NC Commission for the Blind Call for Nominees
The NCMS has the opportunity to appoint a new member to the NC Commission for the Blind. Learn more about responsibilities of the NC Commission for the Blind here.
The commission serves in an advisory capacity on issues relating to services for persons with disabilities, especially independent living programs and services. The council also develops and submits a state plan to monitor, review and evaluate such issues and programs.
Physicians interested in the NC Commission for the Blind position should complete the application form and return it to Evan Simmons, [email protected], by Monday, March 3rd. Interview date for NC Commission for the Blind Appointment (Virtual): the evening of Monday, March 10th.
Appointment Opening for NC Radiation Protection Commission
The North Carolina Medical Society has the opportunity to nominate a member to be appointed by the Governor to the NC Radiation Protection Commission. Learn more about the NC Radiation Protection Commission here.
As described by the N.C. Radiation Protection Act (G.S. §104E), the Radiation Protection Commission is empowered to promulgate rules to be followed in the administration of a radiation protection program. Through its Advisory Committees, the Commission advises the Department of Health and Human Services in the development of comprehensive policies and programs for the evaluation, determination, and reduction of hazards associated with the use of radiation. All 21 members of the Commission (11 voting members from the public and 10 non-voting ex-officio members) are appointed by the Governor.
Physicians interested in the NC Radiation Protection Commission position should complete the application form and return it to Evan Simmons, [email protected], by Monday, March 10th. Interview date for NC Radiation Protection Commission Appointment (Virtual): the evening of Tuesday, March 18th.
NCDHHS, Trillium Health Resources Announces New Crisis Centers

GREENVILLE, N.C. – The North Carolina Department of Health and Human Services and Trillium Health Resources will award $13.15 million to four providers to open community crisis centers and behavioral health urgent care centers (BHUCs) in Lenoir, New Hanover and Pitt counties. The funding was made possible through a historic $835 million investment in North Carolina’s behavioral health system to ensure people have access to the right mental health services at the right time in their communities.
Community crisis centers (also known as facility-based crisis centers or FBCs) and BHUCs give people experiencing a behavioral health emergency alternatives to emergency departments when seeking the care they need. NCDHHS’ investments in the crisis response system will increase North Carolina’s ability to provide behavioral health urgent care by more than 69% and community crisis stabilization by 32% over the next few years.
“People need safe places to go when they are in crisis,” said Kelly Crosbie, MSW, LCSW, Director of the NCDHHS Division of Mental Health, Developmental Disabilities, and Substance Use Services. “NCDHHS is working hard in partnership with LMEs like Trillium and with crisis service providers to ensure that people have a safe place for help when they are experiencing a mental health or substance use crisis.”
NCDHHS partnered with Trillium to select locations for the new centers based on several criteria, including regional data on the number of individuals waiting for mental health and substance use care in emergency departments and the center’s proximity to other community services. Each new facility will help individuals who receive care successfully return home with wrap-around services. The new centers will open in 2025 and join a network of 24 facility-based crisis centers in 22 other counties across the state.
The chosen providers and locations include:
- RHA Behavioral Health NC, New Hanover County
- Easterseals PORT Health, Pitt County
- Integrated Family Services, Pitt County
- S&H Youth and Adult Services Inc., Lenoir County
“Trillium Health Resources is excited to contribute to health equity and access across our counties. These facilities will make it easier for residents to get the care they need when they need it,” shared Joy Futrell, Trillium’s CEO. “Each of these providers are well-respected and recognized in their communities and we are proud to partner with NCDHHS on this project.”
Community crisis centers (FBCs) provide short-term, inpatient mental health stabilization and substance use detox for people in the community who otherwise would need to go to a hospital. Services will increase access to assessments and behavioral health or I/DD treatment. In addition to FBCs, BHUCs are part of a continuum of services that will advance North Carolina’s behavioral health crisis response system by improving options from the moment of crisis to the point of care. These facilities increase the number of spaces where someone can go to get behavioral health care when in crisis. [source]
Nominations Now Open for NCMS Leadership Positions
The NCMS Nominating and Leadership Development Committee Submits:
Call for Nominations:
- NCMS Board of Directors
- NC American Medical Association Delegation
- Nominating and Leadership Development Committee
Overview
The call for nominations for individuals to serve on the NCMS Board of Directors, NC American Medical Association Delegation, and Nominating and Leadership Development Committee are now open.
NCMS Board of Directors
- President-Elect: OPEN
- Region 2 Representative: Charul Haugan, MD (eligible for an additional term)
NC American Medical Association Delegation
- AMA Delegate: Mary Ann Contogiannis, MD (eligible for an additional term)
- AMA Delegate: Justin Hurie, MD (eligible for an additional term)
Nominating and Leadership Development Committee
- NLDC Region 1: OPEN
Nominations are due by May 30, 2025 (click here to view Nomination Form).
Process
Step 1: Candidates are nominated or may nominate themselves for a leadership position on the NCMS Board of Directors, NC American Medical Association Delegation, and Nominating and Leadership Development Committee (click here to view Nomination Form).
Step 2: Once a candidate submits their nomination form, they will receive an email confirmation and made aware of any follow-up if needed.
Step 3: Upon careful review of submitted materials, the Nominating and Leadership Development Committee (NLDC) will select candidates to be interviewed. Candidates will be notified via email by May 30, 2025, if they are selected for an interview. Interviews will take place via videoconference on Saturday, June 14, 2025.
Step 4: The NLDC will present the initial slate of candidates to NCMS membership on July 24, 2025, including a nomination form for Specialty Society-Component Society nominations. Specialty Society-Component Society nominations are due by August 8, 2025.
Step 5: Following any additional candidate interviews, the NLDC will select a final slate of candidates to be approved by the NCMS Board of Directors that will then be brought before the NCMS membership for a vote.
Step 6: The voting period for the elected positions will begin for all Active NCMS Members (Members who have paid 2025 dues) on September 25, 2025, and will end on October 9, 2025. Election results will be announced at the NCMS Annual Business Meeting on October 11, 2025.
All nominations and any information collected as part of the nominating process is strictly confidential.
For more information or questions about the nominating process, please contact Evan Simmons at [email protected].
Funding Available to Practices Impacted by Helene

At his Friday, January 31st press conference in Boone, Governor Josh Stein announced that $30 million in grants is now available to small businesses impacted by Hurricane Helene. The funding application process is now open and can be accessed online here.
A practice that qualifies . . .
- Is a for-profit business actively registered with the North Carolina Secretary of State (or a sole proprietorship with an active DBA filing)
- Is physically located in one of the following Western North Carolina counties: Alexander, Alleghany, Ashe, Avery, Buncombe, Burke, Caldwell, Catawba, Cherokee, Clay, Cleveland, Gaston, Graham, Haywood, Henderson, Jackson, Lincoln, Macon, Madison, McDowell, Mitchell, Polk, Rutherford, Surry, Swain, Transylvania, Watauga, Wilkes, Yadkin, Yancey; or is located in the Qualla Boundary
- Business was formed and in operation on or before 9/27/23
- Had $2,500,000 or less in 2023 annual gross revenue
- Has sustained physical or economic damage (not covered by insurance or other funding sources) from Hurricane Helene
- Is currently operating or plans to reopen
Applications will be accepted until February 21, 2025.
Governor Stein’s announcement is available here.
Capitol Chronicle: Medicare Pay Fix Legislation Introduced

Medicare Pay Fix Legislation Introduced
Congressman Greg Murphy, MD lead sponsor
Among the important unresolved congressional issues that were pending at the conclusion of 2024, the fight to reverse the cut in Medicare payment has resumed. Congressman Greg Murphy, MD (NC-3), along with a bipartisan group of his House colleagues, has introduced new legislation to stop the 2.83% cut in Medicare physician payment while also providing a positive payment update to help practices absorb the increasing costs they are facing.
The bill, Medicare Patient Access and Practice Stabilization Act, provides for a 6.62% payment increase beginning April 1, 2025 and remaining in effect through the end of the year. The adjusted pay rate would offset the cut during the first three months of the year and add an inflation-based payment increase.
Dr. Murphy shared the following statement upon introduction of the legislation:

"Physicians in America are facing unprecedented financial viability challenges due to continued Medicare cuts. Access to affordable and quality health care for millions of seniors is in severe jeopardy," said Congressman Greg Murphy, M.D. "Doctors see Medicare patients out of compassion, not for financial gain. The cost of caring for a Medicare patient far outpaces the reimbursement that physicians receive for seeing them. On top of that, the expense of providing care continues to rise due to medical inflation. This inflation, coupled with declining reimbursement rates, creates enormous financial pressures on physicians, forcing many to retire early, stop accepting new Medicare patients, or sell out to larger, consolidated hospital systems, private equity, or even insurance companies. The future of private practice medicine, the most cost-efficient and personalized care, is in dire straits. This bipartisan legislation prevents further cuts, provides a modest inflationary adjustment to help ease the cost of care, and ensures Medicare remains viable for both doctors and patients."
When adjusted for inflation, Medicare payment to physicians has declined by 33% over the past 24 years.
The NC Medical Society has been and continues be engaged in the fight to reverse the Medicare payment cut and applauds Congressman Murphy and his House colleagues for re-energizing the effort to preserve and increase Medicare beneficiaries’ access to the care they deserve. North Carolina physicians have made it clear that they cannot absorb another Medicare cut and that access to care will decline for Medicare patients if Congress does not take action.
As the pace of legislative activity on Capitol Hill increases, reversing the trend of Medicare physician payment cuts is a top priority. The NCMS is engaged with our members of the House of Representatives to encourage support of the Medicare Patient Access and Practice Stabilization Act, and we are encouraging our members of the Senate to introduce and support a companion bill in that chamber.
🎉It's New Member Monday!🎉

Join us in welcoming these new members to the North Carolina Medical Society!
- Rachel M. Concepcion, DO
- John B. Jasper, II, MD
- Susannah E. Johnson, MD
- Katherine P. Kaufman, MD
- Olan B. Kemp, MD
- Barbara E. Kissam, MD
- Jacqueline A. Lamson, DO
- Andrew H. Marky, MD
- Sean E. McGarr, DO
- Daniel A. Pierce, MD
- Jack E. Pulwers, MD
- Brianna R. Schmidt, MD
- Molly Sohn
- Michael S. Sullivan, MD
- Erin S. Thoma, DO
- Janice M. Westphal, MD
- Jonathan N. Wilcock, DO
- Ruhin Yuridullah, MD
We are thrilled to have you!
Not a member but would like to be? Joining is simple. Visit our membership center here.
Happy Birthday to Our Members Celebrating This Month!
Grab your party hats and noisemakers and let’s celebrate!
Elizabeth Acquista, MD
Amer Adam, MD
J. Wellington Adams, MD
Andrew J. Adamson, MD
Satish P. Adawadkar, MD
Ira N. Adler, MD
Deborah G. Agisim, MD
Sukaina Ahmad, MD
Farhan Ahmed, MD
Richard E. Akers, Jr., MD
Rozita Akhbari, MD
Shereen A. Alavian, MD
Catherine M. Alexander, MD
Eslam G. K. Ali, MD
David R. Allen, Jr., MD
John G. Alley, Jr., MD
Eric D. Alpert, MD
Michael K. Altenburg, MD
Fabian E. Alzamora, MD
David A. Ames, MD
Lisa A. Andersen, DO
William D. Andersen, MD
Kent T. Anderson, MD
Mark W. Anderson, MD
Micaela D. Antzoulatos, PA-C
Howard L. Armistead, Jr., MD
Don M. Armstrong, MD, FACOG
Moogali M. Arvind, MD
George L. Auman, MD
Maria Lourdes C. Austria, MD
Anthony F. Azzi, MD
Carter S. Bagley, MD
Elizabeth R. Bagsby, MD
Khosrow Bahrani, MD
Patrick L. Ballen, MD
Usha Balmuri, MD
Robert J. Baranello, Jr., MD
Jose A. Bardelas, Jr., MD
Graham A. Barden, III, MD, FAAP
Kelly L. Barham, MD
Kelsey J. Barr, MD
Thaddeus J. Barringer, Jr., MD
Michael J. Bartiss, MD
Paul J. Bartleson, DO
Mary E. H. Belet, PA
Eugene D. Bell, III, MD
John M. Benbow, MD
Deanna M. Bencic, PA-C
Suzanne S. Benton, MD
Carl W. Berk, MD
Michael B. Berry, MD
Todd M. Beste, MD
Avery A. Bevin, MD
Michael A. Biggerstaff, MD
Douglas W. Bitzer, PA-C
Justin C. Black, MD
Douglas L. Boertje, MD, FAAP
Terrence D. Bogard, MD
Christina M. Bowen, MD
Stephen L. Bower, MD
Stephen E. Boyce, MD, FACS
Michael E. Brame, MD
Alex G. Brann, PA-C
Simon David Braun, MD
Vaughn G. Braxton, MD
Mark S. Brazinski, MD
Miguel A. Brito, Jr., MD
Michael S. Broder, MD
Dora M. Brodie, MD
Carolyn C. Brookhart, MD
Grant Brown
Mark S. Brown, MD, FACS
Vera C. Bude, MD
John H. Bumgarner, MD
Elizabeth M. Bunting, PA-C
Craig N. Burkhart, MD, MPH
Paul L. Burroughs, Jr., MD
William E. Byrd, MD
Jack R. Cahn, MD
Rebecca S. Carlin, MD
Lindsay A. Carnes, PA-C
Lisa M. Carroll, MD
Trevor D. Carroll, MD
Ralph E. Carter, III, MD
Michael C. Casciello, MD
Sarah H. Cash, MD
Caroline F. Chamberlain, PA-C
Leon D. Charkoudian, MD
C. Lynn Cheng, MD
Samuel J. Chewning, Jr., MD, MBA
Elie B. Choufani, MD
C. Franklin Church, MD
Caroline A. Clark, PA-C
Greg L. Clary, MD
Adriana I. Cline, MD
Kenneth K. Cloninger, MD
Brian S. Coan, MD
G. Glenn Coates, MD
L. Gregg Colvin, MD
Jason T. Combs, MD
Orlando Conty, MD
Jeffrey J. Cook, MD
William C. Corbett, MD
William M. Cottrell, MD
Christopher T. Coughlin, MD
Mark M. Couture, MD
Gary P. Cram, Jr., MD
William F. Credle, Jr., MD
E. Brown Crosby, MD
Kenneth Crosby, Jr., MD
David B. Crosland, MD
Cesar P. Cube, MD
Michael J. Cullura, DO
Richard E. Cummings MD, MD
Robert F. Dallapiazza, MD
Richard C. D'Alonzo, MD
Manish N. Damani, MD
Evan F. Dapo, PA-C
Zaki K. F. Dard, MD
Kimberly A. Darlington, PA-C
Harlan B. Daubert, MD
German D. De Joya, MD
Dawn E. de Neef, MD, FACS
Christian T. deBeck, MD
Joseph M. DeBord, MD
Christopher B. Deery, MD
David Defeo, MD
Alberto E. Del Valle de Laosa, MD
Stephen D. DeMeo, DO
Lindsey M. Deschamps, MD
Zana Devlin, PA-C
Amanpreet S. Dhaliwal, PA-C
E M. DiLizia, MD
W. Roger Domby, MD
Robert Dorlon, Jr., MD
Kristen M. Dorsey-Leake, MD
W. Rodwell Drake, Jr., MD
Matthew J. Duggan, MD
Jack N. Dunn, MD
Elizabeth A. Eagle, MD
Wesley S. Eagle, PA-C
Tally H. Eddings, III, MD
David B. Eddleman, MD
Brian E. Edwards, MD
R. Elizabeth Edwards, PA-C
Howard J. Eisenson, MD
Laura T. Ekka, MD
Daniel W. Entrikin, MD
Samantha Ericksen, PA-C
Stephen D. Ertischek, MD, FACP
John A. Fagg, MD
Heather J. Firebaugh, MD
E. Carl Fisher, Sr., MD
Keri A. Fitzsimmons, MD
George E. Fleming, MD
Damon A. Forbes, MD
Sharon M. Foster, MD, FAAP
William B. Fowler, MD
Douglas G. Freeman, Jr., MD
Mark K. Fromke, MD
Sam R. Fulp, MD
Angela B. Gantt, MD, FACOG
Idalina Garcia-Hruby, MD
Alyssa W. George, MD
Hannah M. Gilbert Brame, PA-C
Jordan M. Glaser, MD
Donald B. Goodman, Jr., MD
John P. Goodson, MD
Karyn B. Gordon, MD
Varun Y. Goswami, MD
Charles D. Graham, DO
Hugh J. Grant, Jr., MD
Gretchen E. Green, MD
Robert L. Green, MD
Eleanor E. W. Greene, MD, MPH
Paul R. Greenlaw, MD
Kyle F. Grimaldi, MD
Matthew M. Grove, DO
Joseph Guarino, MD, MPH, FACOEM
G. Patrick Guiteras, MD
James C. Gunnells, MD
Ashok K. Gupta, MD
Rachel H. Hagler, MD
C. Michael Hahn, MD
W. Dana Haithcock, Jr., MD
Jennifer J. Hall, MD
Nady Hamid, MD
P. J. Hamilton-Gaertner, MD, MHA
Michael G. Hankewycz, MD
Norris B. Harbold, Jr., MD
Rita A. Harbury, PA-C
C. Blair Harkness, MD
Wallace T. Harris, MD
Alexandria C. S. Hart, MD
Allan B. Harvin, MD
Elizabeth H. Hawes, PA-C
Rodney J. Hawk, MD
William L. Haynes, MD
Joseph R. Hedgpeth, MD
Hughes M. Helm, MD
Robert C. Helms, MD, FAAP
William C. Helton, MD
David F. Henderson, PA-C
Nancy S. Henley, MD, FACP
Lloyd A. Hey, MD, MS
John M. Hicks, MD
Steven P. Higgins, MD
James R. Hodges, MD
Katrina J. Hodgkins, PA-C
Christen W. Hoedt, MD
Jeremy J. Hoff, DO
James R. Hoffman, DO
Rachael B. Hollifield, DO
James P. Hooten, Jr., MD
Heather M. Hopper, PA-C
Fatima Hossain, MD
Mahmood H. Hosseinian, MD
William A. Hough, III, MD
G. Van Huffmon, III, MD, FACS
James D. Hundley, MD
Dori L. Hunt, MD
Sarah O. Hunt, MD, FAAP
Gary J. Hunter, DO
Joe P. Hurt, MD, PhD
J. Mark Hylton, Jr., MD
Jennifer A. Ingersoll, MD
Stephen D. Jackson, MD
Giuseppina A. Jacob, DO
Peter L. Jacobson, MD, FAAN
Astrid G. Jain, MD
W. Bryan Jennings, DO
Grace M. Jere, MD
Edward W. Jernigan, III, MD
Albin W. Johnson, MD
Gregory J. Johnson, MD
Lynn R. Johnson, MD
Randall D. Johnson, MD
Sara G. Johnston, PA-C
Jerry D. Joines, MD
Jamande A. Jones, MD, MS
Perrin W. Jones, MD
Timothy D. Jordan, MD
Michael Josilevich, MD
Raymond E. Joyner, MD
teri C. jumpa, PA
Ki S. Jung, MD
Robert H. Kahn, MD
Charlotte K. Karriker, MD
Alison S. Kavanaugh, MD
Arthur E. Kelley, MD
Mark H. Kelly, MD
R. David Kemp, MD
Kevin Z. Kinlaw, MD
Stephen L. Kinser, MD
Hayden P. Kirby, MD
Megan D. Kirk, MD
Nathan R. Knapp, MD
Mary G. Knox, MD
Richard A. Koch, MD
Keith R. Kooken, MD
Aaron C. Kopp, PA-C
Edward W. Kouri, MD
Harald H. Kowa, MD, FAAP
Brian A. Krakover, MD
Gregory J. Kramer, MD
Eric M. Kraus, MD, MS
Larry L. Kroll, MD
Benjamin P. Kunesh, MD
William A. Kutner, Jr., MD
Heston C. LaMar, MD
Leta Sue C. Lamb, MD
Ronald W. Lane, MD
Stephen N. Lang, MD
Grainger S. Lanneau, MD
Kurt K. Lark, MD
Marzena T. Laszewski, MD
Lindsay R. Lavin, MD
William W. Lawrence, Jr., MD
Adrian W. Laxton, MD
Brian H. T. Le, MD
Daniel A. Leach, MD
John M. Leahy, MD
Il S. Lee, MD
W. Hampton Lefler, Jr., MD
Aaron P. Leininger, MD
Anthony P. Leonard, MD
Gabrielle G. Leonard, MD
Kathleen C. Leone, MD
Elizabeth A. Lidiard, PA-C
John D. Lilley, MD
Arthur J. Lim, MD
Meredith S. Linger, PA
Scott W. Lisson, MD, FACS
Bryan J. Loeffler, MD
Kevin J. Logel, MD
Alexandra G. Lorentsen, MD
Shelly S. Lowery, MD
Katie Lowry, MD, MPH
Yuan Lu, MD
Brianna E. Maglio, PA-C
Jonathan A. Malin, MD
Erik A. Manring, MD
Arie Mantin, MD
Monica A. Manzi, PA-C
Kenneth C. Marburg, MD
Patrick S. Markwalter, MD
Rana Marzouq, MD
William T. Mason, MD
Carolyn H. Maynor, MD
Pamela A. Mbang, MD
Benjamin W. McClintock, MD
Diana C. McClinton, MD
Katherine V. McClure, PA-C
Mark W. McClure, MD, FACS
Shannon M. McCrann, DO
Brooks W. McCuen, II, MD
Molly W. McElroy, PA-C, MSPAS
Matthew D. McEntire, PA-C
Leah H. McGuire, PA-C
Grant W. McKenzie, MD
Melvin D. Medlock, Jr., MD
Megan S. Melendez, PA-C
Thomas E. Melin, MD
Gregory S. Metcalf, MD
Jayson R. Miedema, MD
David C. Miller, MD
Horace W. M. Miller, IV, MD
Howard E. Miller, MD
James T. Mills, Jr., MD
Stacy A. Mills, PA
Thomas H. Milner, III, MD
Challie A. Minton, MD
Douglas W. Miyazaki, MD
Robert C. Moffatt, MD
William G. Moorefield, Jr., MD
Edgar S. Moser, Jr., MD
Samuel L. Moskowitz, MD
Morgane E. Naveau, MD
Alexa B. Nelson, PA-C
J. Gregory Nelson, MD
Christopher J. Nguyen, MD
Mai Trang L. Nguyen, MD
Lauren P. Nicola, MD
Jerry D. Nix, MD, FACEP
John R. Nixon, MD
Thomas L. O'Connell, MD
Christopher W. Olcott, MD
Dale W. Oller, MD
Marci L. Olsen, PA-C
Jacob A. Orbock, MD
Sarah R. Orlousky, MD
T. Lane Ormand, MD
Nahla A. M. Osman, MD
Michael R. Ott, MD
Robert A. Ottaviani, MD
Derya Ozkok, MD
Gupta Pandarinath, MD
Steven T. Pantelakos, MD
Young K. Park, MD
Morgan J. Parker, DO
Bhumi A. Patak, MD
Anand R. Patel, MD
Nilesh P. Patel, MD
Nirali M. Patel, MD
David R. Patterson, MD
James B. Patterson, MD
Leigh A. Patterson, MD
Thomas E. Pendergrast, MD
A. Thomas Perkins, IV, MD, PhD
Randy A. Peters, MD
Kirk A. Philpot, MD
Isadore M. Pike, MD
Steven R. Plunkett, MD
Saurav Pokharel, MD
William G. Porter, MD
James M. Potts, MD
Josie D. Prabhakar, PA-C
M. Canaan Prater, DO
Philip A. Price, PA-C
Thomas J. Pulliam, MD, MMM
William R. Purcell, MD
Joseph P. Pye, MD
Megan E. Quigg, PA
Rachel E. Raab, MD
Evelyn A. Rabindran, MD
Dale K. Rader, MD
Wanda L. Radford, MD
Gary T. Raflo, MD
Richard L. Rauck, MD
Ashley R. Rawls, PA-C
Lawrence W. Raymond, MD, FACP, FACOEM
Eileen M. Raynor, MD, FACS, FAAP
Kelli A. Reardon, MD
Erika L. W. Rice, DO
William C. Rice, MD
James J. Richard, PA
Jill R. Roberson, MD
Tia L. Robertson, MD
Stefanie M. Robinson, MD
David A. Rockwell, MD
Danielle M. Rose, MD
Eric R. Rosenberg, MD
Shepherd F. Rosenblum, MD
Charles E. Rowe, Jr., MD
John Rubino, MD
Alfred J. Rufty, Jr., MD
Samuel B. Ryburn, MD
Smita N. Sampat, MD
Kelvin K. Sampson, PA
Fernando A. Sanchez-Brugal, MD
Shiraz M. Sandhu, DO
Melanie B. Sanford, MD
Shireesha Sangineni, MD
Wade H. Saunders, III, MD
Kenneth J. Sauve, MD
Emily R. Sawyer, MD
Dawson E. Scarborough, MD
Kerri R. Scherer, MD
Thomas M. Schmelzer, MD
Derek Q. Schroder, MD, FACP
Beth A. Schulz-Butulis, DO
Christopher J. Schwarz, MD
Fred A. Scialabba, MD
Kacey Scott, MD
Stephen S. Scott, MD
John M. Seddon, MD
John Aldus Alexander Seldomridge, MD
Frank B. Sellers, MD
Elzada H. Sercus, MD
Christopher N. Shatley, PA-C
Michael P. Shea, MD
Donna L. Shelton, PA-C
Lisa P. Shock, DrPH, PA-C, MHS
Douglas J. Shusterman, MD
Tiffany M. Sills, MD
Lawrence R. Singer, MD
Maggie L. Small, PA-C, MHS
Timothy H. Smelzer, MD
Brian S. Smith, MD
Julian K. Smith, PA-C
Mark D. Smith, II, MD, FACS
Melissa M. Smith, MD
Patricia W. Smith, MD
Amy H. Sobel, MD
Anna Melissa Solum, MD
Lewis C. Sommerville, III, MD
Taylor South, MD
Kevin M. Spangler, MD, PhD
John M. Spargo, MD
Jeffrey D. Sparks, MD
Nathaniel L. Sparrow, MD
Michol Stanzione, DO
Kevin R. Stein, MD
James A. Stevens, Jr., MD
Jeremy R. Stinson, PA-C
Scott C. Stoioff, MD
Lauretta G. Stombaugh, DO
Woodhall Stopford, MD, MPH
Maria De Lourdes L. Sturchler, MD
Parker P. Suit, DO
Rebecca Sullenger
Kavita H. Sura, PA-C
Viswanathan Swaminathan, MD
Sandra L. Swanson, MD
Thomas M. Swantkowski, MD, AGAF, FACG
Jonas J. Swartz, MD
Jessica R. Swavely, DO
Munther S. Tabet, MD
Julia W. Tang, MD
Charles S. Tara, MD
Gregory J. Taraska, MD
Nancy L. Teaff, MD
Robert D. Teasdall, MD
Robert K. Thacker, MD
Julie Thamby
Alan E. Thomas, MD
C. Aaron Thompson, MD
Richard W. C. Tim, MD
Oguz Tok, MD
Kenneth G. Tomberlin, MD
Nicole S. Toney, MD
Andres H. Torop, MD
Eric A. Toschlog, MD, FACS, FCCM
Nancy J. Toy, MD
Nicholas A. True, MD
John T. Tseng, MD
Jordan E. Tunno, PA-C
Harrison G. Tuttle, MD
Bhavna Vaidya, MD
Douglas C. Vander Kooi, MD
Jaime J. Vanourny, MD
Jill S. Vargo, MD
Mihaela A. Vatca, MD
Wayne B. Venters, MD
Lizette S. Villacorte, MD
Thomas T. Vradelis, MD, FACOG
Josip Vukina, MD
Tomas Vybiral, MD
Jason A. Walker, MD
Antoinette W. Wall, MD
James W. S. Wallace, MD
Bobby C. Walters, Jr., MD
W. Alan Ward, MD
L. Patrick Warren, Jr., MD
Sean M. Warsch, MD
Steven T. Wasserman, MD
Shannon A. Watterson, PA-C
John C. Watts, III, MD
Michael D. Weaver, MD
Richard A. Weintraub, MD, FACP
Kelly L. Weitz, PA-C
Andrew H. Wells, MD
Matthew C. Wendt, MD
Susan M. West, MD
Carl J. Westcott, MD
Melissa K. Wester, MD
Trent W. Wester, MD
Kenneth S. White, MD
Edward W. Whitesides, MD
Daniel Whitley, Jr., MD
Walter F. Wiggins, MD, PhD
Heather N. Williams, MD
Judson B. Williams, MD
Kathryn S. Williams, MD
Tawanda B. Williams, MD
Michael L. Williford, MD
Jason A. Wilson, MD
Matthew W. Wilson, MD
Gabriel B. Winberry, MD
James E. Winslow, MD
James W. Winslow, MD
Kenneth H. Winter, MD
Steven C. Winters, MD
Joel A. Wissing, MD
Peter H. Wittenberg, MD
Jordan E. Wong, DO
Kully L. Woodruff, MD
Julie C. Woodside, MD
Vanessa S. Workman, MD
Darren S. Wright, MD
David K. Wright, MD
Andrew W. Wyker, DO
Che-Ming Yang, MD
Joylyn D. Yeazell, MD
Adam C. Younis, MD
Terri L. Zacco, DO
Peter A. Zeman, MD
Li Zhou, MD
Shams Zia, MD
James H. Zuger, MD
Charles S. Zwerling, MD
Foundation Friday! Thank You to These NCMS Foundation Donors.

Today, the NCMS Foundation recognizes donors who have joined us on the journey in 2025 to keep the Foundation READY TO RESPOND.
These individuals are contributing to enable clinician leaders to respond quickly to the next health challenge.
- Paul R. G. Cunningham, MD
- Lacy C. Hobgood, MD, FACP
- Joseph T. Inglefield, III, MD
- Michelle F. Jones, FAAFP, MD
- Lyndon K. Jordan, III, MD, FACR
- Jugta Kahai, MD, FAAP
- Katie Lowry, MD, MPH
- Venkat Prasad, MD, MBA, MHA
- Timothy J. Reeder, MD, MPH, FACEP
- Steven M. Shaber, JD
- Edward W. Whitesides, MD
- Yunxiang Zhu, MD
Thank you for your continued support to help all North Carolinians achieve their optimal state of health.
Be part of the solution and learn more about how YOU can make a difference too here.
Bird Flu Hits North Carolina Turkey Flock as Outbreak Intensifies
The North Carolina Department of Agriculture recently confirmed a commercial turkey flock in the state has tested positive for highly pathogenic avian influenza (HPAI), commonly known as bird flu.
The affected flock, located in Sampson County, marks the second case of bird flu in North Carolina this year, according to WRAL-TV. The first case was reported earlier this month in Hyde County.
The U.S. Department of Agriculture (USDA) reported that more than 107 flocks nationwide have tested positive for the virus so far this year.
The USDA says there is currently no evidence that humans can get bird flu from eating poultry or eggs, but health experts emphasize the importance of taking precautions for those working with birds, including washing hands and changing clothes after contact. [source]
Senate Moves to Reauthorize Dr. Lorna Breen Health Care Provider Protection Act

U.S. Senators Tim Kaine (D-VA), Todd Young (R-IN), Jack Reed (D-RI), and Roger Marshall (R-KS) introduced bipartisan legislation to reauthorize the Dr. Lorna Breen Health Care Provider Protection Act, a comprehensive law Kaine, Young, Reed and Marshall successfully passed in 2022 to help prevent suicide, burnout, and mental and behavioral health conditions among health care professionals.
The law has already provided $100 million in funding for mental health care for providers across the country, including $5.6 million in federal funding for Virginia providers at UVA Health, Virginia Commonwealth University, and George Mason University. But provisions of the law that made this funding possible expired last year. The Dr. Lorna Breen Health Care Provider Protection Reauthorization Act would reauthorize these grant programs for five years.
Specifically, Dr. Lorna Breen Health Care Provider Protection Reauthorization Act would:
- Reauthorize a grant program for health care organizations and professional associations for employee education on strategies to reduce burnout, peer-support programming, and mental and behavioral health treatment for five years. Communities with a shortage of health care workers, rural communities, and those experiencing burnout due to administrative burdens, such as lengthy paperwork, will be prioritized.
- Reauthorize a grant program for health profession schools or other institutions to train health care workers and students in strategies to prevent suicide, burnout, mental health conditions, and substance use disorders for five years.
- Reauthorize a national evidence-based education and awareness campaign. Currently, the campaign provides hospital and health system leaders with evidence-informed solutions to reduce health care worker burnout. Reauthorization will provide resources for the campaign to continue and expand beyond its current scope.
Full text of the bill is available below:
Lorna Breen bill text
[source]
Register Now! Collaborative Care Model 2025 Learning Collaboratives
NC AHEC is announcing six (6) Collaborative Care Model (CoCM) Learning Collaboratives for primary care providers, behavioral health professionals, and others who have implemented or are implementing CoCM for integrating behavioral health in a primary care setting. Independent primary care practices, FQHCs, and rural health clinics may find CoCM especially helpful for meeting some of the behavioral health needs of their patients.
CoCM Learning Collaboratives will highlight collaborative care team integration and the role of the CoCM Behavioral Health Care Manager for practices new to the model and those established with implementing CoCM. Sessions will run once a month from noon-1 p.m. January through June 2025 and will include the following topics:
- January 30, 2025 • Best Practices of Care Managers
- February 20, 2025 • Billing and Quality Metrics
- March 20, 2025 • Clinical Assessments for Care Managers & Documentation for Care Managers
- April 17, 2025 • Supportive Language and Engagement Strategies for CoCM Patients
- May 29, 2025 • Effective Tools to Enhance CoCM
- June 19, 2025 • Best Practices Psychopharmacology for BHCMs
View or download a sharable flyer here.
For additional information about the model, click here.
Baxter: All Manufacturing Lines at NC Plant Restarted

On January 28, Baxter announced that it has resumed IV solutions production across all manufacturing lines at its North Carolina facility, which was affected by Hurricane Helene in October.
While some lines will need additional time to ramp up, the company anticipates that production will reach pre-hurricane levels by early Q1 2025.
Let's Get Social! Join NCMS in Raleigh February 28th!
Relax and build community with NCMS!
Join us at the StateView Hotel
February 28th, 2025

Physicians, PAs, Residents & Students
Bring your colleagues, family and friends!
Lobby Bar at the StateView Hotel, Raleigh
2451 Alumni Drive
Raleigh, NC 27606
February 28th
6-8pm
Drinks and snacks will be provided!
REGISTER NOW!
If you cannot register at the above link or need more information, please contact Toni Hill, [email protected].
Preceptor Hub Shaping Healthcare, Bringing Future Doctors to Outer Banks

In response to a growing medical care crisis, Manteo formed a Health Care Task Force in 2022 to tackle the challenge of attracting and retaining medical professionals. As part of this effort, the preceptor program was introduced, which pairs final-year medical students with experienced professionals to gain valuable hands-on experience.
In medical training, a preceptor is an experienced practitioner who provides supervision during clinical practice.
Franklin Walker, Vice President of the North Carolina Medical Society (NCMS), shared that the preceptor program can be an effective recruiting tool, especially for rural communities.
“It’s getting them into the rural communities and getting a taste of what goes on,” he said. “Hopefully this can be a recruitment not just for us, but for the rural communities, to try to entice medical personnel to our communities.”
In February of last year, Walker proposed the idea of Manteo becoming a preceptor hub to the Health Care Task Force. Since then, six students have participated in Manteo, Engelhard, and Ocracoke. The program is currently partnering with two North Carolina schools, Campbell University and UNC School of Medicine. Students typically spend one to three weeks at the preceptor locations, depending on their course requirements.
Any medical professionals who might be interested in working with students can contact Franklin Walker at [email protected].
You can read the full article here.
New Generative AI Tool Unveiled for Emergency Medicine

Abridge launched a new gen AI product for emergency care, and it's currently in use at several health systems including Deaconess Health System, Emory Healthcare, Johns Hopkins Medicine and UChicago Medicine.
Abridge Inside for Emergency Medicine was developed as part of Abridge's participation in the Epic Workshop program. The program features third-party vendors that are co-developing technology with Epic.
Abridge's new gen AI product was developed to suit the needs of emergency medicine as it integrates with Epic’s note drafting workflows for emergency department clinicians and works with Epic’s ASAP module in Haiku and Hyperspace, according to the company.
Clinicians can select patients from the department’s Track Board and begin an ambient recording immediately with Haiku, Abridge executives said.
Abridge’s automatic speech recognition models detect specialty, language and multiple speakers, without manual setting adjustments, to create an accurate transcript and clinical documentation.
Continue to the full article here.
Winter Storms, Illness Fuel Blood Donations Slump

According to the American Red Cross, an increase in respiratory illnesses is contributing to a decline in blood and platelet donations across North Carolina this winter. Records show more than 2,000 cases of respiratory illnesses, including the flu, have been reported among hospital admissions statewide this year. The agency notes that the winter months are especially difficult for blood donations due to seasonal illnesses, harsh weather, and the demands of the holiday season.
Winter storms and wildfires in California have resulted in the American Red Cross cancelling about 500 scheduled donation drives, leading to more than 10,000 missed blood and platelet donations. Platelets are crucial for treating burn victims, trauma patients, cancer patients, and others in need.
January is National Blood Donor Month. Individuals are encouraged to donate. To find out more on blood donation eligibility and donation centers near you, visit he American Red Cross website.
Read the full article here.
In Memoriam: NCMS Life Member Dr. William Gresham Orrison
Dr. William Gresham Orrison
June 30, 1943 - January 15, 2025

NCMS Life member Dr. William Gresham Orrison died on Wednesday, January 15. He was 81 years old.
Gresham's very full life revolved around family, friends, community, and service to others. A caring doctor and skilled eye surgeon, he took pride in improving, and sometimes saving, his patients' eyesight. An entrepreneur and astute businessman, he enjoyed collaborating with others to bring old buildings back to life, help downtowns thrive, and get small businesses off the ground. An active community member, he led and contributed to many worthy causes.
As an ophthalmologist at Morganton Eye, he impacted countless lives. Going anywhere in town with Gresham meant chats with appreciative past and present patients. Weekends, dinners, and sleep were often interrupted by calls to his personal phone from surgical patients with questions or concerns. He was that Doc, the rare, compassionate, and approachable one who said here is my number, call me anytime.
Gresham retired from Morganton Eye Physicians in June 2015. On January 1, 2019, he was inducted into the North Carolina Medical Society's "Fifty Year Club".
Dr. Gresham joined the NCMS in 1978.
The North Carolina Medical Society extends its deepest condolences.
Read Dr. Gresham’s full obituary here.
Mark Your Calendar: February Fireside Chat
Medicaid Managed Care Fireside Chat
Hot Topics
Thursday, February 13 | noon-1 p.m.
Please join this month's Fireside Chat on Thursday, February 13 from noon to 1 p.m., hosted by Dr. Janelle White, Chief Medical Officer of Medicaid.
Topics will include:
- 1115 Waiver Renewal
- Child & Family Specialty Plan Update
- Annual Health Disparities Report
- Making Care Primary
- Clinical Pharmacy Updates
- Community Alternatives Program (CAP) Referral Process
- Collaborative Care Capacity Building Program (CoCM)
Register for the Medicaid Managed Care Fireside Chat
Double Trouble: Diabetes and Falls

People with diabetes are at higher risk for falls. Etiologies include vision changes from retinopathy, damage to both peripheral and central nerves, side effects from medicines, and co-morbidities like osteoarthritis. Through use of a case study illustrating a familiar primary care patient encounter, learners will apply new knowledge, so they can anticipate and intervene appropriately in their work. An optional module on conducting the Diabetic Foot Exam is included. There is no charge for this online course. Course registration is generously supported by the Division of Health Benefits.
NCMS Pushes for Prior Authorization Reform with Bipartisan Support from Lawmakers

RALEIGH -- On Tuesday, January 28, the North Carolina Medical Society (NCMS) held a press conference at its Raleigh headquarters to support a growing coalition of lawmakers dedicated to reforming the state's prior authorization process. The NCMS is fully committed to driving meaningful change during the 2025 legislative long session.
The event featured Amanda Watson as a guest speaker. Watson shared her powerful story of battling cancer and the immense challenges she encountered due to prior authorization hurdles. She was joined by her husband, two children, and mother as she passionately recounted how unnecessary delays from health insurance companies caused her substantial pain and anguish. She also recounted the toll those delays in care took on her young family.
"Throughout my treatment," Watson stated, "we have been flabbergasted by the number of times necessary treatments or medications have been denied by our insurance. When fighting an aggressive form of cancer, the last thing you need is being told your insurance won’t approve lifesaving treatment. It is the ultimate feeling of betrayal and hopelessness."
Dr. John Meier, President of the North Carolina Medical Society, also addressed the press. "As a physician, I cannot sit idly by while my patients die or suffer unnecessary delays. We don't have time to let the health of more North Carolinians be impacted by these predatory prior authorization practices. The time for reform is now," he declared.
The event drew a bipartisan group of North Carolina legislators, united in their support for reform. Attendees included Rep. Allen Buansi (D-Dist. 56), Rep. Grant Campbell, MD (R- Dist. 83), Rep. Maria Cervania (D-Dist. 41), Rep. Allen Chesser (R-Dist. 25), Sen. Mark Hollo (R-Dist. 45), Rep. Timothy Reeder, MD (R-Dist. 9), and Rep. Donna White (R-Dist. 26). Each lawmaker expressed their commitment to addressing this critical issue.
For those who missed the event, a re-play is available on Facebook Live here.
Special thanks to the Watson family for courageously sharing their story, and to the many news outlets that covered this vital issue, including NC Insider, The Associated Press, WRAL, UNC, NC News Network, WPTF Radio, and Curtis Media Group.
Together, we are working toward a future where no one has to endure unnecessary suffering due to broken processes in healthcare.
Lend your voice to this important fight by signing the Prior Authorization petition here.
Deadline Approaching! Essentials of Pain Management CME Event

On March 1, 2025, NCS-ACOFP and the Pain Societies of the Carolinas will host a one-day CME event in Raleigh, NC at the Campbell University Norman Adrian Wiggins School of Law.
The conference is titled: Essentials of Pain Management. Conference content will meet the NC licensure and DEA MATE Act requirements related to prescribing opioids and related topics. Learn the latest techniques, treatments, and options in acute and chronic pain management. Review the conference agenda here. The following CME credit types will be awarded: up to 8 AOA Category 1-A credits AOA and 8 AMA PRA Category 1 Credits™ .
Register by January 31, 2025, to take advantage of the Early Bird Registration Rates. Here is the link to register. Note: registration is done via the site of the Pain Society of the Carolinas.
Need Additional Information about the Conference?
Visit the NCS-ACOFP website or contact Nancy Guy, Director at [email protected] or by phone at 910-658-6501.
NCMS Student Advocacy Fellowship Kickoff!

The NCMS launched its inaugural Student Advocacy Fellowship program on January 18, welcoming 35 medical students from across the state.
Over the next six months, these students will dive into the legislative process, advocacy, and health policy. Their passion for addressing healthcare issues and collaborating with legislators to find meaningful solutions is inspiring.
We’re excited for an incredible year supporting these future physicians and shaping the future of healthcare in North Carolina!
In Memoriam: NCMS Past President Marshall Simms Redding, MD
Marshall Simms Redding, MD
October 14, 1934 — January 20, 2025

NCMS Past President Marshall Simms Redding, MD, died Monday, January 20. He was 90 years old.
Dr. Marshall Simms Redding, born October 14, 1934, passed away age 90 on Monday, January 20, 2025, at Cone Health Wesley Long Hospital after a brief illness. A native of Guilford County, he was the son of the late Herbert Monroe Redding and Ernestine Fulgham Redding, and the youngest of their 7 children.
He graduated from McLeansville High School in 1953 and then attended Duke University from 1954 – 1958 with a major in Chemistry. While at Duke, he met Bobbie Newman who was studying at UNC Chapel Hill, and they married on June 2, 1957. In April 1958, he joined the Navy Aviation Cadet Program in Pensacola, Florida, and in December 1959 was assigned to Fleet Air Wing 14 at San Diego, California, supporting the mission to guard the Southern Sector and West Coast. By 1962 he was a Navy Lieutenant with two young children when he was accepted at Duke University Medical School. He graduated in 1966. He completed his internship at the US Naval Hospital in Portsmouth, Virginia, and a residency in Ophthalmology at the US Naval Hospital in Philadelphia and at Wills Eye Hospital.
Dr. Redding joined the NCMS in 1971.
The North Carolina Medical Society extends its deepest condolences.
Read Dr. Redding’s full obituary here.
Are You Interested in Helping to Shape the Future of Healthcare? Join Us in Raleigh on March 1 to Learn How.
Whether you're a healthcare professional, community leader, or passionate individual, the NCMS Advocacy Summit provides a platform to discuss, learn, and collaborate on shaping the future of healthcare.
We are thrilled to invite you to the NCMS Advocacy Summit, a groundbreaking event dedicated to exploring and advancing crucial topics in healthcare. Join us on Saturday, March 1, 2025, from 9 am to 5 pm at the StateView Hotel, located at 2451 Alumni Drive, Raleigh, NC 27606.
Event Highlights:
- Engaging Sessions: Delve into discussions on Access to Care Solutions, Corporate Practice of Medicine, AI in Healthcare, and much more!
- Diverse Perspectives: Gain insights from esteemed speakers representing various states and local community leaders, providing a comprehensive view of healthcare advocacy.
- Networking Opportunities: Connect with professionals who share your passion for healthcare advocacy. The last session of the day will be a townhall allowing leaders from specialty and county societies to speak.
Registration is Open, but Space is Limited! Don't miss this opportunity to be part of a transformative event. Secure your spot today by registering today!
We look forward to your participation in this impactful event.
What a Pause in External Communications from CDC, FDA, and Other Agencies Means for North Carolina

A newly signed executive order mandates that all federal health agencies pause external communications. This includes the U.S. Department of Health and Human Services, the U.S. Food and Drug Administration, the U.S. Centers for Disease Control and Prevention, and the National Institutes of Health.
Under the order, all external communications must be approved by a presidential appointee, causing delays in the dissemination of critical information like food recalls, drug approvals, and updates on public health threats, such as Norovirus and H5N1 bird flu.
While communications from federal health agencies are paused, you can rely on the following state and local agencies for health information:
- N.C. Department of Health and Human Services
- Mecklenburg County Public Health
- Wake County Public Health and Medical Services
- Durham County Public Health
- Johnston County Public Health
- Orange County Health Department
- Chatham County Public Health
Stay tuned to your NCMS Morning Rounds newsletter to keep informed.
[source]
Lace Up for the Annual Spring into Health ‘Healthraiser’ Run

BWC Gears Up for Annual Spring Into Health ‘Healthraiser’ Run
Brunswick Wellness Coalition (BWC) is preparing for its annual Spring Into Health 5k/1m Run on Saturday, March 15. Participants can run, walk, stroll, or roll along the route to raise awareness about living healthy lifestyles. All ages, skill levels, and abilities are encouraged to participate. Participant medals and age category trophies will be awarded. Form a team to be eligible for the Spunky Team Award which will be presented to the team that harnesses creativity and energy. Dr. Leigh Lane, the Coalition’s Executive Director said, “This year, Cape Fear Fitness is our platinum sponsor. We are grateful to have them as a partner. With this year’s event pairing with the Ides of March, usually a somber time, we expect to see a happier vibe with a lot of Roman toga attire. An after event meet up at Fizzy Jane’s in downtown Southport is also planned.” If an individual or organization cannot participate but wants to contribute, the run has donation options that will be used with proceeds to further BWC’s mission.
As a founding member of BWC and a supporter of community health initiatives, Dosher Memorial Hospital will host the 2025 Spring Into Health 5k/1m Run as a continued demonstration to quality community health involvement. The hospital will serve as the starting and finishing line for the run. Lane said, “Dosher has not only been a committed member of BWC since its inception but continues to serve as a health champion for the community.”
To be a Spring Into Health supporter, donor, or participant, visit the Coalition’s website, brunswickwellness.org. Early registration ends February 14.
The Brunswick Wellness Coalition is a united group of individuals and health-minded leaders with the mission to improve the health of the Brunswick community, and the vision of becoming the healthiest county in North Carolina. BWC is funded through Healthy People, Healthy Carolinas, an initiative of The Duke Endowment. To learn more, visit the website: brunswickwellness.org or Facebook: @BrunswickWellness.
Duke and UNC Partner on New Children's Hospital in the Triangle

AXIOS (January 27): UNC Health and Duke Health, the Triangle's two largest health care providers, will join forces to open a new children's hospital in the Triangle with financial backing from the state, multiple sources familiar with the plans told Axios.
Why it matters: The hospital, which is expected to cost around $2 billion, would be the first standalone children's hospital in the state. It would likely create thousands of jobs, from construction workers to health care professionals.
- The hospital would provide more capacity to treat children with complex pediatric health issues. Many other fast-growing states already have similar hospitals, including the 446-bed Children's Healthcare of Atlanta's Arthur M. Blank Hospital, which opened last year.
Driving the news: State officials and representatives from Duke and UNC are expected to announce the deal on Tuesday in Raleigh.
- Spokespeople for both UNC Health and Duke Health declined to comment.
Zoom in: The state has already pledged $320 million toward the creation of a children's hospital in the Triangle through its budget in 2023, Axios previously reported.
- But around $1 billion in philanthropic funds would also be needed, said the sources, who requested anonymity because they were not authorized to discuss the plans.
- The hospital would have around 500 beds, UNC Health has said in recent months, and a significant amount of resources would be placed toward behavioral health.
- It would be larger than existing children's health facilities located at UNC's hospital in Chapel Hill, Duke's in Durham and WakeMed's in Raleigh.
State of play: The hospital would need to be built on around 100 acres of land — a tough task in the Triangle's competitive real estate landscape — and a location has not yet been finalized.
- But negotiations on land have been had and the preference is to have the hospital in a central location in the Triangle, according to sources.
- UNC Health has said previously the goal is to have the standalone hospital open by the early 2030s. [source]
Join NCDHHS Tomorrow for Fireside Chat and Tele-Town Hall: NC Crisis Services — Get Help 24/7

The North Carolina Department of Health and Human Services will host a live fireside chat and tele-town hall on Tuesday, January 28, from 6 to 7 p.m. to discuss how people can support their mental well-being, find resources and get help for themselves or someone else experiencing a mental health crisis.
Event participants include:
- Kelly Crosbie, MSW, LCSW, Director, Division of Mental Health, Developmental Disabilities and Substance Use Services, NCDHHS
- Cherene Caraco, CEO & Chief Global Strategist, Promise Resource Network
- Joy Brunson-Nsubuga, MA, MBA, LMFT, LCAS, CCS, Chief Operating Officer, Recovery Innovations Inc.
Nearly 1 in 4 adults in North Carolina have reported symptoms of anxiety or depression. Help is available. Mental health crisis services offer non-judgmental, confidential and compassionate care to connect North Carolinians with resources and support — available at little or no cost — to get help with social or family situations, depression, anxiety, thoughts of suicide, substance use or if they just need someone to talk to.
The fireside chat will stream live from the NCDHHS Facebook and YouTube accounts, where viewers can submit questions. The event also includes a tele-town hall, which invites people by phone to listen in and submit questions. People can dial into the event by calling 855-756-7520 Ext. 119232#.
Fireside chat and tele-town hall panelists will discuss:
- Ways to support and improve mental well-being
- When to get help for yourself or a loved one
- What NC crisis services are and how to access them
- Where to find mental health information and resources
NCDHHS recently launched a new Crisis Services page available in English and Spanish to describe and connect people to services, includes a searchable map to find community crisis centers, and has a zip code search to find a mobile crisis team.
If you or someone you love is feeling overwhelmed, NC crisis services are here to help:
- Call, text, or chat with 988 for immediate support, 24/7
- Talk to someone with lived experience through the Peer Warmline: 855-PEERS-NC
- Have help come to you — trained mobile crisis teams will meet you in a safe place at low or no cost
- Visit a community crisis center for fast, in-person help from licensed clinicians
🎉It's New Member Monday!🎉

Join us in welcoming these new members to the North Carolina Medical Society!
- Elizabeth Adolfie, PA-C
- Victoria A. Arendt Kosec, MD
- Clarissa J. Bartolac, PA-C
- Robin Dong, DO
- Andrew P. Fink, PA-C
- Jonathan B. Goldston, PA-C
- Mai-Linh T. Huynh, PA-C
- Eric J. Keller, MD
- Thomas H. Kelly, MD
- Samir D. Mehta, MD
- Gregory A. Melish, MD
- Jon C. Myers, DO
- Soji Ojo, MD
- Ronald C. Reese, MD
- Caleb T. Runyon, PA-C
- Michael J. Schmidt, MD
- Gavin Snyder, PA-C
- Austin F. Weyant, DO
- Clark P. Wise, MD
We are thrilled to have you!
Not a member but would like to be? Joining is simple. Visit our membership center here.
Funding Opportunity Available for Health Disparities Research

The Centers for Medicare & Medicaid Services Office of Minority Health (CMS OMH) has released the Minority Research Grant Program (MRGP) 2025 Notice of Funding Opportunity (NOFO). This grant awards funding to health equity researchers at minority-serving institutions (MSIs) investigating health disparities and improving the health outcomes of minority populations.
As a grantee, you will enhance your impact and visibility in the research community, support our mission to advance health equity, and join a prestigious group of awardees whose collective MRGP-funded research has been cited in more than 190 publications. CMS will award up to six grants, totaling up to $1,275,000, in 2025.
Review the notice of funding opportunity CMS-1W1-25-001 and submit your application on grants.gov by April 1, 2025.
Eligible MSIs include:
- Historically Black Colleges and Universities (HBCUs)
- Hispanic-Serving Institutions (HSIs)
- Tribal Colleges and Universities (TCUs)
- Asian American and Native American Pacific Islander-Serving Institutions (AANAPISIs)
- Native American Serving Non-Tribal Institutions (NASNTIs),
- Alaska Native and Native Hawaiian-Serving Institutions (ANNHSIs), and
- Predominantly Black Institutions (PBIs)
For more information on eligibility and the application process:
- Visit the MRGP website
- Watch the MRGP overview video
- Email [email protected] for more information about eligibility and the application process.
Stay Tuned! CMS OMH will host informational webinars on February 13, 2025, and February 18, 2025. Join to review the grant, understand the MRGP NOFO requirements, learn about resources and tips when applying, and hear from prior grantees. More information about the webinars is forthcoming.
Study: Eight Psychiatric Disorders Share the Same Genetic Causes

In 2019, researchers at the Psychiatric Genomics Consortium, Harvard University, and the UNC School of Medicine identified 136 “hot spots” within the genome that are associated with eight psychiatric disorders. Among them, 109 hot spots were shared among multiple disorders, or “pleiotropic”. However, it was not clear at the time how genetic variations within these hot spots differed from those that only have roles in only one disorder.
A new genetic study, led by Hyejung Won, PhD, associate professor in the Department of Genetics and the UNC Neuroscience Center, and Patrick Sullivan, MD, FRANZCP, the Yeargen Distinguished Professor of Psychiatry and Genetics, has successfully delineated the functional consequences of genetic variants into two groups. Their findings, which were published in Cell, suggest that pleiotropic variants may be optimal targets for treatment, due to their extended roles in development and sensitivity to change.
Continue to the full story here.
Mark Your Calendar! Saving Time: Practice Innovation Boot Camp

This two-day, in-person AMA STEPS Forward® Innovation Academy boot camp is specifically designed for clinical and operational change agents looking to eliminate unnecessary work and free up more time to focus on what matters most–patient care.
Gain proven tools to implement in the following areas:
- Getting rid of stupid stuff
- De-implementation (STOP this and START that)
- Debunking regulatory myths
- EHR inbox optimization
- Team-based care practice fundamentals
- Building bridges between clinicians and administrators
- Reducing barriers to taking PTO
- Making the business case to leadership
Through breakout sessions, interactive activities, thought sharing, tactical strategy breakdowns and how-to examples, this boot camp will equip attendees with the time-saving tools and strategies needed to reform their organizations and enhance professional satisfaction.
Don’t miss this opportunity to gain best practices from top physician experts, network with like-minded peers, engage in cross-sector collaboration, and learn from each other’s successes and mistakes.
Space is limited. Learn more, including how to register, here.
Diabetes Performance Improvement in Primary Care

This self-paced educational activity aims to inform the learner about the status of diabetes and chronic kidney disease in primary care. This activity will explore barriers and facilitators to promote patient engagement in treatment. This activity will focus on performance improvement methods and activities which promote health among patients with diabetes.
North Carolina Set to Receive Additional Opioid Settlement Funds
North Carolina’s state and local governments are set to receive up to $150 million as part of a $7.4 billion settlement with Purdue Pharma and the Sackler family. This lawsuit stems from the impact of OxyContin on communities across the state.
Purdue Pharma, headquartered in Stamford, Connecticut, was named in the lawsuit for its role in fueling the opioid crisis. Plaintiffs argued that the company’s invention, manufacturing, and aggressive marketing of OxyContin over the years significantly contributed to the national epidemic of opioid addiction and overdose deaths.
North Carolina Attorney General Jeff Jackson emphasized the importance of this settlement, stating, “Purdue and the Sackler family are finally being held to account for their role in fueling addiction and deaths across North Carolina and the nation. This settlement means we will receive more funds than originally planned, and the Sacklers will be required to exit the opioid business entirely.”
The settlement, which is still pending court approval, will see the Sacklers paying up to $6.5 billion over the next 15 years, with Purdue Pharma contributing nearly $900 million. Additionally, the Sackler family will be forced to relinquish control of Purdue and will no longer be able to sell opioids in the United States. [source]
Join us in Raleigh on March 1 for the NCMS Advocacy Summit! Secure Your Spot Today!
Whether you're a healthcare professional, community leader, or passionate individual, the NCMS Advocacy Summit provides a platform to discuss, learn, and collaborate on shaping the future of healthcare.
We are thrilled to invite you to the NCMS Advocacy Summit, a groundbreaking event dedicated to exploring and advancing crucial topics in healthcare. Join us on Saturday, March 1, 2025, from 9 am to 5 pm at the StateView Hotel, located at 2451 Alumni Drive, Raleigh, NC 27606.
Event Highlights:
- Engaging Sessions: Delve into discussions on Access to Care Solutions, Corporate Practice of Medicine, AI in Healthcare, and much more!
- Diverse Perspectives: Gain insights from esteemed speakers representing various states and local community leaders, providing a comprehensive view of healthcare advocacy.
- Networking Opportunities: Connect with professionals who share your passion for healthcare advocacy. The last session of the day will be a townhall allowing leaders from specialty and county societies to speak.
Registration is Open, but Space is Limited! Don't miss this opportunity to be part of a transformative event. Secure your spot today by registering today!
We look forward to your participation in this impactful event.
CDC Alerts Clinicians to Accelerate Type A Flu Subtyping in Hospitalized Patients
The Centers for Disease Control and Prevention recently released an advisory recommending clinicians expedite subtyping of type A influenza samples from hospitalized patients, particularly individuals in an intensive care unit.
The CDC recommends that this subtyping occur as soon as possible following admission — ideally within 24 hours — to determine whether the virus is a seasonal influenza A subtype (i.e. A[H1] and A[H3]) or a novel influenza A virus, such as avian influenza A H5N1.
The agency said these efforts can help prevent delays in identifying human H5N1 bird flu infections and support timely infection control and investigation.
The CDC still considers bird flu a low risk to the public. The agency said while seasonal flu levels are high nationally, nearly all individuals currently hospitalized with type A flu infections are likely experiencing a seasonal strain.
Read the advisory here.
Mark Your Calendar! Heart Health Month: Free, Virtual Heart Healthy Seminars

Lake Norman Regional Medical Center is hosting free, virtual (online) seminars in February in recognition of Heart Health Month Awareness. The presentations include: Heart Attack Awareness, February 5, at 12 p.m., presented by Sydney Lawrence, R.N., BSN, chest pain and stroke coordinator at Lake Norman Regional Medical Center; Who Needs Cardiac CT Calcium Scoring?, February 12, at 12 p.m., presented by Tiffany Schweitzer, Ph.D., director of imaging and cardiovascular services at Lake Norman Regional Medical Center; Nutrition and Heart Health, February 19, at 12 p.m., presented by Bernadette Joyce, MS, RD, LDN, registered dietician at Lake Norman Regional Medical Center; Cardiac Rehab: Regaining Your Strength and Reducing Your Risk, February 26, at 12 p.m., presented by Joe Jackson, exercise physiologist at Lake Norman Regional Medical Center.
For more information regarding the Heart Health Month Awareness seminars and to register, visit here.
NCMS at Work: Report from the NCMS AMA Delegation
Report from the NC Medical Society’s delegation to the American Medical Association
2024 AMA Interim Meeting / House of Delegates
A key Q4 event each year is the American Medical Association’s annual Interim Meeting. The meeting is the second of the AMA’s semi-annual House of Delegates sessions, which convene delegates from across the country, representatives of specialty societies, and resident and student members. The AMA House of Delegates sets policy and sets healthcare regulation, legislation and education initiatives into motion.
Representing the NC Medical Society at the 2024 AMA Interim Meeting were the following delegation members.
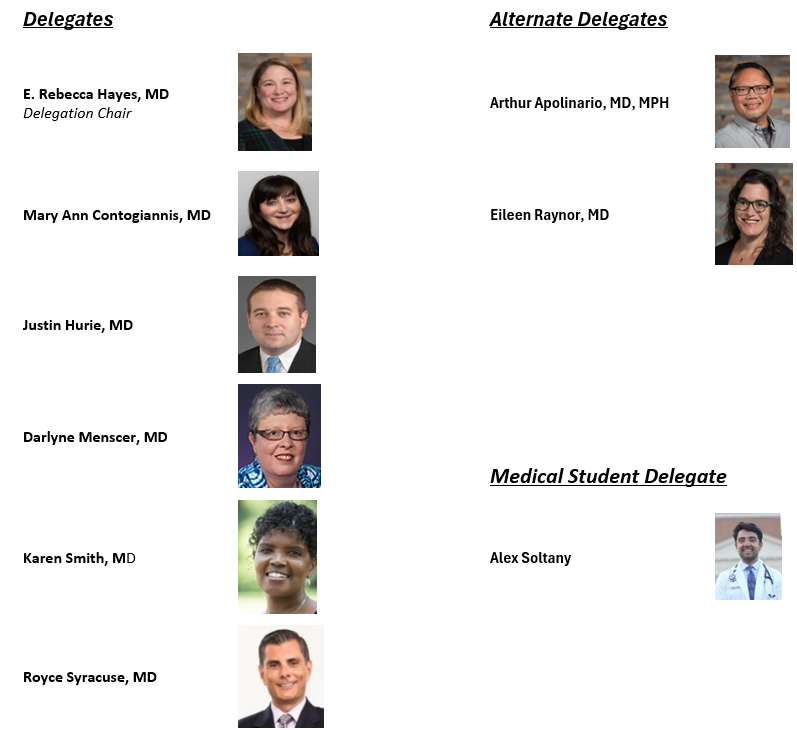
The 2024 AMA Interim Meeting culminated 28 years of service by Dr. Darlyne Menscer as a member of the NCMS delegation to the AMA. She was recognized by the AMA at the 2024 Interim Meeting and also by the NCMS at the 2024 NCMS LEAD Conference when she and Dr. John Fagg were celebrated for their dedicated leadership. Dr. Fagg concluded 25 years on the AMA delegation in 2023.

Among the most pressing topics on the Interim Meeting agenda was Medicare physician payment, which remains a top advocacy priority for the NC Medical Society. Earlier in 2024, the Centers for Medicare & Medicaid Services (CMS) announced a 2.83% physician payment cut for 2025, exacerbating the 29% decline in Medicare physician payment since 2001 when adjusted for inflation. “Fix Medicare Now” was a resounding theme of the meeting. The cut has sadly gone into effect, making the upcoming session of Congress very pivotal for practices and Medicare patient.
The NCMS delegation to the AMA remains involved with House of Delegates activity throughout the year and is extremely engaged at each meeting.

House of Delegates Action
Over the course of several days, the AMA House of Delegates addressed 104 resolutions along with 38 reports from the Board of Trustees and Councils. The following is an abbreviated list of the House’s actions with excerpts from the items adopted.
ED Care – Physician Presence
RESOLVED, That our American Medical Association recognize that the preferred model of emergency care is the on-site presence of a physician in the emergency department (ED) whose primary duty is to provide care in that ED, and support state and federal legislation or regulation requiring that a hospital with an ED must have a physician on-site and on duty who is primarily responsible for the emergency department at all times the emergency department is open.
That our AMA, in the pursuit of any legislation or regulation requiring the on-site presence of a physician who is primarily responsible for care in the emergency department (ED), will support state medical associations in developing appropriate rural exceptions to such a requirement if, based on the needs of their states, the association chooses to pursue certain alternative supervision models for care provided in EDs in remote rural areas that cannot meet such a requirement due to workforce limitations, ensuring that exceptions only apply where needed. These exceptions shall preserve 24/7 physician supervision of the ED and provide for the availability of a physician to provide on-site care.
Corporate Practice of Medicine
Our AMA vigorously opposes any effort to pass legislation or regulation that removes or weakens state laws prohibiting the corporate practice of medicine
Our AMA opposes the corporate practice of medicine and supports the restriction of ownership and operational authority of physician medical practices to physicians or physician-owned groups.
Provider Credentialing
RESOLVED, that our American Medical Association urge the US Department of Labor to establish uniform provider credentialing standards for Third Party Administrator’s (TPA's) serving ERISA Plans to include the following:
- that when a credentialing application is submitted, the insurance carrier must respond in writing within five business days whether the application is complete and acceptable, and
- if incomplete the carrier must send notice to the provider indicating what additional information is needed for completion of the process, and
- acknowledge the completion of a successfully completed application within ten business
Augmented Intelligence (AI) in Health Care
Sections of this lengthy AMA action address:
- National governance policies
- Transparency and disclosure of use of AI
- Physician liability associated with use of AI
- Data privacy
- Cybersecurity
- Mitigation of misinformation
- Payor use of AI in decision making
Combatting the illicit fentanyl crisis
RESOLVED, that our American Medical Association advocate for public education and awareness about the rapidly evolving US illicit drug crisis due to dangers of fentanyl and carfentanil-laced products; and be it further
RESOLVED, that our AMA advocate that federal, state and local government officials and agencies implement measures to curb and/or stop the manufacturing, importation, and distribution of illicit drugs and related chemical compounds; and be it further
RESOLVED, that our AMA support federal legislation that would help Customs and Border Protection (CBP) stop the flow of illicit goods, including fentanyl and counterfeit medications.
Improving rural obstetrical care
RESOLVED, that our American Medical Association strongly supports federal legislation that provides funding for the creation and implementation of a national obstetric emergency training program for rural health care facilities with and without a dedicated labor and delivery unit; and be it further
RESOLVED, that our AMA supports the expansion and implementation of innovative obstetric telementoring/teleconsultation models to address perinatal health disparities and improve access to evidence-informed perinatal care in rural communities; and be it further
RESOLVED, that our AMA encourages academic medical centers and health systems to actively participate in obstetric telementoring/teleconsultation models to support rural physicians and advanced practice providers and improve perinatal health outcomes in rural communities.
ED boarding
RESOLVED, that our American Medical Association immediately collaborate with stakeholders such as hospitals, insurance companies, CMS, and joint commission to resolve this issue; and be it further
RESOLVED, that our AMA advocate strongly for appropriate staffing ratios and appropriate care for patients and the emergency room and those admitted but still physically located in the emergency room to decrease patient harm and physician and nurse burnout.
Outcomes measures
RESOLVED, that our American Medical Association will make public statements calling for a removal of any/all unproven outcomes measures and associated mandates placed on physicians, practices, licensed clinics, nursing homes, hospitals and other places of healthcare; and be it further
RESOLVED, that our AMA will seek legislation or regulation removing any/all unproven outcomes measures and associated mandates placed on physicians, practices, licensed clinics, nursing homes, hospitals and other places of healthcare.
Collective negotiation with hospitals and health systems
RESOLVED, that our American Medical Association develop and distribute comprehensive materials to enable medical staffs to become effective agents for collective negotiation with hospitals and health systems; and be it further
RESOLVED, that our AMA allocate appropriate resources and support to assist medical staffs in understanding their rights, the negotiation process, and strategies for successful collective action; and be it further
RESOLVED, that our AMA advocate for policies at the state and federal levels that support the rights of medical staffs to engage in collective negotiation with hospital systems.
Gender-affirming care
That our AMA unambiguously supports access to and insurance coverage of medically necessary gender-affirming care but does not identify a preferred model of care for determining medical necessity.
Our AMA supports public and private health insurance coverage for evidence-based treatment of gender-affirming care gender dysphoria as recommended by the patient's physician.
Facility fee transparency
RESOLVED, that our American Medical Association advocate for legislation or regulation that mandates the proactive transparency of the added costs to the consumer for health care services rendered at hospital outpatient department designated clinics; and be it further
RESOLVED, that our AMA advocate the additional costs of facility fees over professional services be stated upon scheduling of such services, noting the two are separate and additive charges, as well as prominently displayed at the point of service.
Biosimilars
That our American Medical Association (AMA) support the development and implementation of strategies to incentivize the use of lower cost biosimilars when safe, fiscally prudent for the patient, clinically appropriate, and agreed upon as the best course of treatment by the patient and physician.
Payment for pre-authorized procedures
RESOLVED, that our American Medical Association support the position that the practice of retrospective denial of payment for care which has been pre-certified by an insurer should be banned, except when false or fraudulent information has knowingly been given to the insurer by the physician, hospital or ancillary service provider to obtain pre-certification; and be it further
RESOLVED, that our AMA continue to advocate for legislation, regulation, or other appropriate means to ensure that all health plans including those regulated by ERISA, pay for services that are pre-authorized, or pre-certified by such health plan, including services that are deemed pre-authorized or pre-certified because the physician participates in a “Gold Card” program operated by that health plan.
Cannabis therapeutic claims
That our AMA:
- a) Oppose cannabis and cannabis-based product advertising that includes claims or statements that are not supported by scientific evidence.
- b) Will continue to monitor regulatory approaches to cannabis marketing.
Heat alert and response plans
RESOLVED, that our American Medical Association supports federal, state, and local efforts to use the most updated and evidence-based heat index formulas and other relevant factors to accurately estimate heat-related morbidity and mortality, proactively issue heat alerts, and improve implementation of response plans.
Radiation exposure – healthcare workers
RESOLVED, that our American Medical Association encourage public and private healthcare institutions to ensure more comprehensive coverage of different body types by providing PPE that more completely protects employees of all genders and pregnancy statuses, such as lead and lead-free aprons with capped sleeves, axillary supplements, and maternity aprons.
The AMA House of Delegates will next convene over the dates of June 6-11, 2025 in Chicago.
The AMA’s National Advocacy Conference is scheduled for February 10-12, 2025. You are encouraged to join members of the NC Medical Society in going to Capitol Hill to help advance our health policy priorities. Registration is open.
Grant Opportunity: Telehealth Infrastructure Grant Program. Deadline Approaching

The NC Office of Rural Health has released Wave 2 of the Telehealth Infrastructure Grants funding opportunity!
In Session Law 2023-134, the North Carolina General Assembly (NCGA) appropriated $5,000,000 in SFY 2024 and $15,000,000 in SFY 2025 in receipts (State funds) from the ARPA Temporary Savings Fund to the Office of Rural Health (ORH) in the Department of Health and Human Services to provide competitive grants to rural healthcare providers for Telehealth related items including:
- equipment
- high-speed internet access
- telehealth-related training to staff and patients
- technology equipment to patients
- internet service support for patients to help facilitate telehealth access*
- other infrastructure needed to establish telehealth services
*Eligible rural healthcare patients can benefit from internet service and associated equipment rentals, including modems, routers, and hotspot devices through the Telehealth Infrastructure grant. To receive this support, patients must meet at least one of the eligibility criteria defined below:
- Total household income that is at or below 200% of the federal poverty guidelines or,
- Participation in any ONE of these government benefit programs:
- Lifeline
- Supplemental Nutrition Assistance Program (SNAP)
- Medicaid
- Federal Public Housing Assistance (FPHA) (including Housing Choice Voucher (HCV) Program (Section 8 Vouchers), Project-Based Rental Assistance (PBRA)/202/811, Public Housing, and Affordable Housing Programs for American Indians)
- Veterans Pension and Survivors Benefit
- Supplemental Security Income (SSI)
- Free and Reduced-Price School Lunch or Breakfast Program including through the USDA Community Eligibility Provision
- Federal Pell Grant (current award year)
- Special Supplement Nutrition Program for Women, Infants, and Children (WIC)
Priority will be given to independent primary care practices and independent obstetrics and gynecology (OB-GYN) practices.
For more information, eligibility, and other requirements, click here. Deadline to apply is Friday, January 31, 2025.
Vital Directions for Health and Health Care: Priorities for 2025

The National Academy of Medicine’s Vital Directions for Health and Health Care series is published every four years to align with federal leadership transitions. It provides an in-depth analysis of the nation’s most pressing health policy needs. The 2025 edition, released on January 22 in Health Affairs, identifies six critical priorities: transforming healthcare payment and delivery; integrating AI into healthcare; modernizing public health; addressing the health effects of climate change; improving women’s health; and advancing biomedical research. As leaders across both government and the private sector tackle complex challenges, the Vital Directions series offers nonpartisan, evidence-driven recommendations.
Join the National Academy of Medicine on Thursday, February 27 from 12:00 to 1:00 pm ET for a virtual briefing on key policy actions recommended by authors of the Vital Directions series.
For more information, click here.
NCAHEC Offering Support Webinar for Primary Care Physicians

SPECIAL WEBINAR
Collaborative Care Management Capacity Building Fund
Tuesday, January 28 | 12:15-1 p.m.
The NC General Assembly has earmarked $5 million for capacity building for Medicaid-enrolled primary care practices across the state to adopt Collaborative Care Management (CoCM). NCDHHS is contracting with CCNC to manage the program in partnership with NC AHEC’s Practice Support coaching.
CoCM is an evidence-based behavioral health integration model designed to support primary care clinicians in assessing and treating patients with mild to moderate behavioral health conditions. An evidence-based model shown to be more effective than usual care, CoCM improves patient outcomes, increases satisfaction for both patients and providers, and reduces healthcare costs and the stigma related to mental health and substance use disorders.
The capacity building fund has a maximum award of $50,000 per practice. A primary care practice entity applying on behalf of multiple primary care practice sites may receive a maximum of three awards per entity (covering a maximum of 9 sites). Each clinic site may be eligible to receive awards of $50,000 to begin a CoCM model in-house. Additionally, $30,000 is available for practices to expand an existing in-house CoCM model and $20,000 is available to practice sites meeting Phase 1 eligibility, but planning to outsource staffing to a third-party, turn-key company.
Please join for a webinar on January 28 from 12:15-1 p.m. for a review on the new funding and an opportunity to ask questions.
Webinar learning objectives:
- Provide an overview of the Collaborative Care Management Capacity Building Fund award opportunities
- Define eligibility criteria for practice entities/sites
- Describe the application process
For more information about this program, visit CCNC's webpage on CoCM capacity building fund.
UNC Health "Socking it to" Parkinson's

Minges Wellness Center at UNC Health Lenoir is excited to announce the launch of Punching Through Parkinson’s, a non-contact unique boxing program designed specifically for individuals with Parkinson’s disease. This program aims to improve physical health, strength, balance, and overall quality of life through exercise tailored to the needs of Parkinson’s patients.
Parkinson’s disease can cause motor and non-motor symptoms that affect movement, coordination, and daily life. According to Parkinson Association of the Carolinas, nearly one million people are living with Parkinson’s throughout America and up to 10 million people worldwide. Men are one and a half times more likely to have Parkinson’s than women.
Research has shown that regular exercise, including boxing, can significantly reduce symptoms and improve overall well-being. Studies have shown that activities like boxing can help Parkinson’s patients improve motor function and coordination, enhance cognitive abilities and mental clarity, and boost overall energy and mood. The high-intensity nature of boxing training, combined with its focus on mental sharpness and physical movement, is ideal for combating the physical challenges of Parkinson's.
The program will be led by certified trainers within Minges Wellness Center who have experience in fitness and working with individuals with Parkinson’s disease. Each session will be modified to suit different fitness levels, ensuring every participant can engage safely and comfortably.
Punching Through Parkinson’s will require physician clearance and registration. The class is an at-cost program that starts at $40 per month. Classes will be around one hour long with 15 minutes of set-up and break-down at the beginning and end of class.
For more information or to register for Punching Through Parkinson’s, contact Minges Wellness Center at 252-522-7944. [source]
NC Medicaid: Claims Denial for Services with Identified Third-Party Insurance

NC Medicaid is implementing updates to NCTracks Third Party Liability (TPL) process for NC Medicaid Direct. These updates will impact claims submitted for certain services when a member has other third-party insurance coverage listed in their eligibility record.
What This Means for Providers
Claims for the following services will be denied if third-party insurance is detected in the member’s eligibility record:
- Hospice
- Private Duty Nursing
- Home Infusion Therapy
- Local Health Department (LHD)
- Therapy Services
- Institutional Ambulance
- Hearing Aid
- Independent Diagnostic Testing Facility/Portable X-ray
- Providers are required to submit these claims to the member’s primary insurer before billing Medicaid.
What Providers Need to do to Avoid Claim Denials
- Check Member Eligibility Before Billing: Always verify member eligibility and third-party insurance information in NCTracks prior to submitting claims.
- Submit Claims to Primary Insurance First: Ensure claims for the affected services are submitted to any identified third-party insurance before sending them to NC Medicaid.
- Maintain Documentation: Keep Explanation of Benefits (EOB) records from the primary insurers for audit and resubmission purposes.
Claims submitted prior to December 31, 2024, will not be affected. These updates align with NC Medicaid Direct federally mandated role as the payer of last resort.
Contact
Third Party Recovery; 919-527-7690
Registration Open for the 2025 UNC Eye Symposium

2025 UNC EYE SYMPOSIUM
The William & Ida Friday Center for Continuing Education
April 12, 2025
8:00 AM - 5:00 PM
The UNC Eye Symposium will provide the latest updates and insights in the diagnosis and treatment of eye disorders, including anterior segment, glaucoma, neuro-ophthalmology, ocular oncology, oculoplastic, retina, and pediatric ophthalmology.
Download (pdf) flyer for more information
NC Medicaid: January Tailored Care Management Provider Manual Updates

NC Medicaid has released updates to the January Tailored Care Management (TCM) Provider Manual. These updates aim to enhance clarity and provide flexibility for providers. Notable changes include:
- Clarification on Applicability of the Provider Manual to Tailored Plans / Local Management Entities/Managed Care Organizations (LME/MCOs)
- New Flexibility on Supervising Care Manager’s Role in Reviewing Care Plans/ISPs
- Revised Requirement on Timeframe to Complete the Care Management Comprehensive Assessment
- New Flexibility and Clarifications on the Process for Conducting the Care Management Comprehensive Assessment
- Clarification on Ability to Address Urgent Needs Prior to the Care Management Comprehensive Assessment
- Clarification on the Requirements for Reassessment
- Clarification on Care Manager’s Role in 1915(i) Care Coordination
The January Provider Manual update and summary of updates are available on the Tailored Care Management webpage under Provider Manual.
Eating More Fiber May Help Protect Against Dangerous Bacteria
Consuming more fiber, commonly found in whole grains, vegetables, and fruits, may help defend against harmful bacteria in the gut.
A recent study published in Nature Microbiology reveals individuals with high levels of the beneficial bacteria Faecalibacterium are more likely to have lower levels of harmful bacteria like E. coli. The research, which analyzed gut microbiome samples from over 12,000 people across 45 countries, highlights the potential health benefits of this particular microorganism.
The researchers also discovered that samples rich in Faecalibacterium contained elevated levels of beneficial compounds known as short-chain fatty acids, which are produced when fiber is broken down. Studies have shown that lower levels of this bacteria are associated with inflammatory bowel and gastrointestinal disorders.
Continue to full article here.
Tell the North Carolina General Assembly the Time is NOW to Pass Prior Authorization Reform!
Sign our petition to tell the North Carolina General Assembly, the time is NOW to pass Prior Authorization Reform.
Why reform Prior Authorization?
We've All Felt It. Every one of us, or someone we love, has had a hard time because of something called "prior authorization" in healthcare. Insurance companies use prior authorization to slow down or even stop people from getting the care they need. This is continuing to mess with people's lives.
Prior Authorization reform will allow for timely decisions to be made by the insurance companies, insurance companies must work with the patient's physician before denying coverage, and insurance companies must make prior authorization criteria clear and understandable.
By signing our petition, you are telling the North Carolina General Assembly the time is NOW to pass Prior Authorization Reform.
Capitol Chronicle: Telehealth Flexibilities for Medicare Patients Extended – Future Uncertain, Urgency Persists

Telehealth Flexibilities for Medicare Patients Extended – Future Uncertain, Urgency Persists
On December 20, 2024, Congress passed a short-term spending bill for the purpose of keeping the federal government operational through mid-March 2025. Our primary focus in working with our US House and US Senate members leading up to and during the bill’s debate was the inclusion of Medicare payment fix for physicians. From introduction to enactment, the bill was edited and the Medicare payment provision was ultimately eliminated. There was, however, an important measure that survived the bill edits – a temporary extension of Medicare telehealth coverage.
Section 3027 of the enacted federal funding legislation, H.R. 10545 / American Relief Act, entitled Extension of Certain Telehealth Flexibilities, keeps telehealth considerations under Medicare in place through March 31, 2025. Among those provisions are the following:
1. Audio-only services
2. Geographic and originating site requirements
3. Eligible providers
4. Mental health services
These and other provisions were implemented to maintain access to telehealth services for Medicare patients during the COVID-19 pandemic and public health emergency (PHE). In recognition of the positive impact of the flexibilities implemented, bipartisan health policy discussion on Capitol Hill has acknowledged the value of telehealth and has addressed continued support of the enacted flexibilities.
In March 2024 stand-alone bills that Congress considered last year – H.R. 7623 / S.3967 – Telehealth Modernization Act of 2024. This legislation proposed extending the telehealth coverages through 2026. These extensions follow what was included in the year-end funding package. North Carolina’s House and Senate members who signed on as co-sponsors of these bills included Congresswoman Deborah Ross, Congressman Wiley Nickel and Senator Thom Tillis. Comparable legislation is anticipated in 2025.
What hangs in the balance?
The Medicare telehealth flexibilities currently in place are scheduled to expire on March 31, 2025, if Congress enacts another extension or acts to make them permanent. The initial word from Capitol Hill is encouraging with regard to support of further extensions but there is uncertainty of the focus of cost-cutting targets under the new administration. A failure to extend the flexibilities will have an impact on physicians and other providers as well as patients. Notable flexibilities include:
Telehealth Delivery
Telehealth flexibilities currently allow for patient encounters via audio-only. Prior to the pandemic such engagement with required the use of two-way audio/video technology. An expiration of the Medicare telehealth flexibilities would eliminate the audio-only option.
Geographic/site of care requirements
As a result of the pandemic and the declaration of a public health emergency (PHE), flexibilities were extended to allow Medicare patients to receive care via telehealth at “any site in the United States at which the eligible telehealth individual is located at the time the service is furnished… including the home of an individual.” Eliminating this flexibility would result in an access to care issue for some patients, especially those in rural and underserved areas.
Providers eligible to provide telehealth services
Under the flexibilities extended as a result of the pandemic PHE, Medicare patients were allowed to access care via telehealth from an expanded list of providers, such physical therapists, occupational therapists, etc. If the flexibilities are not extended, the eligibility to provide telehealth services will revert to pre-pandemic rules and a more restricted list of approved providers, which would limit access to care.
Behavioral Health
Under the telehealth flexibilities Medicare patients receiving behavioral health care are eligible to obtain those services via telehealth with no in-person visit requirements. If the flexibilities expire, Medicare beneficiaries receiving mental health services via telehealth will be required to have at least one in-person visit every 12 months.
The outlook for 2025 is that an extension of coverage for Medicare telehealth services will be part of the discussion when Congress again engages in debate over funding of the federal government. Such action will be necessary early in the year since the current funding package expires in March. The reintroduction of standalone bills is anticipated as well.
Appointment Opening for the NC Medical Care Commission

The North Carolina Medical Society has the opportunity to nominate a member to be appointed by the Governor to the North Carolina Medical Care Commission.
The North Carolina Medical Care Commission of the Department of Health and Human Services consist of 17 members appointed by the Governor. Three of the members appointed by the Governor are nominated by the North Carolina Medical Society.
Learn more about the purpose of the NC Medical Care Commission here.
View the 2025 Schedule of quarterly meetings here.
NCMS Application to State Boards and Commissions here.
The Nominating and Leadership Development Committee (NLDC) will interview applicants virtually on the evening of Wednesday, February 26, 2025.
The deadline to submit NCMS Application for North Carolina Medical Care Commission: Wednesday, January 22, 2025.