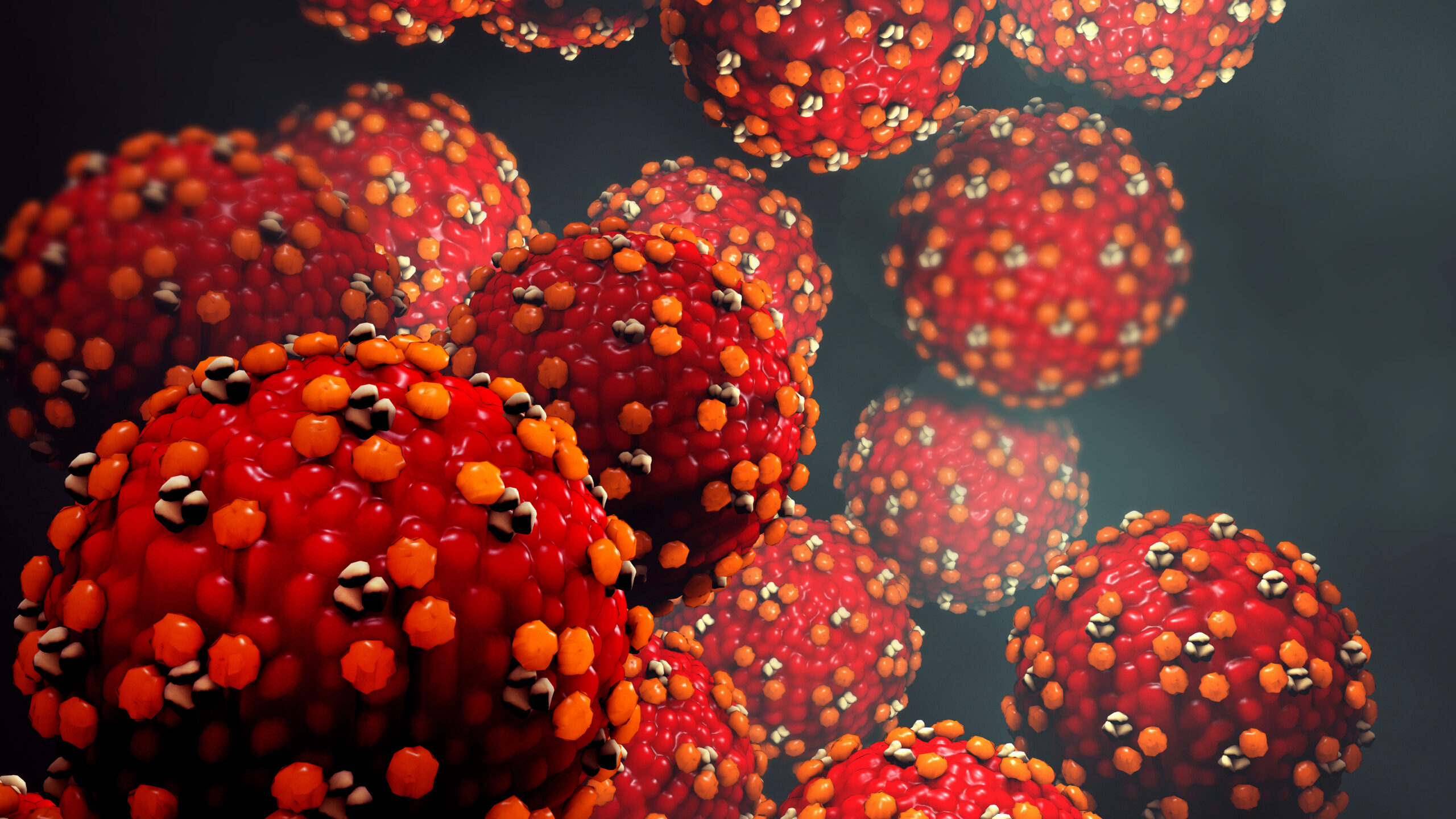
First Case of Measles Identified in North Carolina

The North Carolina Department of Health and Human Services Released A Report of the First Measles Case in NC
RALEIGH — The North Carolina Department of Health and Human Services has confirmed a case of measles in a child who was visiting Forsyth and Guilford counties. The child became ill while traveling to NC from another country where measles outbreaks have recently been reported. To protect the individual and their family’s privacy, no additional information about this individual will be released. This is the first confirmed case of measles in the state in 2025.
NCDHHS is recommending all unvaccinated individuals ages one year and older receive measles vaccination to protect themselves and those around them. NCDHHS is working closely with the Forsyth County Department of Public Health and Guilford County Health Department to identify locations and times where people might have been exposed to measles.
If you visited a listed location during the dates and times below, review your immunization records or contact your health care provider to make sure you are up to date on the measles-mumps-rubella (MMR) vaccine.

Laboratory testing is not recommended for people who were exposed unless they develop symptoms of measles, including fever and rash. Symptoms of measles can start seven to 21 days after being exposed. If symptoms develop, please call ahead before visiting the doctor or emergency room so steps can be taken to prevent exposure to others.
In some situations, people who have been exposed to measles may be eligible to receive postexposure prophylaxis (PEP) to reduce their risk of becoming ill. The timeframe for PEP has passed for most people who were potentially exposed to this case, but those who are at higher risk — including infants too young to receive MMR vaccination, immunocompromised individuals or pregnant women — should contact their doctor or local health department to see if PEP is needed.
“Getting vaccinated against measles continues to be the most important step we can take to protect ourselves and our loved ones,” said NC Health and Human Services Secretary Dev Sangvai. “It is important to check with your health care provider to ensure you are current with all your vaccines.”
North Carolina residents can contact their health care provider or visit their local health department for additional information on ways to obtain the vaccine and schedule an appointment. Children eligible for the Vaccines for Children program may receive the vaccine from a provider enrolled in that program. For more information about measles, please visit dph.ncdhhs.gov/measles.
Measles is a highly contagious, vaccine-preventable disease that is spread by direct person-to-person contact and through the air. The virus can live for up to two hours in the air where the infected person was present. Symptoms of measles usually begin 7-14 days after exposure, but can appear up to 21 days after exposure and may include
• High fever (may spike to more than 104 degrees)
• Cough
• Runny nose
• Red, watery eyes (conjunctivitis)
• Tiny white spots on the inner cheeks, gums and roof of the mouth (Koplik Spots) two to three days after symptoms begin
• A rash that is red, raised, blotchy; usually starts on face, spreads to trunk, arms and legs three to five days after symptoms begin.
With the risk for community spread, parents are encouraged to make sure their children are up to date on all their childhood immunizations, including the measles vaccine. 90% percent of unvaccinated individuals who are exposed to measles will become infected. About one in five people who get measles will be hospitalized. In addition to North Carolina’s case, 1,214 measles cases have been reported in 2025 in 36 other jurisdictions as of June 19, 2025.
Health Plans Take Action to Simplify Prior Authorization

New Commitments Aim to Accelerate Decision Timelines, Increase Transparency, Expand Access to Affordable, Quality Care
Additional reading from HHS, PBS, and others at bottom of this release
(AHIP, 6/23/25 Press Release) -- Health insurance plans today announced a series of commitments to streamline, simplify and reduce prior authorization – a critical safeguard to ensure their members’ care is safe, effective, evidence-based and affordable. Building on health plans’ existing efforts, these new actions are focused on connecting patients more quickly to the care they need while minimizing administrative burdens on providers.
These commitments are being implemented across insurance markets, including for those with Commercial coverage, Medicare Advantage and Medicaid managed care consistent with state and federal regulations, and will benefit 257 million Americans.
For patients, these commitments will result in faster, more direct access to appropriate treatments and medical services with fewer challenges navigating the health system.
For providers, these commitments will streamline prior authorization workflows, allowing for a more efficient and transparent process overall, while ensuring evidence-based care for their patients.
“The health care system remains fragmented and burdened by outdated manual processes, resulting in frustration for patients and providers alike. Health plans are making voluntary commitments to deliver a more seamless patient experience and enable providers to focus on patient care, while also helping to modernize the system,” said AHIP President and CEO Mike Tuffin.
“These measurable commitments – addressing improvements like timeliness, scope and streamlining – mark a meaningful step forward in our work together to create a better system of health,” said Kim Keck, President and CEO, Blue Cross Blue Shield Association. “This is an important foundation to address bigger problems together, at a time when technology and interoperability can deliver real improvements to patient experience.”
Participating health plans commit to:
- Standardizing Electronic Prior Authorization. Participating health plans will work toward implementing common, transparent submissions for electronic prior authorization. This commitment includes the development of standardized data and submission requirements (using FHIR® APIs) that will support seamless, streamlined processes and faster turn-around times. The goal is for the new framework to be operational and available to plans and providers by January 1, 2027.
- Reducing the Scope of Claims Subject to Prior Authorization. Individual plans will commit to specific reductions to medical prior authorization as appropriate for the local market each plan serves, with demonstrated reductions by January 1, 2026.
- Ensuring Continuity of Care When Patients Change Plans. Beginning January 1, 2026, when a patient changes insurance companies during a course of treatment, the new plan will honor existing prior authorizations for benefit-equivalent in-network services as part of a 90-day transition period. This action is designed to help patients avoid delays and maintain continuity of care during insurance transitions.
- Enhancing Communication and Transparency on Determinations. Health plans will provide clear, easy-to-understand explanations of prior authorization determinations, including support for appeals and guidance on next steps. These changes will be operational for fully insured and commercial coverage by January 1, 2026, with a focus on supporting regulatory changes for expansion to additional coverage types.
- Expanding Real-Time Responses. In 2027, at least 80 percent of electronic prior authorization approvals (with all needed clinical documentation) will be answered in real-time. This commitment includes adoption of FHIR® APIs across all markets to further accelerate real-time responses.
- Ensuring Medical Review of Non-Approved Requests. Participating health plans affirm that all non-approved requests based on clinical reasons will continue to be reviewed by medical professionals – a standard already in place. This commitment is in effect now.
“Private-sector collaboration and solution-oriented commitments are critical to improve policy and tackle challenges. With membership spanning the entire healthcare continuum, we appreciate the need to balance appropriate medical management with timely access to care. This announcement from health insurance plans is an important step toward improving the prior authorization process,” said Maria Ghazal, President and CEO of the Healthcare Leadership Council. “We must seize this opportunity to turn these initiatives into real, sustained progress for patients.”
"The National Health Council (NHC) welcomes the commitment of health plans to reform prior authorization practices as an encouraging step toward better access to care. For years, the NHC has called for changes that make the system work easier and better for people living with chronic diseases and disabilities,” said Randall Rutta, NHC’s Chief Executive Officer. “The NHC is a ready partner to AHIP, BCBSA and health plans making these commitments to promote meaningful action that reduces administrative burden, increases transparency and centers on the needs of patients.”
“We are encouraged by this collective commitment to reform prior authorization practices. Physicians have long advocated for reforms that help ensure that patients receive timely, medically necessary care and reduce administrative burden – including the elimination of unnecessary prior authorizations,” said Shawn Martin, Executive Vice President and Chief Executive Officer of the American Academy of Family Physicians. “While this commitment is a step in the right direction, we will ultimately measure its impact by real changes in the day-to-day experiences of patients and the physicians who care for them. We look forward to collaborating with payers to ensure these efforts lead to meaningful and lasting improvements in patient care.”
Progress will be tracked and reported. A full list of participating health plans and additional information are available at: www.ahip.org/supportingpatients and https://www.bcbs.com/ImprovingPA.
Industry Leadership Initiative on Prior Authorization
The undersigned health plans voluntarily commit to six actions to improve prior authorization for patients and providers.
AmeriHealth Caritas
Arkansas Blue Cross and Blue Shield
Blue Cross of Idaho
Blue Cross Blue Shield of Alabama
Blue Cross Blue Shield of Arizona
Blue Cross and Blue Shield of Hawaii
Blue Cross and Blue Shield of Kansas
Blue Cross and Blue Shield of Kansas City
Blue Cross and Blue Shield of Louisiana
Blue Cross Blue Shield of Massachusetts
Blue Cross Blue Shield of Michigan
Blue Cross and Blue Shield of Minnesota
Blue Cross and Blue Shield of Nebraska
Blue Cross and Blue Shield of North Carolina
Blue Cross Blue Shield of North Dakota
Blue Cross & Blue Shield of Rhode Island
Blue Cross Blue Shield of South Carolina
BlueCross BlueShield of Tennessee
Blue Cross Blue Shield of Wyoming
Blue Shield of California
Capital Blue Cross
Capital District Physicians' Health Plan, Inc. (CDPHP)
CareFirst BlueCross BlueShield
Centene
The Cigna Group
CVS Health Aetna
Elevance Health
Excellus Blue Cross Blue Shield
Geisinger Health Plan
GuideWell Mutual Holding Corporation
Health Care Service Corporation
Healthfirst (New York)
Highmark Inc.
Horizon Blue Cross Blue Shield of New Jersey
Humana
Independence Blue Cross
Independent Health
Kaiser Permanente
L.A. Care Health Plan
Molina Healthcare
Neighborhood Health Plan of Rhode Island
Point32Health
Premera Blue Cross
Regence BlueShield, Regence BlueShield of Idaho, Regence BlueCross BlueShield of Oregon, Regence BlueCross BlueShield of Utah, Asuris Northwest Health, BridgeSpan Health
SCAN Health Plan
SummaCare
UnitedHealthcare
Wellmark Blue Cross and Blue Shield
About AHIP
AHIP is the national trade association representing the health insurance industry. AHIP’s members provide health care coverage, services and solutions to more than 200 million Americans. We are committed to market-based solutions and public-private partnerships that make high-quality coverage and care more affordable, accessible and equitable for everyone. Learn more at ahip.org.
About the Blue Cross Blue Shield Association
The Blue Cross and Blue Shield Association is a national federation of 33 independent, community-based and locally operated Blue Cross and Blue Shield companies that collectively provide health care coverage for one in three Americans. For more information on BCBSA and its member companies, please visit bcbs.com.
ADDITIONAL READING
HHS promotes insurer pledge to scale back prior authorization
WATCH: Kennedy, Oz announce insurers’ plan to scale back prior authorizations
Kennedy says health insurers promise to change prior authorization process
Insurance companies vow to fix prior authorization process…again
Prior Authorization Reform Champion Amanda Watson Dies After Long Battle With Breast Cancer
Amanda Watson, mother of two, NCMS Prior Auth Reform Speaker Dies After Cancer Battle
Prior authorization reform champion, Amanda Watson, passed away on June 23, 2025, after a battle with breast cancer. Her physician, NCMS Member Representative Dr. Grant Campbell put out the following statement on social media:
"This wonderful soul and dear friend said cancer will no longer have power over her this morning and is in the arms of our Lord. This mother, wife, daughter, and advocate was a far better speaker for Prior Authorization Reform than me and we promise to keep up the fight to honor you. Rest In Peace Amanda. We love you."
The staff and members of the North Carolina Medical Society are also mourning her loss. NCMS Vice President of Advocacy John Thompson says,
“Amanda’s passion for helping others as they battle a life-threatening disease is an inspiration to all of us at NCMS and to the people of North Carolina. We will always be grateful for her help and will deeply miss our dear friend.”
Additional reading on Amanda Watson:
NCMS Pushes for Prior Authorization Reform with Bipartisan Support from Lawmakers
NCDHHS Director of Mental Health Responds to Elimination of Federal Funding for 988 Suicide Lifeline Dedicated to LGBTQ+ Youth Services
NCDHHS Director of Mental Health, Developmental Disabilities and Substance Use Services on Elimination of Federal Funding for 988 Suicide & Crisis Lifeline Dedicated to LGBTQ+ Youth Services
(NCDHHS, June 20, 2025) -- The United States Department of Health and Human Services recently announced it would eliminate federal funding for the 988 Suicide and Crisis Lifeline service dedicated to LGBTQ+ youth services. On July 17, 2025, people who call 988 will no longer have the option to Press 3, specific to LGBTQ+ youth considering suicide. In response, and to reaffirm North Carolina’s commitment to serving everyone who calls 988 for crisis care, Kelly Crosbie, NCDHHS Director of Mental Health, Developmental Disabilities and Substance Use Services, released the following statement.
"The need for mental health care for young people in North Carolina has never been greater, and we are committed to reaching every person in every community in every corner of our state. North Carolina is a national leader in 988 implementation, with calls being answered in under 14 seconds on average, with every call being answered. This will not end with the elimination of federal dollars to support the 988 option to press 3 for the LGBTQ+ community. More than 8,000 North Carolinians call the 988 Lifeline each month for support. Everyone can and should still call 988, including members of the LGBTQ+ community. Experienced and trained 988 operators will respond to all calls and ensure that people receive the support and resources that they need.
Suicide is the second leading cause of death among young people aged 10 to 14, and a leading cause of death among 15–24-year-olds. LGBTQ+ young people are more than four times as likely to attempt suicide than their peers. In North Carolina, there will always be someone to call, someone to respond and somewhere to go if you are in crisis or just need someone to talk to.
In addition to being a national leader in crisis care, we are working to transform mental health care in North Carolina to build a system that works for everyone and supports people through their mental and behavioral health journey."
UNC Study: Alzheimer's Risk Gene May Disrupt Brain Health

Sarah Cohen’s lab at UNC School of Medicine is studying the impact of the APOE4 protein on brain cells in its search for treatments.
(UNC, Scott Jared) -- A discovery by a UNC School of Medicine cell biology lab could reshape how scientists understand and treat Alzheimer’s disease.
The research team is led by Sarah Cohen, assistant professor in the medical school’s cell biology and physiology department and member of the UNC Lineberger Comprehensive Cancer Center.
Cohen’s lab found that Apolipoprotein E4, a protein long known as the strongest genetic risk factor for late-onset Alzheimer’s, has a surprising effect on certain brain cells.
APOE4 usually works outside the cell, transporting lipids between neurons and support cells. But it can also stick to tiny oil-filled structures called lipid droplets and disrupt the work of astrocytes, star-shaped cells that nourish the brain’s neurons and help maintain brain health.
“It’s causing accumulation of polyunsaturated fatty acids inside lipid droplets,” Cohen said, referring to the types of fats found in foods like fish oil. “We think APOE4 makes the astrocytes more sensitive to stress.”
This effect could explain why APOE4 increases the risk of Alzheimer’s. Understanding whether APOE4 is doing damage inside or outside the cell could be crucial for future drug design. Some companies are trying to develop treatments that reduce APOE levels. “If you have the APOE4 variant, where it’s acting and where it’s bad matters for choosing strategies to get rid of it,” Cohen said.
The work by Cohen’s lab brings new attention to the role of fat metabolism in the brain — an area historically overshadowed by other, higher profile markers of Alzheimer’s. “Lipid accumulation is one of the three hallmarks of the disease, but it’s gotten a lot less attention.”
The lab has mostly researched lipid droplets. With the additional research direction of APOE, the researchers hope to help with finding treatments for neurodegenerative diseases.
Cohen’s interest in APOE’s connections to lipids started when she noticed a University of California, Berkeley, lab study that analyzed all the proteins on the surface of lipid droplets. “APOE came up as a candidate protein,” she said. “That was really intriguing because there was no previous literature about APOE on lipid droplets.”
Initially, Cohen’s team tried to validate APOE’s presence on lipid droplets in liver cells — with no success. But when they turned to astrocytes, where APOE is most abundantly produced in the brain, the protein clearly attached to the lipid droplets. Cohen’s latest study, based on experiments with cultured cells, extends into mouse models of Alzheimer’s in collaboration with Lance Johnson’s lab at the University of Kentucky.
Though the research is in the early stage, its therapeutic implications could be far-reaching. Most Alzheimer’s treatments — including recently approved antibody drugs — target extracellular features like amyloid plaques. These drugs may delay symptoms by several months, but they don’t significantly slow disease progression.
“It’s clear that this treatment alone is not good enough for what patients need,” Cohen said, pointing to the need for new strategies.
Cohen’s lab continues to explore the fundamental biology behind these processes, hoping that the insights might one day refine or even revolutionize treatments for Alzheimer’s disease. “We’re trying to understand what the proteins encoded by these genes normally do, and then what goes wrong when you have a mutation that’s associated with neurodegenerative disease.”
As Cohen’s work reveals, the path to understanding Alzheimer’s may lie in the overlooked fats accumulating inside the brain’s own support cells.
FDA approves new twice-yearly HIV shot. What You and Your Patients Need to know
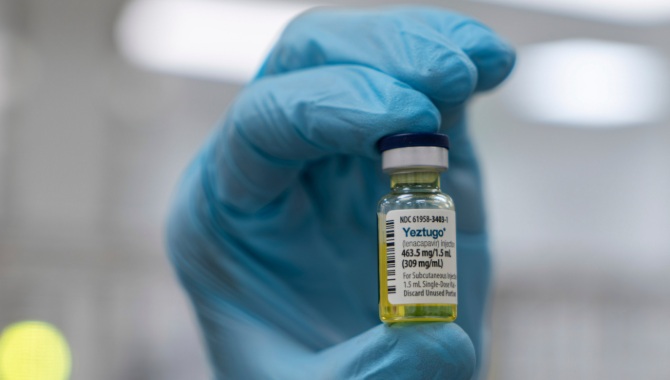
It is expensive, but could it be what your patients are looking for?
(USA Today, Ken Alltucker) -- The Food and Drug Administration has approved Gilead's HIV prevention drug lenacapavir, a twice-a-year injectable medication that clinical trials show prevents new infections.
The drug will be marketed under the name Yeztugo and sell for an annual price of $28,218, or $14,109 per injection. Gilead said the price is comparable to existing HIV prevention drugs and the company will work with insurers to obtain broad coverage of the drug.
Advocates say the long-acting medication is promising because it's more convenient than existing HIV prevention drugs that must be taken daily.
Giving people the option of a twice-a-year injectable is "a game changer, not only for the United States, but around the world," said Carl Schmid, executive director of the HIV+Hepatitis Policy Institute.
Gilead officials lauded the FDA's approval of lenacapavir, which has been studied and developed over nearly two decades.
"We now have a very real opportunity to end the HIV epidemic," said Daniel O'Day, chairman and CEO of Gilead Sciences. "Lenacapavir has shown to be remarkably effective and only needs to be given twice a year, which represents a whole new way of preventing HIV.”
How does lenacapavir compare to other HIV prevention drugs?
Pre-exposure prophylaxis, or PrEP, medications are sold as a daily pill under brand names Truvada and Descovy, as well as generic versions. Another injectable medication, Apretude, is taken every two months after two initial shots taken one month apart.
The overwhelming majority of PrEP users take daily versions, but "it's hard to take a pill every day ... when it's for prevention," said Johanna Mercier, Gilead's chief commercial officer. "So we see adherence levels as low as 50% to 55%," which does not provide adequate protection for at-risk populations.
People are more likely to stay on the medication if they need to take the medication only twice a year rather than daily oral doses, Mercier said.
Dr. Paul Sax, clinical director of the division of infectious diseases at Brigham and Women’s Hospital, said the daily pills and two-month PrEP versions work well for people who consistently take them.
Sax said the twice-a-year shot might appeal to those who aren't willing or able to take a daily pill.
"The key is getting people to take (PrEP) and having them reliably do so," Sax said.
What did the lenacapavir studies show?
In one study of women and adolescent girls in sub-Saharan Africa and Uganda, lenacapavir was 100% effective at preventing HIV infections.
A second study reported the twice-a-year injections lowered the HIV infection rate by 96% in groups of cisgender men and gender-diverse people in the U.S., Argentina, Brazil, Mexico, Peru, South Africa and Thailand.
Schmid said the studies show people are much more likely to take the medication as recommended when it's dosed twice a year compared to daily pills.
"This makes it so much easier and better for adherence and also for people who have other challenges in their life like mental health issues, work or stigma, " Schmid said.
Will insurers cover lenacapavir's cost?
Gilead said the company will work with insurers, health care systems and other payers "with the goal of ensuring broad insurance coverage for Yeztugo."
Out-of-pocket costs for uninsured patients who take Truvada and Descovy, which Gilead also markets, can range from $22,000 to $30,000 a year, according to an analysis by GoodRx, which provides pharmacy drug pricing information.
The U.S. Preventive Services Task Force, an independent advisory panel of national experts that evaluates medical treatments and services, assigned an "A" rating for PrEP medications when prescribed to adolescents and adults at increased risk of HIV.
Under the Affordable Care Act, that means insurers must cover the full costs of the medication as preventive care.
Still, activists say insurers have charged copays or other cost sharing from required lab tests and medical visits. People must test negative for HIV before starting the medication. While on the treatments, they must take routine tests for HIV, other sexually transmitted infections and kidney health.
Sax said insurance coverage of lenacapavir will be key to people getting the drug.
Some insurance companies are more likely to cover generic versions of the daily PrEP pills, and those generics "can be quite inexpensive" compared with the brand versions, Sax said.
More than 1 million new HIV cases a year
Every year, more than 1 million people globally become newly infected with HIV, according to the World Health Organization.
About 10 million worldwide need to take PrEP to meet global HIV prevention goals, WHO said. About 2.5 million take PrEP, WHO said.
More than 39,000 U.S. residents were diagnosed with HIV in 2023, according to the Centers for Disease Control and Prevention. More than 4,700 deaths in 2023 were attributed to HIV, the virus that weakens the immune system and causes AIDS, the CDC said.
A June study estimated as many as 2.2 million Americans could benefit from HIV prevention medications.
Men account for nearly 80% of new cases, mostly involving gay or bisexual men, the CDC said.
Research shows White patients are far more likely to take PrEP than their Black or Latino counterparts, even though White patients are less likely to get infected with HIV.
Geographically, the South accounts for more than half of new HIV cases.
"We hope to reduce those numbers and potentially get to a day when zero infections are reported," Mercier said.
In Memoriam: NCMS Member, Golden Stethoscope Award Winner Dr. Joseph "Joey" Bell
 Dr. Joseph "Joey" Bell Won the 2023 NCMS Golden Stethoscope Award
Dr. Joseph "Joey" Bell Won the 2023 NCMS Golden Stethoscope Award
(Locklear and Son Funeral Home) -- Dr. Joseph “Joey” Tyron Bell, 66, of Robeson County, NC — beloved husband, father, grandfather, son, brother, dedicated physician, and proud member of the Lumbee Tribe — left the loving arms of his family to be welcomed home by his heavenly Father on June 16, 2025 at the Durham VA Hospice Facility. He was born on April 12, 1959 in Laurinburg, NC to James F. “Buddy” Bell and Sarah Sampson Bell. He was the grandson of Furman and Maggie Bell of St. Pauls, NC and Stanley and Eunice Sampson of Pembroke, NC.
Joey was a lifelong advocate for children’s health and well-being. He served his community for decades as a devoted pediatrician, where his kindness, patience, and deep sense of duty left a lasting impact on countless families. Through the years, he attended Harpers Ferry Baptist Church, Pembroke First Baptist Church, and Hyde Park Baptist Church, where he enjoyed leading his small groups. Grounded in faith and culture, Joey was active in both his church and the Lumbee community, mentoring young people and supporting efforts to improve healthcare access in underserved areas.
 He earned his undergraduate degree in Pharmacy from the University of North Carolina at Chapel Hill. In 1986, Joey became the first Lumbee pediatrician and the first American Indian pediatrician in North Carolina as he obtained his medical degree specializing in Pediatrics from the University of North Carolina at Chapel Hill. His career spanned numerous decades, during which he served with distinction as a pediatrician at Carl Albert Indian Hospital, Choctaw Nation Indian Hospital, Robeson Healthcare Corporation, Catawba Indian Health Service Unit, and Children’s Health Pembroke (Pembroke Pediatrics) and was an owner and partner at Children’s Health of Carolina.
He earned his undergraduate degree in Pharmacy from the University of North Carolina at Chapel Hill. In 1986, Joey became the first Lumbee pediatrician and the first American Indian pediatrician in North Carolina as he obtained his medical degree specializing in Pediatrics from the University of North Carolina at Chapel Hill. His career spanned numerous decades, during which he served with distinction as a pediatrician at Carl Albert Indian Hospital, Choctaw Nation Indian Hospital, Robeson Healthcare Corporation, Catawba Indian Health Service Unit, and Children’s Health Pembroke (Pembroke Pediatrics) and was an owner and partner at Children’s Health of Carolina.
Joey was a member of Robeson County Medical Society, North Carolina Medical Society, American Academy of Pediatrics (where he served on the Committee on Native American Child Health), former President of the Association of American Indian Physicians, and the North Carolina Indian Health Board. He was honored throughout his career for his leadership and compassion in medicine, and recently awarded the Order of the Long Leaf Pine by the State of North Carolina.
In addition to his mother, Joey is survived by his loving wife of 36 years, Vicky Cowan Bell; daughter, Victoria “Tori” Bell Alvarado (David); son, Isaac Browning Bell (Peyton); brothers James “Greg” Bell (Bonita) and Ronny Bell (Natalie); several special aunts, uncles, nieces, nephews, and many other extended family members and friends. The joy of his life were his three grandchildren, Elena, Luca, and Rosa Alvarado. He was a steadfast presence in their lives — encouraging, generous, and endlessly devoted to his family.
A public Celebration of Life service will be held on Saturday, July 12, 2025 at Hyde Park Baptist Church in Lumberton, NC. The visitation starts at 11:30 AM and the Celebration of Life service will begin at 1:00 PM. This service will be livestreamed and we will update with the link at a later time. The family appreciates the many expressions of love and support during this time.
We would like to offer a special thank you to the staff of the Durham VA Medical Center for your kindness and compassionate care during our time of need.
In lieu of flowers, memorial contributions may be made to the Dr. Joseph Bell Scholarship Endowment with the UNC School of Medicine at https://go.unc.edu/jtbellendowment
Contributions can also be made to ALS United North Carolina at alsnc.org
Dr. Bell was the recipient of the 2023 NCMS Golden Stethoscope Award. To read the full story of his nomination and win click here.
NCDHHS-DHB Stakeholder Teleconference Scheduled for June 25
NEW WEBINAR SERIES
NC Medicaid Provider Enrollment
NCDHHS-DHB Credentialing Committee Initiative Stakeholder Engagement Session #3
Please join NC AHEC and the North Carolina Department of Health and Human Services (NCDHHS), Division of Health Benefits (DHB), for the third stakeholder teleconference on June 25 from 2-3 p.m. to continue the discussion of a new initiative led in tandem with General Dynamics Information Technology (GDIT). This initiative will establish a Credentialing Committee aimed at maintaining a high-quality, ethical, and competent provider network to support NC Medicaid beneficiaries.
This third forum will offer stakeholders:
- A collaborative forum to discuss the committee’s future role in the provider enrollment and credentialing process to determine compliance of regulatory requirements by NC Medicaid provider applicants.
- A deeper dive into the roles of committee members.
- Status of committee bylaws.
- Review of frequently asked questions and answers pertaining to the development of this project.
These stakeholder engagement sessions will occur monthly, as follows, until the project implementation and are intended to be interactive as the Department values input from partnering stakeholders:
- June 25, 2025
- July 30, 2025
- August 27, 2025
- September 24, 2025
You are encouraged to submit your related questions and comments for targeted open discussion at the meetings to [email protected]. We look forward to connecting with you!
REGISTER HERE
Did you know that all of the materials from the webinar series are archived on ncahec.net? Visit the website to view the recordings, slide decks, and transcripts from Medicaid Managed Care, Advanced Medical Home, and COVID-19 webinars, as well as the Tailored Care Management and Community Health Worker Program learning collaboratives.
NCMS Member Named New State Health Director

NCMS Member Dr. Lawrence Greenblatt Named by NCDHHS as State Health Director
Dr. Lawrence Greenblatt, a distinguished physician, professor and public health champion, has been appointed as State Health Director and Chief Medical Officer for the North Carolina Department of Health and Human Services and will begin his duties on Monday, June 2, 2025. He is widely recognized for his commitment to high-quality care for medically and socially complex patients, his leadership in medical education and his pioneering work to improve mental health and addiction services.
"Dr. Greenblatt is an innovator and public health advocate with a long track record of increasing access to mental and physical health care in North Carolina," said NC Health and Human Services Secretary Dev Sangvai. "He has the vision and experience needed to lead our state’s public health efforts as we work to create a healthier North Carolina for all."
Dr. Greenblatt served for three decades as a general internist, educator and leader in Medicaid policy with Duke University Health System, earning recognition for his work to integrate behavioral health and addiction services into primary care.
Since 2008, Dr. Greenblatt has led Duke’s Medicaid Network, first as Northern Piedmont Community Care, which was part of the statewide Community Care of North Carolina network. He continued as Medical Director of Duke’s Clinically Integrated Network under Medicaid transformation in 2021. This well-run network serves 100,000 Medicaid enrollees and supports dozens of practices.
"I am honored to be chosen for this important role in improving the health and well-being of the more than 11 million North Carolinians that call this great state home," said Dr. Greenblatt. "As a physician and educator, I know the value of making sure every person has access to mental and physical health care when they need it and in the setting that is most appropriate for them."
In 2012, he launched one of the nation’s first academic initiatives to promote safe opioid prescribing and expand treatment for opioid use disorder. He also served as Chair of the NC Medicaid Pharmacy and Therapeutics Committee and Secretary of the NC Medicaid Physician Advisory Group. As a long-time advocate for improved mental health care, Dr. Greenblatt has co-led the Durham Crisis Collaborative and actively contributed to local substance use and mental health planning efforts.
Dr. Greenblatt has been involved with NCMS's leadership programs under the Kanof Institute for Physician Leaders. He is a 2013 Leadership College(LC) graduate and later served as a co-chair of LC, and now co-chair of the renamed program, NCMS Academy for Advanced Healthcare Leaders..
Make Your Plans Now! NCCPRW Joy & Wholeness Summit 2025 is Happening Soon!
NCCPRW Joins the Joy & Wholeness Summit 2025
In every corner of healthcare, there is a growing call for change. A call to prioritize the well-being of the people who care for others, to build systems that support clinicians, and to create a future where physicians and APPs don’t just endure—but flourish.
The North Carolina Clinician and Physician Retention and Well-Being Consortium (NCCPRW) has joined the Joy & Wholeness Summit 2025 as a Platinum Sponsor!
NCCPRW is a driving force in North Carolina, tackling the urgent need for physician and APP retention, well-being, and systemic change. With this sponsorship, they are deepening their impact—bringing North Carolina’s voices, innovations, and solutions to the national stage in Asheville this July.
What This Means for the Future of Clinician Well-Being
- A Spotlight on North Carolina’s Leadership – NCCPRW is strengthening its presence not just regionally, but nationally, ensuring that North Carolina-based initiatives are part of the broader movement for clinician well-being.
- Collaboration That Transcends Borders – With over 200 attendees from more than 100 organizations, this Summit is a gathering place for ideas, strategies, and partnerships that can reshape the future of healthcare.
- A Commitment to Real Change – Attendees will leave with tangible strategies to take back to their organizations, inspired by the collective wisdom in the room.
A Message from The Coalition for Physician & APP Well-Being
“Clinician well-being is not a solitary effort—it’s a shared responsibility. The work being done by NCCPRW to retain, support, and advocate for physicians and APPs aligns so closely with our mission, and we are thrilled to welcome them as a key partner for this year’s Summit. Their presence will help us strengthen the movement for well-being, ensuring that those who care for others receive the support and community they need to thrive.”
— DeAnna Santana, PhD, Executive Director, The Coalition for Physician & APP
Well-BeingA Message from NCCPRW
“Joining the Joy & Wholeness Summit allows NCCPRW to elevate our mission, connect with like-minded organizations, and continue advocating for sustainable solutions in clinician well-being. This partnership represents a shared commitment to creating lasting change for the physicians and APPs we serve.”
— Monecia Thomas, PhD, MHA, Executive Director, NCCPRW
Be Part of the Joy & Wholeness Summit 2025
July 23-25, 2025
Crowne Plaza Asheville, NC
Exclusive Opportunity for North Carolina-Based Attendees: Thanks to NCCPRW’s sponsorship, attendees from North Carolina will have access to an exclusive 15% discount to attend the Summit. Use discount code NC2025.
Surrounded by the breathtaking Blue Ridge Mountains, this is a space designed not just for learning, but for renewal.
This isn’t just another conference. This is an invitation to be part of something bigger.

NC attendees get an exclusive 15% discount with code NC2025
Let’s Make This a Moment That Moves Healthcare Forward
NCCPRW will also be sharing this announcement with their network, ensuring that this message reaches clinicians, healthcare leaders, and organizations who are eager to be part of the conversation. If your organization is looking for meaningful ways to engage in the movement for clinician well-being, we invite you to connect with us.
Together, we are shaping the future of healthcare—one conversation, one partnership, and one bold step forward at a time.
The Coalition for Physician & APP Well-Being
www.bethejoy.org
In Memoriam: NCMS Life Member Dr. Larry T. Burch

Dr. Larry T. Burch, NCMS Life Member Since 1977
(Hinsey-Brown Funeral Service) -- Dr. Larry T. Burch, 91, of New Castle, passed away Monday, May 12, 2025. He was born on November 20, 1933, in Adrian, MI, a son of the late Herbert E. and Lenore (Gould) Burch.
A veteran of the U.S. Navy, Dr. Burch was a medic while serving in the Navy. He received his medical degrees from the University of Michigan. While a general practitioner, he practiced medicine with Dr. Richard Coak in Tecumseh, Michigan and Adrian, Michigan. Later, he did a dual residency in neurology and psychiatry at the University of Michigan. He then headed a Psychiatric Hospital in High Point, NC, and practiced in psychiatry in Winston Salem and Hendersonville, NC. A member of several medical societies, he spent time on several medical missions, including India, Africa, The Orient, Haiti and South America.
In retirement, he enjoyed woodworking and gardening.
He is survived by his wife, Carol (Jones) Coak Burch of New Castle; son, Todd Burch, and another son and daughter; several grandchildren; several nieces and nephews, including a special nephew, David Burch; a sister, Irene Parsons.
In addition to his parents, he was preceded in death by his first wife, Christine, three brothers, Rev. Bruce Burch, Everett Burch and Gene Burch.
A Celebration of Life Mass will be said by Father Bob Sims at 10:00 a.m., Saturday, May 31, 2025, at Immaculate Heart of Mary Catholic Church in Indianapolis, where Dr. Larry and Carol are members. The church address is 5692 Central Ave, Indianapolis 46220. Burial will be at Floral Garden Memorial Park in High Point, NC. Arrangements have been entrusted to Hinsey-Brown Funeral Service in New Castle. Condolences and memories of Dr. Burch may be shared at www.hinsey-brown.com.
Leadership Opportunity: North Carolina Board of Occupational Therapy

The NCMS has an opportunity to appoint a new member to the North Carolina Board of Occupational Therapy. This appointment will fill a term until 6/30/29*.
The commission serves in an advisory capacity on issues relating to the regulation of people offering occupational therapy services to the public. The council also develops and submits a state plan to monitor, review and evaluate such issues and programs.
The North Carolina Board of Occupational Therapy was established by the 1984 session of the N.C. General Assembly. The first Board meeting was held in September 1985 and licenses began being issued in 1986. To learn more about the North Carolina Board of Occupational Therapy, visit their website.
Physicians interested in the North Carolina Board of Occupational Therapy position should complete the application form and return it to Mary Kathryn Kimray, [email protected], by Friday, May 30th.
North Carolina Board of Occupational Therapy Board Meetings
All meetings begin at 9:00 AM
Monday, May 19, 2025
Monday, July 21, 2025
Monday September 15, 2025
Monday, November 17, 2025
Board Meeting Location:
GlenLake One
4140 ParkLake Ave
Raleigh, NC 27612 (4th Floor Conference Room)
*Members of the Board shall serve four-year staggered terms. No member shall serve more than two consecutive four-year terms, unless a member is appointed to fill a vacancy for an unexpired term, then that member may complete the unexpired term and serve one additional four-year term.
Congratulations to the NC Medical Society’s Academy for Future Healthcare Leaders 2025 Graduates!

Raleigh, NC – Eighteen healthcare professional students have completed the NC Medical Society Kanof Institute of Physician Leadership’s Academy for Future Healthcare Leaders.
Each year, the NC Medical Society’s Kanof Institute of Physician Leadership program welcomes healthcare students from academic institutions across NC interested in leadership and professional growth. Interested students are referred and nominated by faculty, mentors, and the alike at their respective colleges to the program.
NCMS Academy for Future Healthcare Leaders (FHL) is a partnership with NC AHEC to provide opportunities of leadership in an interprofessional healthcare environment and networking across institutions. It is a 7-month program designed to build leader identity and master leadership skills including leading teams, communication, and career development.
These esteemed scholars represent health professions such as MDs, DOs, PharmDs, Physician Assistants, etc. and are a class of established and emerging leaders from across the state. Here are the graduates for the 2025 FHL Class.
2025 NCMS Academy for Future Healthcare Leaders Graduates

Visit NCMS Academy for Future Healthcare Leaders (FHL)to view the 2025 Project Presentations.
Want to Improve Your Job Performance? Try a "NASA Nap"

Put down that third cup of coffee, and try to power nap like an astronaut
(Marisa Chen) -- It’s an hour or two after lunch, and you’re fading fast. You’d love nothing more than to snuggle under the covers and take a long, deep sleep, but you’ve got to be awake, alert and on fire for a 4 p.m. Zoom with an important client. Knowing that a long nap will throw you off (and honestly, who has the time?), you just chug down a triple latte and hope for the best.
Instead, do what astronauts and pilots do, and take a NASA nap.
What is a NASA nap?
This short, refreshing catnap doesn’t require drinking Tang or wearing a spacesuit. It simply means taking a nap that’s long enough to boost your performance and alertness, but short enough not to make you groggy and disoriented after you wake. Based on research with long-haul cockpit crews, NASA determined that crew members who took a midday nap of roughly 26 minutes had improved physiological alertness and performance compared with those who didn’t take a nap.
“Most people are carrying some sort of sleep debt — an afternoon nap helps replace some of the sleep that you’re not getting at night,” says Cassie J. Hilditch, Ph.D., senior research associate at the Fatigue Countermeasures Laboratory at San Jose State University. She explains that by keeping your nap to around 20 minutes, “you are less likely to go into the deeper stages of sleep, what we call slow-wave sleep, and you are more likely to stay in the lighter stages.” Hilditch points out that newer research indicates that even 10 minutes of snooze time can make a difference. (One caveat is that if you are truly sleep-deprived, say, after an all-nighter, you may drop into those deep-sleep phases much faster.)
But the key to a successful NASA nap is to wake yourself up before you fall into a deep slumber, including stage 3 and REM sleep, says Terry Cralle, R.D., a certified clinical sleep educator and spokesperson for the Better Sleep Council. “If you get into the deeper stages of sleep, you will get sleep inertia, which is that grogginess you feel when you wake up,” she explains. “The research is very robust on the benefits of short naps,” Cralle adds. “But I think in our culture, which has long looked at needing sleep as a weakness or lack of ambition, we've substituted our intake of excessive caffeine for naps.”
Benefits of a NASA Nap
“We’ve tested different tasks that tap into different cognitive functions, and sleep seems to improve pretty much all of them,” says Hilditch. “If you're getting 10 to 20 minutes of sleep, it can boost your feelings of alertness, but also your objective performance,” she says. Some specific ways a nap helps:
Improves performance.
A 2021 review found that a short daytime map improved cognitive performance, with the benefit lasting around two hours after waking. Physical performance improves, too: In studies with athletes, researchers have found that an afternoon nap leads to faster sprint times, better grip strength, and quicker reaction times, as well as better mood.
Increases alertness.
A nap is so helpful for staying awake and alert that the National Transportation Safety Board recommends pulling over and taking a 20-minute nap if you feel drowsy while driving. In fact, one recent study showed that people who habitually take an afternoon nap are consistently more alert in the afternoon than those who don’t usually nap, even on days they skip the nap, suggesting that napping has a cumulative effect.
Boosts memory.
A nap is so helpful for staying awake and alert that the National Transportation Safety Board recommends pulling over and taking a 20-minute nap if you feel drowsy while driving. In fact, one recent study showed that people who habitually take an afternoon nap are consistently more alert in the afternoon than those who don’t usually nap, even on days they skip the nap, suggesting that napping has a cumulative effect.
Increases creative thinking.
You know how your mind wanders in the moments before you fall asleep? That nodding-off-into-nap time can spark some creative ideas: Researchers at Harvard and MIT found that subjects who napped for 45 minutes scored higher in creative tasks such as story-telling after their nap than those who were kept awake during the same period.
___________________________________________________________
How does a short nap do all this? In addition to restoring energy reserves, there are complex activities going on in your brain while you snooze. “There’s emerging evidence that while you sleep, the byproducts of being awake are flushed from the brain,” says Hilditch. She adds that the critical process of synaptic pruning occurs during sleep. “You’re not actually building new connections among the synapses,” she explains. “It’s more of a reorganization: Sleep reinforces important connections by downplaying the ones that are less important.”
How to take a NASA nap
Obviously, you’ll find it easier to take a quick, refreshing midday nap if you work from home (or perhaps in a mattress store?). But even if you work in an office or other place that generally frowns on anyone curling up in a corner, there are ways to achieve this, says Cralle. “Talk to your supervisor about the all-round benefits of naps, and ask if it’s possible to carve out space in an empty office or break room, where people can take turns going in for 30-minute naps,” she suggests. (Consider sharing this article so they can see how allowing short naps will actually boost work efficiency.) Then, whether you are at a workspace, in your car or at home in the living room, follow these nap hygiene tips:
- If you can’t actually lie down, sit back comfortably
- Use an eye mask to block out light
- Set your watch or phone to wake you after 20 minutes (or 26, if you want to do the full NASA time)
- Use earphones or buds to play calming music or white noise
- Make sure you’re not overheated—it’s easier to sleep in a cooler space
Hilditch adds that it’s important to time your nap so you have at least 20 minutes to recover post-snooze before doing anything important (or dangerous, like driving or operating machinery). “Anytime you're waking up, you could feel like you have some sleep inertia symptoms, so it's always best to leave a buffer period,” she says.
Finally, remember that as helpful as these naps are, they are mainly used to make up for sleep you’re not getting at night. “If you're really tired during the day and need a nap, take a moment to think about how you can improve your nighttime sleep,” Hilditch says. “But if you do need that nap, then you know, this is the way to make the most efficient use of your time.”
New Research: Class of HIV Drugs May Protect Against Alzheimer's Disease

(aidsmap, Zekerie Redzheb) -- A cohort of people with HIV who took NRTIs (a class of HIV drugs) as part of HIV treatment showed lower rates of Alzheimer’s disease than people without HIV. The team of American researchers behind this study published in the journal of Pharmaceuticals suspect HIV-like sequences in our genome to be associated with the disease and thus these HIV drugs protect against its development.
In our genome there is a significant amount of virus-like DNA sequences (estimated at 8% of its length). They are believed to be an evolutionary leftover from previous pandemics. Once integrated in our genome, they are hard to eliminate, as is HIV DNA, therefore our immune system chose a different approach – ‘block, cripple and lock’. Because of this, most of these sequences are seriously damaged and cannot produce intact viruses but can still produce some viral proteins, including a couple of reverse transcriptase (RT) enzymes, thought to be unique to only two groups of viruses, one of which includes HIV.
Up to recently, it was thought that humans should not and cannot have such enzymes, since its function is to convert RNA back into DNA – a largely risky and unnecessary process for non-viral organisms since it is prone to errors. Therefore, the discovery of an RT gene in human genomes is attributed to past HIV-like infections.
Research suggests these RT enzymes may be still able to introduce random genetic recombinations and amplifications (increasing the copy number of certain harmful genes) in the brain cells causing them to produce dysfunctional proteins that clump up and harm the brains of people with Alzheimer’s disease.
Nucleoside reverse transcriptase inhibitors (NRTIs) are a class of drugs that block HIV’s RT enzyme. Since HIV’s RT is similar to the RTs produced in our cells, these same drugs may have the potential to block them too, possibly protecting against Alzheimer’s disease.
The study
The researchers collected data on three cohorts of people – those with HIV taking NRTIs; those with HIV either on an NRTI-free regimen or off treatment; and a third cohort who were not living with HIV nor taking NRTIs. They followed up each cohort for two years and nine months to see whether NRTIs reduced the rate of Alzheimer’s.
The data came from a large number of people, which reduces the likelihood of these findings being a chance event. Over 46,000 people were included in the cohort of those with HIV on NRTI-containing regimens. There were 33,000 people in the cohort of people with HIV not taking NRTIs and 151,000 people in the cohort without HIV and not taking NRTIs.
Only participants above 60 years of age and without a previous diagnosis of Alzheimer’s disease were included.
The median age in the first two cohorts was similar at 64 and 65 years, while the third cohort – without HIV and not taking NRTIs – was slightly older at 69 years. Over two-thirds of the participants in the first two cohorts were men, while in the third cohort two-thirds were women. Both age and sex can affect Alzheimer’s risk and since the first two cohorts and the third one had differing age and sex profiles, the researchers had to adjust for that in the analysis when deriving their final results.
Alzheimer’s rates per cohort
During the two years and nine months of follow-up, the rate of developing Alzheimer’s was lowest in the first cohort – people with HIV on an NRTI-containing regimen. In this cohort only 2.46 in 1000 people developed Alzheimer's disease.
In the second cohort of those with HIV either on an NRTI-free regimen or off treatment the rate of Alzheimer’s was higher compared to the first cohort, but still lower than the third cohort of those without HIV. However, the difference between this cohort and those without HIV became insignificant when age and sex were added to the analysis. In this cohort the rate of Alzheimer’s was 3.55 in 1000 people.
The third cohort had the highest rate of Alzheimer’s at 6.15 in 1000 people.
Interestingly, a further analysis of the first cohort revealed an increased rate of Alzheimer’s in those taking protease inhibitors (another class of HIV drugs) alongside their NRTIs. However, the difference was not statistically significant and it would be early to make any conclusions.
Concluding thoughts
Although previous research has linked different viruses and virus-like elements to Alzheimer’s disease – be it directly or indirectly (as a contributing factor) – the condition is multifactorial. Certainly, some viruses and inflammatory conditions have the potential to contribute to the development of the disease. However, genetic, lifestyle and other environmental factors cannot be ruled out.
While NRTIs seem to decrease Alzheimer’s risk, the mechanism may be different from the one proposed in this study. Some NRTIs can suppress the inflammasome (the inflammation complex in the body), which can indirectly protect the brain.
Last but not least, this was a retrospective study (one that collects data on the past medical records of people). Besides, it has a set of limitations such as a relatively short follow-up period and non-ideal match between cohorts with regards to age and sex. Randomised controlled studies would be required to get a more definitive answer to whether NRTIs protect against Alzheimer’s disease in people without HIV.
Chow T et al. Nucleoside Reverse Transcriptase Inhibitor Exposure Is Associated with Lower Alzheimer’s Disease Risk: A Retrospective Cohort Proof-of-Concept Study. Pharmaceuticals 17: 408, 2024 (open-access).
Nucleoside reverse transcriptase inhibitors (NRTIs) are a class of antiretroviral drugs used to treat HIV and other viral infections. They are often combined with other medications in HAART (Highly Active Antiretroviral Therapy) to suppress the virus and prevent the development of AIDS.
Here's a list of commonly used NRTIs:
-
- Abacavir: (Ziagen)
- Emtricitabine: (Emtriva)
- Lamivudine: (Epivir)
- Tenofovir alafenamide: (Vemlidy)
- Tenofovir disoproxil fumarate: (Viread)
- Zidovudine: (Retrovir)
New Study: Exercise May be Secret Weapon Against Cancer Treatment Negative Effects

New Study Finds Physical Activity May Mitigate Some Side Effects of Cancer Treatment
(NICE NEWS) -- There’s no doubt exercise is good for your heart, bones, balance, and brain. And a new study found that physical activity can also mitigate some side effects of cancer treatment, such as brain fog and heart and nerve damage.
While prior research has shown that exercise can be generally helpful during cancer treatment, this study went a step further and systematically analyzed data from randomized controlled trial results published between 2012 and 2024. The takeaway: Exercise (e.g., tai chi, yoga, high-intensity and interval training) not only reduced adverse effects often associated with cancer and its treatment, but also improved psychological well-being, body composition, and overall quality of life.
“In conclusion, this study reinforces the efficacy of incorporating exercise into cancer treatment protocols,” the researchers wrote. Of course, every cancer patient has their own journey and circumstances, so there’s no one-size-fits-all workout plan.
“It’s important to take things at your own pace and do activities that are right for you,” Celene Doherty, a specialist cancer information nurse at Cancer Research U.K., who was not involved with the study, told The Guardian. She added that patients interested in learning more should speak to their doctors and care team.
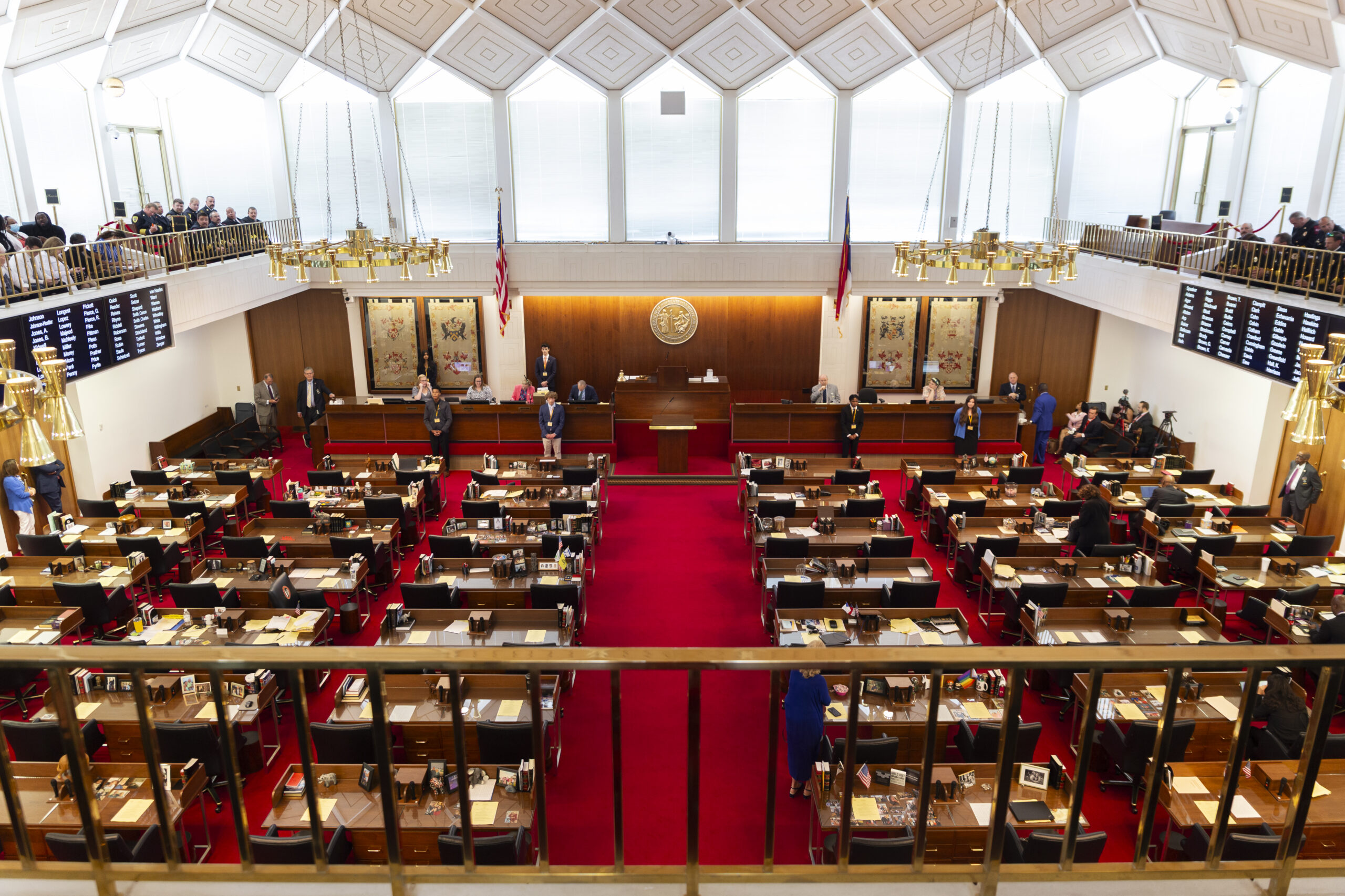
NCMS 2025 White Coat Day Was Huge Success (And A Lot of Fun)!

A Great 2025 White Coat Day That Ended with the NC House Passing HB434!
April 3o, 2025, was a big day for the North Carolina Medical Society! Sixty-five members (and a few future members) joined together to share a unified voice at the North Carolina General Assembly. More than 90 meetings were held with lawmakers on issues important to all North Carolinians. In the end, the group cheered as HB 434 passed the NC House. The CARE FIRST Act is being championed by the NCMS as a way to reform prior authorization in the state. You can read more about it here.
Of course, it is always better to have more voices!
If you are not a member we would love to have you! If you are a member, forward this to your non-member friends! The NCMS is ready to take you on your next step in protecting the profession of medicine and in caring for North Carolinians. CLICK HERE TO JOIN TODAY!
Enjoy these photos of the North Carolina Medical Society 2025 White Coat Day!
2025 NCMS White Coat Day Ends With Huge Win for CARE FIRST Act!

2025 NCMS White Coat Day Ends With Huge Win for CARE FIRST Act!
This CARE FIRST Act passed the house in a 109-1 vote on April 29, 2025, the culmination of years of work by the North Carolina Medical Society staff and members. The announcement came at the end of the 2025 White Coat Day which was attended by more than 65 NCMS members.
The annual white coat day is a a chance for members of the NCMS to learn more about the legislative process and to put that knowledge into action at the NC General Assembly. More than 90 meetings were held with senators and representatives from across the state.
 “(It) was a great day to be a member of the North Carolina Medical Society. Our members advocated for patients across the state when they met with legislators to discuss ways to keep North Carolinians healthy and safe. NCMS has been urging members of the General Assembly to pass the CARE FIRST Act (HB 434)—a piece of legislation that reforms the prior authorization process—and we were pleased to see the House pass it during White Coat Day.” -- NCMS Interim CEO Steve Keene
“(It) was a great day to be a member of the North Carolina Medical Society. Our members advocated for patients across the state when they met with legislators to discuss ways to keep North Carolinians healthy and safe. NCMS has been urging members of the General Assembly to pass the CARE FIRST Act (HB 434)—a piece of legislation that reforms the prior authorization process—and we were pleased to see the House pass it during White Coat Day.” -- NCMS Interim CEO Steve Keene
NCMS thanks the House of Representatives for their support of this essential legislation, especially the bill's primary sponsors. The CARE FIRST Act now heads to the Senate for consideration and is likely to be conferenced between the two chambers.
With the wellbeing of North Carolinians and their physicians at the top of its list of priorities, the North Carolina Medical Society supports House Bill 434, The CARE FIRST Act, which would reform the process of patients seeking prior authorization from their health insurance provider. NCMS firmly believes that physicians should be the ones to make medical decisions for their patients and health insurance companies should take responsibility for the outcome of denied medically necessary care.
-
Set minimum clinical standards for provision of care.
-
Consult with the patient’s physician before refusing to cover medical care.
-
Set time frames and make timely decisions based on treatment urgency.
-
Promote continuity of care for patients.
-
Set limits on retrospective denials.
-
Hold health insurance companies responsible for the outcome of denied care.
 “The physicians and medical professionals NCMS represent have told us prior authorization reform will make healthcare more efficient and effective,” said NCMS VP of Advocacy John Thompson. “We are thrilled to see (Wednesday's) success and will continue to advocate for NC’s patients and medical professionals at the General Assembly.”
“The physicians and medical professionals NCMS represent have told us prior authorization reform will make healthcare more efficient and effective,” said NCMS VP of Advocacy John Thompson. “We are thrilled to see (Wednesday's) success and will continue to advocate for NC’s patients and medical professionals at the General Assembly.”
Here are some photos from White Coat Day. Look for more in future editions of Morning Rounds.
Metrolina Nephrology Associates Honored with Healthcare Innovation's 2025 Innovator Award

Charlotte, N.C. — April 29, 2025 — Interwell Health is proud to celebrate our partner, Metrolina Nephrology Associates, on being named a recipient of Healthcare Innovation’s 2025 Innovator Awards. This national recognition honors standout teams that are driving meaningful change in healthcare. Metrolina was honored for its groundbreaking work in value-based kidney care.
Metrolina is known for its proven record of tracking performance metrics and driving quality outcomes for patients. To expand its impact and enhance patient outcomes further, Metrolina partnered with Interwell Health to form the Charlotte Kidney Contracting Entity (KCE) and participate in the CMS Kidney Care Choices (KCC) model—a value-based initiative aimed at improving care for patients with chronic kidney disease and reducing costs by delaying the need for dialysis and incentivizing transplants.
“This award is more than recognition for nephrology innovation—it highlights a scalable, patient-centric care model that can be applied to other specialties to improve chronic disease management and a more sustainable healthcare future,” said Bobby Sepucha, CEO of Interwell Health. “We’re proud to support Metrolina in delivering high-quality, value-based kidney care.”
Metrolina's success was driven by three core strategies: leveraging data-driven insights to identify at-risk patients, expanding care coordination through interdisciplinary teams, and improving key quality measures such as optimal dialysis starts and depression screening rates.
"This work is about much more than hitting performance metrics—it's about fundamentally improving the lives of people living with kidney disease,” said Dr. Carl Fisher, President, Metrolina Nephrology Associates. “Value-based care allows us to intervene earlier, personalize care, and help our patients lead better, healthier lives.”
"We are proud of the strides we’ve made in improving kidney health and the quality of life for our patients and their families,” said Jennifer Huneycutt, CPA, CMPE, Executive Director of Metrolina Nephrology Associates. “Collaborating with Interwell Health has allowed us to proactively identify at-risk patients and provide personalized, coordinated care. This recognition underscores our commitment to delivering better outcomes through innovation and partnership, and we look forward to building on this success in the future.”
At a time when value-based care models are being carefully evaluated and refined for long-term viability, Metrolina’s partnership with Interwell Health offers a replicable blueprint for achieving better patient outcomes, reducing costs, and supporting sustainable care. To read a case study about this partnership, visit here.
To learn more about Healthcare Innovation’s Innovator Awards program and learn about the other winners, visit here.
About Interwell Health
As a leading provider of value-based kidney care, Interwell Health is on a mission to reimagine healthcare to help patients live their best lives. Interwell is setting the standard for the industry by producing sustainable savings and driving exceptional quality results at unmatched scale. The company leverages a two-pronged approach that includes total patient care and provider enablement to serve patients with chronic kidney disease (CKD) from stage 3 to kidney failure. In partnership with more than 2,200 nephrologists, the Interwell interdisciplinary care team leverages advanced machine learning algorithms to personalize care for patients in all 50 states and Puerto Rico. To learn more, visit interwellhealth.com.
About Metrolina Nephrology Associates
Metrolina Nephrology Associates is the region's most recognized and independent nephrology group in the Charlotte, North Carolina region, providing comprehensive care to patients with kidney disease The practice has been on the forefront of the treatment and management of kidney disease for more than 40 years. Composed of 40 Nephrologists and 41 Nephrology Advanced Practitioners, Metrolina serves patients from seven convenient locations. Its extensive network of physicians and offices allows the practice to deliver care in an atmosphere that is personal, caring, and compassionate.
Congratulations to NCMS member Dr. Christine Khandelwal on election to Federation of State Medical Boards' BOD
Congratulations to North Carolina Medical Society member Christine M. Khandelwal, DO for her election to the Board of Directors of the Federation of State Medical Boards. Dr. Khandelwal is a 2024 NCMS Golden Stethoscope Award winner.

She is a former North Carolina Medical Board Member and Past NCMB President.
Dr. Khandelwal was selected, from a field of eight candidates on April 26 during the FSMB House of Delegates meeting in Seattle, to one of three available At-Large seats on the FSMB Board. She will serve a three year term. FSMB is a national nonprofit organization representing all medical boards within the United States and its territories that license and discipline allopathic and osteopathic physicians and, in some jurisdictions, other health care professionals.
Dr. Khandelwal is a Professor of Family Medicine and Director of Geriatrics and Palliative Medicine with the Campbell University School of Osteopathic Medicine. She is Boarded in both Geriatrics and Hospice and Palliative Medicine, serving in Harnett County within the Cape Fear Valley Hospital System. Dr. Khandelwal rotated off of NCMB in October 2024, following six years of service, including a term as Board President in 2023-2024.
2025 White Coat Day Kicks Off With Huge Group Heading to General Assembly!

NCMS 2025 White Coat Day Attendees Block Traffic on Person St. Heading to General Assembly!
The North Carolina Medical Society 2025 White Coat Day is one of the biggest events of the year! This year, 65 physicians, PAs, residents, and students met at the NCMS headquarters on Person St. in Raleigh for a day of meetings with lawmakers.
The day began with a short orientation and breakfast and then the group gathered for an awesome photo on the steps of the NCMS. Then all 65 headed to meet senators and representatives to discuss the issues important to NCMS members.
The focus is HB 434, the CARE FIRST Act and HB 514, the Team-Based Care Act.
HB 434 is a life-saving piece of legislation that will allow physicians to make medical decision for their patients by reforming prior authorization.
If passed, HB 514 would create risks and reduce patient safety by eliminating physician involvement and further prevent access for rural and underserved patient communities.
For more information on HB 434 click here.
For more information on HB 514 click here.
Look for more coverage of White Coat Day including the Legislative Reception in future Morning Rounds!
Plan Now for Professional Development in 2026!

Add Your Face to This Group in 2026!
The time is now to plan for next year! As you begin your budgeting, do you or members of your group want to take the next step in a leadership journey? Make sure you put a line item in your 2026 budget for the North Carolina Medical Society Professional Development programs.
The NCMS offers 2 healthcare leadership programs:

The NCMS Academy for Advanced Healthcare Leaders is an 8-month, project-based leadership development program tailored for practicing physicians, PAs, medical residents, and healthcare administrators.
The program focuses on enhancing leadership abilities by fostering meaningful connections, improving team dynamics, and driving change through individual initiatives.
Participants work on projects of interest using their leadership abilities to prepare for leadership roles within their workplace environments, local medical societies, specialty associations, and NCMS.
For more information on NCMS Advanced Healthcare Leaders click here.
The NCMS Academy for Executive Healthcare Leaders is a 9-month leadership development program designed to prepare healthcare leaders for executive-level roles within their organization, professional community, and beyond.
The program pairs a deeper understanding and awareness of one’s leadership abilities—gained through a comprehensive 360° leadership assessment and a personalized 1:1 executive coaching session—with an individual experiential change initiative project.
For more information on NCMS Academy for Executive Healthcare Leaders click here.
Each program provides a unique leadership journey that is tailored to meet the needs of healthcare professionals at various stages in their careers. Ideally, we encourage newer/mid-career leaders and residents to enroll in the NCMS Academy for Advanced Healthcare Leaders (AHL) and more senior level healthcare clinicians and administrators to enroll in the NCMS Academy for Executive Healthcare Leaders (EHL). Both programs offer a distinctive curriculum that can support the leadership needs of healthcare professionals.
Click here for more information on all NCMS Professional Growth programs
If you have questions, please email Monecia Thomas at [email protected]
Let Your Patients Know! NCDHHS Distributing Free Fans Starting May 1

Operation Fan Heat Relief Distributing Fans to Eligible Recipients May 1 – Oct. 31
RALEIGH - The North Carolina Department of Health and Human Services’ Division of Aging is partnering with North Carolina area agencies on aging and local service providers to distribute fans statewide to eligible recipients through the Operation Fan Heat Relief program from May 1 – Oct. 31, 2025.
People aged 60 and older, as well as adults with disabilities, are eligible to sign up for assistance from May 1 – Oct. 31, 2025, with local service providers across the state.
Since 1986, the relief program has purchased fans for older adults and adults with disabilities, providing them with a more comfortable living environment and reducing heat-related illnesses. Last year, the NCDHHS Division of Aging received $86,000 in donations, allowing for the distribution of 3,670 fans and 35 air conditioners in 94 North Carolina counties.
Donations from Duke Energy Carolinas, Duke Energy Progress and Dominion allow regional area agencies on aging and local provider agencies to purchase fans for eligible individuals. Local provider agencies can also purchase a limited number of air conditioners for individuals with specific health conditions.
Keeping cool is important because older individuals with chronic medical conditions are less likely to sense and respond to changes in temperature, and they may be taking medications that worsen the impact of extreme heat. Operation Fan Heat Relief helps vulnerable adults at risk for heat-related illnesses stay safe during the summer.
In addition to applying for fans, people can take the following steps during high temperatures:
- Increase fluid intake
- Spend time in cool or air-conditioned environments regularly
- Reduce strenuous activity during the afternoon
- Speak with a physician before summer about how to stay safe while taking medication that can affect the body's ability to cool itself (e.g., high blood pressure medications)
Individuals may contact their area agency on aging or the NCDHHS Division of Aging at 919-855-3400 for additional details.
More information about Operation Fan Heat Relief, including tips on preparing for extreme heat and a list of local agencies distributing fans, is available at on the NCDHHS Operation Fan Heat Relief webpage.
White Coat Day is Wednesday! NCMS Has A Big Announcement on Prior Authorization!
The North Carolina Medical Society's White Coat Day is just two days away! This Wednesday, physicians and PAs from across the state will come together to demonstrate the medical community’s united stance on reforming prior authorization. It will be a pivotal moment as the NCMS Prior Authorization Bill is presented on the House floor.
Stay tuned throughout the day for updates on how NCMS and its members are advocating to improve healthcare for all North Carolinians.
Delayed care, higher costs: the prior authorization crisis.
Our current prior authorization is neither effective nor efficient, leading to weeks or even months of delayed care as patients wait on health insurers—in some cases even leading to patient death.
Physicians and patients across North Carolina agree: our healthcare can’t wait. Join our campaign to reform an unnecessary system that harms patients.
Take Action Now
What is prior authorization?
According to the American Medical Association, prior authorization (sometimes called preauthorization or precertification) is a health plan cost-control process by which physicians and other health care providers must obtain advance approval from a health plan before a specific service is delivered to the patient to qualify for payment coverage.
Delays in care have human and financial costs.
When insurers say “no” to care that physicians and patients have already agreed on in order to protect their own budgets, it leads to costly and dangerous delays that have real impacts on patients’ ability to receive high-quality treatment and may leave them on the hook for thousands or even tens of thousands of dollars in unexpected medical debt.
The Frustrating Prior Authorization Process
What are the real costs of delay?
- $1.8 billion+ annual cost to the healthcare system
- 575+ hours per year spent by physicians on paperwork instead of helping patients
- $2,000+ average higher costs to patients when care is denied
Delays lead to worse health outcomes, and sometimes the death of a patient.
After diagnosing a NC man with treatable bile duct cancer, the physician ordered a standard treatment for this patient. One week later, the insurance company requested a peer-to-peer meeting to discuss the treatment plan. Despite the standard-of-care plan, the insurance company stated that the prescribed regimen was not on its treatment algorithm and would not be approved.
The physician continued submitting three different care plans and had multiple peer-to–peer conversations with the insurer. Each standard care plan was denied by the patient’s insurance. This back-and-forth process took over one month, during which the patient received no care for his aggressive cancer. As a result, the patient’s condition worsened to the point that he was no longer eligible for treatment and had no options remaining besides end-of-life care.

So how do we reform the system?
- Minimum standards for clinical review criteria
- Physician consultation requirements during clinical reviews
- Timely decision requirements during initial reviews and appeals
- Continuity of care provisions to ensure patients don’t go without treatment
- Limits on retrospective denials on treatment that has already occurred
- Transparent plan language that helps patients and physicians understand what is and isn’t covered
NC AHEC Offering Free Clinical Precepting Courses Online

Clinical Precepting Online Series
FREE ONLINE COURSES
These courses are geared to an interprofessional audience of clinical preceptors who work with students, residents, or other advanced learners who are completing academic or program requirements in a clinical environment. Participants may complete any combination of courses.
Faculty:
- Lisa Johnston, PT, MS, DPT, DCE, Professor;
- Brenda O Mitchell, Ph D, CCC-SLP, Clinical Assist Professor;
- Laurie A Ray, MPT, PhD, Consultant; Kathryn L Sorensen, OTD, OTR/L, ADAC, Assistant Clinical Professor;
- Charlene Williams, PharmD, BCACP, CDCES, Clinical Associate Professor
Available Courses:
- Clinical Precepting 101: The Role of the Clinical Preceptor, Host Clinical Site, and Legal Considerations; 2.0 Contact Hours
- Clinical Precepting 102: Planning for and Providing Clinical Learning Experiences; 1.50 Contact Hours
- Clinical Precepting 103: Communication, Learner Self-Assessment and Preceptor Feedback; 1.50 Contact Hours
- Clinical Precepting 104: Managing Difficult Situations in the Clinical Learning Environment; 1.5 Contact Hours
- Clinical Precepting 105: Inclusive Precepting Practices; 1.0 Contact Hours
- Clinical Precepting 106: Disability Inclusion; 1.0 Contact Hours
CLICK HERE FOR MORE INFORMATION AND TO REGISTER
NC Institute of Medicine Hosting Task Force on Veterans' Health

The North Carolina Institute of Medicine invites you to join us for a gathering to kick off the start of a task force on Veterans' health!
REGISTER HERE!
Thursday, May 22 – 2:00 – 5:00 PM
Chapel Hill Post 6 – American Legion
3700 NC Highway 54 West, Chapel Hill, North Carolina 27516
** This event has no registration fee.**
The task force will identify actions to improve the access and experience of care in community-based health care settings for those who have served in the military, their families, and caregivers. With support from the North Carolina Department of Health and Human Services Division of Mental Health, Developmental Disabilities, and Substance Use Services and NC AARP, NCIOM will be convening the task force from Summer 2025 to Spring 2026. A final report with task force recommendations will be published by Fall 2026.
Visit the task force website HERE.
At the event you will have an opportunity to:
- Hear about what NCIOM has learned in preparation for the task force
- Learn about the goals and objectives of the task force
- Share your perspectives on Veterans' health care
- Hear from some of the people who serve Veterans across the state
- Connect with others who are dedicated to serving North Carolina's Veterans, their families, and caregivers
We hope that you can join us to begin this year-long effort with a spirit of strong collaboration and energy! Please feel free to share this invitation with anyone you know who may be interested.
While we value and appreciate your attendance at this gathering, please note that attendance does not guarantee selection for task force membership. Task force members will be selected based on a variety of factors to ensure a diverse and balanced representation of perspectives and expertise.
Would you like to honor a Veteran in your life? We will be displaying pictures and stories of Veterans at the kick-off event. You can submit a photo and story using this easy form HERE.
More about the North Carolina Institute of Medicine:
The North Carolina Institute of Medicine (NCIOM) is an independent organization focused on improving the health and well-being of North Carolinians by providing analysis on the health and well-being of North Carolinians, identifying solutions to the health issues facing our state, building consensus toward evidence-based solutions, and informing health policy at the state and local level. One of the ways that we do our work is through task forces – convening stakeholder groups to identify evidence-based strategies to improve health and inform health policy.
***Previous NCIOM work related to Veterans’ health***
- North Carolina Medical Journal – Armed Services and Veteran Family Health in North Carolina (November/December 2023 Issue)
- Suicide Prevention and Intervention Plan: A Report of the NCIOM Task Force on Suicide Prevention and Intervention (2012)
- Honoring Their Service: A Report of the North Carolina Institute of Medicine Task Force on Behavioral Health Services for the Military and Their Families (2011)
Nearly Half of U.S. Gets Failing Grades for Air

Some NC cities rank high, but that could be changing.
(Axios, Alex Fitzpatrick) -- Nearly half of Americans are now exposed to potentially dangerous levels of air pollution, per a new report.
Why it matters: The findings, which predate the current Trump administration, come as the White House is reconsidering EPA rules and regulations meant to curb pollution and promote cleaner air.
Driving the news: Just over 156 million Americans — 46% of the population — are living in areas with unhealthy levels of ozone or particle pollution, per the American Lung Association's 2025 State of the Air report.
- That's almost 25 million more compared to last year's report, and the highest number in the past decade of the report's history.
Between the lines: Extreme heat, wildfires and drought are degrading air quality nationwide, the Lung Association says. All have been linked to climate change.
- Air pollution is associated with an array of health conditions, from wheezing and coughing to asthma and premature death.
How it works: The report uses local air quality data to grade and rank locations based on ozone pollution, daily particle pollution and annual particle pollution.
- This latest report includes data from 2021-2023, "the most recent three years of quality-assured nationwide air pollution data publicly available."
- Ozone is a gas that, at ground level, is a harmful irritant. Particle pollution involves tiny airborne particles from wildfires, fossil fuel burning and more.
Zoom in: Los Angeles, Visalia and Bakersfield — all in California — lead the Lung Association's new rankings of U.S. metros most affected by ozone pollution.
- Bakersfield; Fairbanks, Alaska, and Eugene, Oregon, topped the list of those most affected by daily particle pollution.
- Bakersfield; Visalia and Fresno, California, were the most affected by annual particle pollution.
Stunning stat: Hispanic people are almost three times more likely than white people to live somewhere with failing grades in all three categories.
The other side: Only one continental U.S. metro — Bangor, Maine — showed up on all three of the group's lists of cleanest cities.
The intrigue: The "geographic distribution of air pollution" shifted eastward towards the end of the covered period, the report notes.
- "The year 2023 ... brought improved conditions to the West Coast but also a deadly heat wave in Texas and an unprecedented blanket of smoke from wildfires in Canada that drove levels of ozone and particle pollution in dozens of central and eastern states higher than they have been in many years."
What they're saying: "Clearly, we need to do more to control the pollutants that are impacting our changing climate and worsening the factors that go into the wildfires and the extreme heat events that are threatening our health, instead of thinking about how to roll them back," says Katherine Pruitt, senior director of nationwide clean air policy at the American Lung Association and report author.
"I’m as Mad as Hell and I’m Not Going to Take This Anymore!” One Doctor's Thoughts on Prior Authorization
With thanks to Dr. David N. Korones and JAMA Neurology
"I’m as Mad as Hell and I’m Not Going to Take This Anymore!”
So shouted news broadcaster Howard Beale in the iconic 1976 film “Network” as he decried pollution, unemployment, inflation, crime, and all that was wrong in the world back then. And so shouted I, as I slammed down the phone after yet another denial from an insurance company—this time denial of treatment for an 8-year-old little girl with a brain tumor.
She is a happy, high-energy girl who showed only the slightest and most innocent of symptoms. Although these subtle changes did not slow her down in the slightest, it was enough to warrant additional investigation.
Her physician ordered a magnetic resonance imaging scan, and to his surprise, she had a large inoperable brain tumor. Fortunately, a biopsy showed it was a low-grade glioma, a treatable, potentially curable tumor. These days we can get a complete profile of the genetic makeup of children’s tumors, and that profile revealed a mutation in her tumor indicating that an oral US Food and Drug Administration (FDA)–approved drug could be effective. Such drugs (often referred to as targeted therapy) are an increasingly used option for children with cancer, and certainly an attractive option for this young girl. The other choice for treatment, the previously established standard, was a year of weekly intravenous chemotherapy. Her parents and I talked long and hard about these options. I explained that chemotherapy is the standard, but targeted therapy is showing promising results with less adverse effects and is rapidly evolving as a new and more humane standard. Not surprisingly her parents were quick to say “we’ll take the pill,” and the young patient promptly started pill training, enthusiastically honing her pill-swallowing skills with Tic Tacs (Ferrero Group).
“Denied,” the insurance company said in so many words when the prescription for targeted therapy was sent to them for review and approval. They went on to explain in their terse letter of denial that the drug is not FDA approved for this specific indication. The letter was not signed by a human being and provided only a phone number with a tangled algorithm of menu options. I did what we so often do when patients are denied a drug or service that we feel they should have, I asked for an urgent (72-hour) appeal. I wrote a letter outlining the rationale for the targeted therapy option and provided references, with data to support that this approach is not voodoo or magic. It really works! We got another anonymous communication that there is no 72-hour appeal, and we will have to wait the standard 30 days. That is a long time to wait when you have a brain tumor. At this point, I also wrote a letter that I did not send, a letter that served as an outlet for my vitriol, filled with many words I would not want my 8-year-old patient to see. It hangs in our nurses’ office, a testament to the daily frustrations we face getting pediatric patients with cancer the medical care they need.
Although that second letter was a necessary catharsis and a feel-good moment, there were more frustrations to follow. I called in an attempt to reverse their decision to wait 30 days to make a decision, requesting an
expedited review. After 30 minutes of pressing 5, then 3, then 8, then 1, and hearing polite and agonizingly slow moving voice messages, I finally reached a human being, who very kindly told me that I am in the wrong department and needed to call the HELP number on the family’s insurance card. So, I called the family, got the number, and started anew, again a morass of phone menus mixed with interminably long holds, and multiple transfers, each new person (or menu) asking for the same information about my patient. Finally, I reached a human being who told me they don’t have anything on record about my patient and couldn’t help me.
My options were 2-fold: I could go outside and scream as Howard Beale did in Network in 1976, “I’m as mad as hell and I’m not going to take this anymore!” or I could call my congressman. I did both. My congressman sent me to a NY State Assemblywoman with expertise in health insurance snafus. She, in turn, put me in touch with an insurance-government liaison, who connected me with one of the insurance company co-executives who arranged the emergency appeal I was hoping for. The next day an independent, non–insurance affiliated pediatric neuro-oncologist called me and listened to my patient’s story. He immediately replied that this is a sound approach to therapy, and he would recommend approval. The following day, the medication was approved.
I wish this was a stand-alone story, but it is not. Every day the phone, email, and text messages mount: an antinausea medication is not approved, oral chemotherapy is denied to a child because it is in liquid form, and only tablets are approved, brain surgery is denied because the patient has the misfortune of not living in the same state as the neurosurgeon who has the unique skill set to remove it, an insurance company that had
previously approved an essential therapy for one of my patients now, for inexplicable reasons, denies refills half way through her prescribed course of treatment.
If we must make these dreadful calls for approvals of drugs and services, I wish it was as simple as calling a number at an insurance company and having a conversation. But it is not. Denials come on letters without names or contact information, a situation I fear now will only become worse. If a phone number appears, we clinicians take a deep breath, because we know it will be a long call, much of which is spent on hold. If we talk to a human being, they are often kind, but they do not share their last name or other department, and all my identifying information is needed again. My call today was “only” 33 minutes. I made out an invoice while I waited and sent them a bill, charging them $350 per hour for my time ($192.50). I do this from time to time, and not surprisingly, I’ve never received a response or a payment for the time I could be spending taking care of patients. But like the vitriolic letter I wrote, at least it provides some release for my mounting frustration.
I believe there is a method to these denials of services. Denial letters are anonymous, making it hard and time-consuming for us to push back. It is a system designed to rob us of time and to plunge us into a byzantine world of rules and regulations that we do not understand. It is designed to minimize human interaction and takeaway the heart that should be a part of good medical care. It is designed to wear us down, so that we say “screw it ,I’ll just try something they’ll approve.” Something cheaper.
I, for one, am still “mad as hell and I’m not going to take this anymore.” Perhaps the more we push back, send them bills for our time, follow that up with bill collectors, call our congressional representatives, and summon our hospital leadership, we can gather a chorus of physicians, patients, hospital leaders, and politicians who all open their windows and, following Howard Beale’s lead, scream in unison that they, too, are mad as hell, and it is long past time to change this unjust system of care. To paraphrase Howard Beale, “our children, our patients are human beings, goddammit, their lives have value!”
Published Online: April 21, 2025.
doi:10.1001/jamaneurol.2025.0782
Conflict of Interest Disclosures: None reported.
Additional Contributions: We thank the patient’s
parents for granting permission to publish this
information.
1. Lumet S. Network film transcript. Accessed
March 18, 2025. https://sfy.ru/?script=network
NC State Health Plan Clear Pricing Project Update
NC State Health Plan Clear Pricing Project Update
Please Complete Survey at Bottom
The State Health Plan (Plan) would like to extend its sincere gratitude to the providers that have supported the Clear Pricing Project (CPP) by being a part of the N.C. State Health Plan Network.
The Plan is facing a $507 million deficit which we are actively trying to close. This means evaluating all programs, like CPP, to determine the best way to stabilize the Plan’s financials.
When CPP launched in 2020, the intention was to promote transparent health care pricing, while trying to promote quality primary care and behavioral health. CPP introduced provider reimbursement rates based on a percentage of Medicare with incenting members to visit participating providers by reducing their copay down to zero. Given that most of the providers that signed up for CPP received an increase in reimbursement rates coupled with members having no cost-share, this model has not proven to be financially viable for the Plan.
Given the current financial situation of the Plan, we must find other solutions that benefits all three parties: the Plan, members and providers. As such, the Plan will be ending CPP in its current form as of December 31, 2025.
The Plan is committed to continuing its effort in promoting affordable access to behavioral health services through reimbursement rates and member cost-share; however, it will not be at the current CPP reimbursement rate and will not have a $0 member cost share.
While the Plan does need to cut costs, we are not willing to compromise on improving member health and recognize this is a balancing act, therefore we are reaching out to the provider community for feedback so we can partner together on something more sustainable for all parties.
Please complete this brief survey by April 25, 2025.
CLICK HERE FOR SURVEY
Is a Blood Test for Postpartum Depression on the Horizon?

Fewer than 10 percent of women seek medical help for postpartum depression
(Sara Novak) -- Postpartum depression is the most common complication of childbirth, affecting about 1 in 7 women after delivery. It causes bouts of severe depression and anxiety, makes bonding with a newborn especially difficult, and can lead to thoughts of self-harm. Suicide is a leading cause of maternal death in the United States.
Yet, only about 6% of women with postpartum depression seek medical help. Shame, stigma, and lack of awareness can delay or deter diagnosis, causing long-term effects on both mother and child.
But a simple blood test that could predict the condition before symptoms appear is offering new hope – hinting at a future where treatments could shift from response to prevention.
The Value of a Predictive Test for Postpartum Depression
Research paving the way for the blood test has been piling up for a decade. Scientists have identified epigenetic biomarkers (indicators in our DNA that reflect changes in how genes are expressed) that can predict postpartum depression with 80% accuracy in the third trimester of pregnancy, according to a 2020 study in the journal Psychiatry Research.
These biomarkers were able to predict postpartum depression in women with a history of depression and in those who, at the time of the test, didn't show any signs of depression, according to results from several studies. If these findings can be used to create a standardized blood test, then high-risk patients would be able to seek treatment before symptoms occur, said Lauren Osborne, MD, second author of the 2020 study and vice chair of clinical research in the Department of Obstetrics and Gynecology at Weill Cornell Medicine in New York City.
Such a test "would alert the clinical care team to the potential risk," helping guide early and targeted intervention and bringing the power of precision medicine to psychiatry, said Jamie Maguire, PhD, a professor of neuroscience at Tufts University School of Medicine in Boston. (Maguire did not take part in the study.)
It could also go a long way toward ending stigma, said Jennifer Payne, MD, a professor at the University of Virginia and an expert in reproductive psychiatry. A blood biomarker provides an objective measure and a biological cause, highlighting the condition as a medical issue that needs treatment.
Two studies led by Payne and Osborne – one local, already underway, and one national, planned for the summer – will explore the test's potential. If they are successful, the test could become available in as little as a few years.
Research suggests there are at least two forms of postpartum depression, each responding to different treatments, said Payne. One is more likely to happen in women with a history of depression, while the other, described as "hormone-dependent," affects patients with no previous mental health issues. The latter is more likely to respond to hormone-based medications.
How Existing Treatments Could Work With a Blood Test
Treatment for postpartum depression typically uses medication along with therapy.
For patients with a history of depression or anxiety, continuing or resuming medications through pregnancy can be an option. Many common antidepressants – including citalopram (Celexa), escitalopram (Lexapro), fluoxetine (Prozac), and sertraline (Zoloft) – are often prescribed during pregnancy and generally considered safe, with benefits largely outweighing the risks to both mom and baby.
Patients with hormone-dependent postpartum depression have a dedicated drug treatment: In 2023, the FDA approved zuranolone (Zurzuvae) for postpartum depression. The drug contains neuroactive hormones that help improve mood regulation.
With a biomarker test, patients with positive results could start the two-week zuranolone treatment in the hospital after giving birth, said Morgan U. Patterson, MD, director of the Perinatal Mood and Anxiety Disorders Program at the University of North Carolina School of Medicine.
Psychotherapy, especially interpersonal therapy and cognitive behavioral therapy (CBT), can give patients better coping tools and help moms identify and change negative thought patterns.
"Therapy can help normalize a mother's experience, help her to process her emotions, and address any possible reproductive trauma," said Marilyn Cross Coleman, a therapist, perinatal treatment specialist, and owner of Shameless Mama Wellness in California. Trauma caused by a serious birth complication that endangers either the mother or child can increase the risk of postpartum depression.
In some cases, group therapy is especially effective. Many women suffer in silence due to feelings of shame, and sharing their experience with other moms helps them know they're not alone.
A biomarker test could lead pregnant people to seek mental health support early, which is crucial because finding care can take months, Osborne said.
How to Lower Your Risk of Postpartum Depression
Another huge thing that helps with postpartum depression is also hard for most new moms to come by: sleep.
Research shows that sleep disturbances put women at a higher risk of postpartum depression. A nightly four- to five-hour block of uninterrupted sleep can effectively stave off symptoms, according to a 2024 study.
That's not easy to achieve with newborns. Hiring a "night nurse" – a caregiver who watches the baby overnight – could help, though at $40-$50 per hour, it's cost-prohibitive for many new parents. You can ask friends and family to contribute through baby nurse registries. Payne also recommends accepting offers from friends and family to help with night feedings, relying on the proverbial village for help.
Have a plan to prevent or treat postpartum depression, Cross Coleman said, because the longer symptoms fester, the more serious the condition can become. "A mother's environment and support network will play a large part in her recovery," she said.
🎉It's New Member Monday!🎉 Say Hello to These New Members or the NCMS!

The NCMS is excited to welcome these new members!
We are thrilled to have you!
Michael A. Abdou, MD
Temitope E. Adebayo, MD
Amanda M. Allen, MD
Bailey C. Allen, MD
Levi A. Almond, PA
Aubrey E. Barker, MD
Cordell R. Beaton, DO
Shannon C. Blake, PA
Yaroslav D. Bodnar, MD
Hannah Boutros-Khoury, MD
Kelly P. Bowers, PA-C
Alexandra L. Chatterton, PA-C
Kendall L. Clark, PA
Tyia S. Clark, MD
Krishna K. Darji, PA-C
Alexis Dubiel
Lillian J. Dubiel, MD
Kate G. Farber, MD
Richard L. Ford, MD
Sarah C. Heminger, PA-C
Megan F. Hoppens, MD
Thomas W. Jenkins, PA-C
Brenna A. Keane, DO
Booker T. King, MD
Lunsford R. King, Jr., MD
Thomas J. Knackstedt, MD
Wafa A. Latif, MD
Jason E. Lee, MD
Julie E. N. Lindsey, MD
Anthony L. Lledo Torres, MD, MPH
Riddhi Mehta, PA-C
Katherine A. Miller, MD
Heather N. Moore, PA
Ward J. Myers, MD
Alvin L. Nguyen, DO
Kevin O. Nyabera, MD
Luther M. Richey, MD
Shiela Marie C. Romanick
Not a member?
Want to be?
Joining is simple.
Visit our membership center here.
What do you get for your NCMS dues dollars?
From advocacy to practice solutions, your membership has its advantages.
The NCMS employs a team of legislative, regulatory, and payer experts who closely monitor and respond to the latest developments that impact the profession of medicine and the care of patients. LEARN MORE...
Take advantage of leadership development opportunities through our award-winning Kanof Institute for Physician Leadership (KIPL) programs such as the NCMS Academy for FUTURE Healthcare Leaders, the NCMS Academy of ADVANCED Healthcare Leaders, and the NCMS Academy of EXECUTIVE Healthcare Leaders. LEARN MORE...
From special rates to specialized insurance options for yourself or your practice, take a look at your options. LEARN MORE...
Plan for your future with these retirement solutions. LEARN MORE...
The Community Practitioner Program (CPP) and CPP 2.0 offer loan repayment for practicing in rural or under-served areas. LEARN MORE...
Gain access to resources designed to improve the health and well-being of healthcare professionals. LEARN MORE...
Receive our daily Morning Rounds e-newsletter to stay up-to-date on all the issues impacting medicine.
Get the latest legislative developments happening at the state and national level delivered to your inbox with our Political Pulse video series, as well as breaking Advocacy Alerts.
Events and Networking Opportunities
Throughout the year we host a number of NCMS Socials, Town Halls, and Regional Meetings across the state to get members together for fun and to learn how to make North Carolina the healthiest state in the country!
NCMS and NCCHCA Hosting 'The Courage to Rebuild: A Fundraiser to Honor the Resilience of WNC Health Centers'

The NCMS is excited to announce we are joining NCCHCA to honor health centers of Western North Carolina
Join us as we come together to honor and support our Western North Carolina health centers as they recover from the devastating effects of Hurricane Helene. In the long road to recovery, the highest need is financial support to rebuild, restock, and offer new services to meet needs of their communities. Our goal is to raise $500,000 to support Western North Carolina community health centers. We thank those who have already donated and contributed to that goal, and are grateful for the continuing support.
The event is at the Umstead Hotel and Spa in Cary on April 23rd
There are several ways you can be involved:
Cant attend? Click here to donate directly to the Helene Recovery Fund

This fundraiser will be taking place at the beautiful Umstead Resort and Spa, located at 100 Woodland Pond Drive, Cary, NC 27513.
We will be located in the Ballroom for the fundraiser, so be sure to utilize the west entrance as opposed to the main entrance to lead you more directly to our space.
Parking is valet, and complimentary. You may give your keys to the valet upon your arrival before entering the event space.
In the Cary area, you have many choices for where to stay.
The Umstead Hotel and Spa - Host Site
Please note: The room block for The Umstead has closed, but you may make independent reservations
Other nearby options include:
Embassy Suites (Raleigh-Durham Airport) (3 minutes from Umstead)
Hilton Garden Inn (Raleigh-Durham Airport) (7 minutes from Umstead)
Sonesta Select (Raleigh-Durham Airport) (8 minutes from Umstead)
TownePlace Suites (Raleigh-Durham Airport/Morrisville) (12 minutes from Umstead)
Now Open: NHSC Scholarship Program

Accepting applications through Thursday, May 8 at 7:30 p.m. ET.
The National Health Service Corps (NHSC) Scholarship Program awards scholarships to students pursuing eligible primary care health professions training. In return, you commit to providing primary care health services in a Health Professional Shortage Area for a minimum of two years or a maximum of four years of full-time service.
What does the scholarship cover?
- Tuition and eligible fees
- Items including books, health insurance, and equipment
CLICK HERE TO LEARN MORE AND APPLY
You must meet all eligibility requirements:
- A U.S. Citizen (U.S. born or naturalized) or U.S. naturalized.
- Enrolled as a full-time student (or accepted for enrollment).
- Attending - or accepted to attend - an accredited school or program in one of the 50 states, the District of Columbia, or a U.S. territory.
- In an eligible discipline: physician, dentist, nurse practitioner, nurse midwife, or physician assistant.
- Eligible for federal employment.
- Without an existing service obligation.
Save the Date!
NHSC Scholarship Application Assistance Webinar
Wednesday, April 2 from 2:00 - 3:30 p.m. ET
New Security Feature: To start your application, you will sign in or set up an account in My BHW. My BHW requires multifactor authentication (MFA), which adds an extra layer of protection to your account and reduces the risk of fraud.
With MFA, you must use Google Authenticator on your mobile phone or tablet each time you log in. Follow the Quick Start Guide to set up your authentication.
NCDHHS: New Primary Care Physicians Initiative Loan Repayment Program
Placement Services Program
DHHS Division/Office issuing this notice: Office of Rural Health
Date of this notice: April 2, 2025
Applications will be accepted beginning April 21, 2025 at 8:00 a.m.
NEW Primary Care Physicians Initiative: Loan Repayment Program
NC DHHS: Medical, Dental, and Psychiatric Recruitment Opportunities for Providers
The Office of Rural Health (ORH) offers qualifying physicians, with educational (student) loan debt, incentive payments to repay their loans tax-free through the Primary Care Physicians Initiative (NC PCPI). With the passage of Session Law 2023-134, incentive payments are awarded to eligible physicians in exchange for providing comprehensive primary care services in outpatient settings at eligible sites serving those with the highest need located within Tier 1 and Tier 2 of the North Carolina’s County Distress Rankings (Tiers).
Funding is limited and the awards will be based on a first-come, first-served basis for eligible and complete applications. ORH anticipates up to 16 awards in each of the six Medicaid Regions. The application portal will not accept more than 20 applications per Medicaid Region.
Applicants are strongly encouraged to review these guidelines carefully and gather necessary documentation so that when the application portal opens on April 21, 2025, at 8:00 am, applicants will be prepared to complete the on-line application in its entirety.
Click here for full details, eligibility, awards and commitments
Crowd Gathers for First NCMS Social and Regional Meeting in New Bern!

The first NCMS Social and Regional Meeting in New Bern Draws Crowd of Local Clinicians!
NEW BERN -- The North Carolina Medical Society (NCMS) hosted a Social and Regional Meeting in New Bern on Tuesday evening, bringing together a dynamic group of area clinicians to learn more about the NCMS mission, activities, and member opportunities.
NCMS Board members Dr. Tracy Eskra and Dr. Claude Jarrett led an engaging presentation, making the event both informative and enjoyable!
Toni Hill, the NCMS Director of Membership and Engagement says, "Our first visit to beautiful New Bern was an unforgettable experience! We were thrilled to meet the dedicated professionals in the region and spend an evening connecting, socializing, and learning about the incredible work NCMS does for its members. The NCMS team truly enjoyed engaging with guests, exploring ways to support them in their work—because that’s exactly why NCMS exists! I want the rest of the state to know that these meetings are more than just gatherings—they’re opportunities to share stories, explore solutions, and help NCMS grow even stronger!"
The next NCMS Regional Meeting is in Asheville on May 22. Click here to register.
Don't forget about the NCMS White Coat Day and Legislative Reception on April 30. Click here to register.
Attorney General Jeff Jackson Sues Federal Government Over Cuts in NC Healthcare Funding

Last week, the U.S. Department of Health and Human Services told several states, including North Carolina, that it was terminating $11 billion in health care funding.
(WITN Web Team) -- North Carolina Attorney General Jeff Jackson has filed a lawsuit against the federal government over hundreds of millions of dollars in healthcare funding cuts.
Last week, the U.S. Department of Health and Human Services told several states, including North Carolina, that it was terminating $11 billion in health care funding.
Jackson says the cuts, which include over $230 million to North Carolina, are unlawful and that the funds were congressionally appropriated.
Jackson is filing the lawsuit jointly with dozens of other state attorneys general.
Jackson listed several items he says would suffer because of the cuts:
- Local health programs in at least 77 of North Carolina’s 86 health departments, particularly in North Carolina’s rural counties.
- Community-based organizations and community health workers who have been providing care and resources to people impacted by Hurricane Helene in western North Carolina.
- County-based nurses who investigate disease outbreaks.
- Collection and analysis of infection control data, which is critical for humans as well as North Carolina’s farming economy and livestock industry.
- EMS programs in six counties (Davie, Durham, Gaston, Surry, Orange, and Cumberland counties).
- Response to outbreaks of infectious disease in high-risk places like nursing homes and assisted living facilities, where North Carolina’s older population is at risk.
- Effective control and prevention of the spread of infections, like the flu. North Carolina just experienced its worst flu season in 15 years, leading to more than 382 deaths.
- Substance use disorder treatment programs, especially in rural areas, and the loss of behavioral health therapists and substance use treatment specialists who are critical to North Carolina’s fight against the addiction crisis.
- Collegiate substance misuse recovery programs that operate in 14 North Carolina colleges and universities (Appalachian State University, Elizabeth City State University, East Carolina University, Fayetteville State University, North Carolina A&T State University, NC State University, North Carolina Central University, UNC Asheville, UNC Charlotte, UNC-Chapel Hill, UNC Greensboro, UNC Pembroke, UNC Wilmington, and Winston-Salem State University).
2025 Match Data Shows Increase in Primary Care

National Resident Matching Program Releases the 2025 Main Residency Match Results, Celebrates the Next Generation of Physicians
The National Resident Matching Program® (NRMP®) proudly announces the results of the 2025 Main Residency Match® (“the Match”), the largest in its 73-year history. A total of 52,498 applicants registered for the Match, an increase of 2,085 (4.1 percent) over last year, and 47,208 of those applicants submitted a certified a rank order list (“active applicant”). This year’s active applicant pool competed for 43,237 positions, an increase of 1,734 (4.2 percent) from 2024. Today at 12:00 pm ET, matched applicants learned where they will begin their medical training.
“This year’s Main Residency Match marks a milestone of continued success for the graduate medical education community as a record number of applicants and residency training programs matched,” said NRMP President and CEO Donna L. Lamb, DHSc, MBA, BSN. “The NRMP continues to be a service that welcomes all who wish to participate, capably advocating for and supporting the aspirations of young physicians and the priorities of residency training programs to collectively address the varied heath needs of communities across the nation.”
Record Breaking Program Participation. This year the NRMP welcomed two new specialties to the Match; Public Health and Preventive Medicine and Occupational and Environmental Medicine. All told, the 2025 Main Residency Match included 6,626 certified program tracks, an all-time high and increase of 231 programs over last year. Of the 43,237 training positions offered, 94.3 percent (40,764) filled when the matching algorithm was processed.
Multiple Application Service Providers. In response to the changing landscape of graduate medical education, the 2025 transition to residency cycle included for the first time multiple application services for applicants to secure residency positions. The NRMP played a pivotal role in fostering collaboration among application service providers, namely working to streamline processes, improve transparency, and fortify data integrity for a more efficient transition experience for applicants.
Performance in the Match. As the primary source of data on physician matriculation into the national pipeline, the NRMP informs constituents, health policy experts, and stakeholders within and outside the medical education community about trends, noting changes over time in match rates among distinct applicant groups, program fill rates, and applicant interest in specialties.
For the 2025 Main Residency Match:
I. Applicant Participation and Match Rates. Among all registrants, 47,208 applicants certified a rank order list of program preferences, an increase of 2,355 or 5.3 percent over last year. Of the applicants who certified a rank order list, 37,667 matched to either a categorical or preliminary (both post graduate year-1 or ‘PGY-1’) position, an increase of 1,683 (4.7 percent) from 2024.
- There were 8,392 active Osteopathic (DO) seniors in the 2025 Main Residency Match, an increase of 4.5 percent over last year. DO seniors achieved a 92.6 percent PGY-1 match rate, an all-time high, and an increase of 0.3 percentage points. DO senior PGY-1 match rates have grown 3.5 percentage points since 2021.
- U.S. MD seniors are the largest applicant type in the Match with 20,368 active applicants. At 93.5 percent, their PGY-1 match rate remained unchanged from last year, despite an increase of 3.1 percent (613) in active applicants. The U.S. MD senior PGY-1 match rate remains within the 92 – 95 percent range that has been steady since 1982.
- There were 4,587 active U.S. citizen international medical graduates (IMGs) in the Match, a decline of 3.5 percent, with a PGY-1 match rate of 67.8 percent, which represents a 0.8 percentage point increase over last year.
- Non-U.S. citizen IMGs saw a large increase in participation this year with 11,465 active applicants, up 14.4 percent over 2024. The marked increase in participation served to push the PGY-1 match rate down but only slightly, 0.5 of a percentage point, to 58.0 percent.
II. Primary Care Positions Continue to Increase. The NRMP routinely reports on the primary care specialties that provide the full training required for board certification in Family Medicine, Internal Medicine, Internal Medicine-Pediatrics, and Pediatrics.
This year’s Match saw continued strength in filling primary care specialties, with 20,300 categorical positions offered, an increase of 877 positions over last year and a new high. Overall, primary care specialties earned a 93.5 percent fill rate.
- Internal Medicine increased the positions placed in the Match by 679 to 11,750, a 6.1 percent increase over 2024. The specialty filled 11,379 positions, up 7.6 percentage points, giving them a fill rate of 96.8 percent.
- Last year, the fill rate for Pediatrics declined from 97.1 to 91.8 percent. This year, Pediatrics offered 3,193 categorical and primary positions, an increase of 54 from 2024, and filled 3,043 for a 95.3 percent fill rate.
- Family Medicine saw a lower fill rate this year, filling 85.0 percent of their 5,357 positions compared to 87.8 percent last year, largely due to the increase of 144 positions placed in the Match.
III. Renewed Interest in Emergency Medicine. In 2025, Emergency Medicine offered 3,068 positions, an increase of 42 positions from 2024, and achieved a 97.9 percent fill rate, an increase of 2.4 percentage points. The specialty had experienced a decline, with an 81.8 percent fill rate in 2023 before climbing back up to a 95.5 percent fill rate in 2024. This year’s performance edges Emergency Medicine even closer to its pre-Covid fill rate of 98 to 99 percent. There were 3,003 applicants who matched to the specialty, a rebound from 2023 which saw 2,456 applicants obtaining PGY-1 positions. The increase in matched applicants to Emergency Medicine is due primarily to increases in DO seniors and IMGs matching to the specialty.
IV. OB-GYN Remains Competitive. Obstetrics and Gynecology continues to be a specialty of interest as national conversations about reproductive healthcare persist in light of the Dobbs v. Jackson Women’s Health Organization Supreme Court decision in 2023. Despite the changing policy landscape, interest in the specialty remains strong. In the 2025 Main Residency Match, only one categorical position and nine preliminary PGY-1 positions remained unfilled out of 1,604 Obstetrics and Gynecology residency positions offered. MD Seniors accounted for 69.4 percent of those who matched, while DO Seniors accounted for 19.6 percent, up from 18.9 percent in 2024. International medical graduates accounted for 6.0 percent of matched applicants in the specialty.
V. Applicant Impact on Specialty Fill Rate. Data also can be examined to assess how various applicant groups impact specialty fill rates, offering a glimpse into shifts and changes in the landscape over time of applicant and specialty preference.
Of note this year:
- U.S. DO seniors increased the percent of positions filled in several specialties including categorical Child Neurology (4.9 percentage point increase), Medicine-Pediatrics (2.9 percentage point increase), and Orthopedic Surgery (1.3 percentage point increase).
- U.S. MD seniors saw increases in the percent of positions filled in a few specialties including categorical Radiation Oncology (16.7 percentage point increase), Anesthesiology (1.8 percentage point increase), and Psychiatry (1.5 percentage point increase).
- Non-U.S. citizen IMGs saw increases in primary care, filling 33.3 percent of categorical Internal Medicine positions (a 1.9 percentage point increase), 20.4 percent of categorical Pediatrics positions (a 2.0 percentage point increase), and 17.6 percent of Family Medicine positions (a 2.2 percentage point increase).
Supplemental Offer and Acceptance Program® (SOAP®). The NRMP’s Match Week Supplemental Offer and Acceptance Program (SOAP) affords eligible applicants who did not match to a residency position the opportunity to try to obtain positions that went unfilled after the matching algorithm was processed. A total of 2,521 positions were placed in SOAP, including positions in programs that did not participate in the algorithm phase of the Match. The number of available positions in SOAP represents a decline of 54 positions (2.1 percentage points) compared to last year, despite an increased number of positions in the Match, a further indication of the success of the NRMP’s Matching Program for placement of young physicians in training programs.
Detailed SOAP results will be available in the Results and Data: 2025 Main Residency Match Report, which is published in the Spring.
New Study: Shingles Vaccine May Protect Against Dementia

It’s been shown that reactivation of the chickenpox virus can lead to the accumulation of aberrant proteins associated with Alzheimer’s.
(NBC News, Linda Carroll) -- Getting vaccinated against shingles — a painful and debilitating condition that can flare up years after infection from varicella zoster — not only lowers the risk of infection, but may also offer some protection against dementia, a provocative new study suggests.
The new research, published Wednesday in Nature, analyzed data from more than 280,000 older adults in Wales and found that people who received the original shingles live virus vaccine were 20% less likely to develop dementia of any type than those who were not vaccinated.
Previous research has found an association between the Shingrix shingles vaccine, which replaced the live virus version in 2020, and a lower risk of dementia, especially in women. But that link wasn't considered as strong because that study design couldn’t account for potential differences between those who were vaccinated and those who were not, such as the possibility that the vaccinated people might have been healthier overall. Shingrex, which targets a tiny bit of viral DNA, turned out to have a longer lasting effect than the original vaccine.
The new study was possible because of an unusual public health policy in Wales that provided a “natural experiment” to explore the potential impact of the vaccine on dementia risk. With the rollout of the vaccine on Sept. 1, 2013, in Wales, shots were offered to people who were 79 on that date but not given to people who had turned 80.
That allowed the German and Stanford University researchers to compare two groups of people with similar health characteristics who differed only by one week in age, making them essentially the same except that the vaccine was available to the younger population but not the older, said Dr. Pascal Geldsetzer, an assistant professor of medicine at Stanford University and senior author of the study.
What’s exciting about the study is that it’s essentially like a randomized controlled trial, considered the gold standard in research, he said.
The way the original vaccine was rolled out in Wales provided a unique opportunity, said Allison Aiello, a professor of epidemiology at the Columbia University Aging Center in New York City.
“It’s like having a control group compared to a treated group,” said Aiello, who was not associated with the new research. “What’s interesting is the finding of 20% protection. That is a pretty strong effect, which does fit with other research suggesting that herpes viruses might have an influence on dementia.”
Scientists don’t know exactly how the chickenpox virus raises the risk of dementia. It’s been shown that reactivation of the virus can lead to the accumulation of aberrant proteins associated with Alzheimer’s, for example, Geldsetzer said. It’s also possible that the virus might spark a reactivation of herpes simplex, which earlier research has linked to dementia.
Herpes viruses never completely go away, but instead lurk in the body until the immune system weakens. Aging leads to a natural weakening of the immune system that can allow the virus to resurface as shingles, a nasty side effect of chickenpox.
The age effect is why the shingles vaccine has been offered only to people ages 50 and older in the U.S. It's given as two doses, two to six months apart.
Herpes viruses, including oral and genital herpes simplex, appear to have the ability to get into the central nervous system, experts said.
In fact, a 2024 study found that among 70-year-olds without dementia at the outset, older adults with a herpes simplex diagnosis were more than twice as likely as uninfected people to develop dementia over a 15-year follow-up.
Herpes simplex can wreak havoc if it passes through the blood-brain barrier. It can cause inflammation of both the meninges (meningitis) and the brain (encephalitis). Both can be fatal.
Bolstering the case for the shingles vaccine protecting against dementia were the findings from a study published in Nature Medicine in 2024 that analyzed medical records from more than 100,000 patients. That analysis suggested the newer shingles vaccine was associated with even better protection against dementia.
In that study, researchers also investigated whether two other vaccines — for influenza and tetanus, diphtheria and pertussis — had any impact on the risk for dementia. They did not.
The most important take-home message from the Stanford study is that getting vaccinated might lower the risk for dementia, said Dr. Aarati Didwania, a professor of medicine and medical education at Northwestern University’s Feinberg School of Medicine in Chicago.
Exactly how the vaccines might protect against dementia isn’t clear, Didwania said. “But it’s an intriguing question,” she added. “Is it by decreasing inflammation or preventing the virus from reactivating?”
There’s certainly a good reason for getting vaccinated, Didwania said.
“Shingles is a terrible, painful and debilitating condition that can lead to horrendous long-term pain,” she said.
There are limitations to the new study. While it indicates the benefit of the vaccine in a real-world setting, it's not the same as a randomized controlled trial, said Dr. William Schaffner, a professor of infectious diseases at the Vanderbilt University Medical Center in Nashville, Tennessee. But it wouldn't be ethical to randomly assign people to get the vaccine or not, he said.
“It’s provocative, interesting and exciting,” he said of the research.
It’s possible that the Food and Drug Administration could review research linking shingles vaccines to a lower risk of dementia and allow the drug company to add that indication to the label, Schaffner said.
Even if that doesn’t happen, doctors can use the study findings to convince patients to choose to be vaccinated.
“Clearly there are lots of people 50 and over who have not received the vaccine,” he said. “If you say there are some data that suggest the vaccine might prevent some cases of dementia, people might be persuaded.”
NC Breaks Records for Pollen Count in 2025

Pollen across state is troubling for allergy sufferers
CHARLOTTE, N.C. (QUEEN CITY NEWS) – If you’ve noticed your allergies seem to be much worse this year – you’re not alone. The Asthma and Allergy Foundation of America reports that allergies are worse this year and may continue in that direction.
The North Carolina Division of Air Quality measured a new record at the end of March. The agency typically measures pollen from February through October. Last week, it measured the highest grass pollen of all time for the month of March since it started gathering data in 1999.
Although spring is blooming in Uptownn (Charlotte), it comes at a price. Deepti Bhave has lived in Charlotte for 20 years and says she’s never had trouble like she is now.
“It’s so beautiful in Charlotte,” Bhave said. “I love the colors in the spring and everything else, but the allergies just dampen the spirit.”
This was a common theme among people at Romare Bearden Park Wednesday.
Daryl Goodman said he’s never had allergies before this year.
“It makes my eyes red, it makes my eyes watery,” Goodman said. “It’s a terrible season. I haven’t had any issues, but this season is definitely an issue.”
They’re not alone. The Asthma and Allergy Foundation of America (AAFA) says a warmer climate is to blame.
Kenny Mendez is the CEO of AAFA. He says allergy growing season starts a lot sooner and ends much later.
“That supercharges the release of pollen so that’s why you have a longer and then a more intense allergy season because of those intense releases of pollen,” Mendez said. “Now because there’s so much more people who’ve never had it before, now their bodies are reacting more. Their triggers might have been much lower, but now because there’s so much more, year-round, then that can be a bigger factor for people.”
Mendez said trees are typically to blame this time of year and the Division of Air Quality has show high levels of tree pollen these last few days.
“It’s really important to have your triggers under control and understand if you have something like allergic asthma and work with a specialist to understand what your triggers are,” Mendez said.
Mendez said we spend close to 90 percent of our time indoors, so if you go outside, he said it helps to leave your shoes at the door when go home and if you walk your dog – wash him or her to keep allergens low in your home. AAFA also reported this year that Charlotte hit No. 18 of the most challenging places to live because of allergies.
NC AHEC Announces Next CoCM Provider Learning Collaborative
 Collaborative Care Model (CoCM) Provider Learning Collaborative
Collaborative Care Model (CoCM) Provider Learning Collaborative
April 17, May 29, June 19, 2025
Time: 12:00 - 1:00 p.m.
Location: Livestream Webinar
Target Audience
These Learning Collaboratives are for primary care providers, behavioral health professionals, and anyone else who has implemented or is considering the Collaborative Care Model (CoCM) for integrating behavioral health in a primary care setting. Independent primary care practices, FQHCs, and rural health clinics may find this collaborative especially helpful for meeting some of the behavioral health needs of their patients.
Program Description
The Collaborative Care Model (CoCM) is an integrated modality that provides patients with medical and behavioral health care in a primary care setting. The CoCM Learning Collaborative sessions will highlight collaborative care team integration and the role of the CoCM Behavioral Health Care Manager for practices new to the model and those established with implementing CoCM.
Objectives
- Participants will be able to describe the principles of the Collaborative Care Model (CoCM).
- Participants will be able to identify key concepts and team member roles/responsibilities for effective implementation of CoCM.
- Participants will be able to explain the value and evidence for measurement-based, treatment to target CoCM care.
- Participants will be able to discuss the contributing factors to successful Collaborative Care implementation.
For more information and to register click here.
NCMS is Sending Match Day Congratulations!
The North Carolina Medical Society congratulates all the new graduating medical students on their Match Day success!
Jonathan Bowling matched into the Internal Medicine-Pediatrics residency at the Medical University of South Carolina in Charleston. He earned his undergraduate degree from UNC-Chapel Hill and will graduate from ECU Brody School of Medicine in May.
Jonathan is also a scholar in the current cohort of the North Carolina Medical Society Future Healthcare Leaders program.
Congratulations Jonathan!


NCMB Board Leadership Opportunities

NCMB is accepting applications for Board Members

NC DHHS Secretary and former NCMS President Dr. Devduttta Sagvai has an important message for potential NCMB Board members.
Click here to hear his thoughts on Board membership..
Board Members are appointed by the Governor. Physicians and PAs must apply according to a process established by state law (N.C. Gen. Stat. § 90-2 and 90-3), which requires interested parties to apply to an independent panel that nominates candidates for the Governor’s consideration. The deadline to apply is June 23, 2025.
Board Members participate in bimonthly meetings as well as disciplinary hearings, which are held up to six times per year depending on caseload. Board Members spend about 20 hours preparing for each meeting or hearing. In addition, many Board Members contribute articles to the Board’s quarterly newsletter and present to medical students, residents, professional meetings, community groups and other audiences as part of their work on the Board. Board Members are appointed to three-year terms and may serve up to two consecutive terms.
Visit the website of the Review Panel for the North Carolina Medical Board for more information.
By law, NCMB has three public members. One is appointed at the discretion of the Governor and two are appointed by the General Assembly upon the recommendations of the Speaker and President Pro Tempore.
For more information application criteria click here.
Take a Look! NCMS Future Healthcare Leaders 3rd Session

RALEIGH -- The NCMS in action! The Future Healthcare Leaders are a group of interdisciplinary graduate healthcare students from across the state.
During their 3rd Learning Session in March, they participated in Leading with Others and Communication Skills workshops.
It is part of the NCMS Kanof Institute for Physician Leaders.
Each program provides a unique leadership journey that is tailored to meet the needs of healthcare professionals at various stages in their careers.
- The Academy for FUTURE Healthcare Leaders (FHL) is an interprofessional leadership development program open to medical, PA, pharmaceutical, and nursing students throughout NC.
- Newer/mid-career leaders and residents can enroll in the NCMS Academy for ADVANCED Healthcare Leaders (AHL) .
- Senior level healthcare clinicians and administrators can enroll in the NCMS Academy for EXECUTIVE Healthcare Leaders (EHL).
For more information click here.
Genomic Sequencing Reveals Previously Unknown Genes That Make Microbes Resistant to Drugs and Hard To Kill

This article was written by Nneka Vivian Iduu, a graduate research assistant in pathobiology at Auburn University, for The Conversation — a nonprofit news organization dedicated to sharing the knowledge of researchers and scientists, under a Creative Commons license. Read the original article here.
(The Conversation) -- In the 20th century, when a routine infection was treated with a standard antibiotic, recovery was expected. But over time, the microbes responsible for these infections have evolved to evade the very drugs designed to eliminate them.
Each year, there are more than 2.8 million antibiotic-resistant infections in the United States, leading to over 35,000 deaths and US$4.6 billion in health care costs. As antibiotics become less effective, antimicrobial resistance poses an increasing threat to public health.
Antimicrobial resistance began to emerge as a serious threat in the 1940s with the rise of penicillin resistance. By the 1990s, it had escalated into a global concern. Decades later, critical questions still remain: How does antimicrobial resistance emerge, and how can scientists track the hidden changes leading to it? Why does resistance in some microbes remain undetected until an outbreak occurs? Filling these knowledge gaps is crucial to preventing future outbreaks, improving treatment outcomes and saving lives.
Over the years, my work as a microbiologist and biomedical scientist has focused on investigating the genetics of infectious microbes. My colleagues and I identified a resistance gene previously undetected in the U.S. using genetic and computational methods that can help improve how scientists detect and track antimicrobial resistance.
Challenges of Detecting Resistance
Antimicrobial resistance is a natural process where microbes constantly evolve as a defense mechanism, acquiring genetic changes that enhance their survival.
Unfortunately, human activities can speed up this process. The overuse and misuse of antibiotics in health care, farming and the environment push bacteria to genetically change in ways that allow them to survive the drugs meant to kill them.
Early detection of antimicrobial resistance is crucial for effective treatment. Surveillance typically begins with a laboratory sample obtained from patients with suspected infections, which is then analyzed to identify potential antimicrobial resistance. Traditionally, this has been done using culture-based methods that involve exposing microbes to antibiotics in the lab and observing whether they survived to determine whether they were becoming resistant. Along with helping authorities and researchers monitor the spread of antimicrobial resistance, hospitals use this approach to decide on treatment plans.
However, culture-based approaches have some limitations. Resistant infections often go unnoticed until antibiotics fail, making both detection and intervention processes slow. Additionally, new resistance genes may escape detection altogether.
Genomics of Antimicrobial Resistance
To overcome these challenges, researchers have integrated genomic sequencing into antimicrobial resistance surveillance. Through whole-genome sequencing, we can analyze all the DNA in a microbial sample to get a comprehensive view of all the genes present — including those responsible for resistance. With the computational tools of bioinformatics, researchers can efficiently process vast amounts of genetic data to improve the detection of resistance threats.
Despite its advantages, integrating genomic sequencing into antimicrobial resistance monitoring presents some challenges of its own. High costs, quality assurance and a shortage of trained bioinformaticians make implementation difficult. Additionally, the complexity of interpreting genomic data may limit its use in clinical and public health decision-making.
Establishing international standards could help make whole-genome sequencing and bioinformatics a fully reliable tool for resistance surveillance. The World Health Organization recommends laboratories follow strict quality control measures to ensure accurate and comparable results. This includes using reliable, user-friendly computational tools and shared microbial databases. Additional strategies include investing in training programs and fostering collaborations between hospitals, research labs and universities.
Discovering a Resistance Gene
Combining whole genome sequencing and bioinformatics, my colleagues and I analyzed Salmonella samples collected from several animal species between 1982 and 1999. We discovered a Salmonella resistance gene called blaSCO-1 that has evaded detection in U.S. livestock for decades.
The blaSCO-1 gene confers resistance to microbes against several critical antibiotics, including ampicillin, amoxicillin-clavulanic acid and, to some extent, cephalosporins and carbapenems. These medications are crucial for treating infections in both humans and animals.
The blaSCO-1 gene likely remained unreported because routine surveillance usually targets well-known resistance genes and it has overlapping functions with other genes. Gaps in bioinformatics expertise may have also hindered its identification.
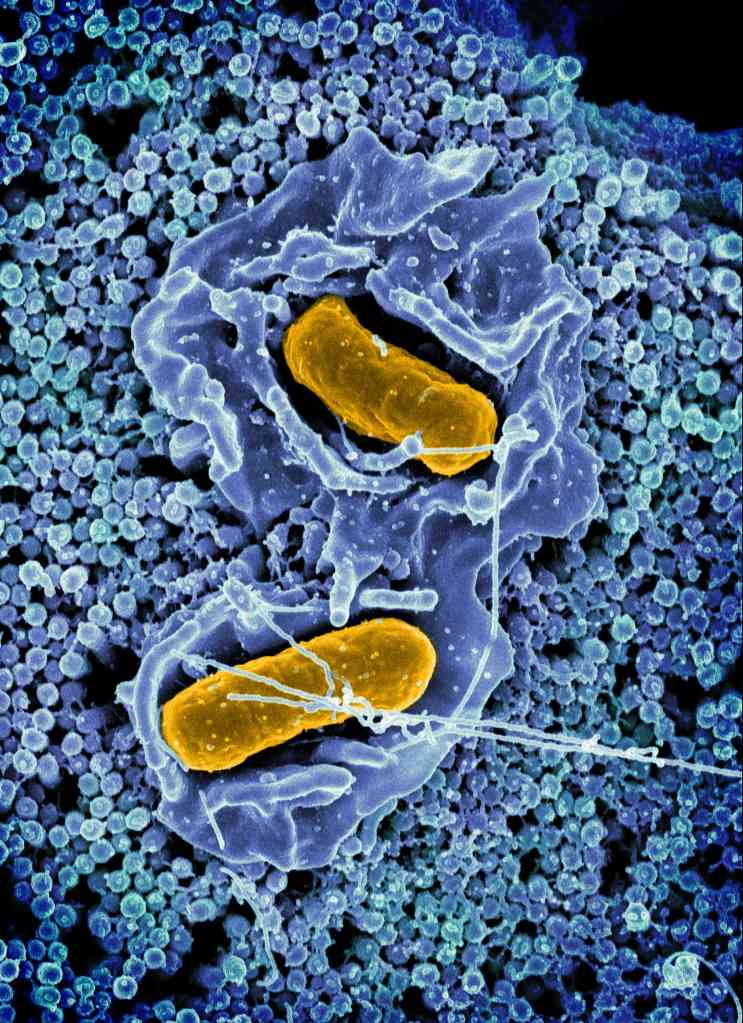
The failure to detect genes like blaSCO-1 raises concern about its potential role in past treatment failures. Between 2015 and 2018, the Centers for Disease Control and Prevention began implementing whole-genome sequencing for routine surveillance of Salmonella. Studies conducted during this period found that 77% of multistate outbreaks were linked to livestock harboring resistant Salmonella.
These missed genes have significant implications for both food safety and public health. Undetected antimicrobial resistance genes can spread through food animals, contaminated food products, processing environments and agricultural runoff, allowing resistant bacteria to persist and reach humans. These resistant bacteria lead to infections that are harder to treat and increase the risk of outbreaks. Moreover, the global movement of people, livestock and goods means that these resistant strains can easily cross borders, turning local outbreaks into worldwide health threats.
Identifying new resistance genes not only fills a critical knowledge gap, but it also demonstrates how genomic and computational approaches can help detect hidden resistance mechanisms before they pose widespread threats.
Strengthening Surveillance
As antimicrobial resistance continues to rise, adopting a One Health approach that integrates human, animal and environmental factors can help ensure that emerging resistance does not outpace humans’ ability to combat it.
Initiatives like the Quadripartite AMR Multi-Partner Trust Fund provide support for programs that strengthen global collaborative surveillance, promote responsible antimicrobial use and drive the development of sustainable alternatives. Ensuring researchers around the world follow common research standards will allow more labs – especially those in low- and middle-income countries — to contribute to global surveillance efforts.
NC Trend: Duke University Drives to Become Bigger Healthcare Force in NC

Business NC takes look at expansion efforts by Duke University
(Business NC, David Mildenberg) -- It hasn’t attracted attention like Blue Devil basketball phenom Cooper Flagg, but the pace of change at Duke University’s healthcare operation has accelerated dramatically.
In December, Duke Health said it would invest $280 million to buy Lake Norman Regional Medical Center and related businesses in Mooresville in Iredell County. It marks the Durham-based system’s first entry into the Charlotte metropolitan area, pending regulatory approval.
In January, Duke Health said it would partner with UNC Health to build a proposed $2 billion pediatric hospital on an undisclosed site in the Triangle. The state-owned, Chapel Hill-based system announced the freestanding 500-bed children’s hospital in September 2023. Beyond its globally respected medical pedigree, Duke is providing fundraising muscle needed to execute the project, a first of its type in the state.

In March, Duke Health announced a partnership with Novant Health to develop locations across the state to improve health outcomes. No specific projects or financial details were provided by the state’s second-largest hospital operator (Novant had about $10 billion in annual revenue last year) and third-biggest (Duke had $6.8 billion of revenue in fiscal 2024.)
The organizations said construction of the first sites would begin this summer, with the facilities opening about 18 months later.
Duke Health officials decline to discuss what is sparking the ambitious moves. But consolidation is a major trend in the healthcare industry because of increasing costs of remaining competitive and perceived advantages from economies of scale. Hospital system executives say they need to achieve a significant size to better negotiate contracts with insurance companies and invest in talent, technology and real estate.
Novant Health, which owns hospitals in the Charlotte, Winston-Salem and Wilmington areas, has said it wants to triple its annual revenue to the $30 billion range over the next few years.
That followed a similarly aggressive expansion effort at Atrium Health sparked after the 2016 hiring of CEO Eugene Woods. The Charlotte-based institution now dwarfs its North Carolina peers, with annual revenue topping $32 billion and operations in six states.
Duke Health’s moves follow a restructuring of leadership after the June 2023 retirement of Eugene Washington as the university’s chancellor for health affairs. He had held the post since 2015.

Upon Washington’s departure, Duke Health created two positions. Dr. Craig Albanese became CEO, overseeing the clinical enterprise, and Dr. Mary Klotman was named executive vice president for health affairs. The dean of Duke School of Medicine since 2017, she would “oversee Duke Health’s academic mission,” university President Vincent Price said in a June 2023 release.

Albanese came to Duke in January 2022 from New York-Presbyterian Hospital, where he had been group senior vice president and chief medical officer of the $9.2 billion, 10-hospital academic health system. He is a surgeon who previously had senior leadership jobs at Stanford University and its healthcare business.
Money won’t be a problem at Duke. The university reported an endowment of $11.9 billion last year and has an alumni roster that includes billionaires such as Apple CEO Tim Cook and Carlyle Group co-founder David Rubenstein.
In December, an anonymous donor gave $50 million to the proton beam therapy center, which is scheduled to open in 2029. It is expected to provide fewer side effects than traditional radiation therapy.
“Hospital affiliations are the new merger,” says Barak Richman, a law professor at George Washington University, referring to the Novant agreement. He is an expert on N.C. healthcare after previously working at Duke. “The idea is you secure patient flows, and you lock up different parts of the market. And, sometimes, that requires less regulatory scrutiny or oversight.”
Duke operates its internationally recognized flagship hospital and a smaller regional one in Durham, plus a third hospital in Raleigh that was acquired in 1998. Since 2011, it has been a partner with Brentwood, Tennessee-based LifePoint Health in the ownership of smaller community hospitals, including nine in North Carolina.
“We recognize the healthcare landscape is changing,” Albanese said about the Iredell County expansion. “While we continue to expand access to care within the communities we serve, it’s also time to do more and deliver care to more people — in more communities.”
NCMS is Sending Match Day Congratulations!
The North Carolina Medical Society congratulates all the new graduating medical students on their Match Day success!
Sophie Hockran matched in General Surgery at St. Elizabeth Hospital.
"I am so excited to match General Surgery in Youngstown, Ohio at St Elizabeth Hospital!" Hockran said. "North Carolina will always hold a special place in my heart for propelling my medical career. It’s been a privilege to work with NCMS the last four years!"

Look for more Match Day successes soon!
Powerful Partnership for Clinician Well-Being – NCCPRW Joins the Joy & Wholeness Summit 2025
NCCPRW Joins the Joy & Wholeness Summit 2025
In every corner of healthcare, there is a growing call for change. A call to prioritize the well-being of the people who care for others, to build systems that support clinicians, and to create a future where physicians and APPs don’t just endure—but flourish.
We are honored to announce that the North Carolina Clinician and Physician Retention and Well-Being Consortium (NCCPRW) has joined the Joy & Wholeness Summit 2025 as a Platinum Sponsor!
NCCPRW is a driving force in North Carolina, tackling the urgent need for physician and APP retention, well-being, and systemic change. With this sponsorship, they are deepening their impact—bringing North Carolina’s voices, innovations, and solutions to the national stage in Asheville this July.
What This Means for the Future of Clinician Well-Being
- A Spotlight on North Carolina’s Leadership – NCCPRW is strengthening its presence not just regionally, but nationally, ensuring that North Carolina-based initiatives are part of the broader movement for clinician well-being.
- Collaboration That Transcends Borders – With over 200 attendees from more than 100 organizations, this Summit is a gathering place for ideas, strategies, and partnerships that can reshape the future of healthcare.
- A Commitment to Real Change – Attendees will leave with tangible strategies to take back to their organizations, inspired by the collective wisdom in the room.
A Message from The Coalition for Physician & APP Well-Being
“Clinician well-being is not a solitary effort—it’s a shared responsibility. The work being done by NCCPRW to retain, support, and advocate for physicians and APPs aligns so closely with our mission, and we are thrilled to welcome them as a key partner for this year’s Summit. Their presence will help us strengthen the movement for well-being, ensuring that those who care for others receive the support and community they need to thrive.”
— DeAnna Santana, PhD, Executive Director, The Coalition for Physician & APP
Well-Being
A Message from NCCPRW
“Joining the Joy & Wholeness Summit allows NCCPRW to elevate our mission, connect with like-minded organizations, and continue advocating for sustainable solutions in clinician well-being. This partnership represents a shared commitment to creating lasting change for the physicians and APPs we serve.”
— Monecia Thomas, PhD, MHA, Executive Director, NCCPRW
Be Part of the Joy & Wholeness Summit 2025
July 23-25, 2025
Crowne Plaza Asheville, NC
Exclusive Opportunity for North Carolina-Based Attendees: Thanks to NCCPRW’s sponsorship, attendees from North Carolina will have access to an exclusive 15% discount to attend the Summit.
Surrounded by the breathtaking Blue Ridge Mountains, this is a space designed not just for learning, but for renewal.
This isn’t just another conference. This is an invitation to be part of something bigger.
Reserve Your Spot Today
Let’s Make This a Moment That Moves Healthcare Forward
NCCPRW will also be sharing this announcement with their network, ensuring that this message reaches clinicians, healthcare leaders, and organizations who are eager to be part of the conversation. If your organization is looking for meaningful ways to engage in the movement for clinician well-being, we invite you to connect with us.
Together, we are shaping the future of healthcare—one conversation, one partnership, and one bold step forward at a time.
The Coalition for Physician & APP Well-Being
www.bethejoy.org
CDC: Nearly 500 Cases of Measles Reported Across 19 States

Almost all of the cases are in unvaccinated individuals or in individuals whose vaccination status is unknown
(ABC News, Mary Kekatos, Youri Benadjaoud, Sony Salzman) -- The number of measles cases associated with an outbreak in western Texas has grown to 400, with 73 cases reported over the last three days, according to new data released Friday.
Almost all of the cases are in unvaccinated individuals or in individuals whose vaccination status is unknown, according to the Texas Department of State Health Services (DSHS). At least 41 people have been hospitalized so far.
Children and teenagers between ages 5 and 17 make up the majority of cases at 164, followed by children ages 4 and under comprising 131 cases, according to the data.
It comes as the CDC has so far confirmed 483 measles cases this year in at least 19 states: Alaska, California, Florida, Georgia, Kansas, Kentucky, Maryland, Michigan, Minnesota, New Jersey, New Mexico, New York, Ohio, Pennsylvania, Rhode Island, Tennessee, Texas, Vermont and Washington
This is likely an undercount due to delays in states reporting cases to the federal health agency.
Meanwhile, reports have emerged that some unvaccinated children hospitalized with measles in Texas are showing signs of vitamin A toxicity.
Health and Human Services Secretary Robert F. Kennedy Jr. and other vaccine skeptics have promoted vitamin A amid the measles outbreak. During an interview on Fox News with Sean Hannity earlier this month, Kennedy said that HHS was currently providing vitamin A to measles patients for treatment, claiming vitamin A can "dramatically" reduce measles deaths.
Vitamin A can be used as part of supportive treatment for those who are already sick, with the World Health Organization recommending two doses of vitamin A in children and adults with measles to restore low vitamin A levels, which can help prevent eye damage and blindness.
However, vitamin A does not prevent measles infections, experts previously told ABC News, nor does it directly fight the virus when used as a treatment.
Covenant Children's Hospital, which has treated dozens of measles patients in Texas amid the outbreak, told ABC News in a statement that some parents appear to have given their unvaccinated children vitamin A for "treatment and prevention." Some of those children now show signs of vitamin A toxicity.
Fewer than 10 children have come in with abnormal liver function in routine lab tests, indicating possible vitamin A toxicity, according to Covenant Children's.
Vitamin A toxicity occurs when someone consumes too much vitamin A, and can result in severe complications including liver and kidney damage.
The American Academy of Pediatrics and the Centers for Disease Control and Prevention says vaccination is the most effective way to prevent measles.
The CDC currently recommends that people receive two vaccine doses, the first at ages 12 to 15 months and the second between 4 and 6 years old. One dose is 93% effective, and two doses are 97% effective, the CDC says. Most vaccinated adults don't need a booster.
State health data shows that Gaines County, which is the epicenter of the Texas outbreak, has seen its number of vaccine exemptions grow dramatically in the last dozen years.
In 2013, roughly 7.5% of kindergartners in the county had parents or guardians who filed for an exemption for at least one vaccine. Ten years later, that number rose to more than 17.5% -- one of the highest in all of Texas, according to state health data.
Among the nationally confirmed cases by the CDC, about 97%, are in people who are unvaccinated or whose vaccination status is unknown, the agency said.
Of those cases, 1% are among those who received just one dose of the MMR inoculation and 2% are among those who received the required two doses, according to the CDC.
DEA Again Delays New Telehealth Prescribing Rules for Veterans, Buprenorphine

As of March 20, 2025, the effective dates of the final rules amending 21 CFR part 1306 and 42 CFR part 12 published in the Federal Register on January 17, are effective December 31, 2025.
(Healthcare Brew, Caroline Catherman) -- As every chronic procrastinator knows, nothing feels better than an extension on a due date.
So we bet it was a big relief for the US Drug Enforcement Administration (DEA) and the Department of Justice (DOJ) to push back the effective date of two new telehealth rules from March 21 to Dec. 31.
The rules would permanently expand some temporary telehealth flexibilities for prescribing buprenorphine—a medication used to treat opioid dependence—and for Department of Veterans Affairs (VA) clinicians to prescribe controlled substances.
These telehealth flexibilities were enacted during the pandemic and are set to expire Dec. 31. But telehealth clinicians have long called for a permanent solution, and these rules—two of three final controlled substances guidelines released on Jan. 16—were part of that solution.
“Unfortunately, the DEA’s decision fosters uncertainty for both healthcare providers and their patients,” Hari Prasad, CEO of mobile patient intake management system Yosi Health, told Healthcare Brew. “Delaying the implementation of these rules signals hesitation at a time when we should be prioritizing access and continuity of care for vets.”
Tell me more. This isn’t the first extension, either. The rules were initially set to take effect on Feb. 18, but were pushed back to March 21 after President Trump took office and issued a regulatory freeze.
Rule one, Expansion of Buprenorphine Treatment via Telemedicine Encounter, would let telehealth providers prescribe the drug for up to six months without an in-person visit. Pre-pandemic, a patient needed to have an in-person medical evaluation to get more than an initial 30-day supply of buprenorphine.
The other rule, Continuity of Care via Telemedicine for Veterans Affairs Patients, would give special prescribing privileges to VA practitioners, allowing them to prescribe controlled substances remotely to patients they have never met in person, as long as that patient has received an in-person medical exam from another VA clinician.
Non-VA providers would have to get special registrations to prescribe Schedule II–V controlled substances—such as hydrocodone, oxycodone, Adderall, or Ritalin—without an in-person visit.
Christopher Adamec, executive director of industry group Alliance for Connected Care, previously told Healthcare Brew he felt these laws didn’t go far enough to expand telehealth access, adding that the buprenorphine rule’s six-month limit means a doctor could be forced to cut off treatment “in a potentially harmful way when the patient needs it most.”
The DOJ said in federal documents that it’s postponing the effective date to address public comments and to add more time to review “any questions of fact, law, and policy that the rules may raise.”
NCMS is Sending Match Day Congratulations!
The North Carolina Medical Society congratulates all the new graduating medical students on their Match Day success!
Pankti Sheth, a 4th year medical student at ECU Brody School of Medicine, matched at Duke for Internal Medicine!

Look for more Match Day successes soon!