Study Reveals Decline In Mental Health Among US Mothers

Study Reveals Decline In Mental Health Among US Mothers
(News Nation, Taylor Delandro) — A new study published in JAMA Internal Medicine reveals a troubling decline in mental health among mothers in the United States.
Researchers at Columbia University and the University of Michigan found the percentage of mothers reporting “excellent” mental health dropped sharply from 2016 to 2023.
Using data from nearly 200,000 mothers in the National Survey of Children’s Health, a nationally representative survey of households with children, researchers tracked health trends among women with children under 18 years old. Most of the mothers were over 30.
Notable findings included a drop in the percentage of mothers reporting “excellent” mental health, from 38% in 2016 to 26% in 2023. Reports of “excellent” physical health also declined, from 28% to 24%.
Additionally, the number of mothers rating their mental health as “fair/poor” increased from 5.5% to 9%, a 63.6% increase.
“Although high rates of maternal morbidity and mortality have been well documented, national data on the health status of mothers beyond pregnancy and the first year postpartum is lacking,” said Jamie Daw, an assistant professor of health policy and management at Columbia’s Mailman School of Public Health.
The study revealed that the decline in mental health started before the COVID-19 pandemic and was observed across nearly every socioeconomic subgroup examined.
Researchers warned the impact extends beyond the mothers themselves, citing links between poor parental mental health and increased risks of developmental delays, behavioral issues and other challenges among children.
Daytime Sleepiness May Signal Serious Health Problems

Daytime Sleepiness May Signal Serious Health Problems
(Earth.com, Jordan Joseph) — Many people dismiss an afternoon slump as a harmless quirk of modern life. In reality, persistent daytime drowsiness can hint at larger concerns that may grow worse over time if left unaddressed.
Experts emphasize the importance of recognizing when repeated yawning and nodding off could be symptoms of an underlying sleep deficit. This is supported by evidence in a position paper co-authored by Dr. Eric Olsen, president of the American Academy of Sleep Medicine.
Dr. Olson is a pulmonologist at the Mayo Clinic in Rochester, Minnesota. He and other researchers highlight how insufficient rest contributes to physical hazards and long-term conditions that can harm well-being.
Daytime sleepiness and health problems
“Sleepiness is a serious health concern with wide-reaching consequences,” said Dr. Olson. Public health studies have indicated that not getting seven to eight hours of quality rest is tied to problems like diabetes and stroke.
Daytime yawning may be easy to ignore, but health specialists suggest viewing it as a warning. Trouble concentrating at work or dozing off in unexpected situations can point to deeper issues.
The researchers encourage anyone who experiences these signs on a regular basis to talk with their physician.
Safety risks of daytime sleepiness
Loss of focus can immediately threaten safety, such as when driving while drowsy. About 100,000 car accidents a year are connected to drivers who doze off behind the wheel.
Even momentary lapses in alertness, known as microsleeps, can be disastrous when operating heavy machinery or simply traveling home. Continued sleep deprivation also disrupts how the brain perceives its own fatigue.
“The unfortunate thing is data shows that with chronic partial sleep deprivation the ability to perceive our own level of impairment is no longer accurate, we think we’re OK when we’re really not,” said Dr. Indira Gurubhagavatula, a professor of sleep medicine at Penn Medicine.
Yawning may boost daytime alertness
Research shows that yawning is not just an individual response. Studies indicate that spontaneous yawns occur in a wide range of vertebrate species to maintain internal processes, but humans and certain social animals also experience contagious yawns.
Some scholars believe that catching another’s yawn might have helped groups remain more alert and watchful. A study led by Andrew Gallup from the State University of New York Polytechnic Institute hinted that seeing someone yawn can raise awareness of possible dangers.
Participants who observed yawns were quicker to spot threatening images, though their recognition of harmless ones stayed the same. Gallup explained that he didn’t see evidence for yawning increasing oxygen levels in the blood, referencing earlier myths about the reflex.
How doctors assess daytime sleepiness
The Epworth Sleepiness Scale is often used in clinics to decide whether daytime drowsiness reaches a concerning level. Participants rate how likely they are to drift off in situations such as sitting down after lunch or reading in a quiet room. Scores above 10 usually call for follow-up.
Doctors may also check for common conditions like sleep apnea, restless leg syndrome, or insomnia.
Certain medications can interfere with normal rest, so pharmacists might review any prescriptions or over-the-counter aids to see if sleep disruption is a side effect.
Improving sleep quality
Outside of medical conditions, choices such as late caffeine use can disturb a person’s rest. Alcohol before bed seems to help some individuals doze off, but it can fragment sleep patterns in the second half of the night.
Many specialists note that cutting back on evening drinks often leads to more refreshing sleep. They also warn that marijuana and other substances can lower the overall quality of nighttime rest.
Sleep loss linked to health issues
Long-term sleep shortage contributes to issues beyond feeling groggy. Research has tied insufficient rest to obesity, high blood pressure, and kidney disease.
The risk of depression can rise as well, possibly linked to changes in brain chemistry and mood regulation. Physicians suggest treating daytime drowsiness as a serious matter, not just a minor frustration.
Routines can reduce daytime sleepiness
The bedroom environment is another important factor. A bedroom that is too bright or too noisy may stop the body from settling into deep stages of rest.
For many people, bedtime routines that avoid screen use and heavy meals close to lights out can promote steadier sleep rhythms. Regular physical activity during the day can also help establish normal body cues, leading to fewer nighttime disruptions.
Health authorities recommend specialized testing if daytime drowsiness continues after these adjustments.
Future research on yawning
Experts continue exploring how yawning relates to vigilance and social bonding. Research continues to examine whether contagious yawns only heighten alertness or offer additional benefits.
As more data emerge, researchers hope these findings may encourage people to notice their own patterns and respond to signs of ongoing fatigue.
The study is published in the Journal of Clinical Sleep Medicine.
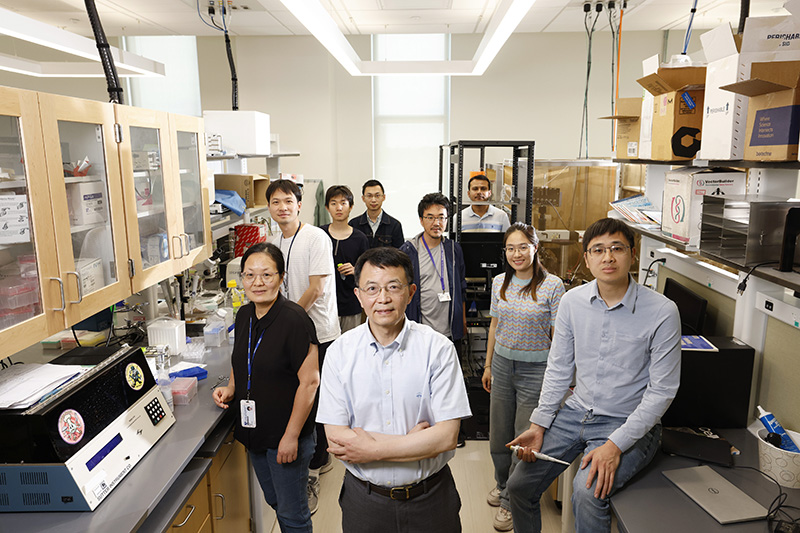
Father’s Death Led UNC Researcher To Seek Treatments For Pancreatic Cancer

Father’s Death Led UNC Researcher To Seek Treatments For Pancreatic Cancer
(The Robesonian, Jennifer Fernandez) — Finding a way to fight pancreatic cancer is personal for Kirsten Bryant.
She was studying cell biology at Cornell University and considering cancer research during the last year of getting her doctorate in 2013 when her father died from pancreatic cancer.
“After going through the process of treatment with him and realizing how few options there were for pancreatic cancer patients … I felt like I was in a position to potentially make a difference with the training that I had,” she said.
The five-year survival rate for pancreatic cancer is stubbornly low at just 13 percent, in part because it tends to be diagnosed only after it’s advanced. It has not been studied as vigorously as other cancers, many of which we have learned much more about — leading to the development of treatments that improve survival rates, Bryant said.
Federal grants helped her launch a pancreatic cancer research lab at UNC Chapel Hill’s Lineberger Comprehensive Cancer Center.
Cuts by President Donald Trump’s administration to the National Institutes of Health, which includes the National Cancer Institute that has funded much of Bryant’s research, have not touched her funding so far. But her lab has not gone unscathed. One of her researchers is waiting on confirmation of a fellowship award that would typically start this summer. Her cohort has been delayed twice already, Bryant said.
Bryant worries what will happen to research like hers when such critical support disappears.
She’s not alone.
UNC Chapel Hill has had 97 grants from federal and state agencies terminated, a spokeswoman told NC Health News in an email on May 12.
“We came to this field to be able to make a difference,” said UNC’s Vice Chancellor for Research Penny Gordon-Larsen, whose research focuses on the molecular and genetic underpinnings of severe obesity.
“We’re committed to getting diseases cured, and we want to do that work desperately,” said Gordon-Larsen, who is waiting on confirmation for expected funding to continue her own work. “So anything that gets in the way is very frustrating.”

Pancreatic cancer
The pancreas is a tadpole-shaped organ about six inches long that sits deep within the abdomen, between the stomach and the spine. It is considered a dual organ because it plays a role in two systems — producing enzymes that help digestion and making hormones that control blood-sugar levels.
More than 67,000 people will be diagnosed with pancreatic cancer this year in the United States, according to the Pancreatic Cancer Action Network.
The American Cancer Society estimates 51,980 people will die of pancreatic cancer this year. Of those, it’s estimated that 1,910 will be North Carolina residents.
Though pancreatic cancer is projected to make up only 3.3 percent of new cancer cases this year, it’s expected to cause 8.4 percent of all cancer deaths, the National Cancer Institute says.
It’s a type of cancer that mostly happens randomly, but smoking, obesity and age put people at a higher risk, according to the Pancreatic Cancer Action Network.
Pancreatic cancer is also difficult to diagnose. The gland’s position deep inside the abdomen makes tumors difficult to see or feel during routine exams. Tumors tend to be found by imaging technology such as MRIs.
In the early stages of the cancer, there aren’t any noticeable signs or symptoms. And once symptoms — which range from back pain to jaundice to weight loss — do appear, they present in a similar way to other illnesses.
The Pancreatic Cancer Action Network says diagnostic tests are “urgently needed” to find this type of cancer in the earliest stages.
Starving growth
Some researchers are working on early detection, while others, like Bryant, are trying to find better ways to treat pancreatic cancer.
Her team has been looking at a family of genes that, when mutated, can cause the disease. The vast majority of pancreatic tumors begin to form after a mutation in one particular gene, which creates a mutant protein that drives pancreatic cancer. This mutant protein is the focus of Bryant’s research.
After decades of investigation, therapies that successfully target and arrest these mutant proteins are relatively new. The first inhibitors were just approved for use three to four years ago, Bryant said.
There are currently very few targeted therapies for pancreatic cancer, and some approved therapies provide an average of only two more weeks of survival, she said. In contrast, this new therapy — which is in phase 2 trials that test effectiveness — showed a 14-month survival advantage.
However, there is still more work to be done, Bryant said, because resistance to the therapy eventually forms. She said her team can observe this in the lab, as well. They saw an increase in a metabolic process where cells seem to actually eat themselves. The team then created a treatment to stop that metabolic process, which is “almost like starving the cancer cells,” she said.
The next step is exploring other ways to prevent the uptick in that cellular self-eating process and to allow targeted therapies to better attack the cancer.
“Our research is really focused right now on understanding mechanisms of therapeutic resistance and coming up with novel combination therapies to treat this disease,” Bryant said.
Funding cuts on the horizon
The specter looming over research like Bryant’s is the current uncertainty in federal funding — especially for health-related research.
Through April, the federal government ended nearly 700 National Institutes of Health grants totaling $1.81 billion, according to a May 8 report in JAMA. In addition, NIH has cut back new grants by at least $2.3 billion since the start of the year, STAT reported.
At UNC Chapel Hill, NIH ended funding for 26 projects, a spokeswoman wrote in an email, and the university was a subrecipient of 16 grants that lost NIH funding. The university also had one project directly terminated by the Centers for Disease Control and Prevention and two where the university was a subrecipient.
It’s not clear how many jobs have been affected by the cuts. The spokeswoman said the university “is still working through programmatic and staffing implications of all the grant terminations.”
Bryant was awarded a special early investigator award through the NIH’s National Cancer Institute that can be extended for two years. Typically, getting the extension would be a given, she said, but she has not yet heard if her award will be extended.
Money has to come from many different pools to fund a cancer research lab, Bryant said. While foundations may play a role, the majority of funding comes from government sources, she said.
One of her early awards came from the Pancreatic Cancer Action Network to help her take her postdoctoral work into her first faculty position. Most researchers who got this type of first award now have their own pancreatic cancer research labs, Bryant said.
That award paid for the first couple of months of her lab, which allowed her to do the initial work to be able to pursue bigger grants from the government, she said.
“That’s how the system usually works,” Bryant said. “You get small foundational grants. They allow you to get the preliminary data that allows you to get the large grants from the federal government. And if we lose that piece, everything will kind of fall apart.”
Momentum
It is crucial to give the kind of support Bryant received to early career researchers, Gordon-Larsen said.
“You don’t get to grow the next generation without that (early investment),” she said. “And there has been a lot of talk in D.C. about … reducing those kinds of early career support programs.”
Amid all of the funding cuts, Bryant is grieving the loss of a fairly recent award focused on pancreatic cancer research.
The Department of Defense has a Cancer Research Program that distributes money to programs for various cancer research projects. Pancreatic cancer was added several years ago, and Bryant said she was one of the first research labs to get that grant funding.
The Trump administration recently cut the program.
“The fact that this is gone is very frustrating,” she said.
Research into pancreatic cancer has recently made some big strides, but it still lags behind the work done on many other cancers, she said.
“I believe that a lot of our lack of progress is just due to a lack of brain power and manpower, and as we bring more and more people into the field, we can make the steps that have already been made in other cancers,” Bryant said.
For instance, extensive research on breast cancer revealed subtypes that require different treatments, she said. That type of work is now being done with pancreatic cancer, and that came out of another UNC lab.
“Now we’re starting to realize that treatments affect one more than the other,” she said. “So it’s earlier days, but we’re already starting to see these steps that other more treatable cancers have gone through.
“I’m encouraged,” she continued, “but we need to keep the momentum going.”
Weight Loss Drugs Like Ozempic Could Soon Be In Reach

Weight Loss Drugs Like Ozempic Could Soon Be In Reach
(The Charlotte Ledger, Lindsey Banks) — At Carolina Family Healthcare in Charlotte, family physician Dimitrios Hondros has seen firsthand the life-changing benefits of weight loss drugs like Ozempic and Wegovy.
Patients not only lose weight but also often see improvements in blood pressure, cholesterol and blood sugar — factors that reduce their risk for heart disease and diabetes.
Yet Hondros estimates that 30 percent to 40 percent of his patients who could benefit from these medications aren’t taking them. They simply can’t afford the high price tag, and health insurance coverage is limited.
The medications, called GLP-1s, can cost roughly $12,000 a year out-of-pocket. While most health insurance plans cover them for diabetes, coverage for obesity alone is far less common.
But with prices starting to fall and policies under review, insurance experts say that could soon change.
Originally developed for diabetes, GLP-1s soon became recognized for their ability to help patients lose 15 percent or more of their body weight through weekly injections. They have also shown broader benefits like better heart health, reduced symptoms of sleep apnea and enhanced liver and kidney function.
Hondros said that means healthcare costs for patients using GLP-1s down the road could be lower for insurance companies.
“Just 3 percent to 5 percent weight loss helps drive down the total cost of healthcare, because you’re improving other chronic disease outcomes,” said Hondros, who served as president of the North Carolina Academy of Family Physicians in 2022 and has been fighting for broader access to GLP-1s on the state level for many years.
The drugs can also help prevent devastating health outcomes, Hondros said. One of his patients, who couldn’t afford the medication, ended up in a wheelchair because of severe arthritis tied to her weight, he said.
Another died of a massive heart attack — an event that might have been prevented with access to weight loss medication, he said.
Who covers GLP-1s for weight loss?
North Carolina is one of just 13 states whose Medicaid program covers GLP-1s for weight loss, meaning the drugs are available to the state’s lowest-income residents.
Meanwhile, 750,000 state employees, including teachers, lost access in 2024 when the state health plan dropped coverage due to rising demand and cost. Dale Folwell, the state treasurer at the time, said the state was on track to spend $170M a year to cover 23,000 members taking the drugs.
For many patients, the deciding factor is employer-sponsored insurance. About 75 percent of working adults in the U.S. receive their insurance through their employer, according to a 2023 study from KFF, a nonprofit that focuses on health policy issues in the U.S.
In Charlotte, it’s unclear how many employers offer GLP-1 coverage.
Of more than a dozen large companies contacted by The Ledger, only one, Ally Financial, responded. The company said it has long covered GLP-1s for both weight loss and diabetes, but recently added new requirements, including documentation from a medical provider and enrollment in a virtual health program called Omada.
Nationally, roughly 18 percent of U.S. employers with 200 or more workers covered GLP-1s for weight loss in 2024, according to the KFF survey. Over half of those plans require participation in lifestyle programs or other criteria, such as consultations with dietitians or mental health professionals, the survey found.
Telehealth In Home Healthcare Faces Setbacks Amid Lack Of Federal Reimbursements

Telehealth In Home Healthcare Faces Setbacks Amid Lack Of Federal Reimbursements
(News Medical Life Sciences) — Many home healthcare agencies adopted telehealth services during the COVID-19 pandemic, but the absence of federal reimbursements for these services has led to an increasing number of providers discontinuing these options, a national survey conducted by the University of California, Irvine, and other institutions reveals. Results are published in Health Services Research.
The National Institute on Aging-funded study offers valuable insights into the role of telehealth in home healthcare, a rapidly expanding sector. As the population ages and seeks alternatives to nursing homes, this field is expected to grow by 10 percent annually.
The survey's findings spotlight the urgent need for policy considerations from the Centers for Medicare & Medicaid Services, which has not reimbursed home healthcare agencies for telehealth services, even during the pandemic.
Conducted from October 2023 to November 2024, the study queried 791 home healthcare agencies, with a response rate of 37 percent. It focused on businesses that served a significant portion of dementia patients, averaging 33 percent of their clientele. The results revealed that only 23 percent of home healthcare agencies had adopted telehealth by 2019. However, that number surged to 65 percent by 2021, primarily driven by the implementation of virtual visits to mitigate disease transmission and address staffing and equipment shortages during the COVID-19 pandemic. Nevertheless, 19 percent of adopting agencies had discontinued telehealth by 2024. The reasons cited for this included a lack of Medicare reimbursement and concerns about the suitability of telehealth for the home healthcare of older, less tech-savvy patients.
This study is the first to provide a comprehensive national picture of telehealth's trajectory in home healthcare. Our findings suggest that without [Centers for Medicare & Medicaid Services] reimbursement, many agencies may abandon telehealth, potentially missing opportunities to improve care and manage costs as home health demand skyrockets."
Dana B. Mukamel, corresponding author, UC Irvine Distinguished Professor of Medicine
The survey revealed that 33 percent of home healthcare agencies never adopted telehealth, even during the pandemic, often believing it inappropriate for the sector's hands-on model. Virtual visits saw the largest adoption spike in 2020 (21.1 percent), but 22 percent of users had discontinued them by about 2022. Among this group, 60 percent echoed concerns about patient suitability, while 55 percent highlighted costs and lack of reimbursement. Remote patient monitoring and client surveys saw smaller adoption increases and similar discontinuation trends.
These patterns suggest that COVID-19 disrupted telehealth's natural diffusion into home healthcare, which was gaining traction pre-pandemic, with 23 percent adoption by 2019. The study posits that without the pandemic, telehealth might have continued spreading as agencies recognized its benefits. However, the lack of reimbursement and perceptions of telehealth's limitations for older adults pose barriers to sustained use.
Rates Of Liver Injuries Rise In The U.S. As Supplements Grow In Popularity

Rates Of Liver Injuries Rise In The U.S. As Supplements Grow In Popularity
(NBC News,Lindsey Leake, Marina Kopf and Emilie Ikeda) — It started with nausea and loss of appetite.
Robert Grafton, of Turnersville, New Jersey, tried to convince himself he was just coming down with something one weekend in mid-March. Then came the itching and dark urine. Grafton, a former interventional radiology technologist whose wife is a nurse, recognized the hallmarks of liver failure.
The otherwise healthy 54-year-old had a gut feeling that his herbal and dietary supplements were the culprit.
“I stopped taking everything, thank goodness,” Grafton said. “If I hadn’t known, if I was not in the medical field, I might have thought, ‘Oh, I think I’m getting sick. I need to take some more of these supplements to help me feel better.’”
When his symptoms had only worsened by midweek, Grafton visited his primary care physician. The doctor, he said, suspected hepatitis A, a liver infection that can be caused by consuming food or drink contaminated with the hepatitis A virus. Grafton’s laboratory test results showed otherwise.
“My liver enzymes were super elevated, my bilirubin was really high — all the signs of liver failure,” Grafton said. “I pretty much broke down, my wife as well. I was, at that point, thinking it was liver cancer, pancreatic cancer or something.”
That Friday, less than a week after his symptoms had begun, Grafton was admitted to Thomas Jefferson University Hospital in Philadelphia, where he received a diagnosis.
“It turns out I had something called a drug-induced liver injury, which came from my supplements.”
Rising rates of liver damage
The liver is responsible for more than 500 functions in the human body, including filtering harmful substances from the blood. Some people’s livers metabolize toxins more slowly than others, but too much of certain drugs can overwhelm even the healthiest liver.
When taken in excess, acetaminophen, for example, the active ingredient in Tylenol, is among the most common causes of drug-induced liver injury, also called toxic hepatitis. Pharmaceutical products aren’t solely the cause. Herbal and dietary supplements are causing liver damage with mounting prevalence.
From 1995 through 2020, supplement-related liver failure requiring U.S. patients to be waitlisted for transplants increased eightfold, according to a 2022 study in the journal Liver Transplantation. In addition, a 2017 review in the journal Hepatology found that 20% of liver toxicity cases nationwide are tied to herbal and dietary supplements. Because “multi-ingredient nutritional supplements” caused the majority of those cases, the authors said, it’s hard to pinpoint which component(s) may be to blame.
Whereas dietary supplements typically contain nutrients such as vitamins, minerals and amino acids from a range of sources such as fish oil, herbal supplements are a subset of dietary supplements composed of plant-based ingredients.
Liver damage linked to supplements is rare. How rare is unclear.
What is known is why cases are on the rise: More Americans are taking supplements. As many as 3 in 4 adults 18 and older take them, according to a 2024 survey by the Council for Responsible Nutrition, a trade group representing the dietary supplement and functional food industry. Almost 4 in 5 users said they prefer supplements to prescription or over-the-counter medications.
By comparison, the 2017–2018 National Health and Nutrition Examination Survey showed that 58% of adults 20 and older had used a dietary supplement in the past 30 days.
“I think people assume these things are safe,” said Dr. Dina Halegoua-De Marzio, a Jefferson Health hepatologist who treated Grafton. “The No. 1 reason we see people taking these are for good health or to supplement their health, and so I don’t think that they realize that there is a real risk here.”
Grafton was one such consumer. The father of five became more health-conscious when he hit 50, going to the gym and starting a supplement regimen that included fenugreek, DHEA, ashwagandha, L-carnitine and nitric oxide. He continued that cocktail, with few changes, for years without incident. About a month before he got sick, Grafton added turmeric pills to the mix, with the goal of reducing inflammation.
Then Grafton saw the social media promo he said helped set his health crisis in motion.
Ironically, he bought an advertised turmeric-based liquid supplement in part because it claims to support long-term liver health. Similar products are widely available.
“The whole push with that is that you’re getting a super-high, concentrated dose of turmeric and dandelion root and milk thistle, which I have always known from my medical past is good for liver health,” Grafton said. “It all sounded good. … I thought I did enough digging.”
He fell ill within a week of adding the liquid supplement to his routine.
Even though Grafton stopped the turmeric pills the day he started the turmeric drink, Halegoua-De Marzio said, turmeric overload most likely caused his liver injury. Not only was the drink ultra-concentrated; the pills contained 2,250 mg of curcumin, a substance that comes from the root of the turmeric plant. The pills also include black pepper extract, which Halegoua-De Marzio warned increases absorption twentyfold.
“When you cook with turmeric, that could be really safe. But some of the supplements now are 2,000 mg plus, which is a very high dose of turmeric,” she said. Coupled with black pepper, “the liver now has to break down that supplement and it can’t. It could make it really sick.”
The supplement spectrum includes everything from powders that claim to promote muscle growth to gummies that promise to reduce stress. When it comes to herbal supplements, natural doesn’t necessarily mean better or safer, Halegoua-De Marzio said.
“That’s what I hear from patients all the time — ‘Oh, I want something natural’ — this fear of prescription medicines being unsafe,” she said, adding that while prescriptions bear their own risks, they’ve gone through rigorous clinical trials.
Supplements aren’t subjected to the same premarket testing.
Among herbal ingredients tied to toxic hepatitis, turmeric is the most commonly consumed in the U.S., according to a study published last year in the journal JAMA Network Open. Following that are green tea extract, ashwagandha, Garcinia cambogia, red yeast rice and black cohosh.
About 15.6 million Americans take supplements containing at least one of these six botanicals, the study found. Most reported doing so on their own, not under a doctor’s advice.
Prescription medications are tightly regulated and therefore more easily quantified; it’s difficult to determine how many people consume supplements whose ingredients can cause liver damage. A goal of the JAMA Network Open research was to capture this magnitude — at least where herbal supplements are concerned — said co-author Dr. Robert Fontana, a professor of internal medicine at the University of Michigan Medical School.
“It’s important for other doctors to know, for the general public to know,” Fontana said. “The denominator of use is going up.”
Fontana and Halegoua-De Marzio are part of the Drug-Induced Liver Injury Network, a research group backed by the National Institute of Diabetes and Digestive and Kidney Diseases, part of the National Institutes of Health. More than 1,800 patients have been enrolled since the program’s 2004 inception, with 19% of cases tied to supplements.
Previous research has estimated that the U.S. sees 44,000 cases of liver damage linked to medications and supplements annually, including 2,700 deaths. The actual incidence is likely higher, Fontana said. Liver failure symptoms can be vague, so some people may be unaware they have the condition. People who sought natural remedies in the form of supplements may be wary of seeing a doctor. Others, Fontana said, may be embarrassed about inadvertently harming themselves; botanical users in his 2024 research were older, wealthier and more educated than nonusers.
“When you’re the patient, you’re like, ‘Why did this happen to me?’” Fontana said. “‘What do you mean, this stuff isn’t safe?’”
FDA doesn’t monitor supplement safety before sale
For Joanne Slavin, a registered dietitian and professor in the department of food science and nutrition at the University of Minnesota, consumer education on the risks and rewards of supplements is critical.
“We really only know human data when something goes wrong,” she said.
The Food and Drug Administration maintains a searchable database of recalls, market withdrawals and safety alerts but can’t vet supplements for safety or effectiveness before they hit store shelves. Only once they’re on the market does the agency have the authority to penalize “adulterated or misbranded” products. That’s thanks to the Dietary Supplement Health and Education Act of 1994, which limited the FDA’s reach. The number of supplements on sale today is almost 20 times as many as three decades ago.
Consuming supplements comes with risks, the FDA warns.
“Dietary supplements may contain ingredients that can have strong effects in the body, even if the ingredients are natural or plant-derived,” the agency said in a statement to NBC News. “Adverse events are more likely to occur if consumers take supplements in high doses, take multiple supplements or take supplements instead of or in addition to medications.”
According to the Council for Responsible Nutrition (CRN), dietary supplements can’t make claims concerning the prevention, diagnosis, mitigation or curing of a disease.
“Dietary supplements can’t say they can cure your cold, they can’t say they can prevent your Alzheimer’s or your cancer,” CRN President and CEO Steve Mister said. “If you see (such) a product out there, it is blatantly illegal.”
Dietary supplements have their place
In short, he said, supplements are intended for healthy people who are trying to stay healthy.
While everyone should ideally get all nutrients through a balanced diet, Slavin said, she recognizes that dietary supplements have their place. People who don’t eat red meat, for instance, may need to seek an alternate source of iron.
“A supplement is fine, sure,” she said. “But that’s on the individual basis rather than the public health basis for the whole world.”
Monitoring how many vitamins or mineral supplements are taken daily is straightforward, Slavin said.
The federal Office of Dietary Supplements has established daily upper limits for nutrients, from vitamin A to zinc, which vary by age and sex. Calcium, for example, has an upper limit of 2,000 mg per day for adults 51 and older — including food, drink and supplements.
Herbal supplements have no such boundaries and aren’t as well studied.
“Everything can be toxic at a certain amount,” said Andrea Wong, CRN senior vice president of scientific and regulatory affairs. “It’s really up to the manufacturers and the researchers who are looking at these ingredients to determine what is the beneficial amount … then also look at what would be the amount where you start seeing some evidence of toxicity.”
She said it’s important to let your doctor know about any supplements you’re taking or starting. Some supplements may interfere with prescription medications or each other, or be unsafe for people with certain medical conditions. For example, the FDA advises against taking any combination of aspirin, vitamin E, prescription warfarin or herbal supplement ginkgo biloba — all are blood thinners and may increase risk of stroke or internal bleeding.
According to Fontana, some people are even genetically susceptible to supplement-induced liver damage.
“That means there’s a biological basis as to why they were the one in 1,000, one in 10,000 people who took this and got into trouble,” Fontana said of supplements. “The same thing is true for prescription drugs; we’re finding genetic associations.”
The federal LiverTox database is a free tool highlighting medicines and supplements linked to liver injury.
The liver is usually a forgiving organ, Fontana said.
Grafton’s was. His hospital stay was brief, and he said his blood work had returned to normal within weeks of ceasing supplements. Additional testing revealed no permanent damage to his liver.
He said he has a new lease on life and resumed his health kick — with one notable exception.
“I don’t take any supplements whatsoever.”

Spotlight on Future Healthcare Leaders and Campbell University

Spotlight on Future Healthcare Leaders and Campbell University
(Campbell University) — The Campbell University medical school is fulfilling its mission to teach and prepare osteopathic, community-based physicians who serve the underserved.
It’s also developing great leaders.

A group of students from Campbell University graduated recently from the 2025 N.C. Medical Society’s Academy for Future Healthcare Leaders, a program designed to develop those respective skills for healthcare students.
The six-month interprofessional leadership development program included four in-person sessions and four virtual learning sessions. Student group presentations May 6 were the culmination of a program that began in November 2024, said Monecia R. Thomas, vice president of Professional Growth for the NCMS.
Myriad healthcare fields were represented, including doctor of osteopathic medicine, medical doctor and doctor of physical therapy, among others.
Representing the Jerry M. Wallace School of Osteopathic Medicine were student Drs. Nesreen Abu Khalaf, Mark Bushhouse, Shiela Marie Romanick and Tamera Hutchinson, whose team project was about fostering diversity in medical education.
“I feel really passionate about this project because diversity isn’t something that only affects students, it affects patients as well, and it’s our job as future leaders in the healthcare field to educate ourselves on this topic,” she said.
Hutchinson and her team explored obstacles, such as recent changes in diversity, equity and inclusion laws, as well as possible solutions, such as mentorship and pipeline programs.
“I gained leadership skills and learned a lot about myself as a person and as a future healthcare leader,” Hutchinson said. “I’m glad I had the opportunity to participate in this program and would encourage other students to consider it.”
Joining Campbell in the recent program were medical school students from the University of North Carolina at Chapel Hill, East Carolina University, Wake Forest University and Duke University.
Also taking part were students from the High Point University School of Dental Medicine, the University of North Carolina at Greensboro School of Nursing, Wingate University Department of Physician Assistant studies, the ECU School of Medicine and Wake Forest School of Medicine.
“Throughout the program, the scholars … had opportunities to identify their own leadership style and their own leadership behaviors through a leadership behavioral self assessment,” Thomas said.
Project-based learning, she said, is an inquiry-based educational approach that builds on one’s capacity to think critically and to problem solve, collaborate effectively and engage deeply with our program’s content.
“(The students) got an opportunity to learn about their strengths and identify areas of improvement, and they were exposed to certain skills related to time management, communications and teamwork.”
Dr. David Tolentino, associate dean for Clinical Affairs and interim dean, watched the presentations.
“They did such a great job,” he said.
For more information about the Medical Society's Future Healthcare Leaders program, see https://ncmedsoc.org/
Former Surgeon General Warns Social Media Is Harming Children’s Health

Former Surgeon General Warns Social Media Is Harming Children’s Health
(Physicians Weekly, Health Day News) — Former U.S. Surgeon General Dr. Vivek Murthy is urging lawmakers to take stronger steps to protect children from the potential dangers of social media.
In a recent interview on NBC News’ “Meet the Press,” Murthy said Congress has failed to act on what he described as a growing crisis.
“Congress has not stepped up to its responsibility to protect our kids,” he said. “They need to act now.”
Murthy served under both the Obama and Biden administrations. He’s asking Congress to pass laws that would require warning labels on social media apps about their impact on kids.
He also said he wants more transparency from tech companies so researchers can better study how the internet affects children.
He compared the situation to the early days of driving before cars had safety features.
“Those have reduced the number of deaths,” Murthy told “Meet the Press” moderator Kristen Welker. “We’ve got to do the same for social media, because what we’re doing now, Kristen, is we’re basically — it’s the equivalent of putting our kids in cars with no seat belts, with no airbags, and having them drive on roads with no speed limits and no traffic lights. And that is just morally unacceptable.”
Two bills aimed at regulating social media use by kids have been introduced in Congress: the Kids Online Safety Act (KOSA) and the Children and Teens’ Online Privacy Protection Act (COPPA 2.0).
Both received bipartisan support in the Senate but have not passed the House, NBC News said.
KOSA would require social media companies to prevent harmful content from reaching kids. COPPA 2.0 would raise the age at which companies can collect kids’ data from the current 12 to 17 and limit targeted advertising.
Critics say the bills could lead companies to censor too much content to avoid legal trouble. Some advertising and civil liberties groups have raised concerns, slowing progress.
Murthy also spoke about the rising rates of loneliness and mental health issues among children.
“A lot of them are trying to be somebody that they’re not online. And they actually don’t have as many friendships in person as we all need. So you put this all together and what you see is escalating loneliness and isolation,” Murthy added.
What’s more, Murthy warned that “more kids are struggling with this intense culture of self-comparison online, which is shredding their self-esteem,” according to NBC News.
He warned that children are especially vulnerable because their brains are still developing.
“They are more susceptible to social comparison, to social suggestion, their impulse control is not as well developed. And that puts them more at risk of the negative effects of social media,” Murthy said.
Former U.S. Rep. Patrick Kennedy, now a mental health advocate, agreed with Murthy.
“Our country is falling down on its own responsibility as stewards to our children’s future,” Kennedy told Welker.
He proposed a “prevention fund” to focus on early mental health care. “We should be investing now in identifying and helping kids who are most at risk,” he said.
More information
Johns Hopkins Medicine has more on social media and mental health in children and teens.
What To Know About the New NB.1.8.1 Covid Variant. And Whether You Should Worry.

What To Know About the New NB.1.8.1 Covid Variant. And Whether You Should Worry.
(Katie Couric Media, Tess Bonn) — It’s more contagious, flying under the radar, and already in the U.S. — meet NB.1.8.1, the latest Covid variant. It hasn’t sparked major outbreaks yet, but experts warn this strain is quietly spreading and may be more transmissible than earlier versions.
Scientists and health officials are closely monitoring the evolution of NB.1.8.1 to compare its characteristics with those of earlier strains, including whether it causes more severe illness and how well current vaccines will protect against it. Early surges in places like China, along with detections in several U.S. states, suggest the variant is slowly gaining ground.
Wondering what this means for you? From symptoms to prevention, here’s a look at everything you need to know to stay safe as the virus continues to evolve.
What is the NB.1.8.1 Covid variant?
NB.1.8.1, a spinoff of the Omicron strain, was first identified in January 2025 and has been steadily spreading since. It evolved from XDV.1.5.1 and is now on the World Health Organization’s radar as a “variant under monitoring” due to its growing global presence.
The earliest surge tied to NB.1.8.1 was reported in China, but it didn’t take long to spread. By late March and early April, U.S. health officials detected it in travelers arriving at California, Washington, Virginia, and New York airports. Additional cases have since been reported in other states, signaling a broader reach. The good news? Numbers remain low. As of now, NB.1.8.1 accounts for fewer than 20 reported cases nationwide, according to USA Today.
What are the symptoms of NB.1.8.1?
While the CDC hasn’t outlined specific symptoms in the NB.1.8.1. variant, experts agree that they mirror those of earlier Covid-19 variants. This includes:
- Fever or chills
- Cough
- Shortness of breath or difficulty breathing
- Sore throat
- Congestion or a runny nose
- New loss of taste or smell
- Fatigue
- Muscle or body aches
- Headache
- Nausea or vomiting
Is the new Covid variant more contagious?
Health officials in Hong Kong say NB.1.8.1 doesn’t appear to cause more severe illness than previous strains. What sets it apart, though, is how quickly it spreads. The variant’s tighter binding to human cells is what makes it more transmissible, according to microbiology professor Subhash Verma, Ph.D., from the University of Nevada, Reno, who spoke with CBS.
Another factor driving the surge in places like China could be the timing. Case numbers often rise during the summer months — and this year appears to be no different.
Do the current Covid vaccines protect against this new variant?
The World Health Organization says the current Covid vaccines should still protect against the NB.1.8.1 variant. But there’s a catch: Getting boosters might become more difficult. The Trump administration plans to limit booster shots mainly to older adults and those with certain health conditions. And Health and Human Services Secretary Robert F. Kennedy Jr. just announced that the CDC will no longer recommend routine Covid shots for healthy kids and pregnant women, even though pregnancy remains a high-risk factor for severe complications.
Alongside vaccination, practicing good hygiene, such as thorough handwashing and covering your mouth when coughing or sneezing, remains crucial. And if you’re going to be out in public, it might be worth dusting off that pack of N95 masks you thought you’d never need again. Staying informed and taking simple precautions can go a long way in keeping you and those around you safe.
Practice Manager Bootcamp Registration Is Open Now

Practice Manager Bootcamp Registration Is Open Now
July 2025 - May 2026
Calling all novice practice managers as well as experienced practice managers -- register now for Practice Manager Boot Camp (PMBC) sessions starting in July! Boot camp consists of nine separate modules that introduce the basic concepts of practice management. The lessons in each module (listed below) are presented in live weekly one-hour sessions and recorded for your review later. You can even customize your learning by taking all the modules or only the modules you need:
- Financial Management | 7/17/25 – 8/4/25
- Insurance | 8/7/25 – 8/25/25
- The Revenue Cycle | 8/28/25 – 9/15/25
- Coding | 9/25/25 – 10/6/25
- Human Resources | 10/9/25 – 11/10/25
- Customer Service | 11/13/25 – 11/24/25
- Leadership | 1/8/26 – 3/9/26
- Operations Management | 3/12/26 – 4/13/26
- Quality Improvement | 4/23/26 – 5/18/26
Participants must complete 100% of the sessions by the end of the module and complete a course evaluation to receive credit (CEUs) for boot camp modules.
Contact Jane Moran, MLS, Project Manager, at [email protected] with any questions. We look forward to connecting with you!
If you need assistance from a Practice Support coach, please contact us at [email protected].
ECU Health’s Mental Health Expo Showcases Resources For Community

ECU Health’s Mental Health Expo Showcases Resources For Community
(ECU Health) — More than 50 organizations focused on mental health participated in ECU Health’s 13th annual Mental Health Expo on Thursday, May 22.
The event, held at Eastern AHEC in Greenville, was free for everyone and helped connect community members with resources available in eastern North Carolina. Glenn Simpson, executive director for behavioral health at ECU Health, said that is the most important part of the Expo – ensuring everyone knows who to connect with if they or a loved one are in need.
“Mental health is health, mental illness is a disease, substance use disorder is a disease, it’s not a character flaw or something like that,” Simpson said. “We want people to know, because there is a stigma attached to mental health in many ways, that it is OK to ask for help. When you want to ask for help, we want to make sure people know who to ask. This is to help eastern North Carolina become aware of the resources available to them.”
Simpson said one in five adults in the United States suffer from a diagnosable mental illness and taking a moment to talk with a provider or a professional about your mental health is just as important as discussing blood pressure and other physical health needs.
The event also featured three presentations on mental health – two by psychiatrists and one by a therapist – covering nature’s benefit on mental health, the mind-body connection and more.
“Having experts here to bring their perspectives and understanding to this community is a great opportunity. I think it’s a great chance for folks to hear from professionals about small ways to improve mental health, like getting outside or healthy lifestyle choices,” Simpson said. “We’re just grateful to have everyone here working toward the same goal and helping get people to the resources they may need.”
He also said it was an exciting opportunity to share information about the upcoming state-of-the-art, 144-bed behavioral health hospital in Greenville, slated to open in 2025.
Welcome Our New Members!

The NCMS is excited to welcome these new members!
Mark A. Cairns, MD
Edwin Conquest
Ferdusy R. Dia, MD
Connor W. Ferguson, MD
Mary E. Hampe, DO
Rachel M. Harrison, MD
Jacqueline B. Hudson, PA-C
Amanda Lee, MD
Jennifer B. Philips, MD
Michael E. Solle, MD
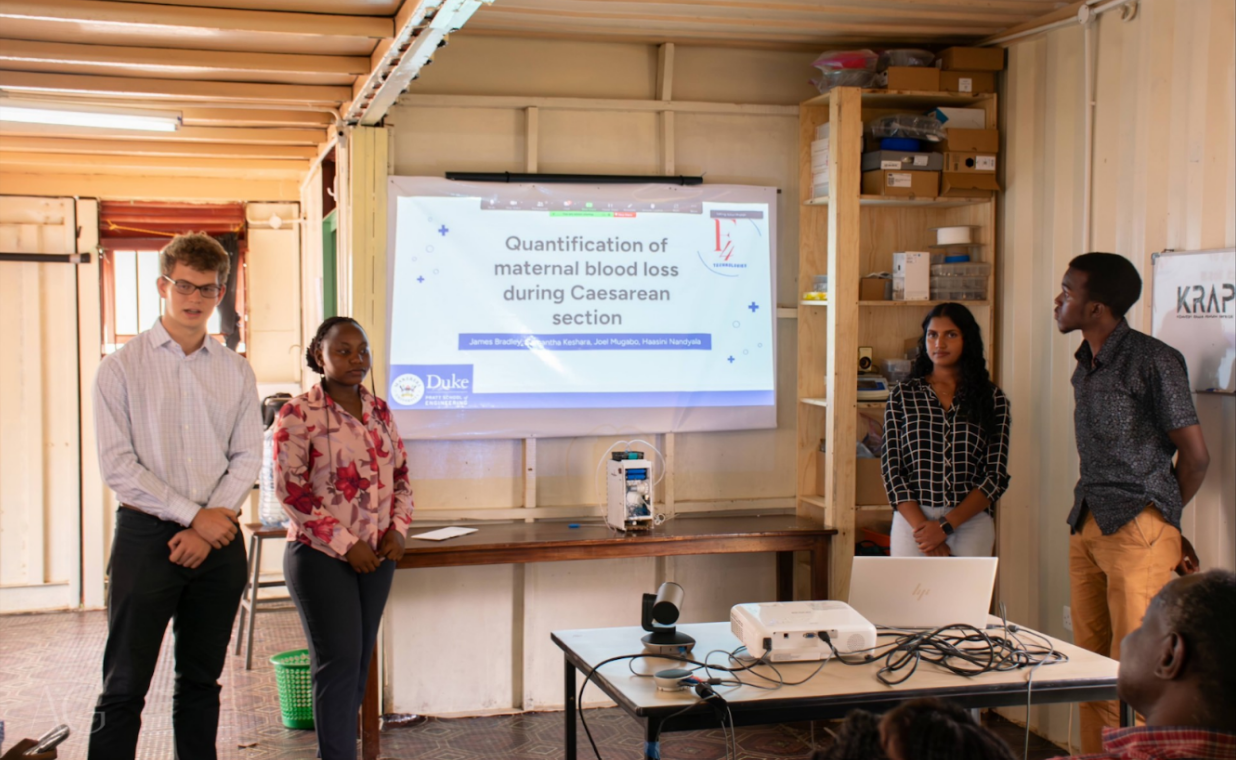
Duke and Uganda’s Makerere University Join to Combat Maternal Mortality

Duke and Uganda’s Makerere University Join to Combat Maternal Mortality
(Duke Research, Monona Zhou) — A recent study about maternal deaths at Kawempe National Referral Hospital in Uganda found that “as many as 1 in 50 maternal deaths worldwide occur in Uganda.” Moreover, between 2016 and 2018, around 84% of maternal deaths within the hospital alone were considered preventable.
Each year, over 70,000 women die from postpartum hemorrhage (PPH), making it the leading cause of maternal mortality in the world. At hospitals like Kawempe, the challenge is further exacerbated by the inability to quantitatively distinguish blood loss from other fluids lost during pregnancy, such as amniotic fluid.
“We noticed no sort of formal collection of blood or fluid,” said Haasini Nandyala, a senior biomedical engineering student at Duke University. “It was all randomly mopped up, and then blood would just go everywhere.”
Despite the ever-present issue of PPH, blood transfusions remain uncommon in Uganda. The combined factors of limited blood donation centers and lingering fears of the HIV pandemic continue to exacerbate the blood scarcity crisis. As a result, the team saw a clear direction: faster detection of hemorrhage was critical, and the current standards were inadequate.
From there, HemoSavetook root. Created by a team of engineering students from Duke and Uganda’s Makerere University – Haasini Nandyala, James Bradley, Mohammed Farah, Desmond Boateng, Joel Mugabo, and Samantha Keshara – the portable, low-cost device measures blood loss during cesarean sections (C-sections) in real-time and signals to the physicians when the patient is nearing a dangerous level of blood loss.
“We wanted our device to be easy to use and only require one person to operate because we saw how much of a workforce shortage there is,” said Nandyala. “There would usually be one surgeon and one nurse in every operating room, that’s it. One surgeon could do ten to twelve C-sections a day.”
The device measures blood loss through two main pathways. The first is collecting fluid through aspiration (i.e., a suction pump) before measuring the amount of the bodily fluid that is blood (using color and weight analysis). Simultaneously, the second method collects the blood soaked into medical cloths and compares the weight before and after use to determine the volume contributed to blood.
The system is able to monitor and warn when the blood loss exceeds eight hundred milliliters. Doing so provides clinicians with a better sense of real-time blood loss, prompting earlier interventions before childbirth becomes fatal for the mother.

Currently, HemoSave is now working towards patenting in Uganda and clinical implementation. Moreover, Nandyala aims to return to Uganda this summer to help refine the manufacturing process and bring the product to market.
For the students, being part of HemoSave has been as much a learning experience as it has been a technical achievement. The team navigated engineering challenges and cross-continental communication while also ensuring all the device’s parts were locally sourced. “This project has shown me what having a passion is like.” Bradley added, “It’s been awesome working with an international team, with our teammates in Uganda.”
Postpartum hemorrhage remains a critical, life-threatening issue that impacts thousands of mothers each year. But HemoSave’s impactful work highlights the possibility of a future where concerns over fatal blood loss during childbirth no longer exist.
“One of our biggest motivations for this whole project is that we’ve seen [post-partum hemorrhage], and we know that it’s an avoidable problem,” said Nandyala. “We truly believe that no matter where you live, no child deserves to grow up without their mother.”
NCDHHS Shares Critical Summer Safety Tips You Can Share With Your Patients

NCDHHS Shares Critical Summer Safety Tips You Can Share With Your Patients
(Goldsboro Daily News, Deonna Starks) — With summer on the horizon and temperatures beginning to climb, the North Carolina Department of Health and Human Services (NCDHHS) is urging residents to take proactive steps to stay safe during outdoor activities. From water safety and heat protection to food handling tips, the agency is highlighting key precautions to help prevent illness, injury and even death during the summer months.
May marks National Water Safety Month, a timely reminder that drowning remains the leading cause of death among children ages one through four — a tragedy that health officials emphasize is preventable.
“Every North Carolinian deserves to enjoy the summer season without risk to their health or safety,” said Dr. Kelly Kimple, Interim State Health Director and NCDHHS Chief Medical Officer. “By taking small, thoughtful actions — like supervising children near water, staying cool during extreme heat, and practicing safe grilling — we can all stay safe this summer.”
Water Safety: Vigilance Saves Lives
As families flock to pools, lakes and beaches, NCDHHS offers several crucial tips to keep swimmers safe:
- Always Supervise children around water — drowning can occur silently in seconds.
- Secure Pools by locking gates and removing ladders when not in use.
- Know Your Surroundings at beaches and rivers, where currents and drop-offs can pose hidden dangers.
- Stay Healthy by avoiding swimming when ill with diarrhea, which can spread waterborne illnesses.
- Check Water Quality at public pools and natural bodies of water; harmful algae blooms and bacteria may be present.
Heat Safety: Staying Cool Could Save a Life
Extreme heat is becoming more common in North Carolina. From May through September 2024, more than 4,600 emergency department visits were reported due to heat-related illness.
To protect against the risks of heat exhaustion or heat stroke, residents are encouraged to:
- Recognize Symptoms such as nausea, dizziness, confusion or a rapid heartbeat.
- Hydrate and Cool Off by sipping water and moving to shaded or air-conditioned areas.
- Be Aware of Vulnerable Groups, including children, seniors, pregnant individuals, outdoor workers, and athletes.
Residents can stay informed by signing up for the NCDHHS Heat Health Alert System, available through the NC Climate and Health team’s website.
Food Safety: Grill Smart This Summer
Grilling season is in full swing, and with it comes a spike in foodborne illnesses. Most foodborne outbreaks in North Carolina occur between May and August.
To avoid getting sick, NCDHHS recommends:
- Washing Hands thoroughly with soap before and after handling food.
- Separating Raw and Cooked Foods to prevent cross-contamination.
- Using a Food Thermometer to ensure meat is cooked to safe temperatures.
- Storing Leftovers Promptly, ideally within two hours.
- Cleaning Grills and Utensils before and after each use.
Stay Informed and Enjoy Summer Safely
For more information, visit:
New Study at UNC Offers New Hope For Safer Bleeding Treatments

New Study at UNC Offers New Hope For Safer Bleeding Treatments
(Medical XPress, University of North Carolina School of Medicine, Lisa Lock and Andrew Zinin) — A new study from UNC School of Medicine researchers, published this week in Blood, provides fresh insight into how the body forms and dissolves blood clots—and may help reshape how doctors treat patients at risk of bleeding.
Led by Alisa Wolberg, Ph.D., professor in the Department of Pathology and Laboratory Medicine and UNC Blood Research Center, the research team found that stopping the breakdown of blood clots does not necessarily increase the risk of dangerous clots, a concern that has long limited the use of certain medications in people who bleed easily.
"For years, we've known that blood clots are essential to stop bleeding, but they eventually need to dissolve so the body can return to normal," said Wolberg. "However, a concern has been that preventing that breakdown might push the body toward harmful clotting. What we've found is that this may not be the case."
The study used a wide range of tools—examining patients who are naturally missing a key clot-dissolving protein, employing genetically modified mouse models, and exploring genes and proteins that control clot breakdown. Across all approaches, the findings were the same: reducing or blocking the protein that causes clot breakdown did not increase the formation of dangerous clots known as thromboses.
The findings are especially important for patients who experience severe or frequent bleeding, such as trauma patients, individuals with bleeding disorders, or women with heavy menstrual bleeding. Medications like tranexamic acid, which help prevent clots from breaking down, have been shown to reduce bleeding—but are sometimes avoided due to concerns about clotting risks.
"This research helps us better understand clot biology, and it also provides reassurance that these bleeding treatments may be safer than previously believed," said Wolberg. "That means more patients who need these medications might be able to receive them."
The study highlights not only an important scientific advance, but also the essential role of biomedical research in improving health outcomes.
"Our work demonstrates the power of discovery science," said Wolberg. "This kind of research can translate directly into better, safer treatments—and ultimately, save lives."
Joy and Wholeness Summit Scholarship Awardee

Joy and Wholeness Summit Scholarship Awardee
The 2025 national Joy & Wholeness Summit, scheduled for July 23-25 in Asheville is a premier event dedicated to advancing the well-being of physicians, APPs, and healthcare teams.
This year’s Summit features dynamic plenary sessions, specialty tracks including “Women & Medicine,” “GME,” and “Well-Being Leadership”, and a “Focus on You” pre-track.
The Summit offers the Dr. Dianne McCallister Memorial Scholarship Program to increase accessibility for current GME residents and fellows to attend the conference.
Dr. Susan Roberts, a General Surgery Residents – PGY3, at East Carolina University recently won one of the McCallister Memorial Scholarships based on her demonstrated interest and involvement in activities that align with physician and APP well-being and mental health. Dr. Roberts is a current NC Medical Society Advanced Healthcare Leaders Scholar, a DO that graduated from Rocky Vista University College of Osteopathic Medicine in Colorado, and a Lieutenant in the United States Navy Reserve.
She is looking forward to her upcoming research year, where she will spend it doing research in the Trauma and General Surgery Departments, getting her MBA, progressing through the NCMS Advanced Healthcare Leaders Program, and serving as the President for RAMOPS, the Resident subset of the Association of Military Osteopathic Physicians and Surgeons.
Congratulations Susan!
Multimillion-Dollar 'NC Care' Initiative To Help Reopen Hospital In Martin County

Multimillion-Dollar 'NC Care' Initiative To Help Reopen Hospital In Martin County
(WUNC, Brianna Atkinson) — A new state initiative for rural healthcare will help reopen a hospital in Martin County. The NC Care Hospital investment will provide $150 million to rural hospitals across North Carolina.
The UNC System is in charge of distributing the funds, and the state's public university hospitals will operate the facilities. Half of the money will go to ECU Health and the other to UNC Health.
Earlier this month, the UNC Board of Governors voted to allocate $35 million for the Martin County reopening. UNC System President Peter Hans said he hopes the money will "jump start" investments in rural healthcare.
"The huge disparities in quality and access of care across the state – you can see it in the life spans that differ by decades, literally from parts of North Carolina," Hans said. "All of this was intended to be a catalyst for (ECU Health and UNC Health) that have a public mission in those rural areas."
Martin General Hospital closed in 2023, after more than half a century serving the county. The vacancy left a rural healthcare desert in the 21,000-population county, with the nearest hospital being over 20 minutes away in Beaufort County.
Dawn Carter, one of the county's healthcare consultants, said the closure had a ripple effect on Martin's medical care options.
"When rural hospitals close, the rest of the healthcare infrastructure is also dismantled," Carter said. "Most of the providers are gone, so it's hard to get an appointment with a physician provider in the community. You're having to travel outside the county for primary care. And it's really had a significant impact (on) EMS… it just puts a huge burden on the system."
Carter is the founder of Ascendient, a company Martin County's Commissioners hired while the hospital was still operational. It shut down two years ago after its operator, Williamston Hospital Corporation, went bankrupt. The county, which now owns the hospital, has been trying to reopen the facility ever since.
"(The process) is not as fast as any of us want, particularly the residents of Martin County," Carter said. "... we pursued several different avenues for getting something reopened, even if it wasn't a permanent facility. But the nature of the (bankruptcy filing) did not enable us to have any open avenues to try to get something even on a temporary basis."
The county's commissioners ultimately decided to reopen the facility under a special federal designation: a Rural Emergency Hospital (REH).
Congress launched the REH designation in 2023 in response to several rural hospital closures. It allows hospitals to still receive Medicare funds without providing full-service inpatient care. The designation is limited to rural facilities with less than 50 beds, and allows them to provide emergency department and observation care services.
Carter said the model is beneficial for Martin County, which fluctuated between only about five to a dozen people receiving inpatient care in the last few years it was operational.
"In so many places, they just have nothing. And so the idea was that we're going to make sure that we have access to critical services, even if inpatient services are not sustainable, too difficult to staff – we want an access point," Carter said.
The federal government also provides Rural Emergency Hospitals with an additional "facility fee," which Carter said is essentially a stipend to provide specialized services.
If Martin County's Commissioners approves its proposal, ECU Health will ultimately decide the specific services the hospital offers. Carter said the county anticipates the emergency department will operate similarly to how it did before it closed.
"You know, emergency rooms across the state, whoever comes into the door is who comes in the door and they have to be ready to take care of them," Carter said. "So any age, any diagnoses – they're going to be ready to, at a minimum, stabilize them and determine where they need to go from there. But many of the patients, we expect, will be able to be treated there."
Eventually, the county plans to either add on to Martin General Hospital or construct a new facility. According to Carter, the current building is equipped to operate as a Rural Emergency Hospital for a few years, but its infrastructure won't last forever.
"We know we're going to need to find funds somewhere to help us with construction of a new facility," Carter said. "... it's very hard for communities on their own, that are already economically challenged, to try to come up with the kind of money that it takes to invest in a facility like this. So, I think help from any corridor to make this be a reality is going to be welcomed."
It's unclear when Martin General Hospital will officially reopen. Carter said ECU Health has outlined four phases in its estimated timeline to resume the facility's services, and the work will likely take months. When the hospital does open back up, however, it'll be the first Rural Emergency Hospital in North Carolina.
Martin County's Commissioners are holding a meeting for the public to hear and respond to ECU Health's proposal. It's set for June 4th at 7:00 pm.
The other counties receiving funds from the $150 million NC Care Hospital initiative are Duplin, Lenoir, Onslow, Rockingham, and Wayne.
’Baby Brain’ Is Real. 3 Things To Know About What’s Happening To Your Patients’ Brains

’Baby Brain’ Is Real. 3 Things To Know About What’s Happening To Your Patients’ Brains
(CNN, Andrea Kane) — Science has pretty well established that the brain isn’t static; it changes and adapts throughout our lives in response to life events in a process called neuroplasticity.
Researchers are discovering this is especially true of female brains, which get remodeled significantly during the three Ps: puberty (as do the brains of adolescent males), pregnancy and perimenopause.
All three transitions are a frequent butt of pop-culture jokes: the sulky, risk-taking teenager who only wants to be with friends; the scattered mom-to-be who leaves her cell phone in the fridge and can’t remember where she parked the car; and the hormonal middle-aged woman who can’t focus and spontaneously combusts with hot flashes.
But far from being laughable, these behavioral stereotypes are the external manifestations of big internal shifts, many of them linked to the effects of fluctuating hormones on the brain.
Cognitive neuroscientist Laura Pritschet, a postdoctoral fellow in the department of psychiatry at the University of Pennsylvania, is fascinated by how female hormones, including estrogen and progesterone, affect the brain’s organization and functioning.
“The reason I chose that field is because I was a budding neuroscientist as an undergrad, interested in brain networks and obsessing over how intricate everything was in the brain to simply allow us to have a personality or remember things,” Pritschet told CNN Chief Medical Correspondent Dr. Sanjay Gupta recently, on his podcast Chasing Life.
“At the same time in my personal life, I was surrounded by menopausal women who were talking about their cognitive complaints and their attention issues,” she said. “I thought we’ve got to connect these two together and understand this more.”
Pritschet even volunteered as a “guinea pig” during graduate school, having her brain scanned and blood drawn for 30 days, across two complete reproductive cycles (both on and off birth control pills), to begin to answer the question of how the day-to-day fluctuations in hormones relate to the day-to-day changes in the brain.
Around this time, other researchers were studying what happens in the brain during pregnancy, Pritschet said, looking at the brain before and after gestation. They found many changes, but because the studies took a snapshot approach, many questions were left unanswered.
“If there’s a 3 to 5% decrease in total gray matter volume, when is that occurring (during pregnancy), and how is it occurring?” Pritschet asked. “We’re missing huge gaps in what we call this metamorphosis.
“We know that the 40-week gestational window leads to these body adaptations to support the development of the fetus: We have increased plasma volume, immune function change, metabolic rate, oxygen consumption,” she said. “What does this trajectory look like over gestation?”
To find out, Pritschet and her team tracked the brain changes in one woman, using MRI and blood draws, from pre-conception and fertility treatment throughout her pregnancy to two years postpartum. Their findings were published in the journal Nature Neuroscience in September.
You can listen to the full episode here.
New Study Finds Fewer Americans Are Developing Dementia—But More Are Living with It

New Study Finds Fewer Americans Are Developing Dementia—But More Are Living with It
(UNC Health) — A major new study published in The British Medical Journal has found that fewer older Americans are being newly diagnosed with dementia, yet the total number living with the condition is growing—a trend with serious implications for the healthcare system.

The latest research, led by experts at UNC School of Medicine, Duke University School of Medicine, and University
of Texas Southwestern Medical Center, spotlights the urgent need for policies that address disparities in dementia prevention, diagnosis, and long-term support.

“We’re seeing encouraging signs that fewer people are being newly diagnosed with dementia each year,” said Jay B. Lusk, MD, MBA, preventive medicine resident at the UNC Department of Family Medicine and visiting research scholar at Duke University. “At the same time, people with dementia are living longer than before, which underscores the need for long-term care planning, caregiver support, and equitable dementia care delivery.”
Dementia is already a leading cause of disability and dependency among older adults. Globally, more than 150 million people are projected to develop dementia by 2050. In the United States, this growing burden will increasingly strain families, caregivers, and the healthcare system—especially in underserved communities.
Researchers analyzed data from more than 25 million traditional Medicare beneficiaries between 2015 and 2021, focusing on trends in dementia incidence and prevalence across age, sex, race/ethnicity, and socioeconomic groups.
They made the following key findings:
- Age- and sex-adjusted incidence of dementia fell from 3.5% in 2015 to 2.8% in 2021.
- At the same time, prevalence rose from 10.5% to 11.8%, with nearly 2.9 million beneficiaries—about 12% of traditional Medicare enrollees—living with a dementia diagnosis by 2021.
- Dementia incidence was highest among Black beneficiaries (3.1%), followed by White (2.8%) and Hispanic (2.6%) beneficiaries in 2021.
- Higher rates of dementia were consistently found in women, racial and ethnic minorities, and people living in socioeconomically disadvantaged neighborhoods.
This work was funded by the Duke-UNC Alzheimer’s Disease Research Center (ADRC) under award P30AG072958 from the National Institute on Aging. The work was additionally funded by the Alzheimer’s Association under award 24HPE-1287087 and the Duke University Department of Neurology.
The North Carolina Medical Society Honors Memorial Day

The North Carolina Medical Society Honors Memorial Day
In observance of Memorial Day, you will not receive the NCMS Morning Rounds on Monday, May 26. As we pause to honor the brave men and women who gave their lives in service to our country, all of us at the North Carolina Medical Society remember their sacrifice with gratitude. Regular email delivery will resume on Tuesday.
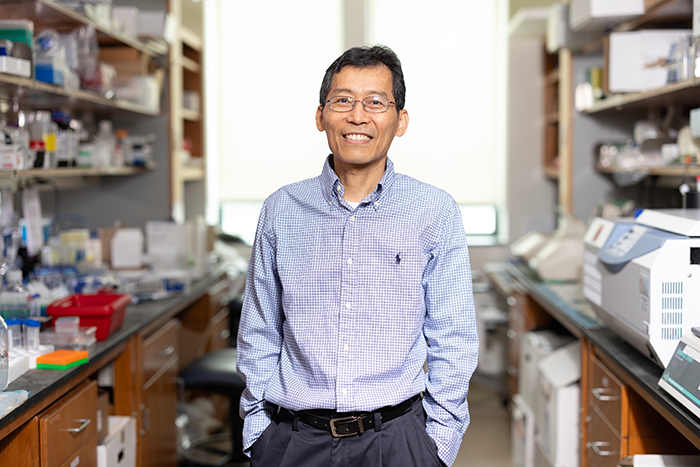
AI Model Predicts Future Lung Cancer Risk From A Single Low-Dose Chest CT Scan

AI Model Predicts Future Lung Cancer Risk From A Single Low-Dose Chest CT Scan
(News Medical Life Sciences, American Thoracic Society) — A deep learning model was able to predict future lung cancer risk from a single low-dose chest CT scan, according to new research published at the ATS 2025 International Conference.
The model, called Sybil, which was originally developed using National Lung Screening Trial (NLST) data by investigators from the Massachusetts Institute of Technology and Harvard Medical School, could be used to guide more personalized lung cancer screening strategies. It could be an especially valuable tool in Asia, where incidence of lung cancer in nonsmokers is rising, and many people without conventional risk factors don't meet screening guidelines, researchers said.
Sybil demonstrated the potential to identify true low-risk individuals who may benefit from discontinuing further screening, as well as to detect at-risk groups who should be encouraged to continue screening."
- Yeon Wook Kim, MD, corresponding author, pulmonologist and researcher at Seoul National University Bundang Hospital in Seongnam, Republic of Korea
Current international guidelines do not recommend lung cancer screening for people considered lower-risk, such as individuals who have never smoked. However, lung cancer rates are rising in this group, and the lung cancer burden in this population is significant.
This disconnect between risk and screening is especially a concern in Asia. The region accounts for more than 60 percent of new lung cancer cases and related deaths globally, with a rising incidence among people who have never smoked, Dr. Kim said. He also noted that the epidemiology of lung cancer in Asia is different from the populations where screening criteria were developed and validated. This has led to an increase in screening that is self-initiated or not consistent with guidelines, but there's a lack of data to suggest who should be screened and who should not.
For the new paper, researchers evaluated more than 21,000 individuals aged 50-80 who underwent self-initiated LDCT screening between 2009 and 2021 and followed their outcomes until 2024. The screening tests were analyzed by Sybil to calculate the risk of future lung cancer diagnosis. The model demonstrated good performance in predicting cancer diagnosis at both one and six years, including in never-smokers.
"Sybil's value lies in its unique ability to predict future lung cancer risk from a single LDCT scan, independent of other demographic factors that are conventionally used for risk stratification," Dr. Kim said.
The model could be used to develop personalized strategies for individuals who have already undergone LDCT screening but have not received further recommendations for additional screening or follow-up. Prospective validation will be needed to confirm the model's potential for clinical use.
Researchers plan to follow up on the study.
"Based on our results, we are eager to conduct a prospective study to further validate and apply Sybil in a pragmatic clinical setting, as well as to enhance the model's ability to predict other important outcomes, such as lung cancer-specific mortality," Dr. Kim said.
One-Of-A-Kind Charlotte Facility Could Tackle ‘Staggering’ NC Mental Health Crisis

One-Of-A-Kind Charlotte Facility Could Tackle ‘Staggering’ NC Mental Health Crisis
(The Charlotte Observer, Mary Ramsey) — Officially, Michael Estramonte is the founder of the Katie Blessing Center for youth behavioral health. But his sons get credit, too. After leading his StarMed Healthcare business through the COVID-19 pandemic, Estramonte looked for another “tough to tackle challenge.”
Mental health, an issue “definitely exacerbated” by the pandemic, seemed like a perfect fit. Gearing the project toward kids and teens was inspired by watching friends struggle to find care for their children. That led to hearing from local doctors about kids having to wait days, weeks or even months for a psychiatric bed, sometimes ending up out of state. “We said to ourselves, what can we do to help?,” he told The Charlotte Observer. That’s when Estramonte’s teenagers, Evan and A.J., stepped in. “They said, ‘Dad, you’re doing all this planning and whatnot, why aren’t you talking to us more?’” he recalled. Bouncing ideas off his kids evolved into putting together a student advisory council that would come to include more than 30 people. The final result will be North Carolina’s “largest and most advanced” pediatric mental health care facility, set to open in two phases in 2026 and 2027 in east Charlotte. It’s one of multiple projects aimed at filling gaps in the region’s mental health care system. Experts and advocates say they’re critical to improving a system vital to the community’s overall well-being. “These different types of services coming in are reflective of the need that’s in our community,” said Cotrane Penn, a division director in Mecklenburg County’s Child, Family, and Adult Services department.
‘Staggering’ problem for Charlotte-area families
Estramonte found statistics ranking North Carolina near the bottom of all states for access to mental health care “staggering.”
As he talked to more experts about what could be done, a common theme arose: a fragmented health care system makes it hard for families to navigate through emergency, inpatient and outpatient care for their children. Solving the problem meant creating a $62 million facility that put as much as possible under one roof — from urgent care to inpatient beds and outpatient treatment options. It was also important, Estramonte said, to have space for young people from Charlotte and across the state. Phase one is set to open in 2026 in a refurbished building across from the former Eastland Mall on Central Avenue in east Charlotte. It will include a behavioral health urgent care, 48 inpatient beds, telehealth facilities, indoor recreation areas and an outdoor courtyard. A three-story addition slated to open in 2027 will add up to 24 additional beds, an indoor gym and more therapy space. “There’s over 150 kids waiting in (emergency departments) throughout North Carolina’s hospital systems right now. So with 72 beds, we’re gonna put a significant dent in that,” Estramonte said. The city of Charlotte and Mecklenburg County have both of which invested millions. So has Novant Health, which is contributing $2.5 million and will help run the facility’s urgent care.
The center can revolutionize youth mental health care in the region, Dr. Uma Suryadevara, clinical physician executive for Novant Health’s Charlotte psychiatry institute, believes. “They could be our one-stop shop,” she said. Evie Thompson, 17, is most proud of the details she and her fellow students advisors helped incorporate. The high school junior — who is diagnosed with autism, ADHD and anxiety — connected with the advisory council through a school counselor who knew about her outspoken passion for mental health. “The mission of it really spoke to me,” she said. She and her fellow students helped design spaces that more closely resemble a college dorm than a hospital, where “kids can decorate and really show their personality.” They also incorporated a store-like area where patients arriving for a stay will be able to pick out a new outfit rather than wearing scrubs or hospital gowns. “A lot of the work that we’ve done is just ensuring that these kids feel like they’re human and not like a number,” Thompson said.
New kind of urgent care
As work continues on the Katie Blessing Center, another new resource in east Charlotte is already up and running.
Nestled around the corner from Bojangles Coliseum, the Smith Family Behavioral Health Urgent Care is a partnership between the Steve Smith Family Foundation and Daymark Recovery Services. In most ways, it looks like any other urgent care. But rather than treating sprained ankles and sore throats, its staff of medical professionals are available 24 hours a day to help people with a mental illness or substance use disorder. It’s averaged about 300 patients a month since opening two years ago, Daymark chief program office Michelle Ivey said. People can stay for up to 23 hours, and they don’t need health insurance to get care. Sometimes, patients are experiencing a mental health crisis. Other times, they’re brought in by a family member or law enforcement. Someone else may arrive in need of support maintaining their sobriety or needing to cool off from a conflict at home. “It gives people a place to go,” Ivey, a 30-year veteran of the social work field, said. When folks arrive, they’re assessed by staff and get a physical health screening. From there, staff determine what services the person needs. That process, Ivey said, can be as straightforward arranging a prescription refill or as complex as setting up inpatient treatment.
The goal is to help people overcome the often “complicated process” of finding appropriate mental health care in a system fragmented and expensive to access. Like Estramonte, Ivey hopes the urgent care can be part of a broader solution to the challenges facing the Charlotte area’s mental health care system. “There are a lot of resources here in Mecklenburg County. The problem is there’s often a delay in getting into those resources,” she said. “And so if we can help bridge that gap and those delays, that is very important.”
Editor’s note: If you or someone you know needs help, the national Suicide & Crisis Lifeline is available 24/7 by calling or texting 988.
Novant Health, UNC Health And UNC School Of Medicine Award $1 Million To Launch Two Regional Research Efforts

Novant Health, UNC Health And UNC School Of Medicine Award $1 Million To Launch Two Regional Research Efforts
(UNC Health) — Thanks to a $1 million investment, Novant Health physicians based in Wilmington are partnering with peer physicians and researchers at the University of North Carolina at Chapel Hill to advance two clinical research efforts in North Carolina.
The pair of $500,000 research grants was awarded by a collaborative involving Novant Health, UNC Health and the University of North Carolina at Chapel Hill School of Medicine. The funding will launch joint Novant Health and UNC School of Medicine studies focusing on evaluating tools that expand access to prenatal scans and advancing efforts to improve surgical care.

“We’re excited to announce two groundbreaking grants to advance collaborative research between Novant Health and UNC focused on improving health outcomes in our coastal communities. These awards will fund studies on maternal health and the post-surgical use of opioids— two important issues in southeastern N.C.,” said Mark King, vice president of research and innovation at Novant Health and the chair of the collaborative’s Research Advisory Council. “In addition, these collaborations will build additional infrastructure for future research here at the coast.”
The organizations formed an expanded alliance as part of Novant Health’s 2021 acquisition of what is now Novant Health New Hanover Regional Medical Center. In addition to expanding clinical research, the organizations are also growing medical education and pediatric specialty care, with an emphasis on Novant Health’s Coastal Region in southeastern North Carolina.
The latest award bolsters previously funded research: this collaborative awarded a separate $1 million grant last year to launch a pair of research projects to reduce health disparities for pediatric asthma and evaluate treatment for advanced prostate cancer. Each study is led by investigators based in both Chapel Hill and Wilmington, and work on those projects continues.
The collaborative also previously invested nearly $1 million to launch 19 individual $50,000 research grants.
“The partnership between UNC and Novant Health in research to benefit all people living in coastal North Carolina is really starting to hit its stride. These two exciting new projects aim to improve obstetric care and surgical care at the coast but also bring new insights to our state, the nation and the world,” said Dr. John Buse, a professor and advisor to the UNC School of Medicine’s Office of Research.
Read more here.
NC Works To Expand Availability Of Donor Breast Milk As Demand Rises

NC Works To Expand Availability Of Donor Breast Milk As Demand Rises
(NC Health News, Rachel Crumpler) — Demand for pasteurized donor breast milk is rising.
More than 10 percent of babies born in North Carolina are premature, according to state data. In 2023, that meant 12,885 premature infants. Breast milk helps protect premature babies’ guts and helps facilitate their growth.
The increased demand is due to growing recognition of the health benefits, as well as an uptick in premature infants in North Carolina receiving the milk.
When a mother’s own breast milk isn’t available the American Academy of Pediatrics and Centers for Disease Control and Prevention say pasteurized donor milk is the best alternative — better than formula. In particular, that’s because human donor milk can dramatically reduce the risk of necrotizing enterocolitis — a serious and even fatal gastrointestinal disease that destroys the lining of a newborn’s intestinal walls.
Pasteurized human donor milk can also bridge the gap until a mother’s milk supply comes in, promoting longer exclusive breastfeeding. And it turns out that the process of quickly pasteurizing breast milk works well to destroy harmful viruses, like HIV, while only minimally altering the nutritional components that protect babies.
Efforts are underway in North Carolina to bolster the supply and availability of donor milk across the state and expand the number of hospitals offering the milk to medically fragile infants.
40 years of milk banking in NC
WakeMed’s Mothers’ Milk Bank in Cary is the only human milk bank in North Carolina accredited by the Human Milk Banking Association of North America. The milk bank has operated since 1985 and is just one of 32 nonprofit milk banks in the United States.
Every month, the milk bank collects thousands of ounces of breast milk from voluntary donors across the state. After pasteurizing it, the milk bank dispenses the donor milk — mostly to about 44 neonatal intensive care units across the state and the Southeast. In fiscal year 2024, the milk bank distributed 306,709 ounces or approximately 2,396 gallons — an increase of 56,243 ounces or more than 439 gallons from fiscal year 2023.
To put that amount in perspective, one gallon of donor human milk can nourish 31 infants for a single day — or sustain one premature infant for an entire month, said Courtney Ramsey-Coleman, who leads an initiative at the N.C. Department of Health and Human Services to improve access to donor milk and improve breastfeeding rates.
Kerrie Gottschall, manager of Mothers’ Milk Bank, said the bank is on track to distribute even more donor milk this year.
“We’ve seen a lot of increased orders with our NICUs locally and out of state. It seems like right now the NICUs are really busy,” she said. “We’re actually dispensing more milk this time of year than this time last year, so we’re always trying to have more donors.”
Last year, in partnership with DHHS, Mothers’ Milk Bank opened five new depots across the state where donors can drop off breast milk. The sites have collected 250 gallons of milk to date, Ramsey-Coleman said.
“The goal is to ensure that no medically fragile infants are denied access to [donor milk] based on geography, income or awareness, so really making this a known and open thing just like formula is,” Ramsey-Coleman said.
Donor Breast Milk Drop Off Locations
North Carolina has 10 donor milk drop off locations, including the addition of five new sites in 2024 to expand donor access. The sites are now spread across Wake, Durham, Cumberland, Jackson, Pasquotank, Johnston and Mecklenburg counties.

Standard of care
Gottschall, who worked for years as a NICU nurse, said pasteurized human donor milk provides premature infants with the best outcomes. She watched this up close as she took care of preemies — and saw the potential consequences of skipping to formula.
A tragedy early in her career, around 2006, still sticks with her. Gottschall said she left her shift thinking the 34-week-old premature infant she had been taking care of was getting stronger and healthier. But the next day, she found that the baby had developed necrotizing enterocolitis, which would turn fatal.
“He went to surgery overnight, and his gut had completely gone dead,” Gottschall recalled. “There was nothing we could do but bring him back up for his parents to hold him.
“For them, it was a language barrier,” she recalled. “We offered donor milk. They said, ‘No, they would prefer to use formula because they had other children they had used formula with previously,’ and we accepted that.”
But in hindsight she said they should have communicated better the importance of donor milk and how risky formula can be for the developing gut. Donor human milk reduces the risk of developing necrotizing enterocolitis by about 50 percent in preterm or low birth weight infants compared to formula feeding, according to a study published last year.
The case sparked Gottschall’s passion “for feeding a baby the right way every time” — a path she’s been on for the past two decades, including the past three years as manager of Mothers’ Milk Bank. More people are starting to understand the importance of donor milk, she said, but there’s still work to do.
“It really should be the standard of care for infants who are born premature to get either mother’s own milk, or if that’s not available, then to use donor milk instead of formula,” Ramsey-Coleman said.
What is donor milk and where does it come from?
Milk banks collect donations from nursing mothers who are producing more breast milk than their babies need; all the mothers are screened for eligibility based on health and lifestyle factors. The milk banks then process and pasteurize the milk to ensure its safety and nutritional content before distributing it.
Mothers’ Milk Bank needs 300 to 350 active donors each month spread from the mountains to the coast to donate their extra breast milk to maintain its pool of donor milk. Some are one-time donors who clean out their surplus of frozen breast milk. Others give on a more regular basis throughout the period they’re still breastfeeding.
“We have a lot of donors who are giving back because they’ve received the milk in the hospital,” Gottschall said. “Knowing that other mothers wanted to give back to them and be able to provide nutrition to their baby was life-changing, so a lot of our donors will give back.”
Notably, about 10 percent of donors are bereaved mothers who opt to pump breast milk in honor of their child, Gottschall said.
Maryanne Perrin, a nutrition professor at UNC Greensboro who studies donor milk, said milk banking has been around for more than 100 years, though she said it’s more recently been in a period of “renaissance” and growth.
The Human Milk Banking Association of North America’s network of 32 milk banks dispensed a record-high 11 million ounces of pasteurized donor human milk in 2024 — a 10 percent increase from 2023, according to a February 2025 news release.
Doctors Perform First-Ever Human Bladder Transplant In U.S

Doctors Perform First-Ever Human Bladder Transplant In U.S
(Physician's Weekly, HealthDay News)—
Doctors in Southern California have performed the first human bladder transplant, offering new hope to people with serious bladder problems.
The surgery was done earlier this month by two doctors from the University of California, Los Angeles (UCLA) and the University of Southern California (USC), The New York Times reported.
The patient, 41-year-old Oscar Larrainzar, had lost most of his bladder due to treatment for a rare form of bladder cancer.
“I was a ticking time bomb,” Larrainzar said. “But now I have hope.”
Doctors plan to do four more bladder transplants as part of a small trial. They want to understand possible risks, including how well the bladder works and if the body rejects the new organ.
Dr. Inderbir Gill from USC called the surgery “the realization of a dream.” He said it could help people with long-term bladder problems like pain, infections and inflammation, The Times said.
Usually, patients who lose their bladder have part of their intestine repurposed, providing a new way to urinate.
But that method has downsides. Bowel tissue contains bacteria and is not sterile, which can lead to health problems in up to 80% of patients. It can also cause digestive issues, The Times reported.
This new transplant surgery was developed over several years. The doctors first practiced on pigs and then tested the method on donated human organs.
One big challenge was carefully removing the bladder with its blood vessels so it could be safely transplanted.
To make the surgery safer, the doctors connected the bladder’s main blood arteries together while the organ was on ice. That way, they only had to attach two arteries instead of four when placing it in the patient.
The transplant team got their first match in early May. They picked up the donor bladder and a kidney from an organ center, then completed an eight-hour surgery at UCLA. Larrainzar needed both organs because he had kidney failure and severe bladder damage, The Times said in a new report.
The results were promising. The new kidney started working right away, and Larrainzar began losing excess fluid.
His creatinine level, a key sign of kidney function, improved fast. Even more surprising, just two days after going home, he felt he was able to urinate on his own.
“He peed!” Dr. Nima Nassiri, Larrainzar’s other surgeon, said excitedly. Dr. Gill replied, “No way! What the hell?”
Still, experts say this kind of transplant may not be right for everyone. People who get transplants must take drugs for life to stop their body from rejecting the new organ. That can come with side effects.
Dr. Rachel Forbes, a transplant surgeon at Vanderbilt University Medical Center who was not involved in the transplant, said there are already options for people without bladders, and without the downside of requiring immunosuppression.
Unless a patient is going to be on those medications anyway, she told The Times, “I would be a little bit nervous that you would be exchanging some complications for others.”
Doctors also weren’t sure if Larrainzar would be able to feel when his bladder was full, or empty it normally. At first, they planned to use catheters or special devices to help him. But his body’s reaction surprised them all.
“It’s the first time he has been able to pee in seven years,” Gill told The Times. “For all of us, this is huge.”
NC Public Health, Threading The QI Needle

NC Public Health, Threading The QI Needle
June 12, 2025 Program: 12:00 p.m. - 1:00 p.m.
Presented via Live Webinar
Description:
Join us for “Threading the Needle”, a compelling presentation on public health clinical and financial quality improvement, led by 30-year veteran Health Director Scott Harrelson and Shannon Peaden, MBA, CPF, NC AHEC Public Health System Consultant. This session will explore the intersection of clinical outcomes and financial metrics that are critical to local health departments (LHDs). A new NC AHEC Public Health Quality Scorecard will be introduced during the session and made available to all attendees via a follow-up link. The presenters will examine public health needs, analyze key financial quality improvement data, and discuss clinical quality measures that not only impact patient outcomes but also influence LHD contracting and reimbursement.
Objectives:
• Describe statewide public health quality improvement needs
• Discuss the foundations of Financial and Clinical Public Health Quality Improvement
• Identify the components of the Public Health Quality Scorecard
• Recognize how the Public Health Quality Scorecard aligns with the NC Medicaid Quality Measures and the AMH (Advanced Medical Home) Measure Set
Registration:
Registration is online only at https://easternahec.net/courses-and-events/75692 and requires a current MyAHEC account. Registration will close at the start of the program.
Registration Fee: Free
Duke Researchers Find Experimental Painkiller Could Outsmart Opioids – Without The High

Duke Researchers Find Experimental Painkiller Could Outsmart Opioids – Without The High
(Duke University School of Medicine, Shantell M. Kirkendoll)— An experimental drug developed at Duke University School of Medicine could offer powerful pain relief without the dangerous side effects of opioids.
Called SBI-810, the drug is part of a new generation of compounds designed to target a receptor on the nerves and spinal cord. While opioids flood multiple cellular pathways indiscriminately, SBI-810 takes a more focused approach, activating only a specific pain-relief pathway that avoids the euphoric “high” linked to addiction.
In tests in mice, SBI-810 worked well on its own and, when used in combination, made opioids more effective at lower doses, according to the study published May 19 in Cell.
“What makes this compound exciting is that it is both analgesic and non-opioid,” said senior study author Ru-Rong Ji, PhD, an anesthesiology and neurobiology researcher who directs the Duke Anesthesiology Center for Translational Pain Medicine.
Even more encouraging: it prevented common side effects like constipation and buildup of tolerance, which often forces patients to need stronger and more frequent doses of opioids over time.
SBI-810 is in early development, but Duke researchers are aiming for human trials soon and have secured multiple patents for the discovery.
There’s an urgent need for non-opioid pain relievers. Drug overdose deaths are declining, but more than 80,000 Americans still die each year most often from opioids. Meanwhile, chronic pain affects one-third of the U.S. population.
Researchers said the drug could be a safer option for treating both short-term and chronic pain for those recovering from surgery or living with diabetic nerve pain.

SBI-810 is designed to target the brain receptor neurotensin receptor 1. Using a method known as biased agonism, it switches on a specific signal—β-arrestin-2—linked to pain relief, while avoiding other signals that can cause side effects or addiction.
“The receptor is expressed on sensory neurons and the brain and spinal cord,” Ji said. “It’s a promising target for treating acute and chronic pain.”
SBI-810 effectively relieved pain from surgical incisions, bone fractures, and nerve injuries better than some existing painkillers. When injected in mice, it reduced signs of spontaneous discomfort, such as guarding and facial grimacing.
Duke scientists compared SBI-810 to oliceridine, a newer type of opioid used in hospitals, and found SBI-810 worked better in some situations, with fewer signs of distress.
Unlike opioids like morphine, SBI-810 didn’t cause tolerance after repeated use. It also outperformed gabapentin, a common drug for nerve pain, and didn’t cause sedation or memory problems, which are often seen with gabapentin.
Researchers said the compound’s dual action—on both the peripheral and central nervous systems— could offer a new kind of balance in pain medicine: powerful enough to work, yet specific enough to avoid harm.
The study was supported by the National Institutes of Health and the Department of Defense.
Additional Duke authors include first authors Ran Guo and Ouyang Chen; Sangsu Bang, Sharat Chandra, Yize Li, Gang Chen, Rou-Gang Xie, Wei He, Jing Xu, Richard Zhou, Shaoyong Song, Ivan Spasojevic, Marc G. Caron, William C. Wetsel and Lawrence S. Barak.
ECU Health Opens Impact Clinic To Serve Patients With Perinatal Substance Use Disorders

ECU Health Opens Impact Clinic To Serve Patients With Perinatal Substance Use Disorders
(ECU Health)— ECU Health is proud to announce the opening of the IMPACT (Integrated Model of Perinatal Addiction Care and Treatment) Clinic, a new outpatient addiction medicine clinic dedicated to providing specialized care for pregnant individuals facing substance use disorders. Located within the high-risk clinic at the Brody School of Medicine at East Carolina University, this clinic is the first and only clinic of its kind in eastern North Carolina.

“We know that perinatal substance use disorder is a medical disease—not a moral failing,” said Dr. David H. Ryan, obstetrician-gynecologist, addiction medicine provider and clinical assistant professor at ECU Health and the Brody School of Medicine. “Many individuals facing this challenge are eager to seek treatment but struggle to access the care they need due to stigma and systemic barriers. The IMPACT Clinic will provide a supportive and comprehensive approach to treatment, helping patients navigate recovery while receiving essential medical and prenatal care.”
Recognizing the unique challenges and barriers to health care that pregnant women with substance use disorders face, ECU Health has assembled a multidisciplinary team to provide integrated treatment, including obstetric care, mental health services, lactation support, social work and educational resources. The clinic will also be serviced by medical residents to train future providers in addiction medicine and obstetrics and gynecology.
“The IMPACT Clinic headed up by Dr. David Ryan is a tremendous step forward in ECU Health’s Department of Obstetrics and Gynecology mission to make eastern North Carolina a better place for mothers and infants to be born and thrive,” said Dr. James Whiteside, department chair, Obstetrics and Gynecology, ECU Health and the Brody School of Medicine. “Given the significance mental health disorders have in maternal death and illness in North Carolina, it is essential these and related services are expanded.”
The IMPACT Clinic aims to improve outcomes for pregnant individuals in North Carolina, where substance-related mortality rates are concerning. According to the North Carolina Department of Health and Human Services from 2019-2020, one in four maternal deaths was attributed to unintentional overdose. With only five other programs in the state offering dedicated OBGYN addiction care within a single setting, ECU Health will become the sixth, filling a critical gap in resources for eastern North Carolina residents.
“Access to specialized health care is often limited in rural communities, and ECU Health is working to change that,” said Brian Floyd, chief operating officer, ECU Health. “By establishing the IMPACT Clinic, we are expanding essential addiction treatment and maternal health services in eastern North Carolina, ensuring that pregnant women receive expert, compassionate care without having to travel long distances. Initiatives like the IMPACT Clinic support our mission and help us build the national model for academic rural health care.”
The clinic began seeing patients on May 7, 2025, through referrals from OBGYN providers, including private practices and health departments. Services will be available to individuals actively experiencing substance use as well as those in recovery. Patients seeking more information about the IMPACT Clinic can call 252-744-2350.
Is There A Doctor On The Beach? NC Outer Banks A Tourism Hub, But A Health Care Desert

Is There A Doctor On The Beach? NC Outer Banks A Tourism Hub, But A Health Care Desert
(Carolina Public Press, Jane Winik Sartwell) — This summer, 5 million tourists will descend on 200 miles of remote North Carolina coastline. The Outer Banks are idyllic — and popular. But for both those visitors and the area’s 38,000 year-round residents, the vacation paradise has one serious problem: health care access.
Dare County Emergency Management Services evacuates about one person a day by helicopter. In the summer, that number can reach four or five.
Outer Banks Health Hospital in Nags Head, with its 21 beds, is the region’s lone hospital, and its capabilities and equipment are limited. The hospital evacuates another 15 to 30 people per month.
On the island of Ocracoke in nearby Hyde County, for example, a ride in a helicopter or ferry is required to reach any kind of specialty, intensive or emergency care. Travel time to the mainland in a ferry can reach three hours, and that’s if weather permits.
Some parts of the Outer Banks are more well-connected, but even there, travel times, and staffing shortages keep people from getting the care they need.
In an emergency, these limitations can result in life-threatening crises. It can take up to six hours for EMS services to respond to a call.
“We’re a rural area that deals with nonrural problems because of the amount of visitors we have,” Dare County EMS chief Jennie Collins told Carolina Public Press. “The population swells from 38,000 to 300,000 in the summer. Everyone that’s coming on vacation brings their problems with them.”
Tropical weather systems and storm surges create a further threat. The region’s singular artery, Highway 12, can flood, leaving residents completely cut off. Traveling over bridges in high winds poses its own dangers. And for a number of populated islands like Ocracoke, no road connects them to the rest of the world.
In the event of a storm surge, Hatteras residents rely on emergency ferries to transport them to beaches farther north, Roanoke Island or to the mainland.
The last time that happened was nearly 10 years ago, noted Sheila Davies, director of Dare County Health Department. But Atlantic hurricanes are getting more and more severe, due in part to warming ocean temperatures.
The area is popular with retirees, many of whom have cardiovascular diseases, lung cancer or other conditions that can cause moments of acute emergency.
Medical calls from people over 50 are the most common form of emergency calls to Dare County EMS, said Collins.
“A lot of times, someone’s doctor back home will say, ‘you need to go on vacation and rest and relax,’” Collins said. “So those people will come to the Outer Banks. And then they want to go for a walk on the beach. Well, that’s very much like a stress test.” And if it doesn’t go well, help is rarely at hand.
Qualified medical professionals don’t tend to move to the Outer Banks. The seasonal economy makes year-round practice financially difficult. The geographic isolation stunts career growth. Housing costs have skyrocketed due to vacation rentals, making it nearly impossible for physicians and nurses to afford living where they would practice.
For locals, this means that treating chronic conditions like diabetes and hypertension is rife with challenges. Dentists as well are few and far between.
The Outer Banks is defined in different ways, but the heart of the island system spans four counties: Currituck, Dare, Hyde and Carteret. Additional island communities farther south along the coast are less isolated. The health department of each plays a key role for folks living on or visiting the Outer Banks. They coordinate emergency responses, collect data on what services are most urgently needed and treat the uninsured.
But under the administration of President Donald Trump, $230 million in health funding for North Carolina is gone. One of the programs most dramatically gutted dealt with behavioral health for vulnerable populations. That funding cut is felt sorely on the local level.
“Services to Ocracoke are limited, mainly based on manpower and geography,” Gibbs said. “In fact, these services to the mainland are limited now based on manpower and funding.”
And what’s more, Outer Banks locals are plagued with rising instances of mental health problems and substance abuse.
“There is a certain amount of anxiety here all the time,” said Kathy Cooper, of the Outer Banks chapter of the National Alliance on Mental Illness. “Lives depend on how the tourist season goes. The rest of the year depends on May through September. Can they earn enough money this summer to get us through the winter?”
For the region’s youth, the situation can be dire.
“For kids growing up here, the only thing they want to do is get the hell off this rock,” Cooper continued. “There’s nothing here for youth. If you don’t surf or fish, you have a problem. And that problem usually ends up being substance abuse.”
On Ocracoke, alcoholism and substance abuse are of grave concern to the locals, Hyde County health director Luana Gibbs told CPP.
The hospital in Nags Head, Outer Banks Health, has no mental health beds. If someone is sent to the hospital under involuntary commitment, they have to find an open bed elsewhere in the state. And that could be as far as Asheville.
This gloom and anxiety factor disproportionately affects those working to keep the tourism economy afloat, and those service industry jobs don’t typically offer health insurance.
“We are seeing a growing number of mental health issues related to working in tourist related jobs such as restaurant and hospitality jobs,” said Linda Leiser, an administrator at Dare Community Clinic. “The American health care system is broken and puts the uninsured and underinsured at greater risk.”
A dearth of psychiatrists and licensed counselors at the clinic leaves some with a six-month wait to get an appointment.
Six months is a long time to wait for a suffering person on an isolated barrier island.
Duke Study Suggests Dosing of Heart Failure Medication Can be Safely Simplified

Duke Study Suggests Dosing of Heart Failure Medication Can be Safely Simplified
(Duke Health, Stephanie Lopez) — An estimated 32 million people globally have heart failure with reduced ejection fraction, a condition where the lower left chamber of the heart does a poor job of pumping blood to the rest of the body.
While there are approved medications for the condition, not all providers escalate patient doses to target levels, increasing the risk of adverse events, hospitalizations and death.
In a study led by a Duke scientist – presented at a late-breaking research session on May 17 at the 2025 European Society of Cardiology conference and to be published May 20 in the European Journal of Heart Failure – researchers found patients could safely start vericiguat (a medication for heart failure with reduced ejection fraction) at a dose of 5 mg instead of the conventional 2.5 mg starting dose, streamlining the process to reach target dosing from three steps to two.
The study was funded by Bayer AG and Merck Sharp & Dohme LLC, a subsidiary of Merck & Co., Inc. Both companies are makers of vericiguat.
Stephen Greene, M.D., is the corresponding author of the study and associate professor in the Department of Medicine in the Duke University School of Medicine. He said reducing the steps to target dosing could help overcome clinical inertia.
“In real-world practice, most patients never achieve the target doses of recommended heart failure medications,” Greene said. “Despite clinic visit after clinic visit, medication changes are relatively rare. If titration of heart failure medications is rare in clinical practice, then it stands to reason that reducing the number of titration steps would give our patients a better chance to ultimately achieve target dosing.”
The study enrolled 106 patients across seven countries who started the 5 mg dose of vericiguat over the course of two weeks. The researchers compared safety and tolerability of the higher dose group with those of study participants receiving the current dosing standard. The study found safety measures for both groups to be comparable, with more than 9 out of 10 patients safely tolerating initiation of vericiguat at the higher 5 mg starting dose.
“I think simplicity is the key when we talk about implementation of heart failure medications in clinical practice,” Greene said. “Real-world settings come with logistical challenges, and oftentimes clinics are very busy with limited appointment availability and limited available time per patient. These factors unfortunately set a stage for clinical inertia and for patients to go without important medication changes. Simplifying the way that we initiate and titrate heart failure medications may help overcome this and improve the quality of care our patients receive.”
In addition to Greene, study authors include Stefano Corda, Ciaran J. McMullan, Giovanni Palombo, Christina Schooss, Vanja Vlajnic, Katrin Walkamp, and Michele Senni.
Volunteering for a Cancer Clinical Trial: 5 Things Your Patients Should Know

Volunteering for a Cancer Clinical Trial: 5 Things Your Patients Should Know
(Atrium Health) — When facing a cancer diagnosis, many people hear about clinical trials but aren’t exactly sure what they involve. Are they safe? Will you still receive effective treatment? Who’s a candidate?
Oncology researchers at Atrium Health Levine Cancer share what they want everyone to know about the power of clinical trials—and why participating can make a real difference, both for current and future volunteers.
1. Clinical trials are responsible for nearly every major breakthrough in oncology
Every major advancement in cancer care—from immunotherapy to targeted therapies—exists today because of clinical trial research. Clinical trials are carefully designed studies that test new ways to prevent, detect, treat or manage cancer. Clinical trials aren’t a last resort; they play a vital role in shaping the future of cancer care and give participants access to highly personalized, expert treatment.
“Successfully completed cancer clinical trials are responsible for virtually all of the treatment and supportive care advances we have made over the past five decades,” says Dr. Glenn Lesser, deputy director, Atrium Health Wake Forest Baptist Comprehensive Cancer Center. “They have provided the evidence and support for us to incrementally improve the effectiveness of our treatment approaches and improve the survival outcomes for patients affected by cancer today.”
There are several different types of cancer clinical trials, including:
- Prevention trials that research strategies for preventing cancer, such as lifestyle changes or vaccines.
- Screening trials that look for ways to improve early detection methods.
- Treatment trials to study new drugs, surgical techniques, radiation approaches or therapy combinations. Treatment trials can also study new methods of using existing cancer treatments.
- Quality-of-life trials (also called palliative care and supportive care clinical trials) that focus on improving patient comfort and managing side effects.
Clinical trials aren’t just for people with advanced forms of cancer: there are research trials for people diagnosed with all stages of cancer.
Each trial has its own set of eligibility criteria, such as:
- Age
- Overall health
- Medical history
- Risk factors
- Treatment history
- Tumor genetic mutations
- Family medical history
Your doctor can help determine if you’re eligible to volunteer for a specific clinical trial.
2. Clinical trials are designed with safety and effectiveness in mind
Clinical trial treatments undergo rigorous lab testing before they are offered to volunteers. They’re designed with safety in mind and patients are closely monitored throughout the entire process.
“Clinical trial protocols are developed by experts and vetted by institutional review boards to ensure patient safety,” says Jai Patel, PharmD, associate vice president of translational research at Atrium Health Levine Cancer and associate director of shared resource management at Atrium Health Wake Forest Baptist Comprehensive Cancer Center. “The reason why a treatment, test or intervention is being evaluated is because there is strong evidence that it works better than the standard of care. This gives you, the patient, the chance to receive a novel intervention that could have better results than the standard treatment. It also helps to answer critical questions that could benefit future patients.”
One common misconception is that all participants receive placebos or “sugar pills” instead of treatment. In cancer clinical trials, placebos are used in limited settings such as when testing combinations of treatments or when no approved treatment exists. In this case, even when patients are randomized to “placebo”, they receive increased monitoring, labs, and visits to track their disease course.
Participation in clinical trials is entirely voluntary, and volunteers may withdraw from the trial at any time.
3. Clinical trials offer access to the latest advancements in cancer care
Participating in a clinical trial can give you access to new treatments before they are widely available.
“Clinical trials give patients access to the latest treatments, diagnostic techniques, screenings and approaches to cancer prevention,” says Dr. Bayard Powell, a medical oncologist and hematologist at Atrium Health Wake Forest Baptist Comprehensive Cancer Center and long-time section chief of hematology and oncology at Wake Forest University School of Medicine. “Participation in clinical trials can also have benefits for other areas of your health. This is especially true for prevention and screening trials.”
4. Volunteers receive support throughout the entire clinical trial process
Because clinical trials are led by top healthcare facilities and researchers, you’ll have access to highly specialized, expert care throughout your treatment. Many trials offer additional resources like patient navigators, social workers and support staff to guide you through each step of your treatment and recovery.
“Volunteers in clinical trials are closely monitored by a specialized medical team,” says Dr. Jimmy Ruiz, a medical oncologist and hematologist at Atrium Health Wake Forest Baptist Comprehensive Cancer Center. “This often means more frequent check-ins, lab work and imaging, leading to highly attentive, individualized care.”
5. Clinical trials give hope to others
When you participate in a clinical trial, you’re also giving hope to others in the future.
“Volunteering for a cancer clinical trial not only means giving you the chance at benefiting from a new treatment or intervention but also gives hope to others by advancing cancer research,” says Patel.
Participating in cancer research can also be incredibly empowering.
“The knowledge you gain can be shared with family and friends and therefore have a positive impact on their lives,” says Powell.
If you would like to learn more about volunteering for a cancer clinical trial, talk to your doctor or visit BeInvolved.AtriumHealth.org to learn more about the clinical trials available at Atrium Health.
Enhancing Support For Patients With Hearing Loss Through Medicaid Communication Access

Enhancing Support For Patients With Hearing Loss Through Medicaid Communication Access
May 21, 2025 | 12 PM–1 PM | Live Webinar
Join us for an upcoming virtual Lunch and Learn with the Division of Services for the Deaf and Hard of Hearing. Meet with the NC Medicaid Communication Access team to learn how you can support your patients with hearing loss and how to register and use the free resources available through the organization. This reimbursement program may help your medical practice with various incentives.
There is no registration fee for this webinar! Please note the registration will close two hours prior to the start of the event.
We look forward to connecting with you!
State Expands Student Loan Repayment For Rural Health Care Providers

State Expands Student Loan Repayment For Rural Health Care Providers
(The Transylvania Times) — To encourage more health care providers to serve in rural areas the N.C. Department of Health and Human Services is offering the opportunity for educational loan repayments. This program, known as the North Carolina Primary Care Physician Incentive, is available to qualifying physicians committed to delivering high-quality, comprehensive care in independent private practices in certain rural counties, according to a news release.
“We deeply value the dedication of our private practice physicians and recognize the essential role they play in ensuring health care access for our rural communities,” said North Carolina Health and Human Services Secretary Dev Sangvai. “Through this program, we aim to offset some of the financial burden and invest in our health care workforce, particularly in our rural counties.”
North Carolina’s rural population is the second largest in the country, reflecting nearly one in three people in the state and more than 4.6 million people live in rural counties. From maintaining healthy lifestyles to treating life-threatening illnesses, people depend on and trust their primary care physicians, the release said.
The N.C. Primary Care Physician Incentive is a part of $50 million in funding allocated by the North Carolina General Assembly to support health care providers, nurses and mental health services. Prior to 2025, independent private practices located in rural, medically underserved areas of the state were not deemed automatically eligible for the state-funded North Carolina Loan Repayment Program. In State Fiscal Year 2024, the NCDHHS Office of Rural Health received one-time funding to launch the incentive.
The program is open to primary care physicians in independent private practices located in Tier 1 and Tier 2 counties based on North Carolina’s County Distress Rankings. Eligible providers include family medicine, general internal medicine, general surgery (within critical access hospitals only), general pediatrics, obstetrics/gynecology or psychiatry physicians operating in these 80 counties.
Applications for the N.C. Primary Care Physician Incentive are now available, but funding is limited. Awards will be provided on a first-come, first-served basis for eligible and complete applications. NCDHHS will provide up to 16 awards in each of the six Medicaid Regions.
Gene Editing Helped A Desperately Ill Baby Thrive. Scientists Say It Could Someday Treat Millions

Gene Editing Helped A Desperately Ill Baby Thrive. Scientists Say It Could Someday Treat Millions
(Associated Press) — A baby born with a rare and dangerous genetic disease is growing and thriving after getting an experimental gene editing treatment made just for him.
Researchers described the case in a new study, saying he’s among the first to be successfully treated with a custom therapy that seeks to fix a tiny but critical error in his genetic code that kills half of affected infants. Though it may be a while before similar personalized treatments are available for others, doctors hope the technology can someday help the millions left behind even as genetic medicine has advanced because their conditions are so rare.
“This is the first step towards the use of gene editing therapies to treat a wide variety of rare genetic disorders for which there are currently no definitive medical treatments,” said Dr. Kiran Musunuru, a University of Pennsylvania gene editing expert who co-authored the study published Thursday in the New England Journal of Medicine.
The baby, KJ Muldoon of Clifton Heights, Pennsylvania, is one of 350 million people worldwide with rare diseases, most of which are genetic. He was diagnosed shortly after birth with severe CPS1 deficiency, estimated by some experts to affect around one in a million babies. Those infants lack an enzyme needed to help remove ammonia from the body, so it can build up in their blood and become toxic. A liver transplant is an option for some.
Knowing KJ’s odds, parents Kyle and Nicole Muldoon, both 34, worried they could lose him.
“We were, like, you know, weighing all the options, asking all the questions for either the liver transplant, which is invasive, or something that’s never been done before,” Nicole said.
“We prayed, we talked to people, we gathered information, and we eventually decided that this was the way we were going to go,” her husband added.

Within six months, the team at Children’s Hospital of Philadelphia and Penn Medicine, along with their partners, created a therapy designed to correct KJ’s faulty gene. They used CRISPR, the gene editing tool that won its inventors the Nobel Prize in 2020. Instead of cutting the DNA strand like the first CRISPR approaches, doctors employed a technique that flips the mutated DNA “letter” — also known as a base — to the correct type. Known as “base editing,” it reduces the risk of unintended genetic changes.
It’s “very exciting” that the team created the therapy so quickly, said gene therapy researcher Senthil Bhoopalan at St. Jude Children’s Research Hospital in Memphis, who wasn’t involved in the study. “This really sets the pace and the benchmark for such approaches.”
In February, KJ got his first IV infusion with the gene editing therapy, delivered through tiny fatty droplets called lipid nanoparticles that are taken up by liver cells.
While the room was abuzz with excitement that day, “he slept through the entire thing,” recalled study author Dr. Rebecca Ahrens-Nicklas, a gene therapy expert at CHOP.
After follow-up doses in March and April, KJ has been able to eat more normally and has recovered well from illnesses like colds, which can strain the body and exacerbate symptoms of CPS1. The 9 ½-month old also takes less medication.
Considering his poor prognosis earlier, “any time we see even the smallest milestone that he’s meeting – like a little wave or rolling over – that’s a big moment for us,” his mother said.
Still, researchers caution that it’s only been a few months. They’ll need to watch him for years.
“We’re still very much in the early stages of understanding what this medication may have done for KJ,” Ahrens-Nicklas said. “But every day, he’s showing us signs that he’s growing and thriving.”

Researchers hope what they learn from KJ will help other rare disease patients.
Gene therapies, which can be extremely expensive to develop, generally target more common disorders in part for simple financial reasons: more patients mean potentially more sales, which can help pay the development costs and generate more profit. The first CRISPR therapy approved by the U.S. Food and Drug Administration, for example, treats sickle cell disease, a painful blood disorder affecting millions worldwide.
Musunuru said his team’s work — funded in part by the National Institutes of Health — showed that creating a custom treatment doesn’t have to be prohibitively expensive. The cost was “not far off” from the $800,000-plus for an average liver transplant and related care, he said.
“As we get better and better at making these therapies and shorten the time frame even more, economies of scale will kick in and I would expect the costs to come down,” Musunuru said.
Scientists also won’t have to redo all the initial work every time they create a customized therapy, Bhoopalan said, so this research “sets the stage” for treating other rare conditions.
Carlos Moraes, a neurology professor at the University of Miami who wasn’t involved with the study, said research like this opens the door to more advances.
“Once someone comes with a breakthrough like this, it will take no time” for other teams to apply the lessons and move forward, he said. “There are barriers, but I predict that they are going to be crossed in the next five to 10 years. Then the whole field will move as a block because we’re pretty much ready.”
Tips For Staying Alive, Decades In The Making

Tips For Staying Alive, Decades In The Making
(The Harvard Gazette, Alvin Powell) — When it comes to the idea that prevention is the best medicine, JoAnn Manson doesn’t mess around.
Since the 1980s, Manson has dedicated her career to teasing out complex threads of human health, with an emphasis on factors under our control: physical activity, diet, sleep, smoking, alcohol consumption, medications such as menopausal hormone therapy, low-dose aspirin, statins, and, most recently, vitamins and other dietary supplements.
“Ever since my early years of medical training, I’ve been astounded by the powerful role of modifiable lifestyle factors as bulwarks against chronic disease,” said Manson, who is the Michael and Lee Bell Endowed Professor of Women’s Health at Harvard Medical School, chief of the Division of Preventive Medicine at Brigham and Women’s Hospital, and a professor of epidemiology at the Harvard Chan School. “I became motivated to devote my research career to testing interventions to reduce chronic disease burden, extend years of good health or ‘healthspan,’ and to try to decrease premature mortality.”
“Ever since my early years of medical training, I’ve been astounded by the powerful role of modifiable lifestyle factors as bulwarks against chronic disease.”
A scan of Manson’s publication history — one major database of medical research returns more than 1,800 hits on her name — reads like a list of national health headlines over the past 20 years: menopausal hormone therapy and cardiovascular disease and breast cancer; passive smoking in the workplace; walking versus vigorous exercise in prevention of heart disease; steps per day and cancer risk; pre-pandemic physical activity and COVID severity. A member of the National Academy of Medicine, she is listed by Research.com as the world’s top female scientist based on citation metrics, with more than 369,000 citations and an h-index, which reflects the scope and influence of her work, of 310.
Her tools have been major randomized prevention trials and large longitudinal studies that follow tens of thousands of people over time, gathering health, diet, and behavioral data, often augmented by blood, tissue, and other physical samples that enrich the picture and provide physical evidence of changes reported by participants. Many of these initiatives have received support from the federal government.
Manson’s research began with the landmark Nurses’ Health Study, which launched in 1976, when most study subjects were white males, and sought to fill gaps around women’s health. The decadeslong study, established by Brigham and Harvard investigators to explore links between contraceptive use, smoking, heart disease, and cancer, expanded over time to provide a broad view of lifestyle and health. Manson has been involved with the project since the mid-1980s and has been a principal investigator of the cardiovascular component for 26 years.
In 1993, Manson became one of the initial principal investigators of a National Institutes of Health-backed study called the Women’s Health Initiative, which enrolled 160,000 postmenopausal women in three large, randomized trials, along with an investigation of major causes of chronic disease and mortality in older women, including cardiovascular disease, cancer, and osteoporosis. Manson leads the study’s clinical center in Boston.
More recently, she has focused on what she has described as the “Wild West” of American healthcare — dietary supplements, whose health claims and distribution are unchecked and unregulated. In the nationwide VITAL randomized trial of 25,000 men and women 50 and older, she and colleagues investigated health claims about vitamin D and omega-3 fatty acids, reporting in 2018 that omega-3 fatty acids in fish oil were associated with a 28 percent reduction in heart attack. The effect was even higher among those who reported minimal fish in their diet, cutting risk about 40 percent. For vitamin D, there appeared to be little effect on heart disease, but a significant 17 percent reduction in advanced cancer, and a 22 percent reduction in autoimmune diseases.
A more recent randomized trial, COSMOS, the COcoa Supplement and Multivitamin Outcome Study, investigated links between cocoa flavanols — the major ingredient in dark chocolate — multivitamins, and health impacts, including effects related to cognition. In 2023 and 2024 it linked the humble daily multivitamin to benefits for cognitive aging and a reduction in cognitive decline, with consistent findings in three separate placebo-controlled studies in COSMOS.
Manson, like all health researchers, is keeping a wary eye on cuts to federal research funding. (A halt to support for the Women’s Health Initiative was reversed after an outcry.) Her own funding hasn’t been affected, though proposed cuts to indirect research costs would have a significant impact, as studies like VITAL and COSMOS have major infrastructure and blood repository costs. She’s concerned about cutbacks beyond her own division’s research, because they will have broad impact on science and prevention nationally, as well as on training programs and pipelines for future generations of scientists.
“It’s distressing what’s happening,” Manson said. “We’re very concerned, obviously, about our faculty and staff supported by federal funding, but it really goes far beyond the impact on any individual division or research program. It’s really the nationwide, and even global, impact on the scientific enterprise and population health.”
Innovative Birth Simulation Mobile Training Unit Enhances Maternal Care

Innovative Birth Simulation Mobile Training Unit Enhances Maternal Care
(Atrium Health) — Atrium Health's Birth Simulation Mobile Training Unit is revolutionizing maternal care by providing hands-on training to health care professionals. This state-of-the-art mobile unit travels to our labor and delivery hospitals, offering realistic birth simulations that help improve skills and preparedness for real-life scenarios.
The Atrium Health's Birth Simulation Mobile Training Unit is designed to train health care providers on how to care for both moms and babies during childbirth emergencies, such as shoulder dystocia, when the baby's shoulder wedges in the pelvis after the baby's head is born.
This collaborative effort between Atrium Health Women’s Care, Atrium Health Levine Children’s Hospital and Carolinas Simulation Center promotes quality and patient safety through high-tech, mannequin-based simulation education. The simulator allows Atrium Health teammates to practice real-life scenarios in a safe environment, enhancing their skills, comfort and confidence. Watch how this cutting-edge tool is making a difference in our commitment to exceptional patient care.
Watch the video here
Duke Helps Young Adults Move Forward After Cancer

Duke Helps Young Adults Move Forward After Cancer
(Duke University School of Medicine, Mary-Russell Roberson and Angela Spivey)— At age 34, Iris Bugbee, of Fuquay-Varina, NC, faced more than a breast cancer diagnosis. She juggled full-time work as a speech-language pathologist while raising her two-year-old daughter, Mila. After taking six weeks off for surgery, she continued working through cancer treatments, adjusting her hours but never stepping away.
She fit in radiation appointments at Duke Women’s Cancer Care Raleigh between her patient sessions. “I’d go to work, travel to Raleigh, and then come back and see the rest of my patients,” she said. Balancing treatment, her patients, and parenting, “I didn’t think a whole lot about my own treatment and diagnosis.”

A year after her mastectomy, a nurse invited her to join a clinical trial testing a structured support program for young adult cancer survivors. Bugbee agreed, hoping to regain strength and she saw it as a good source of motivation. Before surgery, she exercised regularly, but since then, she had struggled with cording syndrome which limited mobility in her right arm and made everyday tasks like picking up her daughter or typing at work challenging.
The program guided her through goal setting, gradual strength-building, and self-compassion. “That’s when I started walking, stretching, and slowly rebuilding,” she said.
Beyond physical recovery, the sessions helped her process her experience. The online support group felt more like conversations with peers than a mandatory class, and psychologists who ran the program made sharing easier.
“It was reassuring to hear from other cancer survivors who are in the middle of this part of their life – raising a family or in the middle of their careers,” Bugbee said. “Hearing everyone’s experiences and their challenges made me feel like, ‘Okay, yeah, I’m not the only one.’ ”
A Life Interrupted
Being diagnosed with cancer and going through treatment isn’t easy for anyone. For those diagnosed as young adults, ages 18-39, cancer brings unique challenges.

“This is a time of transition,” said Caroline Dorfman, PhD, a clinical psychologist at the Duke Cancer Institute and an associate professor in psychiatry and behavioral sciences. Many young adults are focused on milestones—graduation, career growth, marriage, parenthood—when a cancer diagnosis suddenly halts their momentum.
Even after treatment, life doesn’t suddenly switch back to normal. Physical symptoms like pain and fatigue can linger and emotional distress is common in the post-treatment period. Frequent follow-ups add financial and logistical burdens while serving as constant reminders of illness.
“Sometimes they just want the cancer behind them, and to get back to doing what matters to them,” Dorfman said. “The trouble is that when they are in the midst of treatment, they are just trying to get through it, and they don’t stop to process the experience.”
To support young adults in this vulnerable phase, Dorfman designed a 10-week program to help them navigate post-treatment challenges and successfully manage their new lives as cancer survivors.
Listening to Survivors
Dorfman’s interest in the psychological impact of cancer began early. When her mother was diagnosed with breast cancer during Dorfman’s middle school years, she observed how different family members coped. Later, in graduate school, she focused on behavioral interventions to improve cancer patients’ emotional well-being.

As a clinical psychology intern at Duke, she saw a gap in support for young adults: it became apparent that they could benefit from a structured system of post-treatment support tailored to their stage of life.
So, she decided to design and test a program to do that.
Dorfman’s post-treatment curriculum teaches strategies to manage pain, fatigue, and emotional distress through relaxation techniques, goal-setting, strategies to improve self-talk, home-based exercise, and values-driven decision-making. It also includes strategies for improved conversations with family, friends, employers, and health care providers.
“We can educate patients on how normal it is to have continued symptom burden and how normal it is to feel like they are not achieving goals in the way they would like,” she said. “And we can provide them with tools to help them move forward on the important goals they have for their lives while navigating symptoms.”
The content is delivered through eight 90-minute virtual group sessions, supplemented by written materials and a mobile app.
Dorfman secured a grant from the National Institutes of Health in 2019 to pilot the project with mentorship from Kevin Oeffinger, MD, professor in the Department of Medicine, and Rebecca Shelby, PhD, associate professor in the Department of Psychiatry and Behavioral Sciences.

Oeffinger, a family physician who has worked with young adult cancer survivors for 35 years, said post-treatment symptoms in this group have been overlooked. “Caroline is trying to fill that gap, both in her clinical program and her research program. What she is doing is incredibly important.”
Before designing the program, Dorfman interviewed young adult survivors and oncologists to identify key post-treatment struggles. Pain, fatigue, and emotional distress topped the list.
Survivors also wanted guidance on communicating their needs—whether to family, employers, or doctors. Many had never navigated the healthcare system independently before their diagnosis.
“Some had never needed primary care before cancer,” Oeffinger said. “Now they suddenly face new short- and long-term health risks and need to engage with the health care system.”
Young survivors also sought advice on requesting workplace or academic accommodations. In response, Dorfman built assertive communication training into the program. “Sometimes people in their social network said things that were really unhelpful,” Dorfman said. Survivors learned how to identify supportive people in their network and how to effectively ask for what they need.
Building on What Works
The pilot program enrolled 61 participants, and the results were encouraging. Not only did participants like the program, and would recommend it to other people, but their symptoms become less burdensome.
An important feature of Dorfman’s program is the delivery as a package of sessions, each of which builds on the one before. At the Duke Cancer Center, young adult cancer survivors, like all cancer survivors, already have a wealth of supports in place, from support groups to individual counseling. But these resources are offered a la carte and on-demand; it’s up to each patient to pick and choose.
Dorfman’s program stands out because it’s structured as a curriculum that covers a range of skills and topics unveiled over several weeks. “What’s unique is the packaging,” she said. “These strategies in this combination have not been evaluated before.”
Now, with a five-year NIH grant, she’s expanding the program to 250 participants. Based on the pilot feedback, Dorfman plans to tweak a few details -- reducing the number of sessions to six, shifting to one-on-one formats for flexibility, and adding more strategies to help participants gain confidence in taking an active role in their ongoing medical care.
If the program proves to be effective in this larger group, Dorfman hopes it will be used regularly as part of the Duke Cancer Patient Support Program – and beyond.
Novant Health Initiative To Capitalize On The Healing Power Of The Arts

Novant Health Initiative To Capitalize On The Healing Power Of The Arts
(QC Nerve, Ryan Pitkin and Annie Keough)— Pablo Picasso once said, “Art washes away from the soul the dust of everyday life.” One new local art exhibit, however, is challenging that very notion.
In A Slice of Life: The Art of Everyday, local artists draw from the everyday moments and mementos that one may brush off as the dust, debris or detritus of monotony and instead focus in on its beauty and grace.
Fittingly, the exhibit is not showing in a flashy gallery in South End or a lounge in Uptown but on the walls of a cafeteria inside Novant Health Presbyterian Medical Center in the Elizabeth neighborhood, the Charlotte area’s second largest hospital.
Being a patient in care or watching someone you love go through care can become incredibly stressful, said Kristen Howard, VP of corporate affairs at Novant.
“By having these pieces [bring] life and interest and a break from what is happening in your clinical room when you come down to the cafeteria, it’s just an opportunity to step back, take a deep reach and increase that opportunity for healing,” she told Queen City Nerve.
Curated in partnership with nonprofit arts organization Charlotte is Creative, A Slice of Life is just one of many projects underway as part of Novant’s new Art of Remarkable Care initiative. The health care company announced the initiative’s launch in April with a $500,000 investment to explore the connection between art and healing.

With partnerships already in the works with The Bechtler Museum of Modern Art, the Harvey B. Gantt Center for African American Arts + Culture, Charlotte Ballet and the Charlotte Symphony, Novant also plans to expand its focus on arts in its facilities, as with A Slice of Life.
The not-for-profit health care system will partner with Charlotte Is Creative to activate arts programming at seven facilities in the coming months, including hospitals and health centers in Ballantyne, Huntersville, Matthews, Mint Hill and Rowan County.
“Our goal is to create a healthier future for Charlotte, and we recognize that well-being requires more than traditional medicine,” stated Dr. Sid Fletcher, senior vice president of the Novant system and president in the Charlotte region, in announcing the new initiative. “We have seen firsthand the remarkable impact art can have on our patients and their loved ones, and we’re proud to extend the reach of our local artists to create spaces of comfort and connection.
“Art is powerful; it can inspire healing, and when paired with the incredible expertise of our doctors and nurses, it can be transformative,” Fletcher continued. “This initiative, as well as our partnerships with the Charlotte Symphony and others, is part of our larger commitment to ensure our patients thrive.”
Curating A Slice of Life
Studies have shown exposure to and participation in the arts can play a role in lessening the severity of chronic pain, stress and anxiety. According to the American Journal of Public Health, consistent interaction with art, including intentionally listening to music, has been shown to increase immune system responsiveness.
Shana Templin, art support coordinator with Novant and an artist herself, first suggested that her employer offer local artists the chance to display their work for free in Novant Presbyterian’s cafeteria.
As an inevitable hub for hospital patients, family members and staff, Templin wanted to tap into a communal theme for the art, something that engaged a shared human experience, explained Tim Miner, co-founder of Charlotte Is Creative (CIC).

CIC has operated in the Charlotte arts market for almost 10 years providing programs, resources, training, connections and opportunities to emerging artists and creative entrepreneurs. The nonprofit also deals in project management, assisting companies and organizations to support the artistic community, which is how Miner came to be working with Templin.
“When we look at what our lives are in the everyday, that’s something that she was hoping was relational and could be a uniting factor for people while at the same time recognizing that everybody has a different vantage point and comes from a different background,” Miner said of Templin.
CIC helped Novant put out a call for art that lasted from April 23-May 7, inviting artists to submit up to two 2D artworks that celebrate the art of everyday life.
“This exhibit explores the extraordinary within the ordinary, showcasing works that highlight the charm, complexity and significance of everyday experiences,” the call read.
When we spoke to Howard on the last day of the call, there were about 230 submissions vying for 30 spots. Because the selected pieces in the exhibit will be for sale, with each artist maintaining 100% of any proceeds — Howard’s team is considering each work as it’s sold until the exhibit runs its course over six months.
A win-win for the arts community
As the fifth-largest employer in the Charlotte metro area, leadership is aware of the company’s responsibility to lead by example in a rapidly growing city, explained Howard.
“We understand that our commitment to health has to go beyond our clinic walls and we try to invest in the community as a whole,” she said.
Art of Remarkable Care is about more than just beautification for the sake of a more wraparound approach to health and healing; it’s also about funding an arts scene that is growing with the city around it but often doing so under financial constraints.

The new initiative not only allows Novant to support local artists and the economy by investing in works of art and paying performers to share their talents in its facilities, but to support more widespread arts programming around the city.
In collaboration with Charlotte Is Creative, Novant plans to offer many points of connection for local artists in the coming months including visual and performance art, art therapy, murals and wall art installations, and community-based arts events for vulnerable populations.
This is the aspect that got Miner and his team excited.
”There’s a true opportunity here to take [groups of artists] and present them opportunities inside of an unexpected place — in this case, a hospital facility — to do creative work, show off what they do, but also maybe interact with the various audiences that are in the facilities,” he said.
On top of working with individual artists to establish foundational skills, funding, social networks and promotional training, CIC hosts a wide array of innovative arts-centered events and programming.
That includes its monthly Creative Mornings gatherings; its Creative Entrepreneurs Initiative cohort, which provides business training and grant writing advice to local creatives; Charlotte Reciprocity Circles, which are billed as live, facilitated social capital exchange events; and the self-explanatory Coffee with Creatives.
Since 2017, CIC has distributed nearly 500 $250 grants from its HUG micro-grant program.
CIC’s mission is to broaden the opportunities and experiences that emerging creative entrepreneurs have, Miner said. The organization also provides artists with space to create by purchasing studio space at the McColl Center in four increments.
Read more: Divine Barrel Uplifts Local Arts Scene With Mural Collab
Working in multiple Novant facilities, including the 590-bed hospital where A Slice of Life is set to open, allows CIC a chance to help connect local artists with what is likely a larger audience than all of those opportunities combined.
“When people need to go into a hospital, they have trepidation or they’re dealing with something that’s very potentially traumatic or upsetting,” Miner said. “To be able to provide a work of art — be it a performance, or a piece of visual art or even a hands-on experience that lets them feel more at ease and feel more comfortable and repair their soul to a certain degree — that’s powerful.”
U.S. Overdose Deaths Fell 27% Last Year But Remain Above Pre-Pandemic Levels

U.S. Overdose Deaths Fell 27% Last Year But Remain Above Pre-Pandemic Levels
(The Associated Press) — There were 30,000 fewer U.S. drug overdose deaths in 2024 than the year before — the largest one-year decline ever recorded.
An estimated 80,000 people died from overdoses last year, according to provisional Centers for Disease Control and Prevention data released Wednesday. That’s down 27% from the 110,000 in 2023.
The CDC has been collecting comparable data for 45 years. The previous largest one-year drop was 4% in 2018, according to the agency’s National Center for Health Statistics.
All but two states saw declines last year — with some of the biggest in Ohio, West Virginia and other states that have been hard-hit in the nation’s decades-long overdose epidemic.
Experts say more research needs to be done to understand what drove the reduction, but they mention several possible factors. Among the most cited:
- Increased availability of the overdose-reversing drug naloxone.
- Expanded addiction treatment.
- Shifts in how people use drugs.
- The growing impact of billions of dollars in opioid lawsuit settlement money.
- The number of at-risk Americans is shrinking, after waves of deaths in older adults and a shift in teens and younger adults away from the drugs that cause most deaths.
Still, annual overdose deaths are higher than they were before the COVID-19 pandemic. And some experts worry that the recent decline could be slowed or stopped by reductions in federal funding and the public health workforce, or a shift away from the strategies that seem to be working.

“Now is not the time to take the foot off the gas pedal,” said Dr. Daniel Ciccarone, a drug policy expert at the University of California, San Francisco.
The provisional numbers are estimates of everyone who died of overdoses in the U.S., including noncitizens. That data is still being processed, and the final numbers can sometimes differ a bit. But it’s clear that there was a huge drop last year.
Experts note that there have been past moments when U.S. overdose deaths seemed to have plateaued or even started to go down, only to rise again. That happened in 2018.
But there are reasons to be optimistic.
Naloxone has become more widely available, in part because of the introduction of over-the-counter versions that don’t require prescriptions.
Meanwhile, drug manufacturers, distributors, pharmacy chains and other businesses have settled lawsuits with state and local governments over the painkillers that were a main driver of overdose deaths in the past. The deals over the last decade or so have promised about $50 billion over time, with most of it required to be used to fight addiction.
Another settlement that would be among the largest, with members of the Sackler family who own OxyContin maker Purdue Pharma agreeing to pay up to $7 billion, could be approved this year.
The money, along with federal taxpayer funding, is going to a variety of programs, including supportive housing and harm reduction efforts, such as providing materials to test drugs for fentanyl, the biggest driver of overdoses now.
But what each state will do with that money is currently at issue. “States can either say, ‘We won, we can walk away’” in the wake of the declines or they can use the lawsuit money on naloxone and other efforts, said Regina LaBelle, a former acting director of the Office of National Drug Control Policy. She now heads an addiction and public policy program at Georgetown University.
President Donald Trump’s administration views opioids as largely a law enforcement issue and as a reason to step up border security. That worries many public health leaders and advocates.
“We believe that taking a public health approach that seeks to support — not punish — people who use drugs is crucial to ending the overdose crisis,” said Dr. Tamara Olt, an Illinois woman whose 16-year-old son died of a heroin overdose in 2012. She is now executive director of Broken No Moore, an advocacy organization focused on substance use disorder.
Olt attributes recent declines to the growing availability of naloxone, work to make treatment available, and wider awareness of the problem.
Kimberly Douglas, an Illinois whose 17-year-old son died of an overdose in 2023, credited the growing chorus of grieving mothers. “Eventually people are going to start listening. Unfortunately, it’s taken 10-plus years.”
NCWorks Prepares Young Professionals With The Skills And Knowledge For Careers In Health Care

NCWorks Prepares Young Professionals With The Skills And Knowledge For Careers In Health Care
(ECU Health) — NCWorks is an initiative through the state of North Carolina for young adults aged 18 to 24 who are interested in exploring careers in health care. The program brings together various statewide agencies including the Department of Commerce, Public Instruction and the NC community college system to create opportunities for young jobseekers to find employment.
NCWorks offers tools, resources and knowledge needed to build a strong foundation for participants to begin their career. ECU Health is one of many work sites across the state for the NCWorks program.
In addition to helping young adults gain valuable skills, the program also creates a pipeline of talent that potentially leads to participants becoming members of the ECU Health team. By equipping young professionals for success, ECU Health strengthens its workforce and contributes to the local community by acting on the mission of improving the health and well-being of eastern North Carolina.
The program runs for approximately three months during which participants are part-time team members at ECU Health, gaining hands-on experience in a health care setting. During these three months, they learn about roles in health care from their fellow team members.
Throughout the program, participants are supported with continuous coaching from the workforce development team through learning skills and receiving guidance to help them thrive in professional environments. Both technical and soft skills are important for working in a professional environment and the program helps them develop and navigate these skills.
Program participants also receive guidance and mentorship from current ECU Health team members to learn the ins-and-outs of the workplace. At the end of the program, participants understand the importance of ECU Health’s mission, vision and values and have embedded that into their daily work.
Kara Dozier, a member of the Food and Nutrition Services team, is currently serving as an ambassador and the first participant of the NCWorks Project at ECU Health.
Kara got involved in the program when she met Toyta Kee, a talent pipeline consultant at ECU Health, at a job fair at the Greenville Convention Center. “I saw Ms. Toyta’s ECU Health sign and decided I’m going to talk to her and see what this is about. I did, and I gave her my application that I had printed out, and she said she would contact me,” Kara said.
Kara reached out to Toyta and got connected with the NCWorks program, which Kara has now been a part of since October 2024.
“Overall, my favorite thing about the program is it allows me to be more self-sufficient and provides a great opportunity for different positions at ECU Health,” she says, “I definitely would recommend this program to everybody who’s interested because it is a great opportunity for anybody who wants to get their foot into the ECU Health door!”
Free 'Mega Clinic' In Asheville To Offer Medical, Dental, And Vision Care In June

Free 'Mega Clinic' In Asheville To Offer Medical, Dental, And Vision Care In June
(WSPA, Joanna Johnson) — A mega clinic will be hosted in downtown Asheville next month, offering free services to anyone in need.
Liberty and Health Alliance, a registered 501(c)(3) nonprofit organization, is offering all people access to free medical, dental and vision care from June 4 through 6. It will be held from 9 a.m. to 5 p.m., each day.
Attendees will have the opportunity to receive pap smears, back-to-school physicals, medical evaluations, fillings, dental extractions, eye exams, counseling, haircuts and much more.
Those interested do not need to sign up to seek treatment. Officials said the mega clinic is first come, first serve.
Parking is not included.
All services are 100% free, provided by licensed medical volunteers, throughout the county. The mega clinic will be hosted at the Harrah’s Cherokee Center, 87 Haywood Street, in Asheville.
To learn more, visit their website. If you are not in need of medical service but want to donate, volunteer, or learn about the organization you can here.
Annunziato (Ned) Amendola Installed As President Of The American Academy Of Orthopaedic Surgeons

Annunziato (Ned) Amendola Installed As President Of The American Academy Of Orthopaedic Surgeons
The American Academy of Orthopaedic Surgeons (AAOS) announced Annunziato (Ned) Amendola, MD, FAAOS, FRCSC, DABOS, as its new president. Dr. Amendola, professor of orthopaedic surgery and chief of sports medicine at Duke University, assumed leadership of the AAOS at the recent AAOS 2025 Annual Meeting in San Diego. His presidency marks the third in a four-year term of volunteer service, after serving as a vice president of the AAOS for the previous two years.

Dr. Amendola leads Duke’s sports medicine program, a position he has held since 2015, while serving as executive director of the James R. Urbaniak, MD, Sports Sciences Institute in Durham, N.C. As the Virginia Flowers Baker Distinguished Professor, he also maintains his role as head team physician and chief medical officer for Duke Athletics.
Campbell University Selected As NC AHEC Teaching Hub

(Campbell University) — Campbell University’s Community Care Clinic was selected as one of four interprofessional teaching hubs in North Carolina, thanks to the North Carolina Area Health Education Centers (NC AHEC) Rural Hub Grant. The program, funded by the North Carolina state legislature and NC AHEC, supports the development of rural, community-based interprofessional clinical training sites across the state.
Led by Dr. Paige Brown, director of Doctor of Health Sciences, the Campbell team successfully secured grant funding to enhance interprofessional education at clinic sites in Dunn and Harnett County. Currently, these sites host medical students, residents, pharmacy students and physician assistant students in a collaborative, team-based care setting. The initiative aims to improve healthcare access in underserved rural communities by training and retaining a robust primary care workforce.
On April 30, representatives from NC AHEC and Southern Regional AHEC visited Campbell’s Dunn location to tour the clinic and review the first six months of the grant project. The visit included discussions around the benefits and barriers of interprofessional teaching clinics, as well as plans to expand participation to other disciplines such as physical therapy, nursing, public health, and even high school-level shadowing opportunities.
The four selected teaching hubs across the state include:
- Campbell University Community Care Clinic (Dunn and Harnett County)
- Atrium Health/Wake Forest (Randolph, Cleveland, and Stanly Counties)
- Ocracoke Health Center (Dare and Hyde Counties)
- Roanoke Chowan Community Health Center (Hertford, Bertie, Northampton, and Washington Counties)
NC AHEC’s Rural Hub Grant program was developed through the collaboration of statewide stakeholders in education and healthcare. The initiative is designed to prioritize team-based, rural health education models that improve access to quality care where it is most needed.
Visiting AHEC Representatives:
- Dr. Adam Zolotor, UNC-Chapel Hill Department of Family Medicine
- Dr. Nicole Pinelli Reitter, Executive Director for Interprofessional Collaborative Practice, Office of the Provost, UNC-Chapel Hill
- Elyssa Tucker, Health Professions Student Liaison, NC AHEC
Campbell University Hosts:
- Joe Cacioppo, director of Community and Global Health
- Pamela Edwards, director of Interprofessional Education, co-PI of the NC Teaching Hub project
Some Bad News And Some Good News: Rural Maternity Wards Are Closing, But Siler City Opened A New One

Some Bad News And Some Good News: Rural Maternity Wards Are Closing, But Siler City Opened A New One
(Carolina Public Press)— Over the last decade, 10 hospitals have eliminated maternity care in North Carolina. Just one has added it: UNC Health Chatham in Siler City.
The Chatham County center serves as a rare counterexample to the wave of rural maternity closures across the state. That’s where a stark divide has emerged: While hospitals in cities like Charlotte and Raleigh have added dozens of new delivery rooms, many rural facilities have shuttered or downsized their units, citing financial struggles.
It’s a growing problem that was first detailed in Deserting Women, a three-part Carolina Public Press investigation in March that examined state data on every North Carolina hospital over the last decade. CPP found that hospital systems have systematically centralized services in urban areas while cutting them in rural ones. Some rural hospitals have also cut or reduced certain critical OB/GYN services, leaving women more vulnerable to complications.
But not in Siler City. There, much unlike other health systems, the responsibility of maternity care falls to family medicine doctors rather than more specialized practitioners. And the growing number of women giving birth at UNC Health Chatham in the past few years shows that the maternity center is fulfilling a need.
The question remains whether this model can be replicated in rural areas across the state.
‘Everything shut down’
The labor and delivery unit at UNC Health Chatham originally closed in 1991. Nearly 30 years later, the ribbon was cut on a brand new maternity care center.
But the center’s survival has been fraught with challenges. The shock of a global pandemic, low numbers of women giving birth and staffing shortages nearly forced its closure just a year after it opened. Now, it’s out on the other side — and largely an anomaly in a changing rural medical landscape.
Most rural North Carolina hospitals frame the elimination of services for mothers-to-be as a financial inevitability. In Siler City, UNC Health Chatham proved that is not the case.
The idea came out of a rural residency program that Andy Hannapel, a family medicine doctor for UNC Health, was running in Chatham County.
The proposal offered a chance not only to address the gap in maternity services, but also to test a new model of care. Unlike most hospitals that rely on specialized OB/GYNs, UNC Health Chatham primarily uses family medicine physicians to perform maternity care. That’s because OB/GYNs are specialists. They cannot treat general patients, making them an expensive and inflexible option for rural hospitals.
In 2019, UNC Health approved the plan, investing $2.6 million to renovate an existing wing of Chatham Hospital into a five-bed maternity care center.
Then came the pandemic.
“We started construction and two weeks later, everything shut down,” Hannapel recalled.
Almost the end for UNC Health Chatham
Birth rates dropped. Women weren’t getting pregnant when it seemed like the world was ending.
That presented a problem. If births fall but the hospital maintains the same level of service, the per-birth cost of staffing and equipment increases significantly, causing financial strain for the hospital. It’s a major reason why so many rural hospitals end up eliminating maternity services.
But birth rates weren’t the only thing in decline. Staffing also took a hit. A big one.
“We had a lot of nurses that were leaving,” said Jeffery Strickler, president of UNC Health Chatham, “and it became very difficult to staff our unit.”
Tough choices had to be made. The center could no longer stay open day and night. By winter 2021, the facility began shutting down over the weekend.
The reduced hours had a predictable effect: Many women chose to seek care elsewhere for fear that they would go into labor and the unit would be closed.
A coalition of Chatham County community members was formed to find a way forward and commit to the center’s long-term viability. One of these community members was Casey Hilliard, a project manager for the organization Equity for Moms and Babies Realized Across Chatham.
“Based on financial metrics, the center was ready to close,” Hilliard said. “But they decided to turn away from only considering the financial metrics, and instead, decided to collaborate with the community. With that strategy, almost four years later, they’ve been able to sustain the maternity care center.”
Oh, babies
Ultimately, parent company UNC Health provided the hospital with $250,000 to hire contract nurses to fill the gaps in staffing.
After that, things started to improve.
In the years since the height of the pandemic, the number of births at UNC Health Chatham’s maternity care center has steadily increased. In 2022, 124 babies were born.
In 2023, 140 babies were delivered.
In 2024, it was 180.
Projections for 2025 forecast between 230 and 240 babies.
The rising number of births at the hospital runs counter to the conventional narrative that women are having fewer babies across the nation. But the increase is due to the focus on creating a pipeline of patients: having other doctors refer them to the center, and working to attract women with marketing and messaging.
Folks in Chatham County credit UNC Health’s financial support for allowing the hospital to do the improbable. But it’s unclear why UNC Health supported maternity care in Chatham County while simultaneously letting it fall elsewhere. Just a year before the maternity care center in Siler City opened, labor and delivery services were eliminated at UNC Health Caldwell in Lenoir.
Whatever the reason for the system’s support in Chatham County, it’s working. The average travel distance for pregnant women seeking health care was reduced from 35 miles to 16 miles, according to Hannapel. And he says women are becoming more satisfied with the care they’re receiving.
“We really have emphasized being partners with women, not telling them what to do,” Hannapel said. “They have agency. They have the ability to decide. They have options. It’s about building a safe and welcoming environment, where women have a voice and they’re listened to.”
How A Little-Known Protein Powers Energy Production And Fights Cancer

How A Little-Known Protein Powers Energy Production And Fights Cancer
(Duke University School of Medicine, Shantell M. Kirkendoll) — A Duke University School of Medicine study reshapes what scientists know about how our cells generate energy and fend off cancer.
The Nature Cell Biology study led by cancer researcher Hui-Kuan Lin, PhD reveals an unexpected role for the protein ALDH4A1 in energy production. Without it, cells shift into a survival mode linked to cancer growth.
The discovery not only transforms scientific understanding of cellular metabolism but also points to a promising new target for cancer treatment.
“By connecting ALDH4A1 to both energy production and tumor suppression, we have a clearer picture of why cancer cells behave the way they do,” said Lin, the senior study author who is a professor and director of prostate cancer research in the Department of Pathology and professor of pharmacology and cancer biology at Duke School of Medicine.
At the heart of the discovery is pyruvate, a molecule that helps power cells. Pyruvate is produced when the body breaks down glucose and is a key player in energy production. But for pyruvate to do its job, it must first enter the mitochondria—often called the cell’s power plants—where it fuels the TCA cycle, a process that generates energy.
This transport relies on the mitochondrial pyruvate carrier (MPC), a system made up of two proteins, MPC1 and MPC2. Until now, scientists believed those were the only proteins involved. But Duke researchers have discovered that ALDH4A1 is a critical third component. It helps stabilize and maintain the active MPC complex, ensuring pyruvate gets where it needs to go.
Without ALDH4A1, the system breaks down. Pyruvate can’t reach the mitochondria, forcing cells into survival mode. In the new study, researchers reveal ALDH4A1 acts as a tumor suppressor by preventing cells from switching to a less efficient, backup energy process called the Warburg effect that’s often seen in cancer cells.
“Our study provides the molecular basis of why cancer cells often display defective mitochondrial activity,” said Lin, a member of the Duke Cancer Institute.
ALDH4A1 is part of a family of proline metabolic enzymes. “Many human cancers show a loss of ALDH4A1, and patients with lower levels of ALDH4A1 tend to have worse survival outcomes,” he said.
Lin initiated the study while leading the research team at Wake Forest University. After joining the faculty at Duke in May 2023, he and his team completed the work.
In lab experiments using human liver cancer cells and mouse 3T3 cells, researchers demonstrated that the loss of ALDH4A1 encouraged cell transformation and tumor development. Conversely, increasing MPC activity by overexpressing ALDH4A1 slowed or halted tumor growth.
By targeting this protein, scientists hope to develop therapies that can disrupt cancer’s energy supply and stop it in its tracks.
Study authors include Che-Chia Hsu, Chi-Yun Wang, Rajesh Kumar Manne, Zhen Cai, Vasudevarao Penugurti, Rajni Kant; Ling Bai; Bo-Syong-Pan; Tingjin Chen; Yuan-Ru Chen; Hsin-En Wu; Yan Jin; Haiwei Gu; and Chia-Yang Li.
The study was funded in part by the National Institutes of Health (R01CA256158, R01CA248037 and R01CA270617).
The FDA Approves First U.S. At-Home Tool As A Pap Smear Alternative

The FDA Approves First U.S. At-Home Tool As A Pap Smear Alternative
(NPR, Jennifer Ludden) — The Food and Drug administration has approved the U.S.'s first at-home alternative to the Pap smear, a procedure generations of women have dreaded and often found painful.
The new device by Teal Health will offer a "much preferred experience," the company said in its announcement, and also aims to increase screening rates by making the procedure more convenient.
Traditionally, gynecologists have inserted a cold metal speculum deep into a woman's vagina to scrape cells from the cervix.
The Teal Wand — "built with empathy," the company said — uses a swab to collect a vaginal sample. Women will then mail the sample to a lab that will screen for HPV (human papillomavirus), the virus that causes nearly all cervical cancers. A growing body of research has found HPV testing to be highly accurate.
The FDA approval Friday follows a U.S.-based study that found at-home screening was just as effective as that done in a doctor's office. The study also found women overwhelmingly preferred self–screening at home, and said they'd be more likely to stay up to date with cervical cancer screenings that way.
Every year, about 13,000 cases of cervical cancer are diagnosed, and more than 4,000 women die from the disease. Rates are down dramatically since Dr. Georgios Papanicolaou published a 1943 paper on how to use the Pap smear for screening, and it then became common.
But about a quarter of women in the U.S. are behind on such screenings, and medical experts say reducing that is key to the ultimate goal of eliminating cervical cancer. There's also a racial gap, with Black and Native American women far more likely to die from cervical cancer than white women. The HPV vaccine for teen and preteen girls, introduced in 2007, has also led to a global push to tackle the disease that way.
At-home cervical cancer screenings are already available in several other countries, including Australia and Sweden.
Teal Health says its self-testing device will be available starting next month, in California first and then expanding. It will be by prescription, through a telehealth service, for women 25-65 years old who are "at average risk." The company says it's working with insurance companies to provide coverage.
Firefighters Face Higher Skin Cancer Risk. A Winston-Salem Hospital Offered A Free Screening

Firefighters Face Higher Skin Cancer Risk. A Winston-Salem Hospital Offered A Free Screening
(WFMY Ben Briscoe) — Meredith Smith didn’t have to look far to find her motivation. Her husband is a firefighter. And as an oncology nurse, Smith knows firsthand the elevated cancer risks that come with the job — especially when it comes to skin cancer.
That’s why she’s teaming up with Novant Health to offer a free skin cancer screening event for firefighters and first responders on Monday, May 12, at the Derrick L. Davis Cancer Institute in Winston-Salem.
“They’re our heroes,” Smith said. “And we want to protect them from future instances of skin cancer and any type of cancer.”
Why Firefighters Are More at Risk
Firefighters face a 21% higher risk of skin cancer compared to the general population, according to Novant Health oncologist Dr. Andy Dothard. And they’re being diagnosed younger than ever — sometimes as early as age 35.
Part of the problem lies in exposure to carcinogens — both during and after the fire is out.
“The chemicals and substances they’re exposed to during fires often contain carcinogens,” Smith explained. “They can get in through the skin or be inhaled.”
Even their protective gear poses risks. Smith says many firefighter uniforms contain PFAS, chemicals that help make gear more water- and heat-resistant — but are also linked to cancer. When firefighters sweat in extreme heat, their pores open, making it easier for harmful substances to be absorbed.
And in the past, culture played a part, too.
“Years ago, dirty gear was a badge of honor. It meant you had experience,” Smith said. “Now we know that gear was covered in dangerous chemicals.”
Why Early Detection Saves Lives
Dr. Dothard says that identifying skin cancer early makes a major difference in survival rates.
“It’s much easier to treat and leads to better outcomes,” he said. “These events are super important — not just to save lives, but to improve quality of life by catching cancer sooner.”
North Carolina Extends Prior Authorization for Type 1 Diabetes

North Carolina Extends Prior Authorization for Type 1 Diabetes
In its May 2025 pharmacy update, NC Medicaid has provided notice that prior authorization approval for insulin has been extended for up to 3 years. The notice is below.
Insulin Prior Authorization Extension for Type 1 Diabetes
(Excerpt from NC Medicaid’s May 2025 Pharmacy Newsletter)
Insulin Prior Authorization Extension for Type 1 Diabetes To improve patient access and streamline the prescribing process for NC Medicaid beneficiaries with Type 1 diabetes, prior authorization (PA) approvals for certain insulin products may now be extended for up to 3-years, effective May 1, 2025. This applies to the following specific insulin categories:
- Rapid-acting insulin,
- Short-acting insulin,
- Intermediate-acting insulin,
- Long-acting insulin,
- Premixed rapid combination insulin, and
- Premixed 70/30 combination insulin
All other diabetes diagnoses will continue to have a 1-year prior authorization.
To reach NC Medicaid . . .
NC Medicaid Contact Center - 888-245-0179
Provider Ombudsman - [email protected] | 866-304-7062
NCTracks Call Center - 800-688-6696
US Infant Mortality Dropped In 2024. Experts Partly Credit RSV Shots

US Infant Mortality Dropped In 2024. Experts Partly Credit RSV Shots
(AP Health, Mike Stobbe) — The nation’s infant mortality rate dropped last year after two years of hovering at a late-pandemic plateau.
Some experts think one reason for the drop could be a vaccination campaign against RSV, or respiratory syncytial virus, which is a common cause of cold-like symptoms that can be dangerous for infants.
The infant mortality national rate dropped to about 5.5 infant deaths per 1,000 live births in 2024, according to provisional data from the Centers for Disease Control and Prevention posted Thursday. That’s down from about 5.6 per 1,000 live births, where it had been the previous two years.
CDC officials believe the findings will not change much when the final numbers come out later this year.
Infant mortality is the measure of how many babies die before they reach their first birthday. Because the number of babies born in the U.S. varies from year to year, researchers instead calculate rates to better compare infant mortality over time.
U.S. infant deaths fell to about 19,900 last year, according to CDC data, compared with about 20,150 in 2023.
The U.S. infant mortality rate has been worse than other high-income countries, which experts have attributed to poverty, inadequate prenatal care and other things. Even so, the U.S. rate generally has improved over the decades because of medical advances and public health efforts.
The 2022 and 2023 levels were up from 5.44 per 1,000 in 2021 — the first statistically significant jump in the rate in about two decades. Experts attributed those years to a rebound in RSV and flu infections after two years of pandemic precautions.
In 2023, U.S. health officials began recommending two new measures to prevent the toll on infants — one was a lab-made antibody shot for infants that helps the immune system fight off the virus, and the other was giving an RSV vaccine to women between 32 weeks and 36 weeks of pregnancy.
That effort is probably one explanation for the improvement, said Dr. Amanda Williams, interim chief medical officer for the March of Dimes.
In a separate CDC report released Thursday, researchers noted infant hospitalizations in the 2024-25 respiratory virus season were more than 40% lower than past averages.
But more work needs to be done to tease out other reasons, Williams added, noting that much of the improvement in 2024 was in infants who were at least one month old when they died. That could be explained not only by fewer deaths from RSV but also from other causes, like accidents, homicides or SIDS.
Capitol Chronicle: NC Medical Society Sends Congress A “Protect Medicaid” Appeal

Capitol Chronicle: NC Medical Society Sends Congress A “Protect Medicaid” Appeal
With cuts to Medicaid funding and coverage in the crosshairs on Capitol Hill, the NC Medical Society has issued an appeal to each of our US House and US Senate offices to protect the program which has 3.1 million enrollees in North Carolina. Congress is seeking budgetary offsets for a proposed tax package and Medicaid has become a likely target as the debate ensues.
Below is the message issued to each of North Carolina’s congressional offices.
On behalf of the North Carolina Medical Society, our physician and physician assistant members, and the many Medicaid patients they serve, I am writing to express our deep concern over the looming cuts to Medicaid. We urge members of the US House of Representatives and US Senate to preserve Medicaid as a foundational source of healthcare and security for the 3.1 million North Carolinians enrolled in the government-funded program.
In addition to our members and their patients, our state’s hospitals, community health centers, and long-term care facilities are also dependent on Medicaid for meeting the needs of the communities they serve. Medicaid is the single most important source of financial support that keeps rural and safety net hospitals viable and assures nursing home bed availability for those with long-term care needs. I’m sure you are aware of the hospitals that have closed in North Carolina’s rural communities due to financial instability and the access to care issues that have resulted. There are others that are on the brink of closure and a reduction in federal Medicaid support could be disastrous for those facilities and the regions they serve.
Medicaid also ensures people with disabilities can access critical services and secure meaningful job opportunities. Additionally, Medicaid is a lifeline for those with mental health and substance use disorder needs. It helps our working citizens stay healthy so they can maintain employment, feed their families and send their kids to school.
North Carolina’s Medicaid program has demonstrated its ability to effectively and efficiently fulfill its mission to the 1 in 4 North Carolinians that the program serves - 1.5 million of which are children. It is a vital source for perinatal and maternal care with coverage of over 50% of our state’s births annually. Medicaid allows mothers to deliver safely and children to have a healthy start to life; and as we continue to face a maternal mortality crisis, there is no doubt that cuts to Medicaid would exacerbate an already critical situation.
Over the past several months, our members have reached out to you and your staff through multiple communication channels, and many have traveled to Capitol Hill to share our urgent concerns. We appreciate your and their receptiveness to the concerns we’ve presented and we want to again ask that you eliminate Medicaid as a source for offsetting the tax cut extensions that are under consideration.
In follow-up to our past communications and meetings and in consideration of the various possible targets to achieve Congress’ budgetary target, we want to reiterate several points of concern:
Work requirements
Implementing work requirements will place a financial burden on our state, especially at the county level. Each county would take on the costly burden of verifying work status and the process of qualifying exemptions from the requirement. Imposing work requirements on Medicaid recipients will not increase employment levels given that most working-age and able recipients are already employed. But it will create bureaucratic obstacles that will result in a loss of access to coverage and care.
Eligibility determination frequency
Making the redetermination of Medicaid eligibility more frequent will also result in an increased administrative workload and will drive up costs. Administrative backlogs will occur along with delays in care.
Medicaid provider taxes
A significant portion of our state’s Medicaid funding is through provider taxes, which are paid by hospitals, nursing homes and intermediate care facilities. These payments generate more than $2.5 billion annually to help the state meet the non-federal share to fund the program. According to NC DHHS, for every 1% reduction in the 6% cap on provider taxes, federal Medicaid funding received will be reduced by $1.15 billion. Notable is that the providers who are paying the taxes agree that a reduction would be detrimental to meeting the care needs of our state’s Medicaid population.
Per capita caps on the expansion population
We recognize that a cap on per enrollee funding, regardless of the enrollment population, would reduce federal spending, but the resulting cost shift to the state could not be absorbed without significant, detrimental adjustments. The options would be to reduce eligibility, reduce coverage and reduce provider payment rates.
Federal Medical Assistance Program (FMAP)
The NCMS was pleased to work with the NC General Assembly and the Governor in 2023 to get Medicaid expansion enacted for our state. As a result of this bipartisan effort, our state has expanded coverage by 650,000 North Carolinians. That has increased access to care and allowed for more preventive care and early intervention, and unnecessary trips to emergency departments have also been reduced. Under Medicaid expansion, federal funding (FMAP) accounts for 90% of the program’s budget and the state covers the 10% balance. The law which established Medicaid expansion in North Carolina, however, has a “trigger” provision whereby expansion in North Carolina will immediately terminate if the federal government modifies its share of the cost. Should that occur, 650,000 North Carolinians would lose their coverage and among those that would be impacted are veterans and workers without employer-sponsored coverage. Further, the incidence of medical debt is certain to rise as coverage declines or is eliminated.
Block grants
A block grant approach to funding Medicaid would provide a fixed amount of funding to states, which may not adjust adequately for rising healthcare costs or unexpected increases in care demand. This can lead to insufficient resources to meet the needs of Medicaid beneficiaries, especially the more vulnerable, including children, seniors, the disabled, and pregnant women. Block grants do not account for the varying needs and the fluctuating costs associated with these populations and an underfunded block grant would result in states having to limit enrollment, reduce reimbursement for care and assume costs beyond their budgetary capacity.
If any of the Medicaid cuts and coverage modifications under consideration are implemented, North Carolinians will lose access to basic care and lifesaving services and the state will face budgetary deficits. Medical practices, hospitals, nursing homes, and community health centers will also be forced to cut staff and scale back services. Some may not survive. In addition, services that allow seniors and those with disabilities to live independently at home will be cut or eliminated. Our state’s families and workers will be unable to afford essential care and get sicker. That loss in productivity will harm the economy as a result. We therefore urge you to advocate for preserving Medicaid and not advance any proposals in the forthcoming budget reconciliation process that would reduce Medicaid funding and coverage.
I’d like to close on a couple of positive notes regarding Medicaid in North Carolina.
First, the NC Medical Society continues its joint venture with Centene Corporation and the NC Community Health Center Association, to improve the health status of Medicaid enrollees in our state. This ongoing work is being accomplished through Carolina Complete Health, the only Provider-Led Entity among the five Medicaid managed care plans in North Carolina, and the only plan of the five that is consistently top-ranked in metrics that NC Medicaid uses to measure health plan performance. One goal of that partnership is the broadest possible deployment of value-based models of care within Medicaid to simultaneously improve health status and experience of care for our enrollees, while reducing costs for the Medicaid program. This proactive and successful partnership exemplifies a value-oriented, team-based approach to meeting the health needs of North Carolinians.
Second is an accolade-worthy initiative of our North Carolina Medicaid program – the Healthy Opportunities Pilot Program. This project, which launched in 2022 in three regions of the state, resulted in measurable savings and is a success upon which a statewide effort can be pursued. In the program’s specified regions, health care savings were calculated to be $85 per person, per month.
It would be our hope that positive experiences and initiatives like these will serve as a solid foundation for our Medicaid program to continue to grow and improve, rather than being crippled by cuts and unable to meet its mission to meet the care needs of our state.
Thank you for your consideration and for your work on behalf of our state.
Cordially,
John J. Meier, IV, MD, MBA
President
North Carolina Medical Society