HB 1108 - PFAS Contamination Mitigation Measures
HB 1108 /SB 837 - PFAS Contamination Mitigation Measures
Primary House Sponsors: Rep. Pricey Harrison (D-Guilford), Rep. Deb Butler (D-New Hanover), Rep. Rachel Hunt (D-Mecklenburg), Rep. Christy Clark (D-Mecklenburg)
Primary Senate Sponsors: Sen. Michael Garrett (D-Mecklenburg)
Summary
The bill requires the Department of Environmental Quality (DEQ) to require that every person applying for an individual National Pollutant Discharge Elimination System permit fully disclose in its application for a new permit, or permit renewal. The bill would also require the permit holder to disclose the concentration to be discharged. The bill also requires the elimination of PFAS prior to discharge into waters of the State.
Appropriations:
- $5 million non-recurring to DEQ for the Bernard Allen Drinking Water Fund to fund drinking water treatment systems
- $5 million in recurring funds to expand DEQ's water quality monitoring activities
- $ 1 million in non-recurring funds for DEQ to develop a strategy to address toxic chemicals
- $1 million in non-recurring funds to study PFAS destruction and disposal techniques to identify a safe, effective, and scalable technology
- $80 million in non-recurring funds to issue matching grants to water systems to build or improve drinking water systems
History
Filed 5/14/2020
Committee Referrals 5/18/2020: Environment, Appropriations, Rules
NCMS Morning Rounds 5-25-20
Welcome back to a new work week. Enjoy your NCMS Morning Rounds.
May 26, 2020
Update Call on Testing Guidance
Last week the NCMS helped host a call with NC Department of Health and Human Services Secretary Mandy Cohen, MD, MPH and state Health Director Betsey Tilson, MD, MPH along with other NCDHHS area experts to make sure everyone is aware of the latest guidance on COVID-19 testing.
The new guidance, issued on May 15 and available to review on the NCMS COVID-19 webpage, advises clinicians to conduct or arrange for diagnostic testing for any patient in whom COVID-19 is suspected. The guidance also instructs practices to consider sample collection strategies that preserve PPE if possible, such as having a dedicated team, practice site, or testing center that performs sample collections. As new testing sites and modalities are available, the guidance seeks to ensure testing for anyone in close contact with someone who has tested positive.
Sec. Cohen also stressed that regardless of symptoms, anyone who falls in a high risk category (e.g. those who live or have regular contact with those in high-risk settings such as nursing homes; those at risk of serious illness; those from historically marginalized populations; health care workers and first responders and frontline and essential workers like grocery store attendants) should be tested.
Included in the call was an overview of the current testing modalities including the latest on antibody testing; an outline of how the state is reaching out to historically marginalized populations and a summary of the toolkit for long-term care facilities.
Access the slides from the presentation here.
Some of the same information will be covered TODAY, Tuesday, May 26 in the NCMS Foundation’s Lunch & Learn webinar at noon. Director of the North Carolina State Laboratory of Public Health Scott Shone, PhD, HCLD(ABB) and State Epidemiologist Zack Moore, MD, MPH, will discuss ‘Covid-19: Epidemiological & Laboratory Approaches.’ Learn more and register here.
NCMB Answers Supervision Questions During COVID-19
The North Carolina Medical Board (NCMB) has created a ‘Frequently Asked Questions’ page on its website to clarify any questions around supervision during this time of upheaval for many practices.
Several of the questions address reassignment of PAs and resulting supervision arrangements necessary. Another details the requirements for out of state clinicians who may be volunteering in the state.
If you have questions or need clarification on this topic, access the FAQ page here.
Award Nominations for Diabetes Prevention and Management
The North Carolina Diabetes Advisory Council (DAC) will be accepting nominations for the 2020 DAC Awards and applications for the new Diabetes Educator Scholarship from June 12-July 31, 2020 so start considering colleagues who may be deserving recipients of the recognition.
The awards recognize those who have demonstrated exemplary work in diabetes prevention and management including, but not limited to, employers, caregivers, educators, faith communities, health care providers and pharmacists.
Award recipients will be announced in September and awards will be presented at the Nov. 13, 2020 DAC Meeting in Raleigh. Do not miss the opportunity to recognize your diabetes hero or to be selected as an outstanding diabetes educator.
Learn more about the awards and download a nomination form here.
In the News
The World Needs COVID-19 Vaccines. It May Also Be Overestimating Their Power, STAT, 5-22-20
Patients Steadily Return to In-Person Primary Care as Telehealth Plateaus, Healthcare Dive, 5-21-20
Learning Opportunity
The next webinar in the COVID-19 Conversations series by the American Public Health Association and the National Academy of Medicine, will be: ‘Summer of COVID-19 – Mitigating Direct and Indirect Impacts in the Coming Months.’ Public health, infectious disease and risk communication experts will explore the state of the science surrounding the current outbreak of COVID-19 in the United States and globally, with a focus on the emerging evidence on how to best mitigate its impact. Tune in tomorrow, Wednesday, May 27, from 5 to 6:30 p.m. Learn more and access the archived webinars here.
The NCMS Morning Rounds newsletter is published each weekday to provide our physician and PA members with information and resources to help you improve the health of North Carolinians. If you have feedback on how we can do better or information you'd like to see included, please simply reply to this email. If you have policies you'd like your NCMS Board of Directors to consider, please complete the Board input form here. Thanks for reading!
NCMS Morning Rounds 5-22-20
Enjoy the unofficial start of summer and your NCMS Morning Rounds.
May 22, 2020
In observance of the Memorial Day holiday on Monday, May 25, the NCMS Morning Rounds will not be published. Thank you to all who serve our country today and have served in the past. Hope you have a restful and meaningful Memorial Day!
NCMS Monitoring Dozens of Legislative Bills Filed
Yesterday afternoon was the deadline for legislators to file legislation to be considered during this short – and unusual -- session. A flurry of proposals were officially filed including several that your NCMS advocacy staff are watching closely. We routinely monitor dozens of bills that may impact your practice and the health of North Carolinians and have provided brief summaries of those filed this week on our legislative blog. Review those summaries here.
We’re paying particular attention to SB808 – Medicaid Transformation Necessities, which, among other provisions, delays implementation of the planned transformation of the state’s Medicaid program to managed care until Jan. 1, 2021. The proposal also would appropriate funds for the operation of the NC Medicaid program, however, it does not give any funding amounts at this point. This is consistent with other Senate appropriation bills filed this week, which reflect legislators' priorities without actual dollar amounts due to the uncertainty around revenue and the state’s needs due to the ongoing pandemic.
Another bill of note is Rep. Cecil Brockman’s (D-Mecklenburg) proposal, HB1103 – Access to Affordable Health Coverage for All. This bill would create access to health insurance through the federal Health Benefits Exchange for individuals in the coverage gap. The proposed program would be modeled after the federal refundable premium tax credit for purchasing health insurance on the Exchange.
We are encouraged by Rep. Brockman’s proposal as a potentially bipartisan approach to increasing access to health care coverage, long one of our legislative priorities. The NCMS has been working diligently for years in support of a previous proposal – HB655 – NC Health Care for Working Families. We look forward to bringing people together to advance legislation to increase access to care.
Stay tuned to our NCMS legislative blog, our weekly Political Pulse video and your NCMS Morning Rounds for updates from the General Assembly.
NCMS Delivers More PPE
NCMS staff were pleased to provide two eastern NC practices with needed personal protective equipment (PPE) this week. Lumberton Children’s Clinic and Robeson Pediatrics, both part of the NCMS Foundation’s Community Practitioner Program (CPP) providing health care to vulnerable populations in underserved areas of the state, were grateful to receive the equipment in order to continue to serve their communities during the pandemic.
The NCMS is working through many channels to help all our members secure necessary PPE as practices have grappled with the many challenges in responding to the COVID-19 pandemic. So far, we have organized a group purchasing effort, and we worked with Carolina Complete Health (CCH) and its subsidiary Carolina Complete Health Network to distribute PPE to primary care practices in North Carolina. The PPE was obtained by Centene and shipped directly to NCMS and CCH staff for distribution to those CPP practices in need. We are grateful for this work, as we continue to do everything within our capabilities to mitigate the negative effects of the COVID-19 pandemic on our community.
NCMS CEO Thanks YOU for Carrying Forward the NCMS’ Mission
NCMS Executive Vice President and CEO Robert W. Seligson, MBA, MA, wants you to know how much he appreciates all you have been doing to address the health care needs of your patients and the public during this unprecedented time. He also wants you to know that the NCMS is carrying forward its long-standing mission to help you protect and improve the health of all North Carolinians. Watch this brief video, as he delivers his heartfelt message.
In the News
Hallucinations, ‘COVID Toes’ and More: The Emerging Symptoms of COVID-19, The Advisory Board Forum, 5-20-20
Learning Opportunity
REMINDER: Don’t miss today’s NCMS Foundation Kanof Institute for Physician Leadership POWER HOUR beginning at 1 p.m. Today the focus will be on 'New Human Resource Challenges Arising during COVID-19 and How to Address Them.' Learn more and register here.
Also, please note that NCMS Past President Robert Monteiro, MD, will be participating in a live webcast on a Baltimore area radio show, ‘Good Mental Health with Dr. Linda McGhee’ from 1 to 2 p.m. today. The topic will be ‘Moving Forward: How to Protect Yourself from COVID-19 and the Impact of Racial Disparities.’ Listen live here.
The NCMS Morning Rounds newsletter is published each weekday to provide our physician and PA members with information and resources to help you improve the health of North Carolinians. If you have feedback on how we can do better or information you'd like to see included, please simply reply to this email. If you have policies you'd like your NCMS Board of Directors to consider, please complete the Board input form here. Thanks for reading!
NCMS Political Pulse for May 22, 2020
The General Assembly was back in session this week and very busy filing hundreds of bills for consideration. We are tracking all of those that could impact your practice and the health of your patients. In this edition of your Political Pulse video, NCMS Director of Legislative Relations Sue Ann Forrest, MPA, highlights several bills of note and recounts the success of our first virtual White Coat Wednesday.
Community Conversations: Karen Smith, MD - Is COVID-19 a 'Set-Up' or a 'Set-Back' for Vulnerable Populations?

Is COVID-19 a 'Set-Up' or a 'Set-Back' for
Vulnerable Populations?
[5 minute read time]
This is the first in a periodic series of conversations with NCMS members who are on the frontlines in improving the health of North Carolinians and are now responding to the COVID-19 pandemic. If you would like to share your perspective and experiences, please contact Elaine Ellis, [email protected] to discuss being part of the NCMS Community Conversation series.
Today’s conversation is with Karen Smith, MD, a longtime NCMS member and family physician in Raeford, NC who also works as the Hoke County Health Department Medical Director. Dr. Smith serves a diverse and oftentimes vulnerable patient population in this rural area. The current pandemic has magnified some of the existing health disparities in her community, she says, and national data have reinforced what Dr. Smith has been witnessing in her area.
For instance, surveillance data from the Centers for Disease Control and Prevention (CDC), which began tracking COVID-19 hospitalizations through its 14-state COVID-NET network in March, has shown the majority of patients hospitalized for COVID-19 have underlying conditions like hypertension, obesity and cardiovascular disease. The data also suggests “that black populations might be disproportionately affected by COVID-19,” the CDC report states.
In North Carolina as of May 18, the NC Department of Health and Human Services (NCDHHS) reports that for cases where race and ethnicity are known, 33 percent of the confirmed COVID-19 cases are among African Americans and 31 percent are among Hispanics. The US Census estimates as of July 2019 show that African Americans make up 22 percent of the state’s population and Hispanics less than 10 percent.
While many of those who die from the virus have underlying health issues, those are often a result of socio-economic factors like “where a person lives, learns, works and plays,” Dr. Smith said
Underpinning the recent NC Institute of Medicine’s Healthy NC 2030 roadmap to improve the state’s health over the next decade, which has been embraced by the NCMS Board of Directors, lies the conviction that “health inequities are created when people cannot attain optimal health because of unjust, unnecessary and avoidable circumstances (e.g. greater barriers to accessing healthy foods, transportation, physical activity and health care in historically segregated, low-income and racial and ethnic minority communities). These inequities lead to health disparities, or differences in health status and outcomes between groups based on characteristics like race, ethnicity, gender, geography, educational attainment and income.”
The current pandemic has held a magnifying glass to some of these disparities, Dr. Smith said. Her key question is whether the inequities highlighted by the pandemic will lead to positive change in the future.
“Can we get beyond what we know previously existed and actually try to correct some of those socio-economic issues? Is this [pandemic] a set-back for the population or is it actually a set up? We have evidence, we have proof. We know [these socio-economic conditions have] a major impact in creating this disparity. I fear that we as a society will say, ‘ok, we knew this was going to happen, let’s get over it and move on with time’ and we will not take the opportunity to say, ‘yes, we’re going to actively engage and fix the situation.’”
Collaboration, Protocols and Examining Implicit Bias
One incident stands out for Dr. Smith in illustrating some of the challenges many physicians are facing as well as lessons to be learned. On a recent Friday morning, the Hoke County Health Director called Dr. Smith to report a COVID-19 ‘mini-outbreak’ at the Canyon Hills residential facility, a 24-bed, treatment facility for boys ages 6 to 17. Two employees tested positive for the virus and were sent home. Now Dr. Smith and the health director had to decide whether and how to test the remaining staff and children.
“My gut feeling – and not to take ownership of the decision because I worked with the health director – if I were a parent and my kid was in a facility out of my home, out of my reach, I would want to know. The final conclusion -- we will test,” Dr. Smith said. The problem was there were not enough kits to do the necessary testing.
With 28 years in the community, Dr. Smith knew who to call at FirstHealth of the Carolinas Moore Regional Hospital.
“I literally had tears in my eyes because of how the hospital responded. She said to me, ‘you tell me what you need. We’re going to send you the kits.’ Then, they drove the kits to us,” Dr. Smith said. By the time the testing was complete, the courier service had stopped for the day, but the local EMS stepped up and drove the specimens to Raleigh. By Monday morning, they had the surprising results – 14 positives. Canyon Hills then began addressing how to communicate with parents and how best to separate, isolate, trace, treat and monitor both positive and negative cases.
“There was no existing protocol, yet people and things just kind of gelled and came together. People stepped up to the plate. Different organizations stepped up to the plate. It reminded me of “The Practical Playbook” in terms of how community collaboration makes sense even in a non-pandemic or non-crisis,” Dr. Smith said. “It doesn’t matter if you’re working independent, solo, like myself, or if you’re working in a hospital setting. In an issue of this nature, it’s no longer you the physician that takes ownership of the problem and the solution, it’s the team that is going to take ownership of the problem and the solution.”
The importance of collaboration is one lesson driven home by this incident. Having an emergency protocol in place is another – in fact, having a standardized protocol is first on the list of guidance from the CDC when addressing the needs of vulnerable populations during an emergency.
Number two on the CDC’s guidance is to identify and address implicit bias. Dr. Smith recalls examining any bias that may have existed about the kids at Canyon Hills.
“It’s very important to pay attention to the implicit bias. ‘Yes, they are from vulnerable population backgrounds, and yes, their life matters. They matter and therefore yes, we should test,” she said in describing her thought process.
Understanding the Community; Educating the Community
State officials identified testing and contact tracing as key components in understanding and mitigating the spread of the virus and have been working to ramp up both. Dr. Smith has a window into what that may mean in reality for the people in Hoke County.
“The tracing is interesting because this is where we start to see some of the disparities,” she said. “For example, the very first person who was identified and tested positive according to the county data, their telephone was disconnected. So, this person was lost to contact. We have vulnerable populations who may have lost their employment and cannot maintain those services like telephone or internet connectivity. Or maybe they’ve had to move because of a housing situation. These issues will have impact as regards the ability to trace.”
Some of her patients flat out refuse to be tested because a positive test means they will not be able to work.
“They literally have made the decision that ‘I have the disease and my disease is mild enough that I can get away with going into my job because my job, quite frankly, isn’t doing temperature testing. I have to work. I need to make money, and I’m mild and I’m just going to get by.”
Then there are those who have dangerous misinformation. For instance, that the cotton on the testing swab is from China and will actually infect them with the virus. Dr. Smith recently went on the local radio station to try to dispel the myth that drinking bleach – even a small amount – will cleanse the virus from a person’s body.
Her practice also is proactively reaching out to about 350 risk stratified patients identified as very high risk and high risk of serious health impacts if they contract COVID-19. Practice staff screen them for any COVID-19 symptoms as well as other vulnerability factors, such as how they get their food, medications, assess their emotional well-being and health resources and educate them about shelter in place.
“I also ask them about their advanced care decisions,” Dr. Smith said. “I ask the patient. Tell me about what do you want to have happen in the event you can’t speak for yourself? I refer them to the FiveWishes.org. Sometimes I get a response back – well, am I about to die? No, I tell them, you’re not about to die, but we should have held this conversation a long time ago. What it says is that I care about you, your desires as a person and, as your doctor, I want you to be comfortable with shared trust as part of our relationship. I want to do what your heart desires to have done.”
Set Back or Set Up?
As Dr. Smith asked at the outset, is the spotlight the pandemic shining on health disparities yet another set-back for those impacted most severely by the virus or a set-up to make positive and lasting changes to improve the health of everyone in the state?
The NCIOM’s Healthy North Carolina 2030 sets out 21 goals necessary to make real improvements in the state’s health and 21 health indicators to statistically measure progress toward those goals. Among those goals are:
- Decrease the number of people living in poverty to be measured by the number of individuals below 200 percent of the federal poverty level.
• Increase economic security as measured by the unemployment rate.
• Dismantle structural racism as measured by the short-term school suspension rate.
• Decrease the incarceration rate.
• Improve child well-begin by addressing adverse childhood experiences.
• Improve access to healthy food. - Improve housing quality.
At its core, the NCMS’ mission always has been protecting and improving the health of North Carolinians, and the Society has taken up Healthy NC 2030 to further that goal.This means, however, challenging some of our usual thinking about what drives health outcomes and how we, as an organization representing health care professionals, can effect positive change. For instance, income is one of the greatest predictors of disease and mortality rates – and an even stronger predictor of health disparities than race when considering the rates of disease within racial/ethnic groups. For what policies do we advocate in order to decrease the number of people living in poverty? Healthy NC 2030 offers various ‘levers for change’ for each health indicator. Access the full report to review what might activate this change.
The NCMS wants to hear from you about how best to improve the health of our state. What do you see where you live, learn, work and play? What needs to change? How can the NCMS help empower you to make the solutions possible?
Please help us keep the conversation going.
NCMS Morning Rounds 5-21-20
It's Thursday and must be time for your
NCMS Morning Rounds!
May 21, 2020
NCMS Launches First Virtual White Coat Wednesday
Yesterday, at the request of NCMS Board of Directors member Holly Biola, MD, MPH, FAAFP, she and a group of University of North Carolina Preventative Medicine residents met virtually with their legislators to discuss policy issues particularly as they relate to social determinants of health and public health.
The session, arranged by NCMS Director of Legislative Relations Sue Ann Forrest, MPA, generated meaningful interaction and conversation with the legislators never lagged. The group met with Rep. Graig Meyer (D-Orange), Rep. Verla Insko (D-Orange) and Sen. Natalie Murdock (D-Durham).
If you would like to arrange to participate in a virtual White Coat Wednesday during this unusual legislative session in order to advocate for issues of importance to your profession, please sign up here.
MAHEC Receives $4 million Grant for Behavioral Health Clinic
The Substance Abuse and Mental Health Services Administration (SAMHSA) has awarded the Mountain Area Health Education Center (MAHEC) a 2-year, $4 million grant to establish the first Certified Community Behavioral Health Clinic in western North Carolina.
The clinic will provide vital services for people with serious mental illness and substance use disorders across 18 counties in the western part of the state. Funded in part through the federal Coronavirus Aid, Relief and Economic Security or CARES Act, this grant will enable MAHEC to provide comprehensive care to more than 2,500 adults and children, including those who are uninsured and underinsured.
“The COVID-19 pandemic has created additional challenges for those who were already vulnerable,” said MAHEC CEO Jeff Heck, MD in a press release. “This funding ensures we can serve those who need our support now more than ever.”
This is the first Certified Community Behavioral Health Clinic in western NC and the fourth in the state. This model is designed to increase access to comprehensive mental health and substance use treatment including same-day behavioral health care, mobile crisis services, treatment with medication for opioid use disorder, primary care health screenings, community-based treatment, case management and care coordination with community partners who serve veterans, children and those involved with the justice system.
Many of the services under this grant are available through MAHEC now. Learn more here.
Podcast Takes Scientific Look at Many Aspects of COVID-19
NCMS Business Alliance member, Pfizer, recently published the first podcast in the second season of its ‘The Antigen’ series. This season will take a factual, science-based look a past pandemics, outline potential coronavirus treatments in development and look ahead to life after this latest pandemic. This first episode of the new season, ‘COVID-19: Looking Back to Look Forward,’ features David Swerdlow, MD, Pfizer’s medical affairs lead for COVID-19. Listen here to the 18-minute podcast.
The first season of ‘The Antigen’ focused on the scientific, cultural and political elements of vaccination. Over the course of the eight episodes, the podcast looked at the basic science of vaccines, reviewed vaccine history, explored the many facets of their global impact as well as public sentiment about vaccines around the world. Season one is archived here in case you want to listen.
Pfizer is a Leadership Council member of the NCMS Business Alliance meaning their representatives are among a select group of corporate leaders who come together with NCMS members to lead and challenge the status quo in health care. Learn more about the Business Alliance here.
In the News
Preventing a Parallel Pandemic – A National Strategy to Protect Clinicians’ Well-Being, NEJM Perspective, 5-13-20
Learning Opportunity
DON’T FORGET: This evening at 5:30 p.m. the NCMS, the NC Department of Health and Human Services (NCDHHS), NC AHEC and Community Care of North Carolina will virtually host NCDHHS Secretary Mandy Cohen, MD, MPH, and State Health Director Betsey Tilson, MD, MPH along with subject area experts who will provide the latest updates on the state’s response to the COVID-19 pandemic. Tune in from 5:30 to 6:30 p.m. by registering now at this link.
The next in the Rural Talk Advocacy Speaker Series will be held TODAY from 11 a.m. to noon to discuss rural health in North Carolina. Panelists include Laura Gerald, MD, president of the Kate B. Reynolds Charitable Trust and Alan Morgan, CEO of the National Rural Health Association. NC legislators Sen. Mike Woodard (D-Durham) and Rep. Josh Dobson (R-McDowell) will also participate. The panelists will consider issues around access to care, provider needs and shortages, social determinants and drivers, and the impact of COVID-19. Learn more and register.
NCMS Morning Rounds 5-20-20
Halfway through the week! Enjoy Wednesday's
NCMS Morning Rounds.
May 20, 2020
Get the Latest on COVID-19 Response Tomorrow Evening
The NCMS is working with the NC Department of Health and Human Services (NCDHHS), NC AHEC and Community Care of North Carolina to provide the information and resources you need to respond to the COVID-19 pandemic. Tomorrow evening, NCDHHS Secretary Mandy Cohen, MD, MPH, and State Health Director Betsey Tilson, MD, MPH along with subject area experts will be on hand to address issues including new options for telephonic and telehealth delivery of care, changes in testing recommendations, an overview of the testing modalities and a discussion on how NC DHHS is working with community partners to reach high priority populations.
Tune in tomorrow, Thursday, May 21 from 5:30 to 6:30 p.m. by registering now at this link.
ALERT: Advisory on COVID-19 Related Syndrome in Children
The Centers for Disease Control and Prevention (CDC) and the NC Department of Health and Human Services (NCDHHS) have issued a Health Advisory for Multisystem Inflammatory Syndrome in Children (MIS-C) Associated with Coronavirus Disease 2019 (COVID-19). The CDC also hosted a call with clinicians yesterday on this advisory and how you can recognize the symptoms of MIS-C. You can review the presentation slides and download the transcript here.
• Read the CDC’s advisory here.
• Read the NCDHHS advisory, with reporting information, here.
The specific features of this inflammatory syndrome are still being determined, but reports include features of Toxic Shock Syndrome and/or Kawasaki Disease. Additional reported features include laboratory evidence of inflammation and single or multi-organ dysfunction.
NCDHHS is requesting voluntary reporting of cases of this syndrome to the Communicable Disease Branch epidemiologist on call. Please use the patient summary form on page three of this memo and submit to the Communicable Disease Branch via secure fax at 919-733-0490 to the attention of “MIS-C surveillance.” If you have questions, please contact the Communicable Disease Branch epidemiologist hT
Additional Info on CARES Act Provider Relief Fund
To answer some of the questions physician practices have had about the CARES Act Provider Relief Fund, and to clarify the formulas used to figure what a practice might be entitled to receive from the fund, the US Department of Health and Human Services (HHS) has published an updated list of FAQs.
The AMA reported receiving multiple inquiries from physicians who believed they may have received more money from this fund than they were supposed to and were worried the money will be recouped by HHS. Last week, HHS has removed the previous formulas and unclear language about overpayments that were causing the concerns from the website.
Here are the updated FAQs on the Provider Relief Fund General Distribution Portal.
The AMA also has received questions regarding what HHS views as the appropriate use of the CARES Act funds, but no additional guidance beyond what is currently on the Provider Relief Fund website has been provided. The AMA advises that each practice be able to clearly document the revenue losses and expenses it is incurring that are directly due to COVID-19. This could include losses related to social distancing (such as cancellation of visits and procedures, Part B drugs that have passed their expiration date), costs of new infection control practices, PPE, digital health equipment, etc., and that are not reimbursable from other sources (excluding loans that have to be repaid).
In the News
Is 99.5 Degrees a Fever? It’s a Surprisingly Tricky Question – With Big Implications for Coronavirus Response, The Advisory Board Forum, 5-18-20
Learning Opportunity
Join the University of North Carolina Center for Health Equity Research TODAY, Wednesday, May 20 at 1 p.m. for the next edition in its webinar series: “Community Resilience & Healing during COVID-19.” The national experts who are today’s guest speakers will share from their work on how to understand the factors that promote community resilience during COVID-19 and lessons learned about community healing in past traumas. Learn more and register here.
The NCMS Morning Rounds newsletter is published each weekday to provide our physician and PA members with information and resources to help you improve the health of North Carolinians. If you have feedback on how we can do better or information you'd like to see included, please simply reply to this email. If you have policies you'd like your NCMS Board of Directors to consider, please complete the Board input form here. Thanks for reading!
SB 805 - Capital Appropriation - Raise the Age
SB 805 - Capital Appropriation - Raise the Age
Primary Sponsors: Sen. Harry Brown (R-Onslow), Sen. Kathy Harrington (R-Gaston), Sen. Brent Jackson (R-Sampson)
Summary
This bill would fund capital improvements at the Department of Public Safety for facilities implementing raise the age. The bill specifies appropriating funding for Perquimans Youth Detention Center, Moore County, and Rockingham County. The exact amount is not set in this bill as of 5/19/2020.
History
Filed - 5/19/2020
SB 804 - Capital Appropriation - Dix Relocation
SB 804 - Capital Appropriation - Dix Relocation
Primary Sponsors: Sen. Harry Brown (R-Onslow), Sen. Kathy Harrington (R-Gaston), Sen. Brent Jackson (R-Sampson)
Summary
This bill would fund capital improvements related to the relocation of the Dorothea Dix Campus of the Department of Health and Human Services. The exact amount is not set in this bill as of 5/19/2020.
History
Filed - 5/19/2020
SB 802 - Capital Appropriation - Data Centers/DIT
SB 802 - Capital Appropriation - Data Centers/DIT
Primary Sponsors: Sen. Harry Brown (R-Onslow), Sen. Kathy Harrington (R-Gaston), Sen. Brent Jackson (R-Sampson)
Summary
This bill would fund nonrecurring amount for the Eastern and Western Data Centers. An amount is not specified in this bill as of 5/19/2020.
History
Filed - 5/19/2020
SB-800 Law Enforcement and Teacher Protection Act
SB-800 Law Enforcement and Teacher Protection Act
Primary Sponsors: Sen. Harry Brown (R-Onslow), Sen. Kathy Harrington (R-Gaston), Sen. Brent Jackson (R-Sampson)
Summary
This bill allows the State to draw down the maximum funds from the federal CARES Act for public health, testing, addressing shortfalls in state operations, addressing shortfalls in education funding, addressing shortfalls in public safety funding, providing relief to taxpayers.
History
Filed 5/19/2020
HB 1164 - Fund Pitt Mental Health Ct./Pretrial Program
HB 1164 - Fund Pitt Mental Health Ct./Pretrial Program
Primary Sponsor: Rep. Perrin Jones (R-Pitt)
Summary
This bill appropriates funds to be used for grants to Pitt County for an innovative court pilot program and a pre-trial release program.
Appropriations:
- $50,000 non-recurring for the Pitt County innovative court pilot program
- $100,000 non-recurring for the Pitt County pretrial release services
History
Filed - 5/19/2020
Committee Referrals: Appropriations, Rules
HB 1162 - Living Donor Protection Act
HB 1162 - Living Donor Protection Act
Primary Sponsors: Rep. Phil Shepherd (R-Onslow), Rep. Perrin Jones (R-Pitt), Rep. Shelly Willingham (D-Edgecombe)
Summary
This bill protectects living donors from potential insurance discrimination. The bill provides an income tax credit for unreimbursed medical expenses resulting from certain organ and marrow donations. The bill required up to 30 days paid sick leave to state employees who serve as living organ donors and up to 7 days for bone marrow donors
History
Filed 5/19/2020
Committee Referrals: Health, Finance, Rules
HB 1161 - Funds to Study & Abate Ocular Melanoma
HB 1161 - Funds to Study & Abate Ocular Melanoma
Primary Sponsor: Rep. Christy Clark
Summary
This bill appropriates $100,000 in non-recurring finds to the Nicholas School of the Environment at Duke University to study the potential causes and solutions for abating ocular melanoma in Huntersville and Cornelius.
History
Filed 5/19/2020
Committee Referrals: Appropriations, Rules
HB 1120 - UNC/CC/Hunger Free Campus Initiative
HB 1120 - UNC/CC/Hunger Free Campus Initiative
Primary Sponsor: Rep. Zack Hawkins
Summary
This bill would establish the Hunger Free Campus Initiative within the UNC System and the State Community College System.
Appropriations:
- $1.6 million in recurring funds to distribute evenly among each institution within the UNC System
- $5.8 million in recurring funds to distribute evenly among each institution within the NC Community College System
History
Filed 5/14/2020
Referrals: Appropriations, Rules
NCMS Morning Rounds 5-19-20
It's Tuesday and time for your
NCMS Morning Rounds.
May 19, 2020
NCMS Board of Directors Meet
On Saturday, your NCMS Board of Directors met as originally scheduled prior to the COVID-19 pandemic, although they gathered virtually to attend to the Society’s business. To start the meeting, NCMS President Palmer Edwards, MD, DFAPA welcomed the class of 2020 Leadership College participants. Board members all introduced themselves, answered questions from the leadership scholars and offered their insights and expertise as the class completes their year-long individual projects. Learn more about NCMS Foundation’s Kanof Institute for Physician Leadership programs.
In addition to discussing various aspects of the NCMS’ response to the pandemic, Board members also reviewed survey results and member feedback on how to ensure a valuable LEAD Health Care Conference experience in October. The Board asked the LEAD Conference planning committee to make recommendations on how to plan and execute a successful virtual meeting or series of virtual sessions while also respecting the traditions and history of the organization in these unusual circumstances.
Chair of the Nominating and Leadership Development Committee, Timothy J. Reeder, MD, MPH, FACEP reported there has been considerable interest in serving on the Board of Directors. The deadline to submit an application for an open seat on the Board of Directors, the AMA delegation of the Nominating and Leadership Development Committee was yesterday, Monday, May 18. Dr. Reeder reported that the committee had received applications from a “good, diverse group of people” for all open positions on the Board of Directors, some seats have multiple applicants, he said. The committee will begin the interview process on May 30. Watch your NCMS Morning Rounds for information on the slate of candidates and how you can cast your vote for the leadership of your medical society.
Board members reiterated their ongoing desire to receive your feedback on how the NCMS is addressing the issues you are facing and are open to your ideas and suggestions. To propose a policy, please use the Board of Directors online feedback form accessible here and on the NCMS website under About NCMS, Board of Directors. All forms are reviewed by the Board, the policy making entity for the NCMS. For non-policy related suggestions and comments, simply respond to this email.
COVID-19 Updates from NCDHHS
NC Department of Health and Human Services Secretary Mandy Cohen, MD, MPH, is offering this quick, 30-second public service announcement describing the 3 W’s – Wear. Wait. Wash. – as a way to remind the public of preventing the spread of the COVID-19 virus. View the PSA and feel free to share with patients and staff.
Governor Roy Cooper and NCDHHS officials continue to monitor the data as they weigh whether to move the state to Phase 2, lifting more of the restrictions designed to contain the spread of the virus. That could come as early as 5 p.m. this Friday, May 22. Last week, Governor Cooper and Sec. Cohen reported that the key COVID-19 data indicators remain stable. Review the data.
The key metrics are:
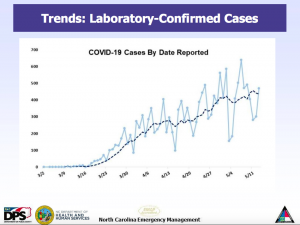
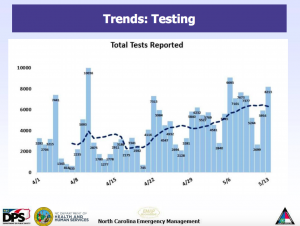
• Trajectory in COVID-Like Illness (CLI) Surveillance Over 14 Days: North Carolina’s syndromic surveillance trend for COVID-like illness is decreasing.
• Trajectory of Lab-Confirmed Cases Over 14 Days: North Carolina’s trajectory of lab-confirmed cases is slightly increasing.
• Trajectory in Percent of Tests Returning Positive Over 14 Days: North Carolina’s trajectory in percent of tests returning positive has been decreasing and is starting to level.
• Trajectory in Hospitalizations Over 14 Days: North Carolina’s trajectory of hospitalizations is level.
In addition to these metrics, the state continues building capacity to be able to adequately respond to an increase in virus spread. These areas include:
• Laboratory Testing: North Carolina has doubled the daily testing rate from approximately 2,500-3,000 to more than 6,000.
• Tracing Capability: The Carolina Community Tracing Collaborative has already hired close to 100 new contact tracers adding to the 250 already working at our local health departments.
• Personal Protective Equipment: Supply chains continue to improve with the exception of gowns.
Phase 2 will only start if data and indicators remain stable, state officials said.
Kudos to These Exceptional Physicians
Even during these dark times, there are still bright spots to celebrate. We offer our congratulations to:
NCMS Foundation Kanof Institute for Physician Leadership alumnus and now faculty member Roy E. Strowd, III, MD, has been named Editor of the Resident and Fellow Section of the American Academy of Neurology's Green Journal.
Longtime NCMS member and New Hanover-Pender County Medical Society’s immediate past president, Clarence L. Wilson II, MD, who, at the county society’s inaugural 2020 meeting in February, received the 2019 Community Service Award and a $1,000 check to the Good Shepherd Center. The center is the largest provider of homeless services in the Wilmington region.
Hannah Masoud, MD, resident physician at New Hanover Regional Medical Center, who won the National American College of Physicians (ACP) abstract competition in the Quality Improvement division. Dr. Masoud examined “Antimicrobial Practices for Acute Bacterial Pharyngitis.” You may listen to her presentation here.
Congratulations to all!
In the News
Life as a COVID-19 Contact Tracer: Sleuthing, Stress and Veering Off-Script, STAT, 5-18-20
Learning Opportunity
This Friday’s NCMS Foundation’s Kanof Institute for Physician Leadership Power Hour will focus on 'New Human Resource Challenges Arising during COVID-19 and How to Address Them.' Tune in for this virtual gathering from 1 to 2 p.m. on Friday, May 22, when Kevin Ceglowski, JD, Kelsey Mayo, JD, and Steve Shaber, JD from Poyner Spruill will address the many workplace related challenges associated with the current national public health emergency and how best to address them. The conversation will be moderated by Franklin Walker, MBA, NCMS VP of Rural Health System Innovation. Learn more and register.
HB 1119 - Food Waste Reduction Act
HB 1119 - Food Waste Reduction Act
Primary Sponsor: Rep. Zack Hawkins (D-Durham)
Summary
This bill creates a process to decrease food waste in landfills.
History
Filed - 5/14/2020
Committee Referrals - Appropriations, Regulatory Reform, Rules
HB 1117- Protect Child Care Workers/COVID-19 Pandemic
HB 1117- Protect Child Care Workers/COVID-19 Pandemic
Primary Sponsors: Rep. Julie Von Haefen (D-Wake), Rep. Mary Belk (D-Mecklenburg), Rep. Susan Fisher (D-Buncombe), Rep. Rachel Hunt (D-Mecklenburg)
Summary
Appropriations:
- ~$121 million in non-recurring funds for addressing child care provider needs
- This includes funding for teachers, staff, sanitation supplies, PPE, out of pocket costs, co-payments, deductibles,and additional child care consultants.
- $16.2 million in non-recurring funds for 2 weeks of paid sick leave for child care teachers and staff providing child care
History
Filed 5/14/2020
Committee Referrals: Appropriations, Rules
HB 1114 - 2020 Omnibus Appropriations Act
HB 1114 - 2020 Omnibus Appropriations Act
Primary Sponsors: Rep. Donny Lambeth (R-Forsyth), Rep. Jason Saine (R-Lincoln), Rep. Dean Arp (R-Union), Rep. William Brisson (R-Bladen)
Summary
This bill was filed as a placeholder for appropriating current operations of state government and other changes in budget operations.
History
Filed - 5/14/2020
Referrals: Appropriations, Rules
HB 1112 - 2020 Omnibus Appropriations Act
HB 1112 - 2020 Omnibus Appropriations Act
Primary Sponsors: Rep. Donny Lambeth (R-Forsyth), Rep. Jason Saine (R-Lincoln), Rep. Josh Dobson (R-Avery)
Summary
This bill was filed as a placeholder for appropriating current operations of state government and other changes in budget operations.
History
Filed - 5/14/2020
Referrals: Appropriations, Rules
HB 1109 - PFAS Manufacture/Use/Sale Ban
HB 1109 - PFAS Manufacture/Use/Sale Ban
Primary Sponsors: Rep. Pricey Harrison (D-Guilford), Rep. Deb Butler (D-New Hanover), Rep. John Autry (D-Mecklenburg), Rep. Marcia Morey (D-Durham)
Summary
This bill would ban the manufacture, use, and distribution of PFAS and PFAS containing products within the state in order to protect public health.
The bill creates financial civil penalties for violations of this act.
History
Filed 5/14/2020
Committee Referrals 5/18/2020: Rules
HB 1104 - Access to Affordable Health Coverage for All
HB 1104 - Access to Affordable Health Coverage for All
Primary Sponsors: Rep. Cecil Brockman (D-Guilford)
Summary
This bill would create access to health insurance through the federal Health Benefits Exchange for individuals in the coverage gap. This program would be modeled after the federal refundable premium tax credit for purchasing health insurance on the Exchange.
An individual would need to meet the following requirements to be eligible for this program:
- Gross income below 100% of the federal poverty level
- between the ages of 19-65
- Not entitled to Medicare
- Not currently eligible for Medicaid
- Not eligible for TRICARE
- Not able to obtain affordable coverage in an employee sponsored plan that provides minimum coverage as determined under federal law
The bill directs DHHS and the Department of Revenue to design a plan that estimates the amount of State premium tax credit an individual is eligible for in the given year and allows the individual to direct any amount to be paid in advance directly to an insurance company offering health benefit plans in this State on the Exchange.
This bill states that it is the intent that this program does not exceed $1 billion.
DHHS and the Department of Revenue would each receive $100,o00 in nonrecurring funding to implement this plan.
History
Filed - 5/14/2020
Committee Referrals: Rules
HB 1101 - Guilford County Funds
HB 1101 - Guilford County Funds
Primary Sponsors: Rep. Ashton Clemmons (D-Guilford), Rep. Jon Hardister (R-Guilford), Rep. Amos Quick (D-Guilford), Rep. John Faircloth (R-Guilford)
Summary
This bill would appropriate $7.7 million to Guilford County for the construction of a mental health crisis center.
*This bill contains other non-health related provisions.
History
Filed - 5/14/2020
Committee Referrals: Appropriations, Rules
HB 1100 - Relief for Business/Religious Orgs/COVID-19
HB 1100 - Relief for Business/Religious Orgs/COVID-19
Primary Sponsors: Rep. Keith Kidwell (R-Beaufort), Rep. Kyle Hyle (R-Stokes), Rep. Mitchell Setzer (R-Catawba), Rep. Michael Speciale (R-Craven)
Summary
This bill would allow operation of certain businesses and religious organizations that comply with social distancing guidelines during an executive order. This bill would provide liability protection from violation of an executive order. The bill would set the maximum fine for violation at $5.00.
History
Filed - 5/14/2020
Committee Referrals: Judiciary, Appropriations, Rules
HB 1097 - Superseding Orders/Domestic Violence
HB 1097 - Superseding Orders/Domestic Violence
Primary Sponsors: Rep. Joe John (D-Wake), Rep. Rogers (R-Burke), Rep. Marcia Morey (D-Durham), Rep. Scott Brewer (D-Montgomery)
Summary
This bill would clarify when subsequent orders will supersede similar provisions related to child custody, child/spousal support, and possession of property in domestic violence protective orders as recommended by the NC Courts Commission.
History
Filed - 5/14/2020
Committee Referrals: Judiciary, Rules
HB 1095 - Policy and Funding for Previous JPS Requests
HB 1095 - Policy and Funding for Previous JPS Requests
Primary Sponsors: Rep. Alan McNeil (R-Moore) Rep. Jamie Boles (R-Moore) Rep. Ted Davis (R-New Hanover)
Summary
Appropriations
- $535,465 in recurring funds to the Administrative Office of the Courts
- $250,000 to the Human Trafficking Commission for one full time Executive Directory position and operating costs
- $187,520 to the NC Innocence Inquiry Commission to support one full time staff attorney, one part time administrative secretary, and investigative services
- $97,945 to the sentencing and Policy Advisory Commission to support one full time research associate.
- ~$3.75 million in nonrecurring funding to the Administrative Office of the Courts
- $3.7 million for implementation of the Integrated Case Management System
- ~$7,000 to the NC Innocence Inquiry Commission
- This bill allows the Department of Public Safety to use funds to reimburse counties for the cost of housing convicted inmates awaiting transfer to the state prison system up to $40 per day.
Policy
- This bill makes a correction to recently enacted to human trafficking language to make prosecutors aware of any expunction of records of certain offenses committed by human trafficking victims.
- *This bill contains other policies that are not listed here that do not directly relate to health.*
History
This bill was filed on 5/14/2020
Committee referrals: Appropriations, Rules
HB 1094 - Protect State Employees & Contractors
HB 1094 - Protect State Employees & Contractors
Primary Sponsors: Rep. Carolyn Logan (D-Mecklenburg), Rep. Kandie Smith (D-Pitt)
Summary
This bill would appropriate funds for the 2020-2021 fiscal year to protect the rights of state government employees and contractors by establishing the Ombud's Office under the State Human Resources's Commission for the independent review of workplace complaints and prohibiting the mistreatment of contract employees working in state government.
History
Filed -5/14/2020
HB 1092 - Health Care Funding Requests/COVID-19-2
HB 1092 - Health Care Funding Requests/COVID-19-2
Primary Sponsors: Rep. Josh Dobson (R-Avery)
Summary
Appropriations
- $300,000 from the Coronavirus Relief Fund Reserve to the Coronavirus Relief Fund under the CARES Act of 2020.
- This $300,000 would be used to provide the Department of Health and Human Services for health care needs related to COVID-19.
History
- Filed - 5/14/2020
- Committee Referrals: Appropriations, Rules
HB 1090 - Funds/State Agencies for Loss of Receipts
HB 1090 - Funds/State Agencies for Loss of Receipts
Primary Sponsor: Rep. Alan McNeill (R-Moore)
Summary
The bill appropriates $30 million in nonrecurring funds for State agencies negatively impacted by the loss of anticipated receipts due to COVID-19.
History
Filed 5/14/2020
Committee Referrals: Appropriations, Rules
HB 1087 - Health Care Funding Requests/COVID-19-1
HB 1087 - Health Care Funding Requests/COVID-19-1
Primary Sponsor: Rep. Donny Lambeth (R-Forsyth)
Summary
Appropriations
- $300,000 from the Coronavirus Relief Fund Reserve to the Coronavirus Relief Fund under the CARES Act of 2020.
- This $300,000 would be used to provide the Department of Health and Human Services for health care needs related to COVID-19.
History
- Filed - 5/14/2020
- Committee Referrals: Appropriations, Rules
HB 1085/SB 740 Front Line State Employee Hazard Pay
HB 1085/SB 740 Front Line State Employee Hazard Pay
House Primary Sponsors:
Senate Primary Sponsors: Sen. Harper Peterson (D-New Hanover), Sen. Michael Garrett (D-Guilford)
Summary
This bill would mandate hazard pay for mandatory state employees.
The bill appropriates $5 million to fund hazard pay for mandatory state employees.
The bill directs that the Legislative Research Commission study the provision of hazard pay to private and local government employees.
History
House
- Filed - 5/14/2020
- Committee Referrals: Appropriations, Rules
Senate
- Filed - 5/14/2020
HB 1083/SB 761 Huntersville Ocular Melanoma Study Funding
HB 1083/SB 761 Huntersville Ocular Melanoma Study Funding
House Primary Sponsor: Rep. Christy Clark (D-Mecklenburg)
Senate Primary Sponsor: Sen. Natasha Marcus (D-Mecklenburg)
Summary
This bill would appropriate $100,000 to the town of Huntersville to study and abate frequent cases of ocular melanoma in the area.
History
House
- Filed - 5/14/2020
- Committee Referrals: Appropriations, Rules
Senate
- Filed - 5/14/2020
NCMS Morning Rounds 5-18-20
Welcome to another week and your
NCMS Morning Rounds.
May 18, 2020
NCMS Legislative Update
Last week legislators were in Raleigh for committee meetings to address different aspects of responding to the COVID-19 pandemic. This week the full General Assembly is scheduled to reconvene this afternoon.
For an overview of the various committees’ work last week, please visit our Legislative blog. There you’ll find meeting summaries for the House COVID-19 committee’s working groups on Health and Economics as well as the General Assembly’s Revenue Laws Study Committee and Program Evaluation Committee. If you have received revenue through the federal CARES Act or the Paycheck Protection Program you will want to check out these summaries to see what the committees are considering as far as tax changes for these programs. Check out the Program Evaluation Committee report to see the discussion around various state programs that could impact the health of North Carolinians.
As reported earlier, our popular White Coat Wednesday is now available virtually. This is a special opportunity for you to connect with your representatives via Zoom or other virtual means. No need to travel to Raleigh! We will guide you through the process of connecting in this way with your legislators.
If you signed up before the pandemic to participate in an upcoming White Coat Wednesday, NCMS Director of Legislative Relations Sue Ann Forrest, MPA, will be in touch to discuss the current hot topics and arrange meetings with legislators. If you would like to take advantage of this unique opportunity, please visit our White Coat Wednesday to sign up page.
With the many pressing issues brought about by the pandemic, now is an important time to share your perspective with elected officials.
Although it has not made much front page news lately, this is an election year and November is going to be here before you know it. The NCMS PAC plays a vital role in establishing and maintaining relationships with state and federal office holders. These relationships are fundamental to our advocacy success in furthering our short and long term priorities! Your contributions to our NCMS PAC are crucially important. Please consider a donation to our PAC today. Make your contribution here.
US House Considers/Passes HEROES Act
The US House on Friday night passed HR 6800 the Health and Economic Recovery Omnibus Emergency Solutions Act or HEROES Act with a vote of 208 to 199 mostly along party lines. This $3 trillion relief package is unlikely to gain traction in the Repulican-led Senate, however.
The AMA has produced a detailed summary of the legislation and how it may impact your practice. Read the AMA’s overview.
Last week, the AMA sent a letter to House leaders, Rep. Nancy Pelosi and Rep. Kevin McCarthy, expressing support for the HEROES Act. The legislation provides “stability for physician practices and promotes public health,” states AMA Executive Vice President and CEO James L. Madara, MD, in the letter. Read the letter.
Helping to ensure the financial stability of NC medical practices during this pandemic is key to our longterm mission of improving the health of North Carolinians.
Emotional Support for You
Two hotlines and a support group are immediately available to help health care professionals deal with the emotional and psychological toll of the COVID-19 pandemic.
As already reported, the Physician Support Line – 1-888-409-0141 – was created in March to provide confidential peer-to-peer support for MD’s/DO’s working on the frontlines of COVID-19. The Line is staffed by over 700 volunteer psychiatrists from across the country, and is now being supported from 8 a.m. until 3 a.m. 7 days a week.
Another North Carolina option is the newly created Hope4Healers hotline – 919-226-2002 – available 24/7 and staffed by a large volunteer force of licensed mental health professionals providing pro bono mental health support for health care workers on the front lines and their families. Callers will be connected to professionals who will provide short-term support to cope and build resilience. The conversations will take place through secure phone or video chat. This hotline now also provides services for childcare workers and first responders.
Hope4Healers is an initiative of the NC Department of Health and Human Services in conjunction with the Disaster Response Network of the North Carolina Psychological Foundation with help from the NC Psychiatric Association.
The NC Professionals Health Program (NCPHP) is offering a series of on-line Covid-19 support groups facilitated by mental health professionals all across the state. The facilitators are experienced in working with medical professionals and are known to NCPHP.
These groups will support and provide a place to share your struggles, your victories and allow you to connect with other medical professionals in your community who are going through the same emotions. NCPHP is providing these groups as a free service and attendance in these sessions will be not be shared with our organization, or any others.
If you are interested, please email your name and closest urban area, e.g., John Doe – Greenville, to [email protected]. The information will be passed along to the group facilitator who will reach out to you with information about the group time and on-line format. NCPHP hopes to get at least six interested group members to start a group.
If you have any questions, please reach out to NCPHP CEO Joe Jordan, PhD, at [email protected] or to NCPHP Medical Director, Clark Gaither, MD at [email protected].
In the News
Childhood Vaccinations Plunge Since COVID-19 Pandemic Started, CDC Says, CNN, 5-8-20
Learning Opportunity
Southern Regional AHEC and Cape Fear Valley Health will present “Addressing Health Disparities During a Pandemic: Inaction and Inequity OR Inclusion and Innovation?” on Wednesday, June 3 from noon to 1 p.m. Kenyon Michael Railey, MD, Assistant Professor in the Department of Community & Family Medicine as well as Assistant Chief Diversity Officer in the Duke University School of Medicine, will present this webinar. There is no charge. Learn more and register here.
HB 1077 - Ban the Box for COVID-19
HB 1077 - Ban the Box for COVID-19 for COVID-19 State of Emergency
Primary Sponsors: Rep. Vernetta Alston (D-Durham), Rep. Marcia Morey (D-Durham), Rep Zack Hawkins (D-Durham)
Summary
This bill would ban the box for employment and prohibit housing discrimination based upon a person's criminal history during the COVID-19 emergency.
The bill would appropriate $130,000 in recurring funds for an attorney position within the Department of Justice to receive, investigate, and respond to complaints.
History
- 5/14/2020 - Filed
- Committee Referrals: Regulatory Reform, Judiciary, Appropriations, Rules
HB 1076/SB 779 - PPE for Working Inmates/PPE Prison Report
HB 1076/SB 779 - PPE for Working Inmates/PPE Prison Report
Primary House Sponsors: Rep. Vernetta Alston (D-Durham), Rep. Marcia Morey (D-Durham), Rep. Zack Hawkins (D-Durham)
Primary Senate Sponsors: Sen. Natalie Murdock (D-Durham), Sen. Joyce Waddell (D-Mecklenburg), Sen. Harper Peterson (D-New Hanover)
Summary
This bill would require inmates working in a State prison or Correctional Enterprises to be provided Personal Protection Equipment during the current State of Emergency.
The bill directs the Department of Public Safety to report to the Joint Legislative Oversight Committee regarding it's distribution of PPE.
The bill appropriates $100,000 for PPE and inmate medical costs.
History
House
- 5/14/2020 -Filed
- Referred to Appropriations, and Rules Committees
Senate
- 5/14/2020 -Filed
HB 1075/SB 792 - Unemployment Modifications
HB 1075 /SB 792- Unemployment Modifications
Primary House Sponsors: Rep. Vernetta Alston (D-Durham), Rep. Sydney Batch (D-Wake), Rep. Yvonne Holley (D- Wake), Rep. Rachel Hunt (D-Mecklenburg)
Primary Senate Sponsors: Sen. Wiley Nickel (D-Wake), Sen. Jay Chaudhuri (D-Wake)
Summary
This bill would amend the unemployment security laws to increase eligibility from 20 weeks to 26 weeks. The bill would increase the maximum weekly benefit from $350 to $450 with the calculation based on the average of the two highest paid quarters. Current payment is calculated based on the last two quarters.
The bill would provide unemployment benefits for spousal relocation, health reasons, or undue hardship.
The bill appropriates $100,000 to the Division of Employment Security to conduct a statewide awareness campaign of these provisions and directs the Legislative Research Commission to study the feasibility of establishing unemployment work sharing or short term compensation program.
HB 1073 - NC Freedom to Work Act
HB 1073 - NC Freedom to Work Act
Primary Sponsors: Rep. Jeff McNeely (R-Iredell), Rep. Wayne Sasser (R-Stanly), Rep. Bobby Hanig (R-Currituck), Rep. Steve Jarvis (R-Davidson)
Summary
This bill would limit penalties for violations of executive orders during COVID-19 and local prohibitions and actions by occupational licensing boards.
This bill would set the maximum violation of $25 and $1 per day for each subsequent violation.
History
- 5/14/2020 - Filed
- Referred to Commerce, Judiciary, and Rules Committees
NCMS Political Pulse for May 15, 2020
Watch as NCMS Director of Legislative Relations Sue Ann Forrest, MPA, updates you on the latest committee meetings, our new White Coat Wednesday format and a reminder about election season, which is just around the corner.
NCMS Morning Rounds 5-15-20
Happy Friday! Be well and enjoy your
NCMS Morning Rounds.
May 15, 2020
State Offers List of COVID-19 Testing Sites
As the state seeks to ramp up testing and contact tracing for the COVID-19 virus, an updated list of testing sites throughout the state is now available. View the list to find locations in your county.
The NC Department of Health and Human Services (NCDHHS) reiterated its guidance that anyone who is suspected of being infected with COVID-19 or has been exposed to someone with the virus should consider being tested. See the updated guidance issued on April 20 on the NCMS COVID-19 webpage.
Practice Resumption Resources
As the state eases some of the restrictions associated with the COVID-19 pandemic, some practices that suspended non-essential procedures or closed completely to stem the spread of the virus, may be looking for how best to resume services. A new AMA checklist provides helpful step-by-step guidance to manage the safe reopening of practices in a manner that protects patients, clinicians, staff and the public. Learn more and download the checklist here.
On the NCMS COVID-19 webpage, we have compiled specialty specific information on resuming practice operations. Access those resources by visiting our COVID-19 webpage and scrolling down to the ‘Resources as You Reopen’ heading.
NC MedAssist Meets Critical Need
NC MedAssist, founded in 1997 by several NCMS members in Mecklenburg County, is the only free mail-order pharmacy serving all 100 counties in NC. Although best known for its mobile pharmacy events where volunteers distribute over-the-counter (OTC) medicine in impoverished communities, this organization’s primary focus is their Free Pharmacy Program. With the COVID-19 pandemic causing massive unemployment and oftentimes accompanying loss of health insurance, this program is critical now more than ever.
Since the COVID-19 outbreak, NC MedAssist has restructured their services to be more digitally available. They have added their enrollment application online, as well as transitioned their Free Over-the-Counter Store (located in Charlotte) into a curbside pick-up retail pharmacy with online ordering available. They have also extended re-certification deadlines for current patients who may need additional time to gather their required documentation. For those who may suddenly need assistance, the enrollment process is now available online. Patients may enroll in the Free Pharmacy Program here.
You can refer patients to the NC MedAssist website or have them call 1(866)331-1348 to learn more about the program and whether they qualify for assistance.
Other actions you can take to increase awareness of the Free Pharmacy Program and connect those in need with NC MedAssist's services include:
• Share NC MedAssist social media posts within your network. Find them at Facebook: @NCMEDASSIST or Linked In.
• Schedule a Mobile Free Pharmacy Drive-Thru event or an OTC Medicine Drop. For more information contact Kinzie Luce, event manager at 704-350-3574 or at [email protected].
• Consider a donation to the NC MedAssist COVID-19 Crisis Fund to ensure the necessary funds to continue to serve the influx of patients due to loss of jobs or insurance due to the COVID-19 pandemic. Learn more and donate.
Last year, NC MedAssist served 18,805 patients and dispensed 229,805 prescriptions valued at $68 million dollars to low-income, uninsured individuals throughout North Carolina. Once enrolled in the Free Pharmacy Program, prescription medication is mailed directly to the patient’s home, usually providing a 90 day supply.
In the News
Telehealth is Having ‘a Moment’ Amid COVID-19. Will It Last?, The Advisory Board Forum, 5-13-20
Learning Opportunity
Two important weekly learning opportunities are taking place today, Friday, May 15:
The NCMS Foundation’s Kanof Institute for Physician Leadership Power Hour from 1 to 2 p.m. will focus on the NC Medical Board’s response to COVID-19. Learn more and join the conversation.
The NC Division of Public Health subject matter experts will be on hand to answer your questions in its weekly Friday Forum from 12:30 to 1:30 p.m. Please send your questions to [email protected]. And tune in via Zoom here. Or call in at +1-646-558-8656 and enter ID number 705979628#
NCGA House Health COVID-19 Working Group
 The NCGA House Health COVID-19 Working Group met on Thursday, May 14, 2020.
The NCGA House Health COVID-19 Working Group met on Thursday, May 14, 2020.
Secretary Mandy Cohen, MD provided a COVID-19 overview. The NCDHHS case count can be found here.
As of May 13, 2020 there were
Sec. Cohen noted that the coordinated action plan includes increasing the number of collection sites and working closely with Local Health Departments for county expertise.
The State will be distributing 1 million sets of PPE to over 3,000 facilities across NC including skilled nursing facilities, adult care homes, and group homes.
Sec. Cohen emphasized the importance of the 3 Ws:
- WEAR a cloth face covering
- WAIT 6 ft. apart
- WASH your hands often or use hand sanitizer
Christie Burris, Executive Director of the NC Health Information Exchange Authority provided an overview that over 55,000 providers have contributed records, with approximately 700k messages flowing into the system daily. There are over 9 million unique patient records.
Burris highlighted that the COVID-19 pandemic has highlighted the systemic issues across the U.S. with clinical data sharing and the need for a comprehensive data sharing ecosystem.
She added that the NC*Notify option has been helpful to providers to receive alerts as their patients seek care. However, there are expansion opportunities to the system that could help the health care community live improving access to data for follow up like COVID-19 results, use of the HIE master patient repository for matching patients, enhancing logic for finding more cases and symptoms, integrating statewide surveillance systems, and publishing current dashboard for real time feedback of policy decisions.
Catherine Moore, PhD, RN, Regulatory Consultant for the NCBON suggested 3 main issues for the NCGA to consider:
- Statutory authority for the creation of waivers
- Organizational policies for nursing
- Personal protection equipment
Representatives from the Association for Home & Hospice Care of NC informed the Committee that 86% of home and hospice agencies surveyed indicated difficulty in obtaining PPE. They also noted that the increased cost of PPE was a limitation.
They requested that the temporary Medicaid rate increases remain permanent through phase 2 of COVID-19. The current rate increases would only get most providers close to national averages in their service areas.
The NC Assisted Living Association made the following suggestions for relief for their members:
- Establishing a dedicated facility for COVID-19 residents
- Funds for additional costs for these facilities
- Funds to cover redesign of visitation areas to address isolation and maintain safety
- Funds to purchase technology to improve communication and safety
- Enhancing testing availability to include rapid test kits
- Supplemental funds for hazard pay
NCMS Morning Rounds 5-14-20
Already Thursday and time for your
NCMS Morning Rounds.
May 14, 2020
More Loan Funding Available for NC Small Businesses
Included in the recently signed into law 2020 COVID-19 Recovery Act legislation is $125 million allocated for small business loans. The loans will be administered through the Golden Leaf Foundation. The initial application for an NC COVID-19 Rapid Recovery loan takes only about 15 minutes to complete and could mean up to $50,000 to assist your practice. Learn more and apply here.
The COVID-19 Rapid Recovery loan is designed to fill lending gaps, including while businesses are waiting on SBA loans. Note: this is not a forgivable loan. These loans are six months payment-free. At the end of the six-month period, the loans will be termed out for 48 months at 5.5 percent interest.
We Appreciate Our Business Alliance Members
With the COVID-19 pandemic changing so many aspects of how we live and work, we are especially grateful to our three newest NCMS Business Alliance members. Welcome to Parsec Financial, AbbVie and Professional Risk Associates (PRA).
These organizations recognize that Business Alliance membership, even during these unusual times, offers a new way to interact with the NCMS and its members to foster long-term, meaningful relationships. Now more than ever, our physicians and PAs are seeking innovative community partnerships as we all respond the pandemic.
We thank all our Business Alliance members and particularly Parsec Financial, AbbVie and PRA for helping provide our members with the necessary tools to improve the health of all North Carolinians now and in the future.
If you or a business in your community would be interested in becoming part of our Alliance, please visit our NCMS Business Alliance webpage to learn more. Or contact Pam Highsmith, [email protected], or (919) 830-4127.
Tool to Assess COVID-19 Impact on Health Care Workers
Clark Gaither, MD, medical director for the NC Professionals Health Program (NCPHP) and family physician in Goldsboro, recently alerted readers of his ‘Dr. Burnout’ blog a new tool to assess the impact of the COVID-19 pandemic on health care workers.
Called the ‘Pandemic Experience & Perception Survey’ (PEPS), the tool is a 35-item questionnaire for working adults, for group administration, and takes about 5- 10 minutes to complete online. It has been designed to measure employees’ experiences working during a pandemic and provides for real-time results reporting. The stated purpose of the survey is to, “measure the extent of pandemic impact, work resources, risk perception, employee work-life, and leadership,” Dr. Gaither writes.
Learn more about how to access this assessment on Dr. Gaither’s blog, which is focused on helping health care workers, who are burned out, retool and reignite their passion and purpose. See the latest blog post on the PEPS.
The NCMS also has compiled a list of Emotional Support Resources specifically for addressing the impacts of the COVID-19 pandemic on health care teams. View those on our webpage.
In the News
No Intubation: Seniors Fearful of COVID-19 Are Changing Their Living Wills, Kaiser Health News, 5-12-20
Learning Opportunity
The National Academy of Medicine’s Action Collaborative on Countering the US Opioid Epidemic will hold a day-long Public Virtual Symposium on May 21 beginning at 8:30 a.m. Speakers will address the highest priority elements of the nation’s response to the opioid epidemic particularly in the context of the COVID-19 pandemic.
Learn more and register to attend this free, virtual symposium – you are welcome to attend for the whole day or for any session that you find interesting.
NCGA Revenue Laws Study Committee
 The NCGA Revenue Laws Study Committee met on Wednesday, May 12, 2020 at 10:00am.
The NCGA Revenue Laws Study Committee met on Wednesday, May 12, 2020 at 10:00am.
The Committee began the discussion of this bill draft at its March Meeting.
The bill contains three parts:
- Relief to auctioneers and estate sale companies
- Expands scope of sales and use tax exemption for equipment purchased by a large fulfillment facility
- Clarifies sales tax on digital property
- Educational service by certain institutions whether live or recorded is not a taxable event
- Homeschool exemptions for sales of digital and audio works
- Pre-recorded or on demand webinars would be taxable, live/real time would remain non taxable
The fiscal note for this bill indicated that these changes would likely result in an insignificant revenue loss.
The bill draft was revised and received a favorable report.
The bill draft was presented by the NCGA Fiscal Research Division and the Legislative Analysis Division.
The draft incorporates the following:
- Consideration of tax changes enacted in the federal CARES Act on March 27, 2020 (new)
- Change the medical expense deduction from 10% to 7.5% fro the 2019 and 2020 tax years
- Loan forgiveness of a covered loan/Paycheck Protection Program
- Increase % of adjustable income limitation on the deduction of business interest from 40% to 50% for 2019 and 2020
- Decouples from income exclusion for forgiveness of debt on primary residence, mortgage insurance deductible as mortgage interest, and deduction for tuition and expenses
- IRC bill draft discussed at February and March meetings
- Two Technical and clarifying bill drafts discussed in the February and March meetings
- Extension of two sunset provisions discussed at the March meeting
NCGA House COVID-19 Economic Working Group
 The NCGA House COVID-19 Economic Working Group met on Tuesday, May 12, 2020.
The NCGA House COVID-19 Economic Working Group met on Tuesday, May 12, 2020.
The Committee staff explained that in recents months NC has seen an increase of debt settlement company activity. With hundreds of thousands of workers losing jobs, they anticipate a surge of debt settlement abuses that can be avoided by updating some laws. The laws regarding debt settlement have not been updated since 2005. The Attorney General’s Office has also identified abusive transactions that this bill draft would help prevent moving forward.
Both the Resident Lenders of NC and the NC Justice Center support modernizing debt settlement to enhance protections for debtors under financial strain caused by COVID-19.
Modernize Debt Settlement Draft
The bill would move the prohibition of debt adjusting and debt settlement from the criminal chapter into the civil chapter on consumer protection and would expand the prohibition to include the following:
- Conduct of affiliates to determine if debt adjusting or debt settlement occured
- Treat any fees pad as consideration, regardless of when paid
- Make debt adjusting and debt settlement under trade practice subject to civil remedies by the Attorney General
- Void any contracts for debt adjusting or debt settlement
The NC Medical Society is following this legislation due to the impact it could have on individuals in this financial situation.
NCMS Morning Rounds 5-12-20
It's Tuesday and time for your
NCMS Morning Rounds.
May 12, 2020
LAST CHANCE TO WIN: Please answer these few questions about the NCMS' LEAD Health Care Conference in October. Beyond helping to ensure the conference is helpful to you, you’ll have a chance to win a $100 Amazon Gift Card. Answer these crucial questions now by clicking HERE.
Medicaid 5 percent ‘Bump’ Will Be Automatic
NC Department of Health and Human Services (NCDHHS) officials have confirmed that the 5 percent Medicaid fee-for-service increase for all providers authorized in the General Assembly’s COVID-19 relief legislation and signed into law by Governor Roy Cooper, will be retroactive to March 1 and will accrue automatically. Practices do not need to refile those Medicaid claims. For a summary of all the provisions in the COVID-19 relief package see the NCMS Legislative blog.
In other news from NCDHHS:
As the state moves into phase one of easing some COVID-19 restrictions, NCDHHS has launched a public awareness campaign around ‘knowing your Ws’ -- Wear a face covering; Wait six feet apart and Wash your hands. The Department is providing materials to post and share on social media in English and Spanish. Download them here. For any questions about face coverings, NCDHHS offers these answers in English and Spanish based on the Centers for Disease Control and Prevention (CDC) guidance.
A new portal has been created to file claims for COVID-19 testing and treatment of uninsured patients retroactive to Feb. 4, 2020. The Health Resources & Services Administration (HRSA) COVID-19 Uninsured Program Portal was launched by the federal Department of Health and Human Services (HHS) to support health care providers in delivering COVID-19 diagnostic testing and treatment at no cost to patients. Access the portal.
New videos detailing the behavioral health impact of COVID-19 are now available including one in which Kody Kinsley, NCDHHS Deputy Secretary for Behavioral Health & Intellectual and Developmental Disabilities, discusses the second curve for COVID-19 - the behavioral health impacts. Watch this 5-minute video here. Other brief, 1-minute videos on a variety of COVID-19 related topics are available online here in English and Spanish.
The NCDHHS COVID-19 website has been updated to be more user-friendly and easier to navigate. Visit the website here.
Survey Confirms Practices Are Financially Struggling
The latest survey results from the joint survey done weekly for the last five weeks by the NCMS, NC Medical Group Management Association and Curi are now available. The survey is designed to track trends in the challenges medical practices are facing as they respond to the COVID-19 pandemic. Last week, the survey took a deeper dive into the financial issues you may be facing and how the federal relief programs are helping – or not.
The striking results show that of those responding to the survey 20 percent of the practices had a revenue drop in excess of 75 percent due to the pandemic. Most of the responding practices (90 percent) had revenue decreases of at least 25 percent.
A more detailed summary of the results is available here.
In addition to the regular questions about demographics and the status of medical practices in the state, this week’s survey takes a closer look at telehealth. Ensuring telehealth parity is a priority for the NCMS advocacy team and we look forward to reviewing the survey results to glean more insights into your experience with telehealth during the pandemic. Please take just a moment to respond to this week’s survey if you haven’t already.
May is Mental Health Awareness Month
As a recent Kaiser Family Foundation (KFF) article stated: “the COVID-19 pandemic and resulting economic downturn have negatively affected many people’s mental health and created new barriers for people already suffering from mental illness and substance use disorders.
“In a recent KFF poll, nearly half (45 percent) of adults in the United States reported that their mental health has been negatively impacted due to worry and stress over the virus. As the pandemic wears on, it is likely the mental health burden will increase as measures taken to slow the spread of the virus, such as social distancing, business and school closures, and shelter-in-place orders, lead to greater isolation and potential financial distress.”
This May’s Mental Health Awareness month observance takes on special significance because of the impact of the COVID-19 pandemic. Federal and state agencies and organizations are offering resources to health care professionals and their patients to address mental health and behavioral issues during these stressful times.
The Centers for Medicare & Medicaid services (CMS) is reminding physicians and PAs that Medicare covers:
• Telehealth counseling services during the COVID-19 public health emergency.
• Other outpatient mental health services, including depression screening, individual and group psychotherapy, and family counseling – learn more here.
• Counseling and therapy services from a Medicare-enrolled opioid treatment program (OTP) by telehealth options or telephone only.
The NC Psychiatric Association offers this reference guide for providers.
And NCDHHS offers a webpage with the latest policies and services to help ensure mental and behavioral health during the pandemic.
The NCMS’s Emotional Support Resources page offers you, our members, a compilation of helpful resources to help support your mental well-being during this unprecedented and challenging time.
In the News
Routine Vaccinations for US Children Have Plummeted During the COVID-19 Pandemic, STAT, 5-8-61
Learning Opportunity
Be sure to tune in for the NCMS Foundation/Kanof Institute for Physician Leadership Power Hour on Friday from 1 to 2 p.m. This week’s hour will focus on the NC Medical Board’s (NCMB) response to the COVID-19 pandemic.
The NC Medical Board has taken many steps since March to support the state’s response to COVID-19. NCMB’s primary goals are to remove barriers and support physicians, physician assistants and the state’s health care system as a whole during this rapidly-evolving pandemic. How has NCMB responded to requests from Gov. Cooper, NC DHHS, health systems, licensees and member associations such as the NC Medical Society? What steps has NCMB taken to be more flexible and responsive during the current state of emergency?
Join a conversation moderated by Franklin Walker, MBA, NCMS VP of Rural Health Systems Innovation with speakers from the NC Medical Board: Bryant Murphy, MD, Board President, Thom Mansfield, Chief Legal Officer, Evelyn Contre, Chief Communications Officer, and Marcus Jimison, Sr. Staff Attorney. Register here.
The KIPL Power Hour aims to provide a forum for ongoing conversation, collaboration and community. Tune in to Power Hour weekly to hear from different experts, decision makers and influencers on a variety of topics. The format is informal and conversational and sessions are easy to access through Zoom. Power Hours will be recorded and made available to you through your NCMS Morning Rounds and on the KIPL webpage.
NCGA Program Evaluation Committee
 The NC General Assembly Joint Legislative Oversight Program Evaluation Committee met on Monday, May 11, 2020.
The NC General Assembly Joint Legislative Oversight Program Evaluation Committee met on Monday, May 11, 2020.
The agenda included a presentation on a new bill draft for ABC violations.
NCMS monitored the Committee to follow the second agenda item which included a brief overview of all of the current Program Evaluation Division projects.
Current Bill Drafts
HB 1047/SB 708 CPS Intake Screening
Primary Sponsors: Rep. Craig Horn (R-Union), Sen. Chuck Edwards (R-Buncombe), Sen. Joyce Kraweic (R-Forsyth), Sen. Jim Burgin (R-Harnett)
These bills prohibit county departments of social services from implementing child protective services intake screening criteria that are more stringent than state policy and requires DHHS to make various policy changes as a means to improve the child protective services intake screening process.
HB 1053 Military Occupational Licensure
Primary Sponsor: Rep. Craig Horn (R-Union)
This bill would require an expedited occupational licensure application response of 30 days when an applicant is military trained or is a military spouse. The bill would also require each occupational licensure board and the Department of Military and Veterans Affairs’s websites to summarize the opportunities available to veterans and spouses.
Program Evaluation Division Work Plan
This plan illustrates the scope of work of the Division during this legislative session.
The next meeting in June will include the report on NC FAST. Progress can be seen on the Program Evaluation Division website.
Some current evaluations underway include Department of Public Safety Reorganization, Diversity in Teacher Workforce, and Coordination with Non-profits in Disaster Recovery.
One evaluation that has not started yet is the, NC Innovations Waiver Services. This evaluation will review the efficiency and effectiveness of the NC Innovations Waiver including eligibility determination, plan of care developmen and approval, development of budgets, and LME/MCO management and monitoring of services.
The NCMS lobbying team will continue to monitor each of these evaluation projects to aid in improving the health of all North Carolinians.
NCMS Morning Rounds 5-11-20
Welcome to a new week and your
NCMS Morning Rounds.
May 11, 2020
REMINDER: Please answer these few questions about the LEAD Health Care Conference in October. Beyond helping to ensure the conference is helpful to you, you’ll have a chance to win a $100 Amazon Gift Card. Answer these crucial questions now by clicking HERE.
NCMS Legislative Update
Last Monday, Governor Roy Cooper signed into law the two bills passed by the General Assembly over the previous weekend. At a signing event, NC House and NC Senate leadership stood with the Governor and said they looked forward to working together to address the impact the COVID-19 pandemic is having on the state.
This week the NC House COVID-19 working groups will meet to address health, education and other issues in response to the pandemic. If you have any issues you are facing in your practice that need to be addressed by the legislature, please reach out to NCMS Director of Legislative Relations Sue Ann Forrest, MPA at [email protected]. The NCMS advocacy team will be working closely with legislators in the coming days and weeks to be sure they fully understand the challenges you are facing.
In particular, we will be focused on telehealth. If you have examples of what telehealth policies and practices are working and which remain challenges, please let us know, so we can better describe the issues to legislators.
We also were pleased to host a call for NCMS members with NC Department of Health and Human Services (NCDHHS) officials last Wednesday. We hope to have another call in which you can get your questions answered by those at NCDHHS. Watch your NCMS Morning Rounds and your email for details.
BCBSNC Extends Certain COVID-19 Related Policies
Blue Cross and Blue Shield of North Carolina (Blue Cross NC) announced last Friday that it is extending its expanded telehealth measure through July 31, 2020 and will reevaluate if an additional extension is needed as July 31 approaches. Learn more about the telehealth extension.
The state’s largest commercial insurer also extended the deadlines for other COVID-19 related policy measures including waiving member copays, deductibles and coinsurance for COVID-19 related clinical visits and testing as well as allowing early medication refills and waiving certain prior authorization requirements. Get the details here.
Also, effective May 15, Blue Cross has said it will no longer cover hydroxychloroquine and chloroquine outside of a hospital setting. Late last month, the FDA updated its drug safety information regarding use of hydroxychloroquine and chloroquine for COVID-19 outside the hospital setting or a clinical trial. The FDA cited the risk of heart rhythm problems. This announcement does not affect FDA-approved uses for malaria, extraintestinal amebiasis, chronic discoid erythematosus, systemic lupus erythematosus and rheumatoid arthritis. Learn more here.
GoFundMe Campaign to Procure Masks for Those at Risk
NCMS Foundation’s Kanof Institute for Physician Leadership faculty member Lawrence Greenblatt, MD along with his colleagues Eric Westman, MD, and Wickham Simonds, MD and medical students from Durham are trying to quickly mobilize large numbers of masks to give to those in the Triangle most at risk because of where they live or where they work.
To help the effort they’re calling ‘Covering the Triangle,’ Dr. Greenblatt has created a GoFundMe campaign with at $50,000 goal. As of last night, more than $27,000 had been raised and more than 30,000 masks procured. Learn more and consider a donation at the GoFundMe campaign page.
The project was recently featured in a Raleigh News & Observer article in which Dr. Greenblatt stated the need for the masks: “Evidence shows if you wear a mask, then there’s a lot less of the asymptomatic spread.”
In the News
To Strengthen the Public Health Response to COVID-19 We Need Community Health Workers, Health Affairs, 5-6-20
Learning Opportunity
Join Southern Regional AHEC for two upcoming Cape Fear Valley Hospital Grand Rounds sessions:
Duke Critical Care Specialist Paul E. Wischmeyer, MD presents ’Critical COVID Illness Recovery: Lessons Learned from Post ICU Syndrome’ on May 20 from 12:30 to 2:30 p.m. Learn more and register.
Duke Family & Community Medicine Professor and School of Medicine Assistant Chief Diversity Officer Kenyon Railey, MD presents ‘Addressing Health Disparities During a Pandemic: Inaction & Inequity OR Inclusion & Innovation?’ June 3 from noon to 1 p.m. Learn more and register.
NCMS Morning Rounds 5-8-20
It's Friday and time for your
NCMS Morning Rounds.
May 8, 2020
REMINDER: Please answer these few questions about the LEAD Health Care Conference in October. Beyond helping to ensure the conference is helpful to you, you’ll have a chance to win a $100 Amazon Gift Card. Answer these crucial questions now by clicking HERE.
SBA Extends Deadline to Return PPP Loans
The US Small Business Administration (SBA) has extended the safe-harbor period for returning Paycheck Protection Program (PPP) funds by one week to May 14. Today, May 8, the original deadline, was initially provided for entities that received PPP funds but then determined they were unable to certify in good faith that their PPP loan was necessary. Learn more here.
For more information on the PPP and other financial relief programs to offset the impact of the COVID-19 pandemic, visit the NCMS Economic Relief Resources page here.
Wake County Planning for Mass Testing
Wake County is gearing up to implement plans for mass testing to support the phased opening of the community as described in Governor Cooper’s latest Executive Order.
The county has asked the NCMS to help them assess how much current testing is being conducted in the county and how many community partners are planning to test in the future.
If you are in Wake County, please take just a minute to complete this survey by NOON TODAY.
Kudos to Dr. Mims!
Longtime NCMS member and NCMS Foundation Leadership College alumna, Susan Mims, MD, MPH, has been named chair of the newly established Department of Community and Public Health at UNC Health Sciences at MAHEC.
Dr. Mims will provide strategic leadership for the Asheville-based master of public health program affiliated with UNC Gillings School of Global Public Health and UNC Asheville. She will work closely with the Director of Academic Affairs, Amy Lanou, PhD, and program faculty to train future public health leaders in innovative models of public health delivery across Western North Carolina.
Dr. Mims will also help guide population health initiatives at UNC Health Sciences at MAHEC that include supporting a regional response to the COVID-19 pandemic, rural health initiatives, and health professions education programs spanning high school through post-fellowship rural teaching practices.
Learn more in this press release. And congratulations, Dr. Mims!
In the News
Doctors Without Patients: 'Our Waiting Rooms Are Like Ghost Towns', The New York Times, 5-5-20
Learning Opportunity
Don’t forget TODAY’s Power Hour from 1 to 2 p.m. This week’s discussion will examine how you can take care of yourself as you deal with the stresses of this unprecedented pandemic. Franklin Walker, MBA, NCMS VP of Rural Health Systems Innovation, will moderate the conversation that features Cormac O’Donovan, MD, and Marion McCrary, MD, who both have a passion for wellness and stress reduction. Please register here for this informative conversation.
RTI is holding a webinar series to share the outcomes of its survey of 2000 Americans to capture their understanding of how the COVID-19 virus is transmitted and level of support for community mitigation strategies. The upcoming webinars include:
- Wednesday, May 13 from noon to 1 p.m. “Knowledge” – what do Americans know and understand about COVID-19?
• Wednesday, May 20 from noon to 1 p.m. “Perceived Threat” – how does the country view the risk of COVID-19 to their families and certain populations?
• Wednesday, May 27 from noon to 1 p.m. “Vaccination” – what are Americans’ perceptions on what a vaccine would mean and would they use it?
NCMS Morning Rounds 5-7-20
Happy Thursday!
Enjoy your NCMS Morning Rounds.
May 7, 2020
Summary: COVID-19 Update Call With State Officials
Last night in a call with NCMS members, State Health Director Elizabeth 'Betsey' Tilson, MD, MPH, and NC Medicaid Chief Medical Officer Shannon Dowler, MD, CMO shared the latest on the state's response to the COVID-19 pandemic.
NC Department of Health and Human Services Secretary Mandy Cohen, MD, MPH led off the conversation stating that thanks to the state's "early and aggressive action" to implement social distancing and other restrictions, the state has 'flattened the curve,' and avoided overwhelming the state's health system resources for the moment.
Secretary Cohen stressed that, even though the restrictions may be easing somewhat, we will be living a new and different style of life for the foreseeable future. Her department is working to educate the public about continued safety measures using the easy to remember '3 W's -- wash your hands, wear a mask and wait six feet apart.' She also said NCDHHS will be working to reassure patients that it is safe and important that they continue to receive routine care, especially getting their children vaccinated.
In her remarks, Dr. Tilson spoke about testing and tracing, saying that lab capacity is high, now the challenge is to "get people's noses swabbed." She noted that testing sites are ramping up including several high volume testing sites at Walgreens and Walmart. Eventually, the state hopes to have 20 of these sites up and running across the state.
In addition to hiring tracers with the help of CCNC and NC AHEC, Dr. Tilson called on practices to become part of the surveillance network charged with tracking both symptomatic and asymptomatic cases, to help gather data on the spread of the virus.
Dr. Dowler outlined the work on all fronts in NC Medicaid to address the impact of the pandemic, but spent the majority of her presentation on telehealth. She said NC Medicaid is closely examining what telehealth elements, many of which have been implemented rapidly in response to COVID-19, should be retained after the pandemic has subsided. She noted that everything that is currently in place will continue until at least July 25. She also reassured those on the call that NC Medicaid would give practices at least a month's notice before anything is 'turned off.'
"We realize this is all incredibly disruptive to you and your patients," she said.
Aaron McKethan, Ph.D, a senior policy fellow at Duke University Margolis Center for Health Policy, gave a high level overview of the COVID-19 modeling process he, and others, are working on for the state. He summed up by saying that we are starting May with lower viral spread thanks to the social distancing put in place and as a result hospital capacity is good in the immediate and near term. The new areas to watch are local hot spots and the shift in growth rates to rural areas of the state, he said.
"It's very important we don't become complacent," he cautioned.
See the slides from all the presentations.
NCMS CPP Practices and Others Are Thankful
This week NCMS staff members continued distribution of masks donated by Centene and Carolina Complete Health (CCH) to our Community Practitioner Program (CPP) practices. These practices in rural and underserved areas of the state and were extremely grateful for the much needed personal protective equipment. Thank you to the generosity of NCMS partners Centene and CCH these practices can continue to serve their communities!
The Carousel Center in Wilmington and G&G Healthcare in Cerro Gordo were two appreciative recipients.
If you are looking to acquire PPE for your practice, the NCMS has arranged group purchasing through the Charleston County Medical Society in South Carolina as well as through North Carolina manufacturers. Learn more and place an order today at this webpage.
Centene and CCH also recently distributed $1,000 worth of Walmart gift cards to Federally Qualified Health Centers (FQHC) in the state. The centers may distribute the $35 gift cards to those in need of essential health care items available at Walmart.
A big thank you to CCH and Centene!
NC HIE/NC HealthConnex Update
The COVID-19 Recovery Act, which Governor Roy Cooper signed into law on Monday, extends the June 1, 2020 connection requirement to the state Health Information Exchange (NCHIE or NC HealthConnex) to Oct. 1, 2021.
In addition, all providers who have shown a good faith effort to connect to NC HealthConnex and have a valid Participation Agreement on file will also have the extended deadline of Oct. 1, 2021 and do not need to take further action. This extension will allow the large queue of health care providers who are in active onboarding to complete the connection process. Connecting to NC HealthConnex can take up 12 months, depending on your EHR software. The NC HealthConnex technical team will reach out when technical discussions are to begin with your practice.
Please email [email protected] with any questions. Visit the NC HealthConnex website for periodic updates.
In the News
Why Weren’t We Ready for the Coronavirus? The New Yorker, 5-4-20
Learning Opportunity
Join the National Academy of Medicine’s Action Collaborative on Clinician Well-Being and Resilience TODAY, Thursday, May 7 from 1:30 to 3 p.m. for a webinar on Supporting Clinician Well-Being During COVID-19. This webinar will provide a timely discussion and platform for physicians, nurses, students and health system leaders to delve into the critical needs, priorities and emerging strategies to support the mental and emotional well-being of clinicians on the frontlines – both during and beyond the COVID-19 pandemic. Learn more and register.
NCMS Morning Rounds 5-6-20
Halfway through the week!
Enjoy your Wednesday NCMS Morning Rounds.
May 6, 2020
Today marks the start of National Nurses Week, celebrated annually from May 6, also known as National Nurses Day, through May 12, the birthday of Florence Nightingale, the founder of modern nursing. We recognize and celebrate our nurses as an important part of the health care team -- now more than ever. Thank you for helping to protect and improve the health of our patients and our communities.
Crucial Questions about LEAD Conference – Please Help
Please help our 2020 NCMS LEAD Health Care Conference planning committee as it considers new and creative options to present conference content while accommodating any need -- or preference -- for virtual educational sessions. Committee members also are mindful of the many benefits of bringing people together and are contemplating how we might accomplish smaller, in-person gatherings to build community when possible.
We need your input, your ideas and opinions on what would be most helpful and appealing to you. Please take just a few minutes to answer the following brief survey. Everyone who responds will be entered into a drawing for a $100 Amazon Gift Card!
Helping Ensure Healthy Moms and Babies
The March of Dimes recently began offering Supportive Pregnancy Virtual Groups to provide social support to expectant individuals during this unusual time. The 30-minute meetings began last week and will be held every Thursday through a secure Zoom line or via phone.
These group sessions are designed to complement medical care and prenatal education, but are not intended to act as a replacement. The primary focus is to engage in conversation to foster peer learning and support. To supplement the Supportive Pregnancy Virtual Group sessions, participants will also have access to Becoming a Mom Online™ resources.
Each session will provide participants with an opportunity to share their knowledge and concerns about a particular topic, hear from an expert on that topic to help gain a better understanding, and learn a new stress relief strategy. March of Dimes staff will be helping to lead and moderate these weekly conversations.
Please visit the registration page for more information on the SPVG schedule.
Helping to ensure maternal and infant health through events like our maternal and infant health summits as well as through resources like these virtual groups is part of the NCMS’ longstanding mission of improving health throughout the state.
NCMS Staff Offers Thanks – to YOU!
The NCMS staff wants to offer a special thank you to YOU for all you are doing in the trenches to serve your patients and your communities during this pandemic.
In the News
Three Potential Futures for COVID-19: Recurring Small Outbreaks, a Monster Wave, or a Persistent Crisis, STAT, 5-1-20
Learning Opportunity
DON'T FORGET the NCMS member call with State Medical Director Elizabeth Tilson, MD, MPH and NC Medicaid Chief Medical Officer Shannon Dowler, MD, along with Aaron McKethan, a senior policy fellow at the Duke University Margolis Center for Health Policy and one of the people working on projection models of the COVID-19 pandemic in the state tonight at 7p.m. You can still submit questions until noon today by responding to this email with what you would like the presenters to address. Join the call by dialing 877-273-4202 and entering Conference Room Number: 8155758#
MAHEC is offering “Parenting in Place: Supporting Clients, Children and Therapists While Socially Distancing,” a three module series the first three Mondays in June (June 1, 8 and 15) designed for clinicians as well as lay people. Clinical psychologist Heather Ulrich, PhD, offers simple methods for helping clients sustain their sanity while simultaneously helping children thrive in a challenging environment. Learn more and register.
NCMS Morning Rounds 5-5-20
It's Tuesday and time for your
NCMS Morning Rounds.
May 5, 2020
News to note: Yesterday Governor Roy Cooper signed into law the COVID-19 relief package passed by the NC General Assembly over the weekend. The legislation included a number of policy provisions and financial relief to address the impact of the COVID-19 pandemic. Legislators are not done, however, and in addition to the House working groups that will continue meeting, both the House and Senate will be back to continue the session in two weeks. Review our summary of this legislative package, now signed into law, as well as more from the Governor’s press conference on the bill.
NCMB’s Guidance on Medical Training During Emergency
As directed in Governor Roy Cooper’s April 8 Executive Order #130, medical licensing boards are to provide guidance on the level of training and qualifications required for medical professionals to meet the state’s needs during the current state of emergency. The NC Medical Board (NCMB) issued that guidance on April 29. Read the NCMB’s memo outlining its guidance on training here.
“In considering how best to offer this guidance, NCMB quickly realized that it can’t predict the specific needs that may arise across North Carolina, or know the level of education, training and experience of clinicians facing new assignments and unfamiliar technologies or modalities,” writes NCMB President Bryant A. Murphy, MD, MBA, in the latest edition of the Board’s Forum newsletter. “That is why NCMB’s guidance boils down to this: self-assess, get training if you need it and rely on everything you’ve learned in your career.”
Dr. Murphy goes on to state that “NCMB believes the people on the ground doing the work are best positioned to know what is needed. We also trust you will assess the skills of any members of the health care team you supervise and ensure they get the training they need to work safely.”
Read Dr. Murphy’s entire Forum article here.
NCMS Business Alliance Partners Offer Resources
NCMS Business Alliance member Professional Risk Associates are standing by to help members like you as you grapple with the impact of COVID-19.
Professional Risk Associates, Inc., a medical professional liability independent agency, represents top-rated insurance companies to bring tailored coverage options to physicians. As a resource to help you be knowledgeable about your liability policy during this pandemic, they offer this one sheet list of potential policy adjustments to watch for.
Learn more about Professional Risk Associates here.
Be Recognized or Recognize Your Peers with an NCMS Award
As we do every year, the NCMS is seeking nominations for two awards – the E. Harvey Estes, MD, Community Service Award and the John Huske Anderson Award.
The E. Harvey Estes, MD, Physician Community Service Award recognizes a physician who has an outstanding record of community service that reflects well on the medical profession apart from their work or identification as a physician. Download the nomination form here.
The John Huske Anderson Award recognizes a layperson whose contributions have had a positive impact on the medical profession and the public health in North Carolina. Download the nomination form here.
Nominations are due to Evan Simmons, [email protected] by Aug. 1, 2020.
In the News
The Essential Workers Filling New York’s Coronavirus Wards, The New Yorker, 5-1-20
Learning Opportunity
This Friday’s Power Hour will examine how you can take care of yourself. While there has been increased attention to stress and burnout among clinicians for some time, dealing with this unprecedented pandemic puts a new spin on how stress affects us in our everyday lives and how we can address that. Please join us on Friday, May 8 from 1 to 2 p.m. for a conversation around self-care and wellness that includes talking about healthy habits but also goes beyond to talk about handling loss of control both personally and professionally. How does, for example, organizational culture impact our well-being and what do we do when we feel we cannot do anything?
Franklin Walker, MBA, NCMS VP of Rural Health Systems Innovation, will moderate the conversation that features Cormac O’Donovan, MD, and Marion McCrary, MD, who both have a passion for wellness and stress reduction. Please register here for this informative conversation.