Vaccine and COVID Research, LGBTQ Studies Among NC Projects Hit by NIH Cuts

More than two dozen NIH grants have been canceled at North Carolina research groups, including Duke and UNC-Chapel Hill.
(The News & Observer, Drew Jackson and Brian Gordon) -- Nearly two dozen grants and millions in research dollars have been canceled at UNC-Chapel Hill, Duke University and other North Carolina institutions as part of the growing list of projects cut by the National Institutes of Health.
Since February, the Trump administration has taken the unprecedented step of canceling hundreds of active research grants at many of the country’s top health and medical institutions.
The national list of cuts to NIH has grown to 638 canceled grants, including 20 at North Carolina colleges and institutions. Another 700 grants have been cut by the Centers for Disease Control and Prevention.
The cuts follow a pledge President Donald Trump made in a February memo called “Radical Transparency About Wasteful Spending”.
“The American people have seen their tax dollars used to fund the passion projects of unelected bureaucrats rather than to advance the national interest,” Trump said in the memo.
Joining UNC-Chapel Hill and Duke among those impacted are UNC Charlotte, the North Carolina Department of Health and Human Services and the Research Triangle Institute.
The canceled grants largely focused on COVID-related research, gender, minority groups, climate research and overseas communities, topics the Trump administration has been critical of since returning to power. In all, the cuts total billions of dollars in federal funding for medical research.
UNC-Chapel Hill saw the highest number of grant cuts in the state, with funding canceled for 11 projects. Among those, funding dollars ranged from $40,441 for a study of addiction within the adolescent LGBTQ+ community, to $65 million for an effort to develop new oral antiviral drugs.
Each of the canceled grants at UNC-Chapel Hill focused on either COVID response, gender identity or minority topics.
The same was true for Duke’s canceled grants, with the largest, a $176 million project, studying the potential effectiveness of six different drugs on treating COVID. Included in that study was the effectiveness of Ivermectin against COVID-19.
Other Duke grants ranged from $116.6 million for COVID testing research and $28 million for general coronavirus vaccine development to $42,014 for a study of sexual health among of Black gay men.
To systematically end active awards is a departure for NIH, the world’s biggest public funder of biomedical research. In past years, the agency had canceled on average around 20 of its approximately 60,000 annual grants early for obvious fraud or potential harms.
“Terminating funding has previously been an uncommon action,” said Cat Long, research communications manager at UNC-Chapel Hill.
This past week, the Centers for Disease Control and Prevention announced it would be scaling back COVID-related funding, canceling more than $11 billion in funding to states.
In North Carolina, that means the department of health and human services will lose around $115.5 million in remaining funding. The department said this past week it anticipated cutting more than 80 jobs.
The funds were part of an $800 million package of COVID funding.
At RTI, two grants were canceled, totaling $250,000. One was intended to study the “Social influences on sexual health among Latinx adolescents and emerging adults who identify as LGBTQ+ in an agricultural community.” The other canceled RTI grant aimed to improve health regulations in Nigeria.
Given North Carolina’s stature as a national leader in research and public health, funding cuts have hit hard. At RTI, which is also affected by cuts to the U.S. Agency for International Development, there have been two rounds of layoffs since Trump returned to office.
Combined, Duke and UNC-Chapel Hill accounted for more than half of the nearly $2 billion in NIH funding North Carolina received in 2024. Driven by these two Research Triangle institutions, North Carolina saw the sixth-most NIH dollars of any state, outpacing its population ranking (No. 9).
Beyond specific grant cuts, other changes at NIH mean universities can expect even less funding. The NIH has put a cap on “indirect grant payments” at 15%, funding that typically covers facility and administrative costs.
In anticipation of these funding cuts, Duke implemented a hiring freeze earlier this month.
All About National Doctors' Day

NATIONAL DOCTORS DAY 2025
All About Doctors Day
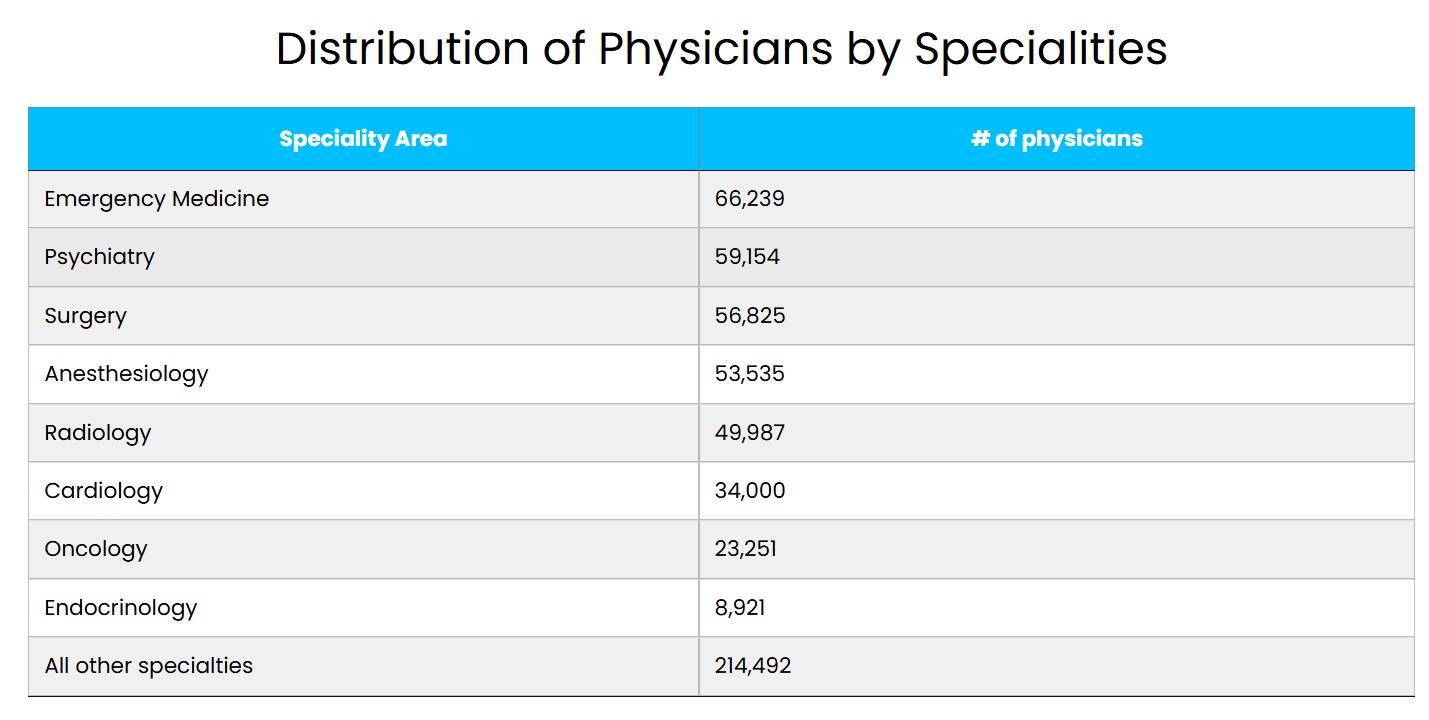
We celebrate National Doctors Day in America on March 30 each year, honoring the dedication and compassion displayed daily by more than one million physicians providing healthcare to patients nationwide.
These providers are the heart of the American healthcare system. In the US, doctors provide care to over 1 billion patients yearly, with an average of 3.2 doctor visits per person — 50% of those visits are made to a primary care physician. About 85% of adults and 95% of children in America visit with a doctor each year.
This country has had a persistent physician shortage in recent years, and the American Association of Medical Colleges predicts a shortage of up to 86,000 physicians by 2036. Our doctors are feeling the heavy demands placed on them daily by the healthcare industry. Most doctors work over 50 hours a week, and many work 80-plus.
If anybody has earned a day of appreciation, it is our doctors. Without their efforts and courage in the face of adversity, our country would be much worse for the wear. Without an adequate supply of doctors, healthcare systems are left with significant strain, leading to longer patient wait times, increased workloads for existing medical staff, and an overall reduced quality of care. In such scenarios, there’s often a greater reliance on locum tenens physicians and other advanced practice providers. We need doctors and want them to know how important they are to each of us.
NationalDoctorsDay.org is here as a resource, with tools to help healthcare staffing agencies celebrate and recognize their doctors. Join us by honoring the dedicated physicians who improve our lives this National Doctors Day, and utilize our marketing toolkit to facilitate your company’s marketing outreach to doctors and the healthcare industry.
A Brief History of Doctors Day
In 1933, Eudora Brown Almond, the wife of a family medicine physician, Dr. Charles B. Almond, felt doctors deserved a little extra recognition in American society for their extraordinary, life-saving, and often thankless work.
Almond turned to her fellow citizens in rural Georgia to send greeting cards to each of their physicians and lay flowers on the graves of late physicians. March 30 was not chosen at random. The day of observance for National Doctors Day was picked to commemorate the first use of anesthesia during surgery in 1842 by physician Dr. Crawford Long, a well-known doctor from Jefferson, Georgia.
On March 30, 1958, Congress adopted a resolution commemorating March 30 as National Doctors Day after the movement gained traction in the medical community over two decades.
In 1990, President George H.W. Bush designated National Doctors Day an official day of recognition by the US government. These days, doctors’ contributions are celebrated nationwide on March 30 and around the world by employers, coworkers, and patients of physicians.
Since National Doctors Day’s founding, the traditions once introduced by Almond to the Winder community have evolved a bit — from hand-written, personalized greeting cards to posts made on social media, where more and more people can show their appreciation for their physicians. Healthcare facilities and physician staffing agencies typically showcase their appreciation for doctors in digital and print marketing campaigns.
The medical field has changed vastly since National Doctors Day’s first celebration. An increasing number of women are pursuing careers in medicine. From 2004 to 2022, the active physician workforce saw a 97% increase in women, compared to a 13% rise in men. Physician diversity has also improved, with more medical students drawn to a broader range of specialties. By 2023, 23% of active physicians across all specialties were 65 or older.
Our doctors’ dedication has remained constant despite the changes in the medical community. Many doctors say that the connection they build with their patients is one of the most rewarding parts of their job. Physicians are entrusted to hold other human beings’ lives in their hands. As we navigate the evolving healthcare landscape, let’s use National Doctors Day to let doctors know we see them, appreciate them, and wholeheartedly support them.
Facts & Stats about Doctors
Here are a few facts and statistics about doctors in the United States that you might not know.
- Physicians played an important role in the formation of this country. John Morgan, Joseph Warren, the director general of the Medical Department of the US Continental Army, and Benjamin Rush were all pivotal figures in establishing medical practice in America. Rush actually signed the Declaration of Independence.
- John Morgan, who had earned his medical degree at the University of Edinburgh, founded the first medical school in the country, which is now part of the University of Pennsylvania.
- Before creating dedicated medical schools, doctors learned by apprenticeship.
- At the end of the Civil War, there were over 12,000 doctors in the Union Army and over 3,000 in the Confederate Army.here are currently over 1.1 million licensed doctors in the US; California has the most licensed physicians, with over 119,000.
- The average age of a doctor is 54, compared to a median age of 42 across other professions.
- 72% of doctors say they are satisfied with their profession. In 2024, physician burnout rates dropped to 48%, the first time below 50% since 2020.
- Women account for about 38% of active physicians, an increase from 26% in 2004.
- According to the most recent Bureau of Labor Statistics Data, the average salary of physicians and surgeons across all specialties is $239,000 a year
- About 52,000 doctors work as locum tenens physicians across the US.
- Doctors typically see 11-20 patients a day.
- According to the most recent AAMC data, 20,855 US medical school students graduated in 2024.

NCMS Member Dr. Damian McHugh Pens Letter: Reflections on National Doctors' Day

Courtesy of the Curi Blog:
Whether or not you subscribe to the popularity of nationally recognized days or weeks for almost anything you can think of, they certainly do exist for our awareness and consumption. These registered days range from the fun and whimsical (National Spanish Paella Day, anyone?) to the more educational and serious, like National Skin Barrier Day, recently celebrated on March 12, and National Health Workforce Well-Being Day celebrated on March 18. One significant standout, though, and one I am proud to reinforce each and every year is National Doctors Day.
National Doctors Day is celebrated annually on March 30 and honors the numerous and varied contributions of my peers. Notation of it was first made March 30, 1933. It flags the date of the first usage of general anesthesia in major surgery by Dr. Crawford Long, way back in 1842. It became officially recognized as a day of appreciation when George H.W. Bush designated it as such in 1990.
Why celebrate our nation’s doctors and designate a day for them?
Well, firstly they deserve it. Before seeing their very first paying patient, most of these dedicated young individuals give up the best years of their lives to study, to tramp the corridors of hospitals day and night, and to sit and be taught by those they are learning how to help and heal. Delayed gratification and delayed “real earnings” happen in the arduous years of Residency and Fellowship. With debt typically north of $300,000, the nervous first-year attending and newly minted medical graduate sets out on their official career pathway somewhere around age 30.
I typically ask new acquaintances, new business contacts, and new colleagues, “What’s your why?” If you know your why, you will find the how. So many of Curi’s member-owners that I get to spend time with knew they were lightworkers at an early age and wanted to train, learn, invest, and grow themselves into a force for good—for the betterment of our country and our broader humanity.
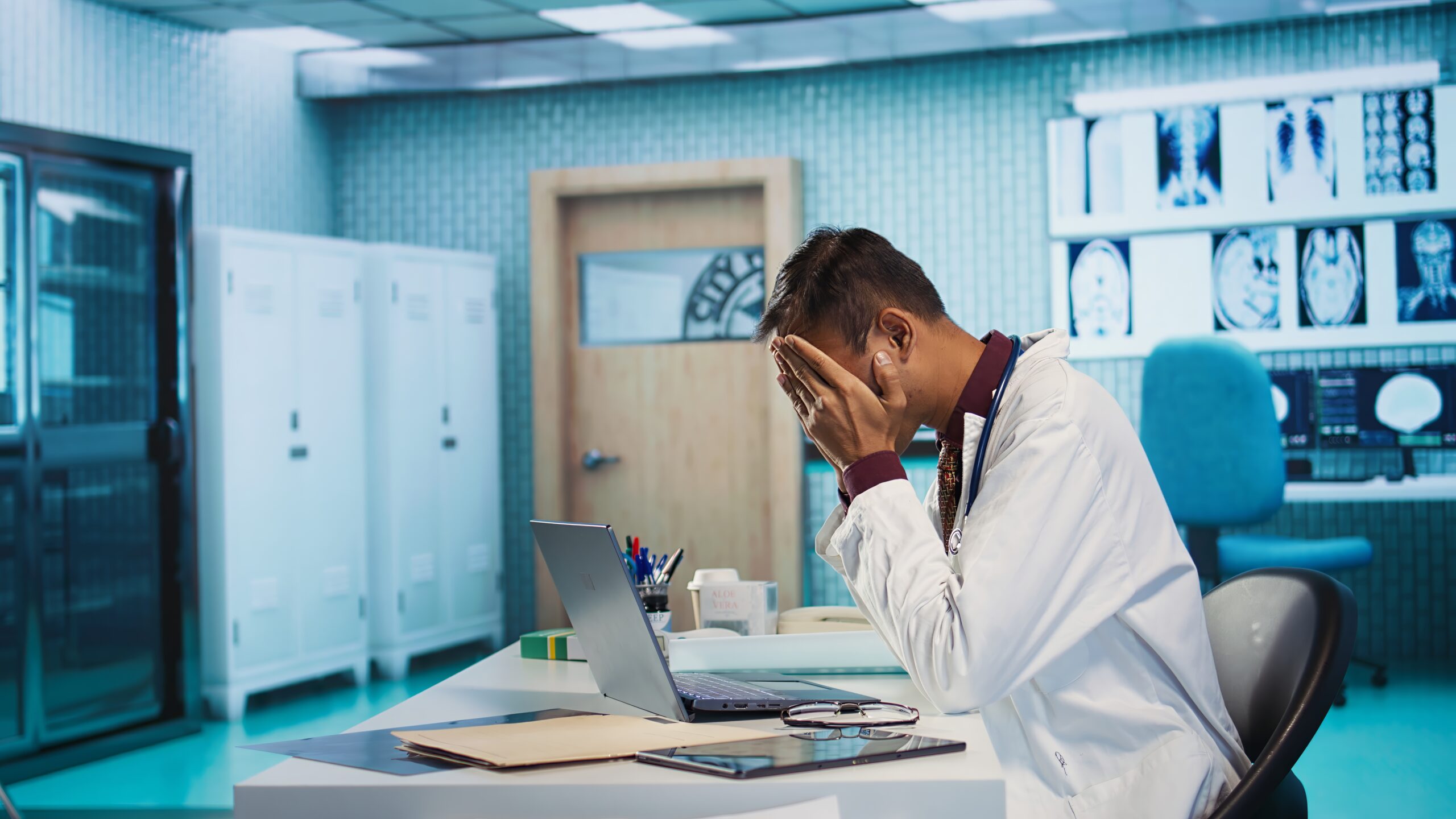
Over the last quarter millennium, we have seen a darkening of the light that burned in these lightworkers. A jaded response to becoming commoditized. An indignant, actually angry retort to a system where for-profit payers and their pharmacy benefit managers call all the shots and erode the autonomy which we once enjoyed as a profession. Wendy Dean coined the term “moral injury.” She plucked that from military medicine, and so many physician leaders agree with her that this is now endemic and eating away at our healthcare system. The Surgeon General confirmed his agreement of the term in the New England Journal of Medicine in 2022:
“Burnout manifests in individuals, but it’s fundamentally rooted in systems. And health worker burnout was a crisis long before Covid-19 arrived. Causes include inadequate support, escalating workloads and administrative burdens, chronic underinvestment in public health infrastructure, and moral injury from being unable to provide the care patients need. Burnout is not only about long hours. It’s about the fundamental disconnect between health workers and the mission to serve that motivates them.”
The terms depression, burnout, and moral injury are simply constructs of physician distress. They culminate in a dilemma that has no actual solution. The term, “wicked problems,” was coined in the 1960s to describe that class of social system problems which are ill-formulated, where the information is confusing, where there are many clients and decision makers with conflicting values, and where the ramifications in the whole system are thoroughly confusing.
The U.S. healthcare system is plagued with complex inter-related wicked problems. If you don’t or can’t believe me, start following one of the many excellent physician threads on LinkedIn and follow some passionate doctors who care enough to disrupt, but always in a polite and positive fashion.
My message and humble request for doctors as we note National Doctors Day is three-fold:
- Despite the ever-increasing headwinds, please try to do the next right thing. Please strive to serve the patient in front of you and not the insurer on the card they carry.
- Build relationships with both patients and colleagues, to support and enjoy one another. This requires the commitment to make social connection a priority and the courage to be vulnerable and truly real and honest with each other.
- Seek out your County or State Medical Society. Attend specialty society meetings and stay an extra couple of days. Go back to our mosques, synagogues and churches or just to our school halls and ball fields.
In his departing prescription, Surgeon General Dr. Vivek Murthy states, “Today, we are faced with a profound choice. Do we continue with the status quo marked by pain, disconnection, and division? Or do we instead choose a different path, the one of joy, health, and fulfillment where we turn toward each other instead of away from each other, where we choose love over fear, when we recognize community as the irreplaceable foundation for our well-being?” In completing his tenure as Surgeon General, his final wish for all of us was the same as mine: choose community.
Curi is proud to be a vibrant part of your community, and we salute you and your teams on National Doctors Day.
🎉It's New Member Monday!🎉

Join us in welcoming these new members to the North Carolina Medical Society!
- Bradley W. Alsip, PA-C
- Maximiliano M. Cavallini Martin, MD
- Sean R. Costello, DO
- Michael P. Cowherd, MD
- Stefano Crosio, DO
- Mili Dave
- Ankita S. Desai, MD
- Erin E. Dunneback, MD
- Raisa J. Durrani, MD
- Jeffrey Foster
- Matthew Greene, PA-C
- Neelam J. James, DO
- Richard T. Kiok, MD
- Adam Z. Kline, MD
- Stanley E. Koontz, Jr., MD
- George D. Kryder, MD
- Amanda R. M. LaBenne, MD
- Kathryn M. Langley, MD
- Jackeline C. L. Larker, DO
- David Lehrburger, BS
- Yasmeen M. Mansour, MD
- Lauren P. Marino, MD
- Divyesh Mehta, MD
- Rodrigo D. Munoz Dayaa, MD
- Ravyn S. T. Njagu, MD
- Reece N. Nuessmeier, PA-C
- Evan A. Plunkett, MD
- Lincoln F. Pratson, II, MD
- Anish Raj, MD
- Katy L. Reines, MD
- Andrew J. Sampson, MD
- Nicolette M. Schreiber, MD
- Katherine S. Schroeder, MD
- Shivani R. Sheth, PA-C
- Lisa M. Spencer, MD
- Ricci St Jules, DO
- Benjamin W. Topper, DO
- Luis M. Vazquez-Montesino, MD
- Daniel P. Waddell, PA-C
- Rukiayah A. Warner-Moxley, MD
- Sebastian A. Werner, MD
- Keith G. Whitlock, MD
- Tyler D. Williams, DO
- Chloe Worner, PA
We are thrilled to have you!
Not a member but would like to be? Joining is simple. Visit our membership center here.
NCMS is Sending Match Day Congratulations!
The North Carolina Medical Society congratulates all the new graduating medical students on their Match Day success!
Daniel van Rooyen will continue to serve Harnett County through the Campbell University Harnett Health Family Medicine Residency. He completed his undergraduate and master’s degrees at Campbell University and will graduate from Campbell University School of Osteopathic Medicine in May.


Look for more Match Day successes soon!
A Message from Western Carolina Medical Society Six Months After Hurricane Helene
Six Months That Changed a 140-Year-Old Institution
Western Carolina Medical Society (WCMS) started in 1885, but, in many ways, it has been “reborn” since Hurricane Helene hit western North Carolina. The agency, which serves as the philanthropic arm of more than 670 physician assistant and physician members, has long been known for Project Access, a program that coordinates free specialty healthcare for individuals ineligible for Medicaid with no other insurance. Over the years, more than $95 million in free care has been arranged through the program.
“WCMS has five incredible programs,” notes Karen Wallace-Meigs, executive director of the nonprofit organization. “We have Project Access, our signature program, but we are also proud of WIN, the largest interpreter network in western North Carolina. CRCSI, the Colorectal Cancer Screening Initiative, is a vital WCMS’ program, as is a scholarship program named in memory of Dr. Charles Blair for high school seniors who complete an internship at MAHEC. Another initiative is the Healthy Healer Program, through which we offer six free, confidential therapy sessions to physician assistant and physician members.”
So, how did the aftermath of Hurricane Helene change the agency? “It added greater urgency to our work. Existing needs were exacerbated, and more people needed our help,” says Wallace-Meigs, who had been on the job less than four months when the storm hit. As soon as each WCMS staff member was accounted for - some on the staff of ten were displaced to far-flung places -they jumped into action, picking up a sixth program: emergency relief to meet pressing Social Determinants of Health Needs.
From September 27, 2024, until today, the WCMS team has:
- Enrolled 153 patients in Project Access while streamlining the application process.
- Made 375 referrals for free, specialty medical services valued at hundreds of thousands of dollars and added new care providers to their roster.
- Donated:
- Rent Assistance: $21,000
- Groceries: $13,750
- Utilities: $5,800
- Medical (bills and Durable Medical Equipment): $4,400
- Transportation: $700 in gas cards to area Federally Qualified Health Centers so patients could reach their appointments
- Provided translation services at 2,722 appointments so patients and providers could understand and pursue the best possible treatments.
- Made scores of free, confidential Healthy Healer therapy appointments for healthcare provider members.
- Distributed dozens of pieces of donated durable medical equipment, boxes of Benadryl, and wasp repellent.
“We did what we needed to do, like many agencies and neighbors,” Wallace-Meigs asserts. “It was challenging emotionally and physically. Our work continues, but we are coming through it as a more responsive, nimble, determined agency. None of this would have been possible without the generosity of so many partners, and my team, which refused to give up on each other or our community.”
For more information about the Western Carolina Medical Society Foundation, contact Niki Duff, Director of Development & Communications, at [email protected] or visit www.mywcms.org.
Register Now! Webinar on Tools to Manage Measles Outbreaks Effectively

Join South Piedmont AHEC (part of NC AHEC) for a FREE live webinar to gain critical insights and practical tools for managing measles outbreaks effectively.
-
Apr 10, 2025 | 12:00 PM - 1:00 PM EST | Live Webinar
Description
Measles is a highly contagious viral disease that can lead to severe health complications. Join us for an in-depth panel discussion where we will explore the critical aspects of measles management tailored specifically for healthcare
professionals. Our distinguished panel of experts will share their extensive knowledge and provide valuable insights on effectively handling measles cases, addressing vaccine-related questions, and implementing effective infection control practices. This session is designed to equip healthcare providers with the essential knowledge and practical tools necessary to manage measles outbreaks and ensure patient safety
This session promises to be an invaluable resource for healthcare professionals seeking to enhance their understanding and management of measles. Don't miss this opportunity to learn from leading experts and improve your practice in the face of measles outbreak
Speakers
Katie Passaretti MD,
Chief Infection Prevention Officer Advocate Health,
Clinical Professor Infectious Diseases Wake Forest
Amina Ahmed MD,
Medical Director Pediatric Infectious Disease and Immunology Levine's Children's Hospital, Pediatric Director Hospital Epidemiology, Professor Pediatrics Wake Forest
Shelley Kester MHA, BSN, RN, CIC, CPHQ,
Enterprise Infection Prevention Lead, Advocate Health
Erica Wilson MD, MPH,
Medical Director, Medical Consultation Unit, Epidemiology Section, Division of Public Health, North Carolina Department of Health and Human Services
Click here for more information and to register
The Life of a Medical Board Complaint
The NC Medical Board Wants to Demystify the Process When a Complaint is Filed
The life of a Medical Board complaint
Imagine checking your email and finding a message indicating that you are the subject of a complaint to the North Carolina Medical Board (Board). While no licensee of the Board wants to receive such a message, knowledge of the Board’s investigatory process may help reduce the stress and anxiety related to the experience. It should be noted that in most Board investigations, the Board’s case review process determines that there is not evidence of misconduct or substandard care.
This article will walk you through the life of a Board complaint from start to finish, to demystify the process and provide you with information to respond appropriately, should the need arise.
Step 1: Information received
The Board is a complaint-driven organization that receives information from a variety of sources, the largest of which is complaints from patients and the public. Staff carefully review each complaint to determine if there is a possible basis for Board action in the form of a violation of the NC Medical Practice Act, the Board’s authorizing statute. In a typical year, staff determine about one in four patient complaints do not allege actionable misconduct or they allege matters outside the Board’s jurisdiction, and the matter ends there with no further investigation. Licensees are notified of ALL complaints but are only asked to respond if the Board investigation advances. You should never ignore a request for information – failure to respond to a Board inquiry is itself a basis for the Board to take disciplinary action, and the licensee’s written response is your first chance to tell your story and ensure that the Board has enough information to understand what occurred.
Step 2: Investigation
Next, Board staff will investigate the allegations. If the case involves the quality of medical care provided, staff review the licensee’s statement, the medical records and, when appropriate, an outside medical review by a medical professional who practices in the same specialty as the licensee, to determine whether care met accepted standards. In some instances, a Board investigator may also seek to interview you and others involved in the case. If you have any doubt about whether you are being contacted by a legitimate agent of the Board, contact the Board by telephone at 919-326-1100 and ask to speak with the Investigations Department.
Step 3: Senior Staff review
At this stage, a committee of senior staff members that includes representatives from the Office of the Medical Director and the Investigations and Legal Departments review the results of the investigation and recommend a possible resolution for each case. If senior staff find insufficient evidence of a violation, the case is closed without further action, and the licensee and complainant are notified. If senior staff determine the case involves one or more violations, they will recommend the Board take either public or private action to resolve the case and submit those recommendations for review by members of the Board.
Step 4: Board review and case resolution
The Board’s Disciplinary Committee reviews all cases in which private or public action is recommended. Board Members who serve on the Committee may accept the staff
recommendation, recommend something new, or request more information. The Board does not decide cases lightly and has the authority to extend an investigation if it does not feel it has a clear understanding of what occurred.
Once the Board votes on a case, the licensee is notified of the resolution. If public action is authorized, Board attorneys negotiate the specific terms of the case resolution with the licensee or, if applicable, their attorney. If the licensee refuses to accept the authorized case resolution, they have the right to a hearing, which is a process similar to a trial, with a panel of Board Members sitting as judges. The Board strongly encourages licensees to obtain counsel to advocate for their interests, but it is ultimately up to you to decide.
At the end of the day, each case is decided on its unique facts and circumstances. Where discipline or remediation is called for, the Board favors a targeted approach to ensure any concerns are addressed fairly and the public is protected.
NCMS in the News: WRAL Posts Story on Possible Changes to Healthcare Rules

RALEIGH -- As nurses gathered in downtown Raleigh, a news station was on hand to cover the event. WRAL Capitol Bureau Chief Laura Leslie covered the story, including reaction from the North Carolina Medical Society.
Additional reading:
NC DHHS to Cut 80 Jobs, Lose $100 Million in Federal Funding

The North Carolina Department of Health and Human Services’ reductions are due to the federal government’s “abrupt and immediate termination of several federal grants,” a department spokesperson said in a statement.
(WRAL) -- The North Carolina Department of Health and Human Services is planning to cut 80 jobs and will lose more than $100 million in funding.
The reductions are due to the federal government’s “abrupt and immediate termination of several federal grants,” a department spokesperson said in a statement.
The cuts are part of the Trump administration cutting $12 billion in federal grants to state health services.
The U.S. Department of Health and Human Services on Thursday said it would eliminate 10,000 more jobs as it restructures. Overall, the agency, which is responsible for monitoring infectious diseases, inspecting foods and hospitals and overseeing health insurance programs for nearly half the country, says it will decrease its workforce from 82,000 to 62,000 positions. That includes 10,000 in layoffs as well as another 10,000 workers who are taking early retirements or buyout offers that were given to nearly all federal employees by the Trump administration.
The $100 million North Carolina is losing in funding directly contributes to the “health, safety and wellbeing of the people we serve,” the NCDHHS spokesperson wrote.
Specifically, the federal grant funding impacts several areas of work, including immunization efforts, funding for the new NC Immunization Registry, infectious disease monitoring and response, behavioral health, substance use disorder services and more. Some of the impacted funding supports work that is done by local health departments, universities, hospitals and local departments of social services.
The NCDHHS is also putting impacted vendors on notice to pause work supported by the funding.
NC AHEC Needs Your Help Assessing AI Adoption Across the State

Survey Should Take 10 Minutes to Complete.
As artificial intelligence (AI) continues to evolve at a rapid pace, organizations across disciplines are exploring its opportunities, challenges, and impact. To better understand the current AI landscape, NC AHEC is conducting a high-level environmental scan, gathering insights from a diverse range of stakeholders and partners like you.
This survey aims to assess the state of AI adoption, key trends, opportunities, and concerns across academia, practice, and regulatory bodies. Your input will help us develop a clearer picture of how AI is being utilized today and where it is headed in the near future. We will share high-level themes and key findings to help inform ongoing discussions in this space while keeping individual response confidential.
The survey should take approximately 10 minutes to complete. Thank you for your time and insights—we appreciate your participation!
Click here to complete survey.
New Research: Chewing Gum Can Shed Microplastics Into Saliva

Pilot Study Could Burst Your Bubble on Chewing Gum
(CNN) -- Are you keeping a mental list of all the sources of microplastics finding their way into your daily life? You may have another culprit to consider: It’s gum, according to a new pilot study that found chewing just one piece can release hundreds to thousands of microplastics into saliva.
The study is currently being peer-reviewed and will be presented at the biannual meeting of the American Chemical Society in San Diego Tuesday. Once the review is complete, the authors hope the report will be published in the Journal of Hazardous Materials Letters later this year.
“Our goal is not to alarm anybody,” said senior study author Dr. Sanjay Mohanty, associate professor at the Samueli School of Engineering at the University of California, Los Angeles. “Scientists don’t know if microplastics are unsafe to us or not. There are no human trials. But we know we are exposed to plastics in everyday life, and that’s what we wanted to examine here.”
Microplastics are fragments of polymers that range in size from less than 0.2 inch (5 millimeters) to 1/25,000th of an inch (1 micrometer). Plastics smaller than that are considered nanoplastics, which are measured in billionths of a meter.
Polymers are chemical compounds with long chains of large and repetitive molecular units called monomers, which are known for durability and flexibility. Most plastics are synthetic polymers, whereas natural polymers include cellulose from plants. Chewing gum typically contains synthetic or natural polymers for better texture, elasticity and flavor retention, the authors said.
Microplastics enter the body via ingestion and inhalation, according to previous research, and scientists have discovered their presence in various body parts or fluids including the blood, lungs, placenta, brain and testicles. That’s why the authors said they wanted to identify other possible sources of microplastic ingestion and their concentrations.
“Chewing gum is one of the foods we chose because it is the only food where plastic polymer is used as an ingredient,” Mohanty told CNN via email. “Other foods are contaminated with microplastics because of how they are processed and packaged.”
To the authors’ knowledge, their study is the first “that examined or compared microplastics in chewing gums available commercially,” Mohanty added.
Isolating microplastics from gum
The team’s findings are based on 10 gums popular in the United States. Half of the samples were synthetic, and the other half were made with natural ingredients.
Most, if not all, gum product labels and websites do not disclose what their gum base includes nor how they are processed. This lack of transparency also leaves researchers “no way to know where and how microplastics came into the gums we tested,” Mohanty said — and no way for consumers to know the full composition of the gums they are buying.
One human participant would chew a gum for four minutes; during that time frame, every 30 seconds a researcher collected the secreted saliva in a centrifuge tube.
The participant then rinsed their mouth three to five times with highly purified water, and the researchers mixed the rinse sample with the saliva sample to ensure all microplastics in the mouth were captured. This entire process was repeated seven times for each gum.
Some gums were chewed for 20 minutes total with saliva collected every two minutes, so the team could determine how the number of microplastics shed depended on the chewing time.
To identify the types and amounts of microplastics in gum, the authors used various methods of filtration and chemical analysis such as microscopy. The research team also subtracted microplastics found in an initial rinse sample from those in the chewing gum saliva samples to accurately estimate the number of microplastics released from chewing gum.
Analysis revealed that just 1 gram of chewing gum released approximately 100 microplastics on average, with 1 gram of some gums releasing as many as 637 microplastics. A typical stick of gum can weigh anywhere from 1 gram to several grams, according to various reports.
Additionally, 94% of microplastics were released within the first eight minutes of chewing.
The authors were surprised to find that chewing natural gums didn’t really make a difference. The average number of microplastics in 1 gram of synthetic gum was 104, and in natural gum it was 96.
Both types also predominantly released four types of synthetic polymers: polyolefins, polyterephthalates (or polyethylene terephthalate), polyacrylamides and polystyrenes. These are some of the same plastics used in everyday plastic consumer products, Dr. Tasha Stoiber, senior scientist at the Environmental Working Group, a nonprofit environmental health organization, said via email. Stoiber wasn’t involved in the research.
“That microplastics were released is not unexpected,” said Dr. David Jones, a teaching fellow in the School of the Environment and Life Sciences at the University of Portsmouth in England, via email. Jones wasn’t involved in the study.
“If we subject any type of plastic to stress, be it heat, friction, sunlight, seawater, or in this case vigorous mastication, we know that microplastics will be released from the plastic material,” Jones, also founder and CEO of the marine conservation charity Just One Ocean, added. “We inhale, ingest and drink something like 250,000 plastic particles a year without trying. … But at least we now have some robust data and it is a good starting point for further research.”
“Gum is safe to enjoy as it has been for more than 100 years,” the National Confectioners Association said via email. The trade group has member companies that make and sell gum. “Food safety is the number one priority for U.S. confectionery companies, and our member companies use only FDA-permitted ingredients.”
What’s unknown about gum microplastics
The average size of gum microplastics was 82.6 micrometers — think the thickness of paper, or the diameter of some human hairs. The chemical analysis tools used in the study can’t identify particles smaller than 20 micrometers, Mohanty said.
This constraint means the findings missed any smaller microplastics and nanoplastics and therefore may be underestimates, said Dr. Leonardo Trasande, director of the New York University Center for the Investigation of Environmental Hazards, via email. Trasande wasn’t involved in the study.
Why synthetic polymers were found in the natural gums, too, is also questionable, experts said. But polyolefins are commonly used in the food industry for packaging, so this could be a reason why, the authors said.
The unexpected finding may also occur if manufacturers use polymers when they shouldn’t, if there was a lab contaminant or if there was a measurement error, Dr. Oliver Jones, a professor of chemistry at RMIT University in Australia, said in a statement released by the Science Media Centre. Jones wasn’t involved in the study.
“As producers rarely report the composition of gums, it is difficult to ascertain the source of microplastics found in natural chewing gums,” they added.
Also, some of the polymers — such as polyterephthalates, often found in water bottles — identified in the synthetic gums aren’t known to be present in synthetic gums in general, Dr. David Jones of the University of Portsmouth said.
Some regulatory agencies have taken the stance that there is no need to be concerned about microplastics in food and water since there isn’t evidence that they cause harm, he said.
“This is totally the wrong approach. We should be taking the precautionary approach and assume that they do,” he added. “We need to be investing in research to understand how this will impact on our health now so that we can start to mitigate the consequences.”
Even if any potential effects on the human body are unknown, the study does put into perspective the other ways chewing gum can contribute to environmental pollution when inappropriately discarded, experts said.
Make Your Plans Now to Attend 3rd Annual Smoky Mountain Primary Care Conference

Smoky Mountain Medical Society 3rd Annual Primary Care Conference is April 26
The event is being held at the beautiful Lake Junaluska and features sessions on weight loss medications, rheumatology, POTS, and psychiatry.
The day long event includes breakfast and lunch with exhibitors and a long list of faculty on hand.
Registration is open. Click here for more information and to register.
NC AHEC Announces Quality Improvement Course for Practice Managers

Quality Improvement Course Starts April 3
Target Audience
Practice managers or leader-providers who are knowledgeable or experienced in other areas of practice management but desire an introduction to the basics of quality improvement.
About the Practice Manager Bootcamp
The Practice Manager Boot Camp (PMBC) is part of the NCAHEC Practice Management Academy. It is designed for the novice practice manager, but experienced practice managers that want to fill gaps in their knowledge of practice management will also benefit, as well as providers who want to learn more about practice management. The PMBC has six virtual modules: financial management, insurance and the revenue cycle, leadership, human resources and customer service, operations management and quality improvement. To accommodate the needs of busy practice managers, sessions are presented live and made available as recordings. The Practice Management Academy’s mobile app makes it easy for you to learn any time or any place that works for you.
Program Description
This completely virtual course is a module of NCAHEC Practice Management Academy’s Practice Manager Boot Camp (PMBC). In this module, you’ll learn quality improvement concepts and skills that will help your practice not only survive but thrive.
Click here for full course outline and to register.
MIPS Penalty Can be Avoided Due to Impact of Hurricane Helene

MIPS penalty can be avoided due to impact of Hurricane Helene
In response to AMA advocacy urging CMS to hold physicians harmless from Merit-based Incentive Payment System (MIPS) penalties as a result of the nationwide IV fluid shortage and to reopen the MIPS Extreme and Uncontrollable Circumstances (EUC) hardship exception, the agency announced that it will accept new applications to avoid a MIPS penalty. We greatly appreciate CMS for recognizing that physicians and their patients continue to face hardships due to the nationwide shortage of IV fluids exacerbated by Hurricane Helene in September 2024 and a severe winter respiratory season leading to lower supply and increased demand for these drug products.
Physicians will be able to submit an EUC hardship exception application between March 31, 2025, and April 14, 2025, to avoid a MIPS penalty of up to -9% if they were affected by the shortage. This hardship exception will apply to the 2024 performance period, which will adjust Medicare payments in 2026. To avoid a MIPS penalty, physicians who were affected by the IV fluid shortage should submit an EUC application requesting reweighting of all four MIPS categories – quality, cost, promoting interoperability, and improvement activities. Note that CMS will not reweight any performance category for which the agency has received data. However, if three performance categories are reweighted to 0% and only one performance category can be scored, then the physician or group will earn a final score equal to the performance threshold and avoid a MIPS penalty. Additionally, because the MIPS cost performance category relies entirely on claims-based measures that do not require submission from physicians or groups, we recommend requesting reweighting of this category if a physician or group needed to conserve IV fluids, use alternatives, restrict access to elective surgery or take any other measures due to the nationwide IV fluid shortage. In addition, CMS is extending the MIPS data submission window for the 2024 performance period for two weeks from March 31, 2025, until April 14, 2025, at 8 pm ET. More information is below.

2024 MIPS Data Submission Deadline Extended and EUC Applications to Reopen in Response to National IV Fluid Shortage
In response to the ongoing national intravenous (IV) fluid shortage, the Centers for Medicare & Medicaid Services (CMS) will reopen the 2024 Merit-based Incentive Payment System (MIPS) Extreme and Uncontrollable Circumstances (EUC) Exception Application to provide relief to practices impacted by the IV fluid shortage.
- The application will reopen Monday, March 31, 2025, at 10 a.m. ET, and will close April 14, 2025, at 8 p.m. ET.
- CMS is reopening the 2024 MIPS EUC Exception Application window in response to the national IV fluid shortage; therefore, CMS will only accept applications citing the shortage as the basis for requesting reweighting under the MIPS EUC Exception. Any applications submitted for reasons outside of the national IV fluid shortage will be denied.
CMS is also extending the MIPS data submission deadline until April 14, 2025, at 8 p.m. ET.
- IMPORTANT! The deadline for certain clinicians, groups, and Alternative Payment Model (APM) Entities to elect to participate in MIPS – because they are opt-in eligible due to the low-volume threshold or are partially qualifying APM participants (Partial QPs) – is still March 31, 2025, at 8 p.m. ET.
This announcement includes details about the following information:
- 2024 MIPS Data Submission Deadline
- Who Can Submit a 2024 MIPS EUC Exception Application Now?
- What If We’ve Already Submitted Some Data?
- How Do I Apply?
- Additional Resources
2024 MIPS Data Submission Deadline Extended to April 14, 2025
MIPS eligible clinicians and their representatives can submit and update their MIPS data until April 14, 2024, 8 p.m. ET. We encourage submission of data as early as possible in advance of this extended deadline.
Please note: This extension will delay the mid-June timeline for releasing final scores and opening Targeted Review.
Opt-in Eligible Clinicians and Groups
- Opt-in eligible clinicians and groups exceed 1 or 2, but not all 3 of the MIPS low-volume threshold criteria.
- Opt-in eligible clinicians and groups who want to report MIPS data must complete their opt-in election by March 31, 2025, at 8 p.m. ET. (Data must be submitted by April 14, 2025, at 8 p.m. ET.)
- No action is required for opt-in eligible clinicians and groups who don’t want to report MIPS data.
- Learn more in the 2024 MIPS Opt-In and Voluntary Reporting Election User Guide (PDF, 2MB).
- Partial QPs received at least 40% of Medicare Part B payments or saw at least 25% of Medicare patients through an Advanced APM Entity during the 2024 QP performance period (January 1 - August 31).
- Partial QPs who want to report MIPS data and get a MIPS payment adjustment must complete their Partial QP election by March 31, 2025, at 8 p.m. ET. (Data must be submitted by April 14, 2025, at 8 p.m. ET.)
- No action is required from Partial QPs who don’t want to participate in MIPS.
- There’s information about Partial QP elections in the 2024 APP Data Submission User Guide (PDF, 3MB, pp. 21 – 24) and 2024 Traditional MIPS Data Submission User Guide (PDF, 3MB, pp. 34 – 37).
Who Can Submit a 2024 MIPS EUC Exception Application?
Individual MIPS eligible clinicians, groups, virtual groups, and APM Entities participating in MIPS (including Shared Savings Program Accountable Care Organizations) affected by the national IV fluid shortage will be able to submit a 2024 MIPS EUC Exception Application between March 31, 2025, 10 a.m. ET and April 14, 2025, 8 p.m. ET. They can apply to request reweighting for any or all MIPS performance categories.
For example, you may need to apply if your practice’s administrative and support staff has needed to focus on supply chains to support patients’ care, affecting their capacity to collect and prepare data for reporting.
What If We’ve Already Submitted Some Data?
Individuals, groups, and virtual groups: We won’t reweight any performance category for which we’ve received data.
However, if 3 of the performance categories are reweighted to 0% and only one performance category can be scored (e.g., because the MIPS eligible clinician, group, or virtual group submitted data for that category), then the MIPS eligible clinician, group, or virtual group will earn a final score equal to the performance threshold and the MIPS eligible clinician(s) will receive a neutral payment adjustment.
For example:
- A MIPS eligible clinician in a small practice reported Medicare Part B claims quality measures during the performance period, resulting in a quality score. Because we’ve received data, we won’t reweight the quality performance category.
- If the other 3 performance categories are approved for reweighting to 0% (and no data was submitted for the improvement activities or Promoting Interoperability categories), the quality performance category would be weighted at 100% of the final score, resulting in a final score of 75 points (the performance threshold).
APM Entities: Data submission for an APM Entity won’t override performance category reweighting.
- If approved, the MIPS eligible clinicians in the APM Entity will receive a score equal to the performance threshold and a neutral MIPS payment adjustment in the 2026 payment year unless the MIPS eligible clinicians had a higher final score (for the same TIN/NPI combination) from individual or group participation.
When the 2024 MIPS EUC Exception Application reopens on March 31st, you’ll take the following steps:
- Sign in to the QPP website.
- Select ‘Exceptions Applications’ on the left-hand navigation.
- Select ‘Add New Exception’.
- Select ‘Extreme and Uncontrollable Circumstances Exception’.
- Complete the application.
When the application reopens, you MUST select “National IV Fluid Shortage” as the Event Type and include the impact to your practice in the Event Description.
If your application is approved, you can still submit data should circumstances change before the submission deadline.
Additional Resources
- Please note that we’re still working to update the QPP website and resources to reflect this information.
- We’ll release an updated 2024 MIPS EUC Exception Application User Guide with additional screenshots by the end of March when we announce that the application has reopened.
For More Information on PY2024 MIPS Data Submission
Review the following submission resources are available on the QPP Resource Library:
- 2024 Traditional MIPS Data Submission User Guide (PDF, 3MB)
- 2024 MVPs Data Submission User Guide (PDF, 4MB)
- 2024 APP Data Submission User Guide (PDF, 2MB)
- 2024 QPP JSON Templates and Instructions (ZIP, 856KB)
- 2024 CMS Web Interface User Guide (PDF, 5MB)

Spring is Here: North Carolina Ranks as One of the Toughest States for Seasonal Allergies

Raleigh is ranked as the 7th most challenging place to live in America with allergies, while Greensboro is ranked 10th
(The Carolina Journal, Brianna Kraemer) -- America’s list of the most challenging places to live with seasonal allergies.
Raleigh is ranked as the 7th most challenging place to live in America with allergies, while Greensboro is ranked 10th. Several other major North Carolina cities, including Durham, Charlotte, and Winston-Salem, are included in the report as places with significant allergy issues. The North Carolina cities are all considered to have worse-than-average seasonal allergies.
For the third year in a row, Wichita, Kansas, is the most challenging city for pollen allergies.

“The burden of seasonal allergies falls heavily on the southern and eastern parts of the country,” the report states.
Spring in North Carolina brings abundant pollen starting in late February, especially from trees, grasses, and weeds, making it tough for residents with allergies. The worst months for allergies in North Carolina are April for tree pollen, May for grass pollen, and September for weed pollen, according to Allermi.
The daily pollen forecast currently indicates high levels across most of the nation as warmer weather arrives.
The AAFA’s report factors in pollen scores, use of over-the-counter medications, and availability of allergists, all of which paint a challenging picture for North Carolinians in the spring.
On the opposite end, Boston, Massachusetts, and Salt Lake City, Utah, are ranked as the least challenging places to live with allergies.
Duke Doctors Perform First Living Mitral Valve Transplant

Doctors saved the lives of Journi Kelly, Margaret Van Bruggen, and Kensley Frizzell by transplanting Kelly's original mitral valves — after she received a full heart transplant — to Van Bruggen and Frizzell.
HealthDay News — In a groundbreaking series of surgeries, doctors at Duke Health have successfully performed the world’s first living mitral valve replacement, saving the lives of three young girls across North Carolina.
The procedure became possible after 11-year-old Journi Kelly, from Wilson, N.C., received a full heart transplant at Duke.
Instead of getting rid of her original heart, doctors saved two healthy valves and transplanted them into two other children.
One valve went to 14-year-old Margaret Van Bruggen, a cross-country runner from Charlotte, N.C., who urgently needed a mitral valve replacement after a severe bacterial infection.
The other valve went to 9-year-old Kensley Frizzell, from Pembroke, N.C., who was born with a genetic condition called Turner’s syndrome that can cause heart defects. She had already endured multiple heart surgeries.
Currently, children who need heart valve replacements receive either preserved non-living tissue or mechanical valves, which don’t grow with the child and often fail within months.
“There’s not a good valve option for kids,” said Dr. Douglas Overbey, assistant professor of surgery at Duke University School of Medicine in Durham, N.C.
“They all require multiple surgeries, and we know they’re going to fail down the road,” Overbey added in a news release. “That’s something that’s really hard to talk to parents about, knowing that you’re going to have to do the same surgery with a new valve, maybe six months later because they’re going to outgrow it.”
Duke’s new approach — called partial heart transplant — uses living valves from donated hearts, giving children valves that can grow with them, potentially reducing the need for future surgeries.
Since pioneering the technique in 2022, Duke has now performed 20 partial heart transplants under U.S. Food and Drug Administration guidance.
Journi’s journey began when she was rushed to Duke after sudden heart failure.
She was placed on the transplant list, and her parents were asked if they would consider donating parts of her old heart after her transplant.
“They explained to us that they could use the healthy parts of it to help other kids. Our next question was, ‘Where do we sign?’ ” Rachel Kelly, Journi’s stepmom, said.
When a donated heart became available for Journi, her original valves were found to be perfect matches for Margaret and Kensley.
For Margaret, the valve transplant came just in time.
After developing a serious bacterial infection called endocarditis, large holes formed in her mitral valve, and her health began to decline fast.
“She was in the hospital, and we could’ve lost her,” Margaret’s mother, Elizabeth Van Bruggen, said in a news release. “But she was so brave, so I knew I had to be brave too. She’s got a lot left to give the world.”
For Kensley, whose heart condition was tied to Turner’s syndrome, the transplant could mean the end of a long series of heart surgeries.
“We were expecting she would need surgery, but we never knew this would be an option,” her father, Kenan Frizzell, said. “The whole situation is extraordinary, whether you look at it from the standpoint of a scientific breakthrough or the average person’s point of view. I can’t imagine all the coordination that’s needed for something like this to take place, but as one of the families that benefited, we can’t be anything other than grateful.”
Wake County to join medical experts, community partners for Ask the Doc town hall series

March and April events to provide sessions in Spanish, English and Arabic
Wake County’s health equity initiative, HealthLit4Wake, is bringing back its popular Ask the Doc: A Wake County Town Hall series for 2025, providing residents with direct access to medical experts and essential health information.
Kicking off the quarterly series, the first event – Pregunte Al Doc: Navigating Primary Healthcare – will take place Wednesday, March 26, from 11 a.m. to noon at the Mexican Consulate, 431 Raleigh View Road, Raleigh. Conducted entirely in Spanish, this session is designed to make crucial healthcare guidance accessible to Wake County’s Spanish-speaking community.
“These town halls are an important step in making sure every resident, regardless of language or background, has access to the information and resources they need to stay healthy,” said Wake County Commissioner Cheryl Stallings. “By hosting sessions in various locations and in multiple languages, we’re breaking down barriers and making county services more inclusive.”
Pregunte Al Doc: Navigating Primary Healthcare
Wednesday, March 26, 11 a.m.–noon
Mexican Consulate, 431 Raleigh View Road, Raleigh
Moderator: María Sánchez, El Centro Hispano
Panelists:
- Dr. Edwin Burkett, MD, Alliance Medical Ministries
- Claudia Rivera, BSN, RN, Wake County Public Health
- Adriana Guerra, RN, Wake County Public Health
- Vanessa Valencia, FNP, Urban Ministries/Open DoorThe event is presented in partnership with El Centro Hispano, The Mexican Consulate, and Ventanilla de Salud.
April Events: Ask the Doc continues in English and Arabic
- Ask the Doc: Chronic Stress
Saturday, April 12
Noon–1:30 p.m.
WellCare Annual Health Fair, 1100 Raleigh Blvd., Raleigh - Ask the Doc: Nutrition and Mental Health
Saturday, April 19
Noon–1 p.m. (Arabic session), 1–2 p.m. (English session)
Muslim Youth and Community Center, 5017 Deah Way, Raleigh
The series will continue throughout the year, offering expert-led discussions in multiple languages on topics that matter most to Wake County residents. Future events will be announced at wake.gov/AsktheDoc.
Ask the Doc Town Halls
Ask the Doc began in 2021 amid COVID-19 as a way for the public to virtually connect with health professionals to understand the changing landscape of the pandemic. Since then, Ask the Doc has moved to in-person events and specialized events tailored to reach our most vulnerable residents.
Hosted quarterly, each session features a panel of local medical professionals who share their expertise and engage with residents to address pressing health concerns.
New Study: Babies form fleeting memories

The human hippocampus constructs short-lived memories from around 1 year of age
(Science) -- When you think of your first memory, it’s probably not from the day you were born. But that’s not because babies are incapable of forming memories; it’s because people have trouble retrieving those early memories later in life, according to a new study.
To study “infantile amnesia,” the researchers went straight to the source: They analyzed MRI brain scans of over two dozen infants between 4 and 24 months old, taken as the little ones were shown a series of images. After the first round of images, the infants then saw two images side by side — one they hadn’t seen before and one they had.
The team recorded activity in the hippocampus, the part of the brain associated with emotions and memory. They also tracked their eye moments, zeroing in on which image the babies looked at longer, something that indicates a level of memory recall. “Infants look at what they find interesting, and researchers have long leveraged this spontaneous behavior to derive information about memory functioning,” Simona Ghetti, a psychology professor at the University of California, Davis, who was not involved in the study, explained to CNN.
The study takeaway: Babies can indeed encode memories, with the hippocampus becoming more active once a baby is 12 months or older — and the reason we cannot retrieve these memories later may simply be due to our adult brains not being able to access them. “This can remind parents that infancy is not idle time,” Ghetti said, “and that infants are learning a great deal.”
Register Now for UNC Eye Symposium
The UNC Eye Symposium is hosted by the UNC Department of Ophthalmology every April at the William & Ida Friday Center for Continuing Education in Chapel Hill, NC. Offering CME credits to attendees, this annual conference provides updates to Ophthalmologists, Optometrists, Ophthalmic Technicians, and Photographers on the latest evidence-based diagnostic and medical/surgical approaches to comprehensive eye care and treating ocular disorders and disease.
Mark your calendars to join us at this year’s UNC Eye Symposium on Saturday, April 12th, 2025. Email [email protected] for more information on the conference agenda, arranging overnight accommodations nearby the Friday Center, etc.
* Physicians (MD, OD): Click HERE to register.
* Ophthalmic Technicians/Photographers: Click HERE to register.
Agendas: 2025 UNC Eye Symposium (Physicians & Technicians)

Click HERE to read more on our 2025 UNC Eye Symposium
Leadership & Distinguished Guest Speakers!
3 NC Cities Among Highest in Country for STD Rates

CDC STI Surveillance Statistics Point to Continuing Struggle in the South
(Innerboody, CDC, Charlotte Observer) -- For our 8th annual study of STI rates, using the latest data published by the Centers for Disease Control and Prevention (CDC), Innerbody Research analyzed statistics on a city-by-city basis and developed our list of the Top 100 metropolitan areas with the highest STI rates. In this year's report, the metro area with the highest overall STI rate was Detroit, MI, overtaking Philadelphia, PA, which moved to 2nd. Memphis, TN, which had formerly been ranked 2nd, improved to 4th this year, while the metro area that came in 3rd last year — Jackson, MS — improved to 12th in 2025. At the same time, Montgomery, AL (formerly ranked 7th) worsened to 3rd.
In addition to ranking the 100 metro areas with the highest STI rates, below we'll provide some takeaways from our report; spotlight urban communities whose STI rates have significantly improved or declined; highlight racial disparities that emerge from the CDC data; and, for the first time in years, share analysis of some encouraging developments.
Quick takeaways
- The South continues to struggle with high infection rates in its metro areas, though there is evidence of positive change.
- Topping our annual study for the first time is Detroit, MI.
- For the second straight year, Provo, UT, comes in 100th, with 99 metro areas having worse STI rates.
- Could the tide be starting to turn in our STI epidemic? Infection rates are near their record-high levels over the past 20 years, but unlike recent years, this year shows a slight decline of nearly 2% in the overall infection rate.
- Despite hopeful signs of improvement in overall national figures, STI rates continue to reveal disturbing disparities that deserve reflection and action, and there is significant room for improvement in all respects as our nation continues to confront the epidemic.
Notable movement or stability in rankings
Detroit, MI, was ranked 9th worst for STI rates last year, but in this year's study, it has unfortunately earned the distinction of the metro area with the highest infection rates. In our years of conducting these studies, Detroit has never before ranked number one. This also comes during a year in which our nationwide list of the hardest-hit metro areas included almost 30% more places located in Detroit's Census-designated region (East North Central U.S., which includes the states of Michigan, Wisconsin, Illinois, Ohio, and Indiana). Motor City has confronted daunting, highly publicized challenges over the past decade and has exhibited great resilience and spirit; we hope that next year's study shows a Detroit that has rebounded and risen back upward in our rankings.
Other cities joining Detroit in our top 25 are also located in the Great Lakes region. For instance, in neighborhing Ohio, Cleveland finds itself ranked 13th, which reflects a slight worsening of relative infection rates from last year when it ranked 15th. But elsewhere in the Midwest, Minneapolis, MN, which ranked 17th last year, improved its ranking to 21st in our study this year. And Milwaukee, WI, escaped the top 25 altogether to rank 29th among U.S. metro areas.
The South, as defined by the U.S. Census Bureau, remains relatively fraught with high STI rates in its metro areas this year (more on that below).
Meanwhile, out west, our study shows evidence of improvement in metropolitan STI rates. San Francisco, CA, and Portland, OR, remain in the top 25 for the second year in a row, though their ranks have improved by a couple positions. But more broadly, fewer cities in the West are found within the top 50 worst cities for infection rates, and the total number of top 100 cities that are located in the West dropped from 31 to 25.
It's also worthwhile to call out a city for remaining remarkably stable in our study, year after year. For the second straight year, Provo, UT, has ranked 100th. And prior to that, it ranked 99th.
The South fights high infection rates
The U.S. South — a region that is home to roughly 39% of the population — accounts for over 60% of the top 25 metropolitan areas with the highest STI rates in this year's study. But, believe it or not, that's actually a slight improvement over last year's study.
The number of Floridian cities in the top 100 has slightly increased, though Miami has improved relative to other cities, ranking 19th now instead of its previous 16th.
Gulf states, in particular, are heavily represented in our top 25 metro areas, accounting for over a third of them. Louisiana alone is home to three of the 25 cities with the highest STI rates, though Montgomery, AL, has jumped several positions and leapfrogged New Orleans, LA, to become the city with the 3rd highest rates. A look into the state-level data from the CDC reveals similar trends seen in the data for major metropolitan areas: seven of the top 10 states with the highest gonorrhea infection rates are located in the South, and the South contributes eight of the top 10 states with the highest rates of chlamydia infection.
However, some metro areas are bucking regional trends. Jackson, MS, which ranked 3rd worst in last year's study, improved its rank to 12th this year -- a dramatic turnaround for a city that has been plagued by high infection rates for several years in our annual studies. And Little Rock, AR, which had the 11th highest STI rates last year, improved its ranking significantly to 27th.
Is the tide turning in this epidemic?
According to the latest data from the CDC, overall STI rates in the United States actually dropped by 1.8% in 2023 compared to 2022. The national infection rates had trended upward for the better part of two decades leading up to the COVID-19 pandemic. This year's updated data from the CDC gives reason for hope that concerted effort and investment may be helping turn the page at last.
- Nationally, the gonorrhea infection rate dropped by 7% compared to the previous year.
- The rate of chlamydia infection remained effectively unchanged, which still signifies a 9% drop since 2019.
- A 1% increase in overall syphilis infections represents a much slower rate of increase than the staggering 29% increase seen in the previous year-over-year analysis.
Despite the improvement, however, we continue to face an epidemic that requires renewed commitment to maintain improvement and achieve greater momentum (which is what compels us to create our annual study). While a drop of nearly 2% in the national STI rate is something to celebrate, this rate remains 90% higher than it was in 2004. What seems like a scant 1% increase overall in the syphilis infection rate still translates to the highest levels of syphilis infection in our country since 1950.
And hiding beneath that 1% statistic are alarmingly high rates of congenital syphilis. Congenital syphilis cases nationally rose only by about a tenth of the amount they had risen in prior years, yet cases among newborns did rise by 3% since 2022 and by 106% since 2019. Despite the slowing of this surge, these stratospheric rates caused 279 stillbirths and infant deaths over the past year.
And within the overall population, certain groups continue to face disproportionate challenges when it comes to curbing STI rates.
Social and racial disparities
Across racial groups, young people and men who have sex with men (MSM) contend with higher STI rates. A staggering 48% of the total cases of chlamydia, gonorrhea, and primary and secondary syphilis occurred among young people ages 15-24.
But social and racial disparities persist; the STI burden within our cities continues to hit minority racial and ethnic groups the hardest. When comparing infection rates of White people to those of some minority racial and ethnic groups, the CDC data shows dramatic disparities.
- Non-Hispanic Black people make up 12.6% of the U.S. population but suffer 32.4% of the cases of chlamydia, gonorrhea, and primary and secondary syphilis.
- The rate of chlamydia infection in the Native Hawaiian / Pacific Islander racial group, according to the latest Census data, is over three times higher than that among White people.
- The rate of gonorrhea infections among Black / African American males is over eight times the rate among White males.
- The rate of congenital syphilis infections within the Hispanic/Latino population is more than double that of White people, and the infection rate among non-Hispanic Black people is higher still — nearly four times higher than the rate among White people.
- American Indian / Alaska Native populations face congenital syphilis rates nearly twelve times higher than those of the White population in our country.
Health leaders stress that differences in sexual behavior aren't the explanation for these differences in rates of infection. What can spell the difference between life and death, or illness and health, are timely testing and treatment — but it has to be both. Nearly 90% of newborn syphilis cases are preventable through testing and treatment during pregnancy.
Barriers to timely testing and treatment include lack of health insurance; poverty and housing issues; substance use disorder; and lack of sufficient public health infrastructure. All of these factors continue to affect minority racial and ethnic groups disproportionately.
3 NC Metro Areas Land in Top 100
Three North Carolina metro areas landed in the top 100 cities in the U.S. with the highest STD infection rates, according to a recent study.
Greensboro ranked No. 30 on the list, followed closely by Charlotte at No. 37. Raleigh was ranked lower on the list at No. 67.
No. 30 Greensboro: With 1,086 cases per 100,000 people, Greensboro reported:
- 206 HIV cases
- 9,297 chlamydia cases
- 3,901 gonorrhea cases
- 413 syphilis cases
No. 37 Charlotte: With 1,014 cases per 100,000 people, Charlotte reported:
- 407 HIV cases
- 16,440 chlamydia cases
- 7,238 gonorrhea cases
- 692 syphilis cases
No. 67 Raleigh: With 770 cases per 100,000 people, Raleigh reported:
- 248 HIV cases
- 11,013 chlamydia cases
- 4,297 gonorrhea cases
- 448 syphilis cases
Click here for the full report
Click here for the full CDC STI Statistics
Plan Now for NCPHP Physician Suicide Prevention Workshop
Join NCPHP for an important workshop on physician suicide prevention:
April 16, 2025 | 6:00 pm | Asheville, NC
Coming Soon! Applications for the Collaborative Care Management Capacity Building Fund
Collaborative Care Management (CoCM) Capacity Building Fund
APPLICATIONS OPEN APRIL 1 FOR PHASE 2
Applications remain open for Phase 1
The NC General Assembly has earmarked $5 million for capacity building for Medicaid-enrolled primary care practices across the state to adopt Collaborative Care Management (CoCM). The NCDHHS Division of Mental Health, Developmental Disabilities, and Substance Use Services (DMHDDSUS) is contracting with Community Care of North Carolina (CCNC) to manage the program in partnership with North Carolina Area Health Education Centers Practice Support coaching.
CoCM is an evidence-based behavioral health integration model designed to support primary care clinicians in assessing and treating patients with mild to moderate behavioral health conditions. An evidence-based model shown to be more effective than usual care, CoCM improves patient outcomes, increases satisfaction for both patients and providers, and reduces healthcare costs and the stigma related to mental health and substance use disorders.
A primary care practice entity applying on behalf of multiple primary care practice sites may receive a maximum of three awards per entity. Phase 1: Each clinic site may be eligible to receive awards of $50,000 to begin a CoCM model in-house. Phase 2: Additionally, $30,000 is available for practices to expand an existing in-house CoCM model and $20,000 is available to practice sites meeting Phase 1 eligibility, but planning to outsource staffing to a third-party, turn-key CoCM company.
Phase 2 application process will open on April 1, 2025 and Phase 1 will remain open.
For more information about this program, visit CCNC's webpage on CoCM capacity building fund. And, to see past recordings and slides on CoCM Capacity Building Fund webinars, click here.
CARE FIRST Act Gains Dozens of Co-sponsors, Rep. Tim Reeder Has a New Message

NCMS Past President Representative Timothy Reeder, MD, is a sponsor of the CARE First Act.
House Bill 434 is gaining traction in the General Assembly quickly. Since the initial introduction of the CARE FIRST Act, the bill has garnered 57 co-sponsors along with the four original sponsors.
Click on image of Dr. Reeder for a message to all our members and health professionals across the state:
For more on the CARE FIRST Act click here.
Bill to Study Medically Assisted Death Filed in NC

MAID is legal in 10 states and District of Columbia
(WGHP, Emily Mikkelsen, Gretchen Stenger, Dolan Reynolds) -- A bill filed in the North Carolina House of Representatives would fund the study of medically assisted death.
HB410, titled “Medical Aid in Dying,” was filed on Tuesday. The bill directs the North Carolina Institute of Medicine to study the impacts of legalizing medically assisted death.
“Medical aid in dying (MAID) is a recognized end-of-life (EOL) option for terminally ill, mentally competent adults who have been diagnosed with a life expectancy of less than 6 months to hasten the dying process,” the bill says.
The bill directs NCIOM to “study the advantages and disadvantages of legalizing medical aid in dying (MAID) in North Carolina.”
It also directs NCIOM to look at factors that impact MAID, such as:
- The factors that contribute most to a person’s decision to seek MAID.
- The characteristics and demographic backgrounds of persons who seek MAID.
- The social and emotional impacts on a person’s family members when MAID is available to a person as an alternative to an extended dying process.
- Which medications have been or are currently being used for MAID, and whether intravenous self-administration would be an improvement over self-ingestion through the gastrointestinal tract.
- The best options for healthcare providers to opt out of participating in MAID.
- Available data from the current MAID states that are reporting on conclusions arising from the legalization of MAID, particularly with respect to the effectiveness of MAID laws in providing an end-of-life option.
- What end-of-life options are currently available in North Carolina and recommendations about whether MAID is an advisable additional alternative.
- To what extent the absence of MAID in North Carolina and other states increases the chance that a terminally ill person will choose to commit suicide by violent or other means.
Additionally, NCIOM would study advancements in MAID since the “Death with Dignity Act” passed in Oregon, develop a hypothetical number of how many people may choose to use MAID based on data available from other states, and the impact on healthcare systems in states where MAID is already legal.
The NCIOM would be required to hold at least one public hearing “to ensure the general public has an opportunity to provide the NCIOM with comments regarding the advantages and disadvantages of legalizing MAID” before submitting a report to lawmakers, which is due by April 1, 2027. The bill would appropriate $150,000 to fund this study, if passed.
MAID is legal in California, Colorado, Hawai’i, Maine, Montana, New Jersey, New Mexico, Oregon, Vermont, Washington and Washington D.C. It’s been legal in Oregon for the longest amount of time, since 1994.
Reps. Pricey Harrison (D-Guilford), Donny Lambeth (R-Forsyth), Julia Howard (R-Davie) and Lindsey Prather (D-Buncombe) are the primary sponsors of the bill.
Advocates Speak Out
The bill looks at the process patients go through in other states to be approved for the medicine.
“Usually it’s six months … You can’t have a mental disability which would include dementia. You have to be of sound mind to make this decision yourself,” Harrison said.
Edmund Tiryakian is the founder of a non-profit in Orange County called Dying Right.
He studies how other states like Oregon help patients and then uses that information to help guide people here in North Carolina
“The one thing we really want to emphasize is we … strongly discourage suicide. If you work in this area, you hear horrible stories where people have an answer. They’re in excruciating pain through the futility of continuing, and they take matters into their own hands violently, and that is a terrible, terrible end of life,” Tiryakian said.
Tiryakian says it gives patients options but only if they can do it themselves.
“Death with dignity … requires that person to have the physical wherewithal to take the drink. It’s a five-drug cocktail. With a straw, they will then suck up the medicine on their own,” Tiryakian said.
If the patient cannot do it on their own, it is against the law for anyone to help. That would be referred to as euthanasia.
NCMS Past President Dr. Devdutta Sangvai Nomination to Lead NCDHHS Clears Key Senate Committee

Gov. Josh Stein's choice to run DHHS was sworn into office in January
(NC Newsline, Lynn Bonner) -- Dr. Devdutta Sangvai received unanimous support Wednesday to run the state’s health care agency from a key state Senate committee.
Sangvai is Gov. Josh Stein’s choice to run the state Department of Health and Human Services. His nomination will eventually move to a vote of the full Senate.
Sangvai was sworn into office in January and has been doing the job leading DHHS.
Before coming to the state agency, Sangvai was president of Duke Regional Hospital. In addition to his medical degree, he has an MBA and a law degree.
Sangvai fielded fewer committee questions than he did at last week’s meeting, where he was pressed on what advice he’d give Stein in a health emergency where disease is spread by close contact.
In his response to another question about that hypothetical event on Wednesday, Sangvai said he’d advise the governor, and conversations would “have to involve all relevant stakeholders.”
Sangvai was also asked about a proposal over which DHHS has no say — the ability of advanced practice nurses to work without supervision from a doctor.
Advanced practice nurses have been trying to free themselves from the supervision requirement for years. Many have said that supervision often amounts to doctors periodically signing paperwork. Doctors’ groups say it’s important for doctors to keep their supervisory roles.
Sangvai said there is room for compromise. Though it’s not an agency decision, DHHS would be happy to provide input, he said.
Sen. Gale Adcock (D-Wake), said she hoped Sangvai would use the connections he’s built throughout his career in the state to help foster an environment that will lead to a compromise on the advanced practice nurse issue.
CCNC CEO Dr. Tom Wroth Talks Primary Care
Pulse on Carolina Health, Episode 2: Primary Care at a Crossroads: Challenges, Changes & the Value-Based Model in North Carolina

Primary care is evolving in North Carolina. Host Robert Shaw talks with Dr. Tom Wroth, CEO of Community Care of North Carolina (CCNC), about the state of primary care in North Carolina and its intersection with value-based care. They discuss primary care challenges, changes over the last decade, the impact on patient care, independent medical practices’ benefits, and how the shift to a value-based care payment model is reshaping primary care. LISTEN HERE.
Dr. Wroth shares insights on how CCNC—the nation’s largest and longest-running medical home system—has reduced healthcare costs while improving outcomes. Learn how value-based care is reshaping primary care and why independent practices may offer better value, continuity and comprehensive care for patients.
Stay tuned for episode 3, where industry leaders will tackle the pressing challenges in today's complicated healthcare system.
Follow Pulse on Carolina Health on your favorite podcast app.
New Study: NC in Top 10 Best States to Practice Medicine

NC ranks sixth in nation for doctors to practice medicine
(WNCN and WalletHub) -- North Carolina is the sixth best state for doctors in the nation, a new study has found.
The study, released Tuesday by WalletHub, is based on 19 metrics, including opportunity and competition, medical environment, average annual wage for physicians, punitive state medical boards, malpractice award payout per capita, and annual malpractice liability insurance.
According to the study, North Carolina ranks:
- 2nd in medical environment
- 2nd in malpractice award payout amount per capita
- 14th in projected physicians per capita by 2023
- 15th in annual wage of physicians
- 17th in average monthly starting salary of physicians
- 19th in annual malpractice liability insurance rate
- 20th in punitiveness of state medical board
- 21st in hospitals per capita
- 24th in opportunity and competition
North Carolina holds a total score of 61.18, according to the study.
The study found Montana is the best state for doctors. Indiana, South Dakota, Iowa, and Utah round out the top five.
Oregon, New Jersey, District of Columbia, Rhode Island, and Hawaii are the bottom five, according to WalletHub.
700+ Rural Hospitals at Risk of Closing

Millions of Americans at risk of losing community care
(Healthcare Brew and CHPQR, Cassie McGrath) -- About 768 rural hospitals in the US are at risk of closing, with 315 at “immediate risk” of closing within three years.
That’s according to a new report by healthcare finance policy organization the Center for Healthcare Quality and Payment Reform (CHQPR), which cited ongoing financial challenges like reimbursement rates for services as the problem. Texas, Oklahoma, Kansas, and Mississippi were identified as the states with the most (more than 20) at-risk hospitals.
In other words, the math just isn’t mathing to pay hospitals what they say they need.
The problem? It’s more expensive to provide acute care for patients in rural communities.
For example, there may be fewer emergency department (ED) visits due to there being fewer patients living in the area, but the cost to staff the ED remains the same as operational costs increase. And, according to trade group the American Medical Association, 65% of rural areas lack primary care access.
CHQPR said private health plans also don’t pay enough to keep the hospitals financially stable so they can deliver care.
“Although the at-risk hospitals are losing money on uninsured patients and Medicaid patients, losses on private insurance patients are the biggest cause of overall losses,” the CHQPR report read.
Rural hospitals reportedly have less than half the median profit margin of urban hospitals, according to a 2017 study from Johns Hopkins Bloomberg School of Public Health.
Continuing care. Last month, Jackson Hospital in Montgomery, Alabama, filed for Chapter 11 bankruptcy, citing low reimbursement rates as one of its challenges.
Grants from the government and local tax revenues have helped these hospitals stay afloat, according to CHQPR, but these funds aren’t guaranteed. As a result of that financial uncertainty, since 2005, 195 rural hospitals have closed and more than 1,000 have cut inpatient services.
Hospital closures can create access problems for patients, especially if there are no other providers nearby. It can also have an economic impact, Sarah Hohman, director of government affairs for the National Association of Rural Health Clinics, told Healthcare Brew, as people are “not interested” in living in areas without access to healthcare. For example, per capita income may decrease between 2.7% and 4% after a rural hospital closure, according to a 2023 study.
“Unfortunately, the [insurance] plans have a lot more leverage at the negotiating table than our small clinics do, and so what that results in is lower and lower [Medicare Advantage] reimbursement,” Hohman said.
CHQPR called on Congress in the report to require Medicare Advantage plans to pay rural hospitals the same as Medicare plans do.
“Private insurance companies and public insurance programs need to make significant changes in both the amounts and methods they use to pay for rural hospital services in order to prevent more rural hospitals from closing in the future,” the report read.
Additional reading:
NCMS - Martin County Seeks Operator to Bring Rural Hospital Back to Life
CDC Issues Update on Measles Outbreak in US and Guidance for Travel Season

CDC issues HAN Health Advisory to notify clinicians and travelers about measles outbreak
CDC and Health Alert Network -- The Centers for Disease Control and Prevention (CDC) is issuing this Health Alert Network (HAN) Health Advisory to notify clinicians, public health officials, and potential travelers about a measles outbreak in Texas and New Mexico and offer guidance for prevention and monitoring. As of March 7, 2025, Texas and New Mexico have reported 208 confirmed cases associated with this outbreak (198 in Texas and 10 in New Mexico). As a part of this outbreak, two deaths have been reported: one in Texas and one in New Mexico. More cases are expected as this outbreak continues to expand rapidly.
With spring and summer travel season approaching in the United States, CDC emphasizes the important role that clinicians and public health officials play in preventing the spread of measles. They should be vigilant for cases of febrile rash illness that meet the measles case definition and share effective measles prevention strategies, including vaccination guidance for international travelers.
The risk for widespread measles in the United States remains low due to robust U.S. immunization and surveillance programs and outbreak response capacity supported by federal, state, tribal, local, and territorial health partners. Measles-mumps-rubella (MMR) vaccination remains the most important tool for preventing measles. To prevent measles infection and spread from imported cases, all U.S. residents should be up to date on their MMR vaccinations, especially before traveling internationally, regardless of the destination.
Background
As of March 6, 2025, a total of 222 measles cases have been reported by twelve U.S. jurisdictions this year: Alaska, California, Florida, Georgia, Kentucky, New Jersey, New Mexico, New York City, Pennsylvania, Rhode Island, Texas, and Washington; 201 of which occurred in New Mexico and Texas. Most of the 222 cases are among children who had not received the MMR vaccine. There have been three outbreaks, with an outbreak defined as three or more related cases, reported in 2025, and 93% of cases are outbreak-associated. For comparison, 16 outbreaks were reported during 2024 and 69% of cases were outbreak-associated.
Measles is a highly contagious viral illness that typically begins with fever, cough, coryza (runny nose), and conjunctivitis (pink eye), lasting 2-4 days prior to rash onset. Measles can cause severe health complications, including pneumonia, encephalitis (inflammation of the brain), and death. The virus is transmitted by direct contact with infectious droplets or by airborne spread when an infected person breathes, coughs, or sneezes. Measles virus can remain infectious in the air and on surfaces for up to 2 hours after an infected person leaves an area.
Infected people are contagious from 4 days before the rash starts through 4 days afterward. The incubation period for measles, from exposure to fever, is usually about 7–10 days, and from exposure to rash onset is usually about 10–14 days (with a range of 7 to 21 days).
Recommendations for Healthcare Professionals
- Ensure all patients without other evidence of immunity, especially those planning international travel, are up to date on MMR vaccine per routine ACIP recommendations:
- Children are recommended to receive 2 doses of MMR. The first dose is given at 12–15 months of age and the second is given at 4–6 years of age before school entry.
- Infants 6 months of age or older can receive MMR prior to international travel or in outbreak settings (see below). MMR is not licensed for children <6 months of age.
- Adults not at high risk of exposure are recommended to have at least 1 documented dose of MMR in their lifetime, or other evidence of immunity (e.g., positive measles immunoglobulin G (IgG)). Adults at high exposure risk, including students at post-secondary institutions, healthcare workers, and international travelers, should have two documented doses.
- Ensure patients who reside in areas with an ongoing measles outbreak follow state and local guidance. Texas Department of State Health Services (DSHS) has issued the following recommendations for the affected counties in Texas:
- Infants 6 through 11 months receive an early dose of MMR vaccine (i.e., infant dose). Subsequent doses should follow CDC’s recommended childhood schedule:
- Another dose at 12 through 15 months of age.
- A final dose at 4 through 6 years of age.
- Children older than 12 months who have not been vaccinated should receive one dose immediately and follow with a second dose at least 28 days after the first. Children older than 12 months with one prior dose should receive an early second dose of MMR vaccine separated by at least 28 days.
- Teenagers and adults previously vaccinated with one dose of MMR vaccine should receive a second dose. Those with no evidence of immunity should receive one dose of MMR vaccine immediately and follow with a second dose at least 28 days later.
- Infants 6 through 11 months receive an early dose of MMR vaccine (i.e., infant dose). Subsequent doses should follow CDC’s recommended childhood schedule:
- Ensure all U.S. residents older than age 6 months without evidence of immunity who are traveling internationally receive MMR vaccine prior to departure:
- Infants 6 through 11 months of age should receive one dose of MMR vaccine before departure. Infants who receive a dose of MMR vaccine before their first birthday should receive 2 more doses of MMR vaccine; the first of which should be administered when the child is 12 through 15 months of age and the second at least 28 days later (generally at age 4-6 years of age but can be administered sooner if indicated).
- Children 12 months of age or older should receive two doses of MMR vaccine, separated by at least 28 days.
- Teenagers and adults without evidence of measles immunity should receive two doses of MMR vaccine separated by at least 28 days.
- Be aware that some patients may develop a mild rash reaction in the 3 weeks following MMR vaccination. This does not typically require testing or public health intervention since a person with a rash due to a vaccine reaction is not infectious. If a symptomatic person who has been recently vaccinated also has a known or suspected measles exposure, consultation and additional testing may be required from the local or state health department to evaluate for acute measles.
- Consider measles as a diagnosis in anyone with fever (≥101°F or 38.3°C) and a generalized maculopapular rash with cough, coryza, or conjunctivitis who has recently traveled internationally, or domestically to a region with a known measles outbreak, or has other known or suspected exposure to measles.
- If you suspect measles:
- Isolate:
- Isolate patients with suspected measles immediately, ideally in a single-patient airborne infection isolation room (AIIR), or in a private room with a closed door until an AIIR is available. Patients with suspected measles should not remain in the waiting room or other common areas of a healthcare facility
- Protect healthcare providers against measles by adhering to Standard and airborne precautions when evaluating confirmed or suspect cases, regardless of their vaccination status. Healthcare providers without presumptive evidence of measles immunity who are exposed to measles should be excluded from work from day 5 after the first exposure until day 21 following their last exposure and offered post-exposure prophylaxis, as appropriate.
- Healthcare systems should ensure all healthcare providers have presumptive evidence of immunity to measles, ensure they can rapidly retrieve healthcare provider immunization status in case of exposures and offer postexposure prophylaxis when indicated.
- Offer measles testing outside of facilities to avoid possible transmission in healthcare settings. Call ahead to ensure immediate isolation for patients referred to hospitals for a higher level of care.
- Notify: Immediately notify state, tribal, local, or territorial health departments (24-hour Epi On Call contact list) about any suspected case of measles to ensure rapid testing and investigation. States report measles cases to CDC.
- Test: Laboratory confirmation should be pursued for all patients with suspected measles. CDC recommends collecting either a nasopharyngeal (NP) swab or throat (OP) swab for reverse transcription polymerase chain reaction (RT-PCR) testing as well as a blood specimen for serology testing from all patients with clinical features compatible with measles. Collecting a urine specimen along with an NP/OP swab may improve sensitivity of testing.
- Manage:
- Post-exposure prophylaxis (PEP): In coordination with local or state health departments, provide appropriate measles PEP to close contacts without evidence of immunity, as soon as possible after exposure, either with MMR vaccine (within 72 hours) or immunoglobulin (within 6 days). The choice of PEP is based on elapsed time from exposure or medical contraindications to vaccination.
- Supportive care: There is no specific antiviral therapy for measles. Medical care is supportive to help relieve symptoms and address complications such as pneumonia and secondary bacterial infections. Consistent with guidance from the American Academy of Pediatrics, vitamin A may be administered to infants and children in the United States with measles as part of supportive management. Children with severe measles, such as those who are hospitalized, should be managed with vitamin A. Vitamin A should be administered under the supervision of a healthcare provider and is not a substitute for vaccination. Overuse of Vitamin A can lead to toxicity and cause damage to the liver, bones, central nervous system, and skin. Pregnant women should avoid taking high levels of vitamin A as it has been linked to severe birth defects.
- Isolate:
Recommendations for State and Local Health Departments
State and local health departments have the lead in investigating measles cases and outbreaks.
- Report measles immediately (within 24 hours) to CDC ([email protected]) and through the National Notifiable Disease Surveillance System (NNDSS). Measles is a nationally notifiable disease.
- Establish measles case reporting within hospitals and to public health authorities.
- Record and report details about cases of measles, including close contacts and locations visited while infectious (i.e. 4 days before and after rash onset).
- Conduct active surveillance for any additional cases and facilitate transportation of specimens immediately to confirm diagnosis if measles is identified.
- Enhance outreach and communications to under-vaccinated communities through trusted messengers.
- Consider utilizing state-based syndromic surveillance to monitor for changes with healthcare seeking behavior for febrile rash illness or vitamin A toxicity.
Recommendations for Domestic Travelers to Outbreak Areas and International Travelers
- Talk to your doctor about the MMR vaccine, especially if you or your child plan to travel to an area with an ongoing outbreak or internationally. Two doses of MMR vaccine provide better protection (97%) against measles than one dose (93%).
- Check your destination and CDC’s Global Measles Travel Health Notice for more travel health advice if you plan to travel internationally, including countries measles outbreaks have been reported.
- After domestic travel to an area with an ongoing outbreak or international travel, watch for signs and symptoms of measles for 3 weeks after returning to the United States. If you or your child gets sick with a rash and a high fever, call your healthcare provider. Tell them you traveled to an area where they identified measles or another country and whether you or your child had received MMR vaccine.
For More Information
- Clinical Overview of Measles | Measles (Rubeola) | CDC
- Interim Infection Prevention and Control Recommendations for Measles in Healthcare Settings | Infection Control | CDC
- Chapter 7: Measles | Manual for the Surveillance of Vaccine-Preventable Diseases | CDC
- Rubeola / Measles | CDC Yellow Book 2024
NCMS Supported Press Conference on New Prior Authorization Reform Bill Gets Statewide News Coverage

CARE FIRST Act Looks to Curb Insurance Barriers to Medical Decisions
North Carolina representatives, the North Carolina Medical Society, and other healthcare leaders from around the state were on hand Tuesday to support House Bill 434, the CARE FIRST Act. The bill aims to reform the process of patients seeking prior authorization from their health insurance provider.
Passage of the bill is a top priority for NCMS members and staff this year.
NCMS Past President Representative Timothy Reeder, MD, NCMS Member Representative Grant Campbell, MD, and Representative Tricia Cotham are sponsoring the bill and introduced it at the standing-room-only press conference. The meeting featured Linsi Franklin, the mother of a 9-year-old boy diagnosed with severe Crohn's Disease. She described her struggle with prior authorization, saying "I would spend hours on the phone daily with the insurance company trying to push the prior authorization through." She added that she is fighting for prior auth reform "so other North Carolina families don't have to."
NCMS President Joh Meier, MD says "On multiple occasions, my patients have suffered because of the delays of unnecessary prior authorization. It is critical that prior authorization in North Carolina is reformed so that patients receive timely, necessary, and consistent care that is not delayed nor withdrawn retrospectively."
The event has been covered extensively across the state. Here is a partial list of stories already posted:
WUNC - NC lawmakers take aim at insurance companies' 'prior authorization' system
AOL - NC House bill takes aim at insurance company prior authorization practices
Blue Ridge Public Radio - NC lawmakers take aim at insurance companies' 'prior authorization' system
WHQR - NC lawmakers take aim at insurance companies' 'prior authorization' system
NCMS Shows Support for CARE FIRST Act at Press Conference to Reform Prior Authorization

(L-R Back Row: NCMS Interim CEO Steve Keene, NCMS BOD Member Dr. Ronnie Laney, NCMS President Dr. John Meier, Josh Dobson. Front Row: Lindsi Franklin, Rep. Timothy Reeder, MD, Rep. Grant Campbell, MD, Rep. John Bell, NCMS Board Member Dr. Charul Haugan, Sumathi Iyendar)
The CARE FIRST Act Looks to Reform Prior Authorization in North Carolina
https://www.youtube.com/watch?v=Pu0Eyw9m-Mo
RALEIGH, March 18, 2025 -- With the wellbeing of North Carolinians and their physicians at the top of its list of priorities, the North Carolina Medical Society (NCMS) showed support for The CARE FIRST Act, which would reform the process of patients seeking prior authorization from their health insurance provider. NCMS firmly believes that physicians should be the ones to make medical decisions for their patients and health insurance companies should take responsibility for the outcome of denied medically necessary care.
Interim NCMS CEO Steve Keene said, “The health of North Carolinians is the main priority of NCMS. When unnecessary prior authorization delays treatment or denies medically necessary care, patient health is negatively affected. I am pleased that legislators are starting this important conversation to safeguard patient-doctor relationships.”
Health care professionals and NCMS members alike shared their personal experiences navigating the ramifications of prior authorization. John Meier, MD, President of the North Carolina Medical Society and internal medicine physician, spoke in support of The CARE FIRST Act saying, “On multiple occasions, my patients have suffered because of the delays of unnecessary prior authorization. It is critical that prior authorization in NC is reformed so that patients receive timely, necessary, and consistent care that is not delayed nor withdrawn retrospectively.”
Linsi Franklin, the mother of a 9-year-old boy who was diagnosed with severe Crohn’s disease, struggled to get prior approval for her son who needed two life-saving surgeries and two rounds of Humira. “While I’m so thankful that we finally were able to receive Isaac’s medication, I was shocked at the time it took to get my son the medication he needed. His immune system was actively attacking his intestines. He was also dealing with the psychological and physical challenges of having an ostomy bag. He had a team of physicians fighting for him, and it still took months to get Isaac the medication he needed. Isaac shouldn’t have had to wait. A child and their parents shouldn’t have to fight that hard to get needed medications and treatments.” She continued at the press conference stating, “For weeks, I would spend hours on the phone daily with the insurance company and the pharmacy, trying to push the prior authorization through. This is especially difficult when you have three small children at home. I am fighting for prior authorization reform in North Carolina because my son, other ten-year-olds, and other families in North Carolina shouldn’t have to.”
Sumathi Iyengar, the Co-Founder and Executive Director of the Wiskott-Aldrich Foundation, shared the prior authorization stories of her son and a 20-year-old UNCG student named Camden who suffers from Wiskott-Aldrich Syndrome (WAS). “It is paramount that prior authorization be reformed in NC so that patients like Camden have a straightforward and easy to understand process where his treatment is approved without these obstacles. Unfortunately, Camden is not alone; I hear the same story repeated time and again. We should do better by John, by our children, our families who are fighting so hard to do their best.”
We Need Your Help! Contacting Your Legislator is Easy! Click Below Today!
Click here for full press conference video
Click here for a link to House Bill 434
Former Governor Roy Cooper and Dr. Betsey Tilson Honored with Levine Award for Contributions to Public Health

The Ron Levine Legacy Award is a prestigious honor named after former North Carolina State Health Director Dr. Ron Levine
RALEIGH -- Former North Carolina Governor Roy Cooper and former State Health Director Dr. Betsey Tilson were recognized for their exemplary accomplishments in public health with the North Carolina Department of Health and Human Services Ron H. Levine Public Health Award at the annual North Carolina Public Health Leaders’ Conference on March 13.
The Ron Levine Legacy Award is a prestigious honor named after former North Carolina State Health Director Dr. Ron Levine. Since its inception in 2004, the award has recognized individuals who have significantly improved the public health system, expanded the scope and capacity of public health services or built new and lasting partnerships that strengthen health outcomes for North Carolinians.
"Former Governor Cooper and Dr. Tilson have made extraordinary contributions to public health, shaping policies and programs that will have a lasting impact on the well-being of all North Carolinians," said Dr. Kelly Kimple, Interim State Health Director and NCDHHS Chief Medical Officer. "Their leadership, dedication and tireless efforts exemplify the spirit of the Ron Levine Award, and we are honored to celebrate their achievements."
Former Governor Cooper’s legacy includes his leadership in successfully expanding Medicaid, extending health care coverage to over 640,000 North Carolinians. He pioneered the creation of a first-of-its-kind medical debt relief program, alleviating nearly $4 billion in medical debt for low- and middle-income North Carolinians.
Additionally, as a champion for public health, former Governor Cooper has been a steadfast advocate for the health and well-being of North Carolinians, demonstrating unwavering leadership during some of the most challenging public health crises of our time. Under his leadership, North Carolina navigated the COVID-19 pandemic with a focus on data-driven public health measures and equitable vaccine distribution, leading to one of the lowest per capita death rates in the Southeast and among the lowest in the nation. He played a critical role in combating misinformation and ensuring North Carolinians received trusted public health guidance throughout the pandemic.
Recognizing firearm violence as a public health issue, former Governor Cooper established the Office of Violence Prevention, which provides a centralized resource for reducing gun-related injuries and deaths. He also championed the Early Childhood Action Plan, reinforcing his belief that investing in early childhood education leads to lifelong positive health outcomes.
As a trusted public health leader, Dr. Betsey Tilson dedicated her career to improving public health systems, ensuring North Carolinians receive evidence-based and accessible health care services. As North Carolina’s State Health Director and Chief Medical Officer for the Department of Health and Human Services for seven years, she led critical health initiatives, including North Carolina’s COVID-19 response, guiding medical professionals and the public through the crisis with transparent, data-driven communication. Under her leadership, nearly 70% of North Carolinians were fully vaccinated at the height of the pandemic.
Dr. Tilson has prioritized whole-person health, championing programs such as Medicaid Expansion and the Healthy Opportunities Pilots — the nation’s first comprehensive initiative to address non-medical drivers of health, including housing, food, transportation and interpersonal safety. The pilots are now showing huge success in North Carolina, with federal partners giving approval to expand statewide. She also played a pivotal role in launching NCCARE360, the state’s first coordinated care network connecting individuals to community resources, ensuring their health and social needs were met.
A strong advocate for reproductive health care, Dr. Tilson worked to expand contraceptive services in pharmacies and enhance syphilis testing coverage under Medicaid Expansion. Additionally, she played a key role in responding to Hurricane Helene’s impact on Western North Carolina, ensuring communities had access to essential public health services during disaster response and recovery.
To learn more about the Ron H. Levine Legacy Award and its past honorees, visit the NCDHHS Division of Public Health website.
Tune in Tuesday for the NCMS Reform Prior Auth Press Conference
The NCMS is taking steps to make the practice of medicine easier for you!
Tune in Tuesday at 12:00 PM for an important press conference, where the North Carolina Medical Society (NCMS) will stand alongside North Carolina Representatives to introduce groundbreaking legislation aimed at reforming health insurance prior authorization. This initiative seeks to address our members' concerns surrounding insurance companies delaying or denying necessary medical treatments, which can negatively impact patient care and potentially lead to death.
The North Carolina Medical Society firmly believes that healthcare decisions should be made by physicians who understand their patients' needs, rather than by insurance companies focused on cost-cutting measures. NCMS continues to advocate for physician-directed care. When insurers interfere with the doctor-patient relationship and restrict access to essential care, patient health and well-being are put at risk.
Join us in supporting this critical effort to ensure that medical decisions remain in the hands of trusted healthcare professionals and that patients receive the timely and appropriate care they deserve. Stay informed, and be part of the movement to improve healthcare in North Carolina!
Click here for the link to the live press conference.
Topical Steroid Withdrawal Diagnostic Criteria Defined by NIH Researchers

Criteria may help guide treatment of dermatitis.
What
Researchers at the National Institutes of Health (NIH) have determined that dermatitis resulting from topical steroid withdrawal (TSW) is distinct from eczema and is caused by an excess of an essential chemical compound in the body. Scientists from NIH’s National Institute of Allergy and Infectious Diseases (NIAID) identified treatments that could be studied in clinical trials for the condition based on their potential to lower levels of the chemical compound—called nicotinamide adenine dinucleotide (NAD+), a form of vitamin B3. The findings were published today in the Journal of Investigative Dermatology.
Dermatitis is characterized by inflammation, itching, or burning sensations on the skin, and can result from various conditions including TSW and eczema. Eczema, also known as atopic dermatitis, is a common cause of dermatitis and affects 10 to 30% of children and 2 to 10% of adults each year in the United States. Topical steroids—specifically glucocorticoids or topical corticosteroids—have long been used as a first-line treatment for dermatitis caused by eczema because the drugs are safe, effective, easy to apply, and considered well-tolerated.
Some people experience dermatitis after using topical steroids for prolonged periods of time and then stopping—a condition called TSW. Diagnosing and treating this condition is difficult because TSW is not well understood. Symptoms include skin redness, burning sensations, skin heat (thermal dysregulation), itching and peeling, which can even occur on parts of the body where topical steroids were not applied. As TSW and eczema have similar symptoms, it has been difficult to distinguish the two disorders.
To better understand TSW, a team led by scientists in NIAID’s Laboratory of Clinical Immunology and Microbiology evaluated a previous survey that included 1,889 adults with symptoms similar to eczema. By dividing the participants into those with self-reported TSW and those without, the researchers identified characteristics unique to TSW. The researchers then conducted a pilot study including 16 people with symptoms consistent with TSW, 10 people with eczema but no symptoms of TSW, and 11 people without skin disease. They found that people with TSW symptoms had elevated levels of NAD+ in their blood serum and skin, while NAD+ levels were within a typical range in people without TSW symptoms.
The researchers subsequently used cultured skin cells and a mouse model to mimic TSW conditions. They found that NAD+ was produced in response to topical steroids and caused inflammation. The models suggested that administration of a drug that blocked the formation of NAD+—called a mitochondrial complex I blockade—would improve TSW symptoms. In a pilot study to further assess this treatment strategy, the researchers evaluated subjective responses among study participants who used the mitochondrial complex I-blocking drugs metformin, berberine, or both. After three to five months of use, most participants reported improvement in TSW symptoms.
The scientists provisionally established criteria that can be used by health care providers to identify TSW in people. People who have stopped topical steroid treatment and meet the criteria may be diagnosed by practitioners as having TSW. The researchers suggest that patients identified as having TSW could be treated using the proposed mitochondrial complex I-blocking drugs.
The results of this study may help practitioners identify TSW in patients and work towards developing safe and effective treatments. According to the researchers, more research is needed to determine whether all patients with TSW have an excess of NAD+, or if there are other features that define TSW. Additionally, the diagnostic criteria will help health care providers and researchers to better understand the prevalence of TSW and evaluate the effects of using topical steroids.
Article
N Shobnam, G Ratley, S Saksena et al. Topical Steroid Withdrawal is a Targetable Excess of Mitochondrial NAD+. Journal of Investigative Dermatology 10.1016/j.jid.2024.11.026 (2025).
Who
Ian Myles, M.D. M.P.H., Principal Investigator, Epithelial Therapeutics Unit in NIAID’s Laboratory of Clinical Immunology and Microbiology is available to discuss this research.
NIAID conducts and supports research—at NIH, throughout the United States, and worldwide—to study the causes of infectious and immune-mediated diseases, and to develop better means of preventing, diagnosing and treating these illnesses. News releases, fact sheets and other NIAID-related materials are available on the NIAID website.
About the National Institutes of Health (NIH): NIH, the nation's medical research agency, includes 27 Institutes and Centers and is a component of the U.S. Department of Health and Human Services. NIH is the primary federal agency conducting and supporting basic, clinical, and translational medical research, and is investigating the causes, treatments, and cures for both common and rare diseases. For more information about NIH and its programs, visit www.nih.gov.
March Madness is in Full Swing! Several NC Teams Are in the Big Dance!

(AXIOS, Zachery Eanes) -- The North Carolina Tar Heels squeaked into the NCAA Tournament, grabbing an 11-seed and a spot in the play-in game against San Diego State.
- Duke, the winners of the ACC Tournament, received a No. 1 seed in the East Region.
Why it matters: North Carolina barely made the cut, earning the last at-large bid into the tournament after an arguably weak showing against elite teams this season.
- Duke's No. 1 seed will mean they get to play in Raleigh on Friday against the winner of American versus Mount St. Mary's.
Here's which North Carolina schools will be competing in the NCAA Tournament:
Men's tournament
 Duke: Duke earned the No. 1 seed in the East Region and will take on the winner of American versus Mount St. Mary's in the No. 16 play-in game.
Duke: Duke earned the No. 1 seed in the East Region and will take on the winner of American versus Mount St. Mary's in the No. 16 play-in game.
 UNC: The No. 11 Tar Heels will play No. 11 San Diego State in Dayton on Tuesday. The winner of that game will go on to play No. 6 Ole Miss in Milwaukee on Friday in the South Region.
UNC: The No. 11 Tar Heels will play No. 11 San Diego State in Dayton on Tuesday. The winner of that game will go on to play No. 6 Ole Miss in Milwaukee on Friday in the South Region.
 UNC-Wilmington: The Seahawks got the No. 14 seed in the West Region and will play No. 3 Texas Tech in Wichita, Kansas, on Thursday.
UNC-Wilmington: The Seahawks got the No. 14 seed in the West Region and will play No. 3 Texas Tech in Wichita, Kansas, on Thursday.
 High Point: High Point got the No. 13 seed in the Midwest Region and will play No. 4 Purdue in Rhode Island on Thursday.
High Point: High Point got the No. 13 seed in the Midwest Region and will play No. 4 Purdue in Rhode Island on Thursday.
Women's tournament
North Carolina schools were also well represented in the women's NCAA Tournament, and the Triangle's three ACC schools will get to host their opening games.
 N.C. State: The Wolfpack got the No. 2 seed in Region 1 and will host No. 15 Vermont in Raleigh on Saturday.
N.C. State: The Wolfpack got the No. 2 seed in Region 1 and will host No. 15 Vermont in Raleigh on Saturday.
 Duke: The Blue Devils received the No. 2 seed in Region 2 and will welcome No. 15 Lehigh to Durham on Friday.
Duke: The Blue Devils received the No. 2 seed in Region 2 and will welcome No. 15 Lehigh to Durham on Friday.
 UNC: The Tar Heels will be the No. 3 in Region 2 and play No. 14 Oregon State in Chapel Hill.
UNC: The Tar Heels will be the No. 3 in Region 2 and play No. 14 Oregon State in Chapel Hill.
 UNC-Greensboro: The No. 16 Spartans will travel to Los Angeles to play No. 1 Southern California in Region 4.
UNC-Greensboro: The No. 16 Spartans will travel to Los Angeles to play No. 1 Southern California in Region 4.
 High Point: The No. 16 Panthers will pay No. 16 William & Mary in the play-in game for Region 3 for a chance to take on No. 1 Texas.
High Point: The No. 16 Panthers will pay No. 16 William & Mary in the play-in game for Region 3 for a chance to take on No. 1 Texas.
If you are into trying to figure out the winner, the odds of a perfect NCAA bracket:
-
1 in 9,223,372,036,854,775,808 (if you just guess or flip a coin)
-
1 in 120.2 billion (if you know a little something about basketball)
If you want to try your hand at the ESPN bracket challenge, click here.
March is Colorectal Cancer Awareness Month. Read an Inspiring Survivor's Story
Young and at Risk for Colorectal Cancer
March is Colorectal Cancer Awareness Month, highlighting the importance of early detection through colonoscopies
(Duke Today, Jodie Valade) -- Even though Ajay Kohli had been experiencing debilitating abdominal discomfort for weeks in late 2021, such excruciating pain that he once had to pull over as he was driving his car, he wasn’t sure if he needed a colonoscopy. He was 42, active and otherwise healthy.
Kohli, an Emergency Medicine Physician at Duke University Hospital, had a full panel of bloodwork and a CT scan done and everything came back normal. He continued with his life and plans and ran a half-marathon in the Bull City Race Fest on Oct. 17, 2021. The next day, when he was supposed to begin his prep for a colonoscopy, he turned to his wife with an idea.
“Let’s go get some pizza,” he said. “I don’t need to do this.”
She insisted, though, and Kohli kept the appointment and continued the prep that included a day of fasting.
He remembers waking up from the anesthetic for the procedure, still groggy and hearing the words “perforation” and “cancer.”
The doctor found a mass in his colon that was eroding the colon wall. He was rushed to emergency surgery where the perforation was repaired, and the tumor was removed.
Both the surgery and the recovery were “brutal,” Kohli said, but if he had waited, the consequences might have been devastating. Kohli had not yet reached the recommended age for his first colonoscopy screening, but Duke medical insurance plans fully cover all colonoscopies from in-network providers.
“All my labs and CT were clean, completely normal, despite having a decent-sized tumor,” Kohli said. “Things can’t really stop at labs and a CT scan. I’m not saying everyone should get a colonoscopy, but don’t ignore these symptoms – especially with the rise of colorectal cancer.”
Colonoscopies now recommended at age 45
In January 2024, the American Cancer Society published a report that said the rates of colorectal cancer are rising rapidly among people in their 20s, 30s and 40s. Colorectal cancer moved up from the fourth leading cause of cancer death in both younger men and women two decades ago to first in men and second in women. The reasons why are unclear, but the U.S. Preventive Services Task Force now says that people at average risk for colorectal cancer should start screening at age 45 rather than 50.

That means a baseline colonoscopy at age 45, a screening that is covered fully with in-network providers by Duke’s medical insurance plans. In 2024, 72% of Aetna members and 77% of Blue Cross members covered by Duke received colonoscopy screenings, both of which exceed industry standards. Colorectal Cancer Awareness Month in March offers a timely reminder: research confirms that colonoscopies remain the most reliable method for detecting colorectal cancer.
Julius Wilder, a Duke Associate Professor of Medicine in Gastroenterology, has seen the rise in younger patients first-hand. Theories for what’s driving the increase include alcohol consumption, diet and obesity. All those factors correlate with having polyps, Wilder said, and polyps can become cancerous.
One aspect not helping with early detection is misinformation spread around colorectal cancer on social media. Wilder studied TikTok users in 2023 who discussed colon cancer, and found that in 35 educational videos, 13 were misleading about causes and treatments – and those misleading videos were shared more often than useful ones.
“It’s scary that people go into a public space and share that information,” Wilder said. “It gets scary because of what that means in terms of people may begin to not get screened appropriately because of something so inaccurate.”
Wilder encourages factual information from physicians, including relaying that the prep is the most difficult part of the colonoscopy.
“I am very transparent with my patients that yes, you're going to probably drink a lot of fluid and you're going to poop a lot,” he said. “We might have a remote-control car on Mars right now with a helicopter on top of it, but that's still how we do colonoscopies.”
Becoming a better patient

Kohli’s recovery from colon cancer surgery and chemotherapy was slow and difficult, but one activity that helped throughout the process was walks with his wife and colleagues. When he felt better, those walks progressed to runs.
And that helped him keep a promise to himself: One year after he was diagnosed, he ran that same half marathon he’d participated in just before his 2021 colonoscopy.
“For me, it was important to do that race again, and I’ve done that race every year since,” he said.
He’s also been diligent about getting the tests and procedures recommended. That includes regular colonoscopies until he’s five years cancer-free in 2027.
“I haven’t always been great about taking my health as seriously as I should,” Kohli said. “I know they say physicians don’t make the best patients, so that’s probably me – or used to be me.”
Not anymore.
ECU Health Offers Remote Healthcare Access for Cardiology Patients

ECU Health Offers Remote Healthcare Access for Cardiology Patients
(WNCT, Lauren Beachy, Elizabeth Pittman) -- ECU Health plans to begin seeing cardiology patients remotely as some people have to travel an hour or more for their appointments.
“So, our first pilot is going to be in Edenton and we’ve started our first few sessions where we’re actually able to communicate with the patients,” Chief of the Division of Cardiology at ECU Health Dr. John Catanzaro said. “And using technology such as Iron Bow, we’re actually able to not only communicate with the patients and talk to them but actually have a way to measure their heart rate and pulse.”
The care the patients receive will be coordinated from nurses at the ECU Health Chowan Hospital while a cardiologist meets with them virtually from Greenville.
“The whole realm of cardiology services that they would get just as if they were seeing the provider right in the clinic,” Manager of Patient Care Services of the Outpatient Specialty Clinics at ECU Health Chowan Hospital Kelli Joco said. “So, they get to see, you know, with heart monitors to where for several weeks, if that’s needed, we’re able to get them and coordinate all the other care that they may need.”
Patients have enjoyed having new access to health care, and ECU Health is hoping to expand this program.
“Like I said, with our first clinic with three patients and we’ve had six clinics so far,” Joco said. “We’ve seen a total of 30 patients and some of them have even been as early as we are in the program, have even been follow up visits, not just new patients that are being seen for the first time.”
See the WNCT report here.
Health Workforce Well-Being Day
Health Workforce Well-Being Day
March 18, the anniversary of the passage of the Dr. Lorna Breen Health Care Provider Protection Act, is now officially recognized as Health Workforce Well-Being Day of Awareness, acknowledging the widespread health worker burnout in the U.S. and the need for solutions.
Healthcare workers experiencing burnout doesn’t just harm individuals, it threatens the entire system. Addressing the mental health crisis now is both financially sustainable and smart policy. Learn more about the Lorna Breen Law and what it protects here: https://www.youtube.com/watch?v=hxb_kt4l21g
The North Carolina Clinician and Physician Retention and Well-being (NCCPRW) Consortium has partnered with the Dr. Lorna Breen Heroes' Foundation. NCCPRW is a collaborative initiative aimed at identifying and developing strategies to improve well-being among the healthcare workforce at the individual, organizational, and state level. The Consortium is part of a 3-phase initiative with hospitals and health systems to improve workplace policies and practices that reduce burnout, normalize help-seeking, and strengthen professional well-being.
But there is more work to be done – and we’re only getting started.
Now is the time to act to support our nation’s health workers.
Click here for opportunities for hospital leaders, policymakers, health workers, and everyone to assist the national efforts with the Dr. Lorna Breen Heroes Foundation
Contact the Consortium’s Executive Director, Monecia Thomas, PhD, MHA, to get your hospital or health system engaged in the Consortium’s state-wide efforts to make North Carolina the healthiest state to practice medicine.
Help care for the mental health of those who care for us.
Martin County Seeks Operator to Bring Rural Hospital Back to Life

First-in-the-nation effort to reopen a shuttered medical center as a Rural Emergency Hospital moves closer to finish line
(NC HealthNews, Jamie Baxley) -- For the past 19 months, officials in rural Martin County have been working on an experimental plan to resurrect the community’s shuttered hospital.
Martin General, the 43-bed facility that for seven decades served generations of residents in the Eastern North Carolina county, closed its doors in August 2023.
The hospital was later placed into bankruptcy, a move that operator Quorum Health attributed to “financial challenges related to declining population and utilization trends.” Ownership of the hospital eventually reverted to the county, which had been leasing the building to Quorum.
The closure has forced residents of Martin County, which was home to about 22,000 people at the 2020 Census, to travel more than 20 miles to neighboring Beaufort County for emergency care. Concerned citizens have repeatedly voiced their frustration with the situation at meetings of the Martin County Board of Commissioners.
“There was, understandably, anger in the community about the closure,” Dawn Carter, health care consultant for Martin County, said in an interview, adding she had been “brought to tears multiple times” by residents’ stories about their struggle to find care.
Over the past year and a half, Carter has helped the county plow through an extensive checklist of requirements that, once completed, will allow Martin General to reopen — albeit in a more limited capacity.
The goal is to reestablish the facility as a Rural Emergency Hospital, a designation created through the U.S. Congress’ Consolidated Appropriations Act of 2021 as a lifeline to small hospitals that are at risk of going under. Hospitals that participate in the program receive millions in federal funding to continue providing 24/7 emergency care, but they are prohibited from offering inpatient services.
At least 38 facilities have converted to Rural Emergency Hospitals since the program launched in January 2023, according to data from the Cecil G. Sheps Center for Health Services Research at UNC Chapel Hill. But all of those hospitals were still functioning when they made the switch.
Carter said Martin General is on track to become the first closed-down hospital in the nation to reopen as a Rural Emergency Hospital.
Now the county needs to find someone to operate it.
Search begins
After holding a public hearing on a resolution to sell or lease the hospital property on Feb. 12, the Martin County Board of Commissioners sent out requests for proposals from potential operators.
Residents will have multiple chances to weigh in before a selection is made, a process that Carter said will likely take “weeks and months” to complete.
“Once the proposals are in and we have a chance to group and review them, there will be an opportunity that the proposals will be made available to the public,” she said. “There will be subsequent public hearings on the proposal. If the county decides to enter into an agreement with one particular operator, then that agreement is also subject to public review, so there will be lots of public input as we move through the process.”
Carter said requests were sent to “everybody who had expressed interest at some point in time” in taking over Martin General.
“We definitely have interested parties,” she said. “I can’t predict, at this point, how many proposals that we are going to end up getting. Some people that had expressed interest along the way have changed their minds, but I am pleased that we do continue to have interest.”
It remains to be seen if the search for a suitable operator will be affected by proposed cuts to federal funding for Medicaid.
Less than five months after Martin General closed, North Carolina became the 40th state to expand eligibility for Medicaid. The measure opened up the government-funded health insurance program to low-income adults who had previously made too much money to qualify.
More than 630,000 people have joined the rolls since expansion took effect, reducing financial strain on struggling hospitals — particularly those in rural towns — that lose money providing uncompensated care to patients without insurance.
The budget passed by Republicans in the U.S. House of Representatives on Feb. 25 directs Energy and Commerce, the committee that oversees Medicaid, to cut spending by $880 billion over the next decade to offset the cost of President Donald Trump’s pledge to extend trillions of dollars in expiring tax breaks.
Jay Ludlam, deputy secretary of the state’s Medicaid program, recently warned state legislators that the cuts could force North Carolina to discontinue expansion — immediately stripping coverage from beneficiaries who only recently became eligible for it.
“The Medicaid uncertainty at the federal level is a concern across rural communities because of the impact on rural health care,” Carter said. “But I think that we’re fortunate that we continue to have interest despite that.”
‘All hands on deck’
Commissioner David “Skip” Gurganus said reopening the hospital is the “number one issue for Martin County.”
“I had no idea, and still don’t really understand, what it’ll look like to get health care reestablished in Martin County,” he said during the board’s meeting on Feb. 12. “Here’s what I do know for a fact: A team of people have worked tirelessly to try to bring this thing to the point that it’s at. You have not seen them work — and for the most part, I have not seen them work — but I can assure you that they have worked.”
Benjamin Eisner, interim manager for Martin County, explained that the county had to wait 60 days after Martin General filed for bankruptcy to find out if the trustee, a bankruptcy and insolvency practice based in Delaware, wanted to “keep the hospital building or not.” He said the county then spent four months working with the State Attorney General’s Office to sort through and distribute the medical records that were left behind.
“It’s been an all-hands-on-deck situation,” Eisner said.
The federal Centers for Medicare and Medicaid Services — which regulates most of the nation’s health care facilities — confirmed last year that Martin General could reopen as a Rural Emergency Hospital, but the county needed to first update and repair the aging building to ensure it met the agency’s requirements for the designation. While there are still some minor issues with the facility that must be addressed, Carter said she’s “confident” that CMS will sign off.
“It’s been a hard row to hoe,” said Commissioner Joe Ayers, chairman of the board. “We’re getting there. We see the end of the road.”
The county’s efforts have not gone unnoticed by residents. In recent months, Carter has observed a shift in the community’s perspective on the situation.
“I feel like folks have gained an understanding that we are not dragging our feet, as much as it may feel like it with how long this is taking,” she said. “They understand that it’s been a process and have expressed gratitude that we are moving forward with the process.”
Martin County is far from the only rural community to lose its local hospital in recent years.
According to the Sheps Center, 152 rural hospitals across the U.S. have either closed or drastically scaled back their services since 2010. Twelve of those facilities are in North Carolina, the center reported.
In addition to being the first hospital in the nation to reopen as a Rural Emergency Hospital, Martin General would be the first hospital in North Carolina to receive the designation. Because the program is not open to facilities that closed before 2023, it cannot be used to bring back the state’s other shuttered hospitals.
Addressing attendees of last month’s board meeting, Gurganus acknowledged that the return of Martin General is still not guaranteed.
His advice to citizens? Pray on it.
“I believe in prayer. I believe that it helps. I believe that it has a profound effect on our lives, and I believe that it can have a profound effect on our county,” he said. “If you subscribe to the same belief, I would ask you to start tonight, if you haven’t already, and continue every night to ask God for guidance to lead us to health care for our citizens in Martin County.”
New Study: Common Vaginal Condition is Really An STD

Only women are currently treated for the infection called bacterial vaginosis, but it’s actually a sexually transmitted disease that sexual partners should receive treatment for as well, a new study found
(CNN Health, Sandee LaMotte) -- A common but potentially dangerous vaginal infection that affects nearly 1 in 3 women globally should be considered a sexually transmitted disease, a new study says.
Bacterial vaginosis, or BV, is currently viewed as a woman’s issue, thus leaving the sexual partner untreated.
“I started getting them quite recurrently. I’d go to doctors and get treated with antibiotics, and it would almost always come back,” said Hanae, a woman who participated in the clinical trial on BV conducted in Melbourne, Australia.
For half of all women with bacterial vaginosis, the infection returns after completion of a week of antibiotics, the preferred medical treatment for BV, said first author Lenka Vodstrcil, a senior research fellow at the Melbourne Sexual Health Centre at Monash University in Australia.
“The bacteria that cause BV can be located in men, especially in penile skin and also in the urethra,” Vodstrcil said in a news release. “This suggests that BV is probably sexually transmitted, and that is why so many women get it back again after treatment.”
When BV was treated as a sexually transmitted disease, with both partners receiving oral antibiotics and men using topical creams, the recurrence rate dropped by over half, according to the study published Wednesday in the New England Journal of Medicine.
“Our trial has shown that reinfection from partners is causing a lot of the BV recurrence women experience, and provides evidence that BV is in fact a STI (sexually transmitted infection),” said senior author Catriona Bradshaw in an email. Bradshaw is a professor at the Melbourne Sexual Health Centre at Monash University.
A potentially dangerous infection
Symptoms of BV can include itching, pain while urinating, an odd odor and a thin, white vaginal discharge. For some women, however, BV is a silent predator, attacking without such telltale symptoms.
If left untreated, bacterial vaginosis can increase the risk of acquiring HIV as well as sexually transmitted infections, according to the World Health Organization. Women with BV can also develop an infection in the fallopian tubes, ovaries or uterus called pelvic inflammatory disease, the WHO states on its website.
Such infections can lead to later infertility, experts say.
“We see very significant changes in a range of inflammatory markers, inflammatory cells and bacterial enzymes and products that result in damage to the epithelium — the lining of the reproductive tract,” Bradshaw said.
Bacterial vaginosis is especially dangerous during pregnancy. The infection can lead to premature birth, spontaneous abortion and low birth weight in the baby, according to the WHO.
It’s time for a ‘paradigm shift’ in treatment
The randomized clinical trial of 164 monogamous couples was conducted at multiple centers in Australia. In 81 of the couples, both partners were treated with seven days of oral antibiotics. During that time, the male partner also used a topical antibiotic on their penis twice a day.
In accordance with current recommended treatment, only the woman in the other 83 couples was treated with an oral antibiotic.
While the study only treated heterosexual couples, it’s “important to note that women in same sex relationships also transmit BV bacteria between each other during sex, and that these same sex couples in monogamous relationships have very high rates of concordance for BV — both have it or both don’t have it,” Bradshaw said.
The trial was meant to last for 12 weeks, but researchers stopped it early when it was quickly apparent that treating both partners reduced BV occurrence by 60%.
Viewing such a common vaginal infection as a sexually transmitted disease would be a “paradigm shift” and would require doctors to encourage a woman’s male partner to share responsibility for transmission and treatment, according to an editorial published alongside the study.
“It will also require a willingness of male partners to commit to taking both oral and topical medications, once notified by their female partner that she has bacterial vaginosis and that it is probably sexually transmitted,” wrote Dr. Christina Muzny and Dr. Jack Sobel, who were not involved in the new research.
Muzny is a professor of infectious disease at the University of Alabama at Birmingham. Sobel is a professor in the Division of Infectious Diseases at the Wayne State University School of Medicine in Detroit.
Men in the study had no problem completing the course of oral and topical antibiotics, with few to no side effects, the study found.
“We have now used this medication in close to 300 men and we have not had any report that side effects from the medication would stop them taking it,” Bradshaw said.
The Melbourne Sexual Health Centre has already changed its protocols and are now treating both partners when BV is detected, Bradshaw added. For health professionals and couples interested in treating both partners, the research team develped a website that provides detailed information on male partner treatment.
“Changes in national and international treatment guidelines always take time, so we felt an obligation to provide accurate online and downloadable information,” Bradshaw said.
Leadership Opportunity: NC Professionals Health Program Board of Directors

Leadership Opportunity: NC Professionals Health Program Board of Directors
The NCMS has the opportunity to appoint two members to the NC Professionals Health Program (NCPHP) Board of Directors. Learn more about the responsibilities of NCPHP Board members.
Since 1988, NCPHP has been dedicated to helping medical professionals experience a lifetime of change and return to health. NCPHP assists with recovery from substance use disorders and other conditions that could impair a clinician’s ability to safely provide care and services to their patients.
NCPHP originated as a physicians’ health committee of the North Carolina Medical Society (NCMS). In 1988, it was established as a formal program of the NCMS and written into the North Carolina General Statutes. To learn more about the important work of this organization, visit the NCPHP website.
Interested members should complete the application form and return it to Mary Kathryn Kimray, [email protected] by Monday, April 28. Interviews for this position will be held virtually on the morning Saturday, June 14, 2025.
Current NCPHP Board Appointees and Terms:
Clyde L. Brooks, Jr., MD
1/1/25 – 12/31/27 1st term
Stephen J. Ezzo, MD
1/1/20 – 12/31/22 1st term
1/1/23 – 12/31/25 2nd term
Vinay Saranga, MD
1/1/20 – 12/31/22 1st term
1/1/23 – 12/31/25 2nd term
Craig E. Webb, MHS, PA-C
1/1/25 – 12/31/27 1st term
Sarah W. Young, MD
1/1/23 – 12/31/25 1st term
(eligible for a 2nd term)
Duke Researchers: AI Model Predicts Risks and Potential Causes of Adolescent Mental Illness

DURHAM, N.C. -- An artificial intelligence (AI) model developed by Duke Health researchers accurately predicted when adolescents were at high risk for future serious mental health issues before symptoms become severe.
Unlike prior models that primarily rely on existing symptoms, the AI model identified underlying causes, such as sleep disturbances and family conflict, that could be used to prescribe interventions. That capability could greatly expand access to mental health services, with assessments and care available through primary care providers.
“The U.S. is facing a youth mental health crisis -- nearly half of teens will experience a mental illness,” said Jonathan Posner, M.D., professor in the Department of Psychiatry and Behavioral Sciences at Duke and senior author of a study appearing March 5 in Nature Medicine.
“Despite this crisis, the U.S. has a critical shortage of mental health providers,” Posner said. “Our AI model could be used in primary care settings, enabling pediatricians and other providers to immediately know whether the child in front of them is at high risk and empowering them to intervene before symptoms escalate.”
Posner and colleagues -- including data scientists Elliot Hill and Matthew Engelhard, M.D., Ph.D., in Duke’s Department of Biostatistics & Bioinformatics -- analyzed psychosocial and neurobiological factors associated with mental illness using data from the ongoing ABCD study. The study has conducted psychosocial and brain development assessments of more than 11,000 children over five years.
Using artificial intelligence, the researchers built a neural network – an AI model that mimics brain connections -- to predict which children would transition from lower to higher psychiatric risk within a year. That model is then used to score a questionnaire that ranks responses from the patient or parent about current behaviors, feelings and symptoms, to predict the likelihood of an escalation.
The model was 84% accurate in identifying patients in the study who went on to have escalating illness within the next year.
Importantly, the Duke researchers analyzed an alternative model that identified the potential mechanisms that might lead to or trigger worsening mental illness. With an accuracy rate of 75%, the new modeling system’s ability to identify underlying causes gives it a unique ability to alert doctors and families to potential interventions.
“It’s a much easier task to say a child who has a fairly high symptom burden of mental illness is going to be ill in a year, than to determine that a child has all of these underlying risk factors for mental illness and is going to become ill,” Hill said. “It’s important to leverage that information to design an intervention for that child.”
Among the most common underlying causes of escalating illness are sleep disturbances, problematic behaviors, adverse events, family mental health history, and family conflict; of those, sleep disturbances emerged as the most powerful predictor of future psychiatric illness.
“It’s important to note that the model does not prove it's a child’s sleep disturbances that are causing an elevated risk, but it does suggest that's one of the limited number of malleable factors that seems to be associated with high rates,” Engelhard said.
The authors said the model demonstrates a way to reach a broader population of young patients with a tool that primary care practitioners could use to assess a child’s mental health risk using simple questionnaires.
“Primary care doctors often do not have the time to conduct a detailed psychiatric assessment, making it difficult to identify which children need early intervention. This AI model would automate the process, analyzing the data in real-time and providing the doctor with a simple output indicating the child’s risk level,” Posner said.
In addition to Posner, Hill and Engelhard, study authors include Pratik Kashyap, Elizabeth Raffanello, Yun Wang, Terrie E. Moffitt, and Avshalom Caspi.
NC House Bill Would Expand Access to Early Screening for Prostate Cancer

Prostate cancer was the second leading cause of cancer deaths in North Carolina men in 2021; the bill aims to lower those rates.
(NC HealthNews, Grace Vitaglione) -- Sherrie Wood and her husband, Kenneth, were newly married when he was diagnosed with prostate cancer in 2003. He experienced extreme back pain and problems with urinating for over a year, but his general practitioner only treated the symptoms. After all, he was only in his early 40s.
 Sherrie Wood and her first husband,
Sherrie Wood and her first husband,
Kenneth.Credit: Sherrie Wood
They were finally referred to a urologist, and that doctor also didn’t think he had cancer because he was so young. But the second urologist they saw diagnosed Kenneth with stage 4 prostate cancer.
The couple’s focus immediately shifted, Sherrie Wood said, from trying to have a baby to getting treatment for Kenneth’s cancer. He underwent radiation, but the cancer came back multiple times. Kenneth died in 2005.
“I didn’t plan to be a widow in my 30s,” Wood, who lives in Stanly County, said.
Raising awareness about early screening is vital, she added, because it can mean the difference between life and death. Rodney D. Pierce, D-Roanoke Rapids, a new member of the North Carolina House of Representatives, filed House Bill 128 in early February that would expand access to prostate cancer screenings to underinsured or uninsured men in the state.
Prostate cancer is the second leading cause of cancer deaths in North Carolina men, according to the UNC Chapel Hill Men’s Health Program. The state ranked 11th highest in the U.S. for rates of new cases in 2023, and the North Carolina Department of Health and Human Services estimated that more than 1,100 men would die from prostate cancer in the state in 2023.
Almost all men whose cancer is found early survive for five years and beyond, but only 34 percent of men who are diagnosed after it has spread survive for five years and beyond. Black men are also more likely to be diagnosed with prostate cancer and more likely to die from it than white men.
House Bill 128 aims to remove barriers to testing and raise awareness about prostate cancer, Pierce said.
Deaths across the state
House Bill 128 would appropriate $4 million between 2025 and 2027 to the state Department of Health and Human Services to establish and administer a prostate cancer control program. The program would provide free or low-cost prostate cancer screenings and follow-up care to men who are uninsured or whose insurance won’t cover this kind of screening and who have a single-person household income below about $37,600.
Men who are between 50 and 70 years old without family history of prostate cancer are eligible for the program. Men with such family history are eligible when they’re 40.
Pierce modeled his bill after the North Carolina Breast and Cervical Cancer Control Program, which provides free or low-cost screenings and follow-up care to eligible women in the state.
Pierce said introducing the bill was especially important to him because the area of the state he represents — an area he calls “the neglected Northeast” — has high rates of prostate cancer.
Halifax County, part of his constituency, has one of North Carolina’s highest rates of deaths from prostate cancer, according to the 2023 Prostate Cancer Report from UNC Chapel Hill.
The counties with the highest rates of deaths due to prostate cancer in 2023 — between 27 to 31 deaths per 100,000 men — were Granville, Halifax, Edgecombe, Martin, Chowan, Hertford, Pasquotank and Yancey. In contrast, Ashe, Watauga, Buncombe, McDowell, Columbus and Carteret counties have some of the lowest death rates in the state: around 11 to 15 deaths per 100,000 men.
Many of those Northeastern counties also had higher rates of new cases than other parts of the state.
Controversial history behind the test
The prostate-specific antigen, or PSA, test is primarily used to diagnose prostate cancer. The antigen is produced both by normal and malignant cells of the prostate gland, according to the National Institute of Health. Prostate cancer can elevate those levels.
North Carolina State University alum T. Ming Chu led the research that developed the PSA test in the 1970s, and the FDA approved it as an early detection tool in 1994, according to Technician, a student-run publication at the university.
Before the PSA test, prostate cancer typically went undetected until the patient had symptoms or a doctor could detect it with a physical exam. By that point, it was often incurable. The test was “transformational,” said Matthew Nielsen, a urologist who chairs the urology department at the UNC School of Medicine at Chapel Hill.
Once men started receiving PSA tests, he said, the fraction of those diagnosed with metastatic cancer, or cancer that has spread to other parts of the body, dropped dramatically.
The test was widely used in the early years of its adoption, but it eventually generated controversy, Nielsen said. Many men have a low-risk, slow-growing type of prostate cancer that might not require immediate treatment. But upon hearing they had cancer, some frightened patients panicked and wound up going forward with surgery or radiation treatments with side effects that could cause more harm than good.
Concerns of overdiagnosis and overtreatment led the U.S. Preventive Services Task Force — a federal group that reviews all the data to find the best recommendations — to recommend against using the PSA test in all men in 2012.
But that “might have thrown out the baby with the bathwater,” Nielsen said.
As PSA testing rates dropped, so did the rates of new cases, he said. In the last few years, though, the incidence rates have increased, and more than half of that increase is in men diagnosed with metastatic disease.
Now, active surveillance helps balance concerns of overtreatment, Nielsen said. Health care providers have better insight into the risk level for a patient’s particular prostate cancer, and they can give patients the option of waiting on treatment, with frequent follow up to make sure more aggressive cancer hasn’t developed.
Pushing early detection
Almost two decades after her husband’s death, Wood started dating a man named Michael. Two months into the relationship, he was diagnosed with stage 4 prostate cancer.
Michael told her she could walk away — but Wood said since she’d already been through this once, she knew how to navigate the system. Michael received six months of chemotherapy and is in remission. They got married in December 2022.
Now, Wood pushes the men in her life to keep getting tested so that if they do have prostate cancer, it’s caught early. Her father and her late husband’s brother were both diagnosed.
Wood said she can understand how people without insurance might not want to go to the doctor, but “hiding your head in the sand” won’t keep someone healthy, either.
“Nobody wants to get it at stage 4 — I can tell you, I’ve been through that twice,” she said.
Catching the cancer early is key. Yet there’s sometimes a stigma around prostate cancer testing, Pierce said.
Men tend to downplay the importance of screening, often because of societal pressures, according to the UNC Men’s Health Program. Affording care is another barrier to regular preventative health appointments.
Passing this bill would at least remove the financial barrier — if not the mental one, Pierce said.
Most people get the PSA test from their primary care provider, Nielsen said. He works with primary care physicians to explain the value of PSA testing to those who may still be wary of overdiagnosis and overtreatment.
Fighting racial disparities
Expanding access to testing may also help address some of the gap between Black men and other groups when it comes to prostate cancer. Black men are 1.7 times more likely to get diagnosed and 2.3 times more likely to die compared with white men, according to the UNC Chapel Hill prostate cancer report card.
One factor in that gap might be genetics; men of African ancestry in many parts of the world have higher rates of prostate cancer, Nielsen said. Even in settings where men of different races have equal access to care, Black men have higher rates of diagnosis.
Access to care and factors such as socioeconomic status, education, employment and social support also play a role, he said.
“The single greatest opportunity to address that disparity from prostate cancer is better access to the PSA test,” Nielsen said.
Rates of Black men taking the PSA test are still lower than other groups, despite their higher risk, he said.
The bill’s aim of getting more men access to the test sounds like a good idea, Nielsen said, because the overall goal is to make those sobering statistics better for the next generation.
Next steps
House Bill 128 has been introduced but has yet to be heard in any legislative committee.
Reps. Timothy Reeder, R-Ayden, an emergency room physician, and Grant Campbell, R-Concord, an obstetrician-gynecologist, are co-sponsors of the bill. Rep. Mark Brody, R-Monroe, another co-sponsor, represents Anson County, which had the highest rate of new prostate cancer cases in the state in 2023.
Pierce said the bipartisan support in the House is a good sign. Sen. Kandie Smith, D-Greenville, said she would support the bill if it made it to the Senate, Pierce said.
“I would hope and pray that my male colleagues will say, ‘This is about saving the lives of not only men we know — our nephews, fathers, grandfathers, uncles, brothers — but also ourselves, possibly,’” he said.
5 Years Later, Long Covid Still A Medical Mystery: What Scientists Have Learned

Why do some people develop disabling chronic conditions after the initial viral infection?
(NBC News, Katie Camero) -- When her school closed down in March 2020, Chimére Sweeney, an English teacher in Baltimore, thought she’d return to her students once the U.S. got a handle on the new SARS-CoV-2 virus. But “life had a different plan” when she got Covid shortly after — and then never recovered, she said.
At first, Sweeney developed only muscle aches. By the second week, she started having panic attacks, blurry vision, constipation and partial hearing loss. Half of her face would freeze “like concrete.” She forgot phone numbers and addresses and she developed a stutter. Within a month after getting infected, she lost 30 pounds.
“I was told that after two weeks I would be better,” Sweeney, now 42, said. “But my two weeks never came.”
Almost five years later, she’s still struggling with severe whole body pain, sleeplessness, depression, painful rashes and boils, uncontrollable urination, short-term memory loss, and irregular periods.
“I went from being a healthy 37-year-old woman who may have had to pop an allergy pill every now and again, to taking over 10 to 12 medications per day to control almost every system in my body,” Sweeney said.

Since the World Health Organization characterized Covid as a pandemic on March 11, 2020, scientists don’t fully understand why some people develop disabling chronic conditions after the initial viral infection. The U.S. may be coming through the first post-pandemic winter without a major surge in cases, but each infection carries a risk of developing long Covid. Some scientists are calling for new types of clinical trials to be designed for the most debilitated long Covid sufferers.
Long Covid is known to cause over 200 different symptoms in nearly a dozen organ systems, including those of the heart, lungs, kidneys, brain, eyes and skin, but there’s no approved test for it or recommended treatment. Research shows long Covid is more common in middle-aged people, particularly women and those with weakened immune systems, but anyone who catches the virus can get it.
The Centers for Disease Control and Prevention has estimated that 1 in 20 adults in the U.S., or about 14 million, are living with long Covid. Other data shows that up to 5.8 million children may be affected by the condition as well. However, experts say these numbers are likely underestimated because there’s no official surveillance system in place.
A $1 billion research initiative called RECOVER launched by the National Institutes of Health to find the causes of long Covid, as well as potential treatments, has fallen short on its promises, scientists and patient advocates say.
Meanwhile, experts fear that the Trump administration’s extreme cuts in federal spending may undermine long Covid research efforts, which could further delay the discovery of therapies. Just last month, President Donald Trump terminated the Health and Human Services Secretary’s Advisory Committee on Long COVID.
Dr. W. Michael Brode, medical director of UT Health Austin’s Post-COVID-19 Program in Texas, said, “We’re building the boat while we’re at sea, trying to figure it out together [with patients] … but we absolutely need to build on the progress we’ve already made.”
“We have not delivered the answers commensurate with the public health crisis we’re facing,” he said.
What causes long Covid
SARS-CoV-2, which causes Covid, isn’t the only virus that causes lingering symptoms. Another condition called myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS), which shares many similarities with long Covid, is thought to be triggered by infections with the Epstein-Barr, influenza and varicella-zoster viruses, among others.
Covid is unique because it seems more likely to cause chronic illness than other pathogens, Brode said. Why it may lead to long-lasting symptoms is as yet undetermined. Experts have so far landed on several theories.
One idea is that remnants of the virus hide in different tissues after an infection subsides, Brode said. These viral particles continue to multiply or stimulate the immune system in ways that trigger long Covid symptoms.
Another potential cause involves the reactivation of other viruses, such as EBV and HIV, that have been sitting in a dormant state in people’s bodies.
It’s also possible that Covid tricks the immune system into producing antibodies that attack a person’s own healthy organs and tissues, said Dr. Igor Koralnik, co-director of Northwestern Medicine’s Comprehensive COVID-19 Center.
Some evidence shows that Covid affects the inner lining of the blood vessels, which can lead to the formation of tiny clots and help explain symptoms like irregular heartbeats and heart failure that some long Covid patients experience, Koralnik said.
It’s unclear whether one or a combination of these factors causes long Covid, experts say. But evidence suggests that they’re all associated with increased inflammation in the body, Koralnik said, which is why your risk of long Covid increases with each Covid infection.
“It’s like a river going over a dam,” Koralnik said. “The more episodes of Covid, the more the river level goes up to the point it overflows and there’s a flooding of long Covid symptoms.”
Diagnosing long Covid can be complicated.
Although we have diagnostic tools to confirm symptoms of long Covid, such as MRI scans for heart abnormalities, there’s no test that can diagnose the condition or distinguish it from similar illnesses, the CDC says.
As a result, people have to step away from work, school or other responsibilities to endure dozens of laboratory tests and scans that are not only expensive, but also stressful and time-consuming. It’s an extensive process of elimination that prevents people from getting the help they need, Brode said.
Clues in the eyes, gut and immune system
The challenge now is finding one or more biomarkers — genes, proteins or other substances associated with a specific condition — that can help diagnose long Covid.
A RECOVER study published last year found that routine lab tests, including 25 standard blood and urine exams, found few differences in biomarkers between people with and without prior Covid infection. The researchers concluded that these tests may not be useful in diagnosing long Covid.
Koralnik and his team recently discovered that people with long Covid have decreased blood flow in the small blood vessels in their retina, the light-sensitive layer behind the eye. This reduced flow is thought to decrease blood circulation in and around the brain, Koralnik said, which might “poison” tiny organelles called mitochondria that convert oxygen into energy.
This theory can explain why many people with long Covid experience cognitive issues, fatigue and exercise intolerance, Koralnik said. Overall, the findings, published in February in the Journal of Imaging, suggest the retina could be a long Covid biomarker.
Other research suggests promising biomarkers might exist in the gut and immune system, but Brode noted that these early findings are based on small groups of people and should be considered with a grain of salt.
As helpful as a diagnostic test would be for people with lingering symptoms, some experts say the lack of one shouldn’t slow scientists down in their search for long Covid treatments.
Julia Moore Vogel, senior program director with Scripps Research and contributor to the Patient-Led Research Collaborative for long Covid, said other conditions like migraine don’t have reliable biomarkers or tests to confirm diagnoses, yet several drugs are approved to treat it.
“I think we’ll get there,” said Vogel, who was a long-distance runner before developing long Covid in 2020 and now needs a wheelchair. “But I don’t personally feel like that should hold anything back.”
Disappointing progress in long Covid treatments
The Food and Drug Administration hasn’t approved any treatments specifically for long Covid. Experts aren’t sure we’ll get any soon.
“When I first got sick, I was like, OK, I just have to survive three to five years and I think there will be, at least, decent symptom management trial data so that we have options. But we’ve made almost no progress on treatments,” Vogel said. “There are now studies starting that are promising, but it’s nowhere near the volume it should be given the burden of disease.”
Most clinical trials are testing whether drugs used to treat other conditions prove helpful for long Covid. Researchers at the University of British Columbia, for example, are looking into low-dose naltrexone — a medication approved for opioid and alcohol use disorder. The drug is thought to have anti-inflammatory and pain-relieving properties, and is used off-label in people with fibromyalgia and ME/CFS, so it carries potential as a long Covid treatment, Brode said.
Other drugs like baricitinib, which is approved to treat rheumatoid arthritis and acute Covid, and temelimab, an experimental drug often given to people with multiple sclerosis, are also being investigated as potential long Covid treatments.
In lieu of specific treatments, people with long Covid must balance their rest and activity in a strategy called pacing, Brode said, and receive physical and cognitive behavioral therapy for further support. More often than not, many people end up relying on several drugs, including the antiviral Paxlovid, to treat symptoms.
Realistically, however, “we may not actually have a single, silver bullet treatment,” said Alison Cohen, an epidemiologist with the University of California, San Francisco who has had long Covid for three years. Long Covid manifests in such a wide variety of ways that it’s going to take a “multipronged approach” to find effective treatments, Cohen said.
What’s ahead for recovery?
As long as SARS-CoV-2 continues to spread, everyone is at risk of long Covid, Cohen said — and right now, evidence shows that recovery from the condition is rare. A study published last month found that only about 6% of people with long Covid recover after two years, according to Cohen. Covid vaccination was associated with better long-term recovery, especially among people who got the booster shots.
Those who do improve experience many “ups and downs,” Koralnik said. “You have to expect a lot of bumps in the road.”
“Living with long Covid is exhausting,” Cohen said. “So it’s important for everyone who is not living with it to think about what they can do to support folks who are.”
In the meantime, clinical trials must be designed to accommodate and include the patients they’re intended for, Vogel said. Many people are house- or bed-bound and can’t travel for multiple in-person visits and risk triggering a flare-up of symptoms, she added. “There’s just too much that you can’t know until you have them at the table,” she said.
There’s no telling when the long Covid community will finally get the answers and relief they need, but Vogel is keeping her head high.
“I know we can do it. I’m very confident that with enough trials that are well-designed, we can at least improve quality of life — if not cure the disease entirely,” Vogel said. “But I also can’t think any other way; I just can’t accept that this is it for my life.”
NCDHHS Livestream Spanish-language Cafecito and Tele-Town Hall: NC Crisis Services — Support for All Ages

NCDHHS Livestream Spanish-language Cafecito and Tele-Town Hall: NC Crisis Services — Support for All Ages
The North Carolina Department of Health and Human Services will host a live Spanish-language Cafecito and tele-town hall on Thursday, March 13, from 6 to 7 p.m., to discuss how people can support their mental well-being, find resources for youth and adults in North Carolina and get help for themselves or someone else experiencing a mental health crisis.
Event participants include:
- Kelly Crosbie, Director of the Division of Mental Health, Developmental Disabilities and Substance Use Services, NCDHHS;
- Carolina Siliceo Perez, MLAS, Acting Director for Latinx/Hispanic Policy and Strategy, NCDHHS;
- Martha Thompson, Community Health Worker, Strong Minds, Strong Communities, UNC Greensboro;
- Dr. Cesiah Hernandez, Psy.D., LCMHC, Mental Health Clinician, Lucy Daniels Center
Anyone can face mental health challenges. People of all ages and stages of life can be impacted themselves or through caring for a loved one who is struggling. Everyone in North Carolina needs access to mental health support and services:
- More than 1 in 3 high school students in North Carolina have reported feeling sad or hopeless, along with almost 1 in 3 middle school students.
- Nearly 1 in 4 adults in North Carolina have reported symptoms of anxiety or depression.
- Nationally, more than 1 in 3 Hispanic adults have reported these symptoms.
Help is available. Mental health crisis services offer non-judgmental, confidential and compassionate care to connect North Carolinians with resources and support — available at little or no cost — to get help with social or family situations, depression, anxiety, thoughts of suicide, substance use or if they just need someone to talk to.
The Cafecito will stream live from the NCDHHS Facebook and YouTube accounts, where viewers can submit questions. The event also includes a tele-town hall, which invites people by phone to listen in and submit questions. People can dial into the event by calling 855-756-7520 Ext. 119684#. Cafecito and tele-town hall panelists will discuss:
- Ways to support and improve mental well-being within the Hispanic/Latinx community
- Mental health resources for youth and adults in North Carolina
- What NC crisis services are, how to access them and how to request support in Spanish
- Where to find mental health information and resources in Spanish
The NCDHHS Crisis Services page, available in English and Spanish, gives North Carolinians someone to call, someone to respond and somewhere to go when they need support. The page includes a searchable map to find community crisis centers, as well as a zip code search to find a mobile crisis team. If you or someone you love feels overwhelmed, NC crisis services are here to help.
Texas Measles Outbreak Spreads to Oklahoma

Two measles case have been reported in the state. Both people were exposed to the outbreak that's growing on the western edge of Texas
(NBC News, Erika Edwards) -- A third state is now part of the growing measles outbreak in the U.S.
On Tuesday, health officials in Oklahoma reported two “probable” cases in the state that appear to be linked to the ongoing outbreak in Texas and New Mexico.
According to the Oklahoma State Department of Health, the two people developed measles symptoms after exposure to cases associated with the Texas and New Mexico outbreaks.
The people isolated immediately after they realized they had been exposed and stayed home throughout the period they were contagious, health officials said.
The two cases come as the outbreak in West Texas continues to grow.
On Tuesday, the Texas Department of State Health Services said that 223 measles cases had been confirmed in the state, up from 198 last week. The New Mexico Department of Health reported 33 cases, up from 30, in Lea County, which borders Texas.
Many of the cases developed in unvaccinated children.
“One of my concerns has been around travel,” said Katherine Wells, director of public health at the health department in Lubbock, Texas. “Communicable diseases do not know borders.”
Lubbock is the city where most of the hospitalized children in the outbreak have been treated.
Measles is one of the most contagious viruses on Earth. Unvaccinated people are most at risk for becoming infected, getting sick enough to be hospitalized and die from the virus.
Measles can be prevented with two doses of an MMR vaccine. The first shot is recommended around age 1, and the second shot at the beginning of kindergarten. Two doses are about 97% effective at preventing measles.
Other individual cases unrelated to the West Texas outbreak have also been reported this week, in patients in Maryland and Vermont who had traveled overseas.
“Everybody’s on high alert,” Wells said.
NC Health Insurance Provider to Stop Coverage at End of June, Impacting Thousands
 Thousands of families across NC could be impacted
Thousands of families across NC could be impacted
(WITN) -- Health insurance coverage for thousands of families across our state is in limbo after a major provider announced they’ll be stopping operations at the end of June.
The NC League of Municipalities’ Health Benefits Trust will be winding down operations effective June 30th.
It offers health benefits, including medical, vision dental and life insurance to government employees and their families.
A good number of local governments are members of NC League, but they don’t all get medical insurance through the trust.
Our WITN First Alert Investigative Team has learned that, at least in the east, it’s predominantly smaller communities that will feel the impact, but the people affects adds up.
NC League says that statewide, this will affect about 6,500 subscribers and their dependents, which is an additional 1,500. That’s a total of around 8,000 people.
WITN called around to more than a dozens towns and cities in Eastern Carolina and learned that Grifton, Farmville, Plymouth and Maysville are on the search for health insurance coverage.
In a statement sent to WITN, the league gives more insight into its decision.
Since 1983, the Health Benefits Trust, also known as the Municipal Insurance Trust (the Trust), has provided North Carolina’s local governments with employee health benefits, including medical, vision, dental and life insurance. On Feb. 12, 2025, the Risk Management Services Board of Trustees voted to close the Trust and wind down its operations effective June 30, 2025. This decision was not made lightly and many factors contributed to it, including the rising prices of medical procedures and specialty drugs. The Trust has taken measures to ensure the smooth transition of services and is actively working to support our members.
Oral Health Mystery Leads Patient to UNC School of Medicine
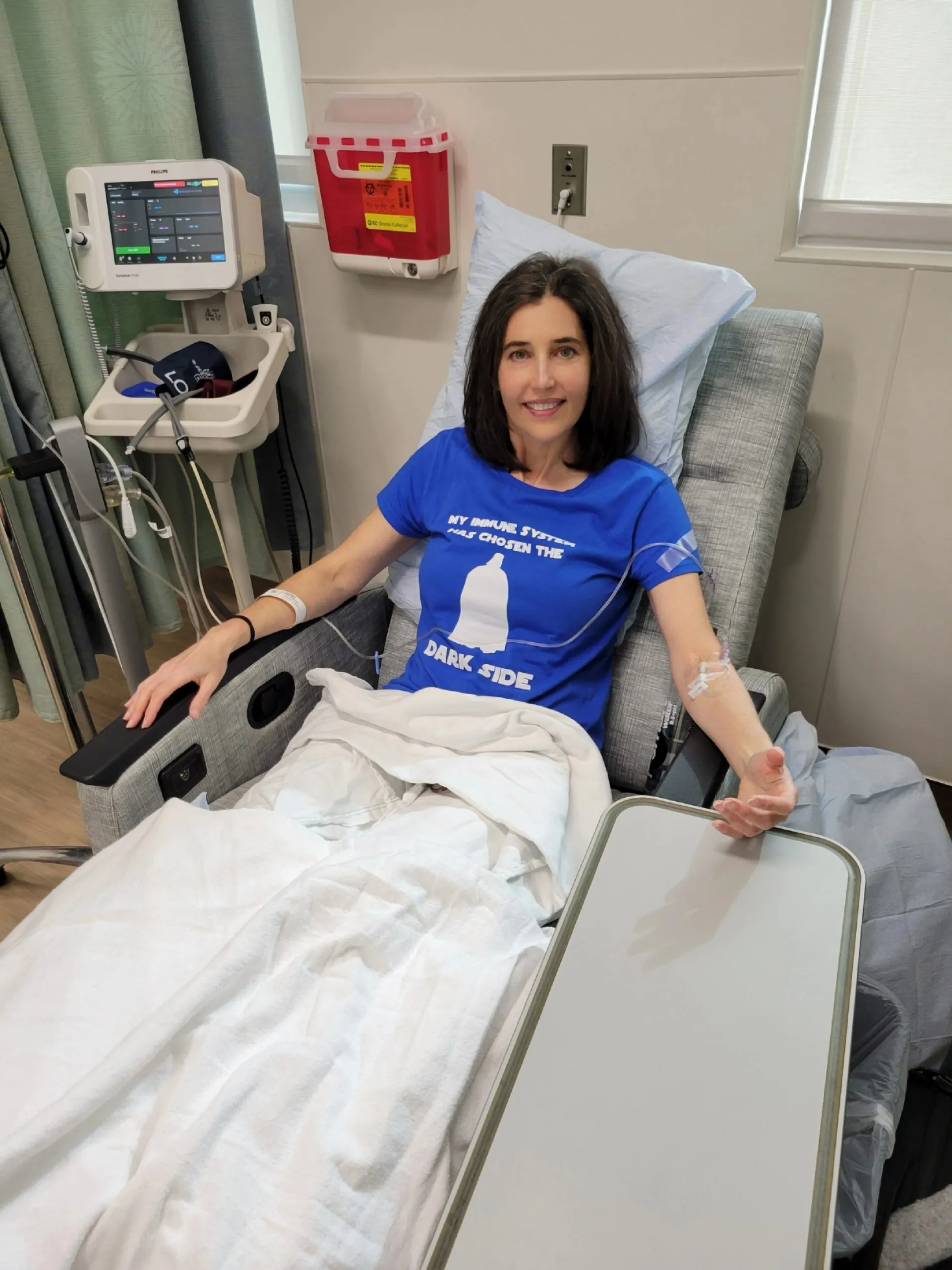
Unraveling an oral health mystery leads to rare autoimmune diagnosis
A Virginia resident’s 18-month medical journey brings her to a Chapel Hill dermatologist with expertise on autoimmune blistering disorders.
(NC HealthNews, Anne Blythe) -- Christine Letsky-Anderson remembers well the day that her medical odyssey began.
It was in the spring of 2023, and the Virginia resident was sipping a Chick-fil-A lemonade one morning. “My mouth burst into blisters everywhere,” Letsky-Anderson told NC Health News in a recent phone interview.
Finding the cause of those painful blisters that erupted into patches of sores sent her from one doctor to another for a year and a half before a dermatologist at UNC Health finally helped her solve the unrelenting mystery.
“Basically I had a bloody open ring that went around the entire perimeter of my mouth,” Letsky-Anderson recalled. “I got sores on the insides of my cheeks, my esophagus, my tongue, on the floor of my mouth, on the roof of my mouth — just exploded in these blisters and ulcers. I couldn’t eat any solid food at all. Even drinking water was painful.”
Letsky-Anderson’s journey is illustrative of a growing refrain in the oral health and broader medical community: the mouth is a window into overall health. Not only because oral conditions can be linked to systemic disease such as heart ailments, diabetes, cancer and, according to growing research, dementia, but also, systemic conditions can manifest in the mouth.
A director of creative services at James Madison University in Harrison, Virginia, Letsky-Anderson had been an active, social person with a wide circle of friends. She liked to hike, climb mountains, be outdoors with her dogs and travel. She led a healthful, mindful lifestyle.
Then, seemingly with no warning, that comfortable existence was pulled out from under her.
Googling for answers
All of a sudden, she was googling phrases like “mouth sores that don’t heal” with the word “autoimmune.” She suspected she might have an autoimmune condition since her father had celiac disease, and a cousin on her father’s side had immune system issues too.
She had just been to the dentist and did not have any problems with her teeth or gums at that time. The blisters weren’t on her gums anyway. Sexually transmitted infections can cause open sores, but she was confident that wasn’t what was going on.
“There were certain things that I knew I didn’t have,” Letsky-Anderson said.
Letsky-Anderson went to her primary care physician first, and he referred her to a rheumatologist. But there was a yearlong wait for her to see a nurse practitioner in the rheumatology practice.
So she was referred to a dermatologist, who could see her sooner.
The first dermatologist she saw “was tossing up things like Lupus, Sjogren’s syndrome — things like that,” Letsky-Anderson said. “She put a possible diagnosis of trench mouth down, and I had been to my dentist. It was not that, and she said, ‘Well, you’re really going to have to wait until you see your rheumatologist because this looks like it’s going to be something rheumatology.'”
When she finally got in to see the rheumatologist — it ended up being about a seven-month wait — she told her it was really the dermatologist she should be seeing. “So I got shuffled back and forth from one to the other,” Letsky-Anderson said. “I can’t eat at all. I mean, I was terrified of what’s happening to my body.”

Along the way, she lost more than 40 pounds.
By January 2024, skin lesions had spread to other parts of her body. That led to referrals to a gastroenterologist, a gynecologist, even a colorectal surgeon. She was given steroids and medication to try to calm the symptoms during the back-and-forth between doctors, but one of the drugs seemed to be exacerbating them.
Eventually, Letsky-Anderson’s rheumatologist referred her to Donna Culton, a dermatologist in the UNC School of Medicine who has a special interest in autoimmune blistering disorders. She draws patients from across North Carolina and neighboring states because of her expertise.
Letsky-Anderson was able to get an appointment within a month and made the trip from Virginia to Chapel Hill last year in late September, the same week the colorectal surgeon had wanted to schedule her for surgery for what at the time was believed to be a fissure related to steroid use.
Culton discouraged her from moving forward with the surgery. “She was like, ‘Don’t do it. …It could have catastrophic consequences for you,” Letsky-Anderson recalled. Because she had just been started on a new drug, Culton wanted to wait a couple of weeks to see if symptoms improved. If not, she wanted to do a biopsy.
In October, Letsky-Anderson was back in Chapel Hill for a biopsy of the blistering in her mouth. Within 24 hours, she heard the news she had been awaiting for 18 months.
“You have pemphigus,” Culton told her.
When Letsky-Anderson informed the surgeon of the pemphigus diagnosis, he told her it was good they had not taken that step. With other pemphigus patients, she said, it has resulted in fecal incontinence. “That’s a life-changing catastrophe,” she added.
The fight ahead
Pemphigus is a rare autoimmune disease for which there is no cure, but it can be controlled through treatment. The condition is known to come on in women when they are between 40 and 60 years old. It causes a person’s antibodies to attack one of the proteins that holds the skin together and causes blistering and sores on the skin and mucosal areas of the body.
Interestingly enough, pemphigus was a diagnosis Letsky-Anderson settled on herself in her early Google searches. She even told one of the doctors she saw toward the start of her quest for treatment that she thought she might have the condition. But a dermatologist in Virginia did only one of two biopsies necessary to fully diagnose the rare disease, and Letsky-Anderson, who had never had a biopsy before, assumed she had performed both.
“I thought from January 2024 until I got the diagnosis from Dr. Culton in October of 2024 that pemphigus had been ruled out,” Letsky-Anderson said.
Subsequently, many of the doctors she visited also thought pemphigus had been ruled out. Still in the back of her mind she’d wondered about the autoimmune disease until receiving the confirmation from Culton.
“I think I may have said to her, ‘I knew it,'” Letsky-Anderson recalled. “I can’t remember, but you know there’s a moment of like, I was still shocked, even though I thought from the beginning — there’s this vindication, validation that you were right. So I felt like, really, ‘Yeah, we got to the bottom of this.’ “
That comforting feeling quickly subsided to a realization of the fight ahead. “There’s a moment of kind of happiness and joy where you find your answer, but then you realize the consequences of the answer — how much the delay in my diagnosis set me back, it makes it less likely I’ll reach remission easily,” Letsky-Anderson said. “You know there’s just so many things that have been shocking to me to learn that if we had gotten on this sooner.”
Raising awareness
Emma Myers, a third year medical student at UNC Chapel Hill, has spent the past year as an Albert Schweitzer fellow trying to bring more awareness to autoimmune diseases and the difficulties diagnosing them — especially for women.
The fellowship is a yearlong service-based program that empowers graduate students to do a community health service project that helps address systemic health inequities. Not only are the students paired with a faculty member to try to identify barriers to care, the overall goal is to improve health equity.
Myers also is an autoimmune dermatology research fellow in the UNC dermatology department who calls Culton her mentor. While in clinic every Thursday, Myers said she hears anecdotes from many patients about “how it’s taken years and years and years to figure out their diagnosis and … hearing the struggle of their journey.”
Myers and Rashmi Deshmukh, a UNC dental student who also is a Schweitzer fellow, started an initiative called OASIS, or the Oral Autoimmune and Support Intervention Squad.
“OASIS is kind of a combination of dermatology, oral medicine and primary care, and it’s all about identifying autoimmune diseases earlier by identifying their oral manifestation,” Myers told NC Health News on a Zoom call with Zachary Brian, a professor at the UNC Adams School of Dentistry who’s working with the Schweitzer fellows and interested in equity-centered oral health policy.
Myers and Culton told NC Health News that many autoimmune conditions present first with vague symptoms in the mouth, and they noted that women are more disproportionately represented than men. Some research estimates that nearly 80 percent, or four of every five people diagnosed with autoimmune disease are women.
Culton and Myers stressed the importance of raising awareness about these rare diseases and of getting more physicians and oral health providers to realize that persistent blistering in the mouth could be early signs of a rare autoimmune condition that could benefit from early intervention.
Brian, who comes at the issue from an oral health perspective, agreed.
“We’ve had a long history talking about oral health as overall health, so a ‘window to the body’ as well as well-being,” Brian said. “And autoimmune, in particular — what’s fascinating about it, if that’s the right use of the word — is it disproportionately affects women, and something I think that’s really important is the gender bias that we have in health care.”
That can lead to much later diagnosis and treatment for some women, Brian added. “And so prognosis often is not as positive because they’re diagnosed much later and suffering for many years.”
Salt-and-vinegar chips
Letsky-Anderson has done much research into autoimmune conditions and her particular diagnosis throughout her medical odyssey. She wonders what would have happened had the first dermatologist she saw delved more into pemphigus.
“I just don’t think that you can dismiss things when someone comes in with weird symptoms. I think you have to look for weird answers,” Letsky-Anderson said.
Now, she’s undergoing a medical therapy that, as she describes it, completely shuts down her immune system for about six months. The hope is that somewhere between six and 18 months it will reboot without the autoimmune antibodies creating the pemphigus symptoms.
She has to work from home and make special arrangements to do something as common as going to a hair appointment. “When I go see a doctor, I wear an N-95 mask,” she said. “I’m getting a haircut next week, and they’re putting me in a private styling suite and making sure my stylist hasn’t been sick days before.”
Now that she can eat more than baby food, she’s gained about 10 pounds back.
“Being able to even chew chicken breast, that was something I couldn’t do for over a year — anything solid would just pull the flesh out of my mouth,” Letsky-Anderson said. “So just being able to bite into a grilled cheese sandwich, like a piece of chicken, or have a salad again, those things have been amazing to be able to eat that kind of food again.”
Still, there are some things she hasn’t been able to add into her diet yet. Acidic salad dressing, citrus, and something she craves — salt and vinegar chips — are still too tangy for her.
“I crave them,” she said. “I love tangy, vinegary things. That’s one thing I haven’t been able to go back to — salt and vinegar chips. They’re both crunchy and tangy. Those are both hard issues still.”
‘Just getting started’
One aspect of her journey that Letsky-Anderson would like to highlight is the toll that a medical mystery can take on a person’s mental health.
“The thing that was underplayed by a lot of the doctors until I got to Dr. Culton was the mental health burden of being sick like this,” Letsky-Anderson said. “Then when I got to Dr. Culton, they had all these resources in place.”
Through the OASIS program that Myers helped create, the two began doing online yoga classes together. One of the offerings is a support group with other patients going through some of the same issues. Not only does an expert come in every month to talk with them, but they have an opportunity to talk patient to patient.
“We’ve been doing OASIS for about a year now,” Myers said. “We’ve helped over 100 women who have oral symptoms who’ve either been diagnosed with or are undergoing workup for a diagnosis with an autoimmune condition.”
The program also does quality of life surveys, and, according to Myers, nearly 75 percent of the women that they’ve treated have “shown improvement with their quality of life scores as it relates to the oral symptoms since initiating care of the symptoms and collaborating with OASIS.”
Culton invited Letsky-Anderson to virtually attend an international conference that also addressed the mental health burden of the diseases.
“That’s a piece I felt was missing for the whole year and a half I struggled with a medical mystery,” Letsky-Anderson said. “Nobody seemed to care that I was falling apart.”
The conference, while interesting and overwhelming, also gave her a jolt of reality. “I started having the inkling that just getting the diagnosis was not the end of the road,” Letsky-Anderson said. “I mean when you search for an answer for over a year and a half and you get the answer, you think, ‘Ah, we did it.’ But going to the conference let me know that we’re just getting started.”
New Research: Nose Cartilage Can Help Repair Knee Injuries

Nose Cartilage Can Help Repair Knee Injuries, Researchers Say
TUESDAY, March 11, 2025 (HealthDay News) -- An awkward fall while running, skiing or playing sports can cause knee injuries that sideline players and increase their risk of future arthritis.
But most of the time, there’s nothing wrong with their noses, and that might prove the key to repairing their knees and getting them back on their feet, a new study suggests.
Replacement cartilage engineered from the nasal septum -- the cartilage wall that separates the left and right airways in your nose -- can be used to repair even the most complex knee injuries, researchers report in the journal Science Translational Medicine.
“Nasal septum cartilage cells have particular characteristics that are ideally suited to cartilage regeneration,” senior researcher Ivan Martin said in a news release. He's head of biomedicine with the University of Basel in Switzerland.
For example, it has been shown that these cells can counteract inflammation in joints, researchers said.
Torn cartilage in the knee can create long-term problems for active people, because this tissue does not heal itself. Cartilage forms a buffer between bones, and a loss of cartilage will eventually lead to arthritis.
The new knee repair process involves extracting cells from a tiny piece of a patient’s nasal septum, and then growing the cells in a lab on a scaffold made of soft fibers, researchers explained in background notes.
The newly grown cartilage is then cut into the required shape and implanted into the knee joint.
For their new clinical trial, researchers recruited 98 patients at clinics in four different countries.
The trial compared two different approaches involving cartilage grafts grown for only two days prior to surgery versus grafts allowed to mature for two weeks.
Results showed clear improvements in both groups, but those who received the more mature grafts fared better, researchers said.
They continued to improve even in the second year following the procedure, overtaking the group with grafts grown in a couple of days.
MRI scans showed that the more mature cartilage grafts resulted in better tissue composition at the site of the implant, even benefitting nearby natural cartilage.
“It is noteworthy that patients with larger injuries benefit from cartilage grafts with longer prior maturation periods,” investigator Andrea Barbero, a research group leader with the University of Basel, said in a news release.
This also applies to cases where previous cartilage treatments with other techniques have been unsuccessful, Barbero noted.
Researchers next plan to test this procedure’s effectiveness for treating wear-and-tear arthritis caused by the degeneration of knee cartilage.
The procedure could prove an alternative to knee replacement surgery if results pan out, researchers concluded.