CDC Alert: Limited Supply of RSV Drug, Options to Help Infants

The Centers for Disease Control and Prevention (CDC) is issuing a Health Alert Network (HAN) Health Advisory to provide options for clinicians to protect infants from respiratory syncytial virus (RSV) in the context of a limited supply of nirsevimab, a long-acting monoclonal antibody immunization product recommended for preventing RSV-associated lower respiratory tract disease in infants.
Read the full alert here.
Updated Community Health Workers Profile in Occupational Outlook Handbook

The U.S. Department of Labor’s Bureau of Labor Statistics (BLS) Occupational Outlook Handbook has updated the Community Health Workers (CHW) profile. HRSA helped inform the update as part of an interagency initiative to address long-term CHW sustainability through novel, whole-of-government solutions.
The new standalone CHW profile better reflects the core duties, competencies, and training and employment sites. While the profile focuses on CHWs, it also mentions other professions such as peer support specialists, community health representatives, and promotores de salud for the first time. They are included in the CHW Standardized Occupational Classification (SOC) code.
Eliminating Disparities in Perinatal Health Funding Opportunity
Applications are now being accepted for funding under the Healthy Start Initiative: Eliminating Disparities in Perinatal Health (Healthy Start or HS) Program.

The purpose of HS is to improve health outcomes before, during, and after pregnancy and reduce the well-documented racial/ethnic differences in rates of infant death and adverse perinatal outcomes.
HS is intended to support projects in communities and populations experiencing the greatest disparities in maternal and infant health outcomes. HS has two focus areas:
1) providing direct and enabling services (for example, screening and referrals, case management and care coordination, health and parenting education, and linkage to clinical care) to enrolled HS participants; and
2) convening Community Consortia (formerly known as Community Action Networks or “CANs”) comprised of diverse, multi-sector partners to advise and inform HS activities as well as to develop and implement plans to improve perinatal outcomes within the selected project area.
Deadline to apply is December 15,2023.
Learn more and how to apply here.
NCDHHS Issues Respiratory Season Guidance

The NC Department of Health and Human Services has issued a notice to clinicians with updated information and guidance on influenza, COVID-19, and RSV for the 2023-2024 respiratory season. Topics covered include testing, clinical management, prevention and control measures including vaccines, and surveillance and tracking.
The notice from NCDHHS is available here.
Additional updates to the guidance will be available on the NC DHHS Flu Website.
If you have questions, please contact the Communicable Disease Branch epidemiologist on-call number (919-733-3419).
CMS Releases Information on Three National Coverage Determinations

CMS continues its commitment, through national coverage determinations (NCDs), to ensure that people with Medicare have access to emerging treatments and technologies that will improve health outcomes.
October 10: CMS announced that the final NCD on Preexposure Prophylaxis (PrEP) Using Antiretroviral Therapy to Prevent Human Immunodeficiency Virus (HIV) Infection would not be posted by the expected date of October 10. CMS received comments on the proposed NCD that expressed concern over the potentially complex transition of coverage of these preventive drugs from Part D to Part B. CMS will work with Part D plans and pharmacies to facilitate an orderly transition as we work towards finalizing the NCD. A final NCD will be forthcoming. Information on the proposed NCD is found here.
October 11: CMS issued a final NCD for Percutaneous Transluminal Angioplasty (PTA) of the Carotid Artery Concurrent with Stenting. This NCD resulted from a request from the Multispecialty Carotid Alliance (MSCA) for a reconsideration of a former NCD. The procedure restores blood flow when arteries are clogged due to peripheral artery disease. In the final NCD, CMS expanded coverage of PTA of the carotid artery with stenting for a broader population and allowed Medicare Administrative Contractors (MACs) to make reasonable and necessary determinations for any other beneficiary seeking coverage.
October 13: CMS announced a final decision to remove the NCD for Beta Amyloid Positron Emission Tomography (PET) in Dementia and Neurodegenerative Disease, permitting Medicare coverage determinations to be made by the MACs. Removing the NCD also removes the current limitation of one PET beta-amyloid scan per lifetime from the coverage requirements.
NCDHHS Encouraging Mpox Vaccinations After New Cases Reported
NCDHHS Encourages Mpox Vaccination for People at Higher Risk After Recent Cases Reported

In addition to the two cases, the mpox virus was recently detected in one out of 12 wastewater sites where monitoring is being conducted. These cases and wastewater detections were all in different counties, suggesting an increased spread of mpox in North Carolina.
Numbers and cases have been low due to vaccinations and community engagement, but now is the time to get vaccinated if you are at higher risk for mpox and have not yet received the vaccine. Eligibility criteria have expanded to include:
- Anyone who has or may have multiple or anonymous sex partners;
- Anyone whose sex partners are eligible per the criteria above;
- People who know or suspect they have been exposed to mpox in the last 14 days;
- Anyone else who considers themselves to be at risk for mpox through sex or other intimate contact.
Take steps to lower your risk during sex or at social gatherings, like using a condom correctly every time you have sex. Avoid close contact with people who have a rash that looks like mpox, avoid contact with objects and materials a person with mpox has used and wash your hands often.
Read more about how the disease is spread, symptoms of mpox, and what NCDHHS is doing to enhance communication efforts with local health departments and community partners, in a news release.
NCMS Board Member Dr. Jugta Kahai Addresses Children's Mental Health Crisis in Rural NC
“When you come from a strapped rural county where funding is cut every year,” Kahai said, “you have to manage by compromising. It’s a sad reality. Often those kids need the facilities the most, yet they end up deprived.”
Dr. Jugta Kahai

Jugta Kahai, MD, FAAP (image credit: Border Belt Independent)
NCMS Board member Jugta Kahai, MD, FAAP, is the pediatric medical director at Columbus Regional in Whiteville. In a recent article, she addresses children’s mental health in rural North Carolina.
According to the article, nationwide, children are dealing with a mental health crisis that experts say is fueled by bullying, the COVID-19 pandemic, discrimination and other stressors. Unfortunately, placement can be hard to find at a pediatric mental health facility in North Carolina.
Read the full article here.
Join a Side-by-Side Webinar with NCDHHS' Division of MH/DD/SUS

Join staff from NCDHHS' Division of Mental Health, Developmental Disabilities and Substance Use Services (MH/DD/SUS) on October 23 at 2 p.m. to learn more about policies and programs that affect the Mental Health, Intellectual and Developmental Disabilities, Substance Use Services, and Traumatic Brain Injury community.
The goal of these monthly webinars is to bring everyone together in one (virtual) place to share ideas for public policy that will improve the lives of North Carolinians.
Register for the meeting and see a flyer (Spanish) for more information.
Registration Now Open for NCNS 2024 Annual Meeting!
Registration is now open!
The NC Neurological Society's
2024 Annual Meeting
February 23-25 at the Grandover Resort
Greensboro, NC

Enhance Your Neurology Practice!
Accommodations: Secure your accommodations online by using this link, or call (336) 294-1800 and mention NC Neurological Society to receive the discounted group rate of just $239, plus tax and fees.
The hotel cutoff date is February 1. Space is limited, so book today!
We look forward to seeing you in Greensboro!
Registration is Open for NCDA 2024 Annual Meeting
Registration is Now Open!
The NC Dermatology Association
2024 Annual Meeting
January 26-28 at the Grandover Resort
Greensboro, NC
Register today!
Accommodations: Secure your accommodations online by using this link, or call (336) 294-1800 and mention NC Dermatology Association to receive the discounted group rate of just $239, plus tax and fees. The hotel cutoff date is January 4. Space is limited, so book today!
We look forward to seeing you in Greensboro!
Foundation Friday! Thank You to These NCMS Foundation Donors.

Today, the NCMS Foundation recognizes some of our Member donors who have joined us on the journey to help make health and well-being attainable for all North Carolinians. These individuals are contributing to make sure clinicians are where they are needed most and that clinician leaders are lighting the way.
Frank H. Moretz, MD * Life Member
Domenic A. Palagruto, II, DO
Lawrence H. Greenblatt, MD, FACP
Venkat L. Prasad, MD, MBA, MHA * First-Time Foundation Donor
Ashok Jain, MD, MBA, FAAP
Thank you for your continued support to help North Carolinians lead healthier lives.
Learn more about how YOU can make a difference too here.
Wake Forest School of Medicine Receives Grant to Study Clinician Shortages in Rural Areas

There are many factors that contribute to poorer health outcomes for rural Americans compared to those who live in urban areas, according to the Centers for Disease Control and Prevention. One reason is a lack of physicians, physician assistants, and nurse practitioners in rural areas, which leads to limited access to convenient health care for rural residents.
To better understand why clinicians choose to practice in specific areas, Wake Forest University School of Medicine has received a two-year, $445,000 grant from the National Institute on Minority Health and Health Disparities, part of the National Institutes of Health.
Using a preference method called a discrete choice experiment, the researchers will gain a better understanding of the specific reasons medical residents and fellows, along with physician assistants and nurse practitioner students, choose a particular clinical position. The study team will look specifically at the rural Appalachia region of the United States.
“Despite job availability in rural areas, many clinicians choose to work in more affluent suburban or urban areas,” said Chris Gillette, Ph.D., associate professor of PA Studies at Wake Forest University School of Medicine and principal investigator of the study. “We want to better understand the complex interplay of personal reasons, job-related needs or community preferences that influence the decision-making process.”
The findings of this study will help identify a set of policy options and incentives that would attract more clinicians to rural areas of the country.
“To design effective policies and incentives that will attract clinicians to rural areas, it is critical to develop a better understanding of their preferences for decision-relevant characteristics, as well as the trade-offs they are willing to make when choosing a job location,” Gillette said.
Gillette and Jan Ostermann from the University of South Carolina Arnold School of Public Health will lead this project in collaboration with offices of rural health from Marshall University Joan C. Edwards School of Medicine, West Virginia University School of Medicine, Ohio University Heritage College of Osteopathic Medicine, and the University of Kentucky School of Medicine. [source]
NC Universities Setting New Revenue Records From Research, Tech Created by Students and Faculty
Duke University brings in record money from its startups and technology

(Axios Raleigh - Zachery Eanes) -- The Triangle's research universities are setting new revenue records from research and technology created by their students and faculty.
Driving the news: Duke University reported bringing in a massive $102.5 million in licensing and equity payments from technology and startups formed on its campus in its fiscal year 2023, which ended June 30.
- It caps an incredibly consistent run by the university, which has brought in more than $50 million via technology created on the campus for the past five years.
Why it matters: The Triangle university ecosystem — the origin of the Research Triangle moniker — has long been the economic backbone of the region, reliably attracting talent, jobs, and money to the region.
- The startups formed by their faculty and students have gone on to become some of its largest employers, including names like Quintiles, now known as IQVIA (UNC); SAS Institute and Wolfspeed (N.C. State); Precision Biosciences (Duke) and RTI International (all three universities).
State of play: The universities have, over the past decade, become much more focused on turning the intellectual property formed on their campuses into financial windfalls.
- In addition to Duke's success, UNC broke its licensing and equity record in 2021 (thanks to Bayer's $4 billion acquisition of Chapel Hill-founded gene therapy company AskBio).
- And since 2015, N.C. State has formed the most startups of any school in the area.
What's happening: Duke can attribute its success to a hot streak of drugs entering the market as well as startups filing for initial public offerings or being acquired, according to Robin Rasor, the school's associate vice president of translation and commercialization.
- In its past fiscal year, five Duke-related startups were acquired, including Durham-based Isolere Bio and InnAVasc Medical.
- The school has also seen six different IPOs in the past five years, which has provided a reliable stream of equity payments.
- Duke Capital Partners, the university's early-stage investment firm, has also become more active in supporting young startups with capital, including investing $10.8 million into 12 startups in fiscal year 2023.
What they're saying: Rasor, who has worked at universities for three decades, said there's been a big shift within schools in recent years.
- Younger faculty are more interested in forming companies, she said, and universities are providing more infrastructure for them to do so.
- "Most of the [faculty] recruits coming in are already innovators ... and they're very interested in what the [startup] environment is going to be like," Rasor told Axios. "That's a big change, and … it's important to have that kind of environment so we can recruit the best and the brightest."
What we're watching: Of the 15 startups formed at Duke in the past year, 66% are headquartered in North Carolina.
- That's a decline from previous years, according to Rasor, who said remote work trends may be leading to more of the university's startups to relocate — even as more Duke students seem to be staying in the area after graduation.
- She said the Triangle's critical mass of talent continues to improve but many startups still weigh whether Boston or the Bay Area might be a better fit.
Register Here for Addiction Medicine Learning Series Webinars
Starting January 2023, all DEA-registered practitioners are required to participate in 8 hours of training in addiction medicine. This Addiction Medicine Series meets the requirements set forth by the DEA and provides participants a broad overview on addiction treatment. This series provides education on a variety of key topics in addiction medicine, including inequities in addiction, impacts of stigma, basics about addiction treatment, integrating addiction treatment in the primary care setting, and treatment of substance use in special populations including the adolescent population, those with mental illness and those with chronic pain.
The registration links for all 8 models are included below:
The End of a Bygone Era: Removal of the X-waiver Next Steps in Buprenorphine Prescribing
Addiction In Primary Care
Responding to Pediatric Substance Use
Treating Chronic Pain and Addictions
Understanding the Impacts of Stigma: Substance Use Disorder
Addiction and Mental Illness
The Impact of Stigma and Bias on Substance Use Disorder Diagnosis and Treatment
Current State of MOUD Access
Additional Resources Related to These Topics
Congratulations to our NCMS LEAD Poster Session Winners!

Clinical Research – Resident
1st place – Jane D. Dewire (ECU) - Impact of child abuse on pediatric patients evaluated in the Emergency Department for psychiatric conditions
Clinical Vignette – Resident
1st place – Bhumi Patak (Novant Health New Hanover Regional Medical Center) - An Unexplained Sudden Cardiac Arrest in Young Adult
Clinical Research – Student
1st place - Avery Wright (WFU) - The Impact of Socioeconomic Status on Pediatric Facial Trauma
1st place - Kyungmin Yoo (WFU) - Age-Related Comparisons on Alzheimer's Disease Manifestations in Ocular Tissue From a Non-Human Primate Model
3rd place – Amritha Jacob (Campbell University) - Discharge Readability: Comparing Reading Levels of Patients and Caregivers of UNCH-Southeastern with the Printed EHR Discharge Instructions
Clinical Vignette – Student
1st place - Andrew Cummingham (ECU) - Pembrolizumab Induced Tumor Shrinkage in Rare Osseous Metastasis of Basal Cell Carcinoma
2nd place – Simran Ohri (UNC) - Retinopathy in a Patient With Influenza Associated Pancytopenia
3rd place – Ayarah Dharanikota (Campbell University) - Intracranial Subdural Empyema Secondary to Streptococcus Bacteremia
Thank you to everyone who participated in this year's Poster Session!
CMS Accepting 2023 MIPS Extreme and Uncontrollable Circumstances Exception and MIPS Promoting Interoperability Performance Category Hardship Exception Applications
The Merit-based Incentive Payment System (MIPS) Extreme and Uncontrollable Circumstances (EUC) Exception and MIPS Promoting Interoperability Performance Category Hardship Exception applications are available for the 2023 performance year. Applications can be submitted until 8 p.m. ET on January 2, 2024.
MIPS Extreme and Uncontrollable Circumstances Exception Application
MIPS eligible clinicians, groups, and virtual groups may apply to reweight any or all MIPS performance categories if they’ve been affected by extreme and uncontrollable circumstances. Extreme and uncontrollable circumstances are defined as rare events entirely outside of your control and the control of the facility in which you practice. These circumstances must:
- Cause you to be unable to collect information necessary to submit for a MIPS performance category;
- Cause you to be unable to submit information that would be used to score a MIPS performance category for an extended period of time (for example, if you were unable to collect data for the quality performance category for 3 months); and/or
- Impact your normal process, affecting your performance on cost measures and other administrative claims measures.
For Alternative Payment Model (APM) Entities
APM Entities participating in MIPS APMs can also submit a MIPS EUC Exception application. However, the policy for APM Entities differs from the MIPS EUC policy for individuals, groups, and virtual groups in that:
- APM Entities are required to request reweighting for all performance categories;
- At least 75% of an APM Entity’s MIPS eligible clinicians must qualify for reweighting in the Promoting Interoperability performance category; and
- Data submission for an APM Entity won’t override performance category reweighting.
Learn more in the 2023 MIPS Extreme and Uncontrollable Circumstances Application Guide (PDF, 1MB).
MIPS Promoting Interoperability Performance Category Hardship Exception Applications
MIPS eligible clinicians, groups, and virtual groups may apply to reweight the Promoting Interoperability performance category to 0% if they:
- Have decertified electronic health record (EHR) technology;
- Have insufficient Internet connectivity;
- Face extreme and uncontrollable circumstances such as disaster, practice closure, severe financial distress, or vendor issues; or
- Lack control over the availability of certified EHR technology (CEHRT); simply lacking the required CEHRT doesn’t qualify you for reweighting.
NOTE: You don’t need to apply for this application if you qualify for automatic reweighting of the Promoting Interoperability performance category based on your clinician type or special status.
As a reminder, small practices qualify for automatic reweighting. Refer to Appendix A of the 2023 MIPS Promoting Interoperability User Guide (PDF, 1MB) for a complete list of clinician types and special statuses that qualify for automatic reweighting in the 2023 performance year. Learn more in the 2023 Promoting Interoperability Hardship Application Guide.
How do I Apply?
You must have a Health Care Quality Information Systems (HCQIS) Access Roles and Profile (HARP) account to complete and submit an exception application on behalf of yourself, or another MIPS eligible clinician, group, virtual group or APM Entity. For more information on HARP accounts, please refer to the Register for a HARP Account document in the QPP Access User Guide (ZIP, 4MB).
Once you register for a HARP account, sign in to the QPP website, select ‘Exceptions Applications’ on the left-hand navigation, select ‘Add New Exception,’ and select ‘Extreme and Uncontrollable Circumstances Exception’ or ‘Promoting Interoperability Hardship Exception.'
Note for Subgroups
Subgroups will inherit any reweighting approved for their affiliated group; if the subgroup encounters an extreme and uncontrollable circumstance that doesn’t affect the entire group, the subgroup can contact the QPP Service Center to request reweighting.
How do I Know if I’m Approved?
You'll be notified by email if your request was approved or denied. You can also check the status of your application by signing in to the QPP website and navigating to ‘Exceptions.’ If approved, this information will also be added to your eligibility profile in the QPP Participation Status Tool on a weekly basis. If your application is approved at the end of the performance year, it may not appear in the QPP Participation Status Tool until the submission window opens on January 2, 2024.
Celebrate the Impact of Community Health Workers at the 2023 NC Community Health Worker Summit
North Carolina Area Health Education Centers (NC AHEC) is thrilled to announce the 3rd Annual
NC Community Health Worker Summit:
CHWs Activators of Legacy

This two-day event will bring together Community Health Workers, healthcare professionals, policymakers, and stakeholders to explore critical topics in the field of community health. This summit serves as a platform to share knowledge, exchange ideas, and strengthen the role of Community Health Workers (CHWs) in improving the health and well-being of North Carolina's diverse communities.
Celebrate the dedication and impact of Community Health Workers in North Carolina and work together to build healthier, more resilient communities.
T-Shirts
NC AHEC will be pre-ordering t-shirts for $20, please select your size to make sure you receive one the day of the summit. Extra will be ordered but limited availability the day of the event for $25.

The Details
Date & Time:
Thursday, November 30, 2023; 2:00 p.m. to 5:00 p.m.
Friday, December 1, 2023; 9:00 a.m. to 5:00 p.m.
Location:
The Conference Center at GTCC, 7908 Leabourne Road, Colfax, NC
Registration Fee:
Pre-Summit Learning Labs $25; Summit Registration for CHWs $40; Summit Registration Allies $50; Virtual Summit $30
Hotel Accommodations:
La Quinta Inns & Suites by Wyndham Greensboro Airport High Point, 7905 Triad Center Dr, Greensboro, NC 27409 (7 mins from the Summit venue) Phone: (336) 840-1550
Credits Offered: Up to 8 contact hours available.
NCDHHS Encourages Mpox Vaccination for Those at Higher Risk
Raleigh — Two cases of mpox were reported to the North Carolina Department of Health and Human Services over the past six weeks, the first cases in North Carolina residents since April 2023. In addition to the two cases, mpox virus was recently detected in one out of 12 wastewater sites where monitoring is being conducted. These cases and wastewater detections were all in different counties, suggesting increased spread of mpox in North Carolina.
"If you are at higher risk for mpox and haven’t yet gotten the vaccine, now is a good time to do so," said Dr. Zack Moore, State Epidemiologist. "Numbers of cases have been low recently thanks to vaccinations and engagement of partners in the LGBTQ+ community, but this is a reminder that mpox is still with us."
NCDHHS is working closely with local health departments and community partners to provide education about mpox, encourage testing and improve vaccine access and uptake for individuals at higher risk. These efforts to enhance communication, education and outreach include the Mpox Equity Report, the Mpox Communications Toolkit and the Take Pride Now campaign.
Mpox typically begins with flu-like symptoms including fever, chills, headache, muscle aches, swollen lymph nodes and exhaustion followed a few days later by a rash that may be located on hands, feet, chest, face or mouth or near the genitals or perianal area. In some recent cases, the rash has appeared before or at the same time as the flu-like symptoms. Mpox can be spread from the time symptoms start until all sores have healed and a fresh layer of skin has formed — this can take several weeks. Symptoms can be more severe for people who are immunocompromised, such as in individuals living with HIV.
The disease is spread person to person through direct skin-to-skin contact, having contact with an infectious rash, through body fluids or through respiratory secretions. Such contact often occurs during prolonged, face-to-face contact or during intimate physical contact, such as kissing, cuddling or sex. While anyone can get mpox, in the current outbreak, most cases have been in men who have sex with men and more than half of the cases in North Carolina have been in people living with HIV.
If you think you have mpox or have had close personal contact with someone who has mpox, visit a health care provider or contact your local health department to help you decide if you need to be tested for mpox. You should also talk with your doctor about getting tested for other sexually transmitted infections including HIV and syphilis, both of which are on the rise in North Carolina. Learn more information about mpox testing and STD testing online.
NCDHHS and the Centers for Disease Control and Prevention recommend five steps to prevent mpox infection:
- Get vaccinated. Vaccines, including the JYNNEOS vaccine, are free and available, regardless of immigration status. Vaccination can protect against mpox infection or reduce disease severity if infection does occur. NCDHHS recommends vaccination for —
- Anyone who has or may have multiple or anonymous sex partners; or
- Anyone whose sex partners are eligible per the criteria above; or
- People who know or suspect they have been exposed to mpox in the last 14 days; or
- Anyone else who considers themselves to be at risk for mpox through sex or other intimate contact.
- Use the mpox vaccine locator to find nearby healthcare locations in your area that provide mpox vaccinations.
- Take steps to lower your risk during sex or at social gatherings, like using a condom correctly every time you have sex.
- Avoid close contact with people who have a rash that looks like mpox.
- Avoid contact with objects and materials a person with mpox has used.
- Wash your hands often.
Information about mpox cases and vaccinations in North Carolina is updated monthly and displayed on NCDHHS’ mpox website.
Versión en español aquí
Duke's first Nobel Prize Winner, Robert Lefkowitz, Celebrates 50 Years!
Nobel Laureates Highlight Symposium Celebrating Robert J. Lefkowitz’s 50 Years at Duke
(Durham, Duke Med School - Dave Hart) -- After completing a residency and fellowship at Harvard and Massachusetts General Hospital, Robert J. Lefkowitz, MD, arrived at Duke University School of Medicine to begin his first faculty job in the summer of 1973. 
He’s been here ever since — conducting pioneering research that has changed the landscape of medicine, mentoring more than 200 trainees, and becoming Duke University’s first Nobel Prize winner, when he was awarded the 2012 prize in chemistry.
On Oct. 2-3, the School of Medicine hosted a remarkable gathering of luminaries (including seven Nobel Laureates, two former chancellors, and a five-time NCAA championship men’s basketball coach) for a symposium to celebrate Lefkowitz’s 50 years at Duke and the discoveries that advance human health.
Duke University Executive Vice President for Health Affairs and School of Medicine Dean Mary E. Klotman, MD, welcomed the large audience in Page Auditorium. She noted that Lefkowitz’s rise as a pioneering biomedical scientist and Duke’s rise as a world-class biomedical institution went hand in hand. Duke provided Lefkowitz with the resources, intellectual freedom, and trainees and colleagues to pursue his groundbreaking research. In turn, his excellence, mentorship, and championing of basic science have attracted other top scientists and elevated Duke’s research environment.

“Duke wouldn’t be the same if not for Bob, and Bob wouldn’t be the same if not for Duke,” she told the large audience. “We are here to celebrate the golden anniversary of a remarkable relationship.”
The event featured lectures by some of the world’s leading researchers, reminiscences from some of Lefkowitz’s closest friends and colleagues, and words of wisdom for students, trainees, and junior faculty about how to achieve and sustain success, in science and in life.
Participants included Nobel Prize Laureates Peter Agre, MD; Michael S. Brown, MD; Joseph Goldstein, MD; Roderick MacKinnon, MD; Stanley Prusiner, MD; Harold E. Varmus, MD; and Brian Kobilka, MD, who was a postdoctoral fellow in Lefkowitz’s lab and shared the 2012 Nobel Prize.
Also taking the stage were leading scientists including Helen H. Hobbs, MD; Gary H. Gibbons, MD; Irving L. Weissman, MD; and Stuart H. Orkin, MD, as well as a host of Duke leaders past and present. Lefkowitz and Klotman joined Duke University President Vincent E. Price, PhD, and former Duke men’s basketball coach Mike Krzyzewski for a lively panel discussion on “Sustaining Success in the Spotlight.”
Chancellor Emeritus for Health Affairs Victor J. Dzau, MD, recalled “how exciting it was to be here as chancellor and bathe in his glory” when Lefkowitz won the 2012 Nobel Prize for his pioneering research on G-protein coupled receptors, which provided the targets for more than one-third of all current prescription drugs.
“For fifty years Bob has been an icon, a role model, and a scientist whose contributions have changed and saved so many lives,” said Dzau, now president of the National Academies of Sciences, Engineering, and Medicine.
Agre, who won the 2003 Nobel Prize in Chemistry and was vice chancellor for science and technology at Duke from 2005-2008, presented his recent research on malaria in sub-Saharan Africa. He also recalled the moment that all Nobel Laureates remember: that life-changing phone call from Sweden. “It’s a very pleasant experience,” he admitted.
Goldstein, who won the 1985 Nobel Prize in Physiology or Medicine, first met Lefkowitz in 1968 when they were in the same cohort of “Yellow Berets” — young physicians commissioned into the National Institutes of Health and the Public Health Service during the Vietnam War. He urged young researchers to approach science with a sense of adventure.
“Have the courage to take risks,” he said. “Try new approaches and avoid bandwagon research. If scientists don’t take risks, science will stagnate.”
Varmus, who won the Nobel Prize in Physiology or Medicine in 1989, was a medical school classmate of Lefkowitz’s at Columbia and also a fellow Yellow Beret.
“The scientific life has changed in many ways, but discovery remains a joy,” Varmus said. “The path to a career is longer and harder, but there are more branches to choose from. The demography of science has become more diverse, but we still have a long way to go. Basic and applied science have moved closer together, but the demand for application threatens broad inquiry. One thing remains the same: friendships are essential for a fulfilling life in science.”
One of Lefkowitz’s closest friends, Duke Chancellor Emeritus for Health Affairs Ralph Snyderman, MD, joined the faculty in 1972, just before Lefkowitz did. The two soon took up the habit of running together — an activity they continued, five or six days a week, for some 30 years.
“We once calculated that we ran over 50,000 miles together,” Snyderman said. “We were like brothers without the sibling rivalry. What I think differentiates Bob as a scientist is the courage to do the really hard experiments and the persistence to stick with it. He has incredibly high standards. He’s totally focused, and he is totally committed to the people who work with him.”
Lefkowitz himself spoke passionately about the need for young scientists to find the right mentor. For many of them over the past 50 years, that mentor has been Lefkowitz: many of his trainees have achieved great prominence and won major awards, including the Nobel Prize. He succeeds, he said, when they succeed.
“I’ve never led anything bigger than my lab,” he said. “But I’ve tried very hard to help my trainees use their powers to maximum effect. Training in science is an apprenticeship. It’s experiential. It requires you to pour yourself completely into your goal.”
Lefkowitz, who turned 80 in April, was moved by the large contingent of alumni from his lab who returned to Duke to reconnect and share in the celebration.
“What an incredible few days we just shared,” he said. “I want to thank everybody who took the time to join in, and especially those who came from long distances to help me celebrate these two very special landmarks in my life. Never have the words been truer than when I say, ‘I couldn't have done it without you.’”
Duke School of Medicine Makes Surprise Discovery That Could Change MS Treatments
Surprise Discovery Reveals Key Factor in Multiple Sclerosis

(Duke Med School - Shantell M. Kirkendoll) -- Researchers at Duke University School of Medicine studying multiple sclerosis made an unexpected discovery that could reshape the understanding of MS treatments.
They identified a protein that boosts the aggressive migration of immune cells into the central nervous system which leads to MS, an autoimmune disease affecting about 1 million adults in the United States. The intrusion of a specific type of immune cell called Th17 is particularly harmful to the brain and spinal cord.
But when Duke scientists blocked the protein integrin α3, slowing Th17 cells from reaching and damaging the central nervous system, they saw major improvement in mice, according to a study published Oct. 13 in Science Immunology.
“We were studying the role of another gene when we stumbled upon integrin α3,” said co-lead author Maria Ciofani, PhD, associate professor in the Department of Integrative Immunobiology at Duke School of Medicine. “We found that when it’s missing, the Th17 cells don’t develop as effectively, and more importantly, they face difficulties entering the central nervous system. This means less damage.”
The Th17 cells, which are vital for the body to fight fungal and bacterial infections, don’t usually cause diseases. But for people with MS, these cells are mistakenly activated and end up attacking the central nervous system.
The Duke team is the first to reveal the selective abundance of integrin α3 on Th17 cells. The protein helps Th17 cells to form connections with other cells, which in turn helps the cells grow and become more aggressive.
But in the absence of the protein, Th17 cells get locked outside the blood-brain barrier, the brain’s protective shield.
While probing inflammatory T cells and disabling a particular gene—a routine practice to grasp its function—researchers stumbled upon a surprise. The altered mice were fully shielded from the MS-like symptoms typically seen in such models.
“They were walking around like nothing happened,” Ciofani said. “When we looked carefully, we found that none of the Th17 cells were entering the central nervous system. It was an opportunity to look at the machinery that controls these cells.”
With the help of computational approaches, Ciofani's team, including co-lead study author Eunchong Park, PhD, identified integrin α3. Park, a scientist at AstraZeneca, is a former graduate student in the Department of Integrative Immunology and member of the Center for Advanced Genomic Technologies.
There’s currently no MS drug that targets integrins on Th17 cells, but the drug natalizumab does target another kind of T cell, Th1 cells, that can also contribute to MS. But natalizumab has its side effects, emphasizing the need for alternative treatments.
“One concern about targeting integrin α3 is that these Th17 cells are vital for our body’s defense against infections,” Ciofani said. “We’ve done preliminary tests to see if inhibiting integrin α3 stops Th17 cells from performing their protective roles, and so far, it seems they can still do their jobs.”
Since integrin α3 is so essential for the harmful actions of Th17 cells, it could be a potential target for new MS treatments.
If scientists could develop a drug that blocks or reduces the function of this protein, it might reduce the severity of MS or prevent its onset.
Additional Duke authors include William E. Barclay; Alejandro Barrera; Tzu-Chieh Liao, Harmony R. Salzler; Timothy E. Reddy; and Mari L. Shinohara.
Funding was provided by National Institute of Health grants R01-GM115474; R01-AI156186; R01-NS120417; RG-4536B2/1; and UM1-HG009428 and a Kwanjeong Educational Foundation Scholarship.
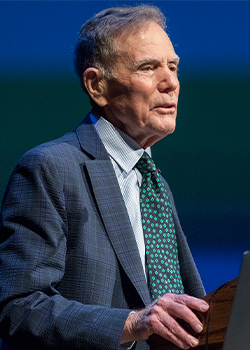
2023 LEAD Recap: State Health Director Gives Annual Report to NCMS
 The 2023 LEAD Conference featured several panels and speakers over two days and a highlight was the annual report from the Department of Health and Human Services. On Saturday, Elizabeth Cuervo Tilson, MD, MPH, State Health Director and Chief Medical Officer offered the annual report to the NCMS. Here are some highlights of her report:
The 2023 LEAD Conference featured several panels and speakers over two days and a highlight was the annual report from the Department of Health and Human Services. On Saturday, Elizabeth Cuervo Tilson, MD, MPH, State Health Director and Chief Medical Officer offered the annual report to the NCMS. Here are some highlights of her report:
EXECUTIVE SUMMARY
As the world continues to recover from one of the largest public health threats in recent history, this past year in North Carolina heralded a transition from COVID-19-specific recovery efforts to broader initiatives aimed at safeguarding and bolstering the overall health of North Carolinians. We leveraged the invaluable lessons learned and the partnerships fortified throughout the pandemic to continue to improve our responses to health challenges. Systems that have been chronically underfunded were further strained by the stressors of the pandemic, mandating thoughtful strategic investment in those systems. We have prioritized activities to advance whole person health and created roadmaps for strategic investment in the health of our people. This annual report outlines our national, state level, and agency strategic priorities and programming to further our commitment to health and opportunity for every North Carolinian.
America’s Health Rankings serves as an annual report for states built upon the World Health Organization’s definition of health. North Carolina’s overall health ranking relative to other U.S. states has consistently improved annually, evidencing our public health successes. In the 2022 Annual Report, North Carolina was ranked 30, up from 34 and 41 in the prior two years, respectively. As in years past, many health indicators on which North Carolina needs to improve are driven in part by North Carolina’s large uninsured population.
Medicaid expansion was signed into law by Governor Roy Cooper in March 2023 and represents a critical step forward to improve the health of North Carolinians and enable a substantial economic investment in the state. Operationalization of Medicaid expansion will be an integral step to improve health in North Carolina. The North Carolina Department of Health and Human Services was given final authority to implement Medicaid expansion through enactment of the state budget in early October, allowing for a launch date of December 1, 2023. We have a new website, bilingual toolkit and a sign-up form to stay updated on the most current information and share with your partners, patients, and stakeholders.
Healthy North Carolina 2030, released in 2020, lays out 21 ambitious, population-level goals and shared objectives for the entire state to solve “wicked problems” and improve the health of North Carolinians for this decade. It aims to mobilize and coordinate a broad array of private sector, public sector, and community organizations that can play a role in making North Carolinians healthier. The North Carolina State Health Improvement Plan (NC SHIP) builds upon HNC 2030 to help create a unified strategy across multiple stakeholders to drive improvement in the indicators throughout the decade covered by HNC 2030. The NC SHIP documents are iterative, describe the process for improvement, and report on progress of any improvements. 2023 NCSHIP lays out the efforts of statewide cross-sector collaboration and launches a Year of Action.
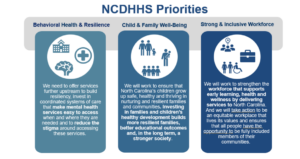
NCDHHS works toward five strategic priorities, guided by our strategic plan. Three priorities are areas of activity that bring together multiple divisions and external partners. They are Behavioral Health and Resilience, Child and Family Well-being, and a Strong and Inclusive Workforce. Two priorities are fundamental ways that we approach our work across the department. Our Health Equity Portfolio synthesizes and guides efforts across NCDHHS and beyond to erase gaps in whole-person health. Our Data Office works the numbers to tell us how we are doing.
As we move out of the COVID pandemic, we have the tools needed to manage COVID-19 like we do other respiratory illnesses, including access to vaccines, testing, and treatment. In addition, we have expanded our focus to other respiratory diseases including Influenza and Respiratory Syncytial Virus and communicable diseases, including Mpox, syphilis and HIV for which there are disparities in rates of infections within our population
Our Public Health Infrastructure has been chronically underfunded and the COVID-19 pandemic brought mainstream attention to public health across the globe and highlighted the challenges of this underfunded patchwork of public health infrastructure to respond to the crisis. These challenges and recommendations to response have been identified by the North Carolina Institute of Medicine's Task Force on the Future of Local Public Health in NC. This report highlights work to strengthen public health foundational capabilities, infrastructure, and workforce to be able to respond to future threats more readily. Finally, this report also serves as the Annual Report on the North Carolina Division of Public Health Strategic Plan as required by Public Health Accreditation Board, and highlights work being done to meet DPH Strategic Priorities.
The full report is available here.
Join NCMS for 2024 National Advocacy Conference in Washington

October 16, 2023
Join us on Capitol Hill
The AMA’s National Advocacy Conference is scheduled for February 12-14, 2024. This yearly event offers an opportunity for personal involvement in the health policy debate on Capitol Hill. We need increased NCMS member engagement with our members of Congress, so mark your calendar and stay tuned for forthcoming details.

2024 National Advocacy Conference
Save the date and join us for our return to Capitol Hill.
February 12-14, 2024
Grand Hyatt / Washington, DC
Plan now to join your colleagues as we advocate for
patients and the medical profession on . . .
Prior Authorization Relief
Medicare Payment Reform
Step Therapy Reform
Workforce Shortage Solutions
Physician Wellness
Registration and additional information coming soon.
https://www.ama-assn.org/about/events/national-advocacy-conference
Welcome NCMS President Dr. Eileen Raynor!

At the NCMS annual meeting held over the weekend, Eileen Raynor, MD, FACS, FAAP, was inaugurated as president of the North Carolina Medical Society.
Dr. Eileen Raynor currently works as an Associate Professor of Surgery and an Associate Professor in Pediatrics in the Department of Surgery, Division of Head and Neck Surgery & Communication Sciences within the Duke University Health System. She has been an active member of the NCMS for a number of years, serving on the NCMS Legislative Cabinet, the Medical Education Committee and the Membership and Communications Advisory Committee. She is an alumna of the KIPL Leadership College Class of 2012 and also served as President of the North Carolina Otolaryngology Society.
Dr. Raynor shares, “I would like to positively impact the quality of life for North Carolina citizens and its physicians through advocacy and collaboration. As a member of the NCMS Board, we will be able to shape the future of health care for all of North Carolina.”
Honoring Dedication: Thank You NCMS Past President Dr. Arthur "Art" Apolinario

On Saturday night, the NCMS celebrated Dr. Arthur Apolinario's commitment and dedication to the North Carolina Medical Society and presented him with the presidential pin.
During his tenure, we witnessed Dr. Art's unwavering commitment to medicine and the medical profession. His contributions will have a lasting impact on the Society.
The NCMS extends our deepest appreciation for an exceptional year of service!
Flashback to #NCMSLEAD22
In Memoriam: Dr. Frank Walter Leak, Sr.
Compassionate physician. Champion of access to care. A special person.
Longtime NCMS member Dr. Frank Walter Leak, Sr., died Wednesday, October 4th. He was 89.
Leak graduated from UNC Medical School in 1967. He completed his residency at Charlotte Memorial Hospital and was awarded the Mead Johnson Award for Family Medicine Residents. He practiced family medicine in Clinton, NC, from 1969-1997 and was one of the founders of the Clinton Medical Clinic. He served as the president of the Sampson County Medical Society and the NC Academy of Family Practice.
Leak received many accolades as a physician, including the NC Academy of Family Practice Physician of the Year (1983) and the National Rural Health Association Physician of the Year (1990).
In 1998, Leak retired from clinical practice, moved to Raleigh, and accepted a position with NC Medical Society in conjunction with the Kate B. Reynolds Foundation Community Practitioner program. Throughout his career, he was dedicated to bringing family physicians to rural areas of North Carolina.
"As a newer NCMS staff member, I remember asking him tons of questions about the health care system and not being able to figure out why, at times, folks just couldn’t get along and do the right thing for patients," says Pam Highsmith, NCMS Vice President, Advancement. "His wise response was, 'Pam, it’s about the almighty dollar! Follow who's keeping the money and who's losing it, and you’ll usually find your answer'. That advice has proven true many times!"
Read Dr. Leak's full obituary here.
Join Us in Greenville for the NCMS Fall Social!
Enjoy the weather with the
NCMS Fall Social!
November 2, 5:30-8:30pm
120 W 5th St, Greenville, NC 27858
NCMS is happy to treat you (and your fellow physicians and PAs) to food and drinks at 5th Street Hardware, Greenville, NC!
This mixer is a fun way for you to learn how NCMS is making your life easier.
Bring your family and friends!
RSVP HERE
or scan this QR code to sign up:

We hope to see you on November 2nd! Questions? Please contact Toni Hill.
Not an NCMS member yet? Now's the time to join!
Learn more here and sign up today!
Sponsored by the NCMS Retirement Plan - Curi Capital, Empower, Pentegra.

2023 LEAD Conference and Gala is Another Success!

RALEIGH -- The 2023 LEAD Healthcare Conference and Golden Stethoscope Awards Gala has concluded! Over the course of two days, attendees, including members of the North Carolina Medical Society, guests, speakers, and exhibitors, gathered at the Sheraton Imperial Hotel in RTP for engaging discussions, camaraderie, and educational sessions. The agenda encompassed a range of vital subjects, such as women's reproductive health and Black maternal well-being, trending topics for young physicians and physician assistants, clinician well-being, and the latest developments in the healthcare field.
On Friday morning, the event commenced with a keynote address from Dr. Amy Bryant, who delved into the topic of women's reproductive health. This was followed by the screening of the Aftershock video and a panel discussion centered on Black maternal health, skillfully moderated by Dr. Karen L. Smith. Joining her on stage were Belinda Pettiford, MPH, and Maria Small, MD, MPH, contributing to the insightful dialogue.
Throughout the day, attendees had the opportunity to engage in networking sessions with peers and gain valuable insights from a diverse array of exhibitors who offered comprehensive support to meet the needs of physicians. The exhibitors included financial advisors, workforce support providers, technology consultants, and a myriad of experts prepared to address the challenges and opportunities within the future of healthcare in North Carolina.
On the first day, there was a panel discussion titled 'Voice of the Young Physician and Physician Assistant,' skillfully moderated by Shawn Scott from NCMS. The panel featured Hans Arora, MD, Jasmine Hemmings, PA-C, Joshua Penninger, PA-C, and Sherry Wang, MD, offering valuable insights. Additionally, attendees enjoyed a lunch session and a Sponsor Showcase discussion on Asthma Care presented by Sanofi-Regeneron. There was also an informative advocacy class led by Seth Palmer, along with the annual CPP Meeting. Throughout the day, the NCMS Board of Directors, Board of Trustees, CCH, and CCHN conducted extensive meetings, culminating in the announcement of new board members on Saturday.
Friday afternoon was brimming with enlightening MedTalks featuring Leadership College Scholars, including Julia Wulforst, PA-C, Jennifer Kipp, DPM, Carla Holder, MD, Susie Fitzgerald, DO, Christine Khandelwal, DO, Michalina Kupsik, MD, Katie Lowry, MD, Jacqueline Njapa, MD, and Dana Point, MD. The MedTalks were followed by a meeting of the Opioid Task Force.
The day reached its climax with a joyous celebration of the Kanof Institute for Professional Leadership. The evening featured a cocktail reception, including a warm Welcome Reception and the formal presentation of graduation certificates to the 2023 KIPL class. The gathering was a moment to reflect on and commemorate the 20-year legacy of Leadership College.
Saturday began with the NCMS PAC Advocacy Breakfast, featuring a presentation by CEO Chip Baggett, who offered insights into the changing landscape of political division in the United States and strategies for advancing both the nation and the NCMS. Attendees enjoyed breakfast while several prizes and raffle items were distributed, and further interactions with exhibitors took place.
Following this, Elizabeth C. Tilson, MD, MPH, the State Health Director and the Chief Medical Officer for the Department of Health and Human Services and Ronald B. May, MD, delivered a presentation on the Public Health Commission.
The morning continued with an chance to see posters created by residents, fellows, and medical students from across the state, along with a final opportunity to engage with exhibitors. After that, NCMS President Dr. Arthur Apolinario participated in a panel discussion alongside NCMS Board members Andrew Lamb, MD, and Claude Jarrett, MD, FAAOS, focusing on the topic of 'When the Physician is the Patient.' The discussion was expertly moderated by NCMS' Dr. Kristina Natt och Dag. The NCMS Annual Meeting was also held Saturday afternoon.
Saturday night marked the moment when the festivities shifted into high gear at the 2023 Golden Stethoscope Awards Gala! The event was kicked off by NCMS' Randy Aldridge and Chip Baggett, who extended a warm welcome to past, present, and future NCMS presidents on the stage. A touching farewell was delivered by Past President Dr. Michael Utecht to President Dr. Arthur Apolinario, who presented him with the presidential pin. Dr. Apolinario, affectionately known as "Dr. Art," then directed his attention to incoming president, Dr. Eileen Raynor, MD, FACS, FAAP. He administered the oath of office and bestowed upon her the President's Medallion. Dr. Raynor then addressed the gathering with her inaugural speech as NCMS president.
Several awards were given including the Golden Stethoscope Awards. They went to:
- Dr. Karen Harum from Region 1
- Dr. Holly Biola from Region 2
- Dr. Joseph Bell from Region 3
- Dr. Alan Story from Region 4
The 2023 T. Reginal Harris Award was given to Dr. Jeffrey Kuremsky
The 2023 John Huske Anderson Award went to Brooks Bell
The 2023 E. Harvey Estes, Jr. Physician Community Service Award went to Dr. Peter Morris.
All of that was followed by a presentation on 20 years of NCMS Leadership College by Kristina Natt och Dag.
The evening wrapped up with comments from CEO Chip Baggett and dancing! All-in-all, it was another wonderful annual conference for the North Carolina Medical Society.
Your Input Needed for the AMA Physician Practice Information Survey

The American Medical Association (AMA) Physician Practice Information (PPI) Survey is underway, and we urgently need all selected physicians to actively engage in this effort. The intent of the survey, which has been endorsed by over 170 medical societies and other health care associations (see full list here), is to collect updated and accurate data on practice costs which are a key element of physician payment. These data have not been updated since last collected over 15 years ago and it is critically important to update these data to ensure accurate payment.
See here for more information about this survey.
Mathematica, a well-regarded consulting firm, is helping the AMA run this survey. Your practice may receive an email (from [email protected]) and an USPS priority mail packet from Mathematica that contained a link to the survey as well as supporting information. We urge you to speak with your practice management colleagues to determine if they have received these communications and ask them to complete this important survey. In the coming weeks or months, your practice, or Mathematica, may ask you to complete a brief survey on the number of weekly hours spent on direct patient care. We urge you to complete this two-minute survey. Help us help YOU to update Medicare physician payment!
Registration Open for "What’s Next with Medicare Payment Reform" Webinar

Payment cuts and temporary fixes have become predictable in Medicare physician payment over the past decade—leaving physician practices and patient access to care at serious risk.
Register for the AMA Advocacy Insights webinar "What’s Next with Medicare Payment Reform" to hear about:
- Where Medicare payment reform stands now
- How the AMA, alongside state and national medical specialty societies, is pushing for permanent payment reform
- How you can get involved in these advocacy efforts
Moderator:
- Willie Underwood III, MD, MSc, MPH, Chair, AMA Board of Trustees
Speakers:
- G. Ray Callas, MD, President Elect, Texas Medical Association
- Katie Orrico, Senior Vice President, Health Policy and Advocacy, American Association of Neurological Surgeons/Congress of Neurological Surgeons
- Todd Askew, Senior Vice President, Advocacy, American Medical Association
What’s Next with Medicare Payment Reform
Wild Raccoons Rabies Vaccine Initiative Underway in Western NC. Find a Packet, Leave it!

RALEIGH -- The North Carolina Department of Health and Human Services is working with the U.S. Department of Agriculture to help prevent the spread of rabies. Wildlife Services will be distributing oral rabies vaccine for wild raccoons in Western North Carolina.
Beginning Oct. 4, 2023, baits containing the oral rabies vaccine will be aerially distributed in Alleghany, Ashe, Buncombe, Cherokee, Clay, Graham, Haywood, Henderson, Jackson, Madison, Macon, Mitchell, Swain, Transylvania, Wilkes and Yancey Counties.
"Avoiding contact with wild animals and vaccinating our domestic animals and pets is the best way to prevent rabies, which can often be fatal," said NCDHHS Deputy State Public Health Veterinarian Erica Berl, DVM, MPH. "The wildlife rabies vaccination program prevents the spread of rabies among animals in the wild, which in turn prevents humans, pets and other animals from becoming infected."
The baits consist of a sachet, or plastic packet, containing the oral rabies vaccine. To make the baits attractive to raccoons, the packets are sprinkled with a fishmeal coating or encased inside hard fishmeal–polymer blocks about the size of a matchbox. When a raccoon bites into a bait, the vaccine packet is punctured, and the animal is exposed to the vaccine. This activates the animal’s immune system to produce antibodies that provide protection against rabies infection.
Anyone who comes in contact with the liquid vaccine should wash the affected area thoroughly with soap and water and call the phone number listed on the bait for further instructions and referral.
Although the oral rabies vaccine products are safe, the USDA Wildlife Services program has issued these precautions:
- If you or your pet find a bait, leave it where you found it unless it is on your lawn, driveway or other area unlikely to attract raccoons. While wearing a glove or other barrier, you can move the bait to an area of thicker cover where raccoons are more likely to find it and pets are less likely to encounter it.
- Eating the baits won’t harm your pet but consuming several baits might temporarily upset your pet’s stomach.
- Do not try to remove an oral rabies vaccine packet from your pet’s mouth, as you could be bitten.
- Wear gloves or use a towel when you pick up bait. While there is no harm in touching undamaged baits, they have a strong fishmeal smell.
- Instruct children to leave baits alone. If a bait is ingested by a child or adult, call 1-866-4-USDA-WS. NCDHHS has never received a report of a human ingesting a bait packet.
- Wash your hands thoroughly with soap and water if there is any chance the vaccine packet has ruptured.
- A warning label on each bait advises people not to touch the bait and contains the rabies information line telephone number.
Rabies is most commonly found in wild animals in North Carolina. This poses a risk to people and domestic animals that encounter wildlife. It is a fatal disease in mammals, including people.
However, there are highly effective vaccines that prevent infection and illness in people and domestic animals. By North Carolina law, cats, dogs and ferrets must be vaccinated by four months of age and be kept up to date throughout their lives.

For more information on rabies prevention or the oral rabies vaccine program, call the USDA Wildlife Services toll-free rabies line at 1-866-487-3297 or the NCDHHS Division of Public Health at 919-733-3419.
Baiting should be completed by late October. The Oral Rabies Vaccination program, originally implemented in the 1990s, helps prevent the raccoon rabies epizootic from moving west of the Appalachian Mountains, where raccoon rabies does not exist. The program has been successful in that regard and the vision is to gradually move the vaccine barrier east until raccoon rabies is eliminated. [source]
You can also find information about the national program on the USDA website.
For general information on rabies, please visit the CDC website.
WakeMed and Siemens Healthineers Offer Free 3D Mammography Screenings

RALEIGH – WakeMed and Siemens Healthineers, a leading medical device company and imaging innovator, are once again teaming up to bring 3D mammography screenings to the community. Last year, more than 250 women participated in the potentially life-saving screenings.
From Oct. 23 – 27 (8 a.m. to 4 p.m.), Oct. 28 (8 a.m. to noon), and Oct. 29-Nov. 2 (11 a.m. to 7 p.m.), women over the age of 40 can receive a 3D mammogram at no cost. The screenings will take place in the state-of-the-art Siemens Healthineers mobile digital mammography unit parked at WakeMed’s Raleigh Medical Park located at 23 Sunnybrook Road. The screenings are free and open to uninsured women over the age of 40 who have not had a mammogram in the last 12 months. Registration is strongly encouraged.
The mobile mammography partnership with Siemens Healthineers is part of WakeMed’s ongoing commitment to provide the community with greater access to critical breast cancer screenings and diagnostic tools to support early detection and intervention. Cancer disproportionately affects the underserved, underinsured and uninsured. Socioeconomic barriers to vital healthcare needs, like cancer screenings, often result in a late-stage cancer diagnosis.
“Early detection is essential when diagnosing and treating cancer. The earlier we can detect a problem, the better the chances are for both survival and remission,” said Dr. Brian Klausner, a physician and medical director for WakeMed’s Community Population Health program, which works to improve the health of uninsured and homeless patient populations. “The mobile mammography unit allows us to reach populations that have challenges that prevent routine medical tests and cancer screening, potentially saving lives.”
“Siemens Healthineers is proud to work with WakeMed for a second year to offer local women access to our advanced digital mammography technology, which has been specifically designed to help ensure a more comfortable screening experience,” said Felicia Kurtz, senior vice president of Advanced Therapies and executive sponsor for Health Equity and Outreach Activities at Siemens Healthineers North America.
Raleigh Radiology, a designated Breast Imaging Center of Excellence by the American College of Radiology and WakeMed’s imaging partner, will review all scans taken during the mobile mammogram event and consult with WakeMed doctors on any necessary next steps.
This is the second year WakeMed and Siemens Healthineers have partnered to offer mammography screenings to the greater Triangle area.
Registration for screenings is strongly encouraged. To register for a mammogram, visit: https://www.wakemed.org/care-and-services/imaging-services/mobile-mammography-event With questions, or to register via phone, call 919-350-1317.
Hospital Violence Protection Act Enacted
In his freshman year as a member of the NC House of Representatives, Dr. Tim Reeder achieved a notable victory in the passage of the Hospital Violence Protection Act. This legislation, initially introduced as a stand-alone bill, HB809, was ultimately incorporated into another bill, HB125. It was passed with broad bipartisan support by both chambers and signed by the Governor on September 29, 2023.
The new law will make hospitals a safer care environment for patients, staff and the public. There will be an increased presence of law enforcement to provide greater security in hospital facilities, with a focus on the emergency department. The bill also includes training and reporting provisions to monitor the measure’s impact and compliance.
Dr. Reeder thanked multiple stakeholders for their support, including the NC Medical Society, the NC Healthcare Association and law enforcement. You may view Dr. Reeder’s summary of the legislation here and the press conference here.

Dr Reeder provided an
overview of the new law and
thanked his legislative colleagues
for their bipartisan support

NCMS President, Dr. Art Apolinario, shared
the NC Medical Society’s support of the
Hospital Violence Protection Act

Joining Dr. Reeder at the October 10
press conference were (left to right) Erik Manring MD,
Craig Mangum MD, Arthur Apolinario MD – NCMS President,
and Greg Cannon MD
NCMS LEAD MedTalk Speaker Showcase: Dr. Dana Point
NCMS Welcomes 2023 Leadership College Scholar
Dana Point, MD
We can't wait to see you at the 2023 LEAD Conference and Golden Stethoscope Awards Gala!
Hear Dr. Point's MedTalk: "Bolstering Awareness of Rare Disease through a Novel Approach"
To learn more about leadership training opportunities at NCMS click here.
NIH’s Build UP Trust Challenge

Racial injustice and inequities in healthcare contribute to health disparities. Lack of trust among underserved populations can lead to reluctance to engage with biomedical research and utilize healthcare technologies. The National Institutes of Health's (NIH) Build UP Trust Challenge will award up to $1.25 million to improve engagement with minority health populations and populations with health disparities.
NIH seeks solutions that increase research participation and the adoption of existing and new tools and approaches to detect, treat, and monitor diseases, conditions, and disorders.
The website includes a Readiness Tool to help you determine eligibility and ensure your solution is a strong fit.
Application Deadline Extended for The Physicians Foundation 2024 Fellowship Program

The Physicians Foundation recently launched a call for applicants for the Fellowship Program! New or early-career physicians are encouraged to apply by November 16.
With a focus on drivers of health (DOH), the Fellowship Program enhances physicians’ leadership skills so they can strengthen the physician-patient relationship, support medical practices’ sustainability and navigate the changing health care system. The fellow will develop and implement a project that supports physicians in their understanding of DOH and integration into medical practices.
Requirements include:
- Open to physicians who are new or early-career in their practice.
- Applicants must demonstrate experience with and/or interest in DOH, physician leadership, health policy, health equity and clinical/care delivery innovation.
- Submit a program application with a current resume/CV and statement of intent that briefly describes how participation will be a transformative experience for you to learn how to make positive, constructive contributions to the medical profession in the future.
Receive two (2) letters of recommendation, one of which is recommended to be from the fellow's state or county medical society.
About The Physicians Foundation
The Physicians Foundation is a nonprofit seeking to advance the work of practicing physicians and help them facilitate the delivery of high-quality health care to patients. As the U.S. health care system continues to evolve, The Physicians Foundation is steadfast in strengthening the physician-patient relationship, supporting medical practices’ sustainability and helping physicians navigate the changing health care system. The Physicians Foundation pursues its mission through research, education and innovative grant making that improves physician wellbeing, strengthens physician leadership, addresses drivers of health and lifts physician perspectives. For more information, visit www.physiciansfoundation.org
Links in Pink Breast Cancer Screening Event Happening this Month

WILMINGTON — Novant Health and the Wilmington Chapter of Links, Incorporated will host Links in Pink next week, where locals can access mammogram screenings and health resources in honor of Breast Cancer Awareness Month.
The event will take place on Saturday, October 21 at the MLK Center, 401 S. Eighth St. in Wilmington from 11 a.m. to 3 p.m. During this time, Links members will educate the community about the importance of breast awareness, self-examinations and mammograms. Novant Health will provide mammograms and share resources for surgical and prosthesis bras.
Breast cancer survivors will also be celebrated, including Mildred Bethea, the event’s featured speaker.
This event is co-sponsored by Novant Health and the YWCA of The Lower Cape Fear.
Appointments are recommended. To schedule, please call (910)721-1485. The minimum age for a screening mammogram on the mobile is 35. Screening mammograms are covered as preventive care under most insurance plans. For convenience, Novant Health will file a claim with the insurance provider. [source]
NC Medicaid – F Code Survey to Gauge Prenatal & Postpartum Care

The Division of Health Benefits of the NC Department of Health and Human Services is requesting North Carolina ob/gyns and primary care practices to help NC Medicaid better track prenatal and postpartum care access. Below is a notice from DHHS/DHB with a link to a survey asking about the use of F codes and feasibility of practices’ EHR incorporating these codes.
F Code Availability within EHRs to Support Measurement of Prenatal and Postpartum Care Visits
To better understand the number of NC Medicaid members receiving prenatal and postpartum care, NC Medicaid encourages providers to use two F codes: 0500F for Initial Prenatal Visits and 0503F for Postpartum Care Visits.
In an effort to determine whether a practice's current Electronic Health Record (EHR) allows for the selection of the above codes, we are asking practices to complete a brief survey.
Survey: The survey is accessible here.
Deadline: Friday, October 20
Thank you for your assistance! If you have any questions, contact Hannah Fletcher at NC Medicaid via [email protected].
NCMGMA Salary and Benefits Survey Now Open
NCMGMA Salary and Benefits Survey is Open
EASIER Data Collection is Here!
Complete your survey by November 22nd
This comprehensive study is designed to bring our members the information they need to see trends specific to the healthcare industry, and provide comparative information your organization can use to assist in making crucial business decisions.
NEW! If you participated last year, you can copy last year's data into this year's survey, effectively reducing the time it takes to complete the survey! New positions have also been added this year, including a traveling nurse position.
Data collection is now open through Wednesday, November 22nd.
Complete 75% to gain access to complimentary reporting!
Access to the Site:
- Link: https://benchmark.ncmgmasalarysurvey.com/
- Enter your Username & Password to begin entering in data:
- If you've forgotten your password, please use the prompt on the page to assist.
New User? Click here to get started
Survey Information:
- Once logged in, check out the Support Page to find the:
- Survey Positions listing: sort by Category, Department or Position.
- Survey Worksheet, a downloadable spreadsheet used to help compile data to get you started prior to entering in data.
- User Guide, which will help answer many of your how-to questions. It can also be found on the Support page in the survey, once logged in.
- The Survey is divided into sections that contain categories of questions. You can begin in any section and complete the survey questions in any order.
- The progress bar on the home page will track your overall progress and the icons will help you see any areas not completed.
- Come back as often as needed to complete the survey. All data is saved as you go.
In order to access results when they are released (December), participants must complete all required questions and a minimum 75% of the survey
Questions:
If you have any questions about the 2023 Salary & Benefits Survey, please contact the NCMGMA offices at [email protected]
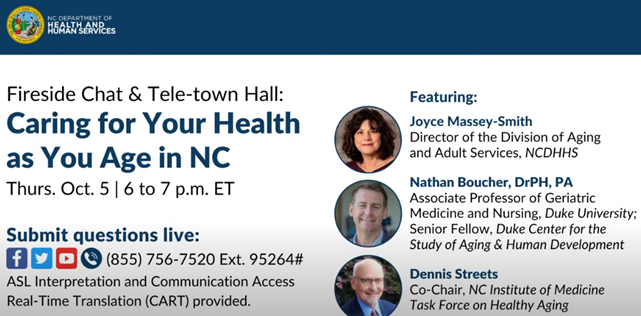
ICYMI: Tele-Town Hall: Caring for Your Health as You Age in NC
On Thursday, October 5, NCDHHS held a tele-town hall discussing how aging adults, particularly those living in rural communities, can support their health and access the care they need. Topics included resources and services for older adults in rural communities, the importance of routine health visits and care, and mental health services.
NCMS LEAD MedTalk Speaker Showcase: Dr. Randall Schisler
NCMS Welcomes 2023 Leadership College Scholar
Randall Schisler, MD
Join us at the 2023 LEAD Conference and Golden Stethoscope Awards Gala in 3 days!
Hear Dr. Schisler's MedTalk: "Developing the Outpatient Palliative Care Clinic"
To learn more about leadership training opportunities at NCMS click here.
NCMS Member, Representative Dr. Kristin Baker Not Running for Re-Election
NCMS Member, Representative Dr. Kristin Baker Decides Against Another Term

2023 SHD Report, CPH Agenda Released for October 14 Meeting

State Health Director Elizabeth Cuervo Tilson, MD, MPH, has announced the CPH agenda and State Health Director Annual Report for the October 14 meeting in Durham.
COMMISSION FOR PUBLIC HEALTH
Commission Conjoint Meeting with the NC Medical Society
October 14, 2023
9:00 a.m.
Sheraton Imperial Hotel Raleigh-Durham Airport at RTP
Room: Imperial 1234
4700 Emperor Boulevard
Durham, NC 27703
I-140 at Exit 282
AGENDA
A. Call to Order Dr. Ron May
B. Invocation
C. Ethics - Conflict of Interest Statement
1. State Health Director’s Annual Report Dr. Betsey Tilson
2. New Business
3. Adjournment
Zoom
Link: https://us06web.zoom.us/j/89924373359
Meeting ID: 899 2437 3359
Passcode: LEAD2023
Phone: +13052241968,,89924373359#
View the Annual Report here: State Health Director Annual Report 2023 FINAL
NCDHHS Receives $14.8 Million Grant to Strengthen Behavioral Health System for Children and Families

RALEIGH — The North Carolina Department of Health and Human Services has received a four-year grant totaling $14.8 million from the Substance Abuse and Mental Health Services Administration to support the mental health of children and families in North Carolina. The funding will be directed towards North Carolina’s System of Care which connects young people and their families with needed services and resources, including mental health care so they can be safe and successful at home, at school and in their community.
The grant comes at a time when children and youth are facing an urgent mental health crisis. During the pandemic, the rate of children in North Carolina discharged from an emergency department with a behavioral health condition increased by 70%. In 2021, about one in five North Carolina adolescents seriously considered taking their own lives.
"These investments further our efforts to provide children with treatment that promote lasting whole person health and whole family healing," said NCDHHS Secretary Kody H. Kinsley. "Forging local partnerships across multiple systems that wrap children and families with care and support that is easy to navigate is key."
The $14.8 million SAMHSA grant enhances the NC System of Care to ensure more children have access to High-Fidelity Wraparound services, which help children and families before, during and after a crisis. The money will be used to bolster the efforts of county departments of social services, the NC Department of Public Safety-Division of Juvenile Justice, local schools and community groups.
"This grant will support High-Fidelity Wraparound, one of our most promising evidence-based programs for children, and it will also build a statewide infrastructure to support communities in their efforts to address service and program gaps," said Yvonne Copeland, Director of the NCDHHS Division of Child and Family Well-Being. "Our local partners are a vital component of our statewide System of Care, and the SAMSHA grant will allow us to continue to support the vital work they do."
"HFW and SOC foster partnership and collaboration that empower youth and families in North Carolina," said Tara Ward, Project Manager of the NC High-Fidelity Wraparound Training Program for NCDHHS. "With properly funded support systems in place, our young people are far more likely to manage and achieve their self-identified goals."
NC SOC grant-funded activities will focus on increasing the utilization of existing services and identifying gaps to reduce the need for emergency department visits and residential treatment by building on the existing program and expanding it into new counties. As the grantee, DCFW will contract with partner organizations as well as build internal capacity to support program implementation.
"Supporting the individual programs that make up the System of Care provides a stronger, more cohesive support structure for North Carolina’s families and young people," said Dr. Kristin Jerger, NC System of Care Project Director at NCDHHS. "One of the most important of which is putting the family and young person in the driver’s seat of their own care." [source]
More information on the NC System of Care can be found on the NCDHHS website.
More People Can Get Health Care Coverage Through Medicaid Beginning December 1
Beginning December 1, 2023, more people can get health coverage through Medicaid. Medicaid will cover people ages 19 through 64 years with higher incomes. North Carolinians may be able to get health care insurance through Medicaid even if they didn’t qualify before.
Medicaid pays for doctor visits, yearly check-ups, emergency care, mental health services and more – at little or no cost to beneficiaries.
Most people will be able to get health care coverage through Medicaid if they meet the criteria below. And if you were eligible before, you still are. Nothing changes for you. To learn more, go to medicaid.ncdhhs.gov.
- Live in North Carolina
- Be ages 19-64
- Be a citizen. Some non-US citizens can get health care coverage through Medicaid. To learn more, go to medicaid.ncdhhs.gov.
- Have a household income that is below 138% of the federal poverty level. That’s about $20,000 for a single adult or about $34,000 for a family of three.
People can apply for Medicaid online at epass.nc.gov. They can also submit a paper application or apply in person at their local Department of Social Services (DSS). Applications may take up to 45 days to process. Incomplete applications may take longer. To help the process go faster, people can:
- Apply online at ePASS and provide all the information requested. If the application is incomplete, it may take longer to process. DSS will need to follow up with the applicant.
- Keep contact information up to date in ePASS, to receive all important information about Medicaid benefits.
- Sign up for an enhanced ePASS account to keep their information updated without having to contact the local DSS office.
To learn more, visit Medicaid.ncdhhs.gov.
Do You Know a Healthcare Professional Who Goes Above and Beyond? Nominate Them to be a Healthcare Hero!
NC State Athletics and North Carolina Healthcare Association are celebrating local healthcare workers!

Do you know a healthcare professional who embodies the true spirit of a healthcare hero through their dedication, compassion, and hard work? If so, recognize their efforts.
Two nominees will each receive one of the following prize packs:
- 4 Football Tickets, Pre-Game Hospitality, and an Autographed Football
- 12 Tickets to a Men's Basketball Game and an Autographed Basketball
To nominate someone, complete the entry form here.
New Cybersecurity Training Videos for Clinicians Available on AMA Ed Hub

The “Cybersecurity for the Clinician” video training series on the AMA Ed Hub™ provides physicians and students in the medical profession with what they need to understand how cyber-attacks can affect clinical operations and patient safety. The eight videos in the series use easy, non-technical language to explain how you can do your part to help keep health care data, systems and patients safe from cyber threats. With October recognized as Cybersecurity Awareness Month, use this resource to stay current on your security training and posture.
Produced by the Healthcare and Public Health Sector Coordinating Council Cybersecurity Working Group, Episode 1 of the series, Cyber Safety Is Patient Safety, discusses the threat cyber-attacks pose to patients, including stealing patient data, disrupting clinical operations, and ultimately harming patients. Other episodes feature discussions on the social engineering techniques that are used to acquire patients' personal information, medical device cybersecurity, and the teams that act after a cyber-attack occurs. Each episode is hosted by Christian Dameff, MD, an emergency medicine physician and medical director for cybersecurity.
Also, in recognition of Cybersecurity Awareness Month, take advantage of other resources. The Department of Health and Human Services (HHS) 405(d) Program is focused on providing the health care sector with impactful resources, products and tools to raise awareness and strengthen its cybersecurity posture against threats. In addition, at its physician cybersecurity webpage, the AMA has curated resources and tips for physicians and health care staff to protect patient health records and other data from cyberattacks.
Check Your Inbox! NCMS Election E-mails Arriving Now. Deadline to Vote is October 12

You should have received an NCMS election email by now. It is coming from our third-party vender, Intelliscan. If you have not seen it, please check your spam folder. The North Carolina Medical Society Nominating and Leadership Development Committee has issued the final slate of candidates. Under the NCMS’ governance structure, online voting for the candidates began on September 28, 2023 and will continue until midnight on October 12, 2023.
Paper ballots will be available to those who need them. If you did not receive your ballot, please contact the NCMS.
Individuals interested in voting in the NCMS Election must be an active NCMS Member (2023 dues paid).
The following slate of candidates was selected by the Nominating and Leadership Development Committee:
NCMS Board of Directors
• President Elect: John J. Meier, IV, MD
• Secretary-Treasurer: Tracy L. Eskra, MD
• Region 3 Representative: Karen L. Smith, MD
• Region 4 Representative: Martin Palmeri, MD
• At-Large Member: Bryant A. Murphy, MD
• At-Large Member: William G. Ferrell, MD
• At-Large Member: Ronald B. Laney, Jr., MD
NC American Medical Association Delegation
• AMA Delegate: Mary Ann Contogiannis, MD
• AMA Delegate: Justin B. Hurie, MD
Nominating and Leadership Development Committee
• NLDC Region 2: John B. Chiavetta, MD
• NLDC Region 2: Damian F. McHugh, MD
Get Ready for December! NCDHHS Releases Medicaid Expansion Toolkit

RALEIGH -- The North Carolina Department of Health and Human Services has released a Tool Kit for the long-awaited expansion of Medicaid in the state. The bilingual kit includes all you need to know to spread the word to your patients and answers some frequently asked questions.
The kit includes:
- Day 1 Flyer: An overview of who is eligible and how to enroll.
- Newsletter Template: Content to include in your newsletters and emails.
- Social Media: Graphics and posts to share on your channels.
- Family Planning Flyer: Information for the approximately 300,000 people who receive limited benefits through Family Planning Medicaid who will be automatically enrolled in full Medicaid.
- Medicaid Essentials Deck: A presentation to share with your community on who is eligible and how to enroll.
- FAQ: Answers to common questions.
- ePass Video: An overview of how to apply online through ePass.
A complete look at all the information from NCDHHS can be found here.
To stay updated with the latest information, be notified when the application process goes live, and receive the newest resources, complete this sign-up form.
Atrium Health Honored for Prioritizing Well-Being of Health Care Workers

CHARLOTTE – Even before the pandemic challenged our health care workers, Atrium Health was focused on making the health system the “best place to care,” seeking feedback from care providers with a goal of ensuring doctors, nurses and other members of the care team weren’t burdened with administrative tasks so they could focus on the fulfilling aspects of treating patients. That, and other programs designed to lift up and support its workforce, has earned Atrium Health the Joy in Medicine™ Gold designation from the American Medical Association (AMA).
The Joy in Medicine Health System Recognition Program honors health systems that demonstrate a commitment to preserving the well-being of clinical care team members in combating work-related stress and burnout. The two-year designation’s scoring criteria is based on demonstrated competencies in commitment, assessment, leadership, efficiency of practice environment, teamwork and support. The recognition extends across the entirety of the Atrium Health footprint, including Atrium Health in the greater Charlotte area, Atrium Health Wake Forest Baptist in Winston-Salem, North Carolina, Atrium Health Navicent in Macon, Georgia, and Atrium Health Floyd in Rome, Georgia.
“We are deeply honored and proud to receive this prestigious designation,” said Dr. Suzanna Fox, senior vice president and deputy chief physician executive for Atrium Health. “Our ‘best place to care’ initiative has made a significant difference in the lives of our clinicians – maximizing their time with patients, which is why they got into medicine in the first place, and reducing the administrative burden. It empowers them to maximize their passion, potential and performance. We’re truly trying to maintain a culture of well-being for all and to receive this type of recognition for our efforts is very meaningful for all of our teammates.”
A total of 72 health systems, nationwide, earned recognition this year, with documented efforts to reduce system-level drivers of work-related burnout and demonstrated competencies in commitment, assessment, leadership, efficiency of practice environment, teamwork and support. Atrium Health was one of only 10 systems to receive the Gold designation this year. After first receiving the award’s Silver designation in 2021, Atrium Health leaders got to work on continuous improvement around this effort. Since that time, they have had workstreams focused on six core competency areas – including efficiency, leadership, teamwork and support – to ensure that improvements were continuing to be made.
“Atrium Health is continually focused on the health of our clinicians,” said Dr. Scott Rismiller, executive vice president and chief physician officer at Advocate Health, of which Atrium Health is now part. “The AMA estimates that only 27% of a clinician’s day is spent meeting one-on-one with patients, so we launched ‘best place to care’ more than four years ago to remove those obstacles that stand in the way of clinicians caring for their patients. Once you remove friction points that get between the clinician and the patient, our clinicians can then do what comes naturally, care for their patients and care for each other.”
"The goal of the Joy in Medicine Health System Recognition Program is to unite the health care community in building a nationwide culture committed to the well-being of clinical care teams by helping health organizations invest in action plans promoting professional fulfillment and meaning that clinicians find in caring for their patients,” said Dr. Christine Sinsky, AMA vice president of professional satisfaction.
“Health organizations that have earned recognition from the AMA’s Joy in Medicine Health System Recognition Program are leading a national movement that has declared the well-being of health professionals to be an essential element for providing high-quality care to patients, families and communities,” said AMA President Dr. Jesse M. Ehrenfeld. “Each Joy in Medicine-recognized organization is distinguished as among the nation’s best at creating a culture of wellness that makes a difference in the lives of clinical care teams.” [source]
Congratulations, Atrium Health!
Time is Running Out! Don't Miss Your Opportunity to Attend LEAD!
The last day to register for the LEAD conference is Sunday. Don't miss your chance to discuss the latest healthcare topics, network, and support your profession!

Below are just a handful of hot topics you'll hear about at this year's LEAD conference:
- Women's reproductive and Black maternal health;
- Young physician and PA hot topics;
- Clinician well-being;
- MEDTalks, featuring emerging issues in healthcare
And don't forget about the 2023 Golden Stethoscope Awards Gala! We'll be celebrating the 20th Anniversary of Leadership College, our flagship leadership development program!
Still on the fence about attending? Listen to why NCMS Board Member Claude Jarrett, MD, enjoys being a part of LEAD every year. Plus, hear why Roy Strowd, III, MD, is excited about the conference.