NCMS Regional Event in Charlotte Draws Enthusiastic Crowd
 The North Carolina Medical Society is on the road again!
The North Carolina Medical Society is on the road again!
NCMS members, guests, and friends joined together in Charlotte Wednesday to enjoy some time together and learn more about the Society's mission.
CEO Chip Baggett spoke on how NCMS is advocating on issues important to members like reforming Prior Authorization. He also talked about the NCMS strategic priorities of relieving your administrative burdens, our lobbying work on issues that impact your practice, and the long list of ways NCMS can help you grow professionally. As always, the NCMS is focused on protecting you, the practice of medicine, and your patients.
The medical community is being siloed and fractured at every turn.
This event is a great example of the importance of being together. The North Carolina Medical Society provides the space for the community to come together, across all specialties, to enhance the profession of medicine as colleagues and medical professionals.
If you are already a member, thank you for your continued support. If you are not a member, please consider JOINING NCMS TODAY!
We plan to continue these community conversations all over the state, so please be on the lookout for our next one!
Register Now! NC Allergy, Asthma, and Immunology Society Annual Meeting is May 18-19
| Download the meeting agenda.
Accommodations: Be sure to reserve your room at the Crabtree Valley Marriott before Thursday, April 25 to get our discounted rate of $159. Use this link to book today! Exhibiting Opportunities: Help ensure a successful meeting by sharing the exhibitor prospectus with the product and service representatives who call on your practice. Questions? Contact Megan Eberle at [email protected] or call 919-833-3836. |
Primary Care in Crisis! New Report From The Physicians Foundation
Scorecard Highlights State-Level Primary Care Performance & Lack of Physician Training in Underserved Communities
The second national Primary Care Scorecard released today reveals an intensifying primary care crisis and identifies five reasons why access to affordable, quality primary care services is expected to get worse.
Developed by researchers at the American Academy of Family Physicians’ Robert Graham Center and co-funded by the Milbank Memorial Fund and The Physicians Foundation, The Health of US Primary Care: 2024 Scorecard report and data dashboard examine critical measures of primary care performance nationally and across all states. Key findings include:
1. The primary care workforce is struggling to meet population demands.
- Despite a rapidly aging population with higher levels of chronic disease, the number of primary care physicians (PCPs) per person has decreased.
- The share of all clinicians practicing primary care (including nurse practitioners and physician assistants) stagnated around 28% between 2016 and 2021.
- PCPs declined from 68.4 to 67.2 per 100,000 people between 2012 and 2021.
- There has been a 36% jump in the share of U.S. children without a usual source of care over the last decade and a 21% increase among adults.
- Demand for PCPs will only increase with time. The National Institute of Health estimates that the number of people 50 or older with at least one chronic disease will increase by 99.5%, from 72 million in 2020 to 143 million by 2050.
2. The primary care sector is experiencing a workforce exodus and lacks real-world community training opportunities.
- Primary care residency does not mean primary care practice. In 2021, 37% of all physicians in training specialized in primary care, yet only 15% of all physicians were practicing primary care three to five years after residency. The remainder subspecialized or became hospitalists who do not work in community settings.
- In 2020, only 15% of primary care residents spent a majority of their time training in community settings (outside of hospitals and academic health centers) — signaling that many residents may lack adequate experience practicing in real-world clinical environments.
- In 2020, fewer than 5% of primary care residents spent the majority of their training in Teaching Health Centers or rural training tracks, two programs that historically serve disinvested communities. Research indicates physicians who train in Teaching Health Centers are more likely to practice in underserved communities.
3. The US continues to underinvest in primary care, despite diminishing supply and growing demand.
- The share of total US health care spending devoted to primary care stayed under 6% from 2012 to 2021.
- Since 2019, investment in primary care has steadily declined across all major health care payers; this decline has been most pronounced for Medicare reimbursements for primary care services and providers, which have dropped by 15%.
- The compensation gap between primary care physicians and specialists discourages residents from choosing primary care.
4. Cumbersome electronic health records burden primary care physicians.
- In 2022, more than 40% of family physicians rated the usability of their electronic health record (EHR) systems as unfavorable. Over 25% reported overall dissatisfaction with their current EHR system.
- According to the American Board of Family Medicine, 16% of family physicians reported spending four or more hours per day on EHRs, taking time away from patient care.
5. Inadequate research funding impacts primary care access and quality.
- Since 2017, only 0.3% of federal research funding (administered through the National Institutes of Health, the Centers for Disease Control and Prevention, the Agency for Healthcare Research and Quality, and the U.S. Food and Drug Administration) per year has been invested in primary care research, limiting new information on primary care systems, delivery models, and quality.
- A lack of adequate data on the prevalence of hybrid primary care payment (a combination of fee-for-service and per-person payments) and the training of nurse practitioners and physician assistants), for example, makes it difficult to track progress on the implementation of high-quality primary care.
“As more and more patients struggle to get appointments with primary care practices, policymakers must come together to address the primary care crisis,” said Milbank Memorial Fund President Christopher F. Koller. “By prioritizing investments in primary care and expanding our physician workforce today, we can ensure that everyone in every community has access to high-quality primary care in the future.”
Key State Scorecard Findings:
- Workforce: Alaska ranks second among all states, following Idaho (38.2%), for having 36.2% of its clinician workforce in primary care overall (compared to 28.6% nationally) and first for primary care clinician density in the most disadvantaged areas, with 269 clinicians per 100,000 people (compared to 111.7 clinicians per 100,000 people nationally).
- Training: North Dakota is the highest-ranked state for physician training measures, with a larger share of new doctors entering primary care (36.4%) each year than the national average (21.6%) and a high rate of physicians, physician assistants, and nurse practitioners working in primary care at 26.6%, 44.2%, and 39.4%, respectively.
- Investment: Oregon has the highest overall investment in primary care, with 7.7% of all health care spending going to primary care, compared to the national average (4.7%). The state also has the highest primary care spending for commercial payers (9.1%) and Medicaid (9.2%), compared to the national averages of 5.6% and 4.7% respectively.
The Scorecard was developed in response to a call for an annual tracking tool to inform primary care policy issued by the National Academies of Sciences, Engineering, and Medicine in their 2021 report, Implementing High-Quality Primary Care Rebuilding the Foundation of Health Care. This seminal report provides policy recommendations for federal and state governments, health care organizations, and payers to strengthen primary care.
“Primary care is the cornerstone of our health care system, playing a pivotal role in improving our nation’s health by delivering accessible and timely care to those in need,” said Ripley Hollister, MD, a board member of The Physicians Foundation and a practicing family physician. “The findings and recommendations from the second national Primary Care Scorecard highlight that investment in primary care is vital for the future of health care. The report implores us to embrace and advance solutions that support primary care and allow everyone to live longer, healthier lives.”
READ THE FULL REPORT
READ THE PRESS RELEASE
About The Physicians Foundation
The Physicians Foundation is a nonprofit seeking to advance the work of practicing physicians and help them facilitate the delivery of high-quality health care to patients. As the U.S. health care system continues to evolve, The Physicians Foundation is steadfast in strengthening the physician-patient relationship, supporting medical practices’ sustainability and helping physicians navigate the changing health care system. The Physicians Foundation pursues its mission through research, education and innovative grant making that improves physician wellbeing, strengthens physician leadership, addresses drivers of health and lifts physician perspectives. For more information, visit www.physiciansfoundation.org
About the Milbank Memorial Fund
The Milbank Memorial Fund works to improve population health and health equity by collaborating with leaders and decision makers and connecting them with experience and sound evidence. Founded in 1905, the Milbank Memorial Fund advances its mission by identifying, informing, and inspiring current and future state health policy leaders to enhance their effectiveness; convening and supporting state health policy decision makers to advance strong primary care and sustainable health care costs; publishing high-quality, evidence-based publications and The Milbank Quarterly, a peer-reviewed journal of population health and health policy. For more information, visit www.milbank.org
Looking for Help? Asthma Medication Now Approved to Help Some Food Allergies

Xolair, the brand name for the drug omalizumab, is first medication approved to reduce allergic reactions caused by accidental exposure to food triggers
(The Hill, WGN) -- For decades, asthma patients have used a drug to help them breathe better. Now, the Food and Drug Administration has given the nod to use that drug to reduce serious reactions from food allergies.
Xolair, the brand name for the drug omalizumab, became the first medication approved to reduce allergic reactions caused by accidental exposure to food triggers. Patients as young as age 1 with allergies can take the drug by injection every two to four weeks, depending on their weight and their body’s response to allergens.
Many people with allergies — and their families — live with constant anxiety about exposure to allergens and often avoid dining out and other social situations.
“To have this protection is going to be life-changing,” said Robert Wood, director of the pediatric allergy division at Johns Hopkins Children’s Center.
The FDA decision is based on a study led by Wood and funded by the National Institutes of Health. It showed that Xolair allowed about 68% of participants with peanut allergies to tolerate about 600 milligrams, or about 1/2 teaspoon, of peanut protein, compared with about 6% of those who received dummy injections.
The results were similar for other allergens such as tree nuts, milk, egg and wheat, a study abstract reported. Full results are expected to be presented at a meeting and published in a peer-reviewed journal later this month.
Wood estimated that 25% to 50% of people with food allergies, particularly children and young adults, would elect to use Xolair.
The drug has been used “off-label” to treat food allergies, said Ruchi Gupta, director of the Center for Food Allergy & Asthma Research at Northwestern University. She welcomed full approval of the product.
Xolair is a monoclonal antibody, a type of treatment that works by blocking the body’s natural response to allergens. It was first approved in 2003 and has been used to treat asthma, nasal polyps and chronic hives. It is produced by drugmakers Novartis and Roche and is distributed by a Roche subsidiary, Genentech.
“This really is a difference maker for patients and parents who have severe food allergies,” said Sai Nimmagadda, an allergist at Lurie Children’s in Chicago.
“Every day here at Lurie, you see two or three kids come in with a reaction,” Nimmagadda said.
“Patients on Xolair were able to tolerate higher quantities of food compared to placebo. It will prevent up to 40 percent of patients who have allergic reactions and 30,000 ER visits a year,” Nimmagadda said.
“It’s the first known medication with the indication to prevent food allergies,” Nimmagadda said.
That means relieving the constant fear of accidental, life-threatening allergies.
“What we’re noticing is patients who are on Xolair can tolerate up to two and a half peanuts before they have a reaction, up to three and a half cashews, up to about two teaspoons of milk and maybe up to a quarter teaspoon of egg,” Nimmagadda said. “So, it brings the threshold up a little bit. So, instead of trace amounts causing the allergic reaction, now you can feel safe you can have accidental exposures and not end up in the emergency room.”
“You don’t have the allergic effects when you ingest the food you are allergic to,” Nimmagadda said.
The most common side effects of Xolair are injection site reactions and fever, but the FDA noted that the drug has also been associated with joint pain, rash, parasitic infections, malignancies and abnormal laboratory tests. Xolair comes with a warning saying the treatment itself can cause anaphylaxis and must be started in a health care setting equipped to manage the reaction.
The medication is not approved for emergency treatment of allergic reactions.
The list price for Xolair ranges from about $2,900 a month for children to $5,000 a month for adults, according to Genentech. Most insured patients typically pay less out of pocket, the company said.
The Associated Press contributed to this report.
UNC Scientists Create New Drug Delivery System
Wireless Drug Patch Shows Promise as Chronic Disease Treatment Delivery System
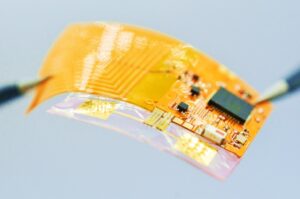
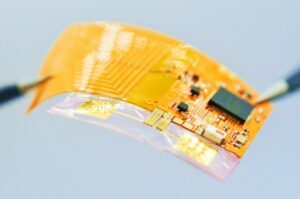 The Spatiotemporal On-Demand Patch’s exposed circuit will be covered by material resembling a Band-Aid. It can receive commands wirelessly from a smartphone or computer to schedule and trigger the release of drugs from individual microneedles.
The Spatiotemporal On-Demand Patch’s exposed circuit will be covered by material resembling a Band-Aid. It can receive commands wirelessly from a smartphone or computer to schedule and trigger the release of drugs from individual microneedles.
Led by Juan Song, PhD, at the UNC School of Medicine, and Wubin Bai, PhD, at the UNC College of Arts and Sciences, research suggests that a wearable patch featuring electrically triggered microneedles for on-demand drug delivery could be the next frontier in treatment of neurodegenerative disorders and neurological injuries.
(UNC Health Newsroom) -- CHAPEL HILL, NC – University of North Carolina at Chapel Hill scientists created a new drug delivery system, called the Spatiotemporal On-Demand Patch (SOP), which can receive commands wirelessly from a smartphone or computer to schedule and trigger the release of drugs from individual microneedles. The patch’s thin, soft platform resembles a Band-Aid and was designed to enhance user comfort and convenience, since wearability is a crucial factor for chronically ill patients.
The research team, led by Juan Song, PhD, professor of pharmacology at the UNC School of Medicine, and Wubin Bai, PhD, assistant professor of applied physical sciences at the UNC College of Arts and Sciences, tested the SOP in a mouse model, using melatonin in the microneedles to improve sleep.
This research, published in the journal Nature Communications, opens the door to researching this wirelessly controlled patch to deliver on-demand treatments for neurodegenerative disorders, including Alzheimer’s disease. To that end, the UNC School of Medicine and UNC Health funded a $25,000 pilot project to test the SOP in a mouse model of Alzheimer’s disease.
“SOP’s ability to enable joint delivery of multiple drugs could address various aspects of Alzheimer’s Disease, such as reducing beta-amyloid plaques, mitigating neuroinflammation and enhancing cognitive function,” said Bai, a co-senior author.
The open access paper titled, “Digital Automation of Transdermal Drug Delivery with High Spatiotemporal Resolution,” was co-authored by Yihang Wang of the Department of Applied Physical Sciences and Zeka Chen of the Department of Pharmacology. Bai said the research highlights not only a multidisciplinary collaboration but also a “passionate involvement of Carolina undergraduate students,” including Priyash Hafiz of the Department of Applied Physical Sciences, and Brayden Davis, Will Lipman, Tian Wang and Sicheng Xing of the UNC/NCSU Joint Department of Biomedical Engineering.
The patch, which has received a provisional patent, enables highly localized treatment – less than 1 square millimeter – of specific tissues, organs or regions within the body, and drug release can be triggered within 30 seconds in response to an electrical signal. Patients could wear more than one patch at a time which would reduce the need for doctors’ visits, or even trips to the hospital, for medical attention.
“The beauty of this device is that it can house dozens, if not hundreds, of concentrated drugs and can program their sequential release automatically,” said Song, who is a member of the UNC Neuroscience Center. “Rapid drug release can be crucial in emergency situations or when immediate therapeutic action is required.”
The microneedles are coated with gold, which protects the drugs and surrounding tissues. When a low-voltage electrical stimulus is applied through the patch, the gold coating disintegrates, exposing the drug-loaded microneedles to the skin and initiating the controlled release of the drugs.
“This level of specificity ensures precise and customized drug delivery, catering to the needs of different conditions or specific regions of the body,” said Wang. “This offers a novel approach to achieving controlled drug release through a combination of materials science and electrical engineering.”
The National Science Foundation and the National Institutes of Health funded this research.
David DeFusco, communications specialist at the UNC Department of Applied Physical Sciences, wrote the original news announcement. The UNC School of Medicine contact is Mark Derewicz, director of research and national news for UNC Health.
2024 Health of US Primary Care Scorecard Webinar is Wednesday
Primary care is the foundation of our health care system. Yet more and more people report not having a regular place for care. In the forthcoming second annual Primary Care Scorecard, Robert Graham Center researchers give five reasons why access to primary care is worsening.
Join the Milbank Memorial Fund and The Physicians Foundation on February 28, at 12 p.m. ET, for a webinar on how the nation and the states are performing on primary care workforce, financing, training and research funding measures — and how challenges within each of these areas contribute to poor access to primary care.
The Physicians Foundation's President, Gary Price, MD, will give opening remarks ahead of a panel discussion moderated by Frances Stead Sellers of The Washington Post. The panel will include:
· Rachel Block, Program Officer, Milbank Memorial Fund
· Margaret Flinter, APRN, PhD, Vice President and Clinical Director, Community Health Centers, Inc.
· Yalda Jabbarpour, MD, Director, The Robert Graham Center
· Kyu Rhee, MD, President and CEO, National Association of Community Health Centers
REGISTER NOW
About The Physicians Foundation
The Physicians Foundation is a nonprofit seeking to advance the work of practicing physicians and help them facilitate the delivery of high-quality health care to patients. As the U.S. health care system continues to evolve, The Physicians Foundation is steadfast in strengthening the physician-patient relationship, supporting medical practices’ sustainability and helping physicians navigate the changing health care system. The Physicians Foundation pursues its mission through research, education and innovative grant making that improves physician wellbeing, strengthens physician leadership, addresses drivers of health and lifts physician perspectives. For more information, visit www.physiciansfoundation.org
Want To Go To Medical School for Free? Here Is A Billion Ways It Is Now Possible

Albert Einstein College of Medicine to offer free tuition after billion-dollar gift
Dr. Ruth Gottesman, 93, who spent 55 years as the chair of the school’s board, made the historic donation in the name of her late husband, David “Sandy” Gottesman, who was an early investor of Berkshire Hathaway and a longtime friend of Berkshire’s famed CEO Warren Buffett.
Philip Ozuah, president and CEO of Montefiore Medicine, the school’s parent company, announced the “transformational gift” on Monday, saying that “this is the largest donation to any medical school in the country.”
Sandy Gottesman, who was the co-founder of New York-based investment firm First Manhattan Co., died in 2022.
The Gottesmans had long been involved in health care philanthropy. In 2010, their gift of $25 million to the Albert Einstein College of Medicine went towards creating the school’s Institute for Stem Cell Research and Regenerative Medicine. Sandy Gottesman also served on the board of New York’s Mount Sinai Hospital.
“I am very thankful to my late husband, Sandy, for leaving these funds in my care, and l feel blessed to be given the great privilege of making this gift to such a worthy cause,” said Dr. Ruth Gottesman in a news release.

Dr. Ruth Gottesman joined the medical school in 1968 and developed screening, evaluation and treatments for children with learning disabilities. In 1992, she founded the Adult Literacy Program at Einstein’s Children’s Evaluation and Rehabilitation Center, “the first of its kind.” She also served as the founding director of the school’s Emily Fisher Landau Center for the Treatment of Learning Disabilities, which opened in 1997.
Few educational donations rival the magnitude of Dr. Ruth Gottesman’s. In 2018, former New York mayor Michael Bloomberg donated $1.8 billion to his alma mater, Johns Hopkins University. And New York hospitals have long drawn the philanthropy of billionaires, with individual donations sometimes amounting to more than $100 million. Home Depot co-founder Ken Langone has heavily invested in New York University’s medical centers. In 2018, in part due to Langone’s donations, NYU’s School of Medicine became the first medical school in the country to offer free tuition to accepted students.
An October survey from the Association of American Medical Colleges found that 70% of medical students who graduated in 2023 have taken on some level of education debt. The average graduate left medical school owing more than $200,000, according to the AAMC.
“This donation radically revolutionizes our ability to continue attracting students who are committed to our mission, not just those who can afford it,” said Dr. Yaron Tomer, the dean at Albert Einstein. “We will be reminded of the legacy this historic gift represents each spring as we send another diverse class of physicians out across the Bronx and around the world to provide compassionate care and transform their communities.”
Warning for Clinicians in Charlotte Region
A message from Erica Wilson, MD, MPH, North Carolina Department of Health and Human Sources
The North Carolina Division of Public Health (NC DPH) is alerting clinicians in North Carolina to an increase in ciprofloxacin- and penicillin-resistant strains of invasive meningococcal disease caused by Neisseria meningitidis serogroup Y (NmY) in the Charlotte Metropolitan region.
Since February 2023, two cases of invasive meningococcal disease have been found to be resistant to ciprofloxacin and penicillin in residents of Mecklenburg County and one case in a resident of neighboring York County, South Carolina. These cases meet the threshold to recommend discontinuing the use of ciprofloxacin for prophylaxis of close contacts per CDC’s updated guidance.
Providers in the Charlotte Metropolitan region including Cabarrus, Gaston, Iredell, Lincoln, Mecklenburg, Rowan, and Union Counties should discontinue the use of ciprofloxacin for prophylaxis of close contacts of invasive meningococcal disease cases and prescribe rifampin, ceftriaxone, or azithromycin instead. Providers treating residents from Chester, Lancaster, or York counties in South Carolina should also follow this guidance for patients being treated in North Carolina medical facilities.
Clinicians should contact their local health departments or the Communicable Disease Branch epidemiologist on-call 24/7 number (919-733-3419) for questions.
Bad News: Your Binge of Yellowstone Likely Means You'll Be In the Bathroom A Lot Tonight

Binge watchers more likely to need multiple night-time bathroom breaks
(The Guardian) -- Sitting down to binge watch the latest TV drama might seem like the perfect way to unwind, but researchers have found that people who spend lengthy periods in front of the box are more likely to need to pee multiple times a night.
Writing in the journal Neurourology and Urodynamics, researchers in China report how they analysed data from the National Health and Nutrition Examination Survey in the US, focusing on responses collected from 2011 to 2016.
The team found that 32% of the 13,294 participants, aged 20 and older, reported experiencing nocturia, the need to wake up and urinate two or more times a night.
After taking into account factors including age, sex, body mass index, ethnicity, education level and whether or not individuals had diabetes, the researchers found that the risk of experiencing nocturia was 48% higher in those who spent five or more hours watching TV or videos a day than those who watched less than an hour.
“To our understanding, this study represents the first exploration of the correlation between TV and/or video viewing time and nocturia,” the researchers write.
The team say the mechanism by which prolonged TV viewing increases the risk of nocturia is poorly understood.
However, they point to a number of possible explanations for the association, noting that lengthy sessions of TV viewing have been associated with an increased risk of developing type 2 diabetes, which is a risk factor for nocturia, while sedentary behaviour is associated with fluid retention in the legs that may also contribute.
“Moreover, TV watching typically aligns with beverage consumption, leading to an elevated fluid intake,” they write, adding that among other possibilities prolonged TV viewing may lead to neurological disorders that could trigger bladder dysfunction, and that TV watching may affect sleep duration or quality.

Watching at least five hours of TV a day associated with higher risk of nocturia, or needing to get up and urinate twice or more a night
The study has limitations, including that it cannot prove cause and effect, and it relied on self-reported data including for TV watching habits.
Despite this, the team say healthcare professionals should tell patients about the link. “Increasing public awareness of this potential health risk encourages individuals to be more mindful of their TV and/or video time,” they write.
James Catto, professor of surgery at the University of Sheffield, who was not involved in the research said there could be a number of factors muddying the waters in the new study. Among them he noted those with nocturia tended to be older, have a higher body mass index than those without, and were less mobile.
“[Have] they got nocturia because they’re watching telly all day, or they watch the telly all day because of other factors and then they just end going to the toilet more often?,” he said, noting that cannot be answered by the current study.
Catto added that nocturia is common, particularly among older people, and that it is not necessarily a cause for concern – although it can occur as a result of cancer, infections or diabetes.
“If you’re going a lot at night, and it’s bothering you, see a GP, they’ll do a few tests to make sure you’ve not got diabetes,” said Catto. But, he added: “Most people are not too bothered by going once or twice at night.”
On Point: Alabama Supreme Court Ruling That Disrupts Healthcare For People Building Families is Unconscionable -- Dr. Amy Bryant
On Point submissions are individual member viewpoints and not North Carolina Medical Society policy.

MSCR, At Large Member of the Executive Committee, NCOGS
Not even a week after the Alabama Supreme Court gave unprecedented and medically unnecessary protections to frozen embryos, several IVF clinics in the state had already halted services, afraid in this dangerous new setting to provide the healthcare they are trained to provide. This disruption to healthcare for people trying to build their families is unconscionable.
Rulings such as the one from the Alabama Supreme Court have an undeniably chilling effect on medical practice. Physicians are trained to provide evidence-based care, and care for patients at their most vulnerable moments. They did not train to understand the nuances of criminal law and precious few want to risk felony charges that could rob them of their ability to support their families and future patients, or even land them in prison.
This bodes poorly for the healthcare workforce in Alabama which already struggles to keep its physician workforce. Alabama also has one of the highest rates of maternal and infant mortality in the nation in the country, with outcomes worse for Black infants and mothers. Over 34% of its counties are “maternity deserts” without adequate access to obstetric care. Further restricting and intimidating physicians, who provide reproductive and primary care, and may also need reproductive services themselves, is counterproductive to improving health outcomes.
Why would people who purportedly care about life at all stages want to put so many people in harm’s way? What about the health and lives of those who need assisted reproductive technology to grow their families? Or those who need contraception or abortion to have a healthy family? It seems that protecting life is not in fact the actual goal. Relegating those who can get pregnant to mere vessels is not meant to protect life, it is a means of coercion and control.
The tactics at play in this case are sadly all too familiar. They are an extension of the tactics that place medically unnecessary restrictions on abortion. This ruling shows that anti-science politicians never intended to stop at abortion. This new type of interference in reproductive healthcare clearly exposes anti-abortion intentions to continue to restrict bodily autonomy, no matter the circumstances. Banning contraception is the next logical step, and even talked about openly in some state legislatures.
Anti-science politicians and judges-most often with no medical training- but with a clear, ideological agenda to control and coerce women, are a serious threat to the healthcare system. This is just not right in a multi-faceted, pluralistic, democratic society where many viewpoints and religious beliefs have the right to coexist.
The Alabama Supreme Court's ruling will fortunately not affect North Carolina. But this ruling should be deeply troubling to all of us, not only because of the devastating impact on people seeking to grow their families using assisted reproductive technology in Alabama. This ruling could embolden other states to pass similar legislation.
North Carolina physicians should take note. The fantasy world of full personhood for embryos that is embodied by rulings such as this does not bode well for our actual patients or healthcare system. Patients and physicians should be allowed to make decisions regarding their fertility based on their personal values and beliefs, not those imposed by the state. A state that sanctions these deeply unpopular intrusions into people’s lives, based on the religious views of a subset of its population, will find itself without the healthcare workforce it needs to have a thriving population.
New Mesothelioma Therapy Offers Hope for Highly Fatal Cancer
Medicine used alongside chemotherapy in trials quadrupled three-year survival rates for mesothelioma
Scientists have reached a breakthrough in the treatment of mesothelioma, a rare and highly deadly form of cancer that’s linked to asbestos exposure. According to a study published last week, the innovative therapy, which combines a new drug with chemotherapy, increased the median survival of participants by about a month and half.
It also quadrupled the three-year survival rates for those who received the drug combination, compared to a placebo group. Lead author Peter Szlosarek, who has been working on this project “from its earliest stages,” said the results are “truly wonderful” in a press release from Queen Mary University of London.
One of the patients who received the new treatment, Mick, was initially given four months to live after he was diagnosed with mesothelioma caused by asbestos exposure during his time working in a factory in the 1970s. He put his trust in Szlosarek and about six years after his diagnosis, he was able to celebrate his 80th birthday with his family.
“This trial has changed the lives of people with mesothelioma, allowing us to live longer,” Mick said. “I have five grandchildren and two great-grandchildren now — I wouldn’t want to miss all that.”

(From The Guardian) -- Scientists have developed a drug to treat mesothelioma, a notoriously hard-to-treat cancer linked to asbestos, in the biggest breakthrough in two decades.
Thousands of people are diagnosed with the disease globally every year, which tends to develop in the lungs and is mainly caused by exposure to asbestos at work. It is aggressive and deadly, and has one of the world’s worst cancer survival rates.
Now scientists are hailing the “truly wonderful” arrival of a new therapy, which they say should offer fresh hope to those with the disease and their families.
In an international trial spanning five countries, led by Queen Mary University of London, a new drug that cuts off the tumor’s food supply quadrupled three-year survival rates. The results were published in the journal JAMA Oncology.
“This trial has changed the lives of people with mesothelioma, allowing us to live longer,” said one of the patients who benefited from the drug. The 80-year-old, who wished to remain anonymous, won compensation from his former employer after being exposed to asbestos in a factory in the 1970s.
He was given four months to live, but thanks to the trial is still alive five years later. “I have five grandchildren and two great-grandchildren now – I wouldn’t want to miss all that,” he said.
The breakthrough is significant, experts say, because mesothelioma has one of the lowest survival rates of any cancer. The new drug, ADI-PEG20 (pegargiminase), is the first of its kind to be successfully combined with chemotherapy in 20 years.
The trial involved patients from the UK, US, Australia, Italy and Taiwan, and was led by Prof Peter Szlosarek at Queen Mary. Each received chemotherapy every three weeks for up to six cycles. Half were also given injections of new drug, while the other half received a placebo for two years.
Among the patients included in the final analysis were 249 people with pleural mesothelioma – when the disease affects the lining of the lungs. They had an average age of 70.
The study, known as the ATOMIC-meso trial, was conducted at 43 centers in the five countries between 2017 and 2021. Those who received pegargiminase and chemotherapy survived for an average of 9.3 months, compared with 7.7 months for those who had the placebo and chemotherapy, according to the results published in JAMA Oncology.
The average “progression-free survival” was 6.2 months with pegargiminase-chemotherapy, compared with 5.6 months among patients who had the placebo and chemotherapy.
“In this pivotal, randomized, placebo-controlled, phase 3 trial in 249 patients with pleural mesothelioma, pegargiminase-chemotherapy increased significantly the median overall survival by 1.6 months and quadrupled the survival at 36 months compared to placebo-chemotherapy,” the authors wrote.
“Pegargiminase-based chemotherapy was well tolerated with no new safety signals.”
The breakthrough follows two decades of work by Szlosarek, after his original discovery that mesothelioma cells lack a protein called ASS1, which enables cells to manufacture the amino acid arginine.
This knowledge was used to develop the drug. ADI-PEG20 works by depleting arginine levels in the bloodstream. For tumor cells that cannot manufacture their own arginine, this means their growth is thwarted.
“It’s truly wonderful to see the research into the arginine starvation of cancer cells come to fruition,” said Szlosarek. “This discovery is something I have been driving from its earliest stages in the lab, with a new treatment, ADI-PEG20, now improving patient lives affected by mesothelioma.”
Dr Tayyaba Jiwani of Cancer Research UK, which funded the research alongside the biotechnology company Polaris Group, said: “This study shows the power of discovery research which allows us to dig deep into the biology of mesothelioma to uncover vulnerabilities that we can now target with ADI-PEG20.”
Liz Darlison, chief executive of the charity Mesothelioma UK, said: “The UK mesothelioma community, including doctors, nurses, patients and families living with mesothelioma, are extremely proud of ATOMIC. It offers another much-needed treatment option and, above all, hope to those living with mesothelioma.
“We look forward to seeing this treatment become available as a standard option to all patients in the future.”
New Study: VR Can Enhance Relationship Between Caregivers and Aging Population

Research conducted by Stanford University's Virtual Human Interaction Lab in collaboration with Mynd Immersive and AT&T 5G Healthcare
(PRNewswire) -- Virtual Reality (VR) technology is not just for the young. It's paving the way for enhancing relationships between the aging population and their caregivers, as research from the Virtual Human Interaction Lab (VHIL) at Stanford University demonstrates.
This research comes just months after the American Medical Association issued CPT codes that recognize VR for various therapeutic services, a major milestone for the growth of digital therapeutics.
The study sought to understand older adults' attitudes towards new technologies, including virtual reality, and how professional caregivers felt about facilitating VR experiences for older adults. Research was led by Dr. Jeremy Bailenson, founding director of the VHIL and one of the world's leading experts on understanding and exploring individual behavior and social responses in VR, and Ryan Christopher Moore, Ph.D. researcher.
"This study showcases how a tool which is typically associated with youthful entertainment has transformative applications in healthcare, particularly geriatric care," said Dr. Bailenson. "The response from both the caregivers and seniors has been quite positive, suggesting
that VR can be a sustainable and beneficial tool in Senior Care communities."
Key findings include that 81.5% of caregivers reported they enjoyed interacting with residents more while using Mynd Immersive (Mynd), formerly MyndVR than while doing other activities, and 94.9% said that using Mynd was moderately to extremely beneficial to their relationship with the resident. Similarly, 83% of residents reported that using Mynd was moderately to extremely beneficial to their relationship with the caregiving staff.
The study also found:
- 74.2% of the caregivers reported that the residents' mood improved after using Mynd, and 79.2% of the residents reported feeling more positive
- 57.9% of older adults reported feeling less isolated from the outside world after using Mynd
- While positive attitudes towards new technology often decline with age, the study population overwhelmingly felt positive about using VR and the decline in attitude was less than compared to other technologies like cell phones and voice assistants

"Shared experiences in VR, like revisiting a senior's hometown or traveling to a place they've always wanted to see, can stimulate greater communication, bridge emotional gaps, and create deeper bonds," said Chris Brickler, CEO of Mynd Immersive. "We are experiencing explosive growth of our aging population, while simultaneously seeing a significant decline in available caregivers, so it's imperative that we create tools like Mynd that can help create a more enjoyable and fulfilling environment for both the cared and caregiver."
Mynd has brought together a powerful consortium of industry collaborators to support this research and beyond, including AT&T, HTC VIVE, Select Rehabilitation, and some of the world's most innovative senior living communities, such as John Knox Village in Pompano Beach, Florida, Commonwealth Senior Living, Sodalis Senior Living, Long Island State Veteran Home and more.
"We're entering a new era of delivering immersive, digital therapeutics," said Joe Drygas, Head of AT&T Healthcare. "The combination of XR experiences with 5G and AI will have a tremendous impact on the many ways we can provide top quality care for our elders and support their caregivers. The Mynd Immersive and AT&T collaboration is bringing the future of connected healthcare into sharp focus for older adults and their families."
"We launched HTC VIVE with a belief that VR could positively impact humanity," said Cher Wang, Chairwoman of HTC. "This type of data from industry partners like Mynd and esteemed independent researchers, such as Stanford University, further supports our belief and moves the entire industry forward."
Stanford's pioneering lab, focused on the psychological and behavioral effects of virtual reality, conducted a survey of 245 older adults and 39 caregivers in 16 Senior Care communities across 10 states. The study, the largest ever conducted on VR and older adults, was done in collaboration with Mynd, the leading provider of immersive therapeutic experiences for the aging population.
The study has already won a "Top Paper Award" by the National Communication Association and will be presented at their upcoming annual convention. The paper has also been accepted by the journal, Cyberpsychology, Behavior, and Social Networking and will be published later in 2023.
NCDHHS Secretary Kody Kinsley Unifies Department's Collaborative Efforts
NCDHHS Wants to Ensure NC Communities and Families Are Center of Department Work
https://youtu.be/qPW4Qk6iqzU?si=TrWZm30fZ2zty4_9
The NCDHHS launched a Community Partner Engagement Plan and website to ensure the voices of North Carolina communities and families are at the center of the department’s work.
Go to ncdhhs.gov/GetInvolved to see the many groups, organizations and commissions that NCDHHS currently partners with. The department will continue to update the website and encourages community members to get involved with a current group or sign on to work with the divisions that focus on your area of interest.
To improve internal processes, Secretary Kinsley issued a Secretarial Directive that unifies the department’s collaborative efforts into a guide for how to best engage with communities.
NCDHHS is excited to deepen its partnerships and collaboration by strengthening connections with communities statewide and listening to their insights. The department’s goal is to grow together with North Carolinians and make major progress toward better health for all.
Learn more in the Community Partner Engagement Guide and watch a video from Secretary Kinsley where he announces the plan. For more information on how to partner with NCDHHS, email [email protected].
North Carolina Stepping Onto National Stage as Biotech Skyrockets in Triangle

Nation's Oldest Biotech Hubs Looking at NC as One of Their Biggest Rivals
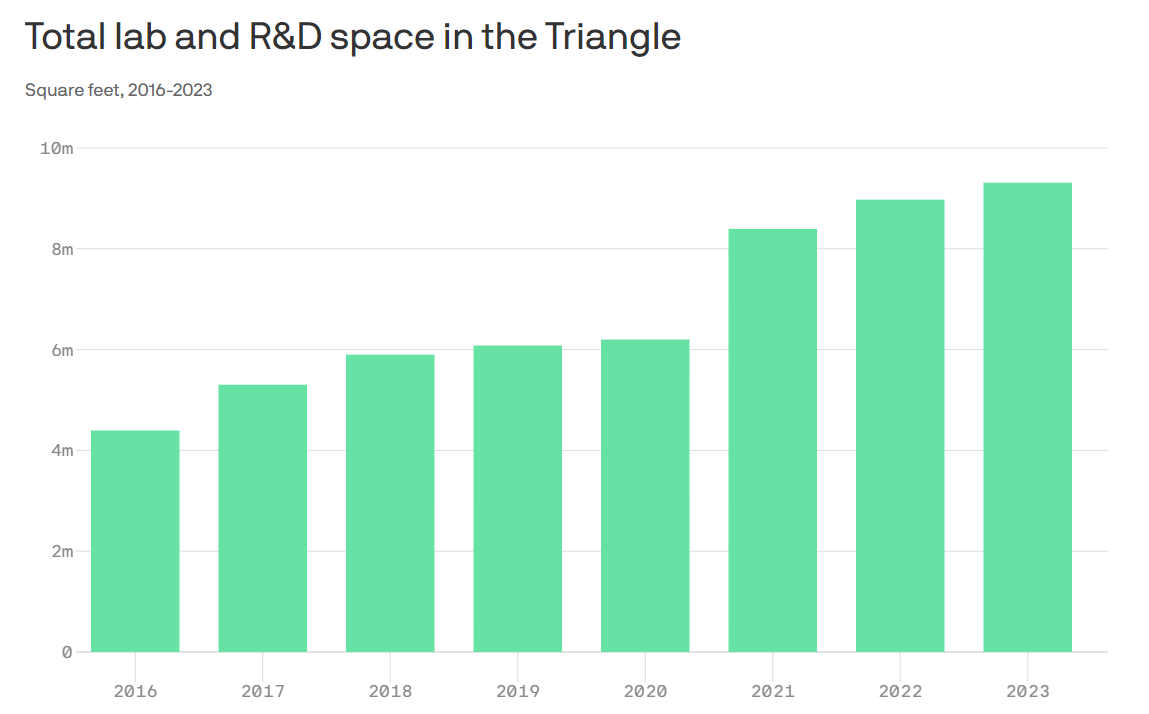
(Axios - Zachery Eanes) -- In less than a decade, the Triangle's biotech industry has more than doubled its lab space and added tens of thousands of new workers, as the region's profile among investors and companies soars.
The big picture: Some of the nation's oldest biotech hubs, like Boston, now see the Triangle as one of their biggest rivals, as a widely shared Boston Globe article noted this month.
- That's because the region not only boasts a talented workforce but also continues to offer comparatively low costs for land, construction, electricity, lab rent and housing, the Globe reported.
Why it matters: The biotech industry has long driven the Triangle's growth, making Research Triangle Park a name brand across the country. From scientists with advanced degrees to community college graduates working in pharmaceutical manufacturing, the high-paying jobs abound.
- And even as investments into office buildings slow down, the building boom in the life sciences industry remains robust.
By the numbers: Around 40,000 people in the Triangle worked in the life sciences industry as of 2022, a significant increase over the past decade, according to research from CBRE.
- From 2016 to 2023, lab and R&D space grew from 4.4 million square feet to 9.3 million square feet.
- Since 2018, nearly 30 life sciences companies, like Fujifilm Diosynth and Eli Lilly, have invested $8.9 billion in the region, and pledged to create nearly 7,000 new jobs.
Zoom in: Research Triangle Park, home to hundreds of companies and where a $1.5 billion development effort is underway, is the epicenter of the Triangle's biotech industry.
- But it's influence has seeped into every corner of the region, with downtown Durham now a hot spot for startups, and manufacturing hubs for pharma companies popping up from southern Wake County all the way to Sanford.
- Chapel Hill and Raleigh are also seeing upticks in lab space construction.
Among the biggest projects underway:
- Spark Life Science in Morrisville, which could span 1.5 million square feet of lab and manufacturing space. The first phase has been completed, with no tenants signed yet.
- Pathway Triangle, a 1 million square foot manufacturing campus under construction across the street from Spark LS, is currently being built by Boston-based King Street Properties.
- Via Labs, which will be Hub RTP's first lab high-rise, could start construction later this year — though Boston-based owner Longfellow is still waiting to sign tenants.
- Fujifilm Diosynth's $2 billion manufacturing campus in Holly Springs will be completed in 2025. Janssen Supply Group recently signed a lease there as well.
Between the lines: The growth simply wouldn't be happening without the presence of three tier-one research universities, Lee Clyburn, executive vice president at CBRE's Raleigh office, told Axios.
- In 2023 alone, Duke, UNC, the Research Triangle Institute and others brought in $1.9 billion in National Institute of Health funding.
- And thanks to the universities, the Triangle boasts one of the highest concentrations of life science researchers in the country.
Threat level: With so much lab and manufacturing space on the way, vacancy rates are expected to rise, CBRE noted, and already they are hovering around 10%.
- A combination of higher interest rates and a slowdown in venture capital funding could slow down the industry's growth in the Triangle as well.
- Forge Nano — a battery company, not a life sciences company — was the only major manufacturing lease in the four quarter of 2023.
Yes, but: The real estate firm JLL also recently named the Triangle as the No. 1 biomanufacturing market in the country.
- And JLL notes that the Triangle's pipeline of construction, while large, is not as speculative as markets like Boston or the Bay Area.
What's next: Novo Nordisk, the Danish pharmaceutical company behind the weight-loss drug Ozempic, could be the next life sciences company to plot a Triangle expansion.
- The company has purchased an additional 163 acres around its facility in Johnston County and filed permits for an expansion of its Durham County manufacturing facility, CBRE noted.
Webinar Opportunity! Next-Generation Genomic Sequencing

Two Webinars Offered by Southern Regional AHEC with Duke University
Southern Regional AHEC, in partnership with Duke University, is hosting a live webinar highlighting rare genetic diagnoses titled “Next-generation Genomic Sequencing for Rare Genetic Diagnoses: Engagement with Community Health Providers."
Program Description
For this interactive educational program, the objectives are two-fold. The first is to discuss current diagnostic approaches to patients presenting with clinical features suggestive of a genetic disorder and what are the “next steps” if clinical genetic testing does not result in a diagnosis for your patient. The second objective is to learn from providers about how important access to clinical genetics is to their practice, their experiences with referring patients to clinical genetics, barriers they have encountered as well as possible approaches to mitigating barriers.
Objectives
Upon completion of this program, participants will be able to:
- Identify genomic sequencing technologies, clinical applications, and interpretation of genomic sequencing.
- Discuss the benefits of genomic sequencing for patients and management of patients who undergo genomic sequencing.
- Identify patient phenotypes that would most benefit from genomic sequencing.
- Review the use of genomic information for direct patient care.
- Review barriers beyond clinical care that affect patients in rural areas participating in genetic evaluations in genomic sequencing.
- Analyze modalities that would improve access to genomic medicine for the patients
Speaker
Dr. Vandana Shashi is a board-certified Clinical Geneticist with over two decades of experience in rare/ultra-rare genetic disorders. She is the Principal Investigator of the NIH Undiagnosed Diseases Network (UDN) Clinical Site at Duke, wherein patients from all over the USA, with difficult to diagnose rare/ultra-rare diseases are evaluated for diagnostic purposes. Next- generation genomic sequencing (NGS) inclusive of exome and genome sequencing for diagnoses is a major focus of the UDN and under Dr. Shashi’s leadership the Duke UDN clinical site has been successful in diagnosing 40% of patients who had not been able to obtain diagnoses previously, with a consequent impact on medical management. Dr. Shashi is passionate about findings ways for patients with health disparities to also participate in the UDN. She looks forward to engaging with providers in rural NC to discuss cutting-edge genomic technologies for their patients with rare/ultra-rare phenotypes and to identify barriers that they perceive result in low participation by patients with health disparities.
For more information, including CME credits, click here.
Match Day is Coming Soon. Are You Ready?

Match Madness is March 15
(AMA, Brendan Murphy) -- For many medical students, creating a Match rank-order list is about balancing competing priorities and funneling advice—solicited and unsolicited—from faculty members, peers and resident physicians. That was the case for Haidn Foster, MD, when he was considering his options for the Match as a fourth-year medical student at the University of Cincinnati College of Medicine in 2022. In the end, Dr. Foster said, how one constructs a rank-order list is highly personal.
“The whole process is so individualized to what means most to you as an applicant,” said Dr. Foster during an interview for the AMA. “Somebody who interviewed at the same programs but had slightly different priorities for residency may make an entirely different rank-order list and be just as happy with the outcome of the Match as I was.”
In advance of the Feb. 28 deadline for residency applicants to submit their rank-order lists—and with the caveat that the process is going to come down to one’s own instincts and priorities—Dr. Foster offered a few key insights about how he created his list and what he might have done differently with the benefit of hindsight.
Think long-term

“For applicants who are similarly interested in subspecializing, there are a lot of benefits to matching at a program that has your desired fellowship in-house. As a resident, I wanted to get a better feel for my chosen field and learn what it would be like to practice as a hematologist-oncologist, so it was important for me to rank institutions highly that had an associated hematology-oncology fellowship,” he added.
“Future plans aside, as a resident you’ll be in training for at least the next three to seven years, so having a residency program that is both a good cultural fit and responsive to resident feedback—backed up by specific and meaningful examples of program adaptation—were also critical aspects of how I evaluated the programs I interviewed at.”
Make compromises
“I interviewed at a healthy mix of academic and community programs,” Dr. Foster said. “When it came to ranking each program, at times, I was conflicted because of the connection I felt with some of the community programs. I wanted to highly rank the programs that spoke most strongly to my values—those with a demonstrated commitment to diversity, equity, inclusion, and to serving the underserved.
“Still, knowing that I had very clear-cut career ambitions with regards to my plans for fellowship, I knew that I would be best served by matching into an academic program. So I found myself ultimately ranking some programs lower despite having a strong emotional connection to their philosophy and leadership.”
Know your deal-breakers
It is important to keep in mind which factors of a given program are deal-breakers for you, and which are not. What, in other words, can you live with for the duration of your residency? For Dr. Foster, geography was not a big factor in his rank-order list.
“I've had the perspective throughout medical training that I can live anywhere for a limited amount of time,” Dr. Foster said. “And so I was happy to move from my hometown near Seattle to Cincinnati for medical school, and then to move again to Pennsylvania for residency.”
Dr. Foster’s residency interviews were exclusively virtual due to the COVID-19 pandemic, but most interviews, post pandemic remain virtual. Having not visited a number of the schools with which he interviewed, there was a level of uncertainty in the process, he said.
“Some of the process is a leap of faith. I'd never been to Hershey. So that was a really interesting experience: matching to a program in a city I’d never visited, even signing a lease on an apartment sight unseen. It was all a real adventure, one that I’m thankful has turned out well.”
Draw on interview-day feelings
“One of the mistakes I made during interview season was not being diligent enough keeping notes on the day of an interview,” Dr. Foster said. “Especially because interviews are virtual and you may be interviewing at multiple programs per week, everything really starts to blend together. Trying to recall specifics of each program towards the end of interview season can be difficult if you haven’t recorded those details around the time of your interview.
“The standout programs—whether exceptional or otherwise—are easy to recall and rank accordingly. But having a record of day-of observations is incredibly useful when stratifying residencies that fall in the middle of the pack.
“Another helpful aspect of some programs’ interview process was the facilitation of one-on-one conversations with current residents. When I had specific questions about a program or wanted more information about what it would be like as a member of an affinity group at that institution, being able to ask residents their opinions outside of a group setting was invaluable.”
Don’t get bogged down in every detail
“One of the considerations I gave too much weight when interviewing was the specifics of the intern year schedule,” Dr. Foster said. “In my field, internal medicine, you are going to have very full days, very full weeks.
“The rigors of a 60-to 80-hour work week are going to be the reality of pretty much any residency program,” he noted. “And whether that's accomplished through a consistent inpatient schedule of a 6 a.m.–6 p.m. workday versus a regular day, short-call day, long-call day, all those specific details come out in the wash and are not as big of a deal as I thought they were going to be.”
Deam big
“The Match process truly prioritizes applicant preferences,” said Dr. Foster, an AMA member. “There is no downside to an applicant ranking their true No. 1 program as No. 1 in their rank-order list.
“Even if you feel like the odds of matching are low, ranking that program that’s perfect for you highly will not detrimentally impact your match,” he noted. “There is no gaming the system; just rank programs in the order that you actually prefer them.”
Set it—then forget it
“Personally, I took a long time to make my list,” Dr. Foster said. “But then I put it into the system and pressed ‘Certify’ and put it out of my mind. I think going back and changing things after certification would have just added more stress. Then there's the legitimate fear of forgetting a step and not hitting ‘Certify’ a final time.”
The AMA Road to Residency series provides medical students, international medical graduates and others with guidance on preparing for residency application, acing your residency interview, putting together your rank-order list and more.
Find the perfect Match
Podcast: Meet your Match step-by-step residency selection guide
Video: How to choose the best residency program for you
Specialty guide: Simplify your specialty selection for residency
As Nation Grapples with Alabama Decision on Embryos, An NCMS Member Speaks Out

Alabama Says Embryos in a Lab Are Children. What Are the Implications?
Scroll down for response from NCMS Member Dr. Amy Bryant
(NYT, Jan Hoffman) -- The Alabama Supreme Court has opened a new front in the legal debate over when human life begins. Embryos created and stored in a medical facility must be considered children under the state’s law governing harmful death, the court ruled.
Friday’s ruling was cheered by anti-abortion activists nationwide, who have long argued that life begins at conception. They were thrilled that, for the first time, a court included conception outside the uterus in that definition. But the strongest and most immediate effect of the decision will be on fertility patients trying to get pregnant, not women seeking to end their pregnancies.
The Alabama ruling invites states to enact strict new regulations over the fertility industry that could sharply limit the number of embryos created during a cycle of medical treatment and affect the future of millions of stored frozen embryos. A concurring opinion even offered road maps for such statutes. That could have a chilling effect on a person seeking to have children through in vitro fertilization, whether single or part of a same-sex or heterosexual couple.
What did the ruling say?
The ruling is actually somewhat narrow. It applies to three couples who had sued the Center for Reproductive Medicine, a fertility clinic in Mobile, for inadvertently destroying their embryos. The plaintiffs argued that they were entitled to punitive damages under Alabama’s 1872 Wrongful Death of a Minor Act. Two lower state courts disagreed, saying the embryos were neither people nor children. The State Supreme Court reversed those rulings, saying that the embryos fell squarely under Alabama’s definition of minors and that the negligence lawsuits could proceed. The case will now go back to the State District Court for further litigation.
What did the ruling not say?
The decision is silent on the fate of other frozen embryos in Alabama because that issue was not before the court. The ruling is only about the terms under which plaintiffs may bring a negligence case against a fertility clinic for embryo destruction. However, it could eventually have major consequences for Alabama patients and providers.
On Wednesday, the I.V.F. clinic at the University of Alabama at Birmingham announced it was pausing fertility treatments to explore the implications of the court’s ruling on its patients and providers. One fear is that the clinic, doctors and even patients may face daunting new liability issues surrounding the handling of embryos.
What will it mean for fertility patients and clinics?
“The honest answer is that we don’t know for sure,” said Dr. Paula Amato, president of the American Society for Reproductive Medicine, an organization that lobbies on behalf of fertility experts and patients. “But the ruling is very concerning.”
Freezing embryos is a widespread practice. During a standard cycle of in vitro fertilization, a woman takes hormones to maximize her production of eggs. A doctor then retrieves as many eggs as possible and injects them with sperm in the clinic’s lab, with the goal of creating viable embryos for implantation.
That process will often result in numerous embryos. Because of dangers associated with multiple births from I.V.F., protocols now urge doctors to implant only one embryo at a time. But success with implantation is hardly guaranteed, and so typically doctors freeze remaining embryos for subsequent attempts.
But if laws prevent providers in Alabama from freezing embryos, patients may face the medically challenging and financially draining prospect of many more cycles, Dr. Amato said. Success rates would most likely plummet. “It will disproportionately affect lower income people, people of color and people in L.G.B.T. communities,” she said.
Overall, according to federal data, infertility affects 9 percent of men and 11 percent of women of reproductive age in the United States.
The ruling may therefore restrict the ways that reproductive medicine is practiced in Alabama. “The ruling potentially criminalizes or sets a high civil penalty for standard procedures that we do every day,” Dr. Amato said.
Did the Alabama court suggest protocols for frozen embryos?
No. The court was clear that it could not regulate fertility clinics and the practice of reproductive medicine. But in a concurring opinion, Chief Justice Tom Parker strongly urged the Alabama legislature to examine the matter. He said that other countries, including Italy, New Zealand and Australia, limited the number of embryos that could be created as well as implanted, and suggested that states look to them for regulatory templates.
Is this case headed to the U.S. Supreme Court?
Not imminently, legal experts predicted. The clinic would have to appeal the decision, a move that could be risky, said Katherine L. Kraschel, an expert on reproductive law at Northeastern University School of Law. In light of the United States Supreme Court’s 2022 Dobbs ruling that overturned the national right to abortion, she said, the clinic’s chances at even getting to the door of the Supreme Court would be slender, “because the case hinges on a State Supreme Court’s interpretation of its own state statute.”
Lawyers for the clinic did not return requests for comment.
Also, the case is far from finished in Alabama. The State Supreme Court directed the parties to return to the district court to litigate the case in light of the new ruling, including the suggestion that other legal avenues be explored. One issue it identified was whether a clinic’s standard contract with fertility patients, which typically allows providers to donate or destroy embryos at some future point, could limit the clinic’s liability in this case.
Does all this have any effect on abortion?
In recent years, anti-abortion groups have been pressing for fetuses to be granted “personhood” status, which would entitle them to legal protections. In extending that umbrella to cover embryos in a lab, the Alabama Supreme Court employed reasoning that runs through the U.S. Supreme Court’s 2022 abortion ruling: that fetuses deserve a court’s shield under the 14th Amendment’s equal protection clause.
“The Supreme Court is making this bid to think about the fetus as a vulnerable, unprotected minority that courts are obliged to step in and protect, whether that is through upholding anti-abortion restrictions or moving forward toward accepting and recognizing the fetus as a person,” said Melissa Murray, an expert on reproductive law at the New York University School of Law.
Americans United for Life, the country’s oldest anti-abortion organization, was particularly encouraged by Alabama’s embrace of that theme.
“The Alabama Supreme Court held that the text of the Wrongful Death of a Minor Act is clear and applies to all pre-born children, including the plaintiffs’ embryonic pre-born children. In doing so, the Court correctly acknowledged the legal status of embryos as human persons,” Danielle Pimentel, the policy counsel for the organization, said in a statement. “This decision is a step in the right direction toward ensuring that all pre-born children are equally protected under the law.”
Dr. Amato said she found it ironic that anti-abortion groups were supporting rulings that could severely limit I.V.F.
“I.V.F. is about family building,” she said. “It should be viewed by red states as a pro-life activity.”

MSCR, At Large Member of the Executive Committee, NCOGS
Response to the ruling by NCMS member Dr. Amy G. Bryant, MD:
The Alabama Supreme Court's ruling will fortunately not affect North Carolina. But this ruling is deeply troubling because it gives medically unnecessary legal protections to frozen embryos. This will have a devastating impact on people seeking to grow their families using assisted reproductive technology, and could embolden other states to pass similar legislation. The tactics at play in this ruling are an overt attempt to control people who need this assistance to build their families, and are an extension of the tactics that place medically unnecessary restrictions on abortion. This ruling shows that anti-science politicians never intended on stopping at abortion. This new type of interference in reproductive healthcare exposes anti-abortion intentions to continue to restrict bodily autonomy, no matter the circumstances. Patients and physicians should be allowed to make decisions regarding their fertility based on their personal values and beliefs, not those imposed by the state.
If you would like to comment, please contact Randy Aldridge ([email protected]) to submit an article for the NCMS On Point Blog.
First Child Cured of Brainstem Glioma 'Offers Real Hope'
New Breakthroughs Are Raising Hope for Terminal Children
(AFP - Isabelle Tourne and Daniel Lawler) -- When Lucas was diagnosed with a rare type of brain tumor at the age of six, there was no doubting the prognosis.
French doctor Jacques Grill gets emotional when he remembers having to tell Lucas's parents that their son was going to die.
However, seven years later, Lucas is now 13 years old and there is no trace of the tumor left.
"Lucas beat all the odds" to survive, said Grill, head of the brain tumor program at the Gustave Roussy cancer centre in Paris.
The tumor, which has the full name diffuse intrinsic pontine glioma (DIPG), is diagnosed every year in around 300 children in the United States, and up to 100 in France.
Ahead of International Childhood Cancer Day on Thursday, the medical community has praised advances that mean 85 percent of children now survive more than five years after being diagnosed with cancer.
But the outlook for children with the DIPG tumor remains grim -- most do not live a year beyond diagnosis. A recent study found that only 10 percent were alive two years on.
Radiotherapy can sometimes slow the rapid march of the aggressive tumor, but no drug has been shown to be effective against it.
No Other Case Like Him
Lucas and his family travelled from Belgium to France so that he could become one of the first patients to join the BIOMEDE trial which tests potential new drugs for DIPG.
From the start, Lucas responded strongly to the cancer drug everolimus, which he was randomly assigned.
"Over a series of MRI scans, I watched as the tumor completely disappeared," Grill told AFP.
But the doctor did not dare stop the treatment regimen -- at least until a year and a half ago, when Lucas revealed he was no longer taking the drugs anyways.
"I don't know of any other case like him in the world," Grill said.
Exactly why Lucas so fully recovered, and how his case could help other children like him in the future, remains to be seen.
Seven other children in the trial survived years after being diagnosed, but only Lucas's tumor completely vanished.
The reason these children responded to the drugs, while others did not, was likely due to the "biological particularities" of their individual tumors, Grill said.
"Lucas's tumor had an extremely rare mutation which we believe made its cells far more sensitive to the drug," he added.
Reproducing Lucas
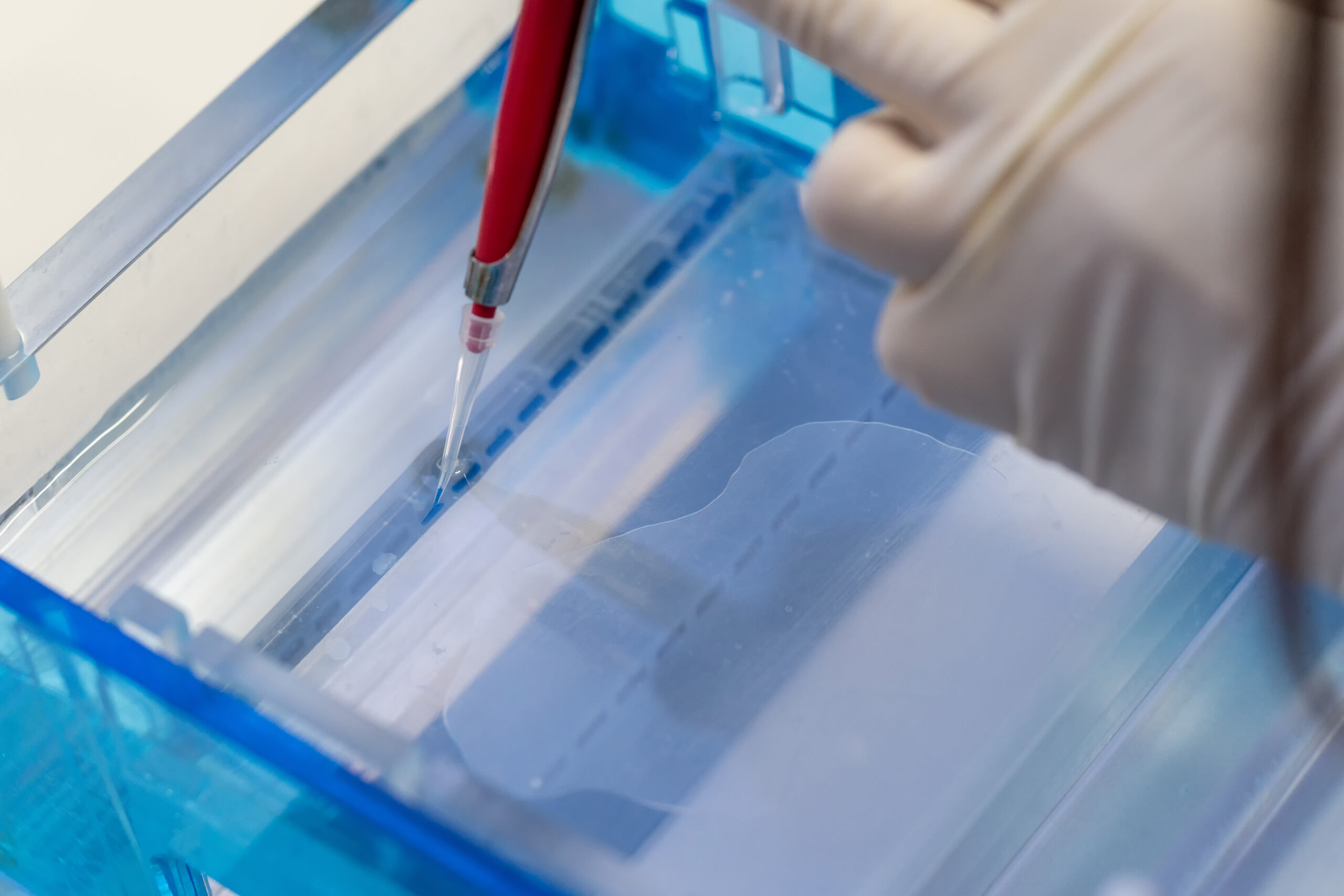
The researchers are studying the genetic abnormalities of patients' tumors as well as creating tumor "organoids," which are masses of cells produced in the lab.
"Lucas's case offers real hope," said Marie-Anne Debily, a researcher supervising the lab work.
"We will try to reproduce in vitro the differences that we have identified in his cells," she told AFP.
The team want to reproduce his genetic differences in the organoids to see if the tumor can then be killed off as effectively as it was in Lucas.
If that works, the "next step will be to find a drug that has the same effect on tumor cells as these cellular changes," Debily said.
While the researchers are excited about this new lead, they warned that any possible treatment is still a long way off.
"On average, it takes 10-15 years from the first lead to become a drug -- it's a long and drawn-out process," Grill said.
David Ziegler, a pediatric oncologist at Sydney Children's Hospital in Australia, said that the landscape for DIPG has dramatically changed over the last decade.
Breakthroughs in the lab, increased funding and trials such as BIOMEDE make "me convinced that we will soon find that we are able to cure some patients," Ziegler told AFP.
Keto Flu, VO2 Max, Bed Rotting. Some New Words Are Being Added to the Dictionary!

There's A Word For That!
Girl dinner, skiplagging, range anxiety, sound bath, shacket! These are just a few of the new words introduced this year and many of them are from the medical field.
by Nick Norlen, Senior Editor, and Grant Barrett, Director of Lexicography
It’s 2024, and the pace of language change is as rapid as it has ever been. Our lexicographers are updating the dictionary more frequently than ever, doing the human-scale work of documenting words across the vast spectrum of the always-evolving English language. And wow, the variety is real.

This snapshot of our most recent additions showcases the breadth of terms that have emerged to name the nuances of modern life, including:
- Terms surfaced from the major topics of the day, including economics (greedflation), climate (climate breakdown), and social issues (intimate partner violence)
- Words for things you didn’t know there were words for (skiplagging, bed rotting, range anxiety)
- Science terms you’ll encounter in the news (stellar nursery, superfog)
- Newly prominent health and wellness words (VO2 max, prebiotic, keto flu).
- Fashion words, including terms for industry trends (slow fashion, circular fashion), aesthetics (Barbiecore), and names for types of garments (shacket, shortalls)
- And so many more words across an all-encompassing range of the English language (energy poverty, sound bath, boobne).
As usual, this update includes words that are new to the dictionary as well as entries that are newly revised (such as newly added senses of existing words like mid and squish). Keep in mind that words that are new to the dictionary are not always new to the language (or even remotely recent), but their addition often reflects a prominent place in the lexicon.
As always, all of our dictionary work is descriptive—we describe language as it is really used (not just how we or others may wish it would be used). Learn more about how new words get added to Dictionary.com—and how the dictionary works.
Of course, some of the terms in the list below have more than one definition. We’ll highlight just the meanings most relevant to this release.
girl dinner noun. an often attractively presented collection of snacks that involve little preparation, such as small quantities of cold cuts, cheese, fruit, cherry tomatoes, etc., deemed sufficient to constitute a meal for one.
Girl dinner went viral after TikTok user Olivia Maher used the term in a video in May 2023, possibly shortening an earlier version, hot girl dinner, that often included decadent or youth-maintaining food.
mid adjective. mediocre, unimpressive, or disappointing.
bussin’ adjective. great; wonderful; amazing. Popular among Gen Z, this term originates in African American culture and is likely based on various senses of bust meaning “to explode,” “to do well,” or “to enjoy.”

the ick noun. a sudden feeling of disgust or dislike, often in response to the actions of another person. This phrase, popular in dating culture and on TikTok, is thought to trace back to the late 1990s TV show Ally McBeal. The ick is also used as an informal term for an illness, especially a cold or flu.
cheat code noun. a ploy or technique that bypasses traditional methods or rules in order to improve oneself or one’s success. This more recent sense of the term is an extension of its use in the context of video games, in which it refers to a hidden command, code, etc., used to gain an advantage, such as by advancing levels or enhancing a character’s strengths.
noun. the apprehension or fear that an electric vehicle’s battery will run out of power before reaching one’s intended destination or a charging station.
enshittification noun. the gradual degradation of an online platform or service’s functionality, as part of a cycle in which the platform or service first offers benefits to users to attract them, then pursues more and more profits at the expense of users. Used in the critical discussion of platforms like TikTok, X (formerly Twitter), and others, this term was popularized by writer Cory Doctorow.
skiplagging noun. the practice of purchasing an air ticket for a flight with a layover at one’s true destination, getting off at the layover point, and skipping the last leg of the flight: a workaround to avoid paying a higher fare for a direct flight to one’s destination. The verb form is skiplag, a compound of skip, “to pass over,” and lag, “an instance of staying behind.”
bed rotting noun. the practice of spending many hours in bed during the day, often with snacks or an electronic device, as a voluntary retreat from activity or stress. Despite the negative connotation of rotting, many use this term in a positive way to refer to what they consider a form of self-care. The verb form is bed rot.
pretty privilege noun. an unearned and mostly unacknowledged societal advantage that a person has by fitting into the beauty standards of their culture. Pretty privilege uses the same construction as white privilege and similar terms.
Science

stellar nursery noun. Astronomy. a molecular cloud in which new stars are being formed. The James Webb Space Telescope has captured some stunning images of these star-forming regions, including the one pictured below, named 30 Doradus and nicknamed the Tarantula Nebula. Located in the neighboring galaxy known as the Large Magellanic Cloud, it is the largest and brightest stellar nursery in the Local Group, a group of galaxies near the Milky Way.

NASA, ESA, CSA, STScI, Webb ERO Production Team
boring billion noun. a period in the earth's development occurring between 1,800 and 800 million years ago that is characterized by relative geological and climatic stability, slow evolutionary development, and low levels of atmospheric oxygen.
geoglyph noun. a large-scale design or pattern on the surface of the land made by arranging stones, rocks, or earth, or by removing ground cover to expose the rock or soil beneath. Geoglyph is the most well-known of the terms listed here ending in -glyph, which comes from the Greek word for “a carving”; geo- means “earth.”
ammoglyph noun. a pattern or design originally created in sand by early humans and now fossilized. Coined in 2019 by Canadian geologist Charles William Helm and colleagues based on the Greek ámmo(s), meaning “sand.”
dendroglyph noun. an image, message, or symbol carved into a tree, especially by Indigenous people and often hundreds of years old, providing cultural and historical information not available from other sources. Coined in 1918 by Australian curator Robert Etheridge, Jr., with the combining form dendro-, meaning “tree." Its use has replaced that of the earlier term arborglyph.
Fashion
Barbiecore
noun. an aesthetic or style featuring playful pink outfits, accessories, decor, etc., celebrating and modeled on the wardrobe of the Barbie doll. We’re likely still fully within the trend of using -core to form names for niche aesthetics, such as cottagecore and normcore.
sustainable fashion noun. a genre of clothing and other fashion products intended to reduce negative impacts on the environment through the use of ecologically responsible materials and manufacturing, the promotion of longer-lasting style trends, and the popularization of product reuse.
slow fashion noun. a movement among clothing producers and consumers that emphasizes eco-friendly, well-made clothing, maintenance and repair of garments to extend their lifespan, and a general reduction of one’s consumption of new clothing items. This term is used in contrast with fast fashion. The fast/slow framing is perhaps best known for its use in the distinction between fast food and slow food, but it will likely continue to be applied in other contexts where there is interest in sustainable practices.
eco-chic noun. of or relating to a style, design, or product that is attractive and fashionable as well as eco-friendly and sustainable.
shacket
noun. a garment in the style of a button-down shirt, made of a thicker fabric and usually worn over other shirts. A combination of shirt and jacket.
shortalls noun. a pair of shorts with a bib or biblike piece to which shoulder straps are attached. A combination of short(s) and overalls.
Entertainment
cozy adjective. relating to a genre of mystery stories with little suspense, explicit violence, or sexual content, often also having amateur sleuths and idyllic, intimate settings. In this context, cozy is also sometimes used as a noun to refer to such a story itself, as in I started out reading cozies and moved on to the hard-boiled detective novels.
Bechdel test noun. a test of gender stereotyping and inequality in fiction, having a number of variations and used especially with movies, based on whether the work includes at least two fairly important female characters who talk to each other about something besides a man. The first recorded uses of the term Bechdel test come from between 2005 and 2010, but the concept was introduced by cartoonist Alison Bechdel in a 1985 comic strip.
Sports
Tommy John surgery noun. an operation to repair a torn ligament on the inner side of the elbow by replacing it with a tendon from elsewhere in the body or from a donor. Common among baseball players, the surgery gets its name from pitcher Tommy John, on whom the procedure was first performed in 1974. It is formally called ulnar collateral ligament reconstruction.
turf toe noun. a sprain at the joint between the metatarsus and the phalanx of the big toe, caused when the ligament connecting them under the toe is overextended: typically a sports-related injury, originally associated especially with artificial grass surfaces.
capped adjective. Chiefly British. (of a player) selected as part of a representative team. Example: When she plays her next match for England, she’ll become the most capped player of all time. Other newly added senses of capped include meanings related to loans, stocks, and landfills.
beer league noun. a community sports league, such as for hockey, softball, or soccer, whose members are amateurs of diverse ages and walks of life and play purely for the fun and socializing involved: games are usually accompanied or followed by alcohol and food
Family & relationships
girl mom noun. a mother of a daughter or daughters, especially one with only a daughter or daughters.
girl dad noun. a father of a daughter or daughters, especially one with only a daughter or daughters.
boy mom noun. a mother of a son or sons, especially one with only a son or sons.
boy dad noun. a father of a son or sons, especially one with only a son or sons. These proud terms are used informally to identify as a certain type of parent—you’re likely to encounter these phrases on T-shirts or as hashtags, for example.
squish noun. an intense feeling of infatuation that is not romantic or sexual in nature; a platonic crush. This term is also used in an entirely unrelated way in the context of U.S. politics as a derogatory term for a politician, especially a Republican, who is perceived by members of their own party as overly moderate or willing to compromise.
Health & wellness
sound bath noun. an instance of sustained listening to the pleasant sounds emanating from a collection of singing bowls, bells, chimes, etc., used to aid in relaxation or meditation and believed to help restore physical and mental wellness.
VO2 max noun. the maximum volume (V) of oxygen (O2) that a particular person’s body can absorb and use during intense exercise, measured in milliliters of oxygen per kilogram of body weight per minute and often used to assess cardiorespiratory fitness.
high-intensity interval training noun. a type of interval training for physical conditioning and fitness that uses short bursts of very intense exertion, alternating with short periods of rest or lighter exertion, to exploit the body’s systems for generating anaerobic energy. Commonly abbreviated as HIIT.
Tabata noun. an exercise or fitness program involving repeated alternation between usually 20-second bursts of strenuous exertion and 10-second periods of rest, totaling four minutes for an entire round. Named after Japanese professor Izumi Tabata, who created the program.
keto flu noun. a temporary feeling of illness or physical unease often experienced by those starting a ketogenic diet, characterized by fatigue, headaches, muscle soreness, etc., as the body adapts to using fat instead of carbohydrates for fuel. Also called carb flu.
micellar water noun. a liquid skin cleanser made up of tiny particles, or micelles, of mild soap or detergent dispersed in purified water, usually with the addition of moisturizers, vitamins, etc.
prebiotic noun. a substance containing dietary fiber that stimulates the growth or activity of beneficial bacteria in the gastrointestinal tract.
Food & drink
bottarga noun. the roe sac of a fish, especially the gray mullet, prepared by salting, pressing, and drying, and served in various ways, including as a grated garnish, on its own with seasoning, or with vegetables. Dining out pro tip: Use Dictionary.com as a menu companion for all those unfamiliar dish components.
soju noun. a colorless, clear, distilled alcoholic beverage from Korea, often made from a mixture of rice and other starches such as sweet potatoes, wheat, barley, tapioca, etc. The word soju comes from Korean, from a combination of so, “to burn, roast,” and ju, “alcoholic beverage.”
natto noun. Japanese cooking. a dish of fermented cooked soybeans, often eaten for breakfast over white rice or with toppings such as soy sauce and mustard.
Economics & finance
greedflation noun. a rise in prices, rents, or the like, that is not due to market pressure or any other factor organic to the economy, but is caused by corporate executives or boards of directors, property owners, etc., solely to increase profits that are already healthy or excessive. The verb form is greedflate. Other recently added inflation words include shrinkflation and shadow inflation.

dry powder noun. cash reserves, liquid assets, or easily liquidated assets such as readily saleable stocks and bonds, held by a corporation or an individual in order to cover current or future obligations, make new purchases, or take advantage of unforeseen opportunities.
bag holder noun. someone who retains an unprofitable investment rather than selling it at a loss, only to suffer an even worse loss when the investment eventually becomes worthless.
Climate, weather, & environment
climate breakdown noun. the collective effects of harmful and potentially irreversible trends in climate, specifically those resulting from unchecked global warming.
global boiling noun. a nonscientific term used to emphasize the trend toward and severity of extreme heat events, especially in regard to public health. Climate breakdown and global boiling have emerged as terms intended to communicate the severity of the effects of climate change, along with other prominent terms like climate crisis and climate emergency.
extreme heat event noun. Meteorology, Climatology. a heat event classified as being excessive enough to pose a serious threat to public health.
fire whirl noun. a tornadolike phenomenon created when turbulent air rapidly rising from the site of burning, as in a forest fire, sucks flaming gases, embers, and other fiery debris up into a twisting column, sometimes hundreds of feet in height.
fire tornado noun. a flaming tornado generated by intense wildfire, rarer, much larger, and more destructive than a fire whirl.
superfog noun. a combination of fog generated by weather conditions and wildfire smoke from damp, smoldering brush, leaves, trees, and other organic materials that often reduces visibility to less than 10 feet.
carbon market noun. a commodity trading system through which countries and organizations can buy and sell permits to produce a set amount of carbon dioxide emissions and other atmospheric pollutants. This term is just one example of how the word carbon has become shorthand for “carbon dioxide emissions.”
Social issues
intimate partner violence noun. acts of violence or abuse within a romantic relationship.
supervised injection site noun. a medically supervised facility at which people can inject illicit drugs they have brought with them, a practice intended to reduce overdoses, disease transmission, and other health problems associated with illicit drug use.
food insecure adjective. having or characterized by limited or uncertain access to adequate food. This is an adjective version of the more established noun form, food insecurity.
energy poverty noun. a lack of adequate access to safe, affordable sources of electricity or fuel for warmth, light, cooking, etc.
Even more words
Uluru noun. a large, isolated mass of red rock in central Australia, in southwestern Northern Territory: a sacred site for the Anangu people indigenous to the region, and a popular tourist attraction. 1,142 feet (348 meters) high. Also called Ayers Rock.
worlding noun. the act or process of bringing a people, culture, nation, etc., into a global sphere of influence, especially the sphere thought of as dominated by Western countries. The concept of worlding, influenced by literary theorist Gayatri Spivak, has become popular in academic discussions about colonialism.
Scouser noun. Informal. a resident or native of Liverpool, England. This other nickname for Liverpudlians comes from the word Scouse, a name for the Liverpool dialect. The word Scouse itself comes from a shortening of lobscouse, a type of sailor’s stew made of meat, vegetables, and hardtack.
fakeness noun. artificial, false, or insincere behavior, speech, etc.; pretense. More generally, fakeness is also used to mean “the quality or condition of being false, artificial, or insincere.”
kennel cough noun. a highly contagious but usually mild respiratory infection in dogs, characterized by a dry hacking or gagging cough and caused by a number of bacteria and viruses.
boobne noun. Informal. pimples or a rash in the area of the breasts or on the upper back, caused by a bra that chafes, is not clean, or is made of material that is allergenic or not breathable. Other acne blend words include bacne and maskne.
circular fashion
noun. a type of sustainable fashion that promotes minimal manufacturing through the ongoing reuse of garments and accessories or their components.
Rising Child Gun Deaths in US Outpace Research Funding; NC S.A.F.E. Focuses on Protection

Rising pediatric firearm mortality rates, decades of inaction on research, and a hopeful program in NC
(CNN Health, Deidre McPhillips with NC Pediatric Society, NC S.A.F.E, and NCDHHS) -- More children die from guns than anything else in the United States, but relatively little funding is available to study how to prevent these tragedies.
From 2008 to 2017, about $12 million in federal research awards were granted to study pediatric firearm mortality each year – about $600 per life lost, according to a study published in Health Affairs. Motor vehicle crashes, the leading cause of death among children at the time, received about $26,000 of research funding per death, while funding to study pediatric cancer, the third leading cause of death, topped $195,000 per death.
By 2020, firearm deaths in the US had reached record levels and guns had surpassed car crashes to become the leading cause of death among children. More than 4,300 children and teens died from guns in 2020, according to data from the US Centers for Disease Control and Prevention – a 27% jump from 2017, and a number that has only continued to rise. But federal dollars haven’t followed proportionately.
Congress has earmarked about $25 million for firearm injury prevention research each year since 2020, split evenly between the CDC and the National Institutes of Health. Even if all of those dollars were spent on studies focused on pediatric deaths from firearm injury, it’d still be less than $6,000 per death.
Decades of stalled progress
When the Parkland school shooting happened in 2018, more than two decades had passed since Congress had dedicated federal funding to research firearm injury prevention. A legislative provision enacted in 1996, known as the Dickey Amendment, specifically prohibits the use of federal funds to advocate or promote gun control, but it had a chilling effect on firearm injury research overall.
In March 2018, a month after Parkland, Congress included a report on the Dickey Amendment in a spending bill, clarifying that it does not prohibit research on the root causes of gun violence. But it wasn’t until 2020 that the budget actually included money specifically for this purpose.
In the nearly quarter century that it took to unwind uncertainties in the interpretation of the provision – a period of time that included Columbine, Sandy Hook and many more deadly shootings – guns killed 789,000 people in the US, including 75,000 children and teens.
After decades of stalled progress, new research shows that the recent bump in federal funding – incommensurate, as it may be – aligns with a rise in all kinds of related work.
From 2020 to 2022, there were about 90% more registered clinical trials and publications related to firearm injury prevention research than there were from 2017 to 2019, according to a research letter published Wednesday in JAMA Surgery. About half were funded and half were unfunded.
For Dr. Megan Ranney, dean of the Yale School of Public Health, progress in the field of firearm injury research is a “dance between hope and frustration.” Ranney, who is also an emergency physician, was involved in both the new research and the earlier study analyzing the federal dollars invested into the leading causes of death among children.
“We know that the $25 million that has been appropriated to NIH and CDC is a drop in the bucket compared to the magnitude of the problem, and compared to the funds that are put into other similar diseases and injuries,” she said. “But nonetheless, it was worth saying, ‘Did this investment make a difference?’ And I was actually quite heartened in the analysis to see this huge correlation between federal funding and the number of publications and studies being initiated.”
Federally-funded research is the gold standard
Federal funding helps destigmatize work on a topic, experts say.
Many researchers who focus their work on firearm injury said they were consistently advised by mentors, colleagues and others to pick a different field of study – as recently as a few years ago.
“As I was just starting out as a researcher, I was advised to steer my research towards areas that will have consistent funding in order to be able to launch a career that is sustainable. The risk is that there will be so many stops and starts to this kind of work until there can be a consistent funding stream,” said Dr. Jennifer Hoffmann, an emergency physician at Lurie Children’s Hospital of Chicago and an assistant professor at Northwestern University.
“It’s a really hard area to start investing a research career, and we’ve lost a whole generation of researchers. We need to start from scratch and entirely rebuild the research workforce.”
Backing from the CDC and NIH also helps validate the strength of the research, thanks to the rigorous project selection process and peer-review system for findings. The extra dollar amounts also allow for researchers to be more ambitious with their work.
In 2019, a group of researchers published a special report in JAMA Pediatrics outlining dozens of urgent research questions to guide a research agenda to better understand firearm injury prevention as a “critical step for reducing pediatric mortality.”
Without federal funding, researchers have done their best to cobble together the public data that is available to start to answer these questions – many without dedicated time or pay for the work.
The CDC’s National Violent Death Reporting System has been an important source, for example. The agency has a separate stream of funding for the dataset, which tracks some specific details about gun deaths, but significant gaps remain.
“The questions that we’re asking and answering are important but they’re just kind of the tip of the iceberg,” Ranney said. “I wish we could go faster and farther.”
In 2020, the CDC was able to fund 16 awards to study firearm injuries with the $12.5 million allocation from Congress.
“Everybody has realized that firearms are a leading mechanism for violent deaths, that has never been questioned. I think what has been harder to say is what can we do about it,” said Dr. Debra Houry, CDC’s chief medical officer.
People haven’t always viewed firearm violence or suicides as preventable, she said. The same perceptions were true for motor vehicle crashes, until research built the scientific evidence to show otherwise – and the hope is that the investments in research offer solutions and help shift perceptions around gun deaths, too.
Political views around firearms have also affected research funding, but preventing firearm injuries and deaths doesn’t have to infringe upon legal firearm ownership, experts say.
“We talk to a lot of people about how to keep their kids safe around pools. We don’t tell them they can’t own a pool,” said Dr. Patrick Carter, an associate professor at the University of Michigan and co-director of the university’s Institute for Firearm Injury Prevention. “Same thing is true of cars. Same thing is true of medications.”
But reducing deaths from car crashes, for example, required looking at the problem from lots of different angles – including seatbelts, airbags, changing driver behavior around drinking and driving, building safer roads – and the same approach will be needed for firearm deaths, he said. But the field is far from that point right now.
“Building that capacity is really critical to moving the needle and reversing the trends that we’re seeing,” Carter said. “It can’t be 12 people around the country doing (full time) research, it really has to be many more than that.”
Good research also takes time. Some of the researchers that the CDC funded in 2020 are just starting to release findings, including a new study from January with early data showing that systems that let schoolchildren report anonymous tips help prevent school shootings and suicides.
Consistent investment is critical to consistent progress, experts say.
“If there isn’t continued funding (from Congress), that research would stop midway. Continued funding will continue to support this work. Increased funding would allow us to find even more competitive applications because there’s been such interest in this,” CDC’s Houry said. “So we will do the best with whatever budget we have. But certainly, if there aren’t dollars for this, we will not be able to continue this work and some of it will stop immediately.”
The North Carolina Department of Health and Human Services is working to improve rates in NC
It only takes a moment for a tragedy to happen. Fortunately, it only takes a moment to help prevent one as well. Protect kids and communities by safely securing your firearms. Too many guns are falling into the wrong hands. Firearms are now the leading cause of injury-related death for children and youth in the state, and gun thefts are on the rise. If you own a firearm, make sure it’s safely secured.
NCDHHS has introduced the NC S.A.F.E. program to teach gun owners how to keep their firearm safely secured. Click here to learn more: SAFE STORAGE 101.
State Health Director, R. Betsey Tilson says "Launching of the firearm safe storage campaign (was) one of the recommended policies in the white paper. This is an area of general consensus around addressing firearm violence. Areas that require safe storage report a drop in unintentional deaths related to firearms of up to 59% and an estimated 32% of youth firearm suicides and unintentional firearm deaths could be prevented through safe storage. 20% of all car break-ins committed by juveniles last year were for the purpose of stealing a firearm. This is double the rate from just three years earlier."

The North Carolina Pediatric Society has made safe storage a priority, including a presentation from Dr. Rebecca Palmer at a recent meeting. Palmer presented strategies for counseling about safe storage including offering gun locks without preview questions. NCDJJDP Dept. Secretary William Lassiter brought 500 gun locks to distribute and noted their website had videos on how to use gun locks, and that the gun locks were very simple to install. Display gun locks were available on the registration table outside the meeting room. A family happened to walk by the table, and the child was looking at the locks, picked one up and asked “what’s that?” NCPEDS President Dr. Kenya McNeal-Trice was there, told the family they were gun locks and asked “Do y’all need any?” The grandfather with the family said he had three guns at home but only one lock. Dr. KMT said, “Then it sounds like you need two more, please take two!” The father replied, “they look complicated.” Dr. KMT said that she had just been learning about how simple they are to use and encouraged the grandfather to practice becoming comfortable stating, “if you could handle a gun, you could definitely handle a gun lock.” The family took two gun locks! The entire encounter took about 30 seconds and the family was very appreciative!
Additional Reading
NCDHHS White Paper on public health approach
NCMS CPP Elevates Healthcare in Dare County and Neighboring Counties Through New Preceptor Hub

NCMS Preceptor Hub is partnership with Manteo Community Health Center in Manteo, Engelhard, and Ocracoke (photo: The Coastland Times)
Improved Healthcare Coming to Dare County
The North Carolina Medical Society (NCMS) in conjunction with the Town of Manteo Healthcare Task Force is happy to announce the formation of a Preceptor Hub in Dare County. Initially, the Hub will be a partnership between the Manteo Community Health Center in Manteo, Engelhard, and Ocracoke, the town of Manteo, and the NCMS. Additional medical practices with preceptors will be added in the future. UNC-Chapel Hill, Campbell University, Elon University, and Wake Forest University will send students to the Hub.
A Preceptor Hub is a community of experienced medical practitioners who supervise medical students, providing training and clinical education. They provide the experiential part of the curriculum by helping student physicians gain clinical medical knowledge by caring for real patients.
The Preceptor Hub in Dare County comes after Outer Banks Medical Group told more than 2,400 patients that it would no longer provide services due to practitioner retirements, resignations or temporary providers not renewing their contracts.
NCMS Vice President Franklin Walker has been instrumental in the formation of the hub, working for more than two years to bring help to the people of Dare County.
Walker says, “The North Carolina Medical Society takes its commitment to the health of North Carolinians very seriously. This Preceptor Hub is a chance for us to bring our expertise and experience to a part of the state that needs quality healthcare. Through our Community Practitioner Program (CPP), we place physicians and PAs in underserved areas and improve access to care. We are very excited to help the people of Dare County.”

NCMS CEO Chip Baggett is also excited about what NCMS is doing for the area. "For over two years, Franklin Walker and the CPP team have dedicated their efforts to enhancing healthcare in Dare and its neighboring counties. The establishment of this Preceptor Hub reflects the commitment of NCMS to always lead toward improved healthcare for North Carolinians. We take pride in our robust partnerships with Manteo Community Health Center and the Town of Manteo Healthcare Task Force. We are also excitedly anticipating the arrival of students from UNC-Chapel Hill, Campbell University, Elon, and Wake Forest, the NCMS to see their contributions to assist the residents of this region."

Joe Rockenstein, CEO of Manteo Community Health Center adds, “We must preserve the future of healthcare by embracing the precepting of the present. With this program, we hope to do that for all the communities we serve in eastern North Carolina.”
Town of Manteo Healthcare Task Force Chairman Malcolm Fearing stated, “Nearly two years ago, our community was in a state of crisis because we had thousands of community members who lost their access to healthcare. We cast a wide net looking for resources to assist our community. Mr. Walker and the North Carolina Medical Society Foundation have been alongside us in the trenches helping to find sustainable solutions to build our provider network for patient care. This preceptorship program will allow students to hone their skills here on the Outer Banks. We are confident that we will prove to them that we all know this is an amazing place to live, work, and raise a family. We are tremendously grateful to have this kind of program coming to Dare County.”
NCMS Community Practitioner Program is helping underserved communities across the state. If you have questions about a Preceptor Hub in your area, please contact Franklin Walker at [email protected].
Some photos from today's meeting:
NCMS Past President Dr. Arthur Apolinario Featured in AMA Medicare Ad as AMA Advocacy Conference Begins
Dr. Arthur Apolinario Joins AMA Campaign to Fix Medicare
 Former North Carolina Medical Society President Dr. Arthur Apolinario adds his voice to the fight to fix the Medicare payment system in a new ad.
Former North Carolina Medical Society President Dr. Arthur Apolinario adds his voice to the fight to fix the Medicare payment system in a new ad.
In the advertisement currently running on social media, Apolinario says, "You have all the physicians of the United States speaking as one voice and making sure the message gets heard."
The American Medical Association National Advocacy Conference is currently underway in Washington, DC. One of the top agenda items is pushing Congress to pass legislation to reverse the 3.37 percent Medicare physician payment cuts that took effect on January 1, 2024. The AMA says failure to reverse the cuts will be harmful to the continued viability of physician practices and their ability to care for patients.
The NCMS currently has several members at the conference including NCMS Vice President of External Affairs Alan Skipper, NCMS President Dr. Eileen Raynor, NCMS Board of Directors member Dr. Karen Smith, and NCMS AMA Delegate Dr. Mary Ann Contogiannis.
To see Dr. Apolinario's ad click here.
Here is the list of the North Carolina Medical Society AMA Delegates:
NCMS CEO Chip Baggett Gives Advocacy Update to NC Chapter of American College of Physicians

Chip Baggett Addresses American College of Physicians
RALEIGH -- The North Carolina Medical Society CEO Chip Baggett addressed the North Carolina Chapter of the American College of Physicians (ACP) Friday in Raleigh. His advocacy update focused on making it easier for physicians to care for patients, making sure physicians have a choice of where and how to practice, and a strong commitment by NCMS to physician wellness.
Key initiatives of the NCMS
- Passage of Prior Authorization/Utilization Management reform legislation currently being considered by the North Carolina General Assembly and the United States Congress.
- Creation of a single, unified credentialing process recognized by government and commercial payers, hospitals, and licensing boards.
- Advocacy for streamlined licensure and renewal process at the North Carolina Medical Board that includes renewal every two years instead of annually.
- Obtaining a Medicaid and Medicare Physician Fee Schedule rate update to adjust for inflation.
- Recruitment of a minimum of 40 new physicians, PAs, and other healthcare team members through the NCMS Community Practitioner Program.
- A Task Force on practice employment issues and structural improvements.
- Improve daily lives of NCMS members through the North Carolina Clinician and Physician Retention and Wellbeing Consortium.
- Recruit 16 practice partnerships to send participants to the NCMS Kanof Institute for Physician Leadership for next 5 years.
- Identify sustainable funding for NCMS Future Clinician Leaders College.
Other highlights of the event include MOC credits, the Residents and Students Poster Competition, special interest roundtables, and the presentation of the 2024 Laureate and Volunteerism Awards.
The ACP event also included NCMS members Marion M. McCrary, MD, FACP and Lawrence Greenblatt, MD, FACP.
Here is the full list of speakers:
- Noel Ivey, MD, FACP
- Michelle E. Perkons, MD
- Denise Pong, MD, MPH
- Former NCMS BOD Member Fatima Syed, MD, MSc, FACP
- Diana B. McNeill, MD, MACP
- J. Bryan Sexton, PhD
- John V. Duronville, MD
- Rebecca Lumsden, MD MS
- Kevin L. Thomas, MD
- Bruce T. Peyser, MD
- Liza I. Genao, MD
- Aatif M. Husain, MD
- Mehri S. McKellar, MD
- Mithu Maheswaranathan, MD
- NCMS PAC Investor Suchita Shah Sata, MD, FACP, SFHM
- David P. Boyte, MD, MBA
- Ruchi S. Doshi, MD, MPH
- Katherine N. Neal, MD
- Bruce T. Peyser, MD, FACP
- Poonam Sharma, MD, SFHM
- Girish Kalra, MD
- Christopher D. Fink, DO
- Neha Kayastha, MD
- William S. Yancy, Jr., MD, MHS
- Christopher A. Jones, MD, FAAHPM, MBA
Chief Resident Presentations:
- Kathryn M. Langley, MD (UNC)
- Alyssa MacKay, DO (Atrium Health)
- Elaina K. Furr, DO (MAHEC)
- Vasili Katsadouros, DO (Cone)
- Joshua Walters, MD (ECU)
- Ashley Bird-Humrickhouse, DO (NHRMC)
- Nathan A. Hirshman, MD (Duke)
- Zachary Pruitt, MD (WFU)
- Randall Reagan, DO (UNC Blue Ridge)

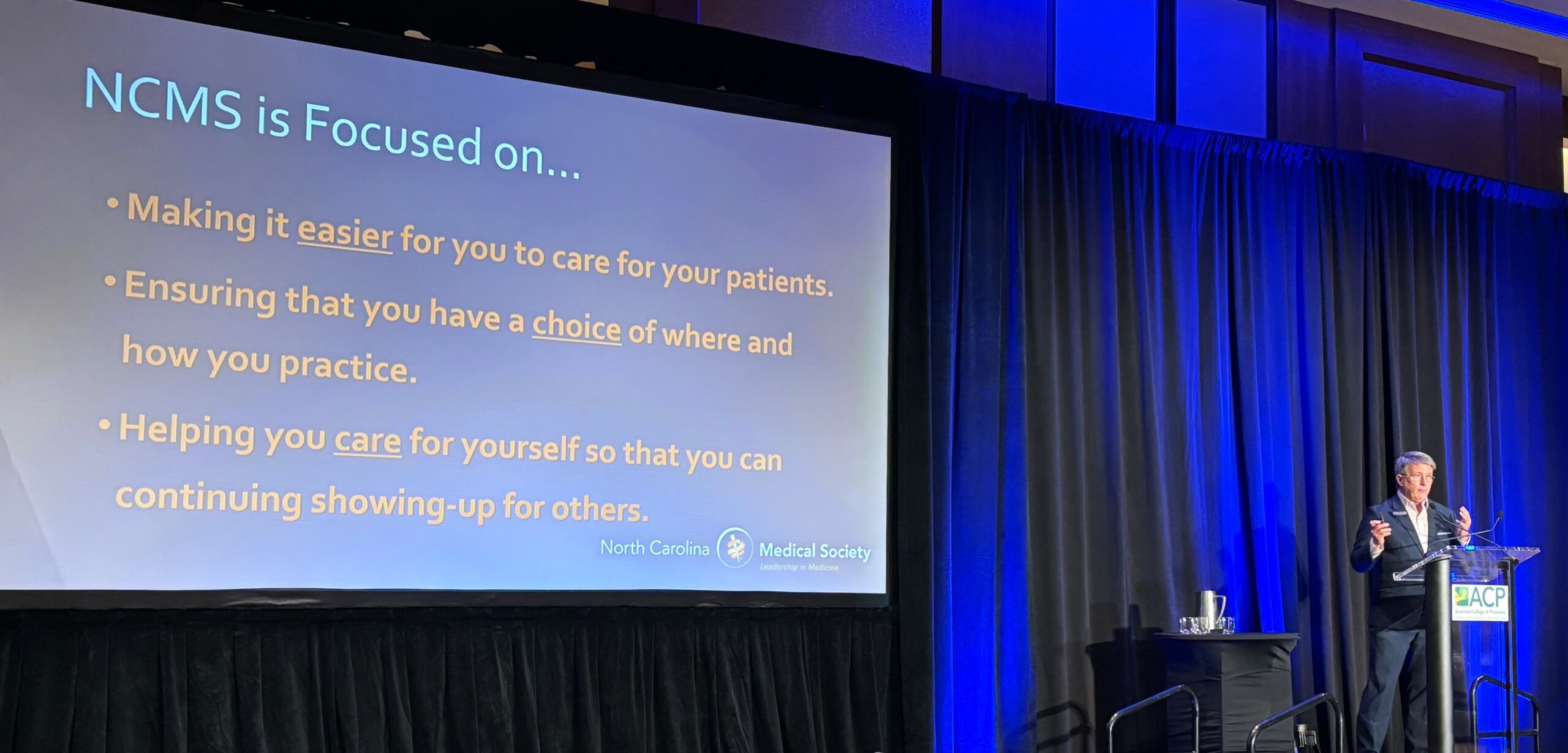


CDC: Syphilis cases at highest levels since 1950s
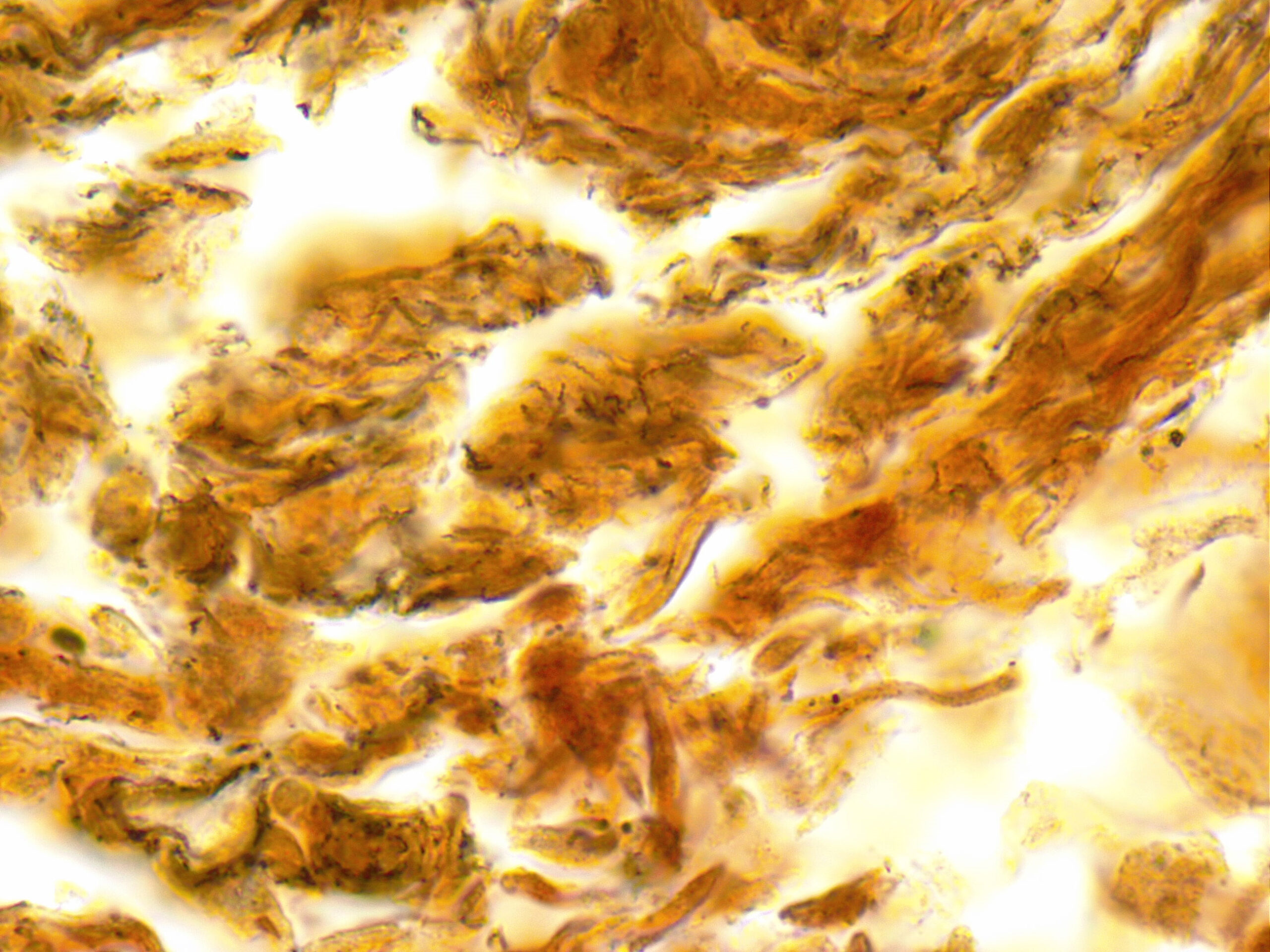
Racial and Ethnic Minorities Disproportionately Affected
The number of syphilis cases in the U.S. are on the rise. According to a new report from the Centers for Disease Control and Prevention, cases increased by nearly 80% to more than 207,000 between 2018 and 2022.
Rates increased among all age groups, including newborns, and in all regions of the country. In 2022, 3,755 cases of babies born with syphilis in the U.S. were reported, which reflects an alarming 937% increase in the past decade, the CDC said.
The report continued that racial and ethnic minorities are most disproportionately affected due to "long standing social inequities that often lead to health inequalities."
Experts point to various reasons for the increase, including increases in substance abuse tied to risky sexual behavior, decrease in condom use, ongoing social and economic conditions and reduction in sexually transmitted infections (STI) services at the state and local level.
"Because STIs often do not show symptoms, and screening is necessary for timely diagnosis and treatment, changes in access to sexual health care can affect the number of infections diagnosed and reported," the CDC said.
The stigma surrounding STIs can also keep people from seeking care, and "buries the truth that all people deserve quality sexual health care," said Laura Bachmann, acting director of the CDC's Division of STD Prevention, in an interview with NPR. "It also can cause issues at the provider level when it comes to talking with people about these issues."
The CDC said that its findings signal an urgent need for a closer look at public health efforts and prevention strategies.
"Some people face tremendous barriers to STI prevention and health services," said Bachmann in a statement. "So, the most important work is often outside the clinic, whether it be reaching out to communities with testing, interviewing patients to offer services to their partners, or delivering treatment directly to someone."
She added that there is still a need for more innovation around diagnosis, treatment and prevention.
"In the United States, syphilis was close to elimination in the 1990s, so we know it's possible to reverse this epidemic," said Jonathan Mermin, director of CDC's National Center for HIV, Viral Hepatitis, STD, and TB Prevention, in a statement. "I have hope for innovative prevention tools – such as a pill after sex that prevents STIs, and better tests for syphilis – but they will only be successful if they reach the people who will benefit. And that is going to require coordinated and sustained efforts at the federal, state, and local levels."
The U.S Department of Health and Human Services is also continuing to address the issue through the establishment of a federal task force last year.
"Addressing the resurgence of syphilis and congenital syphilis requires a concerted effort," said Admiral Rachel Levine, assistant secretary for health and chair of the National Syphilis and Congenital Syphilis Syndemic Federal Task Force, in a statement. "We can collectively work towards reducing the incidence of syphilis and its devastating consequences, and we will turn the tide on the syphilis epidemic."
Without the appropriate funding however, it's difficult for communities to follow through with the recommendations by government officials, said Elizabeth Finley, director of communications at the National Coalition of STD Directors.
Over the past year, there has been a shortage of Bicillin, an antibiotic used to treat syphilis. In addition, last year states lost funding for STD prevention, affecting their ability to respond to syphilis.
"The 2022 data is devastating to see, but it's already a year old," said Finley. As a result, she said that "we have every reason to believe that the 2023 numbers will be much worse."
The CDC report also included data on other sexually transmitted infections, stating that "reported gonorrhea cases declined for the first time in at least a decade while reported chlamydia cases were level."
There were more than 2.5 million cases of syphilis, gonorrhea, and chlamydia reported in the U.S. in 2022 alone.
Without treatment, syphilis can cause serious health problems including damage to the heart and brain, and can cause blindness, deafness and paralysis. If transmitted during pregnancy, it can cause miscarriage, infant death and lifelong medical issues. With the right antibiotics, the STI is curable.
Additional Reading:
Syphilis Among Newborns Continues to Rise
Does Morning After Pill for STI Work?
Old Drug Offers New Stop for STI
The Most Important Part of Super Bowl LVIII? The Commercials! Here Are All The Ones Already Released
Super Bowl LVIII will air on CBS this year, and stream live on Paramount+
Yes, we are all excited to see the San Francisco 49ers and the Kansas City Chiefs on Sunday. Yes, we are all excited to see Usher perform the halftime show, Yes, we are all wondering if Taylor Swift will be there. But, really aren't we all just watching for the ads?
Well, the NCMS is here to help! Here is a look at all of the 2024 Super Bowl commercials released so far!
2024 Super Bowl commercials (so far)!
Advertisers take the Super Bowl very seriously. They know around 1/3 of all Americans watch, and ads can go for millions of dollars. Because of that, advertisers often go all out, lining up celebrity-filled TV spots designed to raise interest in their products.
Paramount Plus Super Bowl commercial
What do Miami Dolphins quarterback Tua Tagovailoa, Patrick Stewart, Drew Barrymore, Arnold from "Hey Arnold" and Peppa Pig all have in common? They're all in the Paramount streaming service's new Super Bowl ad.
In the TV spot, the assorted characters are trapped on an icy glacier, unable to throw a rope to safety. When Tagovailoa says he could make the throw to the top, if there was a football.
Patrick Stewart suggests they use Arnold's football-shaped head to throw the rope all the way.
"We throw the child," the legendary actor plainly states. Despite reservations from some of his fellow stranded explorers, Stewart gets into some old-timey football gear and throws a perfect spiral — straight into the wall...as Creed sings "Higher."
Lamenting his inability to throw just a few feet higher, Stewart out wishes for some "pigskin" to toss. The commercial ends with a pan to Peppa Pig, potentially their last hope to avoid freezing to death.
While a condensed version is likely to be played at the Super Bowl because even a 30-second ad can cost millions of dollars, the full commercial clocks in just under two minutes.
Google's Super Bowl LVIII ad
Google's heartstring-pulling ad follows a blind man as he uses “Guided Frame” — Google's AI-powered accessibility feature for the Pixel camera that uses a combination of audio cues, high-contrast animations and tactile vibrations — to take pictures of the people and places in his life.
M&M Super Bowl commercial with several NFL greats
Retired Miami Dolphins quarterback Dan Marino, Buffalo Bills’ Bruce Smith and wide receiver Terrell Owens never got a Super Bowl ring, but M&M’s and Scarlett Johansson present the “Almost Champions” ring to the almost winners.
“Almost Champions” ring to the almost winners.


OREO Super Bowl ad with Kris Jenner
In OREO's 30-second Super Bowl spot, the iconic chocolate sandwich cookie is imagined at big events throughout the past, helping people make important decisions that altered the course of history.
In ancient Troy, two guards decide to "twist on it" when a man shows up at their gate with the trojan horse -- cream on the right, they let him in. Whoops! We all know how that one turned out. An OREO also helps two UFO witnesses decide not to report their alien sighting.


Then in a flashback scene to pre-"Keeping Up with the Kardashians" days, Kris Jenner, matriarch of the Kardashian empire and long-time OREO fan, is on the phone.
"So every little detail about our family will be on TV?" she asks. "Who would watch that?"
Jenner says she'll "twist on it" to decide, and pulls the cookie apart, and appears to decide to go for it. "Hope you can keep up," she says.
Booking.com Super Bowl ad with Tina Fey
Actress Tina Fey has so many choices on the online travel agency booking.com site she has to hire body doubles: an influencer type played by her 30 Rock co-star, Jane Krakowski, to stay at a fancy hotel, a bigfoot handled by another 30 Rock co-star, Jack McBrayer, to stay at a cabin, and even actress Glenn Close, who stays on a farm.
Doritos Super Bowl ad with Jenna Ortega
Two grandmotherly women ("Dina" and “Mita”) chase after “Top Gun: Maverick” actor Danny Ramirez, who took the last bag of Doritos Dinamita from a store shelf, leaving actress Jenna Ortega behind.


Mountain Dew Baja Blast Super Bowl commercial with Aubrey Plaza
Aubrey Plaza is always having a blast, whether she is stuck in an elevator or being abducted by aliens — or reuniting with her “Parks and Rec” co-star Nick Offerman while riding dragons.


Starry Super Bowl commercial with Ice Spice


"I just needed something more refreshing, more crisp," she says. After the rejection, the spurned soda/lover's head explodes in a fountain of clear soda.
Pringles Super Bowl commercial with Chris Pratt
The Pringles ad features Chris Pratt sporting the chip mascot's iconic mustache. Once a cashier notices and posts about the 'stache, the race is on, with more people commenting about his striking resemblance to the Pringles man.


By the end of the spot, Pratt has starred in a movie about the Pringles mascot, alongside a mustachioed child in a wagon on the prairie. It ends with the same clerk from the beginning of the clip asking "do I get a cut?" Pratt then offers her a tube of Pringles.
Dove Super Bowl LVIII commercial
Dove's ad begins seemingly whimsically showing young girls having mishaps playing sports to the tune of "It’s the Hard Knock Life."


But the ad cuts starkly to a girl looking self-consciously in the mirror. The message: low body-confidence leads to girls quitting sports, not the mishaps.
Budweiser 2024 Super Bowl ad
In Anheuser-Busch's nostalgic spot, a snowstorm threatens to derail a delivery of Budweiser to a small-town bar. But a team of Clydesdales and a Labrador retriever team up to help Budweiser make the delivery.


Experts say the feel-good spot strikes the right chord for Anheuser-Busch, which is trying to win back consumer sentiment following last year’s conservative backlash against Bud Light after the brand sent a commemorative can to transgender influencer Dylan Mulvaney. Bud Light also angered supporters of transgender rights who felt it abandoned Mulvaney.
Bud Light Super Bowl commercial with Post Malone
Speaking of Bud Light, they've also released their Super Bowl ad, aiming for some low-stakes chuckles with their commercial. In the newly-released spot, dubbed "Easy Night Out," a group of friends is hanging out in a garage. As one cracks open a Bud Light from the refrigerator, he unleashes the Bud Light Genie.


"Wishes? Yeah, it's my thing," the Bud Light Genie says. Want to be filthy rich? No problem! Need a sweet new set of wheels? How about a stretch DeLorean limo ride to the bar, where Bud Light magically replenishes itself at the tables. As the night gets crazier and the genie keeps granting wishes, NFL Hall of Famer Peyton Manning, Grammy nominee Post Malone and UFC CEO Dana White all make appearances.
T-Mobile Super Bowl spot with Jason Momoa
Jason Momoa shows off his singing chops in an ad that shows Scrubs duo Zach Braff and Donald Faison singing about T-Mobile home internet to the tune of “Flashdance ... What a Feeling." “Flashdance” star Jennifer Beals pops in to spray Momoa with water and ask him to sing it again — without his shirt.
Michelob ULTRA Super Bowl ad stars Lionel Messi and Ted Lasso star Jason Sudeikis
The Michelob commercial this year is pretty simple. While waiting for a beer at a beachside bar, Lionel Messi takes some time to have some fun with a soccer ball — namely dribbling circles around everybody else on the beach. It also features a brief cameo from "Ted Lasso" star Jason Sudeikis, who comments how the two of them "go way back."


At the end of the relaxingly low-key commercial, the bartender calls for the soccer icon to pick up his drink, and Messi kicks a goal into a volleyball net hanging between a pair of palm trees.
Hellmann's Super Bowl commercial
And a Hellmann's ad focusing on food waste starring Kate McKinnon features a cat that becomes a celebrity and dates Pete Davidson.


In the ad, McKinnon mistakes the cat's meow for the word "mayo," catapulting the "talking" cat to fame with a book deal, keynote speech and eventual red carpet moment with the former SNL cast member.
Kawasaki
A Kawasaki ad shows people riding in their Ridge “side by side” off-road vehicles growing mullets because the vehicle is “business in the front and a party in the back.”
The vehicle's ability to grow 80s hairstyles extends past the occupants, with a bald eagle and a tortoise also growing some luscious locks.
Uber Eats Super Bowl commercial with Jennifer Anniston, David Schwimmer, and David and Victoria Beckham
The ad for Uber Eats is all about being forgetful. From forgetting to put on pants in the morning to forgetting an old Friend, we all lose track of some things.
But the commercial, as it goes through the various forgetful scenarios, reminds watchers to always remember one thing: Uber Eats, because the delivery app has more than just food. You can get office supplies, flowers or beauty products through the app.
And isn't that worth forgetting something else to make room for?
DoorDash
The food delivery app's commercial is simple: they're offering to deliver everything (and yes, we mean everything) being advertised by the other ads during the big game, for free, to one lucky person.
In a teaser, DoorDash says they'll give out a promo code during their game-day ad, which can be redeemed here for a shot to win.
That means everything from Doritos to a new car to tax services. In fact, DoorDash doesn't know everything they're giving away for this promotion. "Who knows what else? We haven't fully thought this thing through," the teaser's narrator says.
Popeyes
Popeyes new it had to go big or go home for its first Super Bowl commercial.
The chicken chain's commercial, released on Feb. 6, features comedian and actor Ken Jeong trying Popeyes' new wings.
In the 60-second ad, Jeong is seen thawing out after he cryogenically froze himself in 1972. Jeong's character waited over 50 years for the "better" wing to be created.
Along with trying an array of Popeyes wings, Jeong goes on a venture to try all the things of the modern age: delivery drones, electric scooters, self-driving cars, robot vacuums and even goldendoodles.
Dunkin' Donuts
Ben Affleck and Dunkin' Donuts are a match made in heaven.
Affleck, who is the official brand ambassador for the coffee chain, returns for another Super Bowl ad this year.
In the minute-long teaser, Affleck is seen watching a news segment calling him the "boredest man in the world" as he sits beside his wife Jennifer Lopez.
The ad cuts to Affleck as he pursues his new dream of becoming a pop star. He's heading into studios, talking to producers and employing the help of TikTok star Charlie D'Amelio for some dance lessons.
Affleck is even seen pitching his "crazy" dream to JLO over the phone.
Latest Trends in Health Technology from 2024 Consumer Electronics Show
Healthcare’s Transformative Technologies at CES 2024
(Caroline Scott, Consumer Technology Association Contributing Editor) -- In recent years, and as was seen at CES 2024, the healthcare industry has benefited from a significant transformation furthered by the integration of digital technologies. The advent of digital technologies across the healthcare landscape has revolutionized the way we approach wellness, making
therapies and a wide range of other services more accessible, personalized and efficient. Promoting these advances, CTA continues to play a catalyzing role in helping industry players shape the future of healthcare through innovation and collaboration. Here’s a closer look at how CTA with CES – the world’s most powerful technology show owned and operated by CTA – have helped foster innovation in the interest of improved wellness and healthcare innovators across the U.S.
Digital Technologies and the Future of Healthcare
The digital health sector employs a wide range of technologies and applications designed to enhance healthcare delivery, improve patient outcomes and streamline medical processes. One of the key advantages of digital health is its ability to empower individuals to take control of their health and well-being. From wearable devices that monitor vital signs to mobile apps that provide real-time health insights, digital health technologies enable individuals to track and manage their health proactively.
Furthermore, digital health can break down traditional barriers to healthcare access. Telehealth, for example, allows individuals to consult with healthcare professionals remotely, eliminating geographical constraints and providing timely medical advice. This is particularly crucial in rural and underserved areas where access to healthcare services may be limited.
And for women, digital health tech is particularly promising as a leveler of imbalances in access to quality care. According to CTA’s most recent study, The Future of Women's Digital Health Solutions, two-thirds (66%) of U.S. women state that digital health solutions are the future of healthcare. Some 64% agree that digital health will aid in lowering healthcare cost. More than half (58%) say digital health solutions will reduce healthcare disparities. Our article, Assessing & Addressing the State of Women’s Healthcare, further explores underrepresentation and underfunding of research in healthcare for women. These are among the challenges digital health tech is countering, as was evidenced across the show floor. A rundown of this and other topics in digital health conference programming at CES 2024 is available on demand.
Healthcare Goes Where You Do with Digital Tech
Wearable medical devices extend beyond basic fitness tracking, offering features like continuous glucose monitoring, ECG monitoring and stress management. CES showcased innovative telehealth solutions designed to enhance the virtual healthcare experience. From immersive virtual reality consultations to remote patient monitoring, telehealth technologies are evolving to provide more comprehensive and engaging healthcare services.
The integration of digital therapeutics, increasingly in wearable and mobile formats, gained prominence at CES with the addition of apps and platforms that deliver evidence-based interventions for various medical conditions. These digital therapeutics aim to complement traditional treatments and improve patient outcomes.
CES 2024 featured breakthroughs in wearable and mobile health tech, and scores of startup products and services for improved wellbeing. The show also reprised the popular Digital Health Summit. Panel topics included health equity, innovations in mental health, women’s healthcare, generative AI and much more.
The Healthcare Network Effect at CES 2024
After a great success at CES 2023, the Digital Health Mixer returned in full force at CES 2024. The informal networking event brought diverse digital-health innovators together to exchange insights and ideas.
In 2023, the Digital Health Mixer attracted nearly 350 attendees. In 2024, the event drew more than 500 attendees. The networking at this venue has consistently fostered important collaborations among healthcare visionaries. It also has proved invaluable for facilitating seamless exchanges of critical information. These connections help continue the conversation long after the show’s close, year after year.
As we navigate the digital age, the importance of digital health tech cannot be overstated. The transformative impact of these technologies, coupled with the advocacy and support of innovative organizations and experts that align with CTA, is paving the way for a more connected, patient-centric healthcare landscape. CES 2024 served as a testament to the power and promise of digital health, offering a glimpse into a healthcare future that’s both technologically advanced and more completely human-centered.
It's not too soon to save the date for CES 2025, January 7-10, in Las Vegas. In the meantime, explore how CTA’s digital health team is working for business innovation and sample extensive on-demand content relevant to this critical topic. Stay tuned for more updates as our work continues in the interest of progress in digital health tech.
Additional Reading:
CES 2024 Sector Trends: Digital Health
Healthcare Leaders Share Takeaways from CES
NCMS Past President Dr. Philip Brown to Present at CARE Project Professional Collaborative

'Do You Speak Patient: TELL ME' by Dr. Philip Brown at CARE Collaborative
(WRIGHTSVILLE BEACH) -- Dr. Philip Brown is speaking at the 6th Annual CARE Project NC Parent Professional Collaborative. Brown is a Past President of the North Carolina Medical Society, former Chief Physician Executive at New Hanover Regional Medical Center, and Chief Community Impact Officer at Novant Health.
The CARE Project Executive Director Dr. Johnnie Sexton, Au.D. says, "Dr. Brown’s ability to bring simplicity out of chaos to help lead organizations and individuals to accountable action is particularly needed in today’s environment. We are inundated with facts and data points that can be and are spun to obscure truth, creating clarity requires both quantitative and qualitative information. His transformational leadership is effective because he is willing to listen, hear and understand diverse perspectives through connection and earned trust.
Click here to attend.
Flu Activity Picking Up Across Country, Including North Carolina

More than a third of all states are still experiencing high or very high levels of respiratory illness this season, according to the CDC.
Respiratory virus season in the US isn’t over yet
(CNN, Diedre McPhillips) -- After a few weeks of decline, some measures show that flu activity is starting to pick up again and respiratory virus levels remain high overall in the United States.
During the week ending January 27, more than 82,000 people who visited an emergency department were diagnosed with influenza, according to data from the US Centers for Disease Control and Prevention — an 8% bump, or about 6,000 more than the week before. The test positivity rate for flu also ticked up in the US overall.
A second surge of flu activity after the winter holidays is common, but experts say it’s notoriously difficult to predict exactly how long or how severe the full season will be. Sometimes this surge is the start of a full second wave, but it could also be a minor blip before a more consistent decrease, the CDC says.
A traditional second wave of influenza usually comes after a more significant downturn, when influenza B viruses start to overtake influenza A viruses that were predominantly circulating, said Alicia Budd, who leads domestic flu surveillance for the CDC.
There’s no evidence of that happening yet, but it’s too early to rule anything out, she said.
“We’re still at the midpoint of the season,” Budd said. “It’s too early to tell exactly where we are in our ultimate trajectory. We just don’t know yet. But we are still seeing a lot of activity right now.”
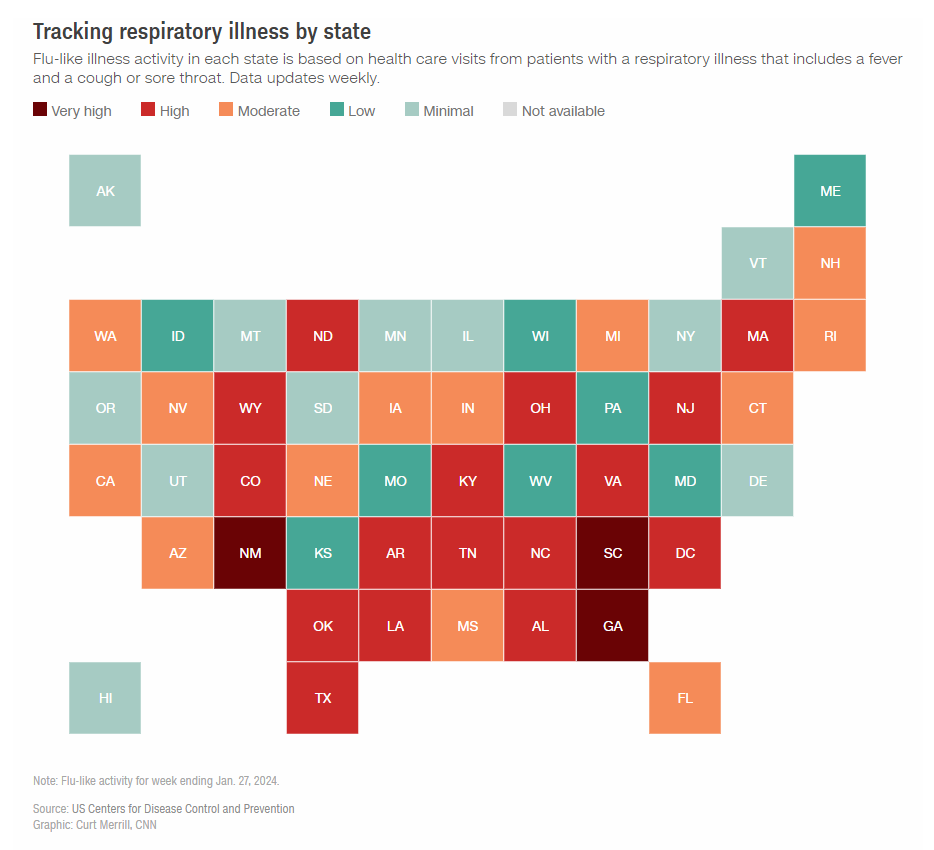
Covid-19 and RSV also continue to circulate at high levels. Emergency department visits for Covid-19 and RSV have been declining for a month, but there were still more than 50,000 emergency department visits and about 23,000 hospitalizations for Covid-19 during the week ending January 27, CDC data shows.
The downward trend for Covid-19 is coming as expected, and the peak for flu may be shifting a bit later this season, said Dr. Michael Mina, an epidemiologist and chief science officer of eMed, a telehealth company focused on at-home testing.
“It’s not so much that flu is now replacing Covid, it’s just like: Covid did its thing and now it’s coming down,” he said. “(Covid is) doing exactly the identical thing as it’s done, and in this case, we just have a flu season that shifted a little bit to the right. Flu shifts by orders of months actually from year to year. Covid is a little bit more consistent.”
While national trends are helpful, expert say that local trends are the best way to gauge risk and make decisions about how to stay safe and healthy.
Overall, 18 states and Washington, DC, are still experiencing high or very high levels of respiratory illness, according to the CDC. New data from the CDC’s Center for Forecasting Analytics suggests that flu infections are growing in four states — Florida, New York, Oklahoma and Texas — and likely growing in five others: Arkansas, Kentucky, Massachusetts, North Carolina and South Carolina. Wastewater surveillance suggests that Covid-19 levels are highest in the South, with forecasted case increases in South Carolina, in particular.
Experts say that trends in the US have stayed within expected ranges so far this respiratory virus season. But the burden of disease is still very high. The CDC estimates that there have been at least 20 million illnesses, 230,000 hospitalizations and 14,000 deaths from flu so far this season.
“It’s normal in terms of the amount of activity but it is a very, very high burden,” Budd said.
There is early data to suggest that the latest Covid-19 vaccine and this year’s flu shot offer strong protection this season, and experts say it’s still not too late to get vaccinated. They also urge the public to practice etiquette — hand washing, covering coughs and sneezes, staying home when sick — to avoid unnecessary spread.
“That’s how we can help each other,” Budd said.
NCMS Past President Dr. Palmer Edwards Appointed to NC Commission for Public Health

NCMS is Honored to Appoint Palmer Edwards, MD to the NC Commission for Public Health
(RALEIGH) -- The North Carolina Medical Society Nominating and Leadership Development Committee has appointed Dr. Palmer Edwards to the North Carolina Commission for Public Health. He fills the unexpired term of Douglas Sheets, MD. Edward's term will expire on November 30, 2027.
Edwards was born in Washington, NC and attended the University of North Carolina at Chapel Hill. He now lives in Winston-Salem with his wife Marty. Over the years, Edwards has served on various committees at the NCMS and been involved in the NCMS Foundation. He is currently a Foundation Trustee. He has been a member of the NCMS since 1992.
The Commission for Public Health is the public health rulemaking body for North Carolina. It is authorized and directed by the N.C. General Assembly to adopt rules to protect and promote the health of the public and to adopt rules necessary to implement public health programs administered by the Division of Public Health. The Commission was first established by the N.C. General Assembly in 1877 as the State Board of Health. It was renamed the Commission for Health Services in 1973 and became the Commission for Public Health in 2007. The Division of Public Health is staff to the Commission. The North Carolina General Assembly has invested the Commission for Public Health with statutory responsibilities to support the mission of the public health system, which is to promote and contribute to the highest level of health possible for the people of North Carolina.
Toby Keith and King Charles Bring Attention to Cancer in Men
How to help your patients when they receive a cancer diagnosis
With the announcement of the death of country music superstar Toby Keith from Stomach Cancer and the cancer diagnosis of Britain's King Charles, the spotlight is shining brightly on men's health. Men are less likely than women to address their health. A recent study by the Cleveland Clinic found that only 3 out of 5 men get annual physicals and 40 percent of men ONLY go to the doctor when they think they have a serious medical condition.
Piedmont Healthcare found that men with a cancer diagnosis are likely to isolate themselves and suppress their emotions.
How men process cancer
Whether dealing with their own cancer diagnosis or that of a loved one, it is common for men to:
- Think asking for support is a sign of weakness. "Men are less likely to seek support because we think we will be perceived as weak," notes Buttimer. "Actually, the opposite is true. It takes a lot of strength to ask for help."
- Believe emotions are reserved for women. As caregivers, men may be tempted to ignore their emotions so they can support their loved one.
- Isolate themselves."When dealing with emotional issues or challenges that scare them, men tend to be loners," explains Buttimer. "It is an instinct for men to want to go into their 'man cave' to figure things out. In our culture, many men believe they are supposed to go it alone and tough it out during trying times, including cancer."
- Try to fix the problem."Men are 'supposed' to fix it, whatever it is," he says. "We pressure ourselves to figure out a solution and if we can't, we may believe something is wrong with us."
In response to the myriad of ways people cope with a cancer diagnosis, the Mayo Clinic released these tips for your patients:
Cancer diagnosis: 11 tips for coping
Learning that you have cancer can be hard. Some people say they felt anxious, afraid or overwhelmed when they were first diagnosed. If you aren't sure what to do to cope, here are 11 ideas to help you deal with a cancer diagnosis.
Get the facts about your cancer diagnosis
Try to get as much basic, useful information as you can. This will help you to make decisions about your care.
Write down your questions and concerns. Bring them with you when you see your health care provider.
You may ask:
- What kind of cancer do I have?
- Where is the cancer?
- Has it spread?
- Can my cancer be treated?
- What is the chance that my cancer can be cured?
- What other tests or procedures do I need?
- What are my treatment options?
- How will the treatment benefit me?
- What can I expect during treatment?
- What are the side effects of the treatment?
- When should I call my health care provider?
- What can I do to prevent my cancer from coming back?
- How likely are my children or other family members to get cancer?
- What happens if I don't get treatment?
Consider bringing a family member or friend with you to your first few appointments. They can help you remember what you hear.
Think about how much you want to know about your cancer. Some people want all the facts and details. This helps them be part of the decision-making process. Others want to learn the basics and leave details and decisions to their health care providers. Think about which works best for you. Let your health care team know what you'd like.
Keep the lines of communication open
Have honest, two-way communication with your loved ones, health care providers and others. You may feel alone if people try to protect you from bad news by not talking about it. Or you might feel alone or less supported if you try to look strong and not share your feelings. If you and others show your real emotions, you can help support each other.
Anticipate possible physical changes
The best time to plan for changes to your body is right after your cancer diagnosis and before you begin treatment. Prepare yourself now so that you'll be able to deal with everything later.
Ask your health care provider what may change. Medicines may make you lose your hair. Advice from experts about clothing, makeup, wigs and hairpieces may help you feel more comfortable and attractive. Insurance often helps pay for wigs and other devices to help you adapt.
Also think about how treatment will affect your daily life. Ask your provider whether you will be able to continue your usual routine. You may need to spend time in the hospital or have many medical appointments. If your treatment will make it hard to perform your daily duties, make arrangements for this.
Plan ahead for your finances. Figure out who will do routine household chores. If you have pets, ask someone to take care of them.
Maintain a healthy lifestyle
A healthy lifestyle can improve your energy level. Choose a healthy diet. Get enough rest. These tips will help you manage the stress and fatigue of the cancer and its treatment.
If you can, have a consistent daily routine. Make time each day for exercising, getting enough sleep and eating meals.
Let friends and family help you
Your friends and family can run errands, take you to appointments, prepare meals and help you with household chores. This can give those who care about you a way to help during a difficult time.
Also urge your family to accept help if it's needed. A cancer diagnosis affects the entire family. It also adds stress, especially to the ones who take care of you. Accepting help with meals or chores from neighbors or friends can help your loved ones from feeling burned out.
Review your goals and priorities
Figure out what's really important in your life. Find time for the activities that are most important to you and give you the most meaning. Check your calendar and cancel activities that don't meet your goals.
Try to be open with your loved ones. Share your thoughts and feelings with them. Cancer affects all of your relationships. Communication can help lower the anxiety and fear that cancer can cause.
Try to maintain your lifestyle
Keep your lifestyle, but be open to changing it. Take one day at a time. It's easy to forget to do this during stressful times. When the future is not sure, organizing and planning may suddenly seem like too much work.
Consider how your diagnosis will impact your finances
Many unexpected financial issues can happen after a cancer diagnosis. Your treatment may require time away from work or home. Consider the costs of medicines, medical devices, traveling for treatment and parking fees at the hospital.
Many clinics and hospitals keep lists of resources to help you financially during and after your cancer treatment. Talk with your health care team about your options.
Questions to ask include:
- Will I have to take time away from work? If I do, what will happen with my benefits?
- Will my friends and family need to take time away from work to be with me?
- Will my insurance pay for these treatments?
- Will my insurance cover the cost of medicines?
- How much will I have to pay?
- If insurance won't pay for my treatment, are there programs that can help?
- Do I qualify for disability benefits?
- How does my diagnosis affect my life insurance?
- Who do I call to talk about what my insurance will cover?
Talk to other people with cancer
It can be hard for people who have not had cancer to understand how you're feeling. It may help to talk to people who have been in your situation. Other cancer survivors can share their experiences. They can tell you what to expect during treatment.
Talk to a friend or family member who has had cancer. Or connect with other cancer survivors through support groups. Ask your health care provider about support groups in your area. You can contact your local chapter of the American Cancer Society. Online message boards also bring cancer survivors together. Start with the American Cancer Society's Cancer Survivors Network.
Fight stigmas
Some old stigmas about cancer still exist. Your friends may wonder if your cancer is contagious. Co-workers may doubt you're healthy enough to do your job. Some may avoid you because they're afraid to say the wrong thing. Many people will have questions and concerns.
Determine how you'll deal with others. In general, others will follow what you do. Remind friends that cancer shouldn't make them afraid to be around you.
Develop your own ways to deal with cancer
Just as each person's cancer treatment is different, so are the ways of dealing with cancer. Ideas to try:
- Practice ways to relax.
- Share your feelings honestly with family, friends, a spiritual adviser or a counselor.
- Keep a journal to help organize your thoughts.
- When faced with a difficult decision, list the pros and cons for each choice.
- Find a source of spiritual support.
- Set aside time to be alone.
- Remain involved with work and leisure activities as much as you can.
- Be ready to say no. This is the time to focus on you.
What helped you through rough times before your cancer diagnosis can help ease your worries now. This may include a close friend, religious leader or a favorite activity. Turn to these comforts now. Also be open to trying new ways to deal with your cancer.
Get Ready! North Carolina Will be Part of Solar Eclipse in April

Millions of Americans live in the path of 2024’s solar eclipse. See where to watch
(CNN, Matt Stiles, Kenneth Uzquiano, Ashley Strickland, and Will Mullery) -- One of the year’s most anticipated celestial events — a total solar eclipse — will put on a dramatic show April 8 as it crosses over Mexico, the United States and Canada.
A total solar eclipse occurs when the moon passes between Earth and the sun, completely blocking the sun’s face and causing the golden orb to temporarily disappear from view. The phenomenon has inspired myths and folklore for millennia.
The event will be visible to millions — including 32 million people in the US alone — who live along the route the moon's shadow will travel during the eclipse, known as the path of totality. For sky-gazers in the areas experiencing totality, the moon’s shadow will completely cover the sun. Those along the very center line of the path will see an eclipse that lasts between 3 ½ and 4 minutes, according to NASA.
The total duration for all phases of the eclipse, however, lasts for hours. Since the moon doesn’t just suddenly appear between Earth and the sun, the event begins with a partial eclipse. The moon's shadow will slowly move across the sun's face during the approach to totality, causing the sun to appear like a sharpening crescent. Depending on your location, the partial eclipse can last between 70 to 80 minutes, according to NASA.
The eclipse will first appear over the South Pacific Ocean and begin its journey across North America. Mexico’s Pacific coast is the first point of totality on the path, expected at 11:07 a.m. PT (2:07 p.m. ET) and the eclipse is expected to end on the Atlantic coast of Newfoundland at 5:16 p.m. local time (3:46 p.m. ET).
During totality, the sky will darken as if it’s dusk or dawn. Depending on humidity and cloud cover, expect to feel a roughly 10-degree Fahrenheit (5-degree Celsius) drop in temperature when the sun disappears from view, according to NASA.
Look out for Baily’s beads just before and after the sun disappears. This scintillating phenomenon occurs when the sun’s rays shine around valleys on the lunar horizon, creating glowing drops of light around the moon.
The location that will experience the longest duration of totality is near Torreón, Mexico, where the peak of the eclipse will last 4 minutes and 28 seconds. But you don’t have to be squarely in the path of this solar spectacle to witness some of its wonders.
Millions more outside of the path of totality, across an area that includes 49 US states, will see a partial solar eclipse, in which the moon blocks a portion of the sun and appears to take a crescent-shaped “bite” out of it.
And be sure to find a pair of certified ISO 12312-2 compliant eclipse glasses ahead of the big day to safely view every stage of the eclipse and enjoy the celestial show while you can. Another total solar eclipse won’t be visible across the contiguous US again until August 2044.
Click here to see how the eclipse will impact your location.
CDC: Preterm Births in US is Rising

US Has Worse Maternal Mortality Rate of Any Undeveloped Nation
The CDC released new data showing the percentage of babies delivered preterm (before 37 weeks) jumped to nearly 8.7% in 2022. The 12% increase from 2014 represents hundreds of thousands of babies each year and poses a threat: Preterm birth is the leading cause of death and health conditions for infants and children. The study also found Black mothers were almost twice as likely as white mothers to give birth early.
Why is this happening?
It’s not always clear — but experts say giving birth later in life can raise risks. It comes as about one in five women in the US are having their first child after age 35. One expert also reportedly pointed to obesity as a potential factor in rising rates. Obesity doesn’t cause early births but complications associated with it, like preeclampsia, can. Stress can also play a role, and it’s possible other environmental factors can, too. Experts suggest pregnant people should see their doctor sooner if they’re experiencing headaches, changes in urination, and increased blood pressure.
The US has the worst maternal mortality rate of any developed nation. Now, this latest report points to another challenge some new mothers face as more than two million live in counties without access to maternity care.
North Carolina Among States Rethinking Reading

States, including NC, rethink reading
(Axios, Erica Pandey) -- Dozens of cities and states across America are overhauling the way their schools teach reading — attempting to close gaps exacerbated by the pandemic.
Why it matters: Nearly 40% of U.S. fourth graders are below the basic proficiency level for reading, according to a standard national exam.
By the numbers: 37 states and D.C. have passed laws or enacted policies changing up the way reading is taught — pursuing new methods that are backed up by studies.
Zoom out: Reading curriculums in America’s schools haven’t kept up with decades of science and research into how kids learn.
- Many districts have long used an approach dubbed “balanced literacy,” which directs teachers to read aloud to kids, inspire a love of books, and teach strategies like guessing words based on pictures or memorizing them.
- The new approach, called “the science of reading,” teaches it much more explicitly. It relies on methods that have evidence demonstrating their efficacy, and stresses some key pillars including vocabulary, comprehension and phonics.
Between the lines: The ability to understand language and stories develops naturally in kids, just like walking and talking, but reading does not, says Tiffany Hogan, director of the the Speech and Language Literacy Lab at MGH Institute in Boston.
- So the balanced literacy approach, which relies on kids’ intuition to pick up reading, only works for some students.
- Studies have shown that phonics-based instruction, however, is effective at raising test scores across the board.
That doesn't mean teachers should abandon stories and take a sterile approach to teaching literacy, says Hogan. Instead, explicit instruction on how to read words and inspiring a love for books should come together, she says.
How we got here: The reading debate had a breakout moment due to the collision of a number of trends over the last few years, The New York Times reports.
- Many parents — home with their kids for the first time during the pandemic — noticed problems with their reading and started a grassroots movement to convince lawmakers and educators to make changes, Hogan said. “The fire was burning, and that threw on the gasoline."
- A podcast from Emily Hanford of American Public Media that dove into the war between teaching methods — and zoomed in on the students who were falling through the cracks — got millions of listens and spread awareness of the issue.
- And some early adopters of the new methods saw stunning results.
Zoom in: Mississippi climbed from 49th out of 50 states for fourth-grade reading proficiency in 2013 to 21st in 2022.
- State legislators and educators tried a number of strategies, including screening kids for literacy, hiring literacy coaches for teachers, and emphasizing phonics.
- “After Mississippi, other states started paying attention,” Hogan said.
Reality check: Most states are rethinking reading, but the progress could take years or decades.
- The system is populated with educators who were taught entirely different methods, and "the resistance is real," said Mark Seidenberg, a psychologist at the University of Wisconsin.
- And teachers across the country are being asked to embrace a great deal of change when burnout levels are high and many are leaving the profession.
On top of that, even those who are open to new methods will have to go back to school to get up to speed per their states' new laws.
- "There's the question of 'Will these professional development programs and trainings be good enough?'" Seidenberg said.
What to watch: The reading movement has thus far focused on elementary school students and preventing problems in their futures, Hogan says. Next, districts will have to grapple with achievement gaps in middle and high school.
- Just 31% of eighth graders and 37% of twelfth graders are at or above basic proficiency. "As students get older, reading ability is a foregone conclusion," says Hogan. "And it shouldn't be."
Five Children With Hereditary Deafness Can Hear for the First Time After Gene Therapy

Researchers "Really Excited" to Test Gene Therapy on Other Types of Genetic Deafness
(NPR, Rod Stein) -- For the first time, gene therapy is showing promise for treating inherited deafness, researchers reported Wednesday.
A study involving six children born with a genetic defect that left them profoundly deaf found that an experimental form of gene therapy restored at least some hearing for five of them.
"We are absolutely thrilled," says Zheng-Yi Chen, an associate scientist at Mass Eye and Ear's Eaton-Peabody Laboratories and associate professor of Otolaryngology–Head and Neck Surgery at Harvard Medical School in Boston. Chen led the research, which was published in the journal The Lancet.
"This is really the first time that hearing has been restored in any adult or children by a new approach — a gene therapy approach," Chen tells NPR in an interview.
For the first time, gene therapy is showing promise for treating inherited deafness, researchers reported Wednesday.
A study involving six children born with a genetic defect that left them profoundly deaf found that an experimental form of gene therapy restored at least some hearing for five of them.
"We are absolutely thrilled," says Zheng-Yi Chen, an associate scientist at Mass Eye and Ear's Eaton-Peabody Laboratories and associate professor of Otolaryngology–Head and Neck Surgery at Harvard Medical School in Boston. Chen led the research, which was published in the journal The Lancet.
"This is really the first time that hearing has been restored in any adult or children by a new approach — a gene therapy approach," Chen tells NPR in an interview.
"Before the treatment they couldn't hear a thing. You could put the loudest sound in the ear and they don't hear anything," Chen says. "And now they can hear."
The children's hearing isn't completely normal — they may still need hearing aids — but improved significantly, Chen says. The treatment appears safe. The children have been followed for between six months and a year so far.
"It worked as well as we imagined," Chen says. "This really was beyond our expectations."
Chen and his colleagues have continued to treat additional patients and will follow the study subjects in the hope that the improvement is permanent.
"This is a very big deal. It's a new dawn for hearing loss," Chen says.
A first for treatment of hereditary deafness
Other researchers agreed.
"This is an incredibly important clinical study," said Dr. Lawrence Lustig, who chairs Columbia University's Department of Otolaryngology - Head & Neck Surgery, says in an email to NPR. "It is the first time it has been shown that genetic deafness can be treated with gene therapy in humans."
Hearing loss affects more than 1.5 billion people worldwide, including about 26 million who are born deaf, according to Mass Eye and Ear. For hearing loss in children, more than 60% stems from genetic causes.
The otoferlin defect accounts for an estimated 1% to 8% of genetic deafness, meaning as many as 100 children are born with the condition in the U.S. each year, Lustig wrote.
Several other groups are pursuing similar gene therapies for genetic deafness and will report their findings Feb. 3 at the annual meeting of the Association for Research in Otolaryngology.
Help Improve Child Welfare System with NCMS, Carolina Complete Health

A special message from NCMS CEO Chip Baggett
The North Carolina Medical Society is proudly part of the partnership that established Carolina Complete Health (CCH), the only Provider-Led Plan established to deliver Medicaid Managed Care in North Carolina.
As we turn to a new year, CCH needs your unique insights. It is looking to learn from providers about your experiences with children and families involved in the foster care system.
This letter outlines how you can get involved in the “Foster Share” Listening Series. I hope you'll take the time to help CCH, and your foster care families, as it looks to improve the experience for children and families in the foster care community.
Register for Listening Series:
Read Revised Policy Paper:
NCMS Member Dr. Seth Hawkins Inducted as a Fellow of The Explorers Club

Morganton doctor named Fellow of The Explorers Club
(The News-Herald) -- Dr. Seth Collings Hawkins of Morganton was recently inducted as a Fellow of The Explorers Club.
The Explorers Club is headquartered in New York City where it was founded in 1904. With current Chapters across the globe, The Explorers Club has been supporting scientific expeditions and field study in all disciplines for over a century.
Hawkins is an anthropologist, writer, and physician, double double-boarded in both emergency medicine and EMS (field medicine). He has decades of experience supporting expeditions throughout the world, particularly in the disciplines of medicine and anthropology.
He serves as medical advisor/director for the NC Outward Bound School, NC State Parks, the Student Conservation Association, Recreational Equipment, Inc (REI), and the National Association for Search and Rescue. He is also the Local Emergency Medical Advisor for all US Forests in North Carolina and the National Park Service Outer Banks (Cape Lookout and Cape Hatteras National Seashores). He is co-author of Vertical Aid: Essential Wilderness Medicine for Climbers, Trekkers, and Mountaineers, editor of the textbook Wilderness EMS, co-editor of the new second edition of Expedition & Wilderness Medicine, and founder of multiple wilderness medicine organizations, as well as medical director for multiple wilderness EMS teams and schools. He earned his Fellowship in the Academy of Wilderness Medicine (FAWM) with the inaugural class in 2007, and also became the first physician designated a Master Fellow by the Academy of Wilderness Medicine in 2014, with specialization in wilderness EMS.
He earned his Fellowship in the Academy of EMS with the inaugural class in 2014. He serves as Associate Professor of Emergency Medicine at Wake Forest University School of Medicine and is the Associate Director of the Wake Forest University School of Medicine Wilderness Medicine Fellowship. He is also currently a graduate student at The University of North Carolina at Charlotte in its dual degree anthropology-public health master’s degree program. He has published widely in the wilderness medicine literature, including as coauthor of several Wilderness Medical Society clinical practice guidelines. He earned his Diploma in Mountain Medicine at the University of New Mexico International Mountain Medicine Center in its 2023-24 Diploma class.
As well as supporting and participating in expeditions around the world, closer to his home in the US state of North Carolina (NC), Hawkins has run the Carolina Wilderness EMS Externship every year since 2011.
This program, frequently cited by its participants as the “best month of medical school,” takes two medical students/resident physicians and intensively trains them in wilderness EMS and expedition medicine over a one-month residential period. The program originated in Burke County, NC, as a county-based program, but in 2021 it became expeditionary and now uses the entire state of North Carolina as its classroom.
Dr. Hawkins comments for NCMS Members:
I very much see activities with The Explorers Club being consistent with an overall theme in my medical career: ensuring the quality of medical care delivered in wilderness areas is equivalent (or even sometimes superior) to the care delivered in other spaces. For sure the type of care may be different, but there is no intrinsic reason the quality should be less. More specifically here in North Carolina, my work is directed towards patients with a medical situation, for example, at the top of Attakulla (now known as Mt. Mitchell), in the waters or the shores of the Outer Banks, or deep in the forests of the Smoky Mountains. From both a medical and a public health perspective, their medical care is as important as the care of anyone anywhere else, and in some senses the stakes are higher. The spirit of The Explorers Club is one of curiosity and scientific enquiry into the interstitial and remote spaces of the world, and I’m excited to bring a medical perspective to that spirit.
In its most recent iteration in September of 2023, Hawkins and Externs David Baskin (Wake Forest University) and Brian Drury (Brown University) collectively traversed more than 18,000 kilometers in only four weeks. Their training and medical care operations took them throughout North Carolina, including both the highest mountain and the deepest gorge in eastern North America as well as a remote Atlantic Ocean island where emergency transport is only accomplished by helicopter or ferry. They trained with one of the oldest North American medical communities, the Eastern Band of Cherokee Indians, and one of the newest, the US Forest Service’s recently established EMS system. They slept on sea dunes and by rivers and mountains throughout the state, with more than half of the work completely in the field, sleeping in tents and training in the natural environment. The Externship also includes the Wake Forest-UNC WildMed Lake Weekend, where dozens of medical students travel to Lake James State Park in North Carolina and paddle out to a water-only accessible peninsula where they train in wilderness and expedition medicine skills for a weekend.
More internationally, Hawkins has contributed to scientific and expeditionary work in Australia, India, Costa Rica, England, Finland, Bhutan, Vietnam, China and Canada, among other locations. His expeditionary interests include both full-scale expeditions and smaller microadventures, a concept popularized by Alastair Humphrey.
Hawkins’s membership as a Fellow of The Explorers Club was advanced by current members Dr. Gregory H. Bledsoe, founder of the Expedition Medicine National Conference and lead editor of Expedition and Wilderness Medicine, and Dr. Kenneth Kamler, author of Doctor on Everest and Surviving the Extremes.
NCMS BOD, Committee Chairs, Staff Have Busy Weekend in Raleigh (Including Visit from Attorney General Josh Stein)

Attorney General Stein Addresses NCMS Board, Staff, Committee Chairs
RALEIGH -- The North Carolina Medical Society is kicking off 2024 with two days of meetings and planning, plus a visit from Gubernatorial candidate Josh Stein.
Attorney General Stein laid out his priorities for healthcare in a speech over lunch on Saturday. Stein says he is committed to improving the working environment of healthcare professionals, dedication to an expanded healthcare workforce in rural areas, and the protection of things such as telehealth. He also said he believes in the strongest support for the rights of patients and their physicians to make their own healthcare decisions.
Stein is running for Governor this year in a crowded field that includes NC Lieutenant Governor Mark Robinson. Robinson was also invited to address the NCMS group but had other commitments.
Meetings included a seminar on Friday afternoon that went over NCMS priorities and guidelines for NCMS Committees. The full list of committees and ways you can get involved can be found by clicking here.
On Saturday, the NCMS Board of Directors met along with staff and several committee chairs to discuss the NCMS 2024 strategic priorities, a report from the Secretary-Treasurer, an update on the 2024 LEAD Conference, and a look at the 2024 election.
The North Carolina Medical Society has several member candidates. We are currently featuring them in interviews in our 2024 Candidate Series. Look for those interviews in Morning Rounds and on our website.
Photos of AG Stein speech:
Photos of the weekend's Committee Training;
Photos of BOD Meeting:
World's First Malaria Vaccine Program for Children Begins
Cameroon starts world’s first malaria vaccine program for children
(ASSOCIATED PRESS) -- Cameroon will be the first country to routinely give children a new malaria vaccine as the shots are rolled out in Africa.
The campaign due to start Monday was described by officials as a milestone in the decades-long effort to curb the mosquito-spread disease on the continent, which accounts for 95% of the world’s malaria deaths.
“The vaccination will save lives. It will provide major relief to families and the country’s health system,” said Aurelia Nguyen, chief program officer at the Gavi vaccines alliance, which is helping Cameroon secure the shots.
The Central Africa nation hopes to vaccinate about 250,000 children this year and next year. Gavi said it is working with 20 other African countries to help them get the vaccine and that those countries will hopefully immunize more than 6 million children through 2025.
In Africa, there are about 250 million cases of the parasitic disease each year, including 600,000 deaths, mostly in young children.
Cameroon will use the first of two recently approved malaria vaccines, known as Mosquirix. The World Health Organization endorsed the vaccine two years ago, acknowledging that that even though it is imperfect, its use would still dramatically reduce severe infections and hospitalizations.
The GlaxoSmithKline-produced shot is only about 30% effective, requires four doses and protection begins to fade after several months. The vaccine was tested in Africa and used in pilot programs in three countries.
GSK has said it can only produce about 15 million doses of Mosquirix a year and some experts believe a second malaria vaccine developed by Oxford University and approved by WHO in October might be a more practical solution. That vaccine is cheaper, requires three doses and India’s Serum Institute said they could make up to 200 million doses a year.
Gavi’s Nguyen said they hoped there might be enough of the Oxford vaccines available to begin immunizing people later this year.
Neither of the malaria vaccines stop transmission, so other tools like bed nets and insecticidal spraying will still be critical. The malaria parasite mostly spreads to people via infected mosquitoes and can cause symptoms including fever, headaches and chills.
FDA: Don't Use Neptune's Fix, Dangerous 'Gas Station Heroin' Showing Up in NC

Tianeptine Poses Serious Risks as NC Cities Report it on Local Store Shelves
Lawmakers sent a letter to the FDA Thursday taking the first steps toward banning the dangerous substance tianeptine, known as 'gas station heroin.'
Tianeptine is not regulated by the FDA, but WRAL News discovered it is still winding up on local store shelves. Often times it is being marketed as a dietary supplement or a mood booster and is sold as Neptune's Fix Elixer.
States across the U.S. have reported a rise in overdoses due to the drug, according to the FDA. The drug is already banned in nine states, including bordering states Tennessee and Georgia.
Thursday's letter received bipartisan support and was led by Reps. Jeff Jackson (D-NC) and Rick McCormick (R-Ga.). Rep. Wiley Nickel (D-NC) was also among signees.
The FDA is warning consumers to not purchase or use any Neptune’s Fix products, or any other product with tianeptine -- a potentially dangerous substance that is not FDA-approved for any medical use but is illegally sold with claims to improve brain function and treat anxiety, depression, pain, opioid use disorder and other conditions.
FDA has received severe adverse event reports after use of Neptune‘s Fix products, including seizures and loss of consciousness leading to hospitalization. Consumers who experience a bad reaction to any tianeptine product should seek immediate medical help.
Neptune Fix’s labels state the product contains tianeptine, but may contain other harmful ingredients not listed on the label. These products, like other tianeptine products, can be purchased online and at gas stations, vape or smoke shops, or other locations. FDA is testing these products and will provide more information as it becomes available. FDA also continues to warn consumers about risks of using tianeptine.
Health care professionals and consumers should report adverse events or side effects related to the use of this product to FDA's MedWatch Safety Information and Adverse Event Reporting Program:
- Complete and submit the report online at MedWatch Online Voluntary Reporting Form, or;
- Download and complete the form, then submit it via fax at 1-800-FDA-0178.
On The Lighter Side - January 19, 2024 - Basketball, Hockey, Pasta, and a Beloved Duo!
Here are some things NCMS employees, members, and YOU are talking about this Weekend and Beyond!
College Basketball is full-court action this weekend!

Men's Basketball
Saturday
- #4 UNC vs. Boston College, 2:15pm
- #7 Duke vs. Pittsburgh, 8pm
- #2 Purdue vs. Iowa, 2pm
- #3Kansas vs. West Virginia, 4pm
- #1UConn vs. Villanova, 8pm
Sunday
- #10 Memphis vs. Tulane, 1pm
- #14 Illinois vs. Rutgers, 1pm
Women's Baskteball
Sunday
- #4 NC State vs. Duke, noon
- #15 Florida State vs. Virginia, 2pm
- #19 Notre Dame vs. Wake Forest, 2pm
- #13 Louisville vs. #23 UNC, 2pm
The Carolina Hurricanes hit the ice TONIGHT!

The Carolina Hurricanes take on the Detroit Red Wings at 7pm tonight. Players to watch include Seth Jarvis and Sebastian Aho. Will the Canes pull out a win! Check it out on ESPN+ or get tickets here.
It is Pasta Festival Time in Asheville!

Make fresh pasta, learn new recipes, and have fun for the whole family Saturday. All you need to know is here.
There will be Two Less Lonely People In The World Saturday with Air Supply!

See the famed duo at the Crown Theater in Fayetteville, Saturday at 7:30pm. Tickets can be purchased here.
If you have an event you would like added to On The Lighter Side, email Randy Aldridge at [email protected].
New Report: Colon Cancer Killing More Younger Women and Men Than Ever

Experts are stumped as to why colorectal cancer is rising dramatically among people in their 30s and 40s
(NBC - Erika Edwards and Jessica Herzberg) -- Colorectal cancer is the deadliest cancer for men under age 50 — and the second deadliest cancer among women in the same age group, behind breast cancer.
The incidence of colon cancer has been rising for at least the last two decades, when it was the fourth-leading cause of cancer death for both men and women under 50.
Among men and women of all ages, lung cancer remains the leading cause of cancer death. Prostate cancer is second for men, and breast cancer is second for women. Colorectal cancer is third, overall, for both sexes.
Even as overall cancer deaths continue to fall in the U.S., the American Cancer Society is reporting for the first time that colon and rectal cancers have become leading causes of cancer death in younger adults. The finding was published Wednesday in CA: A Cancer Journal for Clinicians.
Cancer is traditionally a disease among the elderly, although the percentage of new cases found in people 65 and older has fallen from 61% in 1995 to 58%. The decrease, attributed mainly to drops in prostate and smoking-related cancers, has occurred even though the proportion of people in that age group has grown from 13% to 17% in the general population.
In contrast, new diagnoses among adults ages 50 to 64 have increased since 1995, from 25% to 30%.
Rates of breast and endometrial cancer, as well as mouth and throat disease, have been on the rise. The report did not break down those diagnoses by age.
The findings reflect what cancer doctors have observed for years.
"For a couple of decades now, we have been noticing that the patients coming into our clinic seem to be younger and younger," said Dr. Kimmie Ng, the director of the Young Onset Colorectal Cancer Center at Dana-Farber Cancer Institute in Boston. "What this report now cements for us is that these trends are real." Ng was not involved with the new report.
Dr. William Dahut, the chief scientific officer at the American Cancer Society, said younger people tend to be diagnosed at later stages, when the cancer is more aggressive.
"So it's not only having a colorectal cancer — it's colorectal cancer that’s more difficult to treat, which is why we’re seeing these changes in mortality," Dahut said.
The diagnosis of late-stage colorectal cancer was a shock to Sierra Fuller, 33, of Acton, Massachusetts, just outside Boston. It was around Christmas 2021 when Fuller noticed blood in her stool when she went to the bathroom. With no family history of colon cancer, she figured the problem was most likely an annoying hemorrhoid.
Weeks later, the blood deposits worsened, and she started having abdominal pain.
"It was a month from when I got the symptoms to when I sought help, and I realize that I was pushing it," she said. Tests revealed she had stage 3b colorectal cancer. That usually means the cancer has started to spread through the colon and possibly to nearby lymph nodes, but not any farther, according to the American Cancer Society.
It was a blow to Fuller and her husband, who had just started talking about whether to try for a baby. They decided to freeze embryos before Fuller's treatment protocol, which would include radiation, chemotherapy and surgery.
It is an example of how cancer uniquely affects young patients.
"People younger than 65 are less likely to have health insurance and more likely to be juggling family and careers," Dahut said in a news release announcing the new report. "Also, men and women diagnosed younger have a longer life expectancy in which to suffer treatment-related side effects, such as second cancers."
Just over a year later, Fuller is cancer-free but must get regular scans and blood tests. She said that she feels good but that she is "always going to have that worry" that her cancer will return.
"If I have to go through this again, whatever that looks like, I'll cross that bridge if it comes," Fuller said.
Why is cancer rising in younger people?
Doctors do not know why cancer, especially colorectal cancer, is becoming more common in younger adults. Some hypothesize that increasing obesity rates, sedentary behavior and unhealthy diets could be playing roles.
"But honestly, the patients we're seeing in clinic often do not fit that profile," said Dr. Kimmie Ng, the director of the Young Onset Colorectal Cancer Center at Dana-Farber Cancer Institute in Boston. "A lot of them are triathletes and marathon runners. I mean, super healthy people."
Ng suspects something in the environment may be behind the rise.
"What we suspect may be happening is that whatever combination of environmental factors is responsible for this, that it’s likely changing our microbiomes or our immune systems, leading us to become more susceptible to these cancers at a younger age," Ng said.
How to protect against colorectal cancer
Colonoscopy screening is generally recommended starting at age 45. People with family histories of the illness may need to begin screening earlier.
A person whose parent was diagnosed with colon cancer at age 50, for example, would need to start screening at age 40, Dahut said.
However, only about a third of people diagnosed with colon cancer have some kind of family history or predisposition to the cancer.
Maintaining a healthy body weight and minimizing red meat in the diet may help reduce risk, Ng said.
Signs that could signal a problem, Ng said, include blood in the stool, abdominal pain, unintentional weight loss and changes in bowel habits.
"If it's getting worse, if it's not going away, you know, that's when somebody really needs to start paying attention and talk to their primary care doctor about what's happening," she said.
93-Year-Old Rowing Champ Has Scientists Reconsidering Beliefs About Aging
This 93-Year-Old Indoor Rowing Champion Has the Cardiovascular Engine of a 40-Year-Old

In a recent study, scientists were shocked and had to reconsider two beliefs about aging and longevity.
(The Washington Post, Gretchen Reynolds) -- For lessons on how to age well, we could do worse than turn to Richard Morgan.
Lessons on aging from active older people
Highest heart rate on record
Exercising 40 minutes a day
- Consistency: Every week, he rows about 30 kilometers (about 18.5 miles), averaging around 40 minutes a day.
- A mix of easy, moderate and intense training: About 70 percent of these workouts are easy, with Morgan hardly laboring. Another 20 percent are at a difficult but tolerable pace, and the final 10 at an all-out, barely sustainable intensity.
- Weight training: Two or three times a week, he also weight-trains, using adjustable dumbbells to complete about three sets of lunges and curls, repeating each move until his muscles are too tired to continue.
- A high-protein diet: He eats plenty of protein, his daily consumption regularly exceeding the usual dietary recommendation of about 60 grams of protein for someone of his weight.
How exercise changes how we age
NCCPRW Meets to Talk Future of North Carolina Clinician and Physician Well-Being
Well-Being Consortium Meets at NCMS Headquarters in Raleigh
RALEIGH -- The North Carolina Clinician and Physician Retention and Well-Being Consortium met Thursday at the NCMS headquarters in Raleigh. The agenda included a history of the Consortium by NCMS COO Shawn Scott and a look forward from NCMS CLO Ashley Rodriguez.
The meeting also included an update from Corey Feist from the Dr. Lorna Breen Heroes' Foundation about the Foundation’s partnership with the Consortium to lead the All In: Caring 4 NC’s Caregivers campaign. This initiative is designed to improve and protect the mental health and well-being of clinicians in NC and will be a core focus of the Consortium’s work for 2024.
In attendance were executives from around the state including Thomas Mansfield, CEO of the NC Medical Board, Rep. Timothy Reeder, President of the NCMSF Board of Trustees, NCMS Board member Dr. Charul Haugan, and members of the North Carolina Medical Board.
Here are some photos from the event:
2024 NCMS Candidate Series - Dr. Mary Ann Contogiannis

2024 NCMS Candidate Series Featuring Dr. Mary Ann Contogiannis
The 2024 North Carolina Medical Society Candidate Series kicks off with an exclusive interview featuring Dr. Mary Ann Contogiannis, who is vying for the US House - NC6 seat. Dr. Contogiannis delves into topics such as the impact of Medicare on North Carolina's senior citizens, the workforce shortage, prior authorization, and her vision for the future of medical care in the state.
 All candidates who are members of NCMS and are running for either state or federal office have been extended invitations to articulate their perspectives on these crucial subjects. Stay tuned for forthcoming interviews with other candidates leading up to the November election.
All candidates who are members of NCMS and are running for either state or federal office have been extended invitations to articulate their perspectives on these crucial subjects. Stay tuned for forthcoming interviews with other candidates leading up to the November election.
See the full interview with Dr. Contogiannis here:
https://youtu.be/eiu5pXai7y8
New Law Helps Military Service Members, Spouses Who Work as Physicians and PAs Practice in NC

2024 Brings Changes for Military Physicians and PAs
(Alan Wooten, The Center Square) -- For practicing physicians on North Carolina’s military bases, the new year brings change in state law that will provide help to them and those that can use their services.
Much of a broad bill passed in the General Assembly this year and signed by Democratic Gov. Roy Cooper on Sept. 29 went into effect immediately. A portion impacting relocating military members will be enacted Feb. 1.
North Carolina is home to six major military installations, chief among them Fort Liberty – the base formerly known as Fort Bragg and almost always recipient of any presidential “911 call.”
The Health & Human Services Workforce Act will allow “military relocation licenses for physician and physician assistant servicemembers and spouses.” The state board can issue a “military relocation license” to a “physician or physician assistant not otherwise actively licensed by the Board who meets” certain requirements.
Five criteria include being in the U.S. armed forces or a spouse of a service member; in North Carolina pursuant to military orders for military service; licensed in another jurisdiction with “substantially equivalent” or exceeding requirements of North Carolina; in good standing within that jurisdiction, with no disciplinary actions in the last five years or pending investigations by an occupational licensing board; and actively practicing medicine an average of 20 hours per week in the two years before relocating to North Carolina.
The Army’s Fort Liberty and Pope Air Force Base are in the southeastern part of the state; Seymour Johnson Air Force Base is in eastern North Carolina; and Marine Corps Air Station Camp Lejeune and MCAS New River are along the coast, not more than an hour's drive from the more inland MCAS Cherry Point. Two Coast Guard bases are on the northern coast at Elizabeth City; and the Military Ocean Terminal Sunny Point is on the southern coast in Brunswick County.
Among other things within the legislation are statutes related to over-the-counter hearing aids; credentialing of behavior analysts; optometry laws; audiology laws; oversight of Nurse Aide 1 education; requirement of law enforcement officers in certain hospital emergency departments; punishment for assault convictions against certain personnel; Medicaid reimbursements for dental procedures in ambulatory centers; and an updated definition of a bar in the sanitation statutes.
State-Funded Businesses to Consolidate to Reshape NC's Mental Health System
Consolidation to reshape NC’s mental health system
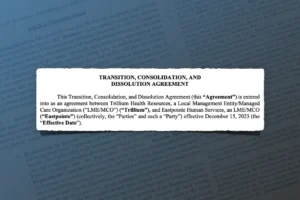
(NC Health News - Jaymie Baxley) -- Two state-funded businesses that manage behavioral health services for low-income residents say they will consolidate to create a single organization to serve 46 counties across eastern North Carolina.
Trillium Health Resources will take control of Eastpointe Human Services under the agreement, which was signed Saturday by the companies’ CEOs. The arrangement will reshape the state’s managed care system for providing care to Medicaid participants with mental health needs, substance use disorders and intellectual or developmental disabilities.
Eastpointe and Trillium are part of a network of six local management entities that operate as managed care organizations (known as LME-MCOs). That network oversees the treatment of those patients. A third such organization, the Sandhills Center, will dissolve in connection with the consolidation, leaving North Carolina with four LME-MCOs.
The consolidation flows from a directive issued in November by Sec. Kody Kinsley, head of the N.C. Department of Health and Human Services. He had been instructed by the General Assembly to reduce the state’s existing number of LME-MCOs to streamline the anticipated rollout of specialized plans for Medicaid participants who require more intensive services than typical beneficiaries.
DHHS has repeatedly delayed the implementation of these so-called tailored plans at the request of the LME-MCOs. Sandhills Center, in particular, struggled to secure tailored plan contracts with providers.
“Our goal is to get the tailored plan operators to a place where they can manage their patient population and the complex risks that they have in a smooth way,” Kinsley said in an interview Monday with NC Health News. “We’ve heard loud and clear from the provider community that their position is ‘less is more’ when it comes to managed care organizations. Getting the LME-MCOs [down] to four is a great opportunity to streamline the number of managed care companies that these providers have to contract with.”
He added that DHHS will be working closely with senior leaders from the consolidated LME-MCOs to prepare for the launch of tailored plans, which is now scheduled for July 1.
‘Sea change moment’
Nearly all of the counties served by Trillium, Eastpointe and Sandhills Center will be combined into one region, which will be managed by a yet-to-be-named company operated by Trillium. The consolidation is scheduled to take effect on Jan. 1, and the organization must have a new name and branding in place by the start of 2025.
“This is really a consolidation of entities that have different strengths,” Kinsley said. “And I think in recognition that they’re coming together as a consolidation, they should come up with a new name to recognize this step forward.”
In a joint statement on Monday, the companies promised that “all existing employees who desire employment and are in good standing will retain their positions.” The companies must “ensure that staff are offered compensation that is no less than employees’ current compensation,” according to the consolidation agreement.
Joy Futrell, CEO of Trillium, will become CEO of the new organization, while Eastpointe CEO Sarah Stroud will serve as its president. The agreement states that Anthony Ward, CEO of Sandhills Center, will be placed in an executive position.
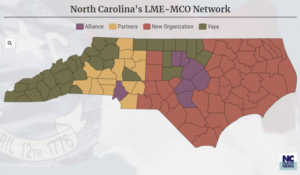 “We will continue to keep members as our primary focus,” Futrell said in a news release. “We know the next few months will contain many new opportunities, but believe the hard work that Trillium, Eastpointe, and Sandhills Center have already put forth will lead to a successful consolidation.”
“We will continue to keep members as our primary focus,” Futrell said in a news release. “We know the next few months will contain many new opportunities, but believe the hard work that Trillium, Eastpointe, and Sandhills Center have already put forth will lead to a successful consolidation.”
The new organization’s board will be made up of 22 members. Eleven of the members will come from Trillium’s board, and the other 11 will picked from the boards of Eastpointe and Sandhills.
“We’re still going to have to have more conversations in the future about how we have a board that will be representative of all the regions that they now share,” Kinsley said.
Three counties that were served by Sandhills Center and Eastpointe have been assigned to other LME-MCOs. Davidson County chose to change management entities to Partners Health Management; Harnett County moved to Alliance Health; and Rockingham County moved to Vaya Health.
While Kinsley acknowledged that the consolidation “was not an easy process,” he praised the companies for working together to “better serve the people of North Carolina.”
“I think we all know that the behavioral health system desperately needs it,” he said of the new organization. “This is a big sea change mo
The Biggest Health and Medicine Stories of 2023. There is Plenty to be Awed by.

In world with so much urgent and depressing news, it can be hard to take a moment and reflect on all of the encouraging scientific and medical progress that has happened. But looking back at 2023, there was plenty on the health beat to be awed by.
(Scientific-American, Tanya Lewis) -- From the arrival of the first safe and effective vaccines for a common respiratory disease to the first U.S. Food and Drug Administration–approved CRISPR gene editing treatment, these were some of the biggest stories in the health world this year.
NEW WEIGHT-LOSS DRUGS REVEALED NEW TRICKS
A new generation of drugs that result in significant weight loss appeared on the scene a few years ago with dramatic effects. This past year we learned a lot more about other potential benefits of the drugs, which include Novo Nordisk’s Wegovy and Ozempic and Eli Lilly’s Mounjaro. These range from reducing the risk of heart attack or stroke to possibly treating addiction. But the medications come with side effects such as gastrointestinal problems and muscle loss. They’re not cheap, either—they can cost around $1,000 or more out of pocket—and it’s not clear whether insurance will cover them. Still, these drugs are driving significant interest as we continue to learn more about them.
THE COVID PUBLIC HEALTH EMERGENCY ENDED
The federal public health emergency put in place to combat the COVID pandemic ended on May 11. The end of the public health emergency marked the conclusion of a set of policies that made it easier and cheaper to access COVID tests, vaccines and treatments, as well as telehealth visits. Consumers must now obtain many of these things with coverage through private insurance, Medicare, or Medicaid or bear the cost themselves. SARS-CoV-2, the virus that causes COVID, continues to circulate and pose a threat to public health. But in May the World Health Organization declared that disease no longer constituted a public health emergency of international concern and said that it was time to transition to long-term management of the COVID pandemic.
WE GOT CLOSER TO XENOTRANSPLANTS
There’s an enormous need for organ transplants, but donor organs are in short supply. Improvements in transplant science have made more organs available and usable. Yet too many people still die waiting for one. Now some scientists are exploring another approach: transplanting organs from nonhuman animals. In the past year they have made significant progress in such “xenotransplants.” Following the first transplant of a genetically engineered pig heart into a human in early 2022, this year doctors completed the second such transplant. (Both surgeries were performed on a compassionate use basis because the recipients were terminally ill.) Sadly, the man who received the heart in the latest surgery died after six weeks, likely because his immune system rejected the organ. Other researchers completed successful xenotransplant experiments in people who had suffered brain death, and monkeys that received pig kidneys survived for up to two years. Scientists are hopeful that they can improve the procedures enough to test these techniques in clinical trials in people soon.
RSV VACCINES FINALLY ARRIVED
Respiratory syncytial virus (RSV) causes annoying coldlike symptoms in most people, yet in very young children or older adults the disease can be deadly. For decades scientists have tried to develop a vaccine to protect against RSV, but a series of disastrous clinical trials in the 1960s ended up making the illness more severe, leading to the deaths of two children. Researchers persisted, however, and as of this year, several safe and effective RSV vaccines were approved by the FDA to protect pregnant people and older adults. The agency also approved an antibody drug that protects children after they’re born.
THE FIRST CRISPR-BASED TREATMENT WAS APPROVED
Nearly a decade after it was first discovered, the gene editing method known as CRISPR is resulting in its first treatments. In December the FDA approved the first CRISPR-based treatment for sickle cell disease. The new therapy is known as exa-cel and made by the biotech companies Vertex Pharmaceuticals and CRISPR Therapeutics. It deactivates a faulty gene for the hemoglobin protein, which transports oxygen around the body. Without the treatment, the gene causes blood cells to develop a sicklelike shape, making them clog up blood vessels. The illness, which disproportionately affects Black people, causes debilitating pain and fatigue. The new treatment, as well as another gene therapy approved at the same time, prevented symptoms of the disease for a year in clinical trials. But longer follow-up is needed to see if there are any side effects, and the cost could make it hard for many people to access.
WE GAINED NEW INSIGHT INTO LONG COVID
Even as the immediate danger of COVID has receded somewhat, tens of millions of people continue to be affected by long COVID—a cluster of symptoms such as fatigue, body aches and brain fog that linger long after an infection. The causes of long COVID are still mysterious, yet as Stephani Sutherland wrote in our March issue, it increasingly resembles a neurological disease. Not only does it cause cognitive problems with memory, attention, sleep and mood, but it also has symptoms such as pain and postexertional malaise—extreme fatigue after exercise—that seem to stem from the autonomic nervous system, the autopilot system that controls breathing and digestion, among other things. This new understanding could help guide treatments.
CHAT-BASED AI SYSTEMS ENTERED MEDICINE
When ChatGPT was released in November 2022, it caused ripples throughout numerous fields—and medicine was no exception. This chat-based artificial intelligence program made by the company OpenAI—along with large language models made by Google and others—is capable of generating text that convincingly mimics human writing. People have already begun to use these programs to diagnose medical conditions, and while the AIs appear surprisingly accurate in some early studies, doctors caution that they are not a substitute for professional medical care. Other people are turning to AI chatbots for therapy. Such apps could help meet the growing demand for mental health services, but as with using them for medical advice, experts urge caution.
FIRST FACE AND EYE TRANSPLANT WAS COMPLETED
Xenotransplants weren’t the only groundbreaking type of transplant to occur this year. In May doctors in New York City completed the first partial face and whole-eye transplant in an Arkansas man who had suffered severe electrical burns while working as a lineman. While corneal transplants are routine, this was the first time an entire human eye was transplanted and remained healthy six months later, according to the transplant team. The recipient, 46-year-old Aaron James, has not regained sight in that eye, but doctors say the eye’s retinal tissue is intact, and there are signs it may be sending signals to the brain. The feat opens the door to restoring the appearance—and possibly, one day, the function—of people who have had traumatic eye injuries.
Put your favorite health and medicine story of 2023 in the comments!
10 Biggest Health Risks Many Face During Christmas

**This article is with thanks to the South Coast Medical Group
The 10 Biggest Health Risks Many Face During Christmas
Christmas is a wonderful time of year, but it is also a time when people make their way into the ER with some unusual injuries. Before you curl up on the couch with a loved one and enjoy Elf, Christmas Vacation or Miracle on 34th Street, please take 2 minutes to read these reminders for having a safe and healthy holiday season.
1. Decorating Injuries
Slow down Clark Griswold!
Although you may be excited to put up the Christmas lights, there are many risks that come with that. One of the biggest risks is trying to hang the Christmas lights in hard to reach places on an unsteady ladder.

Tens of thousands of people get injured each year doing this simple task. The best way to stay safe is to stabilize a ladder on a flat surface before using, wear sturdy shoes, and decorate before you have too much eggnog.
2. Electric Shocks
In addition to ladder safety, it is important to be careful hanging lights, especially if they are plugged in. Old light sets that have spent several 11-month increments twisted up in storage can become brittle, and the wires may end up exposed. Be careful of any faulty lights that could cause you to get shocked. Faulty lights can also contribute to Christmas tree fires. Also, be mindful of how many things are going into one outlet.

3. Colds and Contagious Illnesses
Typically around the holidays, you are surrounded by many more people compared to normal. This year, the pandemic changes things, but it is still important to be mindful of who you are seeing and to avoid touching your face and consistently wash your hands. Even if you are limiting your contact, social distancing, and consistent mask usage can help you avoid germs.

4. Overeating
It’s hard to pass up mom’s signature dish during the holidays, and it seems like we never run out of sweets in December, but be careful. Overindulgence can cause weight gain that may only seem like a couple of pounds in the winter, but that gain could be a trend you don’t want to continue. Obesity comes with a whole new set of health issues. Try to be mindful of how much you are eating and drinking, and try to portion control. You know how wild the holidays are for Kevin McCallister.

5. Food Poisoning
In addition to overeating, another risk associated with food is food poisoning. Food poisoning can be caused by:
- Eating food that has sat out long without being refrigerated
- Food not cooked to a proper temperature
- Food exposed to cross-contamination
The best way to avoid this is to follow the food safety guidelines outlined by the CDC. Food poisoning can ruin all that fun, even dancing, during the holidays.

6. Anxiety
Anxiety can be a real challenge for many this holiday season, and the source of it can vary from person to person. Some people feel anxious being alone, while others feel anxious being around relatives they don’t see very often. Others simply develop anxiety for shopping or preparing for the season. Money issues can cause people a lot of stress. To help, take time to yourself and start your shopping and cleaning earlier.

7. Deep Cuts
The holidays call for a lot of preparation, and we’ve seen plenty of accidents in the kitchen and around the home related to sharp objects. Lacerations and cuts are a common injury, and they can come from chopping food for dinner, cutting wrapping paper for gifts or picking up broken glass from ornaments and decorations. There is no way to avoid these cuts entirely, but the best way to prevent them is by being careful and slowing down. Most of these accidents happen when you are in a rush.

8. Smoke Inhalation and Burns
If you think about it, there are many flammable items in your home during the holidays. These items include Christmas trees, burning candles, fireplaces, and food that is getting cooked in your home. When burning or cooking these items, you will want to make sure you keep an eye out for them, and never leave those items unattended. If you are deep-frying a turkey over the holidays, make sure you have ample space and protective clothing. When that cold turkey hits the hot oil, injury-causing accidents can happen.
Who hasn’t seen The Santa Clause? These things happen!

9. Choking
We know you’re excited to dig into Grandma’s homemade pumpkin or pecan pie, but please slow down when you eat. Also, avoid overstuffing yourself with stuffing. Choking on our favorite food is a serious health concern during the holidays.
Another thing to look out for is small toys that your pets and younger children may mistake for food. Watch over your pets and children and make sure that there are no small toys or parts laying around. Also, since it’s the season of chocolate, make sure it is kept at a safe distance away from our four-legged friends.
Nobody loved a good meal like Shaggy and Scooby, but please do so safely!

10. Binge Drinking
The holidays are a time to celebrate, but it doesn’t mean you need to go overboard. Please enjoy alcohol responsibly, and if your celebrations exceed your expectations, take a rideshare home, cozy up on the couch for the night where you’re celebrating, or get a ride from a friend.
If you’re a real Family Guy, maybe Peter Griffin will be your designated driver.

What have we missed? Leave tips for your colleagues below!
Poison Centers See Nearly 1,500% Increase in Calls Related to Injected Weight-Loss Drugs. Are Your Patients At Risk for Overdose?

Calls to poison centers increase
(CNN - Brenda Goodman) -- Poison control centers across the US say they are seeing a steep increase in calls related to semaglutide, an injected medication used for diabetes and weight loss, with some people reporting symptoms related to accidental overdoses.
Some have even needed to be hospitalized for severe nausea, vomiting and stomach pain, but their cases seem to have resolved after they were given intravenous fluids and medications to control nausea.
From January through November, the America’s Poison Centers reports nearly 3,000 calls involving semaglutide, an increase of more than 15-fold since 2019. In 94% of calls, this medication was the only substance reported.
In most of the calls, people reported dosing errors, said Dr. Kait Brown, clinical managing director of the association.
“Oftentimes, it’s a person who maybe accidentally took a double dose or took the wrong dose,” Brown said.
Compounded versions may require different doses
Semaglutide was approved by the US Food and Drug Administration in 2017. It is sold as Ozempic when used for diabetes and Wegovy when used for weight loss. Even when used as directed by a doctor, people can have stomach and bowel side effects, including nausea, vomiting and constipation, especially when they start the drugs.
After celebrities began openly embracing Ozempic on social media in 2022 as a way to lose weight, demand overwhelmed supply. It went into shortage in the FDA’s database in March 2022, which opened the door for certain qualified pharmacies to make compounded versions.
The compounded versions of semaglutide are often different from the patented drug. Many contain semaglutide salts called semaglutide sodium and semaglutide acetate. The FDA says the salt forms of the drug have not been tested and approved to be safe and effective the way the patented form of the medication has, and thus they don’t qualify for the compounding exemption in the law for drugs in shortage. In other cases, the compounded versions are sold in unapproved dosages.
The FDA has sent letters to at least two online sellers warning them to stop. Drugmaker Novo Nordisk has sued to stop six medical spas, medical clinics and weight loss clinics from selling knock-off versions.
But these compounded versions are popular because they may cost less out-of-pocket, especially if the treatment isn’t covered by insurance.
The FDA warned the public in June against taking compounded versions of the medication if the prescription forms were available. The agency said it had received adverse event reports after people used compounded versions of the drug.
Poison control centers say the reported symptoms don’t allow them to know whether the calls stem from the patented drugs or the compounded versions, Brown said, but some state poison center directors say they believe that compounded versions are behind many of the calls.
Calls to poison centers increase
Dr. Joseph Lambson, director of the New Mexico Poison and Drug Information Center, detailed what happened to three people who called the Utah Poison Control hotline, which saw calls related to semaglutide nearly quadruple between 2021 and 2022. He wrote about the cases in the Journal of the American Pharmacy Association
Two of the callers had accidentally taken 10 times the standard dose of the drug.
“We were getting reports of people giving themselves doses we had never heard of before,” Lambson said. “That’s kind of what sparked our interest” in tracking the calls.
The name-brand drugs are sold in pre-filled pens, which come with some safeguards. Patients dial to the correct dose and click to inject, so it’s harder to make mistakes. Ordinarily, people start at lower doses and work up over time to the therapeutic amount so their bodies can adjust.
Compounded versions, however, typically come in multidose glass vials, and patients draw their own doses into syringes. It’s easy to get confused.
“This is where we see a lot of errors. They end up drawing too much,” Lambson said.
One of the calls Lambson’s team received was from a 37-year-old woman who accidentally gave herself 1 milliliter instead of 0.1 milliliter – 10 times the recommended amount – as her first dose for weight loss.
A 50-year-old man accidentally gave himself 50 units instead of 5 units as his first dose for weight loss. He vomited for two days and had nausea for a week.
“I think that whenever we have to rely on a patient to discern what the right dose is, to draw up and then administer, you’re putting more chances in there for there to be errors,” Brown said.
A third caller, a 33-year-old woman, reported getting semaglutide at a spa but didn’t know the dose. She went to the ER for persistent vomiting and abdominal pain. She got an anti-nausea medication and IV fluids, and she was discharged later that day.
Julie Weber, director of the Missouri Poison Center, said it got 28 calls related to semaglutide in 2021. This year, through October, it has had 94.
Calls about semaglutide stand out in the data in other way, too. Although most calls to poison centers concern young kids who’ve accidentally ingested something, these calls are from adults ages 40 to 70, with the largest group in the 60-to-69 range.
Weber says the calls they see in their system aren’t only related to injections of compounded forms of the drug. Weber said many of their calls are related to the click pen that comes with the prescription drug.
In one case, a caller said they were having trouble with the pen and accidentally dialed it all the way up, giving themselves an entire month of doses at once.
“They misunderstood the pen. They did not know how to use it properly and dialed it up too and took like the whole pen instead of just the dose that was supposed to happen,” Weber said.
In other cases, reported at this year’s meeting of the American College of Medical Toxicology from the New York City Poison Control Center, people needed to be hospitalized. One of those patients accidentally took 20 times the recommended amount.
In a written statement, Novo Nordisk, the manufacturer of Ozempic and Wegovy, said patient safety is its top priority.
“We are taking multiple steps to ensure responsible use of our semaglutide medicines which are detailed on semaglutide.com,” the statement said.
There’s no specific antidote for a semaglutide overdose. The drug has a half-life of about a week, meaning it takes one week to clear half of it from your body. Emergency departments and hospitals can only help support patients with intravenous fluids and anti-nausea drugs as the drug works its way out out of their bodies.
In addition to nausea and vomiting, the Missouri Poison Center warns people who think they may have overdosed to watch for signs of low blood sugar, or hypoglycemia, which can be dangerous. Hypoglycemia is more common with semaglutide if you are also taking other medications for diabetes.
According to the Missouri Poison Center, signs of a semaglutide overdose include:
- Feeling lightheaded or dizzy
- Feeling shaky or jittery
- Sweating, chills and clamminess
- Irritability or impatience
- Headache
- Weakness
- Fatigue
- Nausea and/or vomiting
- Seizures
- Confusion
- Passing out
If you think you have overdosed on a weight loss drug, Brown said the best thing to do is call your local poison control center or the national hotline at 800-222-1222.
“That way, one of the specialists will be able to take specific information to their case regarding how much they administered, the type of overdose they’re experiencing … and decide if they’re safe to stay at home or if they are going to need to seek medical attention, especially if they’ve developed symptoms,” Brown said.
UNC-Chapel Hill Named National HIV Residency Pathway Consortium Site

UNC-Chapel Hill was recently named a National HIV Residency Pathway Consortium Site and awarded a year-long, $68,000 grant to support its efforts in training family medicine and internal medicine residents in caring for people with HIV. UNC’s site Investigators, Rick Moore, MD, and Louise Rambo King, MD, have a storied history of caring for patients with HIV.
(UNC Health Newsroom) -- UNC-Chapel Hill recently was named a National HIV Residency Pathway Consortium Site and awarded a year-long, $68,000 grant to support its efforts in training family medicine and internal medicine residents in caring for people with HIV. UNC’s site Investigators, Rick Moore, MD, and Louise Rambo King, MD, have a storied history of caring for patients with HIV.
This Health Resources and Services Administration (HRSA) grant through the National HIV Pathway Consortium (NHRPC) is part of a broader effort to enhance training in the management of HIV within primary care residencies at several sites throughout the country.
King and Moore work in partnership to lead longitudinal, integrated training in HIV care for training track residents to enable them to independently provide care for people with HIV in their clinical practices and thereby enhance access to HIV care on the state and national level.
“We are delighted to be part of this sub-award from HRSA to promote an area of concentration in HIV medicine for family medicine and internal medicine residents at UNC,” King said. “There is a real need for primary care physicians who are able to care for people living with HIV. This grant will give us the resources to support this area of concentration and develop it so that it is sustainable for the future.”
“This grant gives us the opportunity to strengthen and deepen experiences within the HIV and viral hepatitis training program,” Moore said. “We are thrilled to be taking part in this grant and what it allows us to do for resident education and development.”
“We are grateful for the collaboration between the family medicine and internal medicine departments and the invaluable contributions from the UNC infectious diseases division and the NC AIDS education training center, housed at UNC,” King said. “We are definitely better together!”
NHRPC is supported by the HRSA HIV/AIDS Bureau Ryan White Program through funding provided to the New England AIDS Education and Training Center, and is led by Philip Bolduc, MD, at UMass Memorial Health.