NC Medical Society to Honor 2025 Academy for Executive Healthcare Leaders Graduates
NC Medical Society to Honor 2025 Academy for Executive Healthcare Leaders Graduates
The North Carolina Medical Society (NCMS) invites you to celebrate the accomplishments of the 2025 NCMS Academy for Executive Healthcare Leaders graduating class.
The NCMS Academy for Executive Healthcare Leaders is a rigorous, 9-month leadership development program designed to cultivate high-potential healthcare professionals for senior-level responsibilities.
This program integrates a deep dive into individual leadership capabilities—leveraging a comprehensive 360° assessment and personalized executive coaching—with a hands-on, strategic change initiative project.
The upcoming graduation and project presentations will highlight the culmination of this rigorous program. Graduates will present their key learnings and demonstrate how they will apply these insights to their professional roles. They will also present their capstone projects, which are initiatives of their choosing with direct applicability to their workplaces, local medical societies, and the NCMS.
Event Details
The presentations will take place in person on September 27th at NCMS Headquarters 222 N. Person Street Raleigh, NC 27601 from 9:30 a.m. to noon, followed by a luncheon, a graduation speaker, and a formal ceremony concluding at 3:30 p.m. See the presentation schedule below to include topics and presenters.
Register here: https://ncmedsoc.wufoo.com/forms/z1p9eeb30ocigdb/
Presentation Schedule
| 9:30 am – 9:40 am | Provider Data Integrity (PDI)
Troy D Schilling |
| 9:45 am – 9:55 am | Weekend Labs
Ronnie Laney Jr., MD |
| 10:00 am – 10:10 am | The CCM Imperative: Data-Driven Healthcare Leadership
Michol Stanzione, DO |
| 10:15 am – 10:25 am | A Safe Landing
Claire Paris, MD, MBA, FHM |
| 10:30 am – 10:45 am | Break |
| 10:45 am – 10:55 am | Building and Sustaining Membership in the Mecklenburg County Medical Society
Chirag Patel, MD |
| 11:00 am – 11:10 am | A New Hope
Timothy J. McGrath, MD, MBA |
| 11:15 am – 11:25 am | Disaster Response and Recovery
Janelle White, MD |
| 11:30 am – 11:40 am | QI Charter Improving Communication Among Dialysis Access Specific Specialties
Jennifer Stoddard, MD |
NC Medical Society to Honor 2025 Academy for Advanced Healthcare Leaders Graduates

NC Medical Society to Honor 2025 Academy for Advanced Healthcare Leaders Graduates
The North Carolina Medical Society (NCMS) invites you to celebrate the accomplishments of the 2025 NCMS Academy for Advanced Healthcare Leaders graduating class.
The NCMS Academy for Advanced Healthcare Leaders is an intensive, 8-month leadership development program designed for experienced physicians, PAs, residents, and healthcare administrators. This program is dedicated to cultivating advanced leadership skills, focusing on strengthening professional networks, optimizing team performance, and implementing strategic changes through high-impact, individual projects.
The upcoming graduation and project presentations will highlight the culmination of this rigorous program. Graduates will present their key learnings and demonstrate how they will apply these insights to their professional roles. They will also present their capstone projects, which are initiatives of their choosing with direct applicability to their workplaces, local medical societies, and the NCMS.
Event Details
These virtual events will be held over the course of two days and conducted via Zoom. Attendees can join or leave the sessions as their schedules allow. See the Presentation schedule below to include topics and presenters.
Register for each virtual session using the following links.
Part 1: Monday, September 15, 2025 | 6:00 PM - 8:00 PM ET
Part 2: Tuesday, September 30, 2025 | 6:00 PM - 8:00 PM ET
| Presentations:
Part 1: Monday, September 15, 2025
|
||||||||||||||||||||||||||
YOUR Feedback on ways to Reduce Low-Value Care in Medicaid and Improve Efficiency

YOUR Feedback on ways to Reduce Low-Value Care in Medicaid and Improve Efficiency
Two weeks ago, Medicaid providers were notified of a potential rate cut stemming from conflicting views on the Medicaid rebase number between the General Assembly’s non-partisan Fiscal Research Division and the Governor’s Office. The Department of Health and Human Services, alongside House Leadership and staff, continues to engage in discussions to reconcile the differing rebase figures. A House package, anticipated in the coming weeks, is expected to address the rebase issue without implementing provider rate cuts. We requested physicians and PAs provide us with ideas regarding possible improvements in Medicaid that may obviate the scheduled cuts.
Thank you to everyone who shared feedback on ways to reduce low-value care in Medicaid and improve efficiency. Here are the main themes from your responses:
1. Low-Value or Unnecessary Services
2. Administrative & System Inefficiencies
3. Suggestions for Improving Efficiency
4. Impact of Rate Cuts
Your feedback underscores both the urgency and complexity of these issues. We will continue using these insights to guide our advocacy and ensure physicians and patients are supported. If you have not had a chance to respond, please do so here. |
Virtual Annual Business Meeting: Join us on October 4!

NCMS Members, As NCMS undergoes exciting changes, we are evolving the ways we connect and collaborate to ensure your voice is at the center of our work. In place of our traditional LEAD conference this year, we’ll be holding a member-only, virtual Annual Business Meeting that you are invited to attend. Annual Business Meeting Details: When: October 4, 2025, from 9-11:00 am Where: Zoom webinar (Register Here) Your everyday experience and concerns guide our work. On October 10-11, 2025, Directors from NCMS, the NCMS Foundation, Carolina Complete Health, and Carolina Complete Health Network will gather for a strategic planning meeting. As we prepare for that meeting, we want to hear from you. Please complete this form—whether or not you can attend the virtual meeting—so your voice is represented! This form allows you to share insights regarding:
While the most common and pressing themes from your feedback will be briefly highlighted at the Virtual Annual Business Meeting on Oct. 4. Your input will be used at our Oct. 10-11 gathering to help shape the NCMS' strategic direction. We hope you will save the date and plan to join us virtually on October 4. Your participation will guide the future of NCMS through meaningful discussion and collaboration. We look forward to seeing you! |
Latest Update on NC Health Insurance Payers Implementing Downcoding Claims Review Programs
Latest Update on NC Health Insurance Payers Implementing Downcoding Claims Review Programs
The NCMS recognizes several health insurance companies have recently implemented claims and code review programs resulting in the down coding of certain Level 4 and 5 Evaluation and Management (E/M) claims.
Our leadership team met with representatives from Aetna sharing concerns about the significantly negative impact their program has on physician practices in our state. Aetna representatives shared their “Evaluation and Management (E&M) Program Claim and Code Review” does not target all Level 4 and 5 E&M codes nor include all providers in the state. While we are aware of the participation details and how providers are identified and placed in the program, there is still confusion about the applicability and reason for its implementation. NCMS has requested clarification and will continue working with representatives.
Cigna’s “Evaluation and Management Coding and Accuracy Program” takes a more sweeping approach applying to all physicians but limiting their review to six codes: 99204-99205 (new patient), 99214-99215 (established patient) and 99244-99245 (consult for new & established patients). This program is to be implemented nationally on 10/1/2025. The AMA and several state and specialty societies are working together to address this with Cigna. NCMS staff is working to meet with Cigna leadership. For questions or comments, please contact Jenni Hines, Director of Payer & Practice Engagement at [email protected]. NCMS remains committed to resolving this issue.
If you find yourself included in Aetna’s claims review program and don’t agree with their edits, please follow the appropriate appeals process to ensure issues are addressed in a timely fashion. Note, some contracts have special dispute provisions – please make sure you know your options.
What the Pharmacist Collaborative Practice Law Means for Team-Based Care
What the Pharmacist Collaborative Practice Law Means for Team-Based Care
| NCMS Members,
House Bill 67 was passed by the NC House on June 24th and signed into law by Governor Josh Stein on July 1st. The bill combined health-care provisions from about 10 different bills. In addition to the team-based care update we emailed you recently, HB 67 includes a Pharmacist Collaborative Practice law that reforms the regulatory requirements for Clinical Pharmacist Practitioners (CPPs) practicing under a collaborative practice agreement with physicians and gives supervising physicians more flexibility in how they choose to collaborate with the CPPs. Here’s what this law means for our members and patients: NCMS was supportive of these changes as they better enable CPPs to be included in healthcare teams outside of a hospital setting and strengthen value-based care. NCMS worked with Senator Sawrey, the primary sponsor of this proposal, and the Pharmacy Association to refine the proposal’s language and deepen our shared understanding of CPPs’ role in team-based care.
As always, your Medical Society will continue to work on the development and implementation of this law. |
In Memoriam: NCMS Past President Jack Hughes, MD
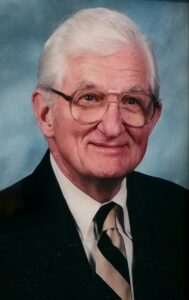
Jack Hughes MD
Durham, NC
November 24, 1919 – August 21, 2025
Dr. Jack Hughes, 105, of Durham, NC, died on August 21, 2025.
Dr. Hughes was born in Tabor City, NC on November 24, 1919, the son of Willa Leon Leggett and David James Hughes. He was a graduate of the University of North Carolina at Chapel Hill (1939) and earned his medical degree at the University of Pennsylvania School of Medicine (1944). He was a nationally known urologist practicing in Durham at Lincoln, Watts and Durham Regional Hospitals from 1950 until his retirement in 1988. He also served as an adjunct professor at Duke University and the UNC School of Medicine.
He was preceded in death by his parents, first wife Helen Schley of Savannah, GA, brothers Phil (Christine) and Don (Esther), both of Tabor City, sisters Lillian Webster (Willie Brooks) of Fairmont, NC, and Gwen Barnes (Henry) of Raleigh.
Survivors include wife Scott Tyree Evans Hughes; six children – Dr. John Schley (Patricia Dillon) of New Haven, CT; James Philip of Wilson, NC; Charles MacDonald (Sharon) of Charlottesville, VA; Elizabeth Hughes Hall (Joseph W.) of Gordonsville, VA.; William Leggett (Rebecca Chase) of Vero Beach, FL; Robert Pickens (Catherine) of Atlanta; step-daughter Scottie Chastain (Ben) of Tega Cay, SC; nine grandchildren and seven great-grandchildren.
Dr. Hughes was one of the oldest veterans of D-Day, serving as medical officer with the US Navy as Lieutenant JG at Normandy Beach in June 1944.
He was active in civic, volunteer and medical organizations at the local, state, regional and national levels. He served as president of the NC Medical Society from 1983 to 1984. He also was president of the Southeast American Urological Society and the North Carolina chapter of the American College of Surgeons. He was instrumental in the founding of the NC physician-owned HMO, later acquired by Cigna.
He was a vice president of the Durham Chamber of Commerce and chairman of the board of Durham Operation Breakthrough. He was a member of St. Stephen’s Episcopal Church and sang in the choir for more than 40 years.
In lieu of flowers, the family asks that donations be given to St. Stephen’s Episcopal Church, Hospice of Durham or the charity of your choosing.
Eastern NC Physicians Rally Behind Murphy’s Medicare Payment Reform Efforts in Congress

Eastern NC Physicians Rally Behind Murphy’s Medicare Payment Reform Efforts in Congress
Dr. Joe Healy and Dr. Kenneth Wilkins, Jr. at Coastal Carolina Health Care in New Bern have issued a public message supporting Medicare physician payment reform and the efforts of Congressman Greg Murphy MD to advance legislation targeting that critical issue. Their op-ed was published in the August 23, 2025 edition of the Sun Journal which has a circulation covering eastern North Carolina.
Dr. Healy’s and Dr. Wilkins’ message echoes that of the North Carolina Medical Society and our partner stakeholders, emphasizing the non-sustainability of the Medicare payment cuts that physicians have absorbed for many years. Those cuts have impacted accessibility of care for our state’s Medicare population and is an ever-increasing threat to the viability of medical practices across North Carolina.
Since 2001, Medicare physician payment has declined by 33% when adjusted for inflation in practice cost. Unlike other Medicare providers, physicians' annual payment updates are not tied to the Medical Economic Index (MEI), which reflects practice cost inflation.
Some good news, but only temporary relief
The recently enacted budget reconciliation bill, H.R. 1 / One Big Beautiful Bill, provided a modest payment update for 2026. Next year, physician payment will see a one-year positive adjustment of 2.5%. This payment relief is welcome, but more is needed to offset two and a half decades of payment reductions.
Congress’ inaction will continue to impact independent and rural practices the most resulting in further access to care problems for North Carolina’s elderly and low-income citizens. This makes your relations with members of Congress like Dr. Murphy all the more important.
Urgency
North Carolina presently has over 2.2 million Medicare enrollees and the 65+ population in the state is expected to approach 3 million by 2040. Declining Medicare payment for physicians is exacerbating the access to care challenge this patient population is facing, which has intensified the need for collective advocacy on this issue.
Add your voice
Physicians across the state are encouraged to follow Dr. Healy’s and Dr. Wilkins’ lead in making your voice heard. If you need assistance in connecting with your member of Congress, we’ll be glad to help ([email protected]).
Do you know your state and federal legislators?
More importantly, do your legislators know you?
Be a key contact for your legislators
Help NCMS Respond to Medicaid Cuts and Protect Care

Help NCMS Respond to Medicaid Cuts and Protect Care
Share Your Insights on Low-Value Care and Wasteful Spending
North Carolina physicians face an immediate threat to fair Medicaid reimbursement. In response to the General Assembly’s Medicaid budget, passed in June 2025, NCDHHS issued this recent statement:
“By the end of this month, NCDHHS will begin to cut $319 million from Medicaid by implementing rate reductions of 3% across all providers, as well as rate reductions of 8% or 10% for select providers, and elimination of certain services altogether – all with an effective date of October 1, 2025."
At the heart of these cuts is a dispute between the General Assembly’s Fiscal Research Division and DHHS Medicaid experts about whether current funding is enough to sustain the program through the 2026 fiscal year.
NCMS is meeting with legislators, NCDHHS officials, physician leaders and other affected groups to understand our options in response to these rate cuts. We are also working to get clear answers on the funding gap behind these cuts.
Physicians are uniquely positioned to identify inefficiencies in the Medicaid program. We are asking you to share your insights on low-value care and examples of wasteful spending or any other ideas that you may have. Your feedback can help shape alternative solutions to these cuts.
Please respond HERE.
HHS Announces Request for Nominations of Federal Healthcare Advisory Committee Members

HHS Announces Request for Nominations of Federal Healthcare Advisory Committee Members
The U.S. Department of Health and Human Services (HHS) and Centers for Medicare & Medicaid Services (CMS) are establishing the Healthcare Advisory Committee—a group of experts charged with delivering strategic recommendations directly to HHS Secretary Robert F. Kennedy Jr. and CMS Administrator Dr. Mehmet Oz to improve how care is financed and delivered across Medicare, Medicaid and the Children's Health Insurance Program (CHIP), and the Health Insurance Marketplace.
"Every American high-quality, affordable care – without red tape, corporate greed, or excessive costs," said HHS Secretary Robert F. Kennedy Jr. "This new advisory committee will unite the best minds in healthcare to help us deliver real results, hold the system accountable, and drive forward our mission to Make America Healthy Again."
"This is a moment for action," said CMS Administrator Oz. "This committee will help us cut waste, reduce paperwork, expand preventive care, and modernize CMS programs with real-time data and accountability, all while keeping patients at the center. We are calling on experts across the country to join us in this effort to help us Make America Healthy Again."
Nomination Process
CMS is accepting nominations for advisory committee members. Individuals with expertise in chronic disease prevention and management, federally administered health care financing, and delivery system reform are encouraged to apply. Individuals may either self-nominate or be nominated by an organization. Nominations must be submitted within 30 days of the publication date in the Federal Register and members will be selected later this year.
Committee Deliverables
The advisory committee will focus on developing:
- Actionable policy initiatives to promote chronic disease prevention and management;
- Opportunities for a regulatory framework of accountability for safety and outcomes that reduce unnecessary red tape and allow providers to focus on improving patient health;
- Levers to advance a real-time data system, enabling a new standard of excellence in care, rapid claims processing, rapid quality measurement, and rewards;
- Structural opportunities to improve quality for the most vulnerable in the Medicaid program; and
- Sustainability of the Medicare Advantage program, identifying opportunities to modernize risk adjustment and quality measures to assess and improve health outcomes.
For more information or to submit nominations, visit the Federal Register Notice at: https://www.federalregister.gov/d/2025-16136.
Standing Together for Colleague Well-Being

Standing Together for Colleague Well-Being
In North Carolina, the NC Clinician & Physician Retention & Well-Being Consortium (NCCPRW), in partnership with The Dr. Lorna Breen Heroes’ Foundation, is leading Caring for NC Caregivers, an initiative where hospitals and health systems commit to:
- Eliminating barriers to mental health care for licensed health workers
- Participating in training to understand burnout and improve well-being
- Implementing 12-month plans to reduce operational and administrative burdens
National Physician Suicide Prevention Awareness Day is September 17, a day to raise awareness and take action to support our colleagues.
North Carolina to Apply for the Rural Health Transformation Program

North Carolina to Apply for the Rural Health Transformation Program
The North Carolina Department of Health and Human Services (NCDHHS) has announced that it will submit an application for funding from the federal Rural Health Transformation Program (RHTP). The program is part of H.R. 1 (One Big Beautiful Bill), which was signed into law on July 4, 2025. The program was established to address rural health concerns due to federal cuts to the Medicaid program.
NCDHHS is inviting input and has set up a website for providers to give input on North Carolina’s application and will also host several opportunities in the coming months for partner organizations to provide input for the state’s RHTP application.
The Medicaid program will see cuts resulting in approximately $1 trillion in losses nationwide in the next 10 years as a result of H.R. 1. The impact in North Carolina is projected to be $49.9 billion. The cuts are anticipated to especially impact those living in rural communities.
"We are rooted in our commitment to improve the health and well-being of all North Carolinians, and that includes the more than 3 million people who live in our rural communities," said NCDHHS Secretary and NCMS Past President, Dr. Dev Sangvai. "As we navigate changes at the federal level, we will not lose sight of the mission to create a healthier North Carolina for all, despite the steep cuts to Medicaid and rural health."
RHTP funding would help relieve the anticipated financial strain of rural providers, including hospitals. The program would provide temporary funding over the next five years but would not replace the funds North Carolina’s rural hospitals and providers would have received if H.R. 1 had not been enacted. RHTP would replace approximately half of the $3.7 billion in anticipated losses that North Carolina rural hospitals will face due to the Medicaid cuts in H.R.
RHTP funding will total $50 billion nationally and will be issued in 10 payments to all 50 states over the next five years.
- $25 billion will be disbursed evenly between all 50 states each year for the next five years.
- The second $25 billion will be distributed among all 50 states at CMS’ discretion.
As part of the plan North Carolina submits to CMS to opt into the RHTP, NCDHHS will specify how it will:
- Improve access to rural hospitals and other health care providers;
- Improve health care outcomes for rural residents;
- Foster partnerships between rural providers; and
- Strengthen the rural health care workforce.
CMS expects to approve state plans for participation in the RHTP by December 31, 2025. Once the application is approved, a public notice will be issued to advise providers and hospitals when they are able to apply for a portion of the funding.
ICYMI: What the Interstate Medical Licensure Compact (IMLC) Law Means for You

ICYMI: What the Interstate Medical Licensure Compact (IMLC) Law Means for You
| NCMS Members,
On June 24th, House Bill 67 was passed by the NC House and quickly signed into law by Governor Josh Stein on July 1st. One important portion of this bill is the Interstate Medical Licensure Compact (IMLC) law, which is designed to improve access to health care by creating an efficient licensure process that allows physicians to become licensed in all participating states. Here’s what this law means for our members and patients: NCMS has actively supported the IMLC and has included the proposal in its legislative priorities since it was first introduced. To date, 41 states have adopted some portion of the IMLC. Once fully implemented, the IMLC will allow physicians to more efficiently obtain a medical license in multiple states in one single process. The IMLC also has the potential to reduce the negative impact of non-compete clauses as non-compete clauses are generally unenforceable across state lines.
|
|||||
Community Practitioner Program Meeting
Community Practitioner Program Meeting
The NCMS Foundation's Community Practitioner Program (CPP) will hold its 37th Annual Meeting on September 26th at the NCMS office. CPP participants will hear about the NC Physicians Health Plan, NC Clinician and Physician Retention and Well-Being Consortium, NCMS Practice Solutions, and other subjects that will enhance their ability to practice medicine.
Breaking Barriers to Substance Use Recovery
Breaking Barriers to Substance Use Recovery
NCMS Foundation's Project VBOT is proud to host the Post Overdose Response Team (PORT) Summit. PORTs provide outreach, engagement, and resource navigation to individuals who have serious opioid and other substance use challenges. Summit speakers will include NCDHHS Chief Medical Officer, Dr. Larry Greenblatt, chair of the NCMS Opioid Task Force, Congresswoman Deborah Ross, and other subject matter experts.
BBSUR_PortSummit_SaveTheDate (1)CMS Listening Session: Opportunities to Enhance Real-Time Claims Processing & EDI Cybersecurity Controls

CMS Listening Session: Opportunities to Enhance Real-Time Claims Processing & EDI Cybersecurity Controls
Wednesday, August 13 from 3–4 pm ET
Register for this online event.
As part of CMS’ 2025 priorities, we’re holding a listening session to gather feedback from our industry partners for innovative ideas and opportunities for real-time claims processing. We’re also looking to improve Medicare’s Electronic Data Interchange (EDI) cybersecurity controls that support the security and integrity of electronic transactions physicians, suppliers, and other providers use to submit Medicare Part A and Part B claims.
We’re interested in getting your feedback based on your experiences with other insurers with real-time claims processing integration and solutions in the industry (such as revenue cycle health, denials, rejections, appeals, reimbursement time frames).
We also want to hear your feedback to improve and enhance our processes related to strengthening Medicare’s EDI cybersecurity controls to better protect the integrity and availability of information systems involved in processing Medicare claims and the security and privacy of the sensitive beneficiary data being exchanged.
Email comments or questions in advance of the listening session to [email protected] with “Real-Time Claims & EDI Cybersecurity” in the subject line. We may address them during the listening session or use them to develop other resources following the session.
Read the full announcement (PDF) for more information.
NCMS Team Member Receives AENC’s Highest Accolade
 NCMS Team Member Receives AENC’s Highest Accolade
NCMS Team Member Receives AENC’s Highest Accolade
At its recent 2025 Annual Meeting, the Association Executives of North Carolina (AENC) recognized North Carolina Medical Society (NCMS) team member, Alan Skipper, with its highest accolade, the Timothy D. Kent Award. This honor is presented by AENC to the association profession’s most esteemed ambassador and mentor in recognition of the recipient’s impact on the organization, the profession and their peers.
The award was introduced this year following the passing of one of AENC’s most revered members and respected leader in the association management community – Timothy D. Kent. Mr. Kent was a 30-year member of AENC having served as CEO of North Carolina associations that represent the state’s architects, realtors and beer and wine wholesalers. He was a past president of AENC and highly regarded among his state and national association management colleagues, as well as among his fellow lobbyists and legislators at the NC General Assembly.
Skipper, a 45-year member of AENC, has also served as the organization’s president and in many committee and leadership roles. He is a past recipient of AENC’s awards recognizing legislative and political achievements and impact on the association management profession.
Skipper began his career with the NCMS in August of 1980. He is a 2024 recipient of the NCMS’ John Huske Anderson Award, which annually honors a layperson whose contributions have had a positive impact on the medical profession and public health, and received the 2025 Distinguished Service Award from the NC Ob/Gyn Society. He has previously received similar national accolades from the American Academy of Ophthalmology and the American Academy of Orthopaedic Surgeons.
The AENC award was presented at its 2025 Annual Meeting and 70th anniversary event in Raleigh, which featured Governor Josh Stein as the keynote speaker. Presiding was AENC’s 2024-2025 president, Kathryn Atkinson with the NC Academy of Family Physicians. Present and participating in the special recognition were Mr. Kent’s wife, Andra Zarins, and his son, Stephen Kent.
Exciting Job Opportunities to Improve Mental Health Access in Robeson and Scotland Counties!

Exciting Job Opportunities to Improve Mental Health Access in Robeson and Scotland Counties!
Old North State Medical Society (ONSMS) is hiring for three impactful positions as part of a new DHHS-funded initiative aimed at expanding mental health access and reducing ER visits related to behavioral health among youth in underserved communities.
This innovative program will utilize mobile hubs to proactively address behavioral health needs—bringing education, assessments, and connection to resources directly into the community. The integrated care model will not only empower individuals to seek appropriate mental health services but also support healthcare providers with culturally and linguistically appropriate resources to reduce burnout and promote clinician well-being.
Now Hiring at ONSMS:
1. Behavioral Health Team Lead (Licensed Nurse – RN/NP or Physician Assistant): Lead a mobile behavioral health team in delivering community-based care and coordination.
2. Behavioral Health Team Social Worker: Provide direct outreach, education, and connection to mental health resources with a focus on youth and families.
3. Behavioral Health Teams Assistant: Support operational logistics and ensure smooth delivery of mobile services across Robeson and Scotland counties.
Interested or know someone who might be? Join ONSMS and the Let’s Talk campaign in transforming mental health access in Robeson and Scotland communities.
Duke Health and Atrium Health Honored as 2025 Wellbeing First Champions

Duke Health and Atrium Health Honored as 2025 Wellbeing First Champions
At the North Carolina Hospital Association’s (NCHA) Summer Meeting, Duke Health and Atrium Health were named 2025 Wellbeing First Champion Award recipients by the North Carolina Clinician and Physician Retention and Wellbeing (NCCPRW) Consortium and the national Dr. Lorna Breen Heroes’ Foundation.
This award recognizes hospitals that have taken significant action to remove stigmatizing language related to mental health from their credentialing applications—a key step in making it easier for clinicians to seek the help they need without fear of professional repercussions.
With the inclusion of Duke and Atrium, 79 hospitals across North Carolina have now committed to this important reform, supporting health workers’ ability to access care when they need it most.
“This is more than a paperwork change—it’s a culture shift,” said Monecia R. Thomas, Executive Director of NCCPRW. “By removing unnecessary barriers to care, we’re protecting not just the wellbeing of our clinicians, but also the quality of care they provide to patients across the state.”
Ensuring that health workers can seek mental health care without stigma is a critical step toward building a healthier, more resilient healthcare workforce—and a healthier North Carolina.
Join Us in the movement or to learn more about our work state-wide.
The NCCPRW Consortium encourages all hospitals and health systems to take this step. Reviewing and revising credentialing forms to eliminate stigmatizing language helps protect clinicians' mental health and strengthens the entire care delivery system.
Atrium Photo
• Corey Feist, JD, MBA, Founder/Chief Executive Officer, Dr Lorna Breen Heroes Foundation
• Andrea S. Fernandez, MD, MA, FACOG, Chief Medical Officer, Atrium Health – Wake Forest Baptist Market & Clinical Professor of Ob/Gyn, Wake Forest University School of Medicine
• Monecia R Thomas, PhD, MHA, Executive Director of NCCPRW & VP of Professional Growth at NCMS
Duke Photo
• Corey Feist, JD, MBA, Founder/Chief Executive Officer, Dr Lorna Breen Heroes Foundation
• Uzuri Holder, Program Manager and a licensed clinical social worker
• Charles Mallett, MBA, Sr. HR Business Partner at Duke University Hospital
• Thomas A. Owens, MD, Executive Vice President and Chief Operating Officer, Duke University Health System & Associate Professor of Medicine and Pediatrics, Duke University School of Medicine
• Monecia R Thomas, PhD, MHA, Executive Director of NCCPRW & VP of Professional Growth at NCMS
2025 Mid-year Congressional Advocacy Update

2025 Mid-year Congressional Advocacy Update
A New Year / A New Administration / A New Congress
Following the presidential election every four years, there is typically a period of several months for things to settle in on Capitol Hill. The transition with arriving members of Congress, along with new committee appointments, presidential cabinet hearings and a shuffle in office assignments takes some time, and substantive business usually gets underway before spring arrives. 2025 has seen a delay in that timeline due to the President’s and the new administration’s exertion of authority and influence. Since the first of the year, numerous executive orders have been issued, with considerable impact on multiple branches of government, and the emergence of the Department of Government Efficiency (DOGE) has also been a jolt to the status quo across multiple government agencies. Most notable targets include research funding (NIH) and public health guidelines (HHS).
Issues that were on the short list of federal legislative priorities at the outset of 2025 included:
- Medicare payment fix
- Medicare telehealth coverage
- Prior authorization relief
- Step therapy relief
- Workforce expansion needs
- Research funding preservation
- Physician/clinician wellness
Medicare Physician Payment
2024 wrapped up with an intense push to avert the anticipated 2.8% Medicare physician pay cut scheduled to go into effect on January 1, 2025. The prospect of eliminating the cut was very good until the President’s new Department of Government Efficiency (DOGE) torpedoed the year-end legislative package – known as a Continuing Resolution – which was to be the vehicle for a remedy for Medicare payment.
The 2.8% cut ultimately went into effect (“Grinched by Congress) as of the first of the year so the new year brought with it a renewed commitment to reform Medicare physician payment. The 2025 reduction represents the fifth straight year of cuts to physicians, and from 2001 to 2025, physicians have now seen a decline in Medicare payment of 33% when adjusted for inflation (graphic below).

To address the growing Medicare payment dilemma, Congressman Greg Murphy, MD (NC-3), along with a bipartisan group of his House colleagues, introduced new legislation – H.R. 879 / Medicare Patient Access and Practice Stabilization Act to stop the 2.8% cut in Medicare physician payment while also providing a positive payment update to help practices absorb the increasing costs they are facing. Upon introducing the legislation, the goal was to get it incorporated into the Congress’ next funding measure, another Continuing Resolution, that was enacted at the end of March. The NCMS went “all in” to get all 14 of our North Carolina members of the House on the bill as co-sponsors to help its potential for advancing. The Society partnered with a coalition of national and state medical society partners in sending a letter to US Senate and US House leaders emphasizing the urgency of fixing Medicare payment. A March 5, 2025 Alert urged North Carolina physicians to contact their US House members, followed by another Alert on March 9, and we were successful in getting nine N.C. members of the House to formally join the bill. The measure was ultimately not included in the March funding package as hoped, so the House of Medicine redoubled its efforts to keep the Medicare payment reform issue as a foremost priority.
Recent NCMS messaging to Congress has emphasized the impact of Medicare payment cuts in North Carolina, as evidenced by the survey of NCMS members in 2024 Q4 – Results. And, NCMS board member, Dr. Karen Smith, helped strengthen that advocacy effort and message through an op-ed column in her local newspaper, the Fayetteville Observer.
H.R. 1 / One Big Beautiful Bill
In addition to the delays in getting up to “business as usual” speed that resulted from the waves of directives coming out of the White House and new administration, the introduction and controversy around H.R. 1 / One Big Beautiful Bill (OBBB) has been the most time consuming issue on the federal legislative front through the first half of 2025. This legislation was the President’s number one priority at the outset of his term in office. Though the bill drew a lot of attention for its impact on Medicaid and other healthcare-related issues, it was actually a tax funding bill to extend the tax cuts that were enacted in 2017 and due to expire in 2025. To cover the cost of the tax cut extension, Congress was charged with making budget cuts to absorb the cost of the cuts. That directive put Medicaid in the crosshairs along with the Supplemental Nutrition Assistance Program (SNAP) an student loan funds.
At the outset of the discussion of the measure and with several areas of concern emerging, the NCMS sent North Carolina’s members of the US Senate and US House a letter to call attention to how the OBBB would be very consequential for North Carolina. Additionally, the NCMS had multiple meetings with our congressional offices and subsequently sent each of our 14 House members a follow-up letter outlining the various elements of the proposal that would be detrimental to our state. The bill eventually passed the House and the NCMS similarly reached out to our Senate members with a letter of concern as they deliberated over the legislation.
In addition to our Society-initiated advocacy and member communications in May and June, the NCMS also partnered with multiple other stakeholders to help add volume to our messaging. The Society joined multiple sign-on letters that were delivered to Capitol Hill.
Coalition of State Medical Associations letter – February 28, 2025
Coalition of State Medical Associations letter – June 4, 2025
Coalition of State Medical Associations letter – June 24, 2025
As broadly publicized in the media and through NCMS communication, the OBBB passed and was signed into law by the President on July 4, 2025. One bright spot in the enacted legislation is that Medicare physician payment will increase by 2.5% for 2026 – a one-year adjustment. An initial impact assessment from NCDHHS has reported the following.
Work requirements
- Adds a work requirement for Medicaid expansion states (Ages 19–64) – 80 hours per month minimum.
- Exemption: Parents, guardians and caretakers with children 14 or younger.
- Effective: December 31, 2026. (Can appeal for a 2-year extension)
- 250,000 North Carolinians projected by to be impacted.
Provider taxes
- Reduces the current 6% Provider Tax cap down to 3.5%
- Project $ Impact to NC: $22.5 billion over 10 years
- Effective: October 1, 2026.
Healthcare Access and Stabilization Program (HASP)
- HASP payment cuts will begin in 2028
- Impact: $6B
Eligibility / Enrollment
- States will be required to check eligibility every 6 months instead of annually, starting December 31, 2026.
- The change in frequency will result in county social services offices being challenged to double their productivity.
- Delays in eligibility determinations are anticipated.
Medicaid Expansion
- R. 1 will result in increased cost to NC Medicaid due to the work requirement and the lower ceiling for provider tax.
- Work requirements bring new administrative costs.
- Capping provider taxes at 3.5% instead of 6% will add new cost to the state.
- State/federal funding shift expected to activate the “trigger” provision in Medicaid expansion law.
Action Options for the NC General Assembly
- Enact technical correction to the hospital provider tax funding formula to cover the administrative costs needed for work requirements.
- Change the “trigger law” and appropriate state funds.
- Change the “trigger law,” which could result in Medicaid Expansion being discontinued and authorize an alternative financing mechanism.
Mid-Year Re-set
With the OBBB having been enacted and signed into law, attention has shifted back to the legislative issues that had been prioritized at the first of the year . . .
- Medicare payment reform
- Prior authorization relief
- Step therapy relief
- Telehealth flexibilities extension
- Workforce
- Physician/clinician wellness
One additional issue that has emerged recently is inappropriate upcoding by Medicare Advantage plans. As a result, S.1105 / No UPCODE Act was introduced in the Senate to ensure that charges for treatment align with patients’ relevant medical conditions and that Medicare Advantage health plans aren’t able to overstate the severity of their plans’ enrollees’ health condition. A companion bill in the House is anticipated.
North Carolina Physicians Go to The Hill
Multiple groups of physicians have headed to Washington, DC this year to take medicine’s message to Congress. The NCMS has engaged with numerous partner organizations, such as the American Medical Association at their National Advocacy Conference, to advocate for quality patient care and the medical profession.

Leadership in Action - Dr. Karen Smith Leads VBC Discussion

Leadership in Action - Dr. Karen Smith Leads VBC Discussion
As part of the American Medical Association’s forum devoted to physician-led innovation strategies, Dr. Karen Smith was selected to lead a July 8, 2025 course on Value-based Care (VBC). Dr. Smith is a member of the NC Medical Society board of directors and the NCMS delegation to the AMA House of Delegates.
In the Practical Steps for Aligning Payment in Value-Based Care session, Dr. Smith
addressed opportunities and best practices related to quality performance, levels of financial risk, payment timing/accuracy, and payment methods. The session conveyed how these practices can drive improvements in care delivery and better align payment to enhance core VBC goals, including improved quality, reduced costs and a better experience for both patients and clinicians.
Burnout Down For Women Physicians, Yet Closing Gender Gap Still Key

Burnout Down For Women Physicians, Yet Closing Gender Gap Still Key
(AMA, Sara Berg, MS) — Physician burnout in the U.S. continues to trend downward, yet gender inequities persist, according to an exclusive AMA survey. That continuing gap underscores how workload, workplace culture and work-life balance pressures continue to weigh more heavily on women in medicine. But some innovative health systems are working to change that.
Nearly 18,000 responses from physicians across 43 states were received from more than 100 health systems and organizations who participated in the AMA Organizational Biopsy® last year. The AMA national physician comparison report—which is exclusive data to the AMA that is not published anywhere else—reflects 2024 trends on six key performance indicators—job satisfaction, job stress, burnout, intent to leave an organization, feeling valued by an organization and total hours spent per week on work-related activities (known as “time spend”).
The purpose of the aggregated data is to provide a national summary of organizational well-being and to serve as a comparison for other health care organizations. The results represent data from all organizations that surveyed with the AMA in 2024.
As the leader in physician well-being, the AMA is reducing physician burnout by removing administrative burdens and providing real-world solutions to help doctors rediscover the Joy in Medicine®.
For 2024, 43.2% of physicians reported experiencing at least one symptom of burnout, down from 48.2% in 2023 and 53% in 2022. But women physicians were still more likely to suffer from symptoms of burnout—at 47.2%—compared with 38.9% of men. This is a drop from 54.5% of women physicians and 42% of men in 2023.
Women physicians are also less likely to feel valued, at 51.6% compared to 58.2% of men. Meanwhile, 49.9% of women physicians reported feeling a great deal of job stress, compared to 40.2% of their male counterparts.
Additionally, 77.4% of women and men physicians felt satisfied with their jobs, up from 71.7% and 73.9% respectively. But 29.1% of women physicians said they intended to leave their current roles, compared to 32.7% of men.
All the figures—for both women and men—improved at least slightly according to exclusive AMA survey data in 2024, but the gender gap remained steady for most areas.
Explore how the AMA Health System Member Program works with health care leaders to tailor solutions that maximize support for physicians and care teams.
Health systems are making changes
The reduction in burnout rates for women physicians signals a promising trend that highlights the powerful impact of prioritizing well-being. It shows that ongoing efforts and programs that health systems have implemented can help—but the gender gap in physician burnout remains.
These examples from health care organizations that are part of the AMA Health System Member Program—which provides enterprise solutions to equip leadership, physicians and care teams with resources to help drive the future of medicine—show commitment to ongoing change to reduce the gender gap in burnout.
-
Washington Permanente Medical Group is incorporating AI to help
- Mary Pan, MD, remembers what it was like tracking patient conditions on paper charts. She also remembers the frustrations she had as the widespread adoption of EHRs led to more challenges for her and her fellow physicians.
- As augmented intelligence (AI)—often called artificial intelligence—becomes more commonplace in health care, Dr. Pan is not feeling quite so frustrated. Frankly, she's excited about how AI is already supporting those in her medical group and its potential to have a lasting impact on physician well-being.
- For women physicians within Washington Permanente Medical Group, two of the biggest factors that contributed to burnout were documentation and work outside the office. That is another reason why she's optimistic about incorporating AI into the workflow.
-
Privia Health helps physicians in private practice reclaim autonomy
- People are driven to choose a career in medicine not only because of their passion for the art and science of healing, but their deep capacity for care. However, the bureaucracy, systematic redundancies and chronic inefficiencies that are commonplace in some practices can interfere with that calling, leading to frustration and burnout, as it did for Nalini Casey, MD, a pediatrician at Privia Health.
- After years of wrestling with administrative overload, clinical bottlenecks and practice-level obstacles, she was questioning her future in medicine. Today, thanks to Privia Health, Dr. Casey is thriving there and practicing medicine as determined by her values and standards, and an actively hands-on approach is no longer out of reach.
-
Sutter Health took these seven steps to improve well-being
- After an alarming increase in physician burnout at Sutter Health in Northern California in 2021 and 2022, the large health system formed a broad interdisciplinary well-being committee and encouraged the formation of local well-being committees at each of its 22 hospitals to try to turn the tide.
- “We were able to see a significant decrease in our burnout level and improvement in well-being,” said Jill M. Kacher Cobb, MD, chief wellness officer for Sutter Health system.
- “We felt that it was due to multiple things that we did over the course of that year: setting up the systemwide interdisciplinary well-being program, asking for local leadership in well-being at each of our hospitals and also within our medical groups, setting up peer support and really engaging the leaders and sharing tools with them,” said Dr. Kacher Cobb.
-
Northwest Permanente builds community and culture through leadership
- When Stella Dantas, MD, and her husband traveled to the Taiwan Association of Obstetrics and Gynecology conference, many attendees eagerly greeted her husband.
- “People were coming up and shaking his hand, likely because they thought he was the president. But then I got up to the stage to give my presidential address and surprised people,” said Dr. Dantas, an ob-gyn at Northwest Permanente in Hillsboro, Oregon.
- As a leader, Dr. Dantas is committed to creating psychological safety. This serves as the foundation on which to build a strong culture. Naturally, establishing that psychological safety starts at the top with strong, diverse leadership.
-
Marshfield Clinic encourages women physicians to pursue their passion
- When Susan Turney, MD, took over as CEO of Marshfield Clinic Health System more than a decade ago, she scarcely could have imagined how a once-in-a-lifetime pandemic would test her leadership abilities to the limit. Dr. Turney has since retired as CEO, but with women health care leaders still too rare, she shared some of her hard-won wisdom with younger women physicians. One key is to strive for authenticity.
- “Be yourself. None of us are really obligated to carry the mantle of all women as it relates to our career trajectory,” Dr. Turney said.
-
Atlantic Health System embraces physician work groups
- As a response to the COVID-19 pandemic, Atlantic Health System established a committee that was largely focused on physician well-being. It was very effective for the need at that moment and for the time it was in place. But with the health system’s goal to be the best place for physicians to practice in New Jersey, they recognized that the work is broader than what could have been done through just that committee structure.
- Part of the systemwide well-being strategy included embracing physician work groups. Atlantic Health System has about 20 committees and work groups for physicians to be involved with. For example, a women in medicine work group is available to discuss what’s working, what’s not and share best practices.
AHA Scientific Statement Advocates for ‘Food Is Medicine’ as Intervention for Chronic Cardiometabolic Diseases

AHA Scientific Statement Advocates for ‘Food Is Medicine’ as Intervention for Chronic Cardiometabolic Diseases
(Medscape, Katherine Wandersee) — Rates of cardiometabolic illnesses among American adults have reached an astonishing 50%. For diabetes, cardiovascular disease, and related inflammatory conditions, the root cause often boils down to poor diet. Nearly 45% of all deaths from cardiometabolic diseases are attributable to unhealthy eating. Clinicians know they should be giving diet advice, but some programs are taking it a step further, showing it works better to provide patients with the food itself.
Enter Food Is Medicine initiatives. These programs are based on the concept that improving access to healthy food is cheaper and more efficient than paying for the inevitable results of a lifelong poor diet. They target segments of the population struggling with purchasing and preparing healthy food due to social, economic, and other barriers.
Features typically consist of:
- Produce prescriptions, designed to increase access to fruits and vegetables either through vouchers or by providing specific produce items.
- Medically tailored groceries, a prepackaged selections of unprepared foods often selected by nutritionists or dietitians to address the specific nutritional needs of the individual.
- Medically tailored meals, similar to medically tailored groceries, but consisting of fully prepared, ready-to-eat meals.
How well do Food Is Medicine programs offset the cost of caring for cardiometabolic diseases? The answer, in short: a mixed grocery bag.
The American Heart Association (AHA) recently issued a scientific statement based on a systematic review of these programs in the US. The review, published in the journal Circulation, analyzed randomized controlled trials of Food Is Medicine programs to quantify how such services can influence health outcomes — in this case, noncommunicable diseases.
The researchers assessed 14 randomized controlled trials, concluding the evidence is strong to justify current efforts to implement and disseminate Food Is Medicine programs. However, they acknowledged that the benefits of Food Is Medicine can be difficult to generalize across studies because of the broad variations in population, intervention design, duration of the program, and intensity of the intervention.
“A nutritious diet improves health outcomes; we know that clearly,” said Hilary Seligman, MD, MAS, a professor of medicine and epidemiology at the University of California, San Francisco, and lead author of the AHA statement. “We are still trying to figure out the best way for healthcare to help support patients in getting a healthy diet in a way that improves health outcomes, especially in the short term. Who should we be giving healthy food to? How, and for how long? These are some of the outstanding questions.”
Cheaper Than a Trip to the Emergency Room
“We can say with confidence that Food Is Medicine programs help people manage chronic illness and diet-related diseases, reduce emergency visits, reduce amputations from diabetes, and beyond,” said Devon Klatell, MA , vice president of Food Initiatives at the Rockefeller Foundation, a national philanthropic organization.
Robust studies are starting to show well-designed, effectively implemented programs can bring down costs and reduce the need for expensive healthcare services. A recent study from Cleveland Clinic showed patients receiving medically tailored meals had fewer visits to the emergency department (ED) and inpatient hospital days, resulting in an average cost saving of about $12,000 per patient.
Another study of Medicaid beneficiaries in Massachusetts found nutrition support led to 23% fewer hospitalizations and 13% fewer ED visits. Among adults enrolled in the government-funded program for over 90 days between 2020 and 2023, average healthcare costs dropped by an average of more than $2500 per person.
“I think all clinicians are aware that problems like food insecurity and poor nutrition can harm health, but we’ve had few tools to be able to address these problems in clinical care,” said Seth Berkowitz, MD, MPH, an associate professor of medicine and vice chief for Research at the University of North Carolina at Chapel Hill.
 Berkowitz, who is deputy scientific director for the AHA’s Health Care by Food initiative, said referring patients to these programs “really should be no different than placing a referral to a registered dietitian or nutritionist, or similar collaboration that clinicians engage in regularly.”
Berkowitz, who is deputy scientific director for the AHA’s Health Care by Food initiative, said referring patients to these programs “really should be no different than placing a referral to a registered dietitian or nutritionist, or similar collaboration that clinicians engage in regularly.”
Grocery Bills in the Healthcare Budget?
A recent Rockefeller Foundation survey showed nearly 80% of the American public would be personally interested in Food Is Medicine programs. “We know that Americans want these programs,” Klatell said.
Patients and clinicians who participate in these programs like and recommend them, she added. The catch is getting policymakers to endorse the approach.
“Integrating food into healthcare delivery can improve health, help to manage costs, and in many ways is common sense — but it’s also a new ‘muscle’ that the healthcare system needs to build and adapt to,” she said.
“For some reason, programs in healthcare that are prevention-oriented or address social needs are often held to a cost standard,” Seligman said. “This is a double standard because we approve new medications for use based on whether they work — not whether they save money,” she said. “Healthy food can be more effective than medication in preventing and treating chronic disease, at least over the long term. This should be all we need to know to justify their cost.”
North Carolina, It's Time to Lead the Way. Meet us at the Summit

North Carolina, It's Time to Lead the Way. Meet us at the Summit
As a platinum sponsor of the upcoming Joy & Wholeness Summit in Asheville (July 23-25), NCCPRW is committed to a healthier future for healthcare workers across our state.
This year, our goal is to host as many healthcare leaders and clinicians from North Carolina as possible. We know that true transformation in caring for North Carolina's caregivers requires more than conversation–it demands collective action.
That’s why we’re counting on you to join us.
Your presence is more than attendance. It’s a declaration that the health of healthcare professionals matters.
Plus, thanks to NCCPRW’s sponsorship, attendees from NC will access a 15% discount on registration with code NC2025. Don’t miss out on this invitation to be a part of something bigger!
What NCCPRW Leadership is Saying
“Joining the Joy & Wholeness Summit allows NCCPRW to elevate our mission, connect with like-minded organizations, and continue advocating for sustainable solutions in clinician well-being. This partnership represents a shared commitment to creating lasting change for the physicians and APPs we serve.”
– Monecia Thomas, Executive Director of NCCPRW
Learn more about the Summit and secure your spot! Every voice matters in growing the clinician and physician wellness movement. Thank you for using yours.
Measles Cases In The U.S. Hit The Highest Total Recorded In More Than 30 Years

Measles Cases In The U.S. Hit The Highest Total Recorded In More Than 30 Years
(CBS News, Sara Moniuszko)— The United States has recorded 1,288 measles cases so far this year, the highest total in 33 years, according to Centers for Disease Control and Prevention data out Wednesday.
This is now the worst year for measles in the U.S. since 1992, when 2,126 cases were confirmed. The virus was officially declared eliminated in the U.S. in 2000, after high rates of vaccination succeeded at halting nearly all domestic spread.
The largest share of this year's infections are connected to an outbreak in West Texas that led to the deaths of two children. The number of cases in Texas alone has grown to more than 750. Measles infections have been confirmed in 38 states.
"Measles risk is higher in U.S. communities with low vaccination rates in areas with active measles outbreaks or with close social and/or geographic linkages to areas with active measles outbreaks," the statement said, adding, "CDC continues to recommend MMR vaccines as the best way to protect against measles."
How measles cases spread
The measles virus is airborne and is one of the most contagious infectious diseases. A person can be contagious for several days before they develop the rash that often accompanies measles, the CDC says. The virus spreads through the air when an infected person coughs, sneezes, talks or even just breathes, and it can continue to infect others in the area for up to two hours after the infected person leaves.
Measles is primarily a respiratory virus, and in some cases it can cause severe infections in the lungs and brain that can lead to cognitive issues, deafness or death. But the vaccine, which is normally given as part of the combination measles-mumps-rubella (MMR) vaccine, is safe and highly effective at preventing it, doctors and health experts say.
Before the first measles vaccine became available in the 1960s, between 400 and 500 Americans — mostly children — died every year from measles.
Health experts point to lower vaccination rates as a reason for the increase in measles. Nationwide, a recent study found the MMR vaccination rate decreased from 93.92% in the 2017-2018 school year to 91.26% in the 2023-2024 school year, looking at county-level data in 33 states. A 95% vaccination rate is needed for herd immunity, which prevents outbreaks.
The Texas outbreak was originally centered in a rural Mennonite community with a lower vaccination rate, and most of those affected have been children and teenagers, nearly all of whom were unvaccinated or had an unknown vaccination status. State and local health officials confirmed the first patient who died was an unvaccinated school-aged child, and the second was an unvaccinated 8-year-old girl. Neither of the children had underlying health conditions, the Texas health department said. The death of one adult in New Mexico was also linked to measles.
Measles symptoms
Initial measles symptoms include fever, cough, runny nose, red eyes and a characteristic rash that begins to develop a few days later.
While most people's symptoms improve, about 1 in 5 unvaccinated people who get measles will be hospitalized. About 1 out of every 1,000 children with measles will develop brain swelling that can lead to brain damage, and up to 3 of every 1,000 children who become infected will die, the CDC says.
There is no antiviral drug or treatment that can cure measles, but medical care can help relieve symptoms. Doctors have some treatment options available to address complications like pneumonia or bacterial infections that can develop in measles patients.
Secretary and Former NCMS President Dr. Dev Sangvai Releases Statement on the U.S. House Passage of the Senate Reconciliation Bill

NCDHHS Secretary Dev Sangvai Releases Statement on the U.S. House Passage of the Senate Reconciliation Bill
(NCDHHS) — On July 3rd, the U.S. House passed the Senate reconciliation bill. The bill includes significant changes to federal funding for Medicaid, the Supplemental Nutritional Assistance Program (SNAP) and other public health and social support programs. The North Carolina Department of Health and Human Services is reviewing the final legislation to determine its full impact on the state and its residents. NCDHHS will provide additional information as more details become available and will remain focused on serving the people of North Carolina.
In response to the bill’s passage, NC Health and Human Services Secretary Dev Sangvai released the following statement regarding the impact of the legislation on North Carolinians.
"Today's passage marks a significant moment with real consequences for North Carolina. While the full impact will become clearer in the coming weeks, we already know that it will result in billions of dollars being taken out of our state’s economy and will undermine the health of North Carolinians.
This bill includes major changes to Medicaid and SNAP – programs that provide vital support to millions of North Carolinians. There will be a significant reduction in federal funding for services that are core to the well-being of individuals and families across North Carolina. These cuts not only impact the people that rely on them directly but also strain the systems and communities that hold us all together.
The mission of the North Carolina Department of Health and Human Services remains unchanged – we will continue to work to improve the health and well-being of all North Carolinians. This moment presents real challenges, and while our ability to offset these losses may be limited, our resolve is not. We will continue this work with determination, and compassion and a focus on the people we serve."
Family Experiences Unexpected Improvements of Personalized Treatment for Batten Disease at UNC

Family Experiences Unexpected Improvements of Personalized Treatment for Batten Disease at UNC
(UNC Health) — June 2025 marks one year since Amelia and Makenzie Kahn received their first dose of Zebronkysen, a personalized treatment developed by University of Michigan, Michelle Hastings, PhD, for their specific mutation associated with juvenile Batten disease, or CLN3. So far, benefits of the drug have helped Makenzie walk farther on her own while Amelia is taking bites of food, including ice cream.
Batten disease is an inherited, fatal pediatric neurodegenerative disorder in which patients experience loss of abilities; from motor, communication and cognitive decline to vision loss. They also suffer from seizures, anxiety, pain, and systemic effects, such as feeding and breathing difficulties. Life expectancy is from the teenage years to early twenties.
The ForeBatten Foundation, a nonprofit that was founded in 2017, funds juvenile Batten disease research and support for families whose lives have been affected by the disease. In June 2024 it launched the “N-of-2” clinical trial: the first in human RNA treatment tailored to a rare mutation of CLN3. The trial is the culmination of investigational drug development efforts, from laboratory research to manufacturing to establishing a trial protocol, with UNC serving as the study site. Yael Shiloh-Malawsky, MD, a professor of neurology at the UNC School of Medicine, leads the clinical study.
This new type of personalized trial, frequently referred to as an “N-of-1” study, is a type of clinical trial that focuses on just one individual rather than a large group of people. In the case of Makenzie and Amelia, this specific treatment was created for two patients, an “N-of-2” study.
Over the past year, Zebronkysen proved in being well-tolerated and demonstrated benefit for the girls. The drug was created to help restore the function of Amelia and Makenzie’s CLN3 gene ultra rare mutation and prevent further decline.
Thriving in the face of Batten disease: Makenzie’s Progress
A step in the right direction sparked for Makenzie. From less drowsiness to walking unassisted, profound moments were seen.
“Before the trial started one of the protocols in collecting data was to measure Makenzie’s steps as she walked for two minutes without help,” said Shiloh-Malawsky. “Before the start of the drug, she walked 22 yards and did not walk the full two minutes. Six months after receiving the treatment, she walked 48 yards.”
Dystonia can be a symptom of Batten disease. It occurs when a patient experiences involuntary muscle contractions, spasms, pain and lack of mobility. Prior to start of the trial Makenzie’s motor abilities were severely affected by dystonia, her dystonia has greatly decreased after receiving the treatment. She also regained the ability to get out of bed and to get up from the floor with no assistance, which was not possible for more than two years before starting the drug trial.
Makenzie’s energy level and stamina also improved, “Makenzie used to nap a lot and be sleepy. Now, she’s more alert and awake,” said Karen Kahn, Amelia and Makenzie’s mom.
Amelia’s Progress
Moments of joy appeared in Amelia and her smiles have become second nature.
“Before the treatment Amelia experienced sensory overload with Batten,” Karen said. “Now she tolerates noise in a restaurant and is happy. She wakes up in the morning and smiles at me.”
For the first time in about two years, Amelia started taking food and drink by mouth, like sipping water and taking bites of ice cream and yogurt. She also would normally need about two liters of oxygen to sleep at night, but now the amount has dropped to half a liter.
“Amelia also has more energy,” said Karen. “We used to use PRN rescue meds, as needed medications to help with pain, muscle spasms, and anxiety, to calm Amelia, and now we rarely need them. We still use daily medicines for the girls but not using the rescue medicines on a daily basis is a huge deal,” she said.
“We were pleasantly surprised by some of girls’ abilities appearing to come back,” said David Kahn, Amelia and Makenzie’s dad. “They didn’t last the complete three months between treatments, but there was the spike and plateau of benefits that we were very welcomed to see,” he said.
A Treatment Pathway
The girls started off receiving an intrathecal injection of 15 milligrams of Zebronkysen in June 2024. They received additional dose every three months, and the dosage was increased with a goal of seeing the progression of the disease lessen.
“After four doses, 12 months from the first dose in June 2024, we have seen an impact that is more positive than what we expected on multiple domains,” said Shiloh-Malawsky. “Our hypothesis was that restoring CLN3 protein function would stabilize this neurodegenerative disorder and prevent further decline. We did not expect to see improvement in addition to a slowing of decline, seeing improvements is more than we hoped for.”
Throughout the year researchers observed how abilities were temporarily regained after each dose. Symptoms improved in neurologic, psychological, and general health areas, like gastrointestinal issues, which became less severe. The positive effects appeared in multiple ways, like changes in mood, ability to tolerate noisy environments, a decrease in irritability and anxiety, and improved motor abilities. Importantly, no serious adverse events related to the study drug were observed. Increasing the drug dosage has led to longer-lasting benefits.
In June 2025, the girls received the target high dose of 45 milligrams. As of now, that amount will be the girls’ maintenance dose. With the higher dose the study team hopes to achieve lasting and sustained benefits. Dr. Shiloh-Malawsky says as long as the girls continue to benefit from it, they will continue to receive the high dosage every three months.
New Possibilities on the Horizon
The ForeBatten Foundation, Vanguard Clinical Rare Disease Foundation (VCRDF), a team of scientists and drug developers, and the UNC team are working to raise funding to develop treatment for other mutations that cause CLN3 Batten disease, medications that could benefit a larger patient population.
“Seeing the beneficial results from this trial puts an emphasis on the urgent need to develop similar interventions for people with other mutations in this gene of Batten disease,” said Shiloh-Malawsky.
With Zebronkysen becoming unquestionably life-changing and researchers continuing to develop individualized investigational antisense oligonucleotides (ASOs), the science is reaching new heights and potential for treating the common mutation of CLN3.
“We haven’t had any more loss of abilities while being on the drug over the last year,” said David. “That speaks to the stabilization of the decline of the disease. Zebronkysen looks very promising in our eyes.”
RFK Jr. Fires ‘Opening Salvo’ On Vaccine Status Quo

RFK Jr. Fires ‘Opening Salvo’ On Vaccine Status Quo
(The Hill, Nathaniel Weixel) — Public health experts say Robert F. Kennedy Jr is exactly who they thought he was.
The Health and Human Services (HHS) secretary — who is also the nation’s most well-known vaccine skeptic — is remaking the agency in his image, casting doubt on the benefits of vaccines, and erecting new barriers that will make it harder for people who want shots to get them, like requiring new vaccines to be tested against placebos.
During his confirmation hearings and other recent congressional testimony, Kennedy sought to distance himself from the anti-vaccine movement.
He argued he is simply seeking good data about vaccine safety. He assured lawmakers he would not take away anyone’s vaccines and specifically pledged to Sen. Bill Cassidy (R-La.) that he would not make any changes to the Centers for Disease Control and Prevention’s (CDC) vaccine advisory panel.
While testifying at a House Appropriations Committee hearing on May 14, Kennedy said his views on vaccines were “irrelevant.”
“I don’t want to seem like I’m being evasive, but I don’t think people should be taking medical advice from me,” he told lawmakers, after being asked whether he would vaccinate his own children today against measles.
Yet in the past week, Kennedy made an end run around the traditional process to change the recommendations about who should get a COVID-19 vaccine.
He threatened to bar government scientists from publishing in leading medical journals, and his office revoked hundreds of millions of dollars pledged to mRNA vaccine maker Moderna to develop, test and purchase shots for pandemic flu.
Kennedy has been critical of mRNA vaccines, and HHS said the funding was canceled because of concerns about the safety of “under-tested” mRNA technology.
Georges Benjamin, executive director of the American Public Health Association, said the public should take Kennedy at his word.
“He’s right. We shouldn’t trust him,” Benjamin said. “He’s unbridled. He’s out of control, and so I am fearful that he will do more to undermine vaccine access and quality in the United States.”
Kennedy has a long history of opposition to vaccines. He petitioned the Food and Drug Administration (FDA) in 2021 to revoke the emergency use authorizations of the COVID-19 vaccines and threatened to sue the agency if it authorized COVID vaccines for children.
His latest moves to change the COVID vaccine recommendations for healthy children and pregnant women are raising serious concerns about the potential to pull back on even more vaccines.
“What I see is COVID has provided this natural starting point … to sort of have that opening salvo in a bigger, longer-term effort to reconstruct, undermine vaccine policy,” said Richard Hughes IV, an attorney at Epstein Becker Green and former vice president of public policy at Moderna.
The decision to change COVID vaccine policy was announced in a 58-second video clip shared on the social media site X.
“I couldn’t be more pleased to announce that as of today the COVID vaccine for healthy children and healthy pregnant women has been removed from the CDC-recommended immunization schedule,” Kennedy said.
Days after Kennedy’s pronouncement, the CDC issued new guidance that removed the recommendation for pregnant women to get a COVID shot but kept the vaccine on the childhood immunization schedule.
The agency changed the recommendation from its previous wording of “should” to say healthy children “may” get the COVID vaccine after consulting with a health provider, an apparent contradiction to Kennedy’s plan.
Despite the new wording, the changes buck the traditional method of making new vaccine recommendations.
The FDA decides whether to approve or authorize a vaccine, and the CDC’s independent vaccine advisory panel convenes in an open public meeting to decide questions like who should get it, when and how often. It then sends recommendations to the CDC director, who can endorse or reject the recommendations.
The director nearly always defers to the panel.
The HHS secretary isn’t typically involved in vaccine decisions, but there currently isn’t an acting CDC director.
“We’re seeing a total side-stepping of the nation’s leading public health agency,” said Richard Besser, a former acting director of the CDC and president of the Robert Wood Johnson Foundation.
Besser said doctors rely on the recommendations of federal health experts, which are supposed to be based on the best available science and evidence. But doctors can’t be assured that’s the case anymore, he said.
Both Hughes and Benjamin said other changes to HHS vaccine policy are likely to be more nuanced and subtle than the agency’s actions on COVID.
“I would have said a couple months ago, obviously measles, obviously polio, those are childhood vaccines [that could be changed]. … But I think it’s going to be a little more subtle [than banning a shot]. It’s going to be a little more slow,” Hughes said.
In April, the CDC’s vaccine advisers met after a two-month delay to vote on recommendations for chikungunya vaccines, meningitis vaccines and respiratory syncytial virus (RSV) vaccines.
About a month later, Kennedy personally signed off on recommendations for the chikungunya shot.
He has not acted on the other recommendations from the panel’s April meeting, including the use of a new meningitis vaccine and an expansion of RSV vaccines to high-risk adults ages 50-59.
The vaccine panel isn’t scheduled to vote on COVID vaccine recommendations until late June. Experts said it’ll be important to listen to what the panel members say, and whether they feel they have the freedom to discuss HHS’s recent actions.
“You’ve got a committee of advisers who were cut out of the loop. How are they going to handle that in a public forum?” Benjamin said.
Medical Societies and Patient Sue HHS & RFK

Medical Societies and Patient Sue HHS & RFK
Medical Societies and Patient Sue HHS, Secretary Robert F. Kennedy, Jr. for Unlawful, Unilateral Changes to Vaccine Recommendations
The American Academy of Pediatrics (AAP), American College of Physicians (ACP), American Public Health Association (APHA), Infectious Diseases Society of America (IDSA), Massachusetts Public Health Alliance (MPHA), Society for Maternal-Fetal Medicine (SMFM), and a pregnant physician, filed suit in American Academy of Pediatrics v. Robert F. Kennedy, Jr. in the U.S. District Court for the District of Massachusetts to defend vaccine policy.
Plaintiffs in the case are suing the U.S. Department of Health and Human Services (HHS) and Secretary Kennedy for acting arbitrarily and capriciously by unilaterally changing Covid-19 vaccine recommendations for children and pregnant patients. The lawsuit asks for preliminary and permanent injunctions to enjoin Secretary Kennedy’s rescissions of Covid vaccine recommendations and a declaratory judgment pronouncing the change in recommendations as unlawful.
ACP President Jason Goldman stated, “As physicians, we require reliable, science-based guidance that is based on the best available evidence, developed through an evidence-based and transparent process, to ensure the safety, welfare, and lives of our patients.”
“This administration is an existential threat to vaccination in America, and those in charge are only just getting started. If left unchecked, Secretary Kennedy will accomplish his goal of ridding the United States of vaccines, which would unleash a wave of preventable harm on our nation’s children,” said Richard H. Hughes IV, partner at Epstein Becker Green and lead counsel for the plaintiffs. “The professional associations for pediatricians, internal medicine physicians, infectious disease physicians, high-risk pregnancy physicians, and public health professionals will not stand idly by as our system of prevention is dismantled. This ends now,” he added.
The lawsuit charges that a coordinated set of actions by HHS and Secretary Kennedy were designed to mislead, confuse, and gradually desensitize the public to anti-vaccine and anti-science rhetoric, and that Secretary Kennedy has routinely ignored federal procedural rules.
The anonymous individual plaintiff in the lawsuit is a pregnant woman who has been denied the Covid-19 vaccine booster since the HHS-issued directive, despite being at high risk for exposure to infectious diseases.
Atrium Health Levine Children’s Opens Union County’s First and Only Pediatric Emergency Department

Atrium Health Levine Children’s Opens Union County’s First and Only Pediatric Emergency Department
(Atrium Health News) — Families in Union County now have access to emergency care designed just for children for the first time. Atrium Health Levine Children’s Emergency Department Union has officially opened its doors as the first and only pediatric emergency department in Union County — delivering expert, around-the-clock care in a space thoughtfully designed for children and their families.
Located at Atrium Health Union, the new pediatric emergency department features a bright, welcoming environment with a child-friendly waiting area — making visits less intimidating and more comfortable for young patients. Backed by a team of pediatric-trained specialists, children can receive advanced emergency care for serious or life-threatening injuries and illnesses.
“When you walk through the doors of Atrium Health Levine Children’s Emergency Department Union, we want families to feel safe and truly cared for from the very first interaction with our team,” said Denise White, facility executive and chief nurse at Atrium Health Union. “This healing environment is brought to life by our pediatric-trained clinicians — experts in emergency care who know our community and understand all of our patients.”
The emergency department addresses a critical gap in access to pediatric-specific care by providing a convenient location for families in Union County and surrounding areas. With doors open 24 hours a day, 7 days a week, the new department ensures that dedicated care for children is always within reach, day or night.
“Atrium Health Levine Children’s is proud to enhance access to lifesaving, pediatric emergency care in Union County,” said Callie Dobbins, senior vice president of Atrium Health Levine Children’s. “By adding this first-ever pediatric emergency department in Union County, families now have access to a full range of dedicated pediatric services, from primary care to hospital-level care, when and where they need us most.”
If needed, children can be seamlessly admitted to the pediatric unit at Atrium Health Union where they’ll remain under the trusted care of Atrium Health Levine Children’s providers — ensuring comfort and familiarity throughout their care. Families also have direct access to additional expert services at Levine Children’s Hospital in Charlotte, ranked as North Carolina’s #1 Children’s Hospital by U.S. News and World Report.
Atrium Health Levine Children’s Emergency Department Union is part of a growing network of pediatric services in Union County, including Atrium Health Levine Children’s Urgent Care Union, Atrium Health Levine Children’s Indian Trail Pediatrics and Atrium Health Levine Children’s Union Pediatrics. Together, these locations offer families in Union County and surrounding areas a comprehensive range of pediatric care — all close to home.
States Brace For Added Burdens Of Trump’s Tax And Spending Law

States Brace For Added Burdens Of Trump’s Tax And Spending Law
(New York Times, David W. Chen and Pooja Salhotra) — The ink is not even dry on the far-reaching domestic policy law that President Trump signed on Friday, and already state governments are bracing for impact as Washington shifts much of the burden for health care, food assistance and other programs onto them.
Gov. JB Pritzker, Democrat of Illinois, and legislative leaders might hold a special session to deal with the new law, even though the recently passed state budget already includes $100 million to cover shortfalls in federal funding.
Another Democrat, Gov. Katie Hobbs of Arizona, has warned that even her state’s $1.6 billion emergency fund will be insufficient to weather what’s coming, because “even if we cut every single thing in the state, we don’t have the money to backfill all these cuts.”
Even before the bill’s final passage, state capitals were contending with a slowing economy and federal spending cuts implemented by the Department of Government Efficiency run by Elon Musk. Now they will be expected to administer complex new work requirements for Medicaid and food aid; rework some state health insurance exchanges under the Affordable Care Act; and decide how much they can do to keep their citizens insured and fed once they start losing federal assistance.
“What’s happening in Washington, D.C., is undermining everything we’ve been working on,” said Gov. Laura Kelly of Kansas, a Democrat.
State budgets have been generally strong in recent years as a result of billions in Covid-19 relief money, economic growth and a record-breaking stock market that has generated more taxes than anticipated. A robust jobs report on Thursday looked rosier than expected, in large part because gains in state and local government employment last month obscured stagnant job growth in the private sector.
Many states, both red and blue, have also enthusiastically cut taxes for residents and businesses. In the face of deep federal cuts, some states will probably be inclined to pause those reductions rather than reverse them, said Jared Walczak, the vice president of state projects at the Tax Foundation, a nonprofit tax policy group that generally favors lower taxes.
But in recent weeks, states have been balancing budgets that are fraught with uncertainties. Most state governments’ fiscal years began on Tuesday, but governors and legislators have had to keep an eye on specific provisions in the federal bill that could have outsize effects, such as a $50 billion fund for rural hospitals to offset the impact of Medicaid cuts (which was ultimately included) and the sale of millions of acres of public lands (which was not).
Now that the fine print in the president’s package is coming into focus, Carl Davis, the research director at the Institute on Taxation and Economic Policy, a left-leaning research group, said that states would have three main options for dealing with the new law.
“They can scale back their investments in health and food assistance that are directly affected by the federal legislation,” he said. “They could shuffle money around to preserve health insurance — ‘Hey, we don’t want 600,000 North Carolinians to lose health insurance, but we’re going to take money away from education to do it.’”
“Or,” he said, “we can see tax increases.”
Some states will use “a mix of all three,” Mr. Davis added.
Mr. Trump’s law includes nearly $1 trillion in cuts to Medicaid by 2034, scaling back the program that pays for the health care of roughly 78 million adults and children. It also sharply curtails federal spending on the Supplemental Nutrition Assistance Program, or SNAP, which provides monthly food assistance payments to about 42 million people.
A new requirement that Medicaid enrollees prove they are employed every six months also leaves states with the difficult task of building out software systems to track eligibility by the end of 2026. Experts said states could face software glitches that may cause delays in enrollment or leave eligible children and parents without health care.
In addition, states that run their own exchanges to sell subsidized health insurance through the Affordable Care Act will have to institute additional paperwork burdens for recipients. And states are also required to administer new SNAP work requirements.
In Georgia, which expanded Medicaid in 2023 to low-income people who could prove their employment, only 3 percent of uninsured Georgians with qualified incomes were enrolled in the program, which cost nearly $92 million, according to the nonprofit Georgia Budget and Policy Institute.
For the 40 states that expanded Medicaid to lower-income workers under the Affordable Care Act, the fate of that extra coverage has loomed particularly large.
Many states, especially those that expanded Medicaid, impose taxes on medical providers to leverage a larger federal contribution; the federal government reimburses hospitals and other providers for that tax payment, enabling the state to give much of the tax back. The new law reduces the rate at which certain states can tax providers, a big blow that will hit beginning in 2028.
Among the states that could lose more than 7.5 percent of their total federal Medicaid funding are Arizona, New Hampshire, Nevada, Iowa, Vermont, Michigan and Oregon, according to a New York Times analysis.
Still, response to the new law from governors has largely broken down on party lines.
In a statement posted on social media, Iowa’s Republican governor, Kim Reynolds, said that “public assistance should be a hand up, not a lifestyle.”
“By requiring able-bodied adults to work, volunteer, or train as a condition of receiving benefits, the bill reinforces the dignity of work,” she said.
Andy Beshear, the Democratic governor of Kentucky, predicted that the law would “devastate rural America” and that “our economy will suffer.” He called it “the worst piece of legislation I’ve seen in my lifetime.”
Elisabeth Shepard, a spokeswoman for Gov. Tina Kotek of Oregon, another Democrat, said that “just the provider assessment cuts alone” would cut more than $10 billion over 10 years from the state’s Medicaid program.
As a result, she said, “the governor is directing state agencies to urgently evaluate impacts of the federal budget to Oregon.”
In California, state officials said the law would most likely cause 3.4 million people to lose health insurance and at least 735,000 people to lose food benefits.
Rural parts of the state are expected to be hardest hit. Hospitals are scarce in the less populous parts of California, and a loss of federal funding could cause some of them to close or pare back staffing. State officials project that about 217,000 Californians will lose jobs because of funding cuts, most of them in the health care system and some of them in food distribution.
During a news conference last week, Gov. Gavin Newsom, Democrat of California, highlighted several financially distressed hospitals in Republican districts that now face even greater risk.
“They’re gutting an already vulnerable system,” he said.
It should be noted, said Mr. Walczak of the Tax Foundation, that even after January 2027, when the biggest changes kick in, states will be able to apply for extensions of up to two years to implement the Medicaid work requirements. That may limit how much states will need to scramble to address these issues immediately.
At least one Democratic governor sounded less pessimistic, at least for the immediate future. In an interview with a local television station this week, Gov. Josh Green of Hawaii, who is also a medical doctor, said he did not anticipate any hospitals closing, partly because of his own appeals to Dr. Mehmet Oz, the administrator of the Centers for Medicare and Medicaid Services, about rural health care.
“People should know we’re going to be OK,” Governor Green said. “We won’t need a special session, and I won’t have to adjust anything else right now, not the tax breaks that we’ve given to people who are struggling.” Like his Democratic colleagues, however, Mr. Green did express deep concerns that once the cuts begin to be implemented, they will hurt many of his most vulnerable constituents and likely will then threaten the nation’s rural hospitals.
Some Republican governors adopted a more wait-and-see posture, neither optimistic nor gloomy.
“It’s clear I’ve supported this legislation,” Gov. Bill Lee of Tennessee said. “America needs that. But we will look at the outcome of it when it’s finally done and determine how it impacts Tennesseans, and then the state will decide what response it has to make sure our people are taken care of.”
On Wednesday, after Vice President JD Vance cast the tiebreaking vote in the Senate, Gov. Jim Pillen of Nebraska praised the measure on social media for “supporting families, growing agriculture, extending tax cuts, preserving federal safety net programs, and strengthening our military and critical national security operations.”
On the same day, a clinic in southwest Nebraska announced that it would be closing after 30 years.
“Unfortunately, the current financial environment, driven by anticipated federal budget cuts to Medicaid, has made it impossible for us to continue operating all of our services, many of which have faced significant financial challenges for years,” said Troy Bruntz, the chief executive of Community Hospital in Curtis, a town of around 800 people, more than three hours west of Lincoln.
Physician = Health Policy Official
Physician = Health Policy Official
Your path to running for office lies ahead
Ever wonder what it takes to become a candidate for elected office and run a successful campaign? AMPAC, the political education and advocacy program of the American Medical Association, is a go-to resource for guidance and expertise. AMPIC annually hosts a Campaign School to help physicians have a greater understanding of the process and their potential and they have announced their next session scheduled for September 11-14, 2025. The program will be held at the AMA offices in Washington, DC, just off Capitol Hill.
Registration for 2025 Campaign School is now OPEN!
In pursuing elected office, running an effective campaign can be the difference between winning and losing a race. The AMA’s Campaign School is designed to provide the skills and strategic approach that are vital on the campaign trail. A solid team of political experts will share everything you need to know to position yourself for success.
"Come join me at this year’s AMPAC Candidate Workshop. I know it will be a good experience for physician legislators like me and colleagues who are dedicated to making a difference for our
profession and our patients.”
Dr. Tim Reeder, Member, NC House of Representative
Emergency Medicine Physician / ECU Emergency Medicine
Participants in the Campaign School will learn about overall strategy, voter targeting, social media as a tool, campaign ad development and more. From the expertise shared, participants will go through a team exercise of running a simulated campaign to demonstrate how the guidance shared can be put into action.
“AMPAC's Candidate Workshop provided a wealth of information that showed me how to get more involved in the political process at any level. After completing the workshop alongside like-minded physicians, I felt more prepared, more confident in my personal decision to pursue political office, and would recommend the workshop.”
Bradley Christoph, DO, MPH, MS
Family Medicine / UNC Health Caldwell Lenoir, NC
Program participants include physicians, spouses of physicians, residents and medical students, as well as state medical society staff. A typical class consists of colleagues with a span of interests, from those attracted to grassroots advocacy efforts to those looking to run for public office. As a graduate of the AMPAC program, you will not only be better positioned to pursuing your on political ambitions, but you will also be more capable of supporting candidates and their campaigns with advice on strategy, messaging and engagement.
Some key details about the program:
- Space is limited.
- The registration fee is $350 for AMA Members and $1000 for non-AMA members. The fee is waived for AMA resident and student members.
- The registration fee covers the expense of faculty, materials and all meals.
- Participants are responsible for their registration fee, travel to/from Washington, DC and hotel accommodations (the AMA will provide a list of nearby hotels within walking distance of the AMA office).
- Participants will be required to bring a laptop or Wi-Fi enabled tablet with them.
Registration for the 2025 Campaign School is now OPEN. Space is limited and the deadline to register is August 8, 2025 (or sooner if maximum capacity is reached).
For more information contact the AMA at: [email protected]
NCMS Joins Stakeholders In Backing Vaccination Against Respiratory Viruses

NCMS Joins Stakeholders In Backing Vaccination Against Respiratory Viruses
With respiratory viruses expected to surge in the fall, the North Carolina Medical Society joined 79 affiliated societies in expressing support for vaccination to protect against the flu, COVID-19 and RSV and their potentially serious complications. The NCMS and partner organizations call on insurers, hospitals, and public health agencies to ensure these life-saving vaccines remain available to patients without cost sharing.
The open letter the NCMS and other medical societies is available here.
The full text is below:
An open letter to the American people:
With the severe influenza season the U.S. experienced during the 2024-25 respiratory virus season, and the recognition that we will likely see another surge in respiratory viruses this fall, we know strong physician leadership is essential to reducing preventable illness, hospitalizations, and death. Vaccines for influenza, RSV, and COVID-19 remain among the best tools to protect the public against these illnesses and their potentially serious complications—and physicians are among the most trusted voices to recommend them. We come together as physicians from every corner of medicine to reaffirm our commitment to these lifesaving vaccines.
Recent changes to federal immunization review processes raised concerns across the medical and public health community. In this moment of uncertainty, physicians must align around clear, evidence-based guidance for patients.
We commit to working together to promote public understanding and confidence in the use of vaccines to avoid another severe respiratory virus season and resurgence of vaccine-preventable illnesses and deaths. We call on our partners—from insurers to hospitals to public health agencies—to ensure vaccines remain available to patients without cost sharing.
The health and safety of the public remains our top priority, and we will continue to support evidence-based immunizations to help prevent severe disease and protect public health.
Your continued partners in health,
North Carolina Medical Society
Proposed Federal Cuts Put Rural Behavioral Health Resources On The Line

Proposed Federal Cuts Put Rural Behavioral Health Resources On The Line
(Daily Yonder, Madeline de Figueiredo) — Ten years ago, Nancy Winmill’s son survived an opioid overdose. In her search for support, she found almost nothing available in her Burley, Idaho community.
“I had no idea what to do or where to go. I had no help. I had no resources,” Winmill said.
That experience pushed her to create what was missing: support groups, counseling, and eventually Simply Hope Family Outreach—a nonprofit for families struggling with addiction, codependency, divorce, grief, and suicide for rural southern Idaho. The organization has rapidly expanded due, in part, to funding from the Substance Abuse and Mental Health Services Administration (SAMHSA) under the Building Communities of Recovery Grant (BCOR).
“For rural communities like ours in Cassia and Minidoka counties, where access to behavioral health and recovery services is already limited, this grant has been nothing short of transformational,” Winmill said.
But now, the grant that helped build this community lifeline is on the chopping block.
The proposed FY2026 Department of Health and Human Services (DHHS) budget would cut nearly $1 billion and dozens of programs from SAMHSA following a March announcement that SAMHSA would be one of five agencies folded into a new, centralized Administration for a Healthy America. BCOR is one of the grants eliminated in the current budget proposal.
“In a region where stigma still silences many, this grant has empowered us to bring these issues into the light, and offer pathways to healing and hope,” Winmill said. “Eliminating this funding would not only stall progress, but potentially reverse hard-earned gains in recovery support for our rural neighbors.”
Rural mental health stakes
“We’re not being extremist when we say that there is a mental health crisis in rural America,” said Don Hannaford, vice president of public policy at Rural Minds, a nonprofit advocating for rural mental health equity.
Rural areas face a serious mental health care gap, with similar rates of mental illness as urban areas but nearly double the suicide rate, fewer primary care providers, and slower workforce growth. Sixty-five percent of rural counties lack a psychiatrist, 81 percent lack a psychiatric nurse practitioner, and 47 percent lack a psychologist.
Rural communities also face a 45 percent higher opioid overdose rate than urban areas, yet only 14 percent of behavioral health facilities are rural, and fewer than half treat substance use disorders.
ICYMI — Message From The President

ICYMI — Message From The President
|
||||||
DOJ Fraud Takedown – No North Carolina Physicians Among Named Defendants
 DOJ Fraud Takedown – No North Carolina Physicians Among Named Defendants
DOJ Fraud Takedown – No North Carolina Physicians Among Named Defendants
On Monday, June 30, the U.S. Department of Justice (DOJ) held a press conference and issued a press release to announce the results of its largest-ever national health care fraud takedown. The operation resulted in charges against 324 individuals with fraud allegations exceeding $14.6 billion. Charges stemmed from schemes that defrauded Medicare and Medicaid.
DOJ published a list of the 324 defendants who have been charged with Medicare and Medicaid fraud, 25 (8%) of which are physicians. Of the 14 from North Carolina or associated with illegal activity in North Carolina, none are physicians.
Below is an excerpt from the DOJ’s announcement listing North Carolina defendants and summarizing the charges against each.
Criminal Division | Case Summaries
Federal Court Eastern District of North Carolina
Kimberly Mable Sims (a lab company owner), Francine Sims Super (an office manager), and Keke Komeko Johnson (a compliance officer), were charged by information in connection with the payment of more than $1 million in illegal remunerations in the form of gift cards to patients of Life Touch, LLC (“Life Touch”), a North Carolina substance abuse treatment company, and in connection with false statements to Medicaid auditors regarding the same. The inducements resulted in more than $25 million in payments from Medicaid to Life Touch. As alleged, over four years, Life Touch, through its compliance officer and managers, routinely paid patients based upon the number of days per week that they received services. Life Touch staff also received kickbacks from a lab company that it utilized for drug testing services. The charging documents further allege that Medicaid auditors were deceived regarding these ongoing practices at Life Touch and the lab company. In addition, Super and Johnson were each charged with failure to file a tax return. Life Touch and Brandon Eugene Sims were previously charged in this case. More than $6 million in assets in the form of cash, real estate and other assets have been seized. The cases are being prosecuted by Special Assistant U.S. Attorney Tasha Gardner, and Assistant U.S. Attorney William M. Gilmore of the U.S. Attorney’s Office for the Eastern District of North Carolina.
Randal Fenton Wood, 56, of Flagler Beach, Florida, was charged by information with conspiracy to commit health care fraud in connection with a scheme to bill Medicare, the Civilian Health and Medical Program of the Department of Veterans Affairs (CHAMPVA), and other insurance programs for medically unnecessary durable medical equipment (“DME”). As alleged in the information, Wood and others partnered with purported marketing entities which solicited Medicare beneficiaries to accept durable medical equipment, such as braces and pneumatic compression devices, by illegally waiving copays and pressuring beneficiaries to accept the equipment without verifying that the equipment was medically necessary. The marketing entities sold the beneficiary information and the prefilled orders to Wood and other DME supply companies, who developed and implemented a “doctor chase” model to pressure physicians into signing or altering orders so that they could be billed in full. The DME supply companies owned by or affiliated with Wood received over $39 million in reimbursement from Medicare for DME ordered through this scheme. The case is being prosecuted by Assistant U.S. Attorney David G. Beraka of the U.S. Attorney’s Office for the Eastern District of North Carolina.
Federal Court Western District of North Carolina
Crystal Sherrell Jackson, 39, of Charlotte, North Carolina, was charged by information with health care fraud and money laundering in connection with a scheme to defraud North Carolina Medicaid by submitting fraudulent claims for drug testing and psychotherapy. Jackson, a licensed clinical addiction specialist at the time of her offenses, and the owner of Jackson Consulting Services, LLC, was an enrolled provider with North Carolina Medicaid. Jackson used her company to submit $1.9 million of false and fraudulent claims in the names of North Carolina Medicaid beneficiaries for drug tests that were not performed or were medically unnecessary, of which $1.6 million were paid. The case is being prosecuted by Assistant U.S. Attorney Michael Savage and Special Assistant U.S. Attorney Kristina Fleisch of the U.S. Attorney’s Office for the Western District of North Carolina.
Donald Calvin Saunders, 62, of Charlotte, North Carolina; Vanessa Ragin Boatright, 59, of Manning, South Carolina; Latarsa Hitchcock, 56, of Raleigh, North Carolina; Dajuan Strickland, 46, of Buffalo, New York; Cynthia Jenkins Harris, 60, of Elgin, South Carolina; Stephanie Corbett, 59, of Jonesboro, Georgia, and Karen McClary, 51, of Kingstree, South Carolina, were charged by indictment with conspiracy to defraud the United States. Additionally, Saunders, Boatright, Strickland, and Jenkins were charged with health care fraud; Saunders, Boatright, and Strickland were charged with purchasing and selling Medicaid numbers without lawful authority; Saunders, Boatright, Strickland, and Jenkins were charged with conspiracy to commit money laundering; and Saunders and Strickland were charged with money laundering, all in connection with a $21 million scheme in which behavioral health providers in North Carolina submitted false and fraudulent claims to the South Carolina Medicaid program for services that were not performed. David Cory Hill, 54, of Charlotte, NC, was charged separately in an information with conspiracy to defraud the United States and commit offenses against the United States and money laundering. As alleged in the indictment, Saunders, Boatright, Hitchcock, Strickland, and Hill would set up or acquire behavioral health care companies and enroll them with South Carolina Medicaid under a program in which beneficiaries could select providers within 25 miles of South Carolina. Saunders and his conspirators used companies under their control to submit thousands of claims for behavioral services that were not provided. Jenkins, a former state of South Carolina employee, used her consulting firm to obtain the credentials of licensed professionals needed to bill South Carolina Medicaid and to create false clinical notes in the event of an audit. Corbett, who operated a third-party medical billing service, submitted false claims to South Carolina Medicaid, for which she was paid for each successful claim. McClary, a social worker with access to Medicaid beneficiary information, sold Medicaid beneficiary names and numbers to the conspirators, for which she was paid $200 to $300 for each eligible beneficiary. The case is being prosecuted by Assistant U.S. Attorneys Michael Savage and Graham Billings of the U.S. Attorney’s Office for the Western District of North Carolina, with substantial assistance from the South Carolina Attorney General’s Office, Medicaid Fraud Control Unit.
Federal Court Eastern District of Virginia
Lori Adcock, 54, of Hampstead, North Carolina, was charged by complaint with conspiracy to commit health care fraud in connection with a scheme to overcharge Medicaid for environmental modifications to homes or vehicles such as installing wheelchair ramps or grab bars in showers, which scheme cost Medicaid approximately $213,210.69 attributable to Adcock. As alleged in the complaint, Adcock was the operations manager of Ability Unlimited, a Medicaid provider whose business centered on facilitating but not performing environmental modifications, and Medicaid did not allow facilitators that performed no actual labor to charge a separate profit margin. Adcock was the manager of the fraudulent scheme to hide Ability Unlimited’s arbitrary and often exorbitant profit margins in the subcontractor costs. For example, Ability Unlimited purchased a generator from Amazon.com for less than $1000 and had it shipped directly to the Medicaid recipient, but charged Medicaid $3,395.16, listing the generator cost in an altered invoice as $2,610.16, and including an additional labor cost of $785 despite the direct shipment of the generator. The case is being prosecuted by Assistant U.S. Attorney Shea Gibbons of the U.S. Attorney’s Office for the Eastern District of Virginia.
NCMS to Congress: Protect Medicaid, Reform Medicare Payment ... Help North Carolina

NCMS to Congress: Protect Medicaid, Reform Medicare Payment ... Help North Carolina

The President's tax bill, H.R. 1 / One Big Beautiful Bill, which passed both the US Senate and US House and signed into law on July 4th, has drawn considerable attention since it was introduced on May 20, 2025. The bill was presented to Congress to make tax cuts enacted in 2017 permanent, while also introducing new tax considerations. It includes tax cuts for individuals and businesses and offsets the cost of the cuts through measures that will impact Medicaid, Supplemental Nutrition Assistance Program (SNAP), the ACA Insurance Marketplace, and Student Loans.
On and encouraging note, the legislation includes a positive adjustment to Medicare physician payment though not to the extent that the NCMS and other physician organizations have advocated for. In 2026, payment will increase 2.25%.
Since the first of the year, when anticipation of H.R. 1 took center stage, the NCMS has remained in contact with our fourteen US House and two US Senate offices. Over the course of six months, 75+ meetings on Capitol Hill and many communications, concern has been shared over the projected loss of coverage and care for Medicaid beneficiaries. A key point of emphasis has focused on the resulting threat of Medicaid expansion ceasing due to an automatic “trigger” provision which eliminates the program in the event the existing funding formula is changed.
NCMS appeals to Congress
In the lead up to final action on H.R. 1 and in follow-up to earlier communications, the NC Medical Society issued appeals to each of our state’s members of the US Senate and US House outlining concerns over the impact of H.R. 1. Below are links to the text of each of those letters.
Message to North Carolina members of the US Senate
Message to North Carolina members of the US House
We know that many NCMS members have reached out to their members of Congress on this issue. Those calls and emails are appreciated and have helped elevate our collective voice on behalf of patients and the medical profession.
As the impact of H.R. 1 is assessed, the NCMS will continue to engage with elected officials, both at the state and federal levels, to preserve and promote coverage and care for our state’s citizens.
Do you know your state and federal legislators?
More importantly, do your legislators know you?
Be a key contact for your legislators
ECU Graduate, Deallaney Hudson, Continues To Defeat More Odds Through ECU Health Internship

ECU Graduate, Deallaney Hudson, Continues To Defeat More Odds Through ECU Health Internship
(WITN, Merit Morgan) — The inspiring story of East Carolina University graduate Deallaney Hudson is one WITN has been following for months.
Hudson has faced uncertainty since her birth and the diagnosis of Neonatal Progeroid Syndrome, a rare disorder characterized by accelerated aging.
Following her graduation from ECU on May 9th, she started an internship at ECU Health Medical Center in pediatric inpatient rehabilitation.
“I just love being able to provide fun activities while also helping them,” Hudson told WITN.
She says her love for the medical field stems from a long medical background. “I have a huge medical background, and things are going on with me. I’ve been in and out of the hospital my whole life, so basically, I received recreational therapy services when I was a patient, and that sparked my interest.”
The past few months of her life have been busy yet exciting.
“I graduated from ECU on May 9th, and I started here on May 12th, so I didn’t have a lot of turnaround time, but I will say, I was very exhausted the first few weeks, but it’s been really good. I’ve learned so much, and I’m so thankful that I was able to get this internship,” Hudson said.
Kristen Jones, an ECU Health Recreational Therapist, says Hudson’s story is inspiring to see.
“She’s been a wonderful student. We’ve been very surprised by the caliber of the student that she is, just coming in and starting, so we’ve been very happy to see that. Deallaney has a passion that other students don’t have, just coming from her background in being in rehab, and I think that helps her to connect with our patients a lot more,” Jones told WITN.
Though it hasn’t been easy along the way, Hudson says she’s encouraged by all she’s overcome. “A lot of kids go through the ‘I want to do this or that’ so for me, it was PT, OT, then I wanted to be a surgical tech but I quickly realized my physical strength limited me in doing those things so I looked into recreational therapy and that’s what I started. I was a patient here about 9 months ago, so it’s different being on the patient side vs. the therapist side. I think I’d much rather be on the therapist side of things.”
As she moves forward into her future, she encourages others to believe in themselves, too.
“Never let anything hold you back. Go after whatever you hope and dream for, and just do big things and set your mind to whatever you want to do,” Hudson said.
Jones says her hope for Hudson is to continue growing and learning different skills in the recreational therapy field.
Hudson’s internship ends August 15th.
She says her next steps include getting certified as an RT and then searching for a job.
Duke Regional Hospital Gets Top Rank In National Survey

Duke Regional Hospital Gets Top Rank In National Survey
(Business North Carolina, David Mildenberg) — Duke Regional Hospital ranked No 1 in social responsibility in a national survey of nearly 2,700 acute-care hospitals, marking the third straight year the Durham hospital has received the top honor.
The survey by the Needham, Massachusetts-based Lown Institute looks at data from various sources related to equity, value, and patient outcomes. Duke Regional, which is part of Duke University’s healthcare system, was one of 27 N.C. hospitals achieving an “A” grade for social responsibility; there are 77 acute-care hospitals in the state.
“It’s an amazing testament to our team. This is not just a `Gosh we think we’re doing a good job’ thing,” says Jason Carter, president and chief operating officer of Duke Regional Hospital. “To be recognized says a lot about Duke Regional and the work that we do in the community.”
Two other N.C. hospitals ranked in the top 100: Hoke Hospital in Raeford was 40th, while Sentara Albemarle Medical Center in Elizabeth City was 75th.
Duke Regional’s community investments include $10 million in direct and in-kind resources to Durham’s Lincoln Community Health Center, which provides care to underserved patients. Carter credits the hospital’s effort to “get people in the hospital for the shortest amount of time and with the best care,” and then reduce readmissions, as keys to Duke Regional’s success.
The 388-bed hospital was formed in 1976 through the merger of Lincoln Hospital, which mainly served Black citizens, and Watts Hospital, which catered to white people. Durham County ran the hospital until 1998, when Duke University signed a management contract. In 2013, the hospital was renamed Duke Regional Hospital.
The Lown Institute is a nonpartisan think tank advocating for equitable, affordable health care.
Data sources for the ranking include claims to Medicare and Medicare Advantage; datasets on patient safety, patient experience, and hospital costs provided by the Centers for Medicare and Medicaid Services; and information from the Internal Revenue Service.
Carter joined Duke Regional about 18 months ago after previously working for the University of Maryland Health System, Wake Forest Baptist Health, Novant Health and ECU Health.
Kyphoplasty Turned Runner’s Back Injury Into Comeback

Kyphoplasty Turned Runner’s Back Injury Into Comeback
(Novant Health, Carole Tanzer Miller) — When David Freeze recently took the baton in a Southwest relay to run a leg that gained more than 1,150 feet in elevation over a scant 3.4 miles, it was just his latest uphill battle to conquer.
The 72-year-old distance runner and cross-country cyclist spent the past year recovering from a catastrophic back injury suffered while trimming trees on his farm in China Grove, North Carolina, about 35 miles north of Charlotte. Freeze was 12 feet up in the bucket of a front-end loader when he was suddenly tossed in the air as the driver backed up.
"I went flying over the back of the bucket, hit my head on a bar that runs back there, and then landed right just about on my lower back," he recalled. "As soon as I landed, I knew I was in big trouble."
 Freeze's return to the Reno-Tahoe Odyssey, a little more than a year after breaking his back, was made possible by a minimally invasive operation performed by spine surgeon and NC Spine Society member Dr. Gene Eline of Novant Health Orthopedics & Sports Medicine - Manning Park.
Freeze's return to the Reno-Tahoe Odyssey, a little more than a year after breaking his back, was made possible by a minimally invasive operation performed by spine surgeon and NC Spine Society member Dr. Gene Eline of Novant Health Orthopedics & Sports Medicine - Manning Park.
The outpatient procedure — called balloon kyphoplasty — repaired two compression fractures (see more on this below) in Freeze's spine in just about an hour's time. Within weeks, he was on the run again.
Freeze, who writes a column in the Salisbury Post called "Gotta Run," had good odds for success, Eline said. Unlike many patients his age, his bones were strong.
"He was also in shape, not obese and was motivated — extremely motivated — and was willing to undertake certain risks because of the kind of activities and goals he had," Eline said.
Simply put: Freeze couldn't imagine his life without biking and running. His cross-country cycling adventures have been chronicled in many of his 10 books, and after almost 50 years of running and 24 marathons, he was on the verge of a much-anticipated milestone.
Metal rods and pins? No.
The fall put it all at risk. One of his fractured vertebrae — T12 in the lower back — would be a relatively routine repair. But the other — L3 a little farther below — was not only severely compressed, it was also fragmented. Because it had almost burst, fixing it was no sure thing, and Eline didn't mince words about the risk.
"I told him you may have 100% success, or you may get no relief whatsoever," he said. "And then, we'd have to go back in … and put metal rods in your back."
That was the last thing Freeze wanted to hear.
Metal rods were exactly what doctors recommended at the trauma center (not part of Novant Health) where Freeze was taken after his accident. He had been in the emergency room for hours, unsure of his status, when a doctor on duty recognized him as an old family friend.
He reviewed Freeze's chart and told him he was headed for the operating room come morning. Surgeons planned to fix the fracture with rods and pins, an appropriate but potentially life-changing treatment for his injury.
"He told me, 'Nothing will be the same about your life if they put a rod on each side of your spine and a bunch of pins to hold it in place. You'll have no mobility,' " Freeze recalled.
When morning came and Freeze was asked to OK the spinal fusion, he got straight to the point: Would he still be able to cycle and run after the surgery?
"The doctor said, ‘No … nothing like that ever again,' " Freeze recalled. He'd have to scale back on heavy lifting around the farm, too. "Well, then," Freeze responded, "I don't want it."
Back surgery recommendation: Kyphoplasty
Three days later, he headed home in a back brace, and drawing on his expertise as a fitness coach, would soon embark on a do-it-yourself rehab regimen.
He started slow, walking his gravel driveway from end to end and back again — about 0.2 mile in all — with his nephew carrying a chair alongside, just in case. A day later, he did it twice. And within six weeks, Freeze was cutting the lawn, leaning on his sturdy, professional mower for support.
"I ended up mowing 3.2 miles," Freeze said. "So I began walking, and I worked my way up to 5 miles."
One day, a fellow member of the Salisbury Rowan Runners club and doctor of physical therapy told him about kyphoplasty, a treatment to stabilize compressed bone that was less likely to limit his activity. Word-of-mouth and Google led him to Eline.
But Freeze wasn't over the finish line yet: His insurer put one final hurdle in his road to recovery, refusing to cover the procedure. He felt so strongly that kyphoplasty was his key to an active life that he was willing to pay out of pocket and made a $6,000 down payment.
Five months after his accident, he was finally on the calendar for back surgery at Novant Health Wilson L. Smith Outpatient Center in Salisbury.
On operating day, Freeze was in and out in roughly three hours and walked to his car afterward on his own power. Concerned about risking the tricky L3 repair, Eline told Freeze to keep moving but not to run until his next visit.
"I waited till two days before the appointment, and then I went to a flat part of the road here, close to the farm and ran a half-mile just like any other time," he recalled. "There was no pain. I was in tears then, and I'm a little bit in tears telling about it now."
Hitting the 100,000-mile running mark
A year after his fall, Freeze runs 4 to 6 miles a day and thanks God for steering him to Eline.
Recent imaging shows that the repair is not only holding, but that bone is starting to grow around it, the best possible outcome. "It should be a permanent repair," Eline said.
On April 18, less than a year after his injury, David Freeze reached the milestone he'd chased since the 1970s. With his 5-year-old granddaughter, Monroe Bishop, running at his side for the last half-mile, he hit the 100,000-mile mark.
What is balloon kyphoplasty?
Balloons and cement are a 21st-century surgical treatment for compression fractures of the spine.
The treatment is called balloon kyphoplasty, (pronounced ky-PHO-plasty) and Dr. Gene Eline of Novant Health Orthopedics & Sports Medicine - Manning Park in Salisbury, North Carolina, has performed hundreds of these outpatient procedures in more than 20 years of spine surgery.
Compression fractures occur when all or part of a vertebra collapses, often due to the bone-wasting disease osteoporosis. Simply put, balloon kyphoplasty restores the integrity of the fractured vertebra, allowing for pain-free movement.
It's performed with the patient under general anesthesia. Continuous X-ray imaging lets the surgeon view the vertebrae from front-to-back and side-to-side.
To begin, tiny incisions are made on either side of the spine. Roughly the size of a No. 2 pencil (about 1/10 inch), these allow for insertion of a hollow tube called a cannula through which the operation is performed.
Using a tiny drill, the surgeon enters the bones and clears away any fragments. A balloon is then threaded through the cannula, placed into the vertebra, and inflated to get the bones back in place. The space created is then filled with a quick-hardening liquid cement that solidifies the bone and prevents it from further collapse.
Once the patient is awake and the anesthesia has worn off, they can get up — and go. They're usually directed to take things slow but keep moving. Stitches are typically removed about two weeks later.
"By the next morning, most patients notice a substantial improvement in their condition," Eline said. "Typically, no physical therapy is needed."
But, he added, each patient is different. This procedure is not for every spinal condition. It is only used to treat compression fractures, which are typically caused by severe osteoporosis or spinal tumors.
Child Visiting NC Diagnosed With Measles As Vaccination Rates Decline

Child Visiting NC Diagnosed With Measles As Vaccination Rates Decline
(WFMY 2, Ben Briscoe, Madelyn Ricket) — The state health department confirmed a child visiting Guilford and Forsyth counties has the measles.
This case comes as a growing number of parents across the country and here in North Carolina decide not to vaccinate their kids for the Measles.
WFMY News 2's Ben Briscoe dug into CDC records and found the percentage of unvaccinated kids in North Carolina has tripled over the past 15 years.
It's gone from less than 1% in 2011 to almost 3% of students now.
Doctors said it's those unvaccinated kids who are most at risk.
"Measles is one of the most contagious infectious diseases we know of," said Dr. Loryn Dass with Cone Health.
"It can live in the air for two hours. So if someone walks into a room with measles breathing and you walk in 2 hours later, you are exposed," said Dr. Nicholas Preziosi with Novant Health.
Doctors said measles starts with a fever and a runny nose.
The virus causes rashes across the body, attacks white blood cells, and weakens the immune system.
If untreated, it can turn deadly.
"The risk of developing what we call encephalitis or inflammation in the brain. Um, and the concern with that is that there can be permanent brain damage from that, and children can also die as a result of those complications," said Dr. Dass.
Scary stuff, but here's what can calm us down a little bit: kids who are vaccinated have a 97% protection rate against the measles, so they are likely to be just fine.
And that protection lasts for your entire life, so it also goes for adults who got the vaccine a long time ago.
UNC Study Shows Promise for Patients Who Struggle to Manage Type 2 Diabetes

UNC Study Shows Promise for Patients Who Struggle to Manage Type 2 Diabetes
(UNC Health Care, Brittany Phillips) — One of the biggest struggles for people with type 2 diabetes is to manage blood glucose levels to the general target of less than 7% on the A1c test. About half of people with type 2 diabetes do not achieve an A1c less than 7.5%, even though many are treated intensively with substantial lifestyle efforts and multiple medications. The effects can lead to many people developing complications of diabetes over years.
In Phase 1 of the CATALYST study, research led by John Buse, MD, PhD, director of the University of North Carolina’s Diabetes Center, revealed that nearly 1 in 4 people with difficult to control diabetes had hypercortisolism – a condition characterized by abnormally high levels of the hormone cortisol in the body.
Now, new findings uncovered in Phase 2 of the CATALYST study suggest the use of the drug mifepristone (brand name Korlym) can help lower blood glucose levels and weight of type 2 diabetes patients who have hypercortisolism.
The new results showed that patients treated with mifepristone had a 1.5% reduction in A1c, on average nearly to the target of 7%. The reduction was much greater than with placebo or inactive tablets. This outcome occurred despite many patients on mifepristone decreasing or even stopping other diabetes medications, including insulin. In addition, research indicated this A1c reduction was also associated with weight loss and reduction in waist size.
“This is proof of a new paradigm in diabetes care, and this is an example of precision, targeted care,” said Buse. “If you treat the hypercortisolemia, you may benefit many processes beyond A1c and weight loss. The second phase of this trial indicates that with more study and greater art in practice, cortisol-directed therapy in difficult-to-control diabetes will be transformational in diabetes care practices and people’s lives.”
Phase 2 study results were presented today at the American Diabetes Association 85th Scientific Sessions.
'They Can Just Be Kids': Summer Camps in ENC Provide Refuge For Pediatric Patients

'They Can Just Be Kids': Summer Camps in ENC Provide Refuge For Pediatric Patients
(Reflector, Kim Grizzard) —The room grew quiet Thursday when Tamika Mackey interrupted a craft activity for pediatric hematology and oncology patients to announce that someone needed to get a few shots.
Nevah Hill stopped coloring and sat wide-eyed, worried about what might come next. The 7-year-old’s smile returned when she learned that these were camera shots, not the kind that come from a needle.
“All our sickle cell kids, they have to get blood drawn every time they come to the clinic,” said Mackey, a child life specialist serving children with cancer, hemophilia and sickle cell disease at a clinic at East Carolina University’s Brody School of Medicine.
But for five days in June, patients like Nevah had nothing to dread. Instead of appointments at the clinic, there were activities at a camp where fun and games were just what the doctor ordered. For more than 30 years, Camp Rainbow and Camp Hope have been the best medicine.
“The kids get to focus on being kids and not going to the clinic,” said Craig Harper, who has volunteered at the camps for the last decade. “They get to forget about some of their daily world.
“Some kids have never fished,” he said last week as he helped to bait hooks for campers waiting to cast a line at the camp near Ayden. Harper remembers similar firsts from camp during his childhood. He spent four summers going to Camp Hope with his sister, who had sickle cell disease.
Back then, both programs took kids to Camp Don Lee in Arapahoe, some 65 miles from ECU Health Medical Center. But in 2024, the camps moved about 50 miles closer. Today, dozens of kids and teens facing health challenges find sanctuary at a place called The Refuge.
“We switched to The Refuge because it’s closer,” said Mackey, who serves as camp director. “If a child was at camp and we needed to take them back to the hospital, versus riding an hour and a half, we’re only 20 minutes to 25 minutes up the road.”
Just 14 miles from Maynard Children’s Hospital, The Refuge seems a world away. Campers bunk in repurposed farm houses, some more than a century old, and enjoy modern-day attractions including an aqua park and a ropes challenge course. On hundreds of acres in rural Greene County, kids and teens spend their days singing and swimming, going hiking and horseback riding, practicing art and archery. But along with those rites of passage of camp comes medical monitoring provided as a protection for young patients.
“We pack a mini-hospital,” said nurse Kathy Barnhill, who has worked a week at camp for the last three summers. “I think it gives the parents a sense of peace to know there’s a doctor there, there’s a nurse there. They’re going to get their medicine. They’re safe, and at the same time, they can just be kids.”
Physicians take turns making the rounds at camp, where at least one doctor is always on duty. Like Barnhill, Mackey arrives on Sunday and stays until the last camper heads home. She has served as co-director of the camps since 2016 and took the lead this year following the retirement of Jacquelyn Sauls. A child life specialist for nearly 40 years, Sauls was instrumental in helping the camp go from a one-day outing to a local park to a weeklong experience for children.
“She (Sauls) was in the ground work of it,” Mackey said of Camp Rainbow, which opened for cancer patients in 1982. Camp Hope, for children with sickle cell disease, got its start a little more than a decade later. “Camp was her baby.”
By the early 2000s, the two camps were meeting together as one, although campers spend much of their time in groups of children who share the same medical conditions.
Those common experiences are among the welcome aspects for campers like Lawsen Ziemba of Greenville, who attended for the first time this year. Lawsen, 12, was diagnosed with leukemia in early childhood.
“People with other cancers are here, too,” he said. “It’s pretty neat that you can get the perspective from other people that have gone through the same thing you have and have a relationship with them about what you have gone through.”
Heaven Glaspie knows what many of these campers go through. Glaspie, 23, is a sickle cell patient who started out as a camper at age 8.
“Just being in each other’s presence at camp … just being able to bond with your friends that also have similar things going on as you is really one of the best things about it,” he said.
When Glaspie aged out of the program, he returned as a volunteer, serving as a counselor for other kids with sickle cell disease.
“Being able to relate to the kids and help them out, I feel like it’s a gift because not a lot of people can relate,” he said. “Also the smile on their face that they give you when they’re having the best time of their life at camp is very heart-warming.”
Volunteers like Glaspie serve alongside The Refuge camp staff members, meaning that sometimes there are nearly as many adults as campers. Staffers from The Refuge lead daily devotion times, engaging children in songs and Bible lessons.
“Our purpose is to share and model the hope of Jesus,” Executive Director Sammy Hudson said. “When we see kids that are battling really hard things, it brings to light the importance of what we do even more and it gives us greater purpose in what we do.
“These kids are really resilient. They just want to be kids,” he said. “They are full of life and that’s fun to see.”
Hudson said health care staff members and other Camp Rainbow and Camp Hope volunteers have shown a dedication that goes beyond campers’ medical needs, from dealing with discipline issues to tucking them into bed at night.
“It’s great to work with the team of people that put this together because they truly care,” he said. “They care about these kids.”
For Mackey, whose work involves helping support kids through their medical treatment, camp presents a different set of challenges, such as overcoming fears of going under water. But it requires the same kind of calm reassurance and encouragement.
“Some kids were kind of scared to do it, but they faced their fears and they did it,” Mackey said. “It was good to watch them (go from) ‘No, I’m not doing that’ to putting their head in the water.
“Some things they’ve never tried before,” she said. “They may be a little reluctant at the beginning, but the counselors work with them. Whatever challenges we come across, we help them through it.”
Alert - Medicare Fraud Scheme

Alert - Medicare Fraud Scheme
The Center for Medicare and Medicaid Services (CMS) has issued an alert for all Medicare providers. CMS has identified a fraud scheme targeting those enrolled as Medicare providers as well as Medicare suppliers where scammers are impersonating CMS. The fraudulent ploy includes a phishing fax request for medical records and documentation, falsely claiming to be part of a Medicare audit.
CMS does not initiate audits by requesting medical records via fax. You are advised to be alert ant to protect all records. If you receive a suspicious request, you should not respond. If you feel you received a fraudulent request, you are encouraged to work with your Medical Review Contractor to confirm its validity.
New Research: Diabetes Medication Shows Promise In Cutting Migraine Days By More Than Half

New Research: Diabetes Medication Shows Promise In Cutting Migraine Days By More Than Half
(News Medical, European Academy of Neurology Congress 2025) — A diabetes medication that lowers brain fluid pressure has cut monthly migraine days by more than half, according to a new study presented today at the European Academy of Neurology (EAN) Congress 2025.
Researchers at the Headache Centre of the University of Naples "Federico II" gave the glucagon-like peptide-1 (GLP-1) receptor agonist liraglutide to 26 adults with obesity and chronic migraine (defined as ≥15 headache days per month). Patients reported an average of 11 fewer headache days per month, while disability scores on the Migraine Disability Assessment Test dropped by 35 points, indicating a clinically meaningful improvement in work, study, and social functioning.
GLP-1 agonists have gained recent widespread attention, reshaping treatment approaches for several diseases, including diabetes and cardiovascular disease. In the treatment of type 2 diabetes, liraglutide helps lower blood sugar levels and reduce body weight by suppressing appetite and reducing energy intake.
Importantly, while participants' body-mass index declined slightly (from 34.01 to 33.65), this change was not statistically significant. An analysis of covariance confirmed that BMI reduction had no effect on headache frequency, strengthening the hypothesis that pressure modulation, not weight loss, drives the benefit.
"Most patients felt better within the first two weeks and reported quality of life improved significantly. The benefit lasted for the full three-month observation period, even though weight loss was modest and statistically non-significant."
Dr. Simone Braca, lead researcher
Patients were screened to exclude papilledema (optic disc swelling resulting from increased intracranial pressure) and sixth nerve palsy, ruling out idiopathic intracranial hypertension (IIH) as a confounding factor. Growing evidence closely links subtle increases in intracranial pressure to migraine attacks. GLP-1-receptor agonists such as liraglutide reduce cerebrospinal fluid secretion and have already proved effective in treating IIH. Therefore, building on these observations, Dr Braca and colleagues hypothesised that exploiting the same mechanism of action might ultimately dampen cortical and trigeminal sensitisation that underlie migraine.
"We think that, by modulating cerebrospinal fluid pressure and reducing intracranial venous sinuses compression, these drugs produce a decrease in the release of calcitonin gene-related peptide (CGRP), a key migraine-promoting peptide", Dr Braca explained. "That would pose intracranial pressure control as a brand-new, pharmacologically targetable pathway."
Mild gastrointestinal side effects (mainly nausea and constipation) occurred in 38% of participants but did not lead to treatment discontinuation.
Following this exploratory 12-week pilot study, a randomised, double-blind trial with direct or indirect intracranial pressure measurement is now being planned by the same research team in Naples, led by professor Roberto De Simone. "We also want to determine whether other GLP-1 drugs can deliver the same relief, possibly with even fewer gastrointestinal side effects", Dr Braca noted.
If confirmed, GLP-1-receptor agonists could offer a new treatment option for the estimated one in seven people worldwide who live with migraine, particularly those who do not respond to current preventives. Given liraglutide's established use in type 2 diabetes and obesity, it may represent a promising case of drug repurposing in neurology.
Carolina SeniorCare Helps Residents in Seven NC Counties Age At Home

Carolina SeniorCare Helps Residents in Seven NC Counties Age At Home
(The Sun Journal, Caramia Valentin) — Carolina SeniorCare-East, an EveryAge Program, is now open and serving seniors ages 55 and older in seven area counties.
Carolina SeniorCare, located at 3681 Neuse Blvd. in New Bern, provides the Program of All-inclusive Care for the Elderly, also known as PACE.
The provider-based health plan helps provides people with access to services they need without moving out of their homes.
PACE programs provide comprehensive medical, preventative and social services, supported by the Centers for Medicare and Medicaid Services and the N.C. Department of Health and Human Services.
The program focuses on prevention, wellness and a commitment to enhance the quality of life for seniors and their families through care and support.
Carolina SeniorCare-East will serve seniors ages 55 and older who live in Beaufort, Carteret, Craven, Jones, Lenoir, Onslow and Pamlico counties. Those within the service area who qualify by the North Carolina Medicaid Agency as eligible for nursing home care can join the program.
Lee Syria, president and chief executive officer of EveryAge, said EveryAge has a rich history of more than 50 years of providing care and services for older adults.
Syria said that by expanding Carolina SeniorCare into eastern North Carolina, EveryAge continues to build on its mission to provide vibrant living, compassionate services and diverse outreach programs.
“The PACE program is filling a need in the community by providing the opportunity for a person to remain in their home longer while receiving the necessary care and services,” she said. “We are grateful for the outpouring of support that has been shown by the city of New Bern and the wider community, along with the health care providers in the area who are working closely with us to provide the services needed for the participants.”
The services Carolina SeniorCare-East provide include physician care, nursing services, vision care, dental care, physical therapy, occupational therapy, speech rehabilitation therapy, prescription drugs, preventative services, preventative education, laboratory services, diagnostic testing, recreational activities, nutritional counseling and meals, transportation, home health care and personal care.
Mayor Jeffrey Odham said the city appreciates the investment.
“In New Bern, we don’t lack for ideas,” he said. “Everybody would like to see Krispy Creme or Cracker Barrel and we love those things, we want them to come here as well, but what’s so special about this facility is that it actually meets a need.
“We don’t necessarily need those restaurants. They’re certainly nice to have, but this is something in our community that is a need.”
Kevin Roberts, president and chief executive officer of the New Bern Area Chamber of Commerce, agreed that the services will benefit the city and area residents
“This is such a special facility but also, the services that come out of this facility, are so important for our market,” Roberts said.
The facility has a large adult day health center, where participants can mingle and participate in various activities Monday through Friday.
Carolina SeniorCare-East provides wheelchair-accessible transportation, a registered dietitian and meals for its participants.
There is also a room with cardio machines and other equipment that provide occupational therapy and physical therapy. The room is complete with a staged bedroom and bathroom to help people practice mobility skills inside a home setting.
A sensory room at CarolinaSenior Care-East is a safe space for people to relax with comfortable chairs, dim lighting and white noise machines.
Participants also have access to a secure outdoor space and an on-site medical facility. The care team includes doctors, nurses, therapists, pharmacists, social workers and personal care aides.
Carolina SeniorCare-East also provides in-home services including health care, personal care, homemaker services and routine chores.
People who qualify for Medicare can receive some of the services at no cost. Those who also qualify for the North Carolina Medicaid program receive the long-term care portion of the PACE benefit at no cost or with a small monthly payment.
Those with an income over the Medicaid threshold may still be eligible to participate in the program by paying a premium or patient monthly liability, which is based on the individual’s assets and income.
Those who only qualify for Medicare can receive services by paying a set monthly fee.
Sabrena Lea, deputy director of long-term services and support for North Carolina Medicaid, said PACE is the state’s oldest managed care model.
“(With this facility) we moved the needle toward the manifestation of an actual person-centered practice that strikes the balance between what is important to an individual with what is important for them,” Lea said. “Your mission statement of honoring the past, celebrating the present and embracing the future reminds us it is possible to serve people with dignity in the settings of care.”
For more information about Carolina SeniorCare visit CarolinaSeniorCare.org.
Duke Researchers: Severe Heat is Here! Learn What’s Important for Living Under Dangerous Conditions

Duke Researchers: Severe Heat is Here! Learn What’s Important for Living Under Dangerous Conditions
(Duke Today, Ashley Ward) — Plus: Duke guidelines on working outside in severe heat
It’s going to be blazing this week, as what meterologists call “a heat dome” settles in across the country, putting some 200 million Americans at risk for severe heat.
Forecasters predict 100 degree temperatures in the Triangle for three consecutive days, before thunderstorms might slightly cool temperatures late Thursday and Friday. Overnight temperatures will be in the mid to high 70s for several days. Humidity is also expected to be high.
This is a template for dangerous conditions for humans, particularly those working outside for any extensive amount of time, and a good moment to recall that heat is the number one weather-related killer in the United States. The range of heat-related illnesses includes heat cramps, heat exhaustion and heat stroke – and heat can also strain many other systems within the body, exacerbating other health conditions.
But Duke experts at the Nicholas Institute for Energy, Environment & Sustainability have advice for surviving severe heat. In a short video, Ashley Ward, director of Duke’s Heat Policy Innovation Hub, provides 10 tips for protecting yourself from heat-related illness.
Cooler evenings are essential for the body to recover from the stresses of daytime severe heat. “Your body needs a reprieve,” Ward told the Associated Press last week. “You don’t get that overnight, we start the next day at a deficit.”

When overnight temperatures do not drop below 75 degrees, she said, “you start to see some pretty extraordinary outcomes with respect to heat illness and heat stroke, and even mortality.”
While there is still much to understand about severe heat and its impacts on the body, research has grown significantly this past decade. Duke researchers from across the university are contributing to analysis of heat’s impacts on human health and the economy – as well as potential solutions. Ashley Ward and the Heat Policy Innovation Lab have received national attention for work advising decisionmakers in government, the private sector and civil society.
One of Ward’s messages is that 2025 will bring the coolest summer of the remainder of our lifetimes. The trend toward a warming climate isn’t going to be changing anytime soon.
She advises that people start dealing with heat as a year-round, long-term effort rather than reacting to it as it arises. “Government, companies, and community organizations must start working together on developing the strategies, tools, and partnerships needed to reduce heat exposure and enhance resilience,” Ward explained in an interview with Duke Today. “Through the hub, Duke is helping catalyze promising collaborations to effectively protect people and the economy.”
The hub is working on this challenge at the national and international levels — as well as locally. For example, in 2024, the hub partnered with state agencies to release a Heat Action Plan Toolkit featuring a template that each of North Carolina’s 100 counties can customize to fit their specific needs and circumstances.
The toolkit also includes outreach resources for communities, as well as recommended actions for health care staff and local leaders when extreme heat is in the forecast.
In 2025, the hub helped state agencies improve the precision of the North Carolina Heat Health Alert System, which citizens, local businesses and government officials can use to assess heat’s localized risks to health.
Outdoor Work at Duke
Managing heat is a top priority for Duke Facilities and other university units where employees are working outside. The university also collaborates with independent contractors to take similar steps to protect workers doing construction and other outdoor activities.
Here are key points of Duke Facilities heat guidelines:
• We adjust schedules so teams can arrive earlier, allowing them to start and finish their workday sooner
• Employees have the freedom to evaluate their own needs regarding extreme heat
• We supply water and ensure access to indoor break room facilities where employees can complete safety training or fulfill other indoor responsibilities
• Managers remain attentive to ongoing work and focus on scheduling the more demanding tasks during the cooler, earlier hours of the day
• Our outdoor employees possess a heightened awareness of their limits, enabling them to better recognize when to hydrate, take breaks and effectively manage the heat.

New Atrium Health Hospital Set To Open July 1

New Atrium Health Hospital Set To Open July 1
(WCNC, Hank Lee) — Atrium Health Lake Norman, the Charlotte area's newest hospital, will open its doors to patients on July 1, Atrium Health announced.
Located near Lake Norman between Huntersville and Cornelius, Atrium Health Lake Norman offers state-of-the-art technology and care for patients in northern Mecklenburg County and surrounding areas. Atrium Health announced the new location in 2021 and broke ground on the facility in 2023.
“The population of the Lake Norman region is growing rapidly, and the demand for high quality care is growing right alongside it,” Eugene Woods, the CEO of Atrium's parent company Advocate Health, said. “Now, this community will have access to comprehensive care at a new, state-of-the-art hospital closer to home — improving lives and contributing to the vibrant future of Lake Norman.”
The 200,000-square-foot hsopital includes a brand-new emergency department, as well as an advanced labor and delivery floor. Specialty services located on-site include Atrium Health Musculoskeletal Institute, cardiovascular services, One Health OB-GYN services and concierge medicine.
“This hospital was designed with community at the heart,” facility executive Brian Wofford said. “From the layout of patient rooms to the healing garden, every detail reflects our commitment to the healing journey and providing the best possible care for this community.”
UNC School of Medicine OBGYN is Making Pregnancy Sonograms More Accessible

UNC School of Medicine OBGYN is Making Pregnancy Sonograms More Accessible
(UNC, Alyssa LaFaro) — When Dr. Jeffrey Stringer was in the middle of his medical program at Columbia Presbyterian Hospital in the mid-1990s and distraught at the death of a patient, his chief resident led him away from the deathbed to another part of the hospital: the nursery.
“It was a circle of life moment,” Stringer says. “It was so renewing to see new life. And I decided I’d rather be on that side of medicine.”
He’s now an OB-GYN and the Clarke-Pearson Distinguished Professor at the UNC School of Medicine, where he also leads the Global Women’s Health division. This group of more than 150 clinicians, researchers and public health practitioners are actively addressing global women’s health issues, including birth outcomes, contraception and HIV prevention.
In May, Stringer received the 2025 Oliver Max Gardner Award from the UNC System for his work on maternal healthcare in low-resource settings around the world.
A global health advocate
That work began in 2001, when Stringer and his family moved to Lusaka, Zambia, where he collaborated with the government to implement a pilot project focused on mother-to-child HIV transmission. Eventually, it became the Centre for Infectious Disease Research in Zambia, a nongovernmental health organization focused on improving health care access through research and public health programs.
As CIDRZ expanded, Stringer saw fewer patients and spent more time being the organization’s CEO — managing staff, forming partnerships and writing grants. What was intended to be a one-year research project in Zambia stretched into 11 years for Stringer. By 2012, CIDRZ employed over 700 people and brought in over $30 million per year in funding for research, training and clinical work.
At CIDRZ, Stringer uncovered a major barrier to care for pregnant women: access to ultrasounds. The machines were too expensive, there weren’t enough trained sonographers to do the scans, and there were even fewer radiologists to interpret them.
This stayed with Stringer as he returned to the U.S. in 2012, when UNC-Chapel Hill recruited him and 30 of his team members to create the Global Women’s Health division.
“We came here because of the excellent global health program, school of public health and OB-GYN department,” he shares. “We felt like it would be a place where we could really thrive.”
A tech innovator
Stringer, specifically, is interested in capturing better obstetric ultrasounds. These exams enable health care providers to determine how far along a pregnancy is, assess whether the baby is developing properly and identify any potential risks.
He and his team are developing a portable ultrasound device that plugs into a phone or tablet and uses artificial intelligence to interpret the scans captured. This reduces the need for a large, high-end ultrasound machine, which can cost $40,000, or more and trained sonographers and radiologists. These resources can be hard to come by in many places around the world, including rural parts of the U.S. Nearly 65% of people in North Carolina, for example, live in areas lacking access to primary care physicians, so this technology could make a big difference for small clinics.
In collaboration with the UNC Gillings School of Global Public Health, they are implementing the app in public sector sites in Zambia to see how it works. Stringer hopes to get FDA approval for the device by the end of 2025. While his focus has been on global health settings, he now sees how beneficial it could be across rural regions in the U.S.
“My lifelong goal is to build something that’s going to improve health care for women around the world,” he says. “I think this technology could be transformative.”
New Study: Immune Changes Predict Heart Risks In Cancer Patients

New Study: Immune Changes Predict Heart Risks In Cancer Patients
(News Medical, European Society of Cardiology) — New research has uncovered immune changes in cancer patients that could help identify which patients are most at risk of dangerous heart complications from cancer drugs, known as immune checkpoint inhibitors.
The study was led by Assistant Professor Pilar Martín, Head of the Regulatory Molecules of Inflammation Lab at the Spanish National Center for Cardiovascular Research (CNIC) and group leader at CIBER-CV, she explained, "Immune checkpoint inhibitors have revolutionized cancer treatment, but they can also damage the hearts of some patients. In this study we monitored how levels of immune cells, that are known to be involved in the development of heart diseases, change after treatment.
"We were surprised to see an early and rapid loss of protective immune cells, called regulatory T cells, after cancer patients started treatment. This suggests a window of vulnerability early in treatment." - Assistant Professor Pilar Martín, Head of the Regulatory Molecules of Inflammation Lab, Spanish National Center for Cardiovascular Research
The new research is being presented at European Cardio-Oncology 2025, a scientific congress of the European Society of Cardiology.
Immune checkpoint inhibitors are drugs that work by harnessing the patient's own immune response to attack cancer cells. Unfortunately, they can also have side-effects including causing heart damage, or cardiotoxicity, in some patients. Approximately 1 in 100 patients treated with these drugs develop myocarditis, a life-threatening heart complication.
Researchers found that patients with lower levels of a blood biomarker, called CD69 and found in protective immune cells, experienced a greater decrease in protective immune cells and a resulting increase in destructive pro-inflammatory immune cells. Such a decline in protective immune cells has previously been associated with a greater risk of developing cardiovascular complications such as myocarditis1.
"We put patients into two groups based on their levels of a protective biomarker called CD69, and saw these groups had very different response to the cancer treatments. Those who had lower levels of CD69 before starting treatment had a more negative immune response which puts them at much greater risk of heart damage.
"More work is needed to validate this biomarker and fully understand the immune changes that are taking place, but testing patients for this biomarker with a blood test is relatively cheap and easy and has the potential to help doctors identify which patients are at greatest risk of complications. This could allow doctors to monitor these patients more closely, and in time I hope we can develop new treatments to prevent the immune dysregulation we see in these patients" Professor Martin continued.
Researchers analysed blood samples from 215 cancer patients from the Spanish Immunotherapy Registry of Cardiovascular Toxicity (SIR-CVT)2 before treatment and at 24 weeks, 1012 weeks, 6 months, and 1 year after treatment with immune checkpoint inhibitors. The patients had a range of different cancers, including lung, breast and skin cancer, and were treated with different types of immune check point inhibitor treatments, including anti PD1, PDL1 and CTLA4.
Patients were put into two groups dependent the amount of biomarker for a specific protective T-cell (CD69) in their blood and changes in levels of their immune cell populations were monitored over time.
While both patient groups experienced some decline in levels of a specific type of a protective immune cell (CD69 positive regulatory T cells) in response to treatment, those patients with low starting levels of the protective biomarker had a much larger decrease. These patients also had an increase in immune cells with a role to kill other cells and others that have a role in inflammation.
Regulatory T cells are found in the blood and are important to maintain immune balance and stop the immune system damaging healthy tissues, including the heart and blood vessels. Previous research has shown how the wrong levels of these cells can result in damage to blood vessels and the heart, and this study suggests they could be key in mediating the heart damaging effects of immune checkpoint inhibitor cancer drugs.























 John Meier, IV, MD, MBA
John Meier, IV, MD, MBA