Registration is a Breeze at 2024 LEAD Conference in Greensboro
Day one of the 2024 LEAD Conference kicked off with Kelly Wilson and Beth Remhoff manning the registration booth. Once registered, attendees proceeded to the Practice Solutions Hall after seeing the NCMS History Hall.
NCMS LEAD Exhibitors Make 2024 Event Amazing Time for Attendees
This is a selection of some of the vendors at 2024 LEAD Conference! Thanks to all of the people who helped make this an amazing event!
$200 Million in FEMA Grants Approved in North Carolina
 Image credit: Santiago Ochoa/WFDD
Image credit: Santiago Ochoa/WFDD
A month after Helene ravaged much of western North Carolina, teams from the Federal Emergency Management Agency are still going door to door and connecting impacted residents to emergency financial aid.
In Watauga, Ashe and Avery counties, FEMA has approved just over $19 million worth of disaster grants for a total of 12,480 households.
According to Shirley Tracey, a FEMA spokesperson, over $200 million has been distributed to 121,000 households across all affected areas in North Carolina.
Though what aid from FEMA looks like will change as the months pass, Tracey added that the agency’s disaster assistance workers will continue signing residents up for disaster grants.
"Putting the money in people’s pockets is really a major step forward in the recovery process," Tracey said. "It’s one step, it’s not the entire thing, but it is certainly a major step to jumpstart the recovery for homeowners and for renters."
Tracey said as the first month post-Helene comes to a close, the federal agency is working to move the 3,700 families placed in short-term rentals and hotels into a more stable living situation.
Those affected can also visit disasterassistance.gov, download the FEMA app, call 1-800-621-FEMA or visit one of their county's FEMA disaster recovery centers to apply for federal assistance. [source]
Happy Birthday to Our Members Celebrating This Month!
Grab your party hats and noisemakers and let’s celebrate!
Moses Y. Aboagye-Kumi, MD
Jeffrey E. Abrams, MD
Richard W. Adams, MD
Puneet Agarwal, MD
Masoud Ahdieh, MD
Diana M. Alexandru, DO
Elizabeth Allen, MD
Joanne B. Allen, MD
Carrie D. Alspaugh, MD
Frank V. Aluisio, MD
Elaina G. Alzaibak
Paul N. Andrews, MD
Robert A. Appert, MD
Aman Arora, MD
John H. Arrington, III, MD
Caudrean L. Avery-Benjamin, MD
Gillian A. Aylward, MD
Saiyyed O. Aziem, DO
Mirela Bacevac, MD
Aaron H. Baer, MD
Marty A. Baker, MD
Scott M. Baker, MD
Eulalia C. Barajas-Graham, PA
Daniel H. Barco, MD
Spencer K. Barrett, MD
Thomas D. Batchelor, Jr., PA-C
Daren M. Beam, MD
Mark E. Beamer, MD
Thomas L. Beardsley, MD
Jeremy M. Belch, MD, MPH
William T. Benesky, Jr., PA-C
Sanford P. Benjamin, MD
Thomas N. Bernard, III, MD
Duncan E. Berry, MD
Bruce H. Berryhill, MD
Charles S. Betts, MD
Raymond J. Biersbach, MD
Kyle S. Bingham, MD
Courtney R. Bitzer, PA-C
James N. Blackerby, MD
Joseph C. Boals, IV, MD, FAAP
Paul V. Bobryshev, MD
Hayley M. Boisseau, PA-C
Lindsay C. Boole, MD
Eduardo Borja Lascurain, MD
Gregory A. Bortoff, MD
Katay C. Bouttamy, DO
Cynthia Bowers-Lee, MD, FACEP
Michael H. Bowman, PhD, MD, FAAN
Robert E. Boykin, MD
H. Ezell Branham, Jr., MD
Eric T. Breiter, MD
Michael W. Brennan, MD
William Z. Bridges, Jr., MD
Clyde L. Brooks, Jr., MD
Paul E. Brown, MD
Rhett L. Brown, MD
Robert L. Brownlow, Jr., MD
Nicole Buddenbaum
Leamor D. Buenaseda, MD
Nigel A. Buist, MD
Larry T. Burch, MD
Rachel M. Burch, MD
William J. Burchfield, MD
Jordan M. Burner, MD
Richard R. Burris, Jr., MD
Mark A. Burt, MD
Harry G. Burton, III, MD
Shannon J. Bybee-Driscoll, MD
Vernon D. Byrd, MD
Kyle L. Cabbell, MD
Milagros P. Cailing, MD
David S. Caldwell, MD
Harold H. Cameron, MD
Angelo C. Cammarata, MD
Elizabeth A. Campbell, MD
Woodward Cannon, MD
Manuel E. Cantillo, DO
Christa J. Canto, PA-C
Marc A. Caragea, DO
L. Keely Carlisle, MD
Sally L. Carpenter, MD
P. Sean Carroll, PA-C
Robert W. Carter, MD
Robin L. Casey, MD
Amy L. Cassidy, MD
Francisco A. Castillos, III, MD
John Catanzaro, MD
Amanda N. Centner, PA-C
Serena M. Chacko, MD
Christina M. Chaconas, MD
Kenneth H. Chambers, MD
Malini Fonseka Chandra Serharan, MD
Kirk L. Charles, MD, FACS
Sameer N. Chawla, MD
James X. Chen, MD
Cherry Chevy, MD
John Cho, MD
Bradley T. Christoph, DO
William M. Clark, MD
George H. Clarke, MD
Charles H. Classen, Jr., MD
Kevin E. Coates, MD
Linda I. Collazo-Batista, MD
Nicole A. Collins, MD
Joseph L. Colosimo, II, MD
Joseph C. Contento, MD
Grayson D. Coon, MD
Ryan J. Cooper, MD
Rick J. Cornella, MD
Carey G. Cottle, Jr., MD
John C. Council, Jr., MD
China G. Cox, MD
Matthew Crabtree, DO
Nathan K. Craig, DO
Jack L. Crain, MD
John L. Crawford, III, MD
Maria E. Crespo, DO
Elizabeth D. Cressy, MD
Michael Creta, DO
Thomas D. Crowder, MD
Asantewaa B. Crumpler, MD
Julian C. Culton, MD
Andrew B. Cutler, MD
Tabitha L. Dabkowski, PA-C
Raj M. Dalsania, MD
Sembua S. Danieli, MD
Michael Dasso, MD
Nailesh D. Dave, MD
Gregory B. Davis, MD
William H. Davis, PA
J. C. B. Dean, MD
Arturo D. DeLeon, MD
Kiersten S. Derby, MD, MPH, FAAP
Benjamin W. Deschner, MD
Shirish D. Devasthali, MD
Robert G. Deyton, Jr., MD
Jennifer R. DiStefano, PA-C, MPAS
George H. Dornblazer, MD
Jamie Doster McIntyre, MD
Kevin G. Dover, MD
Amelia F. Drake, MD
Melinda J. DuBose, MD
Charles H. Duckett, MD
Gary P. Dupuy, MD
William F. Durland, Jr., MD
Kimberly R. Edwards, MD, MS, FAAD
Patrick S. Edwards, MD
Kurt J. Ehlert, MD
Returi P. R. Elkins-Williams, MD
Jessica D. Ely, PA-C
Daniel M. Entwistle, MD, FAAP
J. McDonald Ernest, III, MD
Sarah M. Escott, MD
Tracy L. Eskra, MD, MBA
Frank W. Farrell, Jr., MD
Cecil M. Farrington, Jr., MD
Alan B. Fein, MD
Todd A. Feltz, PA-C
Andrea S. Fernandez, MD
Carol A. Filomena, MD
Terence J. Fleming, MD
Jonathan Flescher, MD
Elizabeth N. Fojtik, MD
Maggie E. Foster, PA-C
William W. Foster, MD
JacQuetta M. Foushee, MD
Chelsea E. Fowler, DO
Amy W. Fox, MD
Sabina P. Francis, MD
Robert W. Fraser, III, MD
M. Gena Frederick, MD
Natalee S. French, MD, FAAP
Robert C. Frere, MD, FAAN
John R. Fry, MD
Glenn E. Fusonie, MD
Kathleen A. Gallagher, MD
T. Ryan Gallaher, MD
Jagadeesh R. Ganji, MD, FACC
Erika G. Gantt, MD
Jerome B. Gardner, MD
Richard Gellar, MD
Donald D. Getz, MD
David B. Gilbert, MD
Kathryn F. Glenn, MD
Joseph L. Godfrey, MD
Michael J. Goebel, MD
Ugo Goetzl, MD, FAAN
Phillip J. Goldstein, MD
Stephen C. Gooding, MD
Kathleen G. Gordon, MD
Ronald G. Gore, MD
Ernesto J. F. Graham, MD
Christopher C. Gratian, MD
Frank R. Graybeal, Jr., MD, FACR
Shayne Greenberg, MD, MSc
Nicole G. Greyshock, MD
Ormond D. Grice, MD
Ericka C. Griffin, MD
Raymond R. Groller, MD
Marc P. Guerra, MD
Mark A. Guirguis, DO
Gregory G. Gunsten, MD, FAAP
Gool K. Gupta, MD
Nitin Gupta, MD
pankaj gupta, MD, FACS
Sachin K. Gupta, MD
Andrew K. Gustavson, PA-C
Gary A. Haakenson, MD
Nizar Habal, MD, FACS
Zeina A. Haddad, MD
James B. Hall, MD, FACOG, FACS
Alfred W. Hamer, Jr., MD
William F. Hancock, Jr., MD
L. Robert Hanrahan, Jr., MD
Hunter A. Hardaway, PA-C
Joshua L. Hardison, MD
R. Paul Harris, MD
Frank N. H. Harrison, Jr., MD
William F. Harriss, MD
Charul G. Haugan, MD
Richard I. Hayes, MD
Andrew T. Healy, MD
Jeffrey J. Henefeld, PA
Alyssa K. Henson, DO
Sherry J. Hinson, PA-C
Charles R. Hoidal, MD
Derrick J. Hoover, MD
George C. Hughes, IV, MD
Julia T. Hughes, MD
Jordan C. Humphrey, MD
Karen C. Hunt, MD
Zehra Husain-Syed, MD
Georgina D. D. Ishak, PA-C
Travis H. Jackson, MD
Selina L. James, MD
Peter J. Jarosak, MD
Claudius D. B. Jarrett, MD
Brian L. Jerby, MD, FACS, FASCRS
James E. Jewell, MD
Soma S. Johnkutty, MD
Robert B. Johnson, MD
Jennifer Johnson Holley, PA-C
David S. Jones, MD
Mary M. Jones, MD
Perry E. Jones, MD
Jennifer F. Jordan, MD
Tom Jose, MD
Jugta Kahai, MD, FAAP
Neelima Kamineni, MD
David J. Kammer, MD
Gordon C. Kammire, MD
Kelly D. Kamp, MD
Matthew G. Kanaan, DO, MS
Akanksha S. Kashyap, MD
Nicolas-George Katsantonis, MD
Jeffrey A. Katz, PA-C
Marc S. Katz, PA-C
Mark A. Katz, MD
Justin R. Kauk, MD
Amarpreet Kaur, MD
Rebecca E. Keiffer, MD
Brendan P. Kelley, MD
Michael J. Kelley, MD
Andrea M. Kelly, PA-C
Susan L. Kennedy, MD
Jean B. F. Kenny, MD
Kevin J. Kerlin, MD
Kendra E. Kesty, MD
Shaukat A. Khan, MD
Pamina S. Kim, MD
George D. Kimberly, MD
Houston M. Kimbrough, Jr., MD
Bradley M. King, MD
Michael B. King, MD, FACC
Stephen C. King, MD
Michael B. Kodroff, MD
Daniel N. Koehler, DO
David J. Koenig, MD
Phillip M. Kostelic, MD
Sage P. Kramer, MD
Johanna E. Kreafle, MD
George H. Krebs, Jr., MD
Brian A. Krenzel, MD
Steven P. Kubicki, MD
Satish K. Kumar, MD
James E. Kurz, MD
Michael A. Lach, DO
David C. Lachman, MD
Andrew P. Lange, MD
Adam D. Langenbrunner, MD
Jocelyn E. LaRocque, DO
Richard E. Lassiter, MD
Aimee M. Lawson, PA-C
Alicia H. Lazeski, MD
Yeonhee Lee, MD
Catherine C. Legrande, PA-C
Laurie LeMauviel, DO
Michael R. Leone, MD
Robert H. Lester, MD
David D. Lewis, MD
Heather K. Lewis, MD
Zachary A. Lindsey, MD
David Ling, MD
A. Stanley Link, Jr., MD
Daniel J. Linn, MD
W. A. Litzenberger, MD
Joseph T. Liverman, MD
David F. Locascio, MD
Choomsang Lohavichan, MD
Verachai Lohavichan, MD
Marchi V. Lopez-Linus, MD
Michael R. Love, PA-C
Jonathan C. Lowry, MD
Joy S. Lowry, MD, FAAP
Miha S. Lucas, MD
Alvin J. Lue, MD
Evelyn M. Lyles, MD
Jennifer M. Mabry, MD
Scott A. MacDiarmid, MD
Christopher R. Madden, MD
Christian E. Magura, MD
Rafat Mahmood, MD
Shailesh S. Male, MD
Anna M. Malysz Oyola, DO
Stanley R. Mandel, MD
P. Prasad Manne, MD
Christopher R. Mantyh, MD
Howard F. Marks, Jr., MD
David A. Martin, Jr., MD
Jeffrey B. Martin, PA-C
Habib A. Masood, MD, FACP
Christopher W. Mattern, MD
Mark A. Mattioli, MD
Gary E. Mauldin, MD
John E. McAuliffe, MD
Ryan N. McCarter, MD
Hannah M. McCloskey, MD
Patrick J. McConville, MD
Bobby K. McCullen, Jr., MD
Stacey L. McDonald, PA-C
Christopher M. McDowell, DO
Steven J. McEldowney, MD
William F. McGuirt, Sr., MD
Adam B. McKenzie, DO
Warren W. McMurry, MD, FACS
D. Clinton McNabb, MD
Jesse N. McNiel, MD
John F. Mearns, DO
Lloyd C. Meeks, MD
Gwenesta B. Melton, MD
Michele L. Mercer, MD
Eric M. Meredith, MD
Richard H. Merrill, MD
James M. Mertesdorf, MD
David R. Messerly, MD
Margaret C. Metts, MD
David D. Meyer, MD, MBA
William F. Milam, MD
Carolyn A. Miller, MD
Jacqueline H. Mims, MD
Stanley G. Minor, MD
Gregory C. Mitro, MD
Robert L. Mittl, Jr., MD
Simone P. Montoya, MD
Brittany A. Moore, PA-C
Stephen I. Moore, III, MD
Ana V. Morais, MD
Elizabeth B. Moran, MD
Mark W. Morgan, MD
Stephanie E. Morgan, MD
Kenny J. Morris, MD
Peter J. Morris, MD, MPH
Crystal D. Mosteller Hopson, PA-C
George W. Mozingo, III, MD
Clarisse S. Muenyi, MD
Amit M. Mukhia, MD
Brian E. Munro, MD
Christina E. Murray, MD
Evelyn E. Murray, DO
Gina M. Murray, MD
Ryan P. Murray, MD
Thomas P. Mutton, MD
Susan G. Myers, MD
Menaka M. Nadar, MD
C. Hughes Napper, MD
Richard Natale, II, MD
Lee Ann Naylor, MD
J. Thomas Newton, MD
Brett C. Niblack, MD
William P. Nixon, Jr., MD
H. B. Noah, MD
Andrew M. Norris, MD
H. T. Norris, MD
Joseph A. Noto, MD
Joseph F. Nutz, Jr., MD
Dustin W. O'Keefe, MD
Eric L. Olson, MD
John S. O'Malley, MD
Todd J. Oswald, MD
Adam C. Ottley, MD
Gaylon V. Owens, MD
Sakine Ozyurt, MD
MaryEllen D. Pace, MD
Kristen R. Page, MD
Gaurang Palikh, MD, FAAN
James F. Palombaro, MD
Brittney T. Panella, PA
Clarito M. Pang, MD
Anup H. Parikh, MD
Ashesh S. Parikh, MD
Seth T. Parker, MD
Walter T. Parkerson, MD
James A. Pascale, MD
George W. Paschal, III, MD
Mary L. Passannante, PA-C
Ashish B. Patel, MD
Hetal P. Patel, MD
Jitendra K. Patel, MD
Kalpesh G. Patel, MD
Ashwin A. Patkar, MD
H. Clifton Patterson, MD
Jaime Pedraza, MD
William B. Pemberton, MD
Sarah Peters, MD
Eric W. Peterson, MD
Amanda J. Pettibone-Pond, MD
Rebecca E. Pettigrew, PA-C
John K. Petty, MD
Christina R. Peyton, MD
Marc A. Pilato, MD
Maria D. Pincus, MD, FAAP
Jesse C. Pittard, MD
Sean Ploof, MD
Nicholas G. Plundo, DO
Tereza Poghosyan, MD
Jeffrey M. Potter, MD
Alexandra N. Powell, MD
Stephen H. Powell, MD
Donna L. Prather, MD
Ian S. Pratt, MD
Crystal M. Pressley, MD
Thomas B. Price, MD
Kelly A. Pring, MD
Raeford T. Pugh, MD
Evan M. Pushchak, MD
Shelby K. Pushchak, MD
Misbah U. Qadir, MD, FACP
Richard D. Ramos, MD
Maria Rana, DO
Cecil H. Rand, Jr., MD
Melissa H. Ratliff, MD
Carl E. Ravin, MD
Bradley H. Reddick, MD
Keshavpal G. Reddy, MD
Kevin J. Reese, MD
Mary Ann Reeves, MD
David E. Rentz, MD, MPH
Gregory B. Reynolds, MD
John O. Reynolds, Jr., MD
Audrey C. Rhee, MD
Brian B. Rhodes, MD
Alfred L. Rhyne, III, MD
Lindsey N. Rice, PA-C
James C. Riley, MD
David A. Rinehart, MD
Ahren C. F. Rittershaus, MD
Jessica N. Rittler, PA-C
John D. Roberson II, MD
Benjamin S. Robey, MD
William L. Robinson, MD
Danielle B. Rocchio, MD
J. Gardiner R. Roddey, MD
John T. Roper, MD
Daniel T. Rose, MD
Vincent J. Rossi, MD, MBA
Todd J. Roth, MD
Jonathan S. Rubens, MD, FACEP
Roger B. Russell, MD
Sean C. Russell, PA-C
Lori D. Russell-Smith, MD
Edmund J. Rutherford, MD
Robert K. Sackmann, MD
Joseph J. Salfity, MD
Carolyn M. Sampson, MD
Gurinder P. S. Sandhu, MD
Devdutta G. Sangvai, MD, MBA, FAAFP
Joshua W. Sawyer, MD
Drew D. Schnyder, MD
Nicholas R. Schoenbachler, MD
Jared N. Schwartz, MD, PhD
Kevin S. Scully, MD
Stephen R. Seal, MD
Jennifer L. Seddon, MD
Jay C. Sellers, MD
Karen Sennewald, MD
Dipen R. Shah, MD
Nimesh B. Shah, MD
Joseph C. Shanahan, MD, FACR
Nael Shanti, MD
Mark T. Shapiro, MD, FAAO
Arsha Sharma
Melissa J. Shelton, PA-C
Ajay Shreenath, MD
Tracy A. Shuford, PA-C
Leslie Sierra-Renten, MD
W. Reginald Sigmon, Jr., MD
Manmohan Singh, MD
Brian A. Singleton, MD
B. Todd Smith, MD
Danielle E. Smith, DO
Scott L. Smith, MD
Vynedra A. Smith, MD
Tamas Soos, MD
Jacob B. Sooter, PA-C
Davey B. Stallings, MD
Karrie A. Stansfield, MD, FAAP
Paul B. Starling, MD
Craig H. Steffee, MD
Tiffany Stephens, PA-C
Kristine C. Stevens, PA-C
Jessica K. Stewart, MD
Lori D. Stiegemeier, DO
Taylor H. Stroud, MD
Roy E. Strowd, III, MD
Allston J. Stubbs, Jr., MD
Erin H. Stubbs, MD
Jennifer L. Sumner, MD
David K. Sutton, MD
William R. Sutton, MD
David W. Swayne, MD
Brian J. Swinteck, MD
Darden C. Swords, MD
James J. Szabo, MD
Kayla J. Szolek, DO
Paula E. Szypko, MD
Charles V. Taft, MD
Leonard J. Tananis, Jr., MD
Teerath P. Tanpitukpongse, MD
Velma V. Taormina, MD, FACOG
Wallace C. Tarry, MD
Za'Vette M. Tatum-Kodzai, MD
Joshua Tayloe, MD
Marshall C. Taylor, MD
Melinda Taylor, MD, FAAP
William C. Taylor, MD
Wendy L. Taylor Book, MD
Anand Tewari, MD
Sandya Thimmappa-Cohen, MD
James M. Thomas, MD, FACS
Jessica G. Thomas, PA-C
Emily H. Thompson, MD
Brittain H. Tulbert, MD
Lindsey H. Tyler, MD
Joseph J. Urash, DO, FAOCD
Val Pierre Vallat, MD
Robert A. van der Vaart, MD
Jan A. van Ravesteyn, MD
Elizabeth F. Vandergriff, MD
Harold M. Vandersea, MD
Steven A. Vernali, MD
Maria J. S. Villena, MD
Neil C. Vining, MD
Andrew R. S. Vinson, MD
Emily L. Voynovich Parrella, PA-C
Matthew J. Vreeland, MD
Eugene H. P. Wade, MD
David T. Walker, MD
Cheryl L. Walker-McGill, MD, MBA
James G. Wall, MD
Mark J. Warburton, MD
Scott A. Washburn, MD
Pearlie B. Watkins, III, MD
Bradley A. Watling, MD
Patrick Watterson, PA-C
Paul R. Weaver, DO
LaShawn A. Weaver-Lee, MD
William W. Webb, Jr., MD
Leah M. G. Webster, DO
Spencer G. Weig, MD
Scott M. Wein, MD
Thaddeus C. West, III, MD
Alan S. Wheeler, PA-C
Benjamin J. White, MD
Arthur W. Whitehurst, MD
Lelan F. Whitmire, MD
Joseph G. Wiater, MD
Steven F. Wiegand, MD
Tammie F. Wiley, MD
Stanley A. Wilkins, Jr., MD
Ernest C. Williams, MD
Joseph E. Williamson, MD
Stephen E. Willis, MD
Jonathan W. Winter, MD
S. Bradley Winter, MD
Donald B. Winters, MD, FAAP
Mary L. Wisniewski, MD
Kenneth A. Wolfson, MD
John M. Wooten, MD
Glenn T. Yamagata, MD
Marguerite M. Yao, MD, MPH
Siegfried C. Yeh, MD
Garret P. Young, MD
James R. Young, MD
John E. Yurko, MD
Veronica P. Zachry, MD
MaryShell B. Zaffino, MD
Bradley R. Zagol, MD
Jeffrey S. Zaidman, MD
Leonardo M. Zara, MD
Mark K. Zeller, MD
Andrew J. Zerkle, MD
Jinyu Zhang, MD
Yunxiang Zhu, MD
Michael D. Zimmerman, DO
Taylor J. Zuber, MD
Let's Get Social! Join NCMS November 14th at Rosecomb Beer Garden in Cary.

Relax and build community with NCMS!
Physicians, PAs, Residents & Students
Bring your colleagues, family, and friends!
Drinks and snacks will be provided!
November 14
6:00 pm-8:00 pm
Rosecomb Beer Garden, Cary
1143 Parkside Main St.
Cary, NC 27519

REGISTER NOW!
If you cannot register at the above link, or need more information, please contact Toni Hill, [email protected].
Pneumococcal Vaccine Recommended for People 50 and Older

U.S. health officials recommended that people 50 and older get a shot against bacteria that can cause pneumonia and other dangerous illnesses.
The recommendation was made by a scientific advisory panel and then accepted by the Centers for Disease Control and Prevention. The decision lowered — from 65 — the minimum recommended age for older adults to get the shot.
“Now is a great time to get vaccinated against pneumococcal disease in preparation for the winter respiratory season,” CDC Director Dr. Mandy Cohen said in a statement Wednesday night.
The advisory committee voted 14-1 to make the change during a meeting earlier in the day in Atlanta. The guidance is widely heeded by doctors and prompts health insurers to pay for recommended shots.
Pneumococcal shot recommendations are sometimes called the most complicated vaccination guidance that the government issues. The CDC currently recommends shots for children younger than 5 and adults 65 or older, as long as they have never been vaccinated against pneumococcal disease. Officials also recommend the shots for children and adults at increased risk for pneumococcal disease, such as those with diabetes, chronic liver disease or a weakened immune system.
Lean more about the recommendations here.
NCMS Recognizes NCMS Disaster Relief Fund Contributors

A heartfelt THANK YOU to these individuals and organizations for their contribution to the NCMS Disaster Relief Fund. Your generous donation is far more than just a financial contribution; it’s a lifeline for the many affected by Hurricane Helene, and vital in providing support to healthcare professionals and communities impacted by this disaster.
We invite you to spread the word about the NCMS Disaster Relief Fund and stay engaged with us as we work together to help restore our Western North Carolina neighbors.
We are grateful to have you in our community!
- Amar M. Amaresh, MD
- Edwin C. Bartlett, Sr., MD
- Deanna M. Boyette, MD
- Edwin K. Burkett, MD
- Cobb County (GA) Medical Society
- John A. Fagg, MD
- Barbara Hodde
- Martha G. Peck, MD
- Gary Price, MD
- Eugene E. Wright, Jr., MD
- Kathy F. Wright
- Curi
- Anonymous
- Christopher T. Grubb, MD
- Lyndon K. Jordan, III, MD, FACR
- Katie Lowry, MD, MPH
- Laura J. Luckadoo, MD
- Robeson Pediatrics
- Kirby Sheridan
- Catherine L. Sotir, MD
- Vinod C. Vallabh, MD
- Ian D. Archibald, MD
- Preecha Bhotiwihok, MD, MPH
- John W. Black, MD
- Anonymous
- Gay M. Bowman
- Georgi N. Brockway, MD
- Michael T. Brohawn
- Anonymous
- Carolina Complete Health Network
- Sharon M. Foster, MD, FAAP
- Donna C. Graves, MD
- M. Mark Hester, MD
- Suneya G. Hogarty, DO
- Marius J. Ilario, MD
- Linda W. Lawrence, MD
- Douglas S. McFarlane, MD
- Mark B. Moeller, MD
- Anonymous
- Raleigh Orthopaedic Clinic, PA
- Timothy J. Reeder, MD, MPH, FACEP
- Alan J. Rosenbaum, MD
- Anonymous
- Marshall Z. Schwartz, MD
- Douglas D. Sheets, MD, FACOG
- W. Alan Skipper, CAE
- Jennifer K. Stoddard, MD
- STUSQU, PLLC
- Lisa W. H. Thompson, MD
- Cheryl L. Walker-McGill, MD, MBA
- Craig E. Webb, MHS, PA-C
- Johnathan D. Williams, MD
- Anonymous
- Idil Aktan, MD
- R. D. Almkuist, II, MD
- American Board of Pediatrics Inc
- Caroline D. Ames, MD, FACS
- James H. Antoszyk, MD
- Joy Avery
- Timothy M. Beittel, MD
- Anonymous
- Anonymous
- Cedar Mount Behavioral Health, PA
- Center For Pain Management, PLLC
- Melissa M. Coale, MD
- Anonymous
- Kim D. Dansie, MD
- Jackie M. Davis-Jones
- Jessica F. Doerrler, PA
- Patricia Duncan
- Peter A. Eweje, MD
- Mark W. Featherston, MD
- Anonymous
- Joanne M. Fruth, MD
- Lisa M. Gangarosa, MD
- Highland Medical Associates
- Anonymous
- Joseph P. Hunstad, MD, FACS
- Kitsie Jones
- Christopher P. Jordan, MD
- Kerry Kendall
- Eugenie M. Komives, MD, FAAFP
- Ted R. Kunstling, MD, FCCP
- Andrew S. Lamb, MD
- Keith LaScalea, MD
- Anonymous
- Elizabeth G. Livingston, MD
- Anonymous
- Laura L. Martinez, MD
- Darlyne Menscer, MD
- Ashley Newton
- J. Thomas Newton, MD
- Carolyn O'Conor, MD
- Michael K. Patrick, MD
- Patricia Petrick, MD
- Emily Rayes-Prince, MD
- Anonymous
- Corianne D. Rogers, MD
- Nimesh B. Shah, MD
- Kristen M. Shipherd
- Maria J. Small, MD
- Anonymous
- Michol Stanzione, DO
- Steele Creek Dermatology
- Al Steren, MD and Diane Snyder Steren, MD
- Martha Strange, MD
- Thomas M. Swantkowski, MD, AGAF, FACG
- Marian L. Swinker, MD, MPH
- Christopher L. Tebbit, MD
- Monecia Thomas, PhD
- Dimitri G. Trembath, MD
- Michael J. Utecht, MD, FACEP
- Lynnea Villanova, MD
- Bonnie E. Wagner, PA-C
- Rebecca Y. Weinshilboum, DO
- Carl J. Westcott, MD
- Thomas R. White, MD
- Anonymous
- Women's HealthCare Consultant PC
- Nagarjuna Yerra, MD
- Michael Bartiss, MD / Family Eye Care of the Carolinas
- David Boone, MD
- Carolina Complete Health
- Karl Chiang, MD
- John Chretien, MD
- Anonymous
- Kelly Fedoriw, MD
- Carolyn Ferree, MD
- Alison Gardner, MD
- John Goldfield, MHS, PA-C
- Akilah Grimes, MD
- Sandra Jackson / Eastern Pediatrics
- Matthew Katz, MS / MCK Health Strategies
- Melissa Kenny
- Donna McGee, MD
- Larry Napolitano, Jr., MD
- Michael P. Reddy-Miller, MD
- Anonymous
- Andrew Pasternak, MD
- Antonio Ramirez, MD
- Beth Remhof
- Jennifer Root, MD
- Richard Savage, MD
- Anonymous
- Soma Sengupta, MD
- Nimesh Shah / Noble Hospitality Investment
- Amanda Trimpey, MD, MPH, FACOEM
- Yunxiang Zhu, MD
*Please note: List reflects donations received through Tuesday, October 22.
Reminder: Disaster Relief Applications for Health Care Professionals Not Currently Enrolled as an NC Medicaid Provider

The NC Department of Health and Human Services is committed to ensuring continued access to care for NC Medicaid beneficiaries, as well as reimbursement to qualified providers for services rendered, in good faith, throughout the period of impacts from Hurricane Helene, retroactively from Sept. 25, 2024, through Dec. 31, 2024, (unless otherwise communicated by DHHS).
- The Centers for Medicare & Medicaid Services (CMS) granted approval effective October 1, 2024, for DHHS to implement a temporary, expedited enrollment process for health care professionals to become an NC Medicaid provider due to a natural disaster. This process is not for providers who regularly see NC Medicaid beneficiaries.
Health care professionals who will be rendering services to NC Medicaid beneficiaries due to Hurricane Helene can complete and submit an application through the NCTracks Provider Portal. Please refer to the disaster provider enrollment job aid Disaster Relief Provider Enrollment Application Job Aid (PRV703) located under Quick Links on the NCTracks Provider Enrollment home page for necessary instructions to complete the temporary disaster provider enrollment application. Be sure to review the job aid before starting to complete the application, as several preliminary steps are necessary.
Providers must indicate the application is for Disaster Relief by answering “Yes” to the Disaster Relief enrollment question on the Online Application page of the application.
Note: This is not for providers who see NC Medicaid beneficiaries on a regular basis.
Please review North Carolina Medicaid Provider Enrollment Disaster Relief and Waiver or Modification of Requirements Under Section 1135 of the Social Security Act from the Secretary of Health and Human Services for additional information.
Information about Governor Cooper’s Declaration of a State of Emergency can be found at Governor Cooper Declares State of Emergency Ahead of Hurricane Helene.
Contact
- NCTracks Call Center: 800-688-6696
- Provider Ombudsman: 866-304-7062
[email protected]
$5 Million Investment Announced to Expand Access to Behavioral Health Care in Primary Care Offices
The North Carolina Department of Health and Human Services announces $5 million to help providers build capacity and implement the Collaborative Care Model in primary care offices across the state. Through the Collaborative Care Model, primary care providers work with an integrated behavioral health case manager and a psychiatric consultant to monitor and treat patients for mild to moderate behavioral health conditions. The need for integrated medical and behavioral health care is greater than ever as rates of anxiety and depression have substantially increased following the COVID-19 pandemic.
"Too many individuals with mental health and substance use disorders delay the care they need because they struggle finding a provider," said NC Health and Human Services Secretary Kody H. Kinsley. "Collaborative Care can serve more people earlier by supporting primary care providers in reaching people at the onset of behavioral health symptoms."
Collaborative Care is covered by NC Medicaid, Medicare and most commercial insurance plans in North Carolina, helping to break down barriers that separate how physical and behavioral health services are delivered and paid for. Patients are able to receive services through a provider, and in a setting, they already know and trust, which gives them easier access to the care they need. Collaborative Care improves patient outcomes, reduces health care costs and reduces stigma related to mental health and substance use disorders.
NCDHHS’ investment is designed to help with the startup costs of implementing Collaborative Care, particularly for primary care providers in rural or high-need areas that have limited access to behavioral health services. The department is partnering with Community Care of North Carolina (CCNC) to select eligible provider applications and distribute funding to approximately 100 providers across the state.
As of Oct. 10, providers can apply for up to $50,000 per site to help with hiring and start-up costs. Primary care practices are encouraged to apply and can find more information through CCNC’s dedicated Collaborative Care website. Efforts will be made to ensure primary care practices in western North Carolina impacted by Hurricane Helene will have an opportunity to apply for inclusion in the program, even if they are unable to apply for funds at this time.
"The need is greater than ever before," said Dr. Carrie Brown, Chief Psychiatrist for NCDHHS. "From 2019 to 2021, the percentage of Americans reporting symptoms of anxiety and depression nearly quadrupled, from 11% to 41%. The Collaborative Care partnership between primary care and psychiatrists is one example of the department’s efforts to increase access to behavioral health care for those who need it as we focus on whole-person health."
Nationally, the Collaborative Care Model is a strategic response to the shortage of mental health care professionals across the country. Recent data show more than 123 million people in the U.S. live in a Federally Designated Mental Health Professional shortage area, including one in four North Carolina counties. In North Carolina, a recent study finds there are 28 counties without a practicing psychiatrist, and it can take weeks or even months to get an appointment with a mental health provider.
With the Collaborative Care Model, a behavioral health care manager is embedded within a primary care office and, through consultation with a psychiatrist, helps the primary care physician implement evidence-based interventions for patients who screen positive for targeted behavioral health conditions. In this model, one psychiatrist can reach far more North Carolinians with mild to moderate behavioral health needs than they could directly provide care for through traditional behavioral health services.
"Through this partnership with primary care professionals, we are working to create a more accessible mental healthcare system," said Kelly Crosbie, MSW, LCSW, Director of the NCDHHS Division of Mental Health, Developmental Disabilities, and Substance Use Services. "This ensures our community receives the mental health care they need and deserve, in a setting where they are most comfortable."
The $5 million investment in capacity building is made possible by the NC General Assembly through the signing bonus North Carolina received from the federal government when it approved Medicaid Expansion. The investment builds on the department’s strategic work to enhance access to the Collaborative Care Model, which has already resulted in a nearly 100% increase in utilization among NC Medicaid primary care providers between April 2023 and May 2024.
NC Medicaid, in coordination with key stakeholders, has led a statewide effort over the past two years to align requirements and reimbursement for Collaborative Care across payors, increase NC Medicaid reimbursement for behavioral health services to 120% of Medicare rates and remove copays for Medicaid beneficiaries. Additionally, NC Medicaid has provided training and technical assistance to support model implementation through Area Health Education Centers, connected interested primary care practices with psychiatric consultants, and created a customized Collaborative Care registry for providers through CCNC. These efforts are outlined in detail in a white paper published by NC Medicaid in December 2023.
NCDHHS’ investment in the Collaborative Care Model is part of a broader commitment to build an integrated behavioral health system in North Carolina. The NC General Assembly last year allocated a historic $835 million to strengthen the behavioral health system, and millions of North Carolinians are already benefiting from the sweeping, systemic improvements these funds are making for their health, well-being and day-to-day lives. More information is available in the NCDHHS Transforming North Carolina’s Behavioral Health System white paper. [source]
Starlink Assistance for Facilities Impacted by Helene

NCDHHS may be in a position to assist practices with securing Starlink and is seeking your input about practices in the Hurricane impacted counties that need Starlink. DHHS will use your information to link Starlink resources with practices.
Please share the following information with Nicole Fields-Pierre, MPA, NCCM, Community Health Program Manager, Office of Rural Health at [email protected]:
- County
- Practice/clinic name
- Specialty
- Address
- Point of contact: name, cell phone number, email addresses
In-Person Early Voting Ends Saturday!

In-Person Early Voting Ends Saturday, November 2nd!
During the early voting period, voters may cast a ballot at any early voting site in their county. This is different than Election Day, when registered voters must vote at their assigned polling place. During the early voting period, eligible individuals may also register to vote and vote at the same time (see Same-Day Registration below).
For an overview of North Carolina’s current elections, visit Upcoming Election.
Early Voting Dates and Sites
- The in-person early voting period for the 2024 general election:
- Began Thursday, October 17, 2024.
- Ends 3 p.m. Saturday, November 2, 2024.
- The general election is on Tuesday, November 5, 2024.
- Find early voting sites and schedules in your county: Early Voting Site Search.
- Locations and voting hours are also available here: Early Voting Sites for the Nov. 5, 2024 General Election (PDF).
Unsure if You Are Registered?
Find out if you are registered to vote by entering your information into the Voter Search.
Don’t Forget Your Photo ID
North Carolina voters will be asked to show photo ID when they check in to vote. Learn more: Voter ID.
Same-Day Registration
When you check in to vote at an early voting site, you may update your name or address within the same county if necessary. Individuals who are not registered to vote in a county may register and immediately vote at that same site. This process is called “same-day registration.” Find more information at Register in Person During Early Voting. Although same-day registration is available for voters during early voting, same-day registration is not available for most voters on Election Day.
Your Sample Ballot
To view sample ballots, registered voters must enter their information into the Voter Search and navigate to “Your Sample Ballot.” Voters can practice making selections with the accessible sample ballot: “Option 4” at the NC Absentee Ballot Portal.
Note: Sample ballots for each election are only available once finalized.
By-Mail Absentee Ballot Drop-Off
Voters who receive an absentee ballot by mail may deliver their ballot to their county board of elections office or to an election official at an early voting site during any time that site is open for voting. Ballots will be kept securely and delivered to the county board of elections for processing.
Voting Equipment
Curious which equipment will be at your voting site? Check the interactive map and table: Early Voting Equipment by County.
Voter Assistance and Curbside Voting
Any voter who qualifies for assistance may ask for help at their polling place under Assistance to voters (N.C.G.S. § 163-166.8). To find more information, visit Help for Voters with Disabilities. Curbside voting is available for eligible individuals. For more information, see Curbside Voting.
After You Vote
You can find out whether your vote counted in the “Your Absentee Ballot” section of the Voter Search database. Under North Carolina law, all early votes — by-mail or in-person — are considered absentee votes. Your ballot status also will show up in the “Voter History” section as soon as your county completes the post-election process of assigning voter history to your record. This may take up to a few weeks after Election Day.
Learn about NCMS member candidates here.
Grant Opportunity: Primary and Preventive Care for Vulnerable, Underserved, and Medically Indigent Patients

These grant funds, supported through the North Carolina General Assembly, are for assuring access to primary and preventive care to meet the health needs of vulnerable, underserved and medically indigent patients, with emphasis on providing primary and preventative medical services to uninsured or medically indigent patients. An important component of this work is to strengthen the safety net through increased levels of collaboration and integration of services to meet and sustain the needs of those served more effectively. When an eligible primary care medical home safety net organization provides integrated care, grant funding may also support dental, pharmacy, maternal, and behavioral health services.
Primary care safety net organizations that currently provide primary and preventive health care for underserved and medically indigent patients in North Carolina are eligible to apply for this funding to pay for patient care through encounter-based reimbursement (Track A) or through reimbursement for eligible expenses (Track B). Telehealth services and equipment are eligible expenses in both tracks. Applicants must select ONE track.
Learn more here.
Retainer Payments for Home and Community-Based Service Providers Impacted by Hurricane Helene
Home and Community-Based Service (HCBS) providers may be eligible to receive retainer payments for employed Direct Care Workers (DCWs) who are unable to deliver HCBS services under an active, approved service plan to one or more Medicaid beneficiaries due the impacts of Hurricane Helene. These retainer payments are for DCWs as defined in 42 C.F.R. § 441.302(k)(1)(ii) and 42 C.F.R. § 441.311(e)(1)(ii) and are intended to help maintain the NC Medicaid provider network.
Eligibility Criteria
To receive retainer payment, qualifying providers and their DCW(s) must comply with terms set out in the attestation along with the following:
- Home and community-based service (HCBS) provider delivering one of the following services:
- 1915 (c) Community Alternatives Program for Children (CAP/C) Waiver
- 1915 (c) Community Alternatives Program for Adults (CAP/DA) Waiver
- 1915 (c) Innovations Waiver
- Specific 1915(i) services
- Community Living and Supports
- Supported Employment
- Individuals Placement and Supports
- Individuals and Transitional Supports
- Home Health
- Personal Care Services (PCS)
- Private Duty Nursing (PDN)
- Provider’s employed DCW(s) is unable to provide services under an active, approved service plan due to the impacts of Hurricane Helene
- Provider’s employed DCW(s) or member receiving HCBS services has a physical address within a FEMA declared disaster individual assistance county
- Retainer payments are limited to hours/services under a service plan approved prior to Sept. 25, 2024
- Retainer payments are limited to no more than one (1) 30-day billing period per DCW and Member that is unable to be served
- Providers must complete and upload the required attestation
Providers must retain the required DCW attestation for each DCW for which a retainer payment is requested.
To receive retainer payments, providers will initially submit an attestation and collect attestations from their DCWs. Once a completed attestation has been submitted, providers may request a retainer payment by submitting claims using the process described below to the Managed Care plan with whom the Member unable to receive services is enrolled or to NCTracks based on eligibility of the Member unable to receive services. The following sections provide additional information on the process.
Continue to full release here.
Baxter Announces Expiration Dating Extensions for Certain Products Related to IV Solutions Disruption

As part of its efforts to mitigate the disruption to the supply of IV solutions after Hurricane Helene temporarily closed its North Cove, N.C., manufacturing plant, Baxter said Monday that it is now authorized by the Food and Drug Administration (FDA) to extend the use date of some products to provide a 24-month expiration from the manufacture date without relabeling the products.
Please see the Baxter document that contains the full list of Baxter product codes, lot/serial numbers, labeled expiration dates, and extended expiration dates. The extended expiration dates apply only to product codes manufactured prior to September 30, 2024.
Read more in the Special Bulletin released from the American Hospital Association here.
Register Now! NCTracks November 2024 Provider Training Schedule
Registration is now open for the NCTracks November 2024 training courses.
The courses are virtual, via Zoom, and can be attended remotely from any location.
Courses offered this month include:
- New Office Administrator
- Submitting a Time Limit Override
- Submitting a Dental/Ortho Claim
- ES User Role_Abbreviated MCRs_Upload Documents
- Submitting a Professional Claim
- Prior Approval Institutional
Click here for more information on course schedule and access to zoom links.
Register Now! Exploring Recent Data: Pfizer Medical Affairs Updates on COVID-19 from ACIP and More
Exploring Recent Data: Pfizer Medical Affairs Updates on COVID-19 from ACIP and More
Thursday, 14 November 2024: 12:00 pm – 12:30 pm ET
Speaker:
Rajeev M. Nepal
US Medical Director, Pfizer mRNA Vaccines, Medical and Scientific Affairs
The Pfizer Vaccines US Medical Affairs Team invites you to attend an educational webinar series titled Translating mRNA which is focused on providing education on COVID-19 and vaccination.
The webinar series is designed to communicate scientific information which may include recent study results to inform healthcare providers regarding Pfizer and BioNTech's COVID-19 vaccines.
The webinar series will include a live question-and-answer session with Pfizer medical experts.
Intended Audience: US healthcare professionals including but not limited to physicians, nurse practitioners, pharmacists, and physician assistants.
CDC: Walking Pneumonia Surging Among Kids

Children who have coughs that go on for weeks may have a type of walking pneumonia that’s been surging in the US this year, and they may need a different antibiotic regimen to treat it, infectious disease experts say.
“It’s very much been on our radar since early summer, when we started to see a remarkable increase in the number of kids with pneumonia who seemed to have this particular type of pneumonia,” said Dr. Buddy Creech, a pediatric infectious disease specialist at Vanderbilt University Medical Center.
Creech says that on the same day in August, four Nashville-area pediatricians reached out to him to ask why so many kids were coughing in the summertime. These doctors wanted advice, he says, because their go-to antibiotic for pneumonia – amoxicillin – didn’t seem to be working in these cases.
Continue reading this story here.
🎉It's New Member Monday!🎉

Join us in welcoming these new members to the North Carolina Medical Society!
- Tanya E. Anim, MD
- Ilya Boykov
- Taylor S. Corum, PA-C
- Callie R. Faust, PA
- Robyn Guo
- Hunter A. Hardaway, PA-C
- Rama K. Kethineni, MD
- Kenyn L. Koop, MD
- Crystal M. Mackie, MD
- Chad J. Michel, PA-C
- John S. Muus, MD
- Stephen A. Naymick, II, DO
- Emily E. Propst, PA-C
- Zachary Schrank
- Amanda A. Scott, MD
- Hyoungjun Sim
- Rebecca Sullenger
- Robin S. Tanner, MD
- Nina Westcott
- Marcus Wilson, DO
- James B. S. Wise, MD
We are thrilled to have you!
NCMS Recognizes NCMS Disaster Relief Fund Contributors

A heartfelt THANK YOU to these individuals and organizations for their contribution to the NCMS Disaster Relief Fund. Your generous donation is far more than just a financial contribution; it’s a lifeline for the many affected by Hurricane Helene, and vital in providing support to healthcare professionals and communities impacted by this disaster.
We invite you to spread the word about the NCMS Disaster Relief Fund and stay engaged with us as we work together to help restore our Western North Carolina neighbors.
We are grateful to have you in our community!
- Curi
- Anonymous
- Christopher T. Grubb, MD
- Lyndon K. Jordan, III, MD, FACR
- Katie Lowry, MD, MPH
- Laura J. Luckadoo, MD
- Robeson Pediatrics
- Kirby Sheridan
- Catherine L. Sotir, MD
- Vinod C. Vallabh, MD
- Ian D. Archibald, MD
- Preecha Bhotiwihok, MD, MPH
- John W. Black, MD
- Anonymous
- Gay M. Bowman
- Georgi N. Brockway, MD
- Michael T. Brohawn
- Anonymous
- Carolina Complete Health Network
- Sharon M. Foster, MD, FAAP
- Donna C. Graves, MD
- M. Mark Hester, MD
- Suneya G. Hogarty, DO
- Marius J. Ilario, MD
- Linda W. Lawrence, MD
- Douglas S. McFarlane, MD
- Mark B. Moeller, MD
- Anonymous
- Raleigh Orthopaedic Clinic, PA
- Timothy J. Reeder, MD, MPH, FACEP
- Alan J. Rosenbaum, MD
- Anonymous
- Marshall Z. Schwartz, MD
- Douglas D. Sheets, MD, FACOG
- W. Alan Skipper, CAE
- Jennifer K. Stoddard, MD
- STUSQU, PLLC
- Lisa W. H. Thompson, MD
- Cheryl L. Walker-McGill, MD, MBA
- Craig E. Webb, MHS, PA-C
- Johnathan D. Williams, MD
- Anonymous
- Idil Aktan, MD
- R. D. Almkuist, II, MD
- American Board of Pediatrics Inc
- Caroline D. Ames, MD, FACS
- James H. Antoszyk, MD
- Joy Avery
- Timothy M. Beittel, MD
- Anonymous
- Anonymous
- Cedar Mount Behavioral Health, PA
- Center For Pain Management, PLLC
- Melissa M. Coale, MD
- Anonymous
- Kim D. Dansie, MD
- Jackie M. Davis-Jones
- Jessica F. Doerrler, PA
- Patricia Duncan
- Peter A. Eweje, MD
- Mark W. Featherston, MD
- Anonymous
- Joanne M. Fruth, MD
- Lisa M. Gangarosa, MD
- Highland Medical Associates
- Anonymous
- Joseph P. Hunstad, MD, FACS
- Kitsie Jones
- Christopher P. Jordan, MD
- Kerry Kendall
- Eugenie M. Komives, MD, FAAFP
- Ted R. Kunstling, MD, FCCP
- Andrew S. Lamb, MD
- Keith LaScalea, MD
- Anonymous
- Elizabeth G. Livingston, MD
- Anonymous
- Laura L. Martinez, MD
- Darlyne Menscer, MD
- Ashley Newton
- J. Thomas Newton, MD
- Carolyn O'Conor, MD
- Michael K. Patrick, MD
- Patricia Petrick, MD
- Emily Rayes-Prince, MD
- Anonymous
- Corianne D. Rogers, MD
- Nimesh B. Shah, MD
- Kristen M. Shipherd
- Maria J. Small, MD
- Anonymous
- Michol Stanzione, DO
- Steele Creek Dermatology
- Al Steren, MD and Diane Snyder Steren, MD
- Martha Strange, MD
- Thomas M. Swantkowski, MD, AGAF, FACG
- Marian L. Swinker, MD, MPH
- Christopher L. Tebbit, MD
- Monecia Thomas, PhD
- Dimitri G. Trembath, MD
- Michael J. Utecht, MD, FACEP
- Lynnea Villanova, MD
- Bonnie E. Wagner, PA-C
- Rebecca Y. Weinshilboum, DO
- Carl J. Westcott, MD
- Thomas R. White, MD
- Anonymous
- Women's HealthCare Consultant PC
- Nagarjuna Yerra, MD
- Michael Bartiss, MD / Family Eye Care of the Carolinas
- David Boone, MD
- Carolina Complete Health
- Karl Chiang, MD
- John Chretien, MD
- Anonymous
- Kelly Fedoriw, MD
- Carolyn Ferree, MD
- Alison Gardner, MD
- John Goldfield, MHS, PA-C
- Akilah Grimes, MD
- Sandra Jackson / Eastern Pediatrics
- Matthew Katz, MS / MCK Health Strategies
- Melissa Kenny
- Donna McGee, MD
- Larry Napolitano, Jr., MD
- Michael P. Reddy-Miller, MD
- Anonymous
- Andrew Pasternak, MD
- Antonio Ramirez, MD
- Beth Remhof
- Jennifer Root, MD
- Richard Savage, MD
- Anonymous
- Soma Sengupta, MD
- Nimesh Shah / Noble Hospitality Investment
- Amanda Trimpey, MD, MPH, FACOEM
- Yunxiang Zhu, MD
*Please note: List reflects donations received through Tuesday, October 22.
Health Officials Recommend People 50 and Older Get Pneumococcal Vaccine

U.S. health officials recommended that people 50 and older get a shot against bacteria that can cause pneumonia and other dangerous illnesses.
The recommendation was made by a scientific advisory panel and then accepted by the Centers for Disease Control and Prevention. The decision lowered — from 65 — the minimum recommended age for older adults to get the shot.
“Now is a great time to get vaccinated against pneumococcal disease in preparation for the winter respiratory season,” CDC Director Dr. Mandy Cohen said in a statement Wednesday night.
The advisory committee voted 14-1 to make the change during a meeting earlier in the day in Atlanta. The guidance is widely heeded by doctors and prompts health insurers to pay for recommended shots.
Pneumococcal shot recommendations are sometimes called the most complicated vaccination guidance that the government issues. The CDC currently recommends shots for children younger than 5 and adults 65 or older, as long as they have never been vaccinated against pneumococcal disease. Officials also recommend the shots for children and adults at increased risk for pneumococcal disease, such as those with diabetes, chronic liver disease or a weakened immune system.
Lean more about the recommendations here.
CDC Updates COVID Vaccine Recommendations for Older Americans

CDC Director Mandy Cohen endorsed the CDC Advisory Committee on Immunization Practices' (ACIP) recommendation for people 65 years and older and those who are moderately or severely immunocompromised to receive a second dose of 2024-2025 COVID-19 vaccine six months after their first dose. These updated recommendations also allow for flexibility for additional doses (i.e., three or more) for those who are moderately or severely immunocompromised, in consultation with their healthcare provider (a strategy known as shared clinical decision making).
The recommendation acknowledges the increased risk of severe disease from COVID-19 in older adults and those who are immunocompromised, along with the currently available data on vaccine effectiveness and year-round circulation of COVID-19. The recommendation also provides clarity to healthcare providers on how many doses should be given per year to people who are moderately or severely immunocompromised and is meant to increase coverage of this second dose for that group.
Data continues to confirm the importance of vaccination to protect those most at risk for severe outcomes of COVID-19. Receiving recommended 2024-2025 COVID-19 vaccines can restore and enhance protection against the virus variants currently responsible for most infections and hospitalizations in the United States. COVID-19 vaccination also reduces the chance of suffering the effects of Long COVID, which can develop during or following acute infection and last for an extended duration.
CDC and ACIP will continue to monitor COVID-19 vaccine safety and effectiveness. CDC continues to recommend that everyone stay up to date on their COVID-19 vaccines, especially people ages 65 years and older and those with weakened immune systems.
For more information on updated COVID-19 vaccines visit: Coronavirus Disease 2019 (COVID-19) | CDC.
The following statement is attributable to CDC Director Dr. Mandy Cohen:
"This vote allows people to make the best decisions possible to keep themselves and their loved ones safe from COVID-19. CDC will continue to educate the public on how and when to get their updated vaccinations so they can risk less severe illness and do more of what they love." [source]
NCMS Regional Meeting a Huge Success!

Thank you to everyone who attended the NCMS Regional Meeting on Wednesday, October 23rd, at WakeMed's Andrews Center for Medical Education.
We kicked things off with NCMS President-elect Dr. John Meier, who emphasized the importance of getting involved in shaping the future of healthcare.
CEO Chip Baggett shared key updates on NCMS priorities and our ongoing efforts in the aftermath of Hurricane Helene. He also opened the floor to questions.
It was fantastic to see both members and non-members come together to share insights and network with colleagues from across the state.
Keep an eye on your Morning Rounds for updates on our next Regional Meeting. We can't wait to see you there!

Novant Health Recognized for Promoting Clinician Well-being and Reducing Burnout

Novant Health has earned bronze level recognition from the American Medical Association (AMA) as a Joy in Medicine health organization. The prestigious distinction is granted to organizations across the country that meet the rigorous criteria of the Joy in Medicine Health System Recognition Program and are national leaders in prioritizing proven efforts to enhance the well-being and professional fulfillment of physicians and advanced practice providers (APP). Novant Health is one of three health systems recognized in North Carolina.
“This recognition from the AMA affirms our work to prioritize our physicians’ and APP’s well-being so they can thrive both personally and professionally,” said Dr. Navin Bhojwani, senior vice president, Novant Health Medical Group Clinical Operations. “Our physicians and APPs are essential to the remarkable care we provide our patients. Ensuring they have a voice at every level of the organization – from our clinics to the C-suite – is crucial. I’m proud that our teams have been proactive in developing programs and initiatives that reduce burnout and ultimately ensure our clinicians can have a fulfilling career while providing the best possible care for their patients.”
After peaking during the COVID-19 pandemic, the physician burnout rate has dipped under 50% for the first time in four years, according to AMA survey data.
“Physicians are humans caring for other human beings, strained by factors beyond their control and challenged by the enormous expectations placed on them to continuously deliver high quality, compassionate care. There is no doubt change is needed, but what needs to change is not the doctors,” said AMA President Bruce A. Scott, M.D. “A national movement is gaining momentum to transform health care work systems and fix the root causes of physician burnout. Health organizations that have earned the AMA’s Joy in Medicine recognition are leading this movement with bold visions for redesigned clinical systems to foster professional well-being and support quality care.”
Novant Health has had programs in place to support physicians and APPs and reduce burnout for more than a decade, including:
- The Novant Health Leadership Development Program, which has been in place since 2013, has been completed by thousands of Novant Health physicians, advanced practice providers, nurses and leaders. The program focuses on wellness, resiliency and leadership, and is supplemented with a mentoring program and teams that focus on addressing obstacles to experiencing joy and fulfillment practicing medicine.
- A dedicated initiative to reduce the administrative burden associated with providing care. This program is built around direct feedback from physicians and advanced practice providers and has led to a reduction in nearly 75 million clicks in the electronic health record, saving 105,000 hours (or about 12 years) of work.
- Residency opportunities to build the physician pipeline and train the next generation of providers, including family medicine, general surgery, internal medicine and OB-GYN. Novant Health also has two UNC School of Medicine Branch campuses in Charlotte and in Wilmington where third- and fourth-year medical students can complete their rotations, as well as a partnership with Cambell University’s School of Osteopathic Medicine for medical school rotations. Novant Health’s first APP pipeline is currently in development to strengthen the pipeline for advanced practitioners as well.
Since its inception in 2019, the AMA Joy in Medicine Health System Recognition Program has recognized more than 100 organizations across the country. In 2024, a total of 62 health systems nationwide earned recognition with documented efforts to reduce system-level drivers of work-related burnout and demonstrated competencies in commitment, assessment, leadership, efficiency of practice environment, teamwork and support. These 2024 organizations join a strong cohort of currently recognized organizations from the 2023 program. [source]
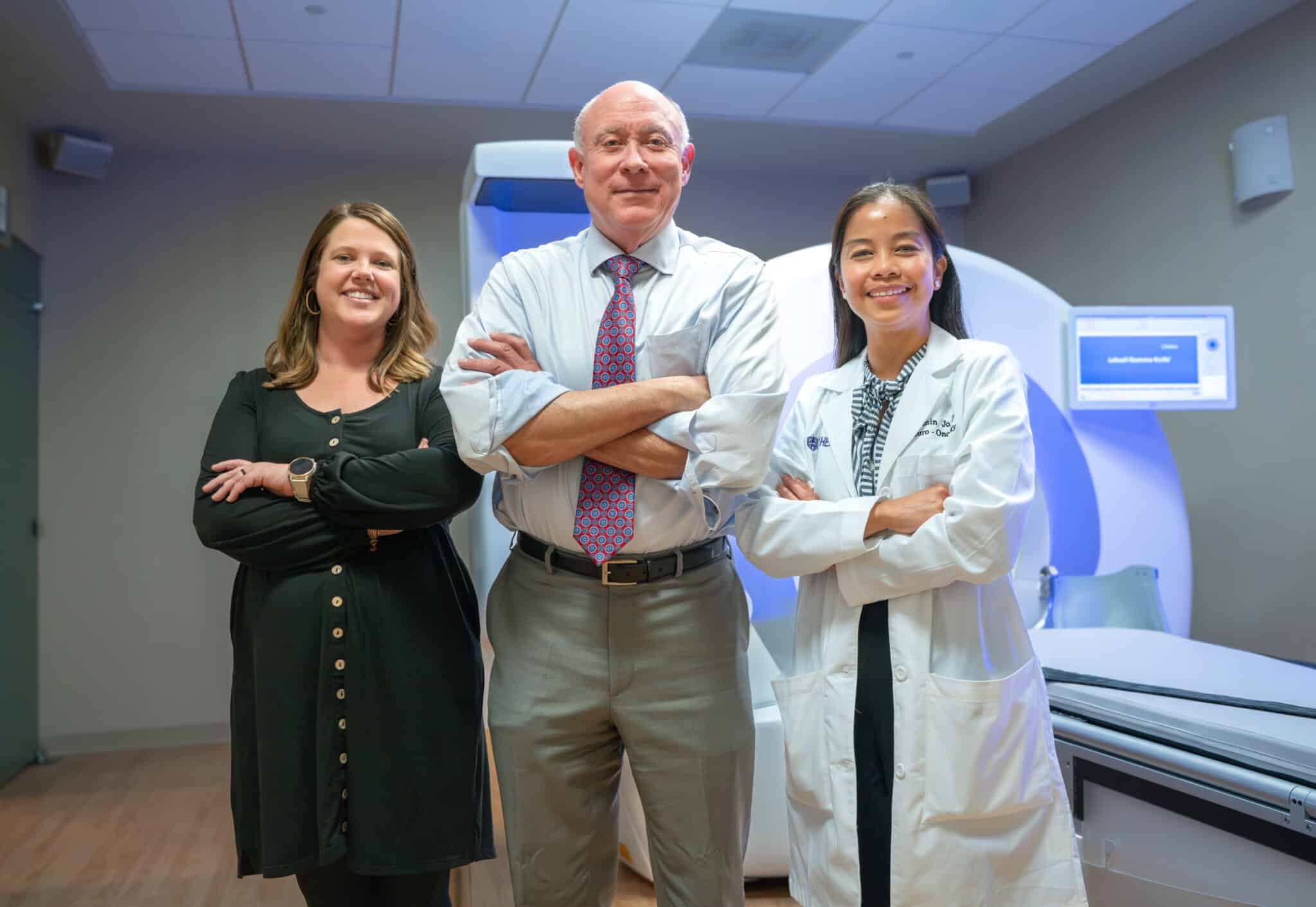
ECU Health Medical Center Earns Gold Seal of Approval® for Brain Tumor Care
ECU Health Medical Center has earned The Joint Commission’s Gold Seal of Approval® Certification for brain tumor care, recognizing the program’s ongoing dedication to delivering safe, high-quality patient care. According to The Joint Commission, the Gold Seal is a symbol of quality that recognizes health care organizations that provide comprehensive care for patients with brain tumors.
“This recognition from The Joint Commission is a testament to the incredible neuro-oncological expertise, technology and research available here at ECU Health Medical Center,” said Jay Briley, president, ECU Health Medical Center. “It is immensely humbling to witness the incredible efforts that take place within the walls of the hospital every single day to further our understanding of brain tumors and brain tumor treatment. We could not be more proud of every team member who helped receive this prestigious certification.”
ECU Health Medical Center underwent a rigorous onsite review in July. During the visit, the Joint Commission reviewer evaluated compliance with related certification standards including compliances with consensus-based national standards, effective integration of evidence-based clinical practice guidelines to manage and optimize care, and organization of approach to performance measurement and performance improvement, including data collection and analysis. Joint Commission standards are developed in consultation with health care experts and providers, measurement experts and patients. The reviewers also conducted onsite observations and interviews.
Continue reading about this honor here.
Grandover Resort is FULLY BOOKED! But Don't Fret Because We've Got You Covered!

Space at the Grandover is FULLY BOOKED!
But don't worry, we have acquired overflow rooms at the Sheraton Greensboro at Four Seasons.
Reserve your room online: NC Medical Society Grandover Overflow - Start your reservation (passkey.com) or call the Sheraton directly at 888-236-2427.
Sheraton Greensboro at Four Seasons
3121 West Gate City Boulevard
Greensboro, NC 27407
Capitol Chronicle: Members of Congress Press Leadership on Medicare Payment Cut

Members of Congress Press Leadership on Medicare Payment Cut
Last week, 233 members of the House of Representatives, led by Rep. Greg Murphy, MD, asked House Speaker Mike Johnson and Minority Leader Hakeem Jeffries to avert the anticipated 2.8% cut in the Medicare Physician Fee Schedule for 2025. Additionally, they urged, 1) action on enact reforms to statutory budget neutrality requirements and 2) physician payment updates reflective of inflationary pressures.
This letter of urgency comes after several months of advocacy by the NC Medical Society and partner organizations in an effort to avoid a fifth year of consecutive Medicare payment cuts. The letter calls for greater certainty and stability for clinicians serving Medicare beneficiaries as the proposed cut by CMS would jeopardize access to care.
North Carolina members of Congress have committed to working with House and Senate leadership to pass bipartisan legislation before the close of the 118th Congress, but the clock is ticking and there is uncertainty about what the post-election session will yield. Have you reached out to your House and Senate members to alert them to what another Medicare payment cut will mean to your practice and to your patients? If you’d like to do so, please respond to this column ([email protected]) to help raise the volume on Capitol Hill.
Your engagement matters.
Do you know your state and federal legislators? More importantly, do your legislators know you?
The NCMS can help you connect with policy makers as a constituent and advocate!
Register Now! Integrating Behavioral Health into Non-Primary Care Settings Webinar.

Integrating Behavioral Health into Non-Primary Care Settings
Thursday, October 31, 2024
12:00 PM Central Daylight Time/1:00 PM Eastern Time
While much of the focus to date has been on enabling integrated behavioral health care within primary care settings, there continues to be a huge need for more timely, equitable access to whole-person care in other specialty care settings – including both cardiology and oncology. In this live event with the American College of Cardiology (ACC) and the American Society of Clinical Oncology (ASCO), hear how their organizational members are enhancing patient care through behavioral health integration (BHI). Glean insights from these two organizations on actionable strategies for recognizing and addressing these needs within their specialties and what they think the future of BHI looks like. Physician experts will also cover the importance of BHI within these care settings, particularly as it relates to the interplay between relevant chronic care conditions and behavioral health conditions.
Are You Taking Advantage of Collaborative Care Model Training Series?
The North Carolina Department of Health and Human Services (DHHS) has partnered with NC AHEC to provide educational and practice-based support to primary care practices interested in implementing the Collaborative Care Model (CoCM) -- a team-based, interdisciplinary approach to deliver evidence-based diagnoses, treatment, and follow-up care for patients with mild to moderate behavioral health needs.
CoCM is an integrated modality that provides patients with medical and behavioral health care in a primary care setting. An increasing number of primary care settings are incorporating behavioral health services. Benefits of CoCM include better patient outcomes, improved patient and provider satisfaction, and reduction in health care costs. In addition, using CoCM may reduce health disparities in access to behavioral health. Most payors in North Carolina already cover the CoCM billing codes.
NC AHEC is offering CoCM virtual learning opportunities, including Education Modules designed for providers interested in learning about the CoCM. Currently, 15 modules are available, with additional modules being added regularly.
Modules currently available on demand include (listed in order of release date):
Module 15: Improving CoCM Quality Using Technology
Module 14: Collaborative Care in Perinatal Populations
Module 13: Diversity, Equity, and Inclusion in Collaborative Care: A Review of the Evidence in Minority Populations and Next Steps
Module 12: Collaborative Care Model in Substance Use Disorders
Module 11: Primary Care Provider Engagement
Module 10: Best Practices in Pediatric Collaborative Care
Module 9: Behavioral Health Care Manager (BHCM) Best Practices
Module 8: Best Practices for Collaborative Care Management Behavioral Health Care Manager
Module 7: Brief Therapeutic Interventions
Module 6: Billing the Codes and the General Business Model for Collaborative Care
Module 5: The Role of the Psychiatric Consultant in the Collaborative Care Model
Module 4: Collaborative Care Management for Primary Care Providers
Module 3: Putting Collaborative Care Principles into Practice: Planning for Clinical Practice Change
Module 2: Laying the Foundation for Collaborative Care Through Practice Transformation
Module 1: Collaborative Care Model (CoCM) Rationale and Evidence
View a collection of informercials to learn more about CoCM and how it’s being implemented in practices statewide!
Visit NC AHEC's Collaborative Care Model Webpage here.
Take advantage of this useful and helpful training opportunity today.
Share Your Helene Stories!

The North Carolina Medical Society invite you to share your Hurricane Helene stories. It can be through a photo that captures the storm’s aftermath, a video of your community coming together to help neighbors, or a personal story you want/need to share.
Please send your submissions to Randy Aldridge at [email protected].
Thank you for sharing your experience with us!
Starlink Assistance for Facilities Impacted by Helene

NCDHHS may be in a position to assist practices with securing Starlink and is seeking your input about practices in the Hurricane impacted counties that need Starlink. DHHS will use your information to link Starlink resources with practices.
Please share the following information with Nicole Fields-Pierre, MPA, NCCM, Community Health Program Manager, Office of Rural Health at [email protected]:
- County
- Practice/clinic name
- Specialty
- Address
- Point of contact: name, cell phone number, email addresses
Influenza Vaccine and Reimbursement Guidelines for 2024-2025 for NC Medicaid

NC Immunization Program/Vaccines for Children (NCIP/VFC)
Under NC Immunization Program/Vaccines for Children (NCIP/VFC) guidelines, the NC Division of Public Health (DPH) Immunization Branch distributes all childhood vaccines that are recommended by the Advisory Committee on Immunization Practices (ACIP) to local health departments, Federally Qualified Health Centers (FQHC), Rural Health Clinics (RHC), hospitals and private providers.
For the 2024-2025 influenza season, NCIP/VFC influenza vaccines are available at no charge to providers for children six months through 18 years of age who are eligible for the VFC program, according to the NCIP coverage criteria. The current NCIP coverage criteria and definitions of VFC categories can be found on DPH’s Immunization Branch web page.
For providers interested in enrolling in the VFC program, information can be found on the CDC information page and the NC DPH website.
Eligible VFC children include ALL Medicaid beneficiaries (through 18 years of age).
For VFC/NCIP vaccines administered to VFC-eligible children, providers must report only the vaccine code(s) with $0.00. Providers may bill NC Medicaid for the administration fee for Medicaid.
Providers who administer privately purchased vaccines to VFC eligible beneficiaries will NOT be reimbursed for the vaccine and cannot bill the beneficiary for that cost. Only the administration fee(s) will be reimbursed.
Providers must purchase vaccines for beneficiaries who are not VFC-eligible. For Medicaid-eligible beneficiaries aged 19 years and older, purchased vaccine and administration costs may be billed to NC Medicaid, according to the guidelines stated in Tables 2 and 3 below. To determine who is eligible for NCIP influenza and other vaccines, visit DPH’s Immunization Branch web page.
For providers interested in enrolling in the VFC program, information can be found on the CDC information page and the NC DPH website.
Eligible VFC children include ALL Medicaid beneficiaries (through 18 years of age).
Continue to full bulletin here.
NCDHHS Urges Safety Measures for Heating Homes in Western NC as Temperatures Drop

As cooler weather arrives in Western North Carolina, the NC Department of Health and Human Services urges individuals, families and communities impacted by Hurricane Helene to take safety precautions when heating homes, buildings or other enclosed spaces.
Using gas or wood-burning heat sources without proper safety measures can lead to carbon monoxide poisoning and other hazards, especially if fuel sources or appliances have been damaged by the storm.
Safe Practices for Wood-Burning Stoves
Properly installed, correctly used wood-burning appliances should generate very little smoke. If you regularly see or smell smoke, you may have a problem. Take the following steps to reduce smoke inside and outside your home:
- What NOT to burn: Do not burn household trash (including cardboard, plastics, foam, magazines, boxes and wrappers), coated wood, painted wood, pressure-treated wood, driftwood, plywood, particle board, wood with any glue on it, wet or green wood, rotted wood, moldy wood, asbestos, rubber, manure or animal remains. These materials can release toxic or harmful chemicals when burned and may also damage your stove.
- What to burn: Try to burn mainly dry, split, well-seasoned wood. Properly seasoned wood is darker, weighs less and sounds hollow when hit against another piece of wood. You can also use branches, sticks or limbs from fallen trees that are off the ground. Do not use wet or green wood.
- Use a starter: Start fires with newspaper, dry kindling or all-natural fire starters. Never start a fire in a wood-burning stove with gasoline, kerosene or charcoal starter.
- Keep flammable items away: Maintain a safe distance between stoves and items like curtains, furniture, newspapers, books or paper. Regularly remove ashes into a covered, metal container, and store the container outdoors on a nonflammable surface.
- Keep the fire hot and door closed: For most appliances, a smoldering fire is not safe or efficient. Build a hot fire and keep the doors of your wood-burning appliance closed unless loading or stoking the live fire. Harmful chemicals, like carbon monoxide, can be released into your home through an open stove door.
- Keep a fire extinguisher handy: In case of a fire, have a fire extinguisher, fire blanket or ample sand or water on-hand to put it out before it can spread.
Safe Practices for Generators and Fuel-Burning Heat Sources
In previous hurricanes in North Carolina, people have died from carbon monoxide poisoning caused by generators running indoors. Carbon monoxide is an odorless, colorless gas produced whenever fuel is burned. In an enclosed space, such as a home, garage, car or camper, carbon monoxide can build up to deadly levels quickly.
High levels of carbon monoxide can be deadly within minutes. Carbon monoxide poisoning can be fatal to anyone, especially children, pregnant women, older adults and those with chronic illness. People who are sleeping can die from carbon monoxide poisoning without ever becoming aware of their symptoms.
Anyone testing or using a generator or other fuel burning device during should take proper safety precautions, including the following:
- Do not use gasoline-powered tools or engines in enclosed or partially enclosed spaces. Use them outdoors at least 20 feet from all doors, windows and air vents.
- Do not use charcoal grills or propane stoves indoors, even in a fireplace.
- Never use the kitchen stove or other gas appliances to heat your home.
- Do not idle your car, truck or other vehicle in the garage, even if the garage door to the outside is open. Fumes can build up quickly in the garage and living area of your home.
- Keep rooms well ventilated.
- Read and follow all instructions that accompany fuel-burning devices. Use the proper fuel and make sure there is enough air for ventilation and fuel burning.
Even low levels of carbon monoxide can cause dizziness, fatigue, nausea, headaches, confusion or fainting. If you are experiencing these symptoms, get to fresh air immediately and seek medical attention as soon as possible.
For additional questions on how to safely use woodstoves and generators and prevent carbon monoxide poisoning, contact the Occupational and Environmental Epidemiology Branch, NC Division of Public Health, NCDHHS, at 919-707-5900. For more information about Hurricane Helene and resources available for people who are impacted, please go to ncdhhs.gov/helene and ncdps.gov/helene. [source]
Disruptions in Availability of Peritoneal Dialysis and Intravenous Solutions from Baxter International Facility in North Carolina

The Centers for Disease Control and Prevention (CDC) is issuing this Health Alert Network (HAN) Health Advisory to inform healthcare providers, pharmacists, healthcare facility administrators, and state, tribal, local, and territorial health departments of a supply disruption of peritoneal dialysis (PD) and intravenous (IV) solutions from the Baxter International’s North Cove facility in North Carolina, due to Hurricane Helene. The supply disruption may impact patient care and require adjustments to the clinical management of patients. Healthcare providers, pharmacists, healthcare facility administrators, and state, tribal, local, and territorial health departments, regardless of supply chain disruptions, should immediately assess their supply and develop plans and mitigation strategies to reduce the impact on patient care.
Read the full official CDC HEALTH ADVISORY here.
FTC Increases Premerger Notification Requirements Despite Objections

The Federal Trade Commission finalized changes to a rule that will require healthcare companies to provide more information to regulators ahead of merger and acquisition deals.
The agency said the changes that will improve the ability of the FTC and Antitrust Division of the U.S. Department of Justice (DOJ) to detect illegal mergers and acquisitions prior to consummation.
"The final rule requires additional information that is necessary to determine which deals require an in-depth antitrust investigation," the FTC said in a press release.
Learn more about the premerger notification requirements here.
ICYMI: Baxter Imports IV Fluids as Hurricane Helene Triggers U.S. Shortage

Baxter International began shipments of intravenous products to the United States from two international facilities last week, it said on Monday, as it works to bring a hurricane-hit plant in North Carolina back online amid a shortage of the essential medical product.
The medical device maker also received the U.S. Food and Drug Administration's clearance on October 9 to temporarily import products from five facilities in Canada, China, Ireland, and the UK, and was working to secure authorization for more sites amid a nationwide shortage following flooding of the plant by Hurricane Helene late last month.
On Monday, Baxter said its current priority is deep cleaning the facility and assessing the status of all equipment and production lines.
The Marion, North Carolina, site makes 60% of the nation's supply of IV fluids and peritoneal dialysis solutions, amounting to 1.5 million bags daily, according to the American Hospital Association.
A shortage of IV fluids, which provide nutrients to the body or replenish fluids lost due to injury or illness, has forced hospitals to curtail elective procedures.
While the flooding has disrupted the production of peritoneal dialysis solutions, the company said it is actively delivering supplies to patients.
"We do not yet have a timeline for when we expect production to be fully restored to pre-hurricane levels," the company said, while urging conservation of both IV and peritoneal dialysis solutions.
The company last week said it plans to restart its plant in phases and aims to meet 90% to 100% of customer needs by the end of the year. [source]
NCMS Recognizes NCMS Disaster Relief Fund Contributors

A heartfelt THANK YOU to these individuals and organizations for their contribution to the NCMS Disaster Relief Fund. Your generous donation is far more than just a financial contribution; it’s a lifeline for the many affected by Hurricane Helene, and vital in providing support to healthcare professionals and communities impacted by this disaster.
We invite you to spread the word about the NCMS Disaster Relief Fund and stay engaged with us as we work together to help restore our Western North Carolina neighbors.
We are grateful to have you in our community!
- Ian D. Archibald, MD
- Preecha Bhotiwihok, MD, MPH
- John W. Black, MD
- Anonymous
- Gay M. Bowman
- Georgi N. Brockway, MD
- Michael T. Brohawn
- Anonymous
- Carolina Complete Health Network
- Sharon M. Foster, MD, FAAP
- Donna C. Graves, MD
- M. Mark Hester, MD
- Suneya G. Hogarty, DO
- Marius J. Ilario, MD
- Linda W. Lawrence, MD
- Douglas S. McFarlane, MD
- Mark B. Moeller, MD
- Anonymous
- Raleigh Orthopaedic Clinic, PA
- Timothy J. Reeder, MD, MPH, FACEP
- Alan J. Rosenbaum, MD
- Anonymous
- Marshall Z. Schwartz, MD
- Douglas D. Sheets, MD, FACOG
- W. Alan Skipper, CAE
- Jennifer K. Stoddard, MD
- STUSQU, PLLC
- Lisa W. H. Thompson, MD
- Cheryl L. Walker-McGill, MD, MBA
- Craig E. Webb, MHS, PA-C
- Johnathan D. Williams, MD
- Anonymous
- Idil Aktan, MD
- R. D. Almkuist, II, MD
- American Board of Pediatrics Inc
- Caroline D. Ames, MD, FACS
- James H. Antoszyk, MD
- Joy Avery
- Timothy M. Beittel, MD
- Anonymous
- Anonymous
- Cedar Mount Behavioral Health, PA
- Center For Pain Management, PLLC
- Melissa M. Coale, MD
- Anonymous
- Kim D. Dansie, MD
- Jackie M. Davis-Jones
- Jessica F. Doerrler, PA
- Patricia Duncan
- Peter A. Eweje, MD
- Mark W. Featherston, MD
- Anonymous
- Joanne M. Fruth, MD
- Lisa M. Gangarosa, MD
- Highland Medical Associates
- Anonymous
- Joseph P. Hunstad, MD, FACS
- Kitsie Jones
- Christopher P. Jordan, MD
- Kerry Kendall
- Eugenie M. Komives, MD, FAAFP
- Ted R. Kunstling, MD, FCCP
- Andrew S. Lamb, MD
- Keith LaScalea, MD
- Anonymous
- Elizabeth G. Livingston, MD
- Anonymous
- Laura L. Martinez, MD
- Darlyne Menscer, MD
- Ashley Newton
- J. Thomas Newton, MD
- Carolyn O'Conor, MD
- Michael K. Patrick, MD
- Patricia Petrick, MD
- Emily Rayes-Prince, MD
- Anonymous
- Corianne D. Rogers, MD
- Nimesh B. Shah, MD
- Kristen M. Shipherd
- Maria J. Small, MD
- Anonymous
- Michol Stanzione, DO
- Steele Creek Dermatology
- Al Steren, MD and Diane Snyder Steren, MD
- Martha Strange, MD
- Thomas M. Swantkowski, MD, AGAF, FACG
- Marian L. Swinker, MD, MPH
- Christopher L. Tebbit, MD
- Monecia Thomas, PhD
- Dimitri G. Trembath, MD
- Michael J. Utecht, MD, FACEP
- Lynnea Villanova, MD
- Bonnie E. Wagner, PA-C
- Rebecca Y. Weinshilboum, DO
- Carl J. Westcott, MD
- Thomas R. White, MD
- Anonymous
- Women's HealthCare Consultant PC
- Nagarjuna Yerra, MD
- Michael Bartiss, MD / Family Eye Care of the Carolinas
- David Boone, MD
- Carolina Complete Health
- Karl Chiang, MD
- John Chretien, MD
- Anonymous
- Kelly Fedoriw, MD
- Carolyn Ferree, MD
- Alison Gardner, MD
- John Goldfield, MHS, PA-C
- Akilah Grimes, MD
- Sandra Jackson / Eastern Pediatrics
- Matthew Katz, MS / MCK Health Strategies
- Melissa Kenny
- Donna McGee, MD
- Larry Napolitano, Jr., MD
- Michael P. Reddy-Miller, MD
- Anonymous
- Andrew Pasternak, MD
- Antonio Ramirez, MD
- Beth Remhof
- Jennifer Root, MD
- Richard Savage, MD
- Anonymous
- Soma Sengupta, MD
- Nimesh Shah / Noble Hospitality Investment
- Amanda Trimpey, MD, MPH, FACOEM
- Yunxiang Zhu, MD
*Please note: List reflects donations received through Tuesday, October 15.
Study: Thousands of Cancer Cases Went Undiagnosed in Covid Pandemic
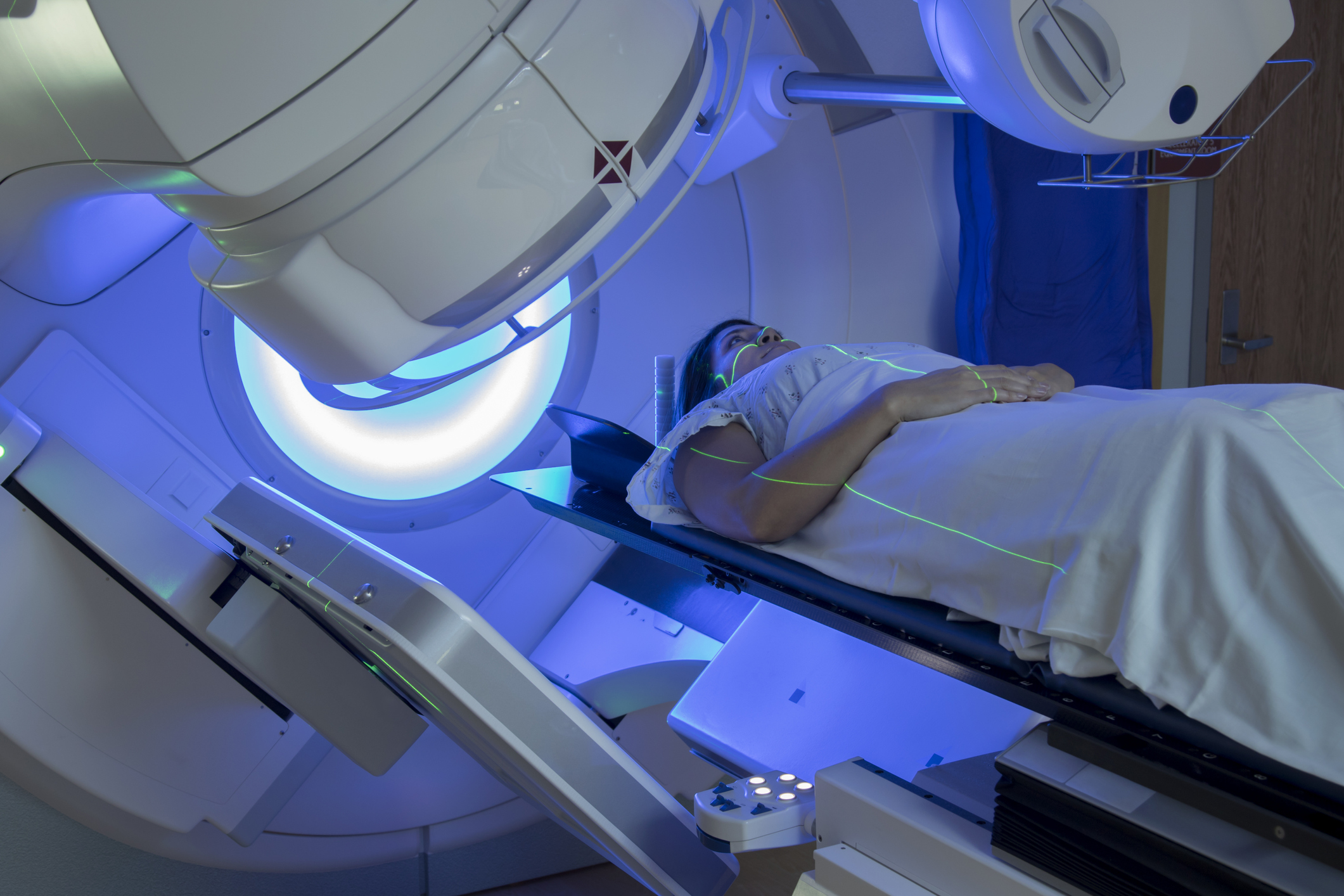
When the U.S. health care system pivoted to meet Covid-19 in 2020, routine health visits and screenings where many cancer cases would have been caught didn’t happen. It wasn’t ideal, but many health experts thought that as the country opened back up, screenings would help “catch up” to these missed cases. A new paper published Monday in JAMA Network Open suggests that didn’t happen as quickly as experts had hoped.
Instead, the new analysis suggests that cancer diagnoses recovered to pre-pandemic levels by the end of 2021 — but didn’t make up for any of the lost cases from earlier in the pandemic. That leaves a troubling mystery for epidemiologists, as it means experts still don’t know what happened with the roughly 130,000 cancer cases that were missed in 2020.
Continue to full article here.
North Carolina Ranks 10th Worst State for Healthcare Access

North Carolina is the 10th worst state for healthcare access, according to a study from Forbes Advisor.
According to Forbes Advisor, North Carolina has the:
- Fifth-lowest number of nurse practitioners per 10,000 residents (4.3).
- Eighth-highest average premium for employees with single coverage through employer-provided health insurance ($1,847 annually).
- 10th-highest percentage of residents who lack health insurance coverage (9.3%).
- 10th-highest average deductible for employees with single coverage through employer-provided health insurance ($2,247 annually).
North Carolina employers also cover the sixth-lowest percentage of employees’ annual health insurance premiums (76% for employees with single coverage), according to Forbes Advisor.
The study says North Carolina has a strong need for more qualified healthcare professionals.
Rounding out the worst states for healthcare access in the study are Utah at No. 1, Nevada at No. 2, Texas at No. 3, Arizona at No. 4, Georgia at No. 5, South Carolina at No. 6, Indiana at No. 7, Wyoming at No. 8 and Idaho at No. 9. [source]
Examining Critical Mental Health Issues Across the Reproductive Life Cycle

Examining Critical Mental Health Issues Across the Reproductive Life Cycle
October 23, 2024 | 1 - 2:30 p.m. ET
The National Academies Standing Committee on Reproductive Health, Equity, and Society will host a public webinar to explore mental health issues that individuals face across the reproductive life cycle, including issues around sexual education, sexual coercion, and violence.
Speakers, including researchers and practitioners, will touch upon social determinants of health, misinformation, and access to care for marginalized communities, among other topics. Discussions will also include identifying potential contextual and systemic solutions to address these issues. Learn more on the event page.
Speakers include:
- Elizabeth Miller, MD, PhD, FSAHM, Professor of Pediatrics, Public Health and Clinical and Translational Science, University of Pittsburgh
- Inger Burnett-Zeigler, PhD, Associate Professor of Psychiatry and Behavioral Sciences, Northwestern University Feinberg School of Medicine
- M. Antonia Biggs, PhD, Associate Professor and social psychologist at ANSIRH, Bixby Center for Global Reproductive Health, University of California San Francisco
- Ruth Shim, MD, MPH, Luke & Grace Kim Professor in Cultural Psychiatry and Professor of Clinical Psychiatry, Associate Dean of Diverse and Inclusive Education, University of California Davis
Moderator:
Katherine L. Wisner, MD, MS, Professor of Psychiatry and Behavioral Sciences and Pediatrics and Associate Chief, Prenatal Mental Health, Developing Brain Institute, Children’s National Hospital, Washington DC; Professor of Obstetrics and Gynecology, George Washington University School of Medicine and Health Sciences
Merit-based Incentive Payment System Automatic EUC Policy Applied to MIPS Eligible Clinicians Following Hurricanes Helene and Francine

The U.S. Department of Health and Human Services (HHS) Secretary Becerra recently released a letter to healthcare leaders and stakeholders on the impacts of Hurricane Helene, which can be found on the HHS website.
In response to Hurricanes Helene and Francine, the Centers for Medicare & Medicaid Services (CMS) has determined that the MIPS automatic EUC policy will apply to MIPS eligible clinicians in the following designated affected counties of Florida, Georgia, North Carolina, South Carolina, Tennessee, and Louisiana:
- HHS Public Health Emergency (PHE) declaration
- Hurricane Helene: Florida, Georgia, North Carolina, South Carolina, and Tennessee
- Hurricane Francine: Louisiana
- Federal Emergency Management Agency (FEMA) disaster declaration
- Hurricane Helene: DR-4828-FL, DR-4830-GA, DR-4827-NC, DR-4829-SC, and DR-4832-TN
- Hurricane Francine: FEMA-4817-DR
MIPS eligible clinicians in these areas will be automatically identified and have all 4 performance categories reweighted to 0% during the data submission period for the 2024 performance period (January 2 to March 31, 2025). This will result in a score equal to the performance threshold, and they'll receive a neutral payment adjustment for the 2026 MIPS payment year.
However, if MIPS eligible clinicians in these areas submit data on 2 or more performance categories, they’ll be scored on those performance categories and receive a 2026 MIPS payment adjustment based on their 2024 MIPS final score.
NOTE: The MIPS automatic EUC policy doesn’t apply to MIPS eligible clinicians participating in MIPS as a group, subgroup, virtual group, or Alternative Payment Model (APM) Entity. However, groups, virtual groups, and APM Entities can request reweighting through the EUC Exception application. Subgroups will inherit any reweighting approved for their affiliated group; they can’t request reweighting independent of their affiliated group’s status.
For More Information
Please reference the MIPS EUC Exception section on the Quality Payment Program Exception Applications webpage.
Western North Carolina Residents Can Apply for Help Buying Food
Residents in 25 western counties and the Eastern Band of Cherokee Indians impacted by Hurricane Helene can apply for help buying food through the Disaster Supplemental Nutrition Assistance Program (D-SNAP) which will begin on October 18, 2024, the North Carolina Department of Health and Human Services announced. D-SNAP is open to individuals and households not currently receiving Food and Nutrition Services benefits who were impacted by Hurricane Helene. NCDHHS estimates more than 150,000 people will apply for up to $120 million in D-SNAP benefits.
"We are making up to $120 million available to more than 150,000 individuals to buy food for their families — an essential step on the road to recovery from the devastation of Hurricane Helene," said N.C. Health and Human Services Secretary Kody H. Kinsley. "We are committed to using every tool to support the recovery of our friends, families, and fellow North Carolinians in western NC — now and for the long haul."
NCDHHS received federal approval to begin phase one of the program from the U.S. Department of Agriculture beginning on October 18, 2024. People can start applying for assistance three days before the program starts during online pre-registration beginning Oct. 15 and will have seven days from the start of the program to apply. The application period will close on October 24, 2024.
Eligible households will be notified within three days of completing the application and receive a one-time benefit on a special debit card (called an Electronic Benefits Transfer, or EBT card) to help buy food. The exact amount will depend on household size, income and disaster losses. While there are income eligibility standards, a number of considerations are taken into account. Individuals above these limits may still be eligible dependent on disaster expenses, so we encourage everyone who needs support to purchase food to begin their application by calling the DSNAP Virtual Call Center at 1-844-453-1117.
The benefits are good for up to nine months. Benefit cards will be available for pick up at the D-SNAP locations in each county or you can get the EBT card mailed to you overnight at the address you specify on your application.
Continue to full press release here.
HRSA: Extension of Public Health Emergency Telehealth Guidance for Non-current Health Center Patients

Message from HRSA:
We’ve extended the expiration date for our guidance on using telehealth for people who are not current health center patients. You can find the updated telehealth FAQ in the Health Center Program Compliance FAQs.
We initially posted this FAQ during the COVID-19 Public Health Emergency and extended last year’s expiration date. The FAQ's telehealth guidance is now in effect until we issue the final new policy or until December 31, 2025, whichever comes first.
We anticipate releasing the draft Health Center Program Scope of Project Policy Manual for public comment this fall. The manual will include a chapter on telehealth. We will announce the release broadly — we truly value your feedback.
Register Now! How to Protect Your Practice and Patients from Cybersecurity Threats
How to Protect Your Practice and Patients from Cybersecurity Threats
Friday, October 18
12:30 p.m. Central Time/1:30 p.m. Eastern Time
After the Change Healthcare cyberattack earlier this year, cybersecurity has become a central concern for physicians and patients alike. Attend this AMA Advocacy Insights webinar to learn about how to implement appropriate cybersecurity measures to protect your practice as well as your patients against the cybersecurity challenges of today. Also hear about advocacy that is underway to strengthen cybersecurity systems and provide support to physician practices for enhancing their cyberhygiene.
MODERATOR
- Michael Suk, MD, JD, MPH, MBA, chair, AMA Board of Trustees
SPEAKERS
- Christian Dameff, MD, Department of Emergency Medicine, School of Medicine, University of California, San Diego
- Greg Garcia, executive director for cybersecurity, Health Sector Coordinating Council
If you are unable to attend live, a recording of the presentation will be emailed out to all registrants.
If you are unable to attend live, a recording of the presentation will be emailed out to all registrants.
Disaster Relief Applications for Health Care Professionals Not Currently Enrolled as an NC Medicaid Provider
The NC Department of Health and Human Services is committed to ensuring continued access to care for NC Medicaid beneficiaries, as well as reimbursement to qualified providers for services rendered, in good faith, throughout the period of impacts from Hurricane Helene, retroactively from September 25, 2024, through December 31, 2024, (unless otherwise communicated by DHHS).
- The Centers for Medicare & Medicaid Services (CMS) granted approval effective October 1, 2024, for DHHS to implement a temporary, expedited enrollment process for health care professionals to become an NC Medicaid provider due to a natural disaster. This process is not for providers who regularly see NC Medicaid beneficiaries.
Health care professionals who will be rendering services to NC Medicaid beneficiaries due to Hurricane Helene can complete and submit an application through the NCTracks Provider Portal. Please refer to the disaster provider enrollment job aid Disaster Relief Provider Enrollment Application Job Aid (PRV703) located under Quick Links on the NCTracks Provider Enrollment home page for necessary instructions to complete the temporary disaster provider enrollment application. Be sure to review the job aid before starting to complete the application, as several preliminary steps are necessary.
Providers must indicate the application is for Disaster Relief by answering “Yes” to the Disaster Relief enrollment question on the Online Application page of the application.
Note: This is not for providers who see NC Medicaid beneficiaries on a regular basis.
Please review North Carolina Medicaid Provider Enrollment Disaster Relief and Waiver or Modification of Requirements Under Section 1135 of the Social Security Act from the Secretary of Health and Human Services for additional information.
Information about Governor Cooper’s Declaration of a State of Emergency can be found at Governor Cooper Declares State of Emergency Ahead of Hurricane Helene.
Contact
- NCTracks Call Center: 800-688-6696
- Provider Ombudsman: 866-304-7062, [email protected]
Reminder: Nominating and Leadership Development Committee Issues Final Slate of Nominees
The North Carolina Medical Society (NCMS) Nominating and Leadership Development Committee (NLDC) issues the final slate of candidates. Under the NCMS’ governance structure, online voting for the candidates will begin on Monday, October 14, 2024, and continue until midnight on Wednesday, October 30, 2024. Paper ballots will also be available to those who need them.
The following slate of nominees was selected by the Nominating and Leadership Development Committee:
NCMS Board of Directors
- President Elect: Carl Westcott, MD
- Region 1 Representative: Claude Jarrett, MD
- At-Large Member: Jugta Kahai, MD
- At-Large Member: C. Labron Chambers, Jr., MD
NC American Medical Association Delegation
- AMA Delegate: E. Rebecca Hayes, MD
- AMA Delegate: Karen Smith, MD
- AMA Delegate: Royce Syracuse, MD
- AMA Delegate: Arthur Apolinario, MD
Nominating and Leadership Development Committee
- NLDC Region 1: Joe Navejar, MD
- NLDC Region 1: Sherry Ikalowych, MD
- NLDC Region 2: Hans Arora, MD
- NLDC Region 3: Katie Borders, MD
- NLDC Region 3: Sankalp Puri, MD
- NLDC Region 3: Mary Knox, MD
- NLDC Region 4: Benjamin Deschner, MD
- NLDC Region 4: Shannon Dowler, MD
- NLDC Region 4: Eric Luk, MD
UNC Health Appalachian: Caring for Your Emotional Health After Hurricane Helene

Grief hangs heavy in the air after Hurricane Helene. We’ve experienced an overwhelming and profound sense of loss. It’s a feeling so crippling, it is hard to put into words. Familiar faces are displaced or still missing, and our towns have been transformed into reminders of what once was. We ask ourselves; how can we possibly move on from this? In the wake of Hurricane Helene, we are left with a mix of emotions – grief, anger, confusion, and even guilt.
The sudden shift can feel so isolating, as though the rest of the world and state has moved on, and yet we are still here, trying to process what has happened. We are left to assess the damage, pick up the pieces, and navigate this emotional toll. During this time, we encourage you to care for your mental and emotional health the best that you can – because you can’t help take care of others if you do not take of yourself. Here are some tips to care for your emotional health:
Allow yourself to grieve
Feel all the feels. Just as you would after any loss, grieve for what you’ve lost. There is no right way to do it, and there’s certainly no timeline. Sometimes, reactions to traumatic events like this appear immediately after the chaos, surfacing in the form of anxiety or shock. Other times, they can linger, emerging days, weeks, or even months later, as the weight of the experience settles in.
Cry if you need to. Yell if you want to. All these feelings are a natural response to trauma, and you have permission to feel and express them. Grief is a complicated journey. One moment, you might find yourself smiling at a memory, and the next, you’re overcome by sadness. Acknowledge these feelings – they are simply a reflection of the love we hold for what we’ve lost.
Moving forward, together
Seek support from family, friends, or community groups who understand what you’ve gone through. Share your story, listen to theirs, and hug someone. Continue to reach out and support one another – through connection, compassion, and our beautiful community spirit, we will heal. Together, we can weather any storm that comes our way.
Establish a routine
In times of chaos, establishing a loose daily routine can provide a sense of normalcy. Start your day with a morning routine and small, manageable tasks that can set the tone for the day. For example, try waking up around the same time each day, even if you’re relying on natural light to greet you. Or try spending a moment each day in quiet reflection or gratitude. Consider writing down what you are grateful for, no matter how small. This practice can help shift your mindset and pull you out of a funk.
Seek professional help
Seeking help from a mental health professional can provide a safe space to process these feelings. Therapists are trained to help individuals navigate the emotional aftermath of disasters like Hurricane Helene. They can offer coping strategies, support, and a listening ear during a time when you may feel the need for connection the most.
For instance, if you’ve lost your job due to the storm, a therapist can help you work through the stress and uncertainty about your future. They can assist in reframing your perspective, helping you focus on the small steps you can take each day to move forward.
Find joy in the small things
As you navigate your grief, remember that it’s okay to find moments of joy amidst the loss and sadness. Maybe it’s the hot shower you took at your neighbor’s house because you are still without power, or the warmth of the sun on your face as you step outside, or perhaps it’s a text from a friend from long ago checking in on you – these moments can coexist with your feelings of loss. Allowing yourself to experience joy doesn’t diminish your grief.
Just as the physical rebuilding of our community will take time, so does emotional healing. Be kind to yourself, be gentle, and stay safe.
If you are experiencing feelings of loss and depression, know that you are not alone. There are trained professionals from the Disaster Distress Hotline who want to talk and who are ready to assist you at 800-985-5990. [source]