Jeff Bezos Group Sending $30M to N.C. State for Food Protein Studies

Bezos Center for Sustainable Protein at NCSU will also involve NC A&T, UNC-P, Duke, and Forsyth Tech
(Business NC, David Mildenberg) -- A group led by Amazon founder Jeff Bezos is giving $30 million over five years to NC State University to help create healthy food products that will be plant-based or use fermentation and animal cells.
The Bezos Center for Sustainable Protein at the Raleigh University will create a manufacturing hub for proteins that are environmentally friendly, healthy, tasty and affordable, according to a university press release.
Bezos started his Earth Fund with $10 billion to address climate-change challenges. It has committed $100 million to establish open-access research and development centers focused on sustainable protein.
“As a land-grant university in a state with significant animal agriculture, NC State is uniquely positioned to help shape the future of sustainable food production,” said Chancellor Randy Woodson in a statement He said the effort can help “feed a growing world population in an economically and environmentally sustainable way.
The state legislature’s funding of the Food Innovation Lab in Kannapolis and new facilities in the College of Engineering have made NC State incredibly competitive for this grant.”
NC State said N.C. A&T State University, UNC Pembroke, Duke University, and Forsyth Tech Community College in Winston-Salem will be involved in the project tied to research and workforce development. About 20 industry partners will also take part in the center for technology transfer and student internships.
Bezos is among the five wealthiest persons in the world with a net worth topping $200 billion. He founded Amazon in 1994 and stepped down as CEO in 2021.
He sold Amazon shares valued at $4 billion in February. His ex-wife, MacKenzie Scott, has received massive publicity for donation more than $12 billion over the past five years to more than 1,200 nonprofit groups.
FDA Considering Approval of MDMA for PTSD
Decadeslong Effort Could Move Psychedelic Drugs into Mainstream
(AP - Matthew Perrone) -- Federal health regulators are questioning the safety and evidence behind the first bid to use MDMA, the mind-altering club drug, as a treatment for PTSD, part of a decadeslong effort by advocates to move psychedelic drugs into the medical mainstream.
The Food and Drug Administration posted its initial review of the drug Friday, ahead of a meeting of outside advisers who could help decide whether MDMA — currently illegal under federal law — becomes the first drug of its kind to win U.S. approval as a medication.
In their assessment, FDA scientists said that patients who received MDMA and talk therapy showed “rapid, clinically meaningful, durable improvements in their PTSD symptoms.” But they also called the research “challenging to interpret,” and questioned how long the benefits might last.
They said it’s difficult to know how much of the improvement came from MDMA versus simply undergoing intensive therapy, and also raised several safety concerns, including MDMA’s heart risks and potential for abuse.
The outside experts will take a nonbinding vote on the drug’s overall benefits and risks during Tuesday’s meeting. The FDA will make the final decision, likely in August.
Antidepressants are now the only FDA-approved drugs for post-traumatic stress disorder, which is closely linked to depression, anxiety and suicidal thinking and is more prevalent among women and veterans.
If approved, MDMA would be reclassified as a prescription medicine and made available to specially certified doctors and therapists. Currently, the drug is in the same ultra-restrictive category as heroin and other substances the federal government deems prone to abuse and devoid of any medical use.
MDMA, also known as ecstasy or molly, is the first in a series of psychedelics that are expected to be reviewed by the FDA in coming years. It’s part of a resurgence of research into the potential of psychedelics for hard-to-treat conditions like depression, addiction and anxiety. MDMA’s main effect is triggering feelings of intimacy, connection and euphoria.
Companies are studying MDMA, psilocybin, LSD and other mind-expanding drugs for numerous mental health problems.
Until recently, psychedelic research was mainly funded by a handful of nonprofit advocacy groups, including Multidisciplinary Association for Psychedelic Studies, or MAPS. The company seeking approval for MDMA, Lykos Therapeutics, is essentially a corporate spinoff of MAPS, which conducted all the studies submitted for FDA review.
In two studies, patients received MDMA as part of an intensive, four-month course of talk therapy lasting more than a dozen sessions, only three of which involved taking the drug. The drug is thought to help patients come to terms with their trauma and let go of disturbing thoughts and memories.
The approach was studied in nearly 195 adults with moderate-to-severe PTSD who were randomly assigned to undergo the therapy with MDMA or with a dummy pill. Following treatment, patients who received MDMA had significantly lower PTSD scores and were more likely to be in remission.
But FDA reviewers noted that the vast majority of patients correctly guessed whether they had received MDMA or a dummy pill, making it “nearly impossible” to maintain the so-called “blinded” objectivity considered essential for high-quality drug research. The agency also questioned how long the drug’s benefits might last. The studies tracked some patients for up to two years, but reviewers noted that about a quarter of patients quickly dropped out of the follow-up study, limiting the usefulness of the results.
The most common side effects of MDMA included headache, nausea, muscle tightness and decreased appetite. More serious issues included heart palpitations and elevated blood pressure, which FDA reviewers said had the “potential to trigger” life-threatening heart problems.
They also raised concerns about the potential for patients to abuse MDMA, which functions similarly to amphetamines and other stimulants.
While MDMA would be a first-of-a-kind approval, U.S. doctors and the FDA itself have already laid some of the groundwork for working with drugs that can cause intense, psychological experiences.
Hundreds of clinics across the U.S. already offer ketamine — the powerful anesthetic sometimes used as a party drug — to treat a host of ailments, including depression, anxiety, chronic pain and PTSD. The FDA has only formally approved the drug for use during surgery, but its availability allows doctors to prescribe it “off-label” for various mental and physical ailments.
In 2019, the FDA approved Johnson & Johnson’s proprietary form of the drug, Spravato, a nasal spray that treats severe depression. Similar to ketamine, the drug is offered at doctor’s offices and clinics where patients usually spend several hours reclining in a chair.
UNC Health Championship Tees Off Today!

Raleigh's Premier Golf & Hospitality Event Returns!
(Axios Raleigh, UNC Health) -- The UNC Health Championship presented by Stitch, formerly Rex Hospital Open, has a new venue at Raleigh Country Club and more exciting ways to watch the Korn Ferry Tour players chase their dream.
The UNC Health Championship has become one of the region's premier golf tournaments, attracting up-and-coming pro golfers and local favorites every year.
- Proceeds from the tournament go toward funding a new children's hospital in the Triangle.
What to know: The opening round begins tomorrow and will come to a close on Sunday. Grounds tickets start at $40.
- Former UNC basketball coach Roy Williams is the chairman of the tournament this year and will play in the pro-am.
- The tournament will recognize the late Raleigh golfer Grayson Murray, who died by suicide last week, and place green ribbons around the course for Mental Health Awareness Month.
Several players with local ties will be competing, including:
- Raleigh natives and former UNC players Ryan Gerard and Carter Jenkins
- Raleigh native Doc Redman
- Campbell University alum Pontus Nyholm and Brett McLamb, who played at both Campbell and N.C. State
- Ryan Blaum, a Duke alum who lives in Durham
- David Ford, a rising senior at UNC.
2024 Physician Compensation Report lists NC City as a Metro Area With Highest Compensation

Average Physician Compensation Up Nearly 6 Percent
Between 2022 and 2023, the average compensation for U.S. physicians increased nearly 6% (5.9%), rebounding from a slight decline of 2.4% in the previous year. Physicians in the San Jose metropolitan area experienced one of the most significant surges in compensation, with an annual growth rate of 13.5%. This sizable increase propelled San Jose from being the fourth-highest metro area in average physician compensation in 2022 to claiming the number-one spot in 2023.
Notably, all ten of the metropolitan areas with the lowest average physician compensation in 2023 saw growth last year, with growth rates exceeding 10% in Baltimore, Providence, and Virginia Beach.


To read the full report click here.
NCMS Opposes Attempt to Put North Carolinians' Safety at Risk

NCMS Opposes Proposals on House Bill 681 That Continue to Promote NP Pathways to Independent Practice
The situation over House Bill 681 continues to evolve. The NCMS lobbying team learned on Tuesday that a third Proposed Committee Substitute (PCS) would be introduced at the Wednesday meeting of the Senate Health Care Committee. Each version continues to put patient safety at risk and demonstrates the the proponents of this effort are more concerned with financial gain than they are about quality healthcare in North Carolina. Each version has also sought to progressively limit and even remove physician involvement from patient care.
At their core, these changes:
-
Sever the critical role of physicians from the healthcare process, undermining the very foundation of medical care.
-
Devastate access to essential healthcare for North Carolinians residing in rural and underserved areas, leaving these communities vulnerable and neglected.
-
Jeopardize the safety of every citizen in North Carolina, creating a perilous healthcare landscape fraught with risk and uncertainty.
The changes promote pathways for Nurse Practitioners to practice independently. The second version removed the increased requirements for supervision and further restricted anesthesia care by anesthesiologists and AAs, while allowing CRNAs to work independently. These are topics that have been debated for years.
The NCMS has been able to acquire bipartisan opposition to this effort, as demonstrated over the past two weeks, when Democrats and Republicans came together in the best interest of North Carolinians.
NCMS Members Dr. William Ferrell and Dr. Bryant Murphy worked with the NCMS team yesterday, speaking with individual members of the Senate Healthcare Committee. Our allies in the Senate continue to give us valuable guidance to refine our strategy for opposing these proposals.
NCMS VP of Advocacy John Thompson says "The NCMS maintains the stance that opposing changes to legislation which jeopardizes patient safety is crucial for upholding the integrity of a healthcare delivery system. The NCMS firmly advocates prioritizing the welfare and safety of patients above all considerations, thereby ensuring that any legislative adjustments maintain stringent standards of care and safeguard individuals from potential harm."
YOU CAN HELP!
Plan now to attend the North Carolina Medical Society White Coat Advocacy Day June 12
The North Carolina Medical Society continues to monitor and work on House Bill 681. Look for a Political Pulse on May 31 with more in-depth analysis of what is happening in Raleigh.
New Report: US FDA Clears Neuralink's Brain Chip Implant in Second Patient

Wall Street Journal reports Elon Musk's Neuralink can implant brain chip in 2nd person
2024 NCMS Board of Directors, Foundation Board of Trustees, & Leadership Team Hold Spring Workshop

Members of the NCMS Board of Directors and Foundation Board of Trustees Celebrate 175 Years!
RALEIGH -- The North Carolina Medical Society hosted its Board of Directors and Foundation Board of Trustees for a weekend of learning, strategic planning, Society updates, and fellowship. Over the course of three days, members and staff enjoyed a presentation from North Carolina Department of Health and Human Services Secretary Kody Kinsley, had a day of learning about practice management and artificial intelligence, and strategic planning.
In addition to Kinsley, speakers included Janelle Rhyne, MD and Cheryl Walker McGill, MD who spoke on artificial intelligence and how it is affecting the healthcare community and the future impacts it is likely to have. The offered an excellent article how on how artificial and augmented intelligence is already creating wide-reaching medical implications. Click here for a link to the AMA article and CME opportunities.
The AI discussion continued with a presentation from Lyle Gravatt and Justin May of Michael Best & Friedrich, LLP. They discussed the legal and regulatory environment that has been created by artificial intelligence. NCMS CEO Chip Baggett then moderated a panel discussion with all presenters that drew great discussion and many difficult questions.
Ron Howrigon, President and CEO of Fulcrum Strategies, led a long conversation on Practice Capitalization. He offered suggestions on managing a medical practice during difficult financial times and tips for improving your bottom line.
Saturday afternoon was followed by a two hour on strategic planning that focused on the NCMS goals for 2024. The session was moderated by Glenn Newsom of Pilgrimage Partners.
Board members and staff discussed ways to move forward including increasing our membership numbers and the importance of our Leadership College.
Saturday evening was the 1849 Society Dinner and Induction Ceremony. The NCMS Foundation's most prestigious giving society, the 1849 Society, recognizes individuals' cumulative lifetime cash gifts. Initial membership in the 1849 Society is set at a minimum of $10,000. This year, former NCMS President Dr. Arthur Apolinario was inducted into the 1849 Society. Guests were entertained by soprano Rush Dorsett and pianist Daniel Spiegel.
On Sunday, the Board of Directors Meeting covered updates on strategic plans, a treasurer's report, the latest on the LEAD Gala and 175th Anniversary Celebration, an update on the NC General Assembly and Uniform Credentialing and was followed by President Eileen Raynor going over the Consent Agenda.
The Foundation Board of Trustees Meeting was led by Dr. Timothy Reeder, with reports from Treasurer Dr. Osi Udekwu, a KIPL update, Chip Baggett speaking on the ONSMS Grant Partnership with NCDHHS, a NCCPRW update and additional board business.
Look for a special e-mal this week from NCMS President Eileen Raynor with a mid-year report on how well the NCMS is doing.
Problematic Proposed Revisions to HB 681 Heard by Senate Healthcare Committee, NCMS Members at Meeting to Answer Questions

NCMS members Dr. Timothy Reeder and Dr. Kristin Baker attend meeting of Senate Healthcare Committee
RALEIGH -- The North Carolina Senate Health Care Committee met Wednesday morning with Senator Kevin Corbin presiding. Proposed revisions to House Bill 681 was considered. The bill is sponsored by North Carolina Medical Society members Dr. Timothy Reeder and Dr. Kristin Baker, who were both in attendance. Additional sponsors are Representatives Donny Lambeth and, Larry Potts, and Senators Jim Burgin, Senator Kevin Corbin, and Senator Joyce Krawiec, all Co-Chairs. Senator Jim Bergin of Harnett county proposed changes that drastically alter the substance of original bill.
The NCMS considers HB 681 revisions problematic for the following reasons:
Creates An Undefined Scope of Practice for Nurse Practitioners
- The proposed PCS to HB 681 lacks clarity on nurse practitioner scope, allowing them to conduct surgery, interpret complex imaging, and manage patients with multiple chronic conditions without physician oversight.
Creates An Unsafe Practice Environment That Puts A Patient’s Safety at Risk
- Lack of physician supervision compromises patient safety. Nurse practitioners, with substantially less training than physicians, could treat severely ill patients with complex conditions under the proposed law.
- A physicians' rigorous training equips them to handle complex medical cases effectively. If nurse practitioners are allowed to work without physician oversight it puts patients at risk of inadequate care if they have complicated conditions, raising the likelihood of misdiagnosis, treatment errors, and unnecessary testing.
Creates a Siloed and Inadequate Health care Delivery System
- Removing physician supervision undermines team-based care. The proposed changes to HB 681 would allow nurse practitioners to work independently, eliminating collaboration among healthcare professionals and potentially leading to inferior health outcomes.
Creates Access To Care Barriers
- HB 681 would drastically limit access to surgical care by reducing the number of anesthesiologist providers one anesthesiologist can supervise from four to one, the most extreme restriction in the nation. This could decrease safe surgical capacity statewide by up to 75%.
 NCMS Chief Legal Officer Ashley Rodriguez says the meeting resulted in a win for members. "It was a great hearing," Rodriguez says, "with a great deal of acknowledgment that team-based care is best for patients and several positive references to prior authorization."
NCMS Chief Legal Officer Ashley Rodriguez says the meeting resulted in a win for members. "It was a great hearing," Rodriguez says, "with a great deal of acknowledgment that team-based care is best for patients and several positive references to prior authorization."
The Senate Health Care Committee held the proposal up for continued discussion and a potential vote as early as next week.
To see the full video click here.
30 Year Study: The Ultra-Processed Foods You and Your Patients Need to Avoid

Health professionals have long warned that ultra-processed foods can have detrimental impacts on the body
(CNN - Madeline Holcombe) -- Eating ultraprocessed foods is associated with an early risk of death, according to a 30-year study — but different foods have different impacts.
Processed meats and sugary foods and drinks aren’t correlated with the same risks as ultraprocessed whole grains, for example, said lead study author Dr. Mingyang Song, associate professor of clinical epidemiology and nutrition at Harvard’s TH Chan School of Public Health.
The study analyzed data from more than 100,000 health professionals in the United States with no history of cancer, cardiovascular disease or diabetes. From 1986 to 2018, the participants provided information on their health and lifestyle habits every two years.
Every four years, they completed a detailed food questionnaire.
The group eating the least ultraprocessed food ate about three servings a day on average, while the highest averaged seven servings a day, according to the study published Wednesday in The BMJ journal.
Those who ate the most had a 4% higher risk of deaths by any cause, including a 9% increased risk of neurodegenerative deaths, the data showed.
Song described the correlation as “moderate,” noting that the connection was not equally strong among all kinds of ultraprocessed foods.
“The positive association is mainly driven by a few subgroups including processed meat and sugar sweetened or artificially sweetened beverages,” he said.
Findings in this study were consistent with hundreds of others in the field, but what makes this one unique is its parsing out of different subgroups within the ultraprocessed food category, said Dr. Marion Nestle, the Paulette Goddard professor emerita of nutrition, food studies and public health at New York University.
Do we need to get rid of all ultraprocessed foods?
Song wouldn’t necessarily advise a complete rejection of all ultraprocessed foods because it is a diverse category, he said.
“Cereals, whole grain breads, for example, they are also considered ultraprocessed food, but they contain various beneficial nutrients like fiber, vitamins and minerals,” he said. “On the other hand, I do think people should try to avoid or limit the consumption of certain ultraprocessed foods, such as processed meat, sugar-sweetened beverages and also potentially artificially sweetened beverages.”
There are also more questions that need to be answered when it comes to ultraprocessed foods.
First, the recent study is strong because of the length of time covered, but it is an observational study. That means that while researchers can observe a correlation, they can’t say that the foods were the cause of the deaths, said Dr. Peter Wilde, emeritus fellow at Quadram Institute Bioscience in the United Kingdom.
Researchers also need to look more at the components of ultraprocessed foods that might be affecting health — whether they be food additives, emulsifiers or flavors — to advise governments and institutions on how to regulate foods, Song said.
Overall diet matters most
Researchers also found that the most important factor to reducing risk of death is the quality of a person’s overall diet, Song said.
“If people maintain a generally healthy diet, I don’t think they need to be like scared or be freaked out,” he said. “The overall dietary pattern is still the predominant factor determining the health outcomes.”
Researchers also need to look more at the components of ultraprocessed foods that might be affecting health — whether they be food additives, emulsifiers or flavors — to advise governments and institutions on how to regulate foods, Song said.
Overall diet matters most
Researchers also found that the most important factor to reducing risk of death is the quality of a person’s overall diet, Song said.
“If people maintain a generally healthy diet, I don’t think they need to be like scared or be freaked out,” he said. “The overall dietary pattern is still the predominant factor determining the health outcomes.”
“If you are worried about food additives, then choose foods that have low levels of additives,” he said in an email. “Just be mindful of the nutritional content of (the ultraprocessed foods) that you do choose to consume.”
It is also important to recognize that foods need to be eaten in balance. Fruit juice contains beneficial vitamins, minerals and antioxidants when consumed in moderation, but too much will have high levels of sugar that may override their benefits, Wilde said.
“This is not black and white,” he said. “A particular food is not either good or bad, it will contain elements of both, and the balance between the two may depend on how much you eat.”
AI is Dreaming Up Drugs That No One Has Ever Seen. Now We've Got to See if They Work.
MIT Technology Review Looks at What is Happening with Artificial Intelligence and Drug Research
(MIT Tech Review, Will Douglas Heaven) -- At 82 years old, with an aggressive form of blood cancer that six courses of chemotherapy had failed to eliminate, Paul appeared to be out of options. With each long and unpleasant round of treatment, his doctors had been working their way down a list of common cancer drugs, hoping to hit on something that would prove effective—and crossing them off one by one. The usual cancer killers were not doing their job.
With nothing to lose, Paul’s doctors enrolled him in a trial set up by the Medical University of Vienna in Austria, where he lives. (Paul's real name is not known because his identify was obscured in the trial.) The university was testing a new matchmaking technology developed by a UK-based company called Exscientia that pairs individual patients with the precise drugs they need, taking into account the subtle biological differences between people.
The researchers took a small sample of tissue from Paul. They divided the sample, which included both normal cells and cancer cells, into more than a hundred pieces and exposed them to various cocktails of drugs. Then, using robotic automation and computer vision (machine-learning models trained to identify small changes in cells), they watched to see what would happen.
In effect, the researchers were doing what the doctors had done: trying different drugs to see what worked. But instead of putting a patient through multiple months-long courses of chemotherapy, they were testing dozens of treatments all at the same time.
The approach allowed the team to carry out an exhaustive search for the right drug. Some of the medicines didn’t kill Paul’s cancer cells. Others harmed his healthy cells. Paul was too frail to take the drug that came out on top. So he was given the runner-up in the matchmaking process: a cancer drug marketed by the pharma giant Johnson & Johnson that Paul’s doctors had not tried because previous trials had suggested it was not effective at treating his type of cancer.
It worked. Two years on, Paul was in complete remission—his cancer was gone. The approach is a big change for the treatment of cancer, says Exscientia’s CEO, Andrew Hopkins: “The technology we have to test drugs in the clinic really does translate to real patients.”
Selecting the right drug is just half the problem that Exscientia wants to solve. The company is set on overhauling the entire drug development pipeline. In addition to pairing patients up with existing drugs, Exscientia is using machine learning to design new ones. This could in turn yield even more options to sift through when looking for a match.
The first drugs designed with the help of AI are now in clinical trials, the rigorous tests done on human volunteers to see if a treatment is safe—and really works—before regulators clear them for widespread use. Since 2021, two drugs that Exscientia developed (or co-developed with other pharma companies) have started the process. The company is on the way to submitting two more.
“If we were using a traditional approach, we couldn’t have scaled this fast,” Hopkins says.
Exscientia isn’t alone. There are now hundreds of startups exploring the use of machine learning in the pharmaceutical industry, says Nathan Benaich at Air Street Capital, a VC firm that invests in biotech and life sciences companies: “Early signs were exciting enough to attract big money.”
Today, on average, it takes more than 10 years and billions of dollars to develop a new drug. The vision is to use AI to make drug discovery faster and cheaper. By predicting how potential drugs might behave in the body and discarding dead-end compounds before they leave the computer, machine-learning models can cut down on the need for painstaking lab work.
And there is always a need for new drugs, says Adityo Prakash, CEO of the California-based drug company Verseon: “There are still too many diseases we can’t treat or can only treat with three-mile-long lists of side effects.”
Now, new labs are being built around the world. Last year Exscientia opened a new research center in Vienna; in February, Insilico Medicine, a drug discovery firm based in Hong Kong, opened a large new lab in Abu Dhabi. All told, around two dozen drugs (and counting) that were developed with the assistance of AI are now in or entering clinical trials.
“If somebody tells you they can perfectly predict which drug molecule can get through the gut … they probably also have land to sell you on Mars.”
Adityo Prakash, CEO of Verseon
We’re seeing this uptick in activity and investment because increasing automation in the pharmaceutical industry has started to produce enough chemical and biological data to train good machine-learning models, explains Sean McClain, founder and CEO of Absci, a firm based in Vancouver, Washington, that uses AI to search through billions of potential drug designs. “Now is the time,” McClain says. “We’re going to see huge transformation in this industry over the next five years.”
Yet it is still early days for AI drug discovery. There are a lot of AI companies making claims they can’t back up, says Prakash: “If somebody tells you they can perfectly predict which drug molecule can get through the gut or not get broken up by the liver, things like that, they probably also have land to sell you on Mars.”
And the technology is not a panacea: experiments on cells and tissues in the lab and tests in humans—the slowest and most expensive parts of the development process—cannot be cut out entirely. “It’s saving us a lot of time. It’s already doing a lot of the steps that we used to do by hand,” says Luisa Salter-Cid, chief scientific officer at Pioneering Medicines, part of the startup incubator Flagship Pioneering in Cambridge, Massachusetts. “But the ultimate validation needs to be done in the lab.” Still, AI is already changing how drugs are being made. It could be a few years yet before the first drugs designed with the help of AI hit the market, but the technology is set to shake up the pharma industry, from the earliest stages of drug design to the final approval process.
The basic steps involved in developing a new drug from scratch haven’t changed much. First, pick a target in the body that the drug will interact with, such as a protein; then design a molecule that will do something to that target, such as change how it works or shut it down. Next, make that molecule in a lab and check that it actually does what it was designed to do (and nothing else); and finally, test it in humans to see if it is both safe and effective.
For decades chemists have screened candidate drugs by putting samples of the desired target into lots of little compartments in a lab, adding different molecules, and watching for a reaction. Then they repeat this process many times, tweaking the structure of the candidate drug molecules—swapping out this atom for that one—and so on. Automation has sped things up, but the core process of trial and error is unavoidable.
But test tubes are not bodies. Many drug molecules that appear to do their job in the lab end up failing when they are eventually tested in people. “The whole process of drug discovery is about failure,” says biologist Richard Law, chief business officer at Exscientia. “The reason that the cost of coming up with a drug is so high is because you have to design and test 20 drugs to get one to work.”
This new generation of AI companies is focusing on three key failure points in the drug development pipeline: picking the right target in the body, designing the right molecule to interact with it, and determining which patients that molecule is most likely to help.
Computational techniques like molecular modeling have been reshaping the drug development pipeline for decades. But even the most powerful approaches have involved building models by hand, a process that is slow, hard, and liable to yield simulations that diverge from real-world conditions. With machine learning, vast amounts of data, including drug and molecular data, can be harnessed to build complex models automatically. This makes it far easier—and faster—to predict how drugs might behave in the body, allowing many early experiments to be carried out in silico. Machine-learning models can also sift through vast, untapped pools of potential drug molecules in a way that was not previously possible. The upshot is that the hard, but essential, work in laboratories (and later in clinical trials) need only be carried out on those molecules with the best chances of success.
Before they even get to simulating drug behavior, many companies are applying machine learning to the problem of identifying targets. Exscientia and others use natural-language processing to mine data from vast archives of scientific reports going back decades, including hundreds of thousands of published gene sequences and millions of academic papers. The information extracted from these documents is encoded in knowledge graphs—a way to organize data that captures links including causal relationships such as “A causes B.” Machine-learning models can then predict which targets might be the most promising ones to focus on in trying to treat a particular disease.
Applying natural-language processing to data mining is not new, but pharmaceutical companies, including the bigger players, are now making it a key part of their process, hoping it can help them find connections that humans might have missed.
Jim Weatherall, vice president of data science and AI at AstraZeneca, says that getting AI to crawl through lots of biomedical data has helped him and his team find a few drug targets they would not otherwise have considered. “It’s made a real difference,” he says. “No human is going to read millions of biology papers.” Weatherall says the technique has revealed connections between things that might seem unrelated, such as a recent finding and a forgotten result from 10 years ago. “Our biologists then go and look at that and see if it makes sense,” says Weatherall. It’s still early days for this target-identification technique, though. He says it will be “some years” before any AstraZeneca drugs that result from it go into clinical trials.
But picking a target is just the start. The bigger challenge is designing a drug molecule that will do something with it—and this is where most innovation is happening.
The interaction between molecules inside a body is vastly complicated. Many drugs have to pass through hostile environments, such as the gut, before they can do their job. And everything is governed by physical and chemical laws that operate at atomic scales. The goal of most AI-powered approaches to drug design is to navigate the vast possibilities and quickly home in on new molecules that tick as many boxes as possible.
Generate Biomedicines, a startup based in Cambridge, Massachusetts, founded by Flagship Pioneering, is aiming to do that using the same kind of generative AI behind text-to-image software like DALL-E 2. Instead of manipulating pixels, Generate’s software works with random strands of amino acids and finds ways to twist them up into protein structures with specific properties. Since the functions of a protein are dictated by its 3D folding, this, in effect, makes it possible to order up a protein capable of doing a particular job. (Other groups, including David Baker’s lab at the University of Washington, are developing similar tech.)
“Patients can have this terrible experience of going in and out of hospital, sometimes for years, getting drugs that don’t work.”
Richard Law, chief business officer of Exscientia
Absci is also trying to create new protein-based drugs using machine learning, but through a different approach. The company takes existing antibodies—proteins that the immune system uses to remove bacteria, viruses, and other unwanted assailants—and uses models trained on data from lab experiments to come up with lots of new designs for the parts of those antibodies that glom onto foreign matter. The idea is to redesign existing antibodies to make them better at binding to targets. After making adjustments in simulation, the researchers then synthesize and test the designs that work best.
In January, Absci, which has partnerships with larger pharmaceutical companies such as Merck, announced that it had used its approach to redesign several existing antibodies, including one that targets the spike protein of SARS-CoV-2, the virus that causes covid-19, and another that blocks a type of protein that helps cancer cells grow.
Apriori Bio, another Flagship Pioneering startup based in Cambridge, also has its eye on covid, hoping in particular to develop vaccines capable of protecting people from a wide range of viral variants. The company builds millions of variants in the lab and tests how well covid-fighting antibodies grab onto them. It then uses machine learning to predict how the best antibodies would fare against 100 billion billion (1020) more variants. The goal is to take the most promising antibodies—the ones that seem able to take on a large range of variants or might combat particular variants of concern—and use them to design variant-proof vaccines.
“It’s just not viable to ever do this experimentally,” says Lovisa Afzelius, a partner at Flagship Pioneering and CEO of Apriori Bio. “There is no way that your human brain can put all those bits and pieces in place and figure out that entire system.”
For Prakash, this is where AI’s real potential lies: opening up a huge untapped pool of biological and chemical structures that could become the ingredients of future drugs. Once you strip out very similar molecules, Prakash says, all of Big Pharma taken together—Merck, Novartis, AstraZeneca, and so on—has an ingredient list of at most 10 million molecules to build drugs from, some proprietary and some commonly known. “That’s what we’re testing across the entire planet—the total product of the last hundred years of toil from a lot of chemists,” he says.
And yet, he says, the number of possible molecules that might make drugs, according to the rules of organic chemistry, is 1033 (other estimates have put the number of drug-like molecules even higher, in the realm of 1060). “Compare that number to 10 million and you see we’re not even fishing in a tide pool next to the ocean,” Prakash says. “We’re fishing in a droplet.”
Crucially, simulation allows researchers to zip past a lot of the messiness that generally characterizes the drug design process. Companies traditionally create batches of molecules they hope have certain properties and then test each in turn. With machine learning, they can instead start with a wish list of basic characteristics—encoded mathematically—and produce designs for molecules that have those properties at the push of a button. This flips the early phase of development on its head, says Salter-Cid: “It’s not something we used to be able to do at the beginning.” A company might ordinarily make 2,500 to 5,000 compounds over five years when developing a new drug. Exscientia made 136 for one of its new cancer drugs, in just one year.
“It’s about speeding up cycles of exploration,” says Weatherall. “We’re getting to the stage now where we can make more and more decisions without actually having to make a molecule for real.”
However they are made, drugs still have to be tested in humans. These final phases of drug development, which involve recruiting large numbers of volunteers, are hard to run and generally take a long time—around 10 years on average and sometimes up to 20. Many drugs take years to get to this stage and still fail.
AI won’t be able to speed the clinical trial process, but it could help drug companies stack the odds more in their favor, by cutting down the time and cost involved in searching for new drug candidates. Less time spent testing dead-end drug molecules in the lab should mean that promising candidates will make it to clinical trials faster. And with less money on the line, companies might not feel as much pressure to stick with a drug that isn’t performing particularly well.
Better targeting of patients could also help improve the process. Most clinical trials measure the average effect of a medicine, tallying up how many people it worked for and how many it didn’t. If enough people in the trial see an improvement in their condition, then the drug is considered successful. If the drug isn’t effective for a large enough percentage, then it’s a failure. But this can mean that small groups of people for whom a drug worked get overlooked.
“It’s a very crude way of doing it,” says Weatherall. “What we’d actually like to do is find the subset of patients who would get the most benefit from a drug.”
This is where Exscientia’s matchmaking technology comes in. “If we can select the right patients, it does fundamentally change the economic model of the pharma industry,” says Hopkins.
It will all also dramatically improve the lives of patients, like Paul, who do not respond to the most common drugs. “Patients can have this terrible experience of going in and out of hospital, sometimes for years, getting drugs that don’t work, until either there’s no drugs left anymore or they finally get to the one that does work for them,” says Law.
After Exscientia found a drug that worked for Paul, the company followed up with a scientific study. It took tissue samples from dozens of cancer patients who had undergone at least two failed courses of chemotherapy and evaluated the effects of 139 existing drugs on their cells. Exscientia was able to identify a drug that worked for more than half of them.
The company now wants to use this technology to shape its approach to drug development, incorporating patient data into the earliest stages of the process to train even better AI. “Instead of starting with a model of a disease, we can start with tissue from a patient,” says Hopkins. “The patient is the best model.”
For now, the first batch of AI-designed drugs is still making its way through the clinical trial gauntlet. It could be months, or even years, before the first ones pass and hit the market. Some may not make it.
But even if this initial group fails, there will be another. Drug design has changed forever. “These are just the first drugs that these companies are trying,” says Benaich. “Their best drugs might be the ones that come after.”
The Physicians Foundation Releases 2023 Annual Report, NCMS CEO Chip Baggett Responds

The Physicians Foundation is celebrating progress on behalf of physicians and spotlighting solutions to safeguard the future of medicine
The Physicians Foundation is releasing its 2023 Annual Report. It highlights the first-ever national primary care scorecard which identifies issues important to physicians and provides a benchmark on the state of primary care. Here are the highlights:
- Primary care scorecard found that underinvestment, workforce shortages, and lack of research threaten healthcare.
- Annual survey on physician wellbeing found a majority of physicians feel burned out and resident and students feel even worse. System changes are needed to improve the future of medicine. Dear FutureDoc has been launched in response.
- Work continues with Dr. Lorna Breen Heroes' Foundation continues.
- Support physicians in addressing DOH remains significant focus area.
- Launched new Leadership Award Program to empower and honor the work of early career physicians
- Continued support for the publication and promotion of new research.

The North Carolina Medical Society EVP/CEO Chip Baggett says of the report: "The Physicians Foundation continues to advance research-based initiatives that support physicians across the US. The primary care scorecard is an essential tool for decision-making for the NCMS, and the Annual Survey serves as a vital reminder that the well-being of our members is key to the future of healthcare in North Carolina. Our joint collaboration with the Dr. Lorna Breen Heroes' Foundation, which reaches millions of people to raise well-being awareness and encourage system changes impacting our members, is especially poignant. As NCMS marks its 175th anniversary, we are excited to continue our 20+ year partnership with The Physicians Foundation, working together to enhance the lives of physicians and PAs."
To read the letter from the President of The Physicians Foundation click here.
Study Sheds Light on How Our “Neural Compasses” Keep Us on Track
New study of human motion-tracking released
Our ability to get from point A to point B, whether we’re just going from the front door to our car or hiking through a forest, is something we often take for granted, and hasn’t been extensively studied. Now, researchers are trying to change that: For the first time, a study has pinpointed how the brain’s “neural compass” helps humans orient themselves and avoid getting lost.
“Keeping track of the direction you are heading in is pretty important,” lead author Benjamin J. Griffiths said in a statement. “Even small errors in estimating where you are and which direction you are heading in can be disastrous.”
He and his colleagues conducted a series of motion-tracking experiments on 52 participants who were asked to orient themselves while an EEG scalp monitor tracked brain activity. They found that the brain sends out a “directional signal” before any physical movement is made, thus indicating an internal “compass” of sorts.
“Isolating these signals enables us to really focus on how the brain processes navigational information and how these signals work alongside other cues such as visual landmarks,” Griffiths explained, noting that the work could be used in research on neurodegenerative diseases like Alzheimer’s and Parkinson’s.
Do People With Diabetes Need to Fast Longer Before Surgery?
Expert Identifies Noteworthy Study Limitations
(Medscape, Miriam Tucker) -- People with diabetes don't have higher gastric volumes than those without diabetes after following standard preoperative fasting instructions, suggested a study from a team of anesthesiologist researchers.
However, an endocrinologist faulted the study in part because the participants appeared to be healthier than typical populations with type 1 and type 2 diabetes. Moreover, the issue is now further complicated by the widespread use of glucagon-like peptide-1 (GLP-1) receptor agonists for the treatment of both type 2 diabetes and weight loss. These drugs, which were introduced after the study's enrollment period, work in part by delaying gastric emptying.
The new data come from a prospective study of 84 people with diabetes (85% with type 2) and 96 without diabetes, all with a body mass index (BMI) < 40, who were undergoing elective surgery. A gastric ultrasound was used to assess their gastric contents after they had followed the standard preoperative fasting guidelines of stopping solids 8 hours prior to the procedure and clearing liquids 2 hours prior.
There was no significant difference between the two groups in gastric volume (0.81 mL/kg with diabetes vs 0.87 mL/kg without) or in the proportion with "full stomach," as designated by the American Society of Anesthesiologists (ASA) guidelines (any solid content or > 1.5 mL/kg of clear fluid), which was seen in 13 with diabetes (15.5%) and 11 (11.5%) without.
Published in Anesthesiology, the findings offer reassurance that different fasting instructions generally aren't needed for people with diabetes in order to minimize the risk for perioperative pulmonary aspiration, lead author Anahi Perlas, MD, professor of anesthesiology and pain medicine at the University of Toronto, Toronto, told Medscape Medical News.
"We never change practice completely based on a single study, but I think in general, based on our findings, that most diabetic patients aren't any different from nondiabetics when it comes to their gastric content after fasting, and our standard fasting instructions seem to be just as effective in assuring an empty stomach."
But she added, "If someone has symptoms of gastroparesis or when in doubt, we can always do a gastric ultrasound exam at the bedside and see whether the stomach is full or empty…it's very quick, and it's not difficult to do."
Expert Identifies Noteworthy Study Limitations
In an accompanying editorial, Mark A. Warner, MD, professor of anesthesiology at the Mayo Clinic in Rochester, Minnesota, said the findings "will be very helpful to anesthesiologists," although he noted that the exclusion of people with a BMI > 40 is a limitation.
However, Michael Horowitz, MBBS, PhD, FRACP, director of the Endocrine and Metabolic Unit at the Royal Adelaide Hospital and professor of medicine at Adelaide Medical School in Adelaide, Australia, disputed the study's conclusions. He noted that the sample was small, and the participants had an average A1c of 7.2%. Fewer than half had microvascular or neuropathic complications. Thus, they were healthier than the general population with diabetes.
People with diabetes don't have higher gastric volumes than those without diabetes after following standard preoperative fasting instructions, suggested a study from a team of anesthesiologist researchers.
However, an endocrinologist faulted the study in part because the participants appeared to be healthier than typical populations with type 1 and type 2 diabetes. Moreover, the issue is now further complicated by the widespread use of glucagon-like peptide-1 (GLP-1) receptor agonists for the treatment of both type 2 diabetes and weight loss. These drugs, which were introduced after the study's enrollment period, work in part by delaying gastric emptying.
The new data come from a prospective study of 84 people with diabetes (85% with type 2) and 96 without diabetes, all with a body mass index (BMI) < 40, who were undergoing elective surgery. A gastric ultrasound was used to assess their gastric contents after they had followed the standard preoperative fasting guidelines of stopping solids 8 hours prior to the procedure and clearing liquids 2 hours prior.
There was no significant difference between the two groups in gastric volume (0.81 mL/kg with diabetes vs 0.87 mL/kg without) or in the proportion with "full stomach," as designated by the American Society of Anesthesiologists (ASA) guidelines (any solid content or > 1.5 mL/kg of clear fluid), which was seen in 13 with diabetes (15.5%) and 11 (11.5%) without.
Published in Anesthesiology, the findings offer reassurance that different fasting instructions generally aren't needed for people with diabetes in order to minimize the risk for perioperative pulmonary aspiration, lead author Anahi Perlas, MD, professor of anesthesiology and pain medicine at the University of Toronto, Toronto, told Medscape Medical News.
"We never change practice completely based on a single study, but I think in general, based on our findings, that most diabetic patients aren't any different from nondiabetics when it comes to their gastric content after fasting, and our standard fasting instructions seem to be just as effective in assuring an empty stomach."
But she added, "If someone has symptoms of gastroparesis or when in doubt, we can always do a gastric ultrasound exam at the bedside and see whether the stomach is full or empty…it's very quick, and it's not difficult to do."
Expert Identifies Noteworthy Study Limitations
In an accompanying editorial, Mark A. Warner, MD, professor of anesthesiology at the Mayo Clinic in Rochester, Minnesota, said the findings "will be very helpful to anesthesiologists," although he noted that the exclusion of people with a BMI > 40 is a limitation.
However, Michael Horowitz, MBBS, PhD, FRACP, director of the Endocrine and Metabolic Unit at the Royal Adelaide Hospital and professor of medicine at Adelaide Medical School in Adelaide, Australia, disputed the study's conclusions. He noted that the sample was small, and the participants had an average A1c of 7.2%. Fewer than half had microvascular or neuropathic complications. Thus, they were healthier than the general population with diabetes.
"They've picked the wrong group of diabetics," said Horowitz, who specializes in gastrointestinal complications of diabetes. "This is not a group where you would expect a very high prevalence of delayed emptying."
Gastric emptying of solids and liquids varies widely even among healthy people and more so in those with type 2 diabetes. About a third of those with above-target A1c levels have gastroparesis, while those more in the target range tend to have accelerated emptying, he explained.
And regarding the use of gastric ultrasound for those who are symptomatic, Horowitz said, "The relationship of symptoms such as nausea, vomiting, fullness, whatever it may be, with the rate of gastric emptying is weak at best. The association is not simply cause and effect."
Are the Fasting Guidelines Flawed, Regardless of Diabetes Status?
Horowitz also faulted the ASA's 2017 guidance revision for allowing clear liquids to be consumed up to 2 hours in advance of anesthesia because it doesn't distinguish between liquids with and without calories.
"Whether you have diabetes or not, if you are allowed to have a sugar drink up to 2 hours before your operation, the majority of people empty at about 4 kcal/min, so they will still have some of that drink in their stomach," he said. "If you want an empty stomach, the ASA guidelines are wrong."
That explains why the study found relatively high rates of "full stomach" in both groups, 15.5% of those with diabetes and 11.5% of those without, he said.
The GLP-1 Agonist Factor
Although the study didn't address GLP-1 receptor agonist use, Warner did in his accompanying editorial, noting that the drugs' rapid expansion "will likely change how we use perioperative fasting guidelines. With these medications delaying gastric emptying times, we now have another risk factor for pulmonary aspiration to consider when applying fasting guidelines. The inconsistent impact of GLP-1 agonists on gastric emptying, ranging from little to significant, makes it difficult for anesthesiologists to gauge whether or not patients taking GLP-1 agonists are likely to have preoperative gastric liquid or solid contents that could cause subsequent damage if regurgitated."
Gastric ultrasound can be helpful in this situation, Warner wrote. In addition, he endorsed the 2023 ASA guidance, which calls for withholding daily-dosed GLP-1 agonists on the day of the surgery and the weekly formulations for a week. And if gastrointestinal symptoms are present, delay elective procedures.
But Horowitz said those recommendations are likely insufficient as well, pointing to data suggesting that daily liraglutide can delay gastric emptying for up to 16 weeks in about a third of patients. Such studies haven't been conducted by the manufacturers, particularly on the once-weekly formulations, and the ensuing risk for aspiration isn't known.
"The slowing occurs in much lower doses than are used for glucose lowering," Horowitz said. "It is very likely that plasma levels will need to be extremely low to avoid gastric slowing. The current guidelines fail to appreciate this. So, to withhold the short-acting drugs for 1 day is probably wrong. And to stop long-acting drugs for 1 week is almost certainly wrong too."
But as for what should be done, he said, "I don't actually know what you do about it. And no one does because there are no data available to answer the question."
Early Voting Ends Saturday! Meet Your NCMS Member Candidates Here

In-Person Early Voting Ends May 11
The nation is at the six month mark for the November election. In North Carolina, there are tight races across the state. The run-off election is May 14, but early in-person voting ends soon.
The North Carolina Medical Society has interviewed several member candidates on issue important to members. Click here to see what they have to say.
Overview of Early Voting
During the early voting period, voters may cast a ballot at any early voting site in their county. This is different than Election Day, when registered voters must vote at their assigned polling place. During the early voting period, eligible individuals may also register to vote and vote at the same time. See Same-Day Registration below.
Note: In-person early voting for the May 14, 2024, statewide Republican second primary election begins Thursday, April 25, and ends at 3 p.m. on Saturday, May 11. New registration of voters is not permitted between the first and second primaries. This means same-day registration is not available during early voting for the second primary. However, individuals who become eligible to vote between the primary and second primary and who are otherwise eligible to vote in the second primary may register and vote on the day of the second primary — May 14.
For an overview of North Carolina’s current elections, visit Upcoming Election.
Early Voting Sites
Early voting sites and schedules for the 2024 statewide Republican second primary election are available at the Early Voting Site Search. Locations and voting hours are also available to download here: Early Voting Sites for the May 14, 2024 Election (PDF).
Unsure if You Are Registered?
Find out if you are registered to vote by entering your information into the Voter Search.
Don’t Forget Your Photo ID
North Carolina voters will be asked to show photo ID when they check in to vote. Learn more: Voter ID.
Same-Day Registration
When you check in to vote at an early voting site, you may update your name or address within the same county if necessary. Individuals who are not registered to vote in a county may register and immediately vote at that same site. This process is called “same-day registration.” Find more information at Register in Person During Early Voting. Although same-day registration is available for voters during early voting, same-day registration is not available for most voters on Election Day.
Note: Same-day registration at early voting sites is not available during second primaries. However, individuals who become eligible to vote between the primary and second primary and who are otherwise eligible to vote in the second primary may register and vote on the day of the second primary.
Your Sample Ballot
To view sample ballots, registered voters must enter their information into the Voter Search and navigate to “Your Sample Ballot.” Voters can practice making selections with the accessible sample ballot: “Option 4” at the N.C. Absentee Ballot Portal.
Note: Sample ballots for each election are only available once finalized.
By-Mail Absentee Ballot Drop-Off
Voters who receive an absentee ballot by mail may deliver their ballot to their county board of elections office or to an election official at an early voting site during any time that site is open for voting. Ballots will be kept securely and delivered to the county board of elections for processing.
Voting Equipment
Curious which equipment will be at your voting site? Check the interactive map and table: Early Voting Equipment by County.
Voter Assistance and Curbside Voting
Any voter who qualifies for assistance may ask for help at their polling place under Assistance to voters. N.C.G.S. § 163-166.8. To find more information, visit Help for Voters with Disabilities. Curbside voting is available for eligible individuals. For more information, see Curbside Voting.
After You Vote
You can find out whether your vote counted in the “Your Absentee Ballot” section of the Voter Search database. Under North Carolina law, all early votes — by-mail or in-person — are considered absentee votes. Your ballot status also will show up in the “Voter History” section as soon as your county completes the post-election process of assigning voter history to your record. This may take up to a few weeks after Election Day.
NCMS is Celebrating 175 Years!
The North Carolina Medical Society is moving into celebration mode! As the 175th Anniversary Gala gets closer, the headquarters building is getting spruced up!
Check the new sign and flags on Person Street the next time you are in Raleigh (we are right behind the Governor's Mansion).
A special thanks to Garry Linton and Kristen Shipherd for the design and creation of these new banners!
Celebrating AAPI Month at Duke Hospital!

Traveling Mural Symbolizes Connection within Duke’s Asian American and Pacific Islander Community
(Duke News, Bernadette Gillis) -- May is Asian American and Pacific Islander Heritage Month. The Duke Asian American and Pacific Islander Affinity Group will kick off a month of celebrations with the unveiling of a unique traveling mural at Duke Regional Hospital on May 3. The unveiling is the culmination of several events that brought together employees from across Duke, symbolizing the sense of belonging and inclusiveness that the affinity group strives to create.
Made up of more than 300 wooden blocks, the mural depicts the affinity group’s logo and is 4 feet by 6 feet when put together. Over the course of a year, the AAPI affinity group held five events where the Duke community was invited to paint the individual blocks.
The first community painting event, held during the group’s AAPI Heritage Month celebration in May 2023, was the first time members of the affinity group had a chance to come together in person. Prior to that, the group, which was founded in 2021, had held meetings and other events by Zoom.
The painting events, which were also held at Duke Health’s three hospitals and Duke TechExpo, were special in that they offered a chance for members to connect and create a sense of community, said Rebecca Lee, one of the affinity group’s founders and a SharePoint Developer II with Duke Health Technology Solutions.
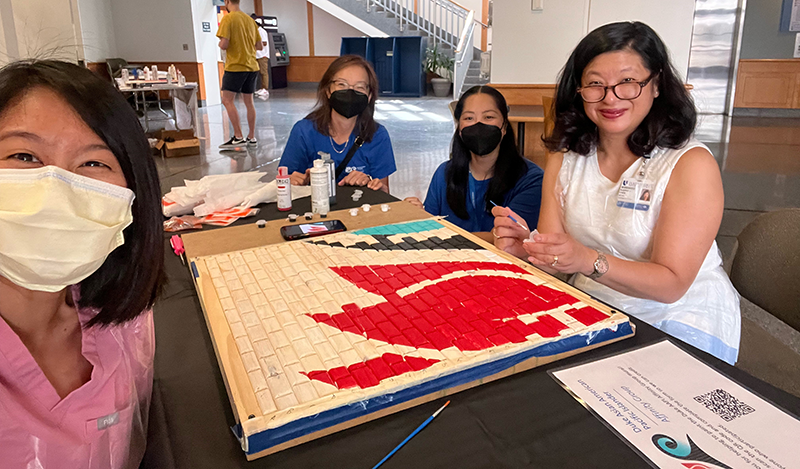
The idea for the AAPI mural first came about after Lee saw a mural that Brandon Johnson created in 2022 for DiversifyIT, a staff-led community that works towards awareness and support for all identities in IT at Duke. The DiversifyIT mural was also created as a community-building event where employees came together to paint the individual blocks.
“With the DiversifyIT project, we found that it was a nice way to build connections between people, so I wanted that for our group as well,” Lee said. “It was very important to us to build these connections because we are stronger together, and it's been a great partnership.”
Lee asked Johnson to partner with the AAPI affinity group. An IT analyst at Duke who enjoys woodworking as a hobby, Johnson described the mural painting events as “art therapy meets the water cooler.”
“People are able to get to know one another and sit beside people that they normally wouldn't have any interaction with on a day-to-day basis, outside of passing them in the hall,” Johnson said. “It facilitates connection.”
Suephy Chen, MD, chair of the Department of Dermatology and one of the AAPI affinity group’s founders, said the mural has created connection for AAPI employees and their allies. She said it was especially meaningful to partner with Johnson and others in the process.
“I thought it was quite symbolic of that partnership with our allies, and given how beautiful the mural is, it is more than the sum of its parts,” Chen said. “The fact that we're having it as a traveling mural is symbolic of its inclusivity. We really want everybody to be able to enjoy it and to understand it.”

The AAPI logo depicts a lotus flower and the Polynesian wave tattoo symbol. Lee said those images were specifically chosen to represent the group’s intention to be inclusive of all AAPI communities.
“The lotus flower is a symbol of rebirth and rejuvenation in a lot of East Asian and South Asian cultures,” Lee said. “And water connects all the Pacific Islands. The wave tattoo is a rite of passage in a lot of Polynesian and Pacific Islander cultures.”
The AAPI Affinity Group mural will be on display at Duke Regional until the fall, after which it will continue its travels to other parts of the Duke campus. Lee said Duke Clinic has offered to provide a permanent home for the mural in the future.
Learn more about upcoming AAPI Heritage Month events hosted by the AAPI Affinity Group.
New Research: Genes Known to Increase Risk of Alzheimer’s May be Inherited
(CNN) -- Alzheimer’s disease may be inherited more often than previously known, according to a new study that paints a clearer picture of a gene long known to be linked to the common form of dementia.
Authors of the study, published Monday in the journal Nature Medicine, say this might even be considered a distinct, inherited form of the disease, and different approaches to testing and treatment may be needed.
Among people diagnosed with Alzheimer’s, researchers recognize familial forms of the disease and sporadic cases. Most cases are thought to be sporadic, which develop later in life. Familial forms, caused by mutations in any of three genes, tend to strike earlier and are known to be rare, accounting for about 2% of all Alzheimer’s diagnoses, or about 1 in 50 cases.
Under the new paradigm, 1 in 6 cases of Alzheimer’s would be considered to be inherited, or familial.
This shifting appreciation of inherited risk, researchers say, is due to a better understanding of the role of a fourth gene that carries the blueprints to make a lipid-carrying protein called apolipoprotein E, known as APOE. APOE ferries cholesterol throughout the body and brain and is thought to play a role in depositing or sweeping away sticky beta amyloid plaques, which are one hallmark of Alzheimer’s.
There are three types of the APOE gene a person can carry. One known as APOE2 is thought to be protective against the development of Alzheimer’s disease. APOE3 is thought to confer a neutral risk of the disease. APOE4, on the other hand, is bad news. It has long been recognized that people with at least one copy of the APOE4 gene have an elevated risk of developing Alzheimer’s disease, while people with two copies had a higher risk still.
Now, researchers say APOE4 shouldn’t just be recognized as a risk factor — it should be viewed as an inherited form of the disease, virtually assuring that a person who has two copies will get the biological changes associated with Alzheimer’s disease in their brains.
Teasing out gene’s role in Alzheimer’s
In the new study, researchers from Spain and the United States compared people in clinical studies with two copies of the APOE4 gene to people with other forms of the APOE gene.
They also compared people with two copies of APOE4 to people with other inherited forms of the disease — early-onset autosomal dominant Alzheimer’s disease (ADAD) and Down syndrome-associated Alzheimer’s disease (DSAD). The study included data from nearly 3,300 brains that are stored at the National Alzheimer’s Coordinating Center and data from another 10,000 people who were participants in five different clinical trials.
Not only were people with two copies of the APOE4 gene much more likely to develop the biological changes that lead to Alzheimer’s disease, similar to people with the other genetic forms of the disease, they were almost assured the diagnosis: Nearly 95% of the people in the studies with two copies of the APOE4 gene had the biology of Alzheimer’s disease by the time they were 82 years old.
When people with two copies of APOE4 do have symptoms, they tend to get them earlier than others. On average, they developed Alzheimer’s about 10 years earlier — around age 65 — compared with people with other forms of the APOE gene. Researchers also found that the buildup of beta amyloid and tau in their brains followed almost the same trajectory as has been noted in people with other inherited forms of the disease. Their disease was more severe earlier in life.
In all the inherited forms of the disease, “there are striking, striking similarities in the way the disease progresses and the symptoms it gets,” said lead study author Dr. Juan Fortea, a neurologist and director of the Memory Unit of the Neurology Department at Hospital de la Santa Creu i Sant Pau in Barcelona, Spain, in a news briefing.
Fortea and his co-authors argue that for these reasons, having two copies of the APOE4 gene should be considered a genetic form of the disease, and not merely a risk for it.
Dr. Charles Bernick, who is associate medical director of the Cleveland Clinic Lou Ruvo Center for Brain Health, said the study was important because it really showed how powerful having two copies of the APOE4 gene was.
“It really drives a disease process,” said Bernick, who was not involved in the study.
Shifting understanding of genetic risks
The strength of APOE4’s role in the development of Alzheimer’s wasn’t recognized earlier, the researchers think, because APOE4 also plays an important role in heart health, and they think many people with two copies of the gene probably died from cardiovascular causes before they developed Alzheimer’s. Previous studies had estimated that 30-35% of people with two copies of the APOE4 gene would develop mild cognitive impairment or dementia.
Researchers say they also found a gene-dose effect. While having two copies of APOE4 assured that a person would see beta amyloid and tau build up in their brains, having just one copy of the gene also increased a person’s risk — but not as much as having two copies of that gene.
That would mean that the APOE4 gene is semi-dominant, Fortea said. Other diseases where genes show semi-dominance include sickle cell anemia and hypercholesterolemia. In sickle cell, for example, two copies of the gene cause sickle cell disease, but one copy causes sickle cell trait. People with sickle cell trait don’t usually have symptoms, but they may be more likely to experience heat stroke or muscle breakdown during strenuous exercise, and they can experience pain crises under certain conditions.
Classifying APOE4 as an inherited form of the disease has some big implications. First, it would mean that a far greater proportion of Alzheimer’s cases are caused by genes than has been previously understood.
Before APOE4, the only gene changes recognized to cause Alzheimer’s were associated with early-onset forms of the disease and with Down’s syndrome. They accounted for about 2% of Alzheimer’s cases — about 1 in 50.
People with two copies of the APOE4 gene make up about 15% of people who are diagnosed with Alzheimer’s, or 1 in 7 cases of the disease.
About 2% of the general population carries two copies of the APOE4 gene, which would make it one of the most prevalent inherited diseases.
Gene testing isn’t currently recommended
It is also likely to change how people who carry the APOE4 gene are diagnosed and treated.
There are tests available to determine a person’s APOE4 status, but they’re not recommended as a routine part of diagnosis. That may need to change, the study authors said.
“The consensus and the guidelines now do not recommend testing for APOE4 and that was because the consensus was that it did not help for the diagnosis,” Fortea said.
APOE testing is recommended for patients who are being evaluated to take new amyloid-clearing medications, such as lecanemab.
Because Alzheimer’s patients with two copies of the APOE4 gene are at greater risk for serious side effects like brain swelling from new amyloid-clearing medications, some treatment centers have decided not to offer them the drugs, said study author Dr. Reisa Sperling, director of the center for Alzheimer’s Research and Treatment at Brigham and Women’s Hospital.
“I find this very problematic given these data,” she said, noting that it would be important to do research to see if it might be possible to find safer dosing or safer treatments for this patient group.
“For me, this just means we need to treat them earlier,” Sperling said, “and this research really suggests that we should be treating them quite early, at a younger age, and at an early stage of pathology because we know they are very, very likely to progress to impairment quickly.”
Dr. Sterling Johnson, who leads the Wisconsin Registry for Alzheimer’s Prevention at the University of Wisconsin, said it would be very important for clinical trials to start to take participants’ APOE4 status into account.
“We may need to start treating these as a separate group in our research papers so that we can really understand the relationship between amyloid and tau and symptoms” in people with two copies of the APOE4 gene, in a way that we kind of have not been able to before, said Johnson, who is also a study author, in the news briefing.
Cyberattack on UnitedHealth Firm Forces Doctors to Dig into Personal Savings

Health providers have been struggling with fallout from the Change Healthcare cyberattack
(CNBC, Ashley Capoot) -- On a Sunday in early March, Dr. Angeli Maun Akey noticed something peculiar while making payroll for her private practice in Gainesville, Florida: She was missing $19,000.
Akey owns and operates a primary care practice that serves around 3,500 patients in the area, many of whom suffer from chronic diseases. She opened in 2000 and manages a staff of nearly 20 people. Over the last two decades, Akey said, her practice and patients have been like an extension of her family.
When Akey first noticed the discrepancy in her cash flow, she thought the funds had been embezzled, something she said she’s experienced three times since graduating from medical school. But after searching online, Akey realized she had a much bigger problem.
The health-care technology company Change Healthcare had been breached in a cyberattack.
Change Healthcare offers payment and revenue cycle management tools, and other solutions such as electronic prescription software. On Feb. 21, UnitedHealth Group, which owns Change Healthcare, discovered that hackers compromised part of the unit’s information technology systems.
UnitedHealth said in a filing with the U.S. Securities and Exchange Commission that it isolated and disconnected the impacted systems “immediately upon detection” of the threat. In its first-quarter earnings report in April, UnitedHealth said the total cost of the cyberattack could be as much as $1.6 billion for the full year. The company’s stock is down nearly 8% year to date.
Akey said the outages from the cyberattack reduced her practice’s cash flow by more than 80% for six weeks. As of early April, she said, she had amassed more than $130,000 worth of insurance claims that she had not been able to get reimbursed for.
Making payroll quickly became a major concern, and Akey said she stopped paying her own salary to help support her staff. Her bank offered her a loan to keep her practice afloat, but it came with an 11% interest rate. Akey said she felt it was too high.
She turned to her patients for help, asking for voluntary $45 advances that would be repaid.
“I’ve had patients for like a quarter century, so a lot of them have been like, ‘No, no, I need to give you more.’ So there’s $100 checks, $200 checks, $500 checks, $2,000 checks,” Akey said. “They have had 0% responsibility for this situation, and they’re fronting the money to keep us going.”
Earlier this month, Akey liquidated her retirement investments as an extra precaution. She said she was feeling frustrated and vulnerable, especially as rumors were swirling about the possibility that a second breach had occurred. UnitedHealth told CNBC earlier this month that there is “no evidence of any new cyber incident at Change Healthcare.”
“I just decided I can’t do this again,” Akey said.
UnitedHealth said in an April 22 press release that it has been working to bring systems back online, and that Change Healthcare has made “continued strong progress.” Medical claims across the U.S. are flowing at “near-normal levels,” and payment processing by the company is at more than 85% of pre-incident levels, the release said.
“We know this attack has caused concern and been disruptive for consumers and providers and we are committed to doing everything possible to help and provide support to anyone who may need it,” UnitedHealth CEO Andrew Witty said in the release.
Akey said payments have begun flowing back into her practice, though levels are still down between 30% and 40% from where they normally are.
She said the restarted payments have lifted a “humongous weight” off her back, but the road ahead will be difficult. Even so, she thinks her practice will be able to pull through, and she will be able to restore her retirement investments some time in the next few months.
“We love our patients, and that’s why I’m fighting so hard,” Akey said.
A quiet health-care giant

(UnitedHealth Group Inc. headquarters stands in Minnetonka, Minnesota, U.S. Mike Bradley | Bloomberg | Getty Images)
Change Healthcare is not a household name for most Americans and even many health-care workers. Much of the company’s technology helps facilitate billing, payments, benefits evaluations and information exchanges behind the scenes.
Change Healthcare is the largest U.S. clearinghouse for medical insurance claims. A clearinghouse is like a middleman for the transactions between providers — such as doctors, hospitals and pharmacies — and payers — such as insurance companies, Medicare and Medicaid.
A clearinghouse helps deliver the right bills to the correct payers. It’s just one of the ways Change Healthcare touches cash flow within the health-care sector.
The company operates on an enormous scale. Change Healthcare processes more than 15 billion billing transactions annually, and 1 in 3 patient records passes through its systems, according to its website. That means Change Healthcare’s reach extends beyond UnitedHealth’s already sizable customer base.
Money stopped flowing when the company’s systems were disrupted due to the cyberattack, and a major source of revenue for thousands of providers across the U.S. screeched to a halt.
It’s caused a lot of sleepless nights for Dr. Barbara McAneny.
McAneny founded a multidisciplinary private practice with another physician in New Mexico in 1987. The practice now supports a staff of 280 people and offers a range of services, including cancer care. She also served as the president of the American Medical Association, or AMA, a research and advocacy group that represents physicians, from 2018 to 2020.
McAneny said she had tried to prepare for the possibility of a cyberattack, so the practice had contingency plans and funds stashed away to cover payroll and other expenses. However, she said she had “no idea” how she could have prepared for a breach of this magnitude. The practice felt the effects immediately.
“The cash flow for the practice went to zero that day,” McAneny told CNBC in an interview.
She said the practice’s partner physicians stopped taking a salary, and they told employees that they couldn’t approve overtime pay. Expenses became a real concern, but her “major fear” was whether the practice could continue purchasing chemotherapy for the cancer patients who rely on it for treatment.
McAneny’s practice buys chemotherapy from group purchasing organizations, or GPOs. It continued to place orders in the weeks following the cyberattack. But while Change Healthcare was down, there was no money to pay for the treatment. By April 10, the practice owed more than $6 million for chemotherapy alone.
“If the flow of chemotherapy stops from the GPOs that supply our chemotherapy, people will die,” she said.
McAneny said she lived in fear that supply would dry up. The thought had been waking her up in a cold sweat at night.
By mid-April, money started trickling back into McAneny’s practice, and it began chipping away at its $15 million claims backlog. She said claims started moving substantially in the last couple of weeks but that the practice’s cash flow is still only around 70% to 80% of what it normally is.
McAneny said the practice is “significantly in debt,” which will take several months to resolve. She said she is very worried about late fees. Even so, signs of progress have come as a relief.
“I might actually sleep through the night,” she said.
Funding assistance
Early in March, UnitedHealth launched a temporary funding assistance program to help support providers that have experienced cash flow disruptions due to the cyberattack. There are no fees, interest or other costs on top of the payments, and providers have 45 days to repay the funds once standard payment operations resume.
Eligible providers will get funds weekly, and the amount they get is based on the difference between their historical weekly claims or payment volume before the breach vs. after, according to the website.
UnitedHealth said it only has “partial visibility” into most providers’ histories and may be “unable to see the full impact of their needs.” Providers could see a gap in their funding amounts and, if they do, they are encouraged to submit a temporary assistance inquiry form through the website for additional support.
But for doctors such as Akey, the program has been a source of frustration. As of Thursday, Akey said she had been approved for around $31,000 worth of funding. She called the total “woefully inadequate” and said it amounts to less than two weeks of help.
Akey said Tuesday she was not aware she could have applied for additional funding support, despite reading the website and making repeated attempts to contact UnitedHealth.
Sarah Carlson, who owns and operates a marriage and family therapy practice in Boulder, Colorado, had a similar experience with the funding program.
Carlson’s practice amassed a $75,000 claims backlog by early April because of the cyberattack, she told CNBC. She said she had been fronting her employees her own money to make payroll, and after a couple of sleepless nights, she decided to temporarily stop accepting some new clients.
Carlson applied for UnitedHealth’s funding assistance program, but she said the payments up to that point had been negligible. One week, she said, she received just $10.
“It was comical. Literally, I think I laughed,” Carlson said in an interview.
UnitedHealth told CNBC that Carlson had not applied for additional funding. Carlson said she thought she had done so by filling out a new form, separate from her initial application, with information about the total amount of claims she was owed.
McAneny said that as of mid-April she had around $28,000 from UnitedHealth sitting in an account, which is only enough to cover the cost of about two drugs.
“It was useless to me,” she said.
McAneny has since applied for and received additional funding. She said she is using that money to help pay off the chemotherapy bills.
UnitedHealth told CNBC in a statement Tuesday: “We have issued more than $6.5 billion in assistance to providers and we continue to encourage any provider to reach out and our goals has always been to help get the word out to as many providers as possible here.”
A controversial merger

UnitedHealth’s ownership of Change Healthcare has raised eyebrows from the outset.
The company has two major business units: Optum and UnitedHealthcare. Optum offers a range of pharmacy services and consulting services and provides medical care for around 103 million consumers, while UnitedHealthcare provides insurance coverage and benefit services to more than 55 million people globally, according to the company’s website.
UnitedHealth’s reach is already substantial, so when it announced that Optum and Change Healthcare had agreed to combine in January 2021, it alarmed organizations such as the AMA.
The AMA sent a letter to the U.S. Department of Justice in April 2021 arguing the $13 billion deal would have “significant anticompetitive effects” on doctors, hospitals and insurers. The group urged the DOJ to look at the merger.
The DOJ sued to block the deal the following year, arguing that UnitedHealth’s proposed acquisition would harm competition in the sector. The suit was unsuccessful, and Optum announced that it completed its combination with Change Healthcare in October 2022.
In UnitedHealth’s quarterly call with investors in April, CEO Andrew Witty said the company’s ownership of Change Healthcare is “important for the country.” He said the cyberattack likely would have happened either way, but if UnitedHealth did not own the company, Change Healthcare would not have had the resources or support necessary to bring its systems back online.
“We’re going to bring it back much stronger than it was before,” Witty said.
The AMA has also been outspoken about the cybersecurity breach. In a letter to the U.S. Department of Health and Human Services in March, for instance, the organization said it is concerned about the “undue financial hardships facing physician practices” if the cyberattack was not resolved quickly. The AMA said it is particularly concerned about small, rural and less-resourced practices, according to the letter.
In late February, the DOJ launched an antitrust investigation into UnitedHealth, according to a report from The Wall Street Journal. The investigation is exploring issues such as its doctor group acquisitions and the relationships between Optum and UnitedHealthcare, the report said. UnitedHealth declined to comment on the matter during its investor call.
The DOJ declined to comment.
‘It’s a mess’

There’s no quick fix for providers affected by the breach. Switching to another clearinghouse can take weeks to months, and submitting claims manually creates mountains of extra work for practices that are often already overwhelmed with administrative and clerical tasks. Some payers don’t even accept paper claims anymore.
“It’s not been fun,” said Dr. Tyler Kisling, who with his wife owns and operates an orthodontic and pediatric dentistry practice in California.
Kisling said the pair have taken out around $20,000 from their personal savings to help keep things afloat since the cyberattack. The breach has created a lot of stress, Kisling said, and he’s resorted to printing out paper calendars to help keep track of bills and due dates.
The company that operates their practice’s patient management software has worked to get set up with another clearinghouse, but as of April 19, Kisling said it was still not running. The workaround has been to fill out all of the practice’s claims by hand, put them in envelopes and mail them off to insurers. Kisling said the task has been like a new full-time job.
Payments are just starting to trickle in, and Kisling said he thinks it is largely because the practice took steps to mail in claims. There’s still a long road ahead.
“I just don’t know how much longer it’s going to take to catch up with all the backlog,” he said.
McAneny said her practice switched to another clearinghouse during the breach but that they all have different peculiarities that can be difficult to work out. She said she had 5,000 rejected claims in a week, which meant the practice had to go through each one to determine what needed to be fixed.
“The comma goes here, or the date of birth goes over there or whatever they want,” she said.
McAneny said it’s been a “huge amount” of work. Her billing staff has been working a lot of overtime.
Dr. Purvi Parikh, an allergist and immunologist with a private practice in New York City, said her practice reconnected with Change Healthcare after seven weeks of outages. It was a welcome sign of progress, especially because Parikh and the other doctors who own the practice had been covering payroll and expenses out of pocket.
But figuring out how to file seven weeks’ worth of claims has been draining for Parikh’s staff and the practice’s already diminished resources.
“It’s such a waste of everyone’s time,” she told CNBC in an interview. “We spend hours and hours, or even days, trying to figure out where to get money from, how to now resubmit through a new clearinghouse, and then resubmit again back through Change Healthcare. It’s a mess.”
UnitedHealth told CNBC that it has been working to communicate with providers, government officials, health systems, trade associations and customers about the breach from the outset.
The company said it has provided updates through Change Healthcare’s product website, and it launched a separate website about its response to the cyberattack that has received millions of page views. UnitedHealth said it also launched a multimillion-dollar social media and digital campaign to raise awareness about its funding assistance program.
Additionally, UnitedHealth has hosted calls with security executives, providers, customers and advocacy groups that have been attended by thousands, the company said.
Nevertheless, some providers said getting information about the breach has been challenging.
As of mid-April, Parikh hadn’t been able to get anyone from Change Healthcare on the phone. She said she was getting all her information directly from her billing company. There has been “zero communication” from UnitedHealth, Optum or Change Healthcare, she said.
Kisling said his office received no formal notification about the breach, and that he heard about it in the media. His office manager had to call one of the practice’s software vendors to ask what was happening.
“We all just kind of had to figure it out on our own,” he said.
Many doctors have been leaning on one another to share information and tips about how to handle the breach. On platforms such as Doximity, which is a medical website used by more than 80% of U.S. physicians, doctors have been “exchanging notes” about how they’ve managed, said Dr. Amit Phull, the chief physician experience officer at Doximity.
Phull said there were a lot of people posting about the breach who didn’t know what to do. Initial feelings of “bewilderment” quickly progressed to anxiety, fear and anger, he said.
Providers are left with questions

UnitedHealth said in late February that the ransomware group Blackcat was behind the cyberattack. Blackcat, which also goes by the names Noberus and ALPHV, steals sensitive data from institutions and threatens to publish it unless a ransom is paid, according to a December release from the DOJ.
The company said its investigation into the breach is ongoing, and it could be months before the company can identify and notify affected individuals. UnitedHealth is working with law enforcement officials, cybersecurity experts and regulators to assess the breach, according to its website.
On April 22, UnitedHealth told CNBC that it paid a ransom in an effort to protect patient data. It did not specify the amount. The company also confirmed that files containing protected health information and personally identifiable information were compromised.
Providers have been left with questions about what happens next.
“How are they going to keep this from happening in the future?” said John Bieda Jr., who owns and operates a marriage and family therapy practice in California.
Bieda said he founded his practice with funds he inherited from his parents after they died. He told CNBC he is very proud of what he has built, and he wishes his father were around to see it. But he said his experience with the Change Healthcare breach has left him feeling lost, and at times like he does not want to own his own company anymore.
As of Friday, Bieda said he had around $109,000 of claims outstanding. He has taken $241,000 out of his retirement accounts to keep the practice afloat.
“I have been on the verge of tears significantly,” Bieda said. “It just is devastating.”
McAneny said many providers have opened lines of credit due to the breach, which raises questions about how UnitedHealth will address problems around interest, late fees and damage to credit ratings.
“They’ve caused a lot of harm to a lot of practices,” McAneny said. “How are they going to make up for the losses that we have had?”
Measles Cases Now Highest in US Since 2019
Several outbreaks, including one in Chicago, led to an early spike in measles cases this year. A chart shows how the case count compares to past years
(NBCNews, Aria Bendix and Joe Murphy) -- This year's measles case total is now the highest of the last five years. The United States has seen 125 cases across 17 states as — its largest annual tally since 2019, according to the Centers for Disease Control and Prevention.
From January to March, the U.S. recorded around 30% of the total cases seen since the beginning of 2020, according to a CDC report released earlier this month.
The authors warned that the rapid increase in cases "represents a renewed threat to elimination."
Most cases reported this year were linked to international travel, and the majority were among people who had not received a measles, mumps and rubella (MMR) vaccine or whose vaccination status was unknown.
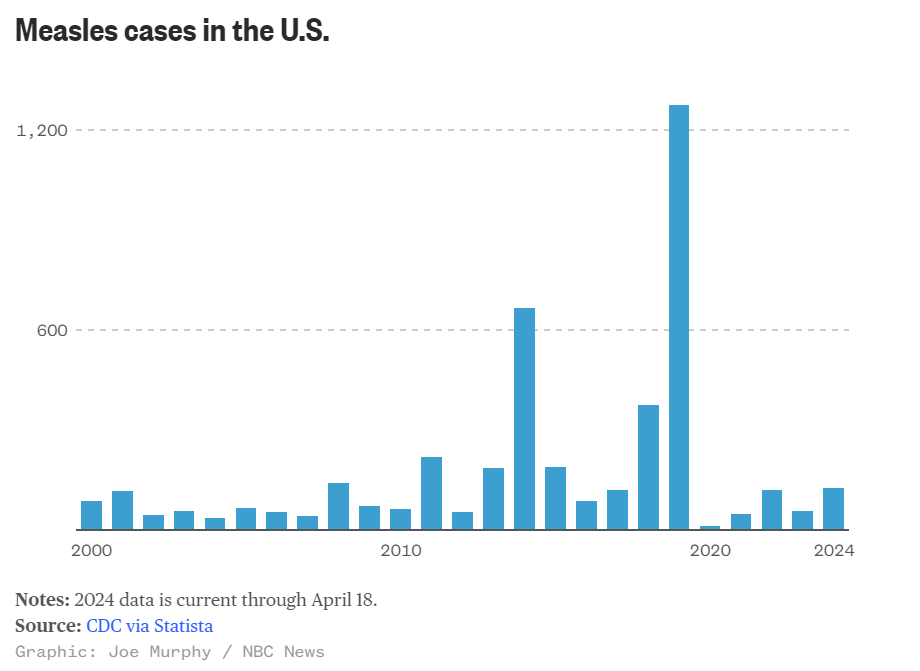
Two doses of the vaccine are 97% effective, but the CDC said in an advisory to health care providers last month that "pockets of low [vaccination] coverage leave some communities at higher risk for outbreaks."
This year's early spike in measles cases was driven in part by outbreaks centered in a migrant shelter in Chicago, an elementary school in southeast Florida and a children’s hospital and a day care center in Philadelphia.
Chicago continues to confront its outbreak. As of Monday, its case count had reached 63, with the most recent recorded last week. More than half of the cases were among children under age 5.
Though disease experts have expressed concern about the early rise in cases, the U.S. isn’t close to its total from 2019, when the country nearly lost its measles elimination status. Most of the 1,249 cases that year were associated with outbreaks in Orthodox Jewish communities in New York.
Measles is highly contagious: An infected person can spread it to up to 90% of people close to them if those contacts aren’t immune. Thanks to widespread vaccination, measles was eliminated in the U.S. in 2000 — meaning that it’s no longer constantly present, though there are still occasional outbreaks.
Most people who get measles now are unvaccinated. Children in the U.S. are meant to get their first vaccine dose between 12 and 15 months and their second between 4 and 6 years old.
However, vaccination rates have fallen in the last few years. For nearly a decade, 95% of U.S. kindergartners had received two doses of the MMR vaccine. That rate fell to 94% in the 2020–21 year, then to 93% in the 2022–23 school year.
Measles symptoms usually start with a high fever, cough, conjunctivitis (pink eye) and runny nose. Two to three days later, people may notice tiny white spots in their mouth. On days three to five of symptoms, a blotchy rash often forms at the hairline before spreading to the rest of the body.
Some people may develop severe complications from measles, including pneumonia, swelling of the brain or a secondary bacterial infection. Before measles vaccines became available in 1963, around 48,000 people were hospitalized and 400 to 500 people died of the disease each year in the U.S.
Today, 1 in 5 unvaccinated people who get measles are hospitalized, and roughly 1 to 3 out of every 1,000 children with measles die from respiratory and neurological complications, according to the CDC.
Want to Slow Down Aging? There May Be A Cheap Way To Do It.

A drug taken by millions of people to control diabetes may do more than lower blood sugar
(NPR, Allison Aubrey) -- Research suggests metformin has anti-inflammatory effects that could help protect against common age-related diseases including heart disease, cancer, and cognitive decline.
Scientists who study the biology of aging have designed a clinical study, known as The TAME Trial, to test whether metformin can help prevent these diseases and promote a longer healthspan in healthy, older adults.
Michael Cantor, an attorney, and his wife Shari Cantor, the mayor of West Hartford, Connecticut both take metformin. "I tell all my friends about it," Michael Cantor says. "We all want to live a little longer, high-quality life if we can," he says.
Michael Cantor started on metformin about a decade ago when his weight and blood sugar were creeping up. Shari Cantor began taking metformin during the pandemic after she read that it may help protect against serious infections.
The Cantors are in their mid-60s and both say they feel healthy and have lots of energy. Both noticed improvements in their digestive systems – feeling more "regular" after they started on the drug,
Metformin costs less than a dollar a day, and depending on insurance, many people pay no out-of-pocket costs for the drug.
"I don't know if metformin increases lifespan in people, but the evidence that exists suggests that it very well might," says Steven Austad, a senior scientific advisor at the American Federation for Aging Research who studies the biology of aging.
An old drug with surprising benefits
Metformin was first used to treat diabetes in the 1950s in France. The drug is a derivative of guanidine, a compound found in Goat's Rue, an herbal medicine long used in Europe.
The FDA approved metformin for the treatment of type 2 diabetes in the U.S. in the 1990s. Since then, researchers have documented several surprises, including a reduced risk of cancer. "That was a bit of a shock," Austad says. A meta-analysis that included data from dozens of studies, found people who took metformin had a lower risk of several types of cancers, including gastrointestinal, urologic and blood cancers.
Austad also points to a British study that found a lower risk of dementia and mild cognitive decline among people with type 2 diabetes taking metformin. In addition, there's research pointing to improved cardiovascular outcomes in people who take metformin including a reduced risk of cardiovascular death.
As promising as this sounds, Austad says most of the evidence is observational, pointing only to an association between metformin and the reduced risk. The evidence stops short of proving cause and effect. Also, it's unknown if the benefits documented in people with diabetes will also reduce the risk of age-related diseases in healthy, older adults.
"That's what we need to figure out," says Steve Kritchevsky, a professor of gerontology at Wake Forest School of Medicine, who is a lead investigator for the Tame Trial.
The goal is to better understand the mechanisms and pathways by which metformin works in the body. For instance, researchers are looking at how the drug may help improve energy in the cells by stimulating autophagy, which is the process of clearing out or recycling damaged bits inside cells.
Researchers also want to know more about how metformin can help reduce inflammation and oxidative stress, which may slow biological aging.
"When there's an excess of oxidative stress, it will damage the cell. And that accumulation of damage is essentially what aging is," Kritchevsky explains.
When the forces that are damaging cells are running faster than the forces that are repairing or replacing cells, that's aging, Kritchevsky says. And it's possible that drugs like metformin could slow this process down.
By targeting the biology of aging, the hope is to prevent or delay multiple diseases, says Dr. Nir Barzilai of Albert Einstein College of Medicine, who leads the effort to get the trial started.
The ultimate in preventative medicine
Back in 2015, Austad and a bunch of aging researchers began pushing for a clinical trial.
"A bunch of us went to the FDA to ask them to approve a trial for metformin,' Austad recalls, and the agency was receptive. "If you could help prevent multiple problems at the same time, like we think metformin may do, then that's almost the ultimate in preventative medicine," Austad says.
The aim is to enroll 3,000 people between the ages of 65 and 79 for a six-year trial. But Dr. Barzilai says it's been slow going to get it funded. "The main obstacle with funding this study is that metformin is a generic drug, so no pharmaceutical company is standing to make money," he says.
Barzilai has turned to philanthropists and foundations, and has some pledges. The National Institute on Aging, part of the National Institutes of Health, set aside about $5 million for the research, but that's not enough to pay for the study which is estimated to cost between $45 and $70 million.
The frustration over the lack of funding is that if the trial points to protective effects, millions of people could benefit. "It's something that everybody will be able to afford," Barzilai says.
Currently the FDA doesn't recognize aging as a disease to treat, but the researchers hope this would usher in a paradigm shift — from treating each age-related medical condition separately, to treating these conditions together, by targeting aging itself.
For now, metformin is only approved to treat type 2 diabetes in the U.S., but doctors can prescribe it off-label for conditions other than its approved use.
Michael and Shari Cantor's doctors were comfortable prescribing it to them, given the drug's long history of safety and the possible benefits in delaying age-related disease.
"I walk a lot, I hike, and at 65 I have a lot of energy," Michael Cantor says. I feel like the metformin helps," he says. He and Shari say they have not experienced any negative side effects.
Research shows a small percentage of people who take metformin experience GI distress that makes the drug intolerable. And, some people develop a b12 vitamin deficiency. One study found people over the age of 65 who take metformin may have a harder time building new muscle.
"There's some evidence that people who exercise who are on metformin have less gain in muscle mass, says Dr. Eric Verdin, President of the Buck Institute for Research on Aging. That could be a concern for people who are under-muscled.
But Verdin says it may be possible to repurpose metformin in other ways "There are a number of companies that are exploring metformin in combination with other drugs," he says. He points to research underway to combine metformin with a drug called galantamine for the treatment of sarcopenia, which is the medical term for age-related muscle loss. Sarcopenia affects millions of older people, especially women.
The science of testing drugs to target aging is rapidly advancing, and metformin isn't the only medicine that may treat the underlying biology.
"Nobody thinks this is the be all and end all of drugs that target aging," Austad says. He says data from the clinical trial could stimulate investment by the big pharmaceutical companies in this area. "They may come up with much better drugs," he says.
Michael Cantor knows there's no guarantee with metformin. "Maybe it doesn't do what we think it does in terms of longevity, but it's certainly not going to do me any harm," he says.
Cantor's father had his first heart attack at 51. He says he wants to do all he can to prevent disease and live a healthy life, and he thinks Metformin is one tool that may help.
For now, Dr. Barzilai says the metformin clinical trial can get underway when the money comes in.
New WFU School of Medicine Study: Racial Discrimination Associated with Alzheimer's Disease

Study Suggests Racial Discrimination During Midlife Associated with Alzheimer’s Disease Pathology
Later in Life
(WakeHealth) -- Racial discrimination experienced during midlife is associated with Alzheimer’s disease pathology, according to a new study from researchers at Wake Forest University School of Medicine and the University of Georgia.
The findings appear online today in Alzheimer’s & Dementia: The Journal of the Alzheimer’s Association.
“We know that Black Americans are at an elevated risk of Alzheimer’s disease and other dementias compared to non-Hispanic white Americans, but we don’t fully understand all the factors that contribute to this disproportionate risk,” said Michelle Mielke, Ph.D., professor of epidemiology and prevention at Wake Forest University School of Medicine.
Mielke, who is a co-corresponding author of the study, said that these racial disparities cannot be attributed to only genetic differences and that research suggests that exposure to racism and its associated stress may increase the risk of dementia.
For the present study, the research team used 17 years of data, which included interviews and blood draws, from a sample of 255 Black Americans who participated in the Family and Community Health Study, a multi-site and longitudinal investigation, which was initiated in 1996 and included more than 800 families in the U.S.
Since the beginning of the Family and Community Health Study, data has been collected every two to three years to study the health and well-being of Black Americans.
In the current study, researchers analyzed serum biomarkers, which are associated with Alzheimer’s disease and related dementias, including serum phosphorylated tau181 (p-Tau181), a marker of Alzheimer’s pathology; neurofilament light (NfL), a non-specific marker of neurodegeneration; and glial fibrillary acidic protein (GFAP), a marker of brain inflammation.
To measure racial discrimination, the study team surveyed individuals about discriminatory events they experienced such as encountering disrespectful treatment by store owners, salespeople or police officers, being called racial slurs, being excluded from social activities, and not being expected to do well because of being a Black American.
“We found no correlations between racial discrimination and increased levels of the serum biomarkers in 2008 at Wave 5 when participants were a mean age of 46 years,” said Ronald L. Simons, Ph.D., professor of sociology at the University of Georgia and co-corresponding author of the study. “However, 11 years later when the study participants were roughly 57 years old, we found that increased discrimination during middle age significantly correlated with higher levels of both p-Tau181 and NfL.”
While additional research is needed to better understand the complexity of these processes, Mielke said it’s clear that future studies should also focus on the challenges and racism experienced by Black Americans to further understand their risk of dementia.
“These findings provide evidence that the chronic stress of racial discrimination often encountered by Black Americans in midlife become biologically embedded and contribute to Alzheimer’s disease pathology and neurodegeneration later in life,” Mielke said. “This research can help inform policies and interventions to reduce racial disparities and reduce dementia risk.”
This work was supported by the National Institute on Aging (RF1 AG077386 and R01 AG055393), and the National Heart, Lung, Blood Institute (R01 HL118045).
NCMS Proudly Graduates the 2024 Health Care Leadership and Management Class
Participants from across North Carolina Gather in Raleigh to celebrate!
On Sunday, April 21, 2024, NCMS proudly graduated it’s 2024 Health Care Leadership and Management (HCLM) class of clinicians and health care administrators. HCLM is led by NCMS members, Drs. Genie Komives, CMO, WellCare of NC, and Bryant Murphy, Vice Chairman for Clinical Operations at UNC HealthCare.
The scholars convened in Raleigh at NCMS headquarters last weekend for their final lecture session led by Jonathan Vehar titled, Mastering Leadership. The session culminated a year’s long training that included 1:1 coaching sessions, lecturing, and CBO site visits to glean new management strategies from CFOs, COOs, CEOs, and CMOs throughout the state. Sunday’s session highlighted the work of the scholars where they presented projects demonstrating leadership insights, strategic thinking, financial understanding, and innovation in tackling a real-world problem.
Team One members were comprised of Sankalp Puri, MD; Tambetta Ojong, MD, FAAFP; Nicole Six, LCSW; Kalpana Iyer, MBA. Their presentation was entitled, Fueling Hope: Your guide to beating food insecurity with flavor and fun.
Team Two members were comprised of Colby Dendy, MD, MPH, FAAP; John Nicholls, MD, JD, DFAPA; Debbie Naylor; and Kelly Phillips, MBA. Their presentation was entitled, Revolutionizing Mental Healthcare in Rural North Carolina.
The 2024 cohort participants hailed from Asheville to Wilmington, NC.
HCLM is a renowned leadership program designed to provide a strong framework for professionals in healthcare administrative roles. The program consists of intensive training sessions and tools to navigate organizational financial strategies, negotiate contracts, master leading C-suite executives and more. Scholars are nominated or self-identified as exceptional leaders in their healthcare community to join other elite healthcare leaders throughout NC. To learn how you can join the next HCLM cohort, contact Erica Neal, Manager, Professional Growth.
Congratulations to our 2024 HCLM graduates!
Foundation Friday! Doctors' Day Special Edition

Doctors’ Day Special Recognition
On Doctors’ Day, the NCMS Foundation offered a chance to extend special recognition to individual physicians by donating $10 to the Foundation in their honor. Thank you to generous donors who felt moved to pay public tribute to the following individuals.
Joseph Bell, MD
Chamaine Brooks-Locklear, MD
Cheryl Davis-Lowry, MD
Christina Hardin-Dial, MD
Ginger Jacobs Locklear, MD
Rachel Keever, MD
Shelly Lowery, MD
Gerri Mattson, MD
Robin Peace, MD
Joseph Roberts, MD
Gail Robinson, MD
Stephen Szabo, MD
John H. Wood, MD
Thank you once again for all you do for your patients each and every day!
"I would be dead." Ali Ingersoll is proof that the time is NOW for Prior Auth Reform

RALEIGH -- Ali Ingersoll has turned a tragic accident into a siren call for change in the American healthcare system. She was left paralyzed at 27 and spend seven years facing life altering diagnoses, surgeries, and mountain-after-mountains to climb as she fought for critical healthcare. Her fight for life happened in step with her fight with insurance companies for treatments, medicines, and equipment.
Along the way she became a professional speaker, disability consultant, fierce advocate, and Ms. Wheelchair America.
Ali’s powerfully authentic story serves as a testament to the power of resilience in order to empower others in adapting to the unknown and advocating for inclusivity.
She sat down with NCMS's Randy Aldridge to talk about the multitude of problems she has faced dealing with prior authorization and roadblocks from insurers. Her story is powerful, poignant, and, ultimately, uplifting.
https://youtu.be/2PkNsOG0QDw
After watching, please click here for how you can tell lawmakers that you support Prior Authorization Reform and how important it is to you and your patients. Feel free to share this video with them.
UnitedHealth Cyber Attack- How You Can Secure Your Practice
An Update on How to Secure Your Practice after UnitedHealth Cyber Attack
On February 21, Blackcat, a ransomware group, accessed Change Healthcare’s systems and 6 TB of data. This included medical and dental records, payment information, and patient information from a variety of Change Healthcare partners.
Sentinel, a risk management and benefit solutions company, has offered the following advice:
UNITEDHEALTH CYBERATTACK:
WHAT TO KNOW AND HOW TO PROTECT YOUR PRACTICE
WHO WAS THE TARGET?
The unlucky target was UnitedHealth Group’s Change Healthcare, which is a critical part of the country’s healthcare infrastructure. They coordinate payments, requests for insurers to authorize care, and more. Change Healthcare processes about 50% of medical claims in the U.S. for around 900,000 physicians, 33,000 pharmacies, 5,500 hospitals, and 600 laboratories.
WHEN WAS THE ATTACK?
On February 21, Blackcat, a ransomware group, accessed Change Healthcare’s systems and 6 TB of data. This included medical and dental records, payment information, and patient information from a variety of Change Healthcare partners.
WAS A RANSOM PAID?
Blackcat received $22 Million in Bitcoin on March 1. However, Change Healthcare has not confirmed any payment of a ransom.
WHO WAS AFFECTED?
Any Change Healthcare partners reliant on its systems for payment, claims, processing, etc.
IS CHANGE HEALTHCARE BACK UP AND RUNNING?
Its pharmacy network was 99% restored on March 7 and the electronic payments platform was running as of March 15. Its claims preparation software went back online on March 18.
HOW CAN YOU PROTECT YOURSELF?
- Enable Multi-Factor Authentication (MFA)
Most email platforms (Outlook, Gmail, etc.) allow you to adjust your settings to enable MFA at no cost. Additional MFA products are available for enhanced security.
- Use Difficult to Guess Passwords
Include uppercase, lowercase, numbers, and characters and update passwords regularly. Consider using phrases versus just words as a password.
- Ensure Employees Are Educated on Phishing Scams
To prevent phishing scams from infiltrating your company’s system, it is crucial to educate your employees on how to recognize them. If you need assistance in training your staff, Sentinel offers helpful webinar courses to ensure they are well-equipped to identify and avoid potential threats.
- Get In Touch with Sentinel
Our IT Service Provider Partners are experts in the field of cybersecurity and can help you assess your current controls, identify vulnerabilities, and recommend enhancements to improve your cybersecurity readiness. By working with our trusted partners, you can rest assured that your organization’s cybersecurity is in good hands. Go to sentinelra.com or call 855-490-2528.
Questions About Telehealth? New Guidance for NC Care

Need help telling your patients where to seek telehealth? Here is some simple guidance.
CAN I PROVIDE TELEMEDICINE TO PATIENTS OUT OF STATE?
The policy guidance of the North Carolina Medical Board to licensees practicing telemedicine is that the practice of medicine occurs in the state where the patient is located.¹ If providing medicine to patients in North Carolina, the provider should be licensed in North Carolina. If a North Carolina licensee is intending to practice medicine using telehealth technology, they should check with the licensing board in the state where the patient is located.² Most states require medical providers to be licensed where the patient is located.
ARE THERE EXEMPTIONS FOR OUT-OF-STATE PHYSICIANS CARING FOR NORTH CAROLINA PATIENTS?
- Provider to provider consultations across state lines where a NC licensee remains responsible for the care of the NC patient, but an out-of-state provider consults “on a irregular basis” is allowed.
- Episodic follow up care in which the patient is temporarily located in North Carolina but has an established relationship with an out-of-state provider (i.e. the patient is attending college or is vacationing in North Carolina) is allowed.⁴
WHAT ARE THE RULES FOR PRESCRIBING VIA TELEMEDICINE?
The North Carolina Medical Board expects proper prescribing and monitoring of controlled substances. Patient encounters conducted exclusively through telemedicine may not be deemed suitable. However, prescribing medications via telemedicine is at the professional discretion of the licensee, as long as it is in accordance with state and federal laws and the standards of practice.⁵
1. North Carolina Medical Board Position Statement, 5.1.4: Telemedicine
2. North Carolina Medical Board Position Statement, 5.1.4: Telemedicine
3. North Carolina Medical Board Position Statement, 5.1.4: Telemedicine
4.North Carolina Medical Board Position Statement, 5.1.4: Telemedicine
5.North Carolina Medical Board Position Statement, 5.1.4: Telemedicine
FOLLOW THIS LINK TO DOWNLOAD A FORM FOR YOUR OFFICE: Telehealth_Guidance
Doctors Call to Expand Syphilis Testing during Pregnancy Amid Recent Surge

(The Hill, Miranda Nazzaro) -- The American College of Obstetricians and Gynecologists (ACOG) published new guidance April 18, recommending doctors screen pregnant individuals for syphilis three times during pregnancy.
Obstetricians, gynecologists and other obstetric care professionals are now advised to screen all pregnant individuals for syphilis at the first prenatal care visit, during the third trimester and again at birth.
Previous guidance recommended risk-based testing in the third trimester for those living in communities with high syphilis rates and for those at risk of acquiring the infection during pregnancy.
“There has been a near eightfold increase in congenital syphilis cases in the last decade or more, and from a public health perspective, we recognize that obstetrician–gynecologists and other obstetric care clinicians play a critical role,” Christopher Zahn, a fellow of ACOG, said in a statement.
Zahn said a timely diagnosis and treatment are “key” to reducing syphilis rates, noting the “majority” of cases can be prevented.
Syphilis is a sexually transmitted bacterial infection that can be contracted through direct contact with a sore, or through casual contact with objects like toilet seats, doorknobs, swimming pools, shared clothing or utensils. The infection can also spread from a pregnant person to a fetus.
More than 3,700 babies were born with congenital syphilis in 2022, marking the most cases in more than 30 years, the Centers for Disease Control and Prevention (CDC) said last year.
In its full advisory, the doctors coalition pointed to the CDC’s finding that nearly 9 in 10 congenital syphilis cases “could have been prevented with timely screening and treatment.”
Syphilis transmission to a fetus can lead to the baby having a low birth weight, and it increases the chances the mother will deliver too early or have a stillborn or miscarriage, according to the CDC.
At birth, a babies might not have signs or symptoms of the disease, but if they do not receive treatment, they can develop health issues within a few weeks. These problems include cataracts, deafness, seizures or death, the CDC added.
Benzathine penicillin G is the preferred treatment for syphilis during pregnancy, though the drug has been in short supply since last year. Pfizer, which is the only company manufacturing the drug, said last year it would take until at least the second quarter of 2024 to increase production enough to end the shortage.
Former NCMS President Named President of Duke Regional Hospital

Devdutta Sangvai Takes on His Next Leadership Challenge at Duke Regional
(Duke University School of Medicine, Synclaire Cruel) -- Having a love of science, an eagerness to help people, and a propensity for leadership has propelled Devdutta Sangvai, MD, MBA, into the role of President of Duke Regional Hospital. It’s the latest achievement in his 22-year career at Duke.
“I've been really lucky with the opportunities that I've had,” Sangvai said. “By having groups of people put their trust in me to take on challenges, I have been able to build experience and confidence.”
Sangvai was named interim president of Duke Regional in 2022 and then named president in 2023 by a national search committee. In just two years, Sangvai has already begun to drive positive change. “This is the strongest bond we’ve had with the divisions of family medicine and community health in the last 20 years,” he said. “We have more family medicine doctors and residents taking care of patients at the hospital, and they provide all of our newborn care.”
It's a role he’s long prepared for, having held several leadership positions while at Duke. “I always knew I was going to go into some form of administration, and family medicine provided the ideal clinical foundation for it,” Sangvai said. “It’s one of the ideal specialties needed for a community hospital because both sides are thinking about the patient, other providers the patient is seeing, and the patients’ living environment, which really takes community into context.”
As a family medicine provider and educator, he gained unique insight on how best to lead fellow providers and staff members. “Having faced some of the challenges family medicine providers experience, I can relate and put myself in their shoes,” he said.
“There's about 2,800 people who work here, and everyone aims to deliver the best care to our patients. To be in an atmosphere where you've got that level of spirit around you is inspiring and uplifting, and you find it in different ways.”
- Devdutta Sangvai, MD, MBA
Sangvai also managed to further open the lines of communication and build a stronger foundation with his team. “In some cases, the role of a leader is not necessarily to bring your own expertise, but to create a framework that facilitates an environment for others to share and leverage their knowledge.”
He’s continuously getting feedback from members about what’s working well and what’s not and is able to apply that information when making decisions. However, Sangvai finds that working with his team is the best part of the job.

“There's about 2,800 people who work here, and everyone aims to deliver the best care to our patients. To be in an atmosphere where you've got that level of spirit around you is inspiring and uplifting, and you find it in different ways,” he said.
“You cannot walk through a hallway without strangers saying, ‘Hello, how is your day?’ That care extends to the way we care for our patients,” Sangvai said. “When we do that for each other, it makes caring for our patients that much easier.”
His interest in leadership began very early in life. “Growing up, I had a real affinity for wanting to help make the lives of others better,” Sangvai said. “But I also always liked the idea of being a leader and growing the next generation of leaders.”
He got his first glimpse into the business of health care by joining the Organization of Student Representatives, the student arm of the American Association of Medical Colleges (AAMC). It’s also where he first connected with Lloyd Michener, MD, previous chair of the department.
“I got a better understanding of how much more there is to medicine than just the bedside. I started to think of it as the administrative backbone that all this clinical care is delivered on,” he said. It’s what drove him to pursue his MBA at Duke’s Fuqua School of Business after completing his family medicine and chief residencies at the Medical College of Ohio.
Sangvai then joined the Duke Department of Family Medicine and Community Health in 2001 as a faculty member. “I liked being able to care for patients not only early in life, but through the later years as well, and in many cases, even before they’re born,” he said. But it’s also where he got the opportunity to perform more administrative duties and gain leadership skills. In addition to seeing patients, he was instrumental in setting up community-based clinics, including Lyon Park and Walltown in Durham.
“The unfortunate thing is, the more administrative you do, the less time you have for clinic,” Sangvai said. Despite this, he still manages to treat patients at Duke Family Medicine Center. “It allows me to stay connected to patients, some of whom I've been seeing for over 20 years. It gives me a deeper appreciation of continuing to deliver care.”
He later became a faculty member in the Duke Departments of Pediatrics and Psychiatry & Behavioral Sciences. Additionally, Sangvai is currently Vice President for Population Health Management, and overseeing DUHS Case Management and Duke HomeCare & Hospice. Previously he was the Director of Medical Services for Student Health, Chief of the Division of Family Medicine, Medical director of DukeWell, and associate chief medical officer of Duke University Health System.
Sangvai also chaired the Durham County Hospital Corporation Board of Trustees and held positions within the North Carolina Medical Society, the American Medical Association, and the Association of American Medical Colleges.
As president of Duke Regional, Sangvai is most looking forward to combining the needs of society and Duke’s mission to make positive change in the surrounding community.
Plan Now! NCDHHS Livestream Town Hall: HPV and Cancer Prevention

The North Carolina Department of Health and Human Services will host a live fireside chat and tele-town hall on Tuesday, April 23, from 6 to 7 p.m., to discuss human papillomavirus (HPV) prevention as well as HPV-related cancer guidance, resources and care.
Event participants include:
- Cushanta Horton, MPH, Branch Head, Cancer Prevention and Control Branch, Division of Public Health, NCDHHS
- Nadja Vielot, Ph.D., Assistant Professor of Family Medicine, University of North Carolina at Chapel Hill
Around 85% of people will get an HPV infection at least once in their life. HPV is a common virus and can cause several types of cancers in people of all ages and genders. In North Carolina, rates of HPV-related cancers are higher than the national rates, with head and neck cancers among men accounting for much of that difference.
HPV vaccines help prevent more than 90% of HPV-related cancers, including cervical cancer. HPV vaccines are recommended beginning around age 11, but adults up to age 45 can also receive the vaccine. However, in North Carolina in 2022, nearly half of youth who were eligible for an HPV vaccine had not received all recommended doses.
Fireside chat and tele-town hall panelists will discuss the following:
- HPV prevention, detection and treatment
- Impacts of HPV-related cancers
- Importance of HPV vaccines and recommended screenings
- How to access health care providers, services and resources
Cancer impacts families and communities across North Carolina, from those who have experienced a diagnosis to their loved ones and caregivers. Resources are available to help people access health services, providers and care, stay up to date on vaccines and recommended screenings, manage a cancer diagnosis and find long-term support.
The fireside chat will stream live from the NCDHHS Facebook, Twitter and YouTube accounts, where viewers can submit questions. The event also includes a tele-town hall, which invites people by phone to listen in and submit questions. People can also dial into the event by calling 855-756-7520 Ext. 100654#.
Medicare's Push to Improve Chronic Care Attracts Businesses, but Not Many Doctors

Medicare enrollees with two or more chronic conditions are eligible for Chronic Care Management, which pays doctors to check in with those patients monthly. The service hasn't caught on.
(NPR, Phil Galewitz, Holly K. Hacker) -- Carrie Lester looks forward to the phone call every Thursday from her doctors' medical assistant, who asks how she's doing and if she needs prescription refills. The assistant counsels her on dealing with anxiety and her other health issues.
Lester credits the chats for keeping her out of the hospital and reducing the need for clinic visits to manage chronic conditions including depression, fibromyalgia and hypertension.
"Just knowing someone is going to check on me is comforting," says Lester, 73, who lives with her dogs, Sophie and Dolly, in Independence, Kansas.
At least two-thirds of Medicare enrollees have two or more chronic health conditions, federal data shows. That makes them eligible for a federal program that, since 2015, has rewarded doctors for doing more to manage their health outside office visits.
But while early research found the service, called Chronic Care Management, reduced emergency room and in-patient hospital visits and lowered total health spending, uptake has been sluggish.
Federal data from 2019 shows just 4% of potentially eligible enrollees participated in the program, a figure that appears to have held steady through 2023, according to a Mathematica analysis. About 12,000 physicians billed Medicare under the CCM mantle in 2021, according to the latest Medicare data analyzed by KFF Health News. (The Medicare data includes doctors who have annually billed CCM at least a dozen times.)
By comparison, federal data shows about 1 million providers participate in Medicare.
$62 per patient, per month
Even as the strategy has largely failed to live up to its potential, thousands of physicians have boosted their annual pay by participating, and auxiliary for-profit businesses have sprung up to help doctors take advantage of the program. The federal data showed about 4,500 physicians received at least $100,000 each in CCM pay in 2021.
Through the CCM program, Medicare pays to develop a patient care plan, coordinate treatment with specialists, and regularly check in with beneficiaries. Medicare pays doctors a monthly average of $62 per patient, for 20 minutes of work with each, according to companies in the business.
Without the program, providers often have little incentive to spend time coordinating care because they can't bill Medicare for such services.
Health policy experts say a host of factors limit participation in the program. Chief among them is that it requires both doctors and patients to opt in. Doctors may not have the capacity to regularly monitor patients outside office visits. Some also worry about meeting the strict Medicare documentation requirements for reimbursement and are reluctant to ask patients to join a program that may require a monthly copayment if they don't have a supplemental policy.
"This program had potential to have a big impact," says Kenneth Thorpe, an Emory University health policy expert on chronic diseases. "But I knew it was never going to work from the start because it was put together wrong."
He said most doctor's offices are not set up for monitoring patients at home. "This is very time-intensive and not something physicians are used to doing or have time to do," Thorpe says.
For patients, the CCM program is intended to expand the type of care offered in traditional, fee-for-service Medicare to match benefits that — at least in theory — they may get through Medicare Advantage, which is administered by private insurers.
But the CCM program is open to both Medicare and Medicare Advantage beneficiaries.
The program was also intended to boost pay to primary care doctors and other physicians who are paid significantly less by Medicare than specialists, says Mark Miller, a former executive director of the Medicare Payment Advisory Commission, which advises Congress. He's currently an executive vice president of Arnold Ventures, a philanthropic organization focused on health policy. (The organization has also provided funding for KFF Health News.)
Not "easy money"
Despite the allure of extra money, some physicians have been put off by the program's upfront costs.
"It may seem like easy money for a physician practice, but it is not," says Dr. Namirah Jamshed, a physician at UT Southwestern Medical Center in Dallas.
Jamshed says the CCM program was cumbersome to implement because her practice was not used to documenting time spent with patients outside the office, a challenge that included finding a way to integrate the data into electronic health records. Another challenge was hiring staff to handle patient calls before her practice started getting reimbursed by the program.
Only about 10% of the practice's Medicare patients are enrolled in CCM, she says.
Jamshed says her practice has been approached by private companies looking to do the work, but the practice demurred out of concerns about sharing patients' health information and the cost of retaining the companies. Those companies can take more than half of what Medicare pays doctors for their CCM work.
Dr. Jennifer Bacani McKenney, who runs a family medicine practice in Fredonia, Kansas, with her father — where Carrie Lester is a patient — says the CCM program has worked well.
She says having a system to keep in touch with patients at least once a month has reduced their use of emergency rooms — including for some who were prone to visits for nonemergency reasons, such as running out of medication or even feeling lonely. The CCM funding enables the practice's medical assistant to call patients regularly to check in, something it could not afford before.
For a small practice, having a staffer who can generate extra revenue makes a big difference, McKenney says.
While she estimates about 90% of their patients would qualify for the program, only about 20% are enrolled. One reason is that not everyone needs or wants the calls, she says.
While the program has captured interest among internists and family medicine doctors, it has also paid out hundreds of thousands of dollars to specialists, such as those in cardiology, urology and gastroenterology, the KFF Health News analysis finds. Primary care doctors are often seen as the ones who coordinate patient care, making the payments to specialists notable.
A federally funded study by Mathematica in 2017 found the CCM program saves Medicare $74 per patient per month, or $888 per patient per year — due mostly to a decreased need for hospital care.
The study quoted providers who were unhappy with attempts to outsource CCM work. "Third-party companies out there turn this into a racket," the study cites one physician saying, noting that companies employ nurses who don't know patients.
Nancy McCall, a Mathematica researcher who co-authored the 2017 study, says doctors are not the only resistance point. "Patients may not want to be bothered or asked if they are exercising or losing weight or watching their salt intake," she says.
How outsourcing works
Still, some physician groups say it's convenient to outsource the program.
UnityPoint Health, a large integrated health system based in Iowa, tried doing chronic care management on its own, but found it administratively burdensome, says Dawn Welling, the UnityPoint Clinic's chief nursing officer.
For the past year, it has contracted with a Miami-based company, HealthSnap, to enroll patients, have its nurses make check-in calls each month, and help with billing. HealthSnap helps manage care for more than 16,000 of UnityPoint Health's Medicare patients — a small fraction of its Medicare patients, which includes those enrolled in Medicare Advantage.
Some doctors were anxious about sharing patient records and viewed the program as a sign they weren't doing enough for patients, Welling says. But she says the program has been helpful, particularly to many enrollees who are isolated and need help changing their diet and other behaviors to improve health.
"These are patients who call the clinic regularly and have needs, but not always clinical needs," Welling says.
Samson Magid, CEO of HealthSnap, says more doctors have started participating in CCM since Medicare increased pay in 2022 for 20 minutes of work, to $62 from $41, and added billing codes for additional time.
To help ensure patients pick up the phone, caller ID shows HealthSnap calls as coming from their doctor's office, not from wherever the company's nurse might be located. The company also hires nurses from different regions so they may speak with dialects similar to those of the patients they work with, Magid says.
He says some enrollees have been in the program for three years and many could stay enrolled for life, which means they can bill patients and Medicare long-term.
New Report: Evidence of Racial Disparities in Healthcare Now Reported in Every US State

Researchers found health system performance is worse for many people of color.
(ABC News) -- Racial and ethnic disparities in health care are evident in every state, even those with robust health systems, according to a new analysis from the Commonwealth Fund.
In the analysis from the organization, which is aimed at promoting equitable health care, researchers found health system performance is markedly worse for many people of color compared to white people.
"Even among high performing states, we see significant disparities," Joseph Betancourt, M.D., President of the Commonwealth Fund, said in a report on the organization’s updated findings.
Six states were found to have better-than-average health system performance among all racial or ethnic groups, including Rhode Island, Massachusetts, Connecticut, Hawaii, New Hampshire and New York. However, even among these high-scoring health systems, racial disparities were observed.
"This report demonstrates that if you don't look under the hood, you won't identify where you're failing people and where you're leaving people behind," Betancourt said.
Particularly when looking at health outcomes, large disparities in premature deaths from avoidable causes are apparent in all states. Black, and American Indian and Alaska Native (AIAN) people are more likely to die before age 75 from preventable and treatable causes, including, but not limited to, some infections such as appendicitis and certain cancers, than white populations, according to the analysis.
There are also large disparities in health care access between white people and other racial or ethnic groups across all states. Despite coverage expansion by the Affordable Care Act in recent years, states' uninsured rates are generally higher and more variable for Black, Hispanic, and AIAN adults compared to Asian American, Native Hawaiian, and Pacific Islander (AANHPI) and white adults, according to the analysis. In particular, Hispanic people had the highest uninsured rates and cost-related difficulties in accessing care in almost all states.
"These groups have more problems accessing care and if quality of care is lower, then they have worse health outcomes compared to white people in many states," Senior Scientist David Radley, Ph.D., of the Commonwealth Fund, said in the report.
The analysis, which was done using publicly available databases reporting outcomes from more than 328,000,000 people during the years 2021 and 2022, concluded that achieving health equity requires policy action and health system action, including:
- Ensuring affordable, comprehensive, and equitable health insurance coverage for all
- Strengthening primary care
- Improving health care quality and delivery
- Health systems and providers prioritizing and centering equity
- Investing in social services
- Improving the collection and analysis of racial and ethnic data to identify gaps
- Developing equity-focused measures to inform and evaluate policy
"Some of the major takeaways of this work is that we still have a lot of work to do," Senior Scholar and Commonwealth Fund Vice President Sara R. Collins said in the organization’s report. "Maybe in a decade we'll look at this data and we'll see some of these gaps closing.”
Dr. Laurie Zephyrin, a senior vice president for the Commonwealth Fund, said undertaking the prescribed action will likely help.
"The reality is we can't improve healthcare if we're not accurately measuring and tracking these outcomes and experiences and using real data as a guidepost to ensure that we are advancing towards equity. ... All these comprehensive actions are truly a start. It really can help us move forward to advance health equity and address many of the inequities that we talked about today," she said in the report.
The Commonwealth Fund’s State Scorecard on Health System Performance series evaluated each state’s health care system and is a tool developed to understand health inequities and disparities. It uses 25 data indicators to designate a "State Health Equity Score," which indicates each state health system’s performance based on health care access, quality, service use and health outcome. Scores were also determined for each of five racial or ethnic groups (Black, AIAN, AANHPI and Latinx/Hispanic) during the years 2021 and 2022, notably incorporating post-pandemic effects on health disparities.
8th Annual Pirates vs. Cancer Event Raises $15k at ECU

ECU medical students lead Pirates vs. Cancer fundraiser for pediatric cancer patients
Some have watched loved ones fight the disease, while others have worked with cancer patients during clinical rotations. Other students and alumni have even been cancer patients themselves.
Whatever their unique experiences with cancer have been, the response has been powerful. Their encounters with cancer turned into a growing tradition that benefits children from across eastern North Carolina who are fighting cancer battles of their own.
The eighth annual Pirates vs. Cancer event on April 12 raised close to $15,000 for pediatric cancer patients at ECU Health’s James and Connie Maynard Children’s Hospital.

Several Brody School of Medicine faculty volunteered to be pied in the face by students as one of the event’s fundraising activities.
Led by Brody students, the fundraiser has gained popularity and momentum over the years, with volunteers having their hair cut and donated, getting their heads shaved and even — for special faculty volunteers — receiving a pie to the face in support of the cause.
“One thing that I love about Pirates vs. Cancer is that you are able to see with your own eyes the direct impact of this work on the children at Maynard Children’s Hospital,” said Carly Uhlir, Brody student and event coordinator for Pirates vs. Cancer. “We know that every dollar we raise will add up to make a difference. Kids with pediatric cancer are more than just patients — they are among the strongest and bravest in our community. I want to continue the Pirates vs. Cancer mission that the founders so strongly believed in years ago and that has transcended all these years.”
Dr. Cedric Bright, senior associate dean of admissions for Brody, volunteered to receive pies in the face during the event on the lawn of the Health Sciences Student Center.
“It does your heart good to help the students with this type of thing to support those that are going through trying times with cancer,” he said. “Patients teach us so much, and this is just one way of us trying to give back to those patients that teach us so much.”
Jillian Berntsen of Kinston had her hair cut as an audience looked on and cheered — much like the health care teams and supporters helping her daughter during her cancer journey.
Berntsen said her daughter is receiving in-patient care at Maynard Children’s Hospital, her latest stay stretching for nine weeks. Pirates vs. Cancer gave the family a welcome respite from the hospital walls.

Jillian Berntsen of Kinston had her hair cut as her family watched. Berntsen said her daughter is receiving in-patient care at Maynard Children’s Hospital. (ECU photos by Steven Mantilla.)
“There are so many things this hospital does, and the people we get to interact with have really become our family at this point from everything she’s been through,” Berntsen said. “We never really thought we’d have to experience anything like this and had no idea that things like this existed. This is the first time we’ve left the hospital in nine weeks, and knowing we had this to look forward to all week was something to get us through another week.”
The event was also eagerly anticipated by Brody students and community volunteers who wanted to help create a memorable and meaningful way to benefit pediatric patients. It has become part of a lifeline of support that keeps this special patient population equipped with resources to help them during their cancer journeys.
“The funds raised by PVC are critical to the maintenance of a positive environment for pediatric cancer patients here in Greenville,” said Grant Irons, Brody student and interdisciplinary chair of Pirates vs. Cancer.
Irons, who plans to pursue medical oncology as a specialty and spent time before medical school working with cancer patients, said the event also offers students a chance to see the realities of what some patients face and an opportunity to pause and look at the bigger picture.
“As future health care leaders, it is important to remember why we are here,” he said. “We entered the health care field to improve the lives of others. To become a well-rounded physician, I believe it is important to be involved outside of the classroom. There are endless opportunities to support our patient population here in Greenville, and I would encourage all health sciences students to lend a hand in these efforts.”
Dr. Cathleen Cook, Brody clinical associate professor of pediatric hematology/oncology and faculty advisor for Pirates vs. Cancer, said the event gives students exposure to the care of pediatric patients right here in eastern North Carolina.
“This fundraiser allows them the chance to see their financial contributions directly help these children while they are hospitalized in James and Connie Maynard Children’s Hospital and cared for in our ECU Pediatric Hematology/Oncology Clinic,” Cook said.
Previous donations through the event, she added, have been used to remodel an inpatient playroom, a space of respite for patients undergoing treatment. Pirates vs. Cancer also helps fund a portion of summer camps for pediatric hematology and oncology patients — Camp Rainbow and Camp Hope.
“Often, donors and volunteers are unaware of the administrative costs that are allocated from the proceeds and not able to see their donations at work,” Cook said. “For Pirates vs Cancer, 100% of the donations are re-invested in our pediatric patients, most specifically our oncology patients. It is my vision to continue to engage these future physicians annually and help support their goal of expanding this fundraiser.”
Brody student Katie Holt decided to get involved with the event to make an impact beyond fundraising. She served as this year’s president of Pirates vs. Cancer.
“Helping to put on this event is awe-inspiring because it puts into perspective the actual size of the Brody and health sciences community,” Holt said. “Applying to Brody, you are frequently told about the passion of the community in serving Greenville and eastern North Carolina. Helping to organize this event gives you a front-row seat to this passion in action.”
Holt said the annual event has caught on across the community.
“People I have never met have reached out to us to offer their help,” she said. “Businesses across the community donate their time and money. Employees from all different departments buy T-shirts to support us. Students across the many health sciences schools donate their hair. The event has shown us firsthand that ECU doesn’t just talk about serving others but goes above and beyond to invest in its community.”
Holt said the event, in addition to benefiting pediatric cancer patients, helps center medical students and remind them why they chose health care careers.
“Serving others, through this event or another community service program, benefits the community as well as serves to fight burnout and protect your mental health,” she said. “I know it has done this for me and many others on the Pirates vs. Cancer team by connecting us to something bigger than ourselves and keeping our sights fixed on a point beyond the next test.”
Uhlir said the event brings participants full circle in seeing their own life journeys while also understanding the magnitude of the battles other people face.
“It is both humbling and inspiring. As medical students, we often lose sight of the big picture. These patients have been through so much, so it is an amazing opportunity to be able to support them directly,” she said. “I also think back to all of the children I have known both personally and indirectly from the time I was a kid myself until now, and how this is such a great way of honoring their spirits.”
ECU Names Deans for College of Health and Human Performance, Graduate School

The East Carolina University Board of Trustees approved the appointment of Dr. Nicole Bromfield as dean of the College of Health and Human Performance and Dr. Debra L. Jackson as dean of the Graduate School during its meeting April 12.
Dr. Nicole Bromfield
Bromfield has been appointed dean of the ECU College of Health and Human Performance, effective July 1.
In addition to extensive international academic experience in a 25-year career, including as an assistant professor at the United Arab Emirates University from 2010-16, Bromfield is a seasoned scholar and administrator with 16 years in academic administration in multiple leadership positions.
Her most recent leadership role was as associate dean for academic affairs for the University of Houston’s Graduate College of Social Work, where she has been an associate professor since 2016. Under her four-year tenure as associate dean, the college enjoyed 30% enrollment growth and received a full program reaccreditation. She previously held administrative appointments at Virginia Commonwealth University as a director of student services and as a student services coordinator.

Dr. Nicole Bromfield
“Being selected as the next dean of East Carolina University’s College of Health and Human Performance is an incredible honor,” said Bromfield, who recently served as a Fulbright Research and Teaching Scholar for 20 months at the University of Namibia. “I am delighted to lead our vibrant HHP community dedicated to fostering holistic well-being through groundbreaking research, service and experiential learning, and to work with the college to further foster a welcoming and collaborative environment that supports each one of our talented faculty, staff and students in reaching their full potential. Our collective commitment to enhancing human well-being, academic excellence and collaborative innovation in research, teaching, service and community engagement will continue to guide us in advancing the college’s legacy and impact on eastern North Carolina and beyond.”
Bromfield has completed research projects in the United Arab Emirates, Bangladesh, India, Namibia and other nations. She co-authored a scholarly book, “From Intercountry Adoption to Global Surrogacy: A Human Rights History and New Fertility Frontiers,” and her research has been highlighted in various media outlets, including The Boston Globe, The National UAE newspaper and BBC News.
“Dr. Bromfield’s expertise, academic experiences, and alignment with the dimensions of College of Health and Human Performance are a few of the reasons why I am very excited to welcome Dr. Bromfield to our ECU team,” said Provost Robin Coger. “I also thank interim dean Stacey Altman for her leadership over the last couple of years in collaborating with the faculty, staff and students of CHHP to ensure the many strengths of this critical college.”
HHP has been led by Altman since July 1, 2022. Her tenure will continue until June 30 when she completes her 22 years of service to ECU. Altman is looking forward to welcoming the new dean.
“Dr. Bromfield’s breadth of experience and collaborative style is ideally suited to lead the HHP community to further success and positive impact as we continue to deliver on the promises associated with the ECU mission,” Altman said. “I look forward to supporting her transition to ECU and the position.”
Bromfield earned a doctoral degree in public policy and administration, with a specialization in health policy, from VCU. She holds two degrees from West Virginia University — a Master of Social Work, with a concentration in community organization, and a Bachelor of Arts in sociology and anthropology as a summa cum laude graduate. She has completed academic leadership training with Harvard University, the Council on Social Work Education, the National Association of Deans and Directors, and the University of Houston.
The College of Health and Human Performance offers a wide range of degrees, certificates and other credentials in health education and promotion, human development and family science, interior design and merchandising, kinesiology, recreation sciences and social work, as well as home to Army ROTC and Air Force ROTC. The college serves the region by providing transformative opportunities for students while collaborating and promoting holistic health and well-being.
Dr. Debra L. Jackson
Jackson has been named dean of East Carolina University’s Graduate School, effective July 1.
Jackson takes over for interim dean Dr. Kathleen Cox, who has held the position since July 2022 following the retirement of Dr. Paul Gemperline.
“The work of our Graduate School benefits all of ECU, and Dr. Jackson’s experience and collaborative leadership style will enable the next phases of the development and growth of our Graduate School,” said Coger. “I am also extremely grateful for the leadership of interim dean Kathleen Cox over the last couple of years. These two leaders have already met and are eager to work together and with their teams in the Graduate School and across the university.”

Dr. Debra L. Jackson
Jackson joins ECU after serving two decades at California State University, Bakersfield. In her most recent role as associate vice president for academic affairs and dean of academic programs, Jackson secured $7 million in funds to support student success.
Under her leadership, CSU Bakersfield received a five-year grant from the Department of Education for “Promoting Excellence in Graduate Education and Increasing Hispanic STEM Related Degree Completion.” She also helped secure the 2023 Award for Innovation in Promoting Success in Graduate Education from the Council of Graduate Schools for a California State University system-wide program titled “The Next Step: Building Career Readiness Among Graduate Schools across the CSU.”
“I am very excited to join the Pirate Nation family and look forward to working with the incredible team in the graduate school,” said Jackson.
While at CSU Bakersfield, Jackson also served as the associate dean for graduate and undergraduate studies, interim associate dean for the School of Arts and Humanities, coordinator for the Women, Gender and Sexuality Studies program, and the assessment coordinator for both the School of Arts and Humanities and General Education program. She recently completed a three-year term on the executive board of the Western Association of Graduate Schools.
She is an active member of the Bakersfield community, volunteering with the Women’s and Girl’s Fund, Girl Scouts of Central California South, and the Panama – Buena Vista Union School District Equity Task Force.
Jackson’s research addresses ethical, political and epistemological issues regarding sexual violence against women. She earned her Doctor of Philosophy from Purdue University in 2002 and an undergraduate degree in philosophy from Middle Tennessee State University in 1996.
ECU’s Graduate School enrolls over 5,000 students and offers 69 master’s degree programs, two intermediate degree programs, five professional doctoral programs, 13 research/scholarship doctoral programs and 77 graduate certificates.
Hit the Trail! It's a Great Time to See National Parks in North Carolina
It is National Park Week!
National Park Week is an annual celebration of America’s national parks – from iconic vistas to significant historical sites. This year, NPF invites you to celebrate our parks while learning more about the ways we all can help preserve these wonderful places.
Here are some spots in North Carolina
-
NATIONAL SCENIC TRAIL
Appalachian
Maine to Georgia, CT,GA,MA,MD,ME,NC,NH,NJ,NY,PA,TN,VA,VT,WV
The Appalachian Trail is a 2,190+ mile long public footpath that traverses the scenic, wooded, pastoral, wild, and culturally resonant lands of the Appalachian Mountains. Conceived in 1921, built by private citizens, and completed in 1937, today the trail is managed by the National Park Service, US Forest Service, Appalachian Trail Conservancy, numerous state agencies and thousands of volunteers.
-
PARKWAY
Blue Ridge
Blue Ridge Mountains of Virginia and North Carolina, NC,VA
A Blue Ridge Parkway experience is unlike any other: a slow-paced and relaxing drive revealing stunning long-range vistas and close-up views of the rugged mountains and pastoral landscapes of the Appalachian Highlands. The Parkway meanders for 469 miles, protecting a diversity of plants and animals, and providing opportunities for enjoying all that makes this region of the country so special.
-
NATIONAL SEASHORE
Cape Hatteras
Nags Head, Buxton, Ocracoke, NC
The sound of ocean waves, the starry night sky, or the calm of the salt marshes, you can experience it all. Shaped by the forces of water, wind, and storms these islands are ever changing. The plants, wildlife, and people who live here adapt continually. Whether you are enjoying the beach, kayaking the sound, or climbing the Cape Hatteras Lighthouse there is something for everyone to explore!
-
NATIONAL SEASHORE
Cape Lookout
Harkers Island, NC
A boat ride three miles off-shore brings you to the barrier islands of Cape Lookout National Seashore. Horse watching, shelling, fishing, birding, camping, lighthouse climbing, and touring historic villages--there’s something for everyone at Cape Lookout. Be sure to bring all the food, water, and supplies you need (and carry your trash out of the park) when visiting these remote beaches.
-
NATIONAL HISTORIC SITE
Carl Sandburg Home
Flat Rock, NC
“I make it clear why I write as I do and why other poets write as they do. After hundreds of experiments I decided to go my own way in style and see what would happen.” Carl Sandburg's free verse style of poetry, journalism, biography, children's stories, prose writing, and social activism provided a popular voice for the American people of the twentieth century.
-
NATIONAL HISTORIC SITE
Fort Raleigh
Manteo, NC
Fort Raleigh National Historic Site protects and preserves known portions of England's first New World settlements from 1584 to 1590. This site also preserves the cultural heritage of the Native Americans, European Americans and African Americans who have lived on Roanoke Island.
-
NATIONAL PARK
Great Smoky Mountains
the states of NC,TN
Ridge upon ridge of forest straddles the border between North Carolina and Tennessee in Great Smoky Mountains National Park. World renowned for its diversity of plant and animal life, the beauty of its ancient mountains, and the quality of its remnants of Southern Appalachian mountain culture, this is America's most visited national park. Plan your visit today!
-
NATIONAL MILITARY PARK
Guilford Courthouse
Greensboro, NC
"I never saw such fighting since God made me. The Americans fought like demons." - Lt. General Charles, Earl Cornwallis On March 15, 1781, six years into the American Revolution, General Greene and Lord Cornwallis' troops faced off at a small courthouse community. The battle would change the course of the Southern Campaign of the American Revolution.
-
NATIONAL BATTLEFIELD
Moores Creek
Currie, NC
In the early morning hours of February 27, 1776, Loyalist forces charged across a partially dismantled Moores Creek Bridge. Beyond the bridge, nearly 1,000 North Carolina Patriots waited quietly with cannons and muskets poised to fire. This battle marked the last broadsword charge by Scottish Highlanders and the first significant victory for the Patriots in the American Revolution.
-
NATIONAL HISTORIC TRAIL
Overmountain Victory
NC,SC,TN,VA
Stretching 330-miles through four states (Virginia, Tennessee, North and South Carolina) the Overmountain Victory National Historic Trail traces the route used by Patriot militia during the pivotal Kings Mountain campaign of 1780. Follow the campaign by utilizing a Commemorative Motor Route which uses existing state highways marked with the distinctive trail logo, or 87 miles of walkable trails.
-
NATIONAL HISTORIC TRAIL
Trail Of Tears
AL,AR,GA,IL,KY,MO,NC,OK,TN
Remember and commemorate the survival of the Cherokee people, forcefully removed from their homelands in Georgia, Alabama, and Tennessee to live in Indian Territory, now Oklahoma. They traveled by foot, horse, wagon, or steamboat in 1838-1839.
-
NATIONAL MEMORIAL
Wright Brothers
Kill Devil Hills, NC
Wind, sand, and a dream of flight brought Wilbur and Orville Wright to Kitty Hawk, North Carolina where, after four years of scientific experimentation, they achieved the first successful airplane flights on December 17, 1903. With courage and perseverance, these self-taught engineers relied on teamwork and application of the scientific process. What they achieved changed our world forever.
PAI Regulatory Advocacy Update

The latest Physician Advocacy Institute advocacy and federal regulatory developments.
PAI Files Amicus Curiae Brief in No Surprises Act Qualifying Payment Amount (QPA) Case Before U.S. Court of Appeals for the Fifth Circuit
PAI’s brief supports the Texas Medical Association’s (TMA) challenge to certain QPA calculation factors that allow insurers to skew the benchmark downward. Read more.
Federal Trade Commission (FTC), Department of Justice (DOJ) and Department of Health and Human Services (HHS) Prompt Investigation into Private Equity and Corporations’ Influence in Health Care
The cross-government public inquiry will investigate the effects of this trend on quality of care, patient health, workers’ safety and cost. PAI will weigh in. Read more.
Centers for Medicare and Medicaid Services (CMS) Releases Background on Federal Independent Dispute Resolution (IDR) Process Showing Physicians Prevailing in 77% of IDR Determinations
The resource shows a large volume of disputes submitted through the Federal IDR portal and substantial complexity in determining the disputes’ eligibility for the Federal IDR process. Read more.
President Biden Releases Fiscal Year (FY) 2025 Budget
The President's budget prioritizes investment in permanent premium tax credits, Medicaid coverage, drug price negotiation, mental health services and substance abuse treatment initiatives. Read more.
Substance Abuse and Mental Health Services Administration (SAMHSA) Issues Final Rule to Enhance Integrated Care and Confidentiality for Patients with Substance Use Conditions
The rule finalizes changes to the Confidentiality of Substance Use Disorder Patient Records regulations to protect the privacy of patients’ substance use disorder (SUD) treatment records. Read more.
CMS Ends Hospice Benefit Component of Value-Based Insurance Design (VBID) Model
CMS will conclude the Hospice Benefit Component at the end of 2024 and will not accept applications for calendar year (CY) 2025 due to escalating operational difficulties and decreasing participation. Read more.
HHS Releases 2023 Equity Action Plan Update
The 2023 update prioritizes child neglect prevention and care improvement, health care access, maternal health outcomes, behavioral health and diversity in clinical research. Read more.
For information on PAI’s advocacy initiatives, physician payment resources and research, please visit PAI’s website. Healthsperien’s Resource Updates page also has information on key issues in health policy and identifies potential reforms under the Biden Administration, Congress and in the states. Additionally, CMS releases their Quality Payment Program (QPP) Small Practices Newsletter, a monthly resource that provides small practices (15 or fewer physicians) with program updates, upcoming QPP milestones and resources to support their continued participation and success in the QPP. You can sign up here to receive this monthly resource.
PAI Files Amicus Curiae Brief in No Surprises Act QPA Case Before U.S. Court of Appeals for the Fifth Circuit
On March 26, PAI announced it filed an amicus curiae brief with the United States Court of Appeals for the Fifth Circuit supporting TMA’s third challenge to federal regulations implementing the No Surprises Act. In August 2023, United States District Court for the Eastern District of Texas Judge Jeremy D. Kernodle ruled partially in TMA’s favor. The ruling struck down provisions of federal agencies’ interim final rules that depressed the QPA and unbalanced the IDR process but upheld its minimal transparency requirements. The Administration subsequently appealed that decision.
PAI is joined on the brief by 15 state medical associations and six medical specialty societies. PAI’s brief supports TMA’s challenge to certain QPA calculation factors that allow insurers to skew the benchmark downward. The inclusion of “ghost rates”—prices for services a physician never or rarely provides—and out-of-specialty rates and the exclusion of incentive or bonus payments like those in value-based care arrangements depress the insurer-calculated QPA and make the IDR process inherently unfair. Addressing insurer payment practices that threaten patient access to care is foundational to PAI. That principle drives PAI’s support of TMA’s challenges to No Surprises Act implementation and will continue to guide its advocacy for as long as needed.
FTC, DOJ and HHS Prompt Investigation Into Private Equity and Corporations’ Influence in Health Care
On March 5, FTC, DOJ and HHS initiated a cross-government public inquiry to address the growing influence of private equity and other corporations within health care. Private equity and other corporate firms are increasingly participating in health care system transactions. The inquiry will investigate the effects of this trend on quality of care, patient health, workers’ safety and cost. The three agencies issued a Request for Information (RFI) soliciting public feedback about transactions conducted by health systems, private payers, private equity funds or alternative asset managers involving physicians, facilities or services. The RFI seeks comments regarding deals related to a wide range of health care entities and seeks to inform policy efforts to target consolidation and promote and preserve competition throughout the health care marketplace.
PAI is preparing an extensive comment letter in response to this RFI to share key research findings that document how practice acquisitions by private equity firms, insurer-owned entities, hospitals/health systems and large national pharmacies over the past decade have dramatically altered how physicians practice medicine in the United States. The related trend of physicians shifting from independent practice into employment has been equally dramatic, growing steadily every year over the past decade and nearing 80% at the start of 2024.
PAI will also share findings from the recently released employed physician survey for PAI by NORC at the University of Chicago that examined the experiences of physicians employed by hospitals and health systems, venture capital and private equity firms, health insurance companies and staffing agencies. Almost 60% of physicians who practice as employees of hospitals and other corporate entities reported that non-physician practice ownership results in a lower quality of patient care. Most physicians surveyed cited decreased time with patients and greater focus on financial success as factors negatively affecting quality at non-physician-owned medical practices. The survey demonstrates a belief among many employed physicians that corporate ownership may erode foundational aspects of the patient-physician relationship and impact patient outcomes.
CMS Releases Background on Federal IDR Process Showing Physicians Prevailing in 77% of IDR Determinations
On February 16, CMS released public use files for the Federal IDR process between January 1, 2023 and June 3, 2023. The resource notes that the first six months of 2023 were characterized by a large volume of disputes submitted through the Federal IDR portal and substantial complexity in determining disputes’ eligibility for the Federal IDR process. Between January 1, 2023 and June 30, 2023, disputing parties initiated 288,810 disputes through the Federal IDR portal. The number of disputes initiated through the Federal IDR portal over this six-month period was 13 times greater than the Departments of Treasury, Labor and HHS initially estimated for a full calendar year and has grown each quarter. Certified IDR entities rendered 83,868 payment determinations in the first six months of 2023. Physicians were the prevailing party in approximately 77% of payment determinations. Despite the increase in payment determinations, some disputing parties are still awaiting eligibility and payment determinations.
On December 28, PAI submitted a comment letter in response to a surprise billing proposed rule published by HHS. Physicians bear the brunt of the inefficient IDR process as medical practices across the nation experience significant payment delays awaiting eligibility and payment determinations. Widespread failure by insurers to make timely payments once determinations have been made exacerbate the issue further. PAI emphasized that the IDR process needs to be further refined, with input from physicians, to ensure that all parties have incentives to settle disputes more quickly and engage in fair contracting practices.
President Biden Releases FY 2025 Budget
On March 11, President Biden released his budget for FY 2025. The President's 2025 budget prioritizes significant health care investments and aims to expand access to high-quality services and lower costs. Key provisions include permanent premium tax credits, Medicaid coverage, drug price negotiation to reduce prescription costs, and initiatives targeting mental health services and SUD treatment. The budget also addresses health equity, veterans' health care needs and bolstering public health infrastructure. The table below highlights relevant provisions for physicians:

SAMHSA Issues Final Rule to Enhance Integrated Care and Confidentiality for Patients with Substance Use Conditions
On February 8, SAMHSA released a final rule that finalizes modifications to the Confidentiality of Substance Use Disorder Patient Records regulations, which protect the privacy of patients’ SUD treatment records. The rule was informed by the Coronavirus Aid, Relief, and Economic Security Act (CARES Act) that, among other things, required HHS to bring the Part 2 program into closer alignment with the Health Insurance Portability and Accountability Act of 1996 (HIPAA) Privacy, Breach Notification, and Enforcement Rules. The final rule includes the following modifications to Part 2:

CMS Ends Hospice Benefit Component of VBID Model
Beginning in CY 2021, the VBID Model permitted Medicare Advantage Organizations (MAOs) to incorporate the Medicare hospice benefit into their Medicare Advantage (MA) benefits package, known as the Hospice Benefit Component. Due to escalating operational difficulties and decreasing MAO participation, CMS announced on March 4 it will conclude the Hospice Benefit Component at the end of this year and will not accept applications for the CY 2025 Request for Applications for the component. The Hospice Benefit Component of the VBID Model aimed to alleviate coverage inconsistencies for MA enrollees electing hospice and assessed if MAOs covering the Medicare hospice benefit would enhance care quality while remaining budget neutral. Policies within the component, including comprehensive palliative care and concurrent care, fostered collaboration between MAOs and hospice physicians, aiming to mitigate care fragmentation at end-of-life stages. CMS gathered insights from various stakeholders to gauge the component's impact on care quality and safety. The decision to discontinue the Hospice Benefit Component does not indicate its success; CMS plans to evaluate it separately. CMS indicated that it would utilize the lessons learned from the Component and release clarifying guidance later this year.
HHS Releases 2023 Equity Action Plan Update
On February 14, HHS released the 2023 update to the Equity Action Plan related to its implementation of President Biden’s Executive Order on Further Advancing Racial Equity and Support for Underserved Communities Through The Federal Government. In alignment with the Biden-Harris Administration’s whole-of-government equity agenda, this Equity Action Plan supports HHS in advancing health equity and well-being for all. The plan includes the following five priority areas:

Since the release of the HHS’ first Equity Action Plan in 2022, HHS has proposed rules on language access and rules that prohibit discrimination based on disability. Additionally, HHS approved the provision of 12 months of continuous postpartum coverage through CMS in 42 states, D.C. and the Virgin Islands.
PAI is focused on addressing health equity issues for both patients and physicians, especially those in rural areas. This is a complex issue, and PAI will draw on the work of The Physicians Foundation, which has studied the problem of health-related social needs, as it works to advance policies that reduce inequities in health care delivery.
Meet Ali Ingersoll, the Quirky Quad, and Hear Her Take on Prior Auth Reform

Ali Ingersoll, the Quirky Quad, tells her life story, advocates for Prior Auth Reform
RALEIGH -- If you've never heard of Ali Ingersoll, this is your lucky day! She is a force of nature who has overcome unbelievable obstacles to emerge as healthcare advocate, public speaker, podcaster, disability consultant, and Ms. Wheelchair America!
Ali’s life took an unexpected turn when a tragic accident left her paralyzed at 27 leaving her paralyzed from the chest down. While she grappled with feelings of hopelessness through 7 years of life altering diagnoses, she was convinced her life had reached its end. Through her journey of self-discovery, she learned how to shift her thinking through harnessing the power of persistence to overcome incredible adversity.
She now calls herself the Quirky Quad, who normalizes disability "through dark humor and determination." Ali took some time to tell her story to the staff of the North Carolina Medical Society. Her presentation was both awe inspiring and motivational. She talked about how her accident led her down a daunting path of healthcare roadblocks and how she knocked them down one by one.
During her talk with NCMS staff she talked about the need for Prior Authorization reform in North Carolina, because, in her words, if she hadn't worked so hard she "would be dead."
Take a moment and hear her conversation. A full interview with Ali will be coming soon.
https://youtu.be/5j6elOh8n_U
Learn more about Ali here:
NCMS CEO Chip Baggett Addresses NHPCMS, Invites You to White Coat Day in June

New Hanover and Pender County Medical Society Gets Outline of NCMS Priorities from Chip Baggett
(WILMINGTON) -- North Carolina Medical Society EVP/CEO Chip Baggett greeted an excited crowd in Wilmington Wednesday night at the New Hanover Pender Counties Medical Society was treated to an evening hosted by NCMS.
Baggett outlined the strategic priorities of the NCMS and answered questions from the crowd. He stressed how NCMS is working for our members and for patients across the state. Issues included how NCMS is making it easier for you to care for your patients, ensuring you have a choice of where and how you practice, the NCMS Leadership College, and helping you care for yourself so you can continue to show up for your patients.
Guests included NCMS Board member Dr. Claude Jarrett and former NCMS President Dr. Michael Utecht.
The presentation ended with Baggett saying "We are a political animal, medicine is a political animal, society is a political animal, you as doctors are political animals. I think it is really important in a time where everybody is talking about absolutes, we need to be the example of how to live a better society. I believe you do that every single day. Every single day in your clinic you show up and talk to patients who you don't know everything about. You don't know everything that is going on in their life. You don't know what brought them to other problems in their life outside of medical issues. You sit down and have a conversation with them about their needs in that moment. Right then right there. You find a solution. You don't worry about if they voted for the person you voted for, you don't care if they are running for office, you don't care if they can pay their bill. You just see them and take care of them.
Go forth and befriend. Befriend those who don't look, live, love, or vote like you. May your friendships so confuse the world that the church and state have to change their rules to make sense of your friendships. I believe we are doing that. If we can get our friends to do what you are doing on a daily basis we will have a better society. "
Empowered Members Power Change
Flood the General Assembly with White Coats June 12!
There is power in numbers, and a great way to demonstrate that is by joining your colleagues for a day of legislative engagement in Raleigh!
We'll gather at the NCMS headquarters in the morning for a brief overview of the day (and breakfast!). Learn about the latest developments at the NC General Assembly and the best messaging to use when meeting with your legislators. Then head down to the Legislative Building to meet one-on-one with your representatives and attend committee meetings on important healthcare issues. We'll wrap up the day with a Legislative Reception at the NC Museum of History. Share your experiences from the day with other attendees and NCMS staff while enjoying light hors d'oeuvres and drinks!
Space is limited, so be sure to register soon!
Shining Red Eyes and Deafening Noise! The Cicadapocalypse Coming Any Time Now

First Time This Has Happened Since
Thomas Jefferson Was President!
Southeast Should See Them Soon
(CNN) -- In a matter of weeks, they will dig their way out from underground, red eyes shining, deafening song filling the air. It will be a confluence of creatures the likes of which hasn’t been seen in the United States since Thomas Jefferson was president — and won’t happen again until 2245. It’s a rare emergence of insects some are referring to as cicadapocalypse.
Billions of cicadas are set to surface this spring as two different broods — one that appears every 13 years, and another every 17 years — emerge simultaneously. The 13-year group, known as Brood XIX, or the Great Southern Brood, is the largest periodical cicada brood, stretching across the southeastern United States. The Northern Illinois Brood, or Brood XIII, emerges every 17 years.
“It’s rare that we see this size of double brood emergence,” said Dr. Jonathan Larson, an extension entomologist and assistant professor at the University of Kentucky. “We’re talking about an absolute oddity of nature, one of America’s coolest insects.”
Though the idea of a cicadapocalypse may seem foreboding, experts predict that the two broods won’t overlap significantly, and the bugs themselves, while loud and numerous, are harmless. Here’s what you need to know going into cicada season.
What to know about cicada broods
This spring’s bugs are part of a genus, or group, of cicadas in the eastern US known as the Magicicada, or periodical cicadas. Three species emerge on a 17-year cycle, and four species are on a 13-year cycle. (Scientists have long debated the significance of these numbers, which are both prime — some researchers have suggested that emerging on these prime-numbered years makes the periodical cicadas less likely to be killed by predators that have two- or three-year life cycles, but the jury’s still out.)
The pattern periodical species follow is different from that of “annual” cicadas, which don’t actually have an annual life cycle, even though you can see them every summer in much of the United States. The nymphs, or babies, of annual cicadas spend two to five years underground, slowly growing, until they are ready to emerge. There are just so many overlapping generations that there appears to be a steady stream of these cicadas every year.
It’s easy to tell annual and periodical cicadas apart. Annuals tend to emerge later in the year than periodicals. For instance, the “dog day” annual cicadas in the genus Neotibicen tend to show up in the dog days of summer, around August, whereas the periodicals make their appearance in the spring. While there are numerous species of annual cicadas, many of them are large and greenish. Periodical cicadas are smaller and mostly black, with bright red eyes and orange-tinged wings and legs.
Cicadas are divided into groups called broods based upon when they emerge. A brood can contain cicadas from multiple species. As long as they are adults in the same 13- or 17-year cycle at the same time, they count as members of the same brood.
When and where will the cicadas emerge?
This spring’s periodical cicadas will make their appearance when the soil temperature 8 inches (20 centimeters) deep reaches 64 degrees Fahrenheit (about 18 degrees Celsius). It will likely happen sometime in mid-May. The individual bugs’ adult life cycles are just a few weeks, but their emergence will be staggered, so there will be about six weeks of cicadas.
That month-and-a-half period will be jam-packed with loud singing, mating and then dying, like “the most macabre Mardi Gras that you’ve ever seen,” Larson said.
Parts of the Midwest and Southeast are due for cicadas this spring.
Northern Illinois, along with southern Wisconsin, eastern Iowa and northwest Indiana are likely to see bugs from Brood XIII; central and southern Illinois, most of Missouri and scattered areas of Kentucky, Tennessee, Virginia, Maryland, North Carolina, South Carolina, Georgia, Alabama, Mississippi, Louisiana and Arkansas are due to get Brood XIX bugs.
There are some areas of central Illinois where the two broods’ geographic ranges have historically been close to each other and could potentially overlap. However, predictions of a cicadapocalypse — in which Brood XIII and Brood XIX show up at the same place at the same time — are probably an exaggeration.
“We’re not even sure that they’re really going to overlap,” said Dr. Chris Simon, a professor of ecology and evolutionary biology at the University of Connecticut. Her research group at the university maintains a website of cicada information, which includes maps showing where the broods have historically emerged.
The double emergence of Broods XIX and XIII is rare, occurring every 221 years (when the 13-year and 17-year cicadas overlap, as 13 times 17 is 221). These two broods haven’t been aboveground at the same time since 1803, and after this year, they won’t be reunited until 2245.
However, the co-occurrence of different cicada broods, somewhere in the United States, isn’t quite as rare. Such an event last happened in 2015; it’ll happen again in 2037.
Preparing for cicadas
Even though a major overlap of the two cicada broods is unlikely, only getting one brood in an area still means countless bugs.
“You should expect lots and lots of cicada exoskeletons to be covering your trees and shrubs. You should expect to hear lots and lots of noise,” Larson said. The insects are likeliest to be in wooded areas near water, he added.
While the sheer volume of insects, along with their distinctive jackhammer-loud sounds and bright red eyes, might give some people pause, Larson notes that cicadas are harmless. They don’t pose a risk to garden plants. However, if you have young trees, cicadas could potentially damage them when the insects cut into branches to lay their eggs. You can mitigate this harm by covering the trees with cicada nets.
Cicadas won’t bite or sting you or your pets. If your dog eats a cicada or two, he said, the animal will be just fine.
Dogs aren’t the only ones tempted to nosh on cicadas; people have eaten them for thousands of years. “They have kind of a natural, sweet nut flavor,” Larson said. (If you’re allergic to shellfish though, you should avoid eating cicadas — a protein in shellfish that’s tied to allergies is also present in many insects.)
If you live in an area with cicadas making an appearance this spring, you can download community science apps to help researchers studying these bugs.
“The main thing we want people to know is that they should download the Cicada Safari app, which is free on the web, and all they have to do is photograph whatever cicadas they see,” Simon said. Those photographs are sent to scientists, who then map where and when the cicadas are emerging: information vital for scientists studying how climate change affects cicadas and predicting future cicada activity.
Beyond the bigger scientific story of cicadas, Larson said he hopes people will embrace cicada spring simply because it’s a rare chance to see some of the world’s most unusual bug behavior.
“These are some of the coolest insects in America,” Larson said. “I really hope that people will appreciate this for what it is: this unique natural phenomenon that you don’t get anywhere else. It’s beautiful.”
Kate Golembiewski is a freelance science writer based in Chicago who’s especially interested in zoology, thermodynamics and death.
Duke Researchers Lead International Study on Jardiance and Heart Failure

Therapy Shows Promise in Delaying Hospitalizations for Heart Failure
Diabetes drug did not prevent all cardiovascular outcomes, but it did affect hospitalizations
(DukeHealth News & Media) -- About 800,000 people in the U.S. suffer a heart attack every year, and about 30% of them will go on to develop heart failure. There are limited treatments to prevent or slow that development.
A large international study led by Duke researchers investigated whether the diabetes drug empagliflozin (marketed under the brand name Jardiance) might prevent heart failure in patients after they had suffered acute myocardial infarction (heart attack).
While the study found that the drug did not reduce deaths, secondary findings show it did slow the time to first hospitalization for heart failure and reduced the total number of subsequent heart failure hospitalizations.
The secondary findings are published in the journal Circulation and presented at the American College of Cardiology’s Annual Scientific Session on April 6. Other findings from the study, called EMPACT-MI, were also simultaneously published in the New England Journal of Medicine and the Journal of the American College of Cardiology.
Empagliflozin was originally approved for use in patients with diabetes, but investigators chose to study the drug based on earlier findings that it showed benefit in preventing active heart failure from becoming worse. The study was funded by two companies that manufacture the drug - Boehringer Ingelheim and Eli Lilly and Company.
The study enrolled 6,522 patients across 22 countries, with roughly half randomly assigned to receive the therapy and the other half placebo. Both groups otherwise received standard care. Investigators credit the study’s simple design to its broad reach.
The Duke Clinical Research Institute coordinated and led the conduct of the trial.
The study findings on lower rates of heart failure offer some hope and underscore the importance of preventing poor outcomes after a heart attack, according to principal investigator and corresponding author, Adrian Hernandez, M.D., director of the Duke Clinical Research Institute.
“Developing heart failure is one of our major public health problems, and any step that gets us closer to preventing it is a step in the right direction,” Hernandez said. “After a heart attack, we should really be focused on how to prevent problems, especially the development of heart failure. This therapy fills in that gap.”
Hernandez said he would be curious to investigate the secondary findings further, especially because there are so many different factors that can play out after a heart attack.
“Heart attacks are pretty dynamic – in the first 24 hours things can change for the better or the worse; you can end up having a small heart attack or a big one,” Hernandez said. “We don’t know if there could be a difference in results from the therapy depending on the type of event and the timing of giving a treatment. Those could be areas to consider.”
In addition to Hernandez, study authors for the Circulation publication include Jacob A. Udell, W. Schuyler Jones, Stefan D. Anker, Mark C. Petrie, Josephine Harrington, Michaela Mattheus, Svenja Seide, Isabella Zwiener, Offer Amir, M. Cecilia Bahit, Johann Bauersachs, Antoni Bayes-Genis, Yundai Chen, Vijay K. Chopra, Gemma Figtree, Junbo Ge, Shaun Goodman, Nina Gotcheva, Shinya Goto, Tomasz Gasior, Waheed Jamal, James L. Januzzi, Myung Ho Jeong, Yuri Lopatin, Renato D. Lopes, Béla Merkely, Puja B. Parikh, Alexander Parkhomenko, Piotr Ponikowski, Xavier Rossello, Morten Schou, Dragan Simic, Philippe Gabriel Steg, Joanna Szachniewicz, Peter van der Meer, Dragos Vinereanu, Shelley Zieroth, Martina Brueckmann, Mikhail Sumin, Deepak L. Bhatt, and Javed Butler.
Mortality Gap Widens Amid Holes in Rural Healthcare Access, South Has Widest Gap

City-country mortality gap widens amid persistent holes in rural health care access
As Roach tracked the health of Arizona residents, the gap between mortality rates of people living in rural areas and those of their urban peers was widening.
The research analyzed Centers for Disease Control and Prevention death data from two three-year periods — 1999 through 2001 and 2017 through 2019. In 1999, the natural-cause mortality rate for people ages 25 to 54 in rural areas was only 6% higher than for city dwellers in the same age bracket. By 2019, the gap widened to 43%.
The researchers found the expanding gap was driven by rapid growth in the number of women living in rural places who succumb young to treatable or preventable diseases. In the most rural places, counties without an urban core population of 10,000 or more, women in this age group saw an 18% increase in natural-cause mortality rates during the study period, while their male peers experienced a 3% increase.
Within the prime working-age group, cancer and heart disease were the leading natural causes of death for both men and women in both rural and urban areas. Among women, the incidence of lung disease in remote parts of the nation grew the most when compared with rates in urban areas, followed by hepatitis. Pregnancy-related deaths also played a role, accounting for the highest rate of natural-cause mortality growth for women ages 25 to 54 in rural areas.
The negative trends for rural non-Hispanic American Indian and Alaska Native people were especially pronounced. The analysis shows Native Americans 25 to 54 years old had a 46% natural-cause mortality rate increase over those two decades. Native women had an even greater mortality rate jump, 55%, between the two studied time periods, while the rate for non-Hispanic White women went up 23%.
The rural-urban gap grew in all regions across the nation but was widest in the South.
The increased mortality rates are an indicator of worsening population health, the study authors noted, which can harm local economies and employment.
As access to and quality of health services in rural areas continue to erode, rural health experts said, the USDA findings should spur stronger policies focused on rural health.
Alan Morgan, CEO of the National Rural Health Association, said he found the report "shocking," though, "unfortunately, not surprising."
The disparity warrants greater attention from state and national leaders, Morgan said.
The study does not address causes for the increase in mortality rates, but the authors note that differences in health care resources could compromise the accessibility, quality, and affordability of care in rural areas. Hospitals in small and remote communities have long struggled, and continued closures or conversions limit health care services in many places. The authors note that persistently higher rates of poverty, disability, and chronic disease in rural areas, compounded by fewer physicians per capita and the closure of hospitals, affect community health.
Roach said his past job as an epidemiologist included working with social vulnerability indexes, which factor in income, race, education, and access to resources like housing to get a sense of a community's resilience against adverse health outcomes. A map of Arizona shows that rural counties and reservations have some of the highest vulnerability rankings.
Janice C. Probst, a retired professor at the University of South Carolina whose work focused on rural health, said many current rural health efforts are focused on sustaining hospitals, which she noted are essential sources of health care. But she said that may not be the best way to address the inequities.
"We may have to take a community approach," said Probst, who reviewed the report before its release. "Not how do we keep the hospital in the community, but how do we keep the community alive at all?"
The disparities among demographics stood out to Probst, along with something else. She said the states with the highest rates of natural-cause mortality in rural areas included South Carolina, Mississippi, Georgia, Alabama, and others that have not expanded Medicaid, the joint federal and state health insurance program for low-income people, though there are efforts to expand it in some states, particularly Mississippi.
It's an observation the USDA researchers make as well.
"Regionally, differences in State implementation of Medicaid expansion under the 2010 Affordable Care Act could have increased implications for uninsured rural residents in States without expansions by potentially influencing the frequency of medical care for those at risk," they wrote.
Wesley James, founding executive director of the Center for Community Research and Evaluation, at the University of Memphis, said state lawmakers could address part of the problem by advocating for Medicaid expansion in their states, which would increase access to health care in rural areas. A large group of people want it, but politicians aren't listening to their needs, he said. James also reviewed the report before it was published.
According to KFF polling, two-thirds of people living in nonexpansion states want their state to expand the health insurance program.
Morgan added the study focused on deaths that occurred prior to the COVID-19 pandemic, which had a devastating effect in rural areas.
"COVID really changed the nature of public health in rural America," he said. "I hope that this prompts Congress to direct the CDC to look at rural-urban life expectancies during COVID and since COVID to get a handle on what we're actually seeing nationwide."
In Arizona, the leading cause of death for people 45 to 64 in 2021 in both rural and urban areas was COVID, according to Roach.
EPA Takes Action on PFAS Pollution in Drinking Water, NC Response

EPA Announces First-Ever National Standard to Address PFAS in Drinking Water, Delivers an Additional $1 Billion through President Biden’s Investing in America Agenda to Combat PFAS Pollution
WASHINGTON -- The Environmental Protection Agency announced on Wednesday, the first-ever national legally enforceable drinking water standard for PFAS, which will protect 100 million people from PFAS exposure, prevent tens of thousands of serious illnesses, and save lives. Per a release, the move "complements the Biden-Harris Administration’s commitment to combatting PFAS pollution and delivering clean water."
Details of the release:
President Biden has secured historic levels of funding to meet this new standard. Today, the Biden-Harris Administration is also announcing an additional $1 billion through President Biden’s Investing in America agenda to help every state and territory fund PFAS detection and treatment systems to meet the new standard. This funding is part of the $9 billion in dedicated funding through the President’s Bipartisan Infrastructure Law to address PFAS and other emerging contaminants in drinking water – the largest-ever investment in tackling PFAS pollution. An additional $12 billion in funding from the Bipartisan Infrastructure Law supports general drinking water investments, including PFAS treatment. The investments are part of the Justice40 Initiative, which aims to ensure that 40 percent of the overall benefits of certain federal investments flow to disadvantaged communities.
These actions will help tackle PFAS pollution that has devastated communities like Oakdale, outside of St. Paul, Minnesota, where decades of PFAS-containing waste dumped by a chemical plant has contaminated the community’s drinking water. In this area, cancer was found to be a far more likely cause of death in children than in neighboring areas. The funding announced today will build on funding from the President’s Bipartisan Infrastructure Law that is already helping communities address PFAS contamination, including a $33 million award for Tucson, Arizona to treat its PFAS-contaminated drinking water wells.
This funding also builds on President Biden’s action plan to address PFAS pollution, safeguard public health, and advance environmental justice – all while advancing the Biden Cancer Moonshot goal of cutting the cancer death rate by at least half by 2047 and preventing cancer before it starts by protecting communities from known risks associated with PFAS exposure.
As the first-ever Safe Drinking Water Act standard for PFAS – and the first for any new contaminants since 1996 – this rule sets health safeguards and will require public water systems to monitor and reduce the levels of PFAS in our nation’s drinking water, and notify the public of any exceedances of those levels. The rule sets drinking water limits for five individual PFAS, including the most frequently found PFOA and PFOS. Because PFAS can often be found together in mixtures, EPA is also setting a limit for any combination of four PFAS, including GenX Chemicals. This standard will reduce PFAS exposure in our drinking water to the lowest levels that are feasible for effective nationwide implementation.
Today’s announcements advance President Biden’s broader commitment to deliver clean water for every American. The President’s Bipartisan Infrastructure Law invests over $50 billion to upgrade water infrastructure – the largest investment in clean water in American history. This includes a historic $15 billion to replace toxic lead pipes and protect children from brain damage, as part of President Biden’s goal of replacing every lead pipe in the country within a decade.
Recent Federal Actions to Protect Communities from PFAS
Under President Biden’s leadership, nearly two dozen federal agencies and offices have made systematic and substantive progress to safeguard public health and protect the environment from PFAS in drinking water and beyond. This work is coordinated by the White House Council on Environmental Quality, which leads the Interagency Policy Committee on PFAS. Other new actions the Biden-Harris Administration has advanced to combat PFAS pollution over the past year include:
Protecting Firefighters from PFAS: The Biden-Harris Administration is committed to protecting firefighters from the harmful effects of PFAS contained in fire suppressing agents and firefighter gear. The Department of Defense is offering PFAS blood tests to military firefighters. The Federal Emergency Management Agency’s U.S. Fire Administration is working to reduce PFAS exposure and promoting access to early cancer screenings and participation in the National Firefighter Registry for Cancer led by the National Institute for Occupational Safety and Health as part of President Biden’s mission to end cancer as we know it.
Reducing PFAS in Fire Suppressants: The Department of Defense (DoD) qualified three fluorine-free foams to replace fluorinated Aqueous Film Forming Foam for shore-based firefighting activities at military installations, which the Federal Aviation Administration (FAA) has authorized for civilian airports. The FAA is assisting airports to transition to these new foams, and funding foam testing systems for airports that prevent environmental discharge. These changes will reduce the release of PFAS in the environment and protect the health of firefighters and local communities.
Supporting Healthcare Providers: The Agency for Toxic Substances and Disease Registry at the Centers for Disease Control and Prevention recently released the PFAS: Information for Clinicians resource guide. This information gives clinicians up-to-date resources and information they need to help patients with questions and concerns about PFAS exposure and health effects.
Phasing Out PFAS in Food Packaging: The Food and Drug Administration (FDA) announced the completion of the voluntary market phase-out of PFAS used on paper and paperboard food packaging, eliminating the primary source of dietary exposure to PFAS. FDA can now also test for 30 PFAS in a variety of foods to further protect people from dietary PFAS exposure.
Testing for and Cleaning Up PFAS Pollution: EPA continues to take key actions to address PFAS. For example, EPA is gathering data on 29 PFAS in the nation’s drinking water systems has collaborated with DoD to develop a method to test for 40 PFAS in various media including biosolids, groundwater, and fish tissue. EPA also updated its interim PFAS disposal and destruction guidance and has released a new method to test for 30 volatile fluorine-containing compounds in air including potential products of incomplete combustion of PFAS. DoD recently identified 40 installations where interim cleanup actions to prevent further PFAS migration are underway or will start in FY2024. These actions will address PFAS in groundwater to protect public health and the environment.
Reducing PFAS in Federal Procurement: EPA and the U.S. General Services Administration announced this week that custodial contracts for federal buildings will now only use cleaning products certified to ecolabels such as EPA’s Safer Choice and certain Green Seal standards, thereby avoiding products that contain intentionally added PFAS. This shift will protect the environment, federal custodial workers, other federal employees, and those visiting government buildings.
Response in North Carolina
NC Health News reports that on Wednesday, a host peakers including state and federal officials gathered at P.O. Hoffer Water Treatment Facility in Fayetteville to praise the new drinking water standards announced by the Environmental Protection Agency the day before. The safe drinking water standards set maximum contaminant levels for six PFAS, including GenX, which were manufactured at the Chemours Fayetteville Works plant.
All six chemicals found their way into the Cape Fear River, a contamination that was revealed in 2017. The river has been a source of contamination and consternation for people living in the lower Cape Fear basin ever since.
Governor Roy Cooper saying "[The administration] made a big promise that for the first time ever, we would set a national limit on PFAS in drinking water,” Cooper said. “Administrator [Michael] Regan and the Biden administration are delivering on that promise that they made not only to North Carolinians, but to all Americans across this country.”
“Drinking water contaminated with PFAS has plagued communities across this country for too long,” Michael Regan, EPA administrator, said on Tuesday on a call with the media. “President Biden has made tackling PFAS a top priority, investing historic resources to address these harmful chemicals and protect communities nationwide.”
Detlef Knappe, the North Carolina State University professor whose research led to the 2017 news story that revealed GenX, one class of PFAS in the Cape Fear River, said he was pleased by the EPA’s announcement and that North Carolina is ahead of many states in efforts to address PFAS.
NCMS Member Named Physician of the Year at AHHC H.O.M.E. Awards!

Dr. Deric Weiss AHHC H.O.M.E. Physician of the Year
NCMS Member Dr. David Tayloe, Jr. Recognized in US Congressional Record
NCMS Member, Congressman Greg Murphy, MD, Recognizes Dr. David Tayloe in the Congressional Record
April 7, 2024 -- Congressman Gregory Murphy, MD, honored NCMS member Dr. David Tayloe in the Congressional Record.
Here is statement:
"I was honored to recognize an incredible physician, Dr. David Tayloe, in the Congressional Record for his commitment to community healthcare and his passionate advocacy for children.
Dr. Tayloe has led an extraordinary life of servant leadership. Be it caring for children at his practice Goldsboro Pediatrics, spearheading pediatric advocacy in the North Carolina General Assembly, or serving as the President to the American Academy of Pediatrics. He has spent his life caring for the less fortunate at home and abroad. I am in awe of his stewardship.
Thank you for being such an incredible leader in Eastern North Carolina. We are lucky to have you!"
Dr. Tayloe is a North Carolina Medical Society Life Member, a member of the NCMS 1849 Society, and has served on the Goldsboro City School and the Wayne County Public School Boards of Education. He graduated from the UNC-Chapel Hill School of Medicine. He founded Goldsboro Pediatrics in 1978.
NCMS Member Dr. Leo Spector Featured in "Business NC"
OrthoCarolina’s CEO has MD-MBA cred
OrthoCarolina’s new leader merges business acumen with a surgical background.
 (BusinessNC, Kevin Ellis) -- When Charlotte spine surgeon Leo Spector returned to the classroom more than four years ago, his fellow students in the Duke University Executive MBA program peppered him with questions. A disconnect existed, he says, about the business of healthcare and his classmates’ familiarity with nonmedical corporations.
(BusinessNC, Kevin Ellis) -- When Charlotte spine surgeon Leo Spector returned to the classroom more than four years ago, his fellow students in the Duke University Executive MBA program peppered him with questions. A disconnect existed, he says, about the business of healthcare and his classmates’ familiarity with nonmedical corporations.
“Running a factory is not the same as running an operating room, although you can apply some of the same principles,” says Spector, who earned his MBA from Duke in 2020 and became CEO at Charlotte-based OrthoCarolina in January.
Spector, the son of a general orthopedic surgeon in Boston, started working at OrthoCarolina during a fellowship at its spine center 18 years ago. Around the same time, about 45 doctors who had been with Charlotte Orthopedic Specialists and Miller Orthopaedic Clinic formed the physician-owned practice in 2005.
Under previous CEOs Dr. Dan Murrey and Dr. Bruce Cohen, both surgeons like Spector, the practice has grown to about 112 physician shareholders, 472 medical providers and 1,700 employees. It has more than 30 orthopedic practices from Boone to Bennettsville, South Carolina, and as far west as Shelby.
Spine surgeon Murrey left in 2016 and is now chief physician executive for a large specialty care division owned by United Healthcare Group. Cohen, who is a foot and ankle surgeon, has returned to his general practice at OrthoCarolina.
While interviewing him for the job, Spector’s colleagues took note of his degree from Duke, which ranked as the fifth-best Executive MBA program last year, according to U.S. News
& World Report. “I think sort of tongue-in-cheek, they said, ‘OK, now that you’ve got your MBA, you’re ready to be the CEO, right?
“And I said, ‘I’m as ready to be the CEO with my MBA as I was ready to be a doctor with my MD,’ meaning, yeah, you’ve got the schoolwork, but you also have to get the actual practical experience,” says Spector.
Pursuing an MBA was a personal choice, supported by his wife and two children, who were 10 and 14 when he started the 18-month program. He says he had grown confident in his skill as a spine surgeon, a responsibility that terrified him when he was starting his practice. He knew his competency as a spine surgeon had grown when repairing a broken ankle caused him more anxiety than cutting into someone’s back, he notes.
CONSTANT GROWTH
Spector has always been interested in the business of medicine, which led him to leadership positions within OrthoCarolina, including chief quality officer and chair of
the Quality/Value Committee.
“I felt if I wanted to grow as an administrator, I should go back and get the formal education,” he says. “Life is all about learning and growing and constantly developing,” he adds. “Once you stop doing that, what’s the point?”
Spector and his wife, who have been married for 24 years, discussed the MBA’s cost and time commitment. Both agreed that if he didn’t pursue his goal, they’d regret the decision in 10 years. He isn’t sure if the degree factored into him getting the CEO position but counts that as a side benefit.
“I recommend business school to anybody. I really did love that 18-month period of time learning,” he says. “Business school is one of those places where every class is so applicable to life. Like, I took my negotiation class, and my wife didn’t like that because now I can negotiate with her on everything.”
He continued his medical practice during his MBA work and he’s still practicing two days a week. The program required him to spend one weekend a month at the Durham campus, with other coursework completed at night and on weekends. Approximately 20% of his class worked in the healthcare industry, and about half of those were physicians.
Nowadays, he spends a day per week seeing patients in a clinic setting, with a second day focused on surgeries. Keeping his hand in the practice of medicine remains important. “There’s obviously high stakes involved with spinal surgery, but like anything in life where there’s high risk there’s also high rewards,” he says. “There’s a great opportunity to really make a high impact in improving someone’s life and that’s what I love about the job.”
In the medical hierarchy, surgeons rank toward the top in pay. In 2022, orthopedic surgeons had the second-highest average annual compensation ($573,000) for specialists, behind plastic surgeons ($619,000), according to a report by Medscape news service.
“Every surgeon thinks they’re a rock star. You have to have a certain ego to think you should be able to cut open a human body and make it better,” he says. “No matter how big the ego is, they all learn that surgery is a very humbling experience. Typically, when your ego gets a little too big, it’s about to get deflated a little bit because unfortunately surgery doesn’t always go exactly the way we want it to despite the best efforts from the team and the surgeon. Those kinds of things help keep the ego in check.”
OrthoCarolina considers it important that a physician lead the practice. “Part of the desire to have an MD/CEO at OrthoCarolina is to have someone who is trained to take care of the patients every single day and sees the challenges that the providers (of care) face and the patient’s face,” says Spector.
He also sees the benefit of doing both. “When I’m working as an administrator, as the CEO, I can have that direct understanding of one-on-one with the tree (patient) and also that 10,000-foot view of the forest (practice.)”
LEARNING CURVE
Early into his CEO role, Spector says he’s learning about the roles and challenges of his different duties.
“As a surgeon, we’re very much used to being in charge,” he says. “As CEO, I can’t do everyone’s job at OrthoCarolina.” One job requires making quick decisions, the other listening, making sure different perspectives are heard. His Duke training helped him understand he didn’t need to be an expert in finance, marketing or business operations to be a successful CEO.
“My job as CEO is not to do everybody else’s job, it’s to make sure we have a great team and that we’re all pulling in the same direction, which is making sure we’re doing a great job of taking care of patients.”
OrthoCarolina is focused on improving access to care and trying to contain healthcare costs, he says. The enterprise is largely content with its existing markets, which benefit from the region’s strong population growth. The most recent clinic opening was in Fort Mill, South Carolina, one of the fastest-growing Charlotte suburbs.
OrthoCarolina and Durham-based EmergeOrtho employ about 50% of North Carolina’s orthopedic surgeons and account for about half of the musculoskeletal spending, says Spector. Emerge is larger, with about 270 physicians and specialists and 45 offices ranging from Beaufort to Waynesville. The two practices don’t compete in the same cities, except for Hickory, reflecting a conviction that direct competition wouldn’t serve anyone’s best interest, he says.
Last year, the two practices partnered with Optum Healthcare, a subsidiary of UnitedHealth Group, to help both practices control costs and improve outcomes. That partnership, called Health Innovation Value Enterprise, could grow into a “good model to other regions or states” to replicate, he says.
“There’s enough waste in the health care system — as in any industry — if we can help
get that out of the system, there’s plenty of savings to go around for patients to the government to doctors,” he says. Minneapolis-based UnitedHealth is the largest U.S.
health insurer.
Both OrthoCarolina and EmergeOrtho have resisted the trend in medicine to sell ownership stakes to private-equity companies. At least 15 PE-backed management companies own practices nationally, with dozens of sales occurring since 2017, KFF Health News reported last year.
OrthoCarolna’s leadership in its field in the Charlotte region means it works closely with the two dominant hospital systems, Atrium Health and Novant Health. Having both institutions benefits the region and physicians, Spector says. “Monopolies from a business standpoint are typically not the best,” he says. “So having some competition pushes both of them to be better and provide better service to the customer.”
In most cases, OrthoCarolina surgeons consider a patient’s primary healthcare provider and then schedule a procedure at the corresponding hospital. That provides easier access to patient medical records and coordination with primary doctors.
Spector says his life changed when he came to Charlotte for a fellowship at OrthoCarolina Spine Center. He planned to return to the Boston area, where he attended the University of Massachusetts Medical School and did a residency, and join his father’s medical practice. But his wife, whom he met while an undergrad at Colgate University in Hamilton, New York, fell in love with the area and its climate. Their oldest daughter was then 6 months old; she’s now a high school junior.
“Life takes interesting turns,” he says. “You just have to be open to where they take you.” The decision made a big difference in his career, he adds. “I don’t think I could have done what I do here if I were in Boston just because it’s so entrenched and not open to different people coming in.”
Spector says he has no timetable for how long he’ll remain in the dual roles. That decision will be balanced with his professional life, his medical practice and his family, he says.
The full article first appeared in Business NC
Going to See the NC State Wolfpack (Men and Women - Woo Hoo!)? Here Are Some Tips for Your Trip

A Historic Weekend for NC State! Both the Men's and Women's Basketball Teams
are Playing in the Final Four!
RALEIGH -- Fans of North Carolina State are getting ready to switch into high gear. On Friday, play begins for two teams hoping to make it to a National Championship! First up will be the women on Friday at 7pm. The Wolfpack take on Number One seed South Carolina. If they survive that matchup, they will take on the winner of the UConn-Iowa game on Sunday.
For the men, who are experiencing a Cinderella tournament that has many recalling State's historic 1983 championship under the legendary Jim Valvano, the action begins Saturday at 6:09pm when they take on Number One seed Purdue. If the men advance they will play the winner of the Alabama-UConn game on Monday.
If you are planning to attend either, here are some things to look forward to:
The women play in Cleveland at the Rocket Mortgage FieldHouse. There are lots of events happening while you're in town. Check out events like the Four Bounce, Party on the Plaza, a FREE open practice by all four teams, and a Super Saturday concert. All you need to know about the events is here.
The men will be in Phoenix at the State Farm Arena and the city is rolling out the welcome mat. Events include the March Madness Music Festival with the Jonas Brothers, The Final Four Fan Fest, and loads of dining deals across the city. All you need to know about the events is here.
Everyone at the NCMS is wishing both teams the best as they represent North Carolina this weekend!
Duke Awarded Up to $33 Million to Develop OA Therapies that Rebuild Bone and Joints
Along with Boston Children’s Hospital and UCLA Health, the federally funded project aims to alleviate the heavy cost burden of osteoarthritis
(DukeHealth) -- Duke Health is part of a multi-institution research team receiving funding from the federal Advanced Research Projects Agency for Health (ARPA-H) to develop an osteoarthritis treatment that regenerates joints.
The research project, which includes teams from Boston Children’s Hospital and the David Geffen School of Medicine at UCLA, was awarded a contract of up to $33 million, funded in two phases over five years. The project director is Benjamin Alman, M.D., chair of the Department of Orthopaedic Surgery at Duke University School of Medicine.
“We need a new approach to treat osteoarthritis, which is a leading cause of disability and represents a $128 billion cost burden on the U.S. health care system,” Alman said. “Regenerating cartilage and bone would be an effective therapy, and we have the technology, resources, and expertise in hand to make this a reality.”
The research team will base its proposed new therapy on recent evidence that joint tissues can heal. They will build on previous findings from project members, including the identification of small molecules and proteins that improve the cartilage regeneration process; the development of methods to deliver agents and target them to relevant joint tissues; the restoration of joint and bone tissue to a more normal “younger” state in animal studies; and an understanding of the genes and pathways needed to generate articular cartilage.
“We will achieve our goal of delivering a regenerative treatment for osteoarthritis by capitalizing on the expertise of our multi-site team, which includes biologists with extensive experience in bone and cartilage regeneration, as well as chemists and bioengineers with expertise in cutting-edge technologies to deliver therapeutic agents to the right place at the right time,” said Thomas Kremen, M.D., orthopaedic surgeon at UCLA Health and lead investigator for the planned clinical trial.
The researchers propose three therapies. The first would be an injection targeted into the joint to release regenerative factors in the bone supporting injured cartilage. The second would be an injection into the joint to regenerate cartilage tissue. A third therapy would be a systemic version of the injectable that could home in on diseased cartilage tissues in patients who have osteoarthritis in multiple joints.
By applying these therapies to specific cell populations over the appropriate time frame, the researchers hope to rebuild and rejuvenate a fully functional joint.
“Our team represents a collective and relentless effort to deliver a solution to those that suffer from joint pain,” said April Craft, Ph.D., assistant professor of orthopedic surgery at Boston Children's Hospital and Harvard Medical School and site director of the research project. “Our goal is to restore function to damaged joints by reactivating our own cells in a way that promotes healthy tissue regeneration.”
The researchers will collaborate across a centrally coordinated process to share findings quickly and capitalize on the diverse expertise within the team. Work will include developing pre-clinical large animal studies, planning for clinical trials with a diverse population of participants, and drafting an effective commercialization and technology transfer plan.
“A unique aspect of the work is considering the diversity of patients who would benefit from the treatment from the start of the project,” Alman said. “Osteoarthritis does not affect all populations equally, and the project will include an arm to identify populations that would benefit the most and to ensure that the proposed therapies are readily available to those patients.”
Funding is through ARPA-H's Novel Innovations for Tissue Regeneration in Osteoarthritis (NITRO) program. Its stated goal is to develop new ways to promote joint repair, including injectables that regenerate bones and cartilage, and replacement joints built from human cells.
ARPA-H is a federal agency established to advance high-potential, high-impact biomedical and health research that cannot be readily accomplished through traditional research or commercial activity.
With Cancer Diagnosis, Catherine, Princess of Wales, Shines Brighter Light on Rise in Disease Among Young People

Over the past 30 years, early-onset cancer rose 79 percent, one global study found
(Rachel Uda) -- When Catherine, Princess of Wales, revealed that she was diagnosed with cancer, it stunned the world.
She’s active, she apparently maintains a diet rich in antioxidants and raw fruits and veggies, and she’s only 42. But sadly, the princess is part of an alarming global trend. Studies show that more and more young people seem to be developing cancer. We’re taking a closer look at the latest research on young-onset cancer.
Studies show cancer is striking more young adults
A 2023 study found that over the past three decades, cases of early-onset cancer — defined as those appearing in people under age 50 — shot up a striking 79 percent, while death among younger cancer patients rose 28 percent.
The paper, published in BMJ Oncology, analyzed data from 204 countries and found that breast cancer accounted for the largest number of these, while windpipe and prostate cancers rose the fastest among younger patients over the 30-year period.
Another study focusing on U.S. patients found a modest bump in under-50 cases, but a substantial increase in people diagnosed between the ages of 30 and 39. Cancers among this group, from 2010 to 2019, rose about 19 percent. In line with the global analysis, breast cancer was found to be the most common among younger patients, while the fastest-growing cancers were gastrointestinal.
What’s causing the rise in cancer rates in young adults?
Researchers don’t know exactly. Experts have long pointed to alcohol, tobacco use, and poor sleep as factors. The rise in obesity and environmental factors like pollutants and toxic chemicals we may encounter in our water and food could play a role too.
Some of it simply has to do with the fact that more people are getting screened and diagnosed earlier, says Katherine Crew, M.D., an oncologist and associate professor of medicine and epidemiology at Columbia University Medical Center.
“We’re offering more patients genetic testing, and when they test positive, are screening those people at a younger age. Women with BRCA-1 or BRCA-2 mutations might start breast MRI screening in their mid-20s or patients with Lynch syndrome might start colonoscopies earlier too,” Dr. Crew tells us. “I think that’s part of what’s driving this.”
Another area of focus has been the gut microbiome, the trillions of bacteria, viruses, and fungi living in your intestinal tract. The composition of this universe of microorganisms can be easily thrown out of whack by antibiotics or diets heavy in processed foods, which has been linked to inflammation and certain cancers.
The chances that there’s a “smoking gun,” or one factor that’s behind this disturbing trend is unlikely, says Peter Liang, M.D., a gastroenterologist and assistant professor at NYU.
“It’s much more likely that it’s a combination of different factors that play a role,” Dr. Liang tells us.
That’s why researchers like him, who are trying to get to the bottom of the rise in early-onset cases, are looking at an impressive array of possible culprits. Surveys from Dr. Liang’s study, called the Colorectal Cancer in Adults at Young Onset (CRAYON), ask participants questions like what kinds of jobs they had as teenagers to determine if they could have been exposed to any toxins, if they were breastfed, and even if they were born by C-section. (One recent study found that women born by cesarean were more likely to develop CRC before 50.)
“We have to do more right now and we need answers to be able to figure out how to protect future generations,” he says.
2024 Dirty Dozen List of Fruits and Vegetables, Clean 15 Released

Report: Strawberries still have the most pesticides of any American produce
(Business Insider - Lauren Edmonds) -- Strawberries continue to reign supreme on the Environmental Working Group's annual "Dirty Dozen" list, which ranks fruits and vegetables by pesticide contamination.
The "Dirty Dozen" list is part of EWG's 2024 Shopper's Guide to Pesticides in Produce published on Wednesday. The report analyzed data collected from tests conducted by the USDA and FDA on 47,510 samples from 46 fruits and vegetables.
Both agencies take precautions to clean the produce before testing, with the USDA peeling or scrubbing produce before washing and the FDA only removing the dirt. Still, the report found that the analyzed produce contained 254 traces of pesticides.
The National Institute of Environmental Health Sciences reports that more than 800 pesticides are registered in the United States, "some of which are used in large quantities and may pose risks for a variety of health problems."
Here are the fruits and vegetables ranked on this year's "Dirty Dozen."
The report also listed Clean 15. The items with the lowest amounts of pesticide residues, according to the EWG analysis of USDA data. Here is that list:
- Avacados
- Sweet corn
- Pineapple
- Onions
- Papaya
- Sweet peas (frozen)
- Asparagus
- Honeydew Melon
- Kiwi
- Cabbage
- Watermelon
- Mushrooms
- Mangoes
- Sweet Potatoes
- Carrots
The full report is available by clicking here.
Register Now for 'Global Impact: Climate Change and Our Health'

Global Impact: Climate Change and Our Health, April 11
Thursday, April 11, 2024, 3:45pm EST
VIRTUAL
From poor air quality and flooding to extreme heat and years-long droughts, devastating weather events take a physical, emotional,
and financial toll on populations across the globe and here in the U.S. especially in marginalized communities. Are increased extreme weather events leading to a rise in health issues? Should those issues be looked at holistically or separately?
Join POLITICO on Thursday, April 11 for a conversation examining links between catastrophic weather events and medical challenges, and how industry and government can better collaborate to tackle disparities at the intersection of climate change and health care.
REGISTER HERE
Match Day Madness! NCMS Celebrates Milestone for All Physicians!

NCMS Match Day Social in Chapel Hill is Roaring Success!
NCMS celebrated Match Day with members, physicians, PAs, students, residents, friends, and supporters. It is a great example of the importance of being together! The North Carolina Medical Society provides the space and community to come together, across all specialties, to enhance the profession of medicine as colleagues and medical professionals.
You can be part of the fun and fellowship with your friends and peers. Make new friends and learn more about how NCMS can help you as you continue your career in medicine.
Our next regional meeting is heading to the beach! Look for more information about the event in Wilmington on April 10.