🎉We're Celebrating New Members!🎉

Join us in welcoming these new members to the North Carolina Medical Society!
- Quentin E. Adams, MD
- Jacob C. Andrews, DO
- Jeffrey R. Ashton, MD
- Philip M. Barber, MD
- Darren A. Bates, PA-C
- Lisa Biswas, MD
- Carley D. Bloomfield, DO
- Brenn A. Bolding, PA-C
- Lindsey K. Cole, PA-C
- Marcus DiLallo, MD
- Joseph R. Dowd, III, DO
- Robert T. Duprey, MD
- Macie Edwards
- Erik A. Eklund, MD
- Caleb T. Epps, MD
- Sanaya Gandhi, PA-C
- Amol Garg
- Brooke Ann Gloria, MD
- David R. Guillen, MD
- Ashok K. Gupta, MD
- Kirsti L. Harris, PA-C
- Maria C. Hatara, MD
- Aubrey A. Hess, MD
- Jaclyn N. Hess, MD
- Olivia B. Hughes, MD
- Ivette E. Hurtado, PA-C
- Rayan N. Kaakati, MD
- Michael P. Kehoe, PA-C
- Farid M. Khan, MD
- Morgan E. Killian, MD
- Crysta I. Kyrazis, MD
- Frank A. Lacy, MD
- Andrew S. Laird, PA-C
- Shahmeer D. Lateef, MD
- Gabrielle G. Leonard, MD
- Johnathan S. Lowe, DO
- Abigail Maiorana-Boutilier, MD
- Dylan P. Matthews, MD
- Lauren E. Maxwell, PA-C
- Kaitlyn E. McDonough, PA-C
- Grant W. McKenzie, MD
- Ryan P. McLynn, MD
- Katherine Myers Dharmasri, MD
- Sarah B. Odom, PA-C
- Jason T. Owens, PA-C
- Nisarg A. Parikh, MD
- Evan C. Pohl, MD
- Yuri A. Pompeu, MD
- Danielle V. Price, DO
- Venkateswaran Ramakrishnan, MD
- Alexander B. Reddy, MD
- Jared J. Rejeski, MD
- Victor C. Showalter, MD
- Stephen B. Smith, MD
- Krista M. Stocke, PA-C
- Parker P. Suit, DO
- Rohit Sukumar, MD
- Carles R. Surles, Jr., MD, MPH
- Ekin Uzunoglu, MD
- Yun Wang, MD
- Morgan E. W. Warren, MD
- David G. Weatherford, MD
- David E. Weil, PA-C
- Matthew M. Yeager, MD
- James A. Yoder, MD
- Alexandra E. Zeitany, MD
We are thrilled to have you!
Not a member but would like to be? Joining is simple. Visit our membership center here.
The Fight Against Alzheimer’s Just Got Stronger: Moore Regional Hospital Introduces PET Amyvid Brain Scans
FirstHealth Moore Regional Hospital is proud to announce the availability of PET Amyvid brain scans, a cutting-edge diagnostic tool designed to detect beta-amyloid plaques, a hallmark of Alzheimer’s disease.
This advanced imaging technology offers new hope for earlier and more accurate diagnosis, empowering patients and their families to make informed decisions about care and treatment.
“The diagnosis of Alzheimer’s dementia requires a combination of history, exams, labs and imaging,” said Joshua Cho, M.D., interventional radiologist and nuclear medicine specialist with Pinehurst Radiology Associates. “While traditional imaging tools like MRI and CT focus primarily on anatomical markers, the PET Amyvid brain scan detects amyloid plaques, a biomarker strongly associated with Alzheimer’s. This capability sets it apart and gives us deeper insights into the disease.”
The PET Amyvid scan utilizes florbetapir, a synthetic compound that crosses the blood-brain barrier and binds to amyloid plaques.
“Florbetapir contains a radioactive isotope, F-18, which creates a signal detected by the PET scanner,” explained Dr. Cho. “This allows us to visualize the presence of plaques, although it doesn’t measure their quantity. It’s a significant step in understanding what’s happening in the brain.”
By identifying beta-amyloid plaques, the scan adds specificity to the diagnosis of Alzheimer’s disease and can help clinicians make earlier and more informed decisions about treatment. “This technology has the potential to improve outcomes,” said Dr. Cho. “If we can confirm the presence of amyloid plaques, we can start treatments earlier, which may help slow the progression of the disease.”
Moore Regional is one of only five hospitals in the state to offer PET Amyvid brain scans.
“The introduction of this advanced technology at Moore Regional Hospital underscores FirstHealth’s commitment to providing leading-edge diagnostics and care for patients,” said Kerri Fogle, MBA, MHA, CNMT, assistant director of nuclear medicine and PET imaging at FirstHealth Moore Regional Hospital.
Patients experiencing persistent or progressive unexplained mild cognitive impairment should consult with their primary care provider or neurologist to determine if this scan is appropriate. A referral from a neurologist is required. [source]
Disaster Energy Assistance Available to 25 Counties Impacted by Hurricane Helene

The North Carolina Department of Health and Human Services’ Low Income Household Energy Assistance Program (LIHEAP) began accepting applications from the general public for the Low Income Energy Assistance Program (LIEAP) on January 2, 2025. For the 25 counties that were heavily impacted by Hurricane Helene, additional Disaster Energy Assistance funding has been appropriated by the NC General Assembly to assist households with heating costs and repairs during the colder winter months.
Beginning January 15, 2025, applications for these additional Disaster Energy Assistance funds will be accepted for eligible households residing in one of the 25 identified disaster counties during and after Hurricane Helene. These counties are Alexander, Alleghany, Ashe, Avery, Buncombe, Burke, Caldwell, Catawba, Clay, Cleveland, Gaston, Haywood, Henderson, Jackson, Lincoln, Macon, Madison, McDowell, Mitchell, Polk, Rutherford, Transylvania, Watauga, Wilkes and Yancey counties.
Households can apply for both LIEAP and the Disaster Energy Assistance funding. Households with heating services or systems that require repairs, are currently inoperable, have been disconnected or are at risk of having their services disconnected can also apply for the Disaster Energy Assistance funds.
Eligible households will receive assistance based on household circumstances and need.
“Our friends and family in western North Carolina will feel the impacts from Hurricane Helene for years to come,” said Carla West, Division Director of Human Services for Child Support, Economic Services, Aging, and Operations. “We are only midway through winter, and these funds are critical to keep residents safe and warm as they continue to recover and rebuild.”
Disaster Energy Assistance is a temporary emergency program that helps eligible households and families afford energy heating services after a natural disaster or an emergency. The program provides assistance for eligible low-income households to provide, restore or continue heating sources. Disaster Energy Assistance is available until funds are exhausted.
Individuals in one of the identified 25 disaster declared counties can apply in-person or via telephone with their local county department of social services.
To be eligible for Disaster Energy Assistance, a household must have at least one U.S. citizen or eligible non-citizen and:
- Have income equal to or less than 60% of the state median income
- Have resided in one of the identified 25 disaster declared counties listed above during Hurricane Helene and are currently residing in one of those 25 counties
- Have been impacted and suffered a loss because of Hurricane Helene
Disaster Energy Assistance was created after NCDHHS was appropriated $9 million in state funds from the NC General Assembly to help assist these disaster areas with heating related costs and repairs as a result of Hurricane Helene.
ADDITONAL LINKS OF INTEREST
Register Now for Friday's North Carolina Infection Control Live Webinar
SPICE North Carolina Infection Control Course: Outpatient Healthcare Setting
January 24, 2025
8:40 AM - 3:45 PM
This approved infection control curriculum developed by SPICE prepares designated healthcare providers to ensure and systematically assess that their facility has the appropriate infection prevention policies and procedures in place to allow healthcare personnel to provide safe patient care consistent with the NC communicable disease rule .0206.
Objectives
- Discuss North Carolina state laws governing infection prevention in healthcare facilities.
- Describe control measures for Human Immunodeficiency Virus (HIV), Hepatitis B and Hepatitis C (10 A NCAC 41A .0202, .0203, and .0214.
- Review the importance of communicable disease reporting.
- Describe NC medical waste rules.
- Discuss bloodborne pathogen risks and other measures used for control of bloodborne pathogens.
- Review the Exposure Control Plan requirements.
- Discuss OSHA’s definition of regulated medical waste.
- Discuss best practices for safe injections and the consequences of unsafe injection practices.
- Discuss the One and Only Campaign to eliminate unsafe medical injections.
- Describe the best practices, principles and hand hygiene in asepsis.
- Explain the role of the environment in disease transmission.
- Discuss principals of disinfection and sterilization for medical devices used in outpatient facilities.
For more information and to register, click here.
Community Health Worker Supervisor Training Q&A
Community Health Worker Supervisor Training Q&A
January 28, 2025
11:30 a.m. - 12:30 p.m.
Curious about how to empower your role as a CHW Supervisor? Join this live Q&A session to explore what CHW Supervisor Training offers! The CHW supervisor training is provided by CHASM in partnership with SRAHEC and supported by the North Carolina Community Health Worker Association (NCCHWA). Training aligns with the competencies required for NCCHWA's Advanced Certification levels addressing factors across the Socioecological Model.
Download the brochure here.
Questions about this program?
Contact Justin Schwartz, MBA, BS, NREMT, CHW, Administrator, Continuing Professional Development / [email protected] / (910) 678-7286
NCMS Recognizes NCMS Disaster Relief Fund Contributors

A heartfelt THANK YOU to these individuals and organizations for their contribution to the NCMS Disaster Relief Fund. Your generous donation is far more than just a financial contribution; it’s a lifeline for the many affected by Hurricane Helene, and vital in providing support to healthcare professionals and communities impacted by this disaster.
We invite you to spread the word about the NCMS Disaster Relief Fund and stay engaged with us as we work together to help restore our Western North Carolina neighbors.
We are grateful to have you in our community!
- Davis Moore Healthcare Practice Group
- Donald Irwin
- Patricia H. Petrozza, MD
- Cary C. Ward, MD
- Janice M. Westphal, MD
- American Medical Association Foundation
- Ana Ayala
- Katherine Beavers
- Sandeepkumar J. Gupta, MD
- Portia Marsh
- Physicians East, PA
- Bangladesh Medical Association of North Carolina
- Rebecca S. Carlin, MD
- Carolina Complete Health Inc.
- Anonymous
- James M. Provenzale, MD
- Moulton Family Fund
- Puraven Beauty and Wellness
- UBS Financial Services, Inc.
- Donald P. Wilcox
- American Medical Association Foundation
- Atlantic Internal Medicine
- Amar M. Amaresh, MD
- Edwin C. Bartlett, Sr., MD
- Deanna M. Boyette, MD
- Edwin K. Burkett, MD
- Cobb County (GA) Medical Society
- John A. Fagg, MD
- Barbara Hodde
- Martha G. Peck, MD
- Gary Price, MD
- Eugene E. Wright, Jr., MD
- Kathy F. Wright
- Curi
- Anonymous
- Christopher T. Grubb, MD
- Lyndon K. Jordan, III, MD, FACR
- Katie Lowry, MD, MPH
- Laura J. Luckadoo, MD
- Robeson Pediatrics
- Kirby Sheridan
- Catherine L. Sotir, MD
- Vinod C. Vallabh, MD
- Ian D. Archibald, MD
- Preecha Bhotiwihok, MD, MPH
- John W. Black, MD
- Anonymous
- Gay M. Bowman
- Georgi N. Brockway, MD
- Michael T. Brohawn
- Anonymous
- Carolina Complete Health Network
- Sharon M. Foster, MD, FAAP
- Donna C. Graves, MD
- M. Mark Hester, MD
- Suneya G. Hogarty, DO
- Marius J. Ilario, MD
- Linda W. Lawrence, MD
- Douglas S. McFarlane, MD
- Mark B. Moeller, MD
- Anonymous
- Raleigh Orthopaedic Clinic, PA
- Timothy J. Reeder, MD, MPH, FACEP
- Alan J. Rosenbaum, MD
- Anonymous
- Marshall Z. Schwartz, MD
- Douglas D. Sheets, MD, FACOG
- W. Alan Skipper, CAE
- Jennifer K. Stoddard, MD
- STUSQU, PLLC
- Lisa W. H. Thompson, MD
- Cheryl L. Walker-McGill, MD, MBA
- Craig E. Webb, MHS, PA-C
- Johnathan D. Williams, MD
- Anonymous
- Idil Aktan, MD
- R. D. Almkuist, II, MD
- American Board of Pediatrics Inc
- Caroline D. Ames, MD, FACS
- James H. Antoszyk, MD
- Joy Avery
- Timothy M. Beittel, MD
- Anonymous
- Anonymous
- Cedar Mount Behavioral Health, PA
- Center For Pain Management, PLLC
- Melissa M. Coale, MD
- Anonymous
- Kim D. Dansie, MD
- Jackie M. Davis-Jones
- Jessica F. Doerrler, PA
- Patricia Duncan
- Peter A. Eweje, MD
- Mark W. Featherston, MD
- Anonymous
- Joanne M. Fruth, MD
- Lisa M. Gangarosa, MD
- Highland Medical Associates
- Anonymous
- Joseph P. Hunstad, MD, FACS
- Kitsie Jones
- Christopher P. Jordan, MD
- Kerry Kendall
- Eugenie M. Komives, MD, FAAFP
- Ted R. Kunstling, MD, FCCP
- Andrew S. Lamb, MD
- Keith LaScalea, MD
- Anonymous
- Elizabeth G. Livingston, MD
- Anonymous
- Laura L. Martinez, MD
- Darlyne Menscer, MD
- Ashley Newton
- J. Thomas Newton, MD
- Carolyn O'Conor, MD
- Michael K. Patrick, MD
- Patricia Petrick, MD
- Emily Rayes-Prince, MD
- Anonymous
- Corianne D. Rogers, MD
- Nimesh B. Shah, MD
- Kristen M. Shipherd
- Maria J. Small, MD
- Anonymous
- Michol Stanzione, DO
- Steele Creek Dermatology
- Al Steren, MD and Diane Snyder Steren, MD
- Martha Strange, MD
- Thomas M. Swantkowski, MD, AGAF, FACG
- Marian L. Swinker, MD, MPH
- Christopher L. Tebbit, MD
- Monecia Thomas, PhD
- Dimitri G. Trembath, MD
- Michael J. Utecht, MD, FACEP
- Lynnea Villanova, MD
- Bonnie E. Wagner, PA-C
- Rebecca Y. Weinshilboum, DO
- Carl J. Westcott, MD
- Thomas R. White, MD
- Anonymous
- Women's HealthCare Consultant PC
- Nagarjuna Yerra, MD
- Michael Bartiss, MD / Family Eye Care of the Carolinas
- David Boone, MD
- Carolina Complete Health
- Karl Chiang, MD
- John Chretien, MD
- Anonymous
- Kelly Fedoriw, MD
- Carolyn Ferree, MD
- Alison Gardner, MD
- John Goldfield, MHS, PA-C
- Akilah Grimes, MD
- Sandra Jackson / Eastern Pediatrics
- Matthew Katz, MS / MCK Health Strategies
- Melissa Kenny
- Donna McGee, MD
- Larry Napolitano, Jr., MD
- Michael P. Reddy-Miller, MD
- Anonymous
- Andrew Pasternak, MD
- Antonio Ramirez, MD
- Beth Remhof
- Jennifer Root, MD
- Richard Savage, MD
- Anonymous
- Soma Sengupta, MD
- Nimesh Shah / Noble Hospitality Investment
- Amanda Trimpey, MD, MPH, FACOEM
- Yunxiang Zhu, MD
*Please note: List reflects donations received through Monday, January13, 2025.
Application Period Open for NCDHHS’ HBCU/MSI and Change Champion Internship Programs – Summer 2025 Cohort

The application period is now open for the 2025 NCDHHS’ Historically Black College/University and Minority Serving Institutions (HBCUs/MSIs) internship program's Summer Cohort. The application period closes on Thursday, February 20. The HBCUs/MSIs Internship program, in coordination with the Division of Public Health, is a component of the department’s workforce development initiative that encourages college students to seek careers in public health and human services in government agencies.
The program is recruiting students from HBCUs and MSIs in North Carolina to allow more equitable opportunities for internship access within NCDHHS, which supports building a strong and inclusive workforce, one of NCDHHS' strategic priorities. The program allows interns to learn more about what public health professionals, public administrators, social workers, and policymakers do at NCDHHS. In-person, hybrid and remote positions with experiential and project-based options are available.
Multiple internships are available for the HBCUs/MSIs Internship program. Sophomores, juniors, seniors, graduate and professional students and/or public health and human services majors are encouraged to apply. Undergraduate interns will be paid $20 per hour, and graduate or professional students will be paid $25 per hour.
The positions have broad requirements, such as the ability to engage and interact with internal and external partners; compile, assimilate and organize printed and electronic information; knowledge of data collection, organization to create reports, charts and other materials; the ability to present ideas clearly and effectively in written and verbal formats, as well as other requirements. Interns will work 40 hours per week, Monday through Friday between 8 a.m. to 5 p.m. Remote and hybrid options are available.
To apply for the HBCU/MSI Internship program, complete the Summer 2025 - Internship Interest Form. You must also email the NC State Government Application to [email protected] by February 20.
If you have questions about the NCDHHS HBCUs/MSIs Internship program, contact HBCUs/MSIs Program Manager Donyea Daniels at 984-303-6834 or Michael Leach, Senior Advisor, at 919-527-7536. You may also email questions/concerns to [email protected].
DEA & HHS Publish Final Rule on Telemedicine Prescribing for OUD

The Drug Enforcement Administration and the US Department of Health and Human Services will be publishing a Final Rule in the Federal Register on January 17, 2025, for prescribing of buprenorphine via telemedicine.
According to the new rule, providers will be permitted to prescribe a six-month initial supply of Schedule III-V medications to treat opioid use disorder via audio-only telemedicine interaction without a prior in-person evaluation. The rule also outlines allowances for follow-up medication prescriptions via telemedicine
The rule will become effective 30 days after publication. Below is a summary, which appears in the rule text.
https://public-inspection.federalregister.gov/2025-01049.pdf
The Drug Enforcement Administration and the Department of Health and Human Services are amending their regulations to expand the circumstances under which practitioners registered by the Drug Enforcement Administration are authorized to prescribe schedule III-V controlled substances approved by the Food and Drug Administration for the treatment of opioid use disorder via a telemedicine encounter, including an audio-only telemedicine encounter. Under these new regulations, after a practitioner reviews the patient’s prescription drug monitoring program data for the state in which the patient is located during the telemedicine encounter, the practitioner may prescribe an initial six-month supply of such medications (split amongst several prescriptions totaling six calendar months) through audio-only means. Additional prescriptions can be issued under other forms of telemedicine as authorized under the Controlled Substances Act, or after an in-person medical evaluation is conducted. This regulation also requires the pharmacist to verify the identity of the patient prior to filling a prescription. The Ryan Haight Online Pharmacy Consumer Protection Act of 2008 generally This document is scheduled to be published in the Federal Register on 01/17/2025 and available online at https://federalregister.gov/d/2025-01049, and on https://govinfo.gov requires an in-person medical evaluation prior to issuance of a controlled substance prescription. However, this regulation falls under one of the exceptions found within the Ryan Haight Act. Additionally, this regulation does not affect practitioner-patient relationships in cases where an in-person medical evaluation has previously occurred. The purpose of this regulation is to prevent lapses of care by continuing some of the telemedicine flexibilities that currently exist for those patients seeking treatment for opioid use disorder.
US Faces 'Quad-Emic' as Four Viruses Surge Simultaneously

Four viruses are surging across the U.S., prompting health experts to sound alarms about a potential 'quad-emic.'
As cases of influenza, respiratory syncytial virus (RSV), COVID-19, and a surge in norovirus continue to climb, the increase in illnesses is concerning, as these viruses can require hospitalization — or even be fatal — if not prepared for or treated properly. Hospitals are bracing for a strain on resources, with fears growing over the impact of multiple viral outbreaks occurring simultaneously.
There are vaccines for the respiratory viruses COVID-19, influenza, and RSV, but currently no vaccine for norovirus, which is commonly called the stomach flu but is not caused by influenza. Here are ways to keep yourself, your family, and your patients safe.
Children and Family Specialty Plan to Launch in 2025
The first-of-its-kind Children and Families Specialty Plan will go live December 1, 2025. This is a single, statewide NC Medicaid Managed Care plan that will wrap Medicaid-enrolled children, youth and their families in the child welfare system with seamless, integrated and coordinated health care.
NCDHHS and Blue Cross NC’s highest priority is to deliver a plan that meets the needs of the children and families of North Carolina and are committed to building the systems and processes needed to ensure the Plan works for families and the counties that serve them. Since the contract was awarded in August 2024, the two organizations have been working together and carefully planning to ensure the launch of the new plan goes smoothly and is ready to serve beneficiaries on day one.
For more on this new plan, click here.
NCTracks: Use of State License Boards Instead of Transcript to Verify Education and Training

Currently, when completing an Enrollment Application or Re-verification Application, NCTracks requests that some providers have their school send transcripts as proof of the highest level of education entered on the application. Effective November. 8, 2021, state licensing agencies that primary source verify education and training and display the information on their websites will be used as verification of education and training in lieu of a transcript.
See the table here (pdf download) for a list of state license agencies that can be used as verification of education and training. If "YES" is indicated in the PSV Education column, NCTracks will verify education and training using that source instead of sending a transcript request to the provider. If "NO" is indicated in the PSV Education column, transcripts will still be required.
For applications submitted prior to January 8, 2025, providers must still have their school send a transcript if one has been requested.
Join us in Raleigh on March 1 for the NCMS Advocacy Summit! Secure Your Spot Today!
Whether you're a healthcare professional, community leader, or passionate individual, the NCMS Advocacy Summit provides a platform to discuss, learn, and collaborate on shaping the future of healthcare.
We are thrilled to invite you to the NCMS Advocacy Summit, a groundbreaking event dedicated to exploring and advancing crucial topics in healthcare. Join us on Saturday, March 1, 2025, from 9 am to 5 pm at the StateView Hotel, located at 2451 Alumni Drive, Raleigh, NC 27606.
Event Highlights:
- Engaging Sessions: Delve into discussions on Access to Care Solutions, Corporate Practice of Medicine, AI in Healthcare, and much more!
- Diverse Perspectives: Gain insights from esteemed speakers representing various states and local community leaders, providing a comprehensive view of healthcare advocacy.
- Networking Opportunities: Connect with professionals who share your passion for healthcare advocacy. The last session of the day will be a townhall allowing leaders from specialty and county societies to speak.
Registration is Open, but Space is Limited! Don't miss this opportunity to be part of a transformative event. Secure your spot today by registering today!
We look forward to your participation in this impactful event.
Grant Opportunity for State Designated Rural Health Centers

These grant funds, supported through the North Carolina General Assembly, allow ORH to partner with local communities to provide funding to improve their ability to serve underserved populations who would otherwise be unable to access needed primary care services due to geographic, economic, or other barriers. State Designated Rural Health Centers have become an integral part of the health care safety net for North Carolina’s rural and underserved residents.
Requests are contingent upon availability of program funding. ORH anticipates that approximately 15 applicants will receive funding. Successful applicants will be required to attend a grant award workshop.
The applicant organization must first assess if it can meet certain criteria. The purpose of the SDRHC program is to increase access to primary care for rural, uninsured, and underinsured residents.
More information, including how to apply, is available here.
Register Now! Essentials of Pain Management CME Event

On March 1, 2025, NCS-ACOFP and the Pain Societies of the Carolinas will host a one-day CME event in Raleigh, NC at the Campbell University Norman Adrian Wiggins School of Law.
The conference is titled: Essentials of Pain Management. Conference content will meet the NC licensure and DEA MATE Act requirements related to prescribing opioids and related topics. Learn the latest techniques, treatments, and options in acute and chronic pain management. Review the conference agenda here. The following CME credit types will be awarded: up to 8 AOA Category 1-A credits AOA and 8 AMA PRA Category 1 Credits™ .
Register by January 31, 2025, to take advantage of the Early Bird Registration Rates. Here is the link to register. Note: registration is done via the site of the Pain Society of the Carolinas.
Need Additional Information about the Conference?
Visit the NCS-ACOFP website or contact Nancy Guy, Director at [email protected] or by phone at 910-658-6501.
Take Action on Prior Authorization NOW! Sign Our Petition Today!
Sign our petition to tell the North Carolina General Assembly, the time is NOW to pass Prior Authorization Reform.
Why reform Prior Authorization?
We've All Felt It. Every one of us, or someone we love, has had a hard time because of something called "prior authorization" in healthcare. Insurance companies use prior authorization to slow down or even stop people from getting the care they need. This is continuing to mess with people's lives.
Prior Authorization reform will allow for timely decisions to made by the insurance companies, insurance companies must work with the patient's physician before denying coverage, and insurance companies must make prior authorization criteria clear and understandable.
By signing our petition, you are telling the North Carolina General Assembly the time is NOW to pass Prior Authorization Reform.
The Future of Psychedelic Use in Healthcare

Last year was tumultuous for the psychedelic medicine industry. Marked by the FDA’s rejection of Lykos Therapeutics’s MDMA-based depression treatment, experts project 2025 will be much more inconsequential, as companies are set to focus on recalibrating to avoid a similar fate.
Lykos’s MDMA therapy was widely expected to be the first FDA-approved psychedelic medicine. But the FDA rejected the company’s application in August, citing concerns about the data submitted. Lykos later agreed to complete a second Phase 3 clinical trial, though it has not announced when it would be able to resubmit its application for approval.
The agency’s decision showed that the psychedelic medicine industry still has a lot to prove to gain mainstream acceptance. But 2025 is off to a positive start, according to Lynn Marie Morski, president of the Psychedelic Medicine Association, pointing to the American Journal of Psychiatry dedicating its January edition entirely to psychedelic medicine.
“It was great to see such a long-standing organization from the mainstream medical side giving legitimacy to psychedelic medicine in that way,” Morski told Healthcare Brew. “It seems like this year is starting with an acknowledgement by some of the mainstream medical associations that…psychedelic medicine is a legitimate form of therapy.”
One of the main theories behind using psychedelic medicine to treat mental health conditions is that the drugs get to the root cause of conditions like anxiety or depression rather than just treating the symptoms, Morski told Healthcare Brew in May 2024. Providers could refer patients to various types of psychedelic therapy if they don’t respond well to traditional treatments, like SSRIs for depression.
For the full article, click here.
New Scholars Program Supports Local Health Sciences Students
 image credit: Haywood Regional Medical Center
image credit: Haywood Regional Medical Center
Haywood Regional Medical Center (HRMC) and Haywood Community College (HCC) are excited to announce the launch of a new Scholars Program, designed to provide a final dollars scholarship for health sciences students in exchange for a commitment to employment at HRMC upon graduation. The agreement will support students enrolled in the Registered Nurse, Nurse Aide I, Medical Assistant, Phlebotomy, and Paramedic programs at HCC, offering a pathway to stable, fulfilling careers in the healthcare field within Haywood County.
Through this partnership, program participants will receive financial assistance to complete their education, allowing them to stay within the local community to pursue career opportunities that contribute directly to the health and well-being of Haywood County residents.
Continue to full article here.
Reminder: Don't Miss the BCBS Antitrust Settlement Webinar on Thursday, January 16.

Physicians, medical groups, and health care facilities may be eligible to submit a claim as part of the settlement reached with the Blue Cross Blue Shield system.
In 2024, a settlement was reached in a long-running class action lawsuit against Blue Cross Blue Shield (BCBS) brought by physicians, hospitals, large health systems and provider organizations. The lawsuit alleged a range of antitrust violations by BCBS, including price fixing and allocating markets using exclusive service areas. In addition to $2.8 billion in damages, the Settlement Agreement requires BCBS to make hundreds of millions of dollars in investments to improve claims processing, including the processing of BlueCard claims.
Physicians, medical groups and health care facilities may be eligible to submit a claim as part of the settlement reached with the BCBS system if they provided health care services, equipment or supplies to Blue Plan patients between July 24, 2008, and October 4, 2024.
Whatley Kallas, LLP will host a webinar for medical providers on how to submit claims.
Medical Professionals/Groups: Thursday, January 16, from 12-1 Eastern:
https://us02web.zoom.us/j/89755230924?pwd=Yp8kGYzmMhGZT7VETzzxfcqkLVH0nT.1
Meeting ID: 897 5523 0924
Passcode: 023811
The webinars are optional, not mandatory.
Speakers:
Patrick Sheehan, Whatley Kallas (Co-Lead Counsel)
Justin Wind, Brown Greer (the Settlement Notice Administrator)
Ed Gentle and Kip Benson, Gentle Turner & Benson, LLC (the Settlement Administrator)
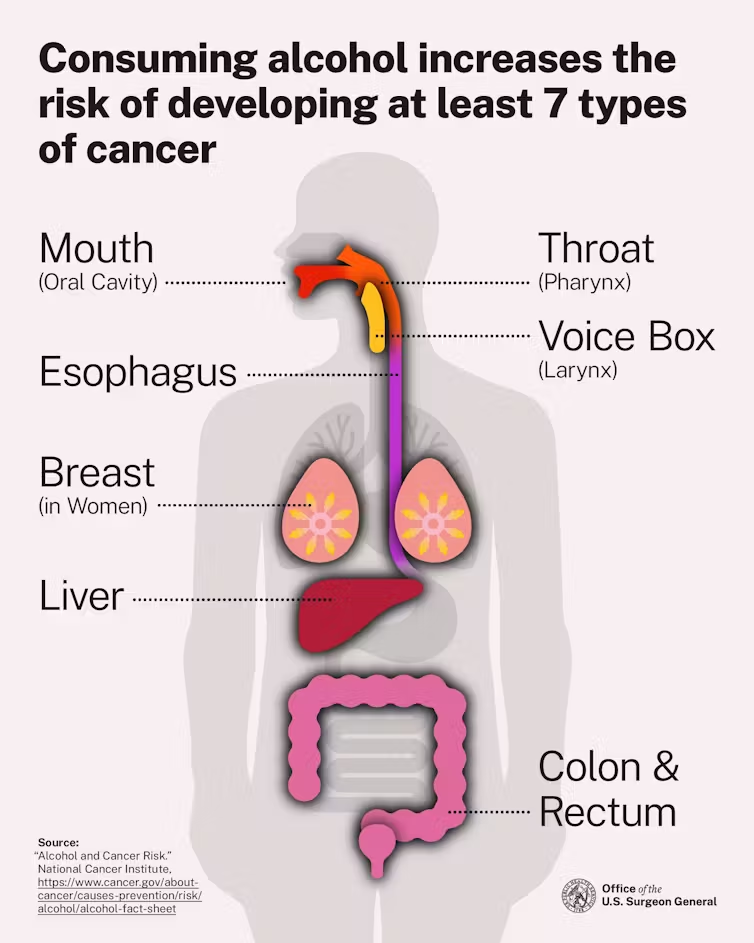
Key Takeaways in the New US Alcohol-Cancer Guidelines

Alcohol is the third-most preventable cause of cancer in the U.S, putting it just behind tobacco and obesity.
U.S. Surgeon General Dr. Vivek Murthy released a new Surgeon General Advisory on January 3, 2025, warning about the link between alcohol and cancer. This report highlighted the evidence and included a call for new cancer warning labels on alcoholic beverages.
The association between alcohol and cancer isn't new news – scientists have been trying to determine the link for decades – yet most people aren't aware of the risks and may only associate drinking with liver disease like cirrhosis. In a 2019 survey from the American Institute for Cancer Research, less than half of Americans identified alcohol as a risk factor for cancer.
As the surgeon general's report highlights, alcohol is associated with approximately 100,000 cancer cases and 20,000 cancer deaths every year, playing a role in breast, liver, colorectal, mouth, throat, esophagus and voice box cancer cases. Alcohol-induced cancer deaths outnumber alcohol-associated traffic crash fatalities every year.
Continue to full article here.
NCMS Past President Dr. Devdutta Sangvai Sworn in as Secretary of the North Carolina Department of Health and Human Services

Dr. Devdutta “Dev” Sangvai was sworn in as the new Secretary for the North Carolina Department of Health and Human Services on Sunday, January 12, 2025. Dr. Sangvai was selected by Governor Josh Stein to lead the department as the state’s 19th Secretary for Health and Human Services. The swearing-in ceremony was held at Dorothea Dix Park where the department is currently headquartered.
“I am honored to lead the Department of Health and Human Services and build on the already strong foundation toward creating a healthier North Carolina for all,” said Secretary Sangvai. “I look forward to working with the incredible team at NCDHHS and Governor Stein to ensure every North Carolinian has access to the right services to support their health, safety and well-being – no matter where they live or how much money they make.”
“Secretary Sangvai is ready for the challenge of improving the health and quality of life for children and families in North Carolina,” said Governor Josh Stein. “I look forward to working with him and the NCDHHS team to make North Carolina safer, healthier, and stronger.”
Secretary Sangvai is a family medicine physician and a professor at Duke University. He is also a member of the North Carolina Medical Board. Prior to his role with NCDHHS, he served as President of Duke Regional Hospital and President of the North Carolina Medical Society. His work has focused improving access, developing the healthcare workforce, and making care more efficient. Dr. Sangvai is the first Indian American cabinet member to serve under a North Carolina governor. See more photos of the swearing in ceremony.
Related Reading
Former NCMS President Dr. Devdutta Sangvai Picked to Lead Health and Human Services
NC Medicaid Direct: New Unit Limitations for Allergy Testing & Allergy Immunotherapy CPT Codes

Effective February 1, 2025, the CPT codes in the table below will have new unit limitations. Clinical coverage policies 1N1 Allergy Testing and 1N2 Allergy Immunotherapy are in the process of being updated to reflect this guidance. A bulletin will be published announcing the final posting of these policies.
Existing coverage will not be revoked; rather, both policies will be updated to reflect current practice standards. Please consult the relevant clinical coverage policy upon its final posting for detailed information regarding this update.
|
CPT Code |
Previous Unit Limitations |
New Unit Limitations |
|---|---|---|
| 1N1 Allergy Testing | ||
| 86003 | 36 units per year | 30 units per 365 calendar days |
| 86005 | n/a | 2 units per day up to 30 allergens per 365 calendar days |
| 95004 | 75 units per year | 80 units per 365 calendar days |
| 95017 | 30 units per date of service | 27 units per date of service |
| 95024 | 20 units per year | 30 units per 365 calendar days |
| 95027 | 20 units per year | 20 units per 365 calendar days |
| 95028 | 20 units per year | 20 units per 365 calendar days |
| 95044 | 36 units per year | 80 units per 365 calendar days |
| 95052 | n/a | 36 units per date of service |
| 95056 | n/a | 1 unit per date of service |
| 95071 | removed due to obsoletion | removed due to obsoletion |
| 1N2 – Allergy Immunotherapy | ||
| 95180 | 12 units per date of service | 6 units per date of service |
| 95145 | 1 unit per date of service | 10 units per date of service |
| 95146 | 1 unit per date of service | 10 units per date of service |
| 95147 | 1 unit per date of service | 10 units per date of service |
| 95148 | 1 unit per date of service | 10 units per date of service |
| 95149 | 1 unit per date of service | 10 units per date of service |
| 95170 | 1 unit per date of service | 10 units per date of service |
The following 10 codes will remain unchanged:
- 1N1 Allergy Testing -95018, 95027, 95028, 95070, 95076, 95079
- 1N2 Allergy Immunotherapy - 95115, 95117, 95144, 95165
This information applies to NC Medicaid Direct.
NC General Assembly Convenes, NCMS Members Sworn In
 North Carolina’s legislature opened its 2025-26 biennial assembly on Wednesday, January 8, 2025.
North Carolina’s legislature opened its 2025-26 biennial assembly on Wednesday, January 8, 2025.
Notable among the members of the General Assembly include three NC Medical Society members.
Rep. Tim Reeder, MD (R – Pitt – incumbent)
Rep. Grant Campbell, MD (R – Cabarrus, Rowan)
Sen. Mark Hollo, PA (R – Caldwell, Catawba)
The new year brings a new Speaker of the House of Representatives, Rep. Destin Hall, who succeeds Rep. Tim Moore who held the gavel from 2015 to 2025. Sen. Phil Berger will again serve as President Pro Tem of the NC Senate.
This year’s political landscape is similar to that of 2023-24 with Republican majorities in both the House and Senate and a Democrat Governor, Josh Stein. A significant difference in the upcoming 2025-26 legislative session, however, is that the Republican’s majority in General Assembly’s will not be veto-proof.
NCMS members’ photos from the January 8th House and Senate swearing-in sessions:

Both chambers will return to Raleigh on January 29th to begin this year’s business of the legislature. The 2025 session of the biennium will be the “long session,” with a clean slate of bills to be deliberated. The long session does not have a pre-set adjournment date.
The 2026 assembly will be the “short session,” a relative description since legislative sessions have no limit on duration. The second session of the biennium is typically devoted to budgetary issues and any bills that passed out of one chamber during the first session.
The NC Medical Society looks forward to working with Mr. Hollo, Dr. Campbell and Dr. Reeder and with all elected officials. NCMS physician and PA members’ involvement in the legislative process will be vital to the Society’s ability to achieve its advocacy goals, so please commit now to actively supporting those efforts. You can show your support by . . .
Signing up for the 2025 Advocacy Summit
Thank you for being involved!
NC Medicaid Releases Annual Health Disparities Report
To help identify and address health disparities, the North Carolina Department of Health and Human Services (NCDHHS) Division of Health Benefits (DHB) developed the 2022 NC Medicaid Annual Health Disparities Report, which outlines health disparities across the entire NC Medicaid beneficiary population.
The report looks at 50 quality measures and identifies health disparities across eight demographic stratifications. The results are organized into six domains: beneficiary experience, child and adolescent health, women’s health, mental health, substance use, and health care utilization. The 2022 results reveal that the domain with the largest count of identified disparities was the substance use domain, and the demographic stratifications with the highest count of identified disparities were beneficiaries who identify as having a disability and those with long-term services and support needs.
In addition to identifying health disparities, the 2022 Annual Health Disparities Report highlights programs across NC Medicaid that are working towards eliminating health inequities. This report will serve as a tool, alongside other Department and Division wide efforts, to identify areas of need and track health disparities over time.
If you have any questions about this report and its results, please email [email protected].
TODAY is the Last Day to Register for the NCMS Advanced Healthcare Leadership Program. Don't Miss this Amazing Opportunity!
Don’t Miss the Opportunity to Become a Healthcare Leader!
Register now for the AHL Program before it's too late!
Deadline to apply is Monday, January 13, 2025!
This program provides a unique leadership journey that is tailored to meet the needs of healthcare professionals at various stages in their careers. Ideally, we encourage newer/mid-career leaders and residents to enroll in the NCMS Academy for Advanced Healthcare Leaders (AHL). The program offers a distinctive curriculum that can support the leadership needs of healthcare professionals.
Why should you and your colleagues enroll in the 2025 NCMS Academy?
Research shows that the long-term benefits of leadership development programs are immeasurable.
What are some benefits of applying to an NCMS Academy for Healthcare Leadership program?
- Individual Leadership Project: Apply your newfound knowledge and skills to a real-world project of interest that drives positive change within your organization/community.
- Networking Opportunities: Connect with a community of like-minded healthcare leaders and build valuable relationships.
- Build Psychological Safety: Participate in learning sessions designed to improve self-awareness and engagement with others.
Sounds fantastic! How do I apply for the program?
Interested applicants can apply by visiting the following link: NCMS Academy for Advanced Healthcare Leaders Application
Deadline to apply is Monday, January 13, 2025.
Contact Erica Neal at [email protected] for more information.
NCMS Past President Dr. Arthur Apolinario Named Mentor of the Year
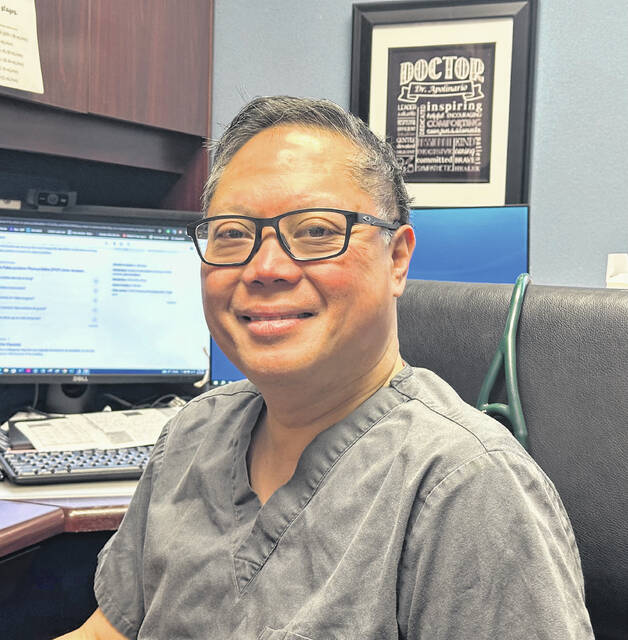 Dr. Arthur Apolinario (image credit: Chuck Thompson | Sampson Independent)
Dr. Arthur Apolinario (image credit: Chuck Thompson | Sampson Independent)
NCMS Past President and Clinton physician Dr. Arthur Apolinario was recently named Mentor of the Year by The Center for Community-Based Primary Care Mentorship Program.
Apolinario, of Clinton Medical Clinic, earned the recognition after taking a medical student under his wing to show him what it was like to be in a small, independent practice, in a more rural setting — something future doctors aren’t taught in a classroom.
“In medical school, they don’t teach you how to run your own practice — which is a business; they don’t teach you how to be a businessman,” Apolinario said during a recent interview. They (medical schools) don’t guide you on how to set up your own practice, so this program was designed to show doctors they can be their own doctor — have their own practice.”
Apolinario said the mentorship program helps medical students better understand life in their profession in many aspects outside of the medical side of the practice. From engaging and understanding the community where they work to budgeting expenses, and employee management, all, he stressed, are often overlooked in medical school, where the focus is purely on medicine, and expecting doctors to go work for a corporate practice when they graduate.
“The program has really helped doctors learn how to be independent,” explained Apolinario. “It teaches them, through mentorship and other resources, how to deal with the legality side, talk with state officials, and manage their finances.”
Army veteran Mark Bushhouse, a former medic with the 10th Special Forces Group, in Colorado, is the mentee that Apolinario has helped under the program. Bushhouse is currently a medical student at Campbell University where he is studying to be a primary care physician.
“Through the community care program — it works in tandem through different medical societies, to connect physicians with medical students, and I put my name in the hat for that, so to speak, and that connected me with Dr. A(polinario).” said Bushhouse. ” Starting out, we did a Zoom meeting, and a couple of email exchanges, and then I had the opportunity where I spent a couple of days shadowing him in Clinton, and got a really great perspective.”
Bushhouse praised Apolinario for his hands-on approach, and the advice that was shared, stating, “He has an incredible longevity in the rural health field, and he has provided a lot of perspective and exposure to different sides of medicine through the community, business, and understanding the independent physician and rural medicine.”
The mentee said Apolinario helped him by showing him that if you find your niche in medicine, and combine that with opening, or joining a practice in the right region best fitted for your life, that is the key to a successful career. Unfortunately, many physicians never set up their own practice, opting out to work for an established practice, that is often own by a huge conglomerate, when in fact, being independent can be more rewarding.
“If you look at the total independent physicians compared to those that are employees — meaning they are not running their own practice, it’s staggering how small the number for independent doctors these days,” added Bushhouse. “It is so important to hang on to those independent practices — and besides, working as an employee for a large company, the patient doesn’t always get to interact with the practicing physician like someone can with a private practice. The connection and trust just isn’t there a lot of the times.”
Apolinario backed up that sentiment stating that physicians are not encouraged to start their own practice right out of med school. “They just don’t encourage that anymore, and it’s important to keep that going and show these young doctors that they can succeed on their own, or in a small group, just as successfully — if not more — than working for some large corporation.
“If you look at the statistics of the state, it’s shocking — about 80 percent of doctors work for other practices. We’re seeing, right here in North Carolina, an alarming number of burnout among physicians that one in 10 have even thought about suicide, if only briefly.
Apolinario’s opinion is that an independent physician seems to be happier than one working for a large company, and taking control of your own business is a big part of that difference.
“That’s the bottom line,” he added. “I’m showing younger doctors that they have a way to control their own career, such as Mark Bushhouse will do one day soon.”
Apolinario, who has been practicing in Clinton for 25 years, has enjoyed his chance to care for patients in a rural county, and get to know his patients on a more personal level.
He said now that he’s been here a quarter of a century he is starting to see the longevity of his work payoff as the babies he delivered are now adults and having children of their own, and the improvements people make in their lives, to want to live longer.
“One of the most rewarding aspects is seeing people make changes in their health,” he said, “Really reaching goals, and enjoying more time with their families. It’s not always something that can be appreciated elsewhere.”
“If anything you can see how much Dr. A really cares about his community, and it shows” Bushhouse concluded. [source]
Study: 13 Genes That Increase Risk of Osteoarthritis

A new study by researchers at the UNC Thurston Arthritis Research Center at the UNC School of Medicine has identified 13 risk genes that can increase chances for developing osteoarthritis, jumpstarting research that could lead to new, targeted treatments.
Osteoarthritis is a painful condition in which cartilage – the protective cushioning between the joints – gradually breaks down. The progressive joint disease, which affects over 32 million people in the United States, can eventually cause bone-on-bone friction, joint stiffness, and pain with every movement.
Multiple factors can influence a person’s risk of developing osteoarthritis, including injury, obesity, aging, and genetics. Recent research has found that nearly half of the risk for osteoarthritis is genetic, which has raised interest in using genetic data to develop a therapy that can stop joint tissue from degrading further.
Read the full article here.
Disaster Energy Assistance Available to 25 Counties Impacted by Hurricane Helene

The North Carolina Department of Health and Human Services’ Low Income Household Energy Assistance Program (LIHEAP) began accepting applications from the general public for the Low Income Energy Assistance Program (LIEAP) on January 2, 2025. For the 25 counties that were heavily impacted by Hurricane Helene, additional Disaster Energy Assistance funding has been appropriated by the NC General Assembly to assist households with heating costs and repairs during the colder winter months.
Beginning January 15, 2025, applications for these additional Disaster Energy Assistance funds will be accepted for eligible households residing in one of the 25 identified disaster counties during and after Hurricane Helene. These counties are Alexander, Alleghany, Ashe, Avery, Buncombe, Burke, Caldwell, Catawba, Clay, Cleveland, Gaston, Haywood, Henderson, Jackson, Lincoln, Macon, Madison, McDowell, Mitchell, Polk, Rutherford, Transylvania, Watauga, Wilkes and Yancey counties.
Households can apply for both LIEAP and the Disaster Energy Assistance funding. Households with heating services or systems that require repairs, are currently inoperable, have been disconnected or are at risk of having their services disconnected can also apply for the Disaster Energy Assistance funds.
Eligible households will receive assistance based on household circumstances and need.
“Our friends and family in western North Carolina will feel the impacts from Hurricane Helene for years to come,” said Carla West, Division Director of Human Services for Child Support, Economic Services, Aging, and Operations. “We are only midway through winter, and these funds are critical to keep residents safe and warm as they continue to recover and rebuild.”
Disaster Energy Assistance is a temporary emergency program that helps eligible households and families afford energy heating services after a natural disaster or an emergency. The program provides assistance for eligible low-income households to provide, restore or continue heating sources. Disaster Energy Assistance is available until funds are exhausted.
Individuals in one of the identified 25 disaster declared counties can apply in-person or via telephone with their local county department of social services.
To be eligible for Disaster Energy Assistance, a household must have at least one U.S. citizen or eligible non-citizen and:
- Have income equal to or less than 60% of the state median income
- Have resided in one of the identified 25 disaster declared counties listed above during Hurricane Helene and are currently residing in one of those 25 counties
- Have been impacted and suffered a loss because of Hurricane Helene
Disaster Energy Assistance was created after NCDHHS was appropriated $9 million in state funds from the NC General Assembly to help assist these disaster areas with heating related costs and repairs as a result of Hurricane Helene.
ADDITONAL LINKS OF INTEREST
Chit Chat and Chocolate Women's Health Event
 Maritza Manrique-Kiniry, MD (image credit: Dosher)
Maritza Manrique-Kiniry, MD (image credit: Dosher)
Dosher Memorial Hospital will host its third annual “Chit Chat and Chocolate” Women’s Health event!
Indian Trail Meeting Hall
113 W. Moore Street
Downtown Southport
Wednesday, January 29
6 to 7 p.m.
Maritza Manrique-Kiniry, MD, a board-certified gynecologist and gynecological surgeon at Dosher Medical-Women’s Health in Southport, will share information on a variety of issues impacting women’s health and will allot time for questions.
Chef Joe Hill from the Dosher Café will serve light refreshments and health friendly chocolate bark to attendees.
This event is free of charge, and all are welcome. RSVP is suggested as space is limited. Visit dosher.org/chitchat or call Dosher Community Relations at (910) 457-3900 to reserve a seat.
Special Webinars Help Physicians Submit BCBS Settlement Claims. The First Happens TODAY at Noon!

In 2024, a settlement was reached in a long-running class action lawsuit against Blue Cross Blue Shield (BCBS) brought by physicians, hospitals, large health systems and provider organizations. The lawsuit alleged a range of antitrust violations by BCBS, including price fixing and allocating markets using exclusive service areas. In addition to $2.8 billion in damages, the Settlement Agreement requires BCBS to make hundreds of millions of dollars in investments to improve claims processing, including the processing of BlueCard claims.
Physicians, medical groups and health care facilities may be eligible to submit a claim as part of the settlement reached with the BCBS system if they provided health care services, equipment or supplies to Blue Plan patients between July 24, 2008, and October 4, 2024.
Whatley Kallas, LLP will host a series of webinars for medical providers on how to submit claims. A session for health care facilities will be held Friday, January 10 at 12:00pm ET, and a session for medical groups and professionals will be held Thursday, January 16 at 12:00pm ET.
Log-in information for both virtual sessions is available here.
The claims period is open and runs until July 29, 2025. Joe Whatley and Edith Kallas were co-lead counsel for providers in the case. Mr. Whatley and Ms. Kallas have a long history of championing physicians’ rights against insurers, having served as lead counsel in the multi-district litigation that established the Physicians Advocacy Institute in a settlement with broad relief for physicians
Medicare Payment Cut Impact Survey Results Are In!

Medicare Payment Cut Impact Survey Results
Over the two-week period of November 14-28, 2024, the North Carolina Medical Society surveyed physicians across North Carolina regarding the 2.8% Medicare physician payment cut scheduled to take effect on January 1, 2025. Just under 500 responses were received. The initial data from the responses, summarized below, accentuates the dire situation that will result from another cut in Medicare physician payment.
The NCMS continues to advocate for a positive adjustment to Medicare payment for 2025 and has joined many state and national partner societies in an appeal to Congress to at least avert the impending cut.
Survey Results
- Are you enrolled as a Medicare provider?
Yes – 92.5%
No – 7.5%
If Medicare payment kept up with inflation, would you become a participating Medicare provider?
Yes – 11%
No - 37%
- How will another Medicare payment cut affect your practice?
| I will reduce the number of appointment slots for existing Medicare patients | 36.0 % |
| I will continue to see existing Medicare patients but not accept new Medicare patient | 23.5 % |
| I will discontinue seeing Medicare patients (unenroll) | 3.5 % |
| No change | 3.5 % |
| Unsure | 1.0 % |
| Other (see below) | 32.5 % |
“Other” / Comments:
“Will make it difficult to hire new staff to meet the increasing demands.”
“There will be longer wait times for patients to be seen.”
“Will do the best i can as a physician.”
“I will retire from practice. This is not sustainable.”
“We turn no one away but still need to keep the doors open. These consistent cuts are not making it easy.”
“Will affect payment for Medicaid”
“We are still evaluating the situation but all of the above are possible”
“Longer waits”
“I will close or leave my rural practice or have to move to a larger corporation that can handle the cuts”
“I may have to stop practicing”
“I will do the best I can, if cost too much will have to cut back on all, already 2-3 week wait”
“I will continue to take care of my Medicare patients at my personal cost”
“I will have to retire. I am just breaking even with Medicare and can no longer afford to stay in business.”
“Medicare cuts will influence private insurance reimbursements and therefore cutting ALL insurances is a risk”
“I may have to close my practice completely”
“Will make it harder to stay in business and seeing all Medicare patients”
“We are urgent care. Have yet to decide”
“It will cost the hospital that supports my practice”
“All of our MD's are taking a pay cut due to declining Medicare reimbursement”
“Affects financials significantly”
“Will greatly decrease number of slots for Medicare new patients”
“Do not have an option but will be very disheartening for future”
- What practice operation factors are impacted by Medicare payment?
| Ability to meet operational expenses (overhead, payroll) | 62.0 % |
| Ability to implement system/tech upgrades | 48.0 % |
| Ability to hire/retain staff | 47.0 % |
| Ability to recruit physicians to join the practice | 44.0 % |
- Medicare payment rates impact other payment rates (Medicaid, State Health Plan, Tricare). Will a cut in Medicare payment result in a reduction in your other patient populations . . .
Medicaid
Yes 76 %
No 24 %
State Health Plan
Yes 67 %
No 33 %
Tricare
Yes 65 %
No 35 %
N.C. Dept. of Insurance Recognized as 2024 Wellbeing First Champion, Supporting Health Worker Well-Being


In September of last year, the NC Department of Insurance revised its Uniform Credentialing Application, verifying their application is free from overly broad and invasive mental health questions. Their efforts were part of the statewide initiative, ALL IN: Caring for NC Caregivers, through the NC Clinician and Physician Retention and Well-being Consortium (NCCPRW) and the Dr. Lorna Breen Heroes’ Foundation (DLBHF).
UPDATED Uniform Credentialing Application
In 2024, HCA Healthcare, Novant Health, Sentara Health, UNC Health, and WakeMed Health & Hospitals joined NCDOI and were recognized as Wellbeing First Champions. To date, Phase 1 of ALL IN: Caring for North Carolina’s Caregivers has positively impacted 45 hospitals and supported over 14,000 credentialed health workers in North Carolina. Find additional details here.
Click here to learn more about ALL IN: Caring for NC Caregiver’s and its 3-phased approach.

Capitol Chronicle: Medicare Physician Providers and Patients Get “Grinched” by Congress - Again

Medicare Physician Providers and Patients
Get “Grinched” by Congress - Again
The waning hours of the 118th Congress offered hope but eventually became a disappointment as a fix for the Medicare physician payment cut was eliminated from the year-end funding package. The legislation enacted was a spending measure – a Continuing Resolution (CR) – to keep the federal government funded to avoid a government shutdown. The bill (H.R. 10545) passed by both chambers and signed into law by the President provides temporary funding through March 14, 2025, when Congress will again have to tackle the budgetary challenge of how it will meet the operational challenges faced by our country which depend on federal appropriations.
Among the priority issues we worked on throughout 2024 and continue to advocate for in the New Year is a fix for Medicare physician payment. The 2.83% cut that went into effect on January 1, 2025, represents the fifth year in a row that physicians have been hit with reduced payment for services, while the cost of maintaining a medical practice continues to rise.
The initial debate on the year-end CR showed promise, with not only an offset of the 2.83% cut included, but also a positive adjustment in acknowledgement of the increasing costs that medical practices are facing. Due to the costs associated with these provisions, and no designated cost offsets, this section of the bill was ultimately eliminated from the final version along with several other provisions that were in the legislation as introduced.
What now?
In our legislative and political advocacy work, there is no “off season,” so we are moving forward with our same message – with a bit more volume since the payment cut has exceeded the pain threshold for many. The 119th Congress has gaveled in, with many new faces, and we are re-engaging our incumbents while connecting with and educating our new congressional delegation members. Medicare payment reform remains a top priority, and we will not relent in our work to achieve an inflationary payment adjustment for physicians, which hospitals and other providers receive.
The first opportunity for action to retract the 2.83% cut will be in March. The House and Senate will again have to take action to avoid a budgetary shutdown of the federal government, and that funding package will be a vehicle for a Medicare payment adjustment. Be on the lookout for more information on the next concerted effort to gain payment relief and on how you can help that effort.
In the meantime, we need you on the team to help our federal advocacy efforts. We need your support . . .
Do you know your state and federal legislators? More importantly, do your legislators know you?
The NCMS can help you connect with policy makers as a constituent and advocate!
Thank you. Your engagement matters.
NCAHEC Offering Support Webinar for Primary Care Physicians

SPECIAL WEBINAR
Collaborative Care Management Capacity Building Fund
Tuesday, January 28 | 12:15-1 p.m.
The NC General Assembly has earmarked $5 million for capacity building for Medicaid-enrolled primary care practices across the state to adopt Collaborative Care Management (CoCM). NCDHHS is contracting with CCNC to manage the program in partnership with NC AHEC’s Practice Support coaching.
CoCM is an evidence-based behavioral health integration model designed to support primary care clinicians in assessing and treating patients with mild to moderate behavioral health conditions. An evidence-based model shown to be more effective than usual care, CoCM improves patient outcomes, increases satisfaction for both patients and providers, and reduces healthcare costs and the stigma related to mental health and substance use disorders.
The capacity building fund has a maximum award of $50,000 per practice. A primary care practice entity applying on behalf of multiple primary care practice sites may receive a maximum of three awards per entity (covering a maximum of 9 sites). Each clinic site may be eligible to receive awards of $50,000 to begin a CoCM model in-house. Additionally, $30,000 is available for practices to expand an existing in-house CoCM model and $20,000 is available to practice sites meeting Phase 1 eligibility, but planning to outsource staffing to a third-party, turn-key company.
Please join for a webinar on January 28 from 12:15-1 p.m. for a review on the new funding and an opportunity to ask questions.
Webinar learning objectives:
- Provide an overview of the Collaborative Care Management Capacity Building Fund award opportunities
- Define eligibility criteria for practice entities/sites
- Describe the application process
For more information about this program, visit CCNC's webpage on CoCM capacity building fund.
Whooping Cough Cases Surging, Highest Levels in a Decade
Whooping cough (pertussis) is a highly contagious respiratory tract infection. In many people, it's marked by a severe hacking cough followed by a high-pitched intake of breath that sounds like "whoop."
Whooping cough spreads easily from person to person through the air. When a person with whooping cough sneezes or coughs, they release small particles with the bacteria in them. Other people can then breathe in the bacteria.

It usually takes 5 to 10 days for symptoms to appear after exposure to the bacteria that cause whooping cough. Sometimes symptoms don't develop for as long as 3 weeks.
Whooping cough appears similar to a common cold early on. Healthcare providers often don't suspect or diagnose it until more severe symptoms appear.
Early symptoms can last for 1 to 2 weeks and usually include:
- Runny or stuffed-up nose
- Low-grade fever (less than 100.4°F)
- Mild, occasional cough
One to 2 weeks after the first symptoms start, people may develop paroxysms, known as coughing fits. These coughing fits usually last 1 to 6 weeks but can last for up to 10 weeks. The cough generally gets worse and becomes more common as the illness continues.
For more on Whooping Cough, click here.
Join us in Raleigh on March 1 for the NCMS Advocacy Summit! Secure Your Spot Today!
Whether you're a healthcare professional, community leader, or passionate individual, the NCMS Advocacy Summit provides a platform to discuss, learn, and collaborate on shaping the future of healthcare.
We are thrilled to invite you to the NCMS Advocacy Summit, a groundbreaking event dedicated to exploring and advancing crucial topics in healthcare. Join us on Saturday, March 1, 2025, from 9 am to 5 pm at the StateView Hotel, located at 2451 Alumni Drive, Raleigh, NC 27606.
Event Highlights:
- Engaging Sessions: Delve into discussions on Access to Care Solutions, Corporate Practice of Medicine, AI in Healthcare, and much more!
- Diverse Perspectives: Gain insights from esteemed speakers representing various states and local community leaders, providing a comprehensive view of healthcare advocacy.
- Networking Opportunities: Connect with professionals who share your passion for healthcare advocacy. The last session of the day will be a townhall allowing leaders from specialty and county societies to speak.
Registration is Open, but Space is Limited! Don't miss this opportunity to be part of a transformative event. Secure your spot today by registering today!
We look forward to your participation in this impactful event.
January is Cervical Cancer Awareness Month! Improve Patient Engagement in Cervical Cancer Prevention.
Join the Health Resources and Services Administration (HRSA), Maternal and Child Health Bureau (MCHB) for “Improving Patient Engagement in Cervical Cancer Prevention.” This webinar is held in observance of Cervical Cancer Awareness Month and will feature speakers from HRSA’s Maternal and Child Health Bureau, Division of Women’s Health.
Improving Patient Engagement in Cervical Cancer Prevention
Thursday, January 16, 2025
2:00 PM ET
Attendees will learn about a new Patient Engagement Toolkit that is publicly available in English and Spanish on the HRSA’s website. The toolkit supports efforts to increase patient and community engagement in cervical cancer prevention, screening, and management. Materials include social media posts, posters, a cervical screening follow-up card, and more. The toolkit was designed to meet the needs of health centers and safety-net settings. It may be useful to other health care organizations that are committed to preventing cervical cancer.
Less Than a Week Remaining! Sharpen Your Leadership Skills This Year!
Don’t Miss the Opportunity to Become a Healthcare Leader!
Register now for the AHL Program before it's too late!
Deadline to apply is Monday, January 13, 2025!
This program provides a unique leadership journey that is tailored to meet the needs of healthcare professionals at various stages in their careers. Ideally, we encourage newer/mid-career leaders and residents to enroll in the NCMS Academy for Advanced Healthcare Leaders (AHL). The program offers a distinctive curriculum that can support the leadership needs of healthcare professionals.
Why should you and your colleagues enroll in the 2025 NCMS Academy?
Research shows that the long-term benefits of leadership development programs are immeasurable.
What are some benefits of applying to an NCMS Academy for Healthcare Leadership program?
- Individual Leadership Project: Apply your newfound knowledge and skills to a real-world project of interest that drives positive change within your organization/community.
- Networking Opportunities: Connect with a community of like-minded healthcare leaders and build valuable relationships.
- Build Psychological Safety: Participate in learning sessions designed to improve self-awareness and engagement with others.
Sounds fantastic! How do I apply for the program?
Interested applicants can apply by visiting the following link: NCMS Academy for Advanced Healthcare Leaders Application
Deadline to apply is Monday, January 13, 2025.
Contact Erica Neal at [email protected] for more information.
NC Medicaid: Delay in Division of Health Service Regulation License Renewal Updates

NC Medicaid requires providers to keep credentials current on their NCTracks provider enrollment record. The expiring credential must be verified as renewed through the licensing entity prior to being updated on the NCTracks record. NC Medicaid is aware and collaborating with the Division of Health Service Regulation (DHSR) regarding the inventory of pending license renewal applications. Any DHSR licensure renewal application that was submitted to DHSR prior to December 31st will remain active with NC Medicaid until DHSR processes all the renewals. Any DHSR Providers due to suspend, due to the expired license, will remain in active status until all renewal applications are completed by DHSR.
In addition, DHSR will send to NC Medicaid a licensure file, each week which is used to update the NCTracks provider enrollment record. As provider licenses are renewed, the information is shared with NC Medicaid and updates are automatically made on the NCTracks record. Providers may also report the license renewal using the NCTracks MCR process upon notification from DHSR that the license is renewed, knowing that NCTracks will verify the status and new expiration date using the file received from DHSR prior to updating the NCTracks enrollment record.
For inquiries related to the status of your license, please contact DHSR.
Low-Income Energy Assistance Program Helps North Carolinians Stay Warm

Older adults and people with disabilities can now apply through county social services departments (DSS) for the state's Low-Income Energy Assistance Program (LIEAP). The federally funded program helps low-income households with a one-time payment directly to their heating vendor to offset the high cost of warming their homes during the cold weather.
Payments will be distributed automatically to heating vendors beginning in December 2024 if a member of the household is 60 or older, is a person with a disability receiving services through NCDHHS' Division of Aging and Adult Services, is currently receiving food and nutrition services, and received a LIEAP payment during the 2023-2024 season.
Beginning on January 2, 2025, all other eligible people who meet the eligibility requirements may begin applying. Applications will be accepted from January 2, 2025 to March 31, 2025, or until funds are exhausted. Households can apply online through the ePASS portal, by phone or by submitting a paper application through mail, fax or dropping it off at their local DSS. Go to the NCDHHS website for more information on the program.
NC Medicaid to Cover FDA-approved Cell and Gene Therapies
Effective January 1, 2025, a new clinical coverage policy (CCP) will provide coverage for U.S. Food & Drug Administration (FDA) approved cell and gene therapies.
Please consult CCP 1S-13 located on the NC Medicaid Program Specific Clinical Coverage webpage for detailed information regarding this new policy.
NC Controlled Substances Reporting System Launches Clinical Alert Program

In December, the NC Controlled Substances Reporting System (NC CSRS) launched clinical alerts, which notify prescribers when a patient has met or exceeded one or more high-risk thresholds.
An alert is triggered when a patient fills controlled substance prescriptions written by 7+ prescribers and filled at 7+ pharmacies within 3 months.
It's important to note that an alert does not indicate illegal or inappropriate behavior. It should be used as a conversation starter to better understand the patient’s specific situation and/or needs.
Learn more about the NC CSRS clinical alert program here.
Norovirus Outbreaks on the Rise Nationwide

According to data from the Centers for Disease Control and Prevention (CDC). Norovirus, a common stomach bug, is surging.
Norovirus is a very contagious virus that causes vomiting and diarrhea. It is sometimes called the "stomach flu" or the "stomach bug." However, norovirus illness is not related to the flu. The flu is caused by the influenza virus. Norovirus causes acute gastroenteritis, an inflammation of the stomach or intestines. Most people with norovirus illness get better within 1 to 3 days.
Anyone can get infected and sick with norovirus. If eaten raw, oysters and other filter-feeding shellfish can contain viruses and bacteria that can cause illness or death. Anyone who consumes raw shellfish is at risk of contracting norovirus. Children younger than 5 years old, older adults, and people with weakened immune systems are more likely to develop severe infections.
Norovirus spreads very easily and quickly in different ways:
- Having direct contact with someone with norovirus, like caring for them, sharing food or eating utensils with them, or eating food handled by them.
- Eating food or drinking liquids that are contaminated with norovirus.
- Touching contaminated objects or surfaces and then putting your unwashed fingers in your mouth.
Take these steps to protect yourself and others from Norovirus:
- Wash your hands well and often.
- Cook shellfish thoroughly and wash fruits and vegetables.
- Clean and disinfect contaminated surfaces.
- Wash laundry in hot water.
- Stay home when sick for 2 days (48 hours) after symptoms stop.
Join Us in Fayetteville for the Next NCMS Regional Meeting!
Feeling More Like a Factory Line Worker Than a Health Care Professional???
Join North Carolina Medical Society members and staff to learn ways NCMS is working to put YOU back in health care decision making!
Luigi's Italian Chophouse and Bar
528 N McPherson Church Road
Fayetteville, NC 28303
Thursday, January 16
6-8pm
Here's what you can expect:
- Complimentary drinks, food and socializing with your colleagues
- An overview on ways NCMS is fighting for physicians and PAs
- Time for You to share solutions, concerns, and ask questions
REGISTER NOW
Physicians, PAs, Residents, and Students
You do not need to be a member to register.
Questions? Contact Toni Hill, [email protected].
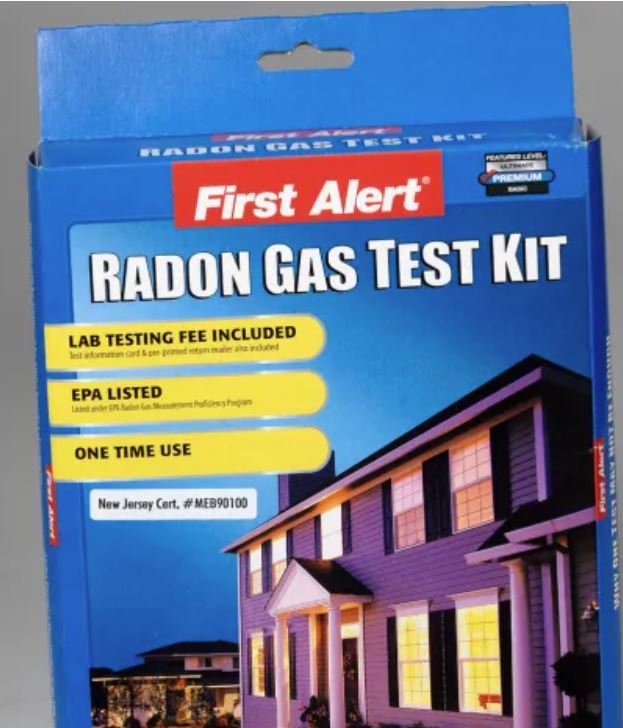
Free Residential Radon Test Kits Now Available! Take Action for Radon Action Month!
In recognition of National Radon Action Month, the North Carolina Department of Health and Human Services is providing 2,000 free radon test kits available beginning January 1, 2025, at radon.ncdhhs.gov. Radon exposure is preventable, and testing is the only way to know if you or your family is at increased risk.
Radon is an odorless, colorless gas released from the ground into outdoor air but can accumulate and reach harmful levels when trapped in homes and other buildings. Radon is responsible for approximately 450 deaths annually in North Carolina, and radon exposure is the number one environmental cause of lung cancer statewide.
"Everyone in North Carolina, from the coast to the mountains, is exposed to some level of radon," said Phillip Gibson, NC Radon Program Coordinator. "The question is not if you are exposed, but whether the level of exposure could be dangerous to your health. Testing for radon is the only way to know."
To support increased radon testing and mitigation, NCDHHS recently published a collection of data to help North Carolinians understand the risk of radon in their communities. Recent data show more than three-quarters of all North Carolina counties have elevated levels of radon present. A level of four picocuries per liter (pCi/L) or higher in your home is considered unsafe. County-level data and recommendations are available on the NCDHHS radon webpage.
Statewide surveys also reveal radon impacts different communities at differing rates. White people are 30% more likely to know about radon than their non-white peers. Efforts are underway to increase equitable awareness through outreach to community organizations and through additional resources available in 16 different languages.
The 2023 North Carolina State Health Improvement Plan and North Carolina Cancer Control Plan includes reducing radon exposure through testing and mitigation as a key strategy to improving life expectancy in North Carolina. In addition to providing free radon test kits and observing Radon Action Month, the department will continue to work to increase education and awareness in communities across the state to ensure people take appropriate action to protect themselves and their families from dangerous levels of radon.
Visit radon.ncdhhs.gov for more information and to order your free test kit while supplies last. Limit one test kit per household. For more information on radon mitigation, visit the NCDHHS radon mitigation webpage.
RELATED READING
What You and Your Patients Should Know About Radon
Grant Opportunity: Telehealth Infrastructure Grant Program

The NC Office of Rural Health has released Wave 2 of the Telehealth Infrastructure Grants funding opportunity!
In Session Law 2023-134, the North Carolina General Assembly (NCGA) appropriated $5,000,000 in SFY 2024 and $15,000,000 in SFY 2025 in receipts (State funds) from the ARPA Temporary Savings Fund to the Office of Rural Health (ORH) in the Department of Health and Human Services to provide competitive grants to rural healthcare providers for Telehealth related items including:
- equipment
- high-speed internet access
- telehealth-related training to staff and patients
- technology equipment to patients
- internet service support for patients to help facilitate telehealth access*
- other infrastructure needed to establish telehealth services
*Eligible rural healthcare patients can benefit from internet service and associated equipment rentals, including modems, routers, and hotspot devices through the Telehealth Infrastructure grant. To receive this support, patients must meet at least one of the eligibility criteria defined below:
- Total household income that is at or below 200% of the federal poverty guidelines or,
- Participation in any ONE of these government benefit programs:
- Lifeline
- Supplemental Nutrition Assistance Program (SNAP)
- Medicaid
- Federal Public Housing Assistance (FPHA) (including Housing Choice Voucher (HCV) Program (Section 8 Vouchers), Project-Based Rental Assistance (PBRA)/202/811, Public Housing, and Affordable Housing Programs for American Indians)
- Veterans Pension and Survivors Benefit
- Supplemental Security Income (SSI)
- Free and Reduced-Price School Lunch or Breakfast Program including through the USDA Community Eligibility Provision
- Federal Pell Grant (current award year)
- Special Supplement Nutrition Program for Women, Infants, and Children (WIC)
Priority will be given to independent primary care practices and independent obstetrics and gynecology (OB-GYN) practices.
For more information, eligibility, and other requirements, click here. Deadline to apply is Friday, January 31, 2025.
Mark Your Calendar! Saving Time: Practice Innovation Boot Camp

This two-day, in-person AMA STEPS Forward® Innovation Academy boot camp is specifically designed for clinical and operational change agents looking to eliminate unnecessary work and free up more time to focus on what matters most–patient care.
Gain proven tools to implement in the following areas:
- Getting rid of stupid stuff
- De-implementation (STOP this and START that)
- Debunking regulatory myths
- EHR inbox optimization
- Team-based care practice fundamentals
- Building bridges between clinicians and administrators
- Reducing barriers to taking PTO
- Making the business case to leadership
Through breakout sessions, interactive activities, thought sharing, tactical strategy breakdowns and how-to examples, this boot camp will equip attendees with the time-saving tools and strategies needed to reform their organizations and enhance professional satisfaction.
Don’t miss this opportunity to gain best practices from top physician experts, network with like-minded peers, engage in cross-sector collaboration, and learn from each other’s successes and mistakes.
Space is limited. Learn more, including how to register, here.
Funding Opportunity: Collaborative Care Management
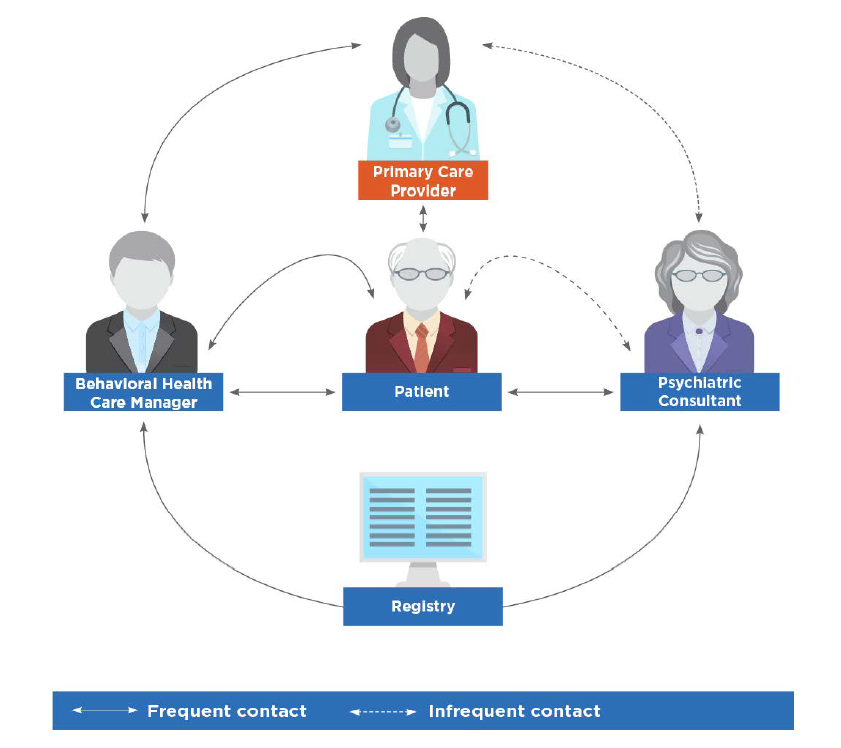 image credit: American Psychiatric Association
image credit: American Psychiatric Association
On behalf of the North Carolina Department of Health and Human Services (NCDHHS), Community Care of North Carolina (CCNC) is accepting applications for the Collaborative Care Management (CoCM) capacity building funding for primary care practice entities.
Collaborative Care Management (CoCM) is an evidence-based behavioral health integration model designed to support primary care clinicians as they assess and treat patients with mild to moderate behavioral health conditions.
CoCM improves patient outcomes, increases satisfaction for both patients and providers, and reduces healthcare costs and stigma related to mental health and substance use disorders. The model complements other integrated models, including the North Carolina Psychiatric Access Line (NC-PAL).
The NC General Assembly has allocated $5 million for capacity building of Medicaid-enrolled primary care practices across the state to adopt CoCM. NCDHHS is contracting with Community Care of North Carolina (CCNC) to manage the CoCM Capacity Building award program in partnership with NC AHEC. The goal is to increase access to evidence-based behavioral healthcare for primary care practices and their patients through the use of the CoCM model.
For more information and how to apply, visit the Community Care of North Carolina Collaborative Care Management Capacity Building Fund Application.
If you are a primary care entity serving Medicaid patients and are interested in learning about CoCM and related capacity building fund opportunities, we invite you to watch the recorded webinar from October 30, 2024 for an overview, here.
Hurricane Helene Note: CCNC is keenly aware that some practices in Western North Carolina are still recovering from the storm and may find it difficult to apply for funds at this time. Efforts will be made to ensure that practices impacted by the hurricane will still have an opportunity to apply for inclusion in the program.
Register Now! Psychiatric Presentations with a Neuroimmune Basis ECHO
Neuroimmune Foundation has partnered with Project ECHO® – an internationally recognized platform with over one million learners in 45+ countries focused on over 1000 medical conditions, to offer weekly didactics and case-based learning to physicians worldwide.