NCMS Partnership Launches Fellowship Opportunity at Stanford University
Stanford University is now accepting applications for the first ever Pediatric Acute-onset Neuropsychiatric Syndrome (PANS) fellowship program in the world, an effort the NCMS proposed in 2021. This opportunity is made possible thanks to a grant from the North Carolina legislature to the North Carolina Medical Society and the Neuroimmune Foundation.
Launching this fellowship is a huge step in setting up patient-centered PANS clinics treating children and adults in insurance-based settings around the country. Applicants are required to make a commitment to practice in North Carolina.
Learn more about this amazing opportunity and apply here.
Join DOCMS for the First Meeting of 2023!
"Firearm Injury Prevention"
Clarence F. Birkhead
Sheriff, Durham County, North Carolina

Clarence F. Birkhead, 62, was first elected in December 2018; becoming the 13th sheriff in Durham County and the county’s first African-American sheriff. On November 8, 2022, Sheriff Birkhead was re-elected to serve a second term in office after receiving overwhelming support from the local electorate in Durham. Sheriff Birkhead has 38 years of law enforcement experience – 17 of those at the Duke University Public Safety Department.
During his first term as Sheriff, the Durham County Sheriff’s Office has worked to increase the transparency, engagement, and accountability of the office by creating a Sheriff’s “Community Advisory Board.” Under his watch, Sheriff Birkhead has also achieved the “triple crown” of accreditation, CALEA (Commission on Accreditation for Law Enforcement Agencies), American Correctional Association (ACA), and the National Commission of Correctional Health Carte (NCCHA). By doing so, DCSO is only one of three agencies in the entire state of North Carolina and just the 29th in the United States to achieve certification from all three national agencies.
In August 2021, he was appointed by North Carolina Governor Roy Cooper to the North Carolina Task Force for Racial Equity in Criminal Justice and later to the Governor’s Crime Commission (August 2022).
University Club, 3100 Tower Boulevard, Suite 1700 - Durham, NC 27707
Wednesday, February 8, 2023 | 6:00pm - 8:00pm
A Zoom link will be sent to all registrants, once the registration closes.
________________________________________
AGENDA:
• 6:00pm-6:30pm– Socializing
• 6:30pm-7:45pm– Dinner, Guest Speaker & Discussion
• 7:45pm-8:00pm– DOCMS 2023 Schedule
CME Credit is available for this session.
DOCMS Members and Prospective Members are welcome to attend.
________________________________________
 Online registration closes on February 7th, 2023 at 12pm.
Online registration closes on February 7th, 2023 at 12pm.
Questions? Email Frank Snyder at [email protected]
And the Winners Are...

First, thank you to everyone of you who took time to read the NCMS Bulletin: 2022 Year in Review and for participating in our daily trivia questions!
Now, for the moment you've all been waiting for!
And the winners are:

Be on the lookout for your NCMS prize pack!
To see the NCMS Bulletin: 2022 Year in Review, click here.
NCMS Alliance 100th Anniversary Celebration

The North Carolina Medical Society Alliance Centennial Celebration is April 27, 2023!
On April 18, 1923, the Woman’s Auxiliary of the Medical Society of the State of North Carolina began, the result of efforts by Dr. John Wesley Long, then president of the NC Medical Society House of Delegates, to start an auxiliary to the medical society. Today’s organization, the North Carolina Medical Society Alliance, is a charitable volunteer organization open to membership for all physician spouses and physicians. The NCMSA is a 501 (c) (3) organization dedicated to building healthy communities and supporting the family of medicine through community service.
After almost 100 years, the founding of many community service initiatives, thousands of volunteer hours and a couple of name changes, the North Carolina Medical Society Alliance is excited to celebrate 100 years of service. The Greensboro History Museum will host the NCMSA Centennial Celebration on April 27 from 5:30-8:30pm.
Sponsorship opportunities for our centennial celebration are available. Thank you to WakeMed Health and Hospitals, a Gold sponsor of our Centennial Celebration. Gold, silver, and bronze sponsors who commit by the February 15 deadline will appear in the Spring 2023 edition of the Tarheel Tandem. Those committing after that deadline will appear in the Fall 2023 Tarheel Tandem. Other Sponsorship benefits are detailed in the sponsorship prospectus, available at the following link.
Historical highlights of the North Carolina Medical Society Alliance, highlighted by the decade, are available on the NCMSA website. More decade reviews will be published in the coming months.
Additional links of interest:
North Carolina Medical Society Alliance Celebrates Centennial
North Carolina Medical Society Alliance Celebrates Centennial – Part 2
North Carolina Medical Society Alliance Celebrates Centennial – Part 3
Session Week 2: What NCMS Members Need to Know

This report is for the week ending February 3, 2023
As the second week of the 2023 NC General Assembly Long Session comes to a close, things are heating up in Raleigh. The Senate Health Committee has begun considering multiple bills that may impact you and your practice.
Especially of note, the Parent’s Bill of Rights, SB 49, which would require written consent of a parent for a clinician to treat a child. It is one of the few bills making moves last week. It moved quickly though the Education and Health Committees and next week will be considered by the Rules Committee.
Other Bills of Note that NCMS is monitoring:
SB 45, Certified Alcohol and Drug Counselor Supervision: Would remove involved supervision requirement for Certified Alcohol and Drug Counselors & Certified Criminal Justice Addictions Professionals.
SB 46, Medical Billing Transparency: Would prevent surprise billing for out-of-network healthcare providers that are in-network with an individual's health benefit plan.
SB 47, PA Team-Based Practice: Would change supervision of PAs by physicians and changes to the licensure of physician assistants, if the PA is working in a team-based environment.
SB 48, Repeal Certificate of Need Laws: Would repeal all of North Carolina's Certificate of Need Laws.
SB 49, Parent’s Bill of Rights: Would give parents explicit rights to monitor/review documents on their children's healthcare, education, religion.
HB 35, Expand Definition of Opioid Antagonist: Would expand the definition of opioid antagonist (naloxone) in North Carolina to include all opioid antagonists approved by the FDA for treatment of drug overdose.
HB 43, Prohibition of Certain Hormone/Surgery/Minors: Would make it illegal for minors to receive any puberty blockers, cross-sex hormones, and other related treatments or procedures.
Click here to view summaries on the bills listed above.
One More for Day 4 of NCMS Bulletin: 2022 Year in Review Trivia!

It's NCMS Bulletin: 2022 Year in Review Trivia Time!
It's the last day of trivia, so we had to make this one good! For a chance to win one (1) of five (5) awesome prizes, simply answer the following question:
Who is the new NCMS President?
The first five people to respond (correctly) to today's NCMS Bulletin: 2022 Year in Review Trivia Question will win a special gift from the NCMS!
To see the NCMS Bulletin, 2022 Year in Review click here.
Update: Winners announced Monday, February 7.
Good luck!
Wear Red for Women Today!

Today is National Women’s Heart Day!
The American Heart Association’s signature women’s initiative, Go Red for Women, is a comprehensive platform designed to increase women’s heart health awareness and serve as a catalyst for change to improve the lives of women globally.
Cardiovascular disease is the No. 1 killer of women, causing 1 in 3 deaths each year. Raise awareness for heart disease and stroke by wearing Red on Today, Friday, February 3, National Wear Red Day.
Learn more about the American Heart Association's initiative here.
Post photos of your red OOTD below! We'd love to see you doing your part!
NCMS Adopts New Policy on Reproductive Health Care

The North Carolina Medical Society Board of Directors has unanimously approved a new policy addressing reproductive health care.
The Access to Comprehensive Reproductive Health Care reinforces the NCMS fundamental belief that medical decisions should be made between a patient and their physician/clinician. This is especially true when it comes to personal and complex decisions around reproductive health.
The policy is a joint effort between the NCMS Policy Committee, NCMS Ethical & Judicial Affairs Committee, and external experts in obstetrics and gynecology, and emergency medicine.
The new policy reflects the NCMS Mission, Vision, and Guiding Principles and underscores the Society’s unwavering support for patients and physicians/clinicians who face some of life’s most difficult decisions.
Yippee! Day 3 of NCMS Bulletin: 2022 Year in Review Trivia!

It's NCMS Bulletin: 2022 Year in Review Trivia Time!
We're back again with a brand-new question! For a chance to win one (1) of five (5) awesome prizes, simply answer the following question:
What is the minimum lifetime donation needed to become a member of the 1849 Society?
The first five people to respond (correctly) to today's NCMS Bulletin: 2022 Year in Review Trivia Question will win a special gift from the NCMS!
To see the NCMS Bulletin, 2022 Year in Review click here.
Winners announced Friday, February 3.
Good luck!
CDC Investigates Popular Eye Drop Brand, Urges Against Using

The US Centers for Disease Control and Prevention is urging health care providers and consumers to stop using EzriCare Artificial Tears as it conducts an investigation into at least 50 infections in 11 states that have led to instances of permanent vision loss, hospitalization and one death.
Read the full article here.
NCMS PAC Thankful Thursday!

On this Thankful Thursday, we are recognizing some of our NCMS PAC Investors! Thank you for your continued support and investment to your patients and profession. Contact Hannah Rice ([email protected]) to learn more about how you can make a difference.
Anton Manasco, MD
Edward Whitesides, MD
Katie Lowry, MD, MPH
Leta Sue C. Lamb, MD
Linda Lawrence, MD
Philip Brown Jr., MD
You Can Now Access Your NCMS Membership Card Anytime, Anywhere!
Need a New or Replacement NCMS Membership Card? You can now access it online!
Here's how (You must log in to access your card):
1. Click here to access the NCMS website

2. Hover over the "Membership" tab at the top of the page
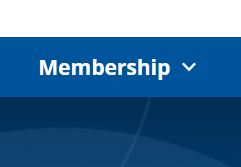
3. Click on "My NCMS Membership Card" from the dropdown list
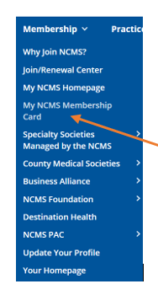
4. If you're not already logged in, you will be prompted to do so.
5. Screenshot or Print Page
That's it! You're done.
February is Black History Month!
The North Carolina Medical Society recognizes and celebrates Black History Month.
The NCMS uses the lessons of the past to shape our future. We continuously strive to become a better organization and are fully committed to ensuring ALL members are equally represented.
View a Historic account of the NCMS--Past to Present.
Curi Holdings and Constellation Sign Agreement to Merge
Curi Holdings, Inc. (Curi) and Constellation, Inc. (Constellation), two of the nation’s leading providers of medical professional liability (MPL) insurance, have signed an agreement to merge. Combined, the two organizations will build on their legacies of mutual ownership, client service, and innovation while creating a national brand that seamlessly delivers the products, services, and valued advice that healthcare providers need to thrive in a rapidly evolving landscape.
Read the full press release here.
Ready, Set, GO! for Day 2 of NCMS Bulletin: 2022 Year in Review Trivia!

It's NCMS Bulletin: 2022 Year in Review Trivia Time!
Who's ready for today's trivia question? For a chance to win one (1) of five (5) awesome prizes, simply answer the following question:
What is the average loan repayment amount for CPP participants?
The first five people to respond (correctly) to today's NCMS Bulletin: 2022 Year in Review Trivia Question will win a special gift from the NCMS!
Winners announced Friday, February 3.
Good luck!
P.S.: THANK YOU to everyone who responded to yesterday's trivia question! We LOVE when our members are engaged!
Is Your Practice Receiving State Funds for Care? Connect to NC HealthConnex

The mandate to connect to the state-designated health information exchange, NC HealthConnex, required that those receiving state funds for care, such as Medicaid and the State Health Plan, initiate their connection by January 1, 2023.
While the law regarding this connection mandate is complex, the following will provide some clarification:
- Signing a participation agreement demonstrates a good-faith effort to meet the connection mandate.
- Once you have an executed agreement, meaning that both your practice and the NC HIEA have signed, you are placed in the onboarding queue where your organization will wait for an invitation to begin your technical connection.
- Actively engaging in the onboarding process with your technical vendor and the NC HIEA also demonstrates a good-faith effort to meet the connection mandate.
At this time, thousands of provider organizations are in various stages to complete their connection.
You're encouraged to begin training while they are in the onboarding queue. Various training materials such as webinars, user guides, and self-paced modules are on the NC HIEA website. You can also request training for your practice using this form.
If you would like more information, reach out to the provider relations team at [email protected] or give them a call at 919-754-6912. You can also view the connection deadline FAQs.
A report of which health care organizations have or have not connected to NC HealthConnex will be submitted to the N.C. General Assembly this legislative session.
Happy Birthday to These Members Celebrating This Month!

Grab your party hats and noise makers and Let's Celebrate!
Mustafa M. Abugideiri, MD
Elizabeth Acquista, MD
Amer Adam, MD
J. Wellington Adams, MD
Satish P. Adawadkar, MD
Ira N. Adler, MD
Deborah G. Agisim, MD
Sukaina Ahmad, MD
Farhan Ahmed, MD
Richard E. Akers, Jr., MD
Shereen A. Alavian, MD
David R. Allen, Jr., MD
John G. Alley, Jr., MD
Eric D. Alpert, MD
Michael K. Altenburg, MD
Fabian E. Alzamora, MD
David A. Ames, MD
William D. Andersen, MD
Kent T. Anderson, MD
Mark W. Anderson, MD
Micaela D. Antzoulatos, PA-C
Howard L. Armistead, Jr., MD
Don M. Armstrong, MD, FACOG
David Arthur Aguilar, MD
Moogali M. Arvind, MD
Behnam Asgharian, MD
Erhan C. Atasoy, MD
George L. Auman, MD
H. Vann Austin, MD
Maria Lourdes C. Austria, MD
Anthony F. Azzi, MD
Carter S. Bagley, MD
Elizabeth R. Bagsby, MD
Khosrow Bahrani, MD
Patrick L. Ballen, MD
Cynthia A. Ballenger, MD
Cecilia W. Banga, DO
Graham A. Barden, III, MD, FAAP
Kelly L. Barham, MD
Kelsey J. Barr, MD
Thaddeus J. Barringer, Jr., MD
Michael J. Bartiss, MD
Sarah E. Bedard, PA-C
Mary E. H. Belet, PA
Eugene D. Bell, III, MD
John M. Benbow, MD
Carl W. Berk, MD
Michael B. Berry, MD
Todd M. Beste, MD, FACOG
Michael A. Biggerstaff, MD
Jack S. Billings, MD
Douglas W. Bitzer, PA-C
Justin C. Black, MD
James R. Boatright, MD
Barry H. Bodie, MD
Douglas L. Boertje, MD, FAAP
Terrence D. Bogard, MD
Katherine E. Bogart, PA
Christina M. Bowen, MD
Stephen L. Bower, MD
Stephen E. Boyce, MD, FACS
Raymond J. Bradley, Jr., MD
Michael E. Brame, MD
Alex G. Brann, PA-C
Simon David Braun, MD
Vaughn G. Braxton, MD
Mark S. Brazinski, MD
Kelly B. Bridgeman, MD, FAAP
Michael S. Broder, MD
Dora M. Brodie, MD
Patrick A. Brooks, MD
Mark S. Brown, MD, FACS
Susan B. Brown, MD
John H. Bumgarner, MD
Craig N. Burkhart, MD
Paul L. Burroughs, Jr., MD
Sean P. Bush, MD
William E. Byrd, MD
Jack R. Cahn, MD
Taylor W. Callahan, PA-C
James A. Campbell, MD
Rebecca S. Carlin, MD
Lindsay A. Carnes, PA-C
Lisa M. Carroll, MD
Ralph E. Carter, III, MD
Michael C. Casciello, MD
Sarah H. Cash, MD
Caroline F. Chamberlain, PA-C
Paul S. Chang, MD
Leon D. Charkoudian, MD
Samuel J. Chewning, Jr., MD, MBA
Vernon S. Chiu, MD
Jennifer H. Christenbury, PA-C
C. Franklin Church, MD
Adriana I. Cline, MD
Kenneth K. Cloninger, MD
Brian S. Coan, MD
G. Glenn Coates, MD
Alexandra V. Cobo, PA-C
Samuel B. Collins, MD
L. Gregg Colvin, MD
Jason T. Combs, MD
Kellie S. Condra, MD
Neil A. Conti, MD
Orlando Conty, MD
David H. Cook, MD
Jeffrey J. Cook, MD
William C. Corbett, MD
Evan S. Corey, MD
William M. Cottrell, MD
Christopher T. Coughlin, MD
Mark M. Couture, MD
Christopher K. Craig, PA-C
Gary P. Cram, Jr., MD
William F. Credle, Jr., MD
E. Brown Crosby, MD
Kenneth Crosby, Jr., MD
David B. Crosland, MD
Cesar P. Cube, MD
Michael J. Cullura, DO
James L. Cummings, MD
Richard E. Cummings, MD
Richard C. D'Alonzo, MD
Manish N. Damani, MD
Louis B. Daniel, Jr., MD
Evan F. Dapo, PA-C
Kimberly A. Darlington, PA-C
Harlan B. Daubert, MD
Robert N. Davis, MD
German D. De Joya, MD
Joseph M. DeBord, MD
Adrian Deese, MD
David Defeo, MD
Stephen D. DeMeo, DO
Andrew C. Demmert, MD
Dawn E. DeNeef, MD, FACS
Christopher M. DeRienzo, MD, MPP
Lindsey M. Deschamps, MD
W. Roger Domby, MD
Andrew J. Doorey, MD
Kristen M. Dorsey, MD
W. Rodwell Drake, Jr., MD
Matthew J. Duggan, MD
Jack N. Dunn, MD
Elizabeth A. Eagle, MD
Wesley S. Eagle, PA-C
Demetri M. Economedes, DO
Tally H. Eddings, III, MD
David B. Eddleman, MD
Brian E. Edwards, MD
R. Elizabeth Edwards, PA-C
Howard J. Eisenson, MD
Laura T. Ekka, MD
Luke A. Elliott, MD
Daniel W. Entrikin, MD
Jonathan M. Epperson, MD
Shanti P. Eranti, MD
Stephen D. Ertischek, MD, FACP
John A. Fagg, MD
Peter A. Fenn, PA-C
E. Carl Fisher, Sr., MD
Timothy S. Fitzgerald, PA-C
Keri A. Fitzsimmons, MD
George E. Fleming, MD
Damon A. Forbes, MD
Charles W. Ford, Jr., MD
Chad M. Fortun, MD
Sharon M. Foster, MD, FAAP
William B. Fowler, MD
Douglas G. Freeman, Jr., MD
Keisha L. French, MD
Amanda M. Froment, MD
Mark K. Fromke, MD
Sam R. Fulp, MD
Parker M. Gaddy, MD
Angela B. Gantt, MD, FACOG
Idalina Garcia-Hruby, MD
Alyssa W. George, MD
Nizar M. Ghuneim, MD
Hannah M. Gilbert Brame, PA-C
Jordan M. Glaser, MD
Lauren D. Golding, MD
Donald B. Goodman, Jr., MD
John P. Goodson, MD
Karyn B. Gordon, MD
Hugh J. Grant, Jr., MD
Benjamin T. Gravatt, MD
Gretchen E. Green, MD
Robert L. Green, MD
Paul R. Greenlaw, MD
Kyle F. Grimaldi, MD
Matthew M. Grove, DO
Joseph Guarino, MD, MPH, FACOEM
G. Patrick Guiteras, MD
James C. Gunnells, MD
Rachel H. Hagler, MD
C. Michael Hahn, MD
W. Dana Haithcock, Jr., MD
Brent D. Hall, MD
Jennifer J. Hall, MD
Nady Hamid, MD
P. J. Hamilton-Gaertner, MD, MHA
Michael G. Hankewycz, MD
Mark A. Hansman, MD
Norris B. Harbold, Jr., MD
Rita A. Harbury, PA-C
C. Blair Harkness, MD
James S. Harrington, MD
Allan B. Harvin, MD
Elizabeth H. Hawes, PA-C
Rodney J. Hawk, MD
William L. Haynes, MD
Gary H. Heck, DO
Joseph R. Hedgpeth, MD
Hughes M. Helm, MD
Robert C. Helms, MD, FAAP
William C. Helton, MD
Katherine A. Hemby, MD
David F. Henderson, PA-C
Nancy S. Henley, MD, FACP
Lloyd A. Hey, MD, MS
John M. Hicks, MD
Tammy L. Hilbert, MD
James R. Hodges, MD
Katrina J. Hodgkins, PA-C
Jeremy J. Hoff, DO
James R. Hoffman, DO
Rachael B. Hollifield, DO
James P. Hooten, Jr., MD
Heather M. Hopper, PA-C
Andrew R. Hordes, MD
Fatima Hossain, MD
Mahmood H. Hosseinian, MD
William A. Hough, III, MD
John D. Howard, MD
Joshua R. Howell, MD
G. V. Huffmon, III, MD, FACS
James D. Hundley, MD
Dori L. Hunt, MD
Sarah O. Hunt, MD, FAAP
Gary J. Hunter, DO
Joe P. Hurt, MD, PhD
J. Mark Hylton, Jr., MD
Jennifer A. Ingersoll, MD
Peter L. Jacobson, MD, FAAN
Astrid G. Jain, MD
W. Bryan Jennings, DO
Grace M. Jere, MD
Edward W. Jernigan, III, MD
Liangyong Jiang, MD
Nneka T. Jimoh, MD
Albin W. Johnson, MD
Gregory J. Johnson, MD
James C. Johnson, MD
Lynn R. Johnson, MD
Randall D. Johnson, MD
Sara G. Johnston, PA-C
Jerry D. Joines, MD
Jamande A. Jones, MD, MS
Jason D. Jones, MD
Perrin W. Jones, MD
Timothy D. Jordan, MD
Michael Josilevich, MD
Raymond E. Joyner, MD
Ki S. Jung, MD
Robert H. Kahn, MD
Charlotte K. Karriker, MD
Alison S. Kavanaugh, MD
Arthur E. Kelley, MD
R. David Kemp, MD
Scott A. Kendrick, MD
Zachary J. Kimball, MD
Kevin Z. Kinlaw, MD
Jennifer Kipp
Hayden P. Kirby, MD
Megan D. Kirk, MD
Nathan R. Knapp, MD
Mary Faison G. Knox, MD
Dibas Koirala, MD
Keith R. Kooken, MD
Aaron C. Kopp, PA-C
Labkhand Kossari, MD
Edward W. Kouri, MD
David A. Kovach, II, MD
Harald H. Kowa, MD, FAAP
Eric M. Kraus, MD, MS
Larry L. Kroll, MD
S. Richard Kruse, MD
Anirudha P. Kulkarni, DO
Archana Kumar, MD
William A. Kutner, Jr., MD
Patrick W. Laber, MD
Leta Sue C. Lamb, MD
William A. Lambeth, III, MD
Philip O. Lamptey, MD
Ronald W. Lane, MD
Stephen N. Lang, MD
Grainger S. Lanneau, MD
Kurt K. Lark, MD
Marzena T. Laszewski, MD
Lindsay R. Lavin, MD
William W. Lawrence, Jr., MD
Daniel A. Leach, MD
Il S. Lee, MD
W. Hampton Lefler, Jr., MD
Aaron P. Leininger, MD
Anthony P. Leonard, MD
Kathleen C. Leone, MD
Jason M. Licht, PA
Arthur J. Lim, MD
Meredith S. Linger, PA
Scott W. Lisson, MD, FACS
Bryan J. Loeffler, MD
Kevin J. Logel, MD
R. E. Lombard, MD
Alexandra G. Lorentsen, MD
Katie Lowry, MD, MPH
Yuan Lu, MD
Brittany D. Macon-Davis, PA-C
Jonathan A. Malin, MD
Erik A. Manring, MD
Arie Mantin, MD
Monica A. Manzi, PA-C
Kenneth C. Marburg, MD
Patrick S. Markwalter, MD
William T. Mason, MD
Carolyn H. Maynor, MD
Daniel E. McBrayer, Jr., MD
Benjamin W. McClintock, MD
Diana C. McClinton, MD
Mark W. McClure, MD, FACS
Shannon M. McCrann, DO
Brooks W. McCuen, II, MD
David L. McCullough, MD
Leah H. McGuire, PA-C
Christina S. McOwen, PA-C
Megan S. Melendez, PA-C
Thomas E. Melin, MD
Douglas F. Messina, MD
Catherine D. Metheney, MD
Kathleen L. Meyer, PA
David C. Miller, MD
Horace W. M. Miller, IV, MD
Howard E. Miller, MD
James T. Mills, Jr., MD
Thomas H. Milner, III, MD
William W. Mims, III, MD
Challie A. Minton, MD
Robert C. Moffatt, MD
Mohamed K. Mohamed, MD
Babak Mokari, DO
William G. Moorefield, Jr., MD
Edgar S. Moser, Jr., MD
Erinn M. Murphy, DO
Ellis F. Muther, MD
Angela N. Nash, PA-C
Morgane E. Naveau, MD
J. Gregory Nelson, MD
Jessica E. Newman, PA-C
Leon B. Newman, MD
Mai Trang L. Nguyen, MD
Michael A. Nichols, MD, PhD
Jerry D. Nix, MD, FACEP
John R. Nixon, MD
Thomas L. O'Connell, MD
Christopher W. Olcott, MD
Dale W. Oller, MD
Marci L. Olsen, PA-C
Jacob A. Orbock, MD
Sarah R. Orlousky, MD
T. Lane Ormand, MD
Nahla A. M. Osman, MD
Michael R. Ott, MD
Robert A. Ottaviani, MD
Dawn P. Owens-Watterson, DO
Sarah E. Owrey, MD
A. T. Pagter, Jr., MD
Frederick V. Palmquist, MD
Gupta Pandarinath, MD
Steven T. Pantelakos, MD
Young K. Park, MD
Anand R. Patel, MD
Jayesh K. Patel, MD, FACC
Nilesh P. Patel, MD
Nirali M. Patel, MD
Shiv S. Patel, MD
David R. Patterson, MD
James B. Patterson, MD
Joseph R. Payne, MD
E. Louis Peak, MD
Thomas E. Pendergrast, MD
A. Thomas Perkins, IV, MD, PhD
Randy A. Peters, MD
Kirk A. Philpot, MD
Maria E. Picton, MD
Isadore M. Pike, MD
Steven R. Plunkett, MD
William G. Porter, MD
James M. Potts, MD
Josie D. Prabhakar, PA-C
M. Canaan Prater, DO
Philip A. Price, PA-C
Jeffrey Probst, PA-C
William R. Purcell, MD
Joseph P. Pye, MD
Megan E. Quigg, PA
Rachel E. Raab, MD
Evelyn A. Rabindran, MD
Wanda L. Radford, MD
Gary T. Raflo, MD
Sonya C. D. Randazzo, MD
Ashley R. Rawls, PA-C
Lawrence W. Raymond, MD, FACP, FACOEM
Eileen M. Raynor, MD, FACS, FAAP
Kelli A. Reardon, MD
Lynn M. Rebello, MD
William C. Rice, MD
Kenneth J. Rich, MD
James J. Richard, PA
Robert D. Richards, MD
Jill R. Roberson, MD
Tia L. Robertson, MD
Stefanie M. Robinson, MD
David A. Rockwell, MD
Danielle M. Rose, MD
Eric R. Rosenberg, MD
Shepherd F. Rosenblum, MD
Charles E. Rowe, Jr., MD
Pinakpani Roy, MD
John Rubino, MD
Alfred J. Rufty, Jr., MD
Samuel B. Ryburn, MD
Smita N. Sampat, MD
Fernando A. Sanchez-Brugal, MD
Shiraz M. Sandhu, DO
Melanie B. Sanford, MD
Shireesha Sangineni, MD
Rujuta T. Saraiya, MD
Wade H. Saunders, III, MD
Kenneth J. Sauve, MD
Dawson E. Scarborough, MD
Kerri R. Scherer, MD
Thomas M. Schmelzer, MD
Derek Q. Schroder, MD, FACP
Beth A. Schulz-Butulis, DO
Christopher J. Schwarz, MD
Fred A. Scialabba, MD
Stephen S. Scott, MD
Whitney V. Scott, MD
John M. Seddon, MD
John Aldus Alexander Seldomridge, MD
Frank B. Sellers, MD
Linda C. Selsor, MD
Pierre S. Selwane, MD
Joshua P. Sesek, MD
Daniel P. Seward, MD
Christopher I. Shaffrey, MD, FACS
Kerry M. Shafran, MD
Christopher N. Shatley, PA-C
Michael P. Shea, MD
Lisa P. Shock, DrPH, PA-C, MHS
Douglas J. Shusterman, MD
Tiffany M. Sills, MD
Lawrence R. Singer, MD
Maggie L. Small, PA-C, MHS
Timothy H. Smelzer, MD
Brian S. Smith, MD
Julian K. Smith, PA-C
Mark D. Smith, II, MD, FACS
Melissa M. Smith, MD
Michael K. Smith, MD
Patricia W. Smith, MD
Amy H. Sobel, MD
Anna Melissa Solum, MD
Lewis C. Sommerville, III, MD
Krichna F. Sowles, MD
Kevin M. Spangler, MD, PhD
John M. Spargo, MD
Jeffrey D. Sparks, MD
Nathaniel L. Sparrow, MD
Steven C. Spruill, MD
Jeffrey D. Stanczak, MD
Richard R. Stark, MD
Peter M. Stein, MD
Michael J. Steiner, MD
Holly A. Stevens, MD, FACOG
James A. Stevens, Jr., MD
Jeremy R. Stinson, PA-C
Scott C. Stoioff, MD
Lauretta G. Stombaugh, DO
Woodhall Stopford, MD, MPH
Ananta Subedi, MD
Brittany A. Sugimoto, PA-C
Ernest O. Sutton, III, MD
Thomas M. Swantkowski, MD, AGAF, FACG
Jonas J. Swartz, MD
Brian T. Szura, MD
Karen D. Szymanski, DO
Munther S. Tabet, MD
Julia W. Tang, MD
Charles S. Tara, MD
Gregory J. Taraska, MD
Anna Greta B. Taylor, MD
Robert D. Teasdall, MD
Robert K. Thacker, MD
Thomas E. Thielen, MD
Alan E. Thomas, MD
C. Aaron Thompson, MD
Marilu Thordsen-Velez, MD
Richard W. C. Tim, MD
Kathryn S. Timberlake, MD
Kenneth G. Tomberlin, MD
Andres H. Torop, MD
Nancy J. Toy, MD
Nicholas A. True, MD
John T. Tseng, MD
Harrison G. Tuttle, MD
Bhavna Vaidya-Tank, MD
Lionel Van Der Westhuizen, MD
Jaime J. Vanourny, MD
Jill S. Vargo, MD
Mihaela A. Vatca, MD
Wayne B. Venters, MD
Thomas T. Vradelis, MD, FACOG
Tomas Vybiral, MD
Jason A. Walker, MD
Antoinette W. Wall, MD
Bobby C. Walters, Jr., MD
W. Alan Ward, MD
L. Patrick Warren, Jr., MD
Sean M. Warsch, MD
H. Gene Washburn, MD
Michael C. Watson, Jr., MD
Peter R. Watson, MD
Shannon A. Watterson, PA-C
John C. Watts, III, MD
David A. Weatherford, MD, FACS
Michael D. Weaver, MD
Martin W. Webb, MD
Richard A. Weintraub, MD, FACP
Gregory M. Weiss, MD
Andrew H. Wells, MD
Susan M. West, MD
Carl J. Westcott, MD
Melissa K. Wester, MD
Trent W. Wester, MD
Kenneth S. White, MD
Edward W. Whitesides, MD
Daniel Whitley, Jr., MD
Judson B. Williams, MD
Michael L. Williford, MD
Danielle L. S. Willis, PA-C
Jason A. Wilson, MD
Gabriel B. Winberry, MD
Nancy C. Winker, MD
James E. Winslow, MD
James W. Winslow, MD
Kenneth H. Winter, MD
Joel A. Wissing, MD
Peter H. Wittenberg, MD
Brian S. Wood, PA-C
Kully L. Woodruff, MD
Julie C. Woodside, MD
Vanessa S. Workman, MD
David K. Wright, MD
Genevieve A. Wroblewski, MD
Che-Ming Yang, MD
Joylyn D. Yeazell, MD
Billie T. W. Yi, PA-C
Terri L. Zacco, DO
Peter A. Zeman, MD
Chunyue Zhang, MD
Li Zhou, MD
Shams Zia, MD
James H. Zuger, MD
Charles S. Zwerling, MD
Interested in an NCMS Leadership Role? Nominations are Now Open!

The NCMS Nominating and Leadership Development Committee submits a call for nominations for individuals to serve on the following: NCMS Board of Directors, NC American Medical Association Delegation, and Nominating and Leadership Development Committee.
Get the details and learn more about the nomination process here.
For more information or questions about the nominating process, please contact Evan Simmons at [email protected]
Nominations are due by May 12, 2023
Have You Read Your NCMS Bulletin: 2022 Year in Review? We Sure Hope So. Prizes Are On The Line!

It's NCMS Bulletin: 2022 Year in Review Trivia Time!
We sure hope you've read your NCMS Bulletin! Why? Because you could win an awesome prize simply by answering the following question:
What is the age of our youngest member?
The first five people to respond to today's NCMS Bulletin: 2022 Year in Review Trivia Question will win a special gift from the NCMS!
Good luck!
We Need You! Become a Key Contact for NCMS.

Do you have a relationship with an elected official or want to grow your involvement in NCMS’s advocacy efforts? Become a Key Contact!
Key Contacts are subject matter experts who will champion for every physician, physician assistant, and patient in North Carolina. The relationships they build with State and Federal legislators are vital for continuing the advocacy success of the North Carolina Medical Society.
In order for NCMS to have effective advocacy, we need each of you to sign up to become a Key Contact now!
UNC Gillings Study Shows Effectiveness of Updated Bivalent Boosters

In a study published in The New England Journal of Medicine, researchers at the University of North Carolina’s Gillings School of Global Public Health found that bivalent boosters are more effective than original monovalent boosters at preventing COVID-19-related hospitalization and death.
“We were able to evaluate not only the effectiveness of the two bivalent booters but also compare their effectiveness to that of monovalent boosters.” [source]
Learn more about the research and findings here.
NCMS & NCMGMA Present: Legislation, Expectations and Advocacy, Oh My!

Join us for the February 2023 Webinar:
Legislation, Expectations and Advocacy, Oh My!
Tuesday, February 21, 2023 | 12:00 pm to 1:00 pm
featuring
The NCMS Legislative Advocacy Team
Your NCMS and NCMGMA invite you to join in as we take a look at what to expect in the 2023 legislative session in North Carolina, and how it may impact your practice and patients.
The key objectives for this webinar are:
- Review the 2022 election results and how they impact your practice and patients
- Introduce you to the 2023 advocacy agenda
- Highlight bills that have been filed (so far) and what to expect
- Put a spotlight on where your advocacy efforts are needed and how
Presented by the North Carolina Medical Society Foundation in partnership with the North Carolina Medical Group Management Association
This webinar is free but you must be registered to attend.
Space is limited so register early!
***After you register, you will receive an emailed confirmation with the webinar link and phone-in instructions. Please check your spam/junk folder if you do not see the confirmation email after you register.***
Our Presenters
Thomas Kincheloe
NCMS Director of Legislative Affairs

Alan Skipper
NCMS Vice President of External Affairs
HASP Should Be on Your Radar! Here's why.

The Healthcare Access and Stabilization Program (HASP) is a reimbursement program for hospitals that have experienced financial losses.
Administered by the Centers for Medicare and Medicaid Services (CMS), HASP will reimburse hospitals at a rate closer to the cost of care. Through HASP, health systems may receive up to $1.8 billion in federal dollars to care for patients covered by Medicaid. [source]
Read the full article here for more details.
Member Spotlight: Eric Morse, MD

NCMS member Dr. Eric Morse was presented with the Nyswander/Dole “Marie” Award at the 2022 AATOD national conference in Baltimore, MD.
The Nyswander/Dole “Marie” Award, is a tribute to those individuals who have been nominated and selected by their peers for extraordinary service in the opioid treatment community.
Dr. Morse recently opened his ninth Opioid Treatment Program in North Carolina, the Morse Clinic of Durham, and is only the second North Carolinian to win the award.
The NCMS and its membership congratulates Dr. Morse!
Back in Session! See The Bills That Could Impact You and Your Patients.

The NC General Assembly is officially back in session. Last Wednesday started with bills which could impact you and your practice.
Three bills were filed in the house and senate in attempt to codify Roe v. Wade and the Senate starts off the year by revisiting Medical Cannabis in North Carolina.
Here is a look at some important legislation as we begin the 2023 long session.
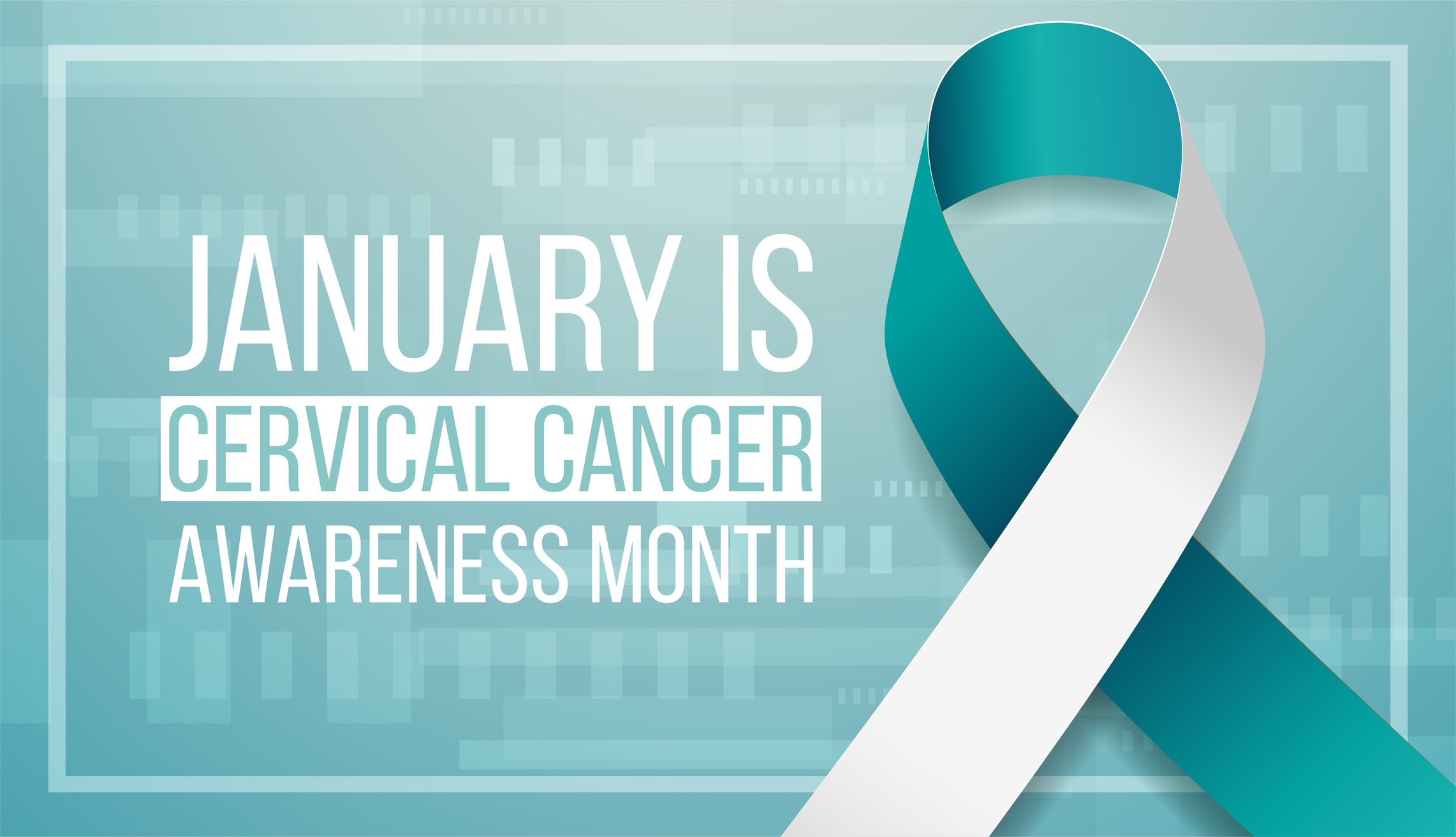
January is Cervical Cancer Awareness Month

The bad news: Each year more than 350 North Carolina women are diagnosed with cervical cancer and over 100 die from the condition. The majority of these deaths occur in women over age 45. The good news: When cervical cancer is found early, it is highly treatable.
Certain types of human papillomavirus (HPV) is the main cause of cervical cancer. HPV is a common virus that is passed from one person to another during sex. At least half of sexually active people will have HPV at some point in their lives, but few women will get cervical cancer.
Some warning signs of cervical cancer are:
Abnormal vaginal bleeding
Increased vaginal discharge
Pelvic pain
Pain during sexual intercourse
Cervical cancer occurs most often in people over age 30 and can affect anyone with a cervix.
Screening tests and the HPV vaccine can help prevent cervical cancer.
See the CDC's wealth of information on cervical cancer here.
Huge Kudos to Atrium Health!

Atrium Health announced that more than 200 of their physicians have been named to SouthPark Magazine Top Doctors in the Charlotte area – more than any other health system in the region.
The list represents physicians in 49 specialties who were selected by their peers with a goal of saluting the area’s leading medical practitioners.
View this impressive list here.
The NCMS congratulates Atrium Health and its physicians on this great accomplishment!
Could Your Patient's Weight Alter the Effects of Vitamin D Supplements?

A new study suggests overweight individuals might not reap the health benefits from taking Vitamin D supplements.
Researchers found a 30% to 40% reduction in cancer, cancer deaths and autoimmune diseases among people with a lower body mass index (BMI) who took vitamin D supplements, but only a small benefit among those with higher BMIs.
"Patients with obesity, despite taking the same amount of supplement, had a lower response," said lead researcher Deirdre Tobias, an assistant professor in the department of nutrition at the Harvard School of Public Health, in Boston. [source]
Read more about the study and its findings here.
Want to Better Your Patient's Brain Function? Get Them Moving.

A study published in the Journal of Epidemiology and Community Health found that skipping exercise in favor of sitting can worsen brain function.
During the study, participants underwent a series of tests that assessed their ability to process and recall information. After analyzing the participants' activity data, the researchers found that those who skipped exercise in favor of eight minutes of sedentary behavior saw 1% to 2% decreases in their cognition scores.
More details on how to help your patients are here.
Could Bird Flu Eventually Pose a Human Threat?

Avian influenza has led to the deaths and culling (the organized, systematic segregating of organisms from the rest of the group because they don't possess desired characteristics) of more than 300 million chickens, ducks and geese and an unknown number of wild birds between 2005 and 2021.
North America is in the midst of the worst outbreak on record.
“There is concern about it having pandemic potential,” says Wendy Blay Puryear, a molecular virologist at Tufts University. “Before Covid was on anybody’s radar, this was the one that we were all watching very closely.” While the virus is currently considered a low risk to humans, she also states: "But anything that has the ability to replicate and evolve rapidly, and anything that has that ability to infect a lot of different hosts is kind of on borrowed time." [source]
Want more details? Read the full article here.
Attention Spans are Shrinking. Here are Tips to Stay Focused for Your Patients!

Dr. Gloria Mark, a professor of informatics at the University of California, Irvine, studies how digital media impacts our lives. In her new book, she explains how decades of research has tracked the decline of the ability to focus.
“In 2004, we measured the average attention on a screen to be 2½ minutes,” Mark said. “Some years later, we found attention spans to be about 75 seconds. Now we find people can only pay attention to one screen for an average of 47 seconds.” [source]
If you have more than 47 seconds available, read the full article here!
A New Prescription Perk for Your Amazon Prime Patients

If you have patients who are Amazon Prime subscribers, their membership just got a little better!
Amazon recently announced a prescription benefit for U.S. Prime members. The new perk, RxPass, will allow Prime members to get as many drugs as they need from a list of 50 generic medications used to treat more than 80 common conditions, including high blood pressure, anxiety and diabetes.
The add-on service costs $5 a month per person, and delivery is free.
Learn more about the program here.
Member Spotlight: Jeane Ashley Marsh, MD

Meet Fellow NCMS Members in Our Member Spotlight!
Take your turn in the spotlight! See the bottom of this story for more information.
1. What is a quote that has significantly influenced your life and why?
“Carpe diem.” It's an oldy, but goody. Life isn't promised, and if you don't live your life now, you may not get the chance to do it tomorrow.
2. Where are you from?
Morehead City, NC.
3. Why did you decide to become a physician?
I wanted to help people. I was working as a paramedic and wanted to do more than triage patients. I wanted more of a long term follow through.
4. What do you like about practicing in an underserved area?
I like that I'm taking care of neighbors and friends. It is great when I go to the store and see families that I've taken care of through pregnancy and the postpartum period.
5. Is your practice using any tools to address social determinates of health for patients?
We have started a program where we give food bags to any patients who need them. This is in collaboration with ECU.
6. What impact has the Covid-19 pandemic had on your practice and what are some of the changes you have made.
It changed the way we work up sick patients and it helped us create a telehealth system that is still working well for us and patients.
7. Do you have any hobbies or activities for self-care?
I like to ride my bike, hike, and garden.
If you would like to be featured in our Member Spotlight, please complete the form here.
In Memoriam: NCMS Lifetime Member George C. Debnam, MD

Lifetime NCMS member George C. Debnam, MD, died January 19, 2023. He was 95.
Dr. Debnam joined the North Carolina Medical Society in 1971. He practiced medicine for over 50 years in Raleigh. Trained in family practice, he provided general medical care, obstetrics and some surgery. He was cited by the Governor for being the physician to deliver the most babies ever in the state of North Carolina - over 10,000.
Starting his practice at Saint Agnes Hospital, the segregated facility for African American citizens of Raleigh, Dr. Debnam was historic in the integration of Raleigh's health care. He was the first physician to admit patients to the new integrated Wake Medical Center (then Wake Memorial Hospital) when it opened.
Dr. Debnam was the recipient of many awards and was nationally recognized for his contributions to healthcare in 1977 when he was named Physician of the Year by the National Medical Association.
The staff and membership of the North Carolina Medical Society extend our deepest condolences to Dr. Debnam's families and friends.
Read Dr. Debnam's full obituary here.
COVID-19 Infection May Induce Fetal Brain Hemorrhages

Evidence has shown COVID-19 in fetal brain tissue in instances of pregnant people passing the infection to their children.
Long before now, scientists have been exploring the effects on the bodies of still-gestating babies.
A study of 661 human fetal tissue samples collected between July 2020 and April 2022--observing hemorrhages in 26 of them--revealed COVID-19 to be present in all of the tissue samples with evidence of hemorrhaging.
Get more details on this research here.
CDC: Child Vaccination Rates Steadily Declining

According to new data from the federal Centers for Disease Control and Prevention, instead of child vaccination rates recovering (after the first year of the COVID-19 pandemic) the historically low rates worsened.
Data show the percentage of U.S. children entering kindergarten with their required immunizations fell to 93% in the 2021-22 school year, 2 percentage points below recommended herd immunity levels of 95% and lower than vaccination rates in 2020-21, when many schools and doctor’s offices were closed.
Public health officials warn that unless child vaccination rates for measles, chicken pox, polio and other diseases are quickly brought back to pre-pandemic levels, outbreaks of preventable diseases — like the measles outbreaks in Ohio and Minnesota in the fall and the polio case in New York last summer — are likely to become commonplace. [source]
The full article can be found here.
Is Leadership Development Among Your Goals for 2023?

If Leadership Development is among your 2023 goals, check out the Health Care Management & Leadership program offered by the North Carolina Medical Society/Kanof Institute for Physician Leadership and join an amazing peer network of alumni!
Health Care Management & Leadership (HCML) focuses on the business side of medicine in both the FFS and value-based world of healthcare.
Read more about the program here.
JAMA Pediatrics: New Tool May Help Identify Cerebral Palsy in Infants Sooner

According to a study published in JAMA Pediatrics, a new prognostic tool may help identify infants with cerebral palsy (CP) earlier, allowing them to receive therapies to improve later outcomes.
Researchers from Canada used 12 clinical variables to predict the condition. The tool accurately predicted 75% of CP cases.
The bedside tool weighs factors such as the use of illicit drugs and tobacco by the mother, the presence of diabetes and preeclampsia during pregnancy, whether the infant is male, birth weight, and the number of miscarriages the mother had prior to the birth. The tool also factors in results from a test that measures how well the infant is adjusting to life outside the womb. [source]
Read the full article here.
New Poll Shows Widespread Support for NC Medicaid Expansion

A new poll shows widespread support for North Carolina expanding Medicaid coverage to more people.
The poll, released by the American Cancer Society Cancer Action Network (ACS CAN), found 78 percent of North Carolina voters support Medicaid expansion. Additionally, 96 percent of Democrats are in favor, with 71 percent of unaffiliated voters and 64 percent of Republicans as well. [source]
Read the full article here.
Provider Funding Opportunity: Closing the Medicaid Coverage Gap
The Kate B. Reynolds Charitable Trust is interested in efforts to educate the public about the opportunity to close the Medicaid coverage gap. The Trust will support communication campaigns to educate people who would benefit most from expansion, as well as key stakeholders such as providers, first responders, and local business leaders.
Learn more and apply here.
Effective Immediately: SAMHSA No Longer Accepting NOIs.

Section 1262 of the Consolidated Appropriations Act, 2023 (also known as Omnibus bill), removes the federal requirement for practitioners to submit a Notice of Intent (have a waiver) to prescribe medications, like buprenorphine, for the treatment of opioid use disorder (OUD). With this provision, and effective immediately, the Substance Abuse and Mental Health Services Administration (SAMHSA) will no longer be accepting NOIs (waiver applications). [source]
All practitioners who have a current DEA registration that includes Schedule III authority, may now prescribe buprenorphine for Opioid Use Disorder in their practice if permitted by applicable state law ... continue here for full details.
UNC Project Addresses Crisis of Physician Stress

A new set of 12 recommendations for hospitals and health care institutions addresses moral stress in clinical practice and the ways that it impedes good care. The recommendations for hospital leaders across the country come from the Study to Examine Physicians’ Pandemic Stress (STEPPS), a project of the University of North Carolina at Chapel Hill and The Hastings Center. [source]
Learn more and get the full list of STEPPS research insights and their accompanying recommendations here.
Leadership College Alum Talks Medicine/Public Health Partnership to Fight Diabetes
Read an article penned by NCMS member Dr. Bonnie Coyle, highlighting the importance of partnerships to combat Diabetes.
Dr. Coyle is a preventive medicine and lifestyle medicine specialist, medical director at the Mecklenburg County Health Department, and one of six physician champions statewide for the National Diabetes Prevention Program (DPP).
Medicare: Comment Period Open for CY 2024 Changes

Medicare Program; Contract Year 2024 Policy and Technical Changes to the Medicare Advantage Program, Medicare Prescription Drug Benefit Program, Medicare Cost Plan Program, Medicare Parts A, B, C, and D Overpayment Provisions of the Affordable Care Act and Programs of All-Inclusive Care for the Elderly; Health Information Technology Standards and Implementation Specifications.
Proposed policy and technical changes for Contract Year (CY) 2024 to Medicare Advantage Program, Medicare Prescription Drug Benefit Program, Medicare Cost Plan Program, Medicare Parts A, B, C, and D Overpayment Provisions in the Affordable Care Act and Programs of All-Inclusive Care for the Elderly (PACE); Health Information Technology Standards and Implementation Specifications
Comments are due by Monday, February 13, 2023.
View the Fact Sheet here.
View the Federal Register here.
Time-Restricted Eating. Could It Be Beneficial To Your Patients?

A study published in the journal Cell Metabolism suggests time-restricted feeding (TRF) — also known as time-restricted eating (TRE) when it applies to humans — was found to have effects on gene activity in mice.
According to Shereen Jegtvig, a nutritionist and author who teaches at the University of Bridgeport in Connecticut, time-restricted eating is a common form of intermittent fasting (IF), which involves eating only during specific hours of the day and fasting for the rest of the time.
Authors of the study noted that TRE/TRF has previously been shown to have multiple potential benefits for human health and has shown to prevent, better manage, or in some cases reverse several health conditions: glucose intolerance, insulin resistance, hypertension, dyslipidemia, fatty liver disease, chronic inflammation, sleep disorders, age-dependent declines in cardiac function and can also help with weight loss because it reduces the amount of time that you can eat.
The full article can be read here.
Give Your Input on a New NCSP Educational Conference

The North Carolina Society of Pathologists (NCSP) is pleased to announce a unique and unprecedented collaborative effort, involving all four NC academic pathology departments, to create a continuing education meeting open to all medical laboratory professionals- Timely Topics in Pathology: Tools to Empower the Modern Laboratory Professional
To best meet the needs of this diverse audience, the NCSP planning committee created a short survey to gauge the overall interest for this type of meeting and topic areas for potential inclusion.
We hope you will support this effort by participating in this very short anonymous survey – State Laboratory Meeting Survey
Atrium Health and WFUSM Celebrates a First in Charlotte

Charlotte is the nation’s largest city without a four-year medical school; however, this will soon change.
On Tuesday, January 17, Atrium Health and Wake Forest University School of Medicine celebrated the groundbreaking for the first four-year medical school in the Queen City.
The school of medicine will anchor the Howard R. Levine Center for Education in the heart of The Pearl, the surrounding innovation district. It will be joined by Carolinas College of Health Sciences, which has announced plans to locate there, along with connections to Wake Forest’s School of Professional Studies and School of Business and other educational opportunities. Wake Forest University School of Medicine Charlotte – the second campus of the school of medicine, based in Winston-Salem – is expected to seat its first class in 2024 and open the following year. [source]
Read more about this exciting news here.
Congratulations, Atrium Health and Wake Forest University School of Medicine!
The Changing Face of Fentanyl-Related Deaths

According to the Families Against Fentanyl organization's website, Fentanyl is now the number one cause of death for Americans aged 18 to 45, with the illicit drug killing 187 Americans every day. Sadly, deaths involving illicitly manufactured fentanyl are on the rise. The organization's THE CHANGING FACES OF FENTANYL DEATHS Fact sheet sheds light on the ongoing crisis.
In North Carolina, death certificates don’t have a specific code for fentanyl’s involvement in a drug overdose. There is a code – T40.4 — for “other synthetic narcotic overdose.” The Epidemiology, Surveillance and Informatics unit of the NC Division of Public Health’s Injury and Violence Prevention Branch notes that most of these cases are “due to illicitly manufactured fentanyl and fentanyl analogues,” but can also include prescription fentanyl and other, less potent synthetic narcotics like Tramadol.
An analysis of statistics from the NC Office of Chief Medical Examiner finds overdose deaths with that code went from 442 in 2016 (the first year for which the office had such statistics) to 3,163 in 2021 — an increase of 616%. [source]
AMA State Advocacy Summit – Dr. Shannon Dowler Featured Presenter

The American Medical Association held its annual State Advocacy Summit this past week, which featured NC Medicaid chief medical officer, Dr. Shannon Dowler, as a presenter. Dr. Dowler provided an overview of NC Medicaid’s experiences and lessons learned over the span of the pandemic.
Additional topics covered at the State Advocacy Summit included:
• Support of physician wellness
• Reproductive health care after Dobbs
• Scope of practice – Evidence to drive health policy
• Engaging state departments of insurance
• Competition and antitrust policy
• 2023 Congressional horizon
• Reforming prior authorization
• Addressing the nation’s overdose and death epidemic
Dr. Dowler reviewed the transition from in-person to telehealth care encounters, the pandemic’s impact on adult and pediatric behavioral health service use, and the disparity of telehealth services provided by race and patient location.
The Summit annually provides an opportunity for the AMA to convene with state and national medical associations to address state level legislative issues and strategies.
Could An Artificial Pancreas Help Improve Blood Sugar Levels?

New research suggests that fully closed-loop insulin therapy may help people with type 2 diabetes improve blood glucose levels without raising their risk of severe hypoglycemia, or dangerously low blood sugar.
Researchers evaluated the CamAPS FX® Android app, which functions as an artificial pancreas by integrating a continuous glucose monitor (CGM) with an insulin pump to automate blood glucose testing and insulin delivery.
Read more about this research here.
Help your patients prevent or delay progression to diabetes by referring them to a CDC-recognized National Diabetes Prevention Program (National DPP) lifestyle change program, like DiabetesFreeNC.
DiabetesFreeNC, a statewide initiative to help prevent Type 2 Diabetes, lets physicians and care teams support their patients who have prediabetes with a free or low cost, evidence based National Diabetes Prevention Program.
Learn more about the initiative and take the pledge by clicking here.