Duke University is Betting on High Schoolers. Is This Good News for the Medical Profession in NC?

Duke University is Betting on High Schoolers. Is This Good News for the Medical Profession in NC?
(Becker's Hospital Review, Kelly Gooch) — In the past few years, a number of health systems have partnered with schools and nonprofits to support healthcare-focused high schools — and leaders say the results have been promising on a number of levels.
Dallas-based Baylor Scott & White Health collaborated with Uplift Education and Bloomberg Philanthropies to launch the Uplift Heights Healthcare Institute in 2024. Tenneil Dutton, senior vice president of talent and belonging at Baylor Scott & White, told Becker’s the high school not only prepares students for high-demand healthcare jobs, but equips them with crucial skills.
Take Neveah Money, for example — a teenager who saved her sister’s life thanks to CPR training she received at the school.
“What an amazing story; one of the first activities that they did as rising ninth graders last summer was to participate in a CPR course,” Phil Kendzior, vice president of workforce development for Baylor Scott & White Health, told NBC affiliate KXAS in May. “… It is very clear that the students are very engaged with the content they’re learning, and it’s wonderful that they’re able to apply it.”
In January 2024, Bloomberg Philanthropies launched an initiative to create healthcare-focused high schools by partnering with public school districts and health systems. Ten communities — urban and rural — were selected to participate in the effort, which graduates students into in-demand healthcare jobs to address workforce gaps.
“Since 2016, Bloomberg Philanthropies has invested over $100 million in career and technical education programs across the country,” Sneha Choudhary, the education communications lead for Bloomberg Philanthropies, told Becker’s. “We’ve learned that the most successful models involve training both within schools and directly at employer sites, and are deeply connected to the needs of specific industries and employers.
“We built upon these insights in 2024 with the launch of our $250 million healthcare high school initiative, partnering with leading health systems to prepare students for in-demand, well-paying careers in their own communities. We’ve found that healthcare systems are eager to invest in early talent development, and students are enthusiastic about pursuing meaningful healthcare careers — many of which don’t require a four-year degree.”
Schools have already opened in Boston (Mass General Brigham), Charlotte, N.C. (Atrium Health), Dallas (Baylor Scott & White) and Houston (Memorial Hermann).
The following schools are set to open in 2025 and 2026:
- Demopolis, Ala. (University of Alabama Health System and 11 other Alabama health systems) — 2026
- Durham, N.C. (Duke Health) — August 2025
- Nashville, Tenn. (HCA Healthcare, Ascension, Vanderbilt University) — August 2025
- New York City (Northwell Health) — September 2025
- Northeast Tennessee (Ballad Health) — August 2025
- Philadelphia (Children’s Hospital of Philadelphia) — August 2025
Becker’s spoke with leaders at several systems about their initiatives, including lessons learned in launching or scaling a healthcare-focused high school and the biggest surprises — positive or challenging — since the program’s inception.
Baylor Scott & White Health
Dallas-based Baylor Scott & White Health is the largest nonprofit health system in Texas, comprising 52 hospitals, more than 1,300 care sites, more than 7,200 active physicians, 57,000 employees and the Baylor Scott & White Health Plan.
As such, the organization is deeply engaged in large-scale medical education programs. Its partnership with Uplift Education and Bloomberg Philanthropies to launch Uplift Heights Healthcare Institute in West Dallas in 2024 aligns with that mission, Ms. Dutton told Becker’s.
Uplift Heights students choose from specialized tracks — biomedical science, nursing, healthcare therapeutic services or healthcare operations — and can earn certifications such as certified medical assistant or phlebotomist. The program includes simulation labs and mentorship from Baylor Scott & White professionals, as well as dual-credit opportunities through universities in the area.
Ms. Dutton noted that the process of launching the school happened at a rapid pace. The health system learned of the Bloomberg award in November 2023 and opened the school in fall 2024.
“As you can imagine, a very short time to completely stand up the program, which is a design of the curriculum — almost a complete redesign of the school,” Ms. Dutton said. “The high school components, the school itself, needed to be completely revamped, and simulation labs put in. And so we were off and running and moving aggressively.”
She said the health system recognized a few months into the development process the need to step back and “further align on our ‘why.'” This effort involved ensuring clarity around the vision as an organization as well as setting priorities for team members.
“Because on the surface it looked like just, ‘How do we fix and address the shortage of labor in the healthcare space?’ But we wanted to do so much more than that,” Ms. Dutton said. “Really homing in on our vision and almost building a new vision for this collaboration between entities was very important and became our North Star.”
During the process of standing up the school, Baylor Scott & White also recognized the need to further integrate clinicians and teachers at the earliest stage possible.
“Because it is an immersion-type experience for our students — or as we refer to the Uplift students, as scholars,” Ms. Dutton said. “We found that our clinicians, all busy, were very passionate about this initiative and ready to step in and help us. So bringing them in early on, where they could help co-design the curricula and the classes so that we could provide the scholars with those very real perspectives, that really was a key point. Anything we do when planning for the future, we make sure that we’re well represented at the table with those individuals.”
Baylor Scott & White also focused on ensuring parents of the students were part of the process early on.
Since the program’s inception, Ms. Dutton has been pleasantly surprised by the feedback.
“We knew people would be passionate about the project, but we could never have imagined how passionate and excited and enthusiastic the team would be,” she said. “Wee have seen from Baylor Scott & White’s end — all the way up to our executive leaderships, our CEO and especially our president, Julie Creamer — has really leaned in with us. And so we haven’t struggled with volunteers. Everyone’s doing their day job and is so willing to help.”
Ms. Dutton said early results from the school also suggest attendance rates are more than meeting expectations.
The success of revamping Uplift Heights into a dedicated healthcare high school has also led to expansion through a program at Uplift Grand, a public, college-preparatory charter school in Grand Prairie, Texas. The career and technical education healthcare pathway at Uplift Grand, which is the second phase of the partnership between Baylor Scott & White Health, Uplift Education and Bloomberg Philanthropies, is set to launch in the fall.
For other systems embarking on similar career and education pipelines, she pointed to the early engagement of the clinicians, the healthcare team.
“Don’t exclude them from the process, thinking that they’re too busy,” Ms. Dutton said. “That makes a difference. But at the same time, it’s not only thinking about the organization or the talent you want to build for today, but the talent for the future. Healthcare is rapidly changing and advancing — especially with AI coming into play — acknowledging solutions that we could not have even imagined. Patients becoming more of a consumer.
“Knowing what you want to build for the future — and it may not look like the talent that you have for today. So really thinking out of that — those competency skills of a future professional healthcare talent. That’s one that I think is very important.”
Ms. Dutton also recommended that systems consider the communities that house the school system.
“We’re not only educating scholars, but we’re also helping to educate, provide awareness and local healthcare resources to the communities that surround that school,” she said. “And that, we’ve seen, has been very powerful. It’s having a ripple effect.”
She said Baylor Scott & White has learned “to move and be resilient and flexible, to assess our program and adjust it and make incremental changes very rapidly. You can’t be focused on, ‘I know this is how we originally designed it, and we can’t be flexible.’
“We have an evolving audience here with students and scholars, so how do we continuously ask for feedback from those scholars, those students? Are we meeting your needs? From the teachers and from our Baylor Scott & White team to say, ‘Is this doing what we set out to do?'”
Along those lines, Baylor Scott & White is constantly meeting as a leadership team around Uplift to ensure the curriculum at the Uplift institute is “exactly what it needs to be for all of these stakeholders. There’s this continuous feedback and adaptation that takes place. It is very critical that we do that, and that anyone who does something like this does that as well.”
Mass General Brigham
Boston-based Mass General Brigham, in collaboration with Boston Public Schools and Bloomberg Philanthropies, launched an initiative in 2024 to expand and transform the Edward M. Kennedy Academy for Health Careers, a healthcare-focused public high school in the Boston Public School system. This expansion includes new health career pathways in surgery, medical imaging, and biotechnology/medical lab science, with a goal to grow enrollment to 800 students over five years.
Elsie Taveras, MD, the inaugural chief community health and equity officer at Mass General Brigham and executive director of the Kraft Center for Community Health at Mass General Brigham, told Becker’s that the system moved quickly to enroll students.
“We didn’t have a prep year,” she said. “We started right away because we already had a very solid and strong partner in Edward M. Kennedy Academy. They are a healthcare-focused high school — have been for years — and so we already knew we had a very strong base for adding on the new pathways for health careers that Bloomberg Philanthropies has made possible.”
She said the biggest takeaway from launching the Kennedy Academy has been about getting partners involved early and building in ample time for planning.
“This isn’t a solo endeavor,” Dr. Taveras said. “It’s a truly collaborative effort that weaves together everything from facilities and Career and Technical Education to Early College and career exploration. All these pieces have to click together just right to create a cohesive and enriching experience for our students within their school day. If you’re developing a similar model, we can’t stress enough: Bring everyone to the table early and invest the time up front to design a program that truly serves students well from day one.”
She also noted that organizers learned the importance of raising awareness about the healthcare high school’s offerings, especially in the Boston area, where students who are entering high school with interest in science, technology, engineering and math have many options. Mass General Brigham spent significant time on recruitment, enrolling and marketing.
Dr. Taveras acknowledged there is still work to do, as the initiative is slightly short of its goal of enrolling more than 200 students in the incoming ninth-grade class.
“So I also wouldn’t underestimate — for a new program — how much effort it is to communicate to students who have really great choices what a career in healthcare looks like, and what they would get out of our relatively new entry into the high school options,” she said.
She said Mass General Brigham has also learned “the power of purposeful planning and scheduling, especially when you’re trying to weave Early College and Career and Technical Education into an already packed school day.”
“Our school partner was phenomenal here,” she added. “They invested serious time adjusting and refining the schedule to ensure our students could truly engage with every single aspect of the program. Creating a schedule that genuinely supports meaningful student participation can make all the difference in crafting a seamless and supportive learning experience.”
One of the biggest positive surprises she pointed to since the program’s inception is discovering how much passion and natural curiosity students have for science, technology and healthcare.
“The on-site visits and guest speakers have been incredible at further igniting those interests and making future career pathways feel genuinely real and accessible,” she added. “I’ll never forget Vital Signs Day, for instance. Watching our students showcase their technical expertise and essential skills was truly inspiring.”
She also pointed to the “extraordinary” number of volunteers from the health system to serve as mentors.
“I think it’s because it pulls at people’s sense of purpose,” she said. “And I couldn’t be prouder of our system and our staff who have really engaged in being part of this initiative — mentoring students, teaching students when they come on site, asking to go to the school to give lectures, to meet one on one. It’s been fantastic.”
As far as scaling the initiative, Mass General Brigham set ambitious goals in its first year. Dr. Taveras said the health system applied for Massachusetts Early College Designation and Career and Technical Education Medical Assisting program approval. It also organized eight on-site visits and hosted 15 guest speaker events.
“We’ve also poured significant time into planning for Year 2 and beyond, always with our sights set on deepening the learning experience and broadening opportunities for our students,” she said. “All in all, we’ve made meaningful progress and feel incredibly optimistic about the even greater potential we see for the years ahead.”
Duke Health
Durham, N.C.-based Duke University Health System has partnered with Durham Public Schools and Durham Technical Community College to develop the Durham Early College of Health Sciences, which will welcome its inaugural ninth-grade class of 105 students in August. DECHS is tuition-free and will be located on Durham Tech’s campus. Students may choose from career pathways including nursing, surgical technology, allied health and clinical research.
Rhonda Brandon, senior vice president and chief human resources officer for Duke Health, told Becker’s leaders from the three educational entities have been collaborating for more than 18 months.
When asked about the most significant lesson learned thus far, she referenced the power of building partnerships from the beginning.
“Health systems can’t simply come in with a plan; co-creating the plan with educators, students, and community members is imperative,” Ms. Brandon said. “Each partner brings unique expertise, and with alignment around a shared vision, something that’s both practical and transformative is designed.”
She said the experience has also taught her that when it comes to workforce development, early exposure, education and understanding about careers, relationships, available opportunities and creating a sense of belonging are crucial.
“Designing with the community, not just for it, unlocks entirely new possibilities — not only for talent development, but for long-term economic mobility and student and family stability,” Ms. Brandon said.
Since the initiative’s inception, she said she has been encouraged by the enthusiasm across Duke Health.
“Our teams — from clinicians to researchers to administrative leaders — are genuinely excited to support this next generation,” Ms. Brandon said. “When our teams engage with this project and the students, our staff feel a great sense of motivation, inspiration and purpose. Many see themselves in these students and are eager to give back as mentors and role models.”
Still, she acknowledged the challenges of creating a program across three large organizations with separate systems, operational workflows, regulations and pressures.
“We’re navigating everything from policies for minors on-site, to training our workforce on how to engage with young students, to data-sharing agreements across institutions,” she said. “Yet, what’s been most inspiring is the shared commitment. Every partner is aligned around the same goal: to give students a unique, hands-on learning experience that prepares them to thrive — both in healthcare and in life.”
The initiative has already exceeded her expectations in terms of engagement among team members and community members. She said scaling has also revealed the importance of building durable infrastructure — including shared governance, funding strategies and cross-sector accountability.
“It’s not enough to have enthusiasm; sustainability requires coordination and long-term commitment across institutions,” Ms. Brandon said. “We’re still learning, but we’ve built a strong foundation.”
Her top lesson for systems embarking on similar education-career pipelines: Start with the “why.”
“For us, this is a strategic investment in the future — in our workforce and our community,” Ms. Brandon said. “We are strengthening the healthcare talent pipeline, improving long-term health outcomes and opening doors for students who may not have seen a healthcare career as something within reach. It’s about creating real opportunities for students to access well-paying, meaningful jobs that make an impact, offer career growth and drive economic mobility.”
She also recommended that systems plan for the full student experience. This includes resources such as counselors, mentorships, internships, transportation, meals and scrubs (uniforms).
These “aren’t ‘extras’ — they’re the foundation for student success,” Ms. Brandon said. “Creating an environment where students feel welcomed, prepared and supported is key. And honoring and respecting the role of families and communities is foundational — early engagement of parents and caregivers makes a lasting difference.”
She also told leaders to “be ready for the unknown.”
“There will be surprises and challenges; it’s part of the process,” Ms. Brandon said. “Trusting the people closest to the work to test, adapting and improving along the way, has been helpful. It’s an investment of time, but the long-term impact — for students, for future healthcare teams, and for the broader community — creates a great return on that investment.”
Deserts For Women’s Health Care Services Expand In Rural NC Counties

Deserts For Women’s Health Care Services Expand In Rural NC Counties
(Carolina Public Press, Jane Winik Startwell) — Rural hospitals could be putting pregnant women and babies at risk by slashing labor and delivery services across North Carolina.
Natasha Fuller delivered her two children at Charles A. Cannon Memorial Hospital in remote and mountainous Avery County in 2011 and 2014. Now, she works with AppHealthCare, assisting Avery County women who no longer have that same option.
Cannon Memorial shuttered its maternity ward in 2015. A substantial number of women in the area are confused and desperate for care.
Most Avery County women now travel at least 45 minutes through the mountains to reach the UNC hospital in Boone. A mother or unborn baby having high-risk pre-existing conditions could force a two-hour ride to Asheville. Some do not reach care in time.
Identifying and accessing care options has become more difficult and involved than ever before, not just in Avery County, but for mothers-to-be in rural counties across North Carolina.
This is part one of the three-part Carolina Public Press investigation Deserting Women, which examines state data on every hospital in North Carolina over the last decade. CPP found that hospital systems have systematically centralized services in urban areas while cutting them in rural ones, resulting in growing maternal health care deserts in nearly every corner of the state. Some rural hospitals have also cut or reduced certain critical OB/GYN services, leaving women more vulnerable to complications.
This article focuses on these data findings and their consequences. Subsequent articles will look at the systemic issues that contribute to these trends and possible solutions.
What NC data on labor and delivery services showed
A stark divide has emerged in North Carolina’s maternity care landscape: While hospitals in cities like Charlotte and Raleigh have added dozens of new delivery rooms, many rural facilities have been shuttering or downsizing their labor and delivery units.
The closures, reductions and existing gaps in service have created four distinct maternity deserts across the state: Far Western NC, Northwestern NC, Northeastern NC and Southern NC.
This analysis is based on documents CPP acquired from the NC Department of Health and Human Services in response to a records request. CPP examined License Renewal Applications from each hospital from 2013, 2018, and 2023. DHHS requires licensed hospitals to self-report annually the number of delivery rooms they offer.
CPP analyzed the number of delivery rooms and bedspace that hospitals reported on these applications, noting changes in the number over time. CPP then contacted the hospitals and relevant public health departments to verify these findings.

Between 2013 and 2023, nine hospitals in mostly rural counties completely eliminated labor and delivery service:
- Avery County
- Bladen County
- Caldwell County
- Cherokee County
- Macon County
- Martin County
- Mitchell County
- Transylvania County
- Davidson County, (although a second hospital continues to provide service in this county)
These closures are geographically distributed all over the state, but the majority occurred in Western North Carolina.
Meanwhile, other hospitals conducted service reductions and consolidation, further reducing the options for pregnant women in rural areas.
At least 29 delivery rooms were cut or repurposed at rural hospitals that did not fully eliminate services over the last decade in North Carolina. No regulatory structure exists to prevent hospitals from reducing the number of delivery rooms in their facilities. Women in counties like Stanly, Johnston and McDowell have reduced access as a result of this trend.
These reductions are not typically enough to make headlines — usually, the hospital just repurposes one or more delivery rooms for non-delivery purposes — but taken together, they demonstrate a willingness of rural hospitals to reduce services for women in silence.
In the 1940s, North Carolina public health officials envisioned having a hospital in every county, according to Ami Goldstein, an associate professor at the UNC School of Medicine’s Department of Family Medicine.
Today, that vision has eroded.
Twenty counties don’t have hospitals at all, and 20 more have hospitals that haven’t offered labor and delivery services in recent memory. That leaves only 60% of counties with any options for mothers-to-be. And those counties without options are often clustered together, compounding the challenges for their residents.
These changes are also having a ripple effect. As smaller facilities reduce services, major hospital hubs are seeing increasing patient volumes, including from residents of outlying areas.

Rural exodus and growth of women’s health deserts
North Carolina hospitals have executed a clear pattern of rural exodus and urban consolidation, from the mountains to the coastal plains.
For this project, CPP identified existing problems in each desert region and when and how they worsened.
Northwestern NC: The Northwestern NC maternity desert is perhaps the most severe. Four hospitals in the region have eliminated maternity services over the last decade.
Cannon Memorial Hospital in Avery County nixed its labor and delivery services in 2015, followed by Blue Ridge Regional in Mitchell County in 2017.
In 2019, UNC Health Caldwell in Caldwell County stopped serving pregnant women. A year later, Atrium Health’s Lexington Medical Center in Davidson County eliminated its labor and delivery services as well.
Beyond that, hospitals in Alleghany, Surry, Stokes and Davie don’t offer labor and delivery services. Two counties in the area — Yadkin and Alexander — don’t have hospitals at all.
In addition to the number of delivery rooms, License Renewal Applications also ask hospitals to report the number of births the hospital oversaw that year.

Lexington Medical Center saw a dramatic decline from 659 births in 2013 to 344 in 2018 before eventually closing its labor and delivery unit. If birth numbers drop and the hospital maintains the same level of service, the per-birth cost increases significantly, causing financial strain on the hospital.
The median number of births per hospital in North Carolina in 2018 was 443. Facilities that closed had birth volumes well below this number.
Many mothers in northwest NC now seek care in the urban center of Winston-Salem, at Novant Health Forsyth Medical Center and Atrium Health Wake Forest Baptist. Both of these facilities have greatly expanded capacity in the last five years, in part to account for the influx of patients from surrounding rural counties.
Women’s health care deserts don’t just impact women at the moment of birth. Women in these areas generally experience a lack of care throughout their entire pregnancies. This makes labor and delivery even more dangerous in places where care is further away, as worrisome conditions go unnoticed.
“Several years ago, we noticed that there weren’t any places to do prenatal care in the community in Alleghany,” Jen Greene, health director at AppHealthCare, told CPP.
“We decided that was a gap we needed to address for public health reasons. Those parents talked a lot about the apprehension they have about going into labor 45 minutes in any direction from a hospital. Some people choose to go over the state line into Virginia. But people want to have more options in their community.”
Northeastern NC: In northeast NC, 13 counties are without any hospital: Franklin, Camden, Currituck, Gates, Greene, Hyde, Jones, Warren, Northampton, Pamlico, Perquimans, Tyrell and Martin, whose hospital shuttered completely in 2023.
Two more counties have hospitals that don’t offer labor and delivery services: ECU Health Bertie in Bertie County and Washington Regional Medical Center in Washington County.
The latter facility went bankrupt in November 2024. Washington County has the highest infant mortality rate in NC. The rate of deaths for children of Black mothers there is five times higher than for white mothers.
Six out of the seven counties with the highest infant mortality rates in the state are in the east.
ECU Health owns eight hospitals in Eastern North Carolina. All are rural except their flagship facility in Greenville. The majority of high-risk deliveries in Eastern North Carolina take place at that hospital, according to ECU. Even so, the facility cut five delivery rooms there between 2013 and 2018.
ECU Health Edgecombe of Tarboro and ECU Health Roanoke Chowan of Ahoskie decreased their capacity by one room each over the years, according to the hospitals’ License Renewal Applications. The same is true for Wilson Medical Center in nearby Wilson County.
The health department in Hertford County has seen an increase in patients asking to receive prenatal care through the department rather than through the hospital in recent months, according to Amy Underhill, spokesperson for the Health Department.
This appears to be evidence of ECU Health quietly reducing services at its rural facilities, resulting in more women across northeastern NC travelling to Greenville or finding other options for care.
But ECU says otherwise.
“The licensed beds weren’t moved from those facilities; rather, the number of L&D (labor and delivery) rooms reported to the state in our license renewal applications was updated in 2019-2020 to reflect the way beds were being utilized, based on volume,” ECU Health spokesperson Brian Wudkwych told CPP.
One problem: No guidelines exist in the License Renewal Application for Hospitals specific to complete the part of the application relating to delivery rooms. How hospitals determine what number to report is entirely up to their discretion.
DHHS has very little regulatory oversight over hospitals’ level of maternity care and doesn’t even standardize the reporting process.
Far Western NC: Between 2013 and 2018, two hospitals eliminated labor and delivery services in far Western North Carolina: Transylvania Regional Hospital in Transylvania County and Angel Medical Center in Macon County.
Both of these hospitals are in the Asheville-based Mission Health network, as is the hospital in Mitchell County. They shuttered their maternity wards in the years before the biggest hospital corporation in the country, Tennessee-based HCA, purchased the previously nonprofit hospital group in 2019.
Yet another hospital in the region eliminated maternity services in 2019: Erlanger Murphy Medical Center in Cherokee County. The facility in Cherokee County was previously a locally owned community hospital, but acquired by the Erlanger group, an affiliate of University of Tennessee Health Science Center College of Medicine – Chattanooga. At the time, Erlanger gave assurances that its involvement would help sustain services.
Erlanger not only cut maternity services, but all obstetrics and gynecology offerings, CPP reported in 2019.
Nearby Swain County is home to two hospitals that don’t offer labor and delivery services: Swain Community Hospital, operated by Duke LifePoint, and the Cherokee Indian Hospital Authority, operated by the sovereign nation of the Eastern Band of Cherokee Indians.
Four more counties in the region are without any hospital at all: Clay, Graham, Madison and Yancey.
Transylvania County, whose services were eliminated in 2015, named maternal health as one of its top priorities in its 2024 Community Health Assessment. In a survey the county conducted, 42% of respondents said maternal health and mortality was a major problem in the county.
“Our nursing director shared that patients loved the labor and delivery services at Transylvania Regional Hospital, but some had always traveled out of county for care due to preference,” said Tara Rybka, spokesperson for the Transylvania County health department.
“(The nursing director) also said that, prior to closing the Transylvania Regional labor and delivery services, providers observed that they were seeing more ‘sick’ babies and were concerned about their ability to provide adequate care and the likelihood of a bad outcome. In smaller communities like Transylvania County, it can be a challenge to fully staff the entire suite of health care providers needed for more complex deliveries, especially as the workforce ages and fewer providers are entering certain specialties.”
Southern NC: The maternity care desert in Southern North Carolina is characterized by isolated pockets of limited care access in counties adjacent to or near the South Carolina line. Anson, Montgomery and Pender counties have hospitals that don’t provide labor and delivery services. Hoke County has two hospitals without these services.
Cape Fear Valley-Bladen County Hospital eliminated labor and delivery services in 2018, citing the extensive damage caused by Hurricane Florence. Hospitals in Sampson and Stanly counties have incrementally reduced services over the years.
The loss of services in just one county is enough to increase the risk for mothers and babies in that area.
On the other hand, Brunswick County, while still mostly rural, is the fastest-growing county in the state. Novant Health Brunswick Medical Center added four delivery rooms between 2018 and 2023.
Cases of increased care for rural women
Across North Carolina, a few hospitals like the one in Brunswick are bucking the trend of reducing and eliminating maternity care and other services for women.
In Western North Carolina, AdventHealth Hendersonville added 12 delivery rooms between 2013 and 2023.
Harris Regional Hospital in Jackson County recently brought on more midwifery and OB/GYN personnel. Hospitals such as UNC Health Pardee in Henderson County and Haywood Regional Medical Center in Haywood County are focused on expanding their breast cancer screening and treatment services.
In Central North Carolina, Chatham County’s hospital, operated by UNC Health, added an entirely new maternity wing in 2020.
Near the state’s southern tip, Columbus Regional Medical Center in Whiteville added eight delivery rooms.
Outcomes of less access to labor and delivery services
When emergencies happen in childbirth, they happen fast. The difference between having a hospital within 20 minutes versus two hours away can have life-altering consequences for both mother and baby.
In late 2024, a woman in active labor showed up at the doors of Angel Medical Center in Macon County. Angel had closed its maternity ward in 2017.
The hospital put her in an ambulance and transferred her to Harris Regional Medical Center in Jackson County, according to Dolly Pressley Byrd, chair of the obstetrics and gynecology department at Mountain Area Health Education Center, or MAHEC. The journey was supposed to take 30 minutes.
But it was too late. She delivered on the way. While she made it through, others in her position may not have been so lucky.
Transportation barriers compound the risks of childbirth, especially in the mountains. These long drives are the direct result of a decade of unit closures in Western North Carolina.
“The hospitals (in Western NC) that have labor and delivery units are primarily on that I-40 or I-26 corridor,” Pressley Byrd said.
“For those women who don’t live on those two major arteries, reaching labor and delivery services can take up to two hours. In the winter, on some pretty winding rural roads, the potential for treachery or a breakdown or inaccessible roads is increased.”
Now, Tropical Storm Helene has further isolated pregnant women and new mothers from life-saving care in Western North Carolina.
The storm interrupted prenatal care visits, forcing rescheduling due to transportation issues and road closures, said Allison Rollans, owner of High Country Doulas. Other impacts included “access to cooking, fresh food, clean water, hygiene for those who were displaced from their homes and those who lost power for weeks,” she said.
“Those who could (leave) often left the area if they were in their late pregnancy or early postpartum. I am sure some even had their babies off the mountain. Mission Hospital in Asheville was greatly affected in its ability to keep labor and delivery open due to the major water issues there.”
Plus, long travel distances and storm-related road closures can be a reason why things like pap smears and breast cancer screenings go unscheduled, leaving life-threatening conditions undetected.
Potential mental health issues in new and expecting mothers, and women generally, are also exacerbated by a lack of local care.
“Geographic and social isolation absolutely contributes to somebody’s ability to cope postpartum,” Karen Burns, program director at NC Maternal Health Matters, told CPP.
The consolidation of maternal physical and mental health care away from North Carolina’s rural counties comes at a cost.
“Instead of building community in rural areas, these hospitals and entities are building distrust of their care,” Rollans said. “Parents don’t necessarily see a provider until they’re deep into labor.”
It is becoming increasingly common for women to schedule a labor induction or C-section at a hospital with a labor and delivery ward, and book a hotel room in that area around the date of delivery, Rollans said.
But a lot of women don’t have the knowledge or funds to support that kind of decision.
“Birth is a beautiful thing punctuated by moments of emergency and sometimes terror,” Pressley Byrd said.
“When complications arise, they often do so quickly and are usually unforeseen. Postpartum hemorrhage, emergencies with moms or babies, respiratory distress for infants — those need to be assessed and addressed quickly. We need to do better.”
NCMB Extends Deadline for Physician Board Member Applications

NCMB Extends Deadline for Physician Board Member Applications
Application deadline extended! Physician applications for NCMB now due by June 30
Applicants are needed for three physician seats on the North Carolina Medical Board for terms beginning Nov. 1.
All positions must be filled by the process set down in statute (N.C. Gen. Stat. 90-2 and 90-3), which requires interested parties to apply via the Review Panel for the North Carolina Medical Board. The Review Panel is an independent body that nominates candidates for consideration by Gov. Josh Stein. By law, the Review Panel must nominate two candidates for each open seat.
One physician seat is currently occupied by individuals who are eligible for reappointment. However, incumbents must apply for reappointment via the normal application process.
Applications will be accepted online through 4:45 p.m. on Monday, June 30. For more information visit this website.
The Review Panel will consider only physicians (MDs or DOs) who hold active, unrestricted NC medical licenses. Applicants must be actively providing patient care at least part time and must have no history of disciplinary action within the past five years.
Applications will be accepted online through 4:45 p.m. on Monday, June 30. For more information, visit this website.
Updated NC Medicaid Standard Plan PCP Change Forms

Updated NC Medicaid Standard Plan PCP Change Forms
The Standard Plans (SP) have updated their PCP Change Forms. These forms may be submitted when a member requests to change their Primary Care Provider (PCP), thereby adding the member to the provider’s panel.
In response to provider feedback, the forms have been revised to allow PCPs to attest to verbal member consent in cases where a written signature cannot be obtained.
Below are the links to each SP’s updated form:
- AmeriHealth Caritas NC https://www.
amerihealthcaritasnc.com/ assets/pdf/provider/request- for-change-of-pcp.pdf - Carolina Complete Health https://network.
carolinacompletehealth.com/ content/dam/centene/ carolinacompletehealth/pdfs/ CCH-PCP-Change-Form-2025.pdf - Healthy Blue NC https://provider.
healthybluenc.com/docs/gpp/ HBNC_CAID_ ChangeRequestFormInst.pdf?v= 202505021752 - United Healthcare https://www.uhcprovider.com/
content/dam/provider/docs/ public/commplan/nc/forms/NC- UHCCP-PCP-Change-Fax-Form.pdf - WellCare https://www.wellcarenc.com/
content/dam/centene/wellcare/ nc/pdfs/NC_Caid_Prov_PCP_ Change_Request_Form_04_2025_R. pdf
NCDHHS Launches PATH NC

NCDHHS Launches PATH NC
(NCDHHS) — The North Carolina Department of Health and Human Services announced the launch of PATH NC (Partnership and Technology Hub for North Carolina), a new statewide information system that marks a major step forward in modernizing the administration of child welfare services. PATH NC equips child welfare staff with real-time data and decision-making tools to better protect children and to improve outcomes for children and families across the state.
Until now, North Carolina’s 100 county departments of social services, who administer child welfare services, have operated with a patchwork of independent data systems – nearly half of counties are still largely reliant on manual processes and paper records for child welfare operations. PATH NC will bring all 100 counties together for the first time into a unified system.
“PATH NC is more than a technology upgrade – it’s an investment in North Carolina’s children and families,” said NC Health and Human Services Secretary Dev Sangvai. “By providing social services staff with better tools, clearer data and integrated support, we are laying the foundation for a safer, more responsive child welfare system that delivers better, more consistent results – no matter where you live.”
NCDHHS' goal for PATH NC was not merely to create a system that collects information, but also to improve child welfare practice through evidence-based tools and actionable insights for the workforce. While developing the new system, the department worked in close collaboration with county leaders to fully redesign the state’s Structured Decision-Making (SDM) tools. Nationally certified by Evident Change for accuracy and consistent results, the new SDM tools within PATH NC help frontline staff better identify and assess risk and safety concerns when responding to reports of child abuse or neglect.
Over the last five years, NCDHHS has worked hand-in-hand with North Carolina’s county departments of social services to plan, develop and test both PATH NC and the SDM tools. The department’s projected total investment for the new system’s design, development, training and implementation is approximately $65 million. An early review of cases supported by PATH NC and the new SDM tools shows promising results – county intake decisions are consistently aligned with state policies and best practice in child protective services.
“We’ve built PATH NC from the ground up in collaboration with county leaders to ensure it meets the current, real-world needs of North Carolina’s child welfare social workers,” said NCDHHS Deputy Secretary for Opportunity and Well-Being Michael Leighs. “It’s designed to improve the everyday experience of staff while making it easier to track, report and respond to what’s happening in real time. PATH NC is a critical part of our work to transform the child welfare system and improve the lives of children and families in North Carolina.”
The new system aligns with NCDHHS’ broader efforts to strengthen system oversight and modernize service delivery. Key features of PATH NC include:
- Mobile-Friendly Design – The system supports documentation from the field, including some offline functionality, so that staff can update case records while conducting assessments, facilitating family visits, attending court and more.
- Decision-Making Tools – PATH NC’s new certified SDM tools provide built-in risk and safety assessments, dashboards and real-time alerts for county staff and supervisors.
- Advanced Capabilities – The system features global search functionality, comprehensive data analytics and dashboards. The platform also has the capability to add automated policy support functions and dedicated portals for providers and families in the future.
- Comprehensive Case Management – Fully implemented, PATH NC will include modules for intake, assessment, in-home services, foster care, adoption, financials, licensing and eligibility all together in one system.
- Data Accessibility – Once all counties have transitioned to PATH NC, staff will be able to access statewide data, including a family’s full history with child welfare services, regardless of whether they move or transfer to a different county.
- Integrated Systems – PATH NC is designed to interface with other child-serving systems such as NC Medicaid, the NC Department of Public Instruction and other partner agencies in the future, which will streamline information sharing and reduce administrative burden across the system.
The statewide rollout of PATH NC began June 2, 2025, with an initial cohort of 15 counties using the system to support child welfare intakes and assessments. Over the next eight months, all remaining counties will transition to PATH NC for intake and assessment. Implementation for ongoing case management modules will begin in early 2026 and is anticipated to be completed in summer 2026. This phased rollout allows NCDHHS to provide targeted training and individualized support as each cohort of counties prepares to transition to PATH NC. The department will continue to update and improve the system based on user feedback throughout the implementation process.
“PATH NC is going to be a game changer for the state, and we’re excited to be among the first counties leading the way,” said Christa Smith, Director of Forsyth County DSS. “The system gives our staff the right tools to make timely, informed decisions, and it gives our supervisors the data they need to identify trends and improve practice. We look forward to seeing everything PATH NC will do for us and our DSS partners across the state.”
PATH NC is a critical step forward in NCDHHS’ ongoing effort to transform child welfare in North Carolina through systemic change, increased access to services, better data and stronger alignment among state and county systems. By streamlining documentation processes and providing real-time access to child welfare data for users across the system, PATH NC offers more opportunity for state and county staff to pinpoint trends or challenges in child welfare practice and address them sooner – ultimately leading to a stronger system and better outcomes for children and families.
To learn more about ongoing initiatives to transform child welfare services in North Carolina, read NCDHHS’ Transforming Child Welfare in North Carolina: A Unified Vision for Children and Families.
Click here for NCDHHS B-roll footage of PATH NC for intake and assessments.
Empowering Future Clinicians: NC Advocacy in Medicine Fellowship Seeking Applicants

Empowering Future Clinicians: NC Advocacy in Medicine Fellowship Seeking Applicants
A groundbreaking new initiative is uniting all five North Carolina medical schools and physician assistant programs to train the next generation of healthcare advocates. The NC Advocacy in Medicine Fellowship is a state-wide program designed to equip medical and PA students with the tools to engage effectively in health policy and advocacy.
Through a series of dynamic workshops—both virtual and in-person—participants will explore the complex healthcare policy landscape of North Carolina, gaining insight into the state’s most pressing policy debates. Students will learn how to critically analyze health policy literature, build constructive relationships with legislators, and communicate persuasively with stakeholders, even when faced with opposing viewpoints. Upon successful completion of the program, all fellows will receive a certificate to honor their accomplishments.
With Intense Heat On The Way, Local Doctor Shares Ways Your Patients Can Stay Safe

With Intense Heat On The Way, Local Doctor Shares Ways Your Patients Can Stay Safe
(WTOC 11, Brontë Sorotsky) — It’s almost officially the first day of summer, but the Southeast is already starting to see those feel like temperatures get into the triple digits.
When it gets this hot, health experts say it can lead to more health concerns like heat exhaustion, especially for more vulnerable folks like young children and the elderly.
While this extreme heat may seem like a good time to hit the pool or the beach, doctors advise you to be on top of any signs of heat stroke before they can get too severe, especially when it comes to leaving kids or pets in the car.
Even if it’s only 80 degrees outside, within 10 minutes a car can start to get up to 99 degrees or more.
The U.S has already seen six reported deaths from kids getting heat stroke in cars.
Babies can’t regulate their temperature as well as older kids--which could pose more of a risk, but overall, anyone can start to experience organ damage if left unattended in a hot space like a car or elsewhere.
Dr. Michael Bossak at Memorial health says it’s important for parents to watch out for signs of heat stroke during these warmer months.
“Any increased tiredness, feeling like they have fevers or they’re hot, that they’re having difficulty with sweating or they’re sweating profusely, increased thirst and not having any urination. Those are all kind of signs that you are dehydrated and overheated," Dr. Bossak said.
As we get into summer, hydration is key.
It’s not just important to drink lots of water, but make sure you’re drinking lots of electrolytes as well.
Doctors also advise you to be cautious of how much time you’re getting in the direct sun. Being in the direct sunlight, especially for prolonged periods of time can be really dangerous, especially for kids and the elderly.
One of those dangers is sunburn, kids skin breaks down very quickly.
“Making sure that we are applying sunscreen on a regular basis and not just applying but reapplying every one to two hours to make sure that we’re maintaining that,” Dr. Bossak said.
He says it’s also important to look out for the older population during these hotter months--many of their heat exhaustion symptoms can be similar to children’s.
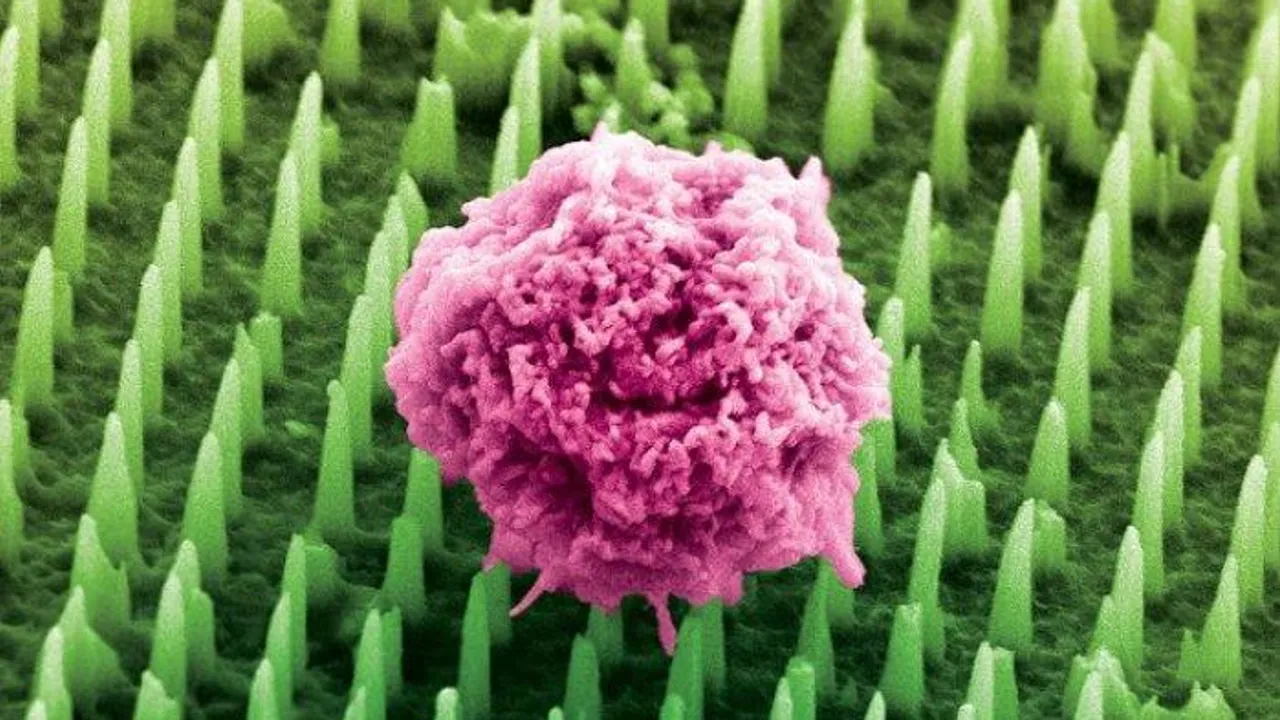
Nanoneedle Patch Could Replace Painful Traditional Biopsies
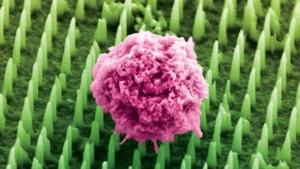
Nanoneedle Patch Could Replace Painful Traditional Biopsies
(News Medical Life Sciences, King's College London) — A patch containing tens of millions of microscopic nanoneedles could soon replace traditional biopsies, scientists have found.
The patch offers a painless and less invasive alternative for millions of patients worldwide who undergo biopsies each year to detect and monitor diseases like cancer and Alzheimer's.
Biopsies are among the most common diagnostic procedures worldwide, performed millions of times every year to detect diseases. However, they are invasive, can cause pain and complications, and can deter patients from seeking early diagnosis or follow-up tests. Traditional biopsies also remove small pieces of tissue, limiting how often and how comprehensively doctors can analyse diseased organs like the brain.
Now, scientists at King's College London have developed a nanoneedle patch that painlessly collects molecular information from tissues without removing or damaging them. This could allow healthcare teams to monitor disease in real time and perform multiple, repeatable tests from the same area – something impossible with standard biopsies.
Because the nanoneedles are 1,000 times thinner than a human hair and do not remove tissue, they cause no pain or damage, making the process less painful for patients compared to standard biopsies. For many, this could mean earlier diagnosis and more regular monitoring, transforming how diseases are tracked and treated.
Dr. Ciro Chiappini, who led the research published today in Nature Nanotechnology, said: "We have been working on nanoneedles for twelve years, but this is our most exciting development yet. It opens a world of possibilities for people with brain cancer, Alzheimer's, and for advancing personalised medicine. It will allow scientists – and eventually clinicians – to study disease in real time like never before."
The patch is covered in tens of millions of nanoneedles. In preclinical studies, the team applied the patch to brain cancer tissue taken from human biopsies and mouse models. The nanoneedles extracted molecular 'fingerprints' - including lipids, proteins, and mRNAs - from cells, without removing or harming the tissue.
The tissue imprint is then analyzed using mass spectrometry and artificial intelligence, giving healthcare teams detailed insights into whether a tumour is present, how it is responding to treatment, and how disease is progressing at the cellular level.
Dr. Chiappini said: "This approach provides multidimensional molecular information from different types of cells within the same tissue. Traditional biopsies simply cannot do that. And because the process does not destroy the tissue, we can sample the same tissue multiple times, which was previously impossible."
This technology could be used during brain surgery to help surgeons make faster, more precise decisions. For example, by applying the patch to a suspicious area, results could be obtained within 20 minutes and guide real-time decisions about removing cancerous tissue.
Made using the same manufacturing techniques as computer chips, the nanoneedles can be integrated into common medical devices such as bandages, endoscopes and contact lenses.
Dr. Chippani added: "This could be the beginning of the end for painful biopsies. Our technology opens up new ways to diagnose and monitor disease safely and painlessly – helping doctors and patients make better, faster decisions."
The breakthrough was possible through close collaboration across nanoengineering, clinical oncology, cell biology, and artificial intelligence-each field bringing essential tools and perspectives that, together, unlocked a new approach to non-invasive diagnostics.
The study was supported by the European Research Council through its flagship Starting Grant programme, Wellcome Leap, and UKRI's EPSRC and MRC, which enabled acquisition of key analytical instrumentation.
Funding Cuts Force One Of North Carolina’s Only Long Covid Clinics To Shut Its Doors

Funding Cuts Force One Of North Carolina’s Only Long Covid Clinics To Shut Its Doors
(The News and Observer, Nora O'Neill) — Finding treatment may soon become more difficult for the thousands of North Carolinians battling long-term COVID-19 symptoms. The UNC COVID Recovery Clinic, one of the only clinics in the state designed to treat patients with Long COVID, closed on June 16 due to funding cuts, according to a news release.
“UNC Health had provided support for the clinical program since 2021 but is unable to continue funding,” a UNC Health spokesperson told The Charlotte Observer without specifying why. The clinic did not receive federal funding, the spokesperson said. Since 2021, the clinic in Chapel Hill has seen thousands of patients, most of whom report fatigue, brain fog, sleep impairment, shortness of breath and anxiety lasting months or years after a COVID-19 diagnosis, according to data from the clinic. Some doctors who work at the clinic will continue to treat patients through the UNC School of Medicine, the release said, and care will remain in the same space as the COVID Recovery Clinic. “We are committed to ensuring that all of these patients continue to receive medical care, with as little disruption as possible,” a spokesperson for UNC Health said in a statement to The Charlotte Observer.
But for patients like Gillian Lizars, a 38-year-old Durham resident living with Long COVID, the closure means decreased access to knowledgeable doctors and worries about long-term recovery. “I got sick at 33 and I’m turning 39 next month… and the Long COVID clinic has been just a lifesaver,” Lizars The Charlotte Observer. “I’m concerned for incoming patients who are on their fifth, sixth, 10th COVID infection, developing Long COVID, not knowing it, going to their (primary care physician) and their (primary care physician) has no one to send them to.”
The closure means patients will no longer be able to visit the clinic for dedicated social workers, doctor referrals outside the local area, disability paperwork and insurance prior authorizations, according to UNC’s release. Lizars said she also is worried that her current doctors will have less time to treat her and other patients with Long COVID. She said developing a medical record is crucial to getting proper insurance coverage, and without regular treatment, it could be hard to get coverage or approval for disability benefits. “When these doctors are exclusively in the Long COVID clinic, those are the only patients they’re treating,” Lizars said. “I will definitely still be trying to see them, but now I have to make an appointment five months in advance.”
What is Long COVID?
Long COVID is a term used to describe a range of symptoms some people experience after developing COVID-19, according to the UNC School of Medicine. For many, the symptoms include fatigue, weakness, shortness of breath, cough, sleep disorders and memory problems. In North Carolina, one out of six people have experienced Long COVID, according to the North Carolina Department of Health and Human Services.
Since symptoms are wide-ranging, many people who are experiencing Long COVID symptoms are “scattered throughout the health system,” John Baratta, a doctor at the clinic, said in a UNC Research article. The clinic was designed to coordinate treatment efforts for these patients and provide access to experts in different areas of medicine, he said. For Lizars, Long COVID has left her feeling sick for years. She said she has an accelerated heart rate, low blood pressure, fatigue, migraines, cognitive dysfunction, difficulty regulating her body temperature, incontinence, tinnitus, and light and sound sensitivity. “Physically, I have lived with the flu every day for the last five years,” Lizars said. “There are periods when symptoms are exacerbated and I have trouble forming sentences, I can’t find words. I forget that I’ve put things in the oven, and then I start smelling smoke. I can’t follow a recipe without messing it up. That never would happen before.”
Proper treatment for patients with Long COVID is hard to come by, Lizars said. People’s symptoms differ and primary care physicians aren’t always knowledgeable about the illness, she said. It has been a struggle living with an illness that does not have a clear path to recovery.
“For all intents and purposes, there is very little care. You don’t want a disease that doesn’t have any answers” Lizars said. “You don’t want a disease that has no plan, no treatment.”
Digital Tool May Predict Childhood Asthma

Digital Tool May Predict Childhood Asthma
(HealthDay, Dennis Thompson) — A new digital tool can flag kids who are at risk for developing childhood asthma, researchers report.
The tool scans electronic health data records and calculates an asthma risk score for children, according to results published recently in eClinical Medicine.
It relies on information that’s routinely collected as part of kids’ medical history, researchers said.
"Our hope is that using the childhood asthma passive digital marker in clinical practice will improve the early detection of asthma risk in high-risk children, allowing for earlier interventions that could improve asthma control and lessen the future risk of hospitalization," lead researcher Arthur Owora, an associate professor of pediatrics at the Indiana University School of Medicine, said in a news release.
For the study, researchers used the tool to comb through records of more than 69,000 Indiana children born between 2010 and 2017, of whom just under 8% had been diagnosed with asthma after age four.
The digital tool was better able to predict which kids at age 3 had a higher risk of developing childhood asthma, results show.
The tool predicted asthma among 37% of those children, versus 26% using an earlier pediatric asthma risk score, researchers found.
Results suggest pneumonia and bronchiolitis are two of the most powerful predictors for childhood asthma, the study says.
The new tool could be an easily adopted means of helping doctors detect children at high risk for asthma, researchers concluded.
"This passive digital marker is very scalable because it requires zero additional minutes from the clinical team by using the already captured data in the electronic health record," senior researcher Dr. Malaz Boustani, director of the IU Center for Health Innovation and Implementation Science, said in a news release.
Prompt diagnosis of asthma can help parents and kids better avoid asthma triggers and improve use of asthma inhalers, researchers said.
"Scalable innovations like this in pediatrics have unbelievable public health impact for the health of the future generation of Americans,” Boustani added.
The team next plans to test the tool using a randomized clinical trial, to see if it actually increases early diagnoses among children at high risk of asthma.
"If the trial is successful, we will explore scaling up the implementation to ensure the benefits of early detection are realized at the state and hopefully at the national level as well," Owora said.
More information
The American Academy of Allergy, Asthma and Immunology has more on childhood asthma.
SOURCE: Indiana University, news release, June 11, 2025
Six 1st-Of-Its-Kind Procedures Performed In 2025, Including One at Duke

Six 1st-Of-Its-Kind Procedures Performed In 2025, Including One at Duke
(Becker's Hospital Review, Mariah Taylor) — In the first half of 2025, eight systems have performed first-of-their-kind procedures and clinical treatments.
1. Morgantown, WV-based WVU Heart and Vascular Institute physicians completed the world’s first robotic transcatheter aortic valve replacement explant and aortic valve replacement. The patient was discharged from the WVU Medicine’s cardiovascular ICU less than a week after undergoing the procedure.
2. A team of surgeons at Keck Medicine of Los Angeles-based University of Southern California and UCLA Health completed the world’s first human bladder transplant May 4. Over the eight-hour procedure, surgeons first transplanted the kidney, followed by the bladder. After the surgery, the kidney began functioning immediately, producing urine that drained properly into the new bladder. The patient has not required dialysis since the procedure.
3. A team from Children’s Hospital of Philadelphia and Penn Medicine successfully treated a patient with a customized CRISPR gene-editing therapy in a world first. The patient was born with severe carbamoyl phosphate synthetase 1 deficiency. Standard treatment for the rare metabolic disease is a liver transplant, but the patient was not eligible for these transplants. The team designed a unique therapy for the patient’s specific variant of CPS1 and delivered it via lipid nanoparticles. The patient received the first dose in February at 6 months old, and received a follow-up dose in March and April. He was discharged on June 2 at 10 months old.
4. The cardiac surgery team at Washington, D.C.-based Children’s National Hospital is the first in the world to replace an artificial heart valve with a live tissue valve through a partial heart transplant. In this procedure, the Children’s National team replaced an 11-year-old male patient’s artificial mitral valve with a live working valve from a donor heart.
5. Clinicians at the University of Maryland Medical Center in Baltimore removed a rare spinal tumor through a patient’s eye socket. The patient had two rare slow-growing developmental bone tumors called chordomas in her spine that wrapped around her brain stem. In two procedures, surgeons removed the tumor around the brain stem through the skull and with an endoscope through her nose.
6. A team from Durham, NC-based Duke Health performed the world’s first living mitral valve replacement after a heart transplant patient donated healthy valves from their original heart to two other patients. Following a full heart transplant on an 11-year-old patient, valves were donated to a 14-year old patient and a 9-year-old patient.
Cuddling With Your Sweetheart Before Sleeping May Decrease Relational Stress, Study Says

Cuddling With Your Sweetheart Before Sleeping May Decrease Relational Stress, Study Says
(Nice News, Rebekah Brandes) — If you share a bed with your sweetie, consider incorporating this step into your nighttime routine if you aren’t already: a snuggle sesh before sprawling out in starfish position or firing up the CPAP machine. A study found that couples who cuddled prior to drifting off experienced less stress and more feelings of security in the relationship.
The research was conducted by psychologist Josh Novak and cognitive development researcher Kaleigh Miller from Alabama’s Auburn University. They analyzed data from 143 heterosexual couples who had been together for an average of 13 years, and accounted for factors like sleep disorder diagnoses and whether kids or pets also slept in the bed.
In general, individual sleep position preferences didn’t match up with the positions couples took when cuddling. “This finding may suggest that individual sleep position may not be a driver or a factor in how a couple chooses to cuddle at night and rather is driven by a desire or need to be close to one’s partner,” the authors wrote, per Science Alert.
But regardless of preferred sleep positions, the subjects who were most physically close to each other at sleep onset reported feeling lower levels of stress, which was indirectly linked to lower levels of relational insecure attachment.
Noting that while further research is needed, the study authors concluded that “physical closeness at sleep onset may be a promising and amenable avenue for improving relational and physiological well-being.”
What perhaps might not come as a surprise to anyone who runs hot or thrashes around during slumber is that the research didn’t find cuddling at sleep onset to have a positive effect on sleep quality — nor a negative one, for that matter. It also only looked at the positions at one specific moment: right at the onset of sleep. It didn’t measure how people felt after staying in a close position during the night, which many might consider uncomfortable. Furthermore, the researchers note that a causal relationship was not determined, and in fact, having more secure attachment could be why couples feel less stress and cuddle more.
But, while everyone is different, it’s been well documented that physical affection — not just in a romantic sense — can improve our mental health. And when it relates to partners specifically, a 2014 study found that 94% of couples who spent the night in contact with each other reported feeling happy with their relationship, compared to 68% who didn’t touch.
Feeling inspired to get snuggly but are tired of playing little spoon? Try these 21 cuddling positions to find what feels most comfortable for you and your person.
Twin Doctors Commit To Rural Healthcare In WNC Amid Provider Shortage
Twin Doctors Commit To Rural Healthcare In WNC Amid Provider Shortage
(ABC News 13, Neydja Petithomme) — The shortage of medical providers in rural Western North Carolina has been a long-standing challenge.
At least 34 physicians, dentists, and pharmacists plan to remain in Western North Carolina after completing their residency or fellowship training, according to the Mountain Area Health Education Center (MAHEC)
Among them are Dr. Kaydie Murphy and Dr. Krystie Murphy, a pair of identical twin sisters from Colorado who have completed their three-year residencies in internal medicine.
They decided to stay in the WNC area to practice hospital medicine.
“We grew up in a rural community ourselves and are outside of town, away from medical hospitals, primary care provider hospitals and we saw the kind of deficit it does to a community,” said Kaydie Murphy. “We are one of three residents who signed a contract where we not only work at Mission Hospital but the rural associated hospitals as well, so we’ll be able to impact those communities as well."
The sisters began their internal medicine residencies at MAHEC in 2022 after earning their Doctor of Osteopathic Medicine degrees.

“Depending on the staffing needs is where we will be sent and right now, it’s looking like McDowell might need that,” said Kaydie, “We’ve been told at this point somewhere between 50% and 75% at Mission Hospital and the rest of that will be in the outlying communities, as they need us. On every other week basis, every few weeks, we will be in those communities.”
Krystie said the sisters plan to start their hospitalist position at the end of September. They will join 134 continuing trainees already at various stages of their medical education.
Out of the 16 graduating doctors specializing in internal medicine, 10 of them have decided to stay in Western North Carolina, including Kaydie and Krystie.
The ceremony was held at MAHEC’s educational building on Hendersonville Road, Asheville, in the Blue Ridge classroom on Friday, June 13.
Researchers Identify Cellular Hotspots That Trigger Ferroptosis

Researchers Identify Cellular Hotspots That Trigger Ferroptosis
(News Medical) — Researchers at the VIB-KU Leuven Center for Cancer Biology have uncovered how a unique interaction between two cellular compartments, namely the endoplasmic reticulum (ER) and mitochondria, can act as a central ignition point for ferroptosis, a form of cell death driven by lipid oxidation and iron. In a study published in Nature Cell Biology, the team of Professor Patrizia Agostinis highlights the role of ER-mitochondria contact sites (EMCSs) in setting off a cascade that leads to the death of cancer cells.
Ferroptosis is a type of cell death that happens when certain fats (called phospholipids, or PLs) in cell membranes get damaged by oxidation, as a consequence of the blockade of the cell's main defense system. This damage is known as lipid peroxidation and it's a key feature of ferroptosis. Once lipid peroxidation starts, it quickly spreads to the cell's outer layer, damaging the main barrier and leading to cell death. Ferroptosis is a recently discovered way that causes cell death, and it has been linked to the development and progression of various diseases, like neurodegenerative disorders and cancer. However, to date, where inside the cell PL peroxidation begins remains unknown.
In a study led by Professor Patrizia Agostinis of the VIB-KU Leuven Center for Cancer Biology, super-resolution live imaging was used to chart spatiotemporal events triggered by ferroptosis at the inter-organelle level. The research team tracked the precise moment PL peroxides form and spread within the cell. They found that the first cellular membranes susceptible to lipid peroxidation are the endoplasmic reticulum-mitochondrial contact sites (EMCSs). EMCSs not only expand rapidly in response to lipid peroxidation, but also play a key role in spreading the damaging lipids to mitochondria. In turn, this causes an increase in the production of reactive oxygen species (ROS) and fragmentation of these energy-producing organelles, which amplifies cellular damage.
Maria Livia Sassano, first author of the study: "Our findings show that EMCSs, because of their specific lipid landscape, act as functional command centers for initiating and propagating lipid peroxidation in cells undergoing ferroptosis. An exciting discovery because we now understand what initiates ferroptosis and how we can potentially control it."
Boosting ferroptosis to defeat cancer cells
Having discovered the role of EMCSs in ferroptosis, the researchers found that disrupting the physical link between the endoplasmic reticulum and mitochondria significantly reduced the accumulation of harmful lipid peroxides. This "untethering" effect effectively shields cells from undergoing ferroptosis. Conversely, enhancing and stabilizing the ER-mitochondria connections intensifies PL peroxidation and accelerates cell death
Building on these findings, the study shows that boosting EMCSs could be an effective strategy to enhance the vulnerability to ferroptosis of aggressive tumors, like triple-negative breast cancer (TNBC). TNBC tumors don't all react the same way to treatment, inducing ferroptosis. Those that naturally have more EMCSs are particularly vulnerable to ferroptosis, while TNBC in which the ER and mitochondria aren't in good contact, are more difficult to kill, but can be sensitized by forcing these organelles to come in close vicinity. Playing into this advantage, scientists can increase the tumor's susceptibility to lipid damage, effectively tipping the balance toward this type of cell death.
"Our findings may have relevant implications for TNBC, hormone-resistant cancers that are much harder to treat than other breast cancer types, since the 'EMCS status' could serve as a biomarker of the vulnerability of these tumors to treatments that induce ferroptosis" explains Professor Patrizia Agostinis of the VIB-KU Leuven Center for Cancer Biology. "On a more general note, with this new fundamental knowledge, we can begin to design strategies that specifically target and modulate these cellular hotspots. By doing so, we hope to enhance ferroptosis vulnerability, especially in those tumors that are resistant to current therapies, while on the other hand, to reduce lipid peroxidation and cell death in neurodegenerative diseases"
What Doctors Wish Patients Knew About Tendinitis

What Doctors Wish Patients Knew About Tendinitis
(AMA, Sara Berg, MS) — Whether you’re chasing home runs like Yankees slugger Giancarlo Stanton or just chasing your kids around the yard, tendinitis doesn’t play favorites. This painful tendon inflammation can strike anyone—regardless of age or fitness level.
While it’s often brushed off as a sign of “getting older,” tendinitis is linked to overuse, improper movement or even sudden increases in activity. The good news? With the right knowledge, it’s treatable—and often preventable.
The AMA’s What Doctors Wish Patients Knew™ series gives physicians a platform to share what they want patients to understand about today’s health care headlines.
In this installment, George C. Umeh, MD, a sports medicine physician at Bayhealth Orthopaedics in Milford, Delaware, took the time to discuss what patients should know about tendinitis.
Bayhealth is a member of the AMA Health System Program, which provides enterprise solutions to equip leadership, physicians and care teams with resources to help drive the future of medicine.
It is inflammation of the tendon
“Tendinitis is characterized as inflammation within the tendon, going from tendon pain to swelling and impaired function,” said Dr. Umeh. “A lot of times there’s the misnomer of tendinitis versus tendinopathy. Tendinitis is the acute inflammation of the tendon, so it’s what happens right away.
“It can be caused by microtears within the tendon, which come from overuse or repetitive motions. Imagine having those steel ropes and they have a little million fibers in them,” he added. “Tendinitis is where you get micro tears within that and it causes inflammation, which then causes pain.”
“Something you see a bit more for patients over a long term—which we’re using this term more now—is tendinopathy, and that describes chronic tendon degeneration,” Dr. Umeh said. “So, maybe you start to have inflammation acutely in the interim, but then over time when it’s become a chronic problem, it’s less of the inflammatory process that’s causing it.
“It’s more like the tendon didn’t really heal as well and the collagen, which is the main fabric or the main buildup of the tendon, is now causing a breakdown,” he added.
Tendinitis is often due to overuse
“What causes tendinitis to develop, is it’s an inflammatory process to start and then sometimes it can also be a degenerative process,” said Dr. Umeh, “similar to what you see with other degenerative things within the body such as disc disease or arthritis.”
“Over time, you keep using that tendon because your tendon is anchored to your muscle and anchored to the bone,” he said. “So, when you put it under a lot of stress with weights or activity or whatever you’re doing, it stretches that tendon.”
“Then once it gets those little damages, our body has inflammation process which goes to help heal it and can lead to things such as swelling and pain,” said Dr. Umeh. “But if you’re still having that swelling, it doesn’t really get a chance to heal appropriately.”
With shoulders, it’s overhead movement
“The most common areas of your body where tendinitis may occur depend on the spore, but the one you see the most is your shoulder. So, that’s rotator cuff tendinopathy,” said Dr. Umeh. “That’s a lot of when people say the rotator cuff is bothering them and they have difficulty with overhead activities. You can see that a lot with overhead athletes—such as baseball and tennis players—and laborers.”
“Your rotator cuff muscles are four muscles that attach into your shoulder,” he said. “And they basically help you stabilize your shoulder and help you with movement such as overhead activities, bringing your shoulders away from your body, reaching to get things overheard, putting on a jacket, taking off your shirt, those kinds of things.”
“Basically, any type of activity where you’re having your shoulders above your head for the most part,” Dr. Umeh said.
Runners often experience tendinitis
Then there is “patella tendinopathy, which is also known as jumper’s knee,” said Dr. Umeh. “You see that a lot with jumping athletes such as basketball or volleyball players. You also see it a lot in runners too because of the mechanism of running.”
“Then the one misnomer, especially for people who are runners, is Achilles tendinopathy,” he said, noting “that is damage within your Achilles tendon, which is the major tendon that goes from your calf and then inserts into your heel.”
With tendinitis, “it feels like a little bit of a headache wherever the joint is bothering you. You may get out of bed, your Achilles is really stiff, it continues to feel stiff and after you walk for a bit or ambulate throughout the day, it actually does start to get better,” Dr. Umeh said. “That gives us an idea that it might be related to tendonitis or tendinopathy.”
Tennis elbow is a form of tendinitis
Another form of tendinitis that sports medicine physicians see is “tennis elbow, which is right at the elbow. And that really is with repetitive wrist extension,” said Dr. Umeh. “We call it tennis elbow because the thought is that when you go to swing a tennis racket, you’re extending your forearm to the elbow.”
“That is one I will see for elbow-pain patients when they come in. It’s the first thing we’re thinking of,” he said. “The fact that you’re using it a lot—it’s not really giving the appropriate time for it to heal and manage well, so it just gets worse and worse.”
It can happen in your wrist too
The other area tendinitis can develop in “that is common too is called tenosynovitis,” said Dr. Umeh, “which is inflammation of the tendons in the wrist, causing pain, swelling and stiffness.”
“You see that a lot for hairstylists, gamers and people who are using their phones because of the position where you’re holding your phone or doing those things where your wrist is going to be in that position,” he said.
Aging can also increase risk
While the main cause of tendinitis is overuse, “there are a couple of risk factors that can predispose it,” said Dr. Umeh. “For example, age you get older, your tendons are more degenerated, so it’s likely to have a change in structure.
“Studies have shown that it is also more prevalent for women compared to men. Although, there is not an exact link,” he added. “There can also be genetic factors and conditions such as obesity, type 2 diabetes, high cholesterol that can lead to higher instances because now it is slowing your healing.”
An X-ray is not needed
Tendinitis requires “a clinical diagnosis from history and a physical exam. We listen to what the patient is saying, and we may get assessment of their strength within that particular tendon that’s bothering them and if they have pain, it is range of motion as well,” Dr. Umeh said. “A lot of these things can give a diagnosis.”
“Also, pain directly at the tendon is not really a symptom where you need imaging,” he said, noting that “X-rays don’t show tendons, so they aren’t really helpful in that sense. But X-rays can rule out a bone issue.”
“An ultrasound can help you take a look at the tendons. Sometimes we will do that because it’s more cost effective, you can get it quicker and it can give you a good look at the tendons to see if there are micro tears and if there’s little damage on the ultrasound,” Dr. Umeh said.
Physical therapy is key
When it comes to treatment of tendinitis, “physical therapy is definitely the cornerstone for it. A lot of times whether I’m giving them home exercises, I’m referring patients to a formal physical therapist,” Dr. Umeh said. “That’s usually the first thing I will always recommend for treating tendinitis.”
“There are different types of training that have been shown to help such as eccentric exercises, which emphasizes the lengthening of the muscle under tension,” he said. “So, imagine you’re doing a bicep curl and when you go to curl up, you let it down slowly. ... That’s been shown to be really helpful for repairing the tendinitis.”
Surgery is rarely needed
With tendinitis, “it’s not something that often needs surgery,” said Dr. Umeh. “It’s actually very rarely needed because more times than not this is just little damage so there’s not much that surgery is going to do to fix it.
“You don’t want it to get to a point where it then progresses to a tendon rupture because then that’s a lot of times where it does potentially need surgery to get it fixed,” he added.
Cortisone injections are temporary
“Patients will often ask if cortisone injections are a good option. I may do them sometimes for the shoulder,” Dr. Umeh said. “But the thing with that is that the more you do them, the more likely it is to damage the rotator cuff.
“I might do it to give a patient a short-term pain relief, but it’s not something that I would give them on a chronic treatment plan because then it’s just going to lead to further damage of that tendon,” he added. “So, if they come in and say they want to go to physical therapy, but their shoulder is really bothering them, I might give them a cortisone injection at that appointment so they can continue to do therapy and at least have a relief of pain while that muscle gets stronger.”
Wearing a brace can help
“Sometimes we talk about wearing braces to help offload the tendon,” said Dr. Umeh. “You can use a brace for your knee and your elbow.”
For example, “there are these tennis elbow braces and a counterforce brace that can help alleviate the tendon,” he added.
Start physical activity slowly
There are also “extrinsic factors—mechanical overloads—that can lead to tendinitis such as engaging in activities that require repetitive movements,” said Dr. Umeh. “If you’re not doing the movements right, then that can put strain on the tendon that you don’t want to happen.”
“The other thing we see too is a lot of times if you have an athlete or someone who says they are going to train for a marathon and they are just going to run 10 miles tomorrow, if you haven’t really run in the past week and try to ramp up, that is when you start to have those injuries too,” he said. “If you have such a sudden increase in activity intensity and you don’t really have good rest between those periods, that can also put you at risk for tendinitis.
“This is when you want to have a good regimen or plan,” Dr. Umeh added. This is especially important “if you’re going from someone who is very sedentary to now wanting to get back into activity because you don’t want to end up getting hurt in the process. Then you’re out longer.”
Make healthy choices
“Diet can also play a role in it too because your tendons are made of collagen,” said Dr. Umeh. “It’s been shown that having good protein and vitamin C or sometimes you can take collagen supplements to help support tendon repair.”
“Things like excessive alcohol and smoke also play a role. Avoiding excessive alcohol and smoking can also be good to making sure the tendon heals appropriately,” he said.
Advice For Trying GLP-1 Drugs For Weight Loss From A Doctor Who's Been There

Advice For Trying GLP-1 Drugs For Weight Loss From A Doctor Who's Been There
(NPR, Andrea Muraskin) — Dr. David A. Kessler has always been in the business of keeping people healthy – but by his own admission, he hasn't always applied that to himself.
Kessler's problem was with food. In medical school, greasy French fries and salted roast beef helped him stay up studying and researching late at night. Over the years, his weight fluctuated. He'd gain 20 or 40 pounds in a relatively short time frame, then slowly lose the weight, usually by going on a low-carb, high-protein diet, and exercising.
He went on to have a long career in public health, including a seven-year tenure as Commissioner of the Food and Drug Administration in the 1990s, where he advocated for better nutrition labels and against the tobacco lobby.
After spending two years stuck at a desk as chief science officer of the White House COVID-19 Response Team, Kessler had gained significant weight. His usual diet and exercise routine didn't help him shed pounds like it had in the past. Then an endocrinologist asked if he'd like to try one of the new class of glucagon-like peptide-1, or GLP-1, drugs that include Wegovy and Mounjaro.
He lost about 60 pounds within seven months of starting the injections. Kessler documents his experience in the new book Diet, Drugs, and Dopamine: The New Science of Achieving a Healthy Weight. He also breaks down the science behind obesity, and what makes these drugs so effective.
Here are eight takeaways from our conversation with Kessler about using the GLP-1 drugs, and the changing landscape of weight loss.

1. Our food environment drives weight gain
Foods high in salt, sugar and fat that are "highly palatable and energy dense" are pretty much everywhere and our brain chemistry drives us to consume them, says Kessler.
"We put [them] on every corner, and we made it available 24/7. We're living in a food carnival," he says. "What did we expect to happen?"
Kessler calls these foods "ultra-formulated" (instead of "ultra-processed") because they've been engineered to manipulate the brain's reward system. They can activate the same reward centers that addictive drugs do. "It's not willpower," he says. "It's biology."
He says GLP-1 drugs are remarkably effective in countering this pattern. "They have changed the landscape of weight loss," says Kessler.
And while he'd like to see the "root cause" of obesity and related chronic diseases tackled, he says he's "not optimistic that we're going to change the food environment overnight. In the meantime, these are effective tools."
2. Being overweight isn't always unhealthy but one kind of fat is
While BMI or body mass index has long been used to measure obesity, Kessler is among a growing number of scientists who say it's not a helpful indicator of health.
Rather visceral fat, which is found in and around abdominal organs including the stomach, liver and intestines, is the driver of metabolic disease, says Kessler. Visceral fat leeches fatty acids called adipokines or chemokines, which cause systemic inflammation in the body.
"And that inflammatory state results in organ damage that leads to cardiometabolic disease, kidney disease, diabetes, certain forms of cancer, and potentially certain neurodegenerative changes," says Kessler.
You can get a rough estimate of whether you're carrying a risky amount of visceral fat by measuring your waist circumference, Kessler says. A circumference greater than 40 inches in men, or 35 in inches in women is a rough indicator. You can also calculate your waist-to-hip ratio.
A body composition scan can offer a more precise measurement.
3. On GLP-1 drugs, get comfortable with being uncomfortable
The great thing about these drugs, says Kessler, is that they allow you to relearn how to eat. But that comes with some caveats.
GLP-1 drugs are powerful appetite suppressants, Kessler says. They increase feelings of satiety, making you feel full after a smaller portion than normal. They do this by slowing down the emptying of the stomach into the small intestine, thus keeping food in the stomach for longer.
This feeling of fullness can be unpleasant. Kessler describes it as being "at the edge of nausea." He compares it to the way your stomach might feel when you've eaten a bit too much at Thanksgiving dinner.
If you push through and keep eating anyway, you might experience GI issues like abdominal pain, diarrhea and vomiting. In the book, Kessler acknowledges that you can't really separate those unpleasant feelings from the effective mechanism of the drugs themselves.
"There's great variability," Kessler says. Some people take the drugs and lose weight with no side effects.
But for most, he says, there's an element of negative reinforcement. "If you know that if you put anything else in that stomach that's going to cause distress, you become conditioned to not to put more food in your stomach." As a result, patients start eating less, he says, and avoiding heavy foods.
At their worst, side effects such as vomiting and nausea or hypoglycemia can land you in the emergency room.
"I don't think the companies have leveled with the American public on how these drugs work," says Kessler. They can be a powerful part of a plan to achieve and maintain a healthy weight, he says, but the drugmakers and the FDA should do more to educate consumers about the side effects.
4. Find a good doctor, or better yet, a team
The side effects are one reason it's important to work with a physician who can monitor your progress and help you find the right drug at the right dose. It could be your general practice doctor or an internist, says Kessler. Working with an obesity medicine specialist, he says, is ideal, though he acknowledges finding one may be a challenge.
And since taking this drug will change your eating habits, Kessler recommends working with a dietician or nutritionist along with a doctor.
With good medical care, he says, many people can still take pleasure in food at those smaller portion sizes.
5. Eat plenty of protein, and fiber
GLP-1 medications don't change the fundamentals of healthy eating, Kessler writes, and it's important to be mindful about your food choices on the drugs.
He says if you're trying to lose weight, with or without drugs, protein is key, because it increases feelings of fullness. And, it can take the place in your meal of some of the bad stuff.
"If you are increasing the protein, you're decreasing the rapidly absorbable carbohydrates, you're decreasing fat, excess calories, and sugar," says Kessler.
And when you are on a GLP-1 drug, he says it's super important to eat foods high in fiber. Remember, the drugs slow down the emptying of the stomach into the small intestine, and that can lead to things getting backed up further down the line, Kessler says.
"People think constipation is just constipation, but that constipation can turn into intestinal obstruction that can cause perforation and people can die," says Kessler. "So keeping the GI tract healthy is essential."
And stay hydrated.
6. Know the risks, including those that aren't on the label
Kessler worries about people taking the drugs going too far in the other direction – from overeating to malnutrition.
"From what I can tell, many people on these highly effective drugs are eating less than a thousand calories a day, some as low as 600 to 800, and that is a level of semi-starvation," says Kessler.
Kessler says drugmakers should do more to inform patients about the risks of developing eating disorders, and gastroparesis – a chronic condition where gastric emptying slows down significantly.
It's also common to lose some muscle mass along with fat while on these drugs, which can be problematic, Kessler writes. One study he cites in the book showed that 40% of the weight loss in patients on once-a-week injections of semaglutide came from lean body mass. And about a third of that was muscle. That's a reason to keep on top of your nutrition and strength-training while on these drugs, he writes, "especially for older people like me, who are [already] susceptible to muscle loss."
There are people who should steer clear of GLP-1 drugs, Kessler notes, including those with a personal or familial history of certain thyroid and endocrine cancers, those with chronic kidney disease, pancreatitis, inflammatory bowel diseases, uncontrolled diarrhea or constipation or gastroparesis, or if you are pregnant.
7. Compounded versions of the drugs may be riskier
Kessler says compounded GLP-1s, which are often cheaper than brand-name drugs and can be ordered online, carry additional risks.
"A drug that's been approved by the brand name manufacturers…There are inspections, there's standards to make sure what's in the injectable actually matches what's on the label. The FDA's on top of it," says Kessler.
Whereas in compounded medicines, the active ingredients are manufactured abroad, shipped in bulk, and distributed to compounding pharmacies through middlemen. "I'm not even sure everyone can trace back where the drugs are being made," he says.
8. When it comes to going off GLP-1s, not much guidance is available
When Kessler reached his personal weight-loss target, he was developing some slight abdominal pains, so he decided to stop.
Once he went off the drug though, Kessler says he was flying blind when it came to maintaining his weight. And he thinks that's a problem.
"The companies and the FDA, no one's identified an endgame with these drugs," Kessler says.
He says there's very little data on whether or how the dose should be titrated to wean patients off, or how to adjust when your appetite and cravings start to return. In addition to working with your doctor to come off the drug, Kessler recommends a high-protein diet, because protein replicates the feelings of satiety you get from a GLP-1 drug, and may help you to sustain a lower weight.
Since that first seven months, he's been on and off the drug again.
AI Tool Developed by Johns Hopkins and Duke Predicts Infectious Disease Outbreaks More Accurately Than Current Methods

AI Tool Developed by Johns Hopkins and Duke Predicts Infectious Disease Outbreaks More Accurately Than Current Methods
(Gene Online, Mark Chiang) — Researchers at Johns Hopkins and Duke universities have developed an artificial intelligence tool designed to improve the forecasting, tracking, and management of infectious disease outbreaks. The tool reportedly outperforms existing state-of-the-art methods in predicting the spread of illnesses such as influenza and COVID-19.
The AI system utilizes advanced algorithms to analyze complex datasets, including historical disease patterns, environmental factors, and population dynamics. By processing this information, the tool generates more accurate predictions about when and where outbreaks may occur. Researchers suggest that its enhanced forecasting capabilities could assist public health officials in implementing timely interventions to mitigate the impact of infectious diseases. The development marks a significant step forward in leveraging technology for epidemic preparedness and response efforts.
Read more on Johns Hopkins' HUB: https://hub.jhu.edu/2025/06/06/artificial-intelligence-infectious-disease-forecasting/
How Incarcerated People Are Helping Prevent Suicide Behind Bars

How Incarcerated People Are Helping Prevent Suicide Behind Bars
(NC Health News, Rachel Crumpler) — For up to four hours at a time, William Buhl attentively monitors a person who is on suicide watch at Nash Correctional Institution — a medium custody prison in Nashville. Buhl sits at a table outside a cell with a direct view of his subject. He observes their behavior, records notes every 15 minutes and offers an open ear.
He’s there as a peer observer — a fellow incarcerated person who has been screened and trained to observe and engage with people in mental distress and on suicide watch.
It’s a duty Buhl and other peer observers said they don’t take lightly. The objective is to keep people alive and see them improve.
“Lives are important, and they’re valuable,” Buhl said. “Somebody out there loves us.”
Prison officials launched the Peer Observer Program as a suicide prevention strategy recommended by the department’s Suicide Prevention and Self-Directed Violence Workgroup. The group convened after a spike in suicides in 2018, when 11 people died in custody — up from six the year before.
Buhl became one of the North Carolina prison system’s first peer observers in November 2019 as part of the program’s pilot at Mountain View Correctional Institution, a medium security prison in Mitchell County.
He was motivated to take part because, about a year before, he lost a friend to suicide. Someone, he said, who was more like a brother.
Buhl, who has been incarcerated for nearly 20 years, can better relate to the struggles in prison that may contribute to mental deterioration: separation from family, the toll of long sentences, and interpersonal conflicts within cell blocks. His shared lived experience often means the people he observes are more likely to open up to him.
“Another inmate will talk to another inmate quicker, a lot of time, than they will staff, especially when they realize that we’re wearing the same clothes they are,” Buhl said.
In 2024, peer observers worked 5,356 hours conducting suicide watches, according to Department of Adult Correction data provided to NC Health News.
Lewis Peiper, chief of behavioral health at the Department of Adult Correction who led the workgroup, said they learned about using peers to help monitor people on suicide watch from Gary Junker, the head of behavioral health at the time. Junker had helped implement a peer observer program at the federal prison in Butner when he worked there.
“They found that not only is there benefit to staff — for the staff not sitting on the watch — but it improved the experience of the watch for the people involved,” Peiper said. “Sometimes a person in a uniform within a prison population, they can be seen almost as an adversary … Having a peer, it can kind of just lower the tenor.”
A 2005 peer-reviewed evaluation paper on the federal peer observer program called it a “win-win solution.” The researchers found people spent less time on suicide watch when watched by another incarcerated person without compromising the standard of care. The researchers also found that observers themselves felt personal gain from being able to help.
Modeled after the federal program, Peiper said the use of peer observers in North Carolina prisons has so far been effective. A March 2022 cost-benefit analysis report by the North Carolina Division of Prisons’ Innovation Institute recommended expanding the program, which has slowly spread to 72 peer observers serving across five prisons.
“It’s simple, yet it works,” Peiper said. “It has an impact on the environment and the experience of suicide watches on the individuals and on the prison.
“There’s something powerful about when you bring folks in and have them trained into a role,” he said. “It’s a trusted role. It’s got guardrails on it for safety purposes, but they become great ambassadors for mental health. And they can have a reach well beyond what a licensed psychologist might be able to have on their own.”
Physician End-of-Life Preferences Expose Stark Differences

Physician End-of-Life Preferences Expose Stark Differences
(Psychiatrist, Denis Storey) — Clinical relevance: Research reveals that while most physicians prefer end-of-life comfort over life-extending measures for themselves, their views vary widely.
- Local laws strongly influence support for assisted dying, with physicians showing higher acceptance where it is legal.
- Specialty and personal beliefs shape physician attitudes more than demographics.
- Ethical tensions arise as doctors balance personal preferences, legal restrictions, and professional responsibility.
The Journal of Medical Ethics has published a new global study that doesn’t just pull the curtain back on how doctors feel about their own end-of-life care. It reveals just how widely those personal preferences vary. Multiple factors figure into that calculus, from geography to local law to their own personal beliefs.
The paper, based on data culled from five countries spread across three continents, reports on physician perspectives on life-extending treatments, palliative care, and assisted dying in a pair of equally tragic scenarios: advanced cancer and Alzheimer’s disease.
Physicians Favor Comfort Over Extreme Measures
The overwhelming majority of the physicians surveyed – more than 90% – expressed a preference for symptom alleviation using medications in end-of-life scenarios. More than 95% would forgo life-sustaining interventions like CPR, mechanical ventilation, and tube feeding.
These findings persist across jurisdictions regardless of local laws and regulations. And they highlight a growing discomfort among doctors over aggressive treatment measures they often oversee in the real world
The surveyed physicians appeared to be equally unsettled about palliative sedation. In Alzheimer’s disease cases, for example, 39% to 66% of physicians would entertain the idea. Those numbers were a little higher for the cancer hypothetical, with 43% to 82% of the survey respondents giving it serious consideration.
Legal Status Shapes Attitudes on Assisted Dying
The study’s primary revelation is the strong link between a jurisdiction’s legal environment and physician support for assisted suicide. Where euthanasia is legal, in areas such as Belgium, Canada, and Victoria, Australia, 59% to 81% of physicians said they would think about euthanasia for themselves in the advanced cancer situation. Physician support was about the same, though slightly lower, when they faced the Alzheimer’s case.
Even in Queensland, Australia, where lawmakers legalized euthanasia (but before it went into effect), half the physicians supported euthanasia in both scenarios.
These results, the authors argue, suggest that when assisted dying is legal (and morally accepted), physicians are more willing to embrace it for themselves. This shift probably stems from greater exposure, familiarity, and comfort with the practice, as well as seeing firsthand how it helps patients.
On the other hand, in jurisdictions where the practice remains illegal or tightly regulated, support fell off dramatically.
Practice Type (and Faith) Matter
Physician backgrounds also played a role. For example, palliative care physicians supported palliative sedation more often than euthanasia. General practitioners – who typically serve as the primary providers of assisted dying where it’s legal – showed higher levels of support for euthanasia.
Faith also emerged as a major factor. Physicians with stronger religious beliefs appeared less likely to support assisted dying, which underscore the ethical conflict between personal convictions and professional obligations.
Notably, other factors – such as age, gender, and ethnicity – seemed to exert little influence.
Ethical Bedside Dilemmas
While many physicians professed clear preferences for their own care, applying these preferences to the care of their patients raised more than a few ethical questions. Should a physician’s personal beliefs influence how they guide end-of-life discussions? Patients usually seek out their doctor’s opinion during making such decisions. But many doctors hesitate to share their views for fear of tipping the scales on what they see as the patient’s decision.
But research has (repeatedly) shown that some patients want to know what their doctor would do in a similar situation. This, the authors contend, points to the need for doctors to maintain a careful balance between professional neutrality and empathetic transparency.
In some places, such as Victoria and South Australia, legal restrictions prevent physicians from even initiating conversations about assisted dying with their patients. It’s obviously meant to protect patients. But, such policies also limit access to comprehensive end-of-life options and contribute to inequities in care.
A Call for Thoughtful Dialogue
The Alzheimer’s scenario that the researchers presented exposed something else: a lot of doctors would consider euthanasia for themselves. And this is despite the disease’s progressive nature, which can make informed consent problematic. This highlights the need for a longer conversation around assisted dying in cases involving cognitive decline, where competency is compromised and laws often erect barriers to such interventions.
Ultimately, the study reminds us of the significant ethical, legal, and emotional challenges physicians face in navigating end-of-life care – both for themselves and their patients. It reveals a robust consensus around avoiding life-prolonging treatments, broad variability in attitudes toward assisted dying, and a complicated relationship between personal beliefs, professional roles, and a shifting legal landscape.
High-End Baby Monitors: When They Help And When They Hurt
High-End Baby Monitors: When They Help And When They Hurt
(Novant Health, Katie Toussaint) — After we brought our baby girl home from the hospital in October 2024, it didn’t take long for the baby monitor to start driving me bonkers. In the first months – especially after a traumatic health scare with a BRUE – I clicked on the video monitor obsessively during her naps to reassure myself that she was fine. If she hadn’t made a sound in 15 minutes, I’d click the monitor to take a look. If she hadn’t changed positions, I’d click-click-click to zoom in and make sure I could see her breathing.
But by six months, I started to get it under control. I realized the monitoring was making me anxious and distracted – I felt frenzied trying to wrap up a work task or house chore when she made the slightest movement. Plus, our house is small and I can easily hear her when she cries. Now, I mostly only look at the monitor when I hear her cry: Do I really need to go grab her, or is she self-soothing back to sleep?
So … am I doing it right? Is it wrong that I’m not monitoring her more closely when there are expensive monitors promising peace of mind and measuring oxygen levels, heart rate and sleep patterns? Is it weird that the camera monitor ramps up my anxiety instead of putting me at ease? How do parents like me monitor our babies to make sure they’re safe, while also protecting our own sanity?
I talked to Dr. Megan Collins, a mother and pediatrician with Novant Health Dilworth Pediatrics, as well as Jaren Doby, a parent and social worker with Novant Health Psychiatric Associates - Randolph. Here’s what I learned.
Does the average healthy baby need digital monitoring?
Collins: The most ideal form of monitoring is your own ears in a room-share, or having your baby sleep within hearing distance. If you can room-share in the first six months, there’s an association with a reduced risk of SIDs, but room-sharing isn’t possible for everyone.
While baby digital monitoring isn’t critical, are there still scenarios where it can be helpful?
Collins: If you’re going to be out of hearing distance, like if you’re playing outside with your older child while your baby naps, an audio monitor can be sufficient.
Is it normal to feel the urge to continually check the baby monitor?
Doby: Parental anxiety is normal – you’re responsible for the well-being of a new person. The concerns we have for our children and making sure they are OK is normal. For parents who have experienced a traumatic event or who have a child with health problems, this can also be an understandable form of hypervigilance. It’s natural to be on guard, looking for potential threats even when there is no real danger.
For some parents, fancy baby monitors do offer peace of mind. For others, they can start to generate an unhealthy fear response, is that right?
Doby: When it becomes clinically distressing, impeding on your ability to function around your home and take care of yourself, this is when we start getting into areas of more concern. We have to be careful that this isn’t placing inherent fear in us: That you have to constantly make sure your baby is OK and, if you don’t, that your baby won't be OK.
Are at-home digital baby monitors accurate when it comes to health information?
Collins: At times, monitors can lead to unnecessary emergency room visits, if parents see something on a monitor at home that indicates changes in pulse rate or oxygen levels, when in reality, everything is totally fine. With oxygen monitoring and respiratory monitoring, even hospital-grade equipment is not always reliable; it notoriously loses signal, for example, when a baby moves around. For these readings to really be accurate, a medical professional needs to be monitoring the baby.
If you’re following safe-sleep recommendations, should you constantly monitor your baby when they’re sleeping?
Collins: Some parents find they spend too much time watching a video monitor. If your baby is sleeping, it’s good to be able to use the time to rest yourself, or to do other things – there’s no benefit to watching them sleep. As long as you’re following safe sleep recommendations – there should be nothing in the crib but the baby, for example – you shouldn’t feel the need to over monitor the baby when they’re sleeping.
So, it’s healthy to trust that you can keep your baby safe with or without a monitor?
Doby: If you are creating an environment that is conducive for a positive and safe sleep, and you’re not increasing risk factors in any way, you can assure yourself that you’re doing the right thing to make sure your baby is safe. Challenge negative, unwanted thoughts with the truth, not with what-ifs.
Tell yourself things like: “I’m not doing anything in my house that can impact their ability to breathe or live long, healthy lives.” And: “I just checked on them five minutes ago and they were fine.” Being mindful of your own anxiety can help decrease it. It just takes practice.
Digital baby monitors: What’s on the market?
Note: For parents following safe-sleeping practices, an audio monitor can be perfectly adequate for monitoring your baby when you’re out of hearing range.
- Audio monitors: May include sound alerts, night light, two-way-talk intercom, sound-level indicator, sound machine
- Audio/video monitors: May include night vision, zooming and panning capabilities, sound alerts, night light, two-way-talk intercom, sound-level indicator, sound machine
- Audio/video/health monitors: May include pulse rate and oxygen tracking, sleep tracking, room-temperature tracking, phone app, health alerts, sound alerts, night light, two-way-talk intercom, night vision, zooming and panning capabilities, sound-level indicator, sound machine.
Duke Health Breaks Ground on Cary Expansion

Duke Health Breaks Ground on Cary Expansion
(Duke Health, Stephanie Lopez) — Duke Health will break ground on a new facility today that adds hospital services at its existing Duke Health Cary location, providing access to health care closer to the homes and workplaces of the community’s rapidly growing population.
The new facility will include phase one of a new inpatient hospital campus, including an emergency department, surgical services, imaging, and a small number of inpatient beds, as well as gastro-intestinal endoscopy, cancer care, and other infusion services in the same building. The building housing these services is expected to be completed in 2027.
“At Duke Health, we strive to provide hope, health, and healing by bringing high-quality care closer to where our patients live and work,” said Craig Albanese, M.D., chief executive officer of Duke University Health System. “Cary, and the broader Wake County community, is one of the fastest-growing areas in North Carolina. We want to grow together by providing greater access to the world-class care Duke Health is known for.”
The new hospital services are part of a broader plan for the 85-acre campus at Duke Health Cary. The health system has already received state approval for 40 hospital beds at the location. When fully built, the Cary hospital campus is projected to employ about 1,600 people.
“In 2022, we were excited to open Duke Health Cary with several clinics including primary care, pediatric care, and urgent care,“ said Morgan Jones, chief strategy officer for Duke University Health System. “This next phase of the campus provides a convenient option for emergency and inpatient care. We envision adding more specialized services in the future to round out the needs of the local community. As a live-work-play-care campus, Duke Health Cary will provide high quality, convenient healthcare in a vibrant, mixed-use community and drive further economic development.”
For Cary residents needing hospital services and emergency care, these new services will reduce travel time, which studies show saves lives. Providing Cary residents with convenient, accessible care is aligned with Duke University Health System’s goals for our patients, including:
- Improved adherence: Reduced travel time can enhance patients' ability to adhere to treatment schedules.
- Lower financial burden: Decreased travel expenses can alleviate the financial strain on patients and their families.
- Enhanced quality of life: Less time spent traveling allows patients more time for rest and recovery, potentially improving overall health.
Why Ramp-Up Time Is Pivotal In First Physician Job Onboarding
Why Ramp-Up Time Is Pivotal In First Physician Job Onboarding
(AMA, Tomothy M. Smith) — To a physician transitioning to practice and looking ahead to that first physician job, onboarding might seem like a formality. It is, in fact, an important first step in every doctor’s career.
An AMA STEPS Forward® toolkit details some of the best practices employers should follow to pave the way for physician success, satisfaction and well-being. Its content can help job applicants determine whether prospective employers provide adequate onboarding.
“A clear and defined clinical ramp-up schedule for a new physician or [nonphysician provider] is critical to the clinician’s well-being and success,” the toolkit says, adding that health professionals should be provided adequate time to complete their onboarding modules and sign up for insurance.
“Importantly, ramp-up schedules should differ for a physician who has been in practice many years versus a physician just out of training,” it notes.
The AMA Transitioning to Practice series has guidance and resources on deciding where to practice, negotiating an employment contract, managing work-life balance, and other essential tips about starting in practice.
What to expect out of the gate
"The ramp-up should start slowly to allow for EHR learning, at-the-elbow support and time for the new physician,” the toolkits advises, “to meet and build relationships with the patients and care team, all while navigating a new system.”
Ramp-up schedules are not one size fits all, the toolkit notes. Rather, they should be tailored to the role and the individual. A physician in practice for many years should see a different ramp-up period than a doctor fresh out of residency training.
The following is a sample ramp-up schedule, available in the toolkit, for new-to-practice physicians from an academic medical center in Illinois. It is designed for an outpatient clinic in which a physician at full capacity would see 16–20 patients in a typical eight-hour workday.
Weeks 1–4:
- Begin with scheduling one patient per hour, or four patients per half-day session.
- Provide a one-hour lunch block to allow for additional catch-up time if needed.
- Schedule daily check-ins with the practice manager. “This time should be built into the schedule template,” the toolkit notes. “Open, frequent and clear communication with the physician helps them feel supported and valued.”
Weeks 4–12:
- When the physician is ready, slowly ramp up their schedule by adding one patient per session.
- Continue weekly or bi-monthly check-ins to see how the ramp-up is going and determine if the physician needs any additional support.
- Continue to provide one-hour lunch breaks.
- “The goal is for the physician to see six to eight patients per session by the end of the first 90 days,” the toolkit says.
Weeks 13–24:
- Continue to slowly increase patients per session with the goal to reach full capacity—eight to 10 patients per session or 16–20 patients per day—by the six-month mark.
- Continue check-ins monthly or every other month.
- If desired by the physician, consider decreasing the amount of time for lunch.
If you’re seeking your first physician job post-residency, get your cheat sheet now.
Dive deeper:
- What to look for when onboarding at your first physician job
- In transition to practice, know these 8 steps for evaluating jobs
- When seeking new physician job opportunities, follow this advice
- What I wish I knew in residency about being an employed physician
Feedback makes it work
Frequent communication between the new physician and operational leaders is central to understanding both what is going well for the physician and what barriers they may be facing, the toolkit notes.
“They will work together to create a plan for increasing the number of patients being seen,” it says.
For residents transitioning to practice or those already in practice who are considering a midcareer switch, a separate AMA STEPS Forward toolkit, “What to Look for in Your First or Next Practice: Evaluate the Practice Environment to Match Your Priorities,” will help you identify available practice settings and understand how they may impact your experience, clarify your priorities, and tailor your search for a fulfilling career in a positive and supportive environment.
Learn more about optimizing onboarding in an Aug. 26 AMA STEPS Forward Innovation Academy webinar featuring Dr. Chen and Balchunas.
Register now.
Learn more about the AMA Young Physicians Section, which gives voice to and advocates on issues that affect physicians under 40 or within the first eight years of professional practice after their training as residents and fellows.
Music Therapy For Stroke Survivors: Songs Boost Mood And Improve Recovery

Music Therapy For Stroke Survivors: Songs Boost Mood And Improve Recovery
(Novant Health, Susan Miller) — When deciding how to help commemorate stroke awareness month, the team at Novant Health New Hanover Regional Medical Center had a creative idea: Let’s make a music playlist.
“The purpose of the playlist is to build some awareness on how music can affect mental health and how it's related to mental health in a positive way,” said music therapist Gabriella Carrizo. “We can use music to promote our wellness, to promote rehabilitation and to promote mood.”
Think about your favorite song. Perhaps it conjures the memory of lowering a needle onto vinyl or sliding a cassette into a boombox. Today, we can simply tap on a playlist when we need a song to lift us out of our bad mood. For stroke survivors, these mood-boosting benefits can be vital, said Morgan Lankford, a mental health counselor in New Hanover Regional Medical Center’s rehabilitation hospital. Depression and anxiety are both common in stroke survivors.
“Music is so therapeutic, but can be really healing for depression, anxiety, and can also treat pain,” Lankford said.
There’s robust evidence for proof. In 2008, researchers published work in the journal ‘Brain’ that showed listening to music for one hour every day improved memory and attention, as well as mood, during the early stages of stroke recovery. A follow-up study in 2014 further examined how and why: Listening to music stimulated structural changes in the areas of the brain responsible for verbal memory and language skills, and also focused attention.
A big bonus: Music is fun and accessible to all. The Mental Health Matters playlist reflects numerous music styles and genres with the goal to uplift the listener and perpetuate joy — everything from “Evergreen” by Barbra Streisand to “Chicken Fried” by the Zac Brown Band.
“We have come up with the idea for this playlist that anybody can contribute to —employees, patients — just to gather some songs that inspire, that motivate and uplift mood,” Carrizo said.
Follow the instructions below to listen to the playlist and add your own song. Happy listening!
How to access the playlist
- Download or open the Spotify app
- Click on the magnifying glass "Search" feature on the bottom toolbar
- Tap the camera icon in the upper right corner
- Hover over the below image
- Or, you can use the Spotify search bar to search for the playlist's name: Mental Health Matters NHNHRMC.

ECU Health Experts Raise Awareness Of Men’s Health During The Month Of June
ECU Health Experts Raise Awareness Of Men’s Health During The Month Of June
(WNCT, Gabby Sartori) — The month of June is men’s health month and ECU Health experts are digging deeper into both the physical and mental health struggle men face every day.
Signs of mental health struggles in men can be disguised as everyday behaviors. This includes work overload, self-diagnosis, and the inability to accept mental illness. Experts like Glenn Simpson, the behavioral health service line director, says there’s a stigma when it comes to mental health, and some men may feel insecure to open up about it
“Many men were taught to be tough, not complain, suck it up,” Glenn Simpson said. “And so, when we come to looking at mental health, we know that ends up being a little bit more stigmatized for a variety of different reasons”
Simpson also says that overall, there is a need to continue raising awareness about men’s mental health, so the stigma can end, and men can speak up without guilt.
“More men die by suicide than women, significantly more,” Simpson said. “And surprisingly, 10% of men do have anxiety or depressive symptoms, often not talked about. And that we know that if somebody is able to reach out and start asking for help, then that is kind of halfway to recovery.”
If you or a loved one is in need of help, the hotline to call is 9-8-8.
Watch the video below from WNCT for more details.
NC Medical Board Policy- Feedback Requested
NC Medical Board Policy- Feedback Requested
The North Carolina Medical Board has requested feedback on the Board’s latest draft of its Position Statement on Self-Treatment and Treatment of Family Members (“Self-Treatment PS”).
The Board previously circulated a proposed revision of this statement for stakeholder comment. Based on the feedback received, it became clear that the draft may have been interpreted as a blanket prohibition on all prescribing to oneself or family members, regardless of whether the medication was controlled or non-controlled. This was not the Board’s intention.
Rather, the Board sought to clarify that licensees should not prescribe non-controlled substances to themselves or family members on a continuing basis for chronic conditions. In response to stakeholder input, the Board has revised the Self-Treatment PS to more accurately reflect this intent.
The Board’s Policy Committee will review the proposed changes at its upcoming meeting in July. We invite you to share any comments you may have as part of that discussion.
If you would like your feedback to be considered, please submit it by Wednesday, June 18, 2025.
Read the draft policy and access the form to submit feedback or comments here; comments will be shared with the NCMB as the purview of NCMS membership.
Governor Stein Announces State Advisory Council to Bring Order to Cannabis Market

Governor Stein Announces State Advisory Council to Bring Order to Cannabis Market
(From the Office of Governor Stein) — Governor Josh Stein released the following statement on the need to protect young people by bringing order to the unregulated cannabis market:
“Today all across North Carolina, there are unregulated intoxicating THC products available for purchase: just walk into any vape shop. There is no legal minimum age to purchase these products! That means that kids are buying them. Without any enforceable labeling requirements, adults are using them recreationally without knowing what is in them or how much THC there is. Our state’s unregulated cannabis market is the wild west and is crying for order. Let’s get this right and create a safe, legal market for adults that protects kids.
“That is why I am announcing a State Advisory Council on Cannabis. I am charging this group with studying and recommending a comprehensive approach to regulate cannabis sales. They will study best practices and learn from other states to develop a system that protects youth, allows adult sales, ensures public safety, promotes public health, supports North Carolina agriculture, expunges past convictions of simple THC possession, and invests the revenues in resources for addiction, mental health, and drugged driving detection.
Governor Stein signed the Executive Order creating the Council on Tuesday morning. The Council will include representatives from the Office of State Budget and Management, the State Highway Patrol, the Eastern Band of Cherokee Indians, the General Assembly, and the Departments of Health and Human Services, Public Safety, Revenue, Transportation, and Justice.
Hemp and marijuana are both types of cannabis. The difference used to be how much THC was in the plant. Today, due to the cannabis industry’s unchecked and creative product development and packaging, the terms “hemp” and “marijuana” have lost their traditional meanings and are essentially the same thing. They both contain intoxicating levels of THC. As a result, anyone, no matter their age, can legally buy cannabis products in vape shops with high concentrations of intoxicating THC here in North Carolina. The status quo of zero protection of our kids is absolutely unacceptable. That’s why the work of this Advisory Council to recommend a regulatory structure for cannabis sales is important and urgent.
In the meantime, at a minimum, the General Assembly should prohibit the sales of products that contain intoxicating THC to anyone under 21 by requiring photo ID age-verification and require packaging that lets adults know what is actually in cannabis products, including the amount of THC.
Members of the Council are:
Co-chairs
• Lawrence H. Greenblatt, MD, State Health Director & Chief Medical Officer, North Carolina Department of Health and Human Services and longtime NCMS member
• Matt Scott, District Attorney, Prosecutorial District 20 (Robeson County)
Members
• David W. Alexander, Owner and President, Home Run Markets, LLC
• Arthur E. Apolinario, MD, MPH, FAAFP, 2022-2023 Past President, North Carolina Medical Society; Family Physician, Clinton Medical Clinic
• Joshua C. Batten, Assistant Director for Special Services, Alcohol Law Enforcement Division, North Carolina Department of Public Safety
• Representative John R. Bell, North Carolina House of Representatives, District 10
• Carrie L. Brown, MD, MPH, DFAPA, Chief Psychiatrist, North Carolina Department of Health and Human Services
• Mark M. Ezzell, Director, North Carolina Governor’s Highway Safety Program, North Carolina Department of Transportation
• Anca E. Grozav, Chief Deputy Director, North Carolina Office of State Budget and Management
• Representative Zack A. Hawkins, North Carolina House of Representatives, District 31
• Colonel Freddy L. Johnson, Jr., Commander, North Carolina State Highway Patrol
• Michael Lamb, Police Chief, City of Asheville Police Department
• Peter H. Ledford, Deputy Secretary for Policy, North Carolina Department of Environmental Quality
• Kimberly McDonald, MD, MPH, Chronic Disease and Injury Section Chief, Division of Public Health, North Carolina Department of Health and Human Services; NCMS member
• Patrick Oglesby, Attorney and Founder, Center for New Revenue
• Forrest G. Parker, CEO / General Manager, Qualla Enterprises LLC / Great Smoky Cannabis Company
• Senator Bill P. Rabon, North Carolina Senate, District 8
• Lillie L. Rhodes, Legislative Counsel, Administrative Office of the Courts
• Gary H. Sikes, Owner, Bountiful Harvest Farm and Partner, Legacy Fiber Technologies
• Senator Kandie D. Smith, North Carolina Senate, District 5
• Keith Stone, Sheriff, Nash County
• Joy Strickland, Senior Deputy Attorney General, Criminal Bureau of the North Carolina Department of Justice
• Deonte’ L. Thomas, Chief, Wake County Public Defender Office
• Missy P. Welch, Director of Programming (Permits/Audit/Product Sections), Alcoholic Beverage Control Commission
North Carolina Election Success at the AMA
North Carolina Election Success at the AMA
North Carolina’s legacy of leadership in the American Medical Association took a giant step forward this week. At this year’s AMA Annual Meeting, two candidates for AMA office were unanimously elected.
Dr. Mary Ann Contogiannis, plastic surgeon from Greensboro and member of the NC Delegation to the AMA, was re-elected to the AMA’s Council on Constitution and Bylaws.
Dr. Kavita Arora, ob/gyn at UNC Chapel Hill and member of the ACOG Delegation to the AMA, was elected to the AMA Council on Science and Public Health.
Congratulations to these two leaders and gratitude to them both for their leadership and work on behalf of their colleagues.


'A Slice Of Life' Exhibit Brings Hope To Medical Spaces

'A Slice Of Life' Exhibit Brings Hope To Medical Spaces
(MSN, Emma Korynta) — A new Novant Health initiative is bringing the arts into health care spaces, and shining a light on how creativity can be a part of healing.
In the cafeteria at Novant Health Presbyterian Medical Center, 28 pieces of art line the walls -- oil paintings, photography, watercolor works, and mixed media from creators ranging from professional artists to schoolchildren.
'A Slice of Life'
The "A Slice of Life: The Art of Everyday" exhibit is aimed at bringing a sense of peace and creativity to a place where many people may be looking for some hope. Kristen Howard, vice president of corporate affairs for Novant Health, said the artwork can help people take a moment and reflect.
"One of the artists shared that he was so excited to see his picture up because his mother had had a stroke and had been treated at Presbyterian Medical Center, and so now to see this piece in a place where he had sat kind of quietly and and contemplatively to now see the brightness and the color in that same space was really inspiring to him," Howard said.
When Novant first started bringing the exhibit to life, they worked with the nonprofit Charlotte is Creative to put out the call. In a matter of just a couple weeks, Howard said they got over 300 submissions.
All the work is for sale, and the proceeds go directly to the artists. On the first day of the exhibit on May 30, Howard said over 20% of the collection sold. The artwork will be up on display and available for purchase through November.
It's all a part of a new initiative Novant Health launched earlier this year: The Art of Remarkable Care. As part of the initiative and through an initial $500,000 investment, Novant is working with local artists and art organizations to implement visual and performance art, art therapy, and events to engage with the community.
'Beauty inspires healing'
Howard said this initiative has already led to more conversations about how people embrace healing, and it’s just getting started.
"I think sometimes people don't expect art to be a part of healing, but evidence shows us that beauty inspires healing," Howard said. "It can bring calm, that working on art projects and being involved in the artistic and creative process works well with our neural pathways and can create a sense of peace, reduce anxiety -- that being in community of art reduces loneliness and depression. So we think of art as a healing tool."
Novant has used art within integrative medicine clinics, Howard said, so the health system already knew art played a role in the healing process.
"It's sometimes scary to come into a hospital," Howard said. "You think treatment might be white blinding lights and plain hallways, and really we want them to know that our environments are actually made to be inviting, to be welcoming, and to be healing, and that we do that not just by ourselves but through our community, that everyone is represented and a part of our health care process and art is a way that we can express that, that passion and that commitment.”
Novant has been working with Charlotte is Creative and Novant hospital presidents across much of the Charlotte area to spotlight local creatives and health facilities. The plan is to bring the visual and performing arts into facilities, and bring the community along for the ride.
"We want to make health accessible and easy and get people excited about accessing care," Howard said.
'Not just a number on a chart'
The next event with the initiative is next Friday, June 13, at 7 p.m. The Charlotte Symphony will perform with over 30 live musicians at the Michael Jordan Family Medical Clinic on Statesville Road. The performance is free to attend and open to the public, and a Novant mobile health unit will be set up at the event to allow people the chance to get health screenings.
Howard said while Novant Health is focused on bringing healthy experiences to the community, "only a small percentage of your health is driven by what happens when you walk into our doors." With this in mind, Novant hopes to use the initiative to support artists and connect people with the healing power of creativity.
"We want to think about the whole person and to demonstrate our commitment to being an economic driver in our communities as well as interested in more than just needles and stitches," Howard said. "We have a broad way of approaching your healing and approaching your care and seeing you as a whole person, not just a number on a chart, but as an important piece of our community."
Physicians Under Pressure In Name, Image And Likeness Era

Physicians Under Pressure In Name, Image And Likeness Era
(Healio, Hunter Firment) — The ruling of the United States Supreme Court in National Collegiate Athletic Association v. Alston, 2021, paved the way for collegiate athletes to monetize their name, image and likeness.
Since then, the professionalization of amateur athletics has evolved rapidly, with name, image and likeness (NIL) policies expanding to apply to high school athletes in states where it has been legalized. However, many physicians fear the rapid, unregulated growth of NIL may put physicians and amateur athletes at risk.
“If done the right way, NIL can be very good,” Eric McCarty, MD, chief of sports medicine and shoulder surgery at the University of Colorado School of Medicine and head team physician at the University of Colorado, told Healio. “But right now, it is out of hand and continues to take turns and courses that put a lot of entities and people in an uncomfortable position.”
New considerations
When treating an athlete with NIL opportunities, Robin V. West, MD, president of the Inova MSK Service Line and team physician for the Washington Nationals, said there are new considerations for both the athlete and the physician.
“As a surgeon, the shift is that these athletes are viewing their bodies from more than just the medical or injured aspect but looking at them as business assets,” West, a Healio | Orthopedics Today Editorial Board Member, said.
Because of that shift, Brian D. Anderson, JD, partner and global head of the sports industry team at the international law firm Sheppard Mullin, said physicians need to recognize that high school or collegiate athletes with NIL opportunities should be treated like professional athletes.
“It does not change the underlying diagnosis and medical advice, but it is more about appreciating the stakes and the pressures that are involved,” Anderson told Healio.
The addition of high school athletics to the NIL landscape poses its own set of unique challenges, according to West.
“This is a different kind of liability because now they have these high school athletes who potentially could earn $8 million a year,” West told Healio. “But if they tear their ACL their senior year and you reconstruct it and they do not get back to play, then all of a sudden are you then bound to that $8 million a year that he potentially could have made?”

Anderson also said high school or collegiate athletes with NIL opportunities may have NIL representatives, agents, accountants and parents involved in their careers and wanting a say in the decision-making process. To navigate the pressures that external stakeholders may place on athletes, Anderson recommends athletes have adequate legal representation and emphasized the importance of involving family, guardians and loved ones to help look out for the best interested of the young athlete and provide crucial support.
“I would recommend having a lawyer and a trusted advisor to help navigate [NIL] issues,” Anderson said. “There are a lot of intermediaries involved that may not have [the athlete’s] best interests in mind. At the high school level, most of these athletes are not legally allowed to sign a binding contract. The parents need to be involved and sign the contract as well to make sure it is enforceable.”
Mental demands
In addition to the physical demands athletes may already experience from performing on the field, NIL has introduced an increased mental burden as well, according to Alex B. Diamond, DO, MPH, FAAP, FAMSSM, professor of orthopedic surgery, pediatrics and neurological surgery at Vanderbilt University Medical Center and team physician for Vanderbilt University.
“It is that dual threat of they are just regular people like the rest of us, and they go through the same things we do, but they also have this entirely separate world that is complex and intense and public that can affect their health and well-being,” Diamond told Healio. “NIL only acts to amplify all of those things.”
He said student athletes from disadvantaged backgrounds may even become “breadwinners” for their families in the NIL era, which can pose additional pressure to provide at such a young age.
The sense of a student athlete’s self-worth may also be tested by the pressures of NIL contracts and opportunities, according to Peter J. Millett, MD, MSc, orthopedic surgeon and partner at The Steadman Clinic in Colorado. Because athletes may associate self-worth with performance, he told Healio an athlete may begin questioning their self-worth after an injury that may prevent them from playing.
“Sometimes there is a level of grief that sets in, an imposter syndrome type situation where they start to feel like maybe they were not as good as they thought they were, or they did not reach their potential because of this injury,” Millett, a Healio | Orthopedics Today Editorial Board Member, said.
Transfer portal
Increased use of the NCAA transfer portal — a compliance tool used to manage the student-athlete transfer process — has also created challenges in the NIL landscape. According to McCarty, the transfer of student athletes can happen quickly and sometimes there is a lack of communication on where they transferred.
But just because a player may leave an institution, that does not mean they leave the physician’s care, according to Diamond.
“They are always still your patient, whether you are actively treating them or passing them along to a friend or partner or colleague,” Diamond said. “You have to do the right thing regardless of whatever emotions may be there from a school team perspective. We are part of that team, but first and foremost we are providers for that patient.”
McCarty said physicians want to be able to adequately care for student athletes transferring into their institution, as well.
“If we have an athlete coming in, we also want to take care of that athlete if they are having surgery or treatment for an injury,” McCarty said. “We want to make sure that they are taken care of when they come in and get all the records.”
However, with no national shared electronic medical record database for student athletes, physicians may not have all of the documents needed and may need to rely on the athletic trainers and administrative staff to obtain medical records from previous institutions, according to McCarty.
Private equity
As NIL contracts continue to increase in value, private equity firms may start to dip their toes in the NIL pool, which may lead to some positive outcomes, such as providing more money to the athletic program, according to Anderson, who represents teams, leagues, sponsors and investors in the sports industry. He said private equity firms can also provide “expertise in professionalizing organizations that have typically been departments within nonprofit academic institutions.”
“I am sure there are efficiency gains that a smart private equity fund would be able to find and optimize,” Anderson said. “In terms of maximizing media rights and revenue generation and bringing in expertise in commercializing the stadiums and the venues, it could be a good thing.”
However, Millett said the entrance of another external stakeholder would only further increase the risk and liability placed on physicians as there may be “significant legal ramifications for poor outcomes.”
“The medical responsibility gets heightened, and if there are increased financial incentives, you can argue if there is a bad outcome that there are bigger lost earnings. It creates a situation that can be challenging,” Millett said.
Advocacy
According to Diamond, the advanced professionalization of youth sports is a major concern, as children should participate in sports to learn the game, build fundamentals and learn about fitness and exercise.
“We are throwing those aside when we start bringing in this concept of social media likes and presence, and contracts and money,” Diamond said. “We are eroding that base of what makes sports so special at a young age.”
With the added pressures and money surrounding student athletes, Diamond said it is important that physicians advocate for their patients and provide them with an outlet for education and trust in the NIL era.
“That is where we can be effective, providing them that support and safe place,” he said. “We are an independent group that certainly care about their success on the field or court, but our only responsibility is their health and wellness. We can be a safe place for them to raise those concerns and questions with us, and we can hopefully help them navigate this new space.”
West said specialty societies can also play an important role in advocating for both physicians and athletes in the NIL landscape.
“We do not have the legal backing, but we can go and explain the surgeon's role. We can help to identify that, define it and advocate for the surgeons, which ultimately we are advocating for our patients,” West said. “We can stay involved by understanding [NIL], by educating ourselves on the latest and greatest of what is going on with NIL and then also representing our members.”
Advice
As the NIL landscape continues to develop, Diamond said the hope is it “becomes more straightforward.”
“We see [NIL] being the Wild West right now,” Diamond said. “The hope is that the larger systems and governing bodies will start working together to provide guardrails and guidance to help with this because the structure helps the families and the kids.”
Regardless of the structure NIL takes as it evolves, Diamond said it is important to recognize that it is not going away, and physicians will need to be involved with the student athlete beyond their injury.
“We have to understand that these [injuries] affect their overall health and well-being,” Diamond said. “We need to be better about recognizing and referring to where they need to be. This is a time where we have to work as a collaborative unit. It is not just the physicians and athletic trainers, but our sports psychologists, mental health professionals and academic partners. It is using that whole network as available to the students and trying to connect them to the right people sooner rather than later.”
According to Millett, it is also important for physicians to overcommunicate with the patient and their team, and to continue to lean on their medical expertise and judgement.
“Do not get caught up in all the noise of the media or the press or the pressure from the team,” Millett said. “If the patient is ready to return to play, you can clear them. If they are not ready to return to play or it is unsafe for them, you do not clear them. If they need surgery, you recommend surgery. If surgery is optional, you tell them it is optional, and then you do a shared decision-making process to help figure out what the best solution is.”
Surgeons should also remain educated on the latest developments in NIL and participate in policy formation and advocacy of both physicians and athletes, according to West.
“The most important thing is staying athlete-centered,” West said. “As this commercialization of sports continues to grow, how do we stay true to our focus and our mission?”
Although the appropriate care of student athletes should be one of the top priorities of physicians, McCarty said it is also important for physicians to protect themselves in the face of financial risk and liability.
“It is important that the physicians make sure they have the appropriate malpractice insurance for the reason that these athletes, because they now have a value attached to them when they are in this NIL, may also have people or agents or attorneys now looking at that value in case they get hurt and cannot return,” McCarty said. “Unfortunately, that is becoming more common, and we need to make sure that physicians and any providers are protected as we do the right thing for these athletes.”
NCMS Member Named Interim Dean Of Campbell School Of Medicine

NCMS Member Named Interim Dean Of Campbell School Of Medicine
(Campbell University) — Campbell University announced the appointment of Dr. David L. Tolentino as interim dean of the Jerry M. Wallace School of Osteopathic Medicine, effective July 1.
In the coming weeks, Tolentino will collaborate with current Dean and Chief Academic Officer Dr. Brian A. Kessler to ensure effective leadership transition.
Tolentino has served in academic leadership at Campbell Medicine since 2016 as associate dean for clinical affairs. During this time, he has overseen the growth of clinical education programs, developed new affiliate partnerships and contributed to advancing medical training across the region. Before his tenure at Campbell, he served as executive assistant dean for Clinical Education at the Ohio University Heritage College of Osteopathic Medicine. Earlier in his career, Tolentino practiced internal medicine in Ohio for over a decade, bringing extensive clinical insight and professional integrity to his work in academic medicine.
Dr. Michael L. Adams, vice president for academic affairs and provost, said of Tolentino, “I look forward to working with Dr. Tolentino as he guides Campbell’s medical school through this transitional phase. [And] I would like to extend my sincere appreciation to Dr. Kessler for his service and leadership as the dean.”
In his role, Tolentino will provide academic and operational leadership to the medical school. Adams said his experience, professionalism and deep understanding of the school’s mission position him to lead the school with confidence and clarity.
Reflecting on the transition, Kessler said, “I have had the privilege of knowing and working alongside Dr. Tolentino for 20-plus years. He is a thoughtful leader, a dedicated physician and a respected educator. I am confident that Campbell will continue to thrive under his leadership.”
Campbell’s medical school, launched in 2013, was the first osteopathic medical school in North Carolina and the first new medical school in the state in 40 years. In 2025, it ranked among the best in the nation for “Medical Schools With the Most Graduates Practicing in Rural Areas,” according to U.S. News & World Report rankings of top medical schools.
In his announcement, Adams stated: “The University expresses its appreciation to the faculty, staff and leadership team for their steadfast commitment to the school’s mission and for supporting this leadership transition. The heart of the Jerry M. Wallace School of Osteopathic Medicine remains its students and graduates. Their commitment to learning, compassion in service and excellence in practice embody the very mission of the institution. As they care for patients, lead in their communities, and advance the profession, they represent the enduring impact of the education and values fostered at Campbell University.
“Campbell University remains committed to preparing future leaders in medicine who are called to serve, lead, and improve health in the communities they represent.”
Using Artificial Intelligence To Improve Health
 Using Artificial Intelligence To Improve Health
Using Artificial Intelligence To Improve Health
(Harvard T.H. Chan School of Public Health, Jay Lau) — Nikhil Vytla, SM ’25, builds AI software with an emphasis on trustworthy results
Nikhil Vytla was in high school when he programmed his first mobile phone app. Along with his friend, he created an app that accessed news articles from different websites, translated them into any language, and then used text-to-speech technology to read them out loud. Vytla’s inspiration for the app was close to home.
“My grandfather loved to read the news, but over time, [he developed] age-related macular degeneration and lost his eyesight. He couldn’t read his favorite newspapers anymore,” he said. “That was my motivation to build technology that helped people in my communities—the people that I cared about.”
Since his first foray into the world of software development, Vytla has continued to pursue his passion for building technology throughout his educational and professional career. His focus on using artificial intelligence (AI) in health care grew from witnessing firsthand how technology could address real human challenges, particularly for vulnerable populations who might benefit most from more accurate and accessible medical tools. In March, he completed his master of science in health data science from the Department of Biostatistics at Harvard T.H. Chan School of Public Health.
Creating technology for social good
For his undergraduate degree, Vytla studied computer science and statistics at the University of North Carolina (UNC) at Chapel Hill. He became interested in applying his technical skills to projects for social good, particularly in the health care field. “Health care represents this incredible intersection where technical innovation can have immediate, life-changing impact,” he said. “When you’re building software that could help doctors save lives or improve patient outcomes, the work takes on a completely different meaning.” He is particularly proud of being a founding member of his college’s chapter of Computer Science + Social Good. In the organization, teams of students partnered with local nonprofits and startups to develop mobile apps and other technologies.
For example, Vytla and his teammates worked with the hospital system UNC Health to make virtual reality (VR) software for immunocompromised children, who had to stay in isolated hospital wings due to their susceptibility to disease. Using VR headsets, the children could take virtual field trips to museums, explore underwater environments, or play interactive games. “Seeing a child’s face light up as they virtually swam with dolphins while confined to a hospital bed—that’s when you realize technology isn’t just about algorithms and code,” he said. “It’s about restoring joy and possibility to people when they need it most.”
After college, Vytla took a job as a software engineer for the startup TruEra, where he developed methods to better explain how AI models work.
“AI is a black box,” he said. “How can you know what features or influences are most important to the model in terms of making a decision—like the prediction of a certain outcome, for example [whether a patient has a] disease or not?”
According to Vytla, AI explainability is also important in determining fairness in how models use protected characteristics—traits like race and gender that are legally protected from discrimination—to make decisions such as loan or credit card approvals or health diagnoses.
“My goal isn’t just to make AI smarter—it’s to make AI that works equitably for everyone. I want to bridge the gap between cutting-edge AI research and practical tools that could actually improve patient care in real clinical settings,” he said. Vytla noted that the need for trustworthy AI in health care is particularly urgent—studies have shown that some medical AI systems exhibit racial bias, such as algorithms that underestimate pain levels in Black patients, or diagnostic tools trained primarily on data from white populations, leading to less accurate diagnoses for people of color. With the aim of working on these types of issues, he set his sights on studying at Harvard Chan School.
Improving diagnoses for traumatic injuries
In the health data science program, Vytla became part of a tight-knit cohort of students. “We were able to build a close network and rely on and support each other through pretty tough classes, coursework, and complex problems,” he said. “I think that camaraderie was really important. I don’t know if I would have made it through the program without that kind of support.”
In addition to classes, he completed his capstone project at the Surgical Informatics Lab at Harvard Medical School and Beth Israel Deaconess Medical Center. The project focused on the process of diagnosing patients who come to the emergency room with traumatic injuries from, for example, car accidents or falls. Vytla worked on developing an AI model to help surgeons make more accurate diagnoses.
“Clinical decision-making in trauma care is highly subjective. There’s a lot of variability in how different surgeons treat patients, which might lead to missed injuries and delayed treatments, or potentially inconsistent outcomes,” he explained.
Vytla’s AI model used several factors as inputs for analysis. The major component was patient results from medical imaging—such as X-rays and CT scans—which were written up by clinicians in reports. According to Vytla, different clinicians rarely use the same exact terminology to describe the same observations, so the initial step of the model involved analyzing the text and converting it into standardized terms for diagnoses. Then, the model incorporated additional information including patient demographics and physical exam results. Based on all of the data, the model produced a list of potential missed diagnoses and recommendations for follow-up medical tests.
“It’s not necessarily that the tool is filling in the diagnoses, but it’s providing suggestions to the surgeon or to the resident [a surgeon in training] of things to check out and potentially test for. It’s designed to complement the surgeon’s expertise, not override it,” Vytla said.
When the model was evaluated using a test dataset, it predicted more injuries than patients had, erring on the side of safety. “In trauma care, false positives are far preferable to false negatives. An extra CT scan might be inconvenient, but a missed internal injury could be fatal. We deliberately designed the system to be cautious—better to be thorough than to miss something critical,” Vytla said. Researchers at the Surgical Informatics Lab are continuing to refine Vytla’s model for future use.
Making AI more trustworthy
Since finishing his degree, Vytla has been working as a software engineer for the company Snowflake (which acquired TruEra last year) to improve the trustworthiness of AI models—specifically, large language models such as ChatGPT and Claude. For example, he is working on methods to trace how the models reach conclusions and help them cite sources and express uncertainty—making AI responses more transparent and verifiable.
Vytla is also looking at whether an answer calculated by an AI model matches what the model actually tells the user. “Do models say what they’re really thinking—and what does it actually mean for a model to think? These are the types of questions I’m interested in answering,” he said.
Physician Practice Trends - Survey Results

Physician Practice Trends - Survey Results
The American Medical Association has published a report presenting the results of its Physician Practice Benchmark Survey. The survey, which focuses on physician practice characteristics, covers the 12-year span of 2012-2024.
The results show that medical practices are:
- increasingly owned by hospitals or other organizations, and not by physicians,
- increasing in size, and
- increasingly likely to be multispecialty
The data shows that small, independent practices are giving way to larger, multi-specialty groups. Between 2012 and 2022, the percentage of physicians who work in private practices dropped 18%, from 60.1% to 42.2%. The trend toward consolidation is accelerating.
The reasons cited for private practices selling to hospitals, private equity firms or insurers include:
- inadequate payment rates,
- costly resources, and
- burdensome regulatory and administrative requirements
Triangle Woman Raises Awareness After Suffering Eye Stroke

Triangle Woman Raises Awareness After Suffering Eye Stroke
(CBS 17, Liz Ortiz) — Imagine relaxing at home, then suddenly losing vision in one eye.
That’s what happened to one Triangle woman. Now, she wants to raise awareness about a rare type of stroke.
According to Elisabetta Vitali, the incident happened just over a year ago.
“I was watching TV with my husband and all of a sudden, I lost my eyesight from my right eye,” Vitali said. “It was really abrupt. It was just like someone put a white wall in front of me.”
Vitali says she waited about 10 minutes to see if her vision would come back. When it didn’t, she and her husband rushed over to Duke University Hospital in Durham. That’s where Vitali learned she suffered an eye stroke.
“At that point, I could see nothing,” she said. “They would come with a light in my eye, nothing.”
According to Duke Health, the hallmark signs of eye stroke are sudden and painless vision loss or changes in vision – like blurriness, floaters, a darkened area in your field of vision, decreased visual contrast, and light sensitivity – in one eye. Eye stroke is considered rare, under 1% of all strokes, but can cause permanent vision loss and devastating quality of life challenges.
“There are a couple of different ways that that can happen, sometimes a clot can go to a major artery in the eye, or sometimes there’s a drop in blood pressure,” said Dr. Nathan Tagg, associate professor of Ophthalmology and Neurology. “Just like in the brain stroke world, time is brain. In the eye stroke world, time is vision.”
Tagg and the team at Duke Eye Center quickly treated Vitali in hopes of saving her vision.
“At Duke, we have a pathway where a patient comes into the ER, they get a very expedited workup and if they’re a candidate, they get not only clot busting medication but they also get hyperbaric oxygen treatment where they initiate hyperbaric oxygen right away and this allows oxygen at higher concentrations to make it to the eye and help preserve some of those tissues that might be lacking oxygen,” Tagg said.
After treatment in the hyperbaric chamber, Vitali noticed the vision in her right eye started to come back. It wasn’t perfect, but improving.
“It was pure magic,” Vitali said. “It became lighter and lighter and transparent, so it was amazing.”
“Hers was a case that was fairly miraculous in the sense that she immediately experienced an improvement of vision when she went into the chamber,” Tagg said.
Vitali considers herself lucky with just minor vision changes today. She hopes her story can help others understand the signs.
“I’m feeling fantastic, and you know, they weren’t sure whether the sight recovery was going to be stable or temporary and knocking on wood, so far it’s been stable,” she said.
An eye stroke is a medical emergency that requires urgent attention. If you or a loved one is experiencing a sudden, painless vision change or vision loss in one eye, seek immediate care.
Click here to learn more about eye stroke.
The NCMS Continues to Advocate on the Budget Reconciliation Process and the Impact of One Big Beautiful Bill on Medicaid

The NCMS Continues to Advocate on the Budget Reconciliation Process and the Impact of One Big Beautiful Bill on Medicaid
On Wednesday, June 4, 2025, the North Carolina Medical Society joined with a national coalition of state medical societies in sending a letter to Capitol Hill expressing concerns over the proposed cuts to Medicaid funding and coverage. The debate in Washington is over H.R.1 / “One Big Beautiful Bill”, which has passed the House and is now in the Senate.
The letter adds another exclamation point to our messages to Congress that the proposed cuts in Medicaid funding and coverage would be detrimental to our state. Our recent messaging to Capitol Hill has addressed multiple areas of concern . . .
Work requirements
Eligibility determination frequency
Medicaid Provider Taxes
Per capita caps on the expansion population
Federal Medical Assistance Program (FMAP)
Block grants
This week’s letter from the NCMS and its partner state associations specifically calls attention to the Provider Tax provisions in the pending package. Provider Taxes have been a long-standing and universally accepted means of sustaining state Medicaid programs in order that they can meet Medicaid patients’ care needs.
Some specific concerns for North Carolina related to the Provider Tax issue include:
- The provision in the budget reconciliation package that effectively freezes the amount or rate of existing provider taxes does not account for a formula-based approach that exists in North Carolina, as well as in some other states.
- Lowering or freezing the provider tax cap could result in cuts to programs, services and access to care.
- The provision will erode necessary funding to facilities, including rural hospitals and nursing homes, forcing them to reduce staffing, and subsequently impact quality of care and facility viability.
As the H.R.1 deliberations continue, we will continue to advocate for what is best for the health of 3.1 million North Carolinians who depend on Medicaid.
Should You Visit The ER or Urgent Care? Raleigh Doctor Explains The Differences

Should You Visit The ER or Urgent Care? Raleigh Doctor Explains The Differences
(News & Observer, Renee Umsted) —When you’re sick, one of your priorities is getting proper medical care as quickly as possible. But sometimes, it’s not easy to tell where you should go to receive attention.
Other times, said Dr. Ryan Lamb, the medical director and chair of the emergency department at UNC Rex Hospital and Rex Holly Springs, people apologize for visiting the emergency room, or may worry that the ER is too busy for them. “I want people to come and get seen if they want to get checked,” Lamb said. Here’s a guide to medical care options and when to use them.
What’s the difference between the ER and urgent care?
The main differences between urgent care facilities and emergency rooms lie in the medical staff and capabilities of the facilities.
At urgent care clinics, patients are usually seen by a family practice provider, physician assistant or nurse practitioner, Lamb said. At the ER, board-certified professionals with training in emergency medicine oversee staff including nurse practitioners and physician assistant.
Some urgent care facilities can handle X-rays and some lab work, such as swabbing to test for COVID-19. ERs can do more and better labs, Lamb said.
When should you go to urgent care?
Visiting an urgent care facility can be helpful if a patient already has a good idea of what their health issue is.
For example, if you’ve had an ear infection in the past, and you’re experiencing similar symptoms, you might just want confirmation on your diagnosis.
“I think being able to go and have them look at your ear and confirm that and treat you is a reasonable thing,” Lamb said. “And most primary physicians cannot break open their schedule to fit in people with acute changes.”
If you’re a healthy person but are experiencing mild symptoms and just want to get checked, that’s another situation that could be handled at an urgent care clinic.
Another example: If you’ve broken a finger, and it’s an isolated issue (i.e., you didn’t fall in, say, a motorcycle crash), you could visit an orthopedic urgent care facility that can do X-rays and get treatment there.
When should you go to the ER?
“If you really need care, if you are sick, you need to come to the emergency room,” Lamb said.
People who are 70 years or older, or who have complex medical problems or take many medications and don’t feel well, should go to the ER, not urgent care — unless the health concern is clear.
There are also some symptoms that warrant a trip to the ER:
Chest or abdominal pain
Confusion, indicating something is wrong with your brain
Should you do a virtual urgent care visit?
If virtual urgent care is staffed well, and a patient doesn’t need something looked at closely (like inside an ear or mouth), then it could be a good option, Lamb said.
A good virtual assessment could treat a patient directly, or recommend an appointment with a primary care physician or a visit to the ER.
“That is what I think most people want,” Lamb said. “It’s like concierge medicine in a sense.”
When should you call 911 or take yourself to the ER?
If you can’t get to the hospital without an ambulance, or you think you need an ambulance, then use one, Lamb said.
But if you’re just using an ambulance out of convenience, it’s better to get to the ER another way.
If someone has fallen and you’re unable to pick them up, or it takes multiple people to get someone up, it might be better to call for help.
Other reasons to call for an ambulance include a person experiencing severe symptoms or a person who is confused.
“You have to get from your car into triage, and so if you can’t imagine that concept happening, then you probably need to come in via an ambulance,” Lamb said.
Which medications should you keep at home?
Medications such as Motrin (ibuprofen), Advil and Aleve are helpful for musculoskeletal pain, headaches, period cramps and post-operative pain.
People who can’t take Motrin or Advil may take Tylenol, which can also be taken by elderly people or those with kidney problems.
However, all of these medications have risk factors and should only be taken for a few days. If symptoms last longer than that or worsen, it’s a good idea to seek medical care, Lamb said.
Allergy medication, such as Benadryl and a non-sedating allergy medication like Zyrtec or Claritin, is also good to have on hand.
Supplies for addressing cuts and wounds, such as bandages and a topical antibiotic or Aquaphor, are also helpful.
Social Withdrawal in Aging Tied to Shifts in Brain Networks

Social Withdrawal in Aging Tied to Shifts in Brain Networks
(Medscape, Paulina Anderson) — There is a natural decline in sociability as a result of aging influenced by brain changes, new research shows.
“Our study suggests that age-related changes in the functional wiring of the brain may impair certain abilities needed to maintain social relationships,” the study’s lead study author Yuet Ruh Dan, Duke-National University of Singapore Medical School, told Medscape Medical News.
The findings were published online on May 28 in PLOS One.
Sociability Critical to Health
Sociability, which is the capacity to communicate effectively, be socially assertive, and to manage emotions, is “critical” for maintaining and promoting health, especially as we age, said Dan.
Research has linked sociability to increased functional connectivity in and between intrinsic brain networks. Overall, the default mode network (DMN), ventral attention network, and limbic structures have been the most strongly correlated with sociability.
The aging process also involves changes in intrinsic brain networks. Studies have shown that aging results in lower within-network connectivity, as well as greater between-network connectivity.
For example, Dan noted that connectivity between the frontoparietal and DMNs decreases with age change that has been linked to poorer self-esteem and memory. Meanwhile, connectivity between the limbic and insular regions increases with age and has been shown to activate in situations involving social exclusion, she added.
Duke-NUS Researchers Compile ‘Handbook’ To Fast-Track Breakthroughs In Scarring Research

Duke-NUS Researchers Compile ‘Handbook’ To Fast-Track Breakthroughs In Scarring Research
(Asia Research News) — In a comprehensive review published in Nature Reviews Immunology, a Duke-NUS-led team compiled a 'handbook' of key insights from over 200 studies on immune cell types, their location and their behavioural changes over time, providing an evidence-based start line to accelerate scarring research.
Imagine a massive traffic jam clogging a busy highway. Horns blare, motorcycles weave through stalled cars—but only when you zoom in do the real culprits emerge: cyclists stubbornly riding against traffic.
In the same way, pinpointing the precise culprits behind harmful biological processes—such as excessive scarring (fibrosis) in organs like the kidneys and lungs—has long remained challenging even though this affects almost a billion people worldwide. But thanks to the emergence of single-cell isolation technologies, researchers have been able to zero in on the specific immune cells causing trouble.
In a comprehensive review published in Nature Reviews Immunology, a Duke-NUS-led team compiled a 'handbook' of key insights from over 200 studies on immune cell types, their location and their behavioural changes over time, providing an evidence-based start line to accelerate scarring research. Their start line points to the changeable behaviour of a type of immune cell, called macrophage, that has emerged as a key driver of excessive scarring.
“Think of macrophages as having 'happy’ faces, promoting healthy tissue repair, or ‘angry’ faces, causing harmful scarring. Recent technological advances have made it possible to identify exactly which cells trigger fibrosis, opening new doors for targeted treatments,” said Associate Professor Jacques Behmoaras from Duke-NUS’ Cardiovascular and Metabolic Disorders Programme, the corresponding author of the review paper.
But what are these instigators of fibrosis like? How do they function and interact with the environment around them? And is there any way to prevent them from harming the body? Since the first study involving single-cell transcriptomics[1] was published in 2009, scientists have come closer than before to fully answering these questions by observing macrophages from a spatial and temporal perspective. In their summary of these findings, Assoc Prof Behmoaras and his team highlight the following crucial discoveries:
- Macrophages vary depending on their environment: Using the single-cell RNA sequencing technique, researchers have constructed atlases that map cells across the various organs in the human body. These human cell atlases have shown that macrophages express different characteristics depending on their locations—for instance, lung macrophages bear the PPARG gene while those found in the kidney bear the CD81 protein.
- Identifying the ‘troublemakers’ in the macrophage community: Originating from monocytes recruited to tissues after injuries, a subset of the macrophage population expressing SPP1, known as SPP1+ macrophages, have been identified as key drivers of harmful scarring in organs such as the heart, liver, lungs. These troublemaker cells bear unique markers such as the TREM2, CD9 and SPP1 genes, the last of which the Duke-NUS team had previously investigated in their quest to find a common ‘scar code’ across fibrotic organs.
- Critical conversations between cells: Macrophages and fibroblasts, cells that produce collagen and other components to repair damaged tissue, work closely in a balanced relationship to maintain tissue health. Using single-cell technologies, researchers have found that communication between the cells is nuanced and involves a network of different signals. In fibrosis, SPP1+ macrophages, which promote scarring, increase in number and signal fibroblasts to produce scar tissue components in excess, disrupting a once-balanced relationship.
- Targeted therapeutic strategies: Deeper understanding of macrophages’ diverse nature and how they interact with the environment around them has presented potential options for treating fibrosis. Disrupting the function of proteins expressed by macrophages, such as CCL5, SPP1 and TREM2, is one tactic that can help curb scarring. Another option being studied by researchers involves inhibiting signals in non-immune cells such as fibroblasts.
Systems geneticist and co-author Professor Enrico Petretto, Director of Duke-NUS’ Centre for Computational Biology, said of the potential of his team’s work: “As we continue making significant progress in fibrosis research, we wanted to create a clear and accessible resource – a 'handbook'—to guide translational researchers globally. Our aim is to accelerate discoveries, foster new ideas and ultimately transform treatment for millions affected by fibrosis.”
With this ‘handbook’ in hand, Duke-NUS researchers hope to turn today's scientific insights into tomorrow's life-changing therapies, bringing fresh hope to millions worldwide battling fibrosis.
NC Teen Who Lost Leg Reunites With Man Who Saved His Life

NC Teen Who Lost Leg Reunites With Man Who Saved His Life
(WRAL News)— A teenager in eastern North Carolina and the man who helped save his life are both on a path to healing.
When 18-year-old Bryson Wilkinson lost his leg after a freak accident while working, Gary Caldwell was nearby and jumped into action. Then, two days later, the two reunited at the hospital after Caldwell had his own accident.
Wilkinson works for a tree service company in Wallace.
"We go out and cut dead pine trees, any dead tree near the power line," he said.
Two weeks ago, a freak accident left him with a new reality. Wilkinson's right leg got caught in a rope during a routine tree removal.
"It was four pine trees -- full-sized pine trees that we wanted cut down," Wilkinson said. "It somehow managed to pull it under that tree. It dug me through the ground. I thought I still had my leg cause all I felt was pressure. Then I go to lift up and I realize that my leg wasn't there."
Video capturing the crucial moments after the accident shows Caldwell, who was living on the property, jumping into action and using a tourniquet to stop the bleeding.
"I thought it was over for me," Wilkinson said. "I thought that was about to be the end of my life."
Wilkinson was rushed to Novant Health New Hanover Regional Medical Center in Wilmington.
Just two days later, Caldwell, the man who saved Wilkinson's life, was fighting for his own life in the same hospital, just down the hall from Wilkinson.
"He ended up in a motorcycle accident," Wilkinson said. "I just couldn't believe what I saw."
After doctors learned that the men were connected, Wilkinson and Caldwell were reunited.
"As soon as I walked in I broke down crying. I couldn't believe it," Wilkinson said.
Wilkinson's family was also there to thank the man who saved their son's life, calling it an act of God.
"I told him, I was like, if it wasn't for you, my son, he might not have been here," said Tim Wilkinson, Bryson Wilkinson's father.
"I'm going to keep staying in touch with him as long as I can," Wilkinson said.
Now home from the hospital, Wilkinson is navigating a new path forward as an amputee. He's been posting about his experience on TikTok.
"I want to be able to tell people that their life's not over if they lose a limb" Wilkinson said. "Things happen. And they can get past it in life. They don't need to give up. They don't need to lose hope."
The teen amassed more than 3,000 followers in just five days.
This Clinic’s Individualized Support Is Helping Kids Build Fit And Healthy Futures

This Clinic’s Individualized Support Is Helping Kids Build Fit And Healthy Futures
(Novant Health, Patrick Flanary) — Stigma and weight bias persist for kids with obesity, a chronic disease that affects one in five children and adolescents in the United States.
Around the world about 160 million children live with obesity, which is caused by several genetic, environmental and socioeconomic factors – rather than solely on one’s diet.
But misconceptions often fuel bullying that can lead to even worse health outcomes for kids, including disordered eating, poor body image and isolation from physical and social activity.
“Many people still think of obesity as a personal or parental failure, and it truly is not,” said Carolanne Majeski, a family nurse practitioner who works in pediatric endocrinology and leads the Novant Health Youth Health and Wellness Clinic in Wilmington. “People want to be healthier, and it’s often very difficult for people with obesity to reach a healthy body mass index (BMI) without a lot of support.”
That support, offered at Novant Health Nunnelee Pediatric Multispecialty Care - Autumn Hall, includes services for toddlers through college age. Since 2023, the clinic has helped families in southeastern North Carolina work with trusted allies to address weight management in a safe space.
The program treats children diagnosed with Class 2 obesity (a BMI at or above 120% of the 95th percentile) who have additional medical conditions like high cholesterol, elevated liver enzymes or depression. (Your pediatrician or family medicine doctor can help with most concerns related to health issues where weight management may be an underlying factor and can make a referral.)
Majeski’s team includes registered dietician Ashley Gousios and medical assistant Morgan Dunleavy, whose treatment methods include personalized exercise and nutrition guidance, medication and counseling. Patients 13 and older are evaluated for bariatric surgery, per American Academy of Pediatrics guidelines.
Here, Majeski addresses how a healthier childhood can set kids up for a healthier adulthood.
What health risks are associated with children and adolescents with obesity?
We are seeing more children with type 2 diabetes, which used to be a disease experienced in middle age. It can affect how multiple organs function, including the eyes and kidneys. Some of the children I treat have liver disease, high cholesterol and high blood pressure.
It makes sense to treat this now so that kids can grow up to live healthy lives. If lifestyle changes aren’t producing the results they want, FDA-approved treatments and medications for children age 12 and older can help improve blood sugar, liver function and blood pressure.
How should parents broach the topic of weight with their kids, and what's the best time to start that conversation?
It’s a really tough thing for families to talk about, so we try to be as sensitive as we can to make it a good experience. Healthy growth, including weight, should be initially discussed during yearly visits with your pediatrician, who assesses whether your child is approaching an unhealthy BMI and can refer them to our program.
Because there are many causes of abnormal weight gain, the first visit allows us to conduct a comprehensive history. We assess depression, anxiety, eating disorders and genetic causes. We also do lab work to be sure there aren’t any endocrine or other medical causes for weight gain. The best approach comes from education.
How active should parents be throughout this wellness program?
We’re working to encourage families to adopt a healthier lifestyle. For all of us, there’s some room for improvement and it does not have to be perfect. You don’t have to go from zero to 60, and you don’t have to give everything up. There should not be restrictions where you’re telling your child that they can never have dessert again. When something becomes too restrictive, it typically doesn’t work, and that’s when kids may develop unhealthy reactions like hiding food, binging or feeling shame.
We might ask a preteen or teenager how difficult it would be to decrease their soda consumption, then come up with a plan for how they can replace soda with water. So it’s not so much telling them what they need to do. It’s more about having a back-and-forth conversation and reaching an agreement.
How is each child treated as an individual?
Kids are embarrassed to talk about weight, so we approach that conversation in a different way. We make a point of getting to know each person and what their goals are. We ask what they enjoy doing, what they like or dislike about school, and how they feel about their health and their bodies.
We find ways to encourage physical activity. That might mean sending a child home with resistance bands or teaching them how to jump rope if they either don’t have the means to join a gym or feel self-conscious about working out in front of others.
What does a successful outcome for a kid at the Youth Health and Wellness Clinic look like?
Small changes accumulate over time. For patients who have graduated from the program, their lab work has improved, their BMI has reached a healthy zone and they’re feeling good.
They have the tools they need and may still benefit from medication and working with a dietician, physical therapist or personal trainer. People are willing to stick with the program because they’re not on this journey alone.
5 tips to help children make healthy changes

1. Make a variety of veggies the norm.
It’s normal and healthy for kids to eat every few hours. Offer a variety of fruits and vegetables throughout the day. Get your kids involved by asking them to pick out a new veggie at the grocery store each week.
Frozen and canned fruits and vegetables are often less expensive than fresh and are still good for you. Look for low sodium or no-salt-added vegetables and fruits packed in 100% fruit juice.
Try out fun ways of eating fruits and veggies, such as cutting them into chip shapes and serving them with dip or threading them onto skewers.
Beverages are important, too. Help kids rethink their drink by replacing sugary drinks, such as soda, fruit drinks and flavored milk, with water or plain low-fat milk.
2. Move more as a family.
Physically active youth have stronger muscles and bones, better cardiovascular fitness and lower body fat than those who are inactive. Children ages 3 to 5 years should be physically active throughout the day. Children ages 6 to 17 years need at least 60 minutes of physical activity every day.
Help your children move more and meet the physical activity recommendations by making it a family affair. Walking the family pet before and after school, riding bikes and having races in the yard all count toward physical activity. Active chores, such as washing the car, vacuuming a room or raking leaves, also count.
Older kids might be motivated by exercise with purpose, such as starting a neighborhood dog-walking or lawn-mowing business.
It’s important for all kids to be physically active. You can learn more here about special considerations for children and adolescents with disabilities.
3. Set consistent sleep routines.
Good sleep helps prevent type 2 diabetes, obesity, injuries and problems with attention and behavior. Children who don't get enough sleep are at risk for weight gain. Researchers are still trying to learn how sleep is linked to weight gain. Some reasons might include that lack of sleep can cause a child to eat more or to be less physically active because of low energy.
4. Replace some screen time with play time.
Reducing screen time can free up time for activities and also remove over-snacking cues.
Turning off screens an hour before bed and removing screens from children's bedrooms can help reduce screen time and improve sleep. The American Academy of Pediatrics recommends creating a family media plan to create clear and consistent media guidelines for each family member.
5. Get rid of the “clean-plate club.”
Help kids honor their own hunger cues by encouraging them to eat until they are satisfied, not until their plate is clean. It’s healthy for kids to learn that leaving some food behind when they’re full is OK. (And if you are concerned about food waste, you can always put leftovers in the fridge for later.)
Pediatric specialty care in your neighborhood
Novant Health is committed to increasing access to pediatric specialty care in Wilmington, and welcomed several new children’s specialists to their team in 2022 to serve the coastal community. This commitment is part of Novant Health’s expanded partnership with University of North Carolina Health, and it allows parents to seek care for their children closer to home, with less travel and shorter wait times.
You'll find new and expanded children's services in Wilmington at Novant Health Nunnelee Pediatric Multispecialty Care - Autumn Hall and Novant Health Betty H. Cameron Women’s & Children’s Hospital.
New Study Suggests Calorie Restriction May Be Linked To Worsening Depression

New Study Suggests Calorie Restriction May Be Linked To Worsening Depression
(CNN, Madeline Holcombe) — Going too far with a diet might have serious impacts on your mental health.
Cutting your calories down too far could be linked with worse depression symptoms, new research suggests.
A study published Tuesday in the journal BMJ Nutrition, Prevention & Health looked at data from more than 28,000 adults from the National Health and Nutrition Examination Survey, which surveyed participants on their diet quality and depressive symptoms.
People who followed a calorie-restrictive diet, particularly men and people with a body mass index considered overweight, were more likely to have higher symptoms of depression, according to the data.
Quality of diet also mattered. People who reported a diet with more ultraprocessed foods, refined carbs, saturated fats, processed meats and sweets were more likely to report higher levels of depression and those who ate more of a Mediterranean-style diet generally had lower risk of depression, the study showed.
“The findings suggest caution with overly restrictive or unbalanced diets, particularly for people already experiencing weight-related stress or challenges,” said lead study author Dr. Venkat Bhat, psychiatrist, clinician-researcher and director of the Interventional Psychiatry Program at St. Michael’s Hospital and University of Toronto.
Instead, Bhat suggests “opting for balanced, sustainable dietary changes that meet nutritional needs and consider individual psychological impacts may help minimize potential negative effects on mood.”
A different finding from previous studies
There are some limitations to consider when looking at the results. The design of the study can only show associations, not definitively say that calorie restriction causes an increase in depression symptoms, Bhat said.
In addition, the study surveyed people on their dietary patterns, which leaves room for error, said Dr. Kary Woodruff, associate professor (lecturer) and director of the nutrition and integrated physiology department’s coordinated master’s program at the University of Utah. She was not involved in the research.
“I could think I am on a calorie-restricted diet when in fact I may be in a calorie surplus — there’s no way to verify participant’s calorie-restriction status,” Woodruff said.
The study is large and controlled for other factors that could drive the associations found, but its findings contrast with those of previous studies around the topic of calorie restriction and depression, Bhat said.

Other studies have found that calorie-restricted diets reduce depressive symptoms, said Dr. Johanna Keeler, postdoctoral researcher at King’s College London. Keeler was not involved in the study.
One difference is that previous research, including a 2023 paper that Keeler coauthored, studied restrictive diets supervised by medical professional.
“Therefore, these findings might reflect that unsupervised dieting, which can produce nutritional deficiencies, might not be good for depressive symptoms,” Keeler said.
More research and randomized control trials may be needed to fully understand how dieting impacts mental health, Bhat said.
When restriction might impact depression
There are several reasons why the calorie restriction seen in the most recent study might be associated with a negative mental health impact.
Previous studies, including Keeler’s, found that low-calorie diets that resulted in weight loss for people classified as overweight or obese was associated with reduced depression symptoms.
That could be because of physiological changes, improved physical mobility or increased positive social feedback, Keeler said.
“Embarking on a calorie restricted diet without experiencing weight loss, or experiencing ‘weight cycling’ might not produce improvements in depression, and on top of that may be frustrating or disheartening to individuals, causing an increase in depression,” Keeler said in an email.
When calories are too restricted or not enough nutrients are being provided by a diet, there could be an interruption in physical processes that could lead to fatigue, sleep problems and difficulty concentrating, Keeler added.
Extreme dieting patterns also are linked to increased anxiety and a higher risk for an eating disorder, Woodruff said.
“The key is to examine what — and how much — is being restricted. Focusing on following a healthful eating pattern that supports mild to moderate caloric restriction may improve depressive symptoms and mood, whereas extreme behaviors can exacerbate mental, emotional, and physical health,” she said via email.
Finding balance
How a person responds to a diet varies among individuals, and the results of the study highlight the need for personalized dietary recommendations and consideration of psychological factors in addition to physical health, Bhat said.
With so much contrasting advice when it comes to nutrition and what’s the best approach for your own nutrition, Keeler recommends input from a medical professional before starting any weight loss efforts.
Even if you want to lose weight, focusing too much on heavy calorie restriction might not be the most sustainable option, said Natalie Mokari, a dietitian in Charlotte, North Carolina.
Instead, she recommends small changes to move toward a more balanced lifestyle.
Start by looking at your meals, Mokari said. Does your plate have a protein, carbohydrate, healthy fat, and some fiber and nutrients through fruits and vegetables?
Try prioritizing adding in the nutrition you need first, then see whether there are elements you don’t need anymore, she said. Perhaps if you eat from all of your food groups and slow your meals down, you will realize you don’t need to grab a second helping or you won’t feel the same urgency to grab a sweet treat after, Mokari said.
“Regardless of weight loss, improving dietary quality can significantly improve overall health and quality of life,” Woodruff said. “Consider working with a registered dietitian to understand what a healthful dietary pattern can look like for you.”
'It Is A Big Need': N.C. Needs Almost 1,000 Doctors For Geriatric Patients

'It Is A Big Need': N.C. Needs Almost 1,000 Doctors For Geriatric Patients
(Spectrum News 1, Syndey McCoy) — From its coast to its mountains, North Carolina has much to offer, including a spot for retirees to settle down. With the Tar Heel State consistently ranking in the top states to retire, special care will be needed to accommodate this age group like geriatricians, but a national shortage in this field may not keep up with the demand.
Everyone has a reason to pursue a future career, including Tamara Damjanac, a fellow in the UNC Geriatric Medicine Fellowship Program.
“I knew the things that were important to me, were focusing on people’s quality of life. And things that were important to patients. I really liked how I got to spend a lot of time with patients and got to really get to know them and all the medications that they were taking and whether or not they really needed those medications,” Damjanac said.
Damjanac, in her early twenties when her mother was diagnosed with cancer, said she’s always felt a calling to medicine. She said she thought of many different fields but landed on geriatrics.
Geriatricians specialize in older adults’ care, as noted on Mount Sinai Hospital’s site.
“The thing that drew me to geriatrics is that I could really be like a full PCP, like a medicine doctor, and also talk about all of these things like end-of-life care and staying comfortable and thinking about quality of life,” Damjanac said.
Her favorite part — hearing her patients’ stories.
Now, she is in her first and only year of the UNC Geriatric Medicine Fellowship Program after completing internal medicine.
After the fellowship, Damjanac said she will become an assistant professor in geriatrics, with goals of being a primary care doctor for geriatric patients.
She is just one of four fellows in this year's UNC Geriatric Medicine Fellowship Program.
Emily Cetrone, a clinical assistant professor and associate program director for the program, said the fellowship has two goals — to teach their fellows how to provide excellent care for patients and to inspire the next generation of geriatricians.
“Our goal is for our fellows to kind of go out into the world then and be excellent geriatricians, and then also sort of create these systems where older adults can thrive,” Cetrone said.
The American Geriatrics Society said, as of 2016, North Carolina had 227 certified geriatricians and is expected to need 931 by 2030.
“The truth is that we won’t have enough geriatricians just based on the kind of that growing population of… North Carolina,” Cetrone said. “It is a big need just across the entire country.”
The N.C. Office of State Budget Management predicts the state’s older adult population, age 65 and up, will double to about 2.7 million in 2040, compared with the 1.8 million it reported in 2023.
This year, all the spots in UNC’s fellowship program are full, with fellows learning and experiencing crucial hands-on learning to better their care.
From working as primary care doctors for geriatric patients, spending time at local nursing homes, UNC’s PACE program for the most vulnerable adults and more, these fellows learn everything to take care of geriatric patients.
“They also get to spend a lot of time learning about quality improvement, working with a lot of inter-professional colleagues such as social work, pharmacy, wound care, nursing,” Cetrone said.
Cetrone said this group of fellows will graduate in June. Other schools in our state have geriatric programs as well, a commodity to North Carolina.
“The number of overall spots in geriatrics fellowship is remaining about the same, but it’s becoming a little bit more spread out, which is nice in terms of geography, but it is still something where many places do not have access to a geriatrician,” Cetrone said.
Nationally, fewer than half of the spots for fellows in geriatric medicine were filled in 2025, according to the National Resident Matching Program.
“Sometimes recruitment into geriatrics can be a little bit of a challenge,” Cetrone said. “Some things that we’re trying to do are really reaching students as early as possible.”
Cetrone says one of the biggest challenges of geriatrics is the complexity of care and medical conditions both past and present, such as frailty, dementia, heart failure and diabetes.
“They need someone who understands how medications affect them very differently as they get older,“ Cetrone said.
Every geriatrician needs to be highly skilled in patient care, understanding individual needs through personal accounts and struggles.
“Another challenge is just the realities of some of our health care system in terms of finding, you know, that as patients get need more and more help and they need more caregivers in the funding for that is not often available,” Cetrone said. “It’s not covered by, you know, Medicare, that home care that they really need. And so trying to find those resources for patients is probably the biggest challenges that I see.”
The UNC Geriatric Medicine Fellowship Program said it has graduated an estimated over 70 fellows since 1988 and two fellows are registered for next year.
“By sharing those stories and sharing the need and sharing the joy, I think we can really capture more students in that way,” Cetrone said.
Read These 7 Stories About Copperhead Snakes In North Carolina

Read These 7 Stories About Copperhead Snakes In North Carolina
(The News & Observer) — North Carolina's copperhead snakes are active much of the year, with experts advising residents to watch for their distinctive hourglass markings and yellow-tipped tails on juveniles. Bites often happen when people reach into dense ground cover or walk barefoot, so wearing boots and gloves is a smart precaution, especially in yards or on trails.
Snake repellents and home remedies like mothballs do not deter these snakes — instead, keeping yards tidy and avoiding piles of wood or brush reduces risk.
In the event of a bite, hospital visits can be costly and painful, but not all bites require antivenom, as shown in recent stories of bite victims with a range of medical treatments.




Shaping The Future Of Medicine Through Education

Shaping The Future Of Medicine Through Education
(AMA, Diana Mirel) — With a nationwide physician shortage looming, recruiting and training the next generation of doctors is critical to shaping the future of medicine. Few understand the challenges—and opportunities—today’s health care workforce environment poses better than Lindsay Mazotti, MD, Sutter Health’s first chief medical officer of medical education and science.
Sutter Health is a member of the AMA Health System Program, which provides enterprise solutions to equip leadership, physicians and care teams with resources to help drive the future of medicine.
Dr. Mazotti has spent her career focused on shaping the future of medicine by thinking outside the box in the present. With a deep passion for the science and strategy of training physicians, she is dedicated to expanding and diversifying medical education, and developing innovative training programs that align with the evolving nature of health care.
Her impressive track record in the field also includes vital work at her previous role as a founding faculty member of Kaiser Permanente’s Bernard J. Tyson School of Medicine, where she was instrumental in developing the medical school’s curriculum.
For Dr. Mazotti, training future doctors is not only crucial to addressing ever-mounting physician workforce challenges, but it’s also deeply personal when it comes to providing excellent patient care.
Graduate medical education (GME) “is an incredible place to spend time because it’s very future focused. It's about looking ahead 15 to 30 years, thinking about the people we want caring for us, our families and our friends,” she said. “Then, we work now to make sure they will be the best possible doctors they can be.”
More than 290 residents and fellows now train across Sutter Health’s 30 accredited GME programs.
At Sutter Health, Dr. Mazotti is leading the system in its bold strategy to attract and retain top clinical talent by growing GME, a plan that began in 2022. By 2030, Sutter will have trained 1,000 residents and fellows across its integrated, community-based divisions.
Reuters recently recognized Dr. Mazotti’s dedication, innovation and success in expanding medical education by naming her a “Trailblazing Woman in Health Care.” The honor recognizes women who excel professionally, influence the industry, make a social impact for people, communities and industries, and demonstrate strong leadership.
In an interview with the AMA, Dr. Mazotti shared why it is so important for health systems today to commit to building and supporting the physician workforce of tomorrow.
AMA: What does it mean to you to be named a trailblazing woman in health care?
Dr. Mazotti:It’s a really big honor—and it’s a very big responsibility. It affirms the work that we've been doing in medical education, strengthening the physician workforce and advancing health care for all.
It also reinforces my commitment to paving the way for the next generation of learners. We know there are significant workforce shortages looming. For a long time, I’ve felt that this work is critical, and this makes me feel like it's being [more widely] recognized that this work is important.
AMA: How has your work in GME influenced the way you mentor and support the next generation of physicians?
Dr. Mazotti: The physician workforce now is more than 50% women. Our trainees are more than 50% women.
Our work in GME has helped me recognize how intentional we must be about mentorship. We need to build supportive networks, advocate for structural changes that foster inclusivity, and develop programs to help bring students from rural and underserved communities into the practice of medicine.
AMA: Is there a moment at Sutter Health where you felt your leadership made a tangible difference?
Dr. Mazotti: Before I came into this role, there wasn't really a physician leader bringing the pieces of medical education together across the Sutter Health network. This is a very large organization with 28 hospitals that take care of 3.5 million people in Northern California.
We needed to bring physicians closer to the “why” around graduate medical education. We also needed to make sure that the physicians who are coming in to do the teaching and the mentorship of our new residents and fellows are prepared and engaged.
Last year, we brought all the faculty leaders and educators who run these residency programs together, [creating] a community of educators. We helped them feel really connected to the intentional work that we're doing, and it was incredible. Creating a community around education where one didn't exist before has been a profound experience.
AMA: What are you looking forward to next?
Dr. Mazotti: I have the best job that I get to do every day! I can look forward to tomorrow and find something exciting. And I can look forward a decade from now and find something exciting.
The growth of our programs year over year is so rapid that sometimes it doesn't sink in until we have our new intern orientation, which happens every summer. When I see the faces of the new group and feel the growth in the number of people present, what we’re doing feels larger.
I love meeting and interacting with our new interns and fellows—the physicians who will be training with us and who will hopefully be our future colleagues. Our learners at Sutter are instrumental to our organization, and we are a top place to practice medicine, conduct research, learn and receive care. I look forward to seeing and feeling the growth and getting to know the residents and fellows. It’s also exciting to see medical education as a bridge to improving patient care and access.
AMA: Do you have any advice for other leaders in this space?
Dr. Mazotti: It can be really easy in today's environment to feel restricted around the opportunity for growth. There are a lot of challenges in pursuing research and education.
But when you think about the future of health care and the needs of our patients, it becomes clear how critical medical education is to address the physician shortage and increasing access to care. So, it is important for medical education leaders to speak broadly about why medical education is important—and how it links back to patient and community health and the mission of our organizations.
AMA: Do you have any advice for residents, fellows and others who are pursuing a career in medicine?
Dr. Mazotti: The practice and the profession of medicine is an incredible privilege. Remember that your career is a journey, not a fixed path. Stay open to growth, seek out mentors and community, and don’t be afraid to lead—because the field of medicine needs your voice, your ideas and your passion now more than ever.
The AMA GME Competency Education Program delivers education to help institutions effectively meet ACGME common program requirements. The program provides an award-winning virtual experience, with quality education designed for residents on the go. It’s easy to use, saves time and cuts administrative burdens with simple reporting tools. Learn more.
First-Ever Four-Year Medical School Opening In Charlotte

First-Ever Four-Year Medical School Opening In Charlotte
(Queen City News, Bailey Striepling) — Charlotte leaders are welcoming the area’s first-ever four-year medical school.
The Pearl is located on McDowell Street in Midtown.
The Charlotte campus of Wake Forest University School of Medicine was created through a partnership led by Atrium Health and Wexford Science and Technology.
Local officials say it’ll usher in a new era for the Queen City and beyond.
This school will also be home to the exclusive North American headquarters of IRCAD, a world-renowned surgical training network.
The facility will welcome its first students in August.
AI’s Role In Health, Unanswered Ethical Questions Take Center Stage At Triangle AI Summit

AI’s Role In Health, Unanswered Ethical Questions Take Center Stage At Triangle AI Summit
(The Chronicle, Max Tendler) — Hundreds poured into the Washington Duke Inn Friday for the Triangle Artificial Intelligence Summit; Duke’s second annual forum focused on engagement with AI technology in the region.
Hosted by Provost Alec Gallimore, the symposium took place a week after he announced a new initiative that aims to increase conversation about the technology and make the University a leader in the field.
“We're not just reacting to the evolving field of artificial intelligence,” Gallimore said in an introductory speech. “We are actively shaping its future.”
The summit — organized by Duke Learning Innovation and Lifetime Education, Duke Libraries, Duke Community Affairs and the School of Nursing — was formatted with four “pillars” in mind drawn from the initiative: trustworthy and responsible AI, advancing discovery with AI, life with AI and sustainability in AI.
Attendees began with an overview from New York Times reporter Cade Metz on the history and functions of AI, then heard from leaders in the AI space in a series of panels framed around the four pillars. The event also featured a showcase of AI projects from across the Triangle and the perspectives of undergraduate participants in Duke’s Code+ summer program.
New AI initiatives at Duke
Tracy Futhey, vice president of information technology and chief information officer, discussed a number of the University’s plans to invest in AI in support of its educational mission — including constructing a data center with an energy output large enough to power “the entire town of Carrboro.”
She said her office is working with Facilities and Management to outline the feasibility of the project, focusing on “how we build a next-generation data center that will be energy efficient [and] … sustainable for the environment.” She noted that Duke is investigating liquid cooling technology as a cost-effective approach to reduce the facility’s climate impact, as data centers are known for their high energy consumption.
The new center is projected to be online in 18 to 24 months.
Futhey listed several AI programs that will be available to community members in the upcoming academic year, including ChatGPT-4o and a new software called DukeGPT.
She also promoted AI training partnerships between Duke and other universities in the state, noting that “there is more that needs to be done than any one institution can do.”
“Our goal here is to have North Carolina be the number one place for AI research and education,” Futhey said.
AI’s uncertain role in health
Moderator Nicoleta Economou-Zavlanos, assistant professor of biostatistics and bioinformatics and director of Duke Health AI evaluation and governance, began her panel with a seemingly simple question: “What does trustworthy and responsible AI mean to you?”
“I'll just be honest with you all; I have no clue,” said Jun Yang, Bishop-MacDermott family professor of computer science. “And I don’t think I’m alone.”
He was not. As the panel turned to the use of AI in health systems, Robert Califf, former commissioner of food and drugs, Trinity '73 and School of Medicine '78, expressed concerns about the inability of AI tested in one health care setting to be deployed in another, a problem which he said comes down to barriers to sufficiently validating AI tools.
“I don't know of a single health system in the country that can actually do what needs to be done to validate AI,” he said.
Califf also said that hospitals often integrate AI for financial reasons, making “patient well-being … a minor part of the equation.”
He pointed to the Department of Health and Human Services’ recent Make America Healthy Again report, which has been accused of being produced with falsity-spouting AI, as an example of a failing national approach to integrating AI into health systems responsibly.
Steve Kearney, medical director at the Cary-based international tech company SAS Institute, said AI’s development has to “move at the speed of trust” but maintained that responsibility for deciding how software products should be integrated into health care lies with practitioners.
“We develop software,” he said. “We are not the experts in how you should apply it to patient care. That should be all of you.”
Yang emphasized that despite the concerns, AI should be embraced.
“The world is using it,” he said. “We have to figure out ways to deal with it.”
Unanswered ethical questions
The “Life with AI” panel continued the discussion of ethical queries that arise with the growing role of AI in society, though speakers settled on few answers.
“There’s going to be bad, and there’s going to be good, and life with AI is going to be figuring out what the balance is,” said Chris Bail, professor of sociology and director of Duke’s Society-Centered AI Initiative.
According to Bail, much of the bad entails how the technology can be used to instill echo chambers and worsen polarization on social media.
Brinnae Bent, executive in residence in the engineering graduate and professional programs, noted the effects on marginalized communities in particular. She referenced teenage girls being “targeted” by waves of deepfake pornography — AI-generated explicit images that seem realistic but have been digitally altered — and AI facial-detection software being used in police stations across the country, despite studies showing these tools to exhibit racial bias.
Moderator Yakut Gazi, vice provost for learning innovation and digital education, pointed out that the developing technology is projected to threaten millions of jobs. She asked the panelists if Americans should “stop pretending that everyone can be re-skilled” and instead “start planning for a society where not everyone needs to … work.”
But Jenny Maxwell, head of Grammarly for Education, rejected the notion that mass layoffs are inevitable. She pointed to financial tech company Klarna’s regret and subsequent wave of rehires after AI failed to adequately replace hundreds of human customer service workers, leading to a roughly $40 billion devaluation of the company.
Later on, Andrew Pace, executive director of the Association of Research Libraries, said AI likely wouldn’t replace jobs directly. Rather, he claimed that “you're going to be replaced by somebody who understands AI” — seeming to identify development and maintenance of the technology as a space for growth.
Panelists also discussed the ramifications of the popularization of generative AI use among students and concerns that certain skills will atrophy as a result. No comprehensive national regulations currently exist for AI’s use or development in educational or professional spaces.
Speakers across the summit’s events underscored the growing gray area within AI development. But many expressed confidence that engaging with that uncertainty in the hopes of answering “hard questions” constitutes a strong path forward.
As Califf put it: “Isn’t that what universities are for?”
Western Carolina Medical Society to End Emergency Relief, But Plans Expanded Client Support

Western Carolina Medical Society to End Emergency Relief, But Plans Expanded Client Support
Asheville, NC – When Hurricane Helene left its mark on Western North Carolina more than eight months ago, countless agencies sprang into action, including the Western Carolina Medical Society (WCMS). With emergency dollars from funders such as the Community Foundation of Western North Carolina, North Carolina Medical Society Association, WNC Bridge Foundation, and the North Carolina Society of Gastroenterology, as well as private donors, the 140-year-old agency met a variety of needs, from purchasing durable medical equipment and prescription replacement to paying overdue light bills and rent. With those funds now distributed to individuals in the agency’s Project Access program and other community members, that phase of recovery ended May 31, 2025.
To date, WCMS has delivered the following support:
• Rent Support: $25,684
• Groceries: $20,559
• Utilities: $7,462
• Medical: $6,723
• Transportation: $1,198 in direct payments
• Gas cards to Four Area Federally Qualified Health Centers: $10,000
WCMS Executive Director, Karen Wallace-Meigs, who had been on the job less than four months when the storm hit, commented that “Out of so much pain came a glimmer of good. WCMS assisted our community by identifying new funding and community partners. In some cases, agencies pooled donations to support neighbors in need.”
The WCMS staff of ten tirelessly worked emergency relief efforts with no additional staff or volunteers to process paperwork, all while managing their signature programs: Project Access, WIN – the largest interpreter network in WNC, and Healthy Healer, a social/emotional support program for member physicians and physician assistants. “We are incredibly grateful to all of our donors,” Wallace-Meigs shares. “WNC Bridge Foundation supported our Healthy Healer program, allowing our agency to offer free therapy and coaching services to providers in the months since the storm. A healthy community is only possible if we have healthy care providers.”
WCMS hopes to create an emergency fund to provide ongoing, as-needed support to Project Access program enrollees. Project Access coordinates free specialty care for lowincome, uninsured residents of Buncombe and Madison counties who are ineligible for Medicaid.
“Going forward, we want to help our most vulnerable neighbors when times are tough for them as individuals. No one can genuinely be healthy if they cannot put food on the table or keep a roof over their heads. Our emergency relief work is entering a new phase, a longterm phase based on our patient-client’s needs in the moment. We want to help them overcome their personal storms.”
To learn more about the many health equity programs of Western Carolina Medical Society or to partner with the agency, contact Niki Duff, Director of Development & Communications, at [email protected] or visit www.mywcms.org.
Healthy Food Choices Found To Be Key In Reducing Heart Disease Risk

Healthy Food Choices Found To Be Key In Reducing Heart Disease Risk
(American Society For Nutrition) — A new study that followed almost 200,000 people for several decades has found that when it comes to heart health, the quality of food consumed matters as much as following a low-carbohydrate or low-fat diet. The results suggest that choosing healthy, high-quality foods is key to protecting the heart.
In the past two decades, low-carbohydrate and low-fat diets have been promoted for their potential health benefits, such as weight management and improved blood sugar and cholesterol levels. However, the impact of these diets on reducing heart disease risk has remained an ongoing debate.
"We found that what you eat on low-carb or low-fat diets matters just as much as the diet itself. Healthy versions of these diets-those rich in plant-based foods and whole grains-were linked to better heart health outcomes and improved metabolic function. In contrast, low-carb and low-fat diets emphasizing unhealthy foods were associated with a higher risk of heart disease."
Zhiyuan Wu, PhD, postdoctoral fellow in the lab of Qi Sun, MD, ScD, at Harvard T.H. Chan School of Public Health
Wu will present the findings at NUTRITION 2025, the flagship annual meeting of the American Society for Nutrition held May 31–June 3 in Orlando.
The study included 43,430 men in the Health Professionals Follow-Up Study (1986-2016), 64,164 women in the Nurses' Health Study (1986-2018) and 92,189 women in the Nurses' Health Study II (1991-2019). The researchers followed the nearly 200,000 study participants for several decades, tracking their dietary habits and whether they developed heart disease.
Based on information from detailed questionnaires completed by the study participants, the researchers assigned scores indicating how healthy or unhealthy their food choices were within low-carbohydrate and low-fat diets.
The researchers classified carbohydrates, fats and proteins from foods such as whole grains, fruits, vegetables, nuts and legumes as high-quality nutrients, or healthy, while carbohydrates from potatoes and refined grains as well as saturated fats and proteins from animal-based foods were categorized as low-quality, or unhealthy.
For more than 10,000 of the study participants, the researchers also measured hundreds of blood metabolites to assess how diet quality influenced their metabolic regulation. "This approach allowed us to better understand the biological effects of these diets and strengthened our findings," said Wu.
The analysis showed that study participants who followed a healthy low-carbohydrate or low-fat diet had a lower risk of developing coronary heart disease, while those on unhealthy versions saw an increased risk. These healthy diet patterns, whether low-carbohydrate or low-fat diet, lowered the risk of developing heart disease by about 15%.
"Our findings suggest that improving food quality is crucial for improving heart health," said Wu. "Regardless of whether someone follows a low-carbohydrate or low-fat diet, emphasizing whole, minimally processed and plant-based foods and limiting refined grain, sugar and animal foods, can significantly reduce the risk of coronary heart disease."
For those looking to improve their diet, the researchers suggest focusing on adding more whole grains, fruits, vegetables, nuts and legumes while cutting back on processed meats, refined carbs and sugary foods. They note that it is also important to check food labels and be mindful of added low-quality ingredients, such as added sugars in juices and processed snacks.
Moving forward, the researchers aim to explore additional factors that may influence the relationship between diet quality and heart health. For example, they want to look at how genetic factors, lifestyle choices and other metabolic markers may further shape these associations. They are also interested in how low-carbohydrate or low-fat diets may impact other health outcomes, such as type 2 diabetes and cancer. This knowledge could help tailor dietary recommendations for individuals based on their unique health profiles.
From Data to Decisions: A Model for Returning Individual Results to Research Participants

From Data to Decisions: A Model for Returning Individual Results to Research Participants
(Duke University School of Medicine) — Returning individual research results to clinical study participants has not historically been the norm, even for participants with abnormal findings. The paradigm, though, is shifting, with return of results becoming not only a scientific responsibility but also an ethical imperative. However, best practices haven’t been established yet.
A team of Duke researchers led by Svati H. Shah, MD, MS, Ursula Geller Distinguished Professor of Research in Cardiovascular Diseases, and Neha Pagidipati, MD, MPH, associate professor of medicine, have developed a model using the Project Baseline Health Study (PBHS) for how to effectively communicate results to patients and help empower them towards their health and medical choices. The study also detailed the large number of abnormal results that were returned to participants, highlighting the need to consider these processes early in study design. Results were published in the American Journal of Medicine Open.

As scientific research shifts to emphasize transparency, participant empowerment, and the democratization of data, this model demonstrates the feasibility and value of a comprehensive, systematic approach to returning clinically significant findings in a research context.
Project Baseline launched in 2017 to create a comprehensive reference point, or “baseline,” of good health and to build a robust data platform for studying how health transitions to disease. Over 2,500 participants across three sites, including Duke and Stanford, enrolled and completed assessments conducted by the study team that included a wide range of health data, like clinical, genetic, behavioral, and environmental information, through baseline eye, heart and lung imaging and annual visits, wearable devices, surveys, and biospecimen collection.
Among the 2,002 participants analyzed, nearly 40% would receive at least one result that required immediate or urgent attention. In some cases, individuals received as many as eight separate findings, again highlighting the need to return results to study participants to help them manage and be in control of their health choices. The participants had abnormal results returned to them for a variety of conditions, including vital signs, clinical laboratory testing, chest CT scans and X-rays, electrocardiograms, echocardiograms, and ophthalmologic assessments.
To accomplish this task, a Return of Results (RoR) Committee was established early in the study to oversee the return of findings. They developed a systematic, ethical, and clinically informed process for returning individual-level urgent and emergent results to participants and detailed determination for what types of results should be returned and within what time period.
Some results were more pertinent to get to participants faster than others, given potential clinical implications of the abnormal findings, so the team developed a color-coded flag system to prioritize and categorize results:
- Red flag: Emergent, requiring immediate clinical attention
- Orange flag: Urgent, but less time-sensitive
- Yellow flag: Actionable or uncertain results
- Green flag: Within expected clinical range
Participants had their results returned to them by site principal investigators — practicing physicians — or their designees.
However, with that many results to return, there is also a strong need for a streamlined process to alleviate the burden placed on health care professionals. So, the Project Baseline team also developed a predictive model using widely available clinical and demographic variables, like age, sex, body mass index, blood pressure, smoking status, and history of chronic conditions, which helped identify which participants were most likely to have actionable results.
As the research community continues to evolve its approach to participant engagement, the Project Baseline study offers a robust framework for returning results ethically and effectively. It also raises important questions for future studies, such as how to define "urgent" findings and how to balance return policies with participant preferences, and the need to consider design and funding for return of results prior to study initiation.
Duke Researchers Find New E-Cigarette Products Contain Highly Potent Sweeteners

Duke Researchers Find New E-Cigarette Products Contain Highly Potent Sweeteners
(Duke Health, Sarah Avery) — A majority of popular disposable e-cigarettes tested by Duke researchers contain a potent, unregulated artificial sweetener that may enhance the appeal to young and first-time users.
The additive neotame is up to 13,000 times sweeter than table sugar and is often used in e-cigarettes that also feature fruity, candy and cool mint flavors. Clinical studies have found that candy flavors and sweeteners increase the appeal, preference, and abuse potential of e-cigarettes and other tobacco products.
“The addition of a potent sweetener may increase the potential for addiction by facilitating initiation and chronic use,” said Eric-Sven Jordt, Ph.D., associate professor in the departments of Anesthesiology and Pharmacology and Cancer Biology at Duke and senior author of a study appearing June 2 in JAMA.
“The presence of neotame also raises toxicity concerns,” Jordt said. “While approved by the U.S. Food and Drug Administration for use in food, it is not known whether it is safe to inhale neotame heated and vaporized by an e-cigarette.”
Jordt and colleagues -- including co-lead authors Hanno C. Erythropel, Ph.D., an analytical chemist at Yale School of Medicine and Sairam V. Jabba, Ph.D., senior research scientist in Duke’s Department of Anesthesiology – analyzed 55 disposable e-cigarettes marketed in 2024, including the popular brands Elfbar, Geekbar, Mr. Fog and Breeze, and products that contained no nicotine or a nicotine-mimicking substance called 6-methylnicotine.
Of the 55 disposable e-cigarettes tested all contained neotame, with an average neotame content that was nearly five times higher than in a mentos mint candy. Disposable e-cigarettes containing the nicotine analog 6-methylnicotine had even higher neotame content.
“Our study demonstrates that the artificial sweetener neotame is a ubiquitous ingredient in popular disposable e-cigarettes sold in the United States,” Jabba said. “Interestingly, less popular FDA-authorized ENDS products such as Vuse or those awaiting an authorization decision that were introduced before 2021 such as Juul do not contain this additive. The addition of neotame to disposable cigarettes may give these products a competitive edge. Youth and young adults strongly favor sweetened products, especially in combination with candy flavors.”
As of now, neither federal nor state regulations address the increasing presence of artificial sweeteners in tobacco products.
“FDA and state regulators need to rein in the spread of heavily sweetened, disposable e-cigarettes that have not been authorized for marketing by the FDA, but are nevertheless available in local stores and from online vendors,” Jordt said. “Otherwise, gains made in the reduction of e-cigarette use by youth may be reversed.”
In addition to Jabba, Jordt and Erythropel, study authors include Remi A. Mellinghoff, Victor Garcia-Gallet, Peter Silinski, and Julie B. Zimmerman.
Funding for the study was provided by the Yale Tobacco Center of Regulatory Science, the National Institute on Drug Abuse, part of the National Institutes of Health (U54DA036151, R01DA060884), and the Center for Tobacco Products of the FDA. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH or the FDA.
Is Your Healthcare Organization ALL IN For Clinician Wellbeing?
Is Your Healthcare Organization ALL IN For Clinician Wellbeing?
The North Carolina Clinician and Physician Retention and Well-Being Consortium (NCCPRW) in partnership with the Dr. Lorna Breen Heroes’ Foundation launched the ALL IN: Caring for North Carolina’s Caregivers initiative. This initiative encourages hospitals and health systems across the state to redesign workplace environments to better support their staff’s wellbeing and mental health. Together, we have positively benefited 26,500+ physicians and other credentialed health workers working across 55 North Carolina hospitals by removing intrusive mental health questions and stigmatizing language from credentialing applications and peer reference forms.
We have now launched Phase 2: Learning the Wellbeing Systems Approach. Over 150 healthcare leaders representing 25 organizations are gaining the knowledge necessary to accelerate quality improvement projects that address the top driver of burnout – administrative burden. This Fall, we’ll begin implementing and evaluating projects to improve health workers’ experience and wellbeing while improving patient experience, improving population health, and reducing costs.
Is your healthcare organization a part of the ALL IN: Caring for NC’s Caregivers initiative? Contact Monecia Thomas, Executive Director-NCCPRW, to learn more and to participate in this opportunity to enhance the well-being of your colleagues.