NCMS at Work: Medical Care Commission

North Carolina Health Commission Meeting
Key Updates
The North Carolina Health Commission recently convened to discuss major healthcare initiatives, funding, and regulatory updates affecting the state. NCMS staff attended this event to keep you informed and advocate for member voices. Find details from the meeting here:
New Appointment to the Commission
Michelle F. Jones, MD, a family physician and NCMS member, has been appointed to the commission, bringing her expertise in community health and patient care.
Bond Program & Healthcare Expansion
With $4.7 billion in outstanding debt from bond series, the commission discussed the impact of Medicaid expansion, which is expected to drive new hospital construction projects across the state.
Duke Health Project Proposal
Duke Health presented a proposal addressing hospital acquisitions and facility expansion, highlighting their $1.1 billion in charity care and $4.8 million in bad debt. The approved motion includes:
- Lake Norman Hospital Refinancing – 123-bed acute care hospital with 24 physicians
- Duke Health Cary Phase II Expansion – Emergency department, imaging, ambulatory surgery center, and infusion services
- Bond Premium – Approximately $460 million
- Regulatory & Licensing Updates
Several healthcare regulations were reviewed and approved for public comment, including:
- Nursing Pool Licensure
- Mammogram & Pap Smear Certification
- Healthcare Personnel Registry
- Hospital Transfers & Discharges
- Emergency Medical Services & Trauma Rules
- Ambulatory Surgical Facility Licensing
- Hospital Licensing Rules
*These updates will ensure healthcare facilities maintain high standards for safety, licensing, and patient care.
For more details, view the full agenda and packet here.
Bird Flu Cases Confirmed in North Carolina Waterfowl

Cases rise across nation as NCDHHS speak out
A bird found dead at a Hendersonville lake has tested positive for bird flu, according to local officials.
The Henderson County Department of Public Health announced on Tuesday that on February 8, officials were notified of five dead birds at Osceola Lake, a privately owned lake in Hendersonville. One of the birds was submitted to the state for bird flu testing and yielded a positive result for H5N1, or bird flu.
The health department has provided guidance to the owner of the lake as well as to homeowners, guests and others who have been allowed to use the lake for recreational purposes.
The owner has also posted signage stating contact with birds should be avoided.
The bird is at least the third confirmed case of bird flu in western North Carolina. In 2024 a dead duck found at Lake Louise tested positive for bird flu, and in January waterfowl at a Buncombe County park also tested positive.
Also in January a small game flock of birds also tested positive for bird flu.
Bird flu is a disease that can affect most species of birds and some mammals, according to the N.C. Department of Health and Human Services. These viruses naturally spread among wild aquatic birds worldwide and can also infect domestic poultry and other birds and animals, health officials said.
The risk of bird flu spreading to humans is low, according to health officials, and most cases happen when someone has direct contact with an infected bird or their feces.
"Avian influenza viruses rarely infect people," NCDHHS officials said.
Symptoms of bird flu include fever, cough, shortness of breath, runny nose and red, irritated eyes.
"Birds, their feces and saliva should be avoided by the public," health officials urge. "People should avoid contact with sick or dead animals."
If a dead bird needs to be disposed of, health officials recommend wearing gloves or using a plastic bag turned inside out. Those who have direct contact with wild birds or sick animals are also advised to wear protective equipment.
"Wild birds can be infected with the virus even if they don't look sick," Health Department officials said.
Click here for a list of bird flu cases in North Carolina over the past few years.
*This article contains information from Spectrum 1 and WSPA
AMA Honors NC Public Health Official with Government Service Award
AMA honors North Carolina public health official with Government Service Award
The American Medical Association (AMA) presented Cumberland County (N.C.) Public Health Director Jennifer Green, PhD, MPH., with the AMA Award for Outstanding Government Service. Having served in her current role since 2019, Green has overseen the delivery and promotion of public health services, strategies, and initiatives in Cumberland County. She played a key role during the COVID-19 pandemic, mobilizing the community, distributing resources, and setting up drive-thru vaccine clinics that prompted Gov. Roy Cooper to praise the County’s response as a shining example of high-quality local government.
The award was presented during the AMA’s annual National Advocacy Conference (NAC) in Washington, DC.

“Across the country, local public health officials played a critical role in combatting COVID-19, educating local communities, and saving lives. Jennifer Green epitomizes that commitment and leadership,” said AMA Board Chair Michael Suk, M.D., JD, MPH, MBA. “For her dedication to improving the lives of people – both during and well beyond the COVID-19 pandemic – and for her creative approach to helping address public health challenges in Cumberland County, it is an honor to present Jennifer Green with the AMA Award for Outstanding Career Public Servant at the Local Level.”
“Dr. Green has provided exemplary care to our citizens with innovative programs and ideas,” said Cumberland County Commissioner Glenn Adams, who nominated her for the award. “She has had a tremendous impact on the lives of our citizens and the health of our county.”

In addition to her vital work during the COVID-19 pandemic, Green opened a WIC clinic to expand the scope of services and promote healthy babies and mothers. She created Healthy Conversations, which promotes public health education by training barbers and stylists to be advocates who can influence positive health behaviors in under-resourced communities. She created the Maternal Health project to address the disparities of mothers of color in seeking pre- and post-natal health care. And she is leading efforts to combat the opioid epidemic in her community by working to establish a recovery resource center.
UNC Study: Some Viruses ‘Freeze’ Their RNA to Replicate
Researchers have discovered that RNA in Zika virus can freeze itself in time to further its spread in the body, revolutionizing how researchers study disease-causing viruses.
(UNC Health Newsroom) -- They say that change takes time. Well, that’s not the case for RNA.
The small biological molecule acts like a switchboard operator, capable of changing its shape every few milliseconds so it can manipulate biological functions in the body. It has big jobs to carry out, after all, like copying genetic information into every living cell and activating the immune response.
A new multidisciplinary study from biophysicists and virologists at the UNC School of Medicine challenges this idea of shape-shifting RNA. Helen Lazear, PhD, associate professor of microbiology and immunology, and Qi Zhang, PhD, professor of biochemistry and biophysics, have discovered that a type of RNA in Zika virus, a mosquito-borne virus, can essentially freeze itself in time in an effort to make more copies of itself and further its spread in the body.
Their findings have not only sent ripples through the field of virology, but it has also given researchers new ammo in the fight against RNA viruses. Their study, which was published in Nature Chemical Biology, paves the way for new therapies that can “un-freeze” these RNA structures to combat other mosquito-borne RNA viruses.
“We know that Zika virus and related viruses rely on these very stable RNA structures to replicate,” said Lazear. “By adjusting the stability of this RNA in the lab, we showed that we can shorten its lifespan and make it harder for the virus to grow and spread. We’re excited to expand on our research to learn more about how these viruses cause human disease and ways to combat them.”
A Surprising Discovery

Researchers in the Qi Zhang’s lab made the discovery back in 2017, when they were performing routine imaging experiments using nuclear magnetic resonance (NMR) imaging. The technology, much like an MRI that is used in humans, allows scientists to visualize shapes and motions of biological molecules, such as RNA, DNA, and proteins, in astounding atom-by-atom detail.
However, lab members were quick to realize that the Zika virus RNA was stuck in this configuration for days—approximately one million times longer than other types of RNA.
Further investigation by the Zhang and Lazear labs revealed that this frozen, stable RNA structure plays an important role in viral replication. They found that this particular configuration can effectively put up a “molecular wall” that protects the viral RNA from being degraded by the host cell, altogether enhancing the ability of the virus to make more copies of itself.
Antivirals and Preparing for Emerging Disease
After analyzing the RNA structure and its mechanisms further, researchers have gotten a better understanding of its strength and also its weakness. If researchers can determine how exactly the RNA structure maintains this strong defense, they might be able to develop new therapies that can disrupt that interaction and interfere with further replication of the virus.

Zika virus is just one of many RNA viruses, termed flaviviruses, that are spread by mosquitoes and ticks around the world, including West Nile virus which is found in North Carolina. As a result, researchers are working to develop new and effective vaccines and to learn more about these viruses before they emerge.
“While some flaviviruses are important causes of disease globally, some of these viruses don’t currently cause large outbreaks but have the potential to do so in the future,” said Lazear.
“It’s really important that we learn about these viruses and have the tools to work with them, so that we’re ready to respond to future emerging outbreaks.”
Revolutionizing How Scientists Understand RNA Molecules
In the field of biochemistry and biophysics, much of their time is spent on analyzing and detailing the shapes of molecular structures. Understanding their shape allows researchers to learn more about their ins-and-outs, such as how they bind to receptors, activate biochemical pathways, or how they function in the body.
Over the last decade, the field has taken a large leap forward with new technologies that can predict molecular structures using AI. However, the latest findings in the Zhang and Lazear labs add a whole new dimension that scientists may need to consider when understanding RNA viruses: time.
“This paper really changed the paradigm of the field,” said Zhang, who is also co-director of UNC RNA Discovery Center at the UNC Lineberger Comprehensive Cancer Center. “We need to start appreciating how long these RNA structures live. Perhaps in the future, we could use AI-based technologies that can not only predict space, but also predict lifetime.”
Zhang is the leader of a recently launched research initiative, called the RNA-targeted Innovation in Drug Exploration (RIDE), in the UNC Department of Biochemistry and Biophysics and co-director of the RNA Discovery Center. Leveraging their latest knowledge about RNA viruses, Zhang and Lazear will further explore drug targeting in RNA viruses, alongside other experts in microbiology, virology, and biochemistry at UNC-Chapel Hill.
Rhese Thompson, PhD, a recent graduate in the Zhang lab, was lead author on the paper. Other authors include Derek Carbaugh, PhD, and Joshua Nielsen in the Lazear lab, Edgar Faison and Bo Zhao, PhD, in the Zhang lab; Jeffrey Bonin, PhD; Rita Meganck, PhD, in the Marzluff lab; Nathan Nicely, PhD, associate professor of Pharmacology; William Marzluff, Kenan Distinguished Professor of Biochemistry and Biophysics at UNC-Chapel Hill; Aaron Frank, PhD, assistant professor of Chemistry and Biophysics at the University of Michigan, Ann Arbor; Ciara Witt, PhD, in the Frank lab; and Atul Rangadurai, PhD, from Duke University.
Funding for this project came from the Emerging Challenges in Biomedical Research (ECBR) pilot award program from the UNC School of Medicine’s Office of Research, the Jefferson-Pilot Award from the UNC School of Medicine, UNC – Chapel Hill, the National Institutes of Health, and the Burroughs-Wellcome Fund.
Researchers would like to acknowledge the Biomolecular NMR Laboratory, which receives funding from the National Cancer Institute of the National Institutes of Health under award number P30CA016086, for spectrometer maintenance and use.
Measles Cases Are Rising in US as Texas Outbreak Grows
A measles outbreak in Texas has grown to 48 cases, all of whom are unvaccinated.
CDC: No cases reported in NC yet.
(ABC News, Mary Kekatos) -- Measles is continuing to spread across the United States as an outbreak in Texas rapidly grows and cases are confirmed in nearby states, according to health officials.
In western Texas, a measles outbreak doubled from 24 confirmed cases on Tuesday to 48 cases on Friday, according to the Department of State Health Services (DSHS). This marks the largest measles outbreak in the state in more than 30 years, according to a DSHS spokesperson.
All of the cases are in unvaccinated individuals or individuals whose vaccination status is unknown, and 13 people have been hospitalized so far. Gaines County is the epicenter of the outbreak, with 42 cases confirmed among residents, according to DSHS.
Meanwhile, in neighboring New Mexico, three unrelated cases of measles were confirmed last week in Lea County, which borders Gaines County, according to the New Mexico Department of Health (NMDOH).
"While a connection to the Texas outbreak is suspected, it remains unconfirmed," according to a news release from the NMDOH.
The Centers for Disease Control and Prevention has separately confirmed 14 cases in five states so far this year, which does not include the recent Texas or New Mexico cases or recently confirmed cases in Georgia.
Public health experts who work in the field of infectious diseases told ABC News they're concerned about the rise in cases and that it could lead to a far bigger outbreak among those who are unvaccinated or undervaccinated.

"This current measles outbreak is very concerning when it comes to the potential for measles to become a lot more widespread," said Dr. Alok Patel, a pediatrician at Stanford Children's Health, and an ABC News contributor. "What we're seeing right now is a crack in the foundation of a building, and we do not want this building to collapse, and so the minute you see a small outbreak of measles -- especially in an un- or under-vaccinated population -- this is a textbook example of how measles can quickly spread."
"A small measles outbreak could be the start of a public health catastrophe that is completely preventable," he added.
Vaccine exemptions among children in Gaines County -- the epicenter of the Texas outbreak -- have grown dramatically in the past few years.
Read full story here.
The NC DHHS reported a confirmed case of measles in a child in Mecklenburg County in September of 2024. That was the first confirmed case in North Carolina since 2018.
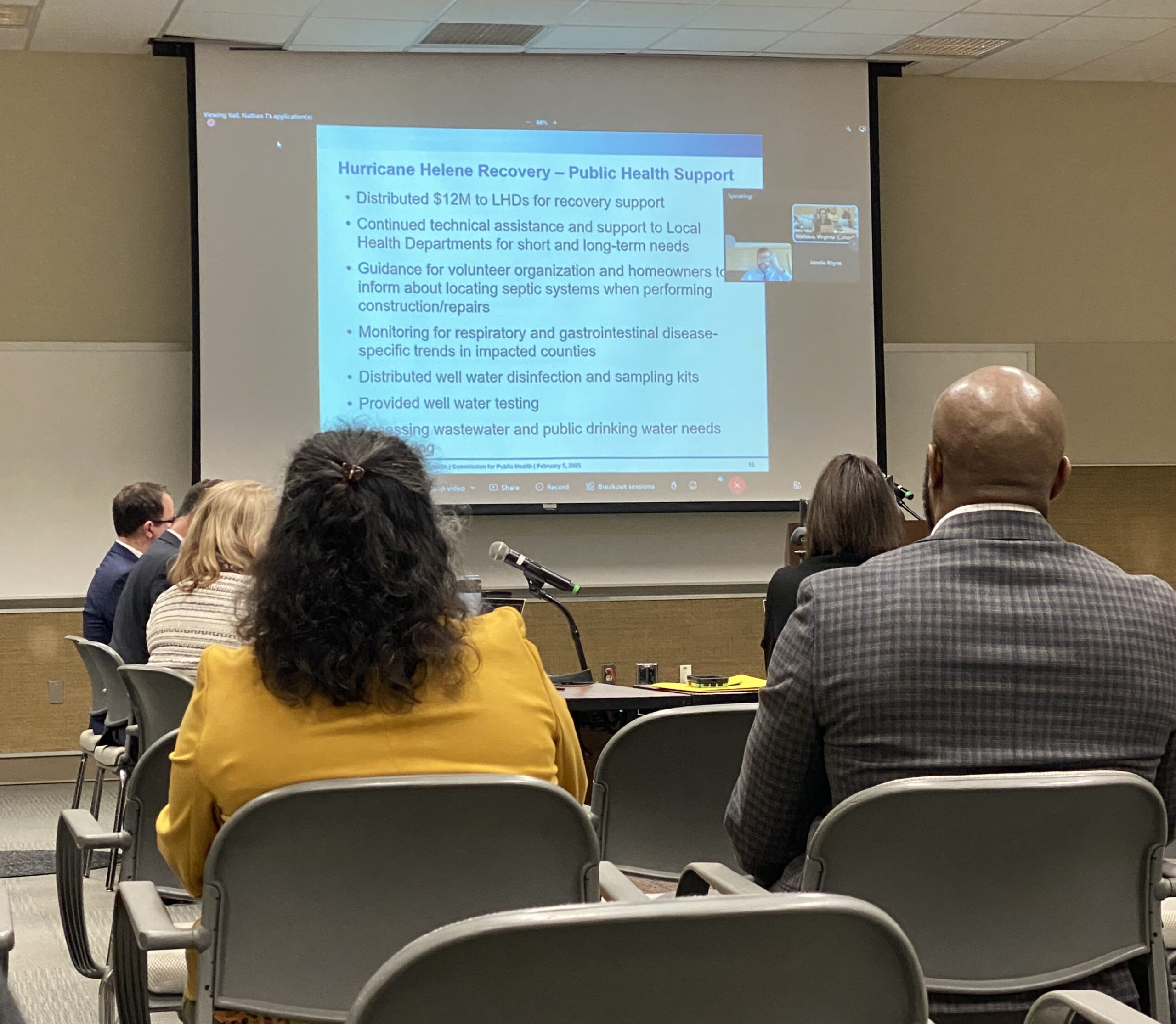
NCMS at Work: NC Public Health Commission
North Carolina Commission for Public Health
February 2025 Update
The North Carolina Commission for Public Health met on February 5th to discuss key public health concerns and initiatives across the state. NCMS staff attended the meeting to monitor outcomes. Here are the key takeaways for NCMS Members:
Respiratory Illnesses on the Rise
Cases of RSV and flu-like illnesses are increasing, leading to more hospital admissions. Public health officials are ramping up outreach and awareness efforts. COVID-19 levels remain moderately high in wastewater monitoring.
H5N1 (Bird Flu) Update
The risk to the public remains low, with no reported human cases in North Carolina. Those working with birds and livestock are at the highest risk. No human-to-human transmission has been recorded, and the CDC anticipates releasing a vaccine by spring.
Surveillance & Emergency Response
- Ongoing monitoring of influenza through emergency departments, hospitals, and wastewater systems
- Rabies testing in cats as part of disease surveillance
- $12 million in Hurricane Helene relief funds distributed to local health departments, including resources for wastewater testing and treatment
Policy & Program Updates
Several public health rules, including standards for services and cancer research registry updates, have been approved for public comment. Additionally, WIC presented an overview of its supplemental food funding program for women and children.
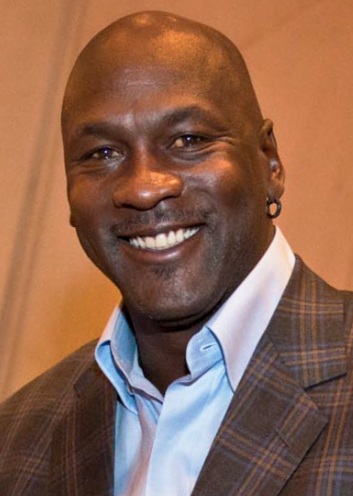
Michael Jordan Opens Another Health Clinic in Home State of North Carolina; Four Clinics Now Serve the Uninsured

The latest clinic in Wilmington will start seeing patients this week
(Goodnewsnetwork) -- After donating tens of millions of dollars, Michael Jordan is celebrating the opening of another vital community health hub—the fourth ‘Michael Jordan Family Medical Clinic’ to open in North Carolina.
The latest is the second clinic opened in Jordan’s hometown of Wilmington, and all are founded in collaboration with Novant Health.
It will officially welcome patients on February 19, focusing on strengthening primary care for all patients—including individuals who are uninsured or underinsured.
The 7,300-square-foot clinic at 416 N. 30th St. has twelve patient rooms and will be open weekdays from 8 a.m. to 5 p.m.
“It’s truly gratifying to know that in less than a year, our first Novant clinic in Wilmington has already made a meaningful impact on the health and well-being of individuals and families in my hometown,” said Mr. Jordan.
“Visiting Wilmington last year for the opening of our first clinic was incredibly moving, and it reinforced just how important access to quality health care is for the community.”
“We are profoundly grateful to Michael Jordan for his generosity and vision in making these two clinics a reality in our community,” said Ernie Bovio, president of the Novant Health Coastal Region.

“Thanks to his philanthropic partnership, our Greenfield Street clinic that opened last year served nearly 1,800 patients in its first nine months.”
ovant Health and Jordan first launched this clinic concept in Charlotte in 2019 with a pair of clinics that were strategically placed to address barriers to care, including transportation.
Many of the Charlotte patients never had a primary care visit before they were welcomed into the Michael Jordan clinics, where patients found “a sense of hope’.
Building on the success of this model, a $10 million gift from Jordan to the Novant Health foundations made it possible to add two more clinics in Wilmington.
NC's New Health Leader Wants to Build on Recent Successes

Dr. Devdutta "Dev" Sangvai is secretary of the North Carolina Department of Health and Human Services. He is also a former president of the NCMS.
(The Charlotte Post, Lynn Bonner) -- North Carolina’s top health officials start their jobs at the beginning of each new administration looking to master the details of the vast agency they lead and with budget recommendations to prepare.
Dr. Devdutta “Dev” Sangvai, the new secretary at the state Department of Health and Human Services is facing that and much more.
The department will be looking for support in the legislature to expand a Medicaid program that addresses non-medical factors that influence health such as nutrition and housing, improve the child welfare system, and build on the work of the last few years improving behavioral health care.
And it will have to do all this while navigating turbulence from Washington that could keep patients, medical providers and policy makers off balance.
Congressional Republicans are contemplating Medicaid cuts that will affect state budgets and people who rely upon the insurance. Robert F. Kennedy Jr., founder of an anti-vaccine organization, holds the nation’s loudest health policy megaphone. Diversity programs and funding are being axed at the same time that North Carolina’s public health goals focus on equity.
Sangvai was president of Duke Regional Hospital in Durham before joining Gov. Josh Stein’s administration to lead DHHS. He spent more than 20 years at Duke and earned an MBA from its business school.
He took over from Kody Kinsley, who was at DHHS for nearly seven years, three of them as secretary.
Sangvai said in an interview that while at Duke he witnessed the benefits of Medicaid expansion and the state’s sharpened focus and increased spending on behavioral health care.
Since North Carolina expanded Medicaid on Dec. 1, 2023, more than 625,000 low-income adults have enrolled in the government health insurance.
Sangvai wants to build on the foundation established under the previous administration with a focus on expanding access to care and to the department’s services.
“Some of my priorities are really thinking about how do we strengthen access in all North Carolina communities? And there are a few areas I think we need to look at – some of our state run facilities. How do we increase access there? And access is just not bricks and mortar. It’s also the services we provide,” he said.
“At the end of the day, we want to make sure that individuals are able to access health care when they need it in a setting that makes sense for them.”
Filling jobs and retaining staff
The agency has struggled with high job vacancy rates for years that could be a bar to expanding access.
Last May, the state Human Resources office reported DHHS had some of the highest vacancy rates among state agencies, at about 26%.
Sangvai put the existing job vacancy rate at 20% to 23%.
Health care technicians are the frontline workers at the three psychiatric hospitals and the three developmental centers the state operates. Entry-level health care technician positions had a vacancy rate of 42% in December 2023, according to the Human Resources report.
Some people with developmental or intellectual disabilities have been unable to obtain help living in their communities because of shortages of direct care workers. These workers are not employed directly by the state, but work for companies that bill Medicaid.
State officials have taken some steps to address workforce shortages.
Last year, DHHS and the state Commerce Department published a workforce development plan that included direct care workers.
In its 2023-24 budget, legislators committed $20 million per year over two years to sign-on or retention bonuses for state healthcare facility workers. The legislature has also allowed DHHS to offer targeted salary increases to recruit and retain some staff.
Creating and strengthening a sustainable workforce is one of Sangvai’s goals.
Sangvai said he wants to add an element to retention efforts by creating ”joy and belonging” at work, and making sure employees know they can move out of entry level jobs. Filling vacancies addresses immediate needs, he said, but people may not stay in those jobs for long.
“Let’s create that growth opportunity, and not just create a situation where that individual then vacates the position and we’re back to where we started before,” he said.
Giving people the chance to fill jobs that fit their professional goals and personal strengths may help keep people from leaving, he said.
“We’re going to have to create career development opportunities. We’re going to have to educate individuals on what the possibility might be, and then think creatively.”
Possible changes to Medicaid
North Carolina’s Medicaid expansion law includes a requirement for DHHS to pursue permission to add work requirements to the benefit if it appears possible that the federal government will endorse it.
In his first term, President Donald Trump’s administration approved state requests to require adults who were able to work to hold jobs in order to receive Medicaid.
Courts stuck down some state’s plans for Medicaid work requirements, and the Biden administration rescinded other permissions.
Georgia survived a court challenge to work requirements. It instituted a “Pathways to Coverage” program that offers most Medicaid services to low-income adults who work, go to school, or perform community service for at least 80 hours a month. A review of the program found 4,231 people were enrolled at the end of its first year, far short of the 25,000 to 100,000 expected to enroll.
The report found that an unwieldy enrollment process and restrictive eligibility requirements hindered enrollment.
Work requirements are back on the list of possibilities for all states, along with other changes that could affect the state’s Medicaid program.
Sangvai wouldn’t speculate on what could happen with North Carolina Medicaid, but said he hopes the same bipartisan cooperation that fueled improvements of the last few years continues.
“It’s in that spirit of consensus and collaboration that I hope prevails as we think through any of the changes that may come before us,” he said.
DHHS “is focused on the work that’s ahead of us, recognizing that we may need to respond to something when it becomes more granular.”
Diversity, equity and inclusion under attack
Last year, DHHS published a detailed report on health disparities that looked at differences in access to health care, incidences of cancer and heart disease, and other measures of wellbeing by race, ethnicity, and geography.
The state’s 10-year plan for improving health, “Healthy North Carolina 2030,” focused on equity and factors that influence good health.
Trump has diversity, equity, and inclusion in his crosshairs. He has abolished federal DEI programs and put workers who were running them on paid leave.
Sangvai stressed that health differences are not based solely on race. Whether people live in rural or metro areas, whether or not they have disabilities, or are military veterans, are also play a role in health and access to health care. There’s significant overlap between rural/urban health disparities and disparities based on race, he added.
“Our focus is going to be on ensuring that our programs meet the needs of most North Carolinians,” he said.
A national health care leader many doctors oppose
Kennedy, who some doctors fear will spread misinformation about vaccines, won confirmation Thursday to become the U.S. Health and Human Services secretary. In his Senate confirmation hearings, Kennedy refused to agree that the COVID-19 vaccine saved lives or to accept the validity of scientific studies that said there’s no link between autism and vaccines.
The American Public Health Association and more than 75 Nobel laureates opposed his nomination.
DHHS and the state’s medical providers will continue to encourage vaccinations, Sangvai said.
Sangvai said when he saw patients, he routinely spent time answering their questions about vaccines. Health care providers should be prepared to have conversations with patients, sometimes more than once.
“People are going to trust their healthcare provider probably more than anyone else,” he said.
Company Says It Received Conditional Approval for Bird Flu Vaccine from USDA

Zoetis Says Scientists Began Updating Avian Flu Vaccine in 2022
(CNN, Dakin Andone) -- The US Department of Agriculture last week issued a conditional license for an avian flu vaccine for use in chickens, amid an outbreak ravaging poultry flocks, contributing to the sky-high price of eggs.
Zoetis, the manufacturer behind the vaccine, announced the conditional approval Friday, saying in a news release its scientists had begun updating its existing avian flu vaccine in 2022.
“We’ve been working with the administration and with Congress, and we’re very excited today to get the licensure for (the vaccine) in poultry, which we think will be a tool that we will help support the government as they deem necessary,” Zoetis CEO Kristin Peck told CNBC on Friday.
The conditional license was granted based on the “the demonstration of safety, purity, and reasonable expectation of efficacy,” Zoetis said. A conditional license can generally be used to address an emergency situation or special circumstance, the company noted, and is issued for a set period of time.
The company has previously developed vaccines for avian flu, including one used by the US Fish and Wildlife Service to protect California condors in 2023, Zoetis said, noting, “The decision to vaccinate commercial poultry flocks rests solely with national regulatory authorities in consultation with their local poultry sector,” the company’s news release said.
CNN reached out to the USDA for comment Sunday.
While other countries already vaccinate chickens against bird flu, the US approach has long been focused on eradicating the virus, mainly through culling flocks of birds when a case is identified. Historically, vaccination has been thought to carry a number of complications, including making it difficult to detect the virus in inoculated birds and trade concerns.
But the strategy may be shifting as bird flu spreads to other types of animals, like cattle, and becomes more difficult to contain: Over the last 30 days, 146 flocks have been confirmed to have avian flu, affecting more than 20.5 million birds, according to the Animal and Plant Health Inspection Service, part of the USDA. More than 150 million birds have been affected since the current outbreak began in 2022.
About 70 bird flu infections have been confirmed in people in the US since March 2024, and an older person in Louisiana died last year. The US Centers for Disease Control and Prevention, however, has said the risk to the public remains low, though those who work on farms with infected animals or who have backyard poultry flocks are at a higher risk of infection.
Director of the National Economic Council Kevin Hassett is preparing, along with Secretary of Agriculture Brook Rollins, to present a plan to President Donald Trump to combat bird flu, including options that would sidestep the need to kill chickens, he told CBS’s “Face The Nation” on Sunday.
“What we need to do is have better ways with biosecurity and medication and so on” to avoid killing chickens, Hassett said. “And so having a smart perimeter is what we’re working on, and we’re finalizing the ideas about how to do that with the best scientists in government.”
In the meantime, Americans can continue to expect high prices for eggs this year due to the ongoing avian flu outbreak and inflation, according to new estimates.
Egg prices are estimated to increase about 20% in 2025, compared to about 2.2% for food prices in general, according to the US Department of Agriculture’s price outlook. Beef, coffee and orange juice are among groceries with higher prices, but eggs are uniquely affected by the aggressive strain of avian flu, which has strained supply.
CNN’s Aileen Graef, Jen Christensen, Brenda Goodman and Jamie Gumbrecht contributed to this report.
NC Medical Society Members Advocate for a Medicare Payment Fix and More

NC Medical Society Members Advocate for a Medicare Payment Fix and More
Over the dates of February 10-12, 600+ participants gathered in Washington, DC for the 2025 National Advocacy Conference hosted by the American Medical Association.
Fixing the 2.83% Medicare Payment Cut that went into effect on January 1st was the primary focus of the meetings with each office of our North Carolina members of the US Senate and US House. Those 16 meetings contributed to the 350 total meetings held across Capitol Hill and followed the delivery of a stakeholder letter to Senate and House leadership encouraging support of the payment fix. The NCMS joined with 130 other partner organizations in signing the letter.
The NCMS delegation to the NAC included . . .
- Art Apolinario, MD, Family Physician/Clinical Medical Clinic/Clinton
- Hans Arora, MD, Urologist/UNC School of Medicine/Chapel Hill
- Janet Colon, RN, Critical Care Registered Nurse/Duke Health System/Durham
- Mary Ann Contogiannis, MD, Plastic Surgeon/Renaissance Center for Plastic Surgery/Greensboro
- Rebecca Hayes, MD, Family Physician/Elizabeth Family Medicine/Charlotte
- Justin Hurie, MD, Vascular Surgeon/Atrium Health, Wake Forest Baptist/Winston-Salem
- Karen Smith, MD, Family Physician/Karen L. Smith, MD,PA/Raeford
- W. Alan Skipper, CAE Senior Officer, Externa Affairs/North Carolina Medical Society

Despite the snow and wintery weather, the NCMS team spent three afternoons on Capitol Hill.
The “ask” of every congressional office was to help advance legislation, HR 879 / Medicare Patient Access and Practice Stabilization Act, which would eliminate the 2.83% cut while providing a 2% positive payment update for the balance of 2025. The bill’s primary sponsor is Rep. Greg Murphy MD (NC-3), from Greenville, NC.
A highlight of the visit to Capitol Hill was a Fix Medicare Now rally to put emphasis on the need for Congress to rectify five straight years of cuts in Medicare physician payment. Keynote remarks from Dr. Murphy received a rousing response of support and helped energize the effort to educate members of Congress and increase bill co-sponsorship. Upon arrival in Washington on Monday, February 10, the bill had garnered 37 bipartisan co-sponsors since introduction on January 31st. By week’s end, the work on Capitol Hill helped increase that support to 71 co-sponsors.

Rep. Greg Murphy, MD (NC-3), addresses The Fix Medicare Now rally
A key factor driving the positive response to the legislation is that, when adjusted for inflation, Medicare physician payment in 2025 is 33% less than in 2021. And, to give specific context to the impact of the payment cut, the results of an Impact Survey of North Carolina physicians and practices were shared.

NC delegation with Rep. Mark Harris and Rep. Greg Murphy, MD

NC delegation with Rep. Virginia Foxx and Senator Thom Tillis
The trip to Capitol Hill also set the stage for engagement on several other federal advocacy issues that are on the near horizon. Topping that list is gaining an extension of Medicare Telehealth Flexibilities. Congress approved an extension of Medicare’s telehealth coverage in its 2024 year-end funding package, but that extension expires on March 31, 2025. The unanimous support of the extension in December bodes well for another affirmative vote, but the effort to gain support is intense, nevertheless, since patients’ access to care hangs in the balance.
Maintaining stability in our state’s Medicaid program is an immediate priority as well.
Additional issues that did not cross the finish line in 2024 and are anticipated in 2025 include:
- Prior Authorization Relief
- Step Therapy Relief
- Workforce Improvements
- Physician/Clinician Wellness Support
- Research Funding Appropriations
Interested in an in-district meeting with your member of Congress? Please share your interest and we’ll work to make it happen. Your support and engagement make a difference.
Do you know your legislator? More importantly, does your legislator know you?
STI Testing at Home? Survey Finds Many Young People Are For It

Many Young Adults Prefer Privacy When it Comes to STIs
(HealthDay News) -- When it comes to testing for sexually transmitted infections (STIs), many young adults prefer the privacy and convenience of at-home testing, a new survey suggests.
Fully 91% of survey participants aged 14-24 said they would use free STI self-collection kits, the survey showed. STI home kits involve collecting a urine sample or vaginal swab at home.
Many commercial at-home STI testing options are available, and free ones are also offered in some parts of the country, according to the American Sexual Health Association.
The U.S. recorded more than 2.4 million cases of syphilis, gonorrhea and chlamydia in 2023, according to the Centers for Disease Control and Prevention (CDC).
Fifteen- to 24-year-olds made up nearly half of STI cases in the country.
Most STIs don't cause any symptoms and are treatable if caught early, but they account for nearly a third of infertility in women and may also increase the risk of pregnancy loss, health problems in newborns and endometriosis, in which cells similar to the uterine lining (endometrium) grow outside the uterus.
“There is an urgent need to prioritize and increase the accessibility of sexually transmitted infection testing among youth,” study author Dr. Okeoma Mmeje, associate professor of obstetrics and gynecology at the University of Michigan (U-M) Medical School, said in a news release.
“STI self-collection is an effective alternative that addresses barriers that often deter this population from seeking traditional reproductive health care services," said Mmeje, who is also an OB-GYN at U-M Health Von Voigtlander Women’s Hospital. "The autonomy and confidentiality offered through this option may empower young people to take charge of their sexual health without fear of judgment or social stigma.”
For the study, 760 young adults were asked six open-ended questions via text message about their perceptions and use of STI self-collection kits.
While the overwhelming majority said they would use free STI self-collection kits, about 6% said they would not due to concerns about their accuracy and discomfort with specimen collection.
“STI screening should be available and accessible to young people in various forms,” said lead study author Jayelin Parker, a researcher at the U-M Medical School's Department of Obstetrics and Gynecology. "User-friendly STI self-collection kits encourage more frequent testing, early detection, and treatment of STIs."
Historically marginalized groups in the U.S., including youth from sexual and gender minority populations, are disproportionately affected by STIs because of sexual stigma, medical mistrust, discrimination and lack of healthcare access, the authors point out.
“It’s a public health priority to address the social and political determinants of health that impact the ability of youth to access reproductive healthcare services,” Mmeje said.
A social media campaign focusing on adolescents and young adults may help increase knowledge and use of STI self-collection kits, the study authors suggested.
It's Valentine's Day! What Happens When Love and Science Double Date?

Sure, your heart thumps, but let’s look at what’s happening physically and psychologically
“They gave each other a smile with a future in it.”
— Ring Lardner
(The Harvard Gazette) -- Love’s warm squishiness seems a thing far removed from the cold, hard reality of science. Yet the two do meet, whether in lab tests for surging hormones or in austere chambers where MRI scanners noisily thunk and peer into brains that ignite at glimpses of their soulmates.
When it comes to thinking deeply about love, poets, philosophers, and even high school boys gazing dreamily at girls two rows over have a significant head start on science. But the field is gamely racing to catch up.
One database of scientific publications turns up more than 6,600 pages of results in a search for the word “love.” The National Institutes of Health (NIH) is conducting 18 clinical trials on it (though, like love itself, NIH’s “love” can have layered meanings, including as an acronym for a study of Crohn’s disease). Though not normally considered an intestinal ailment, love is often described as an illness, and the smitten as lovesick. Comedian George Burns once described love as something like a backache: “It doesn’t show up on X-rays, but you know it’s there.”
Richard Schwartz, associate professor of psychiatry at Harvard Medical School (HMS) and a consultant to McLean and Massachusetts General (MGH) hospitals, says it’s never been proven that love makes you physically sick, though it does raise levels of cortisol, a stress hormone that has been shown to suppress immune function.
Love also turns on the neurotransmitter dopamine, which is known to stimulate the brain’s pleasure centers. Couple that with a drop in levels of serotonin — which adds a dash of obsession — and you have the crazy, pleasing, stupefied, urgent love of infatuation.
It’s also true, Schwartz said, that like the moon — a trigger of its own legendary form of madness — love has its phases.
“It’s fairly complex, and we only know a little about it,” Schwartz said. “There are different phases and moods of love. The early phase of love is quite different” from later phases.
During the first love-year, serotonin levels gradually return to normal, and the “stupid” and “obsessive” aspects of the condition moderate. That period is followed by increases in the hormone oxytocin, a neurotransmitter associated with a calmer, more mature form of love. The oxytocin helps cement bonds, raise immune function, and begin to confer the health benefits found in married couples, who tend to live longer, have fewer strokes and heart attacks, be less depressed, and have higher survival rates from major surgery and cancer.
Schwartz has built a career around studying the love, hate, indifference, and other emotions that mark our complex relationships. And, though science is learning more in the lab than ever before, he said he still has learned far more counseling couples. His wife and sometime collaborator, Jacqueline Olds, also an associate professor of psychiatry at HMS and a consultant to McLean and MGH, agrees.

Spouses Richard Schwartz and Jacqueline Olds, both associate professors of psychiatry, have collaborated on a book about marriage. Stephanie Mitchell/Harvard Staff Photographer
More knowledge, but struggling to understand
“I think we know a lot more scientifically about love and the brain than we did a couple of decades ago, but I don’t think it tells us very much that we didn’t already know about love,” Schwartz said. “It’s kind of interesting, it’s kind of fun [to study]. But do we think that makes us better at love, or helping people with love? Probably not much.”
Love and companionship have made indelible marks on Schwartz and Olds. Though they have separate careers, they’re separate together, working from discrete offices across the hall from each other in their stately Cambridge home. Each has a professional practice and independently trains psychiatry students, but they’ve also collaborated on two books about loneliness and one on marriage. Their own union has lasted 39 years, and they raised two children.
“I think we know a lot more scientifically about love and the brain than we did a couple of decades ago … But do we think that makes us better at love, or helping people with love? Probably not much.”
Richard Schwartz, associate professor of psychiatry, Harvard Medical School
“I have learned much more from doing couples therapy, and being in a couple’s relationship” than from science, Olds said. “But every now and again, something like the fMRI or chemical studies can help you make the point better. If you say to somebody, ‘I think you’re doing this, and it’s terrible for a relationship,’ they may not pay attention. If you say, ‘It’s corrosive, and it’s causing your cortisol to go way up,’ then they really sit up and listen.”
A side benefit is that examining other couples’ trials and tribulations has helped their own relationship over the inevitable rocky bumps, Olds said.
“To some extent, being a psychiatrist allows you a privileged window into other people’s triumphs and mistakes,” Olds said. “And because you get to learn from them as they learn from you, when you work with somebody 10 years older than you, you learn what mistakes 10 years down the line might be.”
People have written for centuries about love shifting from passionate to companionate, something Schwartz called “both a good and a sad thing.” Different couples experience that shift differently. While the passion fades for some, others keep its flames burning, while still others are able to rekindle the fires.
“You have a tidal-like motion of closeness and drifting apart, closeness and drifting apart,” Olds said. “And you have to have one person have a ‘distance alarm’ to notice the drifting apart so there can be a reconnection … One could say that in the couples who are most successful at keeping their relationship alive over the years, there’s an element of companionate love and an element of passionate love. And those each get reawakened in that drifting back and forth, the ebb and flow of lasting relationships.”
Children as the biggest stressor
Children remain the biggest stressor on relationships, Olds said, adding that it seems a particular problem these days. Young parents feel pressure to raise kids perfectly, even at the risk of their own relationships. Kids are a constant presence for parents. The days when child care consisted of the instruction “Go play outside” while mom and dad reconnected over cocktails are largely gone.
When not hovering over children, America’s workaholic culture, coupled with technology’s 24/7 intrusiveness, can make it hard for partners to pay attention to each other in the evenings and even on weekends. It is a problem that Olds sees even in environments that ought to know better, such as psychiatry residency programs.
“There are all these sweet young doctors who are trying to have families while they’re in residency,” Olds said. “And the residencies work them so hard there’s barely time for their relationship or having children or taking care of children. So, we’re always trying to balance the fact that, in psychiatry, we stand for psychological good health, but [in] the residency we run, sometimes we don’t practice everything we preach.”
“There is too much pressure … on what a romantic partner should be. They should be your best friend, they should be your lover, they should be your closest relative, they should be your work partner, they should be the co-parent, your athletic partner. … Of course everybody isn’t able to quite live up to it.”
Jacqueline Olds, associate professor of psychiatry, Harvard Medical School
All this busy-ness has affected non-romantic relationships too, which has a ripple effect on the romantic ones, Olds said. A respected national social survey has shown that in recent years people have gone from having three close friends to two, with one of those their romantic partner.
“Often when you scratch the surface … the second [friend] lives 3,000 miles away, and you can’t talk to them on the phone because they’re on a different time schedule,” Olds said. “There is too much pressure, from my point of view, on what a romantic partner should be. They should be your best friend, they should be your lover, they should be your closest relative, they should be your work partner, they should be the co-parent, your athletic partner. There’s just so much pressure on the role of spouse that of course everybody isn’t able to quite live up to it.”
Since the rising challenges of modern life aren’t going to change soon, Schwartz and Olds said couples should try to adopt ways to fortify their relationships for life’s long haul. For instance, couples benefit from shared goals and activities, which will help pull them along a shared life path, Schwartz said.
“You’re not going to get to 40 years by gazing into each other’s eyes,” Schwartz said. “I think the fact that we’ve worked on things together has woven us together more, in good ways.”
Maintain curiosity about your partner
Also important is retaining a genuine sense of curiosity about your partner, fostered both by time apart to have separate experiences, and by time together, just as a couple, to share those experiences. Schwartz cited a study by Robert Waldinger, clinical professor of psychiatry at MGH and HMS, in which couples watched videos of themselves arguing. Afterwards, each person was asked what the partner was thinking. The longer they had been together, the worse they actually were at guessing, in part because they thought they already knew.
“What keeps love alive is being able to recognize that you don’t really know your partner perfectly and still being curious and still be exploring,” Schwartz said. “Which means, in addition to being sure you have enough time and involvement with each other — that that time isn’t stolen — making sure you have enough separateness that you can be an object of curiosity for the other person.”
NCMS Alliance Holding Program on Mental Health and Support Services in Wilmington

The North Carolina Medical Society Alliance and the New Hanover Pender County Medical Society invite physicians and their spouses to a program on mental health and support resources.
Speakers include Betsy Gall, author of The Illusion of the Perfect Profession, and Joseph Jordan, CEO of the North Carolina Professionals Health Program.
The event is February 26 at the Pine Valley Country Club in Wilmington. Dinner begins at 6:30pm with the program starting at 7. Spouses are encouraged to attend.
Find out more here.
NC DHHS: Two NC Pediatric Flu Deaths Reported

NCDHHS Announces First Pediatric Flu Deaths of 2024-25 Season, Urges Vaccination for Children Ages 6 Months and Older
The North Carolina Department of Health and Human Services is reporting two pediatric flu-related deaths, the first for the 2024-2025 flu season. One child in the Eastern region and another in the Central region of the state recently died due to complications of influenza. To protect both families’ privacy, additional information will not be released about these cases.
"We at the North Carolina Department of Health and Human Services extend our deepest sympathies to the families of these children," said State Epidemiologist Zack Moore, M.D, MPH. "This is a sad reminder that seasonal influenza can be serious and, in some cases, even fatal. If you or your loved ones have not received the flu vaccine this season, please consider doing so to help protect your family and those around you."
North Carolina has seen a rise in flu cases in recent weeks in combination with continued COVID-19 activity, and 171 adult flu-associated deaths have already been reported in North Carolina this season. NCDHHS tracks influenza, COVID-19, RSV and other respiratory viruses that may be circulating and publishes data weekly on the Respiratory Virus Surveillance Dashboard.
Flu vaccinations are especially important for children who are at higher risk of developing severe disease or complications, including those younger than 5 years old, especially under 2 years, or those with chronic health conditions like asthma, diabetes or a weakened immune system.
The CDC recommends all children ages 6 months and older receive a seasonal flu vaccine and an updated COVID-19 vaccine. Parents should also talk with their health care provider about options to protect infants from severe RSV disease, including vaccines for pregnant women during weeks 32 through 36 of pregnancy.
Early testing and treatment with an antiviral drug can also help prevent flu and COVID-19 infections from becoming more serious in children. Antiviral treatment works best if started soon after symptoms begin.
In addition to vaccines and treatment, everyone should take the following preventive actions to protect themselves and their loved ones against respiratory viruses:
- Regularly wash your hands with soap and water or use an alcohol-based cleaner or sanitizer to prevent the spread of viruses to others
- Avoid touching your eyes, nose and mouth
- Clean and disinfect frequently touched surfaces and objects that may be contaminated
- Cover coughs and sneezes with a tissue and then discard the tissue promptly
- Stay home when sick, except to seek medical care or testing, and take steps to avoid spreading infection to others in your home, including:
- Staying in a separate room from other household members, if possible
- Using a separate bathroom, if possible
- Avoiding contact with other members of the household and pets
- Not sharing personal household items, like cups, towels and utensils
- Wearing a mask when around other people
For more information on respiratory viruses, including how to access vaccines, testing and treatment in your community, visit vaccines.gov/en, flu.ncdhhs.gov or covid.19.ncdhhs.gov.
Those Plastic Takeout Containers Might Come With a Free Side of Heart Problems

New Study: Eating from plastic takeout containers can increase heart failure risk
(The Guardian) -- Eating from plastic takeout containers may significantly increase the chance of congestive heart failure, a new study finds, and researchers suspect they have identified why: changes to gut biome cause inflammation that damages the circulatory system.
The novel two part, peer-reviewed study from Chinese researchers adds to mounting evidence of the risks associated with eating from plastic, and builds on previous evidence linking plastic chemicals to heart disease.
The authors used a two-part approach, first looking into the frequency with which over 3,000 people in China ate from plastic takeout containers, and whether they had heart disease. They then exposed rats to plastic chemicals in water that was boiled and poured in carryout containers to extract chemicals.
“The data revealed that high-frequency exposure to plastics is significantly associated with an increased risk of congestive heart failure,” the authors wrote.
Plastic can contain any of about 20,000 chemicals, and many of them, such as BPA, phthalates and Pfas, present health risks. The chemicals are often found in food and food packaging, and are linked to a range of problems from cancer to reproductive harm.
While researchers in the new paper didn’t check which specific chemicals were leaching from the plastic, they noted the link between common plastic compounds and heart disease, and a previous link between gut biome and heart disease.
They put boiling water in the containers for one, five or 15 minutes because plastic chemicals leach at much higher rates when hot contents are placed in containers – the study cited previous research that found as many as 4.2m microplastic particles per sq cm can leach from plastic containers that are microwaved.
The authors then gave rats the water contaminated with leachate to drink for several months, then analyzed the gut biome and metabolites in the feces. It found notable changes.
“It indicated that ingestion of these leachates altered the intestinal microenvironment, affected gut microbiota composition, and modified gut microbiota metabolites, particularly those linked to inflammation and oxidative stress,” the authors wrote.
They then checked the rats’ heart muscle tissue and found it had been damaged. The study did not find a statistical difference in the changes and damage among rats that were exposed to water that had been in contact with plastic for one minute versus five or fifteen.
The study does not make recommendations on how consumers can protect themselves. But public health advocates say to avoid microwaving or adding hot food to plastic containers at home, or cooking anything in plastic. Replacing plastic utensils or packaging at home with glass, wood or stainless steel alternatives is also helpful.
It is more difficult to avoid plastic when getting carryout. One can bring their own glass packaging or transfer food to glass packaging when one gets home.
'E-reporting' Daily Symptoms Boosts Cancer Patients' Well-Being

New Study: Cancer Patients Who Check In Daily Gain Better Quality of Life
(HealthDay News, Ernie Mundell) -- Patients with advanced cancers who checked in daily with their care teams electronically gained a better quality of life, a new study concludes.
This "patient-reported outcome" (PRO) strategy did not improve patients' survival, the study found. But it did help their care teams spot and treat issues such as pain and frailty earlier, easing daily symptoms.
“Doctors and nurses are often unaware of symptoms and side effects that can worsen for cancer patients between office visits, leading to complications and unnecessary suffering,” lead study author Dr. Ethan Basch explained. He's a professor of medicine and chief of medical oncology at the University of North Carolina School of Medicine.
PRO "was developed to enable patients to report their own symptoms and side effects, and our study showed that PRO keeps care teams informed so that they can intervene promptly to help patients," said Basch, who also directs the Cancer Outcomes Research Program at UNC Lineberger in Chapel Hill.
His team published its findings recently in the journal Nature Medicine.
PRO works by electronically providing patients with easy-to-understand checklists they can use to rate daily issues such as pain or mobility. Patients send their feedback, via computer or smartphone, to their care teams, all from the comfort of their homes.
But are these technologies really helping patients?
To find out, the new study involved nearly 1,200 U.S. patients with metastatic (later-stage) cancers, cared for at 52 oncology practices across 26 states.
About half of patients were monitored with the help of the PRO system, while the other half got usual care, checking in with their care teams in the traditional way.
The patients' average age was 63. In all, 26% lived in rural areas and 17% had never used the internet.
Use of PRO had no impact on how long patients lived, the study found.
However, the system did seem to boost a patient's quality of life.
Among the findings:
- Delays in deterioration of physical function. Patients using PRO began to falter in their physical abilities at a median of 12.6 months, versus 8.5 months for those monitored in the traditional way. (Median means half faltered sooner, half later.)
- Better quality of life. Patients using PRO saw a significant (28%) improvement of their quality of life that lasted an average 15.6 months, compared to 12.2 months for folks not using the technology.
- Fewer emergency room visits. People using PRO required an average 6.1% fewer trips to the ER, and had a 16% longer period before their first ER visit, compared to folks using traditional care.
- Better sense of control. Patients using PRO tended to say that they felt more in charge of their well-being (84% saying so), while 77% said it improved communication with their care teams. The vast majority (91%) said they'd recommend PRO to other patients.
Basch noted that the PRO system used in the study did not rely on physicians, who are already often overloaded with paperwork.
“PRO largely circumvents physicians and is managed by nurses and/or patient navigators, whose jobs often encompass symptom management and care coordination," he explained in a UNC news release. "The PRO systems have also proven very easy for patients to use, in terms of technical ability."
The PRO system performed well across a variety of cancer types. While this study focused on patients with advanced cancers, it's hoped that future trials will examine its performance among people battling cancer in its earlier stages, Basch said.
"We certainly hope researchers will take an interest in establishing more studies to provide evidence of that benefit," he concluded.
More information
Find out more about patient-reported outcomes at the Commonwealth Fund.
SOURCE: University of North Carolina at Chapel Hill, news release, Feb. 7, 2025
Learning Opportunity: Long-COVID: Select Updates on Definitions, Burden of Disease, and More

Pfizer Vaccines Offers Webinar on Long-COVID
The Pfizer Vaccines US Medical Affairs Team is holding an educational webinar, Long-COVID: Select Updates on Definitions, Burden of Disease and More
Date and Time: Thursday, 20 February 2025: 12:00 pm – 12:30 pm ET
Speaker: Jenny Boucher, PharmD
US Medical Director, Pfizer mRNA Vaccines, Medical and Scientific Affairs
Click here to Register www.translatingmRNA.com
Intended Audience: US healthcare professionals including physicians, nurse practitioners, pharmacists, and physician assistants.
Continuing medical education credit is NOT associated with this event.
For US Full Prescribing Information and EUA Fact Sheet for Healthcare Providers, please review:
EUA Fact Sheet for Healthcare Providers
Achoo! Flu Season in U.S. is Most Intense it's Been in at Least 15 Years

If it feels like everyone you know is wheezing all over the place, you’re probably right.
(AP) -- The U.S. winter virus season is in full force, and by one measure is the most intense in 15 years.
One indicator of flu activity is the percentage of doctor’s office visits driven by flu-like symptoms. Last week, that number was clearly higher than the peak of any winter flu season since 2009-2010, when a swine flu pandemic hit the nation, according to data posted Friday morning by the Centers for Disease Control and Prevention.
Of course, other viral infections can be mistaken for flu. But COVID-19 appears to be on the decline, according to hospital data and to CDC modeling projections. Available data also suggests another respiratory illness, RSV, has been fading nationally.
The flu has forced schools to shut down in some states. The Godley Independent School District, a 3,200-student system near Fort Worth, Texas, last week closed for three days after 650 students and 60 staff were out Tuesday.
Jeff Meador, a district spokesman, said the vast majority of illnesses there have been flu, plus some strep throat. He called it the worst flu season he could remember.
So far this season, the CDC estimates, there have been at least 24 million flu illnesses, 310,000 hospitalizations and 13,000 deaths — including at least 57 children. Traditionally, flu season peaks around February.
Overall, 43 states reported high or very high flu activity last week. Flu was most intense in the South, Southwest and western states.
In Rochester, New York, the flu season has been intense but not necessarily worse than at the peak of other years, said Dr. Elizabeth Murray, a pediatric emergency medicine doctor at the University of Rochester Medical Center.
She said there’s a lot of flu, but there’s also still a lot of RSV and a surprising number of babies with COVID-19.
“All of the respiratory illnesses are around, with a vengeance,” Murray added.
The CDC declined to let an Associated Press reporter speak to an agency flu expert about recent trends. The Trump administration ordered a temporary “pause” on health agency communications and has continued to refuse interview requests that were routinely granted in the past.
Late Friday afternoon, a CDC spokesperson acknowledged that the new data shows “the highest absolute value” of flu-like illness when compared with other seasons, but added that the statistic is complicated: That value references a baseline estimate for doctor’s office visits, but the baseline is recalculated every year. In late January, the CDC was describing the season as “moderate” in severity.
U.S. health officials recommends that everyone 6 months and older get an annual flu vaccination.
About 44% of adults got flu shots this winter, the same as last winter. But coverage of children is way down, at about 45% this winter. It’s usually around 50%, according to CDC data.
About 23% of U.S. adults were up to date in their COVID-19 vaccinations as of late January, up from about 20% at the same point in time the year before. COVID-19 vaccination rates for kids were about the same, at around 12%.
The government has not yet reported its estimates of how well this season’s flu vaccine is working.
Testing results from patients indicate that two strains of seasonal flu that are causing most illnesses — a Type A H1N1 and a Type A H3N2. Health officials are closely watching a third strain — a bird flu known as Type A H5N1 — that has sickened tens of millions of animals, but is known to have infected only 67 people in the U.S.
To avoid seasonal viruses, doctors say you should avoid touching your eyes, nose and mouth because germs can spread that way. You should also wash your hands with soap and water, clean frequently touched surfaces and avoid close contact with people who are sick.
Call for Nominations to the NCMS Foundation Board of Trustees

The NCMS Foundation Board Development Committee Submits:
Call for Nominations: NCMS Foundation Board of Trustees
Overview
The call for nominations for individuals to serve on the NCMS Foundation Board of Trustees is now open. Nominations are due by May 30, 2025 (view NCMS Foundation Candidate Application Form here).
The North Carolina Medical Society Foundation (NCMSF) is the philanthropic arm of the North Carolina Medical Society. The mission of the NCMSF is to improve access to quality health care for all North Carolinians. Our portfolio of programs demonstrates our commitment to this vision. Learn more about each of these programs here.
Those who serve on the NCMS Foundation’s Board of Trustees have general experience with and understanding of a philanthropic, 501c3 organization. Trustees are willing and able to articulate the purpose of each of the Foundation’s initiatives, and, ideally, will be able to offer details about their firsthand experience with a particular NCMS Foundation program and the value it brings to the profession and to North Carolina. Knowledge about the challenges health care professionals and their patients face and a desire to be innovative and collaborative in finding solutions is essential to this role. Fundraising ability also is crucial to fulfilling the Foundation’s mission of improving access to quality health care for everyone in the state.
In 2025, the NCMS Foundation will be filling the following leadership positions:
- Board of Trustee: Up to three (3) Trustees to serve three-year terms.
- NCMS Foundation Board of Trustee Expectations
- Current NCMS Foundation Board of Trustee Members
Process
- Candidates are nominated or may nominate themselves for a position on the NCMS Foundation Board of Trustees (view NCMS Foundation Candidate Application Form here).
- Once a candidate submits their application form, they will receive a confirmation email and made aware of any follow-up if needed.
- Upon careful review of submitted materials, the NCMS Foundation Board Development Committee will select candidates to be interviewed. Candidates will be notified via email by June 6, 2025 if they are selected for an interview. Interviews will be conducted via videoconference in the evening during the week of July 14, 2025 (date TBD).
- Following candidate interviews, the NCMS Foundation Board Development Committee will vote to select candidate(s) to fill open leadership positions. The NCMS Foundation Board of Trustees will approve the slate of candidates at the August 20, 2025 board meeting.
- The Board of Trustees slate of candidates will be submitted to the NCMS Board of Directors for approval and appointment at the October 10, 2025 board meeting.
*All nominations and any information collected as part of the nominating process is strictly confidential.
UNC Researchers Outline New Research Priorities in Neuropalliative Care

Neurologists Winnie K. Lau, MD, and David Y. Hwang, MD, highlight needed research in the emerging field of neuropalliative care
(UNC Health Newsroom) -- Neurological disease, from Alzheimer’s disease to stroke and epilepsy, can impact a person’s life in many ways. It can alter their ability to speak, move, think or lead an independent life. And it can have a significant impact on their families and loved ones, too.
An emerging field, termed “neuropalliative care,” has taken shape over the past few years to help provide impactful, holistic care for patients with serious neurological disease. And now, experts in the field are seeking ways to improve the overall wellbeing of their patients and loved ones through the power of research.
A special communication in JAMA Neurology, first-authored by Winnie K. Lau, MD, a neurocritical care physician and associate professor of neurology and senior-authored by David Y. Hwang, MD, professor of neurology and division chief of neurocritical care, describes needed research that can help advance patient care, including:
- identification and measurements of key symptoms and outcomes,
- studying effective care delivery and implementation,
- and improving communication about prognosis.
“Neurological disorders are among the leading causes of overall death and disability in the world,” said Hwang. “Research suggests that palliative care-related needs and quality of life needs for neurology patients are comparable to those of some other serious diseases, like cancer, where palliative care has traditionally been more integrated.”
Despite the growing need, relatively sparse research has been done to evaluate and improve palliative care in patients with neurological disease. To draw attention to this critical gap in knowledge, Lau and Hwang met with other members of the International Neuropalliative Care Society (INPCS) Research Committee—comprised of clinicians, researchers, therapists, social workers, people with neurological disease, and their care givers—to help identify new research priorities.

“When we move forward with medical research, we should really be looking at the symptoms and the things that matter the most to the patients and their family members,” said Lau, who also studies stroke and family communications in the ICU.
“And when we think about delivering that care, we need to think about it in the context of the spaces that they live in and the limitations that we should be working around.”
Neurological diseases can affect communication or cognition, making it challenging for patients to effectively communicate with their care team about their health. In cases of severe or progressive neurological disease, patients may need to rely on family members and care partners, termed proxies, to communicate their needs or wishes with their care team.
Lau and colleagues write that more technological tools, such as eye tracking communication devices and sleep trackers, could potentially assist with patient self-reporting and autonomy. In a similar vein, the field should focus on figuring out new ways to carry out goal-concordant care, or care that aligns with the values of the patient, when patients themselves are unable to communicate those goals.
Neuropalliative care is provided everywhere, including acute inpatient settings, nursing facilities, clinics, or even at home. Just like any other kind of medical care, practitioners in the neuropalliative field need to adapt their medical interventions to fit the setting using available resources. Lau and colleagues challenge other practitioners to take interventions proven to be efficacious and find ways to incorporate and adapt them into different setting where neuropalliative care needs exist.

Quality-of-life (QOL) is typically associated with social life, physical health, and general mental health. However, loss of identity, spiritual distress, financial burden, and stigma can also have significant impacts on patients and their care partners. Lau and colleagues write that future research on should focus on more holistic QOL factors, in addition to more traditional quality-of-life factors like pain, anxiety, role limitations, etc.
In addition to outlining research needs, Lau and Hwang challenge funding agencies to consider initiatives that are more focused on supportive care needs, in addition to “cures.” Although cures are incredibly important, many patients with neurological disorders benefit from palliative care throughout their lifetimes, even while pursuing curative treatments.
“We did make a case that that more attention from traditional funding agencies for this type of research would be helpful,” said Hwang. “There are a lot of funding gaps within the medical field, and even within neurology. I think it was important for us to not only highlight what the consensus in terms of where research would be needed, but also make the case of what would need to be in place for that actually to happen.”
New Research: GLP-1 Meds Can Work Wonders for Kidney Health

Benefits of GLP1-RA Therapy Provides Support of the Kidney-Protective Effect
(HealthDay News, Ernie Mundell) -- Ozempic, Wegovy, Saxenda, Trulicity: These and other GLP1-RA diabetes/weight-loss meds can also boost outcomes for folks battling chronic kidney disease, new research shows.
Compared to another common class of kidney medications, called DPP4is, GLP1-RA medications did better in helping slow the progression of kidney disease, keeping kidney disease patients out of the hospital and helping them survive.
“The benefits of GLP1-RA therapy for blood glucose management are well known, but our research provides much-needed evidence in support of the [kidney]-protective effect of GLP1-RAs in high-risk patients with moderate to advanced chronic kidney disease,” said study first author Dr. Shuyao Zhang. She is an assistant professor of internal medicine at UT Southwestern in Dallas.
Over the two-year study, Zhang's team followed the medical records of 64,705 veterans with diabetes and chronic kidney disease (CKD), half of whom took a DPP4i medication and half of whom took a GLP1-RA.
Folks who took one of the latter class of drugs were 16% less likely to die, 10% less likely to need hospital care and 36% less apt to see their kidney disease progress, compared to patients taking a DPP4i drug, the study found.
“People with diabetes and chronic kidney disease have a very high risk of complications" such as low blood sugar, infections or cardiovascular events, study co-senior author Dr. Ildiko Lingvay noted.
“Yet this population is much less likely to be included in clinical trials or be treated with medications that have proven benefits," said Lingvay, a professor of internal medicine at UT Southwestern.
"Our findings demonstrate that GLP1-RAs can lead to fewer cardiovascular events, less progression of kidney disease, and lower health care costs," she added in a university news release. "These are very impactful outcomes that support the widespread benefits of this class of medications in this high-risk population.”
“Historically, diabetic kidney disease has been difficult to address,” Zhang concluded.
“With further research, we could eventually see new guidelines that include GLP1-RAs as part of a comprehensive treatment approach for diabetes-related kidney disease, potentially improving long-term outcomes and enhancing patient quality of life,” she added.
The findings were published recently in Nature Communications.
Health Cuts Temporarily Blocked as Scientists Warn of Crippling Impact, NC is One of 22 States Suing to Stop Cuts

Temporary Block Means NIH Will Continue to Grant Payments
(DailySkim Health) -- What's going on: A federal judge temporarily blocked President Donald Trump's plan to slash billions in research funding to the National Institutes of Health (NIH) on Monday just hours after 22 states sued to stop it. The NIH had planned to cap “indirect costs” — funds that cover essentials like lab equipment and maintenance by 15%, a move that universities and medical centers say would gut key medical research. Scientists warn in the lawsuit that the cuts would derail medical advancements, stating that “cutting-edge work to cure and treat human disease will grind to a halt.” While scientists view these costs as essential, some Republicans have called them unnecessary.
What it means: The judge ordered the NIH to continue grant payments and provide compliance reports within 24 hours. Before the injunction, scientists warned the cuts could undermine facilities tackling critical health issues like cancer and heart disease, while also exacerbating existing disparities in women’s health. A 2023 analysis found that just 8.8% of NIH grants from 2013-2023 went to women’s health research, even as the agency's overall budget grew. The funding cuts also coincide with the NIH's decision to end a decades-long initiative aimed at diversifying the biomedical workforce. Experts argue that curbing diversity narrows the pool of contributors and the scope of the research, potentially leaving valuable discoveries untapped.
Additional Reading:
Judge Blocks Proposed NIH Funding Cap After 22 States File Lawsuit
Attorney General Jeff Jackson Wins Temporary Restraining Order to Prevent Unlawful Health Care Cuts
NIH cuts will cost Triangle universities millions. Now NC is suing Trump to block action
National Council of Nonprofits Report on Executive Orders Affecting Charitable Nonprofits
Share Your Prior Authorization Story!
Are you a physician frustrated with the administrative headaches and their impact on your patients?
Have you ever faced denials for a care plan within standard practice for a patient?
Please tell the NCMS how prior authorization has impacted you and your patients.
We are looking for stories from physicians to highlight and draw attention to this issue that is impacting the health of so many North Carolinians.
Click here to tell the NCMS more!
NIH Announces It's Slashing Funding For Indirect Research Costs

The agency estimated that it could save $4 billion by capping indirect costs at 15%
(NBC News, Alexandra Marquez and Evan Bush) -- The National Institutes of Health announced Friday that the agency is making cuts to grants that support research institutions by limiting the amount of indirect funding for research projects to just 15%.
In the agency’s announcement, the NIH’s Office of Policy for Extramural Research Administration, or OPERA, wrote that $9 billion of the $35 billion total spent on research grants in fiscal year 2023 was allocated from the agency for indirect costs, which cover things like equipment, operations, maintenance, accounting and personnel.
When a scientist receives a federal NIH grant for a project — say $500,000 per year — the institution that houses that scientist’s work receives an additional percentage for those indirect costs. Those rates are negotiated between the grantor and the university or research institution.
“The indirect system makes sense on a certain level. You have to support the infrastructure of a place. I can’t erect a new building every time I get a research grant,” said Michael Eisen, a University of California, Berkeley, biologist. “I’m not paying for electricity in my lab, I’m not paying for HVAC, I’m not paying for janitors.”
The memo noted that the average indirect costs rate for organizations receiving NIH grants was between 27% and 28%, but could sometimes be even higher.
OPERA noted in the memo that it arrived at the 15% standard indirect rate by looking at the indirect cost rates at several private foundations that fund research grants, like the Robert Wood Johnson Foundation, the Carnegie Corporation of New York and the John Templeton Foundation, all of which have maximum indirect cost rates of between 10% and 15%.
“The United States should have the best medical research in the world. It is accordingly vital to ensure that as many funds as possible go towards direct scientific research costs rather than administrative overhead,” OPERA wrote in its guidance.
The agency also estimated that it could save $4 billion by capping indirect costs at 15%.
But scientists at various institutions of research and higher education were quick to point out that cutting indirect costs could be detrimental to research studies because it would mean slashing funding for lab space, researchers and supplies — all considered essential for scientific research.
“A sane government would never do this,” Jeffrey Flier, the former dean of Harvard Medical School, wrote in a post on X.
Eisen said he viewed the indirect funding system as byzantine, opaque and worthy of re-examination.
“I understand the sentiment to look at universities and say, ‘The administrations have grown massively, there’s deans all over the place and there’s money going into this nebulous void. Why should taxpayers being paying for that stuff?’” Eisen said. “I would welcome a real careful rethink of how grants are structured and where money goes in a grant and who is in charge of allocating it, with more transparency and clarity on where the money is going.”
But Eisen said the new guidance from NIH was a “crude” and “poorly thought out” approach that would shift the weight of supporting research to universities rather than the federal government.
“It’s basically saying: ‘You’ve got all this money, universities, you spend it on research, why should the government spend it on research?’” Eisen said. “Most universities don’t have the funds to step in and cover this. It’s not viable.”
Eisen said he thought the effect of the policy, if it remains in its current form, would be less biomedical research, overall.
“This is going to have a bad effect on research. If you don’t want to research to happen, you can accomplish it this way,” Eisen said.
Katie Miller, one of President Donald Trump’s appointees to the newly formed Department of Government Efficiency, or DOGE, celebrated the move in a post on X, writing, “President Trump is doing away with Liberal DEI Deans’ slush fund. This cuts just Harvard’s outrageous price gouging by ~$250M/ year,” accusing researchers at Harvard who accept NIH grants of having high indirect cost rates.
The Senate has not confirmed a new NIH director. Dr. Jay Bhattacharya, a Stanford University professor, was nominated for the position by Trump. His confirmation hearings have not been scheduled yet.
“Certainly, this is going to come up,” Eisen said.
Breast Cancer: Fear of Recurrence Can Haunt Women for Years

Tumor recurrence fear can wreak havoc on a woman's emotions
(HealthDay News, Ernie Mundell) -- A survey of hundreds of breast cancer survivors finds that tumor recurrence fear can wreak havoc on a woman's emotions.
“Cancer is all around us. Everything is a trigger," one survey participant said. "Anniversaries, other family/friends’ diagnosis, commercials about drugs, social media, etc. …it’s a daily thought or a daily emotion.”
All of the 347 women surveyed "were reportedly disease free and trying to rebuild their lives during their post-treatment survivorship," noted study lead author Shelley Johns.
She said the women's testimonials give "clarity about how breast cancer survivors are impacted by fear of recurrence and insight into how they cope with this understandable fear.”
Johns is a researcher-clinician with the Regenstrief Institute at Indiana University in Indianapolis. Her team published its findings recently in the journal Supportive Care in Cancer.
Women reacted with a range of emotions to the knowledge that their cancer did have a chance of returning.
Some said the issue was mildly disrupting to their lives, while others were more severely affected.
In milder cases, intrusive thoughts and worries about cancer recurrence happened only sporadically, while in tougher cases these issues were persistent and easily triggered.
For many women, sleep disturbances were an issue, as were irritability, sadness and stress. Many women worried that they focused on cancer's return more than the average survivor and felt shame that they did so.
One woman said she would sometimes "sit for hours doing nothing, do not turn on TV, sleepless, find hours pass by and I am in the same place just thinking, do not participate in activities, get lost driving because I’m deep in thought, compulsive online shopping, collecting things.”
Physical triggers were also common.
"Whenever I feel any kind of pain or discomfort in the area where I had cancer it concerns me and I feel anxious and irritable," one woman said.
However, many women surveyed said they'd also developed strategies to help them cope with their fears.
“Just trying to be positive, eat healthy, take my meds, get enough sleep, exercise three times a week, and hope for the best," one survivor said.
Prayer and meditation helped another woman, and one survivor cited disconnecting from certain media.
Another said "I also speak with family members who have lived with cancer longer than myself," to help keep her spirits up.
For some, there was a healthy upside to their focus on keeping cancer at bay.
“It motivates me to maintain healthy habits," one woman said. "Such as eating five servings of fruits and vegetables, working out and drinking less alcohol. It also motivates me to maintain mental health and physical health.”
Mood Swings are Like Clockwork. What is Best Part of Day?

New Study: Mental Health is Better in the Morning
(Nice News) -- “Never go to bed angry” is an oft-repeated piece of advice directed toward couples. But a recent study might suggest otherwise.
To explore how mental health and well-being fluctuate throughout the day, researchers from University College London analyzed data from nearly 50,000 people surveyed over a dozen times in a two-year span. The takeaway: Mornings have an edge over evening hours, at least from a mental health perspective.
“On average, people seem to feel best early in the day and worst late at night,” lead study author Feifei Bu told CNN. She added that earlier in the day, people reported less severe depressive symptoms as well as increased happiness, life satisfaction, and sense of life being worthwhile.
These findings could make mental health resources more effective (i.e. increasing late night availability for mental health lines), and potentially help people better manage disagreements and such.
“Research suggests that mood is relatively stable in the late morning, which makes it easier to handle tough topics with a level head and emotional distance,” added Pamela Rutledge, a psychology professor who was not involved in the study. In other words? We may want to take the other time-tested advice and just “sleep on it.”
Are Eggs Safe to Eat as Bird Flu Spreads?

Here’s what experts want you to know
(New York Times, Dani Blum) -- Bird flu is striking chickens across the country, causing shortages and pushing up prices at retailers and restaurants. Last week, one of the nation’s largest egg producers said that hens at one of its Indiana farms had tested positive for avian influenza.
Researchers have stressed that bird flu still poses a minimal risk to the general public, though that may change as the virus continues to circulate and potentially mutate. But the many empty shelves in stores and higher prices on the eggs that people can find have raised concerns among consumers about the safety of the egg supply.
At this point, experts say it’s unlikely that an egg contaminated with avian influenza would make it to grocery stores. Federal regulations require that commercially packaged eggs be washed and sanitized, which helps remove virus particles from the outside of the shell.
The virus itself also rapidly sickens hens. Egg producers, noticing the first infected birds, can respond by culling the rest of the flock. And any birds that are infected would likely die of their illnesses before they could produce contaminated eggs.
“Dead birds don’t lay eggs,” said Dr. Gail Hansen, a veterinary public health expert and consultant in Washington, D.C. When the virus does affect a flock, its eggs are typically removed from the food supply.
Scientists are still trying to figure out whether humans can contract avian influenza by eating or drinking products contaminated with the virus. Most of the at least 66 people infected in the United States since 2024 contracted the virus through contact with sick animals.
Still, it seems likely that the virus can be transmitted through certain foods: Monkeys have fallen ill after drinking raw milk that contained the virus. Cats have died after consuming tainted milk and uncooked pet food.
The virus is especially prevalent in the udders of cows, which means that unpasteurized milk can contain high concentrations of the virus, said Stacey L. Schultz-Cherry, a virologist and influenza expert at St. Jude Children’s Research Hospital. Less of the virus may end up in eggs, although it’s hard to say for certain without comparative studies, said Matthew Moore, an associate professor of food science at the University of Massachusetts Amherst. But “even provided that you somehow did a ‘Rocky’ type thing and just ate it raw,” the probability of contracting bird flu from an egg “is still pretty low,” he said.
If you want to be extra cautious, pasteurized egg products — like liquid egg whites that come in cartons — are considered safe, since pasteurization inactivates the virus.
And cooking eggs thoroughly kills the virus. The Centers for Disease Control and Prevention recommend cooking eggs to an internal temperature of 165 degrees, meaning that yolks should be firm, and that scrambled eggs should not be runny.
“The bottom line is that if people are using good food-handling practices and fully cooking their eggs as recommended, then the risk is extremely low,” said Dr. Meghan Davis, a veterinarian and environmental epidemiologist at the Johns Hopkins Bloomberg School of Public Health.
Experts also recommend common-sense food safety measures: If you’re handling raw eggs, thoroughly wash your hands and clean any cooking surfaces or pans with soap and water after use.
And resist the temptation to grab a spoonful of raw cookie dough or cake batter — not just to minimize any potential risk of avian influenza, but to avoid far more common pathogens, like salmonella, that can cause food poisoning. These infections can be especially serious for young children, older adults, pregnant women and people who are immunocompromised — but they can make anyone feel miserable for a few days.
“Those are really strong reasons to still remind people to handle eggs properly,” Dr. Moore said. “Especially if you’re going to spend a lot of money for them — don’t get diarrhea from it.”
NCDHHS Invests $3 Million to Expand Child First

NCDHHS Invests $3 Million to Expand Child First, Strengthening Support for Young Children and Families Across North Carolina
The North Carolina Department of Health and Human Services is investing $3 million to expand access to Child First, an evidence-based, early childhood intervention program proven to reduce the risk of child maltreatment and prevent young children and families from entering the foster care system. This investment, awarded to Alliance Health, Trillium Health Resources and Vaya Health, will expand Child First services to additional counties across the state, providing critical, community-based access to behavioral health care and family support services.
Child First is a nationally recognized, two-generation care model that provides home-based clinical therapy for young children (prenatal through age five) and their parents or primary caregivers while also connecting families to essential resources in their communities. The program has been proven to strengthen parent-child relationships, reduce maternal depression and build resilience for families experiencing challenges like poverty, domestic violence, substance abuse, homelessness or incarceration.
Child First is a front-end, upstream resource that can support young families before abuse or neglect occurs, preventing the need for intervention through child welfare services in the future.
"We know that the earliest years of life set the foundation for a child’s future health and well-being," said North Carolina Health and Human Services Secretary Dev Sangvai. "By expanding access to Child First, we are ensuring that more families receive the support they need to create stable, nurturing environments where young children can thrive."
The goal of NCDHHS’ $3 million investment is to expand access to evidence-based programs in underserved communities in North Carolina to improve outcomes for children and families. Trillium Health Resources and Alliance Health have been awarded $1 million each to expand Child First into a combined 22 additional counties across the state. Vaya Health has dedicated $350,000 to expanding Child First in western North Carolina, and the remainder of their $1 million award will support other evidence-based behavioral health programs, including Parent-Child Interaction Therapy and Trauma-Focused Cognitive Behavioral Therapy.
Child First is currently available in 31 North Carolina counties through providers such as Children’s Home Society, RHA Health Services, Easter Seals PORT Health and Coastal Horizons. With this expansion, more families will have access to trauma-informed, family-focused care and support in their own homes.
"Investing in early intervention and prevention services is one of the most effective ways we can support children and families, helping them build stability and resilience before a challenge becomes a crisis," said NCDHHS Deputy Secretary for Opportunity and Well-Being Susan Osborne. "By expanding access to Child First, we are ensuring more families receive comprehensive, evidence-based support – laying the foundation for lifelong health and well-being."
To strengthen the overall impact of the program across the state, NCDHHS is launching a Child First Learning Collaborative. The collaborative will bring together providers, the participating LME/MCOs and Child First NC partners to assess the program’s effectiveness, support successful implementation and help to inform the department’s future investments in evidence-based, community-based services.
This initiative is part of the department’s broader $835 million investment to transform behavioral health in North Carolina. Of these funds, $80 million is committed to building a child behavioral health system that improves outcomes for children and families through trauma-informed, family-centered care. The goal is to integrate a continuum of services into North Carolina’s homes, communities and schools to meet children and families where they are, ensuring access to the right services at the right time to meet their needs.
For more information, go to the Child First NC website.
🎉It's New Member Monday!🎉

Join us in welcoming these new members to the North Carolina Medical Society!
- Rozita Akhbari, MD
- Maham Ali, MD
- Michele M. Gandolfi, MD
- Brett L. MacLean, MD
- Jose D. Mena Pasquel, MD
- Claire Namboodri, MD
- Prathna R. Patel, PA-C
- Douglas C. Vander Kooi, MD
We are thrilled to have you!
Not a member but would like to be? Joining is simple. Visit our membership center here.
How Well Do You Know NC State Government? Here's All You Need to Know

As a new session begins, here’s everything you need to know about North Carolina government
A link to the NCMS Advocacy Team efforts is at the bottom of this article.
(EdNC, Chantal Brown and Ben Humphries) -- Welcome to a comprehensive guide to the North Carolina state government. Below is everything you need to know if you want to understand (and participate in) the process of governance.
Much of the information in this article is sourced from the North Carolina constitution and relevant state government websites.
Legislative power
Article II of our state constitution vests legislative power in the N.C. General Assembly.
From 1898-2010, Democrats largely controlled the legislature. Republicans have held power since 2011.
Each session of the General Assembly in North Carolina convenes for two years — often referred to as a biennium. The current session is the “long” session, which started on Jan. 8. During this session, bills are introduced, and a two-year budget is adopted. Each biennium, the state House and Senate alternate which chamber takes the lead on budget legislation; this time around, it is the Senate.
Typically, the long session lasts until around July, although sometimes it stretches on longer. There is no statutory or constitutional requirement for when a session ends.
The “short” session will convene in spring 2026. Bills that have passed one house, recommendations from a study commission, and issues related to the budget are in play during the short session.
There are 120 members in the House of Representatives and 50 members in the Senate. All legislators in both houses serve two-year terms, and there are no term limits for legislators in North Carolina.
Those elected to the General Assembly serve part-time and often have other jobs back home. During session, they typically meet on Monday evenings, Tuesdays, Wednesdays, and Thursdays.
Both chambers — the House and the Senate — are in the Legislative Building. It is located at 16 West Jones Street in Raleigh. Rooms in the building have four digits (e.g. “1226”).
The Legislative Office Building, which houses many of the offices for legislators as well as larger committee rooms, is located across the street from the Legislative Building at 300 North Salisbury Street. There is a bridge over Lane Street that connects the two buildings. Rooms in the Legislative Office Building have three digits (e.g. “544”).
The House of Representatives
The speaker of the House is Destin Hall, R-Caldwell. He was newly elected as speaker this year and is serving his fifth term in the House.
Currently, there are 71 Republicans and 48 Democrats in the House, with one vacancy. There are 17 new members; 35 women members; 28 Black/African American members; one American Indian member; two Asian American members; and one Hispanic member. Here is a folder with member information, including seats, demographics, birthdays, military experience, representation by county, terms served, and occupations and education.
Here is information on House leadership. Here are office assignments. Here is information on committees. Information on bill deadlines can be found here (see rule 31.1).
The Senate
Rachel Hunt, a Democrat, is the lieutenant governor and president of the Senate. Though not a legislator, the lieutenant governor serves as the presiding officer of the Senate and has the power to vote when the members of the Senate are equally divided.
The president pro tempore of the Senate is Phil Berger, R-Rockingham. He has served as president pro tempore since 2011; this is his 13th term.
In the Senate, there are 30 Republicans and 20 Democrats. There are five new members; 16 women members; 10 Black/African American members; two Indian American members; and one Asian American member. Here is a folder with member information including seats, demographics, birthdays, military experience, representation by county, terms served, and occupations and education.
Here is information on Senate leadership. Here are office assignments. Here is information on committees. Information on bill deadlines can be found here (see rule 40.2).
Other things to know about the legislature
On the General Assembly’s website, both the House and Senate post their meeting calendars. Check there to see when bills are taken up in committees and on the floor. Plans are always subject to change as the session goes on.
Other factions that play key roles along the journey of a bill are the fiscal research division, the legislative drafting division, and the legislative analysis division.
This graphic lays out how a bill becomes a law in North Carolina.
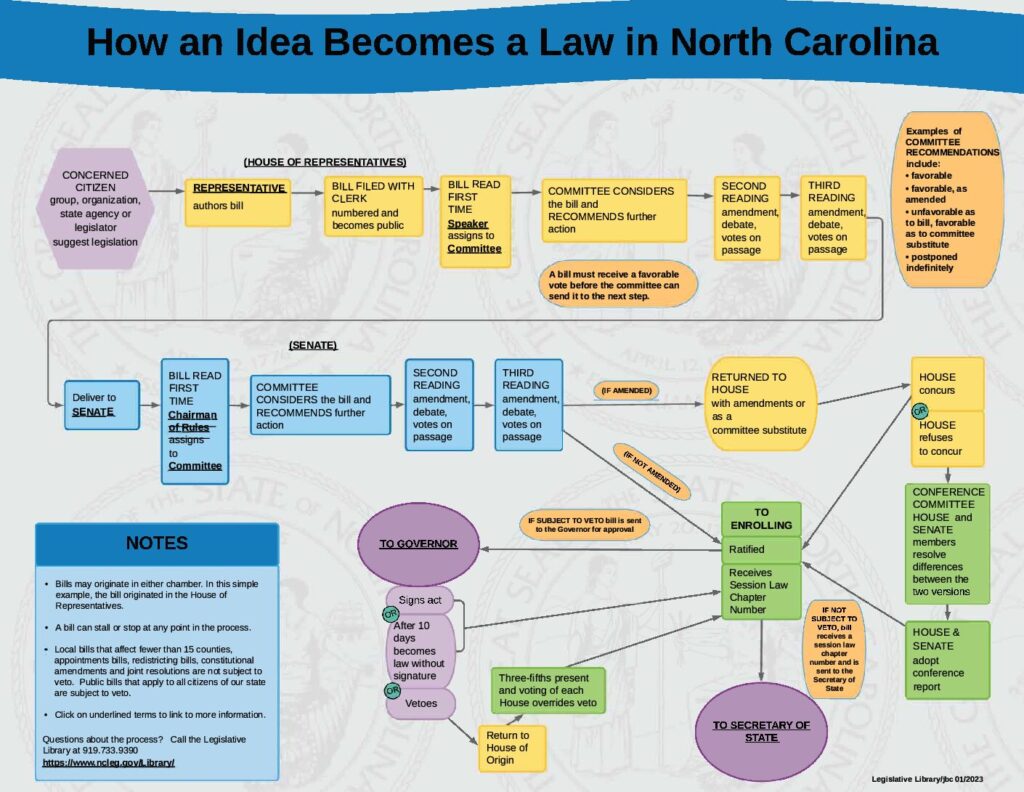
One part of the lawmaking process is lobbying. A lobbyist is a person who works to influence legislators and political decisions. They are often hired by and act on behalf of specific organizations or people. Instructions on how to become registered as a lobbyist are here.
Executive power
Article III of the state constitution vests executive power in the governor. Here is the website for Gov. Josh Stein, a Democrat.
One part of the governor’s role in the long session is to propose a budget.
The governor has a few other powers. One is to issue executive orders. Here is where you can keep track of all executive orders. Another is the power to veto legislation. In fact, North Carolina’s governor was the last in the United States to receive veto power in 1996. Here is where you can see how many bills have been vetoed each session.
Unofficially, the governor can leverage their status as a public figure to sway North Carolina citizens into supporting or opposing legislation coming down the pipeline — also known as using the bully pulpit.
The Council of State includes the lieutenant governor, the secretary of state, the auditor, the treasurer, the superintendent of public instruction, the attorney general, and the commissioners of agriculture, labor, and insurance — all of which are elected positions. There are five Republicans and five Democrats (including the governor) on the Council of State.
Cabinet positions are appointed by the governor. These include the secretaries of administration, commerce, environmental quality, health and human resources, information technology, military and veterans affairs, natural and cultural resources, public safety, revenue, and transportation. The governor’s chief of staff, director of the office of state human resources, and the state budget director meet with the cabinet.
The governor also his his own staff, including Jonathan Krebs as his Western North Carolina Recovery advisor.
By statute, there is also an education cabinet. The governor serves as chair, and the education cabinet also includes the superintendent of public instruction, the chair of the State Board of Education, the president of the UNC System, the president of the N.C. Community College System, and the president of the N.C. Independent Colleges and Universities.
Agencies and offices to note
North Carolina has three independent executive agencies: the Office of Administrative Hearings, the Office of the State Controller, and the State Board of Elections.
The N.C. State Education Assistance Authority (NCSEAA) “is a political subdivision of the state, governed by a nine-member Board of Directors, with administrative support provided by the University of North Carolina.”
Here is the website of the Office of State Budget and Management. Kristin Walker is the state budget director.
Judicial power
Justices of the Supreme Court, judges of the Court of Appeals, and judges of the Superior Courts of North Carolina are all elected positions, all of which serve eight-year terms.
Currently, there is an ongoing legal battle surrounding the results of the 2024 NC Supreme Court elections. Read more about it here.
EdNC has also continuously covered the Leandro lawsuit which established a state constitutional right to access a sound, basic education.
Education
Section 4 of Article IX of our state constitution establishes the roles of the State Board of Education and the superintendent of public instruction. Here is the website of the State Board of Education, here are the members, and here are the meeting dates for 2025. Eric Davis is chair of the Board.
The superintendent of public instruction is Maurice “Mo” Green, a Democrat. Here is the website for the Department of Public Instruction.
Here is where you can find information about charter schools.
There is a Division of Non-Public Education in the state Department of Administration. Here you can find information about home schools, and here you can find information about private schools.
The federal government
The current acting secretary of the U.S. Department of Education is Denise Carter, pending U.S. Senate confirmation of Linda McMahon.
Local governments
North Carolina has 100 counties. Counties provide local funding for education.
There are 115 school districts, often referred to as LEAs or PSUs, or local education agencies and public school units, respectively.
Each district has an elected (partisan or nonpartisan) or appointed school board and a superintendent. Here is where you can explore information about all of North Carolina’s school districts.
Contact your representatives
As the long session ramps up, one of the most important things to know is how to find and contact your representatives so you can advocate and be a part of the legislative process. Here you can search for your representatives by your address.
If you are interested in learning more about the NCMS Advocacy Team efforts click here.
New Study Shows High Burnout in Healthcare Impacting Both Patients and Doctors

Study: 81 percent of doctors can't spend as much time with patients as they'd like
(WITN, GREENVILLE, NC) -- A healthcare group released a new study showing an increase in healthcare burnout in both patients and doctors.
MDVIP is a healthcare group with over 13-hundred primary care physicians nationwide that found that the frustration of long waits for appointments and rushed doctor’s visits aren’t only felt by patients.
The study says 81% of doctors say they can’t spend as much time with their patients as they’d like.
Dr. Andrea Klemes, MDVIP Chief Medical Officer told WITN, “Doctors may have, especially primary care doctors, may have over 2,000 patients in their practice and all these patients are competing for appointments and so while they’re trying to get everyone in, working 50-60 hour work weeks, they’re seeing 20-25 patients a day so there’s really not enough time to spend with patients. 2/3rds of doctors said that healthcare has gotten transactional, not relational so you know, without that doctor/patient relationship, patients just feel like a number.”
The study reports that if doctors had more time, 78% say they would spend it getting to the root cause of patient issues, and 77% would focus on patient health span and longevity.
According to MDVIP, due to the challenges, fewer patients are prioritizing their health by not going to see their primary care physicians.
Regardless of the many frustrations, Klemes says it’s vital to take advantage of your visits.
“Make a list and tell your doctor about the list at the beginning of the appointment so they can leave time. Make that first appointment in the morning or the one after lunch, and if you feel that you’re not getting what you need -- talk to your doctor about it, and if it’s still not a great fit, then you can look for other physicians that maybe have smaller patient panels or that maybe have more time to focus on you,” Klemes said.
The study also showed burnout in healthcare workers with 52% of doctors saying they wouldn’t go into primary care if they could do it over again.
WITN reached out to over a dozen local doctors and patients in the east about the new study. However, many declined or WITN did not hear back in time for this story.
Medical Education Leadership Opportunities Available at AMA Council

Want to get more involved?
The AMA Council on Medical Education is soliciting candidates
The AMA Council on Medical Education is currently soliciting candidates for nomination opportunities for the following:
- American Board of Medical Specialties (ABMS) Stakeholder Council
- American Board of Psychiatry and Neurology – Psychiatry Director
- Accreditation Council for Graduate Medical Education (ACGME) Review Committees for:
-
- Colon and Rectal Surgery
- Medical Genetics and Genomics
- Nuclear Medicine
- Orthopaedic Surgery
- Pathology
- Preventive Medicine
- Psychiatry
- Radiology
-
The deadline for applications for these opportunities is Thursday, February 20, 2025.
Position descriptions and applications for each opportunity can be found on the AMA’s website at: Medical Education Leadership Opportunities.
Questions? Contact Mary Grandau, Program Specialist II, AMA Council on Medical Education, at [email protected].
Whether you're a Red Coater or rooting for The Birds, you're definitely going to be eating on Sunday! NCMS has some ideas for you!
Super Bowl LIX is Sunday at 6:30pm in New Orleans
Whether you're a Red Coater or rooting for The Birds, you're definitely going to be eating on Sunday!
The Kansas City Chiefs are hoping for a three-peat as the Philadelphia Eagles look for payback in New Orleans this weekend.
One way or the other, history will be made at the conclusion of Super Bowl LIX. Either the Chiefs will be the first team to win three Super Bowls in a row, or the Eagles will become the first team to win a Super Bowl "rematch" after losing the first game.
If you are looking to enjoy the day and enjoy some grub without guilt, the NCMS has pulled together some places for you to look for healthier options on your Super Bowl spread.
Let us know if you try any of these!
45 Health Super Bowl Snack Recipes to Keep You Feeling Like A Winner on Game Day
10 Healthy Super Bowl Recipes to Add to Your Lineup
30+ Healthy Super Bowl Recipes That Score Big
50 Healthy Super Bowl Snacks for a Feel-Good Game Day Spread
And if you plan to just go for it on Sunday:
Whip Up These Super Bowl Snacks Inspired by Chiefs and Eagles
17 Super Bowl Recipes for Philadelphia Eagles Fans
19 Super Bowl Recipes That Kansas City Chiefs Fans Will Love
FDA OKs Clinical Trials for Pig Kidney Transplants in People

Two biotech companies have been cleared to begin studies this year.
(HealthDay News, India Edwards) -- The U.S. Food and Drug Administration has approved the first-ever clinical trials testing pig kidney transplants in people with kidney failure, marking a major step forward in cross-species transplantation.
Two biotechnology companies, United Therapeutics Corp. and eGenesis, have been cleared to begin their studies this year.
If successful, these trials could revolutionize organ transplantation, helping address the severe shortage of donor kidneys.
"We are entering a transformative era in organ transplantation," Mike Curtis, president and chief executive of eGenesis, told The New York Times.
United Therapeutics Corp. will start its study with six patients. All have been on dialysis for at least six months and have no other serious medical problems. The trial will eventually expand to 50 participants if the first transplants go well. eGenesis will begin with three patients, increasing in stages.
Doctors will monitor each transplant patient for 24 weeks and require lifelong follow-ups to track health outcomes and potential risks such as pathogens that could cross from pigs to humans, according to The Times.
More than 550,000 Americans have kidney failure, and nearly 100,000 people are on the transplant waiting list. Yet fewer than 25,000 kidney transplants were performed in 2023, and many patients wait years or die before receiving a donor organ, according to The Times.
Genetically engineered pigs offer a promising solution because their organs are similar in size and function to human kidneys.
Both of the companies have modified pig genes to reduce the risk of organ rejection and improve compatibility with human bodies.
United Therapeutics pigs have undergone 10 gene edits, adding six human genes and removing four porcine genes linked to rejection.
eGenesis pigs have undergone 69 gene edits, most to inactivate viruses that could pose a risk to humans.
While the potential benefits of cross-species transplantation are groundbreaking, concerns about safety and ethics persist.
Some experts worry about known pathogens jumping from pigs to humans, though both companies raise their pigs in pathogen-free facilities that adhere to strict biosecurity protocols and regularly screen the animals for pathogens, The Times reported.
Christopher Bobier, an associate professor specializing in bioethics and health policy at Central Michigan University College of Medicine, told The Times that in a worst-case scenario, the recipient of an animal's organ "could become infected with an undetected pathogen from the porcine source."
Others question whether patients can truly give consent, considering how difficult it is for people on dialysis to refuse a potential life-saving solution.
"Saying no would be incredibly difficult," Bobier said. "Fully grasping the lifelong implications of that decision would be even harder."
United Therapeutics expects to begin transplants by mid-2025, with a few months between procedures to assess each outcome before moving forward.
eGenesis plans to wait six months between its first two patients, then three months before transplanting a third.
Even if these trials prove successful, the cost of pig organ transplants and whether insurance will cover them remain unclear, according to The Times.
NCDHHS: Seasonal Respiratory Illnesses Surge in North Carolina

Respiratory Virus Summary Dashboard Shows Increase in Flu-Related Deaths
(RALEIGH) -- The North Carolina Department of Health and Human Services updated its weekly Respiratory Virus Summary Dashboard, which shows an increase in flu activity and flu-related deaths, bringing the total number of deaths this season to 117.
"While fewer flu-related deaths have been reported so far this season compared to last season, we are at the height of seasonal respiratory illnesses and this is a reminder that influenza can be very serious," said State Epidemiologist Zack Moore, M.D., MPH. "Taking preventative measures against flu and other respiratory illnesses like getting vaccinated, regularly washing hands, covering your cough and staying home when sick are important to help protect you and your family."
Influenza is spreading widely throughout the state and is likely to peak in the coming weeks. Fifty-one new flu deaths were added to the statewide dashboard on Wednesday, but the newly added deaths occurred over the last few weeks as there are often delays in reporting. COVID-19 and respiratory syncytial virus (RSV) are also continuing to spread, although RSV levels have been decreasing in recent weeks.
Early testing and treatment with an antiviral drug can help prevent respiratory infections from becoming more serious. Treatments work best if started soon after symptoms begin. If you begin to feel sick, contact your doctor right away to see if you need treatment with a prescription antiviral drug. Treatment for flu and COVID-19 is especially important for people with severe illness and those who are at high risk of serious complications based on their age or medical conditions.
It is not too late to get your flu and COVID-19 vaccinations as vaccinations are the best way to prevent serious illness, hospitalization and death from these infections. Vaccinations are especially important for those at higher risk of severe viral respiratory disease, including people 65 years and older, children younger than 5, pregnant women, those with a weakened immune system and those with certain medical conditions such as asthma, diabetes, heart disease and obesity. Vaccines and treatments to protect against RSV are also available for older adults, pregnant women, and infants.
In addition to vaccination, the following precautions should be taken to protect against the spread of respiratory viruses:
- Regularly wash your hands with soap and water. Alcohol-based cleaner or sanitizer can help prevent the spread of respiratory viruses to others but does not work for some other common viruses like norovirus.
- Avoid touching your eyes, nose and mouth
- Clean and disinfect frequently touched surfaces and objects that may be contaminated
- Cover coughs and sneezes with a tissue and then discard the tissue promptly
- Stay home when sick, except to seek medical care or testing, and take steps to avoid spreading infection to others in your home, including:
- Staying in a separate room from other household members, if possible
- Using a separate bathroom, if possible
- Avoiding contact with other members of the household and pets
- Not sharing personal household items, like cups, towels and utensils
- Wearing a mask when around other people
For more information on respiratory viruses, including how to access vaccines, testing and treatment in your community, visit www.vaccines.gov/en, flu.ncdhhs.gov or covid19.ncdhhs.gov.
A respiratory virus surveillance summary that includes information on flu, COVID-19 and RSV-related activity across North Carolina is updated weekly at covid19.ncdhhs.gov/dashboard.
NC Diabetes Advisory Council Publishes New Guide to Prevention and Management of Diabetes
In North Carolina, 12.4 percent of the adult population have diabetes and 34.6 percent are at high risk of developing type 2 diabetes. The state is 11th in the nation for diabetes-related deaths. To address the complexities of diabetes, the NC Diabetes Advisory Council has developed the third edition of the Guide to Prevention and Management of Diabetes.
The Guide is organized around four levels of social and environmental concepts described by the Centers for Disease Control and Prevention and the Socio-Ecological Model of Health. It addresses what diabetes looks like in North Carolina and focuses on individuals at risk. It provides specific strategies for community groups, employers and healthcare providers and shares opportunities to focus on what can be done to reduce the burden of diabetes.
To see the full Guide to Prevention and Management of Diabetes click here.
New Study: High Levels of Microplastics in Human Brains Appear to be Increasing

Study: People Inhale or Ingest Up to 114,000 Microplastics Yearly
(CBS News Healthwatch) -- Human brains contain higher concentrations of microplastics than other organs, according to a new study, and the amount appears to be increasing over time.
In the study, published Monday in the journal Nature Medicine, University of New Mexico Health Sciences researchers found microplastics in human brains have increased 50% over the past 8 years. They also found that people with dementia had up to 10 times as much plastic in their brains as everyone else.Microplastics are tiny fragments of degraded polymers that are found in the environment, including our air, water and soil, a news release explained. Previous studies have already shown these substances have made their way into the human body.
The lead researcher, toxicologist Matthew Campen, said the rate of accumulation they found mirrors the increasing amounts of plastics waste on the planet. And he said in the news release that their findings should trigger alarm about the potential impact on human health.
The study compared liver, kidney and brain tissue samples from autopsies conducted in 2016 and 2024, and found "substantially higher concentrations" in the 2024 brain tissue. The researchers also conducted similar analysis on older and more recent autopsies for people who died with confirmed dementia diagnoses, and found "far greater" concentrations.
While it's unclear how particles are actually being transported into the brain, Campen said the size of the micro- and nanoplastics, measuring 200 nanometers or less, are not much larger than viruses and therefore small enough to cross the blood-brain barrier.
In the study, researchers detected 12 different polymers, the most common of which was polyethylene, widely used for packaging and containers, including bottles and cups, the release noted.
Campen suspects most microplastics in the body are ingested through food, particularly meat.
"The way we irrigate fields with plastic-contaminated water, we postulate that the plastics build up there," he said. "We feed those crops to our livestock. We take the manure and put it back on the field, so there may be a sort of feed-forward biomagnification."
The team also found high concentrations of plastic in meat bought at grocery stores.
As for the higher levels found in the brains of dementia patients, the researchers noted the study was not designed to prove whether that was the cause of symptoms — it may be the reverse, that the disease process allows more accumulation to happen.
"Atrophy of brain tissue, impaired blood–brain barrier integrity and poor clearance mechanisms are hallmarks of dementia and would be anticipated to increase [micro- and nanoplastic] concentrations," they wrote.
Duke Named a Global Virus Network Center of Excellence

(Duke University School of Medicine, Dave Hart) -- Duke University School of Medicine has joined the Global Virus Network (GVN) as one of its newest Centers of Excellence.
The GVN, headquartered at the University of South Florida, is a coalition of eminent human and animal virologists from more than 80 institutions in over 40 countries. The organization works collaboratively to train the next generation, advance knowledge about how to identify and diagnose pandemic viruses, mitigate and control how such viruses spread and make us sick, as well as develop drugs, vaccines, and treatments to combat them.
The GVN named Duke, along with the Czech Republic’s National Institute of Virology and Bacteriology, the University of Pennsylvania Perelman School of Medicine, and the Yale School of Public Health, as new Centers of Excellence.
“We are pleased to announce GVN’s newest Centers of Excellence,” said Robert C. Gallo, MD, chairman of the Scientific Leadership Board and co-founder of the GVN. "By fostering collaboration, driving innovation, and advancing scientific understanding, we are strengthening and enhancing the global health infrastructure. Each of these four new Centers brings invaluable expertise, and together, we will expand the frontiers of virus research and control, ensuring the protection of future generations from emerging threats."
The GVN announcement said Duke includes several entities that will collaborate well with the GVN. Duke Research and Discovery @RTP is a research hub for School of Medicine scientists devoted to the study of infectious diseases. The Duke Global Health Institute works to achieve health equity for vulnerable groups and individuals around the world through research, education and partnership. The Duke Human Vaccine Institute (DHVI) continues to lead with cutting edge basic immunology and vaccine research against infectious diseases that impact global health.
Scientists at the DHVI conduct basic and translational research to develop novel vaccines, therapeutics, and diagnostics for diseases such as HIV-1, influenza, SARS-CoV-2, tuberculosis, syphilis, and herpes viruses. Products from several DHVI basic science discoveries are currently being produced in DHVI’s Good Manufacturing Practice facilities for early phase vaccine trials.
“We look forward to working with the GVN to help develop diagnostics for emerging pathogens, manufacture investigational biologics for use in Phase I clinical trials, and help conduct human trials of monoclonal antibodies or vaccines for re-emerging or emerging pathogens, ” said Thomas N. Denny, MSc, M.Phil, the new GVN Center of Excellence director and chief operating officer of DHVI, associate dean for Duke Research and Discovery @RTP, and professor of medicine.
New NC Health Secretary Dr. Devdutta Sangvai Outlines Priorities

New NC health secretary reveals priorities: improving healthcare access and child welfare
(News & Observer, Luciana Perez Uribe Guinassi) -- Dr. Devdutta Sangvai* was sworn in last month as the 19th secretary of North Carolina’s Department of Health and Human Services, becoming the first Indian American cabinet member under a North Carolina governor.
Gov. Josh Stein appointed Sangvai, a family medicine physician and Duke University professor, to lead one of the state’s largest agencies.
Having previously served as president of Duke Regional Hospital and the North Carolina Medical Society, Sangvai also brings private sector experience to DHHS — experience he told The News & Observer he hopes to leverage.
“I’m really excited to partner with the General Assembly to continue moving forward on some of these things we’ve already outlined for the future of North Carolina,” he told The N&O. “When I think about the 11 million citizens — and the 11 million people — we serve day in and day out, it’s that perspective that really excites me to be in this role.”
The leadership transition comes as the state faces shifts at both state and federal levels: North Carolina’s new governor and a new slate of Council of State members were elected in November. Nationally, President Donald Trump, in his first weeks in office, has signaled major shifts in policy, including in health care, that are expected to affect states.
Sangvai succeeds Kody Kinsley, who took over the agency in early 2022. Kinsley, the first openly gay cabinet secretary in North Carolina history, oversaw aspects of the state’s COVID-19 pandemic response, the historic expansion of Medicaid, behavioral health investments and more.
However, he also faced challenges, including lawsuits over inadequate services for underserved populations. In an interview, Sangvai outlined his vision for addressing challenges, improving service delivery and expanding access to care for all North Carolinians.
This interview has been edited for clarity and length.
DHHS priorities
Q: What are some of your priorities?
A: Part of my excitement in this role was the incredible foundation that we’ve laid in North Carolina. As you think across health and human services, we probably have the best-in-class Medicaid program and really foundational human services programs.
So when you think about the work we’ve done around everything from behavioral health to medical debt, I was excited to come into the agency at a time when that foundation has been laid.
Note: To encourage states that had not expanded Medicaid to get on board, the federal government allotted a $1.6 billion or so “signing bonus” to new states. After North Carolina passed Medicaid expansion with bi-partisan support, the General Assembly used part of that signing bonus to fund about $835 million for behavioral health. DHHS used some of those funds to increase the rates paid to Medicaid providers for behavioral health services, among other things.
The state also got approval by the federal government last year for a plan that leverages Medicaid funds to relieve existing hospital medical debt for people in the state.
Among my priorities is to continue that work. We’ve got work to continue to do with Medicaid. We have a pretty significant behavioral health investment, and so I’m excited to see how we roll that out.
We are also strengthening our relationship with our stakeholders and county partners, and to that end, there are a few areas that I’m particularly interested in.
One is to really strengthen access in North Carolina and make sure communities have access to the type of services they need. I also want to work to ensure that our programs and services are working for all North Carolinians.
The third piece I’m really focused on is building a sustainable workforce in North Carolina. We have a shortage across almost every healthcare job type and even in the human services job types. So, what can we do to really retain people in North Carolina, and what can we do to recruit individuals into those crucial roles?
Possible Medicaid changes
Q: In terms of Medicaid and continuing to bolster it, as well as behavioral health services, can you share more on how you plan to do that? Especially considering the possibility that Medicaid could face cuts under the Trump administration?
Note: Congressional Republicans are reportedly considering changes to Medicaid to fund immigration initiatives and tax cuts desired by President Donald Trump. But on Friday, Trump said he would not institute cuts to Medicaid, save for fraud and abuse, as reported by various outlets.
A: On the behavioral health front, we have been fortunate to have $835 million appropriated through the General Assembly for the work that we are going to do to improve behavioral health. Part of that has already been allocated to increase rates, so we can really create a cadre of providers in the community.
Our position is that these types of services are best served and meet the needs of people when they are offered in the communities in which individuals live and work. There’s also additional work (needed) to create more community-based services around behavioral health, particularly with the justice-involved population.
One of the things I’m interested in is creating sustainable programs as we spend that money. So, not only how do we meet the immediate need, but how do we lay a further foundation to ensure that those dollars are going to build sustainable programs?
On the Medicaid front, I think we have one of the best Medicaid programs in the country. If you look back at the last six to eight years, a number of very deliberate, thoughtful steps were taken to figure out how to ensure that we have a program that is best in class and meets the needs of as many people as possible. That was achieved through bipartisan support.
I think that’s a really important element of what we have in North Carolina, and nearly every stakeholder —providers, beneficiaries, elected officials, even local law enforcement — were really important in helping us understand how to put together a Medicaid program, and in particular, Medicaid expansion.
I think what you have there is a spirit of collaboration and consensus building, and I’m hopeful that as we start to see changes from the federal government, we can rely on that to really think about what our impact might be.
Until then, our goal is to continue to put people first and serve those who really depend on us.
Access to care
Q: What are some of the ways you’re thinking about improving access to care?
A: When I think about access to care, it’s really across the continuum. It’s not just the services that we provide here that are directly related to the work that the department does, but it’s also the broader health care landscape.
What can we do to ensure that providers, for example, are able to see as many people as possible? So are there technology tools that we can use to give providers more face-to-face time with their patients or their clients? Are there technology tools to reduce administrative burden on that front?
Similarly, on our side, on the agency side, are there things we can do to really get that value, so that the time that individuals are spending is really in direct service to beneficiaries, and not, if you will, spent doing things that don’t provide direct value.
Q: Are there any particular technologies that you’re thinking of, or any particular administrative task or red tape that you see impacting providers being able to give the best care they can give?
A: Well, I think everyone is going to look to figure out the role AI will play across various industries, including health and human services. I’d like to explore where we might have AI tools that can help us better identify individuals at risk or tools that allow those providing direct services to do so more efficiently. Also, some of this doesn’t need to be as fancy as AI. We will be implementing a new software platform that will allow county DSS offices to work more collaboratively with one another, streamline documentation on the case management platform, and help individuals understand what’s happening in adjacent and surrounding counties.
Note: The official name of the new Child Welfare Information System is “PATH NC,” which stands for “Partnership and Technology Hub.”
Child Welfare Services
Q: DHHS is facing lawsuits regarding failures with child welfare services provision in the state. Can you share more details about that tool and any other ideas for how to improve child welfare services in the state?
Note: One lawsuit alleges DHHS unnecessarily warehouses foster children in locked psychiatric facilities and another accuses DHHS of endangering thousands of children by failing to fix the state’s child welfare system. This second lawsuit also accuses DHHS of failing to develop and implement a comprehensive electronic record and case management system.
North Carolina has a county-administered social service system, meaning that counties largely control child welfare services, while the state provides guidance and some oversight.
A: As you know, we have a decentralized model where the department works in close collaboration with the county agencies to help meet those goals together. So what can we do to help support those county agencies, either through processes or procedures? I think the software tool is going to help because, as you may know, part of the work that’s been previously done has been done on paper, and a modern workforce is more accustomed to doing things on an electronic platform.
(PATH NC) is going to allow us to do data and analytics a little more effectively, so we can really understand who the children in the system are, where they are, and what types of services they’ve received. The plan is to start implementation and roll out this year. The other challenge, of course, is staffing at these agencies. These agencies face the same staffing challenges that we have at the central office. As we think about the type of efficiency that a software tool can provide, we might energize individuals into thinking this is a place where they want to start a career or build a career, because it’s modern, effective, and provides data and feedback. I feel like there are multiple things that will move in a forward direction as we start rolling out the software and working more closely with our county partners.
Staffing shortages
Q: So on the challenge of staffing shortages across DHHS, beyond the technological improvements, what steps will you take to recruit more people?
A: My experience in the private sector has informed me well in this space. We faced the same staffing challenges at private hospitals. One of the things I learned is that there is clearly a role for salary and benefits in that conversation. I think the state has done a good job, and this agency has done a good job prior to my arrival, in understanding what we can do to make salaries more competitive. What can we offer in the form of retention bonuses? What can we do in the context of sign-on bonuses? And, of course, we’re working with the Office of State Human Resources to understand what we can and cannot do in that space.
I think we need to take it a step further, based on my further experience, and start asking the question: What does it take to make you feel like you belong, and what does it take for you to find joy in your work? In my previous experience, what I learned is that it’s not always salary and benefits. It’s about, “How do you make me feel like a member of the team? How do I know that the work I’m doing is contributing to the broader mission? What are you providing for me to build a career? Help me understand what other career options I may have.”
So, the career trajectory piece is another part of it. How do we recruit them, and then, importantly, how do we retain them?
Behavioral Health Services
Q: There’s been lots of reports about how behavioral health services are lacking in the state and DHHS is facing a lawsuit on this as well. So what do you think can be done to further improve?
Note: DHHS and plaintiffs in the Samantha R. case reached an agreement that, among other things, gives DHHS two years to transition more people with disabilities into community-based services. That includes those on the heavily backlogged waitlist for Innovation Waivers, North Carolina’s primary program for individuals with intellectual and developmental disabilities.
North Carolina also faces a shortage of resources for people who need urgent mental health treatment, including in the three state-run facilities that specialize in treating individuals with complex developmental disabilities, as previously reported by The News &. Observer.
A: We know the system isn’t perfect, and we know it’s not functioning the way it should. But what I’m committed to is truly understanding the scope of the issues and then thinking about how we can propose solutions.
Many of these issues overlap, and so, as we think about the work we want to do to support those vital team members in the county agencies, some of the issues they’ll raise regarding services for their beneficiaries and clients will be related to behavioral health. So, part of what I want to understand is where those points of connectivity are, so we don’t need to silo the work as much.
Even if I go back to my three priorities, strengthening access will come from having a more stable workforce. A more stable workforce will come from having individuals experience the benefits that their clients and beneficiaries are getting through our programs and services. So, part of it is an intentional model to figure out how efficient we can be as an organization.
Working with legislators
Q: In terms of working with the General Assembly, how has that been going in terms of getting feedback on funding for your priorities, such as for salary raises?
A: When it comes to the agency’s priorities, it’s still very early. I’m still very much in the process of introducing myself to key legislators. My approach is to first understand what their priorities are as I share ours. Again, I think most health and human services are really understood at the local level, so understanding the specific priorities of legislators, both at the local level and how they roll up in North Carolina, will be part of that initial dialogue.
*Dr. Devdutta Sangvai is a former president of the North Carolina Medical Society
NCMS at Work: Success of NCMS Prior Authorization Press Conference

RALEIGH - On January 28, 2025, the North Carolina Medical Society put prior authorization reform in the spotlight at a press conference at its Raleigh headquarters.
Lawmakers, physicians, advocates, and a cancer patient came together to highlight the inefficient, outdated, costly, and often life-threatening nature of the current prior authorization process. To help make the case for reform, Amanda Watson, a stage 4 metastatic breast cancer patient, detailed her long and painful journey through chemotherapy, radiation, and surgery. She described her diagnosis—just three weeks after the birth of her second son—as shocking. She spent the first months of his life unable to hold or feed him, a time she says was made even more difficult by delays in care due to prior authorization denials.
“It’s hard not to waver in your convictions and not to lose hope during this type of battle,” she said. “When an insurance company can so blindly look at you—not as a person, not as a wife, not as a daughter, not as a mother of two babies … just as a simple word, ‘approved’ or ‘denied.’”
Rep. Timothy Reeder (R-Ayden) was also present. “The time is really now,” he said. “For the Senate to not take up this bill, not hear it, not work on this bill, is something that we’re going to push hard on, both personally and as a chamber.”
Rep. Grant Campbell (R-Concord), a physician, also spoke. He described his experience with prior authorization: “This is about forcing patients and physicians to settle for cheaper, less effective care, or ultimately hoping the patient gives up and pays out of pocket,” he said. As an OB-GYN, Campbell talked about how upsetting it is to be told how to treat a patient by someone who is not in the same field. He emphasized that peer-to-peer reviews are an absolute necessity and that insurance companies are not providing them.
NCMS Board of Directors President Dr. John Meier stated that insurance companies look at costs and may base prior authorization decisions on financial considerations. In contrast, he said, providers focus on the long-term health of the patient. He also argued that the administrative burden on providers and staff takes away valuable time that could be spent caring for patients.
SIGN THE NCMS PRIOR AUTHORIZATION PETITION NOW!
In attendance were:
- Rep. Allen Buansi (D-Dist. 56)
- Rep. Grant Campbell, MD (R- Dist. 83)
- Rep. Maria Cervania (D-Dist. 41)
- Rep. Allen Chesser (R-Dist. 25)
- Sen. Mark Hollo (R-Dist. 45)
- Rep. Timothy Reeder, MD (R-Dist. 9)
- Rep. Donna White (R-Dist. 26)
For those who missed the event, a re-play is available on Facebook Live here.
Special thanks to the Watson family for courageously sharing their story, and to the many news outlets that covered this vital issue, including NC Insider, The Associated Press, WRAL, UNC, NC News Network, WPTF Radio, and Curtis Media Group.
Links to coverage of the NCMS Prior Authorization Press Conference:
- The News & Observer, Reform or ban? Prior authorization for health insurance is under negotiation in NC
- WRAL, North Carolina doctors, patients, lawmakers call for health insurance reform in 2025
- State Affairs, Prior authorizations at issue: Lawmakers call for health insurance reform
- WCNC Charlotte, Advocates call for health insurance reforms in North Carolina
- NC HealthNews, 'Approved or denied': Health care providers say insurers too often deny care for profit
- INsurance Newsnet, NC bill would limit insurers' prior authorizations. Proposed NC bill limits reach of insurers' prior authorizations
Additional reading from NCMS:
- NCMS Pushes for Prior Authorization Reform with Bipartisan Support from Lawmakers
- NCMS CEO Chip Baggett Featured in Podcast About Prior Authorization
- States Cranking Up Oversight of Health Insurers, NCMS Focusing on Prior Authorization in 2025
- The North Carolina Medical Society's highest advocacy priority to REFORM PRIOR AUTHORIZATION NOW
SIGN THE NCMS PRIOR AUTHORIZATION PETITION NOW!
Today is World Cancer Day. How to Support Employees Affected by Cancer.

Companies can help support employees affected by cancer through awareness initiatives, workplace accommodations, and inclusive practices.
(Ashley Campanella) -- Every year on February 4, the world comes together to observe World Cancer Day, an international day dedicated to raising awareness about cancer, promoting prevention, early detection, and treatment, and advocating for better support systems for those affected by the disease. Organized by the Union for International Cancer Control (UICC), this global initiative encourages individuals, organizations, and governments to take action in reducing the impact of cancer.
The Significance of World Cancer Day
Cancer is a leading cause of death globally, with millions of new cases diagnosed each year. The disease affects people of all ages, backgrounds, and socio-economic statuses, making it a critical public health issue. World Cancer Day serves as a powerful reminder that, through collective efforts, we can make a difference in preventing and fighting cancer.
The theme for World Cancer Day is “Close the Care Gap,” which focuses on addressing disparities in cancer care and ensuring that everyone, regardless of their circumstances, has access to the necessary treatments and support. This theme highlights the urgent need to break down barriers related to income, education, geography, and discrimination to ensure equal access to cancer prevention, diagnosis, and treatment.
How Workplaces Can Support Employees on World Cancer Day
Workplaces play a crucial role in raising awareness, offering support, and fostering an environment of inclusivity and care for employees affected by cancer. Here are some ways companies can acknowledge World Cancer Day and accommodate employees:
- Raise Awareness and Education by hosting informational sessions, sharing educational resources via email or newsletters, and encouraging employees to wear ribbons or display signs supporting World Cancer Day.
- Offer Workplace Flexibility and Support such as remote work options or adjusted hours for employees undergoing treatment or caring for a loved one with cancer, implementing paid medical leave, and offering Employee Assistance Programs that offer counseling, mental health support and cancer related resources.
- Encourage Preventative Health Measures like organizing free cancer screenings and health check-ups for employees, healthy workplace initiatives (wellness programs, exercise opportunities or nutritious food options), and providing insurance coverage that includes cancer care, screenings and early detection programs.
- Create a Supportive Work Environment by creating a cancer support network, offering training for managers and HR on how to support employees with cancer, and encourage open conversations to reduce stigma and create an inclusive atmosphere.
- Participate in World Cancer Day Campaigns like organizing fundraising events that support cancer research or donate to organizations, charity runs, walks or virtual events that raise awareness, and engage on social media by using #WorldCancerDay.
A Collective Effort for Change
World Cancer Day is more than just a day of awareness—it is a call to action for individuals, businesses, and communities to work together in the fight against cancer. By making workplaces more accommodating and supportive, companies can create an environment where employees feel valued, understood, and empowered in their cancer journey.
NCMS Board of Directors Meeting Includes 2025 Advocacy Initiatives and Helene Relief Update

Speakers included Kelly Phillips, CEO of CCHN, Chip Baggett, NCMS CEO, Dr. Rebecca Hayes, and new Board President Dr. John Meier
RALEIGH -- The North Carolina Medical Society Board of Directors met with members of the NCMS staff and outside stakeholders in Raleigh on Saturday.
Kelly Phillips was the morning's guest speaker who gave an overview report of Carolina Complete Health Network. She was followed by Chip Baggett who spoke about what 2025 looks like for the Medical Society. He discussed how NCMS is focused on reducing administrative burden, improving the practice of medicine, and how NCMS will support personal and professional growth through KIPL and the NCCPRW.
Baggett also spoke about Hurricane Helene relief. To date, the NCMS has had 38 practices apply for funding and 25 have been funded with approximately $425,000. Priority is being given to smaller practices with physical damage, loss of supplies, and loss of vaccines. The NCMS is helping in the following counties:
- Ashe
- Buncombe
- Burke
- Cleveland
- Henderson
- Madison
- Mitchell
- Yancey
Baggett was followed by the Interim Meeting Report from the AMA by Dr. Rebecca Hayes and the Treasurer's Report by NCMS BOD Secretary Dr. Tracy Eskra.
A robust discussion on advocacy initiatives was led by NCMS Chief Legal Officer Ashley Rodriguez and NCMS VP of Advocacy John Thompson. Look for more information about advocacy efforts from the board in the future.
NCMS Vice President of Membership Pam Highsmith gave a presentation on the 2024 membership results as well a a look ahead at 2025 and a new software program coming by the end of the year. Goals for f2025 include a focus on limited health systems and targeted practices. The membership team is also looking to expand recruitment reach and at an increase in retention.
Highsmith reminded everyone to bring two people to the NCMS February social and the 2025 Advocacy Summit.
NCMS CEO Chip Baggett Featured in Podcast About Prior Authorization

Unpacking the Red Tape: How Prior Authorization Affects Patient Care
Smith Anderson has unveiled its new podcast, Pulse on Carolina Health, a platform dedicated to unpacking critical issues shaping the healthcare landscape in North Carolina.
In the inaugural episode, “Unpacking the Red Tape: How Prior Authorization Affects Patient Care,” health care attorney Robert Shaw sits down with Chip Baggett, CEO of the North Carolina Medical Society, to examine the complexities of prior authorization and its impact on patients and providers. Chip has been at the center of the major trends and policy discussions involving health care in North Carolina for almost 20 years and is an advocate for issues facing the medical community.
Prior authorization, originally intended to ensure clinical necessity for expensive treatments, has become a heated topic across the state and country. Chip explores its evolution from a cost-containment tool into a system that sometimes relies on algorithms, which raises questions about technology’s growing influence in medical decision-making. He discusses how this prior authorization shift has led to uncertainty about who is truly practicing medicine—the doctor, the insurer or the algorithm.
“We have to try to make sure that we’re not denying care to patients, that we’re not frustrating patients and leading them not to get care, and that we're not leading to more mental anguish when a patient is already in a tough spot and then told they can’t get the care the doctor says they need,” said Chip. “Those are some things that I think will drive innovation in this space.”
Podcast host Robert has extensive experience advising companies on health care and regulatory matters. He regularly handles complex restructuring, M&A work on the buyer side and seller side, Medicare and Medicaid audits, value-based care projects, tax planning and controversy, hospital joint ventures, employment agreements, corporate advice and regulatory compliance such as HIPAA, Anti-Kickback Statute, and Stark Law matters. He has been recognized in Chambers USA, Health Care (2023-2024) and The Best Lawyers in America®, Administrative/Regulatory Law (2023-2025).
American health care is undergoing an unprecedented transformation, and Smith Anderson’s team of experienced health care lawyers are committed to guiding medical professionals, hospitals, health care facilities and industry organizations through the attendant changes and evolving regulatory environment. We advise clients nationwide on health care policy, legislative advocacy, executive strategy, mergers and acquisitions, privacy and data security, litigation and the complex business requirements of organized medicine. We have been integrally involved in launching innovative health care delivery initiatives such as clinically integrated networks, joint ventures between health systems and practitioners, Community Care of North Carolina and Accountable Care Organizations (ACOs) nationwide.
Stay tuned for future installments, where industry leaders and experts will tackle the pressing challenges in today's complicated health care system.
Listen to the debut episode of Pulse on Carolina Health here.
Listen and follow this podcast:
Apple Podcasts; Spotify; or your favorite podcast app.
NCMS Member Pens Open Letter to People of Los Angeles

Hurricane Helene, which hit the East Coast last September, submerged Derek Moss' pediatric practice under 5 feet of water. He offers notes on grief and hope. | Flooding in the area around Hendersonville Pediatrics, in Hendersonville, North Carolina. courtesy of Jim Marshall.This article was first published in Zocalo Public Square
First, the Loss. Then, the Insurance
A Pediatrician Whose Office Flooded in Hurricane Helene Offers Los Angeles Notes on Disaster
by NCMS member Derek Moss
Watching the images of fires burning in and around Los Angeles is very triggering. I’m sure it is the same for other Western North Carolinians. It has not been that long since Hurricane Helene caused catastrophic flooding that devastated our communities, and it is not over for us.
At first, you are energized to do what is needed to be done in the moment. But, then, you are left with emptiness, exhaustion, pain, trying to regain something resembling what has been lost.
These emotional twists and turns, highs and lows, have been a central part of my experience of natural disaster. How do you prepare someone for these head-spinning feelings, and for the aftermath, the trauma after the trauma of the weeks and months that follow? For the losses: Home? Business? Neighborhoods? Community? Routine? Safety? Life? For the total disruption.
In the beginning, you hear so many awful stories. People you know who have lost family members, friends. Those who have lost their homes. Places that are no longer there. Chimney Rock, the village I would drive my family through on our way to Lake Lure, gone. Highland Football Club’s soccer fields in Asheville, where our sons played, gone. Biltmore Village, where we have eaten, shopped, slept, gone.
And then there is your own story. My family was safe, and our house was fine, for the most part, but the office where I practice as a pediatrician—and which has served our community since 1952—was completely submerged under 5 feet of water. We lost everything on the first floor: walls, examination tables, files, flooring, cabinets, lab equipment, desks, nursing stations. Only the cement slab and the wall studs were left.
So what comes first is the loss. There are those who lose every possession or almost everything or about half of everything. Then there are those who don’t lose any things. They are still affected, but will sometimes, in conversation, almost seem to forget because they’re existing in a usual, comfortable state.
For many of us, after the loss, there is the insurance—or lack thereof. There are those here who didn’t have flood insurance. On the Carolina coast, when hurricanes destroy homes and buildings, it will be someone without wind insurance. In L.A., it may be that people don’t have the right type of fire insurance. If you do have the correct insurance, it takes months to get the money—that is, if your insurance company doesn’t go bankrupt.
My business, Hendersonville Pediatrics, has yet to receive one cent from an insurance company. We have four policies with two different providers—two of which are flood insurance policies.
People tell you the delay in insurance is the way it is. It’s the government, which runs our primary flood insurance program. It’s the paperwork. You’ve got to roll with it.
But, it’s money.
Money doesn’t drive everything or everyone. There are people who will appear out of nowhere to help. Heroes. The ones flying helicopters to pick people up off of mountains, defending dams, clearing roads, putting out fires, getting your power on, your cell phone service up, giving you your clean, safe water back. Our community has received such an influx of food, medicines, clothes, diapers, sanitary products—things you don’t think about until you don’t have them.
People from within your community appear to help, too—people you have never met before.
Pauline Carpenter at Free Clinics gave Hendersonville Pediatrics space for a doctor four days a week. Richard Hudspeth and the Blue Ridge Health administration allowed us to rent an office to house two doctors five days a week.
But these places are not home. At home, four doctors saw over 100 children, every weekday. People say they love children. But they don’t like hearing them screaming and crying. We are constantly worried: Are we quiet enough? Are they going to kick us out? It is something we cannot control. So we just keep working.
The disaster has not ended for us. It won’t, for years. It probably never will. Because things will never be as they were before. From now on, we know disaster can happen.
What do we do in the meantime? It is up to us in our communities to rebuild, to be the backbone, the strength. In our office, it’s been amazing how supervisors have stepped up to bring order to our practice. Staff changing their schedules. Everyone helping us rebuild our lab, our supplies, our vaccine inventory. That’s the beauty in this type of destruction. Neighbors helping neighbors. People being there for others. Being present. Being in this moment.
NCMS Holds First Regional Meeting of 2025 in Fayetteville

Dozens of physicians and PAs meet to learn more about NCMS priorities and member benefits in Fayetteville
The North Carolina Medical Society held it's first Regional Meeting of 2025 at Luigi's Italian Chophouse in Fayetteville Thursday night.
A crowd of physicians, PAs, Residents , and Students gathered to hear the latest on how NCMS is fighting for them across the state. NCMS Board President, Dr. John Meier spoke to the crowd about how the NCMS is working on Prior Authorization reform, AI, physician burnout, and advocacy events planned for the year. He was followed by NCMS Board member Dr. Karen Smith who gave insight into her experience as an NCMS member and representative to the AMA. She also told the crowd about how the NCMS celebrates diversity and is welcoming to both physicans and PAs.
Other NCMS staff was on hand to answer questions about NCMS membership, NCMS leadership training opportunities, the Community Practitioner Program, and other NCMS perks of membership. Vice President of Advocacy John Thompson updated attendees on the upcoming focus on prior authorization reform and what NCMS is working on in the early days of the new General Assembly in Raleigh.
A robust question and answer session focused on prior authorization with questions that included what NCMS was doing, howe NCMS is working with the AMA on a host of issues, and about the NCMS efforts to bring physicians and PAs to rural and underserved areas of the state.
Breaking: FDA Bans Red Dye No. 3 From Food, Drinks, and Ingested Drugs in US

Red dye No. 3 is found in some candy, food, drugs, and ingested beverages in US
(CNN, Kristen Rogers) -- The US Food and Drug Administration has banned the use of red dye No. 3 in food, beverages and ingested drugs, more than 30 years after scientists discovered links to cancer in animals, the agency announced Wednesday.
A synthetic color additive made from petroleum and chemically known as erythrosine, red dye No. 3 is used to give foods and beverages a bright cherry-red color.
The move acts on a November 2022 petition submitted by multiple advocacy organizations and individuals, including the Center for Science in the Public Interest and the Environmental Working Group, which cited links to cancer. The decision by the federal agency also follows in the footsteps of California, whose government banned the additive in October 2023.
Manufacturers using red No. 3 in food and ingested drugs have until January 15, 2027, and January 18, 2028, respectively, to reformulate their products, according to the FDA. Foods imported to the United States also must comply with the requirements.
“Today’s action by FDA is long overdue, is a small step in the right direction, and hopefully signals a renewed effort by FDA to do its job despite the many barriers the food industry places in its way,” said Dr. Jerold Mande, adjunct professor of nutrition at the Harvard University T.H. Chan School of Public Health, via email.
The decision marks a “monumental victory” for consumer health and safety,” said Ken Cook, cofounder and president of the Environmental Working Group, in a news release. “We wouldn’t be celebrating this historic decision today without the relentless leadership of public health champions like Michael Jacobson and others who took up this fight decades ago on behalf of consumers.”
Red dye No. 3 is found in at least dozens of candy, food and beverage products, but some of the most popular brands either never used, or have already stopped using, the additive. Fewer than 10% of products made by the candy company Ferrara, which produces Brach’s candies, for example, contain the additive, as the company began phasing out the use of it in early 2023, a Ferrara spokesperson said via email.
Just Born, the company behind PEEPS, stopped using red dye No. 3 in its production after Easter of 2024, according to a spokesperson.
Some companies instead utilize red dye No. 40, which has been considered a healthier alternative as it hasn’t been as extensively associated with cancer in animals.
However, California also banned red No. 40 from foods and drinks sold in public schools in September due to concerns over links to behavioral and attention difficulties among children. One study found a potential link to accelerated immune-system tumor growth in mice, and other sources say the dye contains benzene, a known carcinogen.
‘The regulatory paradox’ of dye red No. 3
Red dye No. 3 has been permissible for use in food despite the Delaney Clause of the FDA’s Federal Food, Drug, and Cosmetic Act. The clause, in part, “prohibits the FDA from approving a color additive that is ingested if it causes cancer in animals or humans when ingested,” according to the agency.
The FDA already banned the use of red dye No. 3 in cosmetics and topical drugs in 1990 under the Delaney Clause after research found the additive to be carcinogenic at high doses for rats in lab tests. The mechanism for the dye causing cancer in rats doesn’t occur in humans, so those studies didn’t raise safety concerns, and therefore the FDA didn’t revoke the authorization for red dye No. 3 in food, according to the agency.
The FDA has reevaluated the ingredient’s safety multiple times since its initial approval — based on trials conducted in animals, not humans — in 1969, according to the agency.
There don’t appear to be any studies establishing links between red dye No. 3 and cancer in humans, and “relevant exposure levels to FD&C Red No. 3 for humans are typically much lower than those that cause the effects shown in male rats,” the FDA said in its constituent update posted Wednesday. “Claims that the use of FD&C Red No. 3 in food and in ingested drugs puts people at risk are not supported by the available scientific information.”
But “it doesn’t matter, because the FDA mandate under the Delaney Clause says that if it shows cancer in animals or humans, they’re supposed to keep it from the food supply,” said Dr. Jennifer Pomeranz, associate professor of public health policy and management at New York University’s School of Global Public Health.
The FDA’s decision to revoke the authorization for the use of red dye No. 3 is a matter of law, the agency said.
A few other studies have cast further doubt on the safety of red No. 3, including a 2012 report that found a link between the additive and cancer in animals. That same year, researchers concluded artificial food colorings “are not a main cause of (attention deficit hyperactivity disorder), but they may contribute significantly to some cases, and in some cases may additively push a youngster over the diagnostic threshold.”
Then in 2021, the California Office of Environmental Health Hazard Assessment study found red dye No. 3 can make children vulnerable to behavioral issues, such as decreased attention. The report also concluded that federal levels for safe intake of food dyes at that time may not protect children’s brain health. The study noted that the current legal levels, set decades ago by the FDA, didn’t consider new research, according to the Environmental Working Group.
The FDA’s decision “ends the regulatory paradox of Red 3,” said Dr. Thomas Galligan, principal scientist for food additives and supplements at the Center for Science in the Public Interest in Washington, DC. But the agency “has a long way to go to reform the broken system that allowed Red 3 to remain in foods decades after it was shown to cause cancer when eaten by animals.”
The ban also moves the food landscape slightly closer to that of the European Union, which banned the dye in 1994, with the exception of some maraschino cherry products, Pomeranz said. “Europe takes the precautionary principle when it comes to these things.”
“There is not a rational reason within FDA’s mission that they did not ban red dye #3 from food in the 1990s,” and why the agency takes “so long to ban ingredients with known health harms” is unclear, Pomeranz said via email.
At least 10 other states — besides California — have introduced legislation seeking to ban red No. 3 from foods, according to the Center for Science in the Public Interest.
“Americans are sick because of our food,” Mande said. Though the United States is one of the wealthiest nations, in terms of overall life expectancy, the nation ranks as 49th out of 204 countries.
“This is because food companies have lost sight of their primary mission, providing food we will thrive on, and focusing entirely on their profits instead,” Mande added. “Unfortunately, the U.S. government doesn’t fund the research needed to determine the exact health risks posed by Red Dye #3. Industry works with Congress to block funding for the needed research.”
The National Confectioners Association said in a statement that food safety is the number one priority for US confectionery companies.
“Our consumers and everyone in the food industry want and expect a strong FDA, and a consistent, science-based national regulatory framework,” the association said via email. “For years, our industry has been calling for more transparency, more funding, and more staff resources for the FDA to continue fulfilling its mission, and it’s time to put politics aside and work together to fund the FDA at levels that will allow it to continue its work.”
Food and beverage companies will continue to follow the latest science and comply with all food safety regulations to ensure safe and available choices for consumers, Sarah Gallo, senior vice president of product policy and federal affairs at the Consumer Brands Association, said in a statement via email.
Avoiding dyes in your diet
The FDA has already required manufacturers to list red dye No. 3 as an ingredient on food labels — so if you’re concerned about avoiding products containing the dye until the ban is implemented, check ingredient lists before buying. Red dye No. 3 is also listed as “red 3” and “FD&C Red #3.”
Artificial food colorings are mostly found in ultraprocessed foods and beverages you couldn’t make at home, Pomeranz said, so avoiding those products is another way you can eliminate red dye No. 3 from your diet. The Center for Science in the Public Interest recommends parents avoid all numbered dyes, such as yellow No. 5 and red No. 40, as well.
You can find out how much ultraprocessed food you may be eating by taking this quiz.
For medications that aren’t topical, look for dyes in the “inactive ingredients” section of the drug labeling or package insert, or search for dye-free versions of some drugs, Consumer Reports suggests. But always talk with your doctor before switching medications.
New Survey: Radiation Oncology Burden of Prior Auth in 'Dark Place' - Sign Petition for NC Reform
Survey shows radiation oncology in ‘dark place’ as prior authorization burden worsens
(Healio News, Josh Friedman) -- An American Society of Radiation Oncology survey has shined a spotlight on the impact prior authorization has on providers and patients.
Nearly one-third of the more than 750 radiation oncologists who participated in the survey indicated prior authorization delays led to ED visits, hospitalization or permanent disability for their patients.
In addition, 7% of respondents reported prior authorization contributed to the death of at least one of their patients.
The findings — including the “inordinate number of deaths” — highlight the growing burden prior authorization is causing, according to Fumiko Chino, MD, assistant professor in department of radiation oncology at The University of Texas MD Anderson Cancer Center and Healio Women in Oncology Peer Perspective Board member.
“This is our 2024 temperature check to see where we are and, unfortunately, it shows that we’re in a very dark place,” Chino told Healio.
“We know the patients we have had that prior authorization killed,” she added. “We have them in our hearts.”
‘Who’s watching the watchmen?’
Prior authorization can provide benefit, Chino said.
Some clinicians may use outdated information to dictate treatment, or they may not stay up to date on technological or medical advancements.
The current fee-for-service payment model means that providers get “paid per treatment,” and that may incentivize certain longer regimens, Chino said.
“If the structure of your facility is built on doing 30 treatments for breast cancer, it’s harder to figure out how to keep the lights on in 15 treatments,” Chino said.
Prior authorization’s value comes from “utilization management,” Chino said. It is intended to “[make] sure the treatments that we’re providing for our patients are truly evidence based, and that they will help and not harm them.”
She cited American Board of Internal Medicine’s Choosing Wisely campaign as an example of appropriate resource stewardship. For radiation oncology, it includes consideration of shorter treatment fractionalization or not using radiation at all.
However, she said prior authorization has seemingly been used to mitigate increasing costs of care without consideration of its effects on patients living longer, better lives.
“[Prior authorization] is the guardrails on our physician prescribing, but what we found is that there’s no guardrails on the guardrails,” Chino said. “Who’s watching the watchmen?”
Survey background
ASTRO received online survey responses from 754 radiation oncologists between September and October 2024.
Respondents represented both private practices (51%) and academic institutions (47%).
About half of radiation oncologists who responded to the survey served in urban communities (49%), with more than one-third practicing in suburban (39%) areas and 13% practicing in rural areas.
According to the survey, 85% of radiation oncologists said the prior authorization burden has “increased greatly” (60%) or “increased somewhat” (25%) in the past 3 years.
Additionally, 94% said it worsens staff burnout “significantly” (57%) or “somewhat” (37%).
These issues forced 80% of respondents to reallocate staff time to deal with prior authorization requests, and 64% had to hire more employees.
Radiation oncologists reported several issues involving care, as well:
- 92% said prior authorization delayed treatment;
- 68% said those delays lasted at least 5 days, up from 52% in 2020;
- 82% reported it caused them to use a less-optimal treatment;
- 62% said they have to use less-optimal treatment in more than 10% of cases, up from 32% in 2019;
- 58% said it forced them to not follow recommended guidelines;
- 33% reported patients stopped radiation due to prior authorization;
- 30% said prior authorization led to adverse events, including ED visits, hospitalization and disability; and
- 23% reported they had difficulties getting approval for anti-nausea medications.
“Virtually every person I see will have some sort of prior authorization that is required,” Chino said. “Whether that is a barrier and causes a delay is quite variable but, ever since the COVID-19 pandemic, the prior authorization burden we’ve been seeing in our patient clinics, institutions and societies have only gotten worse.”
‘Meaningful’ improvements
On the positive side, 77% of respondents said more than half of their prior authorization requests went through on the first attempt. That number increased from 69% in 2019.
Additionally, 76% reported more than half of their requests that initially got denied received approval on appeal, up from 62% in 2019.
On average, respondents said 71% of prior authorization requests received initial approval, and 73% that initially got denied received approval on appeal.
“I think there’s this idea that if you just say no, some amount of people will just give up,” Chino said. “They don’t have the resources to do the appeals, or they don’t have the knowhow to understand that you have to work the system to get this approved.
“Making it to the appeal is really important, but that takes resources,” Chino added. “It takes time, and I can’t see a patient or make an elegant radiation plan in that time where I’m arguing with insurance companies. At some point, it can’t just be me and my staff fighting.”
Chino identified multiple ways the process could improve.
Although an expedited appeal occurs within 72 hours — a significant improvement from a few years ago — another reduction could be “really meaningful,” Chino said.
“I’ve had patients who’ve literally had a tumor growing out of their chest,” she said. “Waiting 3 days for an appeal means there’s more cancer to treat, even just in the time between when I made the plan for them initially, and when I actually get to start their treatment. Sometimes it means the plan has to change because the tumor has gotten that much bigger in that time period. Every day matters.”
Insurance companies could also green light regimens that are always approved on appeal, Chino said. This is the concept of the Gold Card system, which has made some headway at the state level.
“Can we maybe not spin our wheels and delay patients, and just facilitate those plans that are going to be approved?” Chino said. “Why are you making the patient wait?”
Payment reform could benefit care, as well.
“ASTRO has a proposed payment model that we put forward that would essentially be bundled payments. It’s a case rate based system,” Chino said. “I want to treat someone with breast cancer in 15 treatments. This person wants to treat them in 30 treatments. Whichever is best for the patient you can do, but you’re going to get paid the same thing.”
Institutions can take their own steps to improving the prior authorization process, as MD Anderson has done, Chino said.
“It has to do with taking a deep dive in the most common insurance providers,” she said. “Looking at what are the things they point to as the reason why they’re denying X, Y or Z plan, and then making sure that we’re showing clearly why this needs to be approved, based on your own criteria. It is a lot of work. It’s a lot of investment, but I do think it benefits patients and the institution with facilitated care.”
In the end, she said growth can only occur if all parties work together to solve the problem.
“We can’t keep pointing fingers,” Chino said. “The doctors point to the insurance and the insurance points to the [pharmacy benefit managers], and then everyone points at the government. It would be nice if we could all just work together to improve care. I feel like it really would benefit people.”
Tell the North Carolina General Assembly, the time is NOW to pass Prior Authorization Reform. Sign the petition!
Reference:
- ASTRO. How prior authorization harms cancer care: Results of a nationwide study, Dec. 24. Published Dec. 4, 2024. Accessed Jan. 9, 2025.
Register Now for 2025 NC Summit on Reducing Overdose

2025 NC Summit on Reducing Overdose
March 18, 2025 - March 20, 2025
Raleigh Convention Center
Reserve Your Seat
March 18-20, 2025 • Raleigh Convention Center, Raleigh, NC
The NCACC’s 2025 Summit on Reducing Overdose brings together local government leaders, subject matter experts, service providers, community partners and people with lived experience working in crucial areas of the opioid overdose crisis, including in prevention, early intervention, harm reduction, treatment and recovery efforts. This event will provide a space for county commissioners and staff and their community partners to participate in and learn from experts and each other over a two-and-a-half day conference in Wake County.
Schedule
- Tuesday, March 18, 2025, from 1-5 p.m.
- Reception/Community Service Activity from 5-7 p.m.
- Wednesday, March 19, 2025, from 8 a.m. – 5 p.m.
- Reception/Evening Program from 5-8 p.m.
- Thursday, March 20, 2025, from 8 a.m. – 3 p.m.
Hotel and Travel Information
The Summit will take place at the Raleigh Convention Center. The nearby hotel options for self-booking are listed here.
Information on how to get to the Summit location in Raleigh, NC is listed below:
- Planes: Raleigh-Durham Airport (RDU) is the closest airport. RDU is an 18-minute drive to and from the Raleigh Convention Center.
- Trains: Raleigh Union Station (RGH) serves as a stop for the Carolinian and Piedmont Amtrak trains. RGH is about a 12-minute walk to and from the Raleigh Convention Center.
- Automobiles: To find driving directions, enter in the Raleigh Convention Center address: 500 South Salisbury Street, Raleigh, NC 27601. Parking is available at the Raleigh Convention Center.
Registration Deadline
Deadline to register for the Summit is Tuesday, March 11, 2025, by 11:59 p.m.
Payment and Cancellations
Payment by credit card (Visa or Mastercard) is required at the time of registration. If an alternate payment method is needed, please email [email protected]. Please note, there will be a $40 administrative fee for any cancellations. Any cancellations made after March 11, 2025, will not be refunded.
All attendees and participants in NCACC meetings and events are required to abide by NCACC’s Event Code of Conduct.
Note: If you have any questions about this event registration, please email [email protected].
NCDHHS Offers Tips and Vaccine Recommendations for Providers Caring for Pregnant Persons

Every Mother, Every Baby, Every Time Tip Sheet
NCDHHS / Division of Public Health has produced an infographic “Every Mother, Every Baby, Every Time,” which presents conversation tips and vaccine recommendations for providers caring for pregnant persons. Immunizations can help protect women and their babies against diseases including flu, COVID-19, RSV, and pertussis. Making strong vaccine recommendations, especially during respiratory season and while the state is experiencing an increase in pertussis cases, is an important way providers can help prevent disease.
Cases of pertussis have been on the rise nationally and in 2024 the North Carolina Department of Health and Human Services (NC DHHS) is reporting one of the highest counts of pertussis cases in decades. As of January 6, 2025, state public health officials had recorded 784 cases, including 73 cases in infants. Cases are slightly more concentrated in the western region, but cases have been reported across the state, including 18 reported outbreaks.
Infants have the highest incidence rates in North Carolina and are at greatest risk of hospitalizations and death from pertussis. Approximately half (51%) of all cases have occurred in individuals that were up to date with their age-appropriate pertussis-containing vaccine. More than half (56%) of cases in infants occurred in infants with no record of a maternal Tdap vaccine.
If your office is interested in accessing the North Carolina Immunization Registry to view and record vaccine administrations, please contact the North Carolina Immunization Program’s Help Desk at 1-877-873-6247.
Do New CMS Rules on Prior Auth Go Far Enough? Some Physicians Say No!

Do the new CMS rules on prior authorization go far enough?
— No, say some physicians and advocacy groups.
(MedPage Today, Joyce Frieden, Washington Editor) -- The new CMS regulations on prior authorization have been heralded as a big step forward in reducing administrative burdens on physicians, but some people think it doesn't go far enough.
The CMS regulations, which were issued last January, require federally regulated health plans to "improve the electronic exchange of health information and prior authorization processes for medical items and services," according to a CMS press release. For example, starting next year, affected plans must send prior authorization decisions within 72 hours for urgent requests and 7 calendar days for non-urgent requests. The rule also requires all impacted payers to include a specific reason for denying a prior authorization request, and payers must publicly report prior authorization metrics.
But Alex Shteynshlyuger, MD, a New York City urologist, noted in a phone interview that the regulation is limited to Medicare Advantage (MA) plans, Medicaid HMOs, and some plans on the Affordable Care Act's insurance exchanges, though it also includes plans in the Children's Health Insurance Program. In addition, the prior authorization requirements only apply to requests from physicians who are in the MA plan's network, he said.
That excludes providers like him, who aren't in an MA plan but do accept traditional Medicare and also provide care to MA enrollees who have out-of-network benefits. "They are receiving claims from me; they're receiving medical records from me. I've already been verified by Medicare, right?" said Shteynshlyuger, who brought up some of his concerns at the interim meeting of the American Medical Association (AMA) last November. "[But] CMS comes in and says, 'These providers are not vetted enough,' even though we are sending claims to [Medicare] for the same patients and receiving payments from them ... This is irrational logic by CMS to try to create impediments for physicians who do not want to sign unfair contracts from insurance companies."
Shteynshlyuger also is unhappy that CMS is instituting "enforcement discretion" -- meaning that the agency generally won't be enforcing the rule -- for a provision of the Health Insurance Portability and Accountability Act of 1996 (HIPAA), known as X12, that requires health plans to implement electronic transactions for prior authorization. "The enforcement discretion as issued is overly broad, lacks any rational basis, and lacks reasonable justification," he wrote in a December 29 letter to the agency. "The decision to issue a broad discretion is arbitrary and capricious. CMS lacks legal authority to issue such regulatory guidance and lacks authority to suspend enforcement without going through the [Administrative Procedures Act] required notice and comment period." Shteynshlyuger said he has not yet heard back from CMS about his letter.
Asked about some of Shteynshlyuger's concerns, a CMS spokesperson said in an email that it is not enforcing the HIPAA rule as long as the affected plans instead use a standard programming interface that allows for electronic prior authorizations. "Covered entities may separately continue to make an X12 prior authorization process available to providers," the spokesperson said, adding that "HHS will continue to evaluate the HIPAA prior authorization transaction standards for future rulemaking."
In addition, the spokesperson said, "To encourage providers to adopt electronic prior authorization processes, this final rule also adds a new measure for Merit-based Incentive Payment System (MIPS)-eligible clinicians," as well as hospitals, related to using electronic prior authorizations.
The AMA agrees that prior authorization is still a big problem, AMA President Bruce Scott, MD, said in a phone interview that was conducted with a press person present. "I think there's a growing awareness across health systems that [prior authorization] is overused, unjustified, and needs to be right-sized," he said. "Patients are becoming increasingly aware of this overused blunt cost-control process by insurance companies. As a result, there is anger that's building and frustration among physicians that has grown as well."
The "partial fix" that CMS issued last January "didn't go far enough," Scott said. And he is concerned that even the CMS regulations will have limited effectiveness because of the Supreme Court's Chevron decision, issued last July, which overturned a 1984 ruling saying that whenever a dispute emerges over regulating an ambiguous law, judges should defer to the interpretation of federal agencies, assuming those interpretations are reasonable.
In the wake of the Chevron ruling, the AMA is anxious to see the prior authorization regulations be codified by Congress so they aren't in danger of being challenged. The association therefore is supporting the Improving Seniors' Timely Access to Care Act, which would cement the CMS regulations into law. That bill, which had bipartisan support in the House and Senate, appeared to be on the brink of passage, but was ultimately left out of the budget deal that Congress passed at the end of last year.
"The frustration was that this was a bipartisan, bicameral bill that was in the [budget deal] that would have fixed [prior authorization] in many ways, and instead, it gets cut," Scott said. "We're not pushing for something radical here. We're saying we need to right-size this. We're pushing for transparency, we're pushing for efficiency and for communications that are electronically linked so we don't have to use fax machines."
Shteynshlyuger, who is an AMA member, said he is not a fan of the bill because it lacks an enforcement mechanism. "The original bill had enforcement requirements," but those were removed in order to bring the cost of the bill down and thus increase its chances of passage, he said. "Unfortunately, organized medicine has been either misled as to what the bill says, or is complicit. I requested that the AMA withdraw their support for this bill in Congress."
Instead, the House and Senate "should issue comprehensive rules or prior authorizations that apply to every health plan," including employer-sponsored plans, he said. "We cannot live another day under the disastrous systems we have today." Currently, the Labor Department is looking at whether to regulate prior authorization in employer-sponsored health insurance plans; the AMA testified about the issue at a September 2024 meeting of the department's Employee Retirement Income Security Act Advisory Council.
Another complaint about the CMS rules is that they don't apply to pharmacy services, or to prior authorization for drugs administered inside physician offices. CMS said it is developing a proposed rule to streamline prior authorization for drugs covered under federally regulated plans, and that it plans to issue the proposed rule in March.