Governor Signs COVID-19 Relief Bills
 On Monday May 4, 2020, Governor Roy Cooper signed HB 1043- 2020 COVID-19 Recovery Act and SB 704 - COVID-19 Recovery Act into law.
On Monday May 4, 2020, Governor Roy Cooper signed HB 1043- 2020 COVID-19 Recovery Act and SB 704 - COVID-19 Recovery Act into law.
Elected leadership from the North Carolina General Assembly was present for the signing including House Speaker Tim Moore, Democratic House Leader Darren Jackson, Senate President Pro Tempore Phil Berger, and Democratic Senate Leader Dan Blue.
Each elected official expressed that the bipartisan package helps put North Carolina on the path to recovery.
This relief package includes over $1.5 billion in relief for public health, education, small business assistance, and state government operations.
Some key provisions include:
- $5 million for NCMS to purchase personal protection equipment
- $25 million for enhanced COVID-19 testing and tracing
- $125 million for small business loans administered through the Golden Leaf Foundation
- $75 million for school nutrition programs
- $6 million for food banks
- $20 million to support local health departments and the State Health Lab
- $9 million for rural broadband
- $85 million for vaccine development, antibody testing, community testing, rural health care, and other COVID-19 related research at Duke University, UNC, East Carolina University, Wake Forest University, and Campbell University
- $1.7 million to study COVID-19 health disparities
- Waived interest on tax payments normally due in April
- Medical liability protections
- 5% Medicaid fee for service bump for all providers
For a complete breakdown of the health related portions of both bills view the NCMS Legislative Blog for the NCGA COVID-19 Relief package summary.
NCGA COVID-19 Package
 SB 704 - COVID-19 Recovery Act
SB 704 - COVID-19 Recovery Act
POLICY BILL
This bill includes the policy agreements by the House and Senate on their first coronavirus relief package.
Economic
- Waives interest on franchise, corporate income, or individual income tax return from April 15, 2020 through July 15, 2020
- Affirms flexibility to administer unemployment compensation as encouraged by the Congressional Families First Coronavirus Response Act
Health
Personal Protection Equipment
- The bill directs the Division of Public Health, the Division of Health Service Regulation, and the NC Division of Emergency Management to develop a plan for creating and maintaining a strategic stockpile of PPE.
- The plan would be required to include who should have access to the stockpile, ways to increase production within the state, potential stockpile locations, recommendations of the amount and kinds of items to stockpile, an inventory mechanism, and a 5 year budget.
Health Provider Relief
- Dentists - The bill allows the NC Board of Dental Examiners to waive statutory requirements in an emergency. (The NC Medical Board and the NC Board of Nursing do have this authority currently.)
- The bill allows dentists to administer COVID-19 tests.
- Pharmacists - The bill allows the State Health Director to authorize immunizing pharmacists to administer the COVID-19 vaccine by a statewide order if one is approved by the CDC at a time when the NC General Assembly is not in session. It would be a requirement that the Director develop a written standard screening questionnaire and safety procedures for written protocols for the vaccine to the Joint Legislative Oversight Committee, the NC Medical Board, the NC Board of Nursing and the NC Board of Pharmacy within 10 days of approving the petition. If this order moves forward, it would expire upon the adjournment of the next session.
- The bill also allows pharmacists to use a government issued ID to identify patients picking up prescriptions.
Quality Improvement Plans
- This bill would prohibit the enforcement of any administrative rule that would enforce quality improvement meetings between a PA or NP who had been practicing prior to February 2020. This would expire December 31, 2021.
Workforce Study
- The bill directs the NC Area Health Education Center to study the issues impacting health delivery and the health workforce during a pandemic.
Liability Protections
- This provision states that any health facility, health provider, or entity that holds legal responsibility for a health professional shall have immunity from any civil liability for any harm or damages alleged to have been sustained as a result of an act or omission in the course of providing health services as a response to COVID-19.
NCDHHS Flexibility
- HealthConnex - The bill extends the deadline for providers to connect to HealthConnex from June 2020, to October 2021 to begin submitting demographic and clinical data in order to remain eligible for state funds.
- Inspections - The bill allows facility inspections to be modified.
- Involuntary Commitment - The bill allows for the first and second examinations for involuntary commitment to be conducted via telehealth if the commitment examiner is reasonably certain that a different result would not have been reached in a face to face examination.
- Telehealth - The bill states that the NCGA urges Centers for Medicaid and Medicare coverage for health care provided through audio only communication.
State Government
Masks
- This bill clarifies that masks may be worn on certain private and public premises to ensure physical health or safety.
Health Care Powers of Attorney/Advanced Directives
- This bill waives the requirement of two qualified witnesses related to Health Care Powers of Attorney and Advanced Directives for a Natural Death during the State of Emergency.
Communicable Disease Information
- The bill permits the release of communicable disease health information by the DHHS or a local health department to prevent or lessen a serious health threat as allowed under HIPPA.
State Health Plan
- The bill allows the State Treasurer, with approval of the Board of Trustees for the State Health Plan to allow the option of deferring premiums or debt payments when there is a state of emergency or disaster.
This bill did not include the telehealth payment parity provision that was included in the House version of this legislation. NCMS is committed to continuing to communicate with legislators about the importance of this issue as the legislature is scheduled to return to session in two weeks.
The bill passed in the House with a vote of 119-0.
This bill passed the Senate.
This bill was signed by Governor Cooper on May 2, 2020. This bill is now law.
HB - 1043- 2020 COVID-19 Recovery Act
FUNDING BILL
This funding bill spends ~ $1.571 billion. The Senate's proposal spent ~ $1.3 billion, House's proposal spent ~ $1.7 billion, and the Governor's proposal spent ~ $1.4 billion.
The bill establishes the Coronavirus Relief Fund to be used to provide relief from effects of COVID-19.
Health
- $50 million for PPE divided between the NC Health Care Foundation (50%), NC Senior Living Association and the NC Health Care Facilities Association (15%), NC Medical Society (10%), and Division of Emergency Management (25%).
- $150 million for counties ineligible to receive direct funding from the CARES Act.
- $2 million for the Pandemic Recovery Office
- $20 million to OSBM to allocate to State agencies negatively impacted by loss of anticipated receipts
- $100,000 to Wake Forest University Health Services for COVID-19 research data.
- $15 million to the Duke University Human Vaccine Institute
- $29 million to the NC Policy Collaboratory for the development of countermeasures for COVID-19, including vaccine research.
- $15 million to Brody School of Medicine at ECU for the development of countermeasures.
- $6 million for Campbell University School of Osteopathic Medicine for community testing, health treatment, monitoring rural populations, and supporting community primary care
- $20 million to DHHS for local health departments and rural health providers
- $6 million divided equally to the 6 food banks in the state
- $25 million for the State-County Special Assistance facilities to offset increased costs of living for serving residents
- $50 million to DHHS for rural/underserved communities for health provider grants and enhanced telehealth services
- $5 million for the NC Association of Free and Charitable Clinics
- $1.5 million to NC MedAssist to offset increased costs for prescription assistance
- $5 million to the NC Community Health Centers Association for costs of health service during COVID-19
- $20 million to DHHS to mental health and crisis services
- $19 million to DHHS to provide for food banks, homeless and domestic violence shelters, child care response, and any technology support services
- $1.8 million to Old North State Medical Society for rural and African American communities to address disparities
- $65 million for a grant to the NC Healthcare Foundation for hospitals
- $15 million for teaching hospital relief
- 5% increase in Medicaid rates for all provider types. Rate increase is effective 3/1/20, and expires on the earliest of the following (1)date the national emergency expiration, (2) executive order on COVID-19 is rescinded, or (3) March 21, 2o21
- Authorizes DHHS to provide Medicaid coverage for COVID-19 testing
- Authorizes funding for the purchase and distribution of units of opioid antagonists at no charge to opioid treatment programs
- Disallows funding for testing and contact tracing until requirements of reporting of certain data are met by NC DHHS
- Education
- $75 million to the Department of Public Instruction (DPI) for school nutrition services.
- $1 million to DPI for improving internet connectivity for mobile wifi router devices in school buses.
- $11 million to DPI for improving internet connectivity through mobile access points.
- $30 million to DPI for electronic devices for public school students
- $5 million to DPI for computers or other electronic devices for school personnel
- $10 million to DPI for school health support for physical and mental health personnel
- $44.5 million to UNC Board of Governors for increased costs due to online coursework
Economic
- $125 million for Golden LEAF for small business loan assistance
- $9 million to the Department of Information technology for the GREAT program which provides broadband to rural communities
This bill passed in the Senate.
The House passed this bill with a vote of 120-0.
This bill was signed by Governor Cooper on May 4, 2020. This bill is now law.
NCMS Morning Rounds 5-4-20
Welcome to a new week and your
NCMS Morning Rounds.
May 4, 2020
Special NCMS Call with Sec. Cohen on Wednesday
Mark your calendar for this Wednesday evening at 7 p.m. when NCMS members will have the opportunity to hear firsthand from NC Department of Health and Human Services (NCDHHS) Secretary Mandy Cohen, MD, MPH. Sec. Cohen will address the myriad issues facing the medical community during the pandemic as well as considerations as the state weighs lifting some restrictions.
Watch your email for details on how to join the call.
NCMS Legislative Update
Over the weekend the NC General Assembly approved a COVID-19 relief package that included a variety of policy provisions and $1.5 billion in spending to respond to the pandemic. Of the NCMS’ legislative priorities for the session several made it into the final legislation, which is now being considered by the Governor.
Medical liability protections are included in the final legislation. Your strong response to our Action Alert calling on legislators to support this provision had a definite impact on this positive outcome. Thank you for responding! With lobbyists prohibited from being in the legislative building due to the social distancing restrictions, we will likely call on you again in the coming weeks to contact your representatives through our Action Alerts to make sure they hear firsthand what is important to you during this unprecedented situation. If you aren’t signed up to receive them, you can do so now at this link.
Telehealth payment parity, another of our priorities, did not make it into the final legislation, however, discussions are ongoing. The House COVID-19 working groups will continue to meet and legislators will return to Raleigh in two weeks, so the NCMS advocacy team, with your help, will continue to impress on legislators the importance of telehealth parity for your practice.
The spending portions of the legislation include $125 million in small business relief, administered through the Golden Leaf Foundation; a 5 percent increase in Medicaid reimbursement for fee-for-service providers; approximately $1 million to go to the Old North State Medical Society to study health disparities; funding for the NC Department of Health and Human Services to pay for COVID-19 testing and funds for the NCMS to help procure personal protective equipment (PPE) for medical practices.
For a more detailed summary of what is contained in this bill, visit our legislative blog.
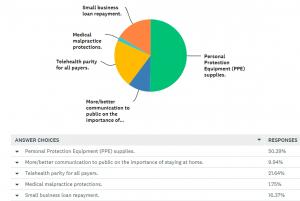
Joint Survey Reveals Practice Challenges, Trends
The joint NCMS, Curi, NC Medical Group Management Association (NCMGMA) survey that many of you may have been completing each week over the last month, has revealed some interesting and useful data relative to the impact the COVID-19 pandemic has had on medical practices across the state. Below is a summary report of the data collected thus far along with a second document, which comments on several notable trends.
The survey will continue to be sent weekly, so please continue to add to this important source of information to help us inform policymakers and legislators as well as how we can help you as you respond to the pandemic and its impact.
If you are not currently receiving requests to take the survey each week, please email us at [email protected] and ask to be added to the Urgent Practice Data Survey list.
Read our analysis of the trends revealed thus far.
In the News
Fear of Coronavirus Propels Some Smokers to Quit, Kaiser Health News, 4-30-20
Learning Opportunity
The National Academy of Medicine’s Action Collaborative on Countering the U.S. Opioid Epidemic and the American Society of Addiction Medicine (ASAM) are hosting a joint webinar, ‘Helping People with Addiction Stay Connected During COVID-19,’ on Thursday, May 7 from 11 a.m. to 12:30 p.m. This 90-minute webinar will provide insights on issues of access to addiction treatment and recovery services, and will include targeted guidance on how to effectively keep patients connected to this essential care during the COVID-19 pandemic. Learn more and register.
SPECIAL NCMS Political Pulse for Saturday, May 2, 2020
Today the NC House and NC Senate reached a $1.5 billion agreement on a COVID-19 pandemic relief package. Watch as NCMS Director of Legislative Relations Sue Ann Forrest, MPA, describes what policy and funding provisions made it into the final legislation and what relief your practice may receive as part of this legislation.
NCMS Political Pulse for May 1, 2020
The NC General Assembly reconvened this week and got right down to business -- although in unusual circumstances due to the COVID-19 social distancing requirements. The NCMS lobbying team is working remotely to advocate on our legislative priorities as the House and Senate members debate how best to address the pandemic both through new policies and appropriations. As of this morning, negotiations are ongoing, and will likely continue over Saturday and Sunday and possibly into Monday. Watch your email over the weekend for updates on what legislative package around COVID-19 response the General Assembly may ultimately vote on and send to the Governor for his signature.
NCMS Morning Rounds 5-1-20
Happy May Day!
Enjoy your NCMS Morning Rounds.
May 1, 2020
ICYMI: NCMS Offers Access to PPE
 Dr. Katie Lowry of Robeson Pediatrics, an NCMS Community Practitioner Program practice, was glad to receive her much-needed masks provided by Carolina Complete Health.
Dr. Katie Lowry of Robeson Pediatrics, an NCMS Community Practitioner Program practice, was glad to receive her much-needed masks provided by Carolina Complete Health.
As we announced yesterday, the NCMS is pleased to offer medical practices statewide a mechanism to procure personal protective equipment (PPE) through group purchasing. This two-pronged effort offers you a chance to place an online order through a joint group purchasing arrangement with the Charleston County (South Carolina) Medical Society and other state and local medical societies and/or to work with local North Carolina manufacturers to produce needed materials. The easy ordering process is detailed on this webpage.
Thresholds for the amount of PPE must be met before the orders can be placed, so this is not an immediate fix for your PPE needs. However, please think ahead to your longer term needs as the volume of in-person patient visits may begin to increase as stay-at-home orders and other restrictions are lifted in the coming weeks and months.
The NCMS has heard from our members that securing necessary PPE has been a challenge as practices have grappled with the many challenges in responding to the COVID-19 pandemic. We responded by organizing the group purchasing effort described above, and we worked with Carolina Complete Health (CCH) and its subsidiary Carolina Complete Health Network to distribute PPE to primary care practices in North Carolina. The PPE was obtained by Centene and shipped directly to NCMS and CCH staff for distribution to those NCMS Foundation Community Practitioner Program (CPP) practices in need of PPE. We are grateful for this work, as we continue to do everything within our capabilities to mitigate the negative effects of the COVID-19 pandemic.
NCMS Legislative Update
The NC General Assembly session continued today, with the House passing their COVID-19 relief package, HB 1043 – Pandemic Response Act, with a vote of 117-1. No amendments were made to this bill, which compiled many of the policies that had been created from the House COVID-19 Working Groups.
The Senate passed its relief package yesterday, SB 704 – COVID Relief Recovery Act, and stark differences in each chamber’s funding amounts and priorities exist. Yet there also are areas of agreement. Both bills include medical liability protections.
The House and Senate Appropriations chairs hoped to reach an agreement today, but instead pushed the vote to Friday. The NCMS lobbying team is in close communication with legislators on the importance of our priorities and remains focused on our mission of improving the health of all North Carolinians.
View our NCMS legislative blog for more information on both bills.
Useful NCMS Summary of Regulatory Changes Due to COVID-19
NCMS staff has been carefully monitoring all of the federal and state regulatory changes prompted by the COVID-19 pandemic – and there have been many -- and how they may impact your practice. To help you quickly access these new regulations here is a helpful grid.
The information includes updated federal regulations regarding Medicare, the Quality Payment Program deadlines, HIPAA and telehealth among others. The grid also includes regulatory changes prompted by Governor Cooper’s Executive Orders, measures taken by the NC Medical Board and advisories from the NC Department of Insurance. We will be updating these as new regulations are enacted.
Access this useful reference tool.
In the News
WHO Says No Evidence Shows that Having Coronavirus Prevents a Second Infection, CNN, 4-25-20
Learning Opportunity
Employee benefits experts from Poyner-Spruill will present “Benefits in the Time of COVID: Important Actions for Your Benefit Plans,” on Tuesday, May 5 from 5 to 6 p.m. Learn more and register for this webinar here.
PLEASE NOTE: Several upcoming medical specialty society meetings have been canceled.
The 2020 NC Dermatology Association Summer Meeting, scheduled for July 31-Aug. 2 at The Greenbrier in White Sulphur Springs, WV, has been canceled due to the continuing challenges posed by the COVID-19 pandemic.
The 2020 NC Society of Otolaryngology and Head and Neck Surgery Annual Meeting, scheduled for July 24-26 at Omni Grove Park Inn in Asheville, NC, also has been canceled.
These groups are both considering meeting options going forward and will send notification about future plans to their respective memberships when available.
NCGA House Coronavirus Package
 On April 30, 2020, the House passed HB 1043 - Pandemic Response Act.
On April 30, 2020, the House passed HB 1043 - Pandemic Response Act.
The House and Senate Appropriations Chairs are currently conferencing to decide which provisions from the House and Senate bills will be included in the final bill. A final bill is expected to be voted on by Friday.
Health Policy
Increase Personal Protection Equipment (PPE)
The bill directs the Division of Public Health, the Division of Health Service Regulation, and the NC Division of Emergency Management to develop a plan for creating and maintaining a strategic stockpile of PPE.
The plan would be required to include who should have access to the stockpile, ways to increase production within the state, potential stockpile locations, recommendations of the amount and kinds of items to stockpile, an inventory mechanism, and a 5 year budget.
Health Provider Support
Dentists
The bill allows the NC Board of Dental Examiners to waive statutory requirements in an emergency. (The NC Medical Board and the NC Board of Nursing do have this authority currently.)
The bill allows dentists to administer COVID-19 tests.
Pharmacists
The bill allows the State Health Director to authorize immunizing pharmacists to administer the COVID-19 vaccine by a statewide order if one is approved by the CDC at a time when the NC General Assembly is not in session. It would be a requirement that the Director develop a written standard screening questionnaire and safety procedures for written protocols for the vaccine to the Joint Legislative Oversight Committee, the NC Medical Board, the NC Board of Nursing and the NC Board of Pharmacy within 10 days of approving the petition. If this order moves forward, it would expire upon the adjournment of the next session.
The bill also allows pharmacists to use a government issued ID to identify patients picking up prescriptions.
Quality Improvement Plans
This bill would prohibit the enforcement of any administrative rule that would enforce quality improvement meetings between a PA or NP who had been practicing prior to February 2020. This would expire 60 days after the Executive Order is rescinded or December 31, 2020 (whichever is earlier).
Workforce Study
The bill directs the NC Area Health Education Center to study the issues impacting health delivery and the health workforce during a pandemic.
NCDHHS Flexibility
HealthConnex
The bill extends the deadline for providers to connect to HealthConnex from June 2020, to October 2021 to begin submitting demographic and clinical data in order to remain eligible for state funds.
Medicaid Coverage
The bill authorizes DHHS to provide Medicaid coverage for COVID-19 testing for the uninsured during the pandemic as allowed under the Families First Coronavirus Response Act.
The bill authorizes DHHS to provide Medicaid coverage to individuals with 200% FPL as described int he 1115 waiver DHHS submitted for federal approval. Coverage includes the prevention, testing, and treatment of COVID-19.
The bill requires DHHS to follow all federal laws necessary to receive enhanced Medicaid funding under the Families First Act.
Telehealth
Involuntary Commitment
The bill allows for the first and second examinations for involuntary commitment to be conducted via telehealth if the commitment examiner is reasonably certain that a different result would not have been reached in a face to face examination.
The bill would require all insurers and the State Health Plan to do the following
- provide coverage for telephonic care and e-visits
- provider coverage for provider to provider consultations
- cover telehealth and virtual health services without prior authorization
- cover physical therapy, occupational therapy, and speech therapy delivered via telehealth
- Reimburse providers the same rate for telehealth services as they do for in person services
Medicaid and Medicare
The NCGA urges CMS to provider coverage for health care provided through audio only communication.
Liability Protections
This provision states that any health facility, health provider, or entity that holds legal responsibility for a health professional shall have immunity from any civil liability for any harm or damages alleged to have been sustained as a result of an act or omission in the course of providing health services.
Health Funding
Behavioral Health and Crisis Services
- $25 million in nonrecrruing funds to support public health efforts, local health departments, and rural health providers
- $25 million in nonrecurring funds to support behavioral health services
Medicaid
- $40 million in nonrecurring funds for coverage of additional costs related to the Medicaid program
- 5% rate increase for all fee for service Medicaid rates for all providers
- Authorization to provide Medicaid coverage for COVID-19 testing for the uninsured
- Authorization to provide Medicaid coverage for to individuals with incomes up to 200% of the federal poverty level
- Authorization to implement temporary Medicaid provider enrollment relief
Personal Protection Equipment
- $50 million in nonrecurring funds to purchase PPE and other supplies and equipment
Testing
- $25 milion in nonrecurring finds to expand public and private testing
Food, Safety, and Child Care
- $6 million in nonrecurring funds to allocate equally among each of the 6 food banks
- $2.5 million in nonrecurring funds to the Reinvestment Partners (non-profit organization) which provides funding to eligible Food and Nutrition Services Recipient enrolled by the recipient’s health care provider
- $2.25 million in nonrecurring funds to assist in serving children in foster care to be used for monthly supplemental payments
Rural and Underserved Communities
- $25 million in nonrecurring funds to support rural and underserved communities for items not addressed by federal funds
- $75 million in nonrecurring funds to support rural hospitals
- $1.4 million in nonrecurring funds to support the 67 free and charitable clinics
- $1.5 million in nonrecurring funds to NC MedAssist to offset increased costs for services for the uninsured
Other Relief
- $25 million in nonrecurring funds for NC Teaching Hospitals
- $100 million to the NC Policy Collaboratory
- $25 million to the Duke Human Vaccine Institute
- $25 million to the UNC Gillings School of Public Health
- $25 million to ECU Brody School of Medicine
- $25 million to Wake Forest School of Medicine
- $10 million to Campbell University Osteopathic School of Medicine
Economic Support
- Would allow employer to initiate an unemployment claim for employees when unemployment is the result of a disaster
- Appropriates $75 million to the Golden Leaf Foundation to provide emergency loan funding for small businesses
HB-1040 Healthcare for Working NC
H B 1040 - Healthcare for Working North Carolinians
B 1040 - Healthcare for Working North Carolinians
Primary Sponsor: Rep. Sydney Batch (D-Wake)
This bill expands Medicaid to individuals under the following provisions:
- Gross income of 133% of the federal poverty level
- Age 19-65
- Not currently eligible for Medicaid coverage
- Nor currently receiving Medicare coverage
Beneficiaries would receive benefits through an Alternative Benefit Plan established by DHHS.
The copayments would be the same as current Medicaid beneficiaries.
A new version of the Hospital Provider Assessment would be used to pay for the program.
The bill appropriates $250,000 for DHHS to prepare for the additional beneficiaries.
HB-1046 COVID-19 Paid Sick Leave
 HB 1046 - COVID-19 Paid Sick Leave
HB 1046 - COVID-19 Paid Sick Leave
Primary Sponsors: Rep. Susan Fisher (D-Buncombe), Rep. Sydney Batch (D-Wake), Rep. Pricey Harrison (D-Guilford)
This bill would provide paid sick leave in response to the COVID-19 Outbreak from April 1, 2020-December 31, 2020.
This bill was referred to the following committees:
- Finance
- Commerce
- Health
- Rules
NCMS Morning Rounds 4-30-20
Enjoy your Thursday
NCMS Morning Rounds.
April 30, 2020
NC Legislature Is Back and Busy
The NC General Assembly reconvened on Tuesday and got right to work -- albeit in unusual circumstances due to social distancing requirements. Legislatiors moved legislation addressing the state's needs as a result of the COVID-19 pandemic through various committees in anticipation of possible floor votes yet this week.
The following is an overview of some of the activity in both the House and Senate over the past two days:
The House Appropriations Committee approved HB 1038 – Omnibus COVID-19 Relief Response Funds. Most of this language was approved by and passed in the House COVID-19 Health Working Group. It includes a 5 percent Medicaid rate increase for all providers, funding to cover COVID-19 testing for the uninsured, $50 million for personal protective equipment (PPE), $6 million for food banks and $25 million for rural health providers. The NCMS summary of the bill can be found here. The bill was referred to the House Rules Committee.
The House Rules Committee passed HB 1037 – Health Care Working Group Policy Rec., which had passed the House Health Committee on Tuesday and contains several key priorities as set by the NCMS Legislative Cabinet, including liability protections and telehealth changes. If you haven't already, please reach out to your legislators via our Action Alert or individually to let them know this issue is important to you. This bill will now move to the House floor for a vote.
The House Rules Committee also passed HB 1043 – COVID-19 Time Sensitive Matters.
To learn more about this bill and the committee's proceedings, go to the NCMS Summary of the House Rules Committee Meeting here.
The Senate Passed SB-704 COVID-19 Recovery Act in Senate Appropriations Committee and on the Senate floor with a 48-0 vote. This bill includes liability protections, small business loan assistance and COVID-19 testing for the uninsured.
The main difference between the House and Senate plans is in the amount of spending. The Senate plan spends approximately $1.2 billion, while the House plan spends roughly $1.7 billion. House and Senate leaders have said a compromise is likely to be reached by Friday.
Senate leaders will decide if they will have a voting session today by 11 am, while the House convenes at noon.
The NCMS lobbying team is tracking all of these issues closely and remains laser focused on improving the health of all North Carolinians. Stay up to date by viewing our NCMS legislative blog or following us on twitter.
NCMS Business Partners Offer COVID-19 Testing
Two NCMS Business Alliance members, MAKO Medical and LabCorp, are commercial labs performing COVID-19 testing in the state. Quest Diagnostics also is a private lab authorized to perform the tests along with the North Carolina State Laboratory of Public Health. Review the state’s latest testing guidance here.
The NCMS fully supports more widespread and on-going testing as outlined by Governor Roy Cooper and NC Department of Health and Human Services Secretary Mandy Cohen, MD, MPH. Ramping up testing for COVID-19 will give the state a better picture of the spread of the virus as well as when and how to reopen the economy now and in the future with public health being our top priority.
LabCorp is offering diagnostic COVID-19 tests, with, depending on demand, test results available on an average of 1 to 2 days from the pickup of the specimen. LabCorp recently began offering anti-body tests (learn more here) in accordance with public emergency guidance from the FDA. Learn more about LabCorp’s COVID-19 testing capabilities.
MAKO Medical is offering rapid, real-time diagnostic tests with a 24- to 36-hour turnaround time. They also are preparing to introduce anti-body tests. Learn more here.
Both LabCorp and MAKO also are valued partners in the NCMS Foundation’s Project OBOT.
The NCMS also is advocating at the NC General Assembly to ensure that the cost of COVID-19 testing and treatment for anyone who needs it will be covered.
TONIGHT: NC Medicaid Ready to Answer Your Questions
As they have for the last several Thursdays, NC Medicaid officials will again be on hand this evening at 5:30 p.m. via webcast to address issues Medicaid providers are facing during the COVID-19 pandemic.
This week they will focus on answering FAQs about telehealth, telehealth guidance for dialysis, skilled nursing and introducing an innovative new appointment type called the Hybrid Home-Telehealth visit. Also they will cover details on the uninsured COVID testing and treatment payments from HRSA, and provide a deep dive on providing well-child and adolescent care using telehealth through case scenarios.
This webinar series is presented in partnership with Community Care of North Carolina and NC AHEC. Learn more and register here.
In the News
[Note: NCMS CEO Robert W. Seligson, MBA, MA, is quoted in the following article.]
Tackling Poverty in a Coronavirus-induced Economic Downturn: Is it Too Risky or the Right Thing to Do?, USA Today, 4-28-20
Learning Opportunity
Even if you couldn’t attend the on-going webinar series by the University of North Carolina at Chapel Hill’s Center for Health Equity Research, recordings of the presentations are available online. Last week’s webinar with Dr. Giselle Corbie-Smith “Black Communities and COVID-19,” examined equitable access to health care, mortality rates and the overall impact of COVID-19 on black people’s mental and physical health. You can listen to a recording of the webinar here.
Yesterday’s webinar, “COVID-19 and Health Equity – Exploring Disparities and Long-Term Health Impacts” is part of the American Public Health Association and National Academy of Medicine’s series. Recordings and notice of future ‘COVID-19 Conversations’ webinars will be posted on this webpage.
NCGA Senate COVID-19 Package
SB 704 - COVID-19 Recovery Act
Establishment of Coronavirus Relief Reserve
- $6 million for DHHS to allocate to the 6 food banks
- $15 million for DHHS for one time payment costs for licensed facilities for State-County Special Assistance
- $2.25 million for Social Services to assist children in foster care
- $10 million for the NC Association of Free and Charitable Clinics
- $5 million for the NC Community Health Centers Association
- $15 million for the Duke University Human Vaccine Institute
- $20 million to the Wake Forest University Health Services for its COVID-19 study
- $1.8 million to the Old North State Medical Society to target rural areas and African American communities with outreach, health education, and testing to address COVID-19 disparities in NC
- $250,000 to the Department of Information Technology to provide funds for the purchase of Wi-Fi routers in designated tier 1 or tier 2 counties
- $15 million for the NC Policy Collaboratory
- $56 million for the Department of Public Instruction to use for school nutrition
- $9 million for the Department of Information Technology to use for the Growing Rural Economies with Access to Technology Fund
- $25 million for DHHS to expand COVID-19 testing initiatives
- $20 million for DHHS to provide support to health departments and rural health providers
- $25 million for DHHS to provide funding for food banks, residential settings, domestic violence shelters, homeless populations, and child care
- $61 million for DHHS to provide funds for rural and underserved communities
- $22 million for the Department of Public Instruction to provide funds for school nutrition programs
- $125 million for small business support through the Golden Leaf Foundation
- Allows the State Treasurer to have flexibility to deter State Health Plan Payments during the COVID-19 emergency
- Provides Medicaid coverage for the COVID-19 testing for uninsured individuals during the COVID-19 emergency
- Medicaid provider rate increases during the emergency
- Permits telehealth involuntary commitment during the emergency
- Medical liability protections that include civil liability protections for any harm or damages
- Establishment of the NC Pandemic Recovery Office to oversee and Coordinate Funds
Amendment by Sen. Gladys Robinson (D-Guilford)
- $20 million to DHHS to provide flexible funds to support local health departments, rural health providers, and mental health services
- $25 million to DHHS for food banks, homeless and domestic violence shelters, housing security, child care, and technology modifications
- $61 million to DHHS to provide funds for rural and underserved communities
- $22 million to the Department of Public Instruction to provide funds for school nutrition programs
This amendment passed and will be included in the bill.
This bill passed the Senate with a vote of 48-0 on April 29, 2020,and will now move to the House.
NCGA House Rules Committee
 The House Rules Committee met on Wednesday, April 29, 2020.
The House Rules Committee met on Wednesday, April 29, 2020.
HB 1037 - Health Care Working Group Policy Rec.
This bill contains the same language passed in the House Health Committee yesterday with only amending the language to fix a staff error regarding a withdrawn amendment yesterday.
View the complete NCMS Summary of this bill here.
Rep. Yvone Lewis Holley introduced an amendment to remove the medical liability language from the bill.
After an intense committee discussion, Rep. Holley withdrew her amendment.
The bill passed unanimously and will now move to the House floor.
This bill does not have any specific health related portions.
This bill passed unanimously and will now move to the House floor.
HB 1043 - COVID-19 Time Sensitive Matters
This bill includes a variety of provisions discussed in the House COVID-19 State Operations Working Group.
Some key health items include
- Allows the exemption of people wearing a mask for ensuring physical health or safety of the wearer or others
- A person wearing mask for physical health/safety of the wearer shall remove the mask upon the request of law enforcement
- Health care powers of attorney executed without two qualified witnesses during the time period of the COVID-19 State of Emergency declaration
- Advanced health directive for a natural death declaration in the presence of two qualified witnesses shall be waived during the COVID-19 State of Emergency declaration
- Broadens the telemedicine definition for involuntary commitment to include any platform where the respondent and commitment examiner can hear and see each other
- Allows a physician to conduct a second examination for involuntary commitment if the physician believes that the findings would not be different if the examination had been completed in person
- Allows communicable disease information to be available by DHHS or a local health department to present or lessen a serious public health threat
- Allows retired physicians to be allowed to be appointed as medical examiners
- Allows State Health Plan premium and debt payment deferral option during a declaration of emergency upon approval of the Board of Trustees
This bill passed unanimously and will move to the House floor.
NCMS Morning Rounds 4-29-20
It's Wednesday and time for your
NCMS Morning Rounds.
April 29, 2020
AMA Issues Ethics Guidance During Pandemic
Yesterday, the same day that the NCMS, NC Healthcare Association and the NC Institute of Medicine offered a webinar for clinicians on the crisis standard of care protocol jointly agreed upon by a broad group of stakeholders in North Carolina, the American Medical Association (AMA) announced ethics guidance for physicians and PAs as they may face challenging situations during this pandemic.
A recording of Tuesday evening's webinar will be available shortly. Watch your NCMS Morning Rounds for a link.
The AMA's Code of Medical Ethics is as relevant in the context of a public health crisis as it is in more familiar circumstances of clinical practice, the Association said in a press release. To help physicians address the challenges of COVID-19, the AMA assembled a series of analyses that apply the Code to issues emerging in the pandemic. Review the analyses here.
These issue-specific analyses range widely, offering guidance not only about allocating limited resources, but also responsible prescribing in the context of the pandemic, the importance of research ethics in the accelerated search for effective treatments for COVID-19, and issues of access to care and equity. New analyses are posted as questions continue to emerge.
As an editorially independent journal, the AMA Journal of Ethics has also created a COVID-19 Ethics Resource Center that includes expert analyses, visual assets, podcasts and video content. Access these resources here.
Joint Survey Gathers Info on Your Financial Needs
The NCMS along with the NC Medical Group Management Association (NCMGMA) and Curi have been sending a weekly survey – Urgent Practice Survey – for the last month to gather information on what physician and PA practices are experiencing during this pandemic. This week’s quick survey focuses more heavily on your financial needs. If you haven’t already responded, please take just three minutes now to complete the survey.
Thank you to those who have been diligent over the past weeks in providing your input via this survey. We are analyzing the data and will provide an overview to you shortly.
The NCMS, NCMGMA and Curi will use the information to inform our advocacy agenda and develop resources to help you.
National Infant Immunization Week Highlights Need
National Infant Immunization Week, which will run until this Saturday, May 2, focuses on the positive impact of vaccination on the lives of infants and children. The NCMS supports routine immunizations as integral to our mission of protecting and improving the health of North Carolinians. Health care professionals are on the front lines of the fight against vaccine-preventable diseases.
The observance of this week is even more important during the current pandemic as parents may be reluctant to visit their physician or PA’s practice and indicators are that foregoing the regular immunization schedules for kids may lead to outbreaks of preventable disease.This New York Times article from last week offers a perspective on the current situation of parents foregoing well visits and immunizations for their children.
According to Centers for Disease Control and Prevention (CDC) research, parents consistently identify health care professionals as their most trusted source of health and immunization information. Research also shows that many parents make vaccine decisions before their babies are even born.
This week, please remind parents and pregnant women about the importance of on-time infant immunization. The CDC, the American Academy of Pediatrics and the American Academy of Family Physicians offers this Provider Resources for Vaccine Conversations with Parents. Other resources include: Talking with Parents about Vaccines for Infants and Preparing for Questions Parents May Ask about Vaccines. In addition, CDC has a slide deck you can use to with staff to discuss how to create a culture of immunization in your practice.
The CDC estimates that routine immunization of children born between 1994 and 2018 will prevent an estimated 419 million illnesses, 26.8 million hospitalizations, and 936,000 early deaths over their lifetimes, at a net savings of $406 billion in direct costs and $1.88 trillion in total economic impact.
In the News
What the Coronavirus Crisis Reveals About American Medicine, The New Yorker, 4-27-20
Learning Opportunity
This week’s NCMS Foundation Kanof Institute for Physician Leadership’s Power Hour on Friday, May 1, from 1 to 2 p.m. will focus on the challenges various specialty practices are facing during the current pandemic and what the future may hold. Join the conversation with Craig Burkhart, MD, and Susan Sanders, MD, both past presidents of the NC Dermatology Association; Sarah Koch, MD, and Dhwani Mehta, MD, from the Dermatology Group of the Carolinas; Janelle Rhyne, MD, a past Governor of the NC Chapter, American College of Physicians and Gaurang Palikh, MD, President of the North Carolina Neurological Society. Moderated by NCMS VP Rural Health Systems Innovation Franklin Walker, MBA, you will have the opportunity to listen and converse about their respective experiences so far during the pandemic and what they envision going forward for their respective specialties. Learn more and register here.
PLEASE NOTE: There is an UPDATED LINK for today’s webinar at noon on ‘Geriatric Medicine and COVID-19: Optimizing Care for Older Adults in a Time of Pandemic’ with Cathleen Colon-Emerec, MD, Chief, Duke Division of Geriatric Medicine. Click here to access the webinar. The event number is 668 538 149 and the password is KnT2pwR7zy6.
NCGA House Health Committee
The NCGA House Health Committee met on Tuesday, April 28.
The Committee discussed the policy bill recommendation from the House Health COVID-19 Woring Group.
View the previous NCMS Summary on that bill here.
The Committee considered several amendments to the previously approved bill.
Rep. Wayne Sasser’s (R-Stanly) Amendment to allow pharmacists to administer COVID-19 diagnostic tests and antibody tests was withdrawn from the committee.
Rep. Wanyne Sasser’s (R-Stanly) amendment to further clarify prescription identification requirements for pharmacists to use during COVID-19 pandemic and up to 60 days afterwards. This amendment passed unanimously.
Rep. Perrin Jones, MD (R-Pitt) introduced an amendment to remove the criminal liability portion in the previous legislation and to set time limits of the protections to include the State of Emergency declaration. This language was agreed upon as a compromise in order to keep the liability portion included in the bill. This amendment passed unanimously.
Rep. Josh Dobson (R-Avery) introduced an amendment to request that NC DHHS consider North Carolina based businesses that can provide response support to reach rural areas of the state. This amendment passed unanimously.
Rep. Donny Lambeth (R-Forsyth) introduced an amendment at the request of NC DHHS to provide criminal and civil liability protections to the State Health Director and pharmacists providing the COVID-19 vaccination, if the State Health Director issues a statewide order to allow pharmacists to give the vaccine. This amendment passed unanimously.
Rep. Perrin Jones, MD (R-Pitt) introduced an amendment to require providers to report both positive and negative COVID-19 results to the Division of Public Health and the Commission for Public Health. The bill requires NC DHHS to post the results of this data on a county by county basis. This amendment passed unanimously.
The bill as amended passed unanimously in the Committee.
NCGA House Finance Committee
 The North Carolina General Assembly House Finance Committee met on Tuesday, April 28 at 1:00pm.
The North Carolina General Assembly House Finance Committee met on Tuesday, April 28 at 1:00pm.
The Committee considered the two bills that were approved by the House COVID-19 Economic Support Working group. Each bill had small changes to the bill language that was approved previously.
HB - 1034 Small Business Emergency Loans
This bill appropriates $75 million to the the Golden Leaf Foundation for small businesses adversely affected by the COVID-19 pandemic. This bill is similar to the small business loans currently offered by the Golden Leaf Foundation with non-state funds. This bill differes from the bill passed in the COVID-19 Working Group because it does the following:
- Allocates federal funds to the program instead of using State funds
- Makes technical corrections to the two entities providing the loans
Importantly, the bill states that for the first 6 months after loan closing, the loans would have no payments due and an interest rate of up to 4%. Thereafter, repayment would commence and the interest rate would increase to not less than 5.5% for the rest of the loan term, which is capped at a total of 66 months and capped in amount at $50k per recipient.
This bill passed unanimously in the Finance Committee.
HB 1039 - COVID Response Act
This bill waives the interest on individual, corporate and franchise tax returns from April 15 to July 15. The relief would apply to partnership and estate and trust tax returns, as well as estimated tax payments for 2020 due on or before April 15, 2020.
This bill affirms the flexibility in administering the State's unemployment compensation laws, as provided in Executive Orders 118 and 131, and provides a SUTA credit equal to the amount of contributions payable by the employer on the SUTA report due on or before April 30, 2020.
The bill also makes three changes recommended by the Division of Employment Security and remove the July 1, 2023, date that would sunset the Joint Legislative Oversight Committee on Unemployment Insurance. This part of the bill is also a recommendation of the Joint Legislative Oversight Committee on Unemployment Insurance.
This bill passed unanimously in the Finance Committee.
NCMS Morning Rounds 4-28-20
Happy Tuesday! Here is your
NCMS Morning Rounds.
April 28, 2020
NC General Assembly Reconvenes Today
The NC General Assembly heads back into regular session today, with both the House and Senate convening at noon. The House has a busy afternoon planned with three scheduled committee meetings, including the Health Committee at 2:30 p.m.
Only members and staff are permitted in the legislative building due to social distancing restrictions, but the public can see and listen to the proceedings via video and audio links. Watch the House Health Committee meeting via this video link or listen in on this audio link. The House Finance and Education, K-12 Committees also will meet this afternoon. Visit the legislature's webpage to get the video and audio links to those meetings.
NCMS advocacy staff expects those committees to take up the bill drafts created from the House COVID-19 working groups. We also expect other bills to be filed as well as a variety of amendments. NCMS staff will be closely monitoring all of the meetings to update members on outcomes. Your colleagues on the NCMS' Legislative Cabinet have identified four priority areas for this session: medical liability, telehealth, financial assistance and tax deferral.
The NCMS remains laser focused on value and our mission of improving the health of all North Carolinians through these legislative efforts during this pandemic.
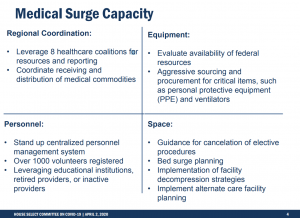
Learn More about the Crisis Standard of Care Protocol
As previously reported the NCMS, the NC Healthcare Association and the NC Institute of Medicine recently released a protocol to provide recommendations for the triage of all inpatients in the event a pandemic creates demand for critical care resources, such as ventilators, that outstrips the supply. The protocol, which was developed at the request of the NC Department of Health and Human Services (NCDHHS), resulted from the input of a broad group of stakeholders and is a consensus document.
The protocol is grounded in ethical obligations (including the duty to care, the duty to steward resources to optimize public health, distributive and procedural justice, inclusivity, equity and transparency), but it also specifically promotes objectivity in decision-making and endeavors to avoid conflicts of commitments and minimize moral distress.
To learn more about the protocol from those involved in the development process be sure to sign up for tonight’s webinar that begins at 7 p.m. Register here.
CMS Suspends Advance Payment Program; Reevaluates Accelerated Payment Program
With new funding allocated for the Provider Relief Fund, the Centers for Medicare & Medicaid Services (CMS) announced it is suspending its Advance Payment Program to Part B suppliers effective immediately and reevaluating the amounts that will be paid under it’s Accelerated Payment Program.
The Accelerated and Advance Payment (AAP) Programs are typically used to provide emergency funding and address cash flow issues for health care providers and suppliers when there is disruption in claims submission or claims processing.
CMS said it had paid over $100 billion through these programs to ensure health care providers had the resources needed to combat the beginning stages of the COVID-19 pandemic. The agency announced over the weekend it will not be accepting any new applications for the Advance Payment Program, and will be reevaluating all pending and new applications for Accelerated Payments in light of direct payments made available through the US Department of Health & Human Services’ (HHS) Provider Relief Fund.
Learn more about the Provider Relief Fund here. For comprehensive information on this and other sources of help, visit the NCMS’ Economic Relief Resources page.
In addition, the recording of last Friday's Centene sponsored webinar featuring financial experts answering your questions about the SBA financial relief programs like the Paycheck Protection Program is now available. Access the recording here.
In the News
Stress of Working on Pandemic Frontlines Could Haunt Health Care Providers Later, WRAL, 4-24-20
Introducing STAT’s COVID-19 Drugs and Vaccine Tracker, STAT, 4-27-20
Learning Opportunity
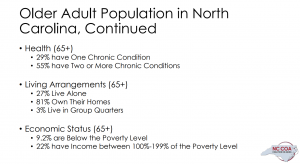
Southern Regional AHEC and Cape Fear Valley Health Systems (CFVHS) will present a webinar on ‘Geriatric Medicine and COVID-19: Optimizing Care for Older Adults in a Time of Pandemic’ with Cathleen Colon-Emerec, MD, Chief, Duke Division of Geriatric Medicine, tomorrow, Wednesday, April 29 from noon to 1 p.m. for the CFVHS Hospital Grand Rounds. Older adults are significantly affected by the novel coronavirus. Dr. Colon-Emeric will update health care providers regarding COVID illness in older adults and discuss strategies for providing care for geriatric patients during this time of pandemic. Register online here or access webinar via WEBEX here. The event number is 663 670 616 and password is tsAcr7EKU97.
NCMS Morning Rounds 4-27-20
Welcome to the new week and your
NCMS Morning Rounds.
April 27, 2020
NCMS Legislative Update
Thank you to everyone who responded to last week’s Action Alert on medical liability protections. A record-setting 1,200+ emails were sent to NC legislators urging them to include such protections in the COVID-19 bill they are considering. Thanks to your efforts and those of Rep. Perrin Jones, MD, (R-Pitt), liability protection language was included in the draft legislation. You can access that Action Alert here.
The draft bill still needs to make its way through the legislative process when the NC General Assembly reconvenes tomorrow, Tuesday, April 28, however. Over the weekend we issued another Action Alert to make sure legislators understand fully the importance of our priorities for the session, which, in addition to liability protections, include tax deferrals, financial relief and telehealth parity. Please take just a minute to review and send this latest alert.
In general, be on the lookout in your email for more Action Alerts in the coming weeks as we ask you to connect directly with legislators to bolster our advocacy efforts as we work remotely on your behalf.
To learn more about the draft legislation considered by the NC House Select Committee on COVID-19, Health subcommittee last week, visit our NCMS Legislative blog for a summary. Guided by your peers on the NCMS Legislative Cabinet, NCMS advocacy staff have been focusing their efforts in four priority areas above at both the state and federal levels with our NC Congressional delegation.
Watch your NCMS Morning Rounds for updates as the NC legislative short session gets underway tomorrow.
Additional Federal Funds Allocated to Paycheck Protection Program
Last week Congress approved an additional $484 billion to replenish and supplement key CARES Act programs including the Paycheck Protection Program (PPP), small business disaster loans and grants and for testing.
The bulk of the additional funding, $321 billion, will go to the PPP with $60 billion set aside for small, midsize and community lenders. The Disaster Loans Program will receive an additional $50 billion and another $10 billion for Emergency EIDL Grants.
Learn more here on our NCMS Financial Resources page.
Congress also is developing an updated CARES Act that will cover a wider range of issues and is expected to be ready for consideration in early May.
Every Day is Earth Day
Last Wednesday was the 50th anniversary of beginning to observe Earth Day. And, while that news may have gotten lost in the headlines announcing the latest statistics and orders surrounding COVID-19, many are making the point that every day is Earth day.
With that in mind, we will include information on programs that address the intersection between health and the environment throughout the year as part of the NCMS’ dedication to improving the health of North Carolinians.
Here is a national child care program that partners with child care professionals to eliminate environmental health hazards found in or around child care facilities. These hazards can adversely impact children’s health. Learn more here.
And, as child care is in high demand for essential workers like health care providers during this time, continue to monitor the Centers for Disease Control and Prevention (CDC) website for guidance for open child care facilities as well as the state and local health departments.
In the News
Vaping, Opioid Addiction Accelerate Coronavirus Risks, Says NIDA Director, Kaiser Health News, 4-24-20
Learning Opportunity
The NCMS, NC Healthcare Association and the NC Institute of Medicine are presenting a webinar for clinicians offering ‘Guidance for Implementing a Crisis Standard of Care for NC on Tuesday, April 28 at 7 p.m. Participants will gain an understanding of the Crisis Standard of Care for North Carolina, including the recently developed North Carolina Protocol. Learn more about the webinar and register here. Review the protocol here.
+
Navigating COVID-19: Charting a New Course Moving Forward as Restrictions Ease will take place on Tuesday, April 28, from 6 to 7 p.m. During this webinar, primary care leaders in NC including Susan Mims, MD, president of the NC Pediatric Society, and David Rinehart, MD, president of the NC Academy of Family Physicians, will discuss strategies that practices are using to prepare to welcome more patients back into the office as restrictions ease. State Health Director and Chief Medical Officer of the NC Department of Health and Human Services Betsey Tilson, MD, MPH, and Chief Medical Officer of NC Medicaid Shannon Dowler, MD, will discuss what easing of restrictions might look like, what practices should be thinking about, the importance of implementing surveillance and the role telemedicine will continue to play in that transition. Click here to connect via Zoom. Or dial: 646-558-8656 using Webinar ID: 131 899 801
Latest FAQs on Provider Relief Fund
The Department of Health and Human Services (HHS) has posted new Frequently Asked Questions regarding the second tranche of disbursement of the CARES Act Provider Relief Fund. This document has answers to questions about eligibility for the funds as well as details about how to apply.
A detailed description of the entire Provider Relief Fund program can be found here.
NCMS Political Pulse for April 24, 2020
Draft legislation has been introduced in the NC House Select Committee on COVID-19 that seeks to address some of the issues you are facing as a result of the pandemic. Watch as NCMS Director of Legislative Relations Sue Ann Forrest, MPA, offers details on what the NC General Assembly will be considering when they reconvene next Tuesday, April 28.
NCMS Morning Rounds 4-24-20
Happy Friday! Enjoy your
NCMS Morning Rounds.
April 24, 2020
NCMB Seeks Physician Applicants for Board
The Review Panel for the NC Medical Board is seeking physician applicants for three seats on the Board, for three-year terms beginning Nov. 1. In accordance with state law, one of the available seats must be filled by a physician who is a member of the Old North State Medical Society. Two of the physician Board Members currently serving are eligible for reappointment; one incumbent physician Board Member is not eligible for reappointment.
The Review Panel will consider only physicians who hold active, unrestricted NC professional licenses, and have practiced in the state for at least five years. Applicants must currently be practicing clinical medicine at least 20 hours per week and plan to continue at least that level of practice in North Carolina for the duration of their service on the Medical Board. In addition, applicants must have no history of disciplinary action (in any jurisdiction) within the past 10 years. The Review Panel will interview qualified applicants Aug. 22 and 23.
Learn more about what is involved in serving on the Board here.
The Review Panel, which operates independent of NCMB, will accept applications online through July 1. Submit your application here.
NC Committee Passes First Draft of COVID-19 Legislation
At its meeting yesterday the NC House COVID-19 Health Committee reviewed draft legislation that addresses many of the issues facing you and your practice during the current COVID-19 pandemic.
NCMS advocacy staff has been working closely with committee members to ensure your interests are protected in this draft legislation. In particular, the NCMS’ areas of focus have been medical liability, financial relief, telemedicine parity and tax deferral.
The draft bill addresses some of our priorities. Other areas in the draft include increasing the state’s stockpile of personal protective equipment; expand COVID-19 testing capabilities; who might be permitted to administer a COVID-19 vaccine once it is approved; a study of how the health delivery system and health care workforce has been impacted by the pandemic; Medicaid coverage for COVID-19 prevention, testing and treatment for the uninsured.
Watch your Political Pulse Video and your NCMS Morning Rounds for further details as this legislation evolves.
Additional Allocation of CARES Act Provider Relief Fund
Yesterday, the US Department of Health and Human Services (HHS) provided additional information about allocation of the $100 billion CARES Act Provider Relief Fund.
As previously reported in your NCMS Morning Rounds, half or $50 billion of the Provider Relief Fund is allocated for general distribution to Medicare facilities and providers impacted by COVID-19, based on eligible providers’ 2018 net patient revenue.
The new allocations include an additional $10 billion to rural hospitals and rural health clinics based on their operating expenses, and $400 million directed to Indian Health Service facilities.
Some portion of the remaining funds is being used to cover the costs of caring for uninsured patients with COVID-19 such as office and emergency visits, including those provided via telehealth, will be reimbursed based on Medicare payment rates. These funds may be claimed beginning April 27. Learn more here.
An unspecified portion of the remaining funding will be used for clinicians, such as obstetrician-gynecologists, and facilities that rely more on Medicaid than Medicare revenues.
Learn more about the latest allocations here.
In the News
Inside America’s Unending Testing Snafu, Politico, 4-22-20
Learning Opportunity
DON’T MISS TODAY’S POWER HOUR!! This week’s NCMS Foundation Kanof Institute for Physician Leadership Power Hour from 1 to 2 p.m. on Friday will focus on what is happening in emergency departments across the state as the physicians who work there are grappling with treating patients today while also bracing to treat a potential surge in COVID-19 cases. The conversation brings together four emergency medicine physicians to more fully understand how they are dealing with the current situation while maintaining a sense of balance and self. Learn more and register. Also, you can access last week’s Power Hour: Stress in the Time of COVID-19 here.
On Monday, April 27, NCAHEC and the NC Office of Rural Health are offering their next telehealth focused webinar from noon to 1p.m. This one will focus on telehealth best practices in responding to COVID-19. Join the webinar through Zoom by clicking here.
NCGA House COVID-19 Health Committee
 The NCGA House COVID-19 Health Committee met on April 23, 2020.
The NCGA House COVID-19 Health Committee met on April 23, 2020.
View the agenda here.
The committee was provided a presentation on the draft policy bill.
Increase Personal Protection Equipment (PPE)
The bill directs the Division of Public Health, the Division of Health Service Regulation, and the NC Division of Emergency Management to develop a plan for creating and maintaining a strategic stockpile of PPE.
The plan would be required to include who should have access to the stockpile, ways to increase production within the state, potential stockpile locations, recommendations of the amount and kinds of items to stockpile, an inventory mechanism, and a 5 year budget.
Health Provider Support
Dentists
The bill allows the NC Board of Dental Examiners to waive statutory requirements in an emergency. (The NC Medical Board and the NC Board of Nursing do have this authority currently.)
The bill allows dentists to administer COVID-19 tests.
Pharmacists
The bill allows the State Health Director to authorize immunizing pharmacists to administer the COVID-19 vaccine by a statewide order if one is approved by the CDC at a time when the NC General Assembly is not in session. It would be a requirement that the Director develop a written standard screening questionnaire and safety procedures for written protocols for the vaccine to the Joint Legislative Oversight Committee, the NC Medical Board, the NC Board of Nursing and the NC Board of Pharmacy within 10 days of approving the petition. If this order moves forward, it would expire upon the adjournment of the next session.
The bill also allows pharmacists to use a government issued ID to identify patients picking up prescriptions.
Quality Improvement Plans
This bill would prohibit the enforcement of any administrative rule that would enforce quality improvement meetings between a PA or NP who had been practicing prior to February 2020. This would expire 60 days after the Executive Order is rescinded or December 31, 2020 (whichever is earlier).
Workforce Study
The bill directs the NC Area Health Education Center to study the issues impacting health delivery and the health workforce during a pandemic.
NCDHHS Flexibility
HealthConnex
The bill extends the deadline for providers to connect to HealthConnex from June 2020, to October 2021 to begin submitting demographic and clinical data in order to remain eligible for state funds.
Medicaid Coverage
The bill authorizes DHHS to provide Medicaid coverage for COVID-19 testing for the uninsured during the pandemic as allowed under the Families First Coronavirus Response Act.
The bill authorizes DHHS to provide Medicaid coverage to individuals with 200% FPL as described int he 1115 waiver DHHS submitted for federal approval. Coverage includes the prevention, testing, and treatment of COVID-19.
The bill requires DHHS to follow all federal laws necessary to receive enhanced Medicaid funding under the Families First Act.
Telehealth
Involuntary Commitment
The bill allows for the first and second examinations for involuntary commitment to be conducted via telehealth if the commitment examiner is reasonably certain that a different result would not have been reached in a face to face examination.
The bill would require all insurers and the State Health Plan to do the following
- provide coverage for telephonic care and e-visits
- provider coverage for provider to provider consultations
- cover telehealth and virtual health services without prior authorization
- cover physical therapy, occupational therapy, and speech therapy delivered via telehealth
- Reimburse providers the same rate for telehealth services as they do for in person services
Medicaid and Medicare
The NCGA urges CMS to provider coverage for health care provided through audio only communication.
Rep./Dr. Perrin Jones (R-Pitt) introduced an amendment to add medical liability protections to the bill.
The amendment states that any health facility, health provider, or entity that holds legal responsibility for a health professional shall have immunity from any civil or criminal liability for any harm or damages alleged to have been sustained as a result of an act or omission in the course of providing health services.
This amendment passed with a 15-1 vote and will be included in the bill as it moved to the House Health Committee.
The committee was provided a presentation on the draft funding policy bill.
Behavioral Health and Crisis Services
- $25 million in nonrecrruing funds to support public health efforts, local health departments, and rural health providers
- $25 million in nonrecurring funds to support behavioral health services
Medicaid
- $40 million in nonrecurring funds for coverage of additional costs related to the Medicaid program
- 5% rate increase for all fee for service Medicaid rates for all providers
- Authorization to provide Medicaid coverage for COVID-19 testing for the uninsured
- Authorization to provide Medicaid coverage for to individuals with incomes up to 200% of the federal poverty level
- Authorization to implement temporary Medicaid provider enrollment relief
Personal Protection Equipment
- $50 million in nonrecurring funds to purchase PPE and other supplies and equipment
Testing
- $25 milion in nonrecurring finds to expand public and private testing
Food, Safety, and Child Care
- $6 million in nonrecurring funds to allocate equally among each of the 6 food banks
- $2.5 million in nonrecurring funds to the Reinvestment Partners (non-profit organization) which provides funding to eligible Food and Nutrition Services Recipient enrolled by the recipient's health care provider
- $2.25 million in nonrecurring funds to assist in serving children in foster care to be used for monthly supplemental payments
Rural and Underserved Commuities
- $25 million in nonrecurring funds to support rural and underserved communities for items not addressed by federal funds
- $75 million in nonrecurring funds to support rural hospitals
- $1.4 million in nonrecurring funds to support the 67 free and charitable clinics
- $1.5 million in nonrecurring funds to NC MedAssist to offset increased costs for services for the uninsured
Other Relief
- $25 million in nonrecurring funds for NC Teaching Hospitals
- $100 million to the NC Policy Collaboratory
- $25 million to the Duke Human Vaccine Institute
- $25 million to the UNC Gillings School of Public Health
- $25 million to ECU Brody School of Medicine
- $25 million to Wake Forest School of Medicine
- $10 million to Campbell University Osteopathic School of Medicine
NCMS Morning Rounds 4-23-20
Already Thursday and time for your daily
NCMS Morning Rounds.
April 23, 2020
After strong winds from recent thunderstorms ripped part of the banner on our building, now there is a new sign gracing the front of the NCMS Center for Leadership in Medicine in Raleigh for all to see. We’ve already had several positive comments from passers-by.
NCMS Action Alert on Malpractice Liability Protections
The NCMS is asking you to send an Action Alert to North Carolina legislators serving on the House Select Committee on COVID-19 asking them to support medical malpractice liability protections as they consider legislation to address issues arising from the COVID-19 pandemic. The NC General Assembly is scheduled to convene next Tuesday, April 28.
As legislation is being developed, this message to your representatives will help make sure that any bill contains protections for direct COVID-19 treatment as well as for those services impacted by the statewide COVID-19 response. Examples might include limitations on the ability to diagnose, treat or otherwise care for patients due to the unavailability of personal protective equipment (PPE), limitations on access to testing and procedures as well as a host of other difficulties due to state orders and guidance.
Please take a moment now to review this ready-to-send message and urge legislators to support liability protections for you.
FCC Offers Telehealth Support
This week the Federal Communications Commission (FCC) announced a $200 million emergency COVID-19 Telehealth Program to help eligible physician and PA practices purchase telecommunications services, information services and devices necessary to provide telemedicine services during this emergency period. The program will provide selected applicants with full funding for these eligible telehealth services and devices. The $200 million program is part of the CARES Act legislation.
The money will be targeted to areas hardest hit by COVID-19 especially areas with a low income population, a health care provider shortage, rural hospital closures and limited broadband/internet access. The program is not limited to only treating COVID-19, it can also be used to “prevent, prepare for and respond to COVID-19. Learn more about the FCC’s Telehealth Program.
In addition, the FCC announced the three-year Connected Care Pilot Program to provide universal service support to help defray health care providers’ qualifying cost of providing connected care services. This pilot program will make available up to $100 million, separate from the Telehealth Program. Learn more about the Connected Care Pilot Program.
In the News
Why Rural America Could be a ‘Tinderbox’ for COVID-19, The Advisory Board Forum, 4-22-20
Learning Opportunity
Eastern AHEC will present a webinar on ‘Using Telehealth to Bridge Social Distancing During COVID-19’ on Tuesday, April 28 from noon to 1:30 p.m. The webinar will provide a practical and evidence-based approach to patient-centered clinical care delivered in whole or in part by technological devices and applications. It will include a discussion of the “nuts and bolts” of delivering telehealth/telepsychiatry services, standardized approaches in telehealth/telepsychiatry care, and discussion of barriers in delivering telehealth/telepsychiatry services. Learn more and register.
NCMS Morning Rounds 4-22-20
Welcome to Wednesday and your
NCMS Morning Rounds.
April 22, 2020
Resources for Maternal and Infant Health During COVID-19
As you know, maternal and infant health has been a focus for the NCMS with plans for another summit meeting in the future. In the meantime, NCMS staff has compiled a few resources for mothers, mothers-to-be and their caregivers.
The University of North Carolina’s Jordan Institute for Families and its 4th Trimester Project updated its postpartum self-care resource, www.newmomhealth.com, to include information related to coronavirus. Access the information here.
Also, Every Mother Counts posted a master list of links related to maternal and infant health in the midst of the pandemic. Review those resources here.
Lastly, practices that utilize group prenatal care models may find the support shared by the Centering Healthcare Institute (CHI) helpful. For example, CHI is offering 1-on-1 time with centering advisors at no cost for Centering sites and is also hosting a Zoom session to share guidance for adapting Centering groups to a virtual format on Thursday, April 24 at 4 p.m. Please note that participants will need a login for a Centering Practice Site to register for the Zoom webinar. Access the CHI COVID-19 resources here.
Virtual Oral health Care Helpline Established
North Carolinians now have access to virtual dental services during the COVID-19 outbreak, thanks to a new initiative at Carolina Dentistry, a part of the University of North Carolina Adams School of Dentistry. A virtual oral health care helpline -- (919) 537-3088 – has been set up to provide a way for patients to manage dental care from the comfort of their homes and to help eliminate the burden of dental emergencies on emergency departments during the COVID-19 outbreak.
The Carolina Dentistry Virtual Oral Health Care Helpline is available Monday through Friday, 8 a.m. to 5 p.m., and offers referrals for dental emergencies that must be addressed in person.
For patients who have urgent needs across the state and cannot easily travel to Chapel Hill, Carolina Dentistry will provide patients with information for their closest dental clinic.
Oral health care providers across North Carolina may also call to speak with a specialist for patient consultations and referring patients with dental emergencies.
Learn more by visiting carolinadentistry.org
Taking to the Skies to Help
Longtime NCMS member Dickson Schaefer, MD, an orthopedic surgeon at Fayetteville Orthopaedics & Sports Medicine has been featured prominently in media reports throughout the state lately. Dr. Schaefer has taken to the skies, flying patients’ specimens and test results to and from Fayetteville to speed up the process of finding out COVID-19 test results.
Dr. Schaefer told reporters he loves to fly planes and in the past he has flown somewhere just to get a hamburger – what his pilot friends like to call a ‘$100 burger.’ Now, Dr. Schaefer is enjoying helping people while participating in a hobby he loves – the perfect melding of his passions for medicine and flying.
Here is some of the coverage:
- Flights Being Used to Get Coronavirus Tests Back Quicker, Spectrum News.
- Local Pilots Volunteer to Fly Specimens to National Lab for COVID-19 Testing, CBS-17.
- Heart of Gold: Physician Lends Own Plane Time to Speed Results to Patients, Bladen Journal
- Fayetteville Surgeon Stops in Asheville on Coronavirus Testing Mission, Asheville Citizen Times
- Hospital Partners with Pilots to Get Quicker COVID-19 Test Results, ABC-11
In the News
Everything We Know About Coronavirus Immunity and Antibodies – and Plenty We Still Don’t, STAT, 4-20-20
Learning Opportunity
The American Public Health Association and the National Academy of Medicine will present the next in their series of COVID-19 Conversations TODAY, Wednesday, April 22, from 5-6:30 p.m. Today’s webinar will focus on COVID-19 Testing: Possibilities, Challenges, and Ensuring Equity. Hear from trusted experts in such fields as public health, infectious disease, risk communication and crisis standards of care. Register Now.
You can also access recordings of previous webinars in the series here.
NCMS Morning Rounds 4-21-20
It's Tuesday and time for your
NCMS Morning Rounds.
April 21, 2020
NCMS Task Force to Address Virus Mitigation and Open Economy
Tomorrow, Wednesday, April 22, the newly formed NCMS Task Force on Virus Mitigation in an Open Economy will convene for its first meeting. As its name suggests, the group of NCMS leaders will work to formulate recommendations on how to mitigate the spread of the COVID-19 virus while seeking to re-open the economy. The group, led by NCMS Board of Directors at-large member Michael Utecht, MD, FACEP, hopes to forward its initial recommendations to the full NCMS Board within the next several weeks.
As NCMS President Palmer Edwards, MD, DFAPA, noted in his message to the Task Force, “It is important for the physician community to be an informed voice in this discussion” of mitigating the public health impacts of COVID-19 while ensuring a stable economic future for those temporarily displaced from their usual employment.
Watch your NCMS Morning Rounds for details on the work of this task force in the coming days.
Dr. Brown Addresses Health Disparities During COVID-19 Pandemic
The current pandemic has served to underscore the health disparities present in our health care system. NCMS President-Elect Philip Brown, Jr., MD, in his capacity as New Hanover Regional Medical Center’s Chief Physician Executive, recently reached out to the African American community in New Hanover County and beyond through a YouTube video in which he speaks frankly about the health disparities faced by African Americans and what everyone can do to help slow the spread of the virus.
Zocdoc Helps Connect Patients and Your Practice -- Virtually
With the current surge in demand for telemedicine appointments, NCMS Business Alliance partner, Zocdoc, can help patients easily connect virtually with your practice, while seamlessly booking those appointments.
As an added incentive to sign on now, Zocdoc is offering NCMS members a $50 Visa gift for taking 30 minutes to learn more about what Zocdoc offers. Just fill out the form here and mention the NCMS when you speak to the Zocdoc team member. Also, for a limited time Zocdoc is offering 50 percent off video visits booked through platform.
In the News
When Duty Calls, and Menaces, The New York Times, 4-17-20
Learning Opportunities
Mark your calendar for two important events this Friday, April 24.
A special Zoom webinar for NCMS members interested in learning more about the financial resources offered by Centene and Carolina Complete Health, will be held on Friday at 4:30 p.m. Two experts from LSN Partners, a Global Consulting Firm will offer their insights and help in understanding the programs and initiatives that are part of the Coronavirus Aid, Relief and Economic Security (CARES) Act and what will be available from the Small Business Administration (SBA) to assist business owners. Learn more and register here. After registering, you will receive a confirmation email containing information about joining the webinar.
This week’s NCMS Foundation Kanof Institute for Physician Leadership Power Hour from 1 to 2 p.m. on Friday will focus on what is happening in emergency departments across the state as the physicians who work there are grappling with treating patients today while also bracing to treat a potential surge in COVID-19 cases. The conversation brings together four emergency medicine physicians to more fully understand how they are dealing with the current situation while maintaining a sense of balance and self. Learn more and register.
NCMS Morning Rounds 4-20-20
Welcome to another week and your Monday NCMS Morning Rounds.
April 20, 2020
NCMS Legislative Update
Last week was a busy one as federal and state officials work to more fully understand and address the financial and policy needs of their constituents, and the NCMS continues to advocate on your behalf.
In the NC General Assembly, the House COVID-19 Health Committee met last Thursday to discuss priorities for the coming session, slated to convene on April 28. They reviewed the various ‘buckets’ of needs, including those impacting health care professionals. You can review all of the documents from the committee’s meeting and hear an audio recording of the proceedings here. The committee is scheduled to meet again this Thursday at 9:30 a.m. The NCMS is reviewing all recommendations of the committee as they develop bill language. Keep up to date on our Legislative blog.
The NCMS remains focused on the priorities approved by the NCMS Legislative Cabinet, which include:
• Telemedicine Parity
• Tax deferral
• Medical Liability
• Financial Relief
Also, last week the Midwifery Joint Committee, the entity with the authority to adopt administrative rules governing nurse midwives, met for an emergency meeting last Wednesday, April 16, to consider proposals designed to modify the practice of nurse midwives in response to the COVID-19 epidemic.
The Committee initially intended to consider the following proposed waivers:
1) temporary waiver of physician supervision for those current midwives who want to work outside their usual practice during the emergency—example to volunteer
2) temporary waiver of physician supervision for those retired or inactive midwives to return to the workforce for purposes of responding to the emergency-example volunteer, birth center, etc.
3) temporary waiver of national certification examination for those newly graduating nurse midwives expected in May –example-many already have job offers, but testing centers are not open
However, the Committee ultimately decided to only consider the waiver of national certification examination proposal after receiving numerous requests from stakeholders for more time to provide feedback and to review supportive data for the other temporary waivers. The remaining proposals were tabled for consideration at a subsequent meeting to be scheduled in the near future.
Following discussion, the Committee approved an order allowing new nurse midwife graduates who have not taken the required national certification testing to be issued a temporary license. The license will be valid until August 1, 2020, or until the current State of Emergency is suspended if sooner than August 1, 2020, and will permit a nurse midwife to practice under the supervision of an on-site physician or certified nurse midwife who has been practicing for a minimum of two years.
Watch your NCMS Morning Rounds for updates on this issue in the future.
Pandemic Response Network Makes Changes to Encourage Participation
As reported earlier in your NCMS Morning Rounds, DukeHealth has introduced the Pandemic Response Network study, which features a 28-day symptom monitoring program without geographic or age restrictions and allows for community informed surveillance to enhance the detection of potential COVID-19 prevalence. The program will help anticipate the course of the illness and timing of needed resources. The study will help everyone learn more about COVID-19 and support participating practices. Learn more and sign up here.
Now, the Pandemic Response Network is making changes to allow greater ease of participation. Soon all materials will be available in Spanish and the Network has already brought on Spanish-speaking team members to reach out to Spanish speaking participants when needed. Also, the team is working on creating a text-based survey tool for those with a flip phone. The Network is able to accommodate registering/consenting new members via a phone call with a member of the team entering all the data. Previously, interested individuals had to do this via smartphone or computer.
Here is a one-page flyer for health care workers with information about the study.
Here is a one-page flyer for patients with information about the study.
NCMS Award Nominations Open
Despite the upheaval wrought by the COVID-19 pandemic, some things remain reassuringly unchanged – recognizing outstanding health care professionals for their service. As we do every year, the NCMS is seeking nominations for two awards – the E. Harvey Estes, MD, Community Service Award and the John Huske Anderson Award.
The E. Harvey Estes, MD, Physician Community Service Award recognizes a physician who has an outstanding record of community service that reflects well on the medical profession apart from their work or identification as a physician. Download the nomination form here.
The John Huske Anderson Award recognizes a layperson whose contributions have had a positive impact on the medical profession and the public health in North Carolina. Download the nomination form here.
Nominations are due to Evan Simmons, [email protected] by Aug. 1, 2020.
In the News
‘It’s Not Over Until It’s Over’: 5 Things to Know About Hitting the COVID-19 Peak, Kaiser Health News, 4-17-20
Learning Opportunity
Two offerings this week promise to help you cope during this unprecedented time:
Navigating COVID-19: Your Resiliency: Protecting Your Practice’s Human Capital webinar will take place on Tuesday April 21 from 6 to 7 p.m. Presenting will be Allan Chrisman, MD, DLFAPA, Associate Professor Emeritus of Psychiatry and Behavioral Sciences for the Duke University School of Medicine. Dr. Chrisman will speak on promoting a sense of “Safety, Self- and Community-Efficacy, Connectedness, Calming and Hope.” Click here to connect or dial: 646-558-8656 using Webinar ID: 131 899 801
Curi Benefits Solutions will present a free webinar on Wednesday, April 22 at noon on ‘Caring for Yourself and Others During the COVID-19 Pandemic.’ Topics will include recognizing the physiological impacts of COVID-19; constructive and positive ways to cope; overcoming isolation and tools to maintain your well-being during this turbulent time. Learn more and register.
NCGA House COVID-19 Health Committee
 The NCGA House COVID-19 Health Committee met on April 16, 2020 to discuss bill priorities for the upcoming short session.
The NCGA House COVID-19 Health Committee met on April 16, 2020 to discuss bill priorities for the upcoming short session.
This list of items the committee considered includes recommendations by groups that presented during the past few weeks, including NCMS.
NCMS is currently reviewing all of these recommendations to help legislators as they develop bill language.
NCMS remains focused on the priorities approved by the NCMS Legislative Cabinet which include the following:
- Telemedicine Parity
- Tax deferral
- Medical Liability
- Financial Relief
NCMS Morning Rounds 4-17-20
Happy Friday! Enjoy your NCMS Morning Rounds.
April 17, 2020
The Kanof Institute for Physician Leadership’s ‘Power Hour’ is today, Friday, April 17 from 1 to 2 p.m. Join us for a conversation with colleagues and psychiatric experts on the actual and potential mental health toll the pandemic is exacting in the health care profession and beyond. Learn more and sign up.
Next Steps in the State’s COVID-19 Response
On Wednesday, Governor Roy Cooper reviewed the actions taken thus far in response to COVID-19 and shared that those actions had begun to ‘flatten the curve’ in North Carolina. He and NC Department of Health and Human Services (NCDHHS) Secretary Mandy Cohen, MD, MPH also laid out a path for moving forward to protect North Carolinians and help recover our economy.
Governor Cooper and Secretary Cohen stressed that the next steps, as were all previous actions, will be driven by science and data. Chief among those new steps will be widespread testing, aggressive contact tracing and data-informed policy decisions.
The next steps depend on progress in:
• Testing or identifying who has COVID-19: Working with private and public partners to increase testing capacity, expand testing sites and address supply challenges.
- Acting quickly to stop spread through tracing: Ramping up staffing and technology to determine who has been exposed when someone tests positive.
- Knowing when to dial up or down social distancing through data trends: Analyzing new data, including number of new cases, hospitalizations, deaths, protective equipment, supplies, hospital capacity and more.
State officials are terming this phase of the COVID-19 response “staying ahead of the curve.” Learn more by downloading their presentation, reading the accompanying press release or watching the press briefing in which they outlined the next steps.
National Physician Support Line
If you need a little extra support as you respond to the unprecedented public health crisis we’re facing, a group of volunteer licensed psychiatrists are standing by to listen and provide that support.
The Physician Support Line (1-888-409-0141) is available 7 days a week between 8 a.m. and 3 a.m. and offers psychiatric help to physicians navigate an immediate stressor. The support is not given as part of a doctor-patient, therapist-client relationship, no medications will be prescribed and no payment is accepted. It is a friendly and professional ear to help you through an immediate tough spot. Learn more here.
The NCMS’ Emotional Supports webpage offers a number of ways to access support services and resources during this trying time.
In the News
A War for Medical Supplies: States Say FEMA Wins By Poaching Orders, NPR, 4-15-20
Learning Opportunity
The 157th National Academy of Science Annual Meeting, to be held online April 25-27, will include a late-breaking session on COVID-19 to provide deeper insights into the latest developments in the COVID-19 response. A diverse panel chaired by National Academy of Medicine President Victor Dzau, MD, and featuring the Director of the National Institute for Allergy and Infectious Diseases Anthony Fauci, MD and CNN Chief Medical Correspondent Sanjay Gupta, MD, and others will speak to the whole experience on dealing with this pandemic—from US to international, to the state of diagnostics, treatment and vaccine development, to the importance of communication. Register to watch the panel.
NCMS Morning Rounds 4-16-20
Enjoy Your Thursday NCMS Morning Rounds
April 16, 2020
Reminder: See bottom of this newsletter for information about help sessions today to access the Presence telemedicine platform, which the NCMS is offering at no charge to practices during the COVID-19 pandemic.
And don’t forget the Kanof Institute for Physician Leadership’s ‘Power Hour’ tomorrow, Friday, April 17 from 1 to 2 p.m. for a conversation with colleagues and psychiatric experts on the actual and potential mental health toll the pandemic is exacting in the health care profession and beyond. Learn more and sign up.
NCMS Supports Federal Advocacy Efforts
Yesterday the American Medical Association (AMA) with the support of the NCMS and most other state and national medical societies sent a letter to Congressional leadership outlining various items needed by the health care community to successfully respond to and financially weather the impact of the COVID-19 pandemic.
The letter outlines a variety of additional steps necessary to “protect patient access to care by preserving the viability of physician practices as part of the nation’s essential health care system.” Areas addressed include refinements to the Medicare Advance and Accelerated Payments program; direct financial support to practices including grants and interest free loans and additional funding for small business loans through the Small Business Administration. The letter also discusses liability issues and urges Congress to provider broader liability protections for physicians and PAs.
Resources for Treating OUD During COVID-19
During this challenging time for everyone those involved with treatment for opioid use disorder (OUD) may be facing additional obstacles. Federal agencies have updated guidance on prescribing and use of telemedicine during this public health emergency.
Below are several sources of information and resources if you are treating patients with OUD. Also, please keep in mind the NCMS Foundation’s Project OBOT, which offers a collaborative approach to treatment, is also making the Presence telemedicine platform available at no charge for the immediate future.
Resources for Treatment Providers:
SAMHSA DEA Buprenorphine Telemedicine Guidance: This updated guidance, released on March 31, 2020, recommends that opioid treatment programs (OTPs) and DATA-waivered physicians should feel free to prescribe and dispense buprenorphine to new patients for OUD maintenance following an evaluation over the phone. This guidance temporarily relaxes new patient initiation protocols for the duration of the COVID-19 public health emergency.
SAMHSA OTP Guidance for Patients Quarantined at Home with Coronavirus: This guidance from SAMHSA outlines steps that should be taken to ensure that people with opioid use disorders are able to continue to use their medications safely during quarantine.
COVID-19 Intervention Actions: Providing Medication Assisted Treatment for Opioid Use Disorder: This resource from the Association of State and Territorial Health Officials provides a list of OTP guidance from the Federal government and states across the U.S.
Please Let Us Know of Practice Closures
As communicated earlier, the NCMS is working with NC Medicaid to assess potential medical practice closures in response to the impact of the COVID-19 pandemic. NC Medicaid will need to redirect Medicaid beneficiaries as closures occur across the state.
If your practice/facility closes in response to COVID-19, or if you become aware of others that close, please let us know and we will relay the information to NC Medicaid.
Even if you do not see Medicaid patients, it would be helpful to be aware of practice and facility closures as we monitor the COVID-19 impact.
The information that NC Medicaid has requested includes:
• Practice/Institution Name
• Specialty
• Does the practice see Medicaid patients
• # of Locations
• Location cities
• NPIs for Affiliated Providers (if available)
Additional information regarding closures would be welcome as well, such as if the practice has provisions for transferring patient care, closure duration, etc.
Please respond to: [email protected] with this information. And please feel free to share this email with colleagues and other practices. Thank you for helping us assist the NC Medicaid program in its efforts to avoid gaps in care.
In the News
Opinion: Will 2020 Be the Year That Medicine Was Saved? The New York Times, 4-15-20
Learning Opportunity
The Office of Rural Health (ORH) and NC AHEC are co-sponsoring a weekly webinar series each Monday from noon to 1 p.m. to address the role of virtual visits in responding to COVID-19. The webinars will enable providers to pose questions directly to telehealth subject matter experts. Recordings and transcripts of previous webinars dating back to March 30 are available here.
Please submit any questions for subject matter experts in advance of Monday’s webinar to [email protected] by noon on the Friday preceding the webinar.
You can access the webinar each week through Zoom at this link or dial in number:
Join the Zoom meeting room or dial-in at (646) 558-8656 with webinar ID 985 104 650
Also, don’t forget Friday’s Forum with NC Division of Public Health subject matter experts. The forum will be held as usual, from 12:30 to 1:30 p.m. Please send questions to [email protected]. You can access the forum from your computer by clicking on this Zoom meeting link or calling in at +16465588656,,705979628# (mobile) or (646) 558-8656 or (301) 715-8592 Webinar ID: 705 979 628
Reminder: The sessions to help you access Presence, the telemedicine platform offered at no-charge to you during the COVID-19 pandemic, will be held at the times listed below. Please call or click on the appropriate link to have an expert walk through the onboarding process with you. Be sure to have an internet connection and your NPI number available when signing in to the session.
TODAY, Thursday, April 16:
7:30 a.m.
Join Zoom https://therecoveryplatform.zoom.us/j/97211518011
Meeting ID: 972 1151 8011
One tap mobile +16465588656,,97211518011#
Noon
Join Zoom https://therecoveryplatform.zoom.us/j/98752933925
Meeting ID: 987 5293 3925
One tap mobile +16465588656,,98752933925#
5:30 p.m.
Join Zoom Meeting https://therecoveryplatform.zoom.us/j/98862662010
Meeting ID: 988 6266 2010
One tap mobile +16465588656,,98862662010#
NCGA House COVID-19 State Operations Committee
 The NCGA COVID-19 State Operations Committee met on April 14, 2020.
The NCGA COVID-19 State Operations Committee met on April 14, 2020.
The Committee discussed potential legislative action on a variety of subjects.
NCMS is following these items:
- Advanced Health Care Directives
- The proposal by the Secretary of State would allow an emergency special provision to allow a notary OR two witnesses to sign these documents. Current law requires a notary AND two witnesses.
- Incompetency and Adult Guardianship
- The School of Government proposed allowing another type of service if sheriffs are unable to go into a facility to serve copies of the petition.
- The School of Government proposed allowing appointment of an interim guardian via video conference.
- Communicable Disease Information
- The School of Government proposed aligning state law with HIPPA to allow disclosures to law enforcement that are necessary to prevent or lessen a serious threat.
- Business Registration
- The Secretary of State proposed waiving fees for businesses that are dealing with economic downturn.
- Involuntary Commitment
- The School of Government proposed expediting the training process for transporting involuntary commitment patients, and allowing telemedicine for the second IVC examination.
- Regulatory Relief
- The Committee Co-chairs proposed authorizing or requiring state agencies to waive, delay, or modify any educational or examination requirements.
- State Health Plan Payment Deadlines
- The NC Treasurer's Office, proposed allowing time-limited flexibility around payment deadlines to extend the due date to help ensure patients are not kicked off the plan due to non-payment.
View the full list here.
NCGA House Health COVID-19 Committee
 The NCGA House Health COVID-19 Committee met on April 14, 2020.
The NCGA House Health COVID-19 Committee met on April 14, 2020.
You can provide input for the House Select Committee on COVID-19 here.
Listen to the entire meeting here.
https://www.ncleg.gov/documentsites/committees/house2019-199/Health%20Care%20Working%20Group/04-14-2020/2020-04-14%20Health%20Care%20-%20Audo.mp3
Impact of COVID-19 on Rural Health Care
Delivery
Dr. Roxie Wells, MD, President of Cape Fear Valley Hoke Hospital provided a rural hospital perspective to the group. She noted that she is passionate about rural hospitals surviving and providing equitable care to patients. She explained that rural communities are the most vulnerable to disparities, and that our rural communities are aging.
Some specific barriers to rural communities include, minimal PPE, lack of equipment for testing, loss of revenue from non essential procedures.
She expressed grave concern about our state's rural hospitals, and the patients that live there. Currently, some skilled nursing facilities are unsure if they should accept new patients.
She closed with stating that North Carolina has 49 rural and independent hospitals in the state, and she was confident we could end the COVID-19 pandemic with that same number.
Impact of COVID-19 on the Delivery of
Behavioral Health/IDD Services
Kody Kinsley, Deputy Secretary, Behavioral Health and Intellectual and Developmental Disabilities, Department of Health and Human Services, stated that their main goals were to maintain services and reduce the need for emergency department visits to keep hospital beds open for COVID-19 patients.
He added that this pandemic increases the potential worsening anxiety and depression disorders due to lack of control and social isolation.
Key DHHS Behavioral Health Actions
- Medicaid flexibility (appendix K and 1135 Waiver)
- New telehealth policies
- Paused oversight functions that do not impact consumer health and safety
Resources and Funding
- Immediate release of remaining single stream funds for current fiscal year
- Authorized use of up to 15% of LME/MCO risk reserve
- Category B funds from FEMA Disaster Declaration
- Increase of 1.5% in Medicaid rates for LME/MCOs
Dr. Atezaz Saeed, MD, MS, Executive Director, NC Statewide Telepsychiatry Program informed the group about challenges psychiatrists are experiencing during COVID-19. A national poll released by the APA in late March found that more than 36% of Americans say that coronavirus is having a serious impact on their mental health.
He added that mental health and substance abuse disorders are common, but services have been in short supply even before the COVID-19 pandemic.
He states that 26.2% of americans ages 18 and older have a mental disorder and about 6% suffer from a serious mental illness.
He advocated on behalf of the NC-STEP program which makes collaborative linkages and develops innovative models of mental health care. The web portal is accessible to all participating providers, and creates a central point for coordinated care.
Impact of COVID-19 on Pharmacists
Rep. Wayne Sasser (R-Stanly), PharmD, presented on behalf of the pharmacy community. He stated that pharmacists are essential and a large number of pharmacies are increasing delivery services. CMS pays 6.2% in Medicaid match to pay for these extra services which helps compensate pharmacists for delivery. This helps pay pharmacists for their delivery.
He informed added that some contracts are not allowing patients to choose their drugstores. He provided an example of a constituent who was forced to get a prescription from a chain drugstore without a pick up window or delivery service which put the patient at risk. Rep. Sasser said “We need to do better for patients.”
Another suggestion he added was to loosen restrictions for pharmacists reviewing prescriptions for assisted living facilities. Currently, they are required reviews every 3 months in these settings.
He also suggested that providing halo one to potential overdose patients could be a way to keep them out of the emergency rooms.
Impact of COVID-19 on Populations with
Health Disparities
Cornell Wright, MPA, Director of Office of Minority Health and Health Disparities, NCDHHS informed the group about the health inequities relating to COVID-19.
He said that there are a variety of factors that impact disparities including the following:
- Environment
- Education,
- Housing,
- Health Care
- Food/Nutrition
- Violence
- Poverty
He noted, trust is a big factor that is not typically discussed.
He spoke about the specific demographics in North Carolina. Minority populations experience higher rates of unemployment. Yet, 63% of all jobs require post secondary education.
Currently, 1 in 5 North Carolinians live in poverty.
People of color may be disproportionately at higher risk for more severe illness from COVID-19. 21% of NC residents are African American. 38% of positive COVID-19 cases are African American. He repeatedly informed the group that more data is needed in order to better understand the layers of factors that may impact this data.
(*Interpret data with caution.)
Impact of COVID-19 on the Health Insurance
Industry
Ken Lewis, NC Association of Health Plans Executive Director provided the health plan perspective to the Committee.
Their member companies provide insurance for more than 6 million North Carolinians. He asked the NCGA to consider assisting providers who have been affected by the emergency, but have not received assistance with CARES Act funding.
He asked for any policy decisions relating to this emergency sunset to end at the sunset in order to allow for a full review of a discussion of what worked and what did not work.
NCMS Morning Rounds 4-15-20
Halfway through the week! Enjoy your
NCMS Morning Rounds.
April 15, 2020
Reminder: See bottom of this newsletter for information about help sessions today and tomorrow to access the Presence telemedicine platform, which the NCMS is offering at no charge to practices during the COVID-19 pandemic.
NCDHHS Requests CARES Act Funds for Medicaid Providers
Yesterday, NC Department of Health and Human Services Secretary Mandy Cohen, MD, MPH asked US Health and Human Services Secretary Alex Azar and Centers for Medicare and Medicaid Services (CMS) Administrator Seema Verma to dedicate a portion of the $100 billion CARES Act Provider Relief Fund to those health care professionals who serve Medicaid beneficiaries and the uninsured.
“Federal strategies to support and stabilize health care providers have, to date, relied heavily on Medicare to distribute federal payments, including using the Medicare program as the vehicle for distributing $30 billion from the Provider Relief Fund and determining the size of the payments received by each provider,” Sec. Cohen wrote in a two-page letter to Azar and Verma. “While this is an efficient and effective way to quickly disburse federal funds to providers serving Medicare beneficiaries, other strategies are needed to shore up those health providers more heavily reliant on Medicaid. These providers are essential to providing care to low-income beneficiaries and the uninsured.”
Sec. Cohen points out that many pediatric, ob-gyn, mental health and safety net practices rely more heavily on Medicaid and should be taken into account when disbursing the CARES Act funding. She asks that a portion of the $100 billion in relief funds authorized under the CARES Act be set aside for essential Medicaid providers and that CMS enlist state Medicaid programs to quickly distribute the funds to the at-risk Medicaid providers in their states in a way that reflects specific needs in each state.
She goes out to outline how such a program could be set up and provide relief to struggling practices in North Carolina. Read the full letter.
This Week’s ‘Power Hour’: Dealing with COVID-19 Upheaval
The last few weeks have been unsettling for most, if not all individuals in our communities and around the world. Everyday life has been dramatically changed and these changes have impacted how we live, work and interact in whatever we do.
There are many questions to be asked as a result of this upheaval: how are our patients doing? Our peers and colleagues? Or our own families and friends? How are people dealing with and making sense of COVID-19 and how well are systems responding? What behaviors do we see among the people we meet? What signs of stress and anxiety are coming to the surface within ourselves and among our co-workers? How do we take care of ourselves as providers while also taking care of loved ones? And how do we balance our care for patients with caring for our families?
This Friday, April 17 from 1 to 2 p.m., join a ‘Power Hour’ chat about the mental health aspects of working in health care during these times and what issues people are dealing with. Moderated by NCMS Vice President of Rural Health Systems Innovation Franklin Walker, MBA and Harold Kudler, MD, you will have the opportunity to listen and converse with NC Psychiatric Association (NCPA) President-Elect Zach Feldman, MD; President of the NC Council of Child & Adolescent Psychiatrists Therese Garrett, MD; and fourth year adult psychiatry resident Nkechi Conteh, MD, about the behaviors we notice around us and how we can handle them. This is an opportunity to share knowledge and learn from each other about the impact of a pandemic on our behavior and stress levels, and to think about how we can integrate our perspectives to achieve better outcomes for our patients, for ourselves and for our families.
The ‘Power Hour,’ brought to you by the NCMS Foundation’s Kanof Institute for Physician Leadership (KIPL), aims to provide a forum for ongoing conversation, collaboration and community. Tune in to the ‘Power Hour ‘weekly to hear from different experts, decision makers and influencers on a variety of topics. The format is informal and conversational and sessions are easy to access through Zoom. Register for this Friday’s ‘Power Hour.’
‘Power Hours’ will be recorded and made available through your NCMS Morning Rounds and on the KIPL webpage.
Resources to Understand Prior Authorization and Coding During COVID-19
The AMA recently produced two resources you may find helpful. The first tracks the rapidly evolving prior authorization policy changes health plans and prescription drug plans are making in response to COVID-19. The second offers coding guidance to reflect the most recent information released by the Centers for Medicare and Medicaid Services (CMS).
Access the Prior Authorization Policy Changes Related to COVID-19 here.
The Coding Guidance document includes 18 different treatment scenarios and recommended coding for each. Download ‘Special Coding Advice During COVID-19 Public Health Emergency’ here.
In the News
States United on Reopening Economies: ‘Science – Not Politics’ – Will Guide Decisions, NPR, 4-13-20
Learning Opportunity
The American Academy of Public Health and the National Academy of Medicine invite you to the next in the series of COVID-19 Conversations webinars, which will focus on ‘Crisis Standards of Care During COVID-19.’ The webinar will be held TODAY, Wednesday, April 15 from 5 to 6:30 p.m. The conversation will include an overview of and challenges for adapting crisis standards of care to rapidly evolving clinical care guidelines for the disease; practical considerations for state health departments and hospital systems; and ethical considerations and decision-making around crisis standards of care. Learn more and register.
Reminder: Sessions to help you access Presence, the telemedicine platform offered by the NCMS at no-charge to you during the COVID-19 pandemic, will be held at the times listed below. Please call or click on the appropriate link to have an expert walk through the onboarding process. Be sure to have an internet connection and your NPI number available when signing in to the session.
TODAY, Wednesday, April 15:
7:30 a.m.
Join Zoom Meeting: https://therecoveryplatform.zoom.us/j/92993467952
Meeting ID: 929 9346 7952
One tap mobile +16465588656,,92993467952#
Noon
Join Zoom Meeting https://therecoveryplatform.zoom.us/j/96280402133
Meeting ID: 962 8040 2133
One tap mobile +16465588656,,96280402133#
5:30 p.m.
Join Zoom Meeting https://therecoveryplatform.zoom.us/j/97240344510
Meeting ID: 972 4034 4510
One tap mobile +16465588656,,97240344510#
TOMORROW, Thursday, April 16:
7:30 a.m.
Join Zoom https://therecoveryplatform.zoom.us/j/97211518011
Meeting ID: 972 1151 8011
One tap mobile +16465588656,,97211518011#
Noon
Join Zoom https://therecoveryplatform.zoom.us/j/98752933925
Meeting ID: 987 5293 3925
One tap mobile +16465588656,,98752933925#
5:30 p.m.
Join Zoom Meeting https://therecoveryplatform.zoom.us/j/98862662010
Meeting ID: 988 6266 2010
One tap mobile +16465588656,,98862662010#
NCMS Morning Rounds 4-14-20
Enjoy your Tuesday
NCMS Morning Rounds.
April 14, 2020
NCMS Legislative Update
Last Thursday, the NCMS Legislative Cabinet met virtually to set its priorities in anticipation of the upcoming Legislative Session, which is still slated to begin on April 28. These priorities will guide the NCMS’ advocacy efforts, and, for the moment, focus on the immediate needs of our members in dealing with the impact of the COVID-19 pandemic. The priorities are:
- Telehealth parity
• Ensuring cash flow
• Tax deferrals
• Liability protections
Legislative Cabinet members discussed what they are experiencing in their own practices as well as what they have been hearing from colleagues and reviewed the results of the NCMS’ Sunday Survey series to arrive at these priorities.
While the Legislative Session is still nearly two weeks away, the NC House Select Committee on COVID-19 has been meeting to address various issues associated with the pandemic including health care and economic supports among others. NCMS staff already is actively communicating our priorities to the chairs and members of this key legislative committee.
Read summaries of the last several COVID-19 committee meetings, which NCMS staff have been attending virtually, on our NCMS Legislative blog.
The Legislative Cabinet also had a broader discussion about how COVID-19 has accentuated health disparities. Their comments centered on this blog post by the NC Institute of Medicine, which addresses limited access to healthy foods, a condition that has been magnified during the pandemic.
Before COVID-19 prompted the current upheaval in all aspects of our daily lives, the NCMS identified the NCIOM’s Healthy NC 2030 report as a focal point for our LEAD Health Care Conference this fall and beyond. Legislative Cabinet members agreed that many of the disparities outlined in the report have been brought into stark relief over the past six weeks, making the need to address them even more pressing.
Special Help with NCMS Telehealth Benefit
As announced earlier this month, the NCMS is offering Presence, a telemedicine platform, to all health care providers in the state at no charge until the COVID-19 pandemic abates. To help remove any barriers to signing up for this valuable tool, experts will be available tomorrow and Thursday at three convenient times to help walk you through the onboarding process. You just need to have your NPI number and an internet connection available in order to complete the process.
Tomorrow and Thursday, help will be available at 7:30 a.m., noon and 5:30 p.m. to accommodate your schedule. Access help at each time by calling or clicking on the appropriate link below. Watch tomorrow's NCMS Morning Rounds for access information for Thursday's sessions.
Wednesday, April 15 at 7:30 a.m.
Join Zoom Meeting: https://therecoveryplatform.zoom.us/j/92993467952
Meeting ID: 929 9346 7952
One tap mobile +16465588656,,92993467952# US (New York)
Wednesday, April 15 at noon
Join Zoom Meeting https://therecoveryplatform.zoom.us/j/96280402133
Meeting ID: 962 8040 2133
One tap mobile +16465588656,,96280402133# US (New York)
Wednesday, April 15 at 5:30 p.m.
Join Zoom Meeting https://therecoveryplatform.zoom.us/j/97240344510
Meeting ID: 972 4034 4510
One tap mobile +16465588656,,97240344510# US (New York)
Presence offers a central portal where patients can schedule a telemedicine visit, look up a physician or PA by practice or name and be given a calendar with times the physician or PA has reserved for telemedicine or phone based appointments. You will receive a notification of scheduled visits and access the Presence dashboard to initiate and manage these patient interactions.
NCPHP Is Here to Help
We are living in truly extraordinary times. The challenge for all of us to be at our best has never been stronger and the communities we serve depend on it.
The North Carolina Professionals Health Program (NCPHP) is here to help medical workers and professionals facing unprecedented challenges and stressors in their workplace due to COVID-19. To this end, NCPHP stands ready to assist NCMS members in facing any of these difficulties.
NCPHP staff is on-call 24 hours a day, 7 days a week, 365 days a year. The office remains open Monday through Friday, 8 a.m. to 5 p.m. and can be reached by calling 919-870-4480. Staff is available to assist any medical professionals in need of help. You may also call after work hours or on the weekend (919-870-4480), and will be automatically routed to a person on-call who can help you access the needed assistance.
None of us were prepared for the current challenges we are facing with a worldwide pandemic. NCPHP is prepared, however, to help anyone get the help they need. It's crucial now more than ever.
In the News
Will an Antibody Test Allow Us to Go Back to School or Work?, The New York Times, 4-10-20
Learning Opportunity
In partnership with the NC Psychiatric Association, this week’s NCMS Foundation‘s ‘Power Hour’ will focus on the psychiatric impacts of the COVID-19 pandemic on the health care community and will be held Friday, April 17 from 1 to 2 p.m. The guest moderator for the discussion will be Harold Kudler, MD, Adjunct Associate Professor in the Department of Psychiatry and Behavioral Sciences at Duke University School of Medicine. Register here.
NCGA House COVID-19 Health Committee
 The North Carolina General Assembly House COVID-19 Health Committee met on April 9, 2019.
The North Carolina General Assembly House COVID-19 Health Committee met on April 9, 2019.
Impact of COVID-19 on Child Care Providers
Donna White, Interim President of Smart Start provided a child care provider perspective to the Committee.
According to the presentation, North Carolina is experiencing widespread closures of child care centers. Most centers are operating at less than 60% capacity.
In order to provide childcare to essential health workers, these centers are asking for cleaning supplies, thermometers, and personal protection equipment. Additionally, they believe direct grants to cover operating costs and funding to recover lost revenue could help keep centers open after COVID-19.
Impact of COVID-19 on Aging Population/Services
Mary Bethel, NC Coalition on Aging Board Member, provided the committee an overview of the challenges for older adults and their provider networks relating to COVID-19.
She added that more than 1 in 5 North Carolinians are over the age of 60. In 2018, 80 NC counties had more people 60 and over than under 18.
Many older adults in North Carolina have chronic conditions which puts them in a higher risk category for COVID-19.
Of the deaths contributed to COVID-19 in North Carolina, 80% were individuals 65+ years and older.
Specifically, concerns were voiced about the increasing reports of scams and fraudulent activities targeted to older adults since the onset of the pandemic. Concern was also expressed for the need for more PPE and the availability of tests.
Impact of COVID-19 on EMS/First Responders
William Kehler, Director of the McDowell County Emergency Services, provided an overview of the front line EMS workers during this pandemic.
He thanked the NCGA for their commitment to funding the community paramedic telehealth pilot programs. Currently, community paramedics are doing welfare checks on older county citizens and are able to provide telehealth services to the community.
Kehler added that flexibility around requiring two paramedics to be in a emergency vehicle at all times has allowed the use of experienced drivers who may not be paramedics to drive while a paramedic provides care to a patient.
He emphasized the importance of child care services to the first responder community.
McDowell County has also partnered with local businesses to obtain more PPE supplies.
NCMS Morning Rounds 4-13-20
It's Monday and time for your
NCMS Morning Rounds.
April 13, 2020
The COVID-19 Surveillance Network Needs You!
In order to show the effectiveness of the Governor’s Stay-at-Home order, the NC Department of Health and Human Services (NCDHHS) Division of Public Health will need to be able to demonstrate the COVID-19 virus is not widely circulating. The Department is using its influenza surveillance strategy or Influenza-Like Illness Network (ILINet) as the most reasonable way to determine the virus’ spread. If you are in a medium to large primary care clinic or urgent care center and currently seeing patients, please consider joining this surveillance effort. There is particular need in Wake and Mecklenburg counties.
New ILINet providers will be asked to collect samples from patients to send to the State Laboratory of Public Health (SLPH) for influenza and SARS-CoV-2 testing. Samples would need to be collected from up to 10 patients with an influenza-like illness (fever >100F and cough or sore throat) and from 10 patients who do not meet influenza-like illness criteria (e.g. patients being seen for other reasons such as well child visits, chronic disease follow-up visits, non-respiratory illnesses, etc) each week. Swabs, shipping boxes and shipping labels are provided by SLPH.
All swabs will be tested for influenza and SARS-CoV-2. Please note that these samples are for surveillance purposes and have a longer turnaround time than samples sent to SLPH for diagnostic purposes. In situations where the result would change patient management, ILINet swabs should not be used and diagnostic testing should be ordered.
If your clinic can assist with this critical COVID-19 surveillance, please go to this webpage and fill out the ILINet provider application at the bottom of the page. For any questions, please contact Anita Valiani at [email protected] or Erica Wilson at [email protected].
NC Medical Board Acts to Help State's COVID-19 Response
During a special meeting on Thursday, April 9, the North Carolina Medical Board (NCMB) took additional actions to ease some licensure requirements for PAs and nurse practitioners, who are jointly regulated with the North Carolina Board of Nursing. The NCMB also extended the term of Limited Emergency Licenses, which are used by out-of-state and recently inactive clinicians to practice in North Carolina during a state of emergency, and approved a provision that will allow NCMB to be more nimble in response to Gov. Cooper’s Executive Order #130. These and other actions provide flexibility to practices and health systems across the state addressing the COVID-19 pandemic.
The Board’s actions include:
- Extending the expiration date of Limited Emergency Licenses to 30 days after the state of emergency is lifted.
- Approved an order allowing new PA graduates who have not taken the required PANCE testing to be issued a temporary license. The license will be valid for up to six months and will allow a PA to practice under the supervision of an on-site physician.
- Approved several provisions related to Nurse Practitioners (NP) that mirror provisions approved for PAs. The North Carolina Board of Nursing (NCBON) is expected to approve the same orders, which are effective only during the current declared state of emergency. These provisions include:
o Restrict prescribing of chloroquine, azithromycin and other medications to ensure that these drugs are available to patients who need them. The rule was requested by NC Department of Health and Human Services (NCDHHS) Secretary Mandy Cohen, MD, MPH, to reduce the occurrence of reported stockpiling or inappropriate prescribing of these medications.
o Permit NPs who have inactivated professional licenses within the last two years to quickly reinstate their licenses. The temporary license will be jointly approved by NCBON and NCMB and will expire on August 1, 2020.
o Allow recent NP graduates who have not taken the required testing to be issued a temporary license. The license will be valid for up to six months and will allow an NP to practice under the supervision of an on-site physician.
o Allow NPs to be temporarily reassigned to a new practice area within the same facility to meet a critical need without formally notifying NCBON of the new practice setting. NPs can only be reassigned to perform medical tasks they are trained and competent to do and must have reasonable access to a physician should a medical need arise. The NP must meet all other requirements, including conferring at least monthly with a physician to ensure meaningful supervision and quality assurance within the new practice setting.
- Gov. Cooper’s order includes a requirement that physicians and PAs who are licensed in other states and want to work or are currently working in North Carolina to seek authorization from NCMB. Out-of-state physicians and PAs should apply here for a Limited Emergency License.
The NCMB is working in partnership with many stakeholders and working quickly to identify opportunities to support the state’s response to the COVID-19 pandemic. Learn more at the NCMB’s COVID-19 webpage.
NCMS’ Dr. Karen Smith Reflects on Impact of COVID-19
Longtime NCMS member and leader Karen Smith, MD, recently shared her reflections on the impact the current COVID-19 pandemic is having on patients at her family medicine practice in Raeford and reiterating the importance of social distancing in the community’s newspaper the News-Journal.
“I ask people to please, please be patient. Be patient. We recognize and appreciate that every individual is of value, but be patient with your doctors, nurses, hospitals, be patient with your family,” Smith says in the article. “Please don’t push back but accept that life is not what it was in January, and if we are to get through this with as little loss of life as possible, follow the guidance, follow the recommendations. They are to preserve the life of the entire community and also to preserve our life.”
In the News
Thousands of Coronavirus Tests are Going Unused in US Labs, Nature, 4-9-20
Learning Opportunity
The next NCMS Foundation and NC Medical Group Management Association Lunch & Learn Webinar on Tuesday, April 21 from noon to 1 p.m. will focus on NC Medicaid Response to COVID-19: The State of Things and will feature Shannon Dowler, MD, FAAFP, CPE, chief medical officer for NC Medicaid. Learn more and register.
NCMS Morning Rounds 4-10-20
Happy Friday!
Enjoy your NCMS Morning Rounds.
April 10, 2020
Child Care Resources for Essential Workers
The North Carolina Department of Health and Human Services (NCDHHS) and the Child Care Resource and Referral Network wants to ensure that all essential workers have safe care for their children and want to make sure the cost of care isn’t a barrier, so they are offering financial assistance to families with need.
Essential workers include:
• emergency and first responders,
• hospital staff and front-line health care providers,
• nursing and adult group home staff,
• child care program staff,
• food service staff,
• and others working to keep our communities safe and healthy as we respond to COVID-19.
They are also prioritizing emergency care for children who receive child welfare services, are homeless, or are in unstable or unsafe living arrangements.
To help essential workers access these child care services, there is a hotline – 1-888-600-1685. Since the hotline was set up on March 24, more than 1,400 children have been connected to care so their parents can report to work. These flyers in English and Spanish also can be downloaded and distributed to spread the word about emergency child care options for essential workers.
Helping Smokers Quit – Now More than Ever
With the spread of COVID-19, a virus that impacts the lungs, now is an important time to encourage your patients who smoke to quit. Here are several resources to help you help them.
The University of North Carolina School of Medicine’s Department of Family Medicine recently issued a news release highlighting the fact that people with any underlying lung condition, including people who smoke, have much higher rates of death if they become infected with COVID-19. Smoking weakens an individual’s lung function, and because of the way COVID-19 attacks the lungs, this increases a smoker’s risk of dying from serious respiratory infection from the virus. Read the release.
Physicians and PAs can promote QuitlineNC to people who want to quit smoking or vaping to reduce their risk. Have them visit www.quitlinenc.com or call 1-800-Quit-Now (1-800-784-8669).
CATCH My Breath, part of the Coordinated Approach to Child Health (CATCH) launched a new resource on vaping and lung health, which is useful for parents on how to speak with children about vaping and how it compromises lung health and immunity. Access the resources here.
Creative Med Students Offer Kids Educational Fun
Two North Carolina medical students, Logan Beyer and Emily Kragel, have used their current downtime to put their knowledge and creativity to use by creating ‘Coloring for COVID-19.’ The series of coloring books for kids seeks to “provide a fun activity for kids, and to hopefully ease some fear and anxiety regarding our current situation,” they say.
There is a book for each age group starting at five and up to 10-years-old and teaches age appropriate lessons about preventing spread of the virus. Learn more at the Coloring for COVID-19 website.
Beyer and Kragel were featured recently in a report on WRAL. Watch the broadcast.
In the News
The Best Hopes for a Coronavirus Drug, The Atlantic, 4-8-20
Learning Opportunity
A live conversation on the coronavirus with former director of the Centers for Disease Control and Prevention (CDC) and commissioner of the New York City Health Department, Tom Frieden, MD, MPH, will be held on Monday, April 13 beginning at 11 a.m. Dr. Frieden, who is now president and CEO of the global public health initiative Resolve to Save Lives, will speak about the state of the pandemic and how both the country and the world can move beyond it. Learn more and register for this free live chat. You may submit questions beforehand at [email protected].
NCMS Political Pulse for April 10, 2020
NCMS Morning Rounds 4-9-20
Time for your Thursday NCMS Morning Rounds.
April 9, 2020
NCMS’ Easy Reference Guide to Telehealth Policies During COVID-19
NCMS Director for Health System Innovation Kristen Spaduzzi has developed a guide to the various insurers’ telehealth policies during the COVID-19 pandemic. You can access this easy reference grid, here and on the NCMS’ COVID-19 webpage under the telehealth heading.
This comprehensive guide covers commercial payers and Medicare Advantage plans, listing answers to the commonly asked questions about reimbursement parity, coding, virtual visit check-ins and others in an easy to use grid format.
Get similar information about Medicaid telehealth policies during the pandemic here.
Reminder: the NCMS has resources and information to help you in many ways during this pandemic. Visit our COVID-19 page to get information on telehealth, the latest clinical guidance from the NC Department of Health and Human Services (NCDHHS) and the Centers for Disease Control and Prevention (CDC) and general resources to help during the pandemic. Our Economic Relief Resources page includes how to get paid for your work today as well as financial relief programs to help offset the impact of COVID-19. Our Emotional Supports page offers just that – resources to protect your mental health and help support you emotionally.
Wake County Seeking Volunteers for Auxiliary Hospital
Wake County is currently working to set up an auxiliary hospital for the potential surge of need in the coming weeks and is looking for volunteers to staff the hospital. The anticipated go-live date is the week of April 20th. The hospital will be in operation for approximately 6-8 weeks.
If you are interested, please call the Donations & Volunteer task team at 919-856-6946, Monday to Sunday between 8 am to 8 pm or through email at [email protected]
NC MedAssist Supports Vulnerable Populations
NC MedAssist, founded by NCMS leaders in Mecklenburg County back in 1997, is continuing its mission to provide access to both over the counter and prescription medication for vulnerable and uninsured patients during this pandemic. Learn more about NC MedAssist and how it is helping now.
Watch this video to see several volunteers in action.
In the News
Viewpoint: Coronavirus Shows Us the Time to Decide on End of Life Care is When You’re Not Sick, NBC News, 4-8-20
Learning Opportunity
This evening, Thursday, April 9, from 5 to 6 p.m. the Centers for Medicare and Medicaid Services (CMS) will hold ‘Office Hours’ to answer your questions about CMS’s response to COVID-19. Areas to be covered include:
- Increase Hospital Capacity – CMS Hospitals Without Walls;
• Rapidly Expand the Healthcare Workforce;
• Put Patients Over Paperwork; and
• Further Promote Telehealth in Medicare
You may submit questions in advance to [email protected], including “Office Hours” in the subject line. There will also be live Q&A.
Conference lines are limited, so they highly encourage you to join via audio webcast, either on your computer or smartphone web browser.
Toll-Free Attendee Dial In: 833-614-0820
Event Plus Passcode: 1881716
Audio Webcast link
NCMS Morning Rounds 4-8-20
Recognizing Public Health Week in today's
NCMS Morning Rounds.
April 8, 2020
It’s National Public Health Week at a time when preserving the public’s health has never been more in the spotlight! A special THANK YOU to all public health professionals during this unprecedented crisis.
NCMS Pushes State for Adequate PPE Supplies
Yesterday, in follow-up to the NCMS member call with Governor Cooper on Monday evening, NCMS Executive Vice President and CEO Robert W. Seligson, MBA, MA, and leaders of several medical specialty groups and county medical societies strongly re-iterated the need for personal protective equipment (PPE) in a conversation with NC Department of Health and Human Services Secretary Mandy Cohen, MD, MPH and State Health Director Elizabeth Cuervo Tilson, MD, MPH.
Seligson together with Executive Vice President of the NC Academy of Family Physicians Greg Griggs, MPA and Executive Director of the NC Pediatric Society Elizabeth Hudgins, MPP expressed serious concerns over the lack of PPE and the negative impact it is having on physician practices throughout North Carolina. They asked state officials to procure the needed equipment rapidly to fulfill the current day-to-day needs of practices as well as in anticipation of a surge in COVID-19 cases that could overwhelm hospital capacity.
The NCMS will continue to work with the state, our partner health care societies and other entities to exhaust every avenue to secure PPE for North Carolina physicians.
Review Your Financial Options
On Monday two experts from the NCMS’ partner Smith Anderson held a call to review the various financial options available to you and your practice. We recorded the call so you can tap into the information provided. Listen here.
Robert Shaw, chair of Smith Anderson's health care practice, and Peter Bosman, a partner in Smith Anderson’s Private Equity group, reviewed the menu of financial options provided thus far by the federal government and offered some strategic considerations as you may weigh the various programs. Topics covered in the hour-long call, in the following order, included:
- An overview of the CARES Act and its two provisions of most interest to small businesses, the Paycheck Protection Program and the Economic Injury Disaster Loan Program (EIDL).
• Payroll tax credits.
• Medicare accelerated or advance payments and what private insurers are doing in this area. They also discussed the NC Department of Insurance and their ‘strongly worded encouragement’ to insurers to defer premium payment requirements to help ensure there is no lapse in coverage for beneficiaries.
• The distinctions between permanent and temporary layoffs of staff and furloughs.
• Obligations if you need to close your practice.
• The Family First Act and its provisions.
Shaw and Bosman also answered questions submitted before the call. If you have a follow up question, you may email it to [email protected]. Watch for details on future calls to address other financial topics of concern to NCMS members as you respond to the economic impact of the COVID-19 pandemic.
NCMS Joins in Urging Azar to Provide Financial Assistance to Physicians/PAs
The NCMS has signed on to a letter calling on US Health and Human Services Secretary Alex Azar to provide immediate financial assistance to physicians and PAs who are on the frontlines in responding to the COVID-19 pandemic.
The letter recommends that “HHS provide immediate relief to ensure a sufficient physician workforce is available in this country now and throughout the pandemic. Specifically, we urge HHS to provide one month of revenue to each physician (MD or DO), nurse practitioner, and physician assistant enrolled in Medicare or Medicaid to account for financial losses and non-reimbursable expenses.” It goes on to outline exactly how to arrive at the amount and the mechanism by which to provide the reimbursement through the CARES Act.
In the News
Dispatch from a Country Doctor: Seeing Patients Differently in the Time of Coronavirus, Kaiser Health News, 4-7-20
Learning/Well-being Opportunity
In response to the COVID-19 pandemic, Stanford Wellness is offering their ‘Fireside Chat’ series free. These 30-minute conversations offer strategies for coping and improving emotional health during crises with national experts, including Bryan Sexton, PhD, from Duke University.
To help maintain your well-being during this stressful period, access the fireside chat series below [this information is also posted on the NCMS’ Emotional Support resource page]:
- Thursday, April 9 from 12:30 – 1 PM with Vic Strecher, PhD REGISTER HERE
• Tuesday, April 14 from 12:30 – 1PM with Kim Cameron, PhD REGISTER HERE
• Thursday, April 16 from 12:30 – 1 PM with Al’ai Alvarez, MD, REGISTER HERE
• Wednesday, April 22 from 12:30 – 1 PM with Robert Emmons, PhD REGISTER HERE
• Tuesday, April 28 from 12:30 – 1PM with J.Bryan Sexton, PhD REGISTER HERE
NCMS Political Pulse Video for April 3, 2020
NCMS Senior VP for Advocacy and Advancement Chip Baggett, JD, describes what our legislative relations staff has been working on this week around personal protective equipment (PPE) procurement; understanding what the CARES Act may mean for your practice and generally making sure legislators and policymakers understand your challenges in responding to the COVID-19 pandemic.
NCMS Morning Rounds 4-3-20
It's Friday and time for your
NCMS Morning Rounds
April 3, 2020
Our message to all who pass our NCMS headquarters:
Reminder: If you would like to volunteer as a medical professional to help when and where needed in response to the COVID-19 pandemic, the state has an online platform where you can sign up. The state will deploy medical volunteers as needed. Learn more and sign up here.
We apologize for the technical difficulties on the call with Governor Roy Cooper yesterday. They were outside of our control. We are working to reschedule a conversation with the Governor in the near future in which all phones will be muted. Watch your email and your NCMS Morning Rounds for details.
Results from Sunday Survey #5 – Help During COVID-19
Thank you to everyone who shared your perspective on what is needed most in response to the COVID-19 pandemic by responding to this week’s NCMS Sunday Survey. The biggest need based on these results show personal protective equipment (PPE) is the top priority among NCMS members right now.
Respondents were asked to select the one priority that is most important to their practice now and in the immediate future. Here are the results:
NC Medical Board Actions in Response to COVID-19
Below is a summary of actions taken by the North Carolina Medical Board (NCMB) to remove barriers and support physicians, physician assistants and the state's health care system in response to the COVID-19 pandemic.
- Approved a new type of emergency licensure to bring recently inactivated licensees back to the work force during the state of emergency. NCMB now has two types of free and quick emergency licensure available:
*Retired or inactive licensure – allows physicians and PAs with a recently inactive NC license to return to service during a state of emergency; must have been inactivated within the last two years.
*Limited Emergency Licensure – allows out-of-state physicians and PAs to volunteer or work in North Carolina during a state of emergency. Examples include: telemedicine or providers coming from other states.
Go to the NCMB’s emergency licensure resource page for more information.
- Temporarily suspended background checks for license applications due to lack of availability of fingerprinting services, which is a key element to conducting a background check. NCMB can access secondary sources to provide this information. Applicants who were granted a license without a background check will be required to complete this process once fingerprinting services resume.
- Adopted rules requested by NC Department of Health and Human Services (NCDHHS) Secretary Mandy Cohen, MD, MPH, to reduce the occurrence of reported stockpiling or inappropriate prescribing of chloroquine, azithromycin and other medications, and ensure that these drugs are available to patients who need them. The rule restricts the use of these drugs as a preventative medication for COVID-19 but does not ban prescribing these medications for treatment of a patient diagnosed with the illness.
- Approved an order to postpone USMLE and COMLEX–USA Step/Level 2 testing requirements for medical students prior to beginning a residency program. This will allow medical students who have otherwise completed the requirements to graduate from medical school and been accepted into a North Carolina residency training program to start their residency, which will almost certainly include assisting in battling the COVID-19 pandemic.
- Approved an order to allow Fellows with a Resident Training License (RTL) to apply for a Limited Emergency License, which provides a temporary unrestricted and full medical license during the declared state of emergency. This action will allow several hundred physicians with proven competence in a primary specialty to take care of patients and ease the potential strain on physicians currently in the health care system.
- Approved an order to allow hospitals, health systems, or multi-specialty group practices to temporarily reassign a physician assistant to a new practice area to meet a critical need without formally notifying NCMB of the new supervisory arrangements. The supervising physician and facility administration should ensure the physician assistant:
*Is reassigned to perform only those medical tasks for which they are competent and qualified to do;
*Has reasonable and immediate access to a physician, either in person or electronically, should medical issues arise;
*Complies with all applicable rules including the requirement to confer at least monthly with a physician to ensure meaningful supervision and quality assurance within the new practice setting.
Visit the NCMB’s COVID-19 page for more information, FAQs and resources.
In the News
Listen: Why It Takes So Long to Get COVID-19 Test Results, Kaiser Health News, 4-1-20
Learning Opportunity
Monday, April 6 from 1 to 2 p.m. Blue Cross and Blue Shield of NC will offer another "Virtual Rounds" with special guest Chief of Behavioral Health Dr. Kate Hobbs Knutson to answer your questions on how to apply the insurer’s expanded telehealth measures to behavioral health services. Sign up on our registration form.
Also, the Centers for Medicare and Medicaid Services (CMS) has been hosting regular calls with a variety of clinicians, hospitals, other facilities and states in an effort to keep stakeholders updated on its COVID-19 efforts. Since not everyone is available to attend the calls live, they have shared access to recordings of the calls along with transcripts here.
NCGA House Health Care COVID-19 Committee
 The NCGA House Health Care COVID-19 Committee met on April 2, 2020.
The NCGA House Health Care COVID-19 Committee met on April 2, 2020.
Listen to the full audio recording of the meeting here. Public input can be provided to the Committee here.
Federal Law Impact Summary for Health and Human Services
Deborah Landry, from the NC General Assembly Staff provided the Committee a detailed federal law summary for legislation passed relating to health and human services.
Department of Health and Human Services
Dr. Mandy Cohen, MD, Secretary of the Department of Health and Human Services provided the group with timely information on the status of coronavirus in NC. Currently, coronavirus is located in 79 of 1oo NC counties with ~1,584 cases, ~204 hospitalizations, and ~9 deaths.
She noted that the federal administration has indicated that supplies are limited. However, DHHS is aggressively looking for sources for critical PPE and ventilators.
Food & Nutrition Programs
NCDHHS received waivers to increase access to food and decrease administrative burdens during this pandemic. Parents are now allowed to have meals delivered or pick up meals for children needing food assistance.
Social Services
NCDHHS relaxed requirements for some face to face interactions for child welfare beneficiaries.
Requests are pending to suspend work requirements for TANF benefits for families who cannot work because of the COVID-19 pandemic.
High Risk Populations and Access to Care
There has been an increase in Medicaid rates by 5% for long term care providers, and a 1.5% increase in Medicaid rates for LME/MCOs.
Hospitals are now able to request a 60 day waiver to limiting their number of licensed beds.
Budget Needs
Secretary Cohen noted that DHHS hopes to maximize federal dollars to the greatest extent possible.
The five areas for budget consideration include:
- Testing and Treatment for Individuals
- Critical Health Care Infrastructure and Support
- Mental Health and Crisis Services
- Food and Shelter Security
- Planning and Support for Recovery
Public Health Department Overview
Gibbie Harris, MSPH, BSN, Mecklenburg County Public Health Director and Dr. Marilyn Pearson, MD, Johnston County Public Health Director provided an urban and rural health department perspective on coronavirus.
Both Directors indicated that their biggest challenge was obtaining personal protection equipment.
North Carolina Nurses Association
Tina Gordon, MPA, CEO of the NCNA, and Dr. Dennis Taylor, DNP, PhD, President of the NCNA indicated that their members on the front lines were concerned about the following:
- Lack of PPE
- Childcare
- Safety
- Bed availability
- Equipment availability
- Workforce
Both presenters encouraged the NCGA to aggressively encourage their constituents to support stay at home orders.
NCMS Morning Rounds 4-2-20
Here is your Thursday
NCMS Morning Rounds
April 2, 2020
Don't forget our first 'Power Hour' will be held tomorrow.
More information is available in the Learning Opportunity section below.
NCMS Launches Telehealth Platform – At No Charge to You
In response to the COVID-19 pandemic and in an effort to ease the burden on North Carolina’s physicians and patients, the NCMS today is launching a telemedicine platform available to all health care providers in North Carolina at no charge, until the COVID-19 pandemic abates. This custom platform, called Presence, was produced in a collaboration between the NCMS Foundation’s Project OBOT NC and The Recovery Platform.
The Presence platform provides a central portal where patients can schedule a telemedicine visit with their provider. In fact, patients can look up their provider by practice or provider name and are given a calendar with times the physician has reserved for telemedicine or phone based appointments. Physicians will receive a notification of scheduled visits and access the Presence dashboard to initiate and manage these patient interactions.
To setup your account you simply need to:
• Go to the onboarding page here.
• Activate your account to setup your Telemedicine Availability Schedule
• Login to the dashboard to see upcoming scheduled visits
• Initiate the patient visit
• Digitally order labs on the platform with our integrated partners
• Charting and billing are performed in your own EHR
After you receive confirmation your account is set-up you will be provided with instructions to:
• Sign the BAA
• Download Zoom at https://zoom.us/download
• Email patient roster (suggested language below)
Learn more about Presence and how you can access this valuable NCMS Foundation resource.
Respiratory Care Board Clarifies Policies on Telehealth
As part of its ongoing efforts to provide health care professionals with critical information during the national response to the COVID-19 virus, the North Carolina Respiratory Care Board wants to address any concerns about possible restrictions on respiratory care practitioners providing respiratory care via a telehealth platform.
Board Rule 21 NCAC 61 .0103 (3) states: "The practice of respiratory care" means the performance of assessments and diagnostic tests, and implementation of treatment procedures and protocols related to the cardiopulmonary system pursuant to G.S. 90-648(10) and the activities defined by the American Association of Respiratory Care (AARC) clinical guidelines. Review those guidelines here. Based on the AARC Position Statement, respiratory therapists may provide all of the following respiratory therapy services in a telehealth setting or platform:
- Patient assessment and education
• Diagnostic evaluation
• Sleep testing
• Home ventilator monitoring and management
• Monitoring patient health and activities
• Managing patients with chronic conditions
• Disease prevention
• Health promotion
• Rehabilitation
• Patient consultations
For these reasons, the North Carolina Respiratory Care Board wants to emphasize that each licensed respiratory care practitioner holding the appropriate competencies and acting under facility policy and procedure, and the written order of physician as outlined in Board Rule 21 NCAC 61 .0103 (3) may provide these services via telehealth.
NCMS Leadership Nominations Still Being Accepted
Here is some important, non-COVID-19 news: the NCMS Nominating and Leadership Development Committee is seeking nominations for openings on the NCMS Board of Directors, NC AMA Delegation and the Committee itself. You have until May 18 to nominate yourself or a colleague for one of these key leadership positions, listed below.
Here is the nomination form. This is a meaningful way to serve your profession and the health of North Carolinians, now more than ever!
Applications will be reviewed by the NCMS Nominating and Leadership Development Committee, with the final ballot being put to a vote of the entire NCMS membership later this year. Review descriptions of what is required of each position.
Board of Directors (Term runs from the NCMS’ Annual Meeting 2020, which will be held Oct. 15-16, to the Annual Meeting 2021):
• Secretary Treasurer: Incumbent (John J. Meier, IV, MD) is eligible for reelection
• Region 3 Representative: Open
• Region 4 Representative: Incumbent (Rachel D. Keever, MD) is eligible for reelection
• At-Large Member: Incumbent (Eileen M. Raynor, MD) is eligible for reelection
• At-Large Member: Open
NC AMA Delegation (Four delegate openings to serve January 2021 to December 2022)
• Incumbent (G. Hadley Callaway, MD) is eligible for reelection
• Incumbent (William E. Bowman, MD) is eligible for reelection
• Incumbent (Darlyne Menscer, MD) is eligible for reelection
• Incumbent (Liana Puscas, MD) is eligible for reelection
Alternate AMA Delegate (One delegate opening to serve January 2021 to December 2022)
• Incumbent (E. Rebecca Hayes, MD) is eligible for reelection
Nominating and Leadership Development Committee (Term runs from Annual Meeting 2020 to Annual Meeting 2022)
Region 1 (represents the eastern third of the state)
• Two open seats
Region 2 (represents 21 counties encompassing the Triangle and Triad)
• Incumbent (Justin Hurie, MD) eligible for reelection
Region 4 (represents the western third of the state)
• Incumbent (Gregory Evans, MD) eligible for reelection
Survey Reminders
Several surveys have gone out recently to help gather information about current conditions in your practice to help us understand them and to help. If you haven’t already responded, please take just a minute to complete these quick snapshots of your experience during this unique time.
- NCMS Sunday Survey (this will close at noon today)
• NCMS Prior Authorization Challenges (this will close Friday at noon)
• NCMS/Curi/NCMGMA Urgent Practice Data Survey (this will be sent weekly to gather data over time).
Thank you! And thank you for all you are doing for your patients and the community!
In the News
These Charts Show Who Is Most Vulnerable to the Coronavirus, The Center for Public Integrity/NPR, 4-1-20
Learning Opportunity
The NCMS Foundation presents its Kanof Institute for Physician Leadership (KIPL) Power Hour: Telemedicine During COVID-19, Friday, April 3 from noon to 1 p.m. Register here. The link to the Zoom meeting login will be sent after you register. If you don't receive the link, please contact Kristina Natt och Dag at [email protected].
Originally created as a way to reach patients remotely, telehealth needs during the COVID-19 pandemic have skyrocketed. Physician practices are working to get telehealth platforms set up and running so they can continue to see patients. This Power Hour is an opportunity to share knowledge and learn from each other about applying telehealth technology during this pandemic. Steve North, MD, a family physician and adolescent medicine specialist in Mitchell County, Reynold Yordy, who has 20 years of health care IT and programming experience and the NCMS' Vice President for Rural Health Systems Innovation Franklin Walker will lead the conversation.
The KIPL Power Hour aims to provide a forum for ongoing conversation, collaboration and community. Tune in to Power Hour weekly to hear from different experts, decision makers and influencers on a variety of topics. The format is informal and conversational and sessions are easy to access through Zoom. Power Hours will be recorded and made available to you through your NCMS Morning Rounds and on the KIPL webpage.
Economic Relief Resources
 Last week Congress passed and the president signed the Coronavirus Aid, Relief and Economic Security or CARES Act, a $2 trillion stimulus package, the largest in the nation’s history. Two programs funded by the CARES Act will help doctors and other small businesses meet payroll and fund their business operations during the COVID-19 pandemic. Below is some information to help explain those particular programs.
Last week Congress passed and the president signed the Coronavirus Aid, Relief and Economic Security or CARES Act, a $2 trillion stimulus package, the largest in the nation’s history. Two programs funded by the CARES Act will help doctors and other small businesses meet payroll and fund their business operations during the COVID-19 pandemic. Below is some information to help explain those particular programs.
The Small Business Administration’s (SBA) new Paycheck Protection Program received $350 billion under the CARES Act. Documents from the National Association of Government Guaranteed Lenders (NAGGL), show that this will include forgiveness of the first six month’s loan payments, including principal, interest and fees. This document prepared by the US Chamber of Commerce summarizes the program, which has not yet begun. Now is the time, however, to familiarize yourself with the program if you think it may be helpful. The loans will be made through local lenders in conjunction with the SBA. Read the Chamber’s summary of the program.
The SBA’s Economic Injury Disaster Loan Program received $10 billion under the CARES Act. These loans are available directly from the SBA. Learn more in this SBA presentation.
The AMA has compiled a summary of the CARES Act highlighting the portions that pertain to health care practices, physicians and PAs and medical students. Read the AMA’s summary document.
The NCMS’ local partner, Smith Anderson, also offers this summary and listing of what’s available in the CARES Act. Read their summary.
The NCMS continues to analyze the CARES Act and its impact on medical practices and personnel. Watch your NCMS Morning Rounds for more information on economic relief for your practice as well as announcement of a new webpage where all the pertinent information will be gathered for your easy reference now and in the future.
Please feel free to comment on this post with your input or questions and we will try to provide answers.
NCMS Morning Rounds 4-1-20
No foolin' -- here's your Wednesday
NCMS Morning Rounds
April 1, 2020
NC Medical Board Eases Some Requirements in Response to COVID-19
The North Carolina Medical Board (NCMB) held an emergency meeting last Friday during which they took several actions to support the state’s response to the COVID-19 pandemic.
Specific actions include:
- Adopted rules requested by NC Department of Health and Human Services (NCDHHS) Secretary Mandy Cohen, MD, MPH, to reduce the occurrence of reported stockpiling or inappropriate prescribing of chloroquine, azithromycin and other medications, and ensure that these drugs are available to patients who need them.
- Approved an order to postpone USMLE and COMLEX–USA Step/Level 2 testing requirements for medical students prior to beginning a residency program. This will allow medical students who have otherwise completed the requirements to graduate from medical school and been accepted into a North Carolina residency training program to start their residency, which will almost certainly include assisting in battling the COVID-19 pandemic.
- Approved an order to allow hospitals, health systems, or multi-specialty group practices to temporarily reassign a PA to a new practice area to meet a critical need without formally notifying the NCMB of the new supervisory arrangements. The supervising physician and facility administration should ensure the physician assistant:
o Is reassigned to perform only those medical tasks for which they are competent and qualified to do;
o Has reasonable and immediate access to a physician, either in person or electronically, should medical issues arise;
o Should comply with all applicable rules including the requirement to confer at least monthly with a physician to ensure meaningful supervision and quality assurance within the new practice setting. - Approved an order to allow Fellows with a Resident Training License (RTL) to apply for a Limited Emergency License, which provides a temporary unrestricted and full medical license during the declared state of emergency. This action will allow several hundred physicians with proven competence in a primary specialty to take care of patients and ease the potential strain on physicians currently in the health care system.
These actions seek to support Gov. Cooper’s call to increase the supply of qualified medical professionals available to help during this pandemic. In addition to the above, the NCMB offers two different emergency temporary license applications to facilitate quickly getting physicians and PAs to work. There are no fees and typically licenses are issued within 48 business hours. Learn more about those licenses and other steps NCMB has taken to address the COVID-19 crisis at www.ncmedboard.org/covid.
NCMS Hosts ‘Power Hours’ Starting Friday
As COVID-19 continues to spread, and we are all full of uncertainty and trying to adjust to a different reality, the NCMS wants to help you any way we can. We know that conversation, collaboration and community are crucial right now. To bolster those crucial values, the NCMS Foundation and its Kanof Institute for Physician Leadership (KIPL) will offer weekly ‘Power Hour’ forums starting this Friday. These virtual gatherings will allow you to hear from different experts, decision makers and influencers on a variety of topics that are likely top of mind for you right now.
Our aim is to provide a community conversation around a range of important issues. You will be able to hear from all participants and share your thoughts and ideas in addition to your questions. The format is informal, conversational and the sessions will be easy to access through Zoom. The sessions will be recorded and made available on the KIPL home page. The first Power Hour will be this Friday, April 3 at noon. Mark your calendar and find the topic and link to join this week’s conversation in tomorrow’s NCMS Morning Rounds.
As the health care leaders on the frontlines in this crisis, we are so grateful for all the work you are doing under very challenging circumstances. We hope our Power Hours will offer you a chance to step away for a moment, to learn and to reflect on the important role you play every day on behalf of your patients and the larger community.
The Medical Student Perspective on COVID-19
This perspective piece was written by Austin Lucke, Diana Dayal and Edward Diaz,
three medical students at the University of North Carolina School of Medicine, who are involved with the NCMS student council and sit on several of our committees. The essay gives some insight into what medical students are thinking about the upheaval wrought by COVID-19.
This spring, we and our classmates were set to begin our fourth and final year of medical school. This was supposed to be a glorious final year before starting our careers in our respective residency programs, but in a matter of weeks, our schedules have been completely turned upside down because of COVID-19. While changes for pre-clinical medical students have been analogous to most other graduate and undergraduate students, changes for medical students in the clinical phase have been quite disruptive. Lectures are easy to digitize. Learning assignments can be done on the couch next to your dog. However, clinical learning is difficult to do remotely. To learn to care for patients, we have to learn by being in the hospital. We must learn to face disease and death in person – not through a computer. So many of our most formative medical experiences occur when the situation is the most frantic, most tense and most dire.
Despite this, our clinical rotations are currently on hold. We have been told that we will return at the beginning of April, as are the majority of medical students around the country. UNC School of Medicine’s administration has worked tirelessly to ensure transparency and communication with students, as they too want medical students back in the hospital as soon as possible. We all know that medical students, even as trainees, can play a pivotal role in patient care. Yet, as of now, shortages of personal protective equipment (PPE) are currently limiting student access to clinical duties.
This puts us in a precarious position. Our medical system—already chronically underfunded, understaffed and stretched thin—is about to be pressured in a historic way by COVID-19. Every hand will be needed in the coming weeks. We’re witnessing this grim reality play out in countries across the globe that are in the throes of this pandemic. Italy has fast-tracked many of its senior medical students to become practicing doctors to respond to the urgent need for health care workers. It’s not unreasonable to predict the United States may soon be in a similar situation. All health care providers, not just doctors, will be working at maximum capacity. We know that we are needed in this unprecedented moment in history.
As formal clinical rotations have been suspended due to the PPE shortage, we have been seeking opportunities to be a part of the COVID-19 response. We have been absolutely amazed by the creativity and passion of our colleagues and friends in the UNC medical student community. Over the course of two days, a team of over 100 students across the state have launched projects to support frontline healthcare workers in the weeks to come. Our student-led task force has developed countless initiatives and has compiled a database of local volunteer opportunities.
We are preparing to reinforce the emergency department’s COVID-19 protective equipment protocols to keep doctors, nurses and other patients safe from exposure. In the face of dangerous shortages, we are literally making protective face shields from scratch. We have a long list of volunteers who are ready to provide free childcare services for all the healthcare workers who desperately need it. We are incredibly proud to go to a school surrounded by peers who choose to run towards a crisis instead of away from it. Moreover, we are inspired by medical schools around the country putting forth similar efforts. Now more than ever, we are proud to be in the field of medicine, and remain hopeful in this strange time.
If you're a medical student and would like to get involved, please contact Austin Lucke at [email protected].
In the News
As Coronavirus Impact Grows, Volunteer Network Tries to Help Health Care Workers Who Have ‘Helped Us,’ STAT, 3-31-20
Learning Opportunity
Here is a question arising out of the COVID-19 situation with an answer from the NC Medical Board’s Chief Medical Officer Karen Burke-Haynes, MD.
Q: My student patients have returned to their home states. Is it legal for me to conduct assessments via telemedicine and prescribe to them?
A: Most medical boards require a physician or PA to be licensed in the state in which the patient care is given. Each state has different laws and rules regarding licensure, telemedicine and prescribing. Some of these restrictions may be lifted during a state of emergency, but you would need to contact the corresponding medical licensing authority of that state to determine its individual requirements.
In North Carolina, patients who are currently in the state but have an established relationship with a physician or PA in another state may receive care, including prescriptions, from the out-of-state clinician via telemedicine.
This Federation of State Medical Boards (FSMB) resource summarizes each states’ emergency policy.
NC Medical Society COVID-19 Member Feedback to Legislators
The North Carolina Medical Society is actively working to solicit feedback on challenges our members are experiencing during the COVID-19 pandemic. Our two physician legislators, Dr. Perrin Jones (R-Pitt) and Dr. Kristin Baker (R-Cabarrus) have specifically asked NCMS to set up an avenue for NCMS members to express concerns and issues you are experiencing.
Please use the comment function on this post to provide information that may be helpful for our elected physician leaders to be aware of as they make legislative decisions moving forward. Be sure to include your name, specialty, and email address in your post in order for us to provide follow up contact if needed.
AMA Summary of the CARES Act
AMA Summary of Selected Provisions in H.R. 748 CARES Act 3-30-20
*This summary was provided by the American Medical Association.
CARES Act Summary from Smith Anderson
*The following summary of the CARES Act is provided by NCMS outside counsel, Smith Anderson.
The Coronavirus Aid, Relief, and Economic Security Act (the “CARES Act” or the “Act”), which the Senate approved on the evening of March 25th, received House approval and was signed by the President into law. The Act will inject up to $2 trillion into the US economy, an historic legislative package that far exceeds the 2009 stimulus legislation adopted during the Great Recession.
The Act is 880 pages long and its application is far-reaching and, in many ways, currently unknown. The following is a high level summary of key provisions contained in the Act. For more comprehensive analyses of the Act’s provisions, please visit our COVID-19 Resource Center over the days and weeks ahead.
SMALL BUSINESS ASSISTANCE
- Paycheck Protection Program. The Act provides for a “Paycheck Protection Program” (“PPP”), which is an amendment to Section 7(a) of the Small Business Act, created to allow participating banks and other lenders to provide loans to small businesses, as well as self-employed individuals and independent contractors, for purposes of funding payroll, rent, mortgages, utilities, and existing debt obligations. Loan size is limited to the lesser of $10 million and 250% of the company’s average monthly payroll. Eligibility is limited to “small business concerns,” as defined by the SBA, and to other businesses with 500 or fewer employees (including both full and part-time workers).
- Note that the SBA’s affiliation rules apply, except in limited specified cases, so a company would need to include the headcount of other entities affiliated with the business – for example, a private equity or venture fund with control of the company and potentially other portfolio companies – when determining eligibility. SBA’s affiliation rules are complex and often fact-specific.
- For eligible borrowers, loans made under the PPP may be forgiven to the extent used for the purposes described above during the period between February 15, 2020 and June 30, 2020, subject to reductions for decreases in employee headcount and decreases in employee compensation greater than 25 percent as compared to prior years. The portion of any employee’s compensation in excess of $100,000 annually is excluded from eligibility for forgiveness.
- Unlike other loans made under the SBA’s 7(a) program, loans made under the PPP will not require personal guarantees or collateral support and all borrower fees will be waived. To the extent not forgiven, principal and interest may be deferred for a minimum of six months and a maximum of one year. Loans would then be repaid over a term of up to 10 years and carry interest at a rate capped at 4%.
- Grants. The Act includes provision for $10,000 grants to be made to applicants for SBA’s Economic Injury Disaster Loan (EIDL) program, whether or not applicants ever receive EIDL funding.
LENDING PROGRAM
The Act authorizes the Treasury Department to make loans and loan guarantees totaling up to $500 billion, as described below. There are general prohibitions on share repurchases and the payment of dividends by businesses participating in this program while any loan is outstanding, plus one year, and there are limits on executive compensation for companies that accept loan assistance.
- Loans to Specific Industries. $46 billion of the loan program is reserved for United States business borrowers in three specific industries: air carriers ($25 billion), cargo air carriers ($4 billion), and businesses critical to maintaining national security ($17 billion).
- Loans in Support of Federal Reserve Facilities. $454 billion of the program is reserved for loans to or investments in Federal Reserve facilities. These facilities are currently geared toward specific credit market segments, such as debt of larger issuers with credit ratings and asset backed securities. The Fed has indicated that it expects to come out with an additional “Main Street Business Lending Program” to support lending to small and medium-sized businesses, supplementing efforts by the Small Business Administration.
- New Mid-Sized Business Facility. The Act also directs the Treasury Department to seek to implement a new facility, included in the $454 billion pool, enabling lending to United States businesses with between 500 and 10,000 employees. Loans under this new facility would carry interest rates of not more than 2% and would not require principal or interest payments for the first six months.
- Government Relief Fund. The Act creates a $150 billion Coronavirus Relief Fund for states, territories, local governments and tribal governments to be used to cover costs incurred in 2020 in response to the COVID-19 pandemic. Aid will be allocated amongst states in proportion to their relative population, with each state receiving a minimum payment of $1.25 billion. The Act directs the Treasury Department to make payments within 30 days of its enactment.
HEALTHCARE
The Act also includes substantial investments in the healthcare system:
- Healthcare Emergency Fund. The Act establishes the ‘‘Public Health and Social Services Emergency Fund’’ to provide $100 billion to health care providers for health care related expenses or lost revenues that are attributable to COVID-19. Funds may be used for construction of temporary structures, leasing of properties, medical supplies and equipment including personal protective equipment and testing supplies, increased workforce and trainings, emergency operation centers, retrofitting facilities, and surge capacity.
- Medicare Reimbursements. Additionally, the Act boosts reimbursement for Medicare providers by suspending sequester which would have reduced reimbursement on most services and by delaying the implementation of planned cuts to Disproportionate Share hospitals (“DSH”) until the fall. It also includes a 20% add-on payment to hospitals for inpatient care for COVID-19 patients and allows hospitals to request advance Medicare payments based on prior years’ payments and allows at least 12 months for repayment. Medicare telehealth capabilities are expanded to include payment for telehealth services provided by federally qualified health centers (FQHC) and rural health clinics (RHC) and for home dialysis patients.
- Medical Supplies. Finally, the Act attempts to address medical product supply shortage by requiring the strategic national stockpile to include certain types of medical supplies and by directing the establishment and maintenance of a medical device shortage list.
EMPLOYMENT
The Act provides assistance to employers and employees, such as the following:
- Pandemic Emergency Unemployment Compensation. Through the use of federal funding to the states, the Act provides for a Pandemic Emergency Unemployment Compensation program for workers who have lost their jobs due to COVID-19-related reasons as follows:
- An additional payment of $600 per week in benefits (over and above existing state benefits) to all workers for unemployment benefits under existing state benefit programs. These extra benefits begin after enactment of the Act and will continue until July 31, 2020.
- Expands eligibility for unemployment compensation to several categories of workers who would not otherwise qualify for unemployment compensation under existing state benefit programs, including those who have exhausted unemployment insurance benefits, who are independent contractors, GIG-workers, self-employed, part-time, or who do not have sufficient work history. This expansion of eligible employees for benefits will cover the period January 27, 2020 through December 31, 2020.
- Individuals are expressly excluded from coverage who have the ability to telework with pay and who are receiving paid sick leave or other paid benefits (even if they otherwise satisfy the criteria for unemployment under the new law).
- Employee Retention Credit for Employer Subject to Closure Due to COVID-19. Eligible employers will receive a credit against applicable employment taxes for each calendar quarter in an amount equal to 50% of the qualified wages (to include certain health plan expenses) paid to employees if an employer, during the applicable quarter, experiences either: (i) a government closure order related to COVID-19 resulting in the partial or full suspension of the employer’s business, or (ii) gross receipts of the employer’s business for the first calendar quarter after December 31, 2019 are reduced by 50% over the same quarter of the prior year, and continuing until the calendar quarter when the employer’s gross receipts are greater than 80% of the gross receipts for the same quarter in the prior year. This credit is subject to caps, including a cap of $5,000 (50% of qualified wages of $10,000) per employee for all calendar quarters. An employer who takes a small business interruption loan provided under the Act may not use the credit. The credit may not duplicate other credits for the same wages, such as those allowed under the Families First Coronavirus Response Act.
- For employers with greater than 100 full-time employees (as measured in 2019), qualified wages include those paid to employees who are not providing services during such calendar quarter due to COVID-19-related reasons. For employers with fewer than 100 full-time employees (as measured in 2019), qualified wages include those paid to employees during such calendar quarter, regardless of whether the employee is still providing services.
BENEFITS
The Act includes a number of benefits plan measures, including the following:
- Early distributions from retirement plans. The 10% early withdrawal penalty otherwise applicable to distributions from qualified retirement plans made before attaining age 59 ½ is waived for coronavirus-related distributions of up to $100,000.
- Qualified plan loans. The ability to take a plan loan from a qualified retirement plan is increased. Loans of up to $100,000 (rather than $50,000) and up to 100% (rather than 50%) of a participant’s vested balance are permitted. In addition, the due dates for repayments due on outstanding plan loans in 2020 are generally delayed for one year.
- Minimum distribution rules. Required minimum distributions otherwise scheduled to be made from certain qualified retirement plans and IRAs in 2020 are no longer required.
- Expand DOL authority to postpone deadlines. The existing provision in ERISA that permits the US Department of Labor to postpone certain filing deadlines in the event of a variety of emergencies is expanded for coronavirus.
TAX
The Act includes numerous temporary tax provisions intended to provide liquidity for businesses by delaying tax payments and creating refund opportunities, such as the following:
- Payroll tax credits. Businesses experiencing COVID-19-related shutdowns or significant revenue losses eligible for refundable employment tax credits.
- Payroll tax payment delay. Employers permitted to delay paying the employer’s share of Social Security taxes otherwise due this year until December 31, 2021 (for one-half of the deferred taxes) and December 31, 2022 (for the other half).
- NOLs. Allows businesses to carry back 2018, 2019 or 2020 net operating losses (“NOLS”) for five years and temporarily would remove the limitation on the amount of income that may be offset by NOLs.
- Excess business losses. Removes the $250,000 cap on business losses of non-corporate taxpayers for 2018 through 2020.
- Differences from original proposal. The Act passed by the Senate does not include several provisions included in the original Senate version, including those relating to repatriated earnings, downward stock attrition and corporate estimated tax payments.
We understand that protecting your business is critical for you during this uncertain time, and Smith Anderson will continue to provide updates on potential sources of relief. Additionally, please visit and bookmark our firm’s Coronavirus (COVID-19) Business Resource Center which is continuously updated with useful materials and resources related to COVID-19. This tool has been made available to ensure that our clients and the broader business community stay informed on key issues that may impact their operations and to navigate the related business and legal issues during these challenging times.
If you have any questions related to this alert, please do not hesitate to contact your regular Smith Anderson lawyer or any other member of our firm.
Special thanks to contributing authors Jenny Bobbitt, Tim Goettel, Charles Kabugo-Musoke, Rose Kenyon, Tim McKeever, Caryn McNeill, Bill Nelson, Bart Norman, Shawn Parker, Robert Shaw and Dana Simpson.
House COVID-19 Economic Support Committee
 The House COVID-19 Economic Support Working Group met on March 31, 2019.
The House COVID-19 Economic Support Working Group met on March 31, 2019.
Lee Lilly, Legislative Director for Governor Roy Cooper provided the Committee with a broad overview of the administration's COVID-19 updates.
This slide illustrates the distribution of cases in North Carolina as of March 31, 2020.
NC US Small Business Association
Thomas Stith, the Director for NC US Small Business Association informed group that SBA support is available in the following avenues for coronavirus circumstances:
- Economic Injury Disaster Loans
- All small businesses are eligible to apply. Criteria for consideration does include credit history, repayment, and collateral for loans over $25,000.
- Eligible entities can qualify for loans up to $2 million. The loan funds could be used for fixed debts, payroll, accounts payable, and other bills.
- Emergency Economic Injury Grants
- Up to $10,000.
- If approved, funds are distributed and are not repaid.
- Express Bridge Loans
- Paycheck Protection Program
- Small Business Debt Relief
*Please click this photo to expand to view the application information.
Scott Hamilton, President of the Golden Leaf Foundation provided an update of their Rapid Recovery Loan Program.
The online application takes less than an hour to complete and the loans have zero interest. The goal of this program is to support as many businesses as possible until they can restart their operations to receive revenue. This program is operated by the NC Rural Center, however, small businesses in all 100 counties are eligible to apply for funding. The average amount requested by applicants is $36,000. Applications will be reviewed in the order that they are received. Visit NCrapidrecovery.org to learn more and apply.
Business Link North Carolina can also help business owners with information and resources to assist their companies.
North Carolina Restaurant & Lodging Association
Lynn Minges, President and CEO of NCRLA provided the group requests from their industry.
North Carolina Retail Merchants Association
Andy Ellen, President and General Counsel of NCRMA provided the group requests on behalf of all retail businesses.
Public Comment to the NCGA House Select Committee on COVID-19 can be provided here.
NCMS Morning Rounds 3-30-20
HAPPY DOCTORS' DAY!!
Thank you for all you do!
March 30, 2020
We are so grateful for your selfless service every day, but during these uncertain times we especially appreciate your knowledge, expertise and compassionate care. We feel honored to work on your behalf. THANK YOU from the NCMS staff!
NCMS Legislative Update
NCMS staff, leadership and committees have been working hard over the past week to listen to you and understand the challenges you are facing during this pandemic. We are working closely with our partners, agencies and elected officials at both the federal and state levels to address your needs.
We are still listening and soliciting your input on what your greatest challenges are in grappling with COVID-19 response in this week’s NCMS Sunday Survey. Access the survey here if you haven’t already responded. This information will be used by our Legislative Cabinet as they formulate our advocacy agenda to lobby on your behalf.
The NCMS Legislative Cabinet convened on Thursday evening after NCMS Board of Directors member Eileen Raynor, MD, FACS, FAAP, and NCMS Senior Vice President for Advocacy and Advancement Chip Baggett, JD, delivered testimony before the NC House Select Committee on COVID-19. Using the NCMS’ written report to the committee as a starting point, Legislative Cabinet members directed staff to use member input to develop a timeline starting with the most urgent, essential needs, followed by what anticipated needs will be during the peak of the pandemic, as life returns to normal and finally recommendations on the lessons learned and areas for improvement. Staff is working to develop with timeline of necessary legislative, regulatory and government actions to present this week. Watch your NCMS Morning Rounds for a summary.
In other important news, on Friday the President signed the $2 trillion stimulus and COVID-19 relief package, which Congress approved last week. Our federal partners at the AMA provided this brief overview of how the package might impact your medical practice.
The stimulus package:
• Creates a new loan product within the Small Business Administration for loans of up to $10 million to help cover payroll and overhead costs, with expanded loan forgiveness criteria. Physician practices with not more than 500 employees may qualify.
• $100 billion in direct financial support to hospitals, physician practices, and other health care providers under the Public Health and Social Services Emergency Fund. This support is for costs of treating COVID-19 patients as well as to ease the financial impact on those who lose revenue due reductions in other services as a result of the pandemic. Exact eligibility criteria and application process is not yet defined pending implementation.
• Suspension of the 2 percent Medicare sequester in May through December 2020.
• Limitations on liability for volunteer health care professionals during COVID-19 emergency response.
• A temporary waiver of the face-to-face visit requirement with home dialysis patients.
• Authority for the Secretary of HHS to waive telehealth coverage requirements for new patients during a national emergency. Previous legislation provided flexibility only for established patients seen within the past three years.
• Secretary will also allow for enhanced use of telehealth under Medicare for federally qualified health centers.
Also of interest, the “health extenders” package that was set to expire on May 22 has now been extended to November 30.
Finding Oral Health Emergency Care
The NC Oral Health Collaborative (NCOHC), a program of the Foundation for Health Leadership & Innovation (FHLI), published a COVID-19 access map for oral health emergency care. Access the interactive map. The map is designed to assist patients in locating nearby Federally Qualified Health Centers, county health departments, free and charitable clinics, and other safety net sites for which they can seeks urgent dental services.
North Carolinians visit emergency departments for non-traumatic oral health issues at twice the national rate. It is especially important now as hospitals are grappling with responding to the COVID-19 pandemic, to keep emergency departments available for trauma and COVID-19 response. While oral health providers have been notified to postpone elective procedures—following guidance from the American Dental Association and the North Carolina State Board of Dental Examiners—many are available to see patients for urgent dental needs.
If patients require care for an urgent oral health need, it is recommended that they find a nearby practice, but call before going in. Clinical practices may have special guidance to ensure the safety of staff and patients alike. Additionally, due to the strain on the entire public health system, hours of operation are subject to change.
NCOHC developed its practice site map in part to aid the UNC Adams School of Dentistry’s efforts in providing safe ways for patients to manage oral health care during the COVID-19 pandemic. NCOHC’s practice map will be updated regularly as new information is available.
Alternative PPE Resource
Since the personal protective equipment (PPE) supply is short, Blue Cross and Blue Shield NC has been working with provider systems and innovators across the state to support efforts to produce PPE through alternative means (i.e., 3D printing, injection molding). They have created a site to gauge your interest and need, and to directly connect you to producers of these materials.
Visit the alternative PPE site.
In the News
Our best defense against Covid-19? Science. STAT, 3-27-20
Learning Opportunity
Get a broader perspective on COVID-19 during this live chat on Wednesday, April 1 at 11 a.m. The pandemic has had profound effects on daily life across much of the globe. To defeat it, public health officials are taking unprecedented steps to stop viral spread, while researchers and drug companies are racing to develop treatments and vaccines.
How is the public health response playing out? And what kinds of treatments might one day help? Join STAT reporters Helen Branswell, Sharon Begley, and reporter Andrew Joseph for a free live chat about these issues and more. Learn more and register here.
NCMS Morning Rounds 3-27-20
It's Friday and time for your
NCMS Morning Rounds!
March 27, 2020
NCMS Testifies Before NC House COVID-19 Committee
Yesterday, NCMS Board of Directors At-large member Eileen Raynor, MD, FACS, FAAP and NCMS Senior Vice President for Advocacy and Advancement Chip Baggett, JD, testified on your behalf before the NC House Select Committee on COVID-19. The committee, which met virtually, heard from representatives of the NC Healthcare Association as well as from the NCMS on the conditions in which health care professionals and hospitals now find themselves and what legislators might do to address supply shortages, financial impacts and how best to protect the public.
Prior to testifying, the NCMS submitted to the Committee members a comprehensive report outlining both short and long-term actions legislators can take to provide resources and support to the health care community and ensure access to care for the people of North Carolina in response to this pandemic. Read the report.
After hearing Dr. Raynor and Baggett speak, NCMS member Rep. Perrin Jones, MD (R-Pitt), a member of the committee and its health care working group, encouraged legislators to approach the needs in three-tiers: acute needs such as adequate personal protective equipment and ventilators; medium range issues like helping financially strapped practices especially in case the virus resurfaces next fall and winter and long-term policies taken from a running list of ‘lessons learned’ in this crisis to avoid the same situation in the future.
Listen to yesterday’s NCMS testimony and questions from legislators.
Results of Sunday Survey #4 – Medical Malpractice Reform
Thank you to everyone who responded -- despite the upheaval caused by COVID-19 -- to our fourth Sunday Survey on medical malpractice reform. The results are below.
On Sunday afternoon, watch for our final Sunday Survey, which will focus on scope of practice. Your input on these surveys over the past four weeks is a most valuable asset to our Legislative Cabinet as they consider our priorities for the coming legislative session.
Here are the results of our survey on Medical Malpractice Reform:
What strategies can the NCMS support to limit medical malpractice costs, deter the filing of baseless claims and insure those who have sustained injury are appropriately compensated? Please check the ONE option below you think the NCMS should make a priority when considering medical malpractice reform.
NCMS’ Kanof Institute for Physician Leadership Offers Virtual Executive Coaching
To all the amazing clinicians out there: THANK YOU for all the work you do during this unprecedented and challenging time to help patients and keep the rest of us safe. We are so grateful for the sacrifices and hard work you do!
Leadership is more important than ever as we navigate this difficult moment of uncertainty and complexity. This is a time that require leaders to show confidence while they may feel the most vulnerable and be able to share a vision for others when it is challenging to even get to the end of the day. To serve you the best we can during this challenging time, we offer free executive coaching via Zoom. If you want to sign up, please send an email to Kristina Natt och Dag at [email protected] or Aubrey Cuthbertson at [email protected].
In the News
What We’ve Learned About the Coronavirus -- and What We Still Need to Know, STAT, 3-26-20
Learning Opportunity
Here are two upcoming opportunities offering help in addressing the impact of COVID-19.
TODAY, March 27: Families First Coronavirus Response Act Webinar, from 12:30 to 1:30 p.m. Attorney Jefferson Whisenant shares updates and basic information employers need to know about the new Families First Coronavirus Response Act, which created mandatory federal paid sick leave for employees unable to work due to the virus. Learn more and register for this free webinar provided by the NC Medical Group Management Association.
On Monday, March 30, from noon to 1p.m. NC AHEC and the Office of Rural Health (ORH) will offer the next in the weekly Telehealth Webinar Series to address the role of virtual visits in response to COVID-19. These webinars allow you to pose questions to telehealth subject matter experts. Join the Zoom meeting room or dial-in at (646) 558-8656 with webinar ID 985 104 650.
Please submit any questions for subject matter experts to prepare for in advance to [email protected].