2023's First Bill Filed: NC Compassionate Care Act to Legalize Medical Cannabis

RALEIGH -- The first day of bill filing was led by Sen. Bill Rabon, R-Brunswick, who filed the NC Compassionate Care Act (SB3), a bill that legalizes medical cannabis. On Wednesday, January 26, 2023, he was joined by Sens. Michael Lee, R-New Hanover, and Paul Lowe, D-Forsyth as primary sponsors.
The North Carolina Compassionate Care Act lists many debilitating medical conditions for which doctors could prescribe medical cannabis as part of a patient’s treatment, including cancer, epilepsy, Crohn’s Disease, Parkinson’s Disease and Post Traumatic Stress Disorder.
According to the bill’s summary posted on the NCGA website, SB3 would require the state Department of Health and Human Services to issue “registry identification cards” to anyone who would qualify to be prescribed medical cannabis by a licensed physician, and set standards for doctors to issue that prescription.
Sens. Rabon and Lee introduced a similar bill last year. It passed the Senate 36-7, but did not make it out of the House Rules Committee.
"The Compassionate Care Act had great momentum and bipartisan support last session," said Rabon. "It's imperative that we continue to fight to ensure that North Carolinians with debilitating illnesses can receive the treatments they deserve."
The North Carolina Medical Society has supported the development of research regarding medical cannabis in the past. See the NCMS Policy here. The NCMS Board of Directors is meeting January 28, 2023, and is expected to discuss the issue again.
NC Doctor Files Lawsuit to Strike Down Restriction to Abortion Pills. Is NC New Battleground in Abortion Battle?

Dr. Amy Bryant has filed a lawsuit in North Carolina that may impact nationwide access to some abortion pills.
According to ABC News, Bryant is seeking to have the state strike down it's restrictions on the abortion pill mifepristone. Bryant says the restrictions do not coincide with rules set forth by the Food and Drug Administration.
Bryant told ABC News that she filed her lawsuit because there’s “no medical reason for politicians to interfere or restrict access” to mifepristone. Bryant's lawyer, Eva Temkin, argued federal rules for the drug preempt state regulations when the two conflict.
The lawsuit names North Carolina Attorney General Josh Stein as a defendant. A spokesperson for Stein told ABC News that they were reviewing the complaint. Advocates in favor of abortion rights are hopeful that this kind of "federal preemption" case will test a new legal strategy that could be applied in other states. They also see North Carolina as a hopeful place to try it out. While Republicans control both chambers of the state legislature, the administration is run by Democratic Gov. Roy Cooper.
The full story is available here.
Register Now: ADA Standards of Care in Diabetes 2023 Update

The American Diabetes Association Institute of Learning is offering the 2023 Standards of Care in Diabetes, Wednesday, January 25, 2023.
It is intended to provide clinicians, patients, researchers, payers, and others with the components of diabetes care, general treatment goals, and tools to evaluate the quality of care.
It includes presenters Brittany Bruggeman, MD, FAAP, Assistant Professor of Pediatric Endocrinology, University of Florida, and Robert Gabbay, MD, Chief Scientific & Medical Officer, American Diabetes Association.
The online meeting is free and offers 1.0 CME/CE.
To learn more about the ADA Scholars program click here. You must register in advance. Details on attending are here.
On the Lighter Side - January 20

There are even more reasons to love Dolly Parton! In addition to being a legend, she is helping us all in the kitchen. Dolly is adding to her Duncan Hines baking mixes collection, including southern favorites like cornbread and biscuits! See how to get those and more here.

For all of us who grew up in the 80s and 90s! Madonna announced she will 'Celebrate' in 2023 with a world tour of her greatest hits! The closest she gets to North Carolina is Washington, DC, so if you want to 'Express Yourself' and 'Vogue' again, you better act fast. Tickets go on sale today. Get yours here.

One of the North Carolina's most storied rivalries is back tomorrow night! The UNC Tar Heels take on the NC State Wolfpack Saturday at 5pm at the Dean Dome in Chapel Hill. Believe it or not, there are still tickets available! See if you can grab some of the few remaining ones here.

The Broadway hit 'Come From Away' is at the Durham Performing Arts Center this week and continues through Sunday. It is based on the events in the Newfoundland town of Gander during the week following the September 11 attacks. Thirty-eight planes, carrying approximately 7,000 passengers, were ordered to land unexpectedly at Gander International Airport. The characters in the musical are based on (and in most cases share the names of) actual Gander residents and stranded travelers they housed and fed. Get your tickets here.
On the Lighter Side - January 13
2023 is kicking off with a bang across the state and across the country. Here are some things we are excited about this week!

It is time for Carnival! January 6 marks the official start to the Mardi Gras season.

January 14 - Girl Scout cookies go on sale. This year Raspberry Rally is going head-to-head with Thin Mints to capture your heart!

January 14 - Carolina Hurricanes vs. Pittsburgh Penguins, 7pm, PNC Arena

January 16 - Martin Luther King, Jr. Day. Events and parades happening across the state and country.
In other good news:

Buffalo Bills Damar Hamlin goes home after his shocking cardiac arrest during a game against the Cincinnati Bengals.
Golden Globe Awards remind us all that being over 60 is fabulous! Angela Bassett, Jennifer Coolidge, and Michelle Yeoh won awards after decades in show business.

Can you spare a moment for Prince Harry? Britain's famed second son releases his first book!
NCMS Members Sworn in at General Assembly

RALEIGH -- The 2023-2024 North Carolina General Assembly reconvened, swearing in two North Carolina Medical Society members.

Doctor Kristin Baker joins the House of Representatives, representing District 82 - Cabarrus County. She was sworn in for her second full term on January 11, 2023. Baker is long-time member of NCMS, she graduated Phi Beta Kappa from UNC-Chapel Hill and attended the UNC School of Medicine.

Doctor Tim Reeder joins the House of Representatives, representing District 9 - Pitt County. He was sworn in for his first term. Reeder is a NCMS Past President (2018-2019) and is the current NCMS Foundation Board of Trustees President-Elect. Reeder graduated from Ohio State University, moving to North Carolina in 1998. He has worked for the East Carolina University Brody School of Medicine and is an emergency physician.

The House of Representatives consists of 120 members who serve a term of two years.
COVID-19 Public Health Emergency Renewed by Biden Administration
WASHINGTON, DC - As expected, the Biden administration has again renewed the COVID-19 Public Health Emergency. The provision gives the administration authority to respond to the pandemic as cases are again on the rise.
US Health and Human Services Secretary Xavier Becerra renewed the declaration on January 11, 2023, the expiration date of the previous renewal. It is an expected move because officials have promised a 60-day notice if they do not plan to renew the emergency.
White House Covid-19 Response Coordinator Dr. Ashish Jha says, "there's still a lot of Covid out there, and the public health emergency and his (Becerra's) determination gives us tools to fight this." Jha stressed that the decision to renew the declaration was based on several reasons, including the new, highly contagious XBB.1.5 variant.
The federal government spending law enacted in December 2022 decoupled several major relief measures from the public health emergency.
The package is now phasing out the requirement that prevents states from disenrolling Medicaid recipients as long as the public health emergency is in effect in exchange for an enhanced federal match. This coverage measure was enacted in March 2020 and led to a record 90 million enrollees in Medicaid, many of whom may no longer meet the income requirements to qualify.
Now, states can begin processing Medicaid redeterminations as of April 1, regardless of when the public health emergency ends. Estimates vary on how many people would lose their Medicaid benefits, though they range as high as 19 million.
Staffing, Burnout Lead to Massive Nursing Strike in New York City
Unsafe conditions, low pay, burnout, and COVID-19 are leading more than 7,000 nurses at two New York City hospitals to walk off the job. On Monday, January 9, 2023, the New York State Nurses Association (NYSNA) said that bargaining late into the night had not led to any agreements to keep nurses on the job.
The strike affects Mount Sinai and Montefiore hospitals and union insists that it is in an effort to improve patient care.
The hospitals were prepared for the strike, planning to pay temporary traveling nurses to fill in for strikers and to transfer some patients to other facilities. Montefiore Hospital also released a notice to staff on how to quit the union and stay on the job if they wanted.
Strikes among are more common than ever. Cornell University released a new report for 2022 saying strikes were up 43 percent from the previous year. The US Labor Department, which tracks only strikes with more than 1,000 workers, says strikes of that size are up 33 percent over the same period.
The US Surgeon General says that health workers are at an increased risk for mental health challenges as a result of distressing environments that strain their physical, emotional, and psychological well-being. The result is more difficulty providing patient care.
The North Carolina Medical Society is focused on protecting the health and well-being of our members and health professionals across the state. For resources available to you now click here.
For a more in-depth look at the strike in New York City click here.
$1.7 trillion federal spending bill, Millions at risk of losing Medicaid

Enrollment in Medicaid surged 30% to more than 83 million people during the pandemic, after Congress basically barred states from kicking people out of the program for the duration of the federal public health emergency declared in response to Covid.
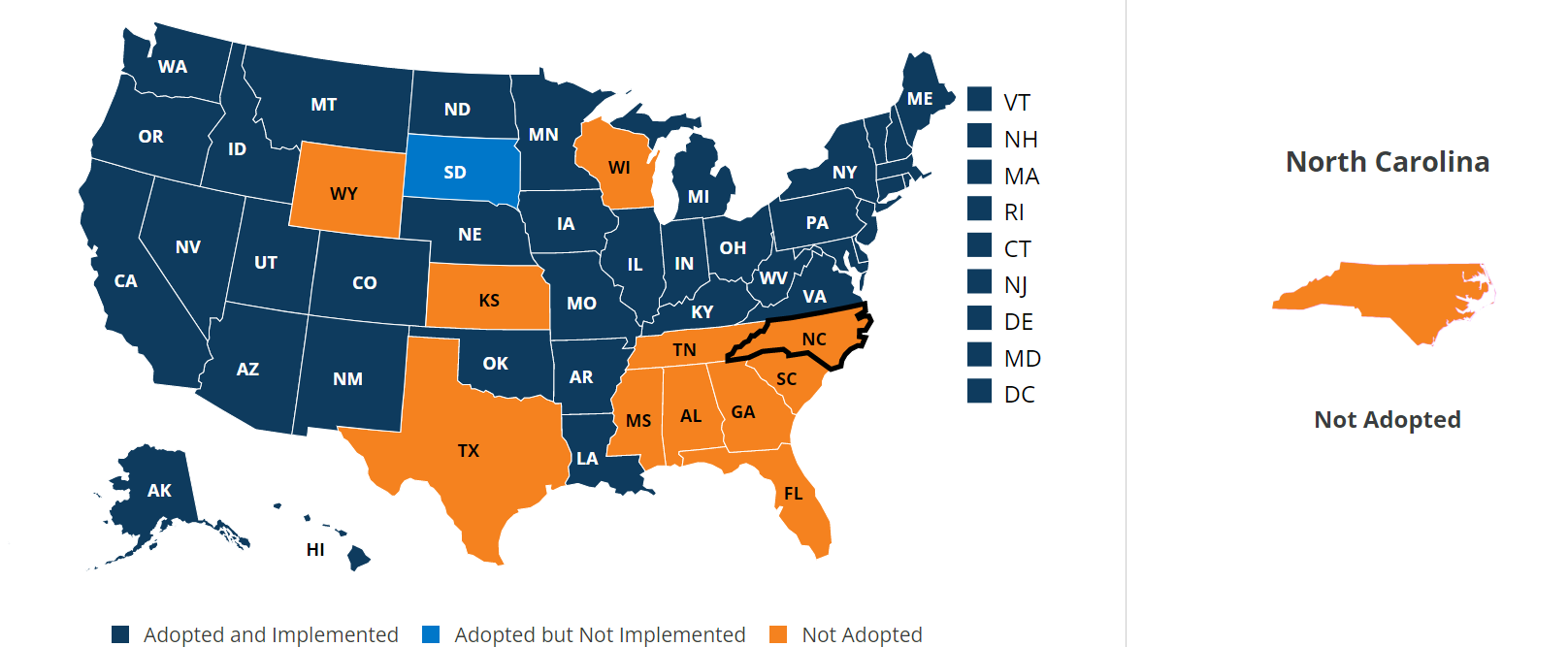
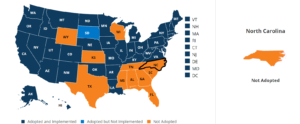
As 2022 comes to an end, millions of people who enrolled in the Medicaid public health insurance program during the Covid pandemic could lose their coverage early next year. That is if their state determines they no longer meet the program’s eligibility requirements and North Carolina is on that list.
Tucked inside a more than 4,000-page, $1.7 trillion bill that funds the federal government through September is a provision that would eliminate the Medicaid coverage protections from the public health emergency. Instead, states could start terminating recipients’ coverage in April 2023 if they no longer meet the program’s eligibility criteria.
Here is a map showing states and their current action on Medicaid expansion.
Winter solstice 2022: What you need to know about the shortest day of the year

As the southern hemisphere celebrates the start of summer, those north of the equator will experience the shortest day of the year, known as the winter solstice. This year, it falls on Wednesday 21 December, the first day of winter.
The word “solstice” derives from sol, the Latin word for sun, and sistere, which means “to come to a stop or make stand”.
For people who live in the Northern Hemisphere, today will be the one day of the year with the shortest period of sunlight. The solstice will begin on 4:48pm ET on 21 December, when the Earth is at its maximum tilt, 23.5 degrees, away from the sun.
For the Southern Hemisphere, it’s the opposite case, as 21 December marks the one day of the year with the longest period of sunlight.
Historically, the winter solstice has been of great importance to many cultures, such as Ancient Egypt and Ancient Rome, often as a marker for the passing seasons, and a possible time of rebirth.
In northern Europe, from the Faroe Islands to Estonia, Germanic peoples have long celebrated the event, which became known as Yule.
While Yule dates back to the Norse people, who celebrated the sun’s rebirth for 12 days, it was also celebrated by Anglo-Saxon pagans.
According to Pliny the Elder, in Britain, druid priests would mark the important date by gathering mistletoe and sacrificing bulls – which was also likely a practical measure to limit the number of mouths to feed during months of famine.
In addition to mistletoe and 12 days of festivities, several Christmas traditions, such as Yule logs and decorating trees, date back to Yule, which were later adopted and adapted by Christians.
While winter may come with its bright holiday spots, figuratively speaking, these are also the darkest days of the year– in the literal sense. The sun rises at its latest, and sets at its earliest.
That could lead to Seasonal Affective Disorder.
Symptoms
The symptoms of Seasonal Affective Disorder look much like the same as symptoms of depression, with one key difference: the symptoms begin and end at around the same time each year. There are also a few common symptoms of depression that appear more frequently with SAD, like overeating, lethargy, and often, as a result of those two symptoms, weight gain. Other common symptoms of SAD include:
- Feelings of depression, which may include, hopelessness, poor self-esteem, guilt, apathy, and despair.
- More intense mood changes
- Trouble sleeping or oversleeping
- Irritability and the urge to isolate oneself
- Loss of libido
- Heightened and persistent anxiety
Coping with SAD
Below you’ll find some strategies for both treating and coping with SAD, all of which can be pursued together for the best results.
See your doctor
- Visit with your doctor to talk about your symptoms. One person’s SAD isn’t necessarily the same as the next, and your doctor will be able to help you understand it better and figure out what your options are
Light Therapy

Eat Well

Maximize your time in the sun

Keep to a regular sleep schedule

Exercise

Keep busy

One way to keep yourself away from the urge to hibernate is to keep your schedule full. This may mean throwing yourself into your work or your studies, or it might mean taking up a new hobby or project.
Socialize

Practice mindfulness


Medication
If your symptoms are relatively severe and don’t seem to be improving, treatment with antidepressants may benefit you. Talk with your doctor to learn more about
pharmaceutical treatment options.
The 988 Suicide and Crisis Lifeline provides free and confidential emotional support to people in suicidal crisis or emotional distress 24 hours a day, 7 days a week, across the United States. Call or text 988, to be connected to the Suicide and Crisis Lifeline or connect via chat at 988lifeline.org
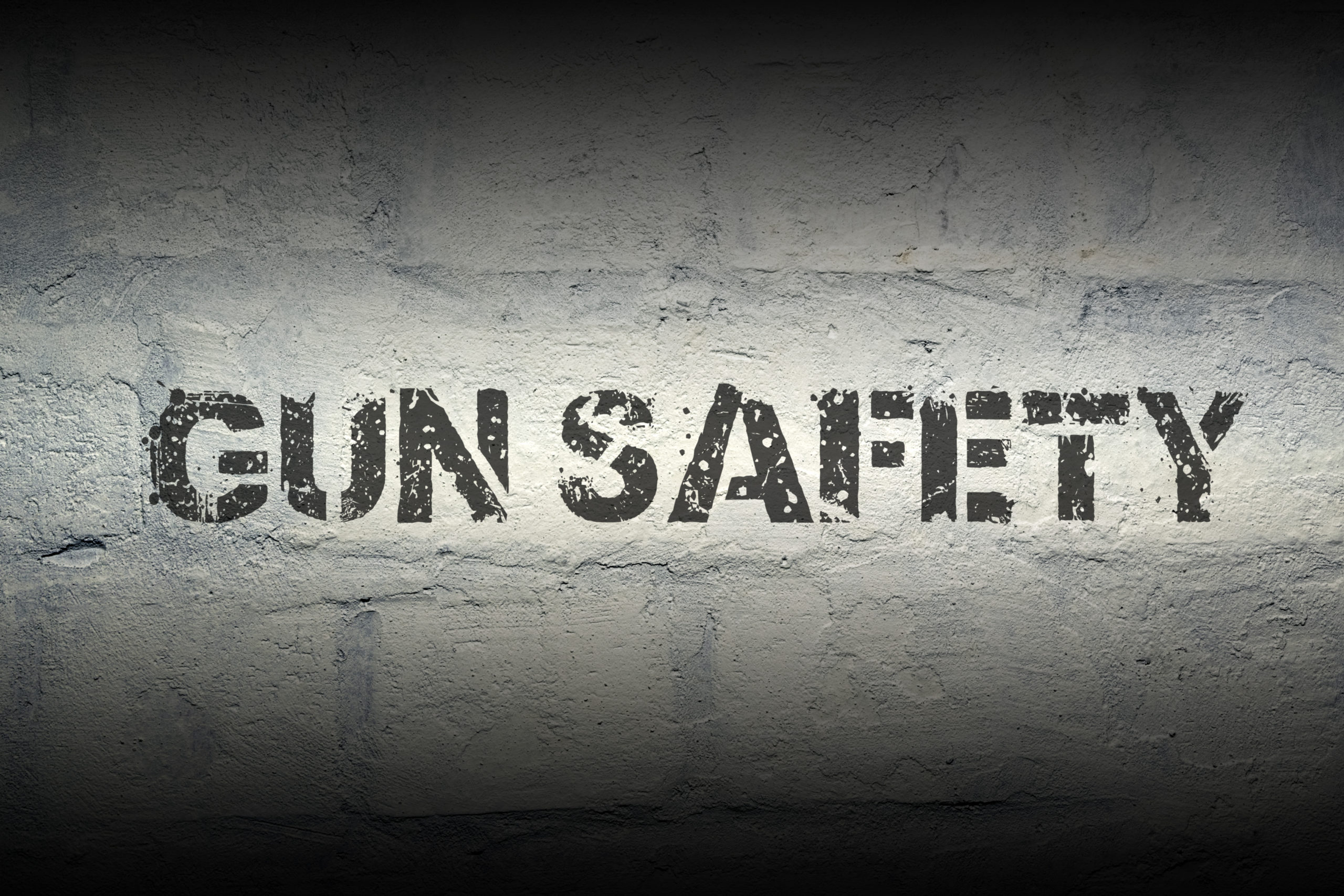
DOCMS December Meeting Highlights - “Prevention of Firearm Injury”

The Durham Orange County Medical Society met December 14, 2022 at the University Club of Durham to talk about the prevention of firearm injury.
DOCMS invited the medical community of Durham Orange County to learn about firearm policy in NC and to discuss opportunities to intervene and prevent firearm injury in our communities. This discussion was moderated by Nancy Henley, MD.
Guest speakers included:

Becky Ceartas is the Executive Director of North Carolinians Against Gun Violence (NCGV) and has been leading the organization since 2014. She has 22 years of experience with non-profit organizations. Becky became involved in gun violence prevention work after the Sandy Hook tragedy. As a new mom, she was compelled to take action. She now works with volunteers and supporters to fulfill NCGV’s mission, which is to make North Carolina safe from gun violence through educating the public about preventing gun violence, enforcing current laws, and enacting needed new laws.
To download the Ceartas Presentation click here

Dr. Brian Eichner is Assistant Professor of Pediatrics at Duke in the Division of General Pediatrics and Adolescent Health and has been at Duke since 2006. Since starting at Duke, he has been interested in the pediatrician's role in preventing gun injury and death and has spoken on this topic in various venues and works with his colleagues on how to discuss firearm injury prevention with families and has worked to improve the provision of gun locks at well child visits across the Duke network. His clinical interests are in the primary care of children with medical complexity and his current research interests are in the early diagnosis of developmental delay and autism.
To download the Eichner presentation click here.
Catalent Expanding in North Carolina

(The News & Observer, Brian Gordon, 12/14/22)
Catalent, a large biotech company based in New Jersey, has announced plans to expand its North Carolina footprint with a new facility — and new jobs — in Research Triangle Park. The firm received a Job Development Investment Grant, or JDIG, from the North Carolina Economic Investment Committee (EIC) to create 201 new jobs over the next five years on the Durham County side of RTP.
Catalent, which partners with pharmaceutical companies to develop and manufacture medicine, will use the site for testing and analytical development. It’s pledged to invest $40 million in the project. The total value of the state’s JDIG is $1,074,000, which the EIC approved Tuesday.
More than $800,000 of the award will be available to Catalent through payroll tax rebates, which will materialize if the company meets annual hiring and investment commitments. The rest of the grant — roughly $268,000, will be put into the state’s utility account, which funds infrastructure improvements in rural areas seeking further economic development. [Source]
HCA Healthcare, Mission Health Push Back on Monopoly Claims in Western NC

(Asheville Citizen-Times, Andrew Jones, 12/14/22)
HCA Healthcare and Mission Health are pushing back on claims they run a monopolistic organization in Western North Carolina, something six area plaintiffs have been trying to prove in court for more than a year.
A Dec. 5 motion to dismiss in WNC’s first antitrust lawsuit against Mission and HCA — so complex that it was in January removed from Buncombe’s Superior Court early and is currently working its way through North Carolina Business Court — claims plaintiffs’ monopoly arguments are lacking proof and fail to properly allege Mission did or is doing anything wrong when it comes to monopoly power.
Specifically, HCA and Mission are fighting new alleged proof that they control a monopoly not only in Asheville but in areas outside WNC’s largest metropolitan footprint, which the lawsuit calls the “outlying” markets. These include Yancey, Transylvania, McDowell and Macon Counties, though Mission Health claims to serve 18 counties near the mountains.
On Oct. 31, plaintiffs’ attorneys filed a revamped complaint that reiterated all the claims made when it was originally filed on Aug. 10, 2021, but also adding data from CMS Medicare discharges, an IBM Watson analysis, the North Carolina Hospital Association, hospital license renewal applications and HCA’s certificate of need application to build 67 new acute care beds at its Asheville location.
Plaintiffs’ attorneys added the new data to double down on an argument they already had made and which Business Court Judge Mark Davis found lacking in a Sept. 19 ruling, namely that HCA doing business as Mission doesn’t hold monopoly power in both Asheville and the outlying markets. Davis noted Medicare data plaintiffs were almost exclusively used to make this argument weren’t enough to prove the monopoly point. He did, however, agree that there was validity to an argument alleging HCA’s operations in WNC restrain trade and could therefore be inflating prices and stifling competition. Though Davis in his opinion dismissed the monopoly arguments, he didn’t do so with prejudice, leaving room for plaintiffs’ to make their new data-oriented argument.
But HCA — the largest hospital system in the U.S. and the purchaser of Mission Health in 2019 for $1.5 billion — in its latest motion to dismiss claims that data argument doesn’t hold water.
Part of its argument against culpability for monopoly practices lies in the fact that Mission already had massive, monopoly-sized ownership of WNC healthcare operations before it was purchased by HCA. Following the new complaint and new motion to dismiss, Davis will have an opportunity to issue a new opinion on the case, one which plaintiffs hope will accept not only the anti-competitive argument but also the monopoly case. (Source)
NCMS reported earlier this year that HCA Healthcare opened a $68 million hospital in Franklin, N.C.. Angel Medical Center is part of HCA’s Mission Health, which is based in Asheville, N.C. For more on that story click HERE.
NC Covid Cases Rise, Hospitals See Overcrowding, State Launches New Telemedicine Program
New COVID-19 cases are climbing again in North Carolina in a sign that Thanksgiving-related spread continues. WNCN reports new cases were up 13 percent last week to nearly 13,000 — the highest weekly total since late September — according to an update Wednesday from the state Department of Health and Human Services.
That is leading to an increase in hospital admissions, up 8 percent in the week of December 3-10. Also noted is an increase in COVID particles in wastewater and more emergency room visits with symptoms of the disease. (SOURCE)
The increase in hospital admissions is leading to headaches in triangle-area hospitals. They are facing major bed space concerns along with concerns over staffing. Celeste Garcia of North Carolina Public Radio says Duke University Hospital and UNC Medical Center are re-purposing certain beds to make more space for patients. At Duke University Hospital, patients and staff are again required to wear masks, wash their hands often and stay home from work if they feel any symptoms (SOURCE)
As a result, North Carolina has launched a new telemedicine program designed to increase access to treatment for COVID-19.
WFDD Radio says the program is the result of a partnership between the North Carolina Department of Health and Human Services and StarMed Healthcare. It supports free telemedicine appointments to gauge COVID-19 treatment eligibility for people who have tested positive via an at-home test or other methods. Health officials say that early treatment following a positive test is key to avoiding serious illness, hospitalization, or post-COVID conditions known as long COVID. (SOURCE)
Stephen "tWitch" Boss Dead at 40, NCMS Reminds You of 988 National Suicide and Crisis Lifeline

Multiple news outlets are reporting the death of 40-year-old Stephen "tWitch" Boss, known for his work on "The Ellen DeGeneres Show."
NBC News reports Boss died by suicide, according to multiple sources familiar with the investigation.
NBC News obtained a statement from his wife, Allison Holker Boss: “It is with the heaviest of hearts that I have to share my husband Stephen has left us."
“Stephen lit up every room he stepped into. He valued family, friends and community above all else and leading with love and light was everything to him. He was the backbone of our family, the best husband and father, and an inspiration to his fans. To say he left a legacy would be an understatement, and his positive impact will continue to be felt.
“I am certain there won’t be a day that goes by that we won’t honor his memory. We ask for privacy during this difficult time for myself and especially for our 3 children. Stephen, we love you, we miss you, and I will always save the last dance for you.”
tWitch and Allison celebrated their 9th anniversary last week. He leaves behind three children.
The North Carolina Medical Society has covered suicide help extensively, including training workshops. NCMS remains committed to helping our members and all North Carolinians who are considering suicide. Read our official policy HERE.
Statistics for physician suicide are shocking. Our most recent piece is available HERE.
If you or someone you know is in crisis, call 988 to reach the Suicide and Crisis Lifeline.
With Fentanyl-Related Deaths On Rise, Is It Time for Change In NC Good Samaritan Law?

(The Charlotte Observer, Kallie Cox, 12,12,22)
A coalition of advocates, including parents who have lost children to overdose deaths, is calling on legislators to expand North Carolina’s Good Samaritan Law. One key change they want is for fentanyl — the biggest driver of fatal overdoses — to be listed alongside drugs like cocaine and heroin. These advocates say North Carolina’s law is behind most of the rest of the country when it comes to saving lives claimed by drug overdoses.
Namely, due to the recent re-classification of fentanyl possession as a felony, it is not covered under the state’s Good Samaritan Law. Expand Good Sam NC, the coalition advocating for change, argues that those who use drugs are terrified to call 911 to report an overdose because of loopholes in the law that can lead to legal repercussions and arrest.
Fentanyl was recently re-classified as a felony drug in the state, meaning the law does not protect those who overdose on it. If bystanders — those who witness someone overdosing on fentanyl — are themselves in possession of the drug, they do not automatically have legal protections. A person who calls for help about their own overdose on fentanyl can also be prosecuted.
“People do not want to call 911,” said Lauren Kestner, Queen City Harm Reduction’s associate director. “So fentanyl expansion is not only required because (our law) was the weakest across the U.S. but also because now fentanyl is pretty much dominating the drug supply.”
The number of fentanyl-related overdose deaths in North Carolina has steadily increased each year since 2016 when deaths rose from 442 to 3,163 in 2021, according to the state Department of Health and Human Services. In 2021 in North Carolina, dying of an overdose was nearly three times more common than dying in a car accident. That’s even when traffic deaths in the state were at an all-time 20-year high according to U.S. News and World Report. There were 3,304 overdose-related deaths in 2021 — the overwhelming majority involved fentanyl — and 1,755 traffic deaths. [Source]
Is Gig Economy Harming Your Patient's Health?
(HealthDay, Dennis Thompson)

Capitalism is thought to bring out the best in workers, but there's a dark side to tying a person's everyday efforts to their weekly paycheck.
Folks relying on short-term, freelanced office jobs, or jobs where pay is linked to hustle -- depending largely on tips, commissions and bonuses -- may often suffer poor health related to their financial insecurity, new research has shown.
Employees with fluctuating and unpredictable pay tend to have poorer sleep, more stress and miserable physical symptoms that affect their work and home life, said lead researcher Gordon Sayre, an assistant professor of organizational behavior at Emlyon Business School in France.
Those symptoms grow worse as a person’s finances become more unstable, Sayre said, and the amount of savings they might have on hand seems to provide no solace.
"There's a lot of research looking at how performance-based pay, commission-based pay, piece-
rate based pay leads to higher levels of motivation or higher levels of performance. That's been sort of fairly well-established, and that’s one of the reasons why these pay practices have become popular," Sayre said.
"But there are some costs to these types of pay arrangements, and we need to consider them in addition to the performance benefits they bring," he added. "They also have these health costs."
Millions of Americans are in jobs where they can't count on a steady salary.
About 57 million Americans -- more than one-third of the U.S. workforce -- work in the "gig economy," taking piece work as freelancers, Uber drivers, food deliverers, landscapers and temp office employees, Sayre said in background notes.
Another 4.8 million work for tips as waiters, hair stylists, taxi drivers and nail technicians, and nearly 15 million work at desks in sales jobs where commissions and performance bonuses are the rule.
The problem is that these people aren't fully in control of what they make, Sayre said. They can be incredibly talented and put in a lot of work, but their efforts can be easily undermined by a tight economy, a business dry spell or a cheapskate customer who won't tip.
o see how unstable pay might affect these workers, Sayre conducted a series of three studies.
In the first, he asked 85 U.S. workers who rely on tips to answer daily online surveys for two weeks about their total daily pay and health.
Participants said tips accounted for a quarter of their total income on average, but they only received tips 4 out of 5 work days.
"Tipped workers who experienced more volatility in their pay over the two weeks that I followed them also tended to report more physical symptoms at the end of those two weeks," Sayre said. "Things like headaches, stomach aches, backaches, eye strain. And they also reported more symptoms of insomnia."
To find out why this is happening, Sayre conducted another study of 375 workers with Amazon's Mechanical Turk, a website where gig workers are paid small fees for piecemeal tasks.
The participants completed weekly surveys for three weeks, with health findings similar to the study on tipped workers.
Sayre found that MTurk workers who experienced extreme swings in pay tended to develop what he calls a "scarcity mindset."
"That's referring to financial worry, financial rumination, worrying about having enough money to make ends meet, worried about being able to cope with unexpected bills, that sort of thing," Sayre said.
Beyond the toll taken by stress, people constantly preoccupied by financial worries tend to neglect other factors in their lives that are important to their health, he said.
"You're focused on remedying that source of scarcity, whether it's earning more money by working more, whether it's trying to find other sources of income, or whether it's focused on budgeting more to save money," Sayre said. "And you're not so worried about eating a healthy dinner or getting your hour of exercise that day because you have basically more pressing issues on your mind."
However, one question remained: Is this a phenomenon only seen in people who are scraping by, or does it affect anyone whose paycheck depends on factors outside their control?
To address that, Sayre conducted a third study involving 252 higher-income employees in finance, marketing and sales, who answered monthly surveys for three months. These people tended to be heathier when their pay was less reliant on commissions or bonuses, he found.
"The relationship is somewhat weaker among these employees that are earning more money, but for people who are highly reliant on volatile forms of pay -- in other words, their monthly commission makes up 40% or 50% or 60% of their total take-home pay -- for those people, I still see this relationship where more volatility predicts more physical health symptoms," Sayre said.
Interestingly, the amount of savings a person had no effect on the stress caused by the scarcity mindset, Sayre found.
People also weren't able to counter their pay-related worries by using techniques like mindfulness, a practice in which people alleviate stress by focusing on the present moment.
"I was surprised -- and not, at the same time -- that mindfulness didn't really impact on it," said Dr. Philip Muskin, a professor of psychiatry at Columbia University Irving Medical Center in New York City. "Because being mindful in your approach to things doesn't pay the bills, and paying the bills for many people is very scary."
It's not just waiters, car salespeople or ad execs who are likely to feel the effects highlighted by Sayre's research, Muskin suspects. Even professionals like doctors and lawyers are under pressure to see more patients or run up more billable hours, with their pay depending on how fast they hustle, he said.
"I think this is not just applicable to gig workers or people sort of at the lower end of income earning. I think this is throughout our society," Muskin said. "And yeah, maybe people who are earning $1 million a year and they didn't get as big a bonus, I’m not going to feel so badly for them, but I treat people like that, and you know, it makes them anxious, too."
These study results align with what's already known about "people having basic psychological needs to feel in control, to feel autonomous and to be able to sort of predict their environments," said Mindy Shoss, an associate professor of industrial/organizational psychology at the University of Central Florida.
"It's this inability to predict and control something as important as the amount of money you take home at the end of the day that really matters," she said.
Based on these results, businesses should reconsider whether performance-based pay really helps their bottom line, Sayre said. They might get more out of workers who have stable compensation.
"It matters how dependent we are on volatile sources of pay," Sayre said. "So basically, if you're working a sales job and 80% to 90% of your pay comes from a steady salary, and you get a small commission or performance based bonus that makes up the other 10% to 20%, that's not so bad. You can handle volatility when it makes up a relatively small proportion of your pay."
The real problem is when people are highly reliant or entirely reliant on this "volatile" base of pay, he said.
"Organizations could keep these pay systems if they want, but just reduce employees' reliance on them and try to increase more predictable and stable levels of pay," Sayre said.
Muskin gave the example of a New York restaurant that did away with tipping, essentially raising its meal prices and doling out the extra charge equitably among all its workers.
"That is a solution at the corporate level, where you alter the pay arrangement so that people are not as dependent upon commissions, bonuses and tips," he said. "But then you still need some sort of incentive process so they don’t say, 'well, I'm getting paid for this so I don't have to work as hard.'"
Muskin pointed to the need to be creative.
There are systems that could be created if companies chose, where employees had a vested interest in the effort they put in so their pay was guaranteed, but their level of work is also reciprocated,” he said.
The new study was published Dec. 8 in the Journal of Applied Psychology.
More information
The Mayo Clinic has more about how stress affects your health.
GenX study finds Chemours-specific chemicals in residents
(Coastal Review Online, Trista Talton)
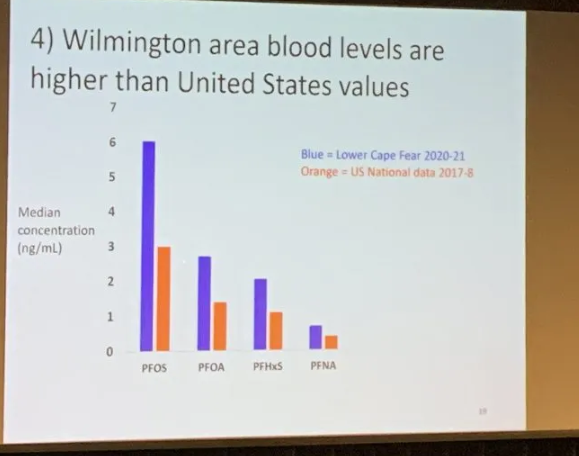
Many people living in the Cape Fear River basin who volunteered to take part in the most recent GenX exposure study had higher levels of four highly fluorinated compounds in their blood than the average American.
While GenX was not found in the blood samples of 1,020 residents in Wilmington, Fayetteville and Pittsboro, three per- and polyfluoroalkyl substances, or PFAS, unique to the Chemours Fayetteville Works facility were in the blood of almost everyone who participated in the 2020-2021 study.
The results of this latest GenX exposure study were discussed Wednesday evening during a public meeting hosted by Cape Fear River Watch in Cape Fear Community College’s Union Station.
Researchers with the North Carolina State University Center for Human Health and the Environment were quick to point out that while GenX was not found in blood samples, that does not mean people were not exposed to the chemical compound. That merely suggests GenX does not last in the blood for a long time.
PFAS found in blood samples from Wilmington-area residents were the same as those found in samples taken from residents who participated in the initial 2017-18 study.
Nearly everyone who participated in the study had perfluorooctanoic acid, or PFOA, perfluorooctane sulfonic acid, or PFOS, perfluorohexanesulfonic acid, or PFHxS, and perfluoronanoic acid, or PFNA.
Butner Substance Abuse Center Will Convert to Psychiatric Hospital for Children

(From Winston-Salem Journal, Richard Craver, 12/11/22)
The N.C. Department of Health and Human Services will convert a substance abuse treatment center in Butner into a 54-bed inpatient psychiatric hospital for children and adolescents. The conversion of the Blackley Alcohol and Drug Abuse Treatment Center is being conducted with UNC Health. The groups project opening the converted facility as early as July 1. They have signed a letter of intent and expect to finalize the agreement in January.
DHHS said that daily more than 250 people wait for behavioral health services in emergency departments, with 20% of them being children and adolescents. The groups said that many end up languishing in emergency rooms or other settings for days because North Carolina has historically lacked the inpatient capacity to meet the behavioral health needs of the community.
“This partnership allows us to move faster to stand-up services urgently needed today for children,” state Health Secretary Kody Kinsley said in a statement. “We will continue to invest and build out a continuum of community-based behavioral health care that prevents, treats and promotes lasting recovery.” Dr. Wesley Burks, UNC Health’ chief executive and dean of the UNC School of Medicine, said that pediatric and adolescent behavioral health “is the largest issue affecting the future health of our state.”
Adults seeking substance use disorder treatment will continue to have the option to receive services at the state’s remaining alcohol and drug abuse treatment centers, or from private providers in the area. At the time of conversion, all permanent employees at the Blackley facility will have an opportunity for continued employment with DHHS based on their skills and experience. Source
Cameron Crazies Could Soon Travel 'Coach K Highway'

(From The News & Observer, Mary Helen Moore, 12/08/22)
The route to Duke basketball games could soon take Cameron Crazies along “Coach K Highway.” Duke University has asked that a portion of N.C. Highway 751 be renamed in honor of longtime men’s basketball coach Mike Krzyzewski. Krzyzewski spent 42 seasons at Duke and won five national titles before retiring last year.
The three-mile section of N.C. 751 under consideration is between Duke University Road and Kerley Road. Also named Cameron Boulevard, it passes near Cameron Indoor Stadium and through Duke Forest. The Durham City Council will vote on a resolution in support of the renaming at its Dec. 19 meeting. The resolution, if unanimous, will kickstart an application to the state Department of Transportation. The NCDOT board gets the final say.
Duke agreed to pay the $2,000 that new signs are expected to cost. Duke’s rival UNC succeeded last year in getting two stretches of Interstate 40 renamed for legendary basketball coaches Roy Williams and Dean Smith. [Source]
Stiff-Person Syndrome and What You Need to Know

Multiple award-winning singer Celine Dion shocked the world Thursday, announcing she has a rare neurological disorder called Stiff-Person Syndrome (SPS).
In Dion's Instagram video she says: “Recently I have been diagnosed with a very rare neurological disorder called Stiff-Person Syndrome, which affects something like one in a million people. While we’re still learning about this rare condition, we now know this is what’s been causing all of the spasms that I’ve been having."
According to the National Institute of Neurological Disorders and Stroke, SPS has features of an autoimmune disease and is characterized by fluctuating muscle rigidity in the trunk and limbs, as well as a heightened sensitivity to stimuli such as noise, touch, and emotional distress, which can trigger muscle spasms. It’s often misdiagnosed as Parkinson’s disease, multiple sclerosis, or fibromyalgia. Researchers are still trying to understand the disorder, and currently there is no cure.
According to Yale Magazine, the cause of this extremely rare disease is still unknown. But researchers suspect that it may be the result of an autoimmune reaction where the body attacks nerve cells in the central nervous system that control muscle movement.
Symptoms can lead to difficulty walking and, over time, even greater disability. People with Stiff Person Syndrome are also more likely to have symptoms of depression and anxiety. In part, this is because of the unpredictability of the disease, but patients also have lower levels of the neurotransmitter GABA, which regulates anxiety.
Most people start experiencing symptoms between the ages of 30 and 60.
Reaching a diagnosis for Stiff Person Syndrome can be difficult. Generally, SPS is suspected based on characteristic symptoms. A comprehensive medical history and examination, along with additional investigations, including blood tests and spinal fluid analysis, can confirm the diagnosis. When conducting those tests, your doctor is looking for elevated levels of GAD antibodies.
Electromyography or EMG is also sometimes recommended to study the electrical activity of skeletal muscles. Your doctor will be looking for typical motor unit activity findings that are common in people with SPS.
Doctors will also rule out other possible causes of symptoms, including Parkinson’s disease, multiple sclerosis, fibromyalgia, psychosomatic illness, or anxiety and phobia.
There is no cure for Stiff Person Syndrome. When doctors treat patients with this condition, they focus on relieving symptoms with medications such as sedatives, muscle relaxants, and steroids. Intravenous Immunoglobulin and plasmapheresis, among other immunotherapies, may also be prescribed. Physical, occupational, and aqua therapy are also important for patients with SPS.
For more from Yale click HERE.
Potentially Landmark Class-Action Lawsuit Filed Against NC
(This story first appeared in Wilmington Star-News, 12/07/02 by Matthew Prensky)
Crystal Klunk’s daughter suffers inside one of North Carolina’s psychiatric residential treatment facilities — a place that resembles solitary prison confinement more than a care facility meant to help kids with mental health issues, the mom says. Spotty supervision, sporadic treatment and only occasional schooling have been part of the girl’s experience, Klunk said. They have not seen their daughter, who first tried to kill herself at age 10, in months. The staff at their daughter Alexis’ center reportedly has not updated Klunk on the teen’s status.
A six-month investigation in 2021 by North Carolina and Virginia journalists in the USA TODAY Network featured Klunk and other families, plus shocking details of neglect and abuse inside these locked centers. Now, citing the “Locked Away” reporting series, a potentially landmark class-action lawsuit has been filed in federal court against the state of North Carolina.
The lawsuit aims to reduce North Carolina’s focus on these institutions and to shift many children to more appropriate support services based in their home communities. The Middle District Court filing by Disability Rights North Carolina, the state NAACP and the children themselves cite gruesome allegations of kids subjected to physical, psychological and sexual abuse at these psychiatric centers — reports that were brought to light in the multi-part Locked Away investigation.
Plaintiffs claim there is a systemic effort by North Carolina health and human services officials to warehouse foster children with mental health disabilities in these locked wards. The state’s decisions have failed vulnerable children and wasted taxpayer money on what is a punishing and expensive system of centers, the filing says. The plaintiffs, which include four children and their guardians, want North Carolina to provide adequate and appropriate services in the community for foster kids who need mental health care. It will take an investment in a web of services at multiple stages of a kid’s mental health journey — and could be financed in part with ample dollars the state is currently sending to PRTFs.
Tuesday afternoon’s lawsuit alleges children inside PRTFs are confined to prison-like settings “under the care of a poorly trained and understaffed workforce, where they are subject to broken bones, sprains, bruises, and dangerous physical and chemical restraints; withstand sexual and physical abuse, bullying, and hate speech by both youth and staff; and face mental health deterioration and cocktails of strong psychotropic medications.”
“DHHS is failing hundreds of children with disabilities in foster care, warehousing them in dangerous, expensive, damaging institutions,” said Virginia Knowlton Marcus, chief executive officer of Disability Rights North Carolina. “These children deserve and have the right to a family and place in our communities where they can meet their full potential. Instead, they receive institutionalization and irreparable harm to their childhood and wellbeing.”
USA TODAY Network-North Carolina has reached out to the state Department of Health and Human Services for comment on the filing. The head of DHHS is the named defendant in the lawsuit, representing the state. [Source
NCMS Goes 'Over the Edge' for Special Olympics!

RALEIGH -- Members of the North Carolina Medical Society went Over The Edge Saturday to support Special Olympics North Carolina!
They each rappelled 30 stories off the 150 Fayetteville Street building in downtown Raleigh (that is 30 stories)! It was to raise awareness for nearly 40,000 North Carolina athletes across the state.
Rappelling is used to demonstrate the courage people with intellectual disabilities face every day. You must have courage to try something that doesn’t come easily to you. Special Olympic athletes bravely face challenges on the field, in the pool and on the court. They are the inspiration for this event.
Over the Edge 2022 for Special Olympics North Carolina is part of the NCMS strategic planning initiative to create community involvement with new partners across the state. This was our 3rd year taking part to honor the medical providers that care for the athletes in this program.

(L-R) Eileen Raynor, MD (NCMS Board of Directors, President Elect), Evan Simmons, NCMS Director of Board and Executive Services, and Cynthia Gary, MPH, PA-C (NCMS Foundation Board of Trustees Member)
Donations are still being accepted. If you would like to support Special Olympics North Carolina, click HERE.
Are You Ready for Interoperability?

That’s interoperability in a nutshell—being able to share patient information easily between different doctors and computer systems to make patient care easier (and save costs, like unnecessary blood tests). Full interoperability would also mean this imagined ER doc would have been alerted upfront that the bloodwork was done, so the onus isn’t on the patient.
That’s not possible today, given that many systems in healthcare are unable to communicate with each other, according to Amit Trivedi, senior director of informatics and health IT standards at the nonprofit Healthcare Information and Management Systems Society. Getting to that point will take significant change and investment in new technology.
But when it comes to adopting new technology, the healthcare industry “tends to be conservative and risk averse, because at the end of the day, any change has to be looked at through the lens of patient safety,” Trivedi said.
Despite that, change is coming. In a big step toward increasing interoperability, an Oct. 6 federal rule now requires that healthcare facilities give patients access to their complete digital health records.
The healthcare industry is working to advance interoperability because it would make patient care a lot easier if providers were able to access a fuller understanding of a patient’s health history. It would also have big implications on population health, as it would give regulators, like the CDC, a much fuller picture of who’s contracting diseases and where, Trivedi said.
NC Case on Congressional Districts Going Before US Supreme Court Wednesday

(This article is from Mark Sherman , The Associated Press, 12/4/22)
The Supreme Court is about to confront a new elections case, a challenge asking the justices for a novel ruling that could significantly increase the power of state lawmakers over elections for Congress and the presidency. The court is set to hear arguments Wednesday in a case from North Carolina, where Republican efforts to draw congressional districts heavily in their favor were blocked by a Democratic majority on the state Supreme Court because the GOP map violated the state constitution. A court-drawn map produced seven seats for each party in last month’s midterm elections in highly competitive North Carolina.
The question for the justices is whether the U.S. Constitution’s provision giving state legislatures the power to make the rules about the “times, places and manner” of congressional elections cuts state courts out of the process. “This is the single most important case on American democracy -- and for American democracy -- in the nation’s history,” said former federal judge Michael Luttig, a prominent conservative who has joined the legal team defending the North Carolina court decision.
The Republican leaders of North Carolina’s legislature told the Supreme Court that the Constitution’s “carefully drawn lines place the regulation of federal elections in the hands of state legislatures, Congress and no one else.”
Three conservative justices already have voiced some support for the idea that the state court had improperly taken powers given by the Constitution when it comes to federal elections. A fourth has written approvingly about limiting the power of state courts in this area. But the Supreme Court has never invoked what is known as the independent state legislature theory. It was, though, mentioned in a separate opinion by three conservatives in the Bush v. Gore case that settled the 2000 presidential election.
If the court were to recognize it now, opponents of the concept argue, the effects could be much broader than just redistricting. The most robust ruling for North Carolina Republicans could undermine more than 170 state constitutional provisions, over 650 state laws delegating authority to make election policies to state and local officials, and thousands of regulations down to the location of polling places, according to the Brennan Center for Justice at the New York University School of Law.
Luttig, who advised former Vice President Mike Pence that he had no authority to reject electoral votes following the 2020 election, is among several prominent conservatives and Republicans who have lined up against the broad assertion that legislatures can’t be challenged in state courts when they make decisions about federal elections, including congressional redistricting. That group includes former California Gov. Arnold Schwarzenegger, law professor Steven Calabresi, a founder of the conservative Federalist Society and Benjamin Ginsberg, a longtime lawyer for Republican candidates and the party.
“Unfortunately, because of ongoing and widespread efforts to sow distrust and spread disinformation, confidence in our elections is at a low ebb,” Ginsberg wrote in a Supreme Court filing. “The version of the independent state legislature theory advanced by Petitioners in this case threatens to make a bad situation much worse, exacerbating the current moment of political polarization and further undermining confidence in our elections.”
The arguments are taking place a day after the final contest of the 2022 midterms, the Georgia Senate runoff between Democratic Sen. Raphael Warnock and Republican Herschel Walker. In that contest, state courts ruled in favor of Democrats to allow for voting on the Saturday before the election, over the objections of Republicans.
Jason Snead, of the conservative Honest Elections Project, said the case is an opportunity for the high court to rein in out-of-control state courts which are being pushed by Democratic attorneys to effectively create new rules governing voting, including the Georgia example. “We’ve seen a fairly pervasive attempt to use courts to rewrite election laws if those laws don’t suit partisan agendas,” Snead said in a call with reporters. “That’s not something we want to see when it flies in the face of the Constitution.”
He is among proponents of the high court’s intervention who argue the case doesn’t represent “a threat to democracy.” The justices can instead write a narrow opinion that places limits on state courts without upsetting the choices New York and other states have made to restrict partisan redistricting, a group of New York voters wrote in a court filing. The New Yorkers implicitly recognize that if the court gives more power to state legislatures over drawing congressional lines, Republicans may not necessarily benefit.
During the last redistricting cycle, states that used independent redistricting commissions rather than legislatures were largely Democratic-dominated ones. Commissions drew 95 House seats in states with Democratic legislatures and governors, as opposed to only 12 in states with GOP control. A ruling that grants legislatures ultimate power over redistricting could eradicate those commissions and let Democrats redraw a major chunk of the House map.
“The bottom line is the impact of this fringe theory would be terrible,” said former Attorney General Eric Holder, chairman of the National Democratic Redistricting Committee. “It could unleash a wave of gerrymandering from both parties.” Even less dramatic changes may not necessarily tilt the GOP’s way on a national redistricting map that was essentially fought to a draw, and where state court rulings cost Democrats about as many House seats as Republicans.
The Supreme Court refused to step into the North Carolina case in March, allowing the court-drawn districts to be used this year. Justices Samuel Alito, Neil Gorsuch and Clarence Thomas dissented. Writing for the three, Alito said “there must be some limit on the authority of state courts to countermand actions taken by state legislatures when they are prescribing rules for the conduct of federal elections. I think it is likely that the applicants would succeed in showing that the North Carolina Supreme Court exceeded those limits.”
Justice Brett Kavanaugh has separately written about the need for federal courts to police the actions of state courts when it comes to federal elections.
Chief Justice John Roberts’ record on this question gives both sides some hope. In 2015, he wrote a strong dissent from the court’s decision upholding an independent redistricting commission in Arizona. Roberts wrote that the Constitution does not permit “a state to wholly exclude ‘the Legislature’ from redistricting. ” But in 2019, Roberts wrote the court’s majority opinion that closed federal courts to claims of partisan gerrymandering but noted state courts remained open. “Provisions in state statutes and state constitutions can provide standards and guidance for state courts to apply,” he wrote, in an opinion joined by Alito, Gorsuch, Kavanaugh and Thomas. The court’s other conservative justice, Amy Coney Barrett, has no track record in this area.
In North Carolina, a new round of redistricting is expected to go forward next year and produce a map with more Republican districts, whatever the outcome of the high-court case. In last month’s elections, voters flipped the majority on the state Supreme Court, electing two new Republican justices that give the GOP a 5-2 edge and make it probable, though not certain, that the court would uphold a map with more Republican districts. [Source]
Work in Moore County? Need NCMS Help?

As widespread power outages caused by vandalism continue in Moore County, the North Carolina Medical Society is looking to help our affected members.
With power out to businesses possibly stretching into Thursday, NCMS wants to remind you that we are a resource for our members.
Duke reported about 38,000 residences and businesses remained without power Sunday. It provides power to nearly the entire county. The outage hit Moore Regional Hospital, which switched to generator power. A hospital spokeswoman in a message to staff said the outage did not affect patients. “The Moore campus is safely operating on backup generator power and we have not experienced any issues or concerns,” Gretchen Kelly said. Kelly told The N&O on Sunday that the hospital has enough fuel on hand for several days for generator power and plans in place to obtain more fuel as needed.
If you have questions or concerns about your practice or patients, or help finding resources, please reach out to your NCMS Team.
NCMS Gets Into Holiday Spirit Early!

Happy Holidays from the staff of the North Carolina Medical Society!
On December 2, CEO Chip Baggett hosted the NCMS final staff meeting of 2022. It was a chance to celebrate the successes of the year, including the return of the LEAD Conference and the first Golden Stethoscope Awards Gala. Chip lauded the staff, Board of Directors, and NCMS members for working through the pandemic and building on our long history of supporting quality healthcare in North Carolina.
He also took time to look forward at a bright 2023 on the horizon for NCMS!
It was no prob-llama in his amazing holiday sweater!
NCMS CEO Chip Baggett getting into the holiday spirit!
The team had a raucous White Elephant Gift Exchange, where the gifts ranged from used Christmas lights, to books, to a some prized holiday decor!





We also prepared to say goodbye to Gail Stephenson, Director of Event Services, who is retiring this month. She is going off with some bling! This her response to her gift from Reeds Jewelers.

As always, everyone at NCMS is looking forward to meeting with our members and working hard!
Here's to 2023!
Is Long Covid the Next Public Health Disaster?

As the United States prepares to enter its fourth calendar year of the coronavirus outbreak, it could also be facing a tough winter. Some new studies suggest that most Americans have had COVID-19 already and the DCD says 2,000 more are still dying each week. Now, long Covid is becoming a concern.
The number of people who are suffering from long Covid are rising and the impact is far reaching. In addition to the toll on health, long Covid also creates issues with disability benefits, life insurance, household debt, retirement and financial ruin.
David Cutler of Harvard University says, all told, long Covid is a $3.7 trillion drag on the U.S. economy — about 17% of our nation’s pre-pandemic economic output. The aggregate cost rivals that of the Great Recession, Cutler wrote in a July report.
With that, a debate still seems to rage about what long Covid actually is. Some studies say women and people of color are higher risk and could also be more likely in bisexual and trans people.
Treatments vary and have different degrees of success. Greg Iacurci wrote an in-depth piece for CNBC about the physical and economic toll of long Covid. Read his insights by clicking here.
Wanted: Surgical Service Teams for AHRQ Safety Program
The Agency for Healthcare Research and Quality is recruiting teams to participate in the AHRQ Safety Program for MRSA Prevention.
It is a FREE 18-moonth program that seeks to reduce surgical site infections with a focus on those caused by methicillin-resistant Staphylococcus aureus (MRSA).
The program begins next month and participants will receive technical assistance, coaching, webinars, and tools to support your infection prevention program.
Continuing education credits will be offered at no charge.
For full information and how to participate click here.
Advent Gets Nod for Buncombe Hospital, Other Contenders Consider Fighting Decision

Florida-based Advent Health, which operates a hospital in Hendersonville, has been approved by the North Carolina Department of Health and Human Services to build a 67-bed acute care facility in Buncombe county. It was announced via Twitter on November 22. Blue Ridge Public Radio says the statement was confirmed by Advent spokesperson Victoria Dunkle, but has not been posted on the NCDHHS website, which lists decisions on a monthly basis.
BPR notse that The N.C. 2022 State Medical Facilities Plan, released earlier this year by the NC Department of Health and Human Services (Division of Health Service Regulation) determined Buncombe, Graham, Madison and Yancey counties will have a projected need of 67 additional acute care beds by 2024.
Advent was one of three contenders. Nashville-based HCA Healthcare which operates Mission Hospital System and Winston Salem-based Novant Health, which operates hospitals in parts of central North Carolina and in South Carolina also put in bids. You can find more on the proposed plans here. Both companies say they they are considering fighting the decision.
In August, the state held a public hearing on the three proposals in Asheville. You can find out more about the application and review process here.
Advent’s plan proposes a site at the Enka Center off Smokey Park Highway in the county’s Enka Candler Community, with a completion date of 2025.
World AIDS Day Events Across North Carolina
Today is World AIDS Day. It is a day for people worldwide to unite in the fight against HIV, to show support for people living with HIV, and to commemorate those who have died from an AIDS-related illness.
Founded in 1988, World AIDS Day was the first ever global health day. Despite only being identified in 1984, more than 35 million people have died of HIV or AIDS related illnesses, making it one of the most destructive pandemics in history.
Globally, more than 40 million people have died from AIDS-related illnesses since the start of the pandemic. Here in the US, according to HIV.gov, about 1.2 million Americans currently have HIV and more than 700,000 have died from the virus.
In North Carolina the latest statistics show that nearly 35,000 people are living with HIV.
Today you can show your support for them at events across the state. Here are a few:
- 24th Annual World AIDS Day Symposium in Chapel Hill
- Seeds of Healing Red Ribbon Event in Wilmington
- World AIDS Day Awareness Event in Charlotte
- Rock the Ribbon in Hickory
There are several other events planned across the state throughout the weekend. Please click here for more opportunities.
North Carolina Awards Honor Two State Doctors

RALEIGH -- The North Carolina Department of Natural and Cultural Resources has announced the 2022 recipients of the North Carolina Award.
Established by the General Assembly in 1961, the North Carolina Award is the highest civilian honor given by the state. Presented annually since 1964, the award recognizes significant contributions to the state and nation in the fields of fine art, literature, public service and science. Though given by the governor, the award is administered by our agency.
History of the Award
Since its inception, more than 250 notable men and women have been honored by the state of North Carolina. Past recipients include William Friday, Romare Bearden, James Taylor, Gertrude Elion, John Hope Franklin, David Brinkley, Maya Angelou, Billy Graham and Branford Marsalis.
2022 Honorees
The 2022 honorees are the Honorable Eva Clayton for Public Service, Honorable Mickey Michaux for Public Service, Eric Church for Fine Arts, David Zucchino for Literature, Dr. Stanley Riggs for Science and Dr. Priya Kishnani for Science.
“These individuals have enriched North Carolina and our nation through their extraordinary accomplishments,” said Reid Wilson, secretary of the N.C. Department of Natural and Cultural Resources. “Each of them has enhanced the lives of North Carolinians through their lasting achievements in the arts, literature, sciences and public service.”
Since the award’s inception, more than 250 notable men and women have been honored by the state of North Carolina. Past recipients include Selma Burke, William Friday, James Taylor, Etta Baker, Charles Kuralt, Maya Angelou, Lee Smith and Branford Marsalis.
Fine Arts: Eric Church
Eric Church was born in Granite Falls, N.C., where his musical journey began at the age of 13 when he started writing songs and taught himself how to play the guitar. He earned a degree in marketing from Appalachian State University before moving to Nashville to pursue a music career. A multi-ACM and CMA Award winner, including the 2020 award for CMA Entertainer of the Year, Church has also earned numerous GRAMMY nominations while amassing a passionate fanbase around the globe known as the Church Choir. In 2013, Church and his wife Katherine founded the Chief Cares Fund, a charitable giving organization that provides aid to those in need, in both the U.S. and around the world.
Public Service: Honorable Eva M. Clayton
Eva M. Clayton, the first African American woman to represent North Carolina in Congress, was also the state’s first Black representative since 1901 when she took office in the closing months of the 102nd Congress in 1992. Clayton, a staunch defender of rural and agricultural interests, revived the Rural Caucus along with Missouri Republican Jo Ann Emerson. They rallied more than 100 House members who pledged to continue federal aid to farmers, create new rural jobs, and expand technology initiatives. After retiring from Congress in January 2003, Clayton spent three years in Rome, Italy, as Assistant Director-General of the Food Agriculture Organization (FAO) of the United Nations. There, she facilitated the establishment of 24 National Alliances to reduce hunger, malnutrition and poverty in countries around the world.
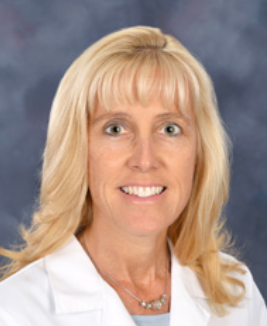
Science: Priya S. Kishnani, M.D.
Dr. Priya S. Kishnani followed a path into medicine first blazed by her mother, a pediatrician in India. She has treated patients and conducted groundbreaking basic and clinical research at Duke University School of Medicine for close to 30 years. Currently, Kishnani is the Chen Family Distinguished Professor of Pediatrics and the chief of the Division of Medical Genetics. Kishnani’s work applies basic science discoveries to clinical trials and pioneering approval of new therapies. Her innovative contributions translate laboratory science into treatment for people with lysosomal storage disorders (LSDs), glycogen storage diseases (GSDs), Down syndrome and other rare inherited disorders.
Public Service: Honorable H. M. “Mickey” Michaux Jr.
H. M. “Mickey” Michaux Jr. has spent more than 50 years as an activist, businessman and politician. He served in the N.C. House of Representatives from 1973-77 and later from 1983-2019. His time in the state House made him the longest serving member of the body. In 2020, at age 89, he was appointed to temporarily fill a seat in the N.C. Senate. Michaux was instrumental in preparing multiple state budgets as senior House Appropriations Committee chair and held numerous leadership positions in the House. Michaux was appointed in 1977 to serve as a U.S. attorney, becoming the first African American to serve in that role in the South since Reconstruction.
Science: Dr. Stanley R. Riggs
Dr. Stanley R. Riggs began his work as a marine geologist in the 1960s during a time when few people recognized the importance of climate change research. Riggs started working at East Carolina University in 1967 and spent 33 years teaching geology and tracking change within North Carolina’s coastal system. He was one of five scientists ECU recruited for its geology department to kickstart the university’s new geology and marine science program. He has published several books on coastal dynamics and climate change, including "Drowning the North Carolina Coast" and "The Battle for North Carolina’s Coast."
Literature: David Zucchino
David Zucchino, contributing writer for The New York Times and winner of the 2021 Pulitzer Prize for his book, "Wilmington’s Lie: The Murderous Coup of 1898 and the Rise of White Supremacy," has covered wars and civil conflicts in more than three dozen countries. Zucchino began his journalism career as a general assignment reporter at the Raleigh News and Observer. He then worked for 20 years at The Philadelphia Inquirer as the bureau chief in Beirut, Lebanon; Nairobi, Kenya; and Johannesburg, South Africa and worked as a foreign and national correspondent for the Los Angeles Times from 2001 to 2016, focusing on Afghanistan, Iraq and Libya. He is the author of “Thunder Run: The Armored Strike to Capture Baghdad” and “Myth of the Welfare Queen.”
Recipients got their awards on November 15 at an event at the North Carolina Museum of Art.
No Matter What You Celebrate This Season, Doctors Love These Gifts!

If you have a full staff you want to treat or a special someone you want to remember, there are plenty of great gift ideas.
This month people across the state will be shopping, wrapping, and exchanging gifts. NCMS thought we would help you get an early start with these ideas.
Some of our favorites include these syringe highlighters,

these anatomy coasters,

This "Spinal" tape,
and this hard-to-forget memory stick.

Whether you need a few or a lot, here is a great spot to start your shopping today.
Have fun!
How Does Cyber Monday Affect Your Practice?

Today is Cyber Monday. It is commonly known as the day Americans hit their computers, rather than stores. Economists have been predicting the eventual collapse of the brick-and-mortar commerce for more than a decade.
In an article in Forbes, Dr. Robert Pearl noted that the coronavirus pandemic came on like a retail wrecking ball in 2020, sending shopping-mall icons like Brooks Brothers, J. Crew and Neiman Marcus into bankruptcy.
1. Doctors must integrate technology with in-person care
It used to be that Black Friday was the end-all-be-all of shopping events. In fact, just eight years ago, a Walmart spokesperson said, “We think about Black Friday as if it were our Super Bowl.”
Cyber Monday, by contrast, always sat at the kiddy table—a holiday afterthought for most retailers. That’s no longer the case. In 2019, Cyber Monday sales hit $9.4 billion, besting Black Friday’s $7.4 billion. This year, amid a pandemic that’s pushing nearly all retail sales online, many traditional sellers are now combining their Black Friday sales with Cyber Monday, hoping to capitalize on the eCommerce opportunities they overlooked for so long.
The healthcare takeaway: Technology-based care belongs at the adult table, alongside office-based care. It’s a lesson many doctors still disregard.
Since the pandemic video visits have been declining. That’s a major error. Most patients want to keep using virtual care after the pandemic. So, instead of rolling back digital offerings, doctors should take a lesson from retailers this Cyber Monday and look for ways to combine digital tools with in-person services.
Of course, doctors can’t deliver all forms of care virtually. But they also can’t continue to overlook the evolving needs of patients either.
Just as online shopping alternatives shifted the balance of power between sellers and consumers, it is realigning the power dynamics in healthcare, too. Patients in need of medical advice, a prescription or specialty expertise once had no choice but to make in-person appointments at the convenience of a local doctor. Technology has changed all that. If physicians continue to resist (rather than embrace) modern IT solutions, patients will vote with their feet.
2. Doctors must combine technologies to maximize value, quality
A survey conducted in 1998 found that only 2% of U.S. healthcare providers had implemented a fully operational computer system in their offices. That same year, two-thirds of American families had a computer in their homes.
Like traditional retailers, most doctors are not “early adopters” of technology. And because many physicians struggle to integrate basic tech into their practices—including video visits, online scheduling and secure emailing—they are missing a much larger opportunity. Not only do these tools add convenience and value to the lives of patients, they can also greatly improve the quality of care provided.
One physician who has seized on this opportunity is Dr. Devi Shetty. The world-renowned heart surgeon currently maintains hospitals in his home country of India and in the Grand Cayman Islands. These facilities are separated by a dozen time zones and yet the two locations operate seamlessly as one. When the cardiology teams in India go home at night, their patients are monitored by physicians on the other side of the globe. And 12 hours later, flow reverses.
Consider how this approach would benefit at-risk patients in the United States, where hospital staffing slows down significantly on nights and weekends. Currently, when a patient experiences a dangerous drop in blood pressure or oxygenation overnight, it can take U.S. doctors an hour or more to notice and respond.
But with video monitoring and a shared medical-record system, doctors located anywhere in the country (or even in other parts of the world) could observe these patients and address their medical needs at the first sign of a problem, making sure no one falls through the cracks.
The future will reward physicians who embrace technology to provide high-quality medical care around the clock. Those who cling to the past will be left behind.
3. Doctors must be the disruptors, not the disrupted
Most of the time, the origins of disruptive innovation can be traced back decades, to an unfulfilled consumer need that a successful incumbent never saw—or recognized but chose not to address.
Nowhere is this truer than in American medicine. Independent research has long confirmed that the U.S. healthcare system is the most expensive and least effective in the developed world. Medical costs have bankrupted millions of patients and sent millions of others deep into debt. Among the world’s wealthiest nations, the United States has the lowest life expectancy, highest infant and maternal mortality rates, and the most preventable deaths per capita.
If ever there was a system primed for disruption, it is American healthcare. As the coronavirus pandemic continues to rage, most doctors are anxiously awaiting a return to “normal.” They will be sorely disappointed. Whether the disruptive innovations are led by big business, global competitors or entrepreneurial doctors and hospitals, the fact remains: Change is coming. The days of healthcare providers surviving by simply raising prices are gone.
People who prefer shopping online during Cyber Monday (rather standing in lines for Black Friday) ought to ask themselves: “What if getting medical care were this easy?” Once patients realize it could be, medicine will never again return to the old normal.
CDC: Updated Guideline for Prescribing Opioids for Pain

Pain affects the lives of millions of Americans every day and improving pain care and the lives of patients with pain is a public health imperative. The Centers for Disease Control and Prevention (CDC) is releasing updated and expanded recommendations for clinicians providing pain care for adult outpatients with short- and long-term pain. These clinical recommendations, published in the CDC Clinical Practice Guideline for Prescribing Opioids for Pain, will help clinicians work with their patients to ensure the safest and most effective pain care is provided. The publication updates and replaces the CDC Guideline for Prescribing Opioids for Chronic Pain released in 2016.
“Patients with pain should receive compassionate, safe, and effective pain care. We want clinicians and patients to have the information they need to weigh the benefits of different approaches to pain care, with the goal of helping people reduce their pain and improve their quality of life,” said Christopher M. Jones, PharmD, DrPH, MPH, Acting Director of CDC’s National Center for Injury Prevention and Control.
The 2022 Clinical Practice Guideline addresses the following areas: 1) determining whether to initiate opioids for pain, 2) selecting opioids and determining opioid dosages, 3) deciding duration of initial opioid prescription and conducting follow-up, and 4) assessing risk and addressing potential harms of opioid use. The Clinical Practice Guideline supports the primary prevention pillar of the HHS Overdose Prevention Strategy – supporting the development and promotion of evidence-based treatments to effectively manage pain.
The guideline is a clinical tool to improve communication between clinicians and patients and empower them to make informed decisions about safe and effective pain care. The recommendations are voluntary and provide flexibility to clinicians and patients to support individualized, patient-centered care. They should not be used as an inflexible, one-size-fits-all policy or law or applied as a rigid standard of care or to replace clinical judgement about personalized treatment.
CDC followed a rigorous scientific process using the best available evidence and expert consultation to develop the 2022 Clinical Practice Guideline. An independent federal advisory committee, four peer reviewers, and members of the public reviewed the draft updated guideline, and CDC revised it in response to this feedback to foster a collaborative and transparent process. CDC also engaged with patients with pain, caregivers, and clinicians to gain insights and gather feedback from people directly impacted by the guideline. The expanded guideline aims to ensure equitable access to effective, informed, individualized, and safe pain care.
“The science on pain care has advanced over the past six years,” said Debbie Dowell, MD, MPH, chief clinical research officer for CDC’s Division of Overdose Prevention. “During this time, CDC has also learned more from people living with pain, their caregivers, and their clinicians. We’ve been able to improve and expand our recommendations by incorporating new data with a better understanding of people’s lived experiences and the challenges they face when managing pain and pain care.”
CDC will continue to work to improve patient safety and outcomes by equipping health care professionals and patients with data, tools, and guidance they need to make informed treatment decisions. The 2022 Clinical Practice Guideline supports patients and clinicians working together to make informed, individualized decisions about safe and effective pain care.
Additional materials associated with the guideline are available for patients and clinicians.
Wake County Medical Society Enjoys NC Arboretum
On September 24, members of the WCMS enjoyed a visit to the JC Raulston Arboretum in Raleigh.
WCMS President Ted Kunstling, MD, planned the outing, in line with his goal to connect the medical community both in and out of their practice settings.



Suicide Rates Declining for White Americans, But Not for Minorities
(HealthDay News) -- In a finding that illustrates just how deeply racial disparities permeate the U.S. health care system, a new government report finds that suicide rates dipped slightly among white Americans while they rose for Black and Hispanic Americans.
"Although the recent decline in suicide rates for non-Hispanic white persons is encouraging, the continued increase for non-Hispanic Black and Hispanic persons is concerning," said study author Sally Curtin, a researcher for the U.S. National Center for Health Statistics.
"Suicide has declined recently for white persons, in total, and for those involving the three leading methods -- firearms and suffocation, including hangings, and poisoning," she added. "Rates continued to increase for Black and Hispanic persons for those involving firearms and suffocation. These differing trends deserve our attention."
Suicide rates for white people increased from 2000 to 2018, but then dropped from 18 per 100,000 people to 17 per 100,000 in 2020. But among Black and Hispanic people, the suicide rate continued to increase to nearly 8 per 100,000.
Still, the decline in suicide rates among white people appears to be short-lived, Curtin noted. Preliminary data for 2021 indicate suicide rates for all three race and ethnicity groups increased from 2020 to 2021, although the increase was less for white people (3%) compared with Black (13%) and Hispanic (8%) people, she said.
"It is well documented that COVID increased some of the risk factors for suicide, including mental health issues, substance use and financial stress," Curtin said. "However, these risk factors increased more for younger people and minority groups."
Suicide is a complex health issue, and there is never one single cause, said Doreen Marshall, vice president for mission engagement at the American Foundation for Suicide Prevention.
Minorities may be especially vulnerable to suicide, she noted, because "suicide most often occurs when stressors and health issues converge to create an experience of hopelessness and despair," Marshall explained.
"Depression is the most common condition associated with suicide, and it is often undiagnosed or untreated. Minority populations face multiple barriers to health care perpetuated by structural racism," she said.
Ongoing stressors, including prolonged environmental stressors and past trauma, can also play a role. "We need more research to understand how racism and prejudice experienced by minority communities might contribute to suicide risk," Marshall added.
Protective factors that can help mitigate risk include access to mental health care, limiting access to guns, community support and cultural and religious beliefs that encourage connection and seeking help, she said.
"Suicide can be prevented," Marshall said. "It requires connecting people to necessary treatment before they are in a suicide crisis, advocating for better access to health care and working to ensure that in a moment of crisis a vulnerable person has limited access to means of committing suicide."
People need to know how to identify risk and look out for warning signs, such as changes in a person's usual speech, behavior and mood, she said.
"Having open, honest conversations about what you or someone else may be experiencing and feeling can help empower our friends, family, colleagues and communities to identify when they or someone they love is experiencing worsening mental health," Marshall said.
For more on suicide, see the U.S. Centers for Disease Control and Prevention.
5 Things You Can Get Easier Than Taylor Swift Concert Tickets!
Tickets to Taylor Swift concerts are all but impossible to find.
Good news! There are other things you can get right now!
1.  The 2023 NCMS Calendar with your membership renewal... Click here
The 2023 NCMS Calendar with your membership renewal... Click here
 2. Become an NCMS PAC Investor ... Click here
2. Become an NCMS PAC Investor ... Click here
 3. Become an NCMS Foundation Donor ... Click here
3. Become an NCMS Foundation Donor ... Click here
 4. Your NCMS Celebrating Medicine Umbrella with a $100 Foundation donation... Click here
4. Your NCMS Celebrating Medicine Umbrella with a $100 Foundation donation... Click here
 5. English to Spanish Medical Terms Download with your NCMS 2023 membership... Click here
5. English to Spanish Medical Terms Download with your NCMS 2023 membership... Click here
NCMS Member Dr. Bonnie Coyle Appears on 'It's A Matter of Your Health' Podcast
North Carolina Medical Society member Dr. Bonnie Coyle is a guest on the hit podcast 'It's a Matter of Your Health.'
Coyle is an AMA Physician Champion and a KIPL Leadership College graduate. She was recently appointed Health Director of Mecklenburg County.
The podcast is hosted by Dr. Veita Bland and they are discussing preventive and lifestyle medicine.
Listen to their conversation and other episodes by clicking here.
Thank You Veterans

Happy Veterans Day to all branches of the military force! We sincerely honor your dedication and sacrifices. The North Carolina Medical Society salutes our veteran members past and present on this special day.
Events will be held across the state to honor those who serve. Here are a few places you can honor veterans:
Friday, Nov. 11:
Saturday, Nov. 12:
NCMS Members Win in Midterm Elections

RALEIGH -- The 2022 midterm elections are, mostly, in the books. As we wait for official election results, it appears Republicans have won a supermajority in the North Carolina Senate and are one seat short of the House supermajority.
Republicans previously held supermajorities in both the House and Senate during the first half of Democratic Governor Roy Cooper’s first term. In 2020, Cooper was reelected to a second term and Republicans kept majorities but did not gain supermajorities in that election.
Three North Carolina Medical Society members won their races Tuesday.

Dr. Kristin Baker will be the House Representative in District 82. In a Facebook post, Baker says "we have articulated our values and our vision, giving our community real hope for the safety and future of our children."

Dr. Timothy Reeder will be the House Representative in District 7. Reeder says in a Facebook post that he is "excited to get to work for the citizens of Pitt County."

And Dr. Greg Murphy beat his challenger in the 3rd congressional district. Murphy, also on Facebook, says of his win: "Thank you, eastern North Carolina! I’m honored to represent you in Washington."

State Senator Michael Lee won re-election in district 07. Lee is the son of a doctor from Dunn.
NCMS wants to congratulate our member winners. We look forward to working with them and all other elected officials in the state to advance medical science and to make sure North Carolinians have access to the best health care in the country.
Taking Action: A Community Conversation After Raleigh's Tragic Mass Shooting

RALEIGH -- There have been 52 mass shootings in the United States since October 13 when a 15-year-old boy shot seven, killing five, in his northeastern Raleigh neighborhood. Less than one month’s mass shootings have claimed 66 lives.
In response, The News & Observer and NCInsider want to hear from you.
On Tuesday, November 15, at the NC Museum of History, there is a free, interactive program to promote meaningful conversation. The goal is to connect local leaders and experts with the public. Four guests will help with the discussion.
Panelists are Raleigh Mayor Mary-Ann Baldwin, Jeffrey Swanson, a professor in psychiatry and behavioral sciences at Duke University School of Medicine who also works with the Center for Firearms Law at Duke Law School; Karen Fairley, executive director of the N.C. Department of Public Instruction’s Center for Safer Schools; and Dr. Elizabeth Cuervo Tilson, North Carolina’s state health director and chief medical officer for the N.C. Department of Health and Human Services.
To guarantee a seat you must register online. To read more and to reserve your seat click here.
Does Paxlovid Reduce Risk of Long Covid?
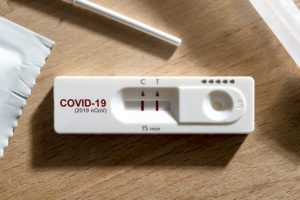
(CNN) - Paxlovid, the antiviral pill that reduces the risk of hospitalization and death from Covid-19, also reduces the risk of long Covid, according to a new study by researchers at the US Department of Veterans Affairs.
The study, posted online Saturday, analyzed electronic records for more than 56,000 veterans with Covid-19, including more than 9,000 who were treated with Paxlovid within the first five days of their infection.
The analysis showed people treated with Paxlovid had a 26% reduced risk of developing several long Covid conditions, including heart disease, blood disorders, fatigue, liver disease, kidney disease, muscle pain, neurocognitive impairment and shortness of breath. That corresponded to 2.3 fewer cases of long Covid conditions per 100 people three months after their diagnosis. Paxlovid also reduced the risk of hospitalization or death following acute Covid-19.
Read the full study report here.
NCMS Has Hit the Road! New Billboards Across the State Promote Annual Medical Exams and Screenings
RALEIGH -- The North Carolina Medical Society has partnered with the North Carolina Business Group on Health to promote annual medical exams and screenings. We now have four billboards across the state - from both corners of the coast, to the piedmont, to the coast!
Be on the lookout for these for the next few months!
CMS Releases 2023 Payment Schedule Final Rule

The Centers for Medicare & Medicaid Services (CMS) released the 2023 Medicare Physician Payment Schedule final rule. Notably, CMS adopted the revised CPT guidelines and codes and the AMA/Specialty Society RVS Update Committee (RUC) recommended relative values for additional E/M visit code families, including hospital visits, emergency department visits, home visits and nursing facility visits. These changes allow time or medical decision-making to be used to select the E/M visit level. In total, the E/M code sets being revised for 2023 comprise approximately 20 percent of all allowed charges under the Medicare Physician Payment Schedule. Therefore, these changes are estimated to require a reduction of about 1.6 percent to the 2023 Medicare conversion factor due to statutory budget neutrality requirements.
The CY 2023 Medicare conversion factor (CF) is $33.06, a decrease of $1.55 or 4.5% from the 2022 CF of $34.61. The decrease is largely a result of an expiring 3 percent increase funded by Congress through 2022. The additional approximate 1.6 percent decrease is the result of budget neutrality requirements that stem from the revised E/M changes. The AMA and the Federation are strongly advocating that Congress avert this payment cut, as well as implement an inflationary update for physicians, extend the 5 percent Advanced APM incentive and prevent the steep increase to the participation requirements for APMs, and waive the 4 percent PAYGO sequester.
In response to the Consolidated Appropriations Act, which extended payment for telehealth services to all communities in the country, not just rural areas, and allowed patients to receive telehealth services in their home for 151 days, or five months, after the end of the COVID-19 public health emergency (PHE) ends, CMS finalized its proposal to extend telehealth coverage for the codes that were only going to be on the telehealth list through the end of the PHE for an additional five months.
AMA staff are closely reviewing the final rule and will draft a detailed summary and analysis to share shortly. Please see the following documents for more information:
- Final Rule - https://www.cms.gov/files/document/cy2023-physician-fee-schedule-final-rule-cms-1770f.pdf
- CMS Press Release - https://www.cms.gov/newsroom/press-releases/hhs-finalizes-physician-payment-rule-strengthening-access-behavioral-health-services-and-whole
- CMS Fact Sheet - https://www.cms.gov/newsroom/fact-sheets/calendar-year-cy-2023-medicare-physician-fee-schedule-final-rule
- CMS QPP Fact Sheet - https://qpp-cm-prod-content.s3.amazonaws.com/uploads/2136/2023%20Quality%20Payment%20Program%20Final%20Rule%20Resources.zip
- CMS MSSP Fact Sheet - https://www.cms.gov/newsroom/fact-sheets/calendar-year-cy-2023-medicare-physician-fee-schedule-final-rule-medicare-shared-savings-program
It's Movember! UNC School of Medicine, Others Promoting No-Shave November

Folks, put away those razors. No-Shave November is here.
Started in Australia in 2003, Movember — a combination of mustache and November — works to raise money for a variety of men’s health initiatives. In its nearly 20 years, No-Shave Movember has funded more than 1,200 men’s health projects around the world, according to the group’s website.
The UNC School of Medicine, The Mo Bros and Mo Sisters of Raleigh-Durham, the MoBro's and MoSista's of Charlotte and many others across the state and country are participating.
To learn more about Movember and to start your own group click here for the national movement.
New Study: Weight, BMI May Increase Risk of Disability in MS Patients

(HEALTHLINE) -- A recent study published online in the Journal of Neurology, Neurosurgery & Psychiatry found that people with a body mass index (BMI) of 30 or more at the time of a diagnosis of multiple sclerosis (MS) were twice as likely to reach disability within six years, no matter what treatment they received.
- According to a new study, people who are overweight with a body mass index (BMI) of 30 or more when diagnosed with multiple sclerosis (MS) have an increased risk of disability.
- The onset of disability was also accelerated for people with a BMI of 30 or more.
- Experts note that many treatments associated with MS, as well as decreased mobility, can impact a person’s eating habits and weight.
Obesity, the researchers indicated, is a modifiable risk factor. Losing weight and reaching a healthy weight can improve clinical outcomes.
More than a thousand people were followed for the study and there are several other factors that can make changes to the outcome.
Read the full report here.
Need a Flu Shot? Find Provider Near You Today

Don't let the flu slow you down this year. The North Carolina Department of Health and Human Services has an easy way to find the closest provider to you.
Click here to get your shot today.
CVS, Walmart, Walgreens agree to $13.8B Opioid Settlement

(Reuters) - CVS Health Corp (CVS.N), Walgreens Boots Alliance Inc (WBA.O) and Walmart Inc (WMT.N) agreed to pay about $13.8 billion to resolve thousands of U.S. state and local lawsuits accusing the pharmacy chains of mishandling opioid pain drugs, potentially bringing years of litigation close to the finish line.
CVS said on Wednesday it had agreed to pay about $5 billion over 10 years, and Walgreens said that it had agreed to pay about $5.7 billion over 15 years. Neither company admitted wrongdoing. Walmart has agreed to pay $3.1 billion, mostly up front, according to two people familiar with the matter.
Paul Geller, one of the lawyers who negotiated for the governments, said that settlements with pharmacies "will bring billions of additional dollars to communities that are desperate for funds to combat the epidemic" of opioid addiction.
"We know that reckless, profit-driven dispensing practices fueled the crisis; but we know just as surely that with better systems in place and proper heeding of red flag warnings, pharmacies can play a direct role in reducing opioid abuse and in saving lives," Geller said.
CVS general counsel Thomas Moriarty said in a statement the company was pleased to resolve the claims and the deal was "in the best interest of all parties, as well as our customers, colleagues and shareholders."
Walgreens in a statement said: "As one of the largest pharmacy chains in the nation, we remain committed to being a part of the solution, and this settlement framework will allow us to keep our focus on the health and wellbeing of our customers and patients, while making positive contributions to address the opioid crisis."
Both CVS and Walgreens said their agreements would not be final until certain non-monetary terms were worked out, and that the total amount could be reduced if not enough government plaintiffs sign on.
Walmart did not immediately respond to a request for comment.
The proposed settlement, which would be the first nationwide deal with retail pharmacy companies, follows nationwide opioid settlements with drug makers and distributors totaling more than $33 billion. read more
Some North Carolina Nursing Homes to Get Increased Federal Scrutiny

The Biden Administration has announced that the Centers for Medicare and Medicaid Services (CMS) will heighten oversight of poor-performing skilled nursing facilities, including at least one in North Carolina.
The goal is to crack down on locations where patients are suffering unnecessarily.
The Administration says changes include:
The announced changes include:
- Making improved quality throughout a facility, rather than a lower level of deficiencies, key to completing the program and escaping its penalties and stigma.
- As in the case of Accordius Health at Statesville, pulling vital federal funding. Under new standards, this denial can take place at an earlier point, when a center is cited for two separate instances of “immediate jeopardy” of the life or health of residents.
- Escalating enforcement, meaning a more severe regimen for SFF Program facilities that “have continued noncompliance and little or no demonstrated effort to improve performance.”
- The new focus on staffing levels as a factor in the decision by state regulators on choosing a facility for the program.
The full story from NC Health News is available by clicking here.