NCDHHS Fireside Chat and Tele-Town Hall: Youth Vaping Prevention and Support in Schools

The North Carolina Department of Health and Human Services will host a live fireside chat and tele-town hall on Thursday, September 12, from 6 to 7 p.m., to discuss how educators and community leaders can address youth vaping and best support North Carolina students.
Event participants include:
- Nnenne Asi, MPH, Youth and Young Adult Tobacco Cessation Coordinator, Tobacco Prevention and Control Branch, NCDHHS
- Teresa Beardsley, Tobacco Prevention Manager, Albemarle Regional Health Services
- Chanda Battle, EdD, Director of Student Support Services, Edgecombe County Public Schools
- Charlene Zorn, Parent Advocate
More than two million students nationwide use e-cigarettes, also known as vapes, and one in four of these students vape every day. In North Carolina, more than 12% of high school students use tobacco products and more than 9% use vapes. Many middle and high school students who vape want to quit and have tried to do so.
Fireside chat and tele-town hall panelists will discuss:
- The impacts of vaping on youth
- Signs children and teens may be vaping and how to help
- Where to find free vaping prevention resources and programs
- Ways schools can help prevent youth from vaping or help them quit, including alternatives to suspension
Tobacco use often begins in youth and can affect children’s and teens’ social, athletic and academic experiences. Resources and materials are available to help teachers, coaches, administrators and school staff support students who want to quit, engage parents and caregivers, and create evidence-based school policies to reduce tobacco use on campus.
The fireside chat will stream live from the NCDHHS Facebook and YouTube accounts, where viewers can submit questions. The event also includes a tele-town hall, which invites people to listen in and ask questions by phone. People can dial into the event by calling 855-756-7520 Ext. #106460.
Wellness Wednesday: How Are You Coping with Stress?

Stress can play a huge part in our daily lives. According to the CDC, stress can cause the following:
- Feelings of fear, anger, sadness, worry, numbness, or frustration.
- Changes in appetite, energy, desires, and interests.
- Trouble concentrating and making decisions.
- Nightmares or problems sleeping.
- Physical reactions, such as headaches, body pains, stomach problems, or skin rashes.
- Worsening of chronic health problems and mental health conditions.
- Increased use of alcohol, illegal drugs (like heroin, cocaine, or methamphetamine), and misuse of prescription drugs (like opioids).
The CDC provides these useful tips for some ways you can manage stress, anxiety, grief, or worry:
- Take breaks from news stories, including those on social media. It’s good to be informed, but constant information about negative events can be upsetting. Consider limiting news to just a couple times a day and disconnecting from phone, TV, and computer screens for a while.
- Take care of your body: Staying physically healthy can improve your emotional well-being. Here are some ways to improve your health:
- Eat healthy. Have fruits and vegetables, lean protein, whole grains, and low-fat or no-fat dairy. Limit foods with unhealthy fats, salt, and added sugars. See Healthy Eating Tips.
- Get enough sleep. Go to bed and wake up at the same time each day to help you sleep better. Adults need 7 or more hours per night.
- Move more and sit less. Every little bit of physical activity helps. Start small and build up to 2 ½ hours a week. You can break it into smaller amounts such as 20 to 30 minutes a day.
- Limit alcohol intake. Choose not to drink, or drink in moderation on days you drink alcohol. Moderation means having 2 drinks or less a day for men or 1 drink or less for women. Find out more at Drink Less, Be Your Best.
- Avoid using illegal drugs or prescription drugs in ways other than prescribed. Don’t take someone else’s prescription. Substance use treatment is available, and recovery starts with asking for help.
- Avoid smoking, vaping, and the use of other tobacco products. People can and do quit smoking for good.
- Continue with regular health appointments, tests, screenings, and vaccinations.
- Make time to unwind.
- Take deep breaths, stretch, or meditate.
- Try to do some other activities you enjoy.
- Connect with others.
- Talk with people you trust about your concerns and how you are feeling.
- Connect with your community-based or faith-based organizations.
Get additional resources here.
Today is World Suicide Prevention Day

More than 1,525 North Carolinians ages 10 and older died by suicide last year, making it the ninth leading cause of death in the state and the second leading cause of death for people between the ages of 10 and 40. Additionally, for every suicide, there were two hospitalizations and eight emergency department visits for self-inflicted injuries. In recognition of Suicide Prevention Month this September, NCDHHS is remembering those affected by suicide and reaffirming its commitment to curb this increasing trend by continuing to work to transform the behavioral health system in North Carolina.
"Every person in North Carolina should have access to the care they need, when and where they need it," said NC Health and Human Services Secretary Kody H. Kinsley. "We are investing in crisis care in our state so there is someone to contact, someone to respond and a safe place for help if you are having a behavioral health emergency."
The department continues to support and manage the 988 Suicide and Crisis Lifeline. Since the Lifeline’s transition to a three-digit number in July 2022, 988 crisis counselors have responded to nearly 190,000 calls, texts and chats, providing critical access to mental health and substance use crisis support. 988 is an important component of NCDHHS’ ongoing work to ensure every North Carolinian has someone to contact when experiencing a mental health crisis. Of the $835 million investment in behavioral health in the 2023 state budget, NCDHHS committed more than $130 million to transforming the state’s behavioral health crisis response services, including 988, to shift the system from a state of crisis to a state of care.
"For anyone struggling with their mental well-being or thoughts of suicide, it’s important to know that you are not alone and that it’s OK to ask for help whenever you need it," said Kelly Crosbie, MSW, LCSW, Director of the NCDHHS Division of Mental Health, Developmental Disabilities and Substance Use Services. "By reducing the stigma around mental health, fostering open conversations, and expanding access to care, we are building a system where every person knows how to access the right support when they or someone they love is facing a mental health crisis."
State leaders will soon be looking for public input as it develops its new Suicide Prevention State Action Plan. Achievements from the 2021-2025 Suicide Prevention Action Plan include:
- Created a Comprehensive Suicide Prevention Team to better coordinate suicide prevention efforts with state and federal partners
- Developed a statewide inventory of suicide prevention resources and programs, accessible to everyone online
- Providing youth primary suicide prevention education and training to school personnel, clinical providers and under-resourced school systems
- Supporting access to Applied Suicide Intervention Skills Training (ASIST); an intensive early suicide intervention training for community helpers who interact with at-risk individuals and require training for those times of crisis.
- Providing Mental Health First Aid training to more than 1,200 educators, youth and emergency response personnel
- Provided crisis intervention training for more than 2,040 law enforcement and emergency response personnel
- Providing community helper training as well as Counseling on Access to Lethal Means (CALM) training is to facilitate the conversation between a practitioner and a person in crisis about temporarily creating a safe environment during the time of crisis
- Expanding and enhancing mobile crisis services including Mobile Outreach Response Engagement and Stabilization teams who respond when someone is experiencing a mental health emergency
- Implementing safe storage practices and creating a gun safe storage map with NC SAFE. NC SAFE has distributed more than 75,000 gun locks through state partnerships
- Created a landing page that gathers all suicide prevention activities across NCDHHS into one clearinghouse: ncdhhs.gov/stopncsuicide
Additionally, NCDHHS partnered with UNC-Chapel Hill's Carolina Across 100 program, creating 15 teams, representing 24 counties, focused on suicide prevention. In May 2024, the program culminated in a successful Suicide Prevention Summit with more than 400 participants. NCDHHS also showcased its Faith Leaders for Life program, which has trained more than 100 faith leaders in 51 counties, reaching more than 50,000 congregants, particularly in rural and Black, Indigenous and People of Color communities.
How These Common Chemicals Could Be Affecting Your Health

Forever chemicals in cookware, food, water, clothes and furniture could cause health issues in individuals.
PFAS, or perfluoroalkyl and polyfluoroalkyl substances — sometimes called “forever chemicals” because they don’t fully break down in the environment — have been used in consumer products since the 1950s.
As more studies and regulations about PFAS are released, Dr. Carmen Marsit has been doing research on the effects of these chemicals during pregnancy. Marsit, Rollins Distinguished Professor of Research at the Rollins School of Public Health at Emory University, wants people to understand what to do about PFAS. Here’s his advice.
Continue to full article here.
NC Sees First Case of Measles Since 2018. Vaccinations Urged For Your Patients
Measles case in Mecklenburg County and what that means for your patients
(additional reading from NCMS at bottom of this article)
The North Carolina Department of Health and Human Services announced a confirmed case of measles (rubeola) in a child in Mecklenburg County. This is the first measles case reported in North Carolina since 2018. The child was likely exposed to measles while traveling out of the country. Fortunately, the parents kept the child at home after returning to North Carolina except for one medical visit, during which appropriate precautions were taken to avoid spreading the virus. To protect patient privacy, no further information about the patient will be shared. NCDHHS’ Division of Public Health is working closely with the Mecklenburg County Health Department to ensure readiness to detect and respond to other possible measles cases or exposures.
Measles is highly contagious and spreads through the air when an infected person coughs or sneezes. You can get measles just by being in a room where a person with measles has been, even up to two hours after that person has left. Measles can cause serious health complications, including pneumonia and encephalitis, especially in children younger than 5 years old. Measles begins with a fever that lasts for a couple of days, followed by a cough, runny nose and conjunctivitis (pink eye). A rash starts on the face and upper neck, spreads down the back and trunk, then extends to the arms and hands as well as the legs and feet. After about five days, the rash begins to fade. Individuals should stay at home when sick and should call ahead when possible before seeking medical attention to help prevent spread of the virus. Providers should contact their local health department as soon as measles is suspected.
To protect your children, yourself and others in the community, it is important to be vaccinated against measles. Children who are not traveling internationally should receive their first dose of MMR vaccine at age 12 to 15 months and their second dose at 4 to 6 years. All U.S. residents older than age 6 months without evidence of immunity who are planning to travel internationally should receive MMR vaccine prior to departure.
- Infants aged 6 through 11 months should receive one dose of MMR vaccine before departure
- Children aged 12 months or older should receive two doses of MMR vaccine, separated by at least 28 days
- Teenagers and adults without evidence of measles immunity should receive two doses of MMR vaccine separated by at least 28 days
"Measles is on the rise globally and in the U.S.," said State Health Director and NCDHHS Chief Medical Officer Dr. Elizabeth Cuervo-Tilson. "Parents, schools, early childhood education providers and health care providers should work to ensure everyone is up to date with their measles vaccinations."
"Measles infections are preventable. Most Mecklenburg County residents are vaccinated against measles and are not at high risk," said Mecklenburg County Public Health Director Dr. Raynard Washington. "This case further demonstrates the critical need for all families to ensure their kids are up to date with measles and other childhood immunizations."
The increased number of measles cases in the U.S. this year is reflective of a rise in global measles cases and a growing global threat from the disease.
According to CDC’s Kindergarten immunization coverage estimates, 94% of North Carolina Kindergarteners were up to date on the MMR vaccine in the ’22-’23 school year, compared to 93% nationally. While statewide coverage remains high, it is important to note that coverage levels vary locally, with some counties and schools having lower vaccination coverage that leaves them at higher risk for a measles outbreak. You can find information on vaccine rates at state, county and school levels on the Kindergarten Immunization Dashboard.
Children who are uninsured can still be vaccinated at low or no cost through the Vaccines for Children program, which offers free vaccines to children through 19 years of age. [source}
ADDITIONAL READING FROM NCMS
Preparing for possibility of measles
Measles in spotlight as cases raise nationally
CDC Health Advisory on measles
Take Advantage of This Primary Care Team E-Learning Series
If you need assistance from a Practice Support coach, please contact [email protected].
Learning Opportunity: Bereavement Care in Oncology

Grief and bereavement are a reality in Oncology care for patients, their families, and for clinicians. Bailey Brislin, MDiv, BCC will review grief and bereavement theory, research, and practice as it relates to caring for Oncology patients and their loved ones.
Learning Objectives
- Describe grief theories and their correlation to providing bereavement support
- Discuss the needs of bereavement care in Oncology in relation to the forms of grief
- Identify tools for providing bereavement and grief support
- List resources for providing bereavement care in Oncology
Learn more here.
NC Medicaid Respiratory Syncytial Virus (RSV) Guidelines for 2024-2025

NC Medicaid is providing guidance on the 2024-2025 Respiratory Syncytial Virus (RSV) season for NC Medicaid Direct and NC Managed Care health plans and is based on products approved by the Food and Drug Administration (FDA) and recommended by the Center for Disease Control (CDC) Advisory Committee on Immunization Practices (ACIP). For details on the 2024-2025 recommendations, please refer to CDC RSV ACIP Vaccine Recommendations.
The North Carolina Division of Public Health has set the RSV season to start on September 15, 2024, for the 2024-2025 RSV season. Please refer to the North Carolina Immunization Branch (NCIP) Memos and Communication webpage and NC Department of Health and Human Services Division of Public Health Provider Memos for Respiratory Illnesses and NC Communicable Diseases Manual for pertinent updates to the RSV season dates from the State of North Carolina.
Summary of NC Medicaid RSV Coverage
- Abrysvo™, Arexvy, and mRESVIATM: ACIP recommends adults 75 years of age and older receive a single dose of RSV vaccine. ACIP recommends adults 60–74 years of age and older who are at increased risk of severe RSV disease receive a single dose of RSV vaccine. It is available to bill as a medical or pharmacy point-of-sale (POS) claim.
- Abrysvo™ for maternal indications: ACIP recommends a maternal RSV vaccine for pregnant people during 32-36 weeks gestation, using seasonal administration, to prevent RSV lower respiratory tract infections in infants. Abrysvo is available to bill as a medical or pharmacy POS claim; pharmacy point-of-sale claims can only be billed for beneficiaries greater than or equal to 19 years of age. Please refer to Clinical Coverage Policy 1E-5 Obstetrical Services for additional coverage information. Abrysvo is available through VFC program to VFC providers for beneficiaries less than 19 years of age. Providers should follow ACIP recommendations to administer Abrysvo.
- Beyfortus™: Nirsevimab-alip is available through the VFC program to VFC providers. ACIP recommends nirsevimab for all infants less than 8 months of age who are born during or entering their first RSV season and for infants and children 8 to 19 months of age who are at increased risk for severe RSV disease and are entering their second RSV season. For additional information about these recommendations see Use of Nirsevimab for the Prevention of Respiratory Syncytial Virus Disease Among Infants and Young Children: Recommendations of the Advisory Committee on Immunization Practices — United States, 2023.
- Synagis®: Coverage starts Sept. 15, 2024, and ends March 31, 2025. Covered at pharmacy POS and prior authorization (PA) is required; Synagis® is not covered through the Physician-Administered Drug Program (PADP).
The clinical criteria used by NC Medicaid for the 2024/2025 RSV season are consistent with guidance published by the American Academy of Pediatrics (AAP): 2024 – 2027 Report of the Committee on Infectious Diseases, 33rd Edition. This guidance for Synagis use among infants and children at increased risk of hospitalization for RSV infection is available online by subscription. Providers are encouraged to review the AAP guidance.
Continue reading the full bulletin released by NC Medicaid here.
Join NCDHHS Tomorrow for Suicide Prevention Week Lunch and Learn Webinar
The North Carolina Department of Health and Human Services is holding a public webinar to mark World Suicide Prevention Day on Tuesday, September 10, 2024. This comes as Governor Roy Cooper proclaims the week of September 8 as Suicide Prevention Week in North Carolina. Suicide is a significant public health issue that affects people across all socioeconomic, racial and ethnic backgrounds.

More than 1,525 North Carolinians ages 10 and older died by suicide last year, making it the ninth leading cause of death in the state and the second leading cause of death for people between the ages of 10 and 40. Additionally, for every suicide, there were two hospitalizations and eight emergency department visits for self-inflicted injuries. In recognition of Suicide Prevention Month this September, NCDHHS is remembering those affected by suicide and reaffirming its commitment to curb this increasing trend by continuing to work to transform the behavioral health system in North Carolina.
"Every person in North Carolina should have access to the care they need, when and where they need it," said NC Health and Human Services Secretary Kody H. Kinsley. "We are investing in crisis care in our state so there is someone to contact, someone to respond and a safe place for help if you are having a behavioral health emergency."
The department continues to support and manage the 988 Suicide and Crisis Lifeline. Since the Lifeline’s transition to a three-digit number in July 2022, 988 crisis counselors have responded to nearly 190,000 calls, texts and chats, providing critical access to mental health and substance use crisis support. 988 is an important component of NCDHHS’ ongoing work to ensure every North Carolinian has someone to contact when experiencing a mental health crisis. Of the $835 million investment in behavioral health in the 2023 state budget, NCDHHS committed more than $130 million to transforming the state’s behavioral health crisis response services, including 988, to shift the system from a state of crisis to a state of care.
"For anyone struggling with their mental well-being or thoughts of suicide, it’s important to know that you are not alone and that it’s OK to ask for help whenever you need it," said Kelly Crosbie, MSW, LCSW, Director of the NCDHHS Division of Mental Health, Developmental Disabilities and Substance Use Services. "By reducing the stigma around mental health, fostering open conversations, and expanding access to care, we are building a system where every person knows how to access the right support when they or someone they love is facing a mental health crisis."
State leaders will soon be looking for public input as it develops its new Suicide Prevention State Action Plan. Achievements from the 2021-2025 Suicide Prevention Action Plan include:
- Created a Comprehensive Suicide Prevention Team to better coordinate suicide prevention efforts with state and federal partners
- Developed a statewide inventory of suicide prevention resources and programs, accessible to everyone online
- Providing youth primary suicide prevention education and training to school personnel, clinical providers and under-resourced school systems
- Supporting access to Applied Suicide Intervention Skills Training (ASIST); an intensive early suicide intervention training for community helpers who interact with at-risk individuals and require training for those times of crisis.
- Providing Mental Health First Aid training to more than 1,200 educators, youth and emergency response personnel
- Provided crisis intervention training for more than 2,040 law enforcement and emergency response personnel
- Providing community helper training as well as Counseling on Access to Lethal Means (CALM) training is to facilitate the conversation between a practitioner and a person in crisis about temporarily creating a safe environment during the time of crisis
- Expanding and enhancing mobile crisis services including Mobile Outreach Response Engagement and Stabilization teams who respond when someone is experiencing a mental health emergency
- Implementing safe storage practices and creating a gun safe storage map with NC SAFE. NC SAFE has distributed more than 75,000 gun locks through state partnerships
- Created a landing page that gathers all suicide prevention activities across NCDHHS into one clearinghouse: ncdhhs.gov/stopncsuicide
Additionally, NCDHHS partnered with UNC-Chapel Hill's Carolina Across 100 program. creating 15 teams, representing 24 counties, focused on suicide prevention. In May 2024, the program culminated in a successful Suicide Prevention Summit with more than 400 participants. NCDHHS also showcased its Faith Leaders for Life program, which has trained more than 100 faith leaders in 51 counties, reaching more than 50,000 congregants, particularly in rural and Black, Indigenous and People of Color communities.
Please join the NCDHHS Division of Mental Health, Developmental Disabilities and Substance Use Services, Division of Public Health and the NC Suicide Prevention Coordinator to discuss efforts to increase suicide prevention and awareness, identify resources and find ways to participate in spreading the word that help is available.
What: Suicide Prevention Week Lunch and Learn Webinar
Who: Hannah Harms, State Suicide Prevention Coordinator
Anne Geissinger, NC Comprehensive Suicide Prevention Program Coordinator, Injury and Violence Prevention, Division of Public Health, NCDHHS
Lisa DeCiantis, Crisis Services Team Lead, Division of Mental Health, Developmental Disabilities, and Substance Use Services, NCDHHS
Jane Ann Miller, NC Comprehensive Suicide Prevention Program Manager, Injury and Violence Prevention, Division of Public Health, NCDHHS
Brittany Jones, 988 Grant Lead, Division of Mental Health, Developmental Disabilities and Substance Use Services, NCDHHS
When: World Suicide Prevention Day
Tuesday, Sept. 10
12:30-1:30 p.m.
Where: Please register for the Webinar at https://www.zoomgov.com/meeting/register/vJItf-2urDgvGqGRI7E-k04DVUOXqA1C-MU.
Members Making Moves: Dr. Syed Hussaini Joins UNC Orthopedics at Goldsboro
UNC Orthopedics at Goldsboro is expanding its services with the addition of Dr. Syed Hanif Hussaini, an Orthopedic Foot and Ankle Surgeon. Dr. Hussaini joins us with an impressive background in orthopedic surgery and a passion for delivering high-quality patient care.
 Dr. Syed Hussaini (image credit: UNC)
Dr. Syed Hussaini (image credit: UNC)
Dr. Hussaini received his Doctor of Medicine degree from Saint Louis University School of Medicine and holds a Bachelor of Science in Mathematics from Duke University. He completed his Orthopedic Foot and Ankle Fellowship at The Orthopedic Foot & Ankle Center in Falls Church, VA, and most recently practiced at Wake Orthopedics in Cary, NC. Throughout his career, Dr. Hussaini has been recognized for his outstanding work, including receiving the North Carolina Orthopedic Association Meeting Opioid Session Award and the SLU M.D. with Distinction in Research Award.
His contributions to the field of orthopedic surgery are extensive, particularly in foot and ankle surgery and opioid prescription practices. Dr. Hussaini’s research and publications have advanced the understanding and treatment of foot and ankle conditions, solidifying his reputation as a leader in the field.
In addition to his clinical and research achievements, Dr. Hussaini is an active member of several professional organizations, including the American Academy of Orthopedic Surgeons and the American Orthopedic Foot & Ankle Society. [source]
Duke Health: Study Solves Testosterone’s Paradoxical Effects in Prostate Cancer

A treatment paradox has recently come to light in prostate cancer: Blocking testosterone production halts tumor growth in early disease, while elevating the hormone can delay disease progression in patients whose disease has advanced.
The inability to understand how different levels of the same hormone can drive different effects in prostate tumors has been an impediment to the development of new therapeutics that exploit this biology.
Now, a Duke Cancer Institute-led study, performed in the laboratory of Donald McDonnell, Ph.D. and appearing this week in Nature Communications, provides the needed answers to this puzzle.
The researchers found that prostate cancer cells are hardwired with a system that allows them to proliferate when the levels of testosterone are very low. But when hormone levels are elevated to resemble those present in the normal prostate, the cancer cells differentiate.
“For decades, the goal of endocrine therapy in prostate cancer has been to achieve absolute inhibition of androgen receptor function, the protein that senses testosterone levels,” said lead investigator Rachid Safi, Ph.D., research assistant professor in the Department of Pharmacology and Cancer Biology, at Duke University School of Medicine.
“It’s been a highly effective strategy, leading to substantial improvements in overall survival,” he said. “Unfortunately, most patients with advanced, metastatic disease who are treated with drugs to inhibit androgen signaling will progress to an aggressive form of the disease for which there are limited therapeutic options.”
Using a combination of genetic, biochemical, and chemical approaches, the research team defined the mechanisms that enable prostate cancer cells to recognize and respond differently to varying levels of testosterone, the most common androgenic hormone.
It turned out to be rather simple. When androgen levels are low, the androgen receptor is encouraged to “go solo” in the cell. In doing so, it activates the pathways that cause cancer cells to grow and spread. However, as androgens rise, the androgen receptors are forced to “hang out as a couple,” creating a form of the receptor that halts tumor growth.
“Nature has designed a system where low doses of hormones stimulate cancer cell proliferation and high doses cause differentiation and suppress growth, enabling the same hormone to perform diverse functions,” McDonnell said.
In recent years, clinicians have begun treating patients with late-stage, therapy resistant prostate cancers using a monthly, high-dose injection of testosterone in a technique called bi-polar androgen therapy, or BAT. The inability to understand how this intervention works has hindered its widespread adoption as a mainstream therapeutic approach for prostate cancer patients.
“Our study describes how BAT and like approaches work and could help physicians select patients who are most likely to respond to this intervention,” McDonnell said. “We have already developed new drugs that exploit this new mechanism and are bringing these to the clinic for evaluation as prostate cancer therapeutics.”
In addition to McDonnell and Safi, study authors include Suzanne E. Wardell, Paige Watkinson, Xiaodi Qin, Marissa Lee, Sunghee Park, Taylor Krebs, Emma L. Dolan, Adam Blattler, Toshiya Tsuji, Surendra Nayak, Marwa Khater, Celia Fontanillo, Madeline A. Newlin, Megan L. Kirkland, Yingtian Xie, Henry Long, Emma Fink, Sean W. Fanning, Scott Runyon, Myles Brown, Shuichan Xu, Kouros Owzar, and John D. Norris.
The study received funding support from the National Cancer Institute (R01-CA271168, P30CA014236) and the North Carolina Biotechnology Center. [source]
Haywood Regional Medical Center Launches Walk-in Mammography Clinic
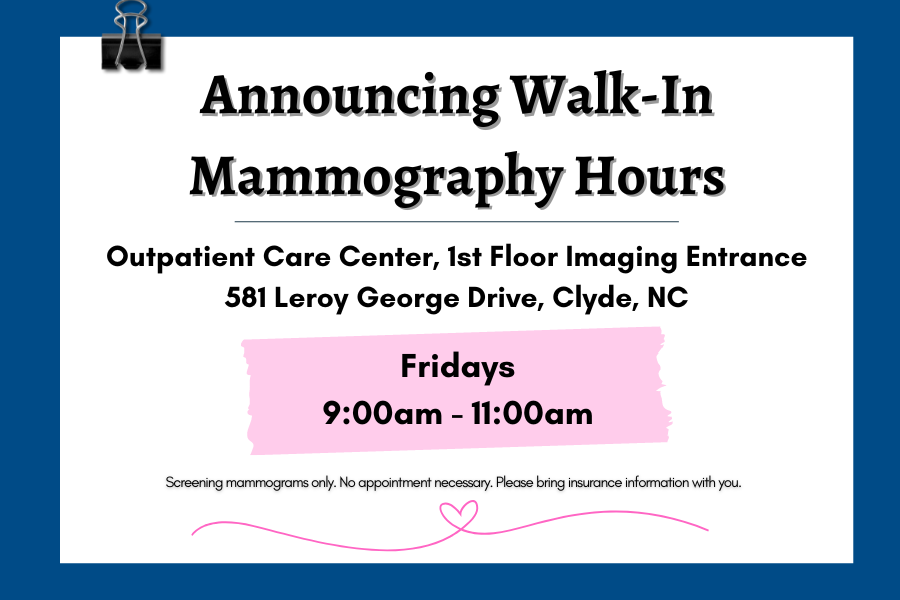
Haywood Regional Medical Center is pleased to announce the launch of a convenient walk-in mammography clinic at the HRMC Breast Center, located on the second floor of the Outpatient Care Center at 581 Leroy George Drive in Clyde.
This new service is available to women who have not had a mammography exam in the past year and is for screening mammograms only. Women with a new lump, discharge, or other breast issues are advised to schedule an appointment with their healthcare provider and inquire about a referral for a diagnostic mammogram.
The walk-in mammography clinic takes place every Friday from 9:00AM – 11:00AM. No appointment is necessary.
To be seen at the walk-in clinic, patients with insurance should bring their current insurance information for billing purposes. For those without insurance, resources and information will be provided during walk-in hours.
Haywood Regional Medical Center is committed to delivering quality breast care with a focus on early detection and treatment. The HRMC Breast Center is equipped with advanced services such as contrast-enhanced mammography, nurse navigation, collaborative local cancer care, and surgical breast services. These offerings ensure that local women can access a complete range of breast health services in their home community.
For more information about breast services, visit MyHaywoodRegional.com or call 828.452.8963. [source]
NCMS Member Delivers Relief to Patients with Chronic Low Back Pain
FirstHealth Interventional Pain Medicine is the first in the Sandhills region to offer an innovative approach to provide relief for patients suffering from a distinct type of chronic low back pain (CLBP) called vertebrogenic pain.
The treatment is the Intracept® Procedure, a minimally invasive, outpatient procedure that targets a nerve located in the vertebrae called the basivertebral nerve (BVN).
During the procedure, James Winkley, M.D., board certified anesthesiologist and pain medicine physician with FirstHealth Interventional Pain Medicine, advances a specialized probe into the vertebrae and uses radiofrequency energy to heat the BVN, rendering it unable to transmit pain signals to the brain.
The Intracept Procedure generally takes an hour to perform and is implant-free, preserving the overall structure of the spine.
“With the Intracept Procedure, we are entering a new and promising era in the treatment and diagnosis of vertebrogenic pain,” said Dr. Winkley. “Not only is the procedure proven to be safe and durable but it also provides patients with the opportunity to get back to living without the burden of chronic low back pain.”
Of the 30 million people in the U.S. with chronic low back pain, 1 in 6 are likely to have vertebrogenic pain, a distinct type of CLBP caused by damage to vertebral endplates, the interface between the disc and the vertebral body. Disc degeneration, and the wear and tear that occurs with everyday living, produces stresses on the endplates that damage them, leading to inflammation and vertebrogenic pain.
In order to qualify for the Intracept Procedure, patients must have chronic low back pain of at least six months duration, have not responded to at least six months of conservative care, and present with degenerative vertebral endplate changes consistent with Type 1 or Type 2 Modic changes at L3 through S1 on an MRI.
To learn more about the Intracept Procedure, call FirstHealth Interventional Pain Medicine at (910) 715-1794 or complete our interest form below to request an appointment.
FirstHealth Interventional Pain Medicine works with chronic pain sufferers to manage and treat conditions with a wide range of pain relief options, including the newest and most advanced treatments. Our goal is to help patients return to their everyday activities and hobbies with minimal to no pain. Established in 1995, we are the longest-standing practice of pain management specialists in the Sandhills. Our team includes seven anesthesiologists and four advanced practice providers with more than 40 years combined experience. Office locations include Pinehurst, Raeford, Sanford, Troy, Rockingham and Fayetteville. [source]
Diabetes Performance Improvement in Primary Care Live Webinar
Diabetes Performance Improvement in Primary Care
Wednesday, October 23, 2024
12 pm – 1pm
Live Webinar

Program Overview
This educational activity aims to inform the learner about the status of diabetes and chronic kidney disease in primary care. This activity will explore barriers and facilitators to promote patient engagement in treatment. This activity will focus on performance improvement methods and activities which promote health among patients with diabetes.
Who Should Participate
Physicians, Physician Assistants, Nurse Practitioners, Nurses, and Primary Care Office Staff
As part of our commitment to diversity and inclusion, the Northwest AHEC provides compassionate education and respectful care for all, regardless of socioeconomic status, race, ethnicity, language, nationality, sex, gender identity, sexual orientation, religion, geography, disability and age.
Objectives
Upon completion of this activity, participants should be better able to:
- Describe barriers and strategies for clinical care teams in the screening, diagnosis, and treatment of patients with diabetes and chronic kidney disease (CKD).
- Utilize new methods to identify how diabetes and CKD disproportionately affect racial and ethnic minorities in clinical workflows.
- Explain processes for screening, diagnosis, and raising awareness about diabetes and its connection to chronic kidney disease (CKD)
Download the event brochure here.

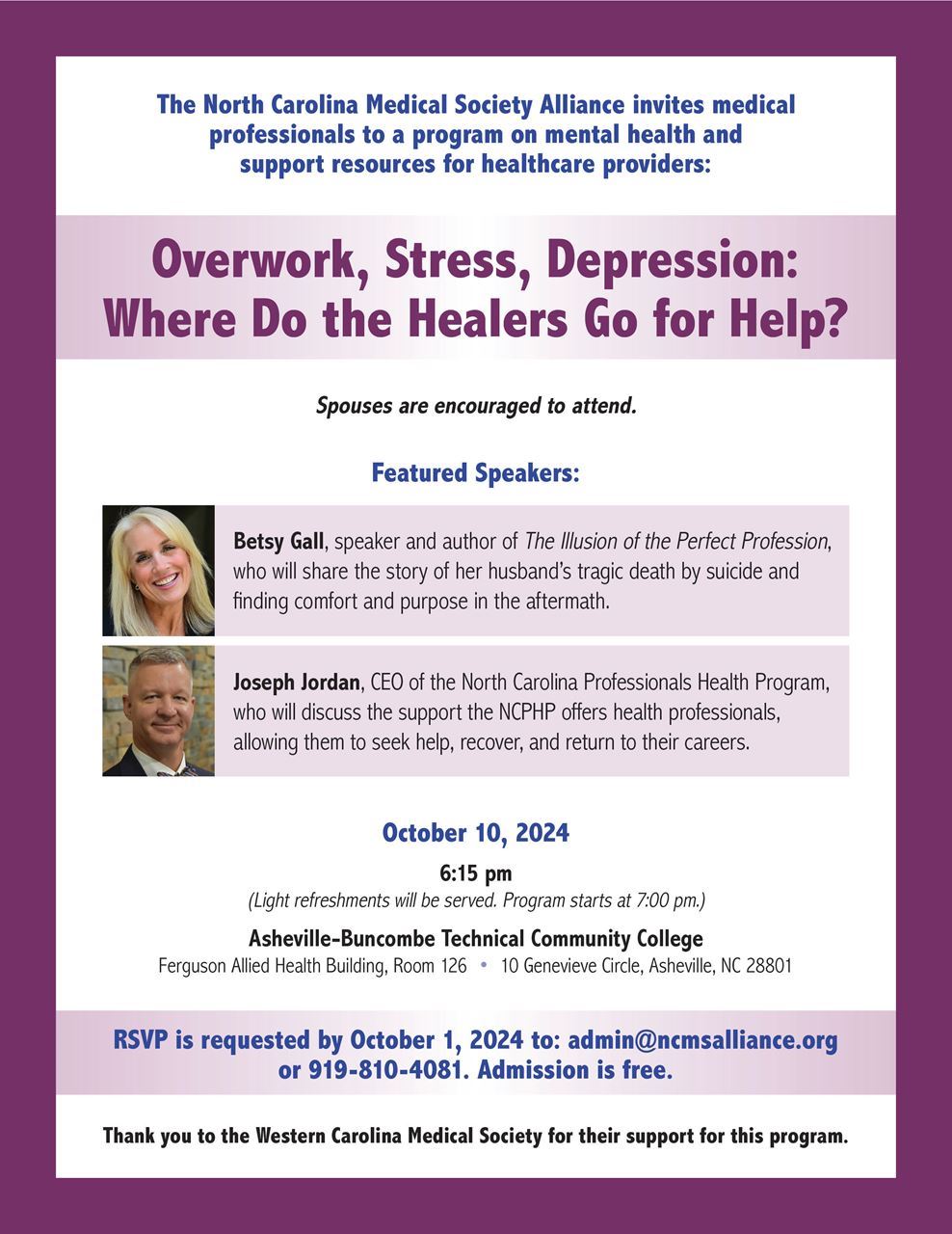
Overwork, Stress, Depression: Where Do the Healers Go for Help?
Mark your calendar for an important program on mental health and support resources for healthcare providers.
Overwork, Stress, Depression: Where Do the Healers Go for Help?
Thursday, October 10 at 6:15pm
RSVP by October 1 to [email protected] or 919-810-4081
Capitol Chronicle: Join NCMS for the 2025 National Advocacy Conference in Washington

Capitol Chronicle: Join NCMS for 2025 National Advocacy Conference in Washington
The AMA’s National Advocacy Conference is scheduled for February 10-12, 2025. This yearly event offers an opportunity for personal involvement in the health policy debate on Capitol Hill. We need increased NCMS member engagement with our members of Congress, so mark your calendar and stay tuned for forthcoming details.

2025 National Advocacy Conference
Save the date and join us for our return to Capitol Hill.
February 10-12, 2025 / Washington, DC
Plan now to join your colleagues as we advocate for patients and the medical profession on . . .
Prior Authorization Relief
Medicare Payment Reform
Workforce Shortage Solutions
Physician Wellness
Mark your calendar! Registration details and additional information coming soon.
Your engagement matters!
Do you know your state and federal legislators? More importantly, do your legislators know you?
The NCMS can help you connect with policy makers as a constituent and advocate!
Register Now! Sustainability of the HIV/AIDS Response – Getting to 2030 & Beyond

The state of the HIV/AIDs endemic is reaching a critical point requiring evaluation of the current state of the global response, progress made thus far, and planning for post-2030 goals. The National Academy of Medicine is hosting a timely international meeting to facilitate discussion on these issues.
This one-day workshop is being held on September 18, 2024, from 9:00 AM – 5:00 PM US Eastern. Ambassador John N. Nkengasong, the Senior Bureau Official for Global Health Security and Diplomacy at the U.S. State Department, will deliver the opening remarks. His address will set the stage for discussions across three subsequent panels.
Broadly, the goals of this workshop are to:
- Explore how we can re-energize the global HIV response to reach the 2030 goals but also to look beyond.
- Craft strategies to increase and sustain political commitment.
- Highlight global accountability and domestic-donor financing.
Grant Opportunity: Telehealth Infrastructure Grant Program

In Session Law 2023-134, the North Carolina General Assembly (NCGA) appropriated $5,000,000 in SFY 2024 and $15,000,000 in SFY 2025 in receipts (State funds) from the ARPA Temporary Savings Fund to the Office of Rural Health (ORH) in the Department of Health and Human Services to provide competitive grants to rural healthcare providers for Telehealth related items including:
- equipment
- high-speed internet access
- telehealth-related training to staff and patients
- technology equipment to patients
- internet service support for patients to help facilitate telehealth access*
- other infrastructure needed to establish telehealth services
*Eligible rural healthcare patients can benefit from internet service and associated equipment rentals, including modems, routers, and hotspot devices through the Telehealth Infrastructure grant. To receive this support, patients must meet at least one of the eligibility criteria defined below:
- Total household income that is at or below 200% of the federal poverty guidelines or,
- Participation in any ONE of these government benefit programs:
- Lifeline
- Supplemental Nutrition Assistance Program (SNAP)
- Medicaid
- Federal Public Housing Assistance (FPHA) (including Housing Choice Voucher (HCV) Program (Section 8 Vouchers), Project-Based Rental Assistance (PBRA)/202/811, Public Housing, and Affordable Housing Programs for American Indians)
- Veterans Pension and Survivors Benefit
- Supplemental Security Income (SSI)
- Free and Reduced-Price School Lunch or Breakfast Program including through the USDA Community Eligibility Provision
- Federal Pell Grant (current award year)
- Special Supplement Nutrition Program for Women, Infants, and Children (WIC)
Priority will be given to independent primary care practices and independent obstetrics and gynecology (OB-GYN) practices.
For more information, eligibility, and other requirements, click here.
Listen Now! NCMS Member Dr. Shannon Dowler Talks STI's and more.

Season 4 of the Addiction Medicine Podcast kicks off with a 2-part episode on Sexually Transmitted Infections (STI). In Part 1 dives into how the term ‘infection’ can reduce stigma, encourage testing, and emphasize the importance of regular screenings. We also discuss current trends, cultural trends, health inequities, and the role of healthcare providers in STI care.
Joining this important conversation are Dr. Shannon Dowler, a board-certified family physician with a national reputation in health policy, public health, and sexual health, and Dr. Amy Marietta, board-certified in family medicine and addiction medicine.
Dr. Dowler is currently Deputy Director in the Mecklenburg County STI Clinic while Dr. Marietta serves as the Medical Director of MAHEC’s Project CARA, a comprehensive perinatal substance use treatment program in Asheville, North Carolina.
Submit Your Application Today! Addiction Medicine Scholarship Opportunity.
The Governor’s Institute offers a limited number of scholarships to attend the Addiction Medicine Conference (Spring) or Addiction Medicine Essentials (Fall).
By attending these events, physician, nurse practitioner, or physician assistant students or residents, who are training in North Carolina with an interest in Addiction Medicine will have the opportunity to receive up-to-date substance use related education, applicable across general medical as well as addiction specialty practices and learn from the experts during didactic lectures on a wide range of addiction medicine related topics.
Help Address Rural Health Challenges! Participate in the 2024 Rural Health Hackathon.

The Centers for Medicare & Medicaid Services (CMS) Center for Medicare and Medication Innovation (“Innovation Center”) announced the 2024 Rural Health Hackathon – a series of in-person, collaborative sessions designed to generate and construct creative and actionable ideas to address rural health challenges.
The 2024 Hackathon builds on CMS’ extensive outreach to rural communities through site visits and listening sessions to better understand rural health care issues. Through these solution-oriented events, the CMS Innovation Center will bring together rural health community care providers, community organizations, industry and tech entrepreneurs, funders, policy experts, and beneficiaries to leverage the wisdom and experience of the crowd.
Hackathon attendees will generate new ideas to address some of the top challenges impacting health care in rural health settings and drive action to improve clinical outcomes, increase access, and better care experience for both patients and providers in rural communities.
Interested parties have two ways to participate:
- In-Person Hackathon: Engage with other dedicated experts to solve some of the toughest challenges facing rural communities through one of the in-person convenings hosted in three cities this summer:
- Wilson, North Carolina: August 29, 2024Please note that there is no virtual option for these events due to their collaborative, hands-on structure.
- Virtual Idea Submission: Submit your written concepts to address top rural health challenges using this form. All concepts must be submitted no later than September 9, 2024, at 11:59PM EST. Please note that late submissions will not be considered.
Top ideas with greatest opportunity for action will be highlighted in a public CMS Innovation Center report and connected with leading health policymakers and potential private or non-profit partners in the field. See below for details on how to participate.
Learn more about this opportunity here.
Register Now! NCTracks September 2024 Provider Training Schedule
Registration is now open for the NCTracks September 2024 training courses.
The courses are virtual, via Zoom, and can be attended remotely from any location.
Courses offered this month include:
- Submitting a Professional Claim
- Submitting a Prior Approval Institutional
- Submitting a Prior Approval Dental
- Provider Reverification
- New Office Administrator
- Ordering, Prescribing, and Referring (OPR) Provider Enrollment
See the document linked below for more information on course schedule and access to zoom links:
Sept. 2024 Provider Training Schedule
Share Your Story- Corporate Practice of Medicine
Please share your stories here on how corporate interventions in medicine have impacted you and your practice. This includes private equity acquisitions, noncompete agreements, management service organizations, and any business intervention that has impacted your ability to practice medicine.
Study: Blood Tests Allow 30-year Estimates of Women's Cardio Risks
"This is good for patients first and foremost, but it is also important information for (manufacturers of) cholesterol lowering drugs, anti-inflammatory drugs, and lipoprotein(a)lowering drugs - the implications for therapy are broad," said study leader Dr. Paul Ridker of Brigham and Women’s Hospital in Boston.
Your Feedback Needed: Help Improve the Medicaid Clinician Experience

NCMS's partners, Carolina Complete Health (CCH) and Carolina Complete Health Network (CCHN) will host their 2nd Annual Medicaid Managed Care Town Hall at the 2024 CPP Annual Meeting during NCMS LEAD Conference in November. In preparation for that session, we want to hear from clinicians across North Carolina who provide care to Medicaid enrollees.
Please share your experiences, challenges and successes, suggestions, and questions to help inform future programs, resources, opportunities, and collaborations that will improve health outcomes and enhance the overall care experience for Medicaid clinicians and enrollees.
All Medicaid clinicians are invited to complete this form, regardless of contract status with any of the PHPs.
Provide your feedback here.
Study: No Increased Risk of Mental Health Issues with Semaglutide Use

Taking the weight loss medication semaglutide did not increase the risk of depressive symptoms, suicidal thoughts, or suicidal behavior in persons without known major mental health disorders, according to a new study led by researchers from the Perelman School of Medicine at the University of Pennsylvania published in JAMA Internal Medicine.
Both the Food and Drug Administration (FDA) and the European Medicines Agency are actively monitoring the psychiatric safety of semaglutide and similar medications after post-marketing surveillance reports of depression, suicidal thoughts (ideation), and suicidal behavior in patients taking the drugs for the management of type 2 diabetes or obesity.
Semaglutide has emerged as a significant advancement in the field of weight management. Initially developed as a treatment for type 2 diabetes, the drug gained widespread attention after clinical trials showed it reduced baseline body weight by approximately 10–15%. Weekly injectable medications like semaglutide have become a popular option for health care providers to prescribe for patients.
As many as 5 million Americans were prescribed semaglutide in 2023, with nearly four in ten taking it for weight management.
The new study, led by Thomas Wadden, Ph.D., a professor of Psychology in Psychiatry and the former director of Penn's Center for Weight and Eating Disorders, analyzed data from over 3,500 participants across four major clinical trials. Researchers examined data from the Semaglutide Treatment Effect in People with obesity (STEP) trials—STEP 1, 2, 3, and 5. These studies were crucial in gaining approval from the FDA to use semaglutide 2.4 mg for obesity.
"The STEP trials provide strong evidence that semaglutide 2.4 mg reduces body weight and improves numerous health complications associated with obesity. Our new analyses provide assurance that the medication, when taken by individuals who are free of significant mental health concerns, does not increase the risk of depression, suicidal thoughts, or suicidal behavior," Wadden said.
He noted, however, that further study is needed of the psychiatric safety of semaglutide 2.4 mg when used by persons with current major depressive disorder, other serious mental illness (such as schizophrenia), or a history of suicide attempt. Individuals with such conditions were not included in the STEP trials.
The study examined changes in depressive symptoms using the Patient Health Questionnaire-9 (PHQ-9) and assessed suicidal ideation and behavior using the Columbia Suicide Severity Rating Scale.
Across the 68-week STEP 1–3 trials, semaglutide-treated participants, as compared to those who received placebo, did not show an increased risk of developing moderately severe symptoms of depression or of suicidal thoughts or behavior. Similar findings were observed in the 104-week STEP 5 study.
Examining all four STEP trials, researchers found that 1% or fewer of participants reported suicidal ideation or behavior during treatment, with no differences between semaglutide 2.4 mg and placebo.
Moreover, only 2.8% of the semaglutide-treated participants, versus 4.1% of those who received placebo, reported levels of depression at some point during treatment that required evaluation by a mental health professional. These rates are consistent with the risk of significant depression in the general population.
"It is certainly possible that individuals with overweight or obesity who take semaglutide may experience depressive symptoms or suicidal ideation or behavior, but the data suggest that persons not taking semaglutide—in the placebo group in this study—are equally likely to experience these conditions," said Gregory Brown, Ph.D., a study co-author and Director of the Penn Center for the Prevention of Suicide at the Perelman School of Medicine.
Wadden and Brown noted that their study's findings for semaglutide are consistent with results of the FDA's most recent analysis of post-marketing surveillance data for this class of medications which did not find "evidence that use of these medicines causes suicidal thoughts or actions." [source]
Register Now! 2024 National Healthy Aging Symposium

National Healthy Aging Symposium: Innovation Across the Age-Friendly Ecosystem
Thursday, September 26
1:00-5:00 p.m. ET
The Office of Disease Prevention and Health Promotion and Trust for America’s Health will host the National Healthy Aging Symposium: Innovation Across the Age-Friendly Ecosystem.
The Symposium will explore successful innovations that have been developed to improve older adult health and well-being and will build upon the successful and ongoing collaborations between aging services and public health that began at the first National Healthy Aging Summit and Workshop in 2015.
Policy makers, researchers, and professionals from across sectors will share their perspectives on important topics related to healthy aging through a series of panels covering topics like caregiving, social engagement, housing, transportation, brain health, and workforce.
NC Medicaid Offering Free Tailored Care Management Service

In July, NCDHHS launched Tailored Plans, a new kind of NC Medicaid Managed Care health plan for approximately 210,000 Medicaid beneficiaries with a serious mental illness, serious emotional disturbance, severe substance use disorder, intellectual/developmental disability or traumatic brain injury.
Tailored Care Management is a free service that pairs members with an expert to help with their healthcare needs, substance use disorder treatment and recovery services, mental well-being and other goals like finding a job.
With Tailored Care Management, eligible members can get personalized help from a Tailored Care Manager who guides them through the healthcare system or assists with basic needs like food and transportation. Visit Tailored Care Management toolkit in English and Spanish to find presentations, flyers, social media graphics, email templates, answers to frequently asked questions and more.
For more information about Tailored Plans, go to the NCDHHS website.
Investment Expands NC Child Treatment Program and Strengthen Behavioral Health Services for Children

The North Carolina Department of Health and Human Services announced a $4.5 million investment in the NC Child Treatment Program, a statewide initiative to train mental health providers in trauma-informed treatment models for children with complex behavioral health needs. NCDHHS is investing to expand access to proven behavioral health treatments so young people and their families receive the support they need sooner, and in the communities where they live and learn.
The investment is part of the department’s ongoing efforts to strengthen the child behavioral health workforce and build a continuum of services to improve outcomes for children and families.
"As we work to transform the child behavioral health system in North Carolina, we’re not only investing to increase access to services but to improve the quality of treatment available to children and families," said NC Health and Human Services Secretary Kody H. Kinsley. "We’re training more clinicians statewide to provide effective, evidence-based treatment with high standards so that children have access to the best possible care in their communities."
The NC Child Treatment Program trains mental health professionals and community agencies in a range of evidence-based treatment models shown to prevent the escalation of behavioral health symptoms by providing effective, timely and trauma-informed intervention. Demonstrated outcomes of treatment include a reduction in symptoms related to depression, suicidal thoughts, post-traumatic stress and other behavioral challenges.
In the first year of this investment, the number of clinicians and community agencies trained in existing and new clinical models through the program will increase by 96%.
"We have amazing caregivers and community professionals in our state who are committed to supporting our youth," said NCDHHS Director of Child and Family Strategy Hanaleah Levy Hoberman. "This is especially important when a young person experiences a behavioral health challenge that may otherwise prevent them from succeeding at home, in school or in their community. That’s why we’re investing to expand treatments that work with families and schools along with the child."
The NC Child Treatment Program is part of the Center for Child and Family Health (CCFH), which specializes in treating and preventing child traumatic stress and is a key partner in NCDHHS’ work to expand access to trauma-informed services. The department is contracting with CCFH to introduce new models into the program’s training curriculum and to extend the program to rural and underserved communities for more equitable access to services across the state.
"The North Carolina Child Treatment Program has been at the heart of the work of CCFH since 2014," said Robert Murphy, Ph.D., Executive Director of CCFH. "The investment of $4.5 million from NCDHHS will ensure that many more children and families, especially children living in rural areas of our state, will have access to cutting-edge treatments. Effectively transforming the lives of children and families served by the NC CTP trained clinicians."
NCDHHS’ investment focus includes the following models, in addition to other select evidence-based treatments effective for children and families:
- Trauma-Focused Cognitive Behavioral Therapy (TF-CBT) – A trauma-informed intervention for youth experiencing symptoms or behavioral challenges related to trauma, with active involvement from the child’s caregiver(s) to support long-term family healing.
- Cognitive Behavioral Interview for Trauma in Schools (CBITS) – A school-based service to address symptoms of traumatic stress for elementary through high school students.
- Cognitive Processing Therapy (CPT) – A tailored treatment for teenagers and caregivers navigating the impact of trauma and post-traumatic stress, often provided in an outpatient setting to help children remain at home or return home quickly.
- Problematic Sexual Behavior Cognitive Behavioral Therapy (PSB-CBT) – Group or family therapy that addresses a child’s difficulty recognizing socially acceptable boundaries for physical or sexual behavior. Most participants are successfully treated through outpatient services, avoiding the need for out-of-home placement.
In addition to training, CCFH will use the funding to provide enhanced consultation for agencies and clinicians to ensure fidelity to evidence-based models. The organization also offers implementation guidance on best practices for evidence-based treatments, helping ensure providers can maintain high quality of practice and services.
NCDHHS’ investment in the NC Child Treatment Program is part of a broader commitment to build an integrated behavioral health system for children in North Carolina. Of the historic $835 million allocated for behavioral health in the 2023 state budget, $80 million is dedicated to improving outcomes for children with complex behavioral health needs and their families. The department continues to invest in a spectrum of services — in homes, schools, communities and residential settings — that expand equitable access to high-quality, trauma-informed, family-centered care.
To help families and care managers find and access behavioral health services, CCFH maintains a statewide roster of NC Child Treatment Program providers. To access the roster and learn more about the program’s therapy models, visit ncchildtreatmentprogram.org.
Happy Birthday to Our Members Celebrating This Month!
Grab your party hats and noisemakers and let’s celebrate!
Sandra M. Abda, MD
James C. Abell, MD
Nicole M. Abello, DO
Patricia L. Adams, MD
Samuel B. Adkins, III, MD
Tehmina Adnan, MD
Vijay K. Agarwal, MD
Robert N. Agnello, DO
Mark D. Aldous, MD
Yousif Z. Alkadhi, MD
John R. Allbert, MD
Angela M. Allen, MD
William G. Allen, MD
Arghavan Almony, MD
Shehabaldin M. H. A. Alqalyoobi, MD
Joseph M. Alvarez, MD
Yashika Amin, MD
Kenneth A. Anderson, Jr., PA-C
George C. Andrinopoulos, MD
Hans C. Arora, MD, PhD
Kavita S. Arora, MD
Pradeep S. Arumugham, MD
Philip E. Ashburn, MD
Sarah Elizabeth W. Atkins, MD, MPH, FAAP
J. Spencer Atwater, Jr., MD
Frederick D. Austin, III, MD
Kirsten H. Avery, MD
Fadi S. Azer, MD
Rocky E. Bacelieri, MD
George T. Bailey, MD
Kristin D. Baker, MD
Matthew F. Baldwin, MD
Bailey S. Balentine, DO
Ricardo G. Baler, MD
A. Rodman Barber, MD
Brad P. Barnes, MD
Sydney F. C. Barnwell, MD
Caroline M. Barrett, MD
Rickey Baskett, Jr., MD
Zane K. Basrawala, MD
Charles R. Beasley, MD
Eric W. Beck, MD
Aileen Beckham, MD
Keith G. Begelman, MD
Carol R. Bell, MD
William B. Bell, MD
Lindsey M. Bellamy, DO
Larry F. Berman, MD
J. Lorraine Birdsong, MD
F. Alice Bishopric, MD
Cary F. Bizzell, MD
John A. Black, MD
Cameron T. Blackman, MD
Robert G. Blair, Jr., MD
Wendy S. Blair, PA-C
Kenneth R. Blanton, PA
Timothy A. Bleckley, MD
Alexander V. Boiwka, MD
Karl E. Bolstad, MD
Kenneth R. Bonfield, MD
Sherif B. Botros, MD
John E. Bourgeois, MD
Michael L. Bowen, MD
Jack W. Bowling, Jr., MD
Patrick Box, MD
Gray T. Boyette, MD
Stephen M. Bracewell, MD
Heather C. Braithwaite, MD
Chadwick R. Brasington, MD
Samantha L. Breen, DO
David C. Brendle, DO
Anthony C. Breuer, MD
Brian K. Brighton, MD
Dahari D. Brooks, MD
David A. Browder, MD
William E. Brown, MD, FACOG
Jon M. Bruce, MD, FACS, FASMBS
Clayton H. Bryan, MD
W. Blair Bryan, MD
Bethany L. Buie, PA-C
Rebecca A. Burbridge, MD
Jennie L. Byrne, PhD, MD, DFAPA
Arthur M. Calabretta, MD
David L. Call, MD
Donald B. Campbell, MD
Grant L. Campbell, MD
John K. Campbell, MD, PT
Antonio M. Carbonell, MD
Kelly A. Carney, MD
Marjorie B. Carr, MD
Sarah E. Carr, MD
Philips J. Carter, MD
L. Franklin Cashwell, Jr., MD
Vincent P. Castellano, MD
Brian J. Caveney, MD, JD, MPH
Stephen G. Cecil, MD
Rajat Chander, MD
Joe T. Chandler, MD
Geoffrey S. Chapman, MD
Timothy L. Chase, MD
Alexander W. Chasnis, MD
Priyank Chaudhary, MD
Christopher H. Chay, MD
Paul R. Chelminski, MD, MPH
Tong Y. Chen, MD
Sendhil K. Cheran, MD
Charles O. Chrysler, MD
Octavio Cieza, MD
Christine M. Ciszek, PA-C
Daniel L. Clarke-Pearson, MD, FACOG, FACS
Elizabeth B. Cleland-Roberts, MD
Michael G. Cloutier, MD
Edmund J. Cody, MD
Jason A. Coffey, MD
Wendy K. Coin, MD
F. Farrell Collins, Jr., MD, FACP
R. Andrew Collins, MD
Lawrence E. Colvin, Jr., PA-C
Jason T. Cook, MD
Lyndsay Cooper
John D. Corey, MD
Francis C. Corrigan, MD
Robert M. Cortina, MD
Billie F. Cosgrove, MD
Ronnie L. Cox, MD
Paul E. Craft, PA-C
Bert J. Crain, MD
James D. Crandall, MD
C. Marston Crawford, MD, FAAP
Dorwyn W. Croom, II, MD
Joseph Cruz, DO
Deepak Cuddapah, MD
Earl Cummings, PA
Ravi R. Dalal, MD
Kimberly A. Dao, MD
James L. Darsie, MD
Ivan David, MD
Vartan A. Davidian, Jr., MD
Dwight D. Davidson, MD
John E. Davis, MD
John S. Davis, MD
Leon D. Davis, MD
Jordan N. De Lay, PA-C
John R. Deans, MD
Andrew R. Deibler, MD
Geoffrey D. DeLeary, MD
Rebecca A. Demorest, MD
Steven H. Dennis, MD
Douglas H. DeSantis, MD
Donald G. Detweiler, MD
James E. DeVente, MD
Bruce M. Distell, MD
Emily A. Diznoff, MD
Katherine D'Orsi Williams, PA-C
Laura B. M. Dosier, MD
Arthur E. Douglas, Jr., MD
Denise E. Duff, MD
Christopher J. Dunatov, MD
David N. DuPuy, MD
Cecil T. Durham, Jr., MD
John R. Dykers, Jr., MD
Thomas S. Dziedzic, MD
James M. Edwards, MD
Palmer Edwards, MD, DFAPA
Yasser J. El-Abd, MD
John N. Ellis, MD
Eric T. Emerson, MD, FACS
James J. Epperly, Jr., DO
Rachel A. Erickson, DO
Darlene M. Esper, MD
Kelly R. Esposito, MD
Carrie A. Fales, MD
Peter F. Farmer, MD
Victoria O. Fashakin, MD
Carolina E. Fasola, MD
Gary J. Fischer, MD
Duane D. Fitch, MD
David P. Fitzgerald, MD
Henry A. Fleishman, MD
Stephen B. Fleishman, MD
Howard Floch, MD
Andrea C. Foiles, MD
Katie E. Fontaine, PA-C
Jonathan L. Forbes, DO
Mark D. Foster, MD
Vickie Fowler, MD
James F. Fraser, MD
Richard E. Frazier, MD
S. Mitchell Freedman, MD, FAAN
Mala A. Freeman-Kwaku, MD
Kevin M. French, MD
R. Everett Frerichs, MD, FAAP
Scott M. Frieary, DO
Michael D. Fried, MD
Douglas I. Friedman, MD
Jerry K. Froedge, MD, FAAP
Robert E. Gaddy, Jr., MD
Manasi Gahlot, MD
Judson P. Garbarino, MD
Ryan M. Garcia, MD
Garth J. Garramone, DO
Dana L. Garrett, MD
Debra J. Gazzuolo, MD
Peter A. Gentling, MD
John B. Gentry, MD
Zachariah Gerger, MD
Manisha Ghimire, MD
James S. Gibbs, MD
Brett J. Gilbert, MD
Brent R. Gill, MD
Brooks W. Gilmore, MD
Christopher A. Gilmore, MD
Thomas M. Ginn, MD
David L. Glenn, Jr., MD
Tapan N. Godiwala, MD
Raj Gondalia, MD
Margaret E. Goodwin, MD, FAAP
Lakshmi Gordon, MD
Raghavender Gotur, MD
Arthur L. Graff, MD
R. Eugene Granger, MD
Kelsey R. Graven, DO
Taylor W. Green, PA-C
Michael W. Grier, MD
Daniel Gutman, MD
Joseph F. Hakas, Jr., MD, FACC
James L. Hamby, MD
Crystal B. Hammons, DO
Emily A. Hannon, MD
Harriet N. Hansell, MD
Marie N. Hardy, MD, FAAD
Brent T. Harkrider, MD
Stewart J. Harley, MD
Revella B. Harmon, MD, MPH
John M. Harrelson, MD
James W. Harris, Jr., MD
Amanda R. Hart, PA
Jessica L. Hart, MD, FAAP
Lisa M. Hartman, MD
John F. Hartness, Jr., MD
Christopher C. Hasty, MD
W. Benjamin Hatcher, MD
Henry C. Hawthorne, Jr., MD
Renee P. Haynesworth, MD
Ansley M. Heath, PA-C
Nathan W. Heath, PA
Samuel A. Heathcote, Sr., MD
Joel A. Hedlund, MD
James F. Hedrick, MD
Mark R. Hedrick, MD
William W. Hedrick, MD
Peter W. Heetderks, MD
Timothy J. Heffron, MD
Melissa A. Helman, MD
Martin M. Henegar, MD
John T. Henley, Jr., MD
John H. Herring, MD
William A. Herring, Jr., MD
Lloyd M. Higgins, MD
Lacy C. Hobgood, MD, FACP
Lauren M. Hodges, MD
Edward W. Hoehn-Saric, MD
James B. Hoer, MD
Suneya G. Hogarty, DO
Chad A. Holder, MD
John C. Holder, MD
W. Claude Hollingsworth, MD
James H. Holmes, IV, MD
Henry D. Holt, MD
Thomas E. Hooper, MD, FACP
Marbry B. Hopkins, III, MD
Kirk A. Howard, MD
Jennifer G. Hudson, MD
Joshua R. Hughes, MD
Kaissar S. Ibrahim, MD
Adam A. Ingraffea, MD
Alexandra B. Inyang, MD
Todd A. Irwin, MD
Latonja M. Ivery, MD
Peter W. Jaber, MD
Ashwin Jain, MD
Andrew M. Jakubowicz, MD
Arvind N. Jariwala, MD
Wayne T. Jarman, MD, FACS
Stanleigh E. Jenkins, Jr., MD
Charles S. Jere, MD
Harriman H. Jett, MD
Donald C. Johnson, MD
John H. Johnson, MD
Kaddijatou S. Johnson, PA-C
Rachel M. Johnson, MD
William M. Johnstone, Jr., MD, JD, MBA
Robert H. Johr, MD
Charles W. Jones, MD
Mary E. Jones, MD
George L. Jordan, III, DO
Cristian A. Jurau, MD
J. Marc Kadyk, MD
Lisa M. Kafer, MD, FAAP
Rajdeep S. Kanwar, MD
Ulf L. Karlsson, MD
Mark A. Kasari, MD
Deepakta Kaur, DO
Hailu M. Kebede, PA-C
Katherine Keck, MD
J. W. Keeling, MD
Claire A. Kelleher, MD
Siva S. Ketha, MD
Faisal M. Khan, MD
Saad S. Khan, MD
Atul Khanna, MD
Jefferson K. Kilpatrick, MD
Paul K. Kim, MD
Brandon S. Kinneman, PA-C
Rex A. Kiteley, II, MD
F. A. Koontz, MD
Lawrence D. Krabill, MD
Alex R. Kroft, PA-C
Daniel P. Krontz, MD
Eric F. Kuehn, MD
Gregory M. Kurkis, MD
Adam J. Lake, MD
Andrew S. Lamb, MD
Christian J. Lambertsen, Jr., MD
Charles G. Lampley, IV, MD
John A. Lang, III, MD
Marianna G. Law, MD
Richard M. Leighton, DO
Evan M. Leitz, MD
Melissa L. Lemnah, PA-C
Philip G. Leone, MD
Peter L. Leuchtmann, MD
Felicia Levine, PA-C
Andrew J. Lewis, Jr., MD
Clifford T. Lewis, MD
Richard S. Lewis, MD
Stacey Lindo-Ukata, MD
Frederick C. N. Littleton, Jr., MD
Tyler P. Litton, MD
Michael S. Loboda, MD
Robert J. Logel, MD
John A. Lowery, MD
Chancy G. Lucas, MD
Wayne B. Lucas, MD
George B. Lutman, MD
Surendrapal S. Mac, MD
Katherine T. MacDonald, MD
Murthy V. S. Madduri, MD
Christopher J. Magryta, MD
Michelle M. Maher, MD
Nicholas H. Mai, MD
Rachel H. Main, PA-C
Lindsay R. H. Maitland, MD, FAAP
Julie E. Manly, MD
Charles H. Mann, MD
Courtney H. Mann, MD
Theodore B. Manny, Jr., MD
Kevin K. Manocha, MD
Lisa I. Mansur, MD
James T. Marino, MD
Anne T. Martinelli, MD
Sameer Mathur, MD
Curtis J. Matthews, Jr., MD
Eric E. Maur, MD
Taylor E. Maxwell, PA-C
Sharidan J. Maxwell Hill, MD
C. Douglas Maynard, MD
Ryan K. McBeth, MD
Robert B. McBride, Jr., MD
Ryan S. McComb, MD
Elizabeth A. McCool, PA-C
W. Jason McDaniel, Jr., MD
Christopher N. McDaniels, MD
Kara A. M. McElligott Park, MD, MPH
Michael L. McGehee, MD
L. Scott McGinnis, III, MD
Erin K. McGloin Shanahan, MD
Patrick L. McKenzie, MD
Ryan L. McKimmie, MD
Tracey M. McKinzie, PA-C, MPAS
C. Scott McLanahan, MD
Christopher W. McQuinn, MD
Thomas J. Meakem, III, MD
Miriam Medero-Eng, MD
William D. Medina, MD
Bettina B. Meekins, MD
Paul D. Mehlhop, MD
Todd D. Meisinger, MD
Radha V. Menon, MD
Darlyne Menscer, MD
Jay W. Meredith, MD
Margaret C. Merrick, MD, FAAP
Michael S. Merrill, MD
David K. Mertz, MD, FAAP
Keri D. Metcalf, MD
Mark R. Mikles, MD
Erik J. Miles, MD
Henry S. Miller, Jr., MD
Farhaan R. Mir, MD
Sanjib P. Mohanty, MD
Daniel J. Mollin, Jr., MD
William M. Monroe, MD
Kelley O. Montoya, MD
George H. Moore, Jr., MD
Richard S. Moore, Jr., MD
Frank H. Moretz, MD
Lynne R. Morgan, MD
Aundrin Moss
Daniel J. Motuz, MD
Joseph P. Mullen, III, MD
Kimberly C. Munro, MD
Richard S. Myers, MD
Larry A. Napolitano, Jr., MD
Nirmala Narasimha, MD
John A. Narron, III, MD
Adnan Nasir, MD
Joe Navejar, IV, DO
John W. Neal, VI, MD
Shelileah R. Newman, MD
William H. Newman, MD
Phillip N. Nguyen, MD
Julia M. Niemi, PA-C
Gary S. Niess, MD, FACC
Ronald A. Noe, DO
Michael E. Norins, MD
Michelle R. Nzuna, DO
Lyndsay A. Oancea, MD
Joseph G. O'Brien, MD
Shelly B. Odom, Jr., MD
Laura N. Okolie, PA-C
Arnold C. Olegario, MD
Fred W. Ortmann, IV, MD
Barry S. Ostrow, MD
William J. Panzo, PA-C
Jonathan M. Parish, MD
James A. Partridge, MD
Barry R. Pate, MD
Anooj D. Patel, MD
Neha Patel, DO
Niyati S. Patel, DO
Shreyang H. Patel, MD
Sunny H. Patel, MD
Swetang M. Patel, MD
Tirth V. Patel, MD
Marissa Patterson
Laura G. Patwa, MD
Nicholas P. Pediaditakis, MD
Sara Perez, PA-C
Jennifer A. Perkins, PA-C
John F. Perrin, MD, FACEP
Joseph W. Ponzi, MD
Karla M. Pou, MD
Dustin C. Powell, MD
LeVonne G. Powell-Tillman, MD
James P. Pressly, MD
Mary E. Price, MD
Robert E. Price, Jr., MD
Camilla A. Proctor, MD
George H. Provosty, MD
Jeremy W. Pyle, MD, FACS
Kiera A. Quinn, PA-C
Amy H. Radzom, DO
Florian J. Ragaz, MD
Robert J. Raible, Jr., MD
Sujatha Raman, MD
Lakshman Rao, MD
Heather R. Ratcliffe, PA-C
Elizabeth M. Rattle, PA-C
Christopher Z. Rayala, MD
Elizabeth C. Reichard, MD
Patricia A. Reichert, DO
Evan R. Restelli, DO
Evan J. Rey, DO
Janelle A. Rhyne, MD, MACP
Alexandra C. Rice, MD
Cynthia W. Richards, MD
David J. Rickard, DO
Stephanie L. Riggins, MD
Syed A. R. Rizvi, MD
John P. Roberson, MD
Ketarah C. Robinson, MD
Timothy M. Robinson, MD
Jim A. Rogers, MD
A. Silvia Ross, MD
Robert E. Ross, Jr., MD
Stephen E. Rostan, MD
Richard E. Roux, MD
Marie S. Rowe, MD, FACOG
Eugene F. Russell, II, MD
Steven M. Russo, DO
Darryl A. Sandidge, PA-C
Justin D. Sargent, DO
Sarah Ann M. Saunders, PA-C
Charles J. Sawyer, III, MD
John R. Scagnelli, MD
Brian P. Scannell, MD
Julie H. Schopps, MD
Joseph J. Schreiber, MD
Jodi Schwab, MD
John L. Scott, MD
Brent W. Seifert, MD
Frank T. Shafer, MD
Dhirenkumar N. Shah, MD, FACC
Erika R. Shah, MD
Priyavadan M. Shah, MD, FACC
Cynthia Shahan, MD
Azra P. Shaikh, MD
Deepti Sharma, MD
Robert A. Sharpe, MD
Michael R. Shaughnessy, MD
Douglas D. Sheets, MD, FACOG
Scott B. Shepard, PA-C
M. Trevor Shick, MD
William R. Shipley, MD
Edwin H. Shoaf, Jr., MD
Christopher J. Shuman, MD
Jason A. Silva, MD
Ashima Singal, MD
Nadine B. Skinner, MD, FAAFP
Collin D. Smith, DO
E. Travis Smith, Jr., MD
Ginger E. Smith, PA-C
Lyman S. Smith, MD
Lynn K. Smith, MD
Rebecca J. Smith, DO
Stephen R. Smith, PA-C
Alexander J. Snyder, MD
John M. Solic, MD
J. Kim Song, MD
James R. Spears, MD
Thomas R. Spruill, MD
George Stamataros, DO
Malcolm T. Stark, Jr., MD
Eric N. Stashko, MD
Jeffrey P. Stein, MD
Henry L. Stephenson, Jr., MD
Shane B. Sterling, MD
E. Walker Stevens, Jr., MD
P. Lindsay Stevenson, MD
Robert I. Steward, MD
Todd I. Stone, PA-C
Phillip E. Stover, MD
Srikar R. Sudini, MD
Thomas E. Sumner, MD
Royce R. Syracuse, MD
John P. Taliaferro, MD
Knox R. Tate, MD
Julian R. Taylor, MD
Christopher L. Tebbit, MD
Michael R. Tedrow, DO
Charles H. Tegeler, IV, MD
Fredrick A. Teixeira, MD
Charles C. Thomas, II, MD, FACRO
Megan R. Thomas, MD
Willard R. Thompson, Jr., MD
Roger Z. Thurman, MD
Karen G. Todd, MD
Stuart K. Todd, MD
David E. D. Tolentino, DO, FACOI
S. Susan Torres, MD
Erron J. Towns, MD, FAAP
Brent A. Townsend, MD
Victoria Trapanotto, DO
G. Earl Trevathan, Jr.
Michael D. Tripp, MD
Andre K. S. Tse, MD
Theodore Tsomides, MD, PhD
Rita M. Tucker, MD
Rosemary H. Tulloh, MD
Chad A. Turner, PA-C
Daniel R. van Rooyen
Indira M. Varia, MD
Alison D. Vasan, MD
Allin C. Vesa, MD
Carrie H. Vice, MD
Sean P. Wagner, MD
Earl W. Walker, Jr., MD
Karen J. Walter, MD, FAAP
Jeffrey T. Waltz, MD
Walter J. Wardell, MD
Craig A. Warner, MD
Susan C. Watson, MD
R. Randolph Weast, MD
Richard T. Weisenburger, DO
Steven T. Welch, MD
Adam H. Wells, MD
John S. Welsh, Jr., MD
Sean S. Wentworth, MD
Aaron A. Westphal, MD
Joseph D. Whisnant, Jr., MD
Shea T. Whittaker, PA-C
Grace K. Wilcox, DO
David M. Williams, III, MD
Johnathan D. Williams, MD
Joseph D. Williams, DO
Meghan B. Williams, MD
Robert C. Williams, Jr., MD, FACS
Rufus D. Williams, Jr., MPAS, PA-C
Linda L. Willis, MD
Julian D. Willoughby, MD
John E. Wise, MD
Joanna B. Wisotsky, PA-C
Kurt P. Wohlrab, MD
Karen E. Wood, MD
Warden L. Woodard, III, MD
LaToya N. Woods, DO
Hannah E. Woriax, MD
Michael A. Worobel, DO
Andrew C. Wu, MD
Robert T. Wyker, MD
Amber C. Yarrison, PA-C
Kimberly B. Yates, MD
Zahra H. Younes, MD
Sarah W. Young, MD
Roland M. Zahn, MD
William M. Zban, MD, FACEP
Julia Zhu, PA-C
Eugenia F. Zimmerman, MD
Robert E. Zipf, Jr., MD
2024-2025 Flu Vaccine Recommendation

CDC recommends everyone 6 months of age and older, with rare exceptions, receive an updated 2024-2025 flu vaccine to reduce the risk of influenza and its potentially serious complications this fall and winter. CDC encourages providers to begin their influenza vaccination planning efforts now and to vaccinate patients as indicated once 2024-2025 influenza vaccines become available.
Most people need only one dose of the flu vaccine each season. While CDC recommends flu vaccination as long as influenza viruses are circulating, September and October remain the best times for most people to get vaccinated. Flu vaccination in July and August is not recommended for most people, but there are several considerations regarding vaccination during those months for specific groups:
- Pregnant people who are in their third trimester can get a flu vaccine in July or August to protect their babies from flu after birth, when they are too young to get vaccinated.
- Children who need two doses of the flu vaccine should get their first dose of vaccine as soon as it becomes available. The second dose should be given at least four weeks after the first.
- Vaccination in July or August can be considered for children who have health care visits during those months if there might not be another opportunity to vaccinate them.
- For adults (especially those 65 years old and older) and pregnant people in the first and second trimester, vaccination in July and August should be avoided unless it won’t be possible to vaccinate in September or October.
Updated 2024-2025 flu vaccines will all be trivalent and will protect against an H1N1, H3N2 and a B/Victoria lineage virus. The composition of this season’s vaccine compared to last has been updated with a new influenza A(H3N2) virus.
For more information on updated COVID-19 vaccines visit: Coronavirus Disease 2019 (COVID-19) | CDC. For more information on updated flu vaccines visit: Seasonal Flu Vaccines | CDC.
The following statement is attributable to CDC Director Dr. Mandy Cohen:
“Our top recommendation for protecting yourself and your loved ones from respiratory illness is to get vaccinated,” said Mandy Cohen, M.D., M.P.H. “Make a plan now for you and your family to get both updated flu and COVID vaccines this fall, ahead of the respiratory virus season.”
Visit the CDC website for more information.
Newly Approved Medical Technology Treats Blocked Stents

Newly approved medical technology offered at Atrium Health has helped a local man get back on his feet after a stent in his artery was blocked by scar tissue.
Stan Ciepcielinski is grateful for time with his grandkids, which is something he didn’t think he would be alive to see 10 years ago. “Back then I had three grandchildren,” he told Channel 9. “Now, I have eight, and I get to enjoy them all the time now.”
Things went wrong when he was hiking the Great Wall of China during a business trip.
“I got up on the wall and couldn’t breathe,” Ciepcielinski said. And the chest pains didn’t go away even after he got home. He went to Atrium Health and after many tests, doctors told him he had congestive heart failure. “They just said, ‘You need a new heart,’” he said. “It was totally a surprise. I thought they were going to give me some more medication.”
Ciepcielinski was lucky enough to receive a new heart eight days after he was put on the transplant list. He gets evaluated every two years, and in June, a stent in his artery was blocked by scar tissue. The narrowing of the artery slowed blood flow to and from his heart in a condition known as in-stent restenosis.
Dr. Nyal Borges at Atrium Health said in-stent restenosis is common with stent patients and now there’s an easy treatment. “We have a big opportunity to help a lot of patients,” Borges said.
The FDA approved new technology this summer that is offered at Atrium Health. It uses a medicated balloon that coats stents.
“It actually chemically changes what is happening in the artery, prevents scar tissue from forming and the chemicals that are produced to heal that scar are no longer made,” the doctor said.
Ciepcielinski said he was home the same afternoon as the procedure and back to normal after two days. He’s back to running marathons and spending quality time with his eight grandkids. “It’s just a huge step forward and it’s so exciting, he said. “Especially for people like me … I needed this technology to keep me alive.”
[source]
What You Should Know About Mosquito-spread Virus Triple E

Eastern equine encephalitis (EEE or Triple E) virus is transmitted by the bite of infected mosquitoes. It can cause serious illness in people as well as horses, donkeys, emus and ostriches. Although uncommon in people, Triple E is one of the most severe mosquito-transmitted diseases in both horses and humans in the United States. Approximately a third of people who become ill with Triple E die. Many people who survive Triple E suffer from long term brain damage. Those under age 15 and over age 50 are at greatest risk of developing severe disease. From 2003 to 2020, 12 human cases of Triple E were reported in North Carolina, with infections occurring from July through December.
In North Carolina, Triple E virus is most commonly detected in the eastern part of the state, where the virus is normally passed between wild birds and mosquitoes. The mosquito species that is the main carrier of Triple E spends most of its time in freshwater swamps and almost exclusively bites birds rather than horses and humans.
People can protect themselves from Triple E by preventing mosquito bites. Consistent use of effective mosquito repellents during the months when they are active is important. A second method is mosquito control efforts, especially in areas near freshwater swamps. There is no vaccine to protect humans from Triple E, and no cure once a human is infected. Treatment is limited to managing the symptoms of the disease.
Autumn is also the time of year when most cases of other mosquito borne viral illnesses are reported, such as West Nile virus and La Crosse virus infections. To prevent mosquito-borne illness, NCDHHS’ Division of Public Health encourages people to practice the “3 Ds”:
- Dress – Wear loose, light-colored clothing that covers your skin.
- Defend – When the potential exists for exposure to mosquitoes, repellents containing DEET (N,N-diethyl-meta-toluamide) are recommended. Picaridin and oil of lemon eucalyptus are other repellent options. Learn more about insect repellent options.
- Drainage – Check around your home to rid of standing water, which is where mosquitoes can lay their eggs.
Most people infected with eastern equine encephalitis don’t develop symptoms, but some can come down with fever or swelling of the brain and about one third of people infected die. There have been three cases of eastern equine encephalitis in the U.S. this year, according to the U.S. Centers for Disease Control and Prevention, one each in Massachusetts, New Jersey, and Vermont. The worst year for the disease was 2019, with 38 cases.
If you have specific questions pertaining to Triple E in humans, please contact the Communicable Disease Branch at 919-733-3419.
For questions about Triple E in horses, please consult your veterinarian or the North Carolina Department of Agriculture and Consumer Services, Veterinary Division, at 919-733-7601.
One More Way We Take Care of You! Explore the NCMS Retirement Association Plan.
Contact Our Plan Manager here.
Duke’s PAS Offers Virtual Grief Support Group for Employees

The Duke Personal Assistance Service (PAS) rolled out four new virtual support groups to provide support to University faculty and staff who are processing grief from the loss of a loved one, presenting an opportunity for them to “process uncomfortable emotions and discuss coping skills.”
The newly-offered support sessions — modeled after a support group held at Duke Raleigh Hospital — will serve a wider community of staff and faculty employed by the University and the Duke Health System. The groups are scheduled to meet 4 p.m. to 5 p.m. weekly beginning Wednesday through October 2.
“[We] realized that a lot of people at Duke Raleigh happened to be experiencing grief around the same time,” said Caryn Christiano, senior EAP counselor for the personal assistance service, speaking of the decision to create the original program. “Because we’re at a place right now where we can do more … that’s kind of why [the expansion] was then rolled out.”
Initially, PAS planned to offer one virtual support group, but an unanticipated spike in interest led to the creation of three more groups. Currently, 26 people remain on a waiting list to join a support group, all of whom are still able to contact PAS for immediate support individually.
Continue to full article here.
Diabetes Performance Improvement in Primary Care Live Webinar
Diabetes Performance Improvement in Primary Care
Wednesday, October 23, 2024
12 pm – 1pm
Live Webinar

Program Overview
This educational activity aims to inform the learner about the status of diabetes and chronic kidney disease in primary care. This activity will explore barriers and facilitators to promote patient engagement in treatment. This activity will focus on performance improvement methods and activities which promote health among patients with diabetes.
Who Should Participate
Physicians, Physician Assistants, Nurse Practitioners, Nurses, and Primary Care Office Staff
As part of our commitment to diversity and inclusion, the Northwest AHEC provides compassionate education and respectful care for all, regardless of socioeconomic status, race, ethnicity, language, nationality, sex, gender identity, sexual orientation, religion, geography, disability and age.
Objectives
Upon completion of this activity, participants should be better able to:
- Describe barriers and strategies for clinical care teams in the screening, diagnosis, and treatment of patients with diabetes and chronic kidney disease (CKD).
- Utilize new methods to identify how diabetes and CKD disproportionately affect racial and ethnic minorities in clinical workflows.
- Explain processes for screening, diagnosis, and raising awareness about diabetes and its connection to chronic kidney disease (CKD)
Download the event brochure here.

Join the 2024–25 NACHC Community Health Center Climate Action Incubator
Do you work in a community health center in the United States?
Are you interested in pursuing decarbonization measures for your health center for a cleaner, greener community?
Are you interested in working with like-minded colleagues from across the United States to help mitigate the impacts of the climate crisis?
The Medical Society Consortium on Climate and Health (MSCCH) and the National Association of Community Health Centers (NACHC) are pleased to invite applicants with a passion for making a difference on climate and health to join the 2024-2025 Community Health Center Climate Action Incubator. The goal of this project is to enable participants to hone their leadership skills in making effective climate action and decarbonization proposals at their own health centers. Specifically, the program is designed to deepen participants’ knowledge and improve their advocacy and communication skills through peer-to-peer learning.
Community health centers are on the frontlines of understanding and responding to the climate crisis as a health crisis. Community health centers are trusted leaders in their communities. Engaging in climate action and decarbonization efforts is a triple win. It helps mitigate the climate crisis, aligns the center’s actions with its mission to improve community health, and leverages its leadership position to help spark wider community impact.
Program participants will engage with top voices in the climate and health movement, learn valuable advocacy and communication skills from industry leaders, and work together to develop and refine proposals to bring back to their own health centers.
Participant learning objectives:
- Understand how climate change drives inequitable health impacts.
- Assess localized climate impacts on health centers and analyze opportunities to mitigate impact through decarbonization and resiliency measures.
- Identify opportunities for decarbonization by understanding the policy and regulatory landscape.
- Develop and use advocacy, communications, and organizing skills to build a compelling case for decarbonization for leadership.
The project will enlist 20 participants from community health centers in the United States and its territories. Health centers are strongly encouraged to form teams of two to three people but applications from individuals are also welcome. No more than three people from any one health center will be accepted. Each team member should complete an application form.Each participant will be awarded $3000 upon successful completion of the program.
Applicant requirements:
- Completed application including CV and signed letter of support from CEO
- Current employment by a community health center in the United States or its territories
- CEO support for participation including willingness to give applicant time to participate in sessions and willingness to allow applicant to present decarbonization proposal to CEO, board, and/or other relevant decision-makers. Letter of support to be completed and uploaded is available here.
- Commitment to participate in sessions, develop and pitch decarbonization proposal, and complete any work between sessions. There will be 7 monthly sessions between September 2024 and June 2025. Each monthly session is 3-4 hours in duration. Additionally, participants will be asked to develop and present a virtual presentation for the MSCCH Annual Meeting. It is expected that participants will work 2-3 hours per week on average completing readings and developing their decarbonization proposals.
Applications close on August 30, 2024. Participants will be notified on September 13, 2024.
[source]
WakeMed Named Best Hospital for Bariatric Surgery

WakeMed Cary Hospital was recently recognized as one of the best hospitals in the nation for bariatric surgery.
Money Magazine’s editorial team analyzed 125,000 data metrics to determine the top 75 bariatric surgery centers in the country. WakeMed Cary Hospital came in at #6 in the U.S. and #1 in N.C. These top hospitals represent excellence, offering safe, effective weight-loss procedures led by skilled bariatric surgeons and specialists.
WakeMed Cary Hospital is accredited as a Comprehensive Center for bariatric surgery by the American College of Surgeons (ACS) Metabolic and Bariatric Surgery Accreditation and Quality Improvement Program (MBSAQIP), in partnership with the American Society for Metabolic and Bariatric Surgery (ASMBS). The hospital has also earned the Cigna Center of Excellence in Bariatric Surgery and is a Blue Distinction Center for Bariatric Surgery (BCBSNC).
WakeMed offers bariatric surgery options performed by exceptional, experienced surgeons who care about the long-term success of their patients. Whether a gastric bypass, sleeve gastrectomy, duodenal switch or a revisional procedure, WakeMed provides the most advanced surgical procedures, a comprehensive weight loss program and highly skilled clinical and support team to help patients reach their goals.
Money partnered with Denniston Data and Definitive Healthcare in creating a methodological approach that favors facilities that have received strong quality care and patient ratings from the federal Centers of Medicare & Medicaid Services as well as accreditation in metabolic and bariatric care from the American College of Surgeons. View more information on the methodology.
[source]
Your Vote is Your Voice! Make Sure It’s Heard Loud and Clear!

As healthcare providers, you have a unique perspective on the challenges facing your communities. Now, more than ever, it's crucial that your voices are heard at the polls. With the upcoming election fast approaching, we want to ensure that you have all the information you need to make your vote count.
Are you registered to vote? If not, instructions are available from the NC State Board of Elections.
Is your voter registration up to date? You can check to make sure their registration information is accurate using the Voter Search tool. Instructions for updating your record are available online as well.
Important General Election dates to note:
- Sept. 6, 2024: County boards of elections begin mailing absentee ballots to eligible voters who submitted an absentee ballot request form.
- Oct. 11, 2024: Voter registration deadline (5 p.m.).*
- Oct. 17, 2024: In-person early voting begins; same-day registration available.
- Oct. 29, 2024: Absentee ballot request deadline (5 p.m.).*
- Nov. 2, 2024: In-person early voting ends (3 p.m.).
- Nov. 5, 2024: General Election Day.
- Nov. 5, 2024: Absentee ballot return deadline (7:30 p.m.).*
*Voter registration and absentee voting deadlines are different for military and overseas citizen voters.
Want to view your sample ballot for the General Election? Registered voters can find their sample ballot in the “Your Sample Ballot” section of their Voter Search profile when they become available.
Don’t forget your photo ID: North Carolina voters will be asked to show photo ID when they check in to vote. Learn more: Voter ID.
Plan ahead. There are three ways you can vote:
7 NCMS Members will be on the 2024 General Election Ballot

North Carolina has six physicians and one physician assistant contending for legislative seats in the 2024 General Election.
NC House of Representatives
Grant Campbell, MD – Ob/Gyn / Concord, NC
Ralph Carter, MD – Orthopaedic Surgery / Laurinburg, NC
Timothy Reeder, MD – (incumbent)Emergency Medicine / Greenville, NC
NC Senate
David Hill, MD – Pediatrics / Wilmington, NC
Mark Hollo, PA – Retired / Conover, NC
US House of Representatives
Steve Feldman, MD – Dermatologist / Winston-Salem, NC
Greg Murphy, MD – (incumbent) Urologist / Greenville, NC
Interviews with each candidate are posted online at the NCMS website and can be accessed at the QR code below.

Register Now! NC Medicaid Managed Care Virtual Office Hours: Hot Topics
Register now for September's Virtual Office Hours on Provider Enrollment!
Medicaid Managed Care
Virtual Office Hours:
NC Medicaid Provider Enrollment Hot Topics
Thursday, September 5
5:30 p.m.
Learn about Provider Enrollment updates and other program initiatives that highlight the good work being done in North Carolina.
NC Medicaid Clarifies Clinical Coverage Policies on Respiratory Equipment and Supplies, Sleep Studies, Polysomnography Services

In response to recent policy and billing questions, NC Medicaid would like to clarify that respiratory supplies needed to conduct a Home Sleep Tests (HST) or Unattended Sleep Study are not covered separately.
Effective October 1, 2020, the following update was made to Clinical Coverage Policy 5A-2, Respiratory Equipment and Supplies in subsection 5.3.2:
The medical necessity criteria for respiratory assist devices to manage central sleep apnea and obstructive sleep apnea were updated to indicate that qualifying polysomnograms must be provided according to the requirements listed in Clinical Coverage Policy 1A-20, Sleep Studies and Polysomnography Services.
Specifically, the requirement for a facility-based polysomnography by qualified personnel was removed, as Clinical Coverage Policy 1A-20, Sleep Studies and Polysomnography Services, allows for home sleep studies of Obstructive Sleep Apnea in subsection 3.2.1, criterion b. “Home Sleep Test (HST) or Unattended Sleep Studies”.
Please also note that Clinical Coverage Policy 1A-20, Sleep Studies and Polysomnography Services, was updated on May 1, 2020, to include 95800 Sleep study, unattended, simultaneous recording, heart rate, oxygen saturation, respiratory analysis (eg, by airflow or peripheral arterial tone), and sleep time.
The device used for an unattended or home sleep test is not coded separately. The physician dispatches the device for the patient to take home and the patient returns or ships back the device to the physician’s office.
Questions? Contact NC Medicaid Contact Center at 888-245-0179
[source]
No-Cost COVID-19 Tests Available Through Mail Again Soon

On the heels of a summer wave of COVID-19 cases, Americans will be able to get free virus test kits mailed to their homes, starting in late September.
U.S. households will be able to order up to four COVID-19 nasal swab tests when the federal program reopens, according to the website, COVIDtests.gov. The U.S. Health and Human Services agency that oversees the testing has not announced an exact date for ordering to begin.
The tests will detect current virus strains and can be ordered ahead of the holiday season when family and friends gather for celebrations, an HHS spokesperson said in an emailed statement. Over-the-counter COVID-19 at-home tests typically cost around $11, as of last year.
The announcement also comes as the government is once again urging people to get an updated COVID-19 booster, ahead of the fall and winter respiratory virus season. Earlier this week, U.S. regulators approved an updated COVID-19 vaccine that is designed to combat the recent virus strains and, hopefully, forthcoming winter ones, too. Vaccine uptake is waning, however. Most Americans have some immunity from prior infections or vaccinations, but data shows under a quarter of U.S. adults took last fall’s COVID-19 shot.
[source]
NCMS Member Named Vice President of Physician Services at UNC Health Caldwell
 Bradley Christoph, DO, MPH, MS
Bradley Christoph, DO, MPH, MS
NCMS member Bradley Christoph, DO, MPH, MS, has been announced as the new Vice President of Physician Services at UNC Health Caldwell!
Dr. Christoph serves the Caldwell County community as a family medicine practitioner at Southfork Medical Park in Cajah's Mountain and as the Medical Director at Helping Hands Clinic in Lenoir.
He completed his residency at The Ohio State University where he was named the Intern of the Year in 2018 and Executive Chief Resident in 2021.
Congratulations, Dr. Christoph, on your new role!
Capitol Chronicle: Join NCMS for the 2025 National Advocacy Conference in Washington

Capitol Chronicle: Join NCMS for 2025 National Advocacy Conference in Washington
The AMA’s National Advocacy Conference is scheduled for February 10-12, 2025. This yearly event offers an opportunity for personal involvement in the health policy debate on Capitol Hill. We need increased NCMS member engagement with our members of Congress, so mark your calendar and stay tuned for forthcoming details.

2025 National Advocacy Conference
Save the date and join us for our return to Capitol Hill.
February 10-12, 2025 / Washington, DC
Plan now to join your colleagues as we advocate for patients and the medical profession on . . .
Prior Authorization Relief
Medicare Payment Reform
Workforce Shortage Solutions
Physician Wellness
Mark your calendar! Registration details and additional information coming soon.
Your engagement matters!
Do you know your state and federal legislators? More importantly, do your legislators know you?
The NCMS can help you connect with policy makers as a constituent and advocate!
Register Now! Sustainability of the HIV/AIDS Response – Getting to 2030 & Beyond

The state of the HIV/AIDs endemic is reaching a critical point requiring evaluation of the current state of the global response, progress made thus far, and planning for post-2030 goals. The National Academy of Medicine is hosting a timely international meeting to facilitate discussion on these issues.
This one-day workshop is being held on September 18, 2024, from 9:00 AM – 5:00 PM US Eastern. Ambassador John N. Nkengasong, the Senior Bureau Official for Global Health Security and Diplomacy at the U.S. State Department, will deliver the opening remarks. His address will set the stage for discussions across three subsequent panels.
Broadly, the goals of this workshop are to:
- Explore how we can re-energize the global HIV response to reach the 2030 goals but also to look beyond.
- Craft strategies to increase and sustain political commitment.
- Highlight global accountability and domestic-donor financing.
A Paw Print Sticker on Your Mailbox? Leave It!

Mail Carriers face the risks of a nip, bite, or even a vicious attack while delivering mail and packages each day. Aggressive dog behavior poses a serious threat to Postal Service employees. In response, USPS is implementing a Dog Paw program to raise awareness for Letter Carriers and customers on the risk of dog bites throughout their workday.
The program involves using color coded stickers to indicate both the home of a dog as well as the house before a dog’s home, to better prepare the Letter Carrier as they approach the mailbox. An orange sticker tells carriers that there is a dog at this home and the yellow cautions the carrier that there is a dog at the next house.
As customers see these stickers posted on their mailbox, they will also receive a postcard explaining the program. When used in conjunction with other methods, such as local alerts as postal employees approach the house and written notification cards within the mail, this program has been successful in other locations that have seen high dog bite rates.
A report from the U.S. Postal Service, part of its 2024 National Dog Bite Awareness Campaign, revealed that North Carolina had the eighth-most dog bites on postal service employees in 2023, with 185 — that’s a 27% increase from the previous year.

Overwork, Stress, Depression: Where Do the Healers Go for Help?
Mark your calendar for an important program on mental health and support resources for healthcare providers.
Overwork, Stress, Depression: Where Do the Healers Go for Help?
Thursday, October 10 at 6:15pm
RSVP by October 1 to [email protected] or 919-810-4081
Conflict Management: Must-Have Skill for New Leaders Webinar
Conflict Management: Must-Have Skill for New Leaders
September 19, 2024
Noon-1 p.m.
Being able to manage conflict as a leader is a critical skill for success. When conflict is managed appropriately, it can be an active force that can build healthy relationships within and between teams.
This webinar will help you gain the conflict management skills you need to flourish in this next stage of your career. Make this part of your leader's toolbox so you can use it when conflict arises within your team with others.
Objectives
- Learn about the different sources, causes and cost of Conflict
- Discover the 5 different styles Leaders use to manage Conflict
- Identify the Skills needed to effectively Manage Conflict
- Develop Conflict Management Strategies for “Working it Out”
Learn more and register here.
NCTracks: Upcoming Changes to Service Location Management

Effective August 25, 2024, providers will no longer be able to modify an existing service location address in NCTracks. Instead, a new service location must be created for address changes. The Begin and End date of the new service location must represent the dates services are rendered at that location.
This will not impact the ability to edit Pay-to or Correspondence addresses.
As a result of these upcoming changes, all draft applications in the NCTracks system will be automatically deleted on August 25, 2024. Please submit all applications in the system prior to this date to avoid loss of data.
The Wait is OVER! 2024 NCMS Photo Contest Results Are In!
We continue to be wowed each year by the impressive photo contest submissions. A stunning array of talent was again on display in this year's contest!
Selecting the winners was a challenge, but in the end, the following images came out on top in their respective categories:
Overall Winner
David Tart, MD - Retired dermatologist from Greensboro
“Dramatic Callanish Sunset”

Nature Category Winner
Karl Chiang, MD - Interventional radiologist from Greenville
“Winter Wonderland”

NC Category Winner
Demetri T. Poulis, MD, FACS - General surgeon from Nags Head
“Fishing Fleet, Oregon Inlet”

Travel Category Winner
Joel B. Miller, MD - Retired OB/GYN from Hickory
"Venice Grand Canal"

Wildlife Category Winner
Tony Huggins, MD - Anesthesiologist from Raleigh
“Sisters”

Congratulations and thank you to everyone who submitted!
Below is the complete list of results...
| David Tart, MD | Overall Winner | Dramatic Callanish Sunset |
| Karl Chiang, MD | Category Winner - Nature | Winter Wonderland |
| Demetri T. Poulis MD FACS | Category Winner - North Carolina | Fishing Fleet, Oregon Inlet |
| Joel B Miller, MD | Category Winner - Travel | Venice Grand Canal |
| Tony Huggins, MD | Category Winner - Wildlife | Sisters |
| Jeffrey Coston, DO, FASA | Finalist | Godafoss Waterfall |
| Steven Andrew Dingeldein, MD | Finalist | Atlantic Puffin |
| Rodger David Israel, MD, MHL | Finalist | Bear with the crooked nose |
| Kurt K. Lark, M.D. | Finalist | Foggy Sunrise |
| Pete Leuchtmann, MD | Finalist | Lower Antelope Canyon |
| Arnold Camacho Olegario, MD | Finalist | Dawn |
| Brian J. Sutton, MD | Finalist | Cliffs of Moher |
| Robert Yapundich, MD | Finalist | Curious Coyote |
| Sarah Atkins | Semi-Finalist | Joshua Tree Sunset |
| Charles H Classen Jr, MD | Semi-Finalist | Red Barn |
| Herb Clegg, MD | Semi-Finalist | Roanoke Marshes Lighthouse at dusk |
| Susan Lynne Evans, MD | Semi-Finalist | Madrid Nightlife |
| P. Mark Gallerani, MD | Semi-Finalist | Horned Grebe with ducklings |
| Lisa Gangarosa, MD | Semi-Finalist | Calliope and Clouds |
| John Goldfield, PA-C | Semi-Finalist | Secret Crater |
| Kathryn McConnell Greven, MD | Semi-Finalist | Transcendental |
| Jim Hill, M.Ed., PA-C Emeritus, DFAAPA | Semi-Finalist | Venturing Out |
| Julia Norem MD | Semi-Finalist | Sunset Holden Beach |
| Lourdes Pereda, MD | Semi-Finalist | Floral sunset at the sunflower farm |
| Leighton A. Raynor, MD | Semi-Finalist | Dry Falls |
| Donna Richardson, MD | Semi-Finalist | Bodega Bay, California |
| Nadine B. Skinner, MD, FAAFP | Semi-Finalist | Spring Mountain Sunset |
| Robert M. Varnell, MD | Semi-Finalist | Baby Humpback Whale Playing in the Sun |
| T. Rupert Ainsley, Jr. MD FACP | Honorable Mention | Hummingbird Hawk Moth |
| Yun L. Boylston, MD MBA | Honorable Mention | A Clear Night in Stari Grad |
| Tracy Eskra, MD | Honorable Mention | Dame de Fer |
| Stephen Ezzo, MD | Honorable Mention | I've waited 17 years to take this photo |
| Cynthia M. Gary, MPH, PA-C | Honorable Mention | Black is Beautiful! |
| Steven M. Genkins, M.D. ("Seadoc") | Honorable Mention | "Komodo Dragon Beach Patrol" |
| Jane Girskis, PA-C | Honorable Mention | Spring Has Sprung |
| Lawrence Greenblatt, MD | Honorable Mention | Flying high above Patagonia |
| Richard M. Griffin, MD | Honorable Mention | "Hand Out" |
| H Slade Howell, MD | Honorable Mention | Mountain Stream After a Rain |
| Kurt Lauenstein, MD | Honorable Mention | hummingbird |
| Marion McCrary MD FACP FAMWA | Honorable Mention | Winter is Coming |
| Steven Mendelsohn, MD | Honorable Mention | Morning on the Blue Ridge Parkway |
| David Mertz MD | Honorable Mention | Over Alaska, endless beauty |
| Danna Park MD, FAAP, FACP | Honorable Mention | Azaleas after the rain |
| Vikas Patel, MD | Honorable Mention | Parisian Nightfall: The Glow of Sacré-Cœur |
| Katherine J. Pierce, M.D. | Honorable Mention | Reaching for the Sky |
| James Salisbury MD | Honorable Mention | ‘ALL ENDS WELL’ |
| Michael Wolff, MD | Honorable Mention | Sailing by the Pitons |