What Primary Election Results Mean for NCMS Members

The results are in. What comes next?
Throughout the electoral process, the North Carolina Medical Society (NCMS) remains vigilant in political engagement to advance our health policy priorities. The Society is engaging with candidates across the state and closely monitoring outcomes, focusing on candidates supported by NCMS.
The top-of-ballot results saw President Joe Biden and former President Donald Trump secure victories, setting up a rematch of the 2020 election. In North Carolina, Attorney General Josh Stein and Lieutenant Governor Mark Robinson both prevailed in what will be a nationally-watched gubernatorial showdown in November.
A trend emerged in North Carolina, with physician candidates demonstrating significant success in State House races. NCMS members Drs. Timothy Reeder, Grant Campbell, and Ralph Carter all navigating competitive primaries to secure victories. This highlights the increasing influence of medical professionals in both local and state politics. Dr. Reeder now faces Renee Kempner, Dr. Campbell is running against Joanne Chesley, and Dr. Carter faces longtime State Representative Garland Pierce.
The influence of physician candidates also extends to the State Senate level with NCMS member Dr. David Hill running unopposed as a Democrat in District 7, securing an automatic advancement to the General election. Retired Physician Assistant Mark Hollo also secured a victory for the Republican nomination in District 45. Hollo is a former member of the NC House. These developments underscore the growing presence of medical professionals in shaping state-level policies supported by the continuing advocacy of the NCMS and its members.
At the Federal level, the success of NCMS member candidates remains evident. Drs. Greg Murphy and Steve Feldman advanced automatically in their unopposed Congressional House primaries. Republican Dr. Murphy is the incumbent and Dr. Feldman is pursuing his first foray into elected office as a Libertarian. Their candidacies demonstrate the increasing recognition of the need for the medical profession to aid in shaping Federal policy that impacts NCMS members and patients in North Carolina.
The primary election showcases a dynamic political landscape, marked by significant voter engagement and the rising influence of physician and physician assistant candidates. As the 2024 electoral process progresses, the North Carolina Medical Society will continue to engage with these and other candidates and advocate for policies that prioritize the well-being of all North Carolinians.
The NCMS congratulates these member candidates for making a professional and personal commitment to run for public office. They reaffirm the vital role of healthcare professionals in shaping the future.
NCDHHS Places Important Focus on Sickle Cell Disease with Federal Partnership
With approximately 6,800 people in North Carolina suffering with sickle cell disease, the North Carolina Department of Health and Human Services (NCDHHS) intends to increase access to new therapies through the Cell and Gene Therapy (CGT) Access Model.
The Cell and Gene Therapy (CGT) Access Model aims to improve the lives of people with Medicaid living with rare and severe diseases by increasing access to potentially transformative treatments.
Cell and gene therapies have high upfront costs but have the potential to reduce health care spending over time by addressing the underlying causes of disease, reducing the severity of illness, and reducing health care utilization.
Initially, the model will focus on access to gene therapy treatments for people living with sickle cell disease, a genetic blood disorder that disproportionately affects Black Americans.
NCDHHS has updated a white paper it issued in December when the U.S. Food and Drug Administration approved the historic therapies named Casgevy and Lyfgenia, which are now available on the market. In clinical trials, both therapies were found to reduce or completely eliminate the extreme pain crises experienced by people living with sickle cell disease.
For additional information on the Cell and Gene Therapy Access Model, see the fact sheet and CGT model page.
Related Reading:
U.S. Set to Approve First Gene-editing Treatment for Sickle Cell Patients
FDA Approves Amivantamab as First-Line Lung Cancer Treatment
The Food and Drug Administration (FDA) has approved amivantamab-vmjw (Rybrevant, Janssen Biotech, Inc.) with carboplatin and pemetrexed for the first-line treatment of locally advanced or metastatic non-small cell lung cancer (NSCLC) with epidermal growth factor receptor (EGFR) exon 20 insertion mutations, as detected by an FDA-approved test.
The FDA also granted traditional approval to amivantamab-vmjw for adult patients with locally advanced or metastatic NSCLC with EGFR exon 20 insertion mutations, as detected by an FDA-approved test, whose disease has progressed on or after platinum-based chemotherapy. FDA previously granted accelerated approval for this indication.
Read the full article here.
New NC Food Program Will Feed Children Over the Summer

Expected to provide food for nearly a million school children this summer
Food and nutrition security means having reliable access to enough high-quality food to avoid hunger and stay healthy. Improving access to nutritious food supports overall health, reduces chronic diseases, and helps people avoid unnecessary health care. That’s why food and nutrition security is one of the key social determinants of health, according to the Centers for Disease Control. A new program in North Carolina is expected to provide food for nearly a million school children this summer.
The North Carolina Department of Health and Human Services (NCDHHS), in partnership with the North Carolina Department of Public Instruction, has announced its intent to administer the U.S. Department of Agriculture's new Summer Electronic Benefits Transfer (S-EBT) Program known as "SUN Bucks."
"Food is foundational to health," said NC Health and Human Services Secretary Kody H. Kinsley. "The SUN Bucks program will help relieve kids' hunger, support their health and promote the ability for them to learn."
Get all the details on this beneficial program here.
Free Community Wellness Event in Greensboro This Saturday

J. Douglas Galyon Depot
234 East Washington Street
Downtown Greensboro
Saturday, March 9
10:00 a.m. to 2:00 p.m.
Cone Health is partnering with Downtown Greensboro, Inc. to provide a free community health screening event on Saturday, March 9, from 10:00 a.m. to 2:00 p.m. at the J. Douglas Galyon Depot located at 234 East Washington Street.
Free blood pressure and blood sugar screenings will be offered at the event. There will also be team members on hand to provide patient education and health resources, including information about where to receive care in the community.
Super Tuesday Results and What They Mean for NCMS

Super Tuesday Results Are In.
What Does That Mean For You?
The North Carolina Medical Society has several member candidates for both state and federal office. Over the past several months, many of them have answered questions important to NCMS members. So what happened?
 On Friday, The NCMS Vice President of Advocacy, John Thompson, will have an analysis of the results and the impact they have on the next several months.
On Friday, The NCMS Vice President of Advocacy, John Thompson, will have an analysis of the results and the impact they have on the next several months.
Look for his report in Friday's edition of Morning Rounds.
AMA Center for Health Equity: Applicants for Medical Justice in Advocacy Fellowship Needed
The AMA Center for Health Equity seeks applicants for the Medical Justice in Advocacy Fellowship program’s 2024-2025 cohort. The program is administered through a partnership between the AMA and the Morehouse School of Medicine’s Satcher Health Leadership Institute.
Using an anti-racist, equity-centered learning framework, fellows engage with equity experts and trailblazers. The fellowship equips and empowers fellows to be part of the next generation of advocacy leaders, driving meaningful policy and structural changes that produce equity and justice in the communities they serve.
Application deadline is April 1, 2024.
Duke, UNC Hospitals Ranked in Top 100 in Nation

Newsweek Ranks Duke, UNC Hospitals Top in Nation
DURHAM, N.C. (WNCN) — Duke University Hospital in Durham has been recognized as one of the top medical centers in the country in 2024.
Newsweek magazine, in partnership with Statista, has released its annual rankings of the world’s best hospitals, with an overall global list as well as ones divided by country.
Duke University Hospital comes in at No. 16 on the list of the best hospitals in the United States, the highest ranking of any hospital in North Carolina. The medical center is also on the list of top 250 hospitals worldwide, ranking at No. 68 globally.
While Duke University Hospital is the only one in North Carolina that ranked globally, several others from around the Triangle made the list of best in the country.
Two UNC-system hospitals ranked in the top 100 — UNC Rex Hospital in Raleigh at No. 71, and UNC Medical Center in Chapel Hill at No. 79.
Another Durham facility, Duke Regional Hospital, comes in at No. 143. Also ranking in the top 200 is FirstHealth Moore Regional Hospital in Pinehurst at No. 171.
Newsweek lists two more Triangle hospitals among its list of the 412 best in the U.S. — UNC Health Johnston in Smithfield (No. 333) and Duke Health Raleigh (No. 408).
The rankings were put together using data from online recommendation surveys taken by medical professionals as well as patient satisfaction surveys, hospital quality metrics and patient-reported outcome measures, or PROMs. [source]
NC Hospital to Host Colorectal Health Lunch and Learn
Harris Regional Hospital in Sylva will host a special “Lunch and Learn” opportunity focused on colorectal health on Thursday, March 21st from noon – 1:00 p.m.
The event, which will be held in the Easton Board Room on the first floor of the hospital, will be led by general surgeon Gilberto Robles, MD, who will share his expertise on the importance of maintaining colorectal health, including prevention, screenings, warning signs, and more.
The event is open to the public and individuals who have questions about colorectal health are encouraged to attend. Lunch will be served at the event and dietary preferences can be accommodated.
For questions or to register for the event call 828.631.7429.
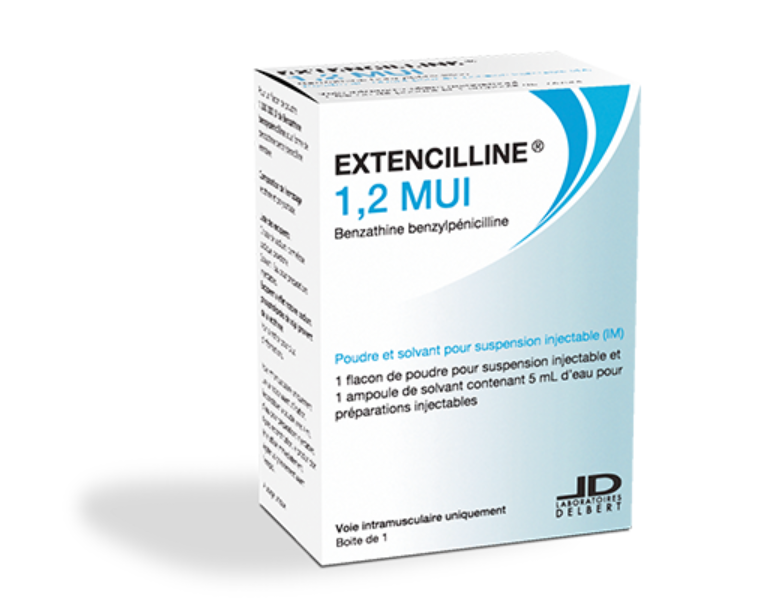
NC Medicaid will now cover imported benzathine benzylpenicillin for syphilis
A message from Elizabeth Cuervo Tilson, MD, MPH, State Health Director and Chief Medical Officer of NC Department of Health and Human Services:
Dear Colleagues:
NC Medicaid will now cover imported benzathine benzylpenicillin (Extencilline) for use in outpatient medical drug claims. This new coverage is being added to address the ongoing national shortages of Bicillin® L-A (penicillin G benzathine injectable suspension).
While we have not heard of major shortages in North Carolina, we wanted to ensure that providers had access to every tool that may be available.
The statement on the policy change is available at https://www.ncdhhs.gov/news/press-releases/2024/03/04/ncdhhs-releases-statement-state-health-director-dr-elizabeth-cuervo-tilson-increasing-access
Provider guidance on extencilline is available at https://dailymed.nlm.nih.gov/dailymed/drugInfo.cfm?setid=5a026d0c-6f91-4ee3-b193-b2186a37e7ca
More detailed information on Medicaid billing is available at NC Medicaid to Cover Imported Benzathine Benzylpenicillin (Extencilline): Billing Guidelines | NC Medicaid (ncdhhs.gov)
First Over-the-counter Birth Control Pill Will Be Available Later This Month

More than 50 years after the oral contraceptive pill went on the market in the United States, the country's first over-the-counter birth control pill will be available in stores and online nationwide later this month.
Known as Opill, the birth control pill will be available without prescription necessary in major retailers and pharmacies nationwide in late March, the drug's maker, Perrigo, announced Monday.
"People have a new choice, a new option to access the oral contraceptive pill without a prescription," said Contraceptive Access Initiative (CAI) Co-founder Dana Singiser.
The medication will cost $19.99 for a one-month supply and $49.99 for a three-month supply in stores. Online customers can buy Opill at Opill.com for $49.99 for a three-month supply and $89.99 for a six-month supply. Patients may begin pre-ordering the drug from select stores as of this week.
Read full article here.
Related Reading:
FDA Approves First Over-the-counter Birth Control Pill
FDA Advisers Vote Unanimously in Support of Over-the-Counter Birth Control Pill
Capitol Chronicle: North Carolina Neurologists Take to The Hill

On February 27, 2024, a delegation of neurologists from North Carolina visited Capitol Hill to advocate for some key issues impacting medicine. Their day, which included stops at each of our state’s Senate and House offices, focused on:
Medicare – Reversal of the 3.37% cut in physician payment
Medicare – Updating the physician payment formula to allow for an annual inflationary adjustment
Step Therapy – Relief from insurers’ unsubstantiated delays in approved care
Research – Funding to help advance research and therapies for treating neurologic diseases
The Washington, DC fly-in was hosted by the American Academy of Neurology and North Carolina’s advocates included:
Robert Armstrong, MD
Asheville Neurology Specialists / Asheville
Zahra Cain-Akbar, DO
Harnett Health / Wade
Amy Guzik, MD, FAAN
Atrium Health Wake Forest Baptist / Winston Salem
Casey Jeffreys, MD
Raleigh Neurology / Raleigh
Maria Minor, MD
Duke University Medical Center / Durham
W. Alan Skipper, CAE
NC Medical Society & NC Neurological Society / Raleigh
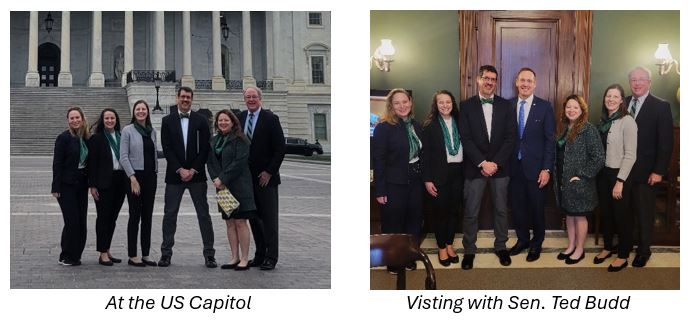
We need you!
Join us for in-district meetings with North Carolina members of Congress. If you would like to be included in a meeting with your member of Congress, please let us know by email.
Today is Super Tuesday! Your Voice, Your Vote. Be Heard!

Today is Super Tuesday! Find your location and voting hours here: Primary Election (PDF).
The North Carolina Medical Society has several members running for state and federal offices. Here are your fellow members who are on the ballot:
Grant Campbell, MD – NC House – 83
www.campbellfornc.com
Ralph Carter, MD – NC House – 48
www.ralphcarterforhouse.com
Mary Ann Contogiannis, MD – US House – NC6
www.drmaryannforcongress.com
David Hill, MD – NC Senate – 7
www.hillforncsenate.com
Greg Murphy, MD – US House – NC3
www.murphy4congress.com
Tim Reeder, MD – NC House – 9
www.drtimreeder.com
Over the past two months, some members have made the journey to Raleigh to sit down and answer questions submitted by NCMS members. View the 2024 Candidate Series videos here.
NCMB Issues Call for Physician, PA and NP Candidates
Applicants are needed for two physician seats, one physician assistant (PA) seat and one nurse practitioner (NP) seat on the North Carolina Medical Board for terms beginning November 1.
All positions must be filled by the process set down in statute (N.C. Gen. Stat. 90-2 and 90-3), which requires interested parties to apply via the Review Panel for the North Carolina Medical Board. The Review Panel is an independent body that nominates candidates for consideration by Governor Roy Cooper. By law, the Review Panel must nominate two candidates for each open seat.
One physician seat and both advanced practice provider seats are currently occupied by individuals who are eligible for reappointment. However, incumbents must apply for reappointment via the normal application process.
Applications will be accepted online through 4:45 p.m. on Thursday, June 27. For more information visit this website.
The Review Panel will consider only physicians (MDs or DOs), PAs and NPs who hold active, unrestricted NC medical licenses. Applicants must be actively providing patient care at least part time and must have no history of disciplinary action within the past five years.
Make an Impact! Secure Your Spot at the NCMS Advocacy Summit Today!

Don't Miss the upcoming NCMS Advocacy Summit This Month!
Don’t forget to register for the NCMS Advocacy Summit - a gathering of healthcare leaders and policy experts dedicated to fostering meaningful discussions around legislative developments crucial to our profession. The event is March 23rd, so register now as space is limited!
Why Attend?
- Stay informed about critical legislative changes affecting your practice.
- Equip yourself with effective communication strategies for impactful advocacy.
- Network with fellow healthcare professionals and policy experts.
- Play a pivotal role in shaping the future of healthcare in our state.
We are confident that your participation in the NCMS Advocacy Summit will not only enrich your understanding of legislative landscapes but also empower you to make a tangible impact on behalf of your patients and the healthcare profession.
McKimmon Center
1101 Gorman Street
Raleigh, NC 27606
March 23, 2024
9:00 AM-5:00 PM
Secure your spot at this influential summit here.
Register Now for the "All Politics is Local" Advocacy Webinar
All Politics is Local: How Engaging Local & State Officials Can Aid Your Congressional Advocacy Efforts
March 13
8pm ET
This AMA Very Influential Physician event will explore the benefits of connecting, interacting, and building personal relationships with state and local legislators. Tracy Mattison Brandon, a current Town Commissioner in Davidson, NC, and Beatrice Lanzi, a former Rhode Island lawmaker with 20 years tenure in the state Senate and House, will share their experiences as elected officials.
Hear how constituents made impressions, both positive and negative, on these public officials; what members of their communities did to endear themselves to these legislators; and, how their roles as local and state government officials were intertwined with the work of their members of Congress.
Space is limited. Be sure to register early.
CDC Recommending Additional Covid-19 Vaccine for Those Over 65

New Guidance From CDC on Vaccines for the Elderly
Arund 98% of the US population has some kind of immunity to Covid-19, whether from infection, vaccination, or both, according to the CDC. But health experts say this only gives some protection against infection or severe disease. In response, the CDC this week recommended people age 65 and older should get an additional dose of the current Covid-19 vaccine. The current Covid-19 vaccine, which was updated last fall, is considered highly effective and may cut the chances of getting a symptomatic infection by half. This comes as the CDC is considering a shift to its Covid-19 isolation guidance to say that people no longer need to isolate once they have been fever-free for 24 hours and their symptoms are mild or improving.
68-Year-Old Man Now in HIV Remission

(NiceNews.com) -- When Paul Edmonds learned he had AIDS in 1988, he viewed it as a death sentence. But therapies helped him take control of the illness for more than three decades — and now he’s in full-blown remission, all thanks to a cancer diagnosis.
Blood cancers are common in older HIV patients, according to the cancer center City of Hope, where Edmonds, pictured on the left with husband Arnold House, was treated for his leukemia. In 2019, he received a transplant of stem cells that had a rare genetic mutation that causes HIV resistance.
As a result, he became the fifth person in the world to be cured of leukemia and reach HIV remission, a milestone recorded earlier this month in a study published by The New England Journal of Medicine. Of those five people, Edmonds, 68, is the oldest and had HIV for the longest period, 31 years.
Though he initially kept his identity anonymous, Edmonds went public with his journey last year. “A big reason I want to tell my story is to bring some hope for people with HIV,” he said at the time. “And I want to remember all those we lost"
Hear Paul in his own words
WSJ: DOJ launches an antitrust probe into UnitedHealth Group

(Yahoo Finance - Seana Smith, Brad Smith) -- Department of Justice (DOJ) officials have launched an antitrust probe into the relationship between UnitedHealth Group's (UNH) insurance division and its Optum health services segment, according to Wall Street Journal reporting.
Yahoo Finance Health Reporter Anjalee Khemlani breaks down the details, highlighting the other challenges UnitedHealth is facing.
For more expert insight and the latest market action, click here to watch this full episode of Yahoo Finance Live.
Editor's note: This article was written by Luke Carberry Mogan.
Video Transcript
BRAD SMITH: Shares of UnitedHealth under pressure this morning after the US Department of Justice reportedly kicks off an antitrust investigation into the company's relationship between its insurance unit and health services arm, according to the Wall Street Journal. For more on this, we've got Yahoo Finance's Anjalee Khemlani here with us with more. Hey, Anj.
ANJALEE KHEMLANI: That's right, guys. Hey. Yeah, this report not surprising a lot of people who have either, you know, looked at United's strategy before, or those who are former employees. We've actually spoken to some of those folks ourselves here at Yahoo Finance.
And I'll say that some of the things listed in this report, including what the relationship is between the two sides, and whether or not the company is inflating costs and inflating claims from one side to the other, really touches on some points of concern that others have had over the years, especially as Optum has grown to be the largest, or one of the largest, employers of physicians. So really setting up the company for a hard look. And it is not a very good year for United.
If you take a look back in the past year, not only did they recently have that cyber attack on their Change Healthcare subsidiary, but they also are facing a class-action lawsuit for denying claims through AI for elderly Medicare Advantage members. So, it really has been a tough year for the company when it comes to a lot of the different moving parts of it. And it's interesting that this is the thing that has really hit the stock.
But what the results of that probe will be, of course, we will have to see. But I've heard over the past several months that, basically, what has happened is, you know, there has been looking like inflation of the business that Optum has done over time, making it look like a really strong growth company when really it was just one side of the company funneling to another. So, will be interesting to see if those claims pan out.
SEANA SMITH: And it's a story we are going to continue to track. Again, UnitedHealth under pressure, off just nearly 4% here.
Additional Reading
2024 NCMS Candidate Series - Ralph Carter, MD

2024 NCMS Candidate Series Featuring Dr. Ralph Carter
The 2024 North Carolina Medical Society Candidate Series has an exclusive interview featuring Dr. Ralph Carter, who is running for North Carolina House District 48. In this episode, Dr. Carter outlines what motivated him to run for office and his most important legislative issues. He is passionate about bringing jobs to his district, improving education in District 48, fighting against government health mandates, and his strong support for pro-life policies.
All candidates who are members of NCMS and are running for either state or federal office have been extended invitations to articulate their perspectives on these crucial subjects. Stay tuned for forthcoming interviews with other candidates leading up to the November election.
See the full interview with Dr. Carter here:
https://youtu.be/eybBCn9yN9o
Eight ECU Brody School of Medicine Students Named to FCLC

(ECU News Service) -- Noor Baloch, Nolan Davis, Michael Denning, Charles Johnson, Hannah Rayala, Emmalee Todd, Ben Wise and Michael Wright will join students from other colleges and universities across the state who are interested in leadership and professional growth.
“The FCLC program provides us with a unique, structured ability to engage with our future colleagues on community-level projects that address the varied landscape of health, health equity and health care,” Denning said. “Gaining intense leadership training alongside other health professions students will allow me both introspection and outward reflection on my future role, as well as mechanisms to ensuring our patients are excellently and compassionately cared for.”
Prospective students are referred and nominated to the program by faculty, mentors and others at their respective colleges. The 2024 class includes 27 students representing disciplines including medicine and pharmacy from ECU, UNC Chapel Hill and Duke, Campbell, Wake Forest, Western Carolina and Wingate universities in North Carolina, as well as St. Georges University in Grenada.
FCLC is a partnership with North Carolina Area Health Education Centers (NC AHEC) to provide opportunities of leadership in an interprofessional health care environment and networking across institutions. The one-year program is designed to enhance health care experience through advocacy, change-driving and individual leadership skills.
Baloch said she wants to be a leader when it comes to ensuring proper care for her patients.
“I felt that in order to be the best leader I could be, I needed additional training alongside other health care professionals to really understand my role as a physician in a health care team as well as establish how I can best serve my patients in that way,” she said. “Through this program, I am able to understand my own leadership style as well as my faults so that I can work on them and ensure I am self-aware regarding how I lead interactions with my patients.”
The program emphasizes leading in interprofessional health care environments and networking across institutions. The interactive learning format encourages participants to engage with their peers and program leaders, faculty and speakers. They also participate in a project that gives them exposure to some of the major health policy challenges relevant to North Carolina.
“This is an incredible opportunity for these eight students to work with other interprofessional students across the state to develop the skills necessary to be a leader in health care tomorrow,” said Dr. Amanda Higginson, Brody’s associate dean for student affairs. “We know our Brody graduates go on to do amazing things; this wonderful program will further develop these students to both improve the health and well-being of the region, but also to augment the already great training they receive here to prepare them to become physicians who will meet the health care needs of the state, both critical mission goals of the school.”
The students will have hands-on experience cultivating leadership skills including team-leading, communication and career development.
“The purpose is to build leadership that centers on self-awareness and fosters authenticity that allows each student to act in alignment with their core values as a leader, encourage and assess information from different perspectives, and balance transparency,” according to the program website. “With the individual core as a foundation for leadership development, this course prepares students for the leadership journey, allowing the individual to establish a strong sense of purpose and understanding of who they want to be as a leader.”
Todd said the nature of medicine as a “team sport” necessitates the ability to collaborate with other health care professionals at any given time.
“In order to do this, it’s important to understand your own teamwork preferences and leadership style and be able to refine them to better suit your purposes,” she said. “I believe my participation in FCLC is providing me the opportunity to do exactly that, which will hopefully lay the groundwork for not just my own success in residency and beyond, but the success of the health care teams of which I will be part.”
Todd said the unique experience to explore a current health-related policy issue in North Carolina is valuable because it gives students a chance to propose potential solutions.
“So much of what impacts our patients’ health are factors that we can’t necessarily do anything about within a half-hour annual physical — their housing situation; the ease of their transportation to work or school; the accessibility of nutritious food, clean water and green space where they live,” she said. “Working towards policy change is one way that physicians can make an impact on these broader societal factors, and it’s something that I would like to be involved in throughout my career. FCLC is equipping me with the experience and skillset I need to begin to pursue this goal.”
NCMS CEO Chip Baggett is excited for the new students. "Helping create the next generation of leaders in North Carolina is one of the core missions of the North Carolina Medical Society," says Baggett. "These eight new students will be ready to face the rapidly evolving world of healthcare and safeguard the quality of patient care for years to come. The KIPL Leadership College Program is a nationally renowned curriculum that will foster these student's leadership skills and help them build a network in the healthcare community. I look forward to meeting them and seeing how they impact the future."
Michael Wright and Hannah Rayala also serve on the NCMS Student Council.
For more information on NCMS Professional Growth programs click here.
Happy Birthday to Our Members Celebrating This Month!
Grab your party hats and noisemakers and let’s celebrate!
Robert B. Abrahams, DO
Yousef S. Abumostafa, MD
Stephen J. Acosta, MD
Jeffery A. Adams, MD
Mia R. Adkins, MD
Mamatha Agrawal, MD
Mahmood G. Aijazi, MD
Lysle K. Ailstock, MD
Raul C. Aizcorbe, MD
Muhammad S. Alam, MD
Kira M. Alatar, MD
Kyle A. Alexander, MD
Kimberly A. Alford, MD
Hassan Alhosaini, MD
David J. Allison, MD
D. Kevin Allred, PA-C
Ishwari S. Amin, PA-C
Rakesh D. Amin, MD
David T. Anderson, MD
Vincent C. Andracchio, MD
Nicole E. Aristy, MD, FAAP
Robert F. Armstrong, MD
Melanie R. Artho, MD
Michael S. Artman, MD, FAAP
Adedayo O. Ashana, MD
Arthur Axelbank, MD
Malick V. Bachabi, MD
J. Russell Bailey, MD, FACC
Donald W. Bales, Jr., MD
Stephanie L. Balkman, PA-C
James D. Ball, MD
Edwin C. Bartlett, Sr., MD
Edgar H. Batcheller, Jr., MD
Shayne E. Bates, MD
Alan S. Baumgarten, MD, MPH
Jeffrey S. Beecher, DO
Nana A. D. Benneh, MD
Christiana J. Bernal, MD
Joe D. Bernard, MD
Gregory M. Bertics, MD
Margaret L. Bertrand, MD
Navin C. Bhojwani, MD
Preecha Bhotiwihok, MD, MPH
George A. Binder, MD
Richard E. Bird, MD
John P. Birkedal, MD
Taylor M. Bishop, PA
Jeffrey R. Blackburn, MD
Jamie E. Bleyer, MD
Zachary T. Blom, MD
Hannah E. Boghosian, PA-C
Jeffrey Borders, MD
Jared B. Bowns, MD
Ker Boyce, MD, FACC, FACP
Brian A. Boyd, MD
Robin Boyd-Kranis, MD
Tyler C. Bradley, PA-C
Ashley J. F. Brandon, MD
Andrew R. Brant, MD
Lori C. Bridges, PA-C
George M. Brinson, MD
Thomas E. Brock, MD
Brian K. Brodwater, MD
Jeffrey A. Brody, MD
Bradley J. Broussard, MD
Cynthia J. H. Brown, MD
Jared W. Brown, MD
Rebecca H. Brown, MD
Richard F. Bruch, MD
Matthew J. Bruehl, MD
Vardaman M. Buckalew, Jr., MD
Philippe I. Bulauitan, MD
Donald K. Bulla, PA-C
Joseph M. Bumgarner, MD
Edwin K. Burkett, MD
Aaron M. Burman, PA-C
D. Patrick Burney, MD
Merle R. Busby, MD
Parag Butala, MD
Jerome M. Butler, Jr., MD
Brian R. Cabarrus, MD
Elaine S. Cabinum-Foeller, MD, FAAP
Dwayne D. Callwood, MD
Bernard C. C. Campo, PA-C
Gerald W. Capps, MD
Thomas K. Carlton, Jr., MD
Dennis D. Carmichael, MD
Laurel E. Carter, MD
Margaret F. Carter, MD
Steven R. Carter, MD
Virginia F. Casey, MD
N. Daniel Catz, MD
Margaret E. K. Champion, MD
John S. Chang, MD
Sarah J. Chapman, PA-C
Danielle N. Chavis, PA-C
Dev R. Cheti, MD
John C. Childress, III, MD
Mohan M. Chilukuri, MD
Katherine E. Chockley-Nystrom, PA-C
Christina H. Choe, MD
Michele M. Clancy, MD
Robert E. Clark, MD, PhD
Jim R. Cleary, MD
David A. Clements, II, MD
Margaret R. Clifton, DO
H. Leslie Clinton, Jr., MD
Timothy E. Cloninger, MD
Michael R. Coan, MD
Joseph A. Coladonato, MD
Ann S. Collins, MD
Dana D. Copeland, MD
Donald L. Copeland, MD
Mark W. Cornelius, MD
Alexandra F. Covington, PA
Michael A. Cowan, MD
Karen D. Coward, MD
Kirsten S. Cox, MD
James S. Coxe, III, MD
William L. Craig, III, MD
Benjamin Craighead, MD
Larry M. Crane, MD
Adam C. Creech, MD
Matthew A. Creighton, MD
Lori K. Crihfield, DO
Daniel L. Crocker, MD
Charles C. Crowell, III, MD
John B. Crudup, III, MD
Nathan S. Cuka, MD
Edith R. Curry, MD
Richard F. Curtis, MD
Thomas L. D'Alessio, MD
Michael B. Daley, MD
Julie Daniel, DO
Laura F. Danile, MD
Stephen M. David, MD
John D. Davis, Jr., MD
Jeffrey R. Daw, MD
Troy C. Dawley, DO
Lindsey E. de Guehery, MD, FACP
Gary J. DeFilipp, MD
Bridget M. Degele, MD
Derek W. DelMonte, MD
William T. Derry, MD
Maureen Despres, MD
Crystal M. Dickson, MD
Robin Dimitrious, MD
Steven A. Dingeldein, MD
Robert M. Doline, MD
Shannon B. Dowler, MD
Shannon M. Drohan, MD
Douglas A. Drossman, MD
Elizabeth D. Dryden, PA-C
Josiah W. Duke, MD
Melissa B. Duncan, MD
Thaddeus L. Dunn, MD
Allyson P. Dupay, PA-C
Michael R. Duran, PA-C
Sarah K. Dusel, PA-C
Daniel P. Dwyer, MD
H. Shelton Earp, III, MD
E. Stephen Edwards, MD
George S. Edwards, Sr., MD
Kent R. Edwards, Jr., MD
Vance H. Edwards, MD
Bryan A. Ehlert, MD
Carl J. Eisenberg, MD
Mohamed T. El-Kara, MD
Justin D. Ellis, PA-C
Sherif O. El-Mahdy, MD
Shandal S. Emanuel, MD
J. Mark Englehardt, MD
Paul N. Erckman, MD
Heath B. Ergas, MD
John M. Erickson, MD
Vaishali G. Escaravage, MD, FAAD
William M. Eubanks, Jr., MD
Uzma S. Faheem, MD
William L. Fangman, MD
John C. Faris, MD
Robert A. Ferguson, DO
Daniel H. Fertel, MD
Nicholas J. Fitzsimons, MD
Gitanjali M. Fleischman, MD
Herbon E. Fleming, MD
Joseph P. Flynn, DO
Adam W. Fosnaugh, MD
John D. Franklin, MD
Earl A. Frantz, DO
Lynn Marie Fraser, MD
Darrell W. Freeman, MD
Jon E. Fromke, MD
Elaina K. Furr, DO
Robert H. Gaither, MD
Lance M. Garber, MD
Michael L. Garner, MD
John W. Garrett, MD
Timothy M. Gast, PA-C
Matthew P. Geib, DO
Mathew George, MD
Wood B. Gibbs, MD
Kathleen Gibson, MD
Herman A. Godwin, Jr., MD
Kyle T. Golden, DO
Jason F. Goldie, MD
Barbara L. Goldman, PA-C
H. Ronald Gollberg, MD
Tristan Gonzalez Sanz, MD
Allison C. Gordon, PA-C
Daniel S. Gordon, MD
Hormoze A. Goudarzi, MD
Matthew R. Grafenberg, MD
William M. Gramig, III, MD
David Josip Grasic, MD
Patrick D. Green, MD
Thomas M. Green, Jr., DO
Chad C. Greer, MD
Amardeep S. Grewal, MD
Amy M. Griffin, MD
John P. Grimm, MD
Sarah R. Grossman, MD
Kelly R. Grove, DO, FAAP
Leah M. Gruber, PA
Mark J. Gruchacz, MD
Marc F. Guerra, MD
Alison P. Guptill, MD
Shauna L. Guthrie, MD, MPH
Amy Guttmann, MD
Jason C. Haag, MD
Trevor Hackman, MD
Jeremy M. Hackworth, MD
Elizabeth Hagenmaier, DO
Brian H. Hamilton, MD
Gene T. Hamilton, MD
Douglas I. Hammer, MD
Jonathan A. Hancher, MD
Charin L. Hanlon, MD, FACP
Perry M. Harmon, MD
Willard C. Harrill, MD, FACS
James A. Harris, MD, FACS
Tina G. Harris, MD
David L. Harshman, MD
Omer A. Hassan, MD
Robert E. Hassler, MD
Michael W. Hauser, MD
James H. Hawkins, Jr., MD
Seth C. Hawkins, MD
Sherman M. Hawkins, Jr., MD
Yasmin Heater, MD
Kathryn J. Hecker-Magee, MD
William D. Heizer, MD
Joel H. Heller, MD
George P. Henderson, Jr., MD
Richard R. Henderson, MD
Mark D. Henin, MD
Victoria M. Herriott, MD
Marc A. Herschelman, DO
David L. Hill, MD, FAAP
Shannon N. Hill, MD
Nancy M. Hill-Price, MD
Thomas R. Hinson, Jr., MD
Jason G. Ho, MD
Audrey J. Hockeborn, PA-C
Marcus A. Hodges, MD
Bennett R. Hollenberg, MD
Kevin D. Hollis, MD
Douglas K. Holmes, MD
Adrian W. Holtzman, MD
Andrea L. B. Honeycutt, MD
Janice R. Hong-Messier, MD
James B. Hooker, MD, MPH
William W. Hope, MD, FACS
Jeffrey J. Horvath, MD
Robert G. Howard, Jr., MD
William C. Hubbard, MD
Edward V. Hudson, MD
Michael B. Huggins, MD
Kathryn J. Hull Wood, MD
Megan A. Hunstad, PA-C
Jacklynn L. Hunt, PA-C
Karrar Husain, MD
Farah S. B. A. Hussain, MD
Odinaka G. Idada, PA-C, MHS
Lourdes Illa-Sanchez, MD
Isaac L. Jaben, MD
Kayla M. Jacobs, PA-C
William R. Jacobs, MD
Elizabeth G. Jarvis, MD
Casey V. Jeffreys, MD
Jerome E. Jennings, MD
Sarah C. Jernigan, MD
Jolene R. Jewell, MD
Andrew E. Johansen, MD
Charles S. Johnson, MD
Kenneth L. Johnson, II, MD
Kamlyn Jones, MD
Steven A. Josephson, MD, FACP
Patrick K. Jowdy, MD
Walton K. Joyner, Jr., MD
Beatriz E. Juncadella, MD, FAAP
Hassan Kahi, MD
Ciamack Kamdar, MD
Barry K. S. G. Kang, MD
Leonardo Kapural, MD, PhD
Kenneth S. Karb, MD
Stephen L. Kash, MD
Rachel Keever, MD, FACC
Mary K. Keith, MD
Jessica K. Kim, DO
Paul S. Kim, MD
Sarah Kim, MD
Seung W. Kim, MD
Stephen W. Kimmel, MD
Edgar W. Kirby, IV, MD
David Kirk, MD
Alvin P. Kitchin, Jr., MD
Bert J. Klein, III, MD
Steven D. Klein, MD
John T. Klimas, MD
Christine T. Knettel, MD
Gilliam J. Knox, MD
Margaret M. Kocsis, MD
Dennis D. Kokenes, MD
Aaron Kollross, MD
Amy M. Kornegay, PA-C, MPAS
Jonathan H. Kornegay, MD
Walter T. Koscielniak, III, MD, FAAP
Jeffrey M. Kotzan, MD
Bruce J. Kowalski, MD
Michael V. Krasnokutsky, MD
Ronald E. Krum, MD
Andrew J. Kubinski, DO, MS
Lydia E. Kuo-Bonde, MD
Jeffrey G. Kuremsky, MD
Robert S. Lackey, MD
Mallory C. Lake, PA-C
Venkatesh Lakshman, MD
Matthew J. Landfried, MD
David R. Lane, MD
Fred D. Lassiter, MD
Adeyemi A. Lawal, MD
Mary Katherine Lawrence, MD
Robert L. Lawrence, MD
Mary Lou Lawson, MD
Daniel P. Leas, MD
Choo H. Lee, MD
Daniel P. Lee, DO
Jinoo T. Lee, MD
Elizabeth R. Lemoine, MD
Julie V. Levengood, MD
Ronald H. Levine, MD
Frederic E. Levy, MD
Jay B. Levy, MD
Caroline H. Lewis, PA
Katherine M. Lewis, MD
Andrew I. Light, MD
Alexander J. Lim, MD
Roger Lim, MD
Chelsea W. Lindley, PA-C
Timothy L. Lockamy, DO
Hillary E. Lockemer, MD
Thomas T. Long, III, MD
William P. Lorio, MD
Jennifer M. Lovin, MD
Macie N. Lucas, PA
Donald T. Lucey, MD
Kondie L. Lykins, PA
Edward B. Mabry, MD
Damien C. Macaluso, MD
J. Alexis MacDonald, Jr., MD
Kevin A. MacDonald, MD
Graham L. Machen, MD
John P. Mahaney, Jr., MD
Alden B. Maier, MD, FACS
Anita M. Makowski, PA
Morton D. Malkin, MD
Michael S. Mallonee, MD
Peter G. Mangone, MD
Charles F. Marshall, Jr., MD
A. Michele Martin, MD
Charles R. Martin, MD
Matthew B. Martin, MD, FACS
Michael M. Marushack, MD
H. Benno Marx, MD
David P. Mason, MD, FACOG
Robert D. Matthews, MD
Lisa L. May, MD
Karen E. Mayer, MD
Bradley T. McCall, MD
Samuel G. McCaskill, Jr., MD
John T. McCormick, MD
Marion M. McCrary, MD, FACP
Gordon R. McDevitt, Jr., MD
John N. McDowell, MD
Barry D. McGinnis, MD
James S. McGrath, MD, MPH
Sheppard A. McKenzie, III, MD
Joseph T. McLamb, MD
Michael E. McLeod, MD
Thomas K. McMahan, MD
J. Eugene McMurry, Jr., MD
Ryan P. McWey, MD
Andrew M. Mealin, DO
Stephen J. Melson, MD
Matthew J. Merritt, DO
Jobe C. Metts, III, MD
Michael A. Meuse, MD
Q. Alexander Mewborn, Jr., MD
Karen V. Meyers, MD
Stephen C. Meyers, MD
Joel B. Miller, MD
Justin D. Miller, MD
Leona A. Miller, MD
Meagan P. Miller, PA-C
David D. Miner, MD
Richard W. Minielly, MD
Bonnie E. Minnick, PA-C
Ann Ree S. Mitchell, MD
Henry T. Mixon, MD
Mark B. Moeller, MD
Ali S. Mofrad, MD
Joseph A. Molitierno, Jr., MD
Michelle J. Moore, PA-C
Scott M. Moore, MD
Derek W. Moss, MD
Gregory J. Mosteller, MD, FACEP
Gary J. Mullen, Jr., MD
Robert L. Munt, Jr., MD
Gregory F. Murphy, MD, FACS
Sean M. Murphy, MD
Laura W. Murray, MD
Wissam E. Nadra, MD
Manjula Nagaraja, MD
Aswani S. Naidu, MD
Patrick J. Nailer, MD
Musharraf Navaid, MD
Shahla Naz, MD
Ronald J. Neimkin, MD
Matthew J. Newsome, MD
Chelsea K. Ngongang, MD
Nathaniel P. Nonoy, MD
Christopher J. Norbet, MD
Ray G. Norby, MD
Sylvanus W. Nye, MD
Tadhg J. O'Gara, MD
Ada T. Ogunsiakan, MD
Alfred E. Okeke, MD, FACE
Nicomedes G. Osalvo, PA-C
Jesse E. Otero, MD
Max M. Palatnik, MD
Jill M. Pappalardi, MD
Kinjal R. Parikh, DO
Norman H. Parks, MD
Laura A. Parra, MD
Cornelius T. Partrick, MD
Ann S. Pate, MD
Bhavesh B. Patel, MD, MBA
Bindit S. Patel, MD
Mahendra S. Patel, MD, FACP
Milan A. Patel, DO
Neha A. Patel, MD
Shil K. Patel, MD
Viral D. Patel, MD
Nadine Pechter, MD
Joshua J. Penninger, MMS, PA-C
Jennifer F. Pensado, DO
James R. Perrott, MD
James L. Perruquet, MD
Kirk D. Peterson, MD
Sommer E. Philips, MD
Wesley F. Phillips, MD
Andy Phung, DO
Michael J. Plakke, MD
George W. Plonk, MD
Edward T. Plyler, MD
George Podgorny, MD
John J. Poggi, MD
Ronald D. Polite, MD
Morris A. Pollock, MD
Frederick L. Potts, III, MD
Demetri T. Poulis, MD, FACS
Jess A. Powell, III, MD
Thomas G. Powers, MD
Claire M. Poyet, MD
Steven D. Prakken, MD
Jessica J. Prestwood, MD
David H. Priest, MD
Randall L. Proctor, Jr., MD
V. Watson Pugh, Jr., MD
Craig S. Purcell, PA-C
Matthew K. Rapp, MD
Eric Rappaport, MD
Michael G. Ribadeneyra, MD
John R. Rice, MD
Lucian C. Rice, Jr., MD
Donna M. Richardson, MD, MBA
R. Paul Rieker, Jr., MD
J. Wayne Riggins, MD
Rebecca C. H. Riley, MD
Kenneth M. Robert, MD
Surry P. Roberts, MD
Justin D. Rodriguez, MD
Kevin P. Rooney, PA-C
Manfred S. Rothstein, MD
Perry J. Roy, MD
Mary K. Rudyk, MD
Donald B. Russ, MD
Michael B. Russell, MD
Sarah D. Ryan, MD, FAAP
Isami Sakai, DO
Richard G. Saleeby, Jr., MD
Rodrigo T. Samodal, Jr., MD
Joseph L. Sampson, Jr., MD
Geetha Samuel, MD
John A. Sanchez, DO
Terry Sarantou, MD
Adam W. Saucerman, MD
Mariam S. Sauer, MD
Shannon M. Sawin, MD
Lauren A. Scarfo, PA-C
W. D. Schaefer, MD
Deanna M. Schantzen, PA-C
Charles P. Scheil, MD
Shadley C. Schiffern, MD
Herbert M. Schiller, MD
Gregory F. Schimizzi, MD
David M. Scholle, MD
Brandon W. Schoonover, PA-C
Amanda L. Schuman, PA-C
Curtis W. Schupbach, MD
Matthew W. Schwanke, PA-C
Joshua D. Schwartz, MD
Blake K. Scott, MD
Zeni Scott, MD
Daniel P. Seeburg, MD, PhD
Christian D. Selby, PA-C
John W. Sensenbrenner, MD
William D. Shaw, Jr., MD
Ronald B. Shealy, MD
Rashid A. Sheikh, MD
Kellie Shell, MD
Meredith L. Shillinglaw, PA
Amy J. Shipley, MD
Melissa F. G. Shipley, MD
F. Philip G. Singer, MD
Rajdeep Singh, MD
Adrienne H. Singleton, MD
Daniel J. Smith, MD
Todd C. Snyder, MD
Ralph Snyderman, MD
Michael F. Soboeiro, MD
Anjali Solanki, DO
Taylor R. Sorensen, PA-C
Andrea H. Sparr, PA-C
Amanda C. Spiritos, PA-C
David E. Spivey, Jr., MD
Daniel J. Stackhouse, MD
Ronald J. Stanley, MD
Joslin Stanton, DO
Anna F. Stephenson, PA-C
Sharon R. Stephenson, MD, FACOG
Wesley H. Stepp, MD, PhD
Joey S. Stevens, PA-C
Amy E. Stinson, DO
F. Keith Stirewalt, PA
Leon E. Stockton, MD
Jennifer K. Stoddard, MD
Taylor J. Stone, MD
Megan K. Straughan, MD
Jacob J. Subash, MD
Sara M. Suh, PA-C
R. Alan Summers, MD
John P. Surratt, MD
Carisa M. Sutherland, MD
Mark J. Sutherland, MD
Dylan J. Suttle, MD
Charlotte A. Sweeney, MD, FACOG
John T. Sweeney, MD
Charlie L. Sykes, Jr., MD
Michael G. Taggart, MD
Christopher P. Tanzie, MD
James A. Tart, MD
Syed T. Tasleem, MD
David H. Tate, MD
David T. Tayloe, Jr., MD, FAAP
Britton E. Taylor, MD
Jeffrey S. Taylor, MD
Paul L. Tenzel, MD
Antonia G. Tettamanti, MD
Vipul V. Thakkar, MD
Ronald L. Thiele, MD
J. Alexander Thomas, MD
Laura O. Thomas, MD
Corey A. Thompson, MD
Ricky A. Thompson, MD
Timothy A. Tolson, MD
Shannon K. Tomlinson, MD
Kevin M. Trapani, DO
Joseph E. Tripp, MD
Bradford A. Tyler, MD
Richard D. Ulstad, PA-C
Hiren M. Umrania, MD
Bailey H. Underhill, PA-C
Henry A. Unger, MD, FACS
Paul A. Vadnais, MD
Bradley S. Van Dyke, MD
William J. Vanarthos, MD
Jennifer Vande Loo, ATC, PA-C
Rajat Varma, MD
Irene Vasko, DO
Ronald J. Viola, MD
Paul E. Viser, MD
Joshua I. Vogel, MD
George M. Wadie, MD, FACS
Joshua A. Wallace, MD
Daniel B. Wallihan, MD
Matthew C. Ward, MD
Jeffrey D. Warden, MD
Alicia L. Warlick, MD
Raymond G. Washington, Jr., MD
Bradley J. Wasserman, MD, FAAP
Tyler S. Watters, MD
H. Boyd Watts, MD
William J. Weatherly, MD
Joseph J. Wehner, MD
James E. Weilbaecher, Jr., MD
Elizabeth S. Weinberg, MD, FACS
Carl L. Welch, MD
Earl P. Welch, Jr., MD
Kimberly E. Wells, MD
Mark G. Wertman, MD
Jennifer K. E. Whitham, MD
Donna J. Whitt, MD
Thomas B. Wiggins, MD
Aaron T. Wild, MD
E. Brooks Wilkins, MD
Kayleigh K. Williams, PA-C
Kristin R. Williams, MD
Rhoderick T. Williams, Jr., MD
William T. Williams, Jr., MD
Sarah B. Wilson, MD
Andrew Win, MD
Emily R. Wirt, PA-C
Benjamin Wise
Daniel E. Wise, MD
Colleen L. Wisnosky, PA-C
James C. Womble, MD
Michael G. Woodcock, MD
Tanya Sue Woodson, PA-C
Robert W. Woodward, MD
Alfred H. Woodworth, MD
Joe H. Woody, MD
Aldona Z. Wos, MD
Eileen M. Wright, MD
Farhad K. Yazdi, MD
Chad A. York, PA-C
Matthew L. Zerden, MD
J. Jean Zhang, MD
James G. Zolzer, MD
Donald L. Zust, Jr., DO
NCMB: Telephone Scams Targeting Licensees Still Active in NC

The North Carolina Medical Board continues to hear from licensees and healthcare employers that physicians and PAs are being targeted by scammers. The caller or callers may claim to be a medical board investigator and may even use technology to make it appear that they are calling you from the actual number of the North Carolina Medical Board. Licensees are told that their license will be suspended, or their practice closed if they do not agree to send money to the false investigator.
NCMB's Chief Investigative Officer has written a letter offering advice on how licensees can protect themselves if they receive a suspicious phone call. Read it now.
New Duke Health Research Could Help Reduce Racial Disparities in Kidney Disease
DURHAM, N.C. – In a finding that could help reduce the racial disparity in kidney disease, Duke Health researchers have detailed how two common gene variants among African Americans can cause kidney failure.

The finding, reported in the Journal of Clinical Investigation, could point to new treatment approaches and advance investigational therapies that block the gene.
“African Americans develop end stage kidney disease at four times the rate of white Americans and represent more than 30% of people on dialysis,” said lead author Opeyemi Olabisi, M.D., Ph.D., associate professor in the Department of Medicine at Duke University School of Medicine. “For more than a decade, we have known that two APOL1 gene variants account for much of the excess risk of non-diabetic kidney failure in African Americans, but we have only a limited understanding of how these variants work. Our study provides that insight."
Read full article here.
NCMS Regional Event in Charlotte Draws Enthusiastic Crowd
 The North Carolina Medical Society is on the road again!
The North Carolina Medical Society is on the road again!
NCMS members, guests, and friends joined together in Charlotte Wednesday to enjoy some time together and learn more about the Society's mission.
CEO Chip Baggett spoke on how NCMS is advocating on issues important to members like reforming Prior Authorization. He also talked about the NCMS strategic priorities of relieving your administrative burdens, our lobbying work on issues that impact your practice, and the long list of ways NCMS can help you grow professionally. As always, the NCMS is focused on protecting you, the practice of medicine, and your patients.
The medical community is being siloed and fractured at every turn.
This event is a great example of the importance of being together. The North Carolina Medical Society provides the space for the community to come together, across all specialties, to enhance the profession of medicine as colleagues and medical professionals.
If you are already a member, thank you for your continued support. If you are not a member, please consider JOINING NCMS TODAY!
We plan to continue these community conversations all over the state, so please be on the lookout for our next one!
Newborn Genetic Screening Study Reaches New Milestone
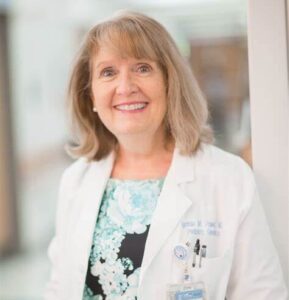 Cynthia Powell, MD (image credit: UNC)
Cynthia Powell, MD (image credit: UNC)

CHAPEL HILL, N.C. – Early Check, a groundbreaking research study that provides free health tests to newborns up to four weeks old in North Carolina, announced that it has screened 1,000 newborns in the state under its genome sequencing study.
The study, launched in September of 2023, screens newborns for hundreds of childhood-onset genetic conditions, many of which are not identified through state newborn screening, and assesses a newborn’s genetic risk of developing type 1 diabetes in their lifetime.
“There are many serious and treatable conditions that traditional newborn screening cannot identify,” said Cynthia Powell, MD, professor of pediatrics and genetics at the UNC School of Medicine and the project’s lead investigator at UNC. “Genomic sequencing allows us to identify infants with genetic changes that indicate a high likelihood of having one of these conditions.”
Read the full article here.
In Memoriam: NCMS Life Member Eugene Bozymski, MD
 NCMS Life member Dr. Eugene Bozymski died Thursday, February 15. He was 88.
NCMS Life member Dr. Eugene Bozymski died Thursday, February 15. He was 88.
Bozymski graduated from John Carroll University and Marquette School of Medicine in a remarkable six years. He trained at Scripps Mercy in San Diego and returned to the Medical College of Wisconsin for his three-year residency as he began his over 50-year career as a gastroenterologist. A fellowship at UNC School of Medicine helped to prepare him to serve as Professor of Medicine and Head of Endoscopy at Carolina for many years.
His commitment to excellence in patient care and dedication to nurturing future generations of gastroenterologists were evident in his leadership roles and mentorship of GI fellows.
Dr. Bozymski joined the NCMS in 1969.
The North Carolina Medical Society extends its deepest sympathies.
Read Bozymski's full obituary here.
Register Now! NC Allergy, Asthma, and Immunology Society Annual Meeting is May 18-19
| Download the meeting agenda.
Accommodations: Be sure to reserve your room at the Crabtree Valley Marriott before Thursday, April 25 to get our discounted rate of $159. Use this link to book today! Exhibiting Opportunities: Help ensure a successful meeting by sharing the exhibitor prospectus with the product and service representatives who call on your practice. Questions? Contact Megan Eberle at [email protected] or call 919-833-3836. |
Primary Care in Crisis! New Report From The Physicians Foundation
Scorecard Highlights State-Level Primary Care Performance & Lack of Physician Training in Underserved Communities
The second national Primary Care Scorecard released today reveals an intensifying primary care crisis and identifies five reasons why access to affordable, quality primary care services is expected to get worse.
Developed by researchers at the American Academy of Family Physicians’ Robert Graham Center and co-funded by the Milbank Memorial Fund and The Physicians Foundation, The Health of US Primary Care: 2024 Scorecard report and data dashboard examine critical measures of primary care performance nationally and across all states. Key findings include:
1. The primary care workforce is struggling to meet population demands.
- Despite a rapidly aging population with higher levels of chronic disease, the number of primary care physicians (PCPs) per person has decreased.
- The share of all clinicians practicing primary care (including nurse practitioners and physician assistants) stagnated around 28% between 2016 and 2021.
- PCPs declined from 68.4 to 67.2 per 100,000 people between 2012 and 2021.
- There has been a 36% jump in the share of U.S. children without a usual source of care over the last decade and a 21% increase among adults.
- Demand for PCPs will only increase with time. The National Institute of Health estimates that the number of people 50 or older with at least one chronic disease will increase by 99.5%, from 72 million in 2020 to 143 million by 2050.
2. The primary care sector is experiencing a workforce exodus and lacks real-world community training opportunities.
- Primary care residency does not mean primary care practice. In 2021, 37% of all physicians in training specialized in primary care, yet only 15% of all physicians were practicing primary care three to five years after residency. The remainder subspecialized or became hospitalists who do not work in community settings.
- In 2020, only 15% of primary care residents spent a majority of their time training in community settings (outside of hospitals and academic health centers) — signaling that many residents may lack adequate experience practicing in real-world clinical environments.
- In 2020, fewer than 5% of primary care residents spent the majority of their training in Teaching Health Centers or rural training tracks, two programs that historically serve disinvested communities. Research indicates physicians who train in Teaching Health Centers are more likely to practice in underserved communities.
3. The US continues to underinvest in primary care, despite diminishing supply and growing demand.
- The share of total US health care spending devoted to primary care stayed under 6% from 2012 to 2021.
- Since 2019, investment in primary care has steadily declined across all major health care payers; this decline has been most pronounced for Medicare reimbursements for primary care services and providers, which have dropped by 15%.
- The compensation gap between primary care physicians and specialists discourages residents from choosing primary care.
4. Cumbersome electronic health records burden primary care physicians.
- In 2022, more than 40% of family physicians rated the usability of their electronic health record (EHR) systems as unfavorable. Over 25% reported overall dissatisfaction with their current EHR system.
- According to the American Board of Family Medicine, 16% of family physicians reported spending four or more hours per day on EHRs, taking time away from patient care.
5. Inadequate research funding impacts primary care access and quality.
- Since 2017, only 0.3% of federal research funding (administered through the National Institutes of Health, the Centers for Disease Control and Prevention, the Agency for Healthcare Research and Quality, and the U.S. Food and Drug Administration) per year has been invested in primary care research, limiting new information on primary care systems, delivery models, and quality.
- A lack of adequate data on the prevalence of hybrid primary care payment (a combination of fee-for-service and per-person payments) and the training of nurse practitioners and physician assistants), for example, makes it difficult to track progress on the implementation of high-quality primary care.
“As more and more patients struggle to get appointments with primary care practices, policymakers must come together to address the primary care crisis,” said Milbank Memorial Fund President Christopher F. Koller. “By prioritizing investments in primary care and expanding our physician workforce today, we can ensure that everyone in every community has access to high-quality primary care in the future.”
Key State Scorecard Findings:
- Workforce: Alaska ranks second among all states, following Idaho (38.2%), for having 36.2% of its clinician workforce in primary care overall (compared to 28.6% nationally) and first for primary care clinician density in the most disadvantaged areas, with 269 clinicians per 100,000 people (compared to 111.7 clinicians per 100,000 people nationally).
- Training: North Dakota is the highest-ranked state for physician training measures, with a larger share of new doctors entering primary care (36.4%) each year than the national average (21.6%) and a high rate of physicians, physician assistants, and nurse practitioners working in primary care at 26.6%, 44.2%, and 39.4%, respectively.
- Investment: Oregon has the highest overall investment in primary care, with 7.7% of all health care spending going to primary care, compared to the national average (4.7%). The state also has the highest primary care spending for commercial payers (9.1%) and Medicaid (9.2%), compared to the national averages of 5.6% and 4.7% respectively.
The Scorecard was developed in response to a call for an annual tracking tool to inform primary care policy issued by the National Academies of Sciences, Engineering, and Medicine in their 2021 report, Implementing High-Quality Primary Care Rebuilding the Foundation of Health Care. This seminal report provides policy recommendations for federal and state governments, health care organizations, and payers to strengthen primary care.
“Primary care is the cornerstone of our health care system, playing a pivotal role in improving our nation’s health by delivering accessible and timely care to those in need,” said Ripley Hollister, MD, a board member of The Physicians Foundation and a practicing family physician. “The findings and recommendations from the second national Primary Care Scorecard highlight that investment in primary care is vital for the future of health care. The report implores us to embrace and advance solutions that support primary care and allow everyone to live longer, healthier lives.”
READ THE FULL REPORT
READ THE PRESS RELEASE
About The Physicians Foundation
The Physicians Foundation is a nonprofit seeking to advance the work of practicing physicians and help them facilitate the delivery of high-quality health care to patients. As the U.S. health care system continues to evolve, The Physicians Foundation is steadfast in strengthening the physician-patient relationship, supporting medical practices’ sustainability and helping physicians navigate the changing health care system. The Physicians Foundation pursues its mission through research, education and innovative grant making that improves physician wellbeing, strengthens physician leadership, addresses drivers of health and lifts physician perspectives. For more information, visit www.physiciansfoundation.org
About the Milbank Memorial Fund
The Milbank Memorial Fund works to improve population health and health equity by collaborating with leaders and decision makers and connecting them with experience and sound evidence. Founded in 1905, the Milbank Memorial Fund advances its mission by identifying, informing, and inspiring current and future state health policy leaders to enhance their effectiveness; convening and supporting state health policy decision makers to advance strong primary care and sustainable health care costs; publishing high-quality, evidence-based publications and The Milbank Quarterly, a peer-reviewed journal of population health and health policy. For more information, visit www.milbank.org
Looking for Help? Asthma Medication Now Approved to Help Some Food Allergies

Xolair, the brand name for the drug omalizumab, is first medication approved to reduce allergic reactions caused by accidental exposure to food triggers
(The Hill, WGN) -- For decades, asthma patients have used a drug to help them breathe better. Now, the Food and Drug Administration has given the nod to use that drug to reduce serious reactions from food allergies.
Xolair, the brand name for the drug omalizumab, became the first medication approved to reduce allergic reactions caused by accidental exposure to food triggers. Patients as young as age 1 with allergies can take the drug by injection every two to four weeks, depending on their weight and their body’s response to allergens.
Many people with allergies — and their families — live with constant anxiety about exposure to allergens and often avoid dining out and other social situations.
“To have this protection is going to be life-changing,” said Robert Wood, director of the pediatric allergy division at Johns Hopkins Children’s Center.
The FDA decision is based on a study led by Wood and funded by the National Institutes of Health. It showed that Xolair allowed about 68% of participants with peanut allergies to tolerate about 600 milligrams, or about 1/2 teaspoon, of peanut protein, compared with about 6% of those who received dummy injections.
The results were similar for other allergens such as tree nuts, milk, egg and wheat, a study abstract reported. Full results are expected to be presented at a meeting and published in a peer-reviewed journal later this month.
Wood estimated that 25% to 50% of people with food allergies, particularly children and young adults, would elect to use Xolair.
The drug has been used “off-label” to treat food allergies, said Ruchi Gupta, director of the Center for Food Allergy & Asthma Research at Northwestern University. She welcomed full approval of the product.
Xolair is a monoclonal antibody, a type of treatment that works by blocking the body’s natural response to allergens. It was first approved in 2003 and has been used to treat asthma, nasal polyps and chronic hives. It is produced by drugmakers Novartis and Roche and is distributed by a Roche subsidiary, Genentech.
“This really is a difference maker for patients and parents who have severe food allergies,” said Sai Nimmagadda, an allergist at Lurie Children’s in Chicago.
“Every day here at Lurie, you see two or three kids come in with a reaction,” Nimmagadda said.
“Patients on Xolair were able to tolerate higher quantities of food compared to placebo. It will prevent up to 40 percent of patients who have allergic reactions and 30,000 ER visits a year,” Nimmagadda said.
“It’s the first known medication with the indication to prevent food allergies,” Nimmagadda said.
That means relieving the constant fear of accidental, life-threatening allergies.
“What we’re noticing is patients who are on Xolair can tolerate up to two and a half peanuts before they have a reaction, up to three and a half cashews, up to about two teaspoons of milk and maybe up to a quarter teaspoon of egg,” Nimmagadda said. “So, it brings the threshold up a little bit. So, instead of trace amounts causing the allergic reaction, now you can feel safe you can have accidental exposures and not end up in the emergency room.”
“You don’t have the allergic effects when you ingest the food you are allergic to,” Nimmagadda said.
The most common side effects of Xolair are injection site reactions and fever, but the FDA noted that the drug has also been associated with joint pain, rash, parasitic infections, malignancies and abnormal laboratory tests. Xolair comes with a warning saying the treatment itself can cause anaphylaxis and must be started in a health care setting equipped to manage the reaction.
The medication is not approved for emergency treatment of allergic reactions.
The list price for Xolair ranges from about $2,900 a month for children to $5,000 a month for adults, according to Genentech. Most insured patients typically pay less out of pocket, the company said.
The Associated Press contributed to this report.
Mark Your Calendar: Workforce Retention and Resiliency Within Integrated Care Setting Webinar

Join this webinar aimed at providing key factors contributing to burnout, compassion fatigue, and employee turnover among primary and behavioral health providers.
In addition, you'll learn:
- How these challenges intensified during the pandemic.
- Effective supervisory strategies for employee engagement, resilience, and retention.
- Key organizational policies and practices that can enhance workforce retention and resilience.
Workforce Retention and Resiliency within Integrated Care Setting
Wednesday, March 6
1:00-2:00 p.m. ET
Earn 1 continuing education credits (CEUs) for attending this webinar.
Meet Your Legislator: Senator Lisa Barnes
 Senator Lisa Barnes (image credit: NCGA)
Senator Lisa Barnes (image credit: NCGA)
Your NCMS Advocacy team has a meeting scheduled with Senator Lisa Barnes on March 7th at 11:30am in Raleigh. If you are a constituent of Senator Barnes and interested in attending, please email Hannah Rice at [email protected] for details.
Senator Barnes represents Franklin, Nash, and Vance counties.
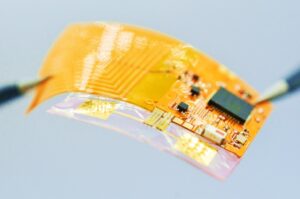
UNC Scientists Create New Drug Delivery System
Wireless Drug Patch Shows Promise as Chronic Disease Treatment Delivery System
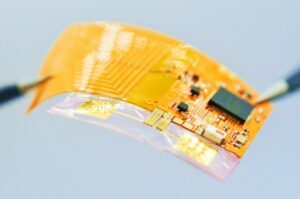 The Spatiotemporal On-Demand Patch’s exposed circuit will be covered by material resembling a Band-Aid. It can receive commands wirelessly from a smartphone or computer to schedule and trigger the release of drugs from individual microneedles.
The Spatiotemporal On-Demand Patch’s exposed circuit will be covered by material resembling a Band-Aid. It can receive commands wirelessly from a smartphone or computer to schedule and trigger the release of drugs from individual microneedles.
Led by Juan Song, PhD, at the UNC School of Medicine, and Wubin Bai, PhD, at the UNC College of Arts and Sciences, research suggests that a wearable patch featuring electrically triggered microneedles for on-demand drug delivery could be the next frontier in treatment of neurodegenerative disorders and neurological injuries.
(UNC Health Newsroom) -- CHAPEL HILL, NC – University of North Carolina at Chapel Hill scientists created a new drug delivery system, called the Spatiotemporal On-Demand Patch (SOP), which can receive commands wirelessly from a smartphone or computer to schedule and trigger the release of drugs from individual microneedles. The patch’s thin, soft platform resembles a Band-Aid and was designed to enhance user comfort and convenience, since wearability is a crucial factor for chronically ill patients.
The research team, led by Juan Song, PhD, professor of pharmacology at the UNC School of Medicine, and Wubin Bai, PhD, assistant professor of applied physical sciences at the UNC College of Arts and Sciences, tested the SOP in a mouse model, using melatonin in the microneedles to improve sleep.
This research, published in the journal Nature Communications, opens the door to researching this wirelessly controlled patch to deliver on-demand treatments for neurodegenerative disorders, including Alzheimer’s disease. To that end, the UNC School of Medicine and UNC Health funded a $25,000 pilot project to test the SOP in a mouse model of Alzheimer’s disease.
“SOP’s ability to enable joint delivery of multiple drugs could address various aspects of Alzheimer’s Disease, such as reducing beta-amyloid plaques, mitigating neuroinflammation and enhancing cognitive function,” said Bai, a co-senior author.
The open access paper titled, “Digital Automation of Transdermal Drug Delivery with High Spatiotemporal Resolution,” was co-authored by Yihang Wang of the Department of Applied Physical Sciences and Zeka Chen of the Department of Pharmacology. Bai said the research highlights not only a multidisciplinary collaboration but also a “passionate involvement of Carolina undergraduate students,” including Priyash Hafiz of the Department of Applied Physical Sciences, and Brayden Davis, Will Lipman, Tian Wang and Sicheng Xing of the UNC/NCSU Joint Department of Biomedical Engineering.
The patch, which has received a provisional patent, enables highly localized treatment – less than 1 square millimeter – of specific tissues, organs or regions within the body, and drug release can be triggered within 30 seconds in response to an electrical signal. Patients could wear more than one patch at a time which would reduce the need for doctors’ visits, or even trips to the hospital, for medical attention.
“The beauty of this device is that it can house dozens, if not hundreds, of concentrated drugs and can program their sequential release automatically,” said Song, who is a member of the UNC Neuroscience Center. “Rapid drug release can be crucial in emergency situations or when immediate therapeutic action is required.”
The microneedles are coated with gold, which protects the drugs and surrounding tissues. When a low-voltage electrical stimulus is applied through the patch, the gold coating disintegrates, exposing the drug-loaded microneedles to the skin and initiating the controlled release of the drugs.
“This level of specificity ensures precise and customized drug delivery, catering to the needs of different conditions or specific regions of the body,” said Wang. “This offers a novel approach to achieving controlled drug release through a combination of materials science and electrical engineering.”
The National Science Foundation and the National Institutes of Health funded this research.
David DeFusco, communications specialist at the UNC Department of Applied Physical Sciences, wrote the original news announcement. The UNC School of Medicine contact is Mark Derewicz, director of research and national news for UNC Health.
2024 Health of US Primary Care Scorecard Webinar is Wednesday
Primary care is the foundation of our health care system. Yet more and more people report not having a regular place for care. In the forthcoming second annual Primary Care Scorecard, Robert Graham Center researchers give five reasons why access to primary care is worsening.
Join the Milbank Memorial Fund and The Physicians Foundation on February 28, at 12 p.m. ET, for a webinar on how the nation and the states are performing on primary care workforce, financing, training and research funding measures — and how challenges within each of these areas contribute to poor access to primary care.
The Physicians Foundation's President, Gary Price, MD, will give opening remarks ahead of a panel discussion moderated by Frances Stead Sellers of The Washington Post. The panel will include:
· Rachel Block, Program Officer, Milbank Memorial Fund
· Margaret Flinter, APRN, PhD, Vice President and Clinical Director, Community Health Centers, Inc.
· Yalda Jabbarpour, MD, Director, The Robert Graham Center
· Kyu Rhee, MD, President and CEO, National Association of Community Health Centers
REGISTER NOW
About The Physicians Foundation
The Physicians Foundation is a nonprofit seeking to advance the work of practicing physicians and help them facilitate the delivery of high-quality health care to patients. As the U.S. health care system continues to evolve, The Physicians Foundation is steadfast in strengthening the physician-patient relationship, supporting medical practices’ sustainability and helping physicians navigate the changing health care system. The Physicians Foundation pursues its mission through research, education and innovative grant making that improves physician wellbeing, strengthens physician leadership, addresses drivers of health and lifts physician perspectives. For more information, visit www.physiciansfoundation.org
Want To Go To Medical School for Free? Here Is A Billion Ways It Is Now Possible

Albert Einstein College of Medicine to offer free tuition after billion-dollar gift
Dr. Ruth Gottesman, 93, who spent 55 years as the chair of the school’s board, made the historic donation in the name of her late husband, David “Sandy” Gottesman, who was an early investor of Berkshire Hathaway and a longtime friend of Berkshire’s famed CEO Warren Buffett.
Philip Ozuah, president and CEO of Montefiore Medicine, the school’s parent company, announced the “transformational gift” on Monday, saying that “this is the largest donation to any medical school in the country.”
Sandy Gottesman, who was the co-founder of New York-based investment firm First Manhattan Co., died in 2022.
The Gottesmans had long been involved in health care philanthropy. In 2010, their gift of $25 million to the Albert Einstein College of Medicine went towards creating the school’s Institute for Stem Cell Research and Regenerative Medicine. Sandy Gottesman also served on the board of New York’s Mount Sinai Hospital.
“I am very thankful to my late husband, Sandy, for leaving these funds in my care, and l feel blessed to be given the great privilege of making this gift to such a worthy cause,” said Dr. Ruth Gottesman in a news release.

Dr. Ruth Gottesman joined the medical school in 1968 and developed screening, evaluation and treatments for children with learning disabilities. In 1992, she founded the Adult Literacy Program at Einstein’s Children’s Evaluation and Rehabilitation Center, “the first of its kind.” She also served as the founding director of the school’s Emily Fisher Landau Center for the Treatment of Learning Disabilities, which opened in 1997.
Few educational donations rival the magnitude of Dr. Ruth Gottesman’s. In 2018, former New York mayor Michael Bloomberg donated $1.8 billion to his alma mater, Johns Hopkins University. And New York hospitals have long drawn the philanthropy of billionaires, with individual donations sometimes amounting to more than $100 million. Home Depot co-founder Ken Langone has heavily invested in New York University’s medical centers. In 2018, in part due to Langone’s donations, NYU’s School of Medicine became the first medical school in the country to offer free tuition to accepted students.
An October survey from the Association of American Medical Colleges found that 70% of medical students who graduated in 2023 have taken on some level of education debt. The average graduate left medical school owing more than $200,000, according to the AAMC.
“This donation radically revolutionizes our ability to continue attracting students who are committed to our mission, not just those who can afford it,” said Dr. Yaron Tomer, the dean at Albert Einstein. “We will be reminded of the legacy this historic gift represents each spring as we send another diverse class of physicians out across the Bronx and around the world to provide compassionate care and transform their communities.”
Warning for Clinicians in Charlotte Region
A message from Erica Wilson, MD, MPH, North Carolina Department of Health and Human Sources
The North Carolina Division of Public Health (NC DPH) is alerting clinicians in North Carolina to an increase in ciprofloxacin- and penicillin-resistant strains of invasive meningococcal disease caused by Neisseria meningitidis serogroup Y (NmY) in the Charlotte Metropolitan region.
Since February 2023, two cases of invasive meningococcal disease have been found to be resistant to ciprofloxacin and penicillin in residents of Mecklenburg County and one case in a resident of neighboring York County, South Carolina. These cases meet the threshold to recommend discontinuing the use of ciprofloxacin for prophylaxis of close contacts per CDC’s updated guidance.
Providers in the Charlotte Metropolitan region including Cabarrus, Gaston, Iredell, Lincoln, Mecklenburg, Rowan, and Union Counties should discontinue the use of ciprofloxacin for prophylaxis of close contacts of invasive meningococcal disease cases and prescribe rifampin, ceftriaxone, or azithromycin instead. Providers treating residents from Chester, Lancaster, or York counties in South Carolina should also follow this guidance for patients being treated in North Carolina medical facilities.
Clinicians should contact their local health departments or the Communicable Disease Branch epidemiologist on-call 24/7 number (919-733-3419) for questions.
Bad News: Your Binge of Yellowstone Likely Means You'll Be In the Bathroom A Lot Tonight

Binge watchers more likely to need multiple night-time bathroom breaks
(The Guardian) -- Sitting down to binge watch the latest TV drama might seem like the perfect way to unwind, but researchers have found that people who spend lengthy periods in front of the box are more likely to need to pee multiple times a night.
Writing in the journal Neurourology and Urodynamics, researchers in China report how they analysed data from the National Health and Nutrition Examination Survey in the US, focusing on responses collected from 2011 to 2016.
The team found that 32% of the 13,294 participants, aged 20 and older, reported experiencing nocturia, the need to wake up and urinate two or more times a night.
After taking into account factors including age, sex, body mass index, ethnicity, education level and whether or not individuals had diabetes, the researchers found that the risk of experiencing nocturia was 48% higher in those who spent five or more hours watching TV or videos a day than those who watched less than an hour.
“To our understanding, this study represents the first exploration of the correlation between TV and/or video viewing time and nocturia,” the researchers write.
The team say the mechanism by which prolonged TV viewing increases the risk of nocturia is poorly understood.
However, they point to a number of possible explanations for the association, noting that lengthy sessions of TV viewing have been associated with an increased risk of developing type 2 diabetes, which is a risk factor for nocturia, while sedentary behaviour is associated with fluid retention in the legs that may also contribute.
“Moreover, TV watching typically aligns with beverage consumption, leading to an elevated fluid intake,” they write, adding that among other possibilities prolonged TV viewing may lead to neurological disorders that could trigger bladder dysfunction, and that TV watching may affect sleep duration or quality.

Watching at least five hours of TV a day associated with higher risk of nocturia, or needing to get up and urinate twice or more a night
The study has limitations, including that it cannot prove cause and effect, and it relied on self-reported data including for TV watching habits.
Despite this, the team say healthcare professionals should tell patients about the link. “Increasing public awareness of this potential health risk encourages individuals to be more mindful of their TV and/or video time,” they write.
James Catto, professor of surgery at the University of Sheffield, who was not involved in the research said there could be a number of factors muddying the waters in the new study. Among them he noted those with nocturia tended to be older, have a higher body mass index than those without, and were less mobile.
“[Have] they got nocturia because they’re watching telly all day, or they watch the telly all day because of other factors and then they just end going to the toilet more often?,” he said, noting that cannot be answered by the current study.
Catto added that nocturia is common, particularly among older people, and that it is not necessarily a cause for concern – although it can occur as a result of cancer, infections or diabetes.
“If you’re going a lot at night, and it’s bothering you, see a GP, they’ll do a few tests to make sure you’ve not got diabetes,” said Catto. But, he added: “Most people are not too bothered by going once or twice at night.”
On Point: Alabama Supreme Court Ruling That Disrupts Healthcare For People Building Families is Unconscionable -- Dr. Amy Bryant
On Point submissions are individual member viewpoints and not North Carolina Medical Society policy.

MSCR, At Large Member of the Executive Committee, NCOGS
Not even a week after the Alabama Supreme Court gave unprecedented and medically unnecessary protections to frozen embryos, several IVF clinics in the state had already halted services, afraid in this dangerous new setting to provide the healthcare they are trained to provide. This disruption to healthcare for people trying to build their families is unconscionable.
Rulings such as the one from the Alabama Supreme Court have an undeniably chilling effect on medical practice. Physicians are trained to provide evidence-based care, and care for patients at their most vulnerable moments. They did not train to understand the nuances of criminal law and precious few want to risk felony charges that could rob them of their ability to support their families and future patients, or even land them in prison.
This bodes poorly for the healthcare workforce in Alabama which already struggles to keep its physician workforce. Alabama also has one of the highest rates of maternal and infant mortality in the nation in the country, with outcomes worse for Black infants and mothers. Over 34% of its counties are “maternity deserts” without adequate access to obstetric care. Further restricting and intimidating physicians, who provide reproductive and primary care, and may also need reproductive services themselves, is counterproductive to improving health outcomes.
Why would people who purportedly care about life at all stages want to put so many people in harm’s way? What about the health and lives of those who need assisted reproductive technology to grow their families? Or those who need contraception or abortion to have a healthy family? It seems that protecting life is not in fact the actual goal. Relegating those who can get pregnant to mere vessels is not meant to protect life, it is a means of coercion and control.
The tactics at play in this case are sadly all too familiar. They are an extension of the tactics that place medically unnecessary restrictions on abortion. This ruling shows that anti-science politicians never intended to stop at abortion. This new type of interference in reproductive healthcare clearly exposes anti-abortion intentions to continue to restrict bodily autonomy, no matter the circumstances. Banning contraception is the next logical step, and even talked about openly in some state legislatures.
Anti-science politicians and judges-most often with no medical training- but with a clear, ideological agenda to control and coerce women, are a serious threat to the healthcare system. This is just not right in a multi-faceted, pluralistic, democratic society where many viewpoints and religious beliefs have the right to coexist.
The Alabama Supreme Court's ruling will fortunately not affect North Carolina. But this ruling should be deeply troubling to all of us, not only because of the devastating impact on people seeking to grow their families using assisted reproductive technology in Alabama. This ruling could embolden other states to pass similar legislation.
North Carolina physicians should take note. The fantasy world of full personhood for embryos that is embodied by rulings such as this does not bode well for our actual patients or healthcare system. Patients and physicians should be allowed to make decisions regarding their fertility based on their personal values and beliefs, not those imposed by the state. A state that sanctions these deeply unpopular intrusions into people’s lives, based on the religious views of a subset of its population, will find itself without the healthcare workforce it needs to have a thriving population.
New Mesothelioma Therapy Offers Hope for Highly Fatal Cancer
Medicine used alongside chemotherapy in trials quadrupled three-year survival rates for mesothelioma
Scientists have reached a breakthrough in the treatment of mesothelioma, a rare and highly deadly form of cancer that’s linked to asbestos exposure. According to a study published last week, the innovative therapy, which combines a new drug with chemotherapy, increased the median survival of participants by about a month and half.
It also quadrupled the three-year survival rates for those who received the drug combination, compared to a placebo group. Lead author Peter Szlosarek, who has been working on this project “from its earliest stages,” said the results are “truly wonderful” in a press release from Queen Mary University of London.
One of the patients who received the new treatment, Mick, was initially given four months to live after he was diagnosed with mesothelioma caused by asbestos exposure during his time working in a factory in the 1970s. He put his trust in Szlosarek and about six years after his diagnosis, he was able to celebrate his 80th birthday with his family.
“This trial has changed the lives of people with mesothelioma, allowing us to live longer,” Mick said. “I have five grandchildren and two great-grandchildren now — I wouldn’t want to miss all that.”

(From The Guardian) -- Scientists have developed a drug to treat mesothelioma, a notoriously hard-to-treat cancer linked to asbestos, in the biggest breakthrough in two decades.
Thousands of people are diagnosed with the disease globally every year, which tends to develop in the lungs and is mainly caused by exposure to asbestos at work. It is aggressive and deadly, and has one of the world’s worst cancer survival rates.
Now scientists are hailing the “truly wonderful” arrival of a new therapy, which they say should offer fresh hope to those with the disease and their families.
In an international trial spanning five countries, led by Queen Mary University of London, a new drug that cuts off the tumor’s food supply quadrupled three-year survival rates. The results were published in the journal JAMA Oncology.
“This trial has changed the lives of people with mesothelioma, allowing us to live longer,” said one of the patients who benefited from the drug. The 80-year-old, who wished to remain anonymous, won compensation from his former employer after being exposed to asbestos in a factory in the 1970s.
He was given four months to live, but thanks to the trial is still alive five years later. “I have five grandchildren and two great-grandchildren now – I wouldn’t want to miss all that,” he said.
The breakthrough is significant, experts say, because mesothelioma has one of the lowest survival rates of any cancer. The new drug, ADI-PEG20 (pegargiminase), is the first of its kind to be successfully combined with chemotherapy in 20 years.
The trial involved patients from the UK, US, Australia, Italy and Taiwan, and was led by Prof Peter Szlosarek at Queen Mary. Each received chemotherapy every three weeks for up to six cycles. Half were also given injections of new drug, while the other half received a placebo for two years.
Among the patients included in the final analysis were 249 people with pleural mesothelioma – when the disease affects the lining of the lungs. They had an average age of 70.
The study, known as the ATOMIC-meso trial, was conducted at 43 centers in the five countries between 2017 and 2021. Those who received pegargiminase and chemotherapy survived for an average of 9.3 months, compared with 7.7 months for those who had the placebo and chemotherapy, according to the results published in JAMA Oncology.
The average “progression-free survival” was 6.2 months with pegargiminase-chemotherapy, compared with 5.6 months among patients who had the placebo and chemotherapy.
“In this pivotal, randomized, placebo-controlled, phase 3 trial in 249 patients with pleural mesothelioma, pegargiminase-chemotherapy increased significantly the median overall survival by 1.6 months and quadrupled the survival at 36 months compared to placebo-chemotherapy,” the authors wrote.
“Pegargiminase-based chemotherapy was well tolerated with no new safety signals.”
The breakthrough follows two decades of work by Szlosarek, after his original discovery that mesothelioma cells lack a protein called ASS1, which enables cells to manufacture the amino acid arginine.
This knowledge was used to develop the drug. ADI-PEG20 works by depleting arginine levels in the bloodstream. For tumor cells that cannot manufacture their own arginine, this means their growth is thwarted.
“It’s truly wonderful to see the research into the arginine starvation of cancer cells come to fruition,” said Szlosarek. “This discovery is something I have been driving from its earliest stages in the lab, with a new treatment, ADI-PEG20, now improving patient lives affected by mesothelioma.”
Dr Tayyaba Jiwani of Cancer Research UK, which funded the research alongside the biotechnology company Polaris Group, said: “This study shows the power of discovery research which allows us to dig deep into the biology of mesothelioma to uncover vulnerabilities that we can now target with ADI-PEG20.”
Liz Darlison, chief executive of the charity Mesothelioma UK, said: “The UK mesothelioma community, including doctors, nurses, patients and families living with mesothelioma, are extremely proud of ATOMIC. It offers another much-needed treatment option and, above all, hope to those living with mesothelioma.
“We look forward to seeing this treatment become available as a standard option to all patients in the future.”
New Study: VR Can Enhance Relationship Between Caregivers and Aging Population

Research conducted by Stanford University's Virtual Human Interaction Lab in collaboration with Mynd Immersive and AT&T 5G Healthcare
(PRNewswire) -- Virtual Reality (VR) technology is not just for the young. It's paving the way for enhancing relationships between the aging population and their caregivers, as research from the Virtual Human Interaction Lab (VHIL) at Stanford University demonstrates.
This research comes just months after the American Medical Association issued CPT codes that recognize VR for various therapeutic services, a major milestone for the growth of digital therapeutics.
The study sought to understand older adults' attitudes towards new technologies, including virtual reality, and how professional caregivers felt about facilitating VR experiences for older adults. Research was led by Dr. Jeremy Bailenson, founding director of the VHIL and one of the world's leading experts on understanding and exploring individual behavior and social responses in VR, and Ryan Christopher Moore, Ph.D. researcher.
"This study showcases how a tool which is typically associated with youthful entertainment has transformative applications in healthcare, particularly geriatric care," said Dr. Bailenson. "The response from both the caregivers and seniors has been quite positive, suggesting
that VR can be a sustainable and beneficial tool in Senior Care communities."
Key findings include that 81.5% of caregivers reported they enjoyed interacting with residents more while using Mynd Immersive (Mynd), formerly MyndVR than while doing other activities, and 94.9% said that using Mynd was moderately to extremely beneficial to their relationship with the resident. Similarly, 83% of residents reported that using Mynd was moderately to extremely beneficial to their relationship with the caregiving staff.
The study also found:
- 74.2% of the caregivers reported that the residents' mood improved after using Mynd, and 79.2% of the residents reported feeling more positive
- 57.9% of older adults reported feeling less isolated from the outside world after using Mynd
- While positive attitudes towards new technology often decline with age, the study population overwhelmingly felt positive about using VR and the decline in attitude was less than compared to other technologies like cell phones and voice assistants

"Shared experiences in VR, like revisiting a senior's hometown or traveling to a place they've always wanted to see, can stimulate greater communication, bridge emotional gaps, and create deeper bonds," said Chris Brickler, CEO of Mynd Immersive. "We are experiencing explosive growth of our aging population, while simultaneously seeing a significant decline in available caregivers, so it's imperative that we create tools like Mynd that can help create a more enjoyable and fulfilling environment for both the cared and caregiver."
Mynd has brought together a powerful consortium of industry collaborators to support this research and beyond, including AT&T, HTC VIVE, Select Rehabilitation, and some of the world's most innovative senior living communities, such as John Knox Village in Pompano Beach, Florida, Commonwealth Senior Living, Sodalis Senior Living, Long Island State Veteran Home and more.
"We're entering a new era of delivering immersive, digital therapeutics," said Joe Drygas, Head of AT&T Healthcare. "The combination of XR experiences with 5G and AI will have a tremendous impact on the many ways we can provide top quality care for our elders and support their caregivers. The Mynd Immersive and AT&T collaboration is bringing the future of connected healthcare into sharp focus for older adults and their families."
"We launched HTC VIVE with a belief that VR could positively impact humanity," said Cher Wang, Chairwoman of HTC. "This type of data from industry partners like Mynd and esteemed independent researchers, such as Stanford University, further supports our belief and moves the entire industry forward."
Stanford's pioneering lab, focused on the psychological and behavioral effects of virtual reality, conducted a survey of 245 older adults and 39 caregivers in 16 Senior Care communities across 10 states. The study, the largest ever conducted on VR and older adults, was done in collaboration with Mynd, the leading provider of immersive therapeutic experiences for the aging population.
The study has already won a "Top Paper Award" by the National Communication Association and will be presented at their upcoming annual convention. The paper has also been accepted by the journal, Cyberpsychology, Behavior, and Social Networking and will be published later in 2023.
NCDHHS Secretary Kody Kinsley Unifies Department's Collaborative Efforts
NCDHHS Wants to Ensure NC Communities and Families Are Center of Department Work
https://youtu.be/qPW4Qk6iqzU?si=TrWZm30fZ2zty4_9
The NCDHHS launched a Community Partner Engagement Plan and website to ensure the voices of North Carolina communities and families are at the center of the department’s work.
Go to ncdhhs.gov/GetInvolved to see the many groups, organizations and commissions that NCDHHS currently partners with. The department will continue to update the website and encourages community members to get involved with a current group or sign on to work with the divisions that focus on your area of interest.
To improve internal processes, Secretary Kinsley issued a Secretarial Directive that unifies the department’s collaborative efforts into a guide for how to best engage with communities.
NCDHHS is excited to deepen its partnerships and collaboration by strengthening connections with communities statewide and listening to their insights. The department’s goal is to grow together with North Carolinians and make major progress toward better health for all.
Learn more in the Community Partner Engagement Guide and watch a video from Secretary Kinsley where he announces the plan. For more information on how to partner with NCDHHS, email [email protected].
North Carolina Stepping Onto National Stage as Biotech Skyrockets in Triangle

Nation's Oldest Biotech Hubs Looking at NC as One of Their Biggest Rivals
(Axios - Zachery Eanes) -- In less than a decade, the Triangle's biotech industry has more than doubled its lab space and added tens of thousands of new workers, as the region's profile among investors and companies soars.
The big picture: Some of the nation's oldest biotech hubs, like Boston, now see the Triangle as one of their biggest rivals, as a widely shared Boston Globe article noted this month.
- That's because the region not only boasts a talented workforce but also continues to offer comparatively low costs for land, construction, electricity, lab rent and housing, the Globe reported.
Why it matters: The biotech industry has long driven the Triangle's growth, making Research Triangle Park a name brand across the country. From scientists with advanced degrees to community college graduates working in pharmaceutical manufacturing, the high-paying jobs abound.
- And even as investments into office buildings slow down, the building boom in the life sciences industry remains robust.
By the numbers: Around 40,000 people in the Triangle worked in the life sciences industry as of 2022, a significant increase over the past decade, according to research from CBRE.
- From 2016 to 2023, lab and R&D space grew from 4.4 million square feet to 9.3 million square feet.
- Since 2018, nearly 30 life sciences companies, like Fujifilm Diosynth and Eli Lilly, have invested $8.9 billion in the region, and pledged to create nearly 7,000 new jobs.
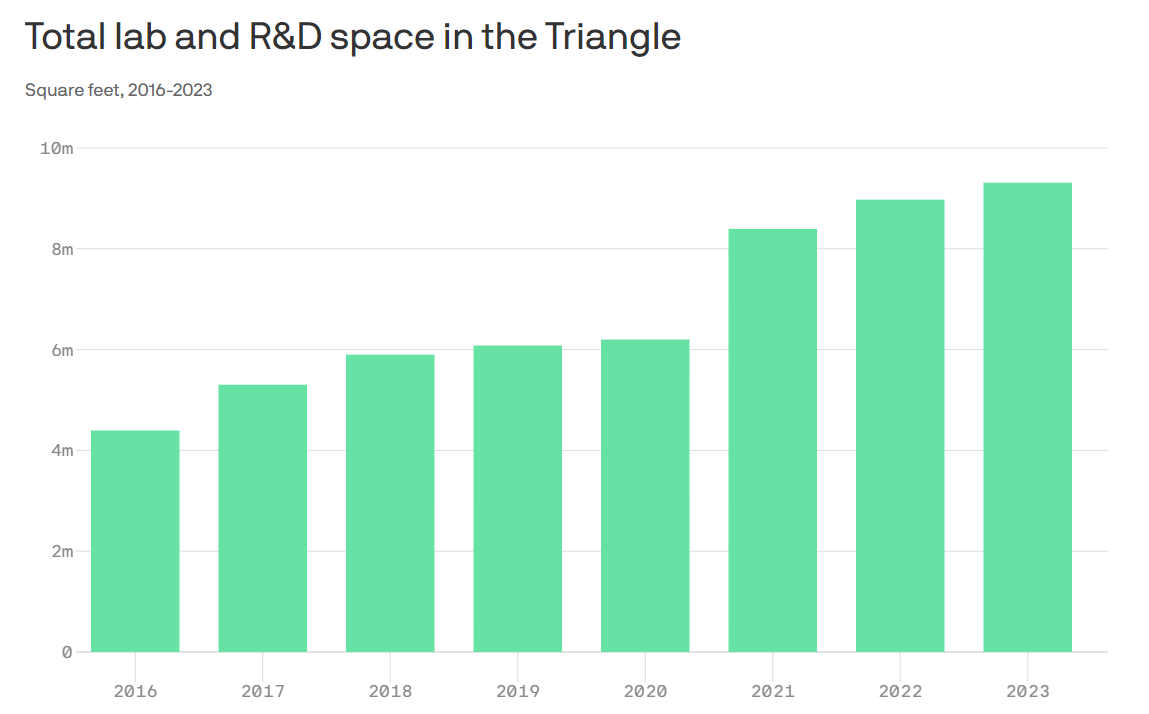
Zoom in: Research Triangle Park, home to hundreds of companies and where a $1.5 billion development effort is underway, is the epicenter of the Triangle's biotech industry.
- But it's influence has seeped into every corner of the region, with downtown Durham now a hot spot for startups, and manufacturing hubs for pharma companies popping up from southern Wake County all the way to Sanford.
- Chapel Hill and Raleigh are also seeing upticks in lab space construction.
Among the biggest projects underway:
- Spark Life Science in Morrisville, which could span 1.5 million square feet of lab and manufacturing space. The first phase has been completed, with no tenants signed yet.
- Pathway Triangle, a 1 million square foot manufacturing campus under construction across the street from Spark LS, is currently being built by Boston-based King Street Properties.
- Via Labs, which will be Hub RTP's first lab high-rise, could start construction later this year — though Boston-based owner Longfellow is still waiting to sign tenants.
- Fujifilm Diosynth's $2 billion manufacturing campus in Holly Springs will be completed in 2025. Janssen Supply Group recently signed a lease there as well.
Between the lines: The growth simply wouldn't be happening without the presence of three tier-one research universities, Lee Clyburn, executive vice president at CBRE's Raleigh office, told Axios.
- In 2023 alone, Duke, UNC, the Research Triangle Institute and others brought in $1.9 billion in National Institute of Health funding.
- And thanks to the universities, the Triangle boasts one of the highest concentrations of life science researchers in the country.
Threat level: With so much lab and manufacturing space on the way, vacancy rates are expected to rise, CBRE noted, and already they are hovering around 10%.
- A combination of higher interest rates and a slowdown in venture capital funding could slow down the industry's growth in the Triangle as well.
- Forge Nano — a battery company, not a life sciences company — was the only major manufacturing lease in the four quarter of 2023.
Yes, but: The real estate firm JLL also recently named the Triangle as the No. 1 biomanufacturing market in the country.
- And JLL notes that the Triangle's pipeline of construction, while large, is not as speculative as markets like Boston or the Bay Area.
What's next: Novo Nordisk, the Danish pharmaceutical company behind the weight-loss drug Ozempic, could be the next life sciences company to plot a Triangle expansion.
- The company has purchased an additional 163 acres around its facility in Johnston County and filed permits for an expansion of its Durham County manufacturing facility, CBRE noted.
Webinar Opportunity! Next-Generation Genomic Sequencing

Two Webinars Offered by Southern Regional AHEC with Duke University
Southern Regional AHEC, in partnership with Duke University, is hosting a live webinar highlighting rare genetic diagnoses titled “Next-generation Genomic Sequencing for Rare Genetic Diagnoses: Engagement with Community Health Providers."
Program Description
For this interactive educational program, the objectives are two-fold. The first is to discuss current diagnostic approaches to patients presenting with clinical features suggestive of a genetic disorder and what are the “next steps” if clinical genetic testing does not result in a diagnosis for your patient. The second objective is to learn from providers about how important access to clinical genetics is to their practice, their experiences with referring patients to clinical genetics, barriers they have encountered as well as possible approaches to mitigating barriers.
Objectives
Upon completion of this program, participants will be able to:
- Identify genomic sequencing technologies, clinical applications, and interpretation of genomic sequencing.
- Discuss the benefits of genomic sequencing for patients and management of patients who undergo genomic sequencing.
- Identify patient phenotypes that would most benefit from genomic sequencing.
- Review the use of genomic information for direct patient care.
- Review barriers beyond clinical care that affect patients in rural areas participating in genetic evaluations in genomic sequencing.
- Analyze modalities that would improve access to genomic medicine for the patients
Speaker
Dr. Vandana Shashi is a board-certified Clinical Geneticist with over two decades of experience in rare/ultra-rare genetic disorders. She is the Principal Investigator of the NIH Undiagnosed Diseases Network (UDN) Clinical Site at Duke, wherein patients from all over the USA, with difficult to diagnose rare/ultra-rare diseases are evaluated for diagnostic purposes. Next- generation genomic sequencing (NGS) inclusive of exome and genome sequencing for diagnoses is a major focus of the UDN and under Dr. Shashi’s leadership the Duke UDN clinical site has been successful in diagnosing 40% of patients who had not been able to obtain diagnoses previously, with a consequent impact on medical management. Dr. Shashi is passionate about findings ways for patients with health disparities to also participate in the UDN. She looks forward to engaging with providers in rural NC to discuss cutting-edge genomic technologies for their patients with rare/ultra-rare phenotypes and to identify barriers that they perceive result in low participation by patients with health disparities.
For more information, including CME credits, click here.
Match Day is Coming Soon. Are You Ready?

Match Madness is March 15
(AMA, Brendan Murphy) -- For many medical students, creating a Match rank-order list is about balancing competing priorities and funneling advice—solicited and unsolicited—from faculty members, peers and resident physicians. That was the case for Haidn Foster, MD, when he was considering his options for the Match as a fourth-year medical student at the University of Cincinnati College of Medicine in 2022. In the end, Dr. Foster said, how one constructs a rank-order list is highly personal.
“The whole process is so individualized to what means most to you as an applicant,” said Dr. Foster during an interview for the AMA. “Somebody who interviewed at the same programs but had slightly different priorities for residency may make an entirely different rank-order list and be just as happy with the outcome of the Match as I was.”
In advance of the Feb. 28 deadline for residency applicants to submit their rank-order lists—and with the caveat that the process is going to come down to one’s own instincts and priorities—Dr. Foster offered a few key insights about how he created his list and what he might have done differently with the benefit of hindsight.
Think long-term

“For applicants who are similarly interested in subspecializing, there are a lot of benefits to matching at a program that has your desired fellowship in-house. As a resident, I wanted to get a better feel for my chosen field and learn what it would be like to practice as a hematologist-oncologist, so it was important for me to rank institutions highly that had an associated hematology-oncology fellowship,” he added.
“Future plans aside, as a resident you’ll be in training for at least the next three to seven years, so having a residency program that is both a good cultural fit and responsive to resident feedback—backed up by specific and meaningful examples of program adaptation—were also critical aspects of how I evaluated the programs I interviewed at.”
Make compromises
“I interviewed at a healthy mix of academic and community programs,” Dr. Foster said. “When it came to ranking each program, at times, I was conflicted because of the connection I felt with some of the community programs. I wanted to highly rank the programs that spoke most strongly to my values—those with a demonstrated commitment to diversity, equity, inclusion, and to serving the underserved.
“Still, knowing that I had very clear-cut career ambitions with regards to my plans for fellowship, I knew that I would be best served by matching into an academic program. So I found myself ultimately ranking some programs lower despite having a strong emotional connection to their philosophy and leadership.”
Know your deal-breakers
It is important to keep in mind which factors of a given program are deal-breakers for you, and which are not. What, in other words, can you live with for the duration of your residency? For Dr. Foster, geography was not a big factor in his rank-order list.
“I've had the perspective throughout medical training that I can live anywhere for a limited amount of time,” Dr. Foster said. “And so I was happy to move from my hometown near Seattle to Cincinnati for medical school, and then to move again to Pennsylvania for residency.”
Dr. Foster’s residency interviews were exclusively virtual due to the COVID-19 pandemic, but most interviews, post pandemic remain virtual. Having not visited a number of the schools with which he interviewed, there was a level of uncertainty in the process, he said.
“Some of the process is a leap of faith. I'd never been to Hershey. So that was a really interesting experience: matching to a program in a city I’d never visited, even signing a lease on an apartment sight unseen. It was all a real adventure, one that I’m thankful has turned out well.”
Draw on interview-day feelings
“One of the mistakes I made during interview season was not being diligent enough keeping notes on the day of an interview,” Dr. Foster said. “Especially because interviews are virtual and you may be interviewing at multiple programs per week, everything really starts to blend together. Trying to recall specifics of each program towards the end of interview season can be difficult if you haven’t recorded those details around the time of your interview.
“The standout programs—whether exceptional or otherwise—are easy to recall and rank accordingly. But having a record of day-of observations is incredibly useful when stratifying residencies that fall in the middle of the pack.
“Another helpful aspect of some programs’ interview process was the facilitation of one-on-one conversations with current residents. When I had specific questions about a program or wanted more information about what it would be like as a member of an affinity group at that institution, being able to ask residents their opinions outside of a group setting was invaluable.”
Don’t get bogged down in every detail
“One of the considerations I gave too much weight when interviewing was the specifics of the intern year schedule,” Dr. Foster said. “In my field, internal medicine, you are going to have very full days, very full weeks.
“The rigors of a 60-to 80-hour work week are going to be the reality of pretty much any residency program,” he noted. “And whether that's accomplished through a consistent inpatient schedule of a 6 a.m.–6 p.m. workday versus a regular day, short-call day, long-call day, all those specific details come out in the wash and are not as big of a deal as I thought they were going to be.”
Deam big
“The Match process truly prioritizes applicant preferences,” said Dr. Foster, an AMA member. “There is no downside to an applicant ranking their true No. 1 program as No. 1 in their rank-order list.
“Even if you feel like the odds of matching are low, ranking that program that’s perfect for you highly will not detrimentally impact your match,” he noted. “There is no gaming the system; just rank programs in the order that you actually prefer them.”
Set it—then forget it
“Personally, I took a long time to make my list,” Dr. Foster said. “But then I put it into the system and pressed ‘Certify’ and put it out of my mind. I think going back and changing things after certification would have just added more stress. Then there's the legitimate fear of forgetting a step and not hitting ‘Certify’ a final time.”
The AMA Road to Residency series provides medical students, international medical graduates and others with guidance on preparing for residency application, acing your residency interview, putting together your rank-order list and more.
Find the perfect Match
Podcast: Meet your Match step-by-step residency selection guide
Video: How to choose the best residency program for you
Specialty guide: Simplify your specialty selection for residency
As Nation Grapples with Alabama Decision on Embryos, An NCMS Member Speaks Out

Alabama Says Embryos in a Lab Are Children. What Are the Implications?
Scroll down for response from NCMS Member Dr. Amy Bryant
(NYT, Jan Hoffman) -- The Alabama Supreme Court has opened a new front in the legal debate over when human life begins. Embryos created and stored in a medical facility must be considered children under the state’s law governing harmful death, the court ruled.
Friday’s ruling was cheered by anti-abortion activists nationwide, who have long argued that life begins at conception. They were thrilled that, for the first time, a court included conception outside the uterus in that definition. But the strongest and most immediate effect of the decision will be on fertility patients trying to get pregnant, not women seeking to end their pregnancies.
The Alabama ruling invites states to enact strict new regulations over the fertility industry that could sharply limit the number of embryos created during a cycle of medical treatment and affect the future of millions of stored frozen embryos. A concurring opinion even offered road maps for such statutes. That could have a chilling effect on a person seeking to have children through in vitro fertilization, whether single or part of a same-sex or heterosexual couple.
What did the ruling say?
The ruling is actually somewhat narrow. It applies to three couples who had sued the Center for Reproductive Medicine, a fertility clinic in Mobile, for inadvertently destroying their embryos. The plaintiffs argued that they were entitled to punitive damages under Alabama’s 1872 Wrongful Death of a Minor Act. Two lower state courts disagreed, saying the embryos were neither people nor children. The State Supreme Court reversed those rulings, saying that the embryos fell squarely under Alabama’s definition of minors and that the negligence lawsuits could proceed. The case will now go back to the State District Court for further litigation.
What did the ruling not say?
The decision is silent on the fate of other frozen embryos in Alabama because that issue was not before the court. The ruling is only about the terms under which plaintiffs may bring a negligence case against a fertility clinic for embryo destruction. However, it could eventually have major consequences for Alabama patients and providers.
On Wednesday, the I.V.F. clinic at the University of Alabama at Birmingham announced it was pausing fertility treatments to explore the implications of the court’s ruling on its patients and providers. One fear is that the clinic, doctors and even patients may face daunting new liability issues surrounding the handling of embryos.
What will it mean for fertility patients and clinics?
“The honest answer is that we don’t know for sure,” said Dr. Paula Amato, president of the American Society for Reproductive Medicine, an organization that lobbies on behalf of fertility experts and patients. “But the ruling is very concerning.”
Freezing embryos is a widespread practice. During a standard cycle of in vitro fertilization, a woman takes hormones to maximize her production of eggs. A doctor then retrieves as many eggs as possible and injects them with sperm in the clinic’s lab, with the goal of creating viable embryos for implantation.
That process will often result in numerous embryos. Because of dangers associated with multiple births from I.V.F., protocols now urge doctors to implant only one embryo at a time. But success with implantation is hardly guaranteed, and so typically doctors freeze remaining embryos for subsequent attempts.
But if laws prevent providers in Alabama from freezing embryos, patients may face the medically challenging and financially draining prospect of many more cycles, Dr. Amato said. Success rates would most likely plummet. “It will disproportionately affect lower income people, people of color and people in L.G.B.T. communities,” she said.
Overall, according to federal data, infertility affects 9 percent of men and 11 percent of women of reproductive age in the United States.
The ruling may therefore restrict the ways that reproductive medicine is practiced in Alabama. “The ruling potentially criminalizes or sets a high civil penalty for standard procedures that we do every day,” Dr. Amato said.
Did the Alabama court suggest protocols for frozen embryos?
No. The court was clear that it could not regulate fertility clinics and the practice of reproductive medicine. But in a concurring opinion, Chief Justice Tom Parker strongly urged the Alabama legislature to examine the matter. He said that other countries, including Italy, New Zealand and Australia, limited the number of embryos that could be created as well as implanted, and suggested that states look to them for regulatory templates.
Is this case headed to the U.S. Supreme Court?
Not imminently, legal experts predicted. The clinic would have to appeal the decision, a move that could be risky, said Katherine L. Kraschel, an expert on reproductive law at Northeastern University School of Law. In light of the United States Supreme Court’s 2022 Dobbs ruling that overturned the national right to abortion, she said, the clinic’s chances at even getting to the door of the Supreme Court would be slender, “because the case hinges on a State Supreme Court’s interpretation of its own state statute.”
Lawyers for the clinic did not return requests for comment.
Also, the case is far from finished in Alabama. The State Supreme Court directed the parties to return to the district court to litigate the case in light of the new ruling, including the suggestion that other legal avenues be explored. One issue it identified was whether a clinic’s standard contract with fertility patients, which typically allows providers to donate or destroy embryos at some future point, could limit the clinic’s liability in this case.
Does all this have any effect on abortion?
In recent years, anti-abortion groups have been pressing for fetuses to be granted “personhood” status, which would entitle them to legal protections. In extending that umbrella to cover embryos in a lab, the Alabama Supreme Court employed reasoning that runs through the U.S. Supreme Court’s 2022 abortion ruling: that fetuses deserve a court’s shield under the 14th Amendment’s equal protection clause.
“The Supreme Court is making this bid to think about the fetus as a vulnerable, unprotected minority that courts are obliged to step in and protect, whether that is through upholding anti-abortion restrictions or moving forward toward accepting and recognizing the fetus as a person,” said Melissa Murray, an expert on reproductive law at the New York University School of Law.
Americans United for Life, the country’s oldest anti-abortion organization, was particularly encouraged by Alabama’s embrace of that theme.
“The Alabama Supreme Court held that the text of the Wrongful Death of a Minor Act is clear and applies to all pre-born children, including the plaintiffs’ embryonic pre-born children. In doing so, the Court correctly acknowledged the legal status of embryos as human persons,” Danielle Pimentel, the policy counsel for the organization, said in a statement. “This decision is a step in the right direction toward ensuring that all pre-born children are equally protected under the law.”
Dr. Amato said she found it ironic that anti-abortion groups were supporting rulings that could severely limit I.V.F.
“I.V.F. is about family building,” she said. “It should be viewed by red states as a pro-life activity.”

MSCR, At Large Member of the Executive Committee, NCOGS
Response to the ruling by NCMS member Dr. Amy G. Bryant, MD:
The Alabama Supreme Court's ruling will fortunately not affect North Carolina. But this ruling is deeply troubling because it gives medically unnecessary legal protections to frozen embryos. This will have a devastating impact on people seeking to grow their families using assisted reproductive technology, and could embolden other states to pass similar legislation. The tactics at play in this ruling are an overt attempt to control people who need this assistance to build their families, and are an extension of the tactics that place medically unnecessary restrictions on abortion. This ruling shows that anti-science politicians never intended on stopping at abortion. This new type of interference in reproductive healthcare exposes anti-abortion intentions to continue to restrict bodily autonomy, no matter the circumstances. Patients and physicians should be allowed to make decisions regarding their fertility based on their personal values and beliefs, not those imposed by the state.
If you would like to comment, please contact Randy Aldridge ([email protected]) to submit an article for the NCMS On Point Blog.
NCMS Political Pulse Introduces New VP of Advocacy John Thompson, SC Primary Results
Political Pulse is back!
As we wait for the legislative session to begin in April, the North Carolina Medical Society Political Pulse is kicking things off by getting to know our new Vice President of Advocacy, John Thompson. From his long professional career to his family and a very unique hobby, John is ready to share with you how he intends to make big changes at the NCMS this year.
The NCMS is committed to keeping you updated on 2024 election news. This weekend was the South Carolina Republican primary where former President Donald Trump defeated former SC Governor Nikki Haley. The next primary is Michigan followed by Super Tuesday (which includes North Carolina) on March 5. NCMS will update you periodically as the nation prepares for the general election in November.
https://youtu.be/aQeOrlQnjes
Join CMS for the Innovation in Behavioral Health Model Overview Webinar
IBH Model Overview Webinar
Thursday, February 29
2 - 3:30pm ET
The Centers for Medicare & Medicaid Services (CMS) will host a webinar on Thursday, February 29, to provide an overview of the Innovation in Behavioral Health (IBH) Model.
During this webinar, the IBH Team will discuss the model’s goals, eligibility, participant types, care delivery framework, and payment structure. The team will also provide additional details on the application process, timeline, and resources.
The IBH Model’s goal is to improve the quality of care and health outcomes for people with moderate to severe behavioral health conditions, including mental health conditions and/or substance use disorders. The model will test a value-based payment approach that enables community-based behavioral health practices to integrate behavioral health care with physical health needs and health-related social needs.
Following the event, presentation materials will be available on the IBH Model webpage.
Please contact the IBH Help Desk at [email protected] with questions.
First Comprehensive Evidence-Based Guideline on Use of Fecal Microbiota-Based Therapies
For use in patients with recurrent CDI at high risk of recurrence
The American Gastroenterological Association (AGA) has released the first comprehensive evidence-based guideline on the use of fecal microbiota-based therapies for gastrointestinal disease, recommending fecal microbiota transplant (FMT) in most cases of recurrent Clostridioides difficile infection (CDI).
Specifically, the guideline recommends the use of FMT-based therapy in patients with recurrent CDI at high risk of recurrence following standard-of-care antibiotics and in hospitalized patients with severe CDI after standard-of-care antibiotics if there is no improvement. Of note, the AGA does not recommend FMT therapies for inflammatory bowel disease (IBD) or irritable bowel syndrome (IBS).
“Using fecal microbiota transplant, we take stool from a healthy donor and transfer it to the colon of the person with recurrent C. diff, restoring balance to their gut microbiome,” Anne Peery, MD, associate professor of medicine and director of the adult inpatient nutrition support team at the University of North Carolina School of Medicine, said in a press release. “FMT is a safe and effective treatment with enough scientific evidence to be offered to most patients with two or more C. diff recurrences.”
Continue to full article here.
Reminder: Missed Opportunities for Preventing Congenital Syphilis Webinar is Wednesday

Missed Opportunities for Preventing Congenital Syphilis
Wednesday, February 28
Noon-1:00 p.m. ET
Join the Bureau of Primary Health Care (BPHC) in collaboration with Centers for Disease Control and Prevention, National Center for HIV, Viral Hepatitis, STD, and TB Prevention for a on Congenital syphilis webinar developed for clinicians and other health care providers.
This webinar will provide an overview of congenital syphilis and explore missed opportunities for preventing congenital syphilis as well as interventions for prevention.
Objectives of this presentation:
1) Understand the epidemiology of syphilis and congenital syphilis in the United States.
2) Diagnosis and counsel about syphilis and congenital syphilis.
3) Practical implementation of syphilis screening and treatment in the clinical setting.
4) Discuss missed opportunities to prevent congenital syphilis in the US and possible interventions.
For more information, contact: Chepkorir Maritim, Nurse Consultant, [email protected]
New CMS Vaccine Coverage and Payment Toolkit Offers Helpful Guidance

Understand federally funded Vaccines for Children program
This new CMS toolkit, Coverage and Payment of Vaccines and Vaccine Administration under Medicaid, the Children’s Health Insurance Program, and Basic Health Program (PDF), can help to understand coverage, cost-sharing, and payment for vaccines and vaccine administration.
The toolkit addresses the federally funded Vaccines for Children program and assists in navigating vaccination coverage requirements. This includes providing guidance regarding the commercialization of COVID-19 vaccines and the end of the American Rescue Plan Act COVID-19 vaccination coverage period (September 2024).