NC DPH: Xylazine (known on the street as Tranq) Abuse Growing. New Exposure Guidance Issued.

Xylazine abuse in the United States is a growing public health problem. The FDA-approved drug, which is legally administered by veterinarians as a sedative, muscle relaxant, or non-opioid analgesic for large animals. Known on the street as “tranq,” xylazine is increasingly mixed with opioids and can increase the risk of overdose. The Centers for Disease Control and Prevention (CDC) reports that xylazine use by humans may cause bradycardia, severe hypotension and ulcers.
In response to the threat of increasing exposure to xylazine, the NC Division of Public Health (NC DPH) has issued an alert with guidance for North Carolina health care professionals (PDF). The notice includes instructions on reporting adverse events and patient education information. Please share this information with colleagues.
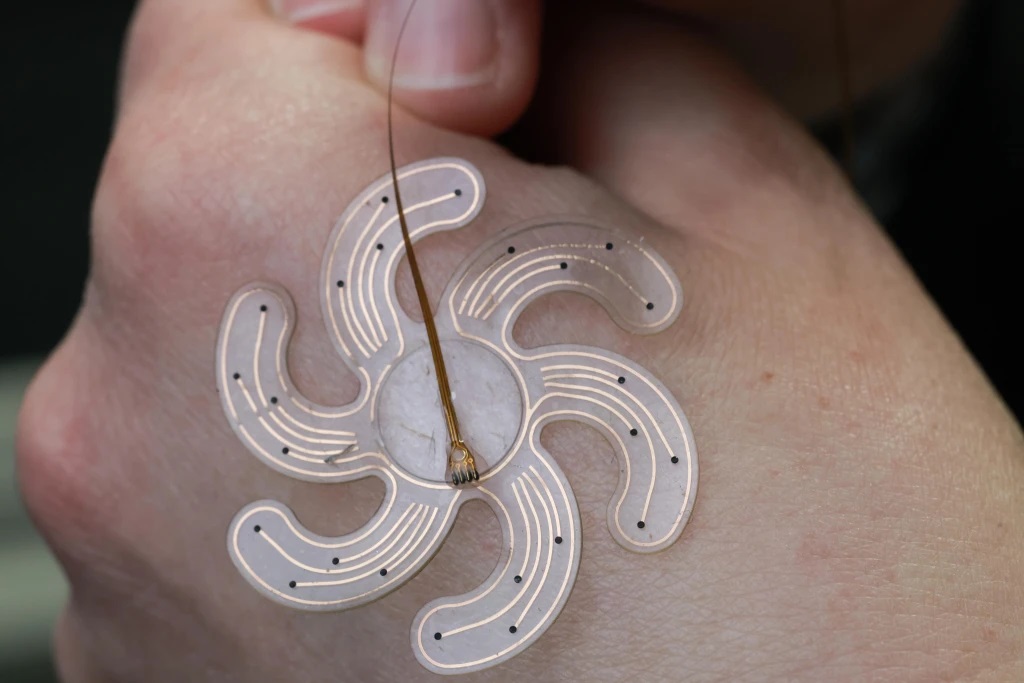
Minimally Invasive Skull Implant Could Treat Epilepsy and Other Neurological Conditions

Researchers at the Ecole Polytechnique Fédérale de Lausanne in Switzerland have developed a flexible, flowerlike device that can be inserted through a tiny hole in the skull and attached to the brain to help treat conditions like epilepsy.
“Minimally invasive neurotechnologies are essential approaches to offer efficient, patient-tailored therapies,” Stephanie Lacour, director of the EPFL Center for Neuroprosthetics, said in a news release. “We needed to design a miniaturized electrode array capable of folding, passing through a small hole in the skull and then deploying in a flat surface resting over the cortex.”
The technology combines soft bioelectronics and soft robotics, creating an extremely thin device with six spiral-shaped arms. The arms start off inverted inside a cylindrical tube and deploy once the array has reached its target, allowing it to cover a 4 cm surface area — double the 2 cm diameter of the hole it’s passed through. It rests within a space only about 1 mm in width between the skull and the brain.
Read the full article here.
Duke Health Leads New Universal Flu Vaccine Trial

Duke Health is leading its first clinical trial under a large federal initiative to develop a new-generation flu vaccine.
The phase 1 clinical trial, which launched last month, is testing the safety of a vaccine candidate devised under the Collaborative Influenza Vaccine Innovation Centers (CIVICs) program. CIVICs is a multi-million-dollar investment by the National Institute of Allergy and Infectious Diseases (NIAID), part of the National Institutes of Health, to develop a modern vaccine that provides longer and broader protection against both seasonal and pandemic influenza viruses.
Read the full article here.
NCMS PAC Thankful Thursday!
On this Thankful Thursday, we are recognizing some of our NCMS PAC Investors! Thank you for your continued support and investment to your patients and profession. Contact Hannah Rice ([email protected]) to learn more about how you can make a difference.
Amanda C. Trimpey, MD, MPH, FACOEM
David K. Mertz, MD, FAAP
James E. Hill, Jr., PA-C, MEd
Kevin B. Shute, MD
Rebecca Y. Weinshilboum, DO
Valerie L. Jewells, DO
TBT: Celebrating 20 years of Leadership in Medicine! Here is Kristen Dorsey, MD's MEDTalk from 2018
This year the North Carolina Medical Society is celebrating 20 years of Leadership in Medicine!
Here is a Throwback Thursday to Dr. Kristen Dorsey's MEDTalk from 2018. Look for a new TBT every Thursday until the 2023 LEAD Conference, October 13-14.
https://youtu.be/m553kTKyAW0
The 2023 LEAD conference registration is NOW OPEN. Click here for more information.
Please contact Erica Hall at NCMS to organize a class table of your own.
CDC Update on Mpox: Warm Weather, Gatherings Could Lead to Resurgence
The Center for Disease Control and Prevention (CDC) recently released a Health Alert Network (HAN) Health Update meant to inform clinicians and public health agencies about the potential for new clusters or outbreaks of mpox cases and to provide resources on clinical evaluation, treatment, vaccination, and testing.
Mpox virus can be spread person-to-person through infected body fluids (including saliva and lesion fluid), items that have been in contact with infected fluids or lesion crusts, and respiratory droplets. The incubation period is usually 7−14 days but can range from 5−21 days. People with mpox are infectious from the start of symptoms (before the rash forms) until the lesions heal and new skin forms underneath scabs and the scabs have all fallen off.
Warmer weather and individuals gathering for events could lead to a resurgence of mpox. The CDC and local partners are investigating a cluster of mpox cases in the Chicago area with 12 confirmed and one probable case.
Read the full Health Update here.
Other links of interest:
NCMS Hosts First Advocacy Summit

On April 29th, NCMS hosted an Advocacy Summit for physicians, physician assistants and other medical professionals across the state. We had thirty members in attendance and had a great line up of speakers and sessions.
One attendee was NCMS Board Member and Durham-Orange County Medical Society President, Ronnie Laney, MD, MPH. Here's what he had to say about the day:
"My recent experience with the NCMS Advocacy Summit continued my passion in the fight for our patients, who seem to continue to lose access to quality, affordable, and timely healthcare. The problems, stress, poor outcomes continue to trickle downward to the very foundation of medicine: doctors and patients. This is why I got involved, and remain involved as a healthcare advocate. The NCMS Advocacy Summit had great energy and passion with a collaboration of advocates from different aspects. The energy was infectious as we discussed the motivations for engaging, staying engaged, and getting others to engage. As advocates, we can do a lot to engage, and get the message out there, in front of our colleagues, our healthcare institutions, and our legislators."
Due to the great feedback and turnout from the summit, NCMS plans to host this again in 2024! Want more information about how to get involved in NCMS advocacy efforts? Reach out to Hannah Rice at [email protected].
NCMS CEO Chip Baggett Makes Business NC's Power List Second Year in a Row!

Congratulations to our very own Chip Baggett for making Business North Carolina’s 2023 Power List in the Health Care category. This is Chip's second year receiving this well-deserved honor!
Business NC's goal is to identify the people who lead North Carolina, based on interviews with business community officials, research and reader suggestions. Their emphasis is on those who have made a particularly noteworthy impact in the last year.
Be sure to send Chip your congratulations in the comments!
Other links of interest:
Business North Carolina's 2022 Power List
Relief Could Be Possible for Your Patients Suffering with Hot flashes and Night Sweats

The Food and Drug Administration (FDA) recently approved a new nonhormonal medication to treat the hot flashes and night sweats often experienced with menopause.
Veozah, or fezolinetant, made by Astellas Pharma, is the first approved neurokinin 3 (NK3) agonist. It blocks receptors in the brain that play a role in the regulation of body temperature.
Women at higher risk of stroke, heart attacks or some kinds of cancer are sometimes advised against using hormone replacement therapies because they increase the risk of blood clots and cancers. Veozah is an alternative to traditional hormone replacement therapies.
In clinical trials that included more than 3,000 women in the US and Canada, Veozah reduced the number of hot flashes women experienced each week significantly more than a placebo. The studies followed women who took the drug for a year.
Read the full article here.
Grant Opportunity for Maternal Health Research

The purpose of the Maternal Health Research Collaborative for Minority-Serving Institutions (MSIs) is to establish a multi-institutional research network that is comprised of and supports minority-serving institutions (MSIs) to build their capacity to conduct research addressing disparities in maternal mortality, severe maternal morbidity, and maternal health outcomes and to find community-based solutions to address these disparities and advance health equity.
Applications must be submitted by to June 12, 2023.
To learn more and apply, click here.
Take the Pledge to Help Stop Diabetes in its Tracks!
DIABETESFREENC is a joint initiative of the NCMS Foundation and the American Medical Association (AMA) aimed to stop the spread of diabetes in NC.
The National Diabetes Prevention Program (DPP) is a lifestyle change program that has free or low-cost options for patients, regardless of their insurance provider and you can refer using any of these convenient platforms: Our Community Health Initiative (OCHI), NC CARE 360 and the DPP Navigator.
Your pledge demonstrates your willingness to support diabetes prevention in NC! Pledge TODAY!
Webinar on New Recommendations for Hepatitis B Screening

On Tuesday, May 16, the Bureau of Primary Health Care (BPHC) is hosting a webinar to brief clinicians and other health care providers about the release of new recommendations for hepatitis B screening and testing.
During the call, Dr. Erin Conners, CDC’s viral hepatitis epidemiologist, will discuss how the updated recommendations differ from the 2008 recommendations, explain the rationale for the changes and why the updated recommendations are beneficial. Dr. Conners will also share key messages.
Participants will have an opportunity to ask questions about the science supporting these changes and the expected impact of these recommendations.
Need more information, Chepkorir Maritim, Nurse Consultant, at [email protected]
Register for the webinar here.
Event details:
Tuesday, May 16
1:00-2:00 p.m. ET
NCMS Loves Early LEAD Adopters! Now is Your Time to Let Your Voice be Heard!
https://youtu.be/6guI0x2U440
Momentum is building for the 2023 LEAD Conference ...
Many thanks to Edward Jones, another confirmed sponsor at the 2023 LEAD Conference!
Be sure to visit Edward Jones at their exhibit booth at LEAD!
Want to attend? Find out how here.
Find out more about sponsorship opportunities here.
... and your company needs to be there!

Physicians Needed for Three NCMB Seats
Applicants are needed for three physician seats on the North Carolina Medical Board for terms beginning November 1, 2023.
All positions must be filled by the process set down in statute (N.C. Gen. Stat. 90-2 and 90-3), which requires interested parties to apply via the Review Panel for the North Carolina Medical Board. The Review Panel is an independent body that nominates candidates for consideration by Governor Roy Cooper. By law, the Review Panel must nominate two candidates for each open seat.
Additionally, one of the open seats must be filled by a physician who is a member of the Old North State Medical Society. Applications from ONSMS members are urgently needed to fulfill the statutory Board composition criteria.
Applications will be accepted online and are due no later than Thursday, June 29 at 4:45 p.m.
The Review Panel will consider only physicians (MDs or DOs) who hold active, unrestricted NC medical licenses. Applicants must be actively practicing clinical medicine at least part time and must have no history of disciplinary action within the past five years.
For more information or to submit an application, visit this website.
FDA Updates Blood Donations for Gay and Bisexual Men

A recent decision by the Food and Drug Administration (FDA) eliminates restrictions that have previously prohibited many blood donations by gay and bisexual men.
In a press release, the FDA said it will recommend a series of "individual risk-based questions" that will be the same for every blood donor, regardless of their sexual orientation, gender or sex. Those who have had anal sex with a new sexual partner, or more than one sexual partner, within the last three months would be asked to wait to donate blood.
Read the full article here.
Updates to Requirements For All DEA-Registered Practitioners. What it Means for Your Practice.

Beginning June 27, the DEA registration will require applicants – both new and renewing – to complete a new, one-time, eight-hour training focusing on substance use disorder, with exceptions for some practitioners.
On December 29, 2022, the Consolidated Appropriations Act of 2023 enacted this training requirement for all Drug Enforcement Administration (DEA)-registered practitioners on the treatment and management of patients with opioid or other substance use disorders.
Below is information on this new requirement:
Who is responsible for satisfying this new training requirement?
- All DEA-registered practitioners, with the exception of practitioners that are solely veterinarians.
How will practitioners be asked to report satisfying this new training requirement?
- Beginning on June 27, 2023, practitioners will be required to check a box on their online DEA registration form—regardless of whether a registrant is completing their initial registration application or renewing their registration—affirming that they have completed the new training requirement.
What is the deadline for satisfying this new training requirement?
- The deadline for satisfying this new training requirement is the date of a practitioner’s next scheduled DEA registration submission—regardless of whether it is an initial registration or a renewal registration—on or after June 27, 2023.
- This one-time training requirement affirmation will not be a part of future registration renewals.
How can practitioners satisfy this new training requirement?
There are multiple ways that practitioners can satisfy this new training requirement:
- First, the following groups of practitioners are deemed to have satisfied this training:
- Group 1: All practitioners that are board certified in addiction medicine or addiction psychiatry from the American Board of Medical Specialties, the American Board of Addiction Medicine, or the American Osteopathic Association.
- Group 2: All practitioners that graduated in good standing from a medical (allopathic or osteopathic), dental, physician assistant, or advanced practice nursing school in the United States within five years of June 27, 2023, and successfully completed a comprehensive curriculum that included at least eight hours of training on:
-
- Treating and managing patients with opioid or other substance use disorders, including the appropriate clinical use of all drugs approved by the Food and Drug Administration for the treatment of a substance use disorder; or
-
- Safe pharmacological management of dental pain and screening, brief intervention, and referral for appropriate treatment of patients with or at risk of developing opioid and other substance use disorders.
- Second, practitioners can satisfy this training by engaging in a total of eight hours of training on treatment and management of patients with opioid or other substance use disorders from the groups listed below. A few key points related to this training:
-
- The training does not have to occur in one session. It can be cumulative across multiple sessions that equal eight hours of training.
-
- Past trainings on the treatment and management of patients with opioid or other substance use disorders can count towards a practitioner meeting this requirement. In other words, if you received a relevant training from one of the groups listed below—prior to the enactment of this new training obligation on December 29, 2022—that training counts towards the eight-hour requirement.
-
- Past DATA-Waived trainings count towards a DEA registrant’s 8-hour training requirement.
-
- Trainings can occur in a variety of formats, including classroom settings, seminars at professional society meetings, or virtual offerings.
What accredited groups may provide trainings that meet this new requirement?
- The American Society of Addiction Medicine (ASAM)
- The American Academy of Addiction Psychiatry (AAAP)
- American Medical Association (AMA)
- The American Osteopathic Association (AOA), or any organizations accredited by the AOA to provide continuing medical education
- The American Dental Association (ADA)
- The American Association of Oral and Maxillofacial Surgeons (AAOMS)
- The American Psychiatric Association (APA)
- The American Association of Nurse Practitioners (AANP)
- The American Academy of Physician Associates (AAPA)
- The American Nurses Credentialing Center (ANCC)
- Any other organization accredited by the Accreditation Council for Continuing Medical Education (AACCME) or the Commission for Continuing Education Provider Recognition (CCEPR), whether directly or through an organization accredited by a State medical society that is recognized by the ACCME or CCEPR
- Any other organization approved or accredited by the Assistant Secretary for Mental Health and Substance Use, the ACCME, or the CCEPR
For information regarding the DEA Diversion Control Division, click here.
If you have any additional questions on this issue, please contact the Diversion Control Division Policy Section at (571) 362-3260.
Buprenorphine Quick Start Guide
DEA Telemedicine Flexibilities for Controlled Substances Extended Through November

The Drug Enforcement Administration (DEA) announced that COVID-19 telemedicine flexibilities for controlled substances will be temporarily extended for six months – through November 11, 2023.
For any practitioner-patient telemedicine relationships that have been or will be established up to November 11, 2023, the full set of telemedicine flexibilities regarding prescription of controlled medications established during the COVID-19 PHE will be extended for one year – through November 11, 2024.
New Hope for Patients with One of the Deadliest Forms of Cancer
Scientists have reported that a new vaccine designed to treat pancreatic cancer prevented the disease from returning in 50% of patients who received it.
In a small study published by Nature, scientists said they tested the vaccine on 16 patients in New York City, and half of the patients were still remaining cancer-free after 18 months — a success for the trial.
Scientists at the German firm BioNTech developed a vaccine that can be tailored to a pancreatic cancer patient's unique genetic makeup, to train their immune system to destroy pancreatic cancer cells.
New York's Memorial Sloan Kettering Cancer Center took tumor samples from 16 patients and sent them to Germany. There, a team of scientists at BioNTech — the company that co-developed COVID-19 vaccines with Pfizer — analyzed the proteins in each sample's cancer cells.
Like the COVID vaccines, these utilized messenger RNA to instruct a patient's immune system to destroy the cancer cells. The key difference was each vaccine being tailor-made to each patient's mRNA.
Pancreatic cancer is notoriously hard to detect and treat. It is widely known as a "silent disease" because symptoms, including abdominal pain and weight loss, often don't arise until the cancer cells have spread to blood vessels and tissue, at which point treatment is difficult.
Read the full article here.
NC Responds to End of Covid-19 Health Emergency

Though the Public Health Emergency declared to respond to COVID-19 has ended, North Carolina will continue to distribute the federally funded COVID-19 vaccines and tests for free to individuals who are uninsured while supplies last.
When supplies of federally purchased vaccines run out, they will be available like flu shots and other routine vaccinations, covered by Medicare, Medicaid, private insurance or out-of-pocket costs for the uninsured. Visit MySpot.nc.gov to learn more or NCDHHS.gov/LHD to contact your local health department.
Community-based organizations can order free tests through June 26, 2023, to distribute in their regions. Visit MySpot.nc.gov/tests for more information.
Federal Test to Treat locations will continue to provide treatment at no cost to those who are uninsured or underinsured, although a fee may be charged for evaluation.
Read the NCDHHS full press release here.
NCMS Member Daniel Fox Receives Old North State Award from Governor Roy Cooper

RALEIGH (WakeMed, May 4, 2023)- Daniel Fox, MD, WakeMed’s executive medical director of Inpatient Hospital & Critical Care Medicine and NCMS member, was recently presented with the Old North State Award from Governor Roy Cooper. Fox was recognized for his excellence in patient care, service, and leadership of the WakeMed Pulmonary & Critical Care team throughout the COVID-19 pandemic. Nominated by his colleagues, he received letters and signatures of support from more than 150 members of the WakeMed community.
The Old North State Award is presented by the governor to recognize “dedication and service beyond expectation and excellence to the Great State of North Carolina.” Recipients must have 20 or more years of service in the state to be considered for this honor.
A pulmonary and critical care medicine physician, Fox treats patients in WakeMed’s intensive care units and provides outpatient pulmonary care services. Throughout the pandemic, Fox worked countless ICU shifts alongside his colleagues while rapidly implementing new COVID therapies and strategies that helped save lives. He ensures every patient receives the most up-to-date, evidence-based care.
His clinical focus includes caring for patients with complex lung diseases including autoimmune disease, asthma, and interstitial lung disease, with a special interest in patients with pulmonary hypertension and pulmonary embolism.
Fox earned his medical degree from the University of North Carolina at Chapel Hill School of Medicine. He completed a residency program in internal medicine at Duke University Medical Center followed by fellowship programs in pulmonary and critical care medicine and pulmonary vascular disease at the University of Colorado Health Sciences Center. He is board certified in internal medicine, pulmonary medicine, and critical care medicine. [source]
TBT: Celebrating 20 years of Leadership in Medicine! Here is David E. Melon's MEDTalk from 2019
This year the North Carolina Medical Society is celebrating 20 years of Leadership in Medicine!
Here is a Throwback Thursday to Dr. David E. Melon's MEDTalk from 2019. Look for a new TBT every Thursday until the 2023 LEAD Conference, October 13-14.
https://youtu.be/-RT_tgghDZk
The 2023 LEAD conference registration is NOW OPEN. Click here for more information.
Please contact Erica Hall at NCMS to organize a class table of your own.
In Memoriam: Former NCMS Team Member Lucia Peel.

The North Carolina Medical Society family is saddened to learn of the passing of a former team member, Lucia Peel. Lucia died Monday, May 8, 2023 at ECU Cancer Center in Greenville, N.C. She was 65.
Lucia served on the Society’s government affairs team from 1994 to 1998 and was integral to advancing NCMS legislative advocacy priorities. She was instrumental in the Medical Society’s engagement in key health policy issues, including Tort Reform, Antitrust Exemptions for Physicians, Patient Safety Regulation, and Managed Care Regulation.
We send heartfelt condolences to the family.
Biggs Funeral Home in Williamston is assisting the family and arrangements are pending.
May is Skin Cancer Awareness Month

The NC Dermatology Association, in partnership with the American Academy of Dermatology, remind us that May is Skin Cancer Awareness Month and an occasion to raise awareness of the most common cancer. It’s estimated that every day about 9,500 people in the United States are diagnosed with skin cancer.
NC Medical Society members are reminded that the entire care community can help educate their patients that . . .
- Many skin cancers could be prevented if people would protect their skin from the sun and stop using tanning beds.
- People of all colors and ages get skin cancer.
- When found early, skin cancer is highly treatable.
- Because skin cancer begins on the skin, you can find it early by performing skin self-exams.
- If you find a spot on your skin that’s growing, bleeding, or changing in any way, see the skin cancer expert, a board-certified dermatologist. This appointment could save your life.
Resources are available from the AAD on a variety of related subjects:
Spread the word – Prevent Skin Cancer!
In 2022, NCMS ran a series of skin care tips from our members called Melanoma Monday. Here are those posts:
Melanoma Monday: Are your ready for summer?
Melanoma Monday: Survive the 4th with Beautiful Skin!
Melanoma Monday: Healthy Life, Healthy Skin
Melanoma Monday: Have Fun at the Lake and Keep Your Skin Safe
Melanoma Monday: Be Safe While You Enjoy A Day at the Beach!
Melanoma Monday: Fun on the Boat Skin Safety
Melanoma Monday: Fun at the Pool!
Melanoma Monday: Summer Skin Care for People Over 55
Melanoma Monday: Keeping Your Skin Clean in Summer!
Melanoma Monday: Fun in the Mountains!
New Study Offers Solution for Reducing Postpartum Hemorrhage

According to a landmark study published by researchers from the World Health Organization (WHO) and the University of Birmingham, a new solution, known as E-MOTIVE, could provide a major breakthrough in reducing deaths from childbirth-related bleeding.
The study, which involved over 200 000 women in four countries, found that objectively measuring blood loss using a simple, low-cost collection device called a ‘drape’ and bundling together WHO-recommended treatments - rather than offering them sequentially - resulted in dramatic improvements in outcomes for women. Severe bleeding – when a woman loses more than a liter of blood after birth - was reduced by 60%, and they were less likely to lose their life.
The recommended E-MOTIVE package includes early and accurate detection of postpartum hemorrhage (PPH) using a blood-collection drape. This is complemented by an immediate treatment bundle where indicated, including uterine massage, medicines to contract the womb and stop the bleeding, intravenous fluid administration, an examination and, when needed, escalation to advanced care.
The Center for Disease Control and Prevention (CDC) characterizes PPH as a severe bleeding by the mother after delivery, labels it a significant public health problem, and the leading cause of death among women during childbirth. Women with von Willebrand disease (VWD)--a hereditary bleeding disorder, caused by a deficiency in the levels and/or function of von Willebrand factor (VWF)--are more likely to experience PPH and are 10 times more likely to die from childbirth complications than women without VWD [source].
Read the full article here.
Catawba Valley Medical Center Awarded America's Best Hospitals for Stroke Care

Catawba Valley Medical Center (CVMC) has been named one of America’s Best Hospitals for Stroke Care by the Women’s Choice Award®, America’s trusted referral source for the best in healthcare. The award signifies that CVMC is in the top seven percent of 4,729 U.S. hospitals offering stroke care services.
Hospitals that meet the stroke center certification requirement, must then meet or exceed the following performance measures from the Centers for Medicare and Medicaid Services (CMS): Hospitals must also score in the top 80% of all hospitals in the percent of patients receiving Head CT scan results within 45 minutes, and cannot have received a rating of Worse than the National Rate for the Deaths from Serious Treatable Complications measure.
CVMC is one of 360 award recipients representing the hospitals that have met the highest standards for stroke care in the U.S. by the Women’s Choice Award.
To learn more about CVMC's award-winning Stroke care, visit CatawbaValleyHealth.org/Stroke.
Congratulations, Catawba Valley Medical Center, for helping to make North Carolina healthier!
Newborn Genomic Screening: Helpful or Harmful?

Experts are divided about how helpful DNA sequencing data really are. The tests often identify mutations that raise someone’s risk of developing a condition, but don’t necessarily cause the disease. Uncertain results may confuse doctors and scare families — causing them to seek doctors’ visits and treatments that most ultimately won’t require, adding to unnecessary health care costs. There are also concerns about false positives and false negatives with sequencing. But a new study has found that among rare disease physicians — the ones to whom worried parents will turn — there is emerging consensus that these sorts of tests should be used on a broader scale.
When 238 rare-disease doctors across the U.S. were surveyed by a research team at Mass General Brigham in Boston, 88% of them agreed that DNA sequencing to screen for certain treatable childhood disorders should be made available to all newborns. The study was published Monday in JAMA Network Open.
Continue to the full article here.
Be sure to share your thoughts in the comments.
CCHN Seeks Provider Advisory Committee Participation

Carolina Complete Health Network is currently seeking provider participation for its Provider Advisory Committee.
The purpose of the CCHN Provider Advisory Committee is to provide input on Carolina Complete Health (CCH) provider incentive programs, administrative practices, and supports development of provider scorecard indicators, useful analyses of the data, and effective means of helping providers improve their performance.
For this committee, the participating providers must be physicians, physician assistants, or nurse practitioners that are particularly interested in these areas. This committee meets once per quarter for one hour.
CCHN is a subsidiary of the North Carolina Medical Society and co-founders of a first-of-its-kind partnership with Centene Corporation, the North Carolina Community Health Center Association and other providers across North Carolina. CCHN offers North Carolina practitioners a platform to improve clinical and administrative processes, as well as a unique voice in governance over medical policy. They combine the best of leading-edge national expertise with deep-rooted local knowledge of what works here in North Carolina.
Carolina Complete Health Network’s mission is to empower physicians and clinicians to provide state-of-the-art care to Medicaid beneficiaries resulting in BETTER HEALTH and GREATER HEALTH EQUITY at LOWER COST.
If interested in this opportunity, please contact Katie McKay at [email protected].
CMS Proposes New Rule on Publishing of Post Payment Rates - Will it Affect Your Practice?

The Center for Medicare and Medicaid Services (CMS) has issued a proposed regulation that, if finalized, would require state Medicaid/CHIP programs to post payment rates for all services on their webpage.
While the proposal does not explicitly mention Federally Qualified Health Centers (FQHCs), it appears to require the publication of FQHC-specific PPS rates. States would also be required to compare their payments to Medicare rates for the same services, and to establish maximum wait times for managed care patients to receive certain types of appointments.
See page 399 of the NPRM.
First LEAD Sponsor Secured!
SouthState Bank is the first to confirm sponsorship at the 2023 LEAD Conference!
SouthState will have an exhibit booth, so make plans to attend LEAD on October 13 & 14 and visit SouthState's booth representatives. Thank you SouthState Bank!
Find out how your company can be involved or sponsor the LEAD Conference here.
Devastating News for the First Pediatric Practice in Morehead City, NCMS Members Affected.

On April 28, police were dispatched to a burglar alarm at the Carteret County Clinic for Adolescents and Children on John Platt Drive, but when they arrived, they saw flames.
Of the rebuilding, Dr. Margaret Merrick, a provider at the practice, says: "Of course, it is going to be a long process, but the community has been very supportive, and we have a great team with a very positive outlook."
72 hours after the fire, that resulted in a total loss, the clinic was able to re-open, in part thanks to the generosity of Carolina Center for Surgery and Carteret OBGYN.
The Carteret County Clinic for Adolescents and Children will see patients at its new location at 221-B Professional Circle, Morehead City.
On its Facebook page, the clinic gives shout outs to many who helped including: Oceanside Pediatrics and Kids Rule Pediatrics and Carteret Healthcare and Oceanside Pediatrics. They also give thanks to Morehead City Fire Department, Morehead City Police Department, Atlantic Beach Fire Department, and Beaufort Fire Department.
No injuries or loss of life (including the fish) were sustained in the fire. The cause is under investigation.
Practitioners at Carteret County Clinic:
Katharine Moorehead, MD (NCMS member)
Margaret Merrick, MD, FAAP
Loreli Rowe, MD (NCMS member)
Keep Your Patients Cool this Summer with Help from Operation Fan Heat Relief!

As temperatures begin rising, the North Carolina Department of Health and Human Services’ Division of Aging and Adult Services is partnering with the NC Area Agencies on Aging and local service providers to distribute fans to eligible recipients through Operation Fan Heat Relief (OFHR).
Beginning May 1, your patients aged 60 and older, as well as adults with disabilities, are eligible to sign up for OFHR assistance at local aging agencies across the state.
Click here to access a list of the 2023 OFHR Local Providers
The OFHR program runs from May 1 to October 31. More information about Operation Fan Heat Relief is available here. Individuals may also contact their area agency on aging or the Division of Aging and Adult Services at 919-855-3400.
Join WCMS for some Crafty Mother's Day Fun!

Join the Wake County Medical Society (WCMS) for a Mother’s Day craft, suitable for any children up to the early teen years.
Local artist and teacher Suzanne Brown will lead children through a charming ceramic project suitable for Mother’s Day (hint, hint….).
Bring your children or grandchildren for a fun, family activity, and then enjoy the sights of downtown Raleigh with free parking at the North Carolina Medical Society (NCMS).
The NCMS is within five blocks of Marbles Kids Museum, the NC Museum of Natural Science, NC Museum of History, and much more!
Pre-registration is appreciated the cost is $10 and payable onsite.
For more information, call 919-621-5919 or email [email protected].


NCDHHS to Hold Next Mental Health Town Hall in Wake County

The next NCDHHS Mental Health Town Hall has been scheduled. The event will be held in Wake County and will be a community discussion on improving minority mental health across North Carolina.
May 11, 2023 • 6:00 - 8:00 p.m.
Wake Tech Community College
1636 Graduation Way, Raleigh, NC 27603
Building L, Student Services Building, 2nd Floor Conference Center
Get more information about the event and register here.
Visit the NCDHHS website to watch recordings of previous town halls. County representatives interested in hosting a Mental Health Town Hall can contact Annelyse Iglesias via email at [email protected].
NCMS Legislative Review - May 5, 2023

Health took center stage last week as many health-related bills passed each chamber. Legislators in Raleigh faced the crossover deadline, which is a date set by which a bill must pass at least one chamber to continue in the legislative process. The deadline was Thursday, May 4th, and took effect for all bills that do not contain appropriations or fees.
The main bill on the forefront of the health space is SB 20, Care for Women, Children, and Families Act. Among other provisions, it would make it unlawful after the 12th week of gestation to have an abortion in North Carolina with other gestational exceptions for fetal anomalies, rape/incest, and medical emergencies. SB 20 did pass both the House and Senate, now heading to the desk of Governor Roy Cooper, who will likely veto it. NCMS issued a statement opposing the bill and NCMS staff are still working to fully understand how the bill will impact access to reproductive healthcare and create new administrative burdens for members.
With the crossover deadline looming, many NCMS supported bills have passed the House. Below is a summary of some:
HB 576: Healthcare Practitioner Transparency Act – also known as “truth in advertising” – This legislation would require a healthcare practitioner to properly identify their license, certification, or registration (MD, DO, etc.) and would not allow the display of any misleading information.
HB 809: Hospital Violence Prevention Act – This legislation seeks to minimize the likelihood of violence by ensuring health care facilities develop safety protocols to address risks identified by hospital employees, security personnel, and local law enforcement.
HB 560: Diagnostic Imaging Parity – Would provide health coverage parity for breast cancer diagnostic imaging and would require coverage for certain other types of imaging.
HB 739: Update Requirements/Advance Healthcare Directives – This patient-focused legislation facilitates access to health care powers of attorney and advance health care directives by modernizing and enhancing the advance care planning process.
Lastly, the NCMS worked tirelessly to remove language repealing protections for minor consent from HB 808. The law currently provides that minors can give consent for medical services in the diagnosis and treatment of pregnancy, abuse of controlled substances, emotional disturbance, and venereal disease. The NCMS remains opposed to the bill due to its interference with the patient-clinician relationship, but we are pleased that the minor consent protections have been preserved.
WHO: Covid-19 No Longer a Global Health Emergency

The World Health Organization (WHO) has declared COVID-19 no longer a global health emergency. The decision was made on the advice of the Covid-19 emergency committee, a panel of independent experts.
“It’s with great hope that I declare COVID-19 over as a global health emergency,” WHO Director-General Tedros Adhanom Ghebreyesus said.
The U.N. health agency’s officials said that even though the emergency phase was over, the pandemic hasn’t ended, noting recent spikes in cases in Southeast Asia and the Middle East. WHO says thousands of people are still dying from the virus every week, and millions of others are suffering from debilitating, long-term effects.
In the U.S., the public health emergency declaration made regarding COVID-19 is set to expire on May 11, when wide-ranging measures to support the pandemic response, including vaccine mandates, will end.
Read more about the decision here.
COVID-19 Reporting Requirements Expire With End of PHE This Month

The Division of Public Health of the NC Department of Health and Human Services has issued notice that, as of May 12, 2023, physicians will no longer be required to report cases of COVID-19 or deaths due to the coronavirus. The May 4, 2023 notice also announced that labs will no longer have to report COVID-19 test results as of the end of the expiration of the declared Public Health Emergency on May 11.
The DHHS/DPH memo can be accessed at here for further details.
Could Mental Health First-Aid Training Help You Better Engage Your Patients?

Mental Health First Aid is a skills-based training course that teaches participants to identify, understand and respond to mental health and substance use challenges.
This basic course on mental health and substance abuse conditions will give you the skills to notice and engage individuals experiencing these symptoms which cause suffering. Through engagement, you can offer understanding and invite them to expand their care team with resources that can help. You will receive a certificate of completion at the end of this course. This course is foundational and part of the training curriculum for NCServes Providers & Staff, Peer Supports, and Community Stakeholders.
Upcoming Trainings:
• Virtual: May 17, 2023
• Virtual: June 5, 2023
• In-Person Raleigh, NC: June 15, 2023
• Virtual: June 27, 2023
• Virtual: July 11, 2023
Learn more and register here.
*Trainings are limited to 30 participants. Register early to secure your spot!
Foundation Friday! Thank You to These NCMS Foundation Donors.

Today, the NCMS Foundation recognizes donors who have joined us on the journey to help make health and well-being attainable for all North Carolinians. These individuals are contributing to make sure clinicians are where they are needed most and that clinician leaders are lighting the way.
Thank you for your continued support to help North Carolinians lead healthier lives.
Learn more about how YOU can make a difference too here.
Richard T. Weisenburger, DO
Joshua I. Vogel, MD
Danilo Bernardo, MD, FACP
Christian G. Anderson, MD
Johnathan D. Williams, MD
Eugene H. Paschold, MD
Karen H. Harum, MD, FAAP
Karen E. Wood, MD
Shannon B. Dowler, MD
First-Ever RSV Vaccine Approved by FDA For Older Adults

The Food and Drug Administration has approved the first-ever vaccine to combat severe respiratory syncytial virus, or RSV, in older adults, giving your patients 60 and older another level of protection.
According to trial data, Arexvy, developed by GlaxoSmithKline, was 82% effective at preventing lower respiratory tract illness caused by RSV and 94% effective in those who had at least one underlying medical condition.
RSV infects nearly everyone by age 2 and is the leading cause of hospitalizations among newborns and younger children; it also strikes late in life, causing more than 177,000 hospitalizations and 14,000 deaths among older adults each year.
Read the full article here.
Statewide Consortium with Key Stakeholders in Healthcare to Move the Needle on Stress and Burnout.
Reignited in September 2022, the North Carolina Clinician and Physician Retention and Well-being (NCCPRW) Consortium is focused on making North Carolina one of the healthiest states to practice medicine. Made up of key stakeholders from organizations across the state, NCCPRW is exploring and identifying drivers of clinician and physician stress and burnout to address wellbeing at the organizational and societal level. You can visit here to find well-being resources.
NCMS PAC Thankful Thursday!
On this Thankful Thursday, we are recognizing some of our NCMS PAC Investors! Thank you for your continued support and investment to your patients and profession. Contact Hannah Rice ([email protected]) to learn more about how you can make a difference.
Alexander Chiaramonti, MD
Donna L. Shelton, PA-C
Greg Griggs, MPA
Lyndon K. Jordan, III, MD, FACR
Matilda W. Nicholas, MD, PhD
Mohammed A. Hannan, MD
Vanessa L. Everett, MD
Wake County Medical Society Plans Membership Activities

Wake County Medical Society (WCMS) Alliance President Zohra Osman (l) plans for membership activities with the WCMS President Ted Kunstling, MD. Both the WCMS and the Alliance work tirelessly to support medical care in the community and the clinicians who provide it.
Happy Birthday to These Members Celebrating This Month!

Grab your party hats and noise makers and let’s celebrate!
Ole S. Aassar, MD
William B. Abernethy, Jr., MD
Surafeal G. Abraha, MD
Peter K. Acheampong, MD
Maureen N. Achuko, MD
Douglas H. Adams, MD, MPH
Van L. Adams, MD
Henry T. Adkins, Jr., MD
Kerry E. Agnello, DO
Julian S. Albergotti, Jr., MD
Dustin B. Alderson, MD
Fuad Y. Aleskerov, MD
Chelley K. Alexander, MD
Erin B. Allen, PA-C
Diane E. Alligood, MD
Sridevi Allu, MD
Ghiath M. Almasri, MD
Terrence P. Almengual, MD
David A. Altman, MD
Harry T. Ameredes, MD
Ginette A. Archinal, MD
Brooktiete Asseres, MD
Emily L. Averbook, MD
Ramesh Avva, MD
P. William Aycock, Jr., MD
Richard E. Babb, PA-C
Gopal H. Badlani, MD
Hasan A. Baloch, MD
John A. Bardini, MD
Victor R. Barnes, MD
James D. Barnwell, MD
Katherine E. Barrett, MD
Robert P. Barringer, MD
Scott J. Bartkoski, MD
Dwight D. Bates, MD
Mckenzie A. Bauman, PA-C
John N. Beard, MD
George H. Beckwith, MD
Matthew T. Bennett, MD
Brendan C. Berry, MD
Jessica E. Berry, PA-C
David S. Bertrand, PA-C
Michelle M. Bertsch, MD
Gideon Besson, MD
Bhavna Bhat, MD
Pouru P. Bhiwandiwalla, MD
William A. Biggers, Jr., MD
Andrew T. Billingsley, MD
Mott P. Blair, IV, MD
Robert A. Blake, MD
Jonathan W. Blank, MD
Kelly T. Blount, PA-C
Elizabeth R. Blyth, MD
Ann L. Bogard, MD
Michael A. Bohl, II, MD
Andrew J. Bojanowski, PA-C
Debra A. Bolick, MD
E. Arthur Bolz, MD
W. Kent Bonney, MD, FAAP
David W. Boone, MD
Bryon J. Boulton, MD
Benjamin C. Bowen, MD
Kellie M. Bowen, PA
James R. Bowers, MD
Umar Bowers, MD
Brian P. Bowman, MD, PhD
Douglas R. Boyette, MD, FACC
Thomas A. Brackbill, MD
J. Lawrence Brady, Jr., MD
Jonathan L. Brandon, MD
Amy E. Brantley, PA-C
David S. Brantley, MD
Charles C. Bremer, MD
Mathijs H. Brentjens, MD
Sarah L. Brewington, MD, FAAP
Dewey H. Bridger, III, MD
James W. Britt, MD, FAAP
Robert C. Brock, MD
Seth C. Brody, MD
Per G. Brolinson, DO
Rebecca M. Brooks, MD
Robert A. Buchanan, Jr., MD
Robert T. Buchanan, MD
Barry D. Bunn, MD
James O. Burke, Jr., MD
Pamela A. M. Burleson, PA-C
Scott J. Burner, MD
Henry W. Burnett, MD
John W. Burnett, Jr., MD
M. Alan Burns, MD
Philip D. Burton, MD
Robert H. Butler, MD
Christopher S. Byrd, MD
Chasitty C. Calhoun, PA-C
Gregory J. Cannon, MD, FACEP
Jeffrey P. Carley, DO
Mark V. Cavaliere, PA-C
T. Brent Chafin, MD
Eric D. Challgren, MD
Peter G. Chan, MD
Pat R. Chappell, MD
Julie S. W. Childers, MD
Monique V. Chireau, MD
Natalie Chrismer, PA-C
Ann Y. Chung, MD
Ian T. Churnin, MD
Justin E. Cimring, MD, FAAP
Kenneth J. Clark, Jr., MD
Lee A. Clark, Jr., MD
Talaya B. Clark, MD
Noellee T. Clarke, MD
John R. Collier, Jr., MD
Michelle S. Collins, MD
David M. Colonna, MD
Christopher D. Connolley, MD
Christopher C. Copenhaver, MD
Christopher D. Corso, MD
Daniel E. Couture, MD
Michael R. Cram, MD
Steven T. Crawford, MD
Trey B. Creech, MD
William D. Crocker, MD
Peter P. Cullen, MD
Lawrence M. Cutchin, MD
Charles L. Czermak, Jr., MD
Seema N. Daigle, MD
Vincent Q. Dam, MD
Danielle M. D'Angelo, PA-C
Nicholas J. D'Avanzo, MD
Melissa S. Davies, DO
Drew E. Davis, MD
W. Hodges Davis, MD
Philip C. Deaton, MD
Robert Deepe, MD
Timothy B. Deering, MD
Martin C. DeGraw, MD
Maria V. Delbono, DO
David T. Dellaero, MD
Donna P. Denier, MD
Priyank K. Desai, MD
Sunil J. DeSai, MD, FACC
Gary J. DeSalvo, MD, DMD
Gautam Dev, MD
Sanjeev K. Deveshwar, MD
Abigail G. DeVries, MD
Tejpal S. Dhillon, MD
Janice F. Dickerson, MD
F. Keels Dickson, MD
Milan M. DiGiulio, MD
Jennifer M. Dimovski, MD
Christopher A. Dixon, DO
Michael L. Dockery, MD
Robert P. Doolittle, MD
Benedict R. Dorsam, PA-C
Nirali M. Dubal, MD, MPH, FAAP
Eric D. Duberman, MD
David A. Dubow, MD
Andrew C. Dukowicz, MD
Jennifer A. Durand-Smith, MD
Edward B. Eadie, Jr., MD
John K. Earl, MD
Randy C. Efird, MD
Dave S. Eichman, MD
Maxlyn L. Ellison, MD
Kelly A. Erola, MD
Vicky Erwin, DO
George K. Escaravage, Jr., MD
James M. Essenberg, MD
E. Harvey Estes, Jr., MD
Bradley H. Evans, MD
D. Evan Evans, MD
Joanna L. P. Evans, MD
William J. Faircloth, MD
Nicholas Farina, MD
Johnny L. Farrow, MD
Sarah L. Fernandez, PA
James V. Ferris, MD
Karen E. Fieselman Stroud, MD, FAAP
Mario G. Fiorilli, MD, MPH, FACPM, FACP
Michael J. Fisher, MD
Otis N. Fisher, MD
James P. Flanagan, MD
Anna M. Fleischman, MD
D. Francis Fleming, Jr., MD, FAAN
Robert A. Flores, MD
Theresa M. Flynn, MD
Toinette H. Fontrier, MD
William W. Fore, MD
Garett R. Franklin, MD
Jonathan P. Fritz, MD
Michael M. Fujimagari, MD
Mary Susan K. Fulghum, MD
Melany Furimsky, DO
Jeffrey G. Gaca, MD
Vikram Gahlot, MD
Robert T. Gallaher, MD, FACP
Dionne P. Galloway, MD
Kenneth R. Gallup, Jr., MD
Jacques P. Ganem, MD
Christopher A. Gardner, MD
Donald N. Gardner, MD
John B. Garrett, Jr., MD
Carolyn M. Garrett Piggott, MD
Sheli R. Garrett-Albaugh, DO
Robert W. Garrison, MD
W. Blake Garside, MD
Michael S. Gart, MD
Leonardo Gendzel, MD
Steven M. Genkins, MD
Michael B. Gentry, MD
Boyan A. Georgiev, MD
P. Pressly Gilbert, MD
Russell V. Gilchrist, DO
C. Lee Gilliatt, Jr., MD
Ronald A. Gioffre, MD
Nathan C. Givens, MD
Brian M. Go, MD
Rolf P. Gobien, MD
Ismael R. Goco, MD
Ronald L. Godbold, MD
Manlio A. Goetzl, MD
David A. Goff, MD
John P. Goldfield, MHS, PA-C
Elizabeth L. Golding, DO
Thomas E. Goodin, III, MD
James O. Goodwin, MD
Maje D. Goodwin, MD
G. Michael Gould, DO
Hannah E. Grabow, PA
Mark L. Graham, II, MD
Arthur G. Green, III, MD
Lawrence H. Greenblatt, MD, FACP
Jerry H. Greenhoot, MD
Ashton T. Griffin, III, MD
Christopher P. Griffin, MD
Elaine C. Griffin, MD
Robert L. Groat, MD
Jeremy G. Gue, MD
Melinda S. Guglielmetti, PA-C
Manu A. Gupta, MD
Paul P. Gwyn, Jr., MD
Robert D. Hagan, Jr., DO
Paul D. Hain, MD
Chad R. Haldeman-Englert, MD
Colin D. Hall, MD
Harold L. Hall, III, MD
John C. Hamrick, Jr., MD
Padma B. Hari, MD, FACC, FASE
David B. Harker, MD
Steven D. Harlan, MD
John S. Harman, MD
Mark D. Harris, MD
Zachary P. Harris, MD
Oliver J. Hart, Jr., MD
D. Daniel Hassell, III, MD
Amber G. Hatch, MD
Samuel P. Hawes, III, MD
Gordon L. Hazen, PA
Timothy R. Heacock, MD
Benjamin L. Hechler, MD
John H. Heinzerling, II, MD
Masoud S. Hejazi, MD
Nicole L. Helmke, MD
Sydney E. Hendry, MD
Thomas Herfurth, MD
Kevin O. Herman, MD
Ruthann A. Heron-Davis, MD
Benjamin W. Herrick, MD
Richard S. Herring, MD
Robert A. Highland, MD
Dennis L. Hill, MD
Patricia K. Hill, MD
Jeremy T. Hines, MD
John C. Hisley, MD
Beverly M. Hockenberger, PA-C
Matthew L. Hoimes, MD
Edward M. Hollander, MD
Robert O. Holmes, Jr., DO
John B. Holt, MD
Tamara S. Housman, MD
Thaddeus D. Houston, MD
Hampton A. Howell, MD
Catherine M. Hren, MD
F. Alan Hubbard, MD
Anthony G. Hucks-Folliss, MD
Janice Huff, MD
Sarah P. Hughes, MD
Matthew W. Hunt, MD
Charles D. Hunter, PA-C
C. Blake Hutchinson, MD
Kimberly F. Ingersoll, MD
Karen M. Isaacs, MD, MPH
Bradley D. Isbister, MD
Rodger D. Israel, MD, MPH
Jonathan D. Jaffe, DO
Amanda H. Janda, PA-C
Thomas E. Jarrett, MD
Casey D. Jenkins, MD
Larry P. Jenkins, MD
Megan E. Jenkins, PA-C
Robert L. Jobe, MD
John A. Johnson, DMD, MD
Lorin E. Johnson, MD
P. Byron Johnson, MD
Gregory L. Jones, MD
Robyn R. Jordan, MD, PhD
Ranjit Joseph, MD
Gurdev S. Judge, MD
Richard D. Kane, MD
Elizabeth P. Kanof, MD
James C. Karegeannes, MD
May M. Kassem, MD
Raghu R. Katuru, MD
Samuel L. Katz, MD
Amantia Kennedy, MD
Scott R. Kennedy, MD
Danielle D. R. Keyton, DO
Neelam S. Khan, MD
Stephen D. Kicklighter, MD
Stanley G. Kinkaid, MD
Alan N. Kirollos, MD
Mark Kirsch, MD
Philip J. Kittner, MD
Valerie D. Knight, PA-C
Harvey D. Kohn, MD, FACOG
Alonzo D. Kornegay, MD
Janelle L. Krasovich, MD
Arthur F. Kriner, MD
Kourtney L. Krohn, DO
Lauree S. Kruyer, PA-C
Alyson R. Kuroski-Mazzei, DO
Cherie M. Kuzmiak, DO
Mark S. LaFave, MD
Melissa J. Lamrissi, MD
Steven E. Landau, MD
Patrick E. Lantz, MD
Clark A. LaPrelle, II, PA-C
E. Joseph LeBauer, MD
James D. LeClair, MD
Esther J. Lee, MD
Jay U. Lee, MD
Robert H. Lee, MD
David P. Lensch, MD
Dante N. Lewis, MD
Jody P. Lewis, MD
Lori B. Lilley, MD
Clinton R. Lincoln, MD
William C. Lippert, MD
Andrew L. Lizek, MD
L. Phillip Lloyd, PA-C
Ginger N. Locklear, MD
William S. Logan, MD
Christine T. Lomboy, MD
Christopher M. Long, MD
Christopher E. Lord, MD
Jason B. Lowe, MD
Christie H. Lowery, PA-C
Michael H. Lowry, MD
Scott N. Lurie, MD
Matthew D. Lyons, MD
Frederick H. Mabry, III, MD
Andrea J. Machnitz, MD
Homa Magsi, MD
Danielle L. Mahaffey, MD, MMM
Mohammed A. Mah'Moud, MD
Jimmy J. C. Mali, MD
Craig A. Mangum, MD
Jennie C. Mangun, MD
Christopher H. Mann, MD
Matthew A. Manning, MD
Sami W. Mardam-Bey, MD
Jordan A. Margo, MD
Marie-Claire Marroum-Kardous, MD
Maria N. Marshall, PA-C
Melanie K. Marshall, MD, DDS
Robert N. Marshall, III, MD
Kristie C. Martin, PA-C, MMS
Willis E. Martin, MD
Damien M. Marycz, MD
James E. Masters, MD
Marjorie E. Matthews, MD
Robert C. Matthews, MD
Michael A. McCall, MD
William McCall, Jr., MD
E. Lee McConnell, III, MD
Leslie A. McCutcheon, PA-C
Noel B. McDevitt, MD
James P. McDonald, MD
Wyman T. McGuirt, MD
Peter F. McIlveen, MD
James D. McLeod, MD
William J. Meggs, MD, PhD
Mark W. Memolo, MD
Michael K. Merz, MD
Robert S. Meyer, MD, FAAFP
Assad Meymandi, MD, PhD
Melinda B. Michelson, MD
Igor D. Middlebrook, DO
Marcia G. Miedema, PA-C
Aaron J. Miller, MD
Donald S. Miller, MD
Jordan H. Miller, MD
Stacey H. Miller, MD
John K. Min, MD
Gregory J. Mincey, MD
Madhur Mittal, MD, FAAP
Michael J. Modrow, PA-C
Vikki M. Mollette, PA-C
Thomas J. Monaco, Jr., MD
Arl V. Moore, Jr., MD
David F. Moore, Jr., MD
Edgar C. Moore, Jr., DO
John H. Moore, III, MD
John R. Moore, IV, MD
Kenneth E. Moore, MD
Laura P. Moore, MD
Franklin J. Mooring, MD
Koreen Morgan, PA-C
Richard E. Morgan, MD
Tiffany M. Morgan, MD
William G. Morrel, IV, MD
Luke L. Morrison, PA-C
Allison Mullin, PA-C
Colin B. Muncie, MD
John C. Murray, MD
Jennifer H. Myatt, MD
Perry B. Myrick, MD
David A. Nachamie, MD
Madjimbaye C. Namde, MD
Sharad Nangia, MD
David C. Napoli, MD
Madison A. Nation, MD
Vandana Nayal, MD
Mark H. Neely, MD
Leonard D. Nelson, Jr., MD
W. Michael Nesbit, MD
Bryan R. Neuwirth, MD, DDS
Howard W. Newell, Jr., MD, FACP
George B. Newsome, MD
Cynthia M. Norris, MD
Abigail W. North, PA-C
Michael Norton, MD
Pedro J. Nunez, MD
Suzanne H. Nutt, MD
Okechukwu E. Nwoko, MD
Daniel M. Oberer, MD
Megan M. O'Brien, PA
Todd E. Ogrodowczyk, MD
Sarah J. Olenick, MD, PhD
James H. Oliver, III, MD
Kenneth L. Oliver, MD
David E. Ormond, MD
Samuel L. Orr, MD
Albert J. Osbahr, MD, MSCM, FACOEM
Thomas A. Ostergard, MD
Gerald V. Otteni, MD
Dean P. Ouano, MD
Preeti P. Ozarkar, MD
Shyamal K. Palit, MD
Gilbert F. Palmer, MD
Sravan Panuganti, DO
Sophia C. N. Paraschos, MD
Yoosun Park, MD
Susan R. Parlow, MD
Justine M. Parmele, MD, FAAP
Thomas E. Parrish, PA-C
Joshua G. Paschall, MD
Pooja S. Patel, MD
Sushma M. Patel, MD
LaTisha D. Patterson, PA-C
Scott M. Paviol, MD
Gerald Pelletier, Jr., MD
Brian A. Perry, II, MD
Catherine R. Perry, PA-C
Rachel L. Perry, PA-C
Robert D. Peters, MD
Cobern V. Peterson, Jr., MD
J. Duncan Phillips, MD, FACS, FAAP
Mark L. Phillips, MD
Douglas W. Picton, MD
Stephanie J. Plummer, DO
Ricardo O. Pojol, MD, FAAP
David C. Pollock, MD
James M. Polo, MD
Jonathan R. Prentice, PA-C
Thomas L. Presson, MD
Carina A. M. Pringle, PA-C
Nicole Proscia, MD
Annie C. Pugh, MD
Sankalp Puri, MD, FACEP
Aveline Quinlan, MD
J. Laurence Ransom, MD
Tariq Rashid, MD
Candice M. Ray, MD
Jeremy K. Reading, MD
Whitman L. Reardon, MD
Kavya E. Reddy, MD
Michael S. Rees, MD
Thomas E. Register, Jr., MD
Mark E. Reiber, MD
Gregory E. Reichert, DO
David P. Reilly, MD
John L. Remington, MD
Stefan A. Renaud, DO
Mary E. Renze, PA-C
Katlyn E. Rhodes, PA-C
Daniel C. Richard, MD
Brad A. Richter, MD
Erin L. Riley, PA-C
Diana Rivera, PA-C
G. Don Roberson, MD
Virgil O. Roberson, III, MD
W. Earl Roberson, MD
William S. Roberts, MD, FACC
Laurie C. Robinson, MD
Taylor J. Robinson, PA-C
Christopher P. Rodgers, MD
Thomas J. Rojy, Jr., MD
Hal J. Rollins, Jr., MD
Ronald Ross J. Romanelli, PA
Jacqueline L. Rookwood, MD
Steven D. Roos, MD
Raymond T. Rosario, MD
Anelia P. Rose, MD
Michael L. Ross, MD
Glen D. Rowe, DO
Kristina D. Rowe, MD
Samuel J. Roy, MD, DDS
Paul F. Rush, MD
Annemarie I. Russell, MD
John H. Russell, MD
Karel F. Rybnicek, MD
Maged H. Saad, MD
Steven M. Salisbury, II, MD
Bailey Sanders, MD
David L. Sappenfield, MD
Joshua D. Sarett, MD, FACEP
Julia M. M. Sargent, DO
Nakshatra Saxena, MD
Robert E. Schaaf, MD, FACR
Randie Schacter, DO
Debra Schardt-Sacco, DMD, MD
Herman E. Schmid, Jr., MD
Andrew M. Schneider, MD
Gregory G. Schnier, MD
G. Kenneth Scholl, Jr., MD
Jennifer B. Scott, PA-C
Melissa S. Scott, PA-C
Craig J. Secosan, MD
Khaing Z. See, MD
William Lawrence Selby, Sr., MD
Thomas J. Sena, MD
Phillip P. Shadduck, MD
Kinchit K. Shah, MD
Poorvi J. Shah, MD
Pratish A. Shah, MD
Sanjay B. Shah, MD
Frank C. Sheldon, MD
Brian T. Sherrington, MD, FAAP
Kristen M. Shipherd
Marc T. Silver, MD
J. Dale Simmons, MD
Rebecca K. Simpkin, MD
Francis J. Sincox, Jr., MD
Kelley B. Singer, MD
Kimberly R. Singletary, MD
Stephen J. Sladicka, MD
Robert F. Sloop, Jr., MD
Thomas W. Smith, MD
Garrett W. Snyder, DO
Lewis C. Sommerville, MD
John P. Sorge, MD
Diana M. Spahlinger McCarthy, MD, MPH, MS
Sharon Y. Speed, MD
Richard S. Stack, MD
Mark J. Stallworth, MD
Sarah E. Starr, DO
Rebecca R. Steffens, MD
Jane L. Steiner, MD
G. Terry Stewart, MD
Volker W. Stieber, MD
Hunter G. Strader, Jr., MD
Michael Y. Streahle, PA-C
Ashley R. Strickland, MD
Lindsay C. Strowd, MD
Bryan D. Stup, MD
Jennifer J. Styons, MD
Raymond C. Sullivan, Jr., MD
Kevin M. Supple, MD
Angelito C. Sy, MD, FAAP
Jeremy P. E. Sylvanus, MD
Stephen A. Szabo, MD
Gamal Tadros, MD
Paul J. Talerico, MD
Amanda T. Taylor, PA-C
Jacob M. Taylor, PA-C
Jimmy L. Taylor, MD
Robert E. Taylor, MD
Myra L. Teasley, MD
Hillary A. Tester, PA-C
Daniel M. Thailer, MD
Leelee Thames, MD
Christopher L. Tharrington, MD
Ann H. Thomas, PA-C
David S. Thomas, MD
Sandhya A. Thomas-Montilus, MD
Jennifer A. Thompson, MD
Sean L. Thompson, PA-C
Brian D. Thorp, MD
W. Virgil Thrash, MD
Sheel Y. Tolia, DO
Gary M. Toppin, PA-C
Nancy L. Tove, MD
G. Reginald Tucker, Jr., MD
Murray W. Turner, MD
Steven H. Turner, MD
Liliane Z. Tyson, MD
Thurlow R. Underhill, MD
Deepu S. Ushakumari, MD
Raja S. Vadlamudi, MD, MPH, FACP
Robert C. Vanderberry, Jr., MD
Rupashree Varadarajan, MD
Ajay K. Veeragandham, MD
Bernard Velardo, MD
Anne M. Verlangieri, MD
H. Ryland Vest, Jr., MD
Sajeev P. Vettichira, MD
Anton Vlasov, DO
S. Elizabeth von Biberstein, MD, FACS
Jaime S. Wagner, DO
John G. Wagnitz, MD
Constance E. Walker- McMullan, MD
Benjamin E. Wall, MD
Jack G. Wall, MD
Juliann S. Wallner, MD
Zane T. Walsh, Jr., MD
Alex J. Warren, MD
Toni Anne Washington, MD
Lawrence J. Watts, MD
Robert M. Wein, MD
Eryn S. Wells, MSPH, PA-C
Hamilton J. Wells, MD
Patricia W. Wesson, MD
Robert L. West, MD
James W. Wheatley, MD
William B. Wheatley, MD
John W. Whelan, Jr., MD
Winfry E. Whicker, MD
James Allen Whitaker, III, MD
Miles W. Whitaker, MD
Jeffrey J. White, MD
James D. Whitehouse, MD
Robert E. Wiggins, Jr., MD
Christy B. Wild, PA
Caroline L. Wilds, MD
Lauren E. Wilkinson, PA-C
Virgil V. Willard, II, MD
Aerik A. Williams, MD
Jefferson G. Williams, MD
Randall W. Williams, MD
Adam K. Wilson, MD
Nicole M. Wilson, DO
Ted R. Winneberger, MD
Lynne S. Wirth, MD
Beverly F. Womack, MD
Francis P. Wong, MD
Frances O. Wood, MD, FACC
Katherine G. Wu, MD
Chileatha D. Wynn, PA
Richard T. W. Wynn, MD
Wendell G. Yarbrough, MD
Joanna E. York, MD
Maghen K. York, PA
N. William Young, Jr., MD
Robert J. Young, III, PA-C
Robert L. Young, DO
Daniel C. Zedek, MD
Adam S. Zivony, MD
Wins Keep Coming as NCMS Works Hard for YOU!

The NC House has passed several pieces of NCMS-supported legislation recently. Below is a brief summary of several:
HB 576: Healthcare Practitioner Transparency Act - also known as "truth in advertising" - This legislation would require a healthcare practitioner to properly identify their license, certification, or registration (MD, DO, etc.) and shall not display any deceptive or misleading information.
HB 560: Diagnostic Imaging Parity - Would provide health coverage parity for breast cancer diagnostic imaging and would require coverage for certain other types of imaging.
HB 739 - Update Requirements/Advance Healthcare Directives - This patient-focused legislation facilitates access to health care powers of attorney and advance health care directives by modernizing and enhancing the advance care planning process.
Stay tuned to our Morning Rounds newsletter and social channels for more legislative updates.
You can catch up on past legislative updates here.
In Memoriam: NCMS Lifetime Member Dr. Lee Andrew Clark, Jr.

Lifetime NCMS member Lee Andrew Clark, Jr., MD, died April 21, 2023. He was 92.
Dr. Clark attended medical school at UNC, Chapel Hill. In medical school he was inducted into the Alpha Omega Alpha Honor Medical Society. He was President of his medical school class, the class of 1956.
A board-certified Ophthalmologist, Dr. Clark practiced Ophthalmology in Wilson, N.C. from 1962 until 2018, served as Wilson County’s representative to the North Carolina Medical Society, as President of the Wilson County Medical Society, and chaired the Ophthalmological section of the North Carolina Medial Society. He served on the North Carolina Governor’s Advisory Council on Comprehensive Health Planning and also served on the admissions board of UNC’s medical school.
Dr. Clark joined the North Carolina Medical Society in 1963!
Read Dr. Clark's full obituary here.
Experts Warn Teen Eating Disorders More Severe Than Ever

Hospitalizations for eating disorders spiked during the pandemic, doubling among adolescent girls, according to the Centers for Disease Control and Prevention. While most teens have returned to a normal life of in-person school, sports and social activities, eating disorders, especially anorexia, remain at an all-time high, experts warn.
Eating disorder-related health visits — which include hospital stays, pediatrician visits, telehealth talk therapy, and everything in between — more than doubled among people younger than 17 in the past five years, according to a recent report from the data company Trilliant Health. From 2018 through mid-2022, visits among this age group jumped 107.4% across all eating disorders, from around 50,000 visits at the beginning of 2018 to more than 100,000 in 2022. Visits related to anorexia nervosa, which has the highest death rate of any mental illness, jumped 129.26%.

Read the full article here.
NCDHHS Establishes Action Plan Focused on the Well-Being of NC Children

The North Carolina Department of Health and Human Services (NCDHHS) has established a vision for children and families in North Carolina that children are healthy and thrive in safe, stable and nurturing families, schools and communities. A key component of supporting child and family well-being is addressing nutrition security for all North Carolinians. Nutrition security is defined as having consistent and equitable access to healthy, safe, affordable foods essential to optimal health and well-being.
In North Carolina, about 10.9% of the population – about 1.2 million people – are experiencing food insecurity. About 394,000 of those individuals are children, with about one in six children facing hunger. NCDHHS is committed to decreasing the food insecurity rate from 10.9% to 10.0% by December 2024.
The NCDHHS State Action Plan for Nutrition Security outlines an innovative, multi-pronged strategy for achieving that vision – including related goals outlined in the NC Early Childhood Action Plan, Healthy North Carolina 2030, the State Health Improvement Plan, and the NCDHHS Strategic Plan 2021-2023.
Read more about the plan here.
NCMS Supports an Inflationary Adjustment for Medicare Reimbursement

The North Carolina Medical Society has reached out to each of our members of Congress encouraging their support of legislation which would tie the Medicare physician payment schedule to the Medicare Economic Index. H.R. 2474 / Strengthening Medicare for Patients & Providers Act would institute an annual inflation-based update to the Medicare reimbursement formula and put physicians on par with other Medicare providers. The failure of Medicare payment policy to account for inflationary adjustments has resulted in a 22% decline in reimbursement over the past 20 years and has jeopardized North Carolina’s 2.1 million Medicare beneficiaries’ access to care. Through its letter to Congress , the NCMS has partnered with other medical societies in advocating for our members and their patients. Please join in that effort by reaching out to your member of Congress. The AMA has set up an easy online messaging tool for you to reinforce our message, so please do so today.
NCMS Legislative Review: April 28, 2023

What a week!
As discussed last week, NCMS aided in the creation of a new bill to address Prior Authorization, HB 649: Ensure Timely/Clinically Sound Utiliz. Review.
In just one week, the bill passed the House Health Committee, House Rules Committee, and was unanimously passed by all members of the House! In a 112-0 vote in favor of the legislation, the bill has passed its first chamber and will now head to the Senate for their consideration.
House Bill 649 started with physician advocacy and passed the House due to physician advocacy.
NCMS members came together in a Payer Relations Taskforce to identify challenges physicians face in this realm. That taskforce determined that Prior Authorization was their biggest concern for physicians and their patients. This led NCMS staff to work with Representative Baker, Representative Reeder, Representative Potts, and Representative Sasser to create House Bill 649.
NCMS is very thankful to the bill's sponsors and cosponsors for their hard work.
We look forward to the next steps in the Senate!
An Endoscopic Procedure May Help Eliminate the Need for Insulin in People with Type 2 Diabetes

Early research suggests an investigational outpatient endoscopic procedure may help eliminate the need for insulin in people with type 2 diabetes.
Re-cellularization via electroporation therapy (ReCET) uses a specialized catheter to deliver alternating electric pulses to the duodenum to induce cellular regeneration. This process is thought to improve insulin sensitivity, in part, by altering gut hormones and nutritional sensing, principal investigator Jacques Bergman, MD, PhD, said.
"This might be a game changer in the management of type 2 diabetes because a single outpatient endoscopic intervention was suggested to have a pretty long therapeutic effect, which is compliance-free, as opposed to drug therapy that relies on patients taking the drugs on a daily basis," said Bergman, professor of gastrointestinal endoscopy at Amsterdam University Medical Center, Netherlands.
Read more about the procedure here.