NCMS Morning Rounds 6-22-20
Happy Monday! Here is your
NCMS Morning Rounds.
June 22, 2020
NCMS Legislative Update
The flurry of activity at the NC General Assembly last week makes our NCMS advocacy team think that the end of this session is near. Many bills moved and the ones that could impact your practice are updated regularly here on our legislative blog.
Here are several bills we’d like to highlight:
SB730—No Patient Left Alone was passed in the Senate and now moves on to the House for consideration. This proposal provides hospital visitation rights that would not be impacted during declared disasters and public health emergencies. The bill states that a hospital would provide the opportunity for at least one visitor per patient subject to the guidelines, conditions and limitations of the normal visitation policy. It remains to be seen if the House will take up this proposal and, if so, what changes if any would be made. Watch the blog for updates.
SB808—Medicaid Funding Act will be considered in the House this week. If passed, the ‘go live’ date for the state’s move to Medicaid managed care would be July 1, 2021. We’re watching this closely.
HB1105 – COVID/Supplementary GREAT Grant Period is one of several broadband proposals under consideration this session. While this is not directly related to health care, but because of the importance of telemedicine for you and your patients, particularly during this pandemic, broadband access is crucial. We are carefully tracking these bills.
You may not expect us to be tracking an education and transportation bond bill, however, HB1125 – WSSU/Online Education/CARES Act Funds contains a provision that would provide funding for a new Brody School of Medicine facility. As this bill was under consideration in the House, two Pitt County representatives, Rep. Kandie Smith and NCMS member Rep. Perrin Jones, MD, both recognized the Brody medical students who were present for the discussion as they were participating in the NCMS’ White Coat Wednesday. NCMS’ Immediate Past President Timothy Reeder, MD, MPH, FACEP has been instrumental in engaging medical students in the NCMS and its advocacy efforts. If you would like to make a difference, please consider signing up for a White Coat Wednesday, which is now available virtually. Learn more and sign up here.
NC Department of Health and Human Services Secretary Mandy Cohen, MD, MPH also appeared before the House Health Committee to answer committee members’ questions about the state’s response to COVID-19. Read a summary of the meeting and see the Secretary’s presentation here.
If the General Assembly completes its business this week, it is likely they will be back later in the summer, especially if Congress allocates more money for COVID-19 relief.
NCMS Joins NCHA and NC Chamber in COVID-19 Message
Last Friday the NCMS issued a joint statement with the NC Chamber and the North Carolina Healthcare Association (NCHA) calling on all North Carolinians to be united in voluntarily practicing CDC-recommended behaviors to limit the spread of the novel coronavirus, including wearing a face covering when in public or high-risk indoor group settings, practicing social distancing and washing hands often.
The unified message urged the public to follow public health guidance “so that the state can move forward toward full economic recovery.” The statement emphasized that “we can relaunch our economy and protect our health simultaneously.”
Read the full statement, which was distributed to statewide media here.
ICYMI: The Latest NCMS Community Conversation
The next in our series focused on NCMS members’ reflections on timely topics features longtime NCMS member Harry Gallis, MD. Dr. Gallis is an infectious disease specialist, who has an interesting perspective on the current pandemic.
Read the NCMS Community Conversation with Dr. Gallis.
If you have some thoughts on a topic you’d like to share with your colleagues, please contact Elaine Ellis, [email protected].
In the News
Patients Are Still Avoiding Medical Care. This Time It’s Not Just About Coronavirus Fears, The Advisory Board Forum, 6-18-20
Learning Opportunity
‘Launching Into Telehealth 2020’ is a virtual conference being co-hosted by the Mid-Atlantic Telehealth Resource Center (MATRC) and the Northeast Telehealth Resource Center (NETRC) over the next three Fridays, June 26, July 10 and July 17 as an alternative to the annual in-person events due to COVID-19.
The pandemic has resulted in a massive and rapid increase in the need for telehealth implementation across the globe, to maintain access to care while physically distancing to protect public health. This virtual event will benefit anyone interested in telehealth and will help your practice ramp up quickly. Learn more and register here.
BONUS opportunity…
"The Talk". You may be familiar with the phrase, ‘the talk,’ referring to a conversation Black parents have with their kids about how to act in the world around white people, especially law enforcement.
Given recent events, Playwright and performer Sonny Kelly’s one-person show, "The Talk," is available to stream until July 10. This one-and-a-half hour production examines the difficult conversation a father must have with his son in a racially-divided America.
Watch here.
If you have policies you'd like your NCMS Board of Directors to consider, please complete the Board input form here. Thanks for reading!
HB 1053/ SB 717 Military Occupational Licensure/Audiology Compact
HB 1053/ SB 717 Military Occupational Licensure/Compact
Primary House Sponsor: Rep. Craig Horn (R-Union)
Primary Senate Sponsor: Sen. Rob Bryan, Sen. Andy Wells (R-Catawba), Sen. Don Davis (D-Pitt)
Summary
This bill would require an expedited occupational licensure application response of 30 days when an applicant is military trained or is a military spouse. The bill would also require each occupational licensure board and the Department of Military and Veterans Affairs’s websites to summarize the opportunities available to veterans and spouses.
The proposed committee substitute presented to the Commerce and Insurance Committee would require an application response within 7 days instead of 30 days.
The proposed committee substitute introduced in the House Judiciary Committee included new language for the audiology interstate compact.
History
- Filed 5/13/20
- Senate Commerce and Insurance Committee - favorable report 5/26/20
- SenateRules Committee - favorable report 5/28/2020
- Passed in the Senate 47-0 with a floor amendment 6/1/2020
- This bill will now move to the House
- This bill was received in the House on 6/3/2020
- This bill passed in the House Judiciary Committee on June 4, 2020
- This bill was referred to the House Rules Committee on June 4, 2020
- This bill passed the House Rules Committee on June 9, 2020
- This bill passed the House on June 10, 2020.
- This bill passed the Senate Commerce and Insurance Committee on June 17, 2020
- This bill passed in the Senate on June 19, 2020
SB 708 - CPS Intake Screening/PED Recommendations
SB 708 - CPS Intake Screening/PED Recommendations
Primary Sponsors: Sen. Chuck Edwards (R-Buncombe), Sen. Joyce Kraweic (R-Forsyth), Sen. Jim Burgin (R-Harnett)
Summary
This bill prohibits county departments of social services from implementing child protective services intake screening criteria that is more stringent than, or in addition to State policy and directs DHHS to make various policy changes as a means to improve intake screening process, as recommended by the Joint Legislative Program Evaluation Committee.
View the full study here.
History
Filed 4/30/2020
Passed Senate Judiciary Committee 6/9/2020
Passed Senate Health Committee 6/17/2020
Passed Senate Rules Committee 6/17/2020
This bill passed on the Senate floor on 6/19/2020
SB 848 - COVID-19 Economic Recovery Grants
SB 848 - COVID-19 Economic Recovery Grants
Primary Sponsors: Sen. Paul Newton (R-Cabarrus), Sen. Ralph Hise (R-Madison), Sen. Jerry Tillman (R-Randolph)
Summary
This bill provides $200,000,000 in funding and economic support to businesses for job retention, recruitment and repatriation during and after the COVID-19 pandemic.
The maximum grant amount would be up to two months of the business's average monthly payroll costs from the last year plus 25% of that amount. This amount could not exceed $500,000.
The bill also appropriates $50,000,000 to be used for the COVID-19 Job Retention Program.
History
- Filed 5/26/20
- Senate Finance - Passed 6/11/2020
- Senate Appropriations - Passed 6/17/2020
- Senate Rules Committee - Passed - 6/19/2020
HB 902 - Temp Open Clubs & Similar Outdoor Establishments
HB 902 - Temp Open Clubs & Similar Outdoor Establishments
Primary Sponsors: Rep. Holly Grange (R-New Hanover), Rep. John Bell (R-Wayne)
This bill was previously a bill to study military occupational licensing reforms.
This bill was transformed into a beverage service bill in the Senate Commerce and Insurance Committee on May 26, 2020.
This bill passed in the Senate Finance Committee on June 16, 2020.
Summary
- Authorizes establishments to operate outdoor beverage service options while following certain guidelines.
- The services would be limited to outdoor seating.
- The seating location would need to be in the same proximity as the establishment.
- The outdoor seating capacity would be limited to 50% of current indoor seating capacity.
- The establishment would be required to comply with all rules and regulation promulgated by the Division of Public Health.
HB 1105 - COVID/Supplementary GREAT Grant Period
HB 1105 - COVID/Supplementary GREAT Grant Period
Primary Sponsors: Rep. Dean Arp (R-Union), Rep. Jason Saine (R-Lincoln), Rep. Brenden Jones (R-Columbus), Rep. Robert Reives (D-Durham)
Summary
This bill provides funding to the Department of Information Technology to expedite and expand broadband infrastructure in the State with a supplementary grant period for the GREAT (Growing Rural Economies with Access to Technology) program. Eligible counties include tier 1 and 2 areas and rural census tracts in tier 3 counties. Single grant awards can not exceed $2.8 million. No single county can be awarded more than $5.6 million.
Appropriations:
- $30 million for the Coronavirus Relief Fund to be used for these grants.
History
Filed - 5/14/2020
Passed House Appropriations Committee: 6/17/2020
Passed House Rules Committee: 6/18/2020
NCMS Morning Rounds 6-18-20
It's Thursday and time for your
NCMS Morning Rounds.
June 18, 2020
The NC General Assembly is in session and the NCMS advocacy staff is closely tracking its work. Keep up-to-date on what could impact your practice and your patients at our Legislative blog. The blog is continually updated with behind-the-scenes, quick summaries as the proposed legislation makes its way through the various committees and floor votes. Go to the NCMS Legislative Blog.
Reflections on Attending George Floyd’s Service in Raeford
As a local public official and prominent community member, Karen Smith, MD, had a front-of-the-house seat for the private memorial service for George Floyd held in Raeford on June 6. Mr. Floyd’s horrific death at the hands of the Minneapolis police has prompted worldwide protests over racial injustice and prompted an outpouring of emotion at the services held in Raeford, near where he was born.
A longtime NCMS member, family physician in Raeford and medical director for the Hoke County Health Department, Dr. Smith was struck by the deep symbolism of Mr. Floyd’s service there.
Mr. Floyd’s relatives, dressed in white, sat on one side of the chapel while the attending dignitaries had been instructed to wear black and were seated on the other side. Mr. Floyd’s shining gold casket was wheeled down the center aisle.
“What a chariot,” Dr. Smith said. “White on one side; black on the other. What a dichotomy! Did these people know each other? How they live, work, what their issues are? Mr. Floyd’s casket in the middle was like a spark to open conversations. His death has opened up these conversations.”
For instance, Harvey Godwin, Jr., chairman of the Lumbee Tribe, addressed the historically co-existing Lumbee and African American communities, both with disproportionately higher vulnerable populations. At the service, he offered a proclamation from the tribe recognizing “that unity and solidarity between the Black and Lumbee communities is necessary to fight” against social and racial injustice. Read the Lumbee Tribe’s Unity Proclamation presented to Mr. Floyd’s family.
Also as part of the service, US Congressman G.K. Butterfield extended condolences to Mr. Floyd’s family “on behalf of the 55 men and women who are part of the Congressional Black Caucus. These leaders have pushed the US House to introduce the Justice in Policing Act.
Dr. Smith sees this time as a “magical moment.” Although racial injustice has a long history in this country, she views the events of the last several weeks as transformational. Like Cinderella being magically made over from rags into a princess, this country will not ever be able to fully return to what it was before thanks to the sad ‘spark’ of George Floyd’s death, she said.
“It’s an internal dream we all have,” Dr. Smith said. “We don’t want to go back.”
Dr. Smith urged everyone to “look at the mission statement of every organization you’re a part of. Look at every policy and procedure. If you see barriers to recognizing diversity – get rid of them.”
Key to a true transformation is being able to see individual human beings, Dr. Smith said.
Those who spoke at Mr. Floyd’s service “personified him as a gentle giant – a man, a brother, a father, a son,” she said. She recalled a recent personal encounter with a new patient. When Dr. Smith entered the exam room, the white patient was clearly taken aback by her race and initially seemed skeptical of her abilities. After conversing for a bit, the patient decided Dr. Smith seemed like “a happy person and could help her with her diabetes.”
“We have to start with what we have in common,” Dr. Smith said. “We have more similarities than differences.”
White Coat Wednesday and Staying Engaged in Advocacy
Yesterday several Kanof Institute for Physician Leadership (KIPL) class of 2020 Leadership College scholars participated in our NCMS virtual White Coat Wednesday – a way to stay engaged in advocating for your profession especially during these times of uncertainty.
NCMS Director for Legislative Relations Sue Ann Forrest, MPA, briefed Zachary Fleming, a medical student at the Campbell University School of Osteopathic Medicine and Marion McCrary, MD, FACP on the many bills currently under consideration by the General Assembly that the NCMS is tracking; answered their questions and gave tips and talking points for their virtual conversations with legislators.
Virtual White Coat Wednesdays offer you the opportunity to stay engaged in our advocacy efforts as legislators weigh important proposals around responding to the pandemic, Medicaid transformation and others that could impact your practice. Now that they are offered remotely, you have more flexibility in when you can participate. Learn more about how to get involved and sign up for a virtual White Coat Wednesday here.
Forrest also gave a 2-hour advocacy update to the LINC Scholar program at ECU’s Brody School of Medicine earlier in the week and several of the students also participated in White Coat Wednesday-type advocacy throughout the week. NCMS Immediate Past President Timothy Reeder, MD, MPH, FACEP is faculty for the LINC program.
Thank you to those who participated this week!
PAI Survey: High-Deductible Health Plans Are Barrier to Care
The results of a survey released last week by NCMS partner the Physicians Advocacy Institute (PAI) revealed that four out of five independent physicians in the United States (80 percent) say their patients refuse or delay medical care due to concerns about cost, and just as many (79 percent) say that high insurance deductibles are a leading cause. The findings come from a survey of more than 700 independent physicians nationwide administered by NORC at the University of Chicago for PAI.
Conducted prior to the COVID-19 pandemic, the survey offers insight into how high-deductible health plans (HDHP), which make patients financially responsible for thousands of dollars in health care costs, are leading physicians to change the way they care for patients.
Other key findings include:
• 55 percent of the independent physicians surveyed said patients’ cost concerns are causing them to alter their preferred approach to the timing of treatments provided
• 66 percent have changed their decision about whether to prescribe drugs;
• 61 percent changed the type of medical treatment provided; and
• 86 percent have changed which type of drugs they prescribe.
• Most say their office staff spends more than 300 hours per year educating patients about their insurance coverage. Yet three-out-of-four independent physicians (75 percent) say they don’t have most of the information they need to have cost of care conversations.
As COVID-19 transitioned from epidemic to pandemic, the Internal Revenue Service issued regulations to require insurers to suspend cost sharing, where patients shoulder all or a portion of the cost for medical services, under high-deductible and other types of insurance plans. No longer having to worry about affording COVID-19 related expenses, more patients received immediate or timely access to essential coronavirus testing and treatment.
Review the key findings of the survey here.
In the News
Missing Data Veils Coronavirus Damage to Minority Communities, Politico, 6-14-20
Learning Opportunity
Southern Regional AHEC is offering a livestream webinar on Saturday, July 25 from noon to 1:30 p.m. titled ‘A Critical Conversation: Listening and Learning Together.’
The persistent and pervasive injustices to black and brown people and other multicultural populations have long been documented over many generations. Persons of color continue to experience health disparities at an alarmingly disproportionate rate as evidenced by recent and historical acts of racism, violence, inequities and power paradigms. While many are sensitive to and saddened by these unfortunate realities, civil unrest across the nation has driven a call to action. The purpose of this activity is to facilitate a critical yet necessary conversation surrounding race relations, providing an open space for dialogue and bridging gaps at the public sector level, so that communities can listen and learn together. Learn more and register here.
If you have policies you'd like your NCMS Board of Directors to consider, please complete the Board input form here. Thanks for reading!
HB 1050 - PED/Low Performing School Districts
HB 1050 - PED/Low Performing School Districts
Primary Sponsors: Rep. Craig Horn (R-Union), Rep. John Fraley (R-Iredell), Rep. Ashton Clemmons (R-Guilford)
Summary
This bill would require that plans for improvement and comprehensive needs of low-performing local school administrative units include consideration and examination of early child hood learning.
History
Filed - 4/29/2020
Passed - House Education K-12 Committee - 6/2/2020
Passed - House Floor - 6/4/2020
Passed - Senate Higher Education - 6/17/2020
Referred to Senate Rules 6/17/2020
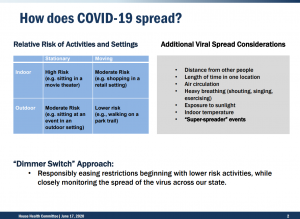
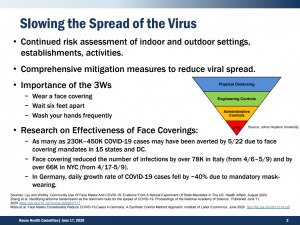
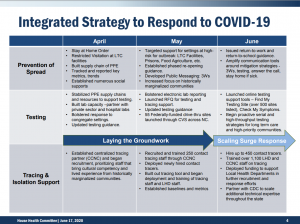
House Health Committee - COVID-19 Update
The NCGA House Health Committee met on Wednesday, June 17, 2020.
NCDHHS Secretary, Dr. Mandy Cohen provided an update on the COVID-19 pandemic. View her presentation here.
Most of the Committee was spent with Secretary Cohen answering specific questions from legislators.
NCMS Morning Rounds 6-18-20
The week is half over! Enjoy your Wednesday
NCMS Morning Rounds.
June 17, 2020
The NC General Assembly is in session and the NCMS advocacy staff is closely tracking its work. Keep up-to-date on what could impact your practice and your patients at our Legislative blog. The blog is continually updated with behind-the-scenes, quick summaries as the proposed legislation makes its way through the various committees and floor votes. Go to the NCMS Legislative Blog.
NC Medicaid Implements 5 percent Rate Increase
The NC General Assembly’s recently approved HB 1043—2020 COVID-19 Recovery Act includes a 5 percent rate increase for all Fee-For-Service (FFS) Medicaid providers who had not yet received a 5 percent increase during the COVID-19 public health emergency.
The rate increases are effective March 1, 2020, and will be applied retroactively to claims already submitted with a date of service on or after March 1, 2020. This increase will end when either the nationwide public health emergency expires; the state’s Declaration of Emergency related to COVID-19 ends or March 31, 2021, whichever comes first.
The rate increases only applies to Medicaid and NC Health Choice services billed through NCTracks and do not apply to behavioral health and I/DD services billed to local management entities/managed care organizations (LME/MCOs). Only those providers who have not previously received rate increases implemented under the Medicaid Disaster State Plan Amendment (SPA) submitted to the Centers for Medicare & Medicaid Services (CMS) in April are eligible for this rate increase.
More information is available in SPECIAL BULLETIN COVID-19 #99: North Carolina General Assembly Mandates Temporary 5 percent Rate Increase for Certain Medicaid Providers.
NC HealthConnex Goes National
NC practices will now be able to receive information when patients present at certain out of state emergency rooms or for inpatient stays thanks to a connection between NC HealthConnex and other participating Health Information Exchanges (HIE) across the nation via the Patient Centered Data Home (PCDH).
The PCDH is a secure health data exchange initiative that can help patients by proactively alerting their health care providers when they have a health event away from home. The patient’s health records can be available wherever and whenever they need them to ensure those treating them have access to real-time information and eliminates potential gaps in care when a patient is seen outside of their normal care area across state lines. The system proactively will notify NC HealthConnex when a care event has occurred outside of the patients’ ‘home’ HIE.
Today is #WellChildWednesday
Leveraging social media as a positive force, the Health Resources and Services Administration (HRSA) is asking physicians, PAs, patients and the concerned general public to post and link to #wellchildwednesday today as a way to encourage keeping up with regular pediatric checkups and immunizations.
The data shows that due to the COVID-19 pandemic, fewer children are receiving timely immunizations this year compared to last year. To encourage parents and stakeholders to keep up with these important well-child visits and immunizations, HRSA launched a new social media campaign with the hashtag #WellChildWednesdays.
Each Wednesday for four weeks, messages will address well-visits, immunizations, adolescent and young adult care, and nutrition, safety, and mental health as topics to be discussed with pediatric providers.
The first message will be posted today, Wednesday, June 17, and more messages will appear on Twitter and Facebook with the handle @HRSAgov and #WellChildWednesdays. Please share, retweet, and promote the hashtag #WellChildWednesdays to help amplify this important message!
In the News
‘An Obligation’: Doctors and Other Health Workers Increasingly See Protesting Racial Injustice as Part of the Job, STAT, 6-16-20
Learning Opportunity
This week’s Power Hour on Friday, June 19 from 1 to 2 p.m. will bring together practice managers and owners to discuss their experiences in keeping their practice afloat during these particularly challenging times, how the reopening process has been going and what the future may hold. Learn more and register here for this engaging conversation with your colleagues.
The KIPL Power Hour aims to provide a forum for ongoing conversation, collaboration and community. Tune in to Power Hour weekly to hear from different experts, decision makers and influencers on a variety of topics. The format is informal and conversational and sessions are easy to access through Zoom. Power Hours will be recorded and made available to you through your NCMS Morning Rounds and on the KIPL webpage.
If you have policies you'd like your NCMS Board of Directors to consider, please complete the Board input form here. Thanks for reading!
SB 803 - Capital Appropriation - Repairs and Renovations
SB 803 - Capital Appropriation - Repairs and Renovations
Primary Sponsors: Sen. Harry Brown (R-Onslow), Sen. Kathy Harrington (R-Gaston), Sen. Brent Jackson (R-Sampson)
Summary
This bill would appropriate $119,000,000 in non recurring funding for repairs and renovations for the UNC System institutions and State agencies.
An amendment was added on June 15, 2020 to include the following:
- $2.5 million to the Department of Natural and Cultural Resources for contextual signage for existing monuments on the State Capitol grounds and additional monuments representing the lives and contributions of African Americans in the state as recommended by the NC Historical Commission
- $1.5 million as a directed Grant to the NC Freedom Monument Project to build a sculpture on land located between the legislative buildings and the Governor's Mansion
History
Filed - 5/19/2020
Passed in Senate Appropriations as Committee Substitute on 6/10/2020
Passed Senate Rules on 6/11/2020
Passed Senate on 6/15/2020
NCMS Morning Rounds 6-16-20
Happy Tuesday! Here is today's
NCMS Morning Rounds.
June 16, 2020
The NC General Assembly is in session and the NCMS advocacy staff is closely tracking its work. Keep up-to-date on what could impact your practice and your patients at our Legislative blog. The blog is continually updated with behind-the-scenes, quick summaries as the proposed legislation makes its way through the various committees and floor votes. Go to the NCMS Legislative Blog.
Update on Paycheck Protection Program
The Small Business Administration (SBA) recently issued regulations to begin implementation of the new Paycheck Protection Program (PPP) Flexibility Act, which was signed into law on June 5. The Act relaxes many of the rules for qualifying for the PPP loan forgiveness that were contained in the original PPP. Read the regulations here.
New PPP flexibilities include:
• Current PPP borrowers can choose to extend the eight-week “covered period” to 24 weeks, or they can keep the original eight-week period. New PPP borrowers will have a 24-week covered period, but the covered period can’t extend beyond Dec. 31, 2020. This flexibility is designed to make it easier for more borrowers to reach full, or almost full, forgiveness.
• The Act changes the threshold for the amount of PPP funds required to be spent on payroll costs to qualify for forgiveness from 75 percent to 60 percent of the loan amount.
• Borrowers can restore their workforce levels and wages to the pre-pandemic levels required for full forgiveness by Dec. 31, a change from the previous deadline of June 30.
• New borrowers now have five years to repay the loan instead of two. Existing PPP loans can be extended up to 5 years if the lender and borrower agree. The interest rate remains at 1 percent.
Learn more about the updated PPP here, where you will also find a new borrower application and a state-by-state listing of lenders.
We Need Health Care Leaders -- Like You!
As our country grapples with the COVID-19 pandemic in addition to the many other challenges facing our health care system, the need for health care professionals with exemplary leadership skills is growing. The NCMS Foundation’s Kanof Institute for Physician Leadership (KIPL) offers an award-winning array of leadership development programs to help you gain insight into your unique leadership talents and empower you to use them to improve our health care system and the health of your patients.
Currently, the Leadership College and Health Care Leadership and Management (HCLM) programs are accepting applications for class of 2021 scholars. Both programs plan to proceed as usual with in-person sessions in the coming year, but also can be held virtually, if necessary.
Learn more about these valuable opportunities at the KIPL webpage and consider applying for this chance to enhance your understanding of your leadership potential and how to leverage it to the benefit of your larger community.
AMA and CDC Joint Survey on Infection Control
The American Medical Association (AMA) and the Centers for Disease Control and Prevention (CDC) are collaborating on an infection prevention and control training initiative for frontline health care personnel. In order for this training to be as responsive to the needs of physicians as possible, the AMA and CDC are asking you, physicians and PAs, to complete this survey on infection prevention and control training interests, needs and preferences. The survey should take less than 10 minutes to complete.
Responses will be used to inform decisions on the development and delivery of training to ensure it best meets your needs. The deadline is 11:59 p.m on June 23, or until the it receives 10,000 responses.
Thank you for your time and all you do to keep your colleagues and patients safe.
In the News
COVID-19 Update: Testing FAQs, the Latest on Vaccine Trials, MedScape, 6-12-20
Learning Opportunity
‘When Will Patients Return and What Role Will Telehealth Play?’ If you have asked yourself these questions, you may be interested in a webinar hosted by NCMS partner Zocdoc next Tuesday, June 23 at 1 p.m. The session will examine what can be learned from patient behavior in states like Georgia and Florida that have already reopened and how can health care practices use this data to plan for recovery? This webinar shares new insights on these questions and more based on Zocdoc patient booking data before, during and after closures – and surprising ways trends differ by location and specialty. Learn more and register.
If you have policies you'd like your NCMS Board of Directors to consider, please complete the Board input form here. Thanks for reading!
NCMS Morning Rounds 6-15-20
Enjoy your first
NCMS Morning Rounds of the week.
June 15, 2020
NCMS Legislative Update
Last week saw a flurry of activity at the NC General Assembly with multiple committee meetings and legislation moving.
A few items of note:
• SB808 – Medicaid Funding Act This proposal was previously called Medicaid Transformation Necessities, but is now the Medicaid Funding Act. The Senate Appropriations Committee did hear it last week. Among its many provisions it sets the go-live date for the state’s move to Medicaid managed care to July 1, 2021.
• The House Health Committee heard from NC Department of Health and Human Services (NCDHHS) Secretary Mandy Cohen, MD, MPH, this week on the state’s response to the COVID-19 pandemic. Read a summary of the questions and discussion with Sec. Cohen and access her presentation here.
• HB1169 – Bipartisan Elections Act is now on the Governor’s desk awaiting his signature. This bill seeks to help ensure public health and safety during the November election in light of the current pandemic.
As activity ramps up, it may signal the session is coming close to an end – at least for now. In the meantime there is much behind the scenes activity that the NCMS advocacy team is keeping up with. Be sure to watch our legislative blog for updated information on the bills we’re tracking.
Policy Committee Sends Two Recommendations to NCMS Board
The NCMS Policy Committee met for its second quarter meeting last Wednesday, June 10 and approved two new policies after robust discussion. The committee recommended to the NCMS Board of Directors for consideration policies on:
The Board of Directors will consider these recommendations at their upcoming meeting later this week.
The Policy Committee’s next meeting will focus on health equity. As a roadmap for its work, the Policy Committee uses the NCMS Guiding Principles, which the committee developed and the NCMS Board of Directors approved last January. Committee members consider key policies through the lens of these principles.
NCMS Partner Mako Medical Offers Test Kits
Mako Medical Laboratory is generously providing 20,000 COVID-19 test kits to NCMS members.
“We are thrilled that our Project OBOT partner, Mako Medical Laboratory, has been able to make available these tests to NCMS members and other health care providers,” said NCMS Vice President for Rural Health Systems Innovation Franklin Walker, MBA. Walker leads the NCMS’ Project OBOT, a collaborative approach to treating opioid use disorder.
You do not need to have a contract with Mako to take advantage of the offer. Simply fill out the online form requesting the tests and Mako will send the tests with a return FED EX to send the tests back to the lab. Once the online form has been completed, a Mako representative will contact your practice.
With the NC Department of Health and Human Services (NCDHHS) urging more testing and expanding the guidelines for those who should be tested, this donation by Mako offers an easy way to access the necessary testing supplies.
Learn more and order your COVID-19 tests here.
In the News
What We Know (and Don’t Know) About Asymptomatic Spread, The Advisory Board Forum, 6-11-20
Learning Opportunity
The Durham Orange County Medical Society had a well-attended virtual dinner meeting on the topic of LGBTQ + Health at its meeting last week. Watch the recorded presentations and discussion here to learn more about this important subject.
Speakers included Tonia Poteat, PhD, PA-C, MPH from the UNC Department of Social Medicine; Kristen Russell, LCSW, MSW, Child Development and Behavioral Health Specialist, Clinical Social Worker at Duke Health; and Dane Whicker, PhD, Medical Instructor in the Department of Psychiatry and Behavioral Sciences, Duke University School of Medicine
Don’t forget tomorrow’s, Tuesday, June 16, NCMS Foundation/NC Medical Group Management Association Lunch & Learn Webinar from noon to 1 p.m., which will feature presenters from the Seniors’ Health Insurance Information Program (SHIIP) speaking on ‘Medicare 2020: Navigating the Unprecedented Waters Together!’ Just when we thought the ever-changing world of healthcare was manageable, along comes a global pandemic. Join us for a conversation focusing on the SHIIP mission to assist Medicare beneficiaries in safeguarding their healthcare benefits as well as serving as a resource to practice managers in North Carolina. Learn more and register.
If you have policies you'd like your NCMS Board of Directors to consider, please complete the Board input form here. Thanks for reading!
NCMS Morning Rounds 6-12-20
Happy Friday! Enjoy your
NCMS Morning Rounds.
June 12, 2020
Practice Reopening Considerations
As practices throughout the state encourage patients to once again seek care for non-emergent issues and routine check-ups, the Centers for Medicare and Medicaid Services (CMS) released guidelines for practices and patients to safely reopen.
Read CMS’ facility guidelines and its guide for patients.
The NCMS, along with our partners the NC Medical Group Management Association and Curi, recently surveyed our members on what they are experiencing as they fully reopen. The results reveal that 69 percent of your responding colleagues had a least a few patients who expressed reluctance about scheduling an in-person visit. See a summary of the survey results here.
The NCMS Board of Directors have initiated a letter-to-the-editor campaign encouraging patients in their communities not to forego routine care. NCMS Immediate Past President Timothy J. Reeder, MD, MPH, FACEP recently had his letter published in his community newspaper, the Greenville Reflector. Read his letter.
Having good solid information on COVID-19 in North Carolina is key to successful planning and understanding the virus’ spread. The state recently announced that data from the NC Department of Health and Human Services (NCDHHS) COVID-19 dashboard is now downloadable and computable for your county or zip code and by demographics. You an learn more about these new functions and view the latest data here.
Another resource to consider as the state responds to the pandemic and practices reopen is this issue brief from the Robert Wood Johnson Foundation, “Health Equity Principles for State and Local Leaders in Responding to, Reopening and Recovering from COVID-19.” These principles are billed as “a compass that continually points leaders toward an equitable and lasting recovery.”
As an organization dedicated to ‘leadership in medicine,’ and to pursuing health equity, the NCMS seeks to provide the information and resources to empower you to make educated and thoughtful decisions.
NC Medical Board News
The latest issue of the NC Medical Board’s Forum newsletter has been published and includes several heartfelt messages from NCMB President Bryant A. Murphy, MD, MBA and NCMB CEO R. David Henderson, JD, responding to the recent national event, including the death of George Floyd and the unrest that followed.
Read these messages and all the NCMB's news in the latest edition of the NCMB’s Forum here.
NCMS Urges Congress to Pass Provider Protections
The NCMS was among dozens of other state medical and specialty societies to sign on to a letter to Congressional leadership urging them to include liability protections for physicians in the next COVID-19 relief package. In particular, the letter praises the provisions included in a bipartisan bill, HR7059, the ‘Coronavirus Provider Protection Act.'
"During this unprecedented national health emergency, physicians and other health care professionals have been putting themselves at risk every day while facing shortages of medical supplies and safety equipment, and making critical medical decisions based on changing directives and guidance,” the letter states. “These physicians and other health care professionals are now facing the threat of years of costly litigation due to the extraordinary circumstances.”
The liability protections sought are intended to provide targeted and limited protections where health care services are provided or withheld in situations that may be beyond physician control. The protections extend to those who provide care in good faith during the COVID-19 public health emergency and not in situations of gross negligence or willful misconduct.
In the News
The Biggest Psychological Experiment in History is Running Now, Scientific American, June 2020
Learning Opportunity
Don’t forget to tune into TODAY’S Power Hour from 1 to 2 p.m. to hear the medical student perspective on the response to COVID-19 and what it has meant to their medical education. Sign up here.
Also, on Monday, June 15 at 2 p.m. the Society of General Internal Medicine (SGIM) Health Equity Commission will present ‘Lessons Learned from the Past: Addressing COVID-19 Disparities for a More Equitable Future.’ COVID-19 has shed a bright light on the deeply rooted inequities in our health system. Health equity experts, and SGIM colleagues will share why it is critical to address racial and ethnic disparities during this pandemic and how we can use this moment to advance health equity in a post-COVID future. Register to attend this webinar here.
If you have policies you'd like your NCMS Board of Directors to consider, please complete the Board input form here. Thanks for reading!
HB 1169 - Bipartisan Elections Act of 2020
HB 1169 - Bipartisan Elections Act of 2020
Primary Sponsors: Rep. Holly Grange (R-New Hanover), Rep. Destin Hall (R-Caswell), Rep. Allison Dahle (D-Wake), Rep. Pricey Harrison (D-Guilford)
Summary
This bill allows for the 2020 general election, for one witness signature for the casting of an absentee ballot instead of two signatures.
The bill allows for completed absentee requests to be emailed or faxed to county boards of elections.
The bill requires DHHS and the State Board of Elections to develop a program on how to safely allow multi-partisan teams to assist registered voters within a congregate living situation durign the 2020 elections.
The bill requires ballots to have a bar code allowing the county board of elections and the voter to track a voted ballot following its return to the county board.
The bill allows an additional 2 weeks to approve applications for absentee ballots.
The bill requires the State Board to create an online portal for voters to submit online requests for absentee ballots by September 1, 2020.
The bill also appropriates funds to the State Board of Elections to respond to COVID-19.
History
- Filed 5/22/2020
- Favorable Committee Substitute - Elections Committee 5/27/2020
- Favorable Committee Substitute - Rules Committee 5/27/2020
- Passed House 116-3
- Passed Senate Redistricting on 6/2/2020 - Amended
- Passed Senate Appropriations - 6/2/2020 - Amended
- Passed Senate Rules 6/9/2020
- Passed Senate with amendments on second reading 6/10/2020
- Passed Senate on third reading on 6/11/2020
- House concurred with the Senate changes with a vote of 105-14 on 6/11/2020
- The bill was presented to the Governor on 6/11/2020
HB 463 - Education in Prisons
Primary Sponsors: Rep. David Rogers (R-Burke), Rep. Mark Brody (R-Anson), Rep. John Hardister (R-Guilford), Rep. Joe John (D-Wake)
Summary
This bill would provide access to education for individuals incarcerated in state prisons. The bill would remove current law that prohibits funds appropriated for community college courses to be used for Associate of Arts, Associate of Science, or Associate of General Education degrees.
History
- Filed - 3/26/2019
- Passed - House Education Community Colleges Committee on June 6, 2019
- Passed - House Rules - June 24, 2019
- Passed - House floor (112-0) 6/25/2019
- Sent to Senate 6/26/2019
- Passed - proposed committee substitute - Senate Education/Higher Education 6/10/2020
- Referred to Senate Appropriations 6/10/2020
- The bill was withdrawn from Senate Appropriations and re-referred to the Senate Rules Committee 6/10/2020
HB 536/SB 592 - Temporary Outdoor Restaurants for Outdoor Seating
HB 536/SB 592 - Temporary Outdoor Restaurants for Outdoor Seating
Summary
This bill would authorize certain existing establishments to offer and operate outdoor dining and beverage service options while considering public health to prevent the spread of COVID-19.
The following provisions would apply:
- Requirement to be defined in statute as a private club, private bar, winery, or distillery
- Outdoor seating capacity is limited to 50% or 100 customers (whichever is less)
- Access to toilet facilities
- Establishment holds ABC permits with vertical boundaries indicating the line from the facility from the public
- Establishment enforces CDC and DHHS social distancing requirements
- Establishment complies with all DHHS outdoor food service regulations
History
This bill was introduced and passed with the current topic in the Senate Commerce and Insurance Committee on May 26, 2020.
- Passed - Senate Rules Committee - May 28, 2020
- Passed - Senate Floor 42 -5 - May 28, 2020
- Concurred - House Floor 65-53 - May 28, 2020
- Vetoed by Governor Cooper - June 8, 2020
- Placed on House Calendar for June 10, 2020
- Referred to the House Rules Committee on June 10, 2020.
NCGA House Health Committee
The NCGA House Health Committee met on Wednesday, June 10, 2o20, at 10:00am.
NCDHHS Secretary, Dr. Mandy Cohen, MD provided a COVID-19 overview.
Data Update
Currently, there are 37,160 laboratory confirmed cases.
- 1,029 deaths
- 525,711 completed tests
- 774 currently hospitalized
She noted that an estimated 51% of adults in NC are at higher risk for severe illness from COVID-19 based on being 65 or older, one underlying health health conditions, or both.
Contact Tracing
There are over 1,100 staff users who have completed the State-led training on contract tracing. 252 additional contact tracers have been hired through Community Care of NC to increase diversity.
Slow the Spread
She stated that North Carolinians can slow the spread of the virus by:
- Wear. Wait. Wash.
- Getting tested when needed.
- Answering the call so that others that may have been exposed get support and resources.
Schools
NCDHHS has worked closely with the NC Department of Public Instruction and the NC State Board of Education to plan for reopening schools for the 2020-21 school year. This includes the StrongSchoolsNC Public Health Tooolkit (K-12) which lays out baseline health practices to minimize COVID-19 exposure.
Executive Order 145 - Racial Equity in Criminal Justice Task Force
On Tuesday, June 9, 2020, Governor Roy Cooper signed Executive Order 145 to establish the North Carolina Task Force for Equity in Criminal Justice. This group will be led by Supreme Court Justice Anita Earls and NC Attorney General, Josh Stein.
The task force's goal will be to develop and implement strategies to help eliminate racism in our criminal justice system.
Cooper stated that NC Public Safety Secretary, Erik Hooks, has directed all state law enforcement agencies under the Department to ensure they have a clear duty to intervene policy. He clarified that his policy means if an officer sees a fellow officer doing wrong, they must step in.
Agencies have been instructed to review their existing policies including arrest procedures, use of force, and de-escalation.
NCMS Morning Rounds 6-9-20
Happy Tuesday! Enjoy your
NCMS Morning Rounds.
June 9, 2020
NCMS Student Section Update
The NCMS is proud to periodically share the work of the medical student leaders in our Student Section. The NCMS Student Section was founded this year with the goal of shaping the future of medicine in North Carolina through medical student involvement and non-partisan collaboration among all state medical schools. Student leaders at institutions across our state have been working tirelessly to respond to the COVID-19 pandemic, as medical schools adjust clinical rotations, graduation requirements and the future of medical education at large in 2020.
This week, NCMS Student Section leaders from Wake Forest School of Medicine offer the following update from their campus. In coming weeks, other schools will be represented.
The COVID-19 pandemic has impacted us all, and it has been a particularly interesting time for medical education. Despite having their schedules altered and being taken out of their clinical rotations, medical students have risen to the occasion and have worked hard to give back to their communities during this pandemic. Here at Wake Forest School of Medicine, we have focused on serving those in our community who have barriers to accessing multitudes of resources, and aiding the faculty, staff, and patients at our institution. A group of students got together and created a COVID-19 Student Literature Review, in an effort to create a resource for students and physicians that makes the rapidly evolving research on COVID-19 more accessible.
Our student-run clinic, Delivering Equal Access to Care (DEAC) Clinic, checked up on and assessed for food insecurity among their patients, through telehealth. They garnered funding for a grocery delivery program, and were able to follow up with their food insecure patients and make a one-time online grocery delivery to their homes.
Through Wake Forest Baptist Health’s House Call Program, student volunteers called over 100 homebound older adults to address potential concerns over stress management, food insecurity, social isolation, and emotional responses during this pandemic.
Lastly, medical students are helping to screen those entering Wake Forest Baptist Medical Center for potential COVID-19 symptoms/exposures and high temperatures.
If you are a medical student and would like to learn more about the activities of the NCMS Student Section, please reach out to NCMS Director, Member Services Richard Simpson at [email protected].
NC Medical Board Seats Open for Nominations
The NC Medical Board has three open seats and the Review Panel for the NCMB is now accepting nominations for those positions through July 1. Under state law, one of the available seats must be filled by a member of the Old North State Medical Society. Two of the physician Board members currently serving are eligible for reappointment; one incumbent physician Board member is not eligible for reappointment.
The Review Panel, which is independent of the NCMB, will interview qualified applicants Aug. 22 and 23. The three-year terms for the open positions on the Board would begin Nov. 1.
You may submit an application for an open position here.
NCMS Offers Advocacy Update to Alamance County
NCMS Director of Legislative Relations Sue Ann Forrest, MPA, is offering physicians and PAs in and around Alamance County and beyond an update on the NCMS’ current advocacy efforts tonight, Tuesday, June 9 at 7 p.m.
The update, which will include information on COVID-19, Medicaid transformation, the State Health Plan and the November elections including local legislative races, will be offered virtually via Zoom at this link, meeting password: 184148. Or call in at 1-301-715-8592 and enter 87661269792#, then 1# and the meeting password, 184148#. All are welcome whether you live in Alamance County or not.
NCMS advocacy staff seeks to keep members informed and involved in our efforts on your behalf through meetings like this one as well as our regularly updated legislative blog, our weekly Political Pulse video and the opportunity to engage directly with legislators in an informed and thoughtful way through our White Coat Wednesdays. Due to the COVID-19 pandemic and the need to socially distance, we have adapted to make White Coat Wednesday and meetings like today’s advocacy update available remotely.
In the News
On the Minds of Black Lives Matter Protesters: A Racist Health System, ProPublica, 6-5-20
Learning Opportunity
‘Communications Challenges Surrounding the COVID-19 Pandemic’, a live webinar presented by the Region IV Public Health Training Center, will be held this Thursday, June 11 from noon to 1:30 p.m. The pandemic continues to present huge challenges to our public health system. One challenge has been huge behavioral changes and long term cooperation necessary on the part of the public at large. This webinar will address how to successfully communicate and persuade during the COVID-19 pandemic including the need for clear, consistent, credible and apolitical communication and looking ahead to the development of a successful vaccine, and public health campaigns to accept vaccination especially in communities which have traditionally had low vaccination rates. Learn more and register here.
HB 1079/SB 718 - Sales Tax Changes
HB 1079/SB 718 - Various Sales Tax Changes
House Primary Sponsors: Rep. Julia Howard (R-Davie), Rep. Stephen Ross (R-Alamance), Rep. Mitchell Setzer (R-Catawba), Rep. John Szoka (R-Cumberland)
Senate Primary Sponsors: Sen. Paul Newton (R-Cabarrus)
Summary
The bill contains three parts:
- Relief to auctioneers and estate sale companies
- Expands scope of sales and use tax exemption for equipment purchased by a large fulfillment facility
- Clarifies sales tax on digital property
- Educational service by certain institutions whether live or recorded is not a taxable event
- Homeschool exemptions for sales of digital and audio works
- Pre-recorded or on demand webinars would be taxable, live/real time would remain non taxable
- History
House
- Filed 5/14/2020
- Passed Finance Committee 5/19/2020
- Passed Rules Committee 5/19/2020
- Passed House 5/19/2020
- Passed Senate Finance 5/20/2020
- Passed Senate Rules 5/21/2020
- Passed Senate 48-0 with an amendment on 5/26/2020
- House concurred with the new version of the bill that included an amendment on 5/28/2020
- Bill presented to the Governor on 6/2/2020
- Signed by the Governor on 6/8/2020 - now law
Senate
- Filed 5/14/2020
SB 476 - School Based Mental Health
SB 476 - School Based Mental Health
Primary Sponsors: Sen. Rick Horner (R-Nash), Sen. Jerry Tillman (R-Randolph), Sen. Deanna Ballard (R-Watauga)
Summary
This bill would require the State Board of Education to adopt a school-based mental health plan that includes a mental health training program and a suicide risk referral protocol.
The model would address the following topics:
- Youth mental health
- Suicide prevention
- Substance abuse
- Sexual abuse prevention
- Sex trafficking prevention
- Teenage dating violence
The referral protocol would provide the following:
- Guidelines on the identification of students at risk of suicide
- Procedures and referral resources that address actions that should be taken to address student needs
The bill would also require every k-12 school to adopt a plan for promoting student mental health and well-being.
History
This bill was submitted to a conference committee on 5/20/20.
This conference report was adopted by the House and Senate on 5/27/20.
This bill was signed by the Governor on 6/8/2020.
NCGA Program Evaluation Committee - Housing and NC FAST
The Joint Legislative Program Evaluation Committee met on Monday, June 8, 2020.
North Carolina Housing Finance Agency
The Program Evaluation Division was charged to examine the efficiency and effectiveness of the NC Housing Finance Agency (NCHFA).
Recommendations
The NCGA should direct NCHFA to study modifications including:
- Eliminate or more broadly define the shopping category
- Eliminate the distinction between primary and secondary amenities
- Create a threshold score that includes amenities and measure of opportunity
The NCGA should direct NCHFA to:
- Examine modifications to 4 community partner programs to ensure access and activity throughout NC
- Develop a strategic plan and performance management system
- Clarify that NCHFA is not exempt from the Sate Budget Act, and direct NCHFA's board to limit contributions to nonprofit entities
- Adjust the strategy to preserve the affordability of Low Income Housing Tax Credit units
The bill draft language for these recommendations can be found here.
The NCMS is following this legislation due to it's potential impact to improving housing quality. This directly relates to to Healthy NC 2030 goals.
The Program Evaluation Division was charged to examine the child welfare case management functionality of NC FAST P4. An evaluation was completed to examine P4 usability and additional child welfare issues.
Findings
- The report found that P4 is functional and meets most of the State's goals with the exception of management reporting and data entry.
- P4 usability is unacceptably low, making it difficult for workers to complete tasks.
- Lack of state budget has delayed improvements in functionality. Indecision about P4 will increase overall project costs and may subject the State to federal penalties.
- Lack of unified child welfare practice model and resource disparities among counties hinder the State's ability to implement the case management system.
- Lack of state policy leadership and insufficient training have slowed development and implementation.
- NC FAST's oversight structure contributed to P4 development and implementation challenges.
Recommendations
The NCGA should direct DHHS to
- Prioritize usability in future vendor contracts
- Require a free proof of concept for any additional software
- Collaborate with a qualified organization to develop a system of standard child welfare processes
- Require future contractors to conduct culture change readiness training
NC DHHS may request $15 million for the personnel to manage this system.
The report noted that if the NCGA chooses to fund NC FAST in Fiscal Year 2020-21, it should direct the Department of Information Technology to embed staff within the NC FAST team to provide additional oversight.
The bill draft language for these recommendations can be found here.
The NCMS is following this legislation due to it's potential impact to improve child well being. This directly relates to to Healthy NC 2030 goals.
NCMS Morning Rounds 6-8-20
Welcome to a new week and your
NCMS Morning Rounds.
June 8, 2020
NCMS PPE Orders Have Arrived!
Most of the ActionPPE orders placed through the NCMS Personal Protective Equipment webpage have arrived! If your order is among the 40 that have been filled, you should have received a call or email from the NCMS to arrange pickup or delivery.
Those orders that have not yet been delivered are on hold until the threshold is reached for that particular piece of PPE. Once that occurs, the order will be fulfilled and delivered to the NCMS.
If you anticipate a need for PPE, please visit our website and place an order through Option 1, the group purchasing arrangement we have with the Charleston County (SC) Medical Society and ActionPPE. In addition to masks, the site now offers gowns and face shields.
NCMS Legislative Update
Last week was another busy week at the NC General Assembly as legislators continue the process of working through a variety of proposals, some of which are health care related. For a complete list of bills we are tracking be sure to visit our NCMS legislative blog, which has summaries of all the proposals and is updated as they make their way through committees and possibly to a full vote of the NC House and Senate.
Here are several bills we’d like to highlight:
HB471 – Exempt Direct Primary Care from DOI Regulations recognizes the relationship between a patient and a provider of direct primary care as an agreement between those two parties and posits that it should be exempt from NC Department of Insurance regulations. The proposal does outline what would be required in such an agreement. The NC Senate passed the bill last week and it now moves to the NC House for consideration.
HB678/SB300 – Amend Counselor/SA/Social Worker Professional Acts examines how state agencies and licensing boards adopt policies. We are watching this closely along with the NC Medical Board and will update you on any element that might have an impact on health care provider licensing boards as it moves through committees. Last week it was under consideration by the Senate Health Care Committee.
NCMS advocacy staff is also monitoring the various ‘mini’ appropriations bills that are being filed instead of the usual, single budget bill. Nothing related to health care has been submitted yet, but your advocacy team is watching for those and will report on any proposals that could impact your practice. Watch the legislative blog and your NCMS Morning Rounds for updates.
Late last week NCMS member Rep. Kristin Baker, MD, (R-Cabarrus) was appointed as a chair of a new bi-partisan legislative working group on law enforcement and community engagement.
Finally, remember to sign up for a virtual White Coat Wednesday to engage with your elected officials on the many important issues now being discussed. NCMS staff will help facilitate virtual meetings with legislators and give you the background information you need to have meaningful and productive conversations. Learn more and sign up here.
Message from NC Academy of Physician Assistants
Our colleagues at the NC Academy of Physician Assistants (NCAPA) sent a letter last week to its membership echoing the sentiments expressed in NCMS President Palmer Edwards’, MD, DFAPA, message about recent events. NCAPA President Alisha DeTroye, MMS, PA-C, DFAAPA sent the following letter:
I am writing to you with a heavy heart as we continue to endure the impact of the Covid-19 pandemic, which has resulted in extraordinary times for our PA workforce. My sadness and concern have been further exacerbated by the events of the past 10 days as I witness the outpouring of pain and frustration due to the death of George Floyd. These events remind me how much pain, inequity, intolerance, and racism exist in our nation today.
As demonstrated by our vision statement, NCAPA is committed to North Carolina PAs providing equitable delivery of patient-centered care. It is time to put those words into further action. Earlier this year, I charged a task force to make recommendations around improving diversity and inclusion among PAs and PA students. This was the beginning of the conversation but certainly not the end. I join my colleague at the North Carolina Medical Society, President Palmer Edwards, and his call to action by making health equity a priority and I plan on raising this discussion with the NCAPA Board of Directors. Please read Palmer Edwards' compelling message.
As PAs, we must dig deep into evidence-based medicine to further explore social drivers of health and their impact on health disparities. We need to listen to our patients to understand their barriers to care rather than label them as non-compliant. We need to understand our individual implicit biases and be humble enough to admit our deficits in knowledge, experience, and our fears. We need to collaborate through dialogue, inviting new and diverse voices to the table, for meaningful discussions. I look forward to hearing your ideas as we strive to be PAs (and Passionate Advocates) for change.
Sincerely,
Alisha DeTroye, MMS, PA-C, DFAAPA
NCAPA President
In the News
How Can the World Avoid Screwing Up the Response to COVID-19 Again?, STAT, 6-5-20
Learning Opportunity
Preventing Youth Vaping Part I: The Extent and Risk Factors for Youth Vaping, a webinar presented by the Danya Institute and the Prevention Technology Transfer Center Network, will be held on Thursday, June 25 from 1 to 2 p.m. This webinar will examine data on the rise and scope of vaping, and how it contrasts with previous tobacco use data. It will also examine the known risk factors that contributed to this rise, such as ease of availability, low perceptions of harm and lack of environmental strategies to prevent use. The webinar will also discuss the issue and current status of acute lung injuries caused by vaping. Register here.
If you have policies you'd like your NCMS Board of Directors to consider, please complete the Board input form here. Thanks for reading!
NCMS Political Pulse for June 5, 2020
Another busy week at the NC General Assembly as legislators continue the process of working through a variety of proposals, some of which could impact your practice. Legislators also are beginning to consider appropriation bills. NCMS Director of Legislative Relations Sue Ann Forrest, MPA, highlights some of the health care related bills along with several other newsy tidbits from this week.
NCMS Morning Rounds 6-5-20
Finally Friday! Here is your
NCMS Morning Rounds.
June 5, 2020
NCMS Staff Delivers More PPE
Over the past few days, NCMS staff members have been busy – safely -- delivering masks and other personal protective equipment (PPE) to practices in the eastern third of the state. The donated equipment is a result of a collaboration between the NCMS and various organizations including Centene, the NC Healthcare Association, Ford, Lowes Home Improvement and Congressman David Rouzer (NC-7th district).
Here are a list of the practices that received PPE:
Wilmington Gastroenterology
Carousel Center
Boiling Spring Lakes Family Medicine
Brad Lee Hilaman, MD, PA
Brunswick Family Medicine
Leland Pediatrics, PC
G & G Healthcare, PC
Chadbourn Family Practice Center, PA
Baldwin Woods GYN, PA
Whiteville Medical Associates
Eastern Medical Associates
Waynesborough Ophthalmology
Wayne Women’s Clinic
Goldsboro Pediatrics
Integrative Arthritis and Pain Consultants
Rocky Point Medical Center
Bryan M. Weckel, MD Family Medicine
Coastal Primary Health Specialists, PLLC
Burgaw Medical Center
Daniel Ricci, MD, PA
Rose Hill Medical Center
State Announces New COVID-19 Testing and Tracing Tools
Yesterday the NC Department of Health and Human Services (NCDHHS) announced new tools to help expand COVID-19 testing capacity, streamline contact tracing and to provide guidance on how to spread the word about how individuals can protect themselves and their community.
The new Check My Symptoms webpage that allows people to enter their symptoms and determine if they should get tested for COVID-19. If they are recommended to be tested, they will receive a link to a list of nearby testing sites via email or text. Note: The symptom checker is an informational tool to help people determine if they may need to be tested; however it is not a physician order. Testing sites may require their own screening.
The public may also access the ‘Find My Testing Place’ website, enter their county or ZIP code and find a list of nearby testing sites.
Your practice team and patients should also be aware of the work of the COVID-19 Community Team, made up of trained contact tracers. Team members reach out to people who have tested positive for COVID-19, or anyone who has been near someone with COVID-19, and get them the information and support they need. This support can include helping someone understand what it means to have been exposed to COVID-19, how to monitor their symptoms, when to get tested, if needed, and how to protect their loved ones.
When the COVID-19 Community Team reaches out, it is important that people answer the call. Individuals being contacted would get an initial text from the number 45394 or email from [email protected] with follow-up phone calls from NC OUTREACH (844-628-7223) or the Local Health Department. The Community Team represents North Carolinians across the state and will be available to provide support and information in multiple languages.
NCDHHS has created a toolkit to help you disseminate this information to your patients via printed materials and social media posts. Access the toolkit here.
Congressional Action Brings Possible Changes to Paycheck Protection Program
On Wednesday, the US Senate passed the Paycheck Protection Program Flexibility Act of 2020, which the US House of Representatives had passed on May 28. The legislation, which is awaiting President Trump’s signature, includes sweeping changes to the Small Business Administration’s Paycheck Protection Program.
Key provisions in the new bill include that PPP borrowers will now have 24 weeks to use the funds rather than the initial 8-week period. Also, the new rules allow borrowers to apportion 60 percent of the PPP funds toward labor costs, whereas the old rule set the threshold at 75 percent of the loan proceeds. Borrowers also would have five years instead of two to pay off the loan.
The SBA’s PPP webpage has not been updated with any of the new information pending the President’s approval of the legislation. This article from the Journal of Accountancy details more about the changes included in the new legislation.
In the News
Hype Collides With Science As FDA Tries to Rein In ‘Wild West’ of COVID Blood Tests, Kaiser Health News, 6-3-20
Learning Opportunity
Join us for an important conversation TODAY, June 5 from 1 to 2 p.m. The events of the last two weeks have focused the nation’s attention on issues of racism and the many ways it is evident in our society. This week’s Power Hour brings together health care professionals who have thought profoundly about these issues and how they impact us, our patients and our communities.
Please join us as we explore the current reality including discussion of health inequities and disparities, as well as what we can do as individual physicians, PAs and as part of an organization like the NCMS to foster positive change.
Participants will include:
• NCMS President Palmer Edwards, MD, DFAPA
• NCMS Past President Paul R.G. Cunningham, MD
• NCMS President-elect Philip M. Brown, Jr., MD
• NCMS Strategy Officer Karen Smith, MD
• NC Medical Board President Bryant A. Murphy, MD, MBA
• Founder, Black Doctors USA George Pride, PhD
The Kanof Institute for Physician Leadership (KIPL) Power Hour aims to provide a forum for ongoing conversation, collaboration and community. Tune in to Power Hour weekly to hear from different experts, decision makers and influencers on a variety of topics. The format is informal and conversational and sessions are easy to access through Zoom.
NCMS Morning Rounds 6-4-20
Enjoy your Thursday
NCMS Morning Rounds.
June 4, 2020
NCMS Statement on Recent Events
In case you missed the message from NCMS President Palmer Edwards, MD, DFAPA sent on Tuesday evening, here is that message once again. Please watch your NCMS Morning Rounds for upcoming opportunities to engage with the NCMS on these challenging and important issues.
In light of the events unfolding over the last 10 days, which sadly reflect the ongoing legacy of racism in our country, I feel it is important to reiterate the values that are the bedrock of the North Carolina Medical Society. The NCMS, representing physicians and PAs throughout the state, holds the safeguarding of human life and health to be the ultimate guiding principle in all we do to protect and advocate for the medical profession.
The death of George Floyd in Minneapolis last week has added yet another layer of pain, outrage and fear in our communities, which are still reeling from a devastating global pandemic. The unrest over the past days has shone a bright light on the deep rifts in our society. Racism, hatred and ignorance persist.
We know that racial and ethnic inequities are a large contributor to health disparities. The medical casualties due to COVID-19 bear witness to this fact. In North Carolina today the data show that African-Americans account for 35 percent of the COVID-19 fatalities, yet African-Americans make up just 22 percent of the state’s population. We need policy action now, along with abiding patience and engagement rather than impulsive and indiscriminate violence to persons and property.
The NCMS, representing a profession duty-bound to do no harm, must focus on opportunities for positive change that are within our realm. We have the power and responsibility as citizens and medical professionals to do our part to address the inequities that have given rise to the rage we currently are witnessing.
We know there are significant disparities within our health care system impacting many North Carolinians. How can we address them through our day-to-day practice; through the institutions of which we are part; through the NCMS? I challenge each of you, my colleagues, to examine your assumptions on how we might accomplish this crucial task.
As your professional society we have made health equity a central theme of our work going forward. We hope to engage you in an ongoing dialogue about how to stop perpetuating the inequities we see. The solutions are infinitely demanding and complex, but the effort is critical to the future of our country. The NCMS will not shrink from the challenge.
We look forward to engaging with you in the coming months as we continue our necessary work to address these issues on many fronts.
Be safe and well!
Palmer Edwards, MD, DFAPA
President, NCMS
[You may post any comments in response to this message here, on our blog.]
Efforts to Sustain Access to Care During and After Pandemic
The NCMS advocacy team and our partners at the federal level like the AMA are working to help ensure that, where beneficial to patients, the policies put in place in response to the COVID-19 pandemic will continue once the public health emergency subsides.
With the NC legislative session in full swing, you can keep up with the latest proposals at our NCMS legislative blog. Among other priorities, we are working to include telehealth parity in legislation being considered.
Earlier this week, the AMA submitted comments to Centers for Medicare and Medicaid Services (CMS) Administrator Seema Verma in response to the interim final rule on policies and regulations in response to the COVID-19 pandemic. The AMA expressed strong support for increased access to services delivered through telecommunications technology, increased access to testing and services in a patient’s home, and improved infection control to limit potential exposure to health care workers. The AMA also urged CMS to maintain several of its policies beyond the COVID-19 public health emergency, and provided detailed comments and examples of telehealth procedures that should continue under Medicare after the COVID-19 public health emergency has ended.
Beach Hotel Offers Discount for Medical Professionals
As a ‘thank you’ to medical professionals like you, serving the community during this stressful time, the Hampton Inn Sneads Ferry-North Topsail Beach is offering you a special reduced rate. Consider a trip to the beach to recharge!
Learn more and book at this link.
In the News
Hiring a Diverse Army to Track COVID-19 Amid Re-Opening, Kaiser Health News, 6-2-20
Learning Opportunity
Please mark your calendar for this week’s POWER HOUR, Friday, June 5 from 1 to 2 p.m. We are still finalizing the speakers to address this week’s timely topic of race and health equity. Please plan to join us for this important conversation with your peers. Watch your email for details on who will be participating. In the meantime, register here.
If you have policies you'd like your NCMS Board of Directors to consider, please complete the Board input form here. Thanks for reading!
SB 836 - State Operations/Increase Federal Funds Use
SB 836 - State Operations/Increase Federal Funds Use
Primary Sponsors: Sen. Harry Brown (R-Onslow), Sen. Kathy Harrington (R-Gaston), Sen. Brent Jackson (R-Sampson)
Summary
This bill would increase the amount COVID-19 relief funds for the continuity of operation needs across state government.
- Increases the amount from Reserves to Relief Fund from $1.2 billion to $1.5 billion
- Increases the amount to OSBM from $1.4 billion to $1.7 billion
History
Filed 5/26/2020
Passed - Senate Appropriations 5/28/2020
Passed - Senate Rules Committee 6/1/2020
Passed Senate 49-0 on 6/2/2020
This bill was sent to the House on 6/3/2020
HB 1187 - Raise the Age Funding
HB 1187 - Raise the Age Funding
Primary Sponsors: Rep. Jason Saine (R-Lincoln), Rep. Donny Lambeth (R-Forsyth), Rep. Chuck McGrady (R-Henderson)
Summary
This bill was filed as a placeholder for making specific appropriations at a later date on 5/26/2020.
On 5/28/2020, this bill was introduced to include improvements at the Department of Public Safety facilities to implement raise the age.
Appropriations
- $2.7 million for the Perquimans Youth Detention Center
- $5.6 million for the C.A. Dillon Youth Development Center campus in Granville County
- $2 million to complete construction of the Youth Development Center in Rockingham County
History
- Filed - 5/26/2020
- Committee Substitute - Favorable- House Appropriation 5/28/2020
- Passed House - 5/28/2020
- Senate - Appropriations Committee - Passed - 6/2/2020
- Senate Rules Committee - Passed - 6/3/2020
HB 1229 - Unemployment Program
HB 1229 - Unemployment Program/ ABAWD Time Waivers
Primary Sponsors: Rep. Julia Howard (R-Davie), Rep. Michael Wray (D-Northampton), Rep. Jason Saine (R-Lincoln)
Summary
This bill appropriates $2 million to the Division of Employment Security to strengthen unemployment insurance program during COVID-19.
The bill also allows DHHS to seek a temporary waiver from the US Department of Agriculture for time limits established by federal law for able bodied adults with out dependents participating in the Food and Nutrition Services program.
History
- Filed 5/27/2020
- Passed Committee Substitute - House Appropriations Committee 6/3/2020
- Calendared for the House floor for 6/6/2020
HB 678 - Health Care Flexibility Act
HB 678 - Health Care Flexibility Act
Summary
This bill would grant authority to the Secretary of Health and Human Services to waive or modify regulations in response to the potential wave of illness brought on by the COVID-19 pandemic to meet the need for additional health care facility beds and technology to treat patients.
The bill would allow this authority through the duration of the State of Emergency plus one year after the State of Emergency is lifted.
This would include authority to do any of the following:
- Increase bed capacity in a licensed health care facility
- Adding kidney dialysis stations to a disease treatment center or hospital
- Allowing an ambulatory surgical facility to operate as a temporary hospital
- Regulations on mental health beds
The bill authorizes health care licensure boards to have authority to waive or modify the enforcement of any legal or regulatory constraints that would prevent or impair any of the following:
- Allowing individuals to provide care if they are licensed in other states
- Allowing individuals to provide care if they are retired or inactive
- Allowing skilled but unlicensed volunteers to provide care
- Allowing students at an appropriately advanced stage of professional study to provide care
History
This bill was passed in the House as a bill regarding social worker statutory updates.
However, a proposed committee substitute to this bill was introduced in the Senate Health Care Committee for discussion only on 5/28/2020.
This bill was calendared to be heard in the Senate Health Care Committee for a vote on 6/2/2020, but was pulled from the Committee.
*The bill is still not available on the NC General Assembly website as of 12:50pm on 6/2/2020
*The information provided here is based of the language NCMS was able to acquire from staff.
NCMS Morning Rounds 6-2-20
It's Tuesday and time for your
NCMS Morning Rounds.
June 2, 2020
The NC General Assembly is back in session and the NCMS advocacy staff is busy tracking its work. Keep up-to-date on all the proposals most likely to impact your practice and your patients at our NCMS Legislative blog. The blog is continually updated with behind-the-scenes, quick summaries as the proposed legislation makes its way through the various committees and floor votes. Go to the NCMS Legislative Blog.
Clarification on Provider Relief Fund
The US Department of Health and Human Services (HHS) announced at the end of May that it had extended the attestation deadline for those health care providers who had received funds through the CARES Act Provider Relief Fund General Distribution of the first $50 billion.
Originally, HHS indicated that those who had received funds needed to accept the HHS Terms and Conditions and submit revenue information to be considered for an additional General Allocation payment by June 3. Subsequently, HHS announced that it had extended the attestation deadline for an additional 45 days, however, the June 3 deadline remains on the Provider Relief Fund website.
The AMA reached out to HHS for clarification on why the website still has a deadline of June 3 when the attestation deadline has been extended. Here is HHS' response:
Folks will have a total of 90 days to attest. However, they will only have until June 3 to access the application portal to submit their revenue / loss information.
Folks must accept or reject funds in order to enter the application portal. So, if on June 3 folks are still deciding whether to accept funds they have already received, but haven’t yet submitted their tax information to the application portal, they should (1) reject the funds; (2) submit info to the application portal for consideration.
They will be reallocated all General Distribution funds they are owed based on their submitted application, and will then have 90 days to attest or reject.
We have implemented this so that we can have all applications by June 3, and can start rolling out other distributions.
The attestation portal (as opposed to the application portal) will remain open for 90 days. Only the application portal will close on June 3.
This HHS FAQ document about the Provider Relief Fund is updated regularly and may address any questions you have.
NC Bar Offers Help to Health Care Workers
The North Carolina Bar Foundation and the North Carolina Pro Bono Resource Center have launched the COVID-19 Frontline Health Planning Project to assist healthcare workers and other essential employees who are on the frontlines of the COVID-19 pandemic.
Pro bono attorneys will provide clients and their families with crucial legal protections by interviewing clients and preparing statutory advance directives remotely.
Two types of documents are being prepared at no cost, and clients can select either or both:
• Health Care Power of Attorney, which allows you to designate a Health Care Agent.
• Living Will, which provides your instructions to your doctors to either withhold or withdraw life-prolonging measures in certain circumstances.
This project is focused on providing services to healthcare workers and other essential workers impacted by COVID-19 who otherwise may not have access to legal services to secure these important documents.
To sign up, click here to access the online client intake form. Email questions to: [email protected]
NCDHHS Seeking COVID-19 Testing, Lab, Tracing Vendors
As part of its response to COVID-19, the NC Department of Health and Human Services (NCHHS) is creating a pool of qualified vendors to expand diagnostic and antibody testing including specimen collection and laboratory processing, and contact tracing. The Department is prioritizing working with minority-owned business vendors or vendors who retain a diverse workforce.
All vendor applicants must be able to demonstrate the ability to support focused testing and tracing efforts for historically marginalized populations. African Americans and LatinX/Hispanic communities make up a disproportionate number of North Carolina’s COVID-19 laboratory confirmed cases and deaths due to long standing health inequities that must be addressed proactively as we respond to this pandemic, NCDHHS stated in its announcement of this Request for Qualifications.
The goal is to screen the various applicants in advance, in order to have a ready pool of vendors to rapidly respond to the COVID-19 pandemic and for work on specific projects in the future.
Testing and tracing are part of North Carolina’s strategy to responsibly ease restrictions, while slowing the spread of COVID-19 and protecting North Carolinians. Applicants must submit their response to the RFQ by 2 PM on June 9, 2020. Qualified applicants will be notified on June 17, 2020. The RFQ is available here.
Learn more about this initiative.
In the News
Leveraging Payment Reforms for COVID-19 and Beyond: Recommendations for Medicare ACOs and CMS’ Interim Final Rule, Health Affairs, 5-29-20
Learning Opportunity
TODAY, Tuesday, June 2 from 3 to 4 p.m., the NC Division of Public Health’s Injury and Violence Prevention Branch is offering a COVID-19 response webinar on ‘Promising Practices in Health Equity’ focused on sharing promising public health practices to reduce COVID-19 related disparities. Presenters will discuss the actions their cities, which include those in Iowa, Kentucky and Louisiana, have taken to mitigate the disproportionate impact on racial and ethnic minorities. Additionally, speakers will take these ideas a step further and examine how they can be integrated into longer-term strategies for lasting impact that strengthens future responses and advances health equity. Register here.
If you have policies you'd like your NCMS Board of Directors to consider, please complete the Board input form here. Thanks for reading!
NCMS Political Pulse for May 29, 2020
The legislative session is in full swing with lots of committee meetings and bills under consideration. NCMS Director of Legislative Relations Sue Ann Forrest, MPA, gives you the highlights and outlines several new bills we're closely tracking including legislation prompted by the COVID-19 pandemic, a bill dealing with direct primary care and Medicaid transformation among others.
NCMS Morning Rounds 5-29-20
It's Friday once again! Enjoy your
NCMS Morning Rounds.
May 29, 2020
The NC General Assembly is back in session and the NCMS advocacy staff is busy tracking its work. Keep up-to-date on all the proposals most likely to impact your practice and your patients at our Legislative blog. The blog is continually updated with behind-the-scenes, quick summaries as the proposed legislation makes its way through the various committees and floor votes. Go to the NCMS Legislative Blog.
NCMS PPE Deliveries Continue
The NCMS has continued to deliver personal protective equipment to our Community Practitioner Program (CPP) practices throughout the state. These medical offices are located in underserved communities. Learn more about our NCMS Foundation’s CPP and how we are helping to ensure every community has the health care they need – especially during this uncertain time.
The masks and test kits delivered to these practices in western NC are thanks to the generous donations from Centene, the NCMS’ partner in Carolina Complete Health, and the University of North Carolina. NCMS Vice President for Member Services Ashley Newton, MBA, delivered the much-needed supplies to the following practices:
- Newton Family Physicians, Newton
• Midway Medical Center, Clyde
• Surry Rural Health Center, Mt Airy
• Silver Creek Family Practice, Morganton
• Morganton Eye Physicians, Morganton
• Hendersonville Pediatrics, Hendersonville
NCMS Urges Senators to Support Additional Help
Yesterday the NCMS reached out to Senators Richard Burr (R-NC) and Thom Tillis (R-NC) to support federal legislation that would offer additional help to patients and medical practices struggling due to the COVID-19 pandemic.
As NCMS CEO Robert W. Seligson, MBA, MA, states in the letter: “It has been a time of incredible disruption of patient care, and the state’s economy and physician practices are being heavily impacted from the effects of this crisis.”
The letter enumerates the provisions in the HEROES Act, recently passed by the US House of Representatives, and urges Senators Burr and Tillis to come together to compromise and support bipartisan legislation to “serve those with COVID-19 and those whose coverage is being displaced. We ask you to support a final bill that will help practices remain open to care for all North Carolina patients.”
Early Access to NCTracks Annual Survey
For those practices that accept Medicaid, NCTracks is offering NCMS members early access to its Annual Provider Survey for 2020. The survey will officially open on Monday, June 1, but NCTracks is offering you advance access now.
This is your opportunity to provide NCTracks feedback on direct customer interaction such as their call center, provider relations, training and communications as well as your thoughts on functional areas such as pharmacy prior approval and provider enrollment.
The survey has been newly designed to take less than 10 minutes to complete. Responses will be accepted until June 15.
In the News
The Epic Battle Against Coronovirus Misinformation and Conspiracy Theories, Nature, 5-27-20
Learning Opportunity
REMINDER: Be sure to tune into today’s NCMS Foundation's Kanof Institute for Physician Leadership Power Hour from 1 to 2 p.m. to discuss diabetes prevention. Learn more and register here.
Also, today from 12:30 to 1:30 p.m. NC AHEC and the NC Department of Health and Human Services (NCDHHS) will continue the weekly forum in which NC Division of Public Health subject matter experts are on hand to answer your questions about the COVID-19 response. Access this webinar through this Zoom link or, for audio only, by calling +1-646-558-8656 and entering meeting ID 705979628#.
NCDHHS has held these forums since the pandemic began and would like to know if you still find them useful. Please share your perspective with NCDHHS’ Maribeth Wooten at [email protected].
If you have policies you'd like your NCMS Board of Directors to consider, please complete the Board input form here. Thanks for reading!
NCMS Morning Rounds 5-28-20
Happy Thursday! Enjoy your
NCMS Morning Rounds.
May 28, 2020
The NC General Assembly is back in session and the NCMS advocacy staff is busy tracking its work. Keep up-to-date on all the proposals most likely to impact your practice and your patients at our Legislative blog. The blog is continually updated with behind-the-scenes, quick summaries as the proposed legislation makes its way through the various committees and floor votes. Go to the NCMS Legislative Blog.
SBA Releases Loan Forgiveness Application
The Small Business Administration (SBA) has released its 11-page Paycheck Protection Program (PPP) Loan Forgiveness Application, which, among other information, provides borrowers with instructions on how to calculate eligibility for forgiveness of their PPP loans and the necessary documentation under the Coronavirus Aid, Relief and Economic Security (CARES) Act.
The PPP was created by the CARES Act to provide forgivable loans to eligible small businesses to keep workers on the payroll during the COVID-19 pandemic. The loan forgiveness documents are designed to help small businesses seek forgiveness at the conclusion of the eight week covered period, which begins with the disbursement of their loans.
The SBA also will soon issue regulations to further assist borrowers as they complete their application and provide guidance to lenders on their responsibilities. Lenders will likely have their own procedures for borrowers to request forgiveness as well.
Download the PPP Loan Forgiveness Application.
Also, keep in mind, Congress is considering a proposal that would extend the current 8-week covered period for the PPP; allow for loan terms of more than 2 years; extend the rehiring date past June 30 to offset the effect of enhanced unemployment benefits and allow more employers with PPP loans to defer payroll taxes, among other provisions.
Learn more about the PPP and loan forgiveness here.
Practices Hope Increased Telehealth Visits Are Here to Stay
The results of the May 11 NCMS, NC Medical Group Management Association (NCMGMA) and Curi survey, which looked more closely at medical practices’ use of telehealth during the COVID-19 pandemic, revealed that a majority of those practices (68 percent), which have increased their use of telehealth, hope to continue the increased use of telehealth after the pandemic subsides.
More than 60 percent of participating practices said that patients have indicated a preference for telehealth visits over in-person visits recently. Respondents decisively said (70 percent) that if all payers were to offer telehealth parity, they would be more likely to pursue telehealth visits as part of their regular practice. Cybersecurity did not appear to be a concern for telehealth visits, according to survey results.
Review a summary of the telehealth survey results.
Don’t forget to take this week’s survey, which focuses on practices considerations around reopening and reassuring patients to come in for routine care. Take this week’s survey now. Results will be reported in an upcoming NCMS Morning Rounds.
Message to Parents: Keep Up with Regular Vaccinations
With routine vaccinations down an estimated 90 percent in places due to possible reluctance of parents to take their children to regular well-visits for fear of exposure to COVID-19, the Centers for Disease Control and Prevention (CDC) is now warning of a possible measles outbreak. To reassure parents – and patients of all ages – that it is safe to continue to seek routine care, longtime NCMS member David Tayloe, Jr., MD, FAAP, a Goldsboro pediatrician and strong advocate for vaccination, spoke with WRAL News to encourage parents to make sure their children are being immunized.
Watch the interview with newscaster David Crabtree.
In the News
Nearly Half of Americans Delayed Medical Care Due to the Pandemic, Kaiser Health News, 5-27-20
Also in the news: NCMS’ partner in Carolina Complete Health, Centene, made number 14 in the new Forbes Corporate Responders ranking, which assesses how well the 100 largest employers among U.S. public companies responded to the public health crisis from mid-March through May 7 across 22 categories. Read more here.
Learning Opportunity
The NCMS Foundation and its Kanof Institute for Physician Leadership (KIPL) is providing a lively and informative weekly virtual forum for ongoing conversation, collaboration and community. Power Hour is held each Friday from 1 to 2 p.m. This week’s discussion will include focus on diabetes prevention. Learn more and register.
The Power Hour archive is always available for browsing here. Previous conversations have included the NC Medical Board’s response to COVID-19; self-care and wellness during this pandemic and telehealth.
If you have policies you'd like your NCMS Board of Directors to consider, please complete the Board input form here. Thanks for reading!
SB 850 - Ensure Healthy Schools/COVID-19
SB 850 - Ensure Healthy Schools/COVID-19
Primary Sponsors: Sen. Wiley Nickel (D-Wake), Sen. Mujtaba Mohammed (D-Mecklenburg), Sen. Harper Peterson (D-New Hanover)
Summary
This bill would appropriate $102 million in recurring funds to increase positions for school nurses in order to provide at least 1 full time school nurse for every school.
History
Filed 5/26/2020
Referred to Appropriations Committee 5/27/2020
SB 866 - Enact Naturopathic Doctors Licensure Act
SB 866 - Enact Naturopathic Doctors Licensure Act
Primary Sponsors: Sen. Joyce Krawiec (R-Forsyth), Sen. Jim Burgin (R-Harnett), Sen. Paul Newton (R-Cabarrus)
Summary
Definitions
Approved naturopathic medicine program must meet all of the following conditions:
- Graduate level, full time didactic and supervised clinical training in naturopathic medicine that is accredited by the Council on Naturopathic Medical Education
- Program offered by a higher education that is accredited by the US Secretary of Education.
- Program approved by the NC Naturopathic Doctors License Board
The bill defines naturopathic medicine as a system of natural health care that employs diagnosis and treatment using natural therapies for the promotion, maintenance, and restoration of health and the prevention of the disease including all of the following:
- Administration of any of the following: natural medicines, natural therapies, natural topical medicines, hydrotherapy, dietary therapy and naturopathic and physical medicine
- Use of diagnostic procedures including physical and orificial examination but excluding endoscopy, sigmoidoscopy and colonoscopy
- Ordering, performing, and interpreting lab tests and diagnostic imaging
- Manual use of massage, stretching, resistance, or nauturopathic manipulation
Scope of Practice
- Dispense, administer, order and advise use of natural remedies
- Order and perform physical examinations and physiological function tests
- Order, perform and interpret laboratory tests, including obtaining specimens to access and treat disease.
- Order diagnostic imaging
- Hydrotherapy
- Health education and health counseling
- Utilize routes of administration for substances
- Perform care incidental to superficial lacerations and abrasions
NC Naturopathic Doctors Licensure Board
- Consists of 7 members
- 2 NDs recommended by the President Pro Tempore
- 2 NDs recommended by the Speaker of the House
- 2 licensed physicians appointed by the Governor
- 2 public members appointed by the Governor
Naturopathic Doctors Formulary Council
- 2 NDs licensed in NC with two years of practice experience
- 1 physician who is involved in the practice of integrative medicine
- 1 physician who practices in NC
- 1 pharmacist who has a background in pharmacognosy
- 1 public member
This bill states that the Board would be responsible for recommending a formulary for use by NDs. The board would review the formulary annually.
Qualifications for Licensure
- Good moral and ethical character
- Graduate of an approved program
- Has either passed the Naturopathic Physicians Licensing Examination or has successfully completed a competency based state or Canadian province licensing examination administered prior to NPLEX
- An agreement to collaborate and consult with a licensed physician
History
Filed - 5/26/2020
Referred to Senate Rules 5/27/2020
SB 845 - Foster Care Youth
Primary Sponsors: Sen. Joyce Krawiec (R-Forsyth), Sen. Jim Burgin (R-Harnett)
Summary
This bill appropriates $500,000 in non-recurring funding for the implementation of the Foster Care Transitional Living Initiative Fund to support youth transitioning from foster care.
History
- Filed 5/26/2020
- Referred to Senate Appropriations Committee 5/27/2020
HB 1206/SB 844 - Student Mental Health Well-Being/COVID-19
HB 1206/SB 844 - Student Mental Health Well-Being/COVID-19
Primary House Sponsors: Rep. Cynthia Ball (D-Wake), Sen. Becky Carney (D-Mecklenburg), Rep. Sydney Batch (D-Wake)
Primary Senate Sponsors: Sen. Jay Chaudhuri (D-Wake), Sen. Erica Smith (D-Northampton)
Summary
This bill would appropriate $480,000 in recurring funds to the Department of Public Instruction to create a tiered system of support for students by increasing positions for the following school mental health support personnel to meet the following ratios:
- 1 school psychologist for every 700 students
- 1 counselor for every 250 students
- 1 social worker for every 400 students
History
Filed 5/26/2020
Appropriations Committee Referral 5/27/2020
SB 839 - PPE and Hazard Pay for Public School Employees
SB 839 - PPE and Hazard Pay for Public School Employees
Primary Sponsors: Sen. Mujtaba Mohammed (D-Mecklenburg), Sen. Terry Van Duyn (D-Buncombe), Sen Harper Peterson (D-New Hanover)
Summary
Appropriations
- $75 million in non-recurring funding to provide surgical and respiratory masks and gloves for all public school employees
- $70 million in non-recurring funds to provide a temporary salary supplement of $5 per hour for all public school employees
History
Filed 5/26/2020
Referred to Senate Appropriations Committee 5/27/2020
HB 471 - Reduce Admin. Duplication MH/DD/SAS Providers
HB 471 - Reduce Admin. Duplication MH/DD/SAS Providers
Primary Sponsors: Rep. Jon Hardister (R-Guilford), Rep. Donna White (R-Johnston), Rep. Josh Dobson (R-Avery), Rep. Gale Adcock (D-Wake)
Summary
This bill would require the Department of Health and Human Services to establish a workgroup to examine and make recommendations about how to eliminate administrative duplication for mental health, intellectual/developmental disability, and substance sue disorder providers.
Thew review would include reviewing the following requirements:
- Training
- Service Delivery
- Documentation
- Claims processing
- Reporting
- Monitoring
- Oversight
- Facility Licensure
- Credentialing
- Accreditation
- Contracts
- Investigations
- Audits
The findings would be reported to the Joint Legislative Oversight Committee on Health and Human Services.
History
- Filed 3/26/2019
- Favorable - House Health Committee 4/9/2019
- Favorable - House Rules Committee 4/15/2020
- Passed - House 4/16/2020
- Senate Health Care Committee - Discussion only 5/27/2020
SB 843 - Close the Medicaid Coverage Gap/Funds
SB 843 - Close the Medicaid Coverage Gap/Funds
Primary Sponsors: Sen. Gladys Robinson (D-Guilford), Sen. Valerie Foushee (D-Orange), Sen. Dan Blue (D-Durham)
Summary
This bill would provide individuals health insurance coverage in the Medicaid coverage gap.
- Income at or below 133% federal poverty level
- Between the ages of 19-65
- Not entitled/enrolled in Medicare
- Not otherwise eligible for Medicaid coverage as of January 1, 2020.
Beneficiaries eligible for this program would receive benefits through an Alternative Benefit Plan established by DHHS.
Copayments for this program would be the same as Medicaid.
This would be paid through a Medicaid Coverage Gap Assessment that will pay for the State share of the program as well as administrative costs.
The bill appropriates $100,000 in nonrecurring funding for the planning and preparation of the Medicaid coverage.
History
Filed 5/26/2020
HB 1192 - Student Health Collaborative Pilot
HB 1192 - Student Health Collaborative Pilot
Primary Sponsors: Rep. Craig Horn (R-Union), Rep. Ashton Clemmons (D-Guilford), Rep. John Fraley (R-Iredell)
Summary
$5 million from the General Fund to DHHS to create a 1 year student health collaborative pilot program.
The Division of Social Services shall select 5 counties to participate in diverse areas of the State.
- 2 tier 1 counties,
- 2 tier 2 counties
- 1 tier 3 county
History
Filed - 5/26/2020
HB-1188 TANF Benefit Increase/COVID-19
HB-1188 TANF Benefit Increase/COVID-19
Primary Sponsors: Rep. John Autry, Rep. Zack Hawkins, Rep. Marcia Morey, Rep. Yvonne Holley
Summary
- Appropriates $13.2 million from the Coronavirus Relief Fund to DHHS to provide additional TANF benefits in response to the COVID-19 pandemic
- Requires DHHS to allocate $2.2 million per month for payments to eligible recipients
- Allows each eligible recipient to receive a monthly payment of $193
History
Filed
- 5/26/2020
HB 1184 - Ensure Safer Voting for 2020 Elections
HB 1184 - Ensure Safer Voting for 2020 Elections
Primary Sponsors: Rep. Marcia Morey (D-Durham), Rep. Zack Hawkins (D-Durham), Rep. John Autry, Rep. Deb Butler (D-New Hanover)
Summary
- Extends voter registration deadline to 14 days before the election
- Expands options for submitting absentee ballot request forms
- Allows for every single voter to receive a mail request form for an absentee ballot
- Pre-paid postage would be included on this form
- Allows for a copy of a utility bill, bank statement, government check, or paycheck to be used for identification, if no witness is available to certify the ballot
- Requires every local board of elections to have one contactless ballot drop box for every 25,000 voters per county
- Allows for poll worker recruitment flexibility
- Allows for county board of elections to have flexibility in voting hours
- Requires Election Day to be a paid State holiday
- States no photo ID shall be required for the 2020 general election
- Provides the Executive Director of the State Board of Elections to have emergency powers due to a pandemic or national health crisis
- Allows curb side voting to be expanded
History
- Filed 5/26/2020
HB 1181 - Certain Appropriations for Education/COVID
HB 1181 - Certain Appropriations for Education/COVID
Primary Sponsors: Rep. John Fraley (R-Iredell), Rep. Ashton Clemmons (D-Guilford), Rep. Craig Horn (R-Union)
Appropriations
- $405,000,000 to be used from the Coronavirus Relief Fund to the Office of State Budget and Management for appropriations within this bill
- $150,000,000 to the Department of Public Instruction (DPI) to improve internet connectivity for students by installing router devices in buses and providing community home access points
- $65,000,000 to DPI to allocate to local school administrative units, charter schools, and regional schools for computers or electronic devices for students and school personnel
- $25,000,000 to DPI to award grants to public school units to support extraordinary costs associated with providing services for exceptional children
- $25,000,000 to DPI for school health personnel to provide additional physical and mental health support services for students
- $15,000,000 to the Board of Governors to cover expenses for resources and supports for students impacted by COVID-19
- $60,000,000 the Board of Governors to be allocated to constituent institutions to provide institutional support for eligible expenses for resources and supports
- $10,000,000 to the Community College System Office for students
- $20,000,000 to the Community College System for support for campuses
- $35,000,000 to the Board of Governors to be allocated to the State Education Assistance Authority
History
- Filed 5/26/2020
HB -1180 Sam's Law
Primary Sponsors: Rep. Steve Jarvis (R-Davidson), Rep. Craig Horn (R-Union), Rep. Jon Hardister (R-Guilford), Rep. Ashton Clemmons (D-Guilford)
Summary
The bill would allow for the parent of any student to petition a school unit for the development of a seizure action plan if the student is diagnosed with a seizure disorder.
The plan, at minimum, would include from the student's health care provider, the students' name, seizure medication, dosage and method of administering the medication, frequency of the medication, symptoms necessitating medication. The plan would also require a written statement from the parents allowing for administration of the medication.
Filed
- 5/26/20
HB 1191 - ECU Brody School of Medicine Funds
HB 1191 - ECU Brody School of Medicine Funds
Primary Sponsors: Rep. Perrin Jones (R-Pitt), Rep. John Bell (R-Wayne), Rep. Christ Humphrey (R-Lenior)
Summary
This bill would appropriate funds for the planning and construction of a new Brody School of Medicine at East Carolina University.
- $15 million for the planning of a new building
- $13 million for the construction of a new building
- $215,000,000 is the total amount authorized for the project.
- 45% of the members of the Board of Trustees of the primary affiliated teaching hospital would be appointed by the Board of Governors
Joint Appropriations Financial Forecast Overview
The Joint Appropriations Committee met on Tuesday, May 26 at 5:00pm.
The Committee requested an general revenue overview by the NCGA's Chief Economist, Dr. Barry Boardman. He noted that this summary is very uncharted territory due to pandemic uncertainty and delayed tax payments.
Process
The Fiscal Research Division and the Office of State Budget and Management developed independent forecasts prior to the release of the Governor's budget.
Revised Forecast
The revised forecast includes a $2.566 million decrease or a 9.9% decline in revenue. This forecast also includes a $1 billion shift in revenue because of delayed tac payments. This forecast does not include a second wave of the COVID-19 pandemic.
Biennium Revenues (2019-2021)
The collections during this time period are projected to be $4.2 billion below September 2019 forecast. There will be an updated forecast after July to include the forecast for each revenue source.
The North Carolina Medical Society is following this information closely to stay up to date on the economic outlook for our state.
HB 1110 - PFAS Studies
HB 1110 / SB 838 - PFAS Studies
Primary Sponsors: Rep. Pricey Harrison (D- Guilford), Rep. Ray Russell (D-Ashe), Rep. Brandon Lofton (D-Mecklenburg), Rep. Robert Reives (D-Durham)
Primary Senate Sponsor: Sen. Michael Garrett (D-Mecklenburg)
Summary
This bill would direct various agencies including DHHS, Wildlife Resources, Office of State Management and Budget, Department of Environmental Quality, NC Policy Collaboratory, Environmental Review Commission to study matters associated with PFAS contamination.
The bill also appropriates $100,000-$200,000 to each agency for these studies.
History
Filed 5/14/2020
Committee Referrals: Regulatory Reform, Environment, Appropriations, Rules