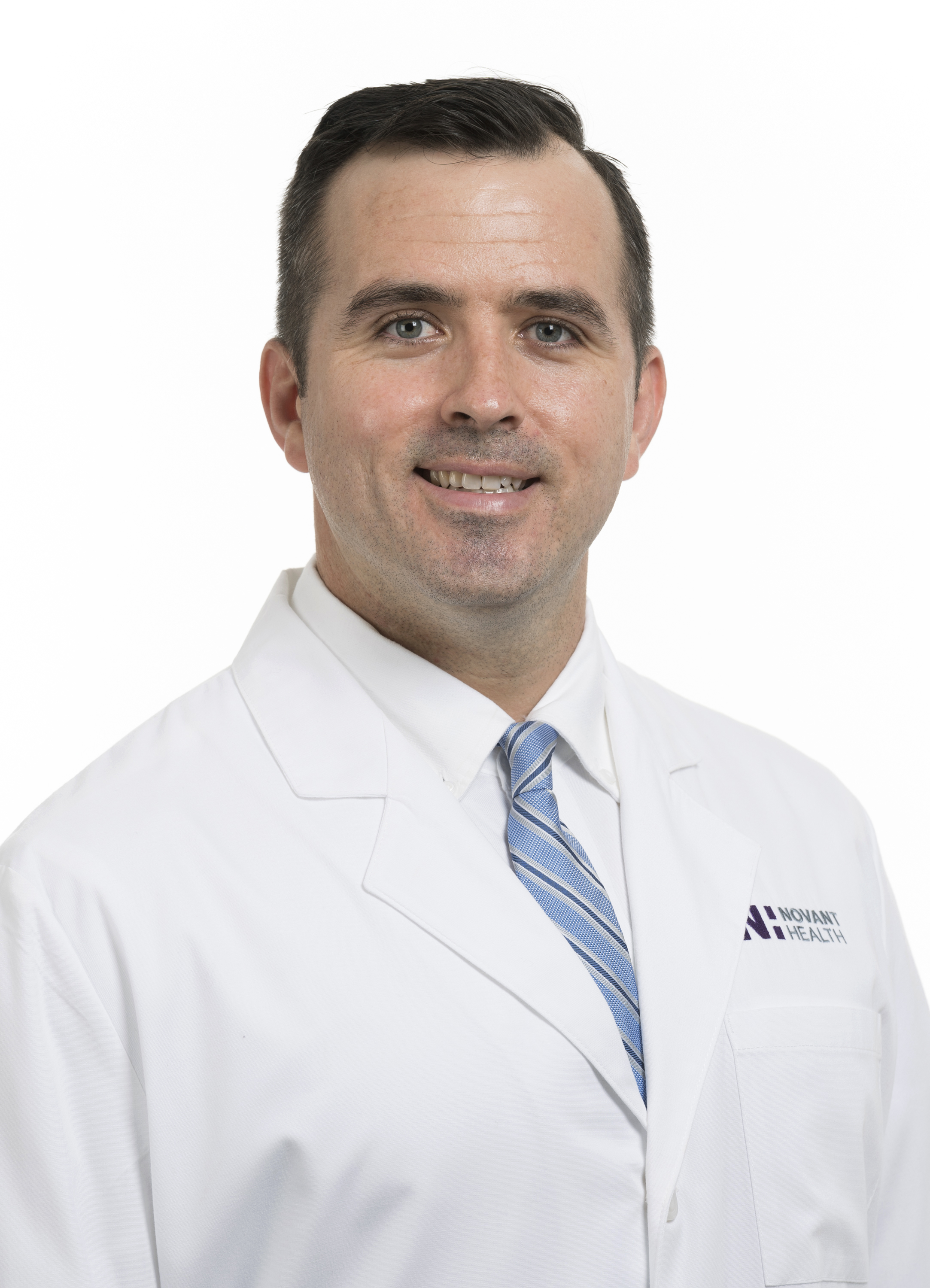
But there’s finally a breakthrough treatment that makes the drug even better, said Dr. Robert Wiggins, a neurologist with Novant Health Neurology & Sleep – Midtown in Charlotte. And Novant Health was among the first in the country to offer it. The name is Vyalev and in simple terms, it’s a form of liquid levodopa with a new delivery system that produces far better results.
Here, Wiggins explains what this leading-edge treatment means for Parkinson’s patients.
Diabetes Performance Improvement in Primary Care

This self-paced educational activity aims to inform the learner about the status of diabetes and chronic kidney disease in primary care. This activity will explore barriers and facilitators to promote patient engagement in treatment. This activity will focus on performance improvement methods and activities which promote health among patients with diabetes.
Register Now! PANS and Related Inflammatory Brain Disorders – Advances in Immunopsychiatry
Join Us for On-Demand CME –Free to North Carolina Physicians
PANS and Related Inflammatory Brain Disorders: Advances in Immunopsychiatry features nationally and internationally renowned experts skilled in diagnostic and therapeutic approaches who will present a diverse range of emerging clinical and research challenges, insights, and advances in the field of inflammatory brain disorders.
Download the pdf here.
Learn more and apply for access here.
Mark Your Calendar! Saving Time: Practice Innovation Boot Camp

This two-day, in-person AMA STEPS Forward® Innovation Academy boot camp is specifically designed for clinical and operational change agents looking to eliminate unnecessary work and free up more time to focus on what matters most–patient care.
Gain proven tools to implement in the following areas:
- Getting rid of stupid stuff
- De-implementation (STOP this and START that)
- Debunking regulatory myths
- EHR inbox optimization
- Team-based care practice fundamentals
- Building bridges between clinicians and administrators
- Reducing barriers to taking PTO
- Making the business case to leadership
Through breakout sessions, interactive activities, thought sharing, tactical strategy breakdowns and how-to examples, this boot camp will equip attendees with the time-saving tools and strategies needed to reform their organizations and enhance professional satisfaction.
Don’t miss this opportunity to gain best practices from top physician experts, network with like-minded peers, engage in cross-sector collaboration, and learn from each other’s successes and mistakes.
Space is limited. Learn more, including how to register, here.
NCDHHS Introduces Toolkit for States to Take Action on Medical Debt

The North Carolina Department of Health and Human Services today released a toolkit aimed at assisting other states seeking to tackle the burden of medical debt. The Medical Debt Toolkit is based on an innovative program recently launched by NCDHHS to address the issue of medical debt among North Carolinians. It builds on record enrollment as North Carolina marks one year of Medicaid expansion.
"North Carolina is leading the nation with an innovative approach to easing the burden of medical debt," said Governor Roy Cooper. "Freeing people from medical debt is life-changing for families and a benefit to our economy, and I hope other states can use the roadmap we've laid out to make a difference."
More than 20 million Americans held $20 billion in outstanding medical debt in 2021. For many low- and middle-income consumers, medical debt causes significant financial distress and can prevent patients from getting the care they need. This issue is particularly acute in states that have not expanded Medicaid as permitted under the Affordable Care Act. Research shows that medical debt relief is a highly bi-partisan issue with strong support from Democratic and Republican leaders. Polling shows 80% of people want their state and federal elected officials to pass policies to reduce health care costs. Medical debt relief is an initiative leadership can use to significantly improve the lives of their constituents.
"Medical debt is a disease in our health system. Relieving this debt can lead to healthier individuals and a stronger health system overall," said Health and Human Services Secretary Kody H. Kinsley. "The financial burden and fear of medical debt — a debt no one ever chooses to have — makes people avoid getting the essential and preventive care they need."
North Carolina’s program is the first in the nation to leverage Medicaid state directed payment authority to encourage hospitals to both relieve historical medical debt and adopt forward-looking protections to prevent the accumulation of debt. While the program is optional for hospitals, all 99 acute care hospitals in the state have agreed to participate. Through the program, hospitals are expected to relieve up to $4 billion in existing medical debt for two million North Carolinians. Participating hospitals also will be required to implement more robust and standardized financial assistance policies, proactively screen patients for eligibility for financial assistance, eliminate reporting of medical debt to credit agencies and implement certain other protections.
Currently, there is a very clear pathway for states to pursue similar initiative. NCDHHS compiled a toolkit providing guidance and discussing key considerations on critical program design and implementation issues. Specifically, the toolkit focuses on the following areas:
- The structure of the state-directed payments (SDP) arrangement.
- Required hospital medical debt mitigation policies (tied to enhanced payments under SDP program).
- Interaction of the program with other federal requirements (e.g., federal fraud and abuse laws).
- Communications and stakeholder engagement strategy.
- Operational considerations.
The toolkit also links to several resources for states to reference, including:
- Key excerpts of relevant documents.
- A landscape assessment of other states’ medical debt mitigation policies.
- Press releases and communications from NCDHHS related to the program.
The toolkit can be found on the NCDHHS website.
NCDHHS is committed to increasing access to the right care at the right time for all North Carolinians. Expanding Medicaid, implementing Medical Debt Relief, investing $835 million in behavioral health, launching Healthy Opportunities Pilots and being supported by a Community Partner Engagement strategy are all examples of the department’s work toward its three priorities of Supporting Child and Family Well-Being, Building an Inclusive Workforce and Investing in Behavioral Health Resilience. [source]
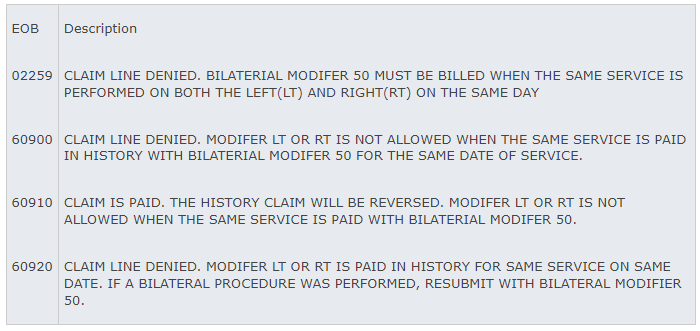
Billing for Bilateral Surgical Procedures

Beginning December 8, 2024, and for services provided on or after January 1, 2020, new guidelines will apply to billing for bilateral surgical procedures with the bilateral RVU indicator of “1” for bilateral procedures (modifier 50). See the Centers for Medicare & Medicaid Services PFS Relative Value Files webpage.
*Reference Column T – BILAT SURG
Codes with the modifier 50 indicator of “1,” are valid for bilateral billing claim submission. With the exception of CPT codes inherently bilateral by definition, Medicaid requires practitioners to report procedures performed bilaterally, left and right, same procedure, same date of service, on one claim line with modifier 50 appended to the code (e.g., xxxxx-50, billed with 1 unit). Failure to report bilateral procedures in this way may result in incorrect processing or denial of claims.
Reporting these bilateral-indicator-1 procedures with either LT or RT and 1 unit of service is appropriate only if the procedure is being performed unilaterally. If the procedure is performed bilaterally, modifier 50 must be appended to the procedure code with 1 unit of service.
When a surgery is performed bilaterally, on the left and right, with the same procedure code and date of service, providers should submit a single claim line billed with the bilateral procedure modifier 50.
The following new edits and EOBs are being implemented to support these changes.
Funding Opportunity: Collaborative Care Management
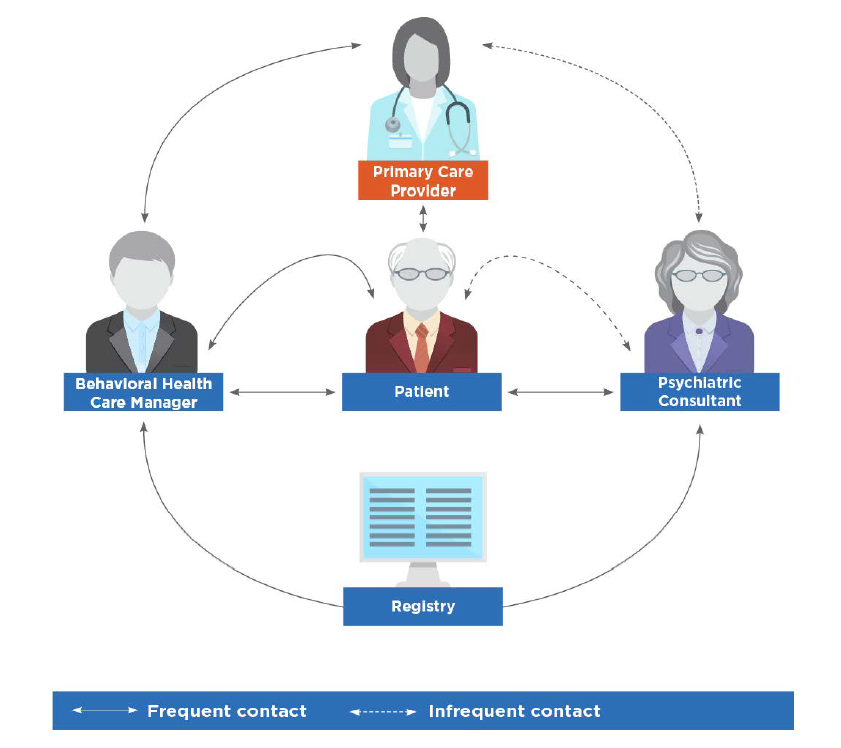 image credit: American Psychiatric Association
image credit: American Psychiatric Association
On behalf of the North Carolina Department of Health and Human Services (NCDHHS), Community Care of North Carolina (CCNC) is accepting applications for the Collaborative Care Management (CoCM) capacity building funding for primary care practice entities.
Collaborative Care Management (CoCM) is an evidence-based behavioral health integration model designed to support primary care clinicians as they assess and treat patients with mild to moderate behavioral health conditions.
CoCM improves patient outcomes, increases satisfaction for both patients and providers, and reduces healthcare costs and stigma related to mental health and substance use disorders. The model complements other integrated models, including the North Carolina Psychiatric Access Line (NC-PAL).
The NC General Assembly has allocated $5 million for capacity building of Medicaid-enrolled primary care practices across the state to adopt CoCM. NCDHHS is contracting with Community Care of North Carolina (CCNC) to manage the CoCM Capacity Building award program in partnership with NC AHEC. The goal is to increase access to evidence-based behavioral healthcare for primary care practices and their patients through the use of the CoCM model.
For more information and how to apply, visit the Community Care of North Carolina Collaborative Care Management Capacity Building Fund Application.
If you are a primary care entity serving Medicaid patients and are interested in learning about CoCM and related capacity building fund opportunities, we invite you to watch the recorded webinar from October 30, 2024 for an overview, here.
Hurricane Helene Note: CCNC is keenly aware that some practices in Western North Carolina are still recovering from the storm and may find it difficult to apply for funds at this time. Efforts will be made to ensure that practices impacted by the hurricane will still have an opportunity to apply for inclusion in the program.
Tailored Care Management Temporary Rate Extension

NC Medicaid will continue the current Tailored Care Management temporary payment rate of $343.97 statewide through June 30, 2025. Effective July 1, 2025, the payment rate will be $294.86.
The continued temporary rate increase reflects the level of effort required by providers, based on available data on provider time and effort to date, to implement the Tailored Care Management model. NC Medicaid is not making any other changes to the payment methodology.
Questions? Contact: [email protected]
This update applies to NC Medicaid Managed Care and NC Medicaid Direct.
New Tool Helps Practices Track Fee-for-service and Value-based Financial Performance
NC AHEC Practice Support developed a new Financial Health Scorecard for your practice. The scorecard is intended for practices in need of a no-cost resource to track their fee-for-service and value-based financial performance, and prioritize strategic opportunities for improvement. Practice Support coaches are available to assist with training, and any identified opportunities for quality improvement, EHR/HIE optimization and workflow optimization based on best practices for your specialty.
If you need assistance from a Practice Support coach, please contact us at [email protected].
Register Now! Psychiatric Presentations with a Neuroimmune Basis ECHO
Neuroimmune Foundation has partnered with Project ECHO® – an internationally recognized platform with over one million learners in 45+ countries focused on over 1000 medical conditions, to offer weekly didactics and case-based learning to physicians worldwide.
Download the pdf document here.
Register here.
FDA Approves New Targeted Therapy for Pancreatic Cancer

The U.S. Food and Drug Administration has granted accelerated approval for a new drug targeting a tumor alteration called NRG1 gene fusion found in roughly 3% of patients with pancreatic adenocarcinoma, the most common type of pancreatic cancer. This approval underscores the promise of precision medicine – treatment based on the biology of a patient’s tumor – and reinforces how critical it is for all patients with this disease to receive biomarker testing of tumor tissue along with genetic testing for inherited mutations as soon as possible after diagnosis.
“The recent FDA accelerated approval of Bizengri is encouraging for people with pancreatic cancer whose tumor has an NRG1 fusion,” said PanCAN Chief Scientific and Medical Officer Anna Berkenblit, MD, MMSc. “This marks another treatment option for patients and highlights the power of a precision medicine approach and the importance of biomarker testing. This is an excellent precedent for rapid drug development in pancreatic cancer. Although only a small percent of pancreatic cancer patients have an NRG1 fusion, the responses seen with Bizengri are clinically meaningful, in the context of this difficult-to-treat cancer.”
BIZENGRI® is a targeted therapy. It has been granted accelerated approval by the FDA for a specific subset of patients diagnosed with pancreatic adenocarcinoma. This drug is available to patients whose tumor has an alteration called neuregulin 1 (NRG1) gene fusion whose cancer has worsened despite having gone through prior treatment. Roughly 3% of patients with pancreatic cancer have this alteration in their tumor, also referred to as NRG1 fusion-positive.
Continue to full article here.
Join DOCMS at the University Club Wednesday, December 11!

Join DOCMS at the University Club!
Wednesday, December 11, 2024 | 6:00pm - 8:00pm
University Club, 3100 Tower Boulevard, Suite 1700 - Durham, NC 27707
AGENDA:
6:00pm- 6:30pm – Socializing & Housekeeping
6:30pm- 7:30pm – Dinner & Guest Speaker
7:30pm- 7:45pm – Q&A
7:45pm- 8:00pm – DOCMS 2024 Business
"Doctors and Empathic Communication: An Oxymoron?
Reading the Room, the skill you were never taught!"
Speaker:
Anthony N Galanos, MA, MD | Professor of Internal Medicine, Duke University
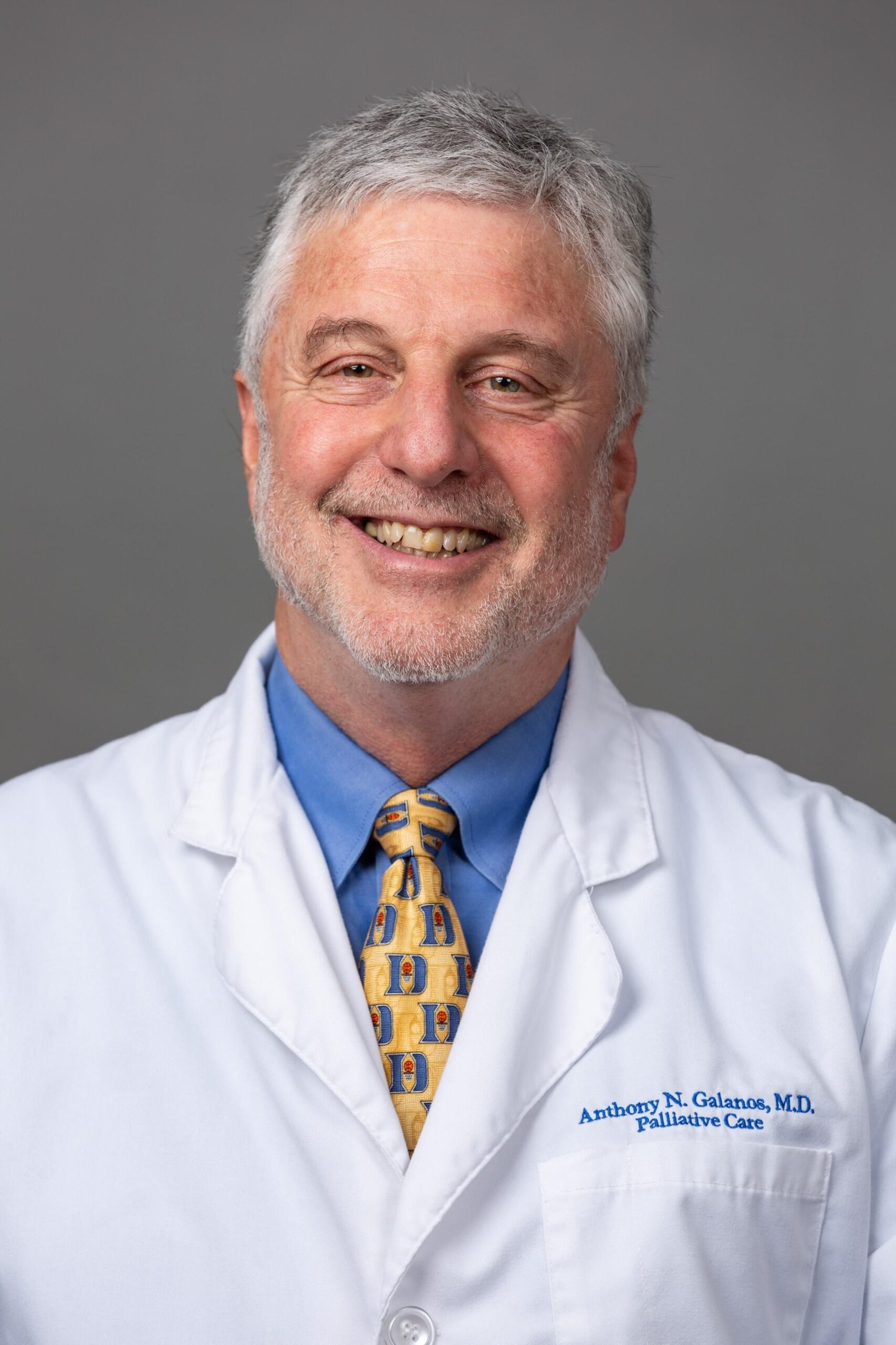
Dr. Galanos (Dr G) came to Duke in 1989 to do a Fellowship in Geriatric Medicine and has never left. He started the Ger Med Consult Service at Duke Univ Hospital in 1995 and started Duke Palliative Care in 1998.He retired from Clinical Med in 2023 and has stayed on to teach, debrief and mentor housestaff, Fellows and Faculty. He has always been interested in clinical teaching and often employs role play and rapping to hold the interest of his audience. He is here to demonstrate the efficacy and fun of role play while teaching a concept like “reading the room”.
1 CME Credit is available! Click here for how to claim your credit.
DOCMS Members & Prospective Members - FREE to attend
Guests - $25 to attend (will be collected at meeting site)
Asheville Lead Exposure Could Be More Widespread, Experts Recommend More Testing

Two independent chemistry experts say lead could be more widespread in Asheville’s drinking water following Tropical Storm Helene than the city has suggested, and both call for more public education and testing.
Sally Wasileski, chair of the UNC Asheville chemistry department, and Abigail Cantor, a chemical engineer and president of Process Research Solutions, LLC, which consults on municipal water issues, said they recommend residents of homes built in or before 1988, when lead was banned in new plumbing, use bottled water until they test their water.
“We cannot risk widespread lead poisoning, especially on top of all that our community has faced in the wake of Helene,” Wasileski wrote in a letter to the media and larger community in November. “We need a broad investigation of the lead levels at the tap of residences, schools, and businesses who source their water from Asheville City Water.”
Cantor, who lives in Madison, Wisconsin, has relatives in Asheville and said she warned them about the risk of lead in the water.
Continue to full article here.
NCMS Member Dr. Ryan Lamb Warns About Health Threats During Frigid Cold

Severe cold can result in bad health outcomes depending on career, pre-existing conditions, age, amount of clothing and lifestyle choices.
The medical director of emergency medicine at UNC Rex Hospital said there are reasons your body has to work harder to stay warm.
“The amount of energy your body has to expend in very cold temperatures, in the 20s, is a lot,” Dr. Ryan Lamb said. “You have to eat a lot of calories just to withstand that cold.”
Lamb has practiced medicine in the Triangle for years.
“The key is to dress appropriately,” Lamb said. “I think if you can wear proper clothing, a hat, gloves, a jacket, warm clothes and an underlayer so that you have a distance between, say, your jacket and your inner layer. The more layers that you have, it allows you to insulate better.”
The National Weather Service says the definition of severe cold varies “in different parts of the country.”
Freezing and near-freezing temperatures are enough to be considered extreme cold in the Deep South.
Young children waiting at bus stops and people working jobs outside for long periods of time can be susceptible.
One element Lamb points to for staying well is to stay dry.
“Trying to prevent it is definitely key,” Lamb said.
Lamb said some of the signs for hypothermia are quickened breathing, reduced cognitive function, a dip in coordination and poor use of motor skills.
“They are trying to unlock a door, open a handle from the outside and they're cold. You'll start to see coordination problems,” Lamb said.
There’s also the element of tracking trends in viral transmissions this winter season.
The Centers for Disease Control and Prevention reports low rates of flu and COVID-19 throughout the country at the present.
“I would suspect as this cold snap is about to occur and we are in it, you are going to see much more people confined into a closed environment, and as we see this slight uptick in the viral load, I suspect next week and the week after we are going to start to see the viruses increase in the community,” he said.
However, Lamb said they are seeing cases of pneumonia at the emergency department. (source)
NC HealthConnex: New Look for Easier Navigation
NC HealthConnex: New Look for Easier Navigation
South Piedmont AHEC’s Maria Goergen will host an informative Lunch n’ Learn session on December 17 from noon-1 p.m. See the latest updates and improvements to NC HealthConnex (NCHIE) that will make navigation simpler and more efficient for your practice.
Take advantage of this learning opportunity.
Register for Lunch n' Learn
If you need assistance from a Practice Support coach, please contact us at [email protected].
Secure Your Spot at the NCMS Advocacy Summit!
Whether you're a healthcare professional, community leader, or passionate individual, the NCMS Advocacy Summit provides a platform to discuss, learn, and collaborate on shaping the future of healthcare.
We are thrilled to invite you to the NCMS Advocacy Summit, a groundbreaking event dedicated to exploring and advancing crucial topics in healthcare. Join us on March 1, 2025, from 9 am to 5 pm at the StateView Hotel, located at 2451 Alumni Drive, Raleigh, NC 27606.
Event Highlights:
- Engaging Sessions: Delve into discussions on Access to Care Solutions, Corporate Practice of Medicine, AI in Healthcare, and much more!
- Diverse Perspectives: Gain insights from esteemed speakers representing various states and local community leaders, providing a comprehensive view of healthcare advocacy.
- Networking Opportunities: Connect with professionals who share your passion for healthcare advocacy. The last session of the day will be a townhall allowing leaders from specialty and county societies to speak.
Registration is Open, but Space is Limited! Don't miss this opportunity to be part of a transformative event. Secure your spot today by registering today!
We look forward to your participation in this impactful event.