
This newsletter outlines key federal regulatory developments and highlights PAI’s advocacy on matters that impact physicians and patients, including:
- Centers for Medicare and Medicaid Services (CMS) Suspends Surprise Billing Independent Dispute Resolution (IDR) Process
- CMS Releases Calendar Year (CY) 2024 Medicare Physician Fee Schedule (MPFS) and Quality Payment Program (QPP) Proposed Rule
- House Committee on Energy and Commerce Holds Hearing on Medicare Access and CHIP Reauthorization Act of 2015 (MACRA)’s Implementation and Remaining Challenges
- Bipartisan Lawmakers Send Letter to CMS on Improving Prior Authorization Processes
- CMS Announces Multi-State Initiative to Strengthen Primary Care
- Center for Medicare & Medicaid Innovation (CMMI) Publishes Strategy to Support High-Quality Primary Care
- Government Accountability Office (GAO) Releases Study on Non-Compete Agreements
- CMS Unwinds Mandatory COVID-19 Vaccination Requirement for Physicians
For information on PAI’s advocacy initiatives, physician payment resources and research, please visit PAI’s website. Healthsperien’s Resource Updates page also has information on key issues in health policy and identifies potential reforms under the Biden Administration, Congress and in the states. Additionally, CMS releases its QPP Small Practices Newsletter, a monthly resource that provides small practices (15 or fewer physicians) with program updates, upcoming QPP milestones and resources to support continued participation and success in the QPP. You can sign up here to receive this monthly resource
Top News & Wins
- CMS suspended the IDR process due to a federal district court ruling in favor of the Texas Medical Association (TMA) to vacate key provisions in CMS’ surprise billing regulations. PAI is pleased with the decision of the court and urges the Departments of Health and Human Services (HHS), Labor and Treasury (collectively, the Departments) to issue additional guidance promptly.
- CMS released its CY 2024 MPFS and QPP Proposed Rule, which is expected to reduce physician reimbursement by 3.36% in 2024. PAI strongly opposes any cuts to physician payments and will submit detailed comments arguing for updates to physician payment that reflect inflationary pressures increasing the cost of providing services.
- The House Committee on Energy and Commerce held an important hearing examining MACRA’s implementation along with the ongoing challenges it poses for physicians and patients.
CMS released the Making Care Primary model, which will provide participants with additional revenue to build infrastructure, make primary care services more accessible and better coordinate care with specialists.
CMS Suspends Surprise Billing IDR Process
On August 3, CMS suspended the IDR process established under the No Surprises Act to reconcile surprise billing payment disputes. CMS based this suspension on a recent ruling that vacated CMS’ December 2022 IDR fee increase and sections from the October 2021 interim final rule on claims batching. The court ruled in favor of TMA, finding that the Administration violated the Administrative Procedures Act with its 600% fee increase and rules on claims batching. CMS noted the Departments have temporarily suspended the federal IDR process, including the ability to initiate new disputes until the Departments can provide additional instructions. CMS has not indicated how long the portal may be suspended.
PAI supports the Court’s ruling, which is the third decision siding with TMA in litigation challenging federal regulations implementing the No Surprises Act. The fee increase from $50 to $350 dramatically curtailed many physicians’ ability to seek arbitration when a health plan offers insufficient payment for out-of-network care. PAI urges CMS to issue additional guidance swiftly to prevent further confusion and harm for physicians.
CMS Releases CY 2024 MPFS and QPP Proposed Rule
On July 13, CMS released (fact sheet here) its CY 2024 MPFS and QPP Proposed Rule. The proposed CY 2024 MPFS conversion factor is $32.75, a decrease of $1.14, or 3.36%, from the CY 2023 conversion factor of $33.89.
As medical inflation continues to add to the costs of providing services, as reflected by the 4.5% Medicare Economic Index, this proposed reduction in physician reimbursement is unsustainable. This misguided payment policy has driven physicians to sell or close their private medical practices to hospitals and other corporate entities like private equity firms. Additionally, small and independent physician practices are continuing to adjust to the wide-reaching and universally detrimental effects of COVID-19. Studies show consolidation diminishes competition and results in higher costs.
PAI strongly opposes any cuts to physician payments as practices cannot continue to absorb the increasing costs of providing services while their payment rates dwindle. A permanent solution is needed to fix this unsustainable payment system and end the need for Congress to “fix” statutory payment cuts each year.
PAI will continue to review key proposals to ensure they support the ability of physicians to sustain their medical practices. PAI will submit detailed comments on this proposal. Healthsperien released a comprehensive summary on this proposed rule which can be found here. Key provisions include:

House Committee on Energy and Commerce Holds Hearing on MACRA’s Implementation and Remaining Challenges
On June 22, the House Energy and Commerce Committee’s Oversight and Investigations Subcommittee held a hearing examining MACRA’s implementation and ongoing challenges it poses for physicians and patients. Chairman Griffith (R-VA) provided opening remarks explaining MACRA has provided many benefits since its enactment in 2015, like eliminating the sustainable growth rate model and transitioning from a fee-for-service system to that of value-based care through MIPS and APMs. The hearing covered concerns about current reporting requirements and quality measures, with members calling requirements bureaucratic and overly burdensome, especially for small and rural practices. Several members raised the issue of inadequate physician reimbursement amidst physician shortages and advocated for legislation implementing an annual inflation-based update.
The hearing featured witness testimony from individuals representing the following organizations:
- Paragon Institute
- National Association of ACOs
- America’s Physician Groups
- Austin Regional Clinic in Texas
- Warren Alpert Foundation Professor of Health Care
- Harvard Medical School Department of Health Care Policy
Healthsperien attended the hearing and full notes are available to view here.
PAI consistently advocates for fair payment policies and rates for all physicians, and strongly opposes the continued budget neutrality rules that force a “zero sum” approach to physician payment. This approach fails to reflect the realities of physician practice expenses and pits certain physician specialties against others. Budget neutrality creates a system of “winners” and “losers” when reimbursement rates under the MPFS are adjusted. It also exacerbates an environment of uncertainty for independent practicing physicians who must respond to reduced reimbursement while maintaining their commitment to providing quality medically necessary care. As evidenced by PAI-Avalere research documenting consolidation trends, these pressures continue to drive physicians away from private practice and into employed arrangements.
Bipartisan Lawmakers Send Letter to CMS on Improving Prior Authorization Processes
On June 21, more than 230 House members and 61 Senators sent a letter to CMS requesting changes to a December 2022 proposed rule that streamlines the prior authorization process for insurers and physicians. The bipartisan group of lawmakers are led by Rep. Susan DelBene (D-WA) and request CMS to promptly finalize the rule and include provisions from DelBene’s Improving Seniors’ Timely Access to Care Act to improve the prior authorization process for Medicare Advantage (MA) plans. The letter asks CMS to establish a mechanism for real-time electronic prior authorization decisions for routinely approved items and services, require that plans respond to prior authorization requests within 24 hours for urgent care, and require detailed transparency metrics.
The letter indicates that both the legislation and CMS’ recent proposals would:
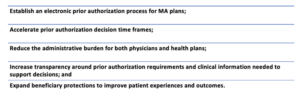
Earlier this year, PAI submitted a comment letter in response to CMS’ 2022 proposed rule with recommendations reflected in this Congressional letter. PAI strongly urged CMS to further enhance the rule’s impact through additional provisions to support adoption by physicians and strengthen the rule’s transparency requirements, including requiring transparency around the specific clinical guidelines used in prior authorization determinations. PAI also recommended additional reporting by payers on metrics that will inform efforts to further streamline and speed prior authorization processes (e.g., through “real time” determinations where appropriate) and protect patients from unnecessary delays in care.
CMS Announces Multi-State Initiative to Strengthen Primary Care
On June 8, CMS announced the Making Care Primary (MCP) Model, which will be tested under CMMI in eight states—Colorado, Massachusetts, Minnesota, New Jersey, New Mexico, New York, North Carolina and Washington. The MCP Model will run for 10 and a half years, from July 1, 2024, to December 31, 2034, and will provide participants with additional revenue to build infrastructure, make primary care services more accessible and better coordinate care with specialists. The primary goals of the MCP are to:

CMS is working with Medicaid Agencies in the participating states to engage in full care transformation across public programs, with plans to engage private payers in the coming months. The model includes a progressive three-track approach based on participants’ experience level with value-based care and APMs. Track One will focus on building infrastructure to support care transformation. In Tracks Two and Three, the model will include certain advance payments and offer more opportunities for bonus payments based on participant performance.
PAI commends CMS for considering the needs of small and rural practices interested in engaging in value-based arrangements (VBAs). Physician participation in VBAs requires considerable administrative support–VBAs are complex and expose physicians and their practices to financial risk and other challenges. PAI developed a comprehensive resource for members on APM financial methodologies, attribution, alignment and benchmark calculation, and other important factors to consider when participating in models, which can be accessed here.
CMMI Publishes Strategy to Support High-Quality Primary Care
On June 9, CMMI released its strategy to support high-quality primary care. The strategy aims to strengthen primary care infrastructure in the United States by creating multiple pathways to support improved financing for advanced primary care, equitable access to high-quality primary care and sustainable transformation among a heterogeneity of practices.
The approach focuses on the following three dimensions:
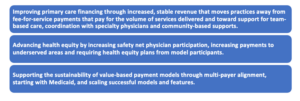
The publication discusses current work addressing these areas, including Making Care Primary, the newest CMMI primary care model. CMMI is also testing a new alignment strategy promoting payer partnership, alignment on key model design features and encouraging payers to innovate for their unique patient population. The strategy also outlines future pathways to addressing the three focus areas. These efforts include exploring ACO-based primary care model tests that may focus on practices in the MSSP and exploring a state-based, total cost-of-care model.
GAO Releases Study on Non-Compete Agreements
On May 11, the GAO released a new report (one-pager) requested by Senators Chris Murphy (D-CT), Todd Young (R-IN), Elizabeth Warren (D-MA), Marco Rubio (R-FL), Ron Wyden (D-OR) and Tim Kaine (D-VA) on non-compete agreements (NCAs). The report found the use of NCAs is widespread throughout the U.S. labor market and serves to protect the interests of businesses while restricting job mobility, lowering wages for workers and discouraging innovation. Fifty-seven percent of health care and social assistance employers surveyed reported requiring new hires to sign agreements that restrict the workers from taking jobs with competing organizations. The reasons health care employers cited for requiring noncompete agreements included: to protect trade secrets, intellectual property and proprietary information; to prevent departing workers from taking clients with them; and to retain trained staff. The Federal Trade Commission proposed rule to ban NCAs is currently pending finalization and is expected to be released early next year.
PAI recognizes that the inclusion of non-compete clauses in contracts can prevent physicians from practicing medicine in their communities when they want to change jobs—limiting patients’ access to their physicians. PAI believes that federal guidance should be kept to a minimum and encourage states to adopt a few core principles for non-competes. PAI believes that non-competes should not be crafted in a way that infringes upon continuity of care.
CMS Unwinds Mandatory COVID-19 Vaccination Requirement for Physicians
On May 31, CMS published a final rule withdrawing COVID-19 vaccination requirements for certain workers at CMS-covered health care facilities. On November 5, 2021, the Biden Administration and CMS issued an interim final rule (IFC) which required Medicare- and Medicaid-certified physicians to be vaccinated against COVID-19. CMS recognizes that vaccines are important for preventing severe illnesses and promoting public health. However, as the incidence of severe COVID-19 has declined significantly since the IFC was issued, CMS will withdraw the health care staff COVID-19 vaccination provisions. CMS still strongly encourages facilities, when the opportunity exists and resources allow, to facilitate the vaccination and education of all individuals who provide services infrequently or frequently.
